Search for
Filter By
Rating
Price in $
Search for Courses, Exams, Books, TEST BANKS, Assignments, notes...
Showing All 0 results
Sort by
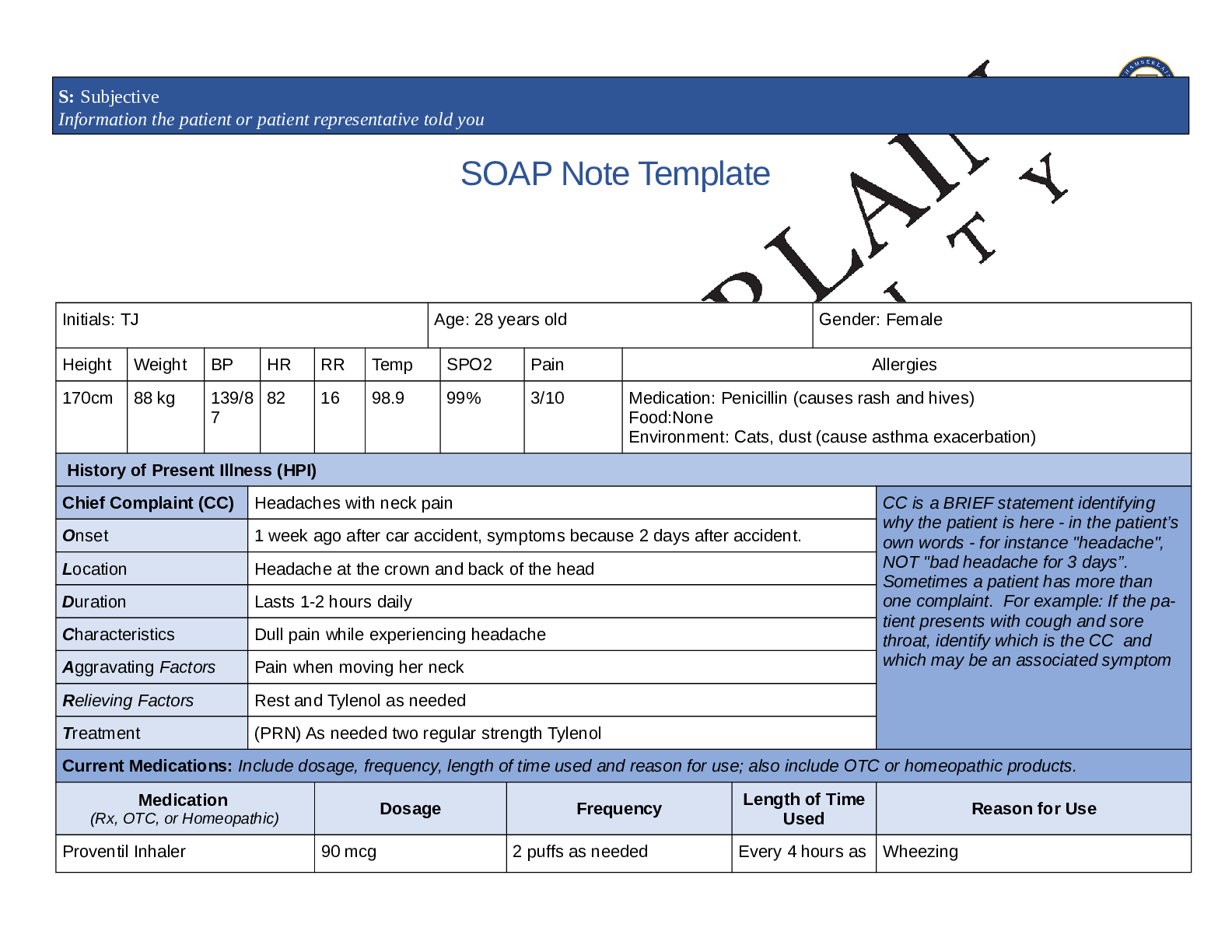
*NURSING > SOAP NOTE > NR509 Week 2 SOAP Note – Chamberlain College of Nursing | NR 509 Week 2 SOAP Note – Grade A (All)
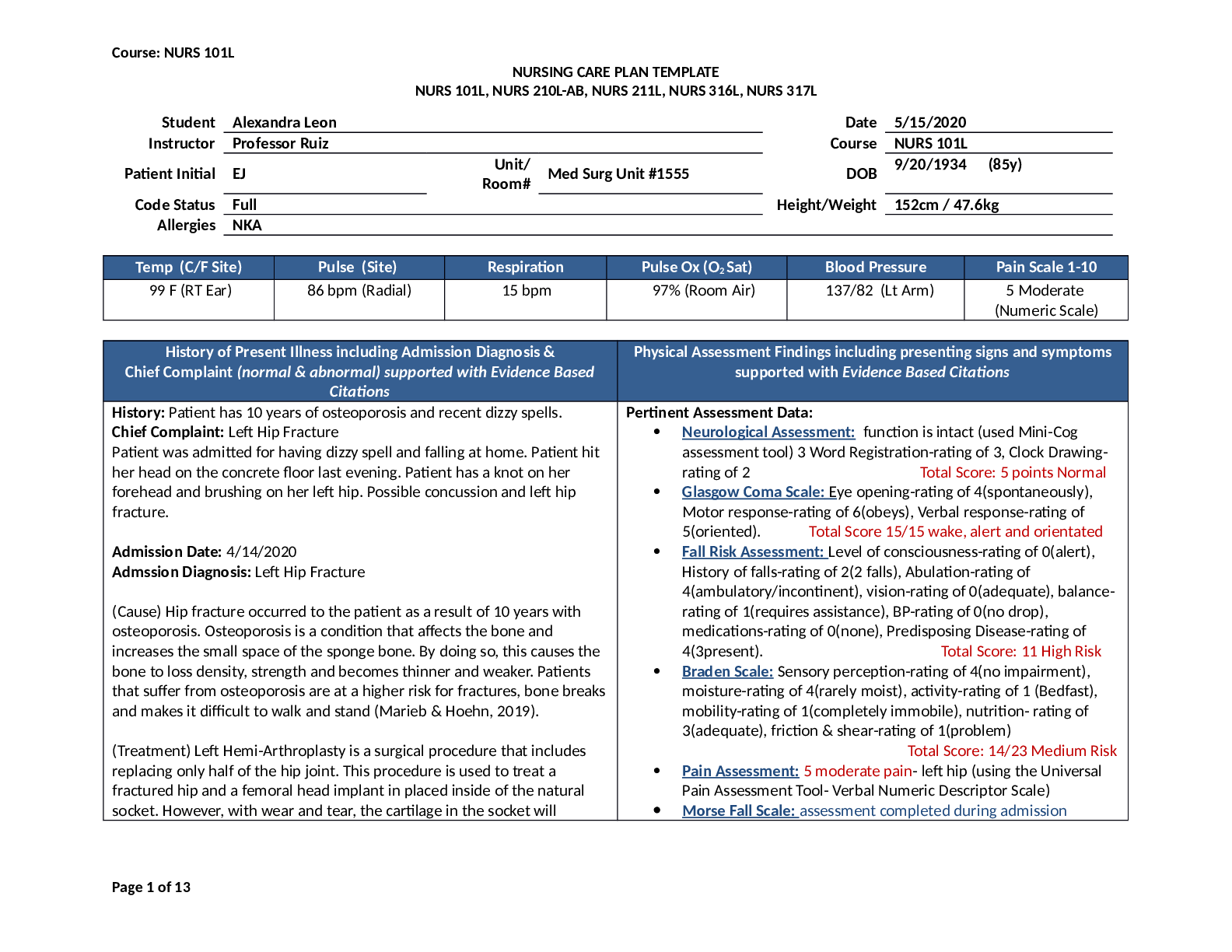
*NURSING > SOAP NOTE > NURS 101L - Nursing Final Care Plan NURSING CARE PLAN TEMPLATE (All)
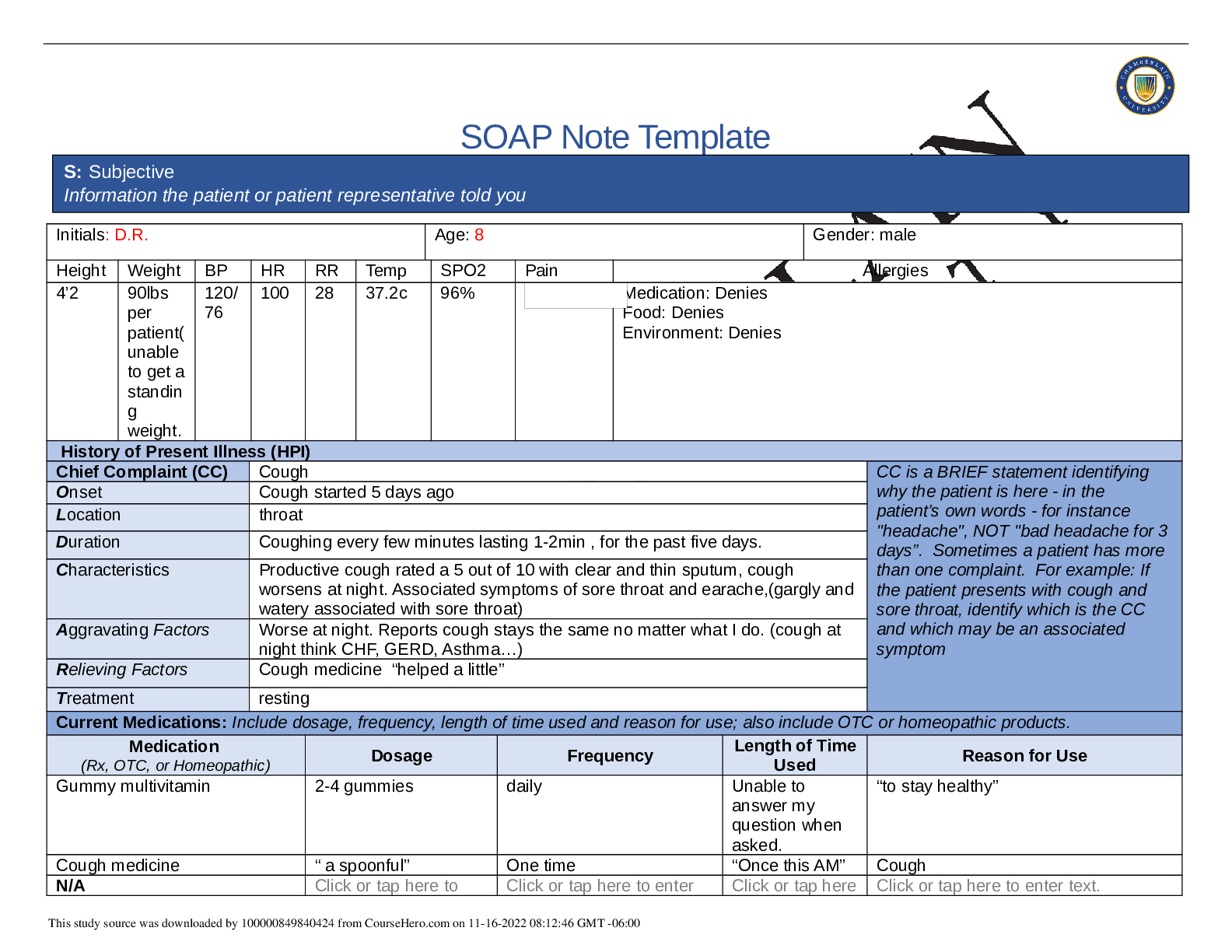
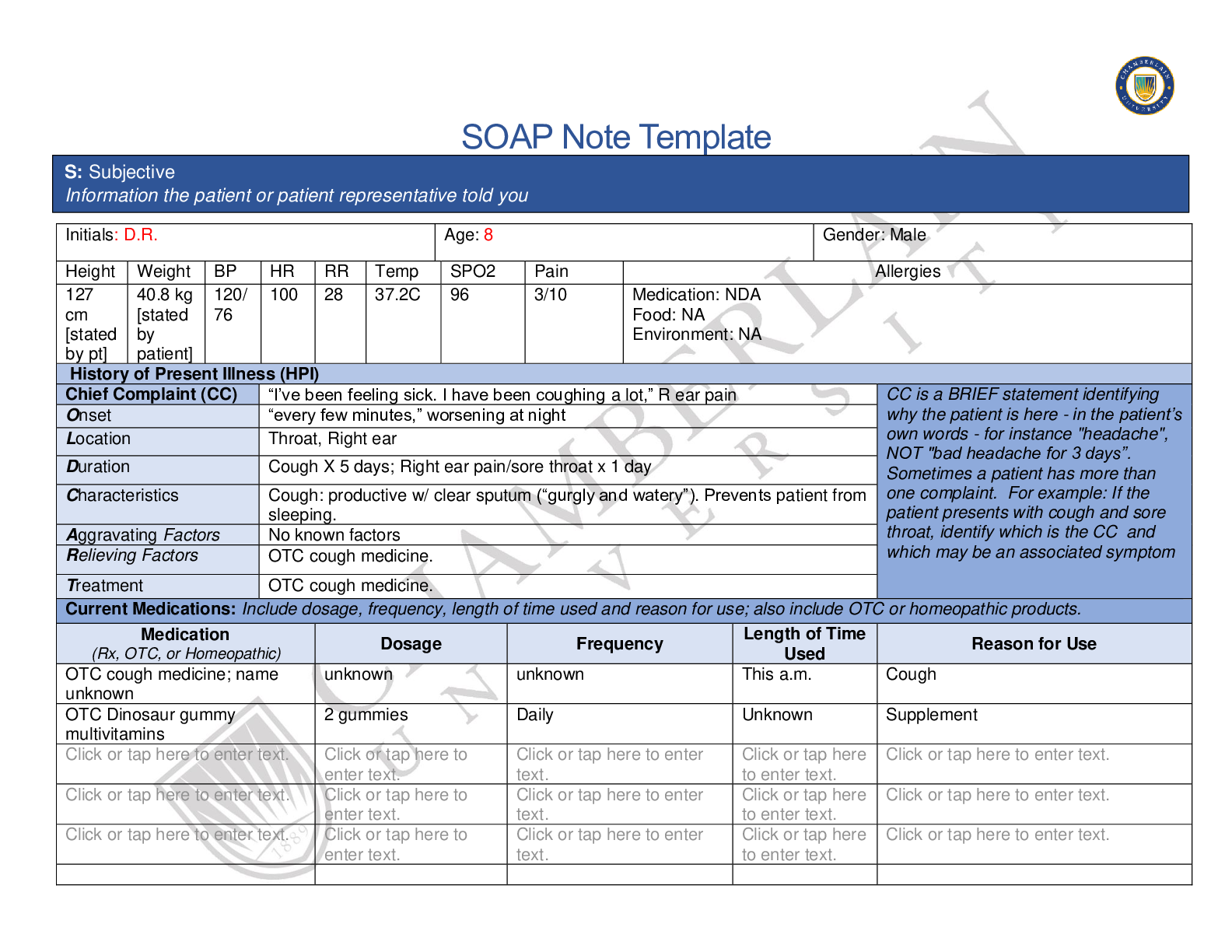
*NURSING > SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution (All)
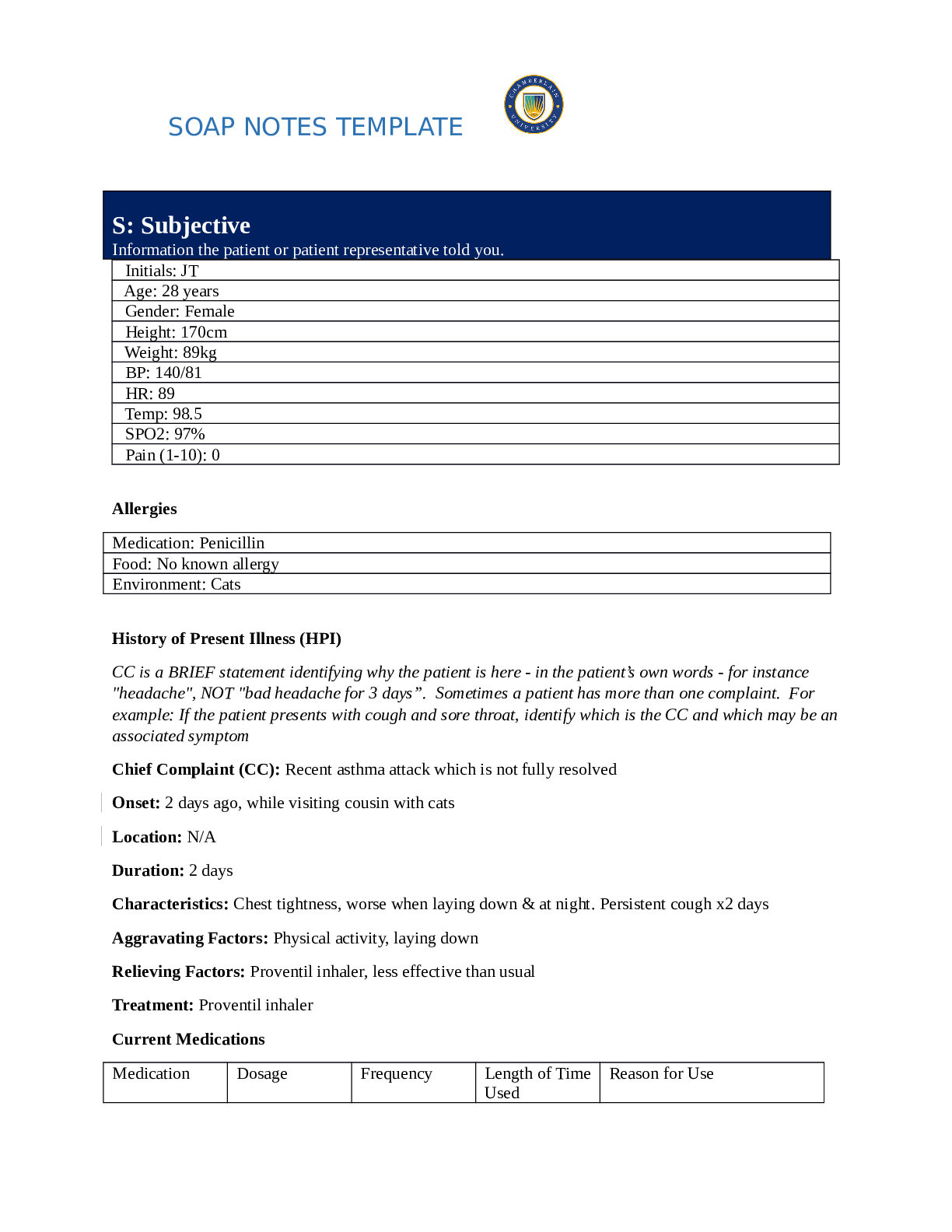
Health Care > SOAP NOTE > soap notes template latest solution 2020 (All)
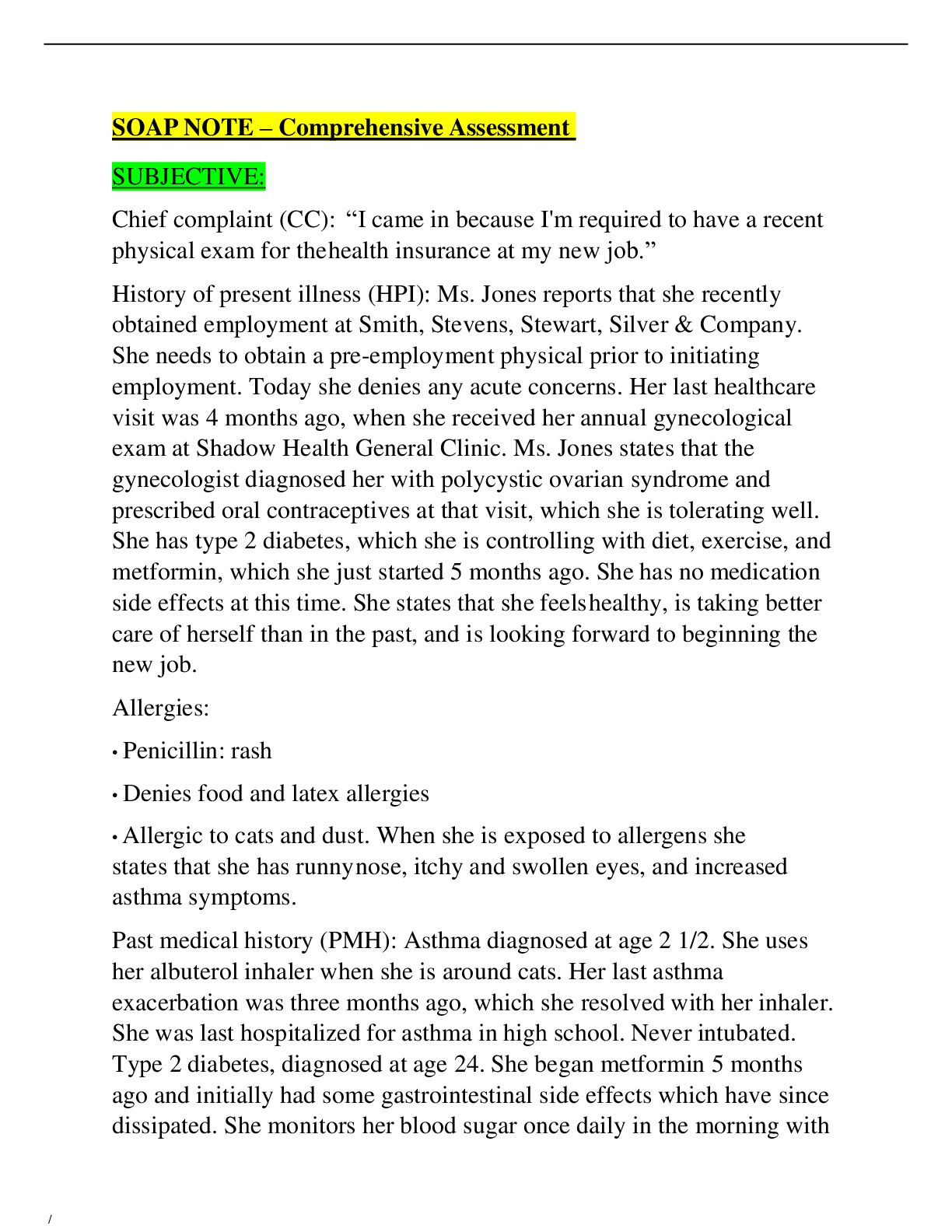
*NURSING > SOAP NOTE > SOAP NOTE – Comprehensive Assessment – Tina Jones – Shadow Health Clinic – Ryan Kent (All)
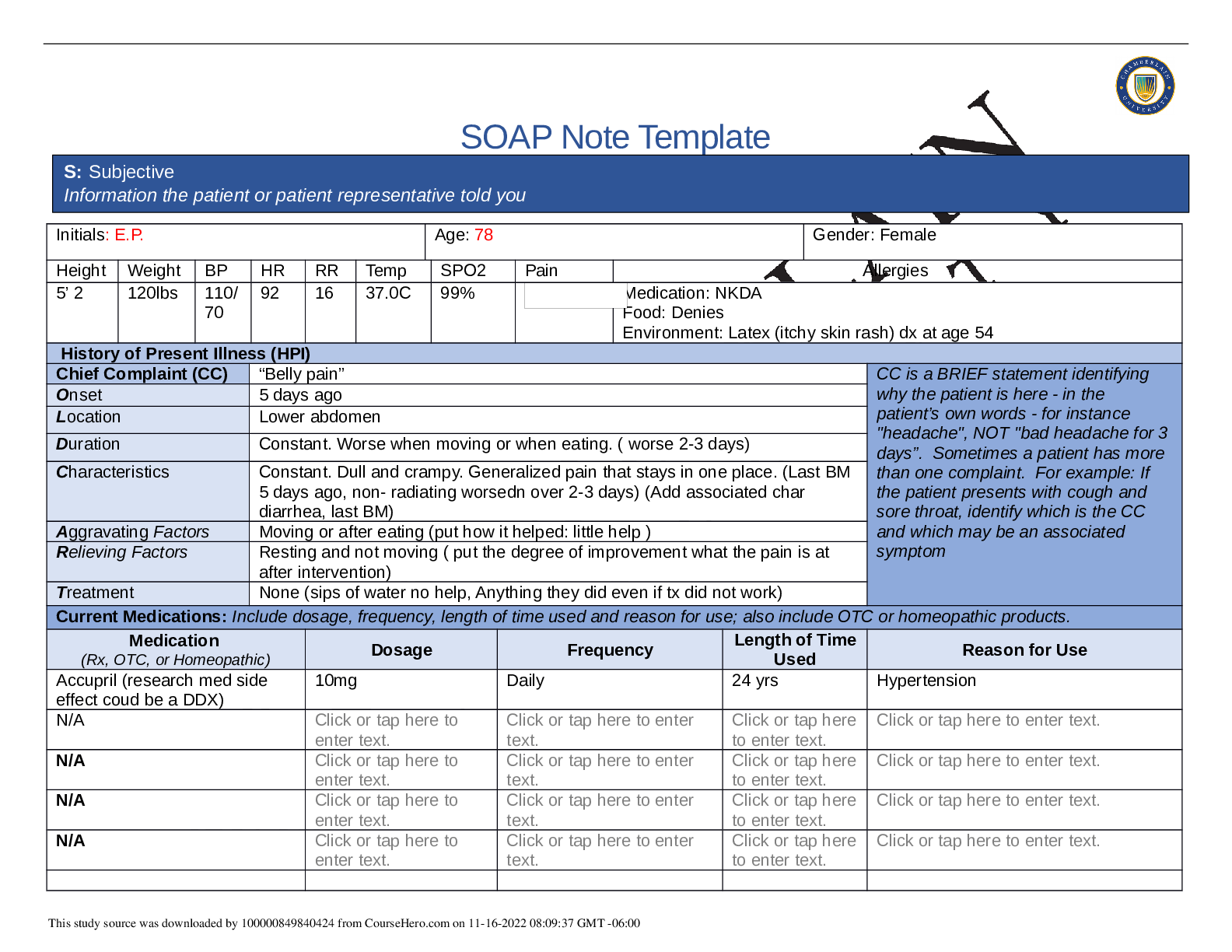
*NURSING > SOAP NOTE > NR509 Week_5_SOAP_Note - Chamberlain College of Nursing | NR 509 Week_5_SOAP_Note - BELLY PAIN (All)
*NURSING > SOAP NOTE > Chamberlain College of Nursing FNP NR511Nwilliams_SOAP_Wk6 2021 (All)
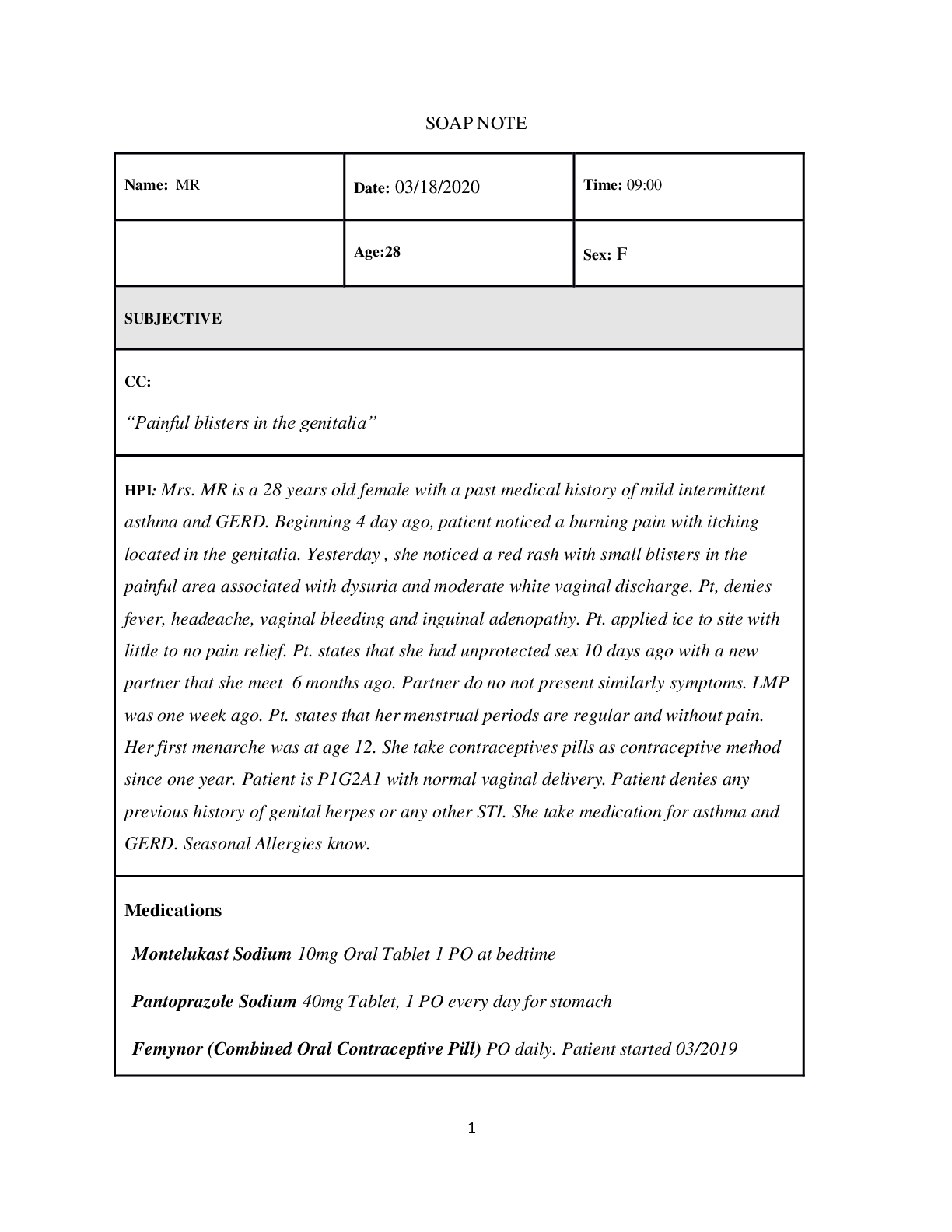
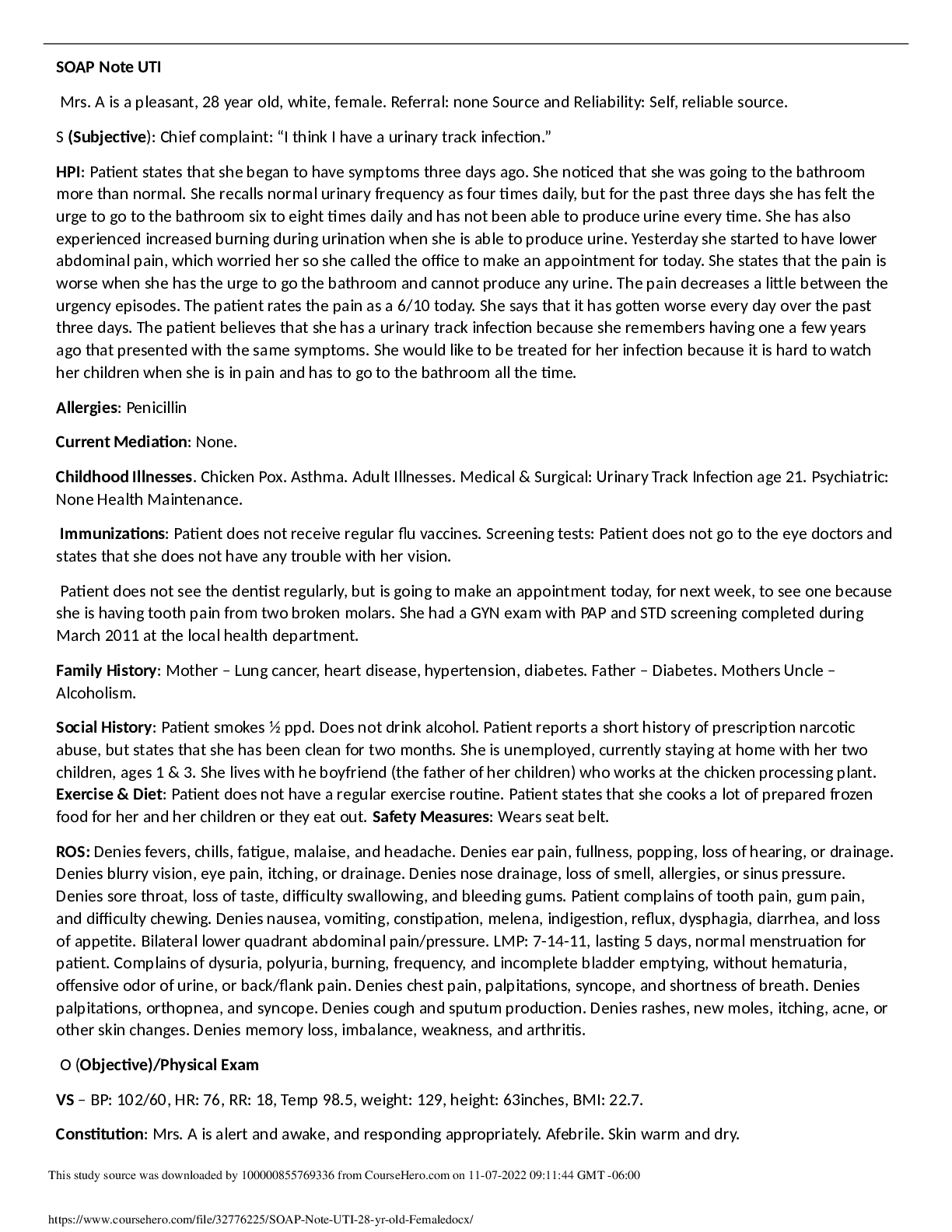
*NURSING > SOAP NOTE > Monroe College NURSING 812 SOAP Note UTI (28 yr old Female) (All)
*NURSING > SOAP NOTE > Chamberlain College of Nursing - NR 509 Soap.Note.Respiratory.TinaJones. (complete updated 2021) (All)