*NURSING > NCLEX-PN > Paediatrics Michael Grant: Notes based on QUB online Med Portal lectures, QUB student manual, NICE G (All)
Paediatrics Michael Grant: Notes based on QUB online Med Portal lectures, QUB student manual, NICE Guidelines, Oxford Clinical handbook and various external online resources
Document Content and Description Below
Paediatrics Michael Grant Notes based on QUB online Med Portal lectures, QUB student manual, NICE Guidelines, Oxford Clinical handbook and various external online resources A) Four Basic Paed... iatric Skills: • How to pick up and hold a baby • Taking a paediatric history (different emphasis to adults) Introduce yourself – name / role Confirm patient details – name / DOB Explain the need to take a history Gain consent to take a history Ensure the patient is comfortable Presenting complaint Give the patient time to explain the problem/symptoms they’ve been experiencing. In a paediatric history this may well be a collateral history from a parent. It’s important to use open questioning to elicit the patient’s or parent’s presenting complaint. “So what’s brought your child in today?” or “What’s brought you in today?” This can sometimes be difficult when talking to children and you may need to adopt an approach involving more direct questioning. So instead of saying “Tell me about the pain” you may need to ask a series of questions requiring only yes or no answers. “Is the pain in your tummy?” “Is the pain in your back?” Allow the patient time to answer and do not interrupt. History of presenting complaint Onset – when did the symptom start? / was the onset acute or gradual? Duration – minutes / hours / days / weeks / months / years Severity – e.g. if symptom is shortness of breath – are they able to talk in full sentences? Course – is the symptom worsening, improving, or continuing to fluctuate? Intermittent or continuous? – is the symptom always present or does it come and go? Precipitating factors – are there any obvious triggers for the symptom? Relieving factors – does anything appear to improve the symptoms e.g. an inhaler Associated features – are there other symptoms that appear associated e.g. fever / malaise Previous episodes – has the patient experienced this symptoms previously? Key paediatric questions Feeding – volume of intake / frequency of feeding Vomiting – frequency / volume / timing – projectile? / bilious? / blood? Fever – confirmed using thermometer vs subjectively feeling hot? Wet nappies / urine output – number of wet nappies a day – ↓ in dehydration Stools – consistency / steatorrhoea? (biliary obstruction) / red currant jelly (intussusception) Rash – any obvious trigger? / distribution? / blanching? Behaviour – irritability / less responsive Cough – productive? / associated increased work of breathing? Rhinorrhoea – often associated with viral upper respiratory disease Weight gain or loss – check baby book if the parent has it with them Sleeping pattern – more sleepy than usual? Unwell contacts – often children become infected from unwell siblings Localising symptoms – tugging at an ear/ holding tummy Pain – if pain is a symptom, clarify the details of the pain using SOCRATES ◦ Site – where exactly is the pain / where is the pain worst ◦ Onset – when did it start? / did it come on suddenly or gradually? ◦ Character – what does it feel like? (sharp stabbing / dull ache / burning?) ◦ Radiation – does the pain move anywhere else? (e.g. chest pain with left arm radiation) ◦ Associations – any other symptoms associated with the pain (e.g. chest pain with SOB) ◦ Time course – does the pain have a pattern (e.g. worse in the mornings) ◦ Exacerbating / relieving factors – anything make it particularly worse or better? ◦ Severity – on a scale of 0-10, with 0 being no pain & 10 being the worst pain you’ve ever felt Ideas, Concerns & Expectations – often addressed to parents Ideas – what are the patient’s / parent’s thoughts regarding their symptoms? Concerns – explore any worries the patient / parent may have regarding the symptoms Expectations – gain an understanding of what the patient / parent is hoping to achieve from the consultation Summarising Summarise what the patient / parent has told you about the presenting complaint. This allows you to check your understanding regarding everything the patient/parent has told you. It also allows the patient/parent to correct any inaccurate information & expand further on certain aspects. Once you have summarised, ask the patient/parent if there’s anything else that you’ve overlooked. Continue to periodically summarise as you move through the rest of the history. Paediatrics: Page 3 of 78 Signposting Signposting involves explaining to the patient/parent: ◦ What you have covered – “Ok, so we’ve talked about the symptoms”” ◦ What you plan to cover next – “Now I’d like to discuss any previous medical history” Past medical history Antenatal period – illnesses or complications during gestation – e.g. rubella Birth – delivery complications / prematurity / birth weight Neonatal period – illness /admission to special care baby unit (SCBU)? Medical conditions Previous hospitalisation – when and why? Previous surgery Accidents & injuries – remain vigilant for signs of non accidental injury Developmental history Current weight and height – weight is required to calculate drug doses Developmental milestones (are they on track for their given age?): ◦ e.g. sitting up, crawling, walking, talking, toilet training, reading Family history Family history of disease – e.g. coeliac / T1DM Genetic conditions – e.g. cystic fibrosis Family tree – useful to draw out if considering genetic disease Drug history Regular medication – e.g. inhalers for asthma Over the counter medication ALLERGIES Immunisations - Is the child up to date with their immunisations? Social history Living situation + Social services – accommodation / main carer / who lives with child? Second hand smoke exposure – risk factor for otitis media / asthma / SIDS Dietary history • Type of food? – formula / breast milk / solids • Intake – e.g. how many ounces of milk? • Frequency of feeding – reduced or increased? • Special dietary requirements? – cow’s milk intolerance / coeliac disease Parents occupation Pets – important when considering allergies / asthma triggers Schooling – stage of learning / any issues? Foreign travel – may be important when considering certain diagnoses e.g. TB Top to bottom: CNS – Vision / Headache / Motor or sensory disturbance/ Loss of consciousness / Confusion GI – Appetite / Nausea / Vomiting / Indigestion / Dysphagia / Weight loss / Abdominal pain / Bowel habit Cardiovascular – Chest pain / Palpitations / Dyspnoea / Syncope / Orthopnoea / Peripheral oedema Respiratory – Dyspnoea / Cough / Sputum / Wheeze / Haemoptysis / Chest pain Urinary – Volume of urine passed / Frequency / Dysuria / Urgency / Incontinence Musculoskeletal – Bone and joint pain / Muscular pain Dermatology – Rashes / Skin breaks / Ulcers • Clinical examination - gaining maximum information with minimum upset (including normal neonate, infant, dysmorphic child, developmental assessment, ENT, eyes for squint). How to modify systematic examination of CVS, RS, GIT, CNS, PNS in light of child’s age, ability to understand and co-operate, and the relevance of signs at different ages. • Learn to: o Understand the anxieties and worries parents have about their ill children. o develop the ability to show parents that you understand and grasp what they perceive to be the problem. o develop communication skills that will allay fears or convey information in a way that is understood by parents and by children. Child Abuse and Neglect Physical abuse: Physical abuse may involve hitting, shaking, throwing, poisoning, burning or scalding, drowning, suffocating, or otherwise causing physical harm to a child. Factors to consider in the presentation of a physical injury are: • The history given by the child (if they can communicate) • The child’s age and stage of development • The plausibility and/or reasonableness of the explanation for the injury • Any background, e.g. previous child protection concerns, multiple attendances to A&E or general practitioner • Delay in reporting the injury • Inconsistent histories or reactions from caregiver (e.g. vague, evasive, aggression) Investigations: • X-rays o If under 30 months, full radiographic skeletal survey with oblique views – esp. posterior ribs o Repeat x-ray at 1-2 weeks later • Bruising: o Rule out coagulation disorders o Be aware of Mongolian blue spots on back or thighs o The age of a bruise cannot be accurately estimated o Can be hard to detect on dark skinned children • Fractures: o Exclude osteogenesis imperfecta – type 1 causes #, autosomal dominant, blue sclerae, wormian bones in skull sutures • Scalds and cigarette burns o Exclude bullous impretigo (Staph aureus scalded skin syndrome) • Head and neck trauma: o Extra dural (direct trauma) Subdural (shearing, shaking trauma +/- retinal haemorrage) or subarachnoid (retinal bleeds, aneurysm) bleeds o Retinal haemorrhages or injury to the eye in a child if there is no major confirmed accidental trauma • RECORDING: o Make sure to clearly document any injuries, the histories and – if consenting – photographic evidence o Discuss with senior paediatrician Sexual abuse: Involves forcing or enticing a child or young person to take part in sexual activities, including prostitution, whether or not the child is aware of what is happening. The activities may involve physical contact, or noncontact activities, such as involving children in looking at or producing pornographic material. • Recognition can occur when: child informs someone, becomes pregnant (automatically sexual absuse if girl >13 years), STI with no clear reason (although they can be contracted from mother during birth) • Physical symptoms: vaginal/rectal bleeding • Behaviour symptoms: soiling, secondary enuresis, self harm, sexualised behaviours, poor school performance • Signs: o Can be difficult to find as gential area heals very quickly in young children o STI screening o Forensic swabs of body, clothing, bedding for semen Emotional abuse: Is the persistent emotional maltreatment of a child resulting in severe and persistent adverse effects on the child’s emotional development. It may involve conveying to children that they are worthless or unloved, inadequate, or valued only insofar as they meet the needs of another person. This may arise form the fact the child is seen as the “wrong” gender, born at a time of parental separation or violence, r is seen as unduly difficult. • Clues come from child’s behaviour: o Babies: Apathetic, delayed development, nondemanding Neglect: Described by the mother as ‘spoiled, attention seeking, in control, not loving her’. o Toddlers and preschool children: Violent, apathetic, fearful. o School children: Wetting, soiling, relationship dif culties, nonattendance, antisocial behaviour. o Adolescents: Selfharm, depression, oppositional, aggressive and delinquent behaviour Paediatrics: Page 5 of 78 Is the persistent failure to meet a child’s basic physical and/or psychological needs; i.e. food, clothing, shelter, supervision Consider the possibility of neglect when the child: • Consistently misses important medical appointments • Lacks needed medical or dental care, immunisations or glasses • Seems ravenously hungry • Is dirty • Is wearing inadequate clothing for weather Or if parent: • Appears to be indifferent to the child • Seems apathetic or depressed • Behaves irrationally or in a bizarre manner • Is abusing alcohol or other drugs. Fabricated or induced illness: Refers to parents (or carers), but usually the mother (>80%), which cause harm to children. It fulfils the parents (or carers) own needs. Organic illness may coexist clouding the picture but clues include frequent unexplained illnesses and multiple hospital admissions with symptoms that only occur in the carer’s presence and are not substantiated by clinical findings. It may consist of; • Verbal fabrication – parents fabricate (i.e. invent) symptoms and signs in the child, telling a false story to healthcare professionals • Induction of illness may involve: suffocation, poisoning (drugs, ordinary substances e.g. salt) Management: • Any injuries or medical findings should be carefully noted, measured, recorded and drawn on a body map and photographed • If abuse is suspected or confirmed, a decision needs to be made as to whether the child needs immediate protection from further harm – this can be achieved by hospital admission – occasionally this will require legal enforcement • If treatment is not necessary but felt to be unsafe for the child to return home, a placement may be found in a foster home • The safety of any other siblings or children at home must be considered Cardiology Important Presenting Symptoms and Signs in Cardiology You should be able to list the 3-4 commonest causes of these symptoms/signs at various ages and be able to differentiate these (by features and investigations): Tachycardia Murmurs Cyanosis Heart failure The Spectrum of Clinical Conditions in Cardiology You should be able to describe - aetiology, presentation, natural history, signs, diagnosis and basic management of an infant/toddler/older child with: ◦ Congenital heart disease - describe anatomical and physiological basis for pathology and physical signs ◦ Heart failure ◦ Innocent versus pathological asymptomatic murmurs ◦ SBE ◦ Rheumatic fever ◦ Kawasaki syndrome ◦ Cardiomyopathy Practical skills You should be able to list the 3-4 commonest causes of these symptoms/signs at various ages and be able to differentiate these (by features and investigations): ◦ Cardiovascular examination ◦ Blood pressure measurement ◦ Recognise heart sounds/murmurs ◦ Recognise signs of heart failure Paediatrics: Page 6 of 78 Genetic conditions affecting the heart: • Trisomies: o 21 – Down’s sundrome – 40% with cardiac abnormalities Atrioventricular septal defect, VSD o 13 (Patau’s), 18 (Edward’s) - >50% with cardiac abnormalities • Turner’s syndrome (Monosomy 45 – XO) – left heart problems; bicuspid aortic valve and coarctation of the Aorta • 22q11 deletion (DiGeorge syndrome) – dominant inheritance o Cardiac abnormality (commonly interrupted aortic arch, truncus arteriosus [embryological structure known as the truncus arteriosus fails to properly divide into the pulmonary trunk and aorta] and tetralogy of Fallot [Pulmonary Infundibular Stenosis, overriding aorta, VSD, right ventricular hypertropy) o Abnormal facies o Thymic aplasia o Cleft palate o Hypocalcemia/Hypoparathyroidism • Noonan’s syndrome is one of the most common causes of cardiac defects o Autosomal dominant congenital disorder o The principal features include congenital heart defect (typically pulmonary valve stenosis; also atrial septal defect and hypertrophic cardiomyopathy), short stature, learning problems, pectus excavatum, impaired blood clotting, and a characteristic configuration of facial features including a webbed neck and a flat nose bridge Fetal circulation: • Oxygenated blood form the placenta enters umbilical vein and mostly bypasses the liver using the ductus venosus • From here it enters the vena cava and travels into the heart where it mostly bypasses the pulmonary circulation via the foramen ovale – into the left atrium • Blood that does enter the pulmonary artery from the right ventricle also passess though the ductus arteriosus to reenter systemic circulation • Deoxygenated blood returns to the placenta via the umbilical arteries that branch off from the internal iliac Paediatrics: Page 7 of 78 Transitional from fetal to baby circulation: • Pulmonary vascular resistance decreases (first few breaths x6 blood flow) while systemic vascular resistance increases - Causes closure of: o Ductus arteriosus, to ligamentum arteriosum o Ductus venosus to ligamentum to venosum o Foramen ovale closes as left atrial pressure increases, becoming the fossa ovalis Cardiac malformations: These can be abnormal connections, holes or obstructions that are described as either cyanotic or acyanotic: Cyanotic (right to left) conditions produce blue babies that can be remembered by the 5 T’s: • Transposition of the great arteries (TGA) o Due to ventriculo‐atrial discordance, with the aorta arising from the right ventricle and the pulmonary trunk arising from the left ventricle. The pulmonary and systemic circulations are thereby completely separate and without some form of septal defect to allow mixing of oxygenated and deoxygenated blood, the condition is rapidly fatal o Maintaining the patency of the ductus arteriosus with a prostaglandin infusion (PGE2, 5-20 ng/kg per min) is mandatory o Correct acidosis o If the infant does not have an ASD, VSD, PFO or PDA, the cardiologists will perform an emergency balloon atrial septostomy to create a large ASD and allow the blood to mix. o Definitive anatomical correction is the surgery of choice (arterial switch operation) o Egg on a string appearance on x-ray • Tetralogy of fallot o Characterised by a VSD, aortic overriding of the septal defect, right ventricular outflow tract obstruction (which may be sub, supra or valvular) and consequent right ventricular hypertrophy Extreme form know as pulmonary atresia, pulmonary valve is not open or does not form At birth, some infants do not show signs of cyanosis, but they may later develop episodes of bluish pale skin during crying or feeding (ie, "Tet" spells) – they may squat to compensate (increases PVR and thus reduces right to left shunting) Cyanosis of the lips and nail bed is usually pronounced at birth; after age 3-6 months, the fingers and toes show clubbing CXR shows a boot shaped heart (severe RVH) with apex lifted off diaphragm with dark lung fields from reduced pulmonary blood flow Maintaining the patency of the ductus arteriosus with a prostaglandin infusion (PGE2, 5-20 ng/kg per min) is mandatory Correct acidosis If the infant does not have an ASD, VSD, PFO or PDA, the cardiologists will perform an emergency balloon atrial septostomy to create a large ASD and allow the blood to mix. • Total anomalous pulmonary venous drainage (TAPVD) o A form of congenital cyanotic heart disease, whereby the pulmonary veins drain into venous structures other than the left atrium o Location of anomalous drainage can be supracardiac, intracardiac or infracardiac o Oxygenatied blood drains into right side of heart • Trunus arteriosus o Failure of separation between pulmonary artery and aorta, resulting in a common truck o Typically overlies a ventricular septal defect causing mixing of blood • Tricuspid atresia o Tricuspid valve doesn’t form meaning that blue blood from the right side must cross atrial septum into left atrium o Only the left ventricle is effective, the right being small and nonfunctional. o A Blalock–Taussig shunt insertion (between the subclavian and pulmonary artery) in children who are severely cyanosed, acts as artificial ductus artriosus o Pulmonary artery banding operation to reduce pulmonary blood flow if breathless. Acyanotic (Left to right) produce breathless babies: • VSD/ASD o Secundum atrial septal defect: Paediatrics: Page 8 of 78 Very well tolerated and often not detected until late in life • PDA • PS Arises from an enlarged foramen ovale, inadequate growth of the septum secundum, or excessive absorption of the septum primum Left to right flow from atria causes gradual enlargement of right atrium, ventricle and pulmonary artery Heard as slight ESM and pronounced AP split due to increased length of time for drainage of right side (that doesn’t not vary with respiration) o Ventricular septal defect (up to 5% of new borns) Typically cause increase flow from left ventricle into pulmonary artery, thus increase pulmonary venous return that can lead to left side hypertrophy Large VSD cause cardiac decompensation or heart failure – not due to pump failure – but due to high output state that circulates significant amount of blood right back into left side Pansystolic murmur as both in systole and diastole there is a gradient in pressure between the ventricles (25/5 in RV, 120/80 in Aorta, 120/5 in LV) o Treatment: Diuretic (e.g. furosemide/spironolactone combo to spare potassium) Vasodilators (e.g. captopril) Additional calorific support Early surgery (at 3-6 months to prevent prolonged pulmonary hypertension from damaging capillary bed, increasing resistance and leading to Eisenmenger syndrome - hunt reverses and the teenager becomes blue, leading to progressive right heart failure and death in 4th/5th decade) • Inhaled nitric oxide, intravenous magnesium sulphate and oral phosphodiesterase inhibitors (e.g. sildenafil a.k.a. Viagra) will help to reduce pulmonary hypertension while waiting for transplant o Ductus arteriosus between pulmonary artery and aorta has failed to close by 1 month after the expected date of delivery due to a defect in the constrictor mechanism of the duct o Creates a continuous murmur due to constant gradient in pressures between aorta and pulmonary arties during both systole and diastole o Closure is with a coil or occlusion device introduced via a cardiac catheter at about 1 year of age • Duct dependant left heart obstruction o AS o Coarctation o Hypoplastic left heart syndrome o Treatment: Prostaglandin E2 infusion (5-20ng/kg/min) Palliation balloon septostomy Consider inotrope (e.g. dobutamine – B1 agonist) In HLHS, maintain mild respiratory acidosis Common mixing defects produce breathless and blue babies: • Complete atrio-ventricular septal defect o Common in Down’s syndrome – most common setting to see this defect o Centre of heart is open (lower atrial septum, upper ventricular septum) creating left to right flow o Management is to treat heart failure medically (as for large VSD) and surgical repair at 3–6 months of age. Signs of “heart failure” in infants and small children: • Tachypnoea (can be greater than 60/min) • Tachycardia • Hepatic enlargement • Peripheral oedema tends to be a very late sign • JVP not reliable in <6 y.o. The features of an innocent murmur can be remembered as the four S’s: • Soft (grade 3 or less, with no clicks) Paediatrics: Page 9 of 78 • Systolic (athough venous hum heard at the base of the neck and resolves upon child rotating head is also innocent) • aSymptomatic (may be pyrexial but will have normal ECG and CXR) • left Sternal edge Rheumatic fever • In susceptible individuals, there is an abnormal immune response to a preceding infection with group A βhaemolytic streptococcus esp. strept pyogenes. • After a latent interval of 2–6 weeks following a pharyngeal infection, polyarthritis, mild fever and malaise develop • Chronic rheumatic heart disease: The most common form of longterm damage from scarring and fibrosis of the valve tissue of the heart is mitral stenosis most frequently affected; however aortic, tricuspid and, rarely, pulmonary valve disease may occur. • Management: The acute episode is usually treated with bed rest and antiinflammatory agents o Aspirin high dose with drug level monitoring o Monthly injections of benzathine penicillin is the most effective prophylaxis until 18-21 y.o. Infective endocarditis All children of any age with congenital heart disease (except secundum ASD), including neonates, are at risk of infective endocarditis • Highest when there is a turbulent jet of blood, as with a VSD, coarctation of the aorta and persistent ductus arteriosus or if prosthetic material has been inserted Should be suspected in any child or adult with a sustained fever, malaise, raised ESR, unexplained anaemia or haematuria (microscopic) • Clinical signs o Fever o Anaemia and pallor o Splinter haemorrhages in nail bed o Clubbing (late) o Necrotic skin lesions • Diagnosis o Multiple blood cultures o Echocardiography may confirm presence of vegetations (fibrin and platelets and contain infecting organisms) • Most common causative organism is αhaemolytic streptococcus (Streptococcus viridans) • Highdose penicillin in combination with an aminoglycoside, giving 6 weeks of intravenous therapy • Prophylaxis good dental hygiene Cardiomyopathy • Dilated cardiomyopathy (a large, poorly contracting heart) may be inherited, secondary to metabolic disease or may result from a direct viral infection • The diagnosis is readily made on echocardiography • Treatment is symptomatic with diuretics and ACE inhibitors and carvedilol (βadrenoceptor blocking agent) Kawasaki disease (KD) is a systemic vasculitis and important diagnosis to make because aneurysms of the coronary arteries are a potentially devastating complication. Subsequent narrowing of the vessels from scar formation can result in myocardial ischaemia and sudden death • Exact cause is unknown but result of immune hyperreactivity to a variety of triggers • Aetiology: o Affects children of 6 months to 4 years old, younger get worse disease o More common in Japanese and afro-carribean o Linked to mutations of ITPKC gene (down regulates T-cell activation) • Clinical features o Kawasaki is a type of motorcycle: o CRASH and BURN o Conjuctivitis, rash (esp. hands and feet), adenitis, strawberry tounge, hands (desquatmation) o Prolonged fever >5 days and four other features of: Paediatrics: Page 10 of 78 Nonpurulent conjunctivitis, red mucous membranes (+/- strawberry tongue), cervical lymphadenopathy, rash, red and oedematous palms and soles or peeling of fingers and toes o Inflammation of their BCG vaccination site • Investigations: o High inflammatory markers (Creactive protein, ESR, white cell count) o Echocardiogram (look at coronary arteries and repeat at 6 weeks) • Treatment: o Intravenous immunoglobulin (IVIG) given within the first 10 days o Aspirin is used to reduce the risk of thrombosis at a high antiinflammatory dose until the fever subsides o Large coronary artery aneurysms may require long-term warfarin o Persistent inflammation and fever may require treatment with infliximab Dermatology You should be able to confidently describe a rash. Note its location, distribution, size, shape, colour and appearance. Revision of dermatological terms: Macule: <1cm circumcised flat area of discoloration Patch: Larger flat area of discoloration Papule: Raised palpable area (small <1cm) Plaque: Large raised disc lesion Nodule: Palpable lesion >1cm diameter Vesicle: Small blister <0.5cm Bulla: Blister >0.5cm Pustule: Blister with visable pus Purpura: Red/ purple non blanching discoloration secondary to extravasation of red cells Petechia: Purpuric area <2mm Telangiectasia: Dilated, visible small blood vessels Wheal: Itchy papule You will remember the ABCDE description of a Pigmented Lesion from your 3rd year Dermatology Teaching and you should practice using this model again during your Paediatrics module. ◦ Asymmetry ◦ Irregular Border ◦ Two or more Colours within the lesion ◦ Diameter > 6mm ◦ Evolution of the lesion (history of change) The Spectrum of Clinical Conditions in Dermatology You should be able to describe - aetiology, presentation, natural history, signs, diagnosis and basic management of common skin problems in Paediatrics: ◦ Napkin rash ◦ Seborrhoea ◦ Atopic eczema ◦ Thrush ◦ Scabies ◦ Herpes simplex ◦ Impetigo Practical Skills Examine and describe a rash or lesion Neonatal urticaria (erythema toxicum) – a common rash appearing at 2–3 days of age, consisting of white pinpoint papules at the centre of an erythematous base. • The fluid contains eosinophils. • The lesions are concentrated on the trunk; they come and go at different sites • Typically resolves by 10 days Milia – white pimples on the nose and cheeks, from retention of keratin and sebaceous material in the pilaceous follicles. • 1-2mm cysts that typically occur on nose, cheeks and nose • Spontaneously exfoliate in first weeks Neonatal acne considers of papules that develop into pustules and are distributed on the face, neck and chest • Caused by trans-placental transfer of androgens • Onset in neonatal period but my last several months • Usually resolves spontaneously but may require topical anti-fungals Birthmarks: • Vascular: o Tumours: e.g. Infantile haemangioma Benign vascular tumours that affect up to 5% that appear in first few weeks as macule and quickly grow Downloaded by browsegrades.com browsegrades.com ([email protected]) If superficial: bright red plaque with telangiectasia If deep: blue/purple swelling that is poorly defined Typically resolves spontaneously over the years but treatment is required in 2% when issues arise like: • Ulceration and bleeding • Functional abnormality – e.g. blockage at eye or nose • Disfigurement may occur at nasal tip, ears and lips • Can be associated with internal structural abnormalities (esp. if multiple or linear distribution) • If large, can cause high output heart failure Rx: Oral propranolol o Vascular malformations; caused by dilated small vessels (superficial for salmon, deeper for port wine) Port wine stains commonly involve a trigeminal nerve distribution; those following V1 can have an ipsilateral leptomeningeal angioma as well (as the possibility of glaucoma or choroidal lesions, Calcification of the gyri used to show characteristic ‘rail-road track’ cal- cification) known as Sturge-Weber syndrome Severe lesions on the limbs with bone hypertrophy (Klippel– Trenaunay syndrome) Rx: Laser • Pigmented birthmarks: o Congenital melanocytic naevi (1% of population) Present at birth Pale to dark macules that become darker and elevated in adolescence Typically have hair Most are benign and asymptomatic and grow with child Large >20cm have 5% risk of melanoma and need follow-up o Café au lait macules are well circumscribed, uniform, light brown patches If multiple, may indicate underlying genetic condition such as neurofibromatosis type 1 • 17 letter = Chromosome 17 • Seen with macrocephaly and lisch nodules (in the eyes) • Autosomal dominant o Mongolian spot or congenital dermal melanocytosis Abnormal collection of melanocytes Common in Asian, black and Hispanic Paediatrics: Page 11 of 78 Salmon patch • Epidermal: Poorly a solitary, well circumscribed, large, dark macular areas in the lumbo-sacral region Usually fade by 10 y.o. and do not require Rx o Epidermal naevus is pigmented but is not melanocyte Overgrowth of the epidermis, making it appear dark Circumscribed, brown, velvet-like plaque Becomes wart-like with age Eczema/Dermatitis Atopic eczema • Affects about 20% of children in the UK, starting in first year of life, and is due to genetic deficiency of skin barrier function • Usually family history of atopic disorders: eczema, asthma, allergic rhinitis (hay fever) and around one-third of children with atopic eczema will develop asthma. • Troublesome in the first year of life but resolves in 50% by 12 years of age, and in 75% by 16 years. • Distribution changes from infant to toddler stage (see right) • Diagnosis made clinically but if tested, most affected children have an elevated total plasma IgE level o If history suggests a particular allergic cause, skin-prick and radioallergosorbent (RAST) tests • Clinical features: o Itching (pruritus) is the main symptom and results in scratching and exacerbation of the rash Acute: Excoriated areas become erythematous, weeping and crusted (from dried serous exudate) Chronic: Lichenification (accentuation of the normal skin markings) +/- hyper/hypo-pigmentation Can readily become infected: • Staphylococcus or Streptococcus releases superantigens which seem to maintain eczema • Management: o Conservative: Paediatrics: Page 12 of 78 • Herpes simplex virus infection, although less frequent, is potentially very serious as it can spread rapidly on atopic skin, causing an extensive vesicular reaction, eczema herpeticum Avoiding irritants and precipitants, e.g. soap, synthetic fabrics, wool Nails need to be cut short/mittens at night Emollients – such as white soft paraffin and liquid paraffin ointments applied liberally two or more times a day and after a bath can replace the skin barrier; the greasier the better Occlusive bandages these are helpful over limbs when scratching and lichenification are a problem. They may be impregnated with zinc paste or zinc and tar paste. The band- ages are worn overnight Dietary elimination esp. egg cows milk and peanut if shown to cause flairs o Medical: Topical corticosteroids: mild 1% hydrocortisone ointment, can be applied to the eczematous areas twice daily, with stronger preparations restricted to acute exacerbations • Risk of skins thinning and systemic effects (cushings) o Use “finger tip units” – amount of steroid cream squeezed in a line along the distal phalanx should be enough to treat the surface area of the hand • Avoid face with moderate preparations Calcineurin inhibitors: Immunomodulators in children over 2 years old, short-term topical use of tacrolimus where there is risk of important adverse effects from further topical steroid use – only prescribed by dermatologically experienced clinician Oral antihistamine can be used for short bursts to control itch Antibiotics or antiviral agents should be reserved for when there is clinical evidence of infection; e.g. weepy/crusting in bacterial, painful vesicles/ulcers in viral • Antibiotics with hydrocortisone can be applied topically for mildly infected eczema • Systemic antibiotics are indicated for more widespread or severe infection • Eczema herpeticum is treated with systemic acyclovir and may require admission for IV treatment o Psychosocial - National Eczema Society provides support and education about the disorder Seborrhoeic eczema Eruption of unknown cause presents in the first 2 months of life, that occurs on area with many sebaceous glands – scalp, face, neck, armpits and diaper area. • The scales form a thick yellow adherent layer, on the scalp - as an erythematous scaly eruption with greasy, yellow-orange patches - commonly called cradle cap • May spread to the face, behind the ears and then extend to the flexures and napkin area • Unlike eczema it is not itchy and child is unperturbed by it • Treatment: o Mild cases will resolve with emollients o Scales on the scalp treated by ointment containing sulphur and salicylic acid applied to the scalp daily for a few hours and then washed off o Shampoos containing ketoconazole o Widespread body eruption will clear with a mild topical corticosteroid Napkin dermatitis. • Irritant/ammonia dermatitis, the most common napkin rash (although much less of a problem with use of absorbent disposable nappies) o May occur if nappies are not changed frequently enough or if the infant has diarrhoea but can occur if cleaned regularly o The rash is due to the irritant effect of urine and feaces on the skin of susceptible infants, that act to impair barrier function: Warm moist environment Friction Proteases from stool Urea-splitting organisms in faeces increase the alkalinity of urine and likelihood of a rash. o The irritant eruption affects the convex surfaces of the groin but the flexures are spared, which differentiates it from other causes of napkin rash o The rash is erythematous and may have a scalded appearance More severe forms are associated with erosions and ulcer formation o Treatment: Mild cases respond to the use of a protective emollient (Sudocream) More severe cases may require mild topical corticosteroids Michael Grant Paediatrics: Page 13 of 78 While leaving the child without a napkin will accelerate resolution, it is rarely practical at home. o Candida infection may cause and often complicates napkin rashes. The rash is erythematous, includes the skin flexures and there may be satellite lesions/pustules. Swab for testing Treatment is with a topical antifungal agent e.g. Nystatin, clotrimazole Bacterial infections: • Impetigo o This is a localised, superficial, highly contagious, staphylococcal and/or streptococcal skin infection, o Lesions are usually on the face, neck and hands and begin as erythematous macules which may become vesicular/pustular or even bullous o Exudation of fluid leads to the characteristic confluent honey-coloured crusted lesions, that readily spread to adjacent areas and other parts of the body by autoinoculation of the infected exudate Swab for C&S Increased risk with pre-existing skin disease, e.g. atopic eczema Not go to nursery or school until the lesions are dry due to contagiousness o Topical antibiotics (e.g. mupirocin - binds to the isoleucyl t-RNA synthetase in Staphylococcus aureus and Streptococcus, resulting in inhibition of protein synthesis) are sometimes effective for mild cases. However, narrow-spectrum systemic antibiotics (e.g. flucloxacillin) may be required o Nasal carriage is an important source of infection which can be eradicated with a nasal cream containing mupirocin • Scalded skin syndrome o This is caused by an exfoliative staphylococcal toxin (exfoliatin A & B from Staph aureus) which causes separation of the epidermal skin through the granular cell layers (break apart desmosomes) Important to consider in ?NAI o Fever and malaise and may have a purulent, crusting, localised infection around the eyes, nose and mouth with subsequent widespread erythema and tenderness of the skin Blister, initially in the flexors, spreads over body o Epidermis separate on gentle pressure (Nikolsky sign), leaving denuded areas but heals without scarring o IV Penicillin, analgesia, emollients and monitoring of fluid balance Viral infections: • Viral warts (HPV) o These are caused by the human papillomavirus, of which there are well over 100 types o Spread from direct, person-to-person contact or contact with infected surfaces o Warts are common in children, usually on the fingers, knees and soles (verrucae) and most disappear spontaneously over a few months or years o Treatment is only indicated if the lesions are painful or are a cosmetic problem; daily application of a proprietary salicylic acid and lactic acid paint or glutaraldehyde (10%) lotion can be used. Cryotherapy with liquid nitrogen is effective treatment but can be painful and often needs repeated application, and its use should be reserved for older children. • Molluscum contagiosum o This is caused by a poxvirus and the lesions are small, skin- coloured, pearly papules with central umbilication o They may be single but are usually multiple lesions that are widespread but tend to disappear spontaneously within a year o Treatment can exacerbate scarring but, if necessary, a topical anti-bacterial can be applied to prevent or treat secondary bacterial infection, and cryotherapy (2–3 s only) can be used in older children, away from the face, to hasten the disappearance of more chronic lesions • The human herpesviruses after primary infection, have a latency and there is an established long-term persistence of the virus that can be reactivated after specific stimuli • Herpes simplex virus (HSV) usually enters the body through the mucous membranes or skin with the primary infection may be associated with intense local mucosal damage. o HSV1 is usually associated with lip and skin lesions, and HSV2 with genital lesions o If severe, Rx: Aciclovir, a viral DNA polymerase inhibitor Local infections: topical aciclovir Wide-spread infections: Systemic aciclovir +/- admission o Presentations can be: Asymptomatic Cold sores Gingivostomatitis in those 10 months to 3 years of age. There are vesicular lesions on the lips, gums and anterior surfaces of the tongue and hard palate Paediatrics: Page 14 of 78 with high fever and lymphadenopathy lasting up to 2 weeks. Eating and drinking are painful which can lead to dehydration - necessitate IV fluids and aciclovir Skin manifestations • Eczema herpeticum – wide-spread vesicular lesions develop on eczematous skin and can cause secondary bacterial infection, which may result in septicaemia. • Herpetic whitlows – These are painful, erythematous, oedematous white pustules on the site of broken skin on the fingers beside nails Eye disease - blepharitis or conjunctivitis that may extend to involve the cornea, producing dendritic ulceration. This can lead to corneal scarring which can lead to loss of vision – examination by slit lamp required Central nervous system infection in the Neonatal setting – The infection may be focal, affecting the skin or eyes or encephalitis or may be widely disseminated. Its morbidity and mortality are high • Chickenpox (primary varicella zoster infection) o Clinical features to the right o The concurrent presence of multiple types of lesions in crops is classical – typically o Secondary bacterial infection may lead to further complications such as toxic shock syndrome or necrotising fasciitis o Encephalitis that has prognosis is good. Most characteristic is a VZV-associated cerebellitis, seen as ataxia with cerebellar signs. It usually resolves within a month. o Purpura fulminans is the consequence of vasculitis in the skin due to production of antiviral antibodies which cross-react and inactivate the coagulation factor protein S. There is subsequent dysregulation of fibrinolysis and an increased risk of clotting, o Rx is usually symptomatic unless: Valaciclovir can be considered for adolescents and adults unlucky enough to develop primary VZV infection, as it is more severe when contracted beyond childhood Human varicella zoster immunoglobulin (VZIG) is recommended for high-risk immunosuppressed Fungal infections • Ringworm is caused by dermatophyte fungi that invade dead keratinous structures in skin (Stratum corneum), nails and hair. The term ‘ringworm’ is used because of the often ringed (annular) appearance of skin lesions o A severe inflammatory pustular ringworm patch is called a kerion • Tinea capitis (scalp ringworm), sometimes acquired from dogs and cats, causes scaling and patchy alopecia with hair loss with broken hairs o Examination under Wood’s light (filtered ultraviolet) may show bright greenish/yellow fluorescence of the infected hairs with some fungal species • Tinea corpius are seen as well circumscribed, red patches that are clear in the middle • Rapid diagnosis can be made by microscopic examination of skin scrapings for fungal hyphae but definitive identification of the fungus is by culture. • Treatment of mild infections is with topical antifungal preparations, but more severe infections require systemic antifungal treatment for several weeks. o Important that any animal source of infection also needs to be treated Scabies is caused by an infestation with the eight- legged mite Sarcoptes scabiei, which burrows down the epidermis along the stratum corneum. Severe itching occurs 2–6 weeks after infestation and is worse in warm conditions and at night. Clinical features: • In older children, burrows, papules and vesicles involve the skin between the fingers and toes webspaces, axillae, penis and buttocks. Paediatrics: Page 15 of 78 • In infants and young children, the distribution often includes the palms, soles and trunk. The presence of lesions on the soles can be helpful in making the diagnosis. The head, neck and face can be involved in babies but is uncommon. • Diagnosis is made on clinical grounds with the history of itching and characteristic lesions. Although burrows are considered pathognomonic (Comma shaped lession that are 2-3mm), they may be hard to identify because of secondary infection due to scratching. • Itching in other family members is a helpful clinical indicator. • Confirmation can be made by microscopic examination of skin scrapings from the lesions to identify mite, eggs and mite faeces. Complications: • The skin becomes excoriated due to scratching and there may be a secondary eczematous or urticarial reaction masking the true diagnosis. Secondary bacterial infection is common, giving crusted, pustular lesions. Sometimes slowly resolving nodular lesions are visible. Treatment: • Whole family should be treated, whether or not they have evidence of infestation • Permethrin cream (5%) should be applied below the neck to all areas and washed off after 8–12 h, repeat after a week o In babies, the face and scalp should be included, avoiding the eyes. • Benzyl benzoate emulsion (25%) applied below the neck only, in diluted form according to age, and left on for 12 h, is also effec- tive but smells and has an irritant action. • Malathion lotion (0.5% aqueous) is another effective preparation applied below the neck and left on for 12 h. Blistering has a number of causes (infection, trauma, drug S/E, inflammatory disease, auto-immune) and can include vesicles (<5mm), bullae (>5mm) and pustules. It is always important when dealing with blisters to: • Take swabs for culture and virology Epidermolysis bullosa This is a rare, inheritied group of genetic conditions with many types, characterised by blistering of the skin and mucous membranes due to impaired connection between cells. • Blisters occur spontaneously or follow minor trauma • Management is directed to avoiding injury from even minor skin trauma and treating secondary infection. • In the severe forms, the fingers and toes may become fused, and contractures of the limbs develop • Mucous membrane involvement may result in oral ulceration and stenosis from oesophageal erosions • Rx: decompressing blisters, emollients, dressings, ABx and geneteic councilling • Development Important Presenting Symptoms and Signs in Development You should be able to describe - aetiology, presentation, signs, diagnosis and basic management of: Delayed motor milestones Delayed speech and language Impaired hearing Impaired vision Squint School refusal Truancy The Spectrum of Clinical Conditions in Development You should be able to describe - aetiology, presentation, natural history, signs, diagnosis and basic management of: Developmental delay (one or more areas) Cerebral palsy (various) Learning difficulties ADHD Autism Practical Skills Development assessment with an understanding of the developmental milestones 6 Weeks Gross motor – Limbs flexed. Head lag. Prone chin lifting. Fine Motor – Hands held in fists. Follows person with moving eyes Speech & Language – turns to sound Social – smiles at mother, watches face Vision – fixes and follows through 90 degrees 6 Months Gross motor – Good head control, Roll over, Sit when held Fine motor – Moves object hand to hand Speech & Language – responsive to word “no” and changes in tone Social – friendly to everyone, has likes and dislikes, talks to mirrors Paediatrics: Page 16 of 78 12 Months Gross motor – Sits unsupported (usuallly after 7 months). Lying -> Sitting. Pulls self up on furniture Fine motor – Pincer Grip Speech & Language – “dada” “mama”, knows the meaning of many words Social – Stranger anxiety 15 Months Gross Motor – Sitting to standing alone. Walks (unstable). Crawl upstairs Fine Motor – Point to what they want. Tower of 2 bricks Speech & Language – listens, enjoys songs Social – understands many phrases 18 Months Gross Motor – Steady gait. Run short distance Fine Motor – Hand dominance normal (Before now can imply pathology of contralateral) Scribbles with crayon. Turns 2/3 pages Speech & Development – can point to 2/3 parts of body 2 Years Gross Motor – Up & down stairs. Climb furniture. Throw & kick ball Fine Motor – Tower of 6 bricks. Vertical line. Shapes in slots Speech & Language – asks for food/drink. 2/3 word sentences 3 Years Gross Motor – Walks upstairs with alternating feet. Stand on one foot. Tricycle Fine Motor – Tower of 9 cubes. Draw circles. Speech & Language – knows nursery rhymes, count to 10, two colours Social – can undress & dress, needs help with buttons and which shoe 4 Years Gross Motor – Walks down stairs using alternating feet. Hop on 1 foot Fine Motor – Can write name. Use scissors. Speech & Language – gives 1st and 2nd name Social – can attend all toilet needs Developmental delay: Global developmental delay implies a delay in the acquesiton of skills in all fields (ross motor, vision and fine motor, hearing and speech, and language and cognition, social/ emotional and behaviour) and is usaully apparent by 2 years. • Must investigate for cause (box to right) • As children become older it is more appropriate to describe them as having a learning disability, motor disorder and communication difficulty Abnormal motor development is a delay in the acquestion of motor skills (e.g. head control, rolling, standing, walking, balance, asymmetry in hand use) and can present as early as 3 months (failure to to develop good head control). Causes include: • Central motor deficit (e.g. cerebral palsy) • Congenital myopathy • Spinal cord lesions (e.g. spina bifida) Important signs to looks for include: • Developing hand preference before 1-2 years Paediatrics: Page 17 of 78 • Late walking (>18 motnhs) although this need to be differentiated from normal locomotion varients (bottom-shuffling, command crawling) Cerebral palsy is an non-progressive abnormaltity of movement and posture, due to brain injury (at birth or up to the age of 2 years) affecting 2 in 1000 live births, that is a major cause of abnormal motor development. Can often be accompanied by issues with cognition, communication, sensation and behaviour. • Causes: o 80% antenatal origin due to vascular occlusion or structural maldevelopment of the brain o 10% from hypoxic-ischaemic injurgy during delivery o 10% postnatal such as meningiits/encephalitis/encephalopathy, head trauma (exclude NAI), symptomatic hypoglyceamia, hyperbilirubinaemia (kernicterus) • Clincal presentation: o Abnormal limb and/or trunk posture o Delayed motor milestones o Asymmetic hand function (before 12 months) o Abnormal gait • Diagnosis is by clinical examination and can be classifed into 3 subtypes: o Spastic – dammage to upper motor neurones (pyramidal or corticospinal tract) casues increased (velocity dependant, clasp knife) lim tone, brisk tendon reflexes and extensor plantar. Basically an early stroke. Hemiplegia: arm more effected than leg, face sparing, tiptoe walk (ttoe-heel gait) Quadriplegia: all four limbs affected sevrealy, trunk involvment (extensor posturingn), poor head control; this more severe form is assocatied with seizures and microcephaly Diplegia: all four limbs, but the legs are effected to greater degree o Dyskinetic – involves involuntary movements due to damage in the basal ganglia or their associated pathways (extrapyramidal). that can be chorea, athetosis (writhing) and dystonia (simultaneous contraction of antagonist muscles of trunk and proximal muscles giving twisting appearance) Common causes; kernicterus due to Rhesus haemolysis and hypoxic-ischaemic encephalopathy o Ataxic – tend to be genetically deteremined damaged to cerebellum; resulting in poor coordination, intention tremor and • Managament is by multidisciplinary approach Abnormal speech and language development involves a deficit in either receptive of expressive speech and language, or both. Causes include: • Hearing loss • Anatomical issue with speech production (e.g. cleft palate, cerebral palsey) • Enviromental deprivation/social neglect • Normal variant (late talking can be familail) A SLT sould be inovled for hearing assessment and to promote alternate forms of communication (e.g. Makaton) Abnormal development of social/communication skills (autistic spectrum disorders) describes the failure to acquire normal social and communication skills. The prevalence of autistic spectrum disorder is 3–6/1000 live births, but particularly affects boys, and usually presents at 2-4 years of age. • Typically seen as certain co-morbities (learning/attention difficulties and seizures) plus a triad of: o Impaired social interaction (perfers own company, avoids eye contact, disregard for others’ thoughts/feelings, failure to grasp social cues) o Speech and language disorder (delayed speech, limited use of gestures/facial expression, formal pedantic language, over-literal interpretation of speech [i.e. raining cats and dogs], refers to self as you) o Imposition of routines with ritualistic behavior (peculiar interests, poverty of imagination) The only treatment with evidence is applied behavioural analysis (ABA), a behaviour modification approach that helps to reduce ritualistic behaviour, develop language, social skills and play and to generalise use of all these skills. It is currently the most widely accepted treatment approach but requires 25–30 h of individual therapy each week, so is costly and time-consuming. Learning difficulites can be described as: • General: typically measures by IQ borderline (70-80), moderate (50-70), severe (35-50) and profound (<35) o Severe tends to have an organic cause (3-4 per 1000) while moderate (30 per 1000) is affected by socioeconomic class • Specific: o Dyspraxia - disorder of motor planning and/or execution with no significant findings on standard neurological examination (seen with poor handwriting, messy eating with dribbling, poorly established laterallity) o Dyslexia – reading skills disproportionate to child’s IQ (more than 2 years behind age) o Dyscalculia – disorder of calculation Hearing impairment can be classifed as: • Sensorineural o Uncommon (1 in 1000 births) and due to lesion in cochlea or auditory nerve o Irreverisble reduction in hearing of any severity o Severe bilateral will require early amplicaiton by hearing aid or, if severe enough, cochlear implants • Conductive o More common and typically casued by otitis media with effusion o Even with infective casues, can last months of years especailly in those with risk factors (Down’s, celft palate, atopy) Michael Grant Paediatrics: Page 18 of 78 o Impedance audiometry tests can measure the air pressure of middle ear and the complianace of tympanic membrane o Treatment: decongestant or long course of ABx, consider grommets if resistant Abnormalities of vision may present with: • Loss of red eye relfex (cataract) • White reflex - Retinoblastoma, cataract or retinopathy of prematurity (disorganized growth of retinal blood vessels which may result in scarring and retinal detachment) • Not smiling by 6 months • Nystagmus • Squint Squint (Strabismus) is a misallignment of the visual axes. Important to note that there can be normal, transient squints up to 3 months and that marked epicanthic folds can give false appearance of squint. Squint persisting beyond 3 months must be assessed. There are due to a failure of binocular vision development caused by refractive errors (cataracts and retinoblastomas must be excluded) . They are divided into: • Concomitant due to refractive error in one or both eyes that can be corrected by glasses. They usually turn inwards • Paralytic (rare) due to paralysis of motor nerves – can be sign of space occupying lesions Testing can involve: • Corneal light reflex test to compare location of reflection in each eye • Cover test in which squinting eye will move to take up fixation when the “good” eye is covered – performed at both 33cm and 6m as some squints are only present at distance Refractive errors: • Hypermetropia (long sight) is the most common refractive error in young children. High degrees or asymmetric hypermetropia should be corrected early to avoid irreversible damage to vision (amblyopia). • Amblyopia is a potentially permanent loss of visual acuity in an eye that has not received a clear image. It affects 2–3% of children. In most cases, it affects one eye; rarely, both are involved. Caused by any interference such as refractive errors, squint or visual deprivation, e.g. ptosis or cataract. Treatment is by relieving deprivation and correction of any refractive error with glasses, together with patching of the ‘good’ eye for specific periods of the day to force the ‘lazy’ eye to work and continued until the vision in the ‘lazy’ eye no longer improves. The longer treatment is delayed, the less likely it is that normal vision will be obtained. Early treatment is essential, as after 7 years of age improvement is unlikely. Hyperactivity In the true hyperkinetic disorder or attention deficit hyperactivity disorder (ADHD), the child is undoubtedly overactive in most situations and has impaired concentration with a short attention span or distractibility. There is a powerful genetic predisposition and the underlying problem is a dysfunction of brain neuron circuits that rely on dopamine and which control self-monitoring and self-regulation. • Estimated as between 10 and 50 per 1000 children, boys exceeding girls three-fold. • Manifests as disorganised, poorly-regulated and excessive activity; have difficulty with taking turns; sharing; are socially disinhibited; and butt into other people’s conversations and play; made worse in familiar or uninteresting situations • They also cannot regulate their activity according to the situation – they are fidgety; have excessive movements inappropriate to task completion; lose possessions; and are generally disorganised • Typically, they have short tempers and form poor relationships with other children, who find them exasperating. • The children do poorly in school and lose self- esteem. Management: • First-line management - in with mild to moderately severe disorder is the active promotion of behavioural and educational progress by specific advice to parents and teachers to build concentration skills, encourage quiet self-occupation, increase self-esteem and moderate extreme behaviour. These involve having clear rules and expectations, and consistent use of rewards to encourage adherence and where appropriate, consequences to discourage unacceptable behaviour. • Medication, although this is usually reserved for children >6 years. Stimulants such as methylphenidate or dexamphetamine and non- stimulants, like atomoxetine, reduce excessive motor activity and improve attention on task, focused behaviour o Yearly trial off medication is recommended to evaluate the need for continuing treatment. Specialist supervision is mandatory. Close liaison with the school is required throughout the years of treatment. • The role of diet in the cause and management of hyperactivity is controversial. Current evidence indicates that the sort of diet which aims blindly to reduce sugar, artificial additives or colourants has no effect. A few children display an idiosyncratic behavioural reaction such as excitability or irritability to particular foods. If this seems likely, trying the child on an exclusion of that particular food may be useful. In general, food and drinks with caffeine are not advised. Michael Grant Paediatrics: Page 19 of 78 Endocrine Important Presenting Symptoms and Signs in Endocrine, metabolism and growth You should be able to list the 3-4 commonest causes of these symptoms/signs at various ages and be able to differentiate these (by features and investigations): Delayed/ precocious puberty Short stature Tall stature Obesity Microcephaly Macrocephaly The Spectrum of Clinical Conditions in Endocrine, metabolism and growth You should be able to list the 3-4 commonest causes of these symptoms/signs at various ages and be able to differentiate these (by features and investigations): ◦ Diabetes mellitus ◦ Hypoglycaemia ◦ Hypothyroidism ◦ Hyperthyroidism ◦ Growth and puberty (normal and abnormal) ◦ Inborn errors of metabolism ◦ Short stature ◦ Tall stature ◦ Abnormalities of head size (macrocephaly/ microcephaly) ◦ Failure to thrive Premature sexual development The development of secondary sexual characteristics before 8 in males and 9 in females is abnormal; when accompanied with a growth spurt it is known as precocious puberty. Precocious puberty can be categorsied according to the level of pituitary-derived gonadotropins (FSH and LH); • Gonadotropin dependant True PC with premature activation of hypothalmic-pituitary-gonadal axis (increased FSH and, especailly, LH) • Gonadotropin independent from excess sex hormones In females the cause is usually idiopathic of familial and follows the normal sequence of puberty – can be seen on USS as multicystic ovaries with enlarging uterus. In males it is uncommon and usually has an organic cause, particularly intracranial tumours. • Examination of the testes is important: o Bilateral enlargement – gonadaotropin realse from intracranial lesion o Unilateral enlargment – gonadal o Small testes – adrenal hyperplasia/tumour Management: • Treat any underlying pathology (e.g. tumour) • Reduce rate of skeletal maturaion if neccesary, to prevent early cessation of growth (bone age study by x-ray of left hand to look at epiphysis calcification) • Address psychological/social difficulties • If Rx required for GnRH dependant disease then gonadotropin-releasing hormone (GnRH) ana- logues are the treatment of choice; for GnRH independent, nhibitors of androgen or oestrogen production or action (e.g. medroxypro- gesterone acetate, cyproterone acetate, testolactone, ketoconazole) may be used. Delayed puberty Defined as the absence of pubertal development by 14 in females and 15 in males. It is more common in males and the most common cause is constitutional delay, which is often familial. Other common causes include excessive dieting or training. Affected children will been seen with: • Short stature during childhood • Delay in sexual maturation • Delayed skeletal maturity on bone age study • Eunuchoid body habitus – long legs compared to back Paediatrics: Page 20 of 78 Assessment should take the form of: • In males; pubertal staging (testicular volume) and identify chronic disease • In females; karyotyping to identify turner syndrome (45 X0), thyroid and sex hormone testing Management • Treat any underlying pathology • Ensure psychological adaption to puberty • In extreme cases; accelerate growth and entry into puberty: o Young males: Oxandrolone – helps growth but not secondary sexual characteristics o Older males: lose dose IM testosterone o Females: Oestradiol Short stature is height below the second centile (1 in 50) with most of these children will be normal with short parents, but the further below they are the more a pathological cause should be sought. • Issues include bullying, poor self-esteem, disadvantage at sports and inappropriate treatment (due to assumed younger age) • Growth velocity is the most important measure and may show growth issues before they go below the second centile. This involves taking two accurate measurements at least 6 months but preferably a year apart allow calculation of height velocity in cm/year o Compared with the weight centile and an estimate of their genetic target (Mean of parents’ height [if male, +9cm] or [if female, -7cm]) • Causes include: o Familial – short parents o IUGR and extreme prematurity – children born in these settings may remain short and growth hormone treatment may be required o Constitutional delay – delayed puberty that is often familial, but may also occur with excessive dieting or exercise. Seen with eunuchoid features (legs longer than bank) o Endocrine - Hypothyroidism, growth hormone (GH) deficiency, IGF-1 (insulin-like growth factor 1 – downstream effector of GH) deficiency and steroid excess (iatrogenic usually, even with low doses of inhaled) o Hypothyroidism – usually due to autoimmune thyroiditis and seen with weight gain. Congenital hypothyroid is detected early and thus doesn’t cause small stature. o Growth hormone deficiency - This may be an isolated defect of pituitary or secondary to panhypopituitarism. Can be treated by synthetic GH. Pituitary function may be abnormal in: Congenital mid-facial defects Craniopharyngioma seen in late childhood with bitemporal hemiopia and/or papilloedema Hypothalamic pathology; trauma, tumour, meningitis, irradiation Laron syndrome in which a person produces defective growth hormone receptors resulting in growth hormone insensitivity. This produces extreme short stature • High growth hormone levels but low levels of the down- stream active product of IGF-1 produced at the growth plate and in the liver • Recombinant IGF-1 therapy can be used o Nutritional/chronic illness - This is a relatively common cause of abnormal growth Inadequate nutrition from poor diet, or reduced appetitive from chronic disease: • Coeliac disease may result in short stature if gastrointestinal symptoms are mild and thus not detected in first 2 years of life o Seen with gluteal wasting o Look for Anti-TTG, EMA, Gliadin antibodies (all IgA) but be aware of IgA deficiency (test for IgG anti-gliadin) o Associated with diabetes type 1 • Crohn disease • Chronic renal failure o Chromosomal disorders especially: Turner syndrome should always be excluded in short girls • Thought to be caused by absence of one of the SHOX (short stature homeobox) on the missing X chromosome Russell–Silver syndromes may present with short stature Prader–Willi syndrome an imprintng disorder resulting in early hypotonia and feeding difficulties followed by short stature, obesity from obsessive eating and learning difficulties caused by the absence of certain genes normally present on the copy of chromosome 15 inherited from the father • Treated with GH to improve strength, body composition and modestly improving final height o Skeletal dysplasias (“Dwarfism”) of which the most common type of skeletal dysplasia is called achondroplasia. This is caused by autosomal dominant mutations in the FGFR3 gene, which normal development FGFR3 has a negative regulatory effect on Paediatrics: Page 21 of 78 bone growth but, in achondroplasia, the mutated form is constitutively active. Legs are longer than back (opposite in mucopolysaccharidoses) Tall stature is less common but typically results, too, from tall parents. o Obesity in childhood may “fuel” early growth but final height will be similar. o Secondary endocrine causes are rare o Both congenital adrenal hyperplasia and precocious puberty lead to early epiphyseal fusion so that eventual final height is reduced o Marfan (a disorder of loose connective tissue) and Klinefelter (XXY – an excess of SHOX dose) syndromes Abnormal head growth Most head growth occurs in the first 2 years with 80% of adult size reached by the age of 5. Heads may be familial and the mid-parental head percentile may need to be calculated. • Head circumference may increase across centiles, especially if small for gestational age. • The posterior fontanelle has closed by 8 weeks, and the anterior fontanelle by 12–18 months. • If there is a rapid increase in head circumference, raised intracranial pressure should be excluded Microcephaly is a head circumference below the 2nd centile, can be due to: • Familial • Autosomal recessive conditions • Congenital infection • Insult to developing brain (e.g. perinatal hypoxia, hypoglycaemia, meningitis) Macrocephaly is a head circumference above the 98th centile. • Rapidly increasing head circumference suggests raised ICP (e.g. hydrocephalus, subdural haematoma, brain tumour) o Investigation by intracranial ultrasound (if anterior fontanelle still open – e.g. <12-18 months) or CT and MRI Type 1 DM is the third most common chronic disease in UK children (after asthma and cerebral palsy). • Typical presentation: Several weeks of polyuria, lethargy, polydipsia, and weight loss ±infection, poor growth; ketosis. • Typical age: 4–12yrs. • Diagnostic criteria: signs of hyperglycaemia with venous blood glucose, ie ≥11.1 mmol/L (random) or ≥7mmol/L (fasting) , or raised venous blood glucose on 2 occasions without symptoms. Oral glucose tolerance tests are rarely required in children, but they are based on glucose levels at 0h and 2h post a 1.75g/kg glucose load • Treatment: Should be delivered by a multi- disciplinary paediatric diabetes care team—which provides 24h access to advice. Inform children and parents that they may experience a partial remission phase (‘honeymoon period’) with the start of insulin. o Starting insulin: Discuss with paediatric endocrinologist and use local protocols. One regimen would be to estimate total daily requirement of insulin (0.8–1 units/kg/24h for prepubertal children; 1.5units/kg/24h if pubertal) this daily dose should be 1⁄3 rapid acting (eg Novorapid®) and 2⁄3 long-acting (eg protaphane) 2⁄3 of the daily dose should be given pre-breakfast, and 1⁄3 should be given pre dinner. Tailor insulin regimen to your patient and their family. o Diet: Ask a paediatric dietician. Energy needs ≈1500kcal/m2 or 1000kcal +100 to 200kcal for each year of age. Aiming for 30% of this with each major meal, and 10% as a bedtime snack suits some children. Giving ~20% of calories as protein, ~50% as unrefined carbohydrate, and ≤30% as fat is a rule of thumb. If the child is mildly to moderately symptomatic and clinically well, subcutaneous insulin and oral diet and fluids may be begun at diagnosis, avoiding hospital admission. • Sick day rules: o Never stop insulin, even if not eating (stress response ups glucose) o Test blood more often, ideally every 4 hours o If vomiting, check urine ketones twice a day – come to hospital if +++ or more o Maintain fluid intake o Consider making a “sick day kit”: extra testing strips, insulin, sugary drinks DKA results from a deficiency of insulin, often in combination with increased levels of counter-regulatory hormones (catecho- lamines, glucagon, cortisol and growth hormone— eg due to sepsis). The big concern with childhood DKA, (as opposed to adult DKA), is the increased frequency of cerebral oedema, which occurs in ~1% of childhood DKA and has a mortality of 25%. Other fatal events in DKA include hypokalaemia and aspiration pneumonia (use NGT if semi-conscious and protect airway). • The patient: Listlessness; confusion, vomiting; polyuria; polydipsia; weight loss; abdominal pain • Look for: Dehydration; deep and rapid (Kussmaul) respirations; ketotic (fruity-smelling) breath; shock; drowsiness; coma. • Diagnosis: Requires the combination of hyperglycaemia (≥11mmol/L), acidosis (venous pH <7.3) and ketones in urine and blood. o Severity is categorized by degree of acidosis: mild—pH <7. 3; moderate—pH <7. 2; or severe—pH <7. 1 • Management: Do GCS; True coma is rare (<10%) in DKA: exclude other causes of coma; remember DKA may be precipitated secondarily • Take the following action if shocked, consciousness, coma, or vomiting: o Resuscitate: ABC: Oropharyngeal airway 100% O2 ± NGT. Consider intubation. Give 10mL/kg IV boluses of 0.9% saline only if shocked, to a max. of 30mL/kg: over-enthusiastic fluid resuscitation may cause cerebral oedema. Paediatrics: Page 22 of 78 • Consider ITU if BP drops, or <2yrs, or ward staff busy (all children with DKA initially require high level of nursing care—usually 1:1) o Rapidly confirm diagnosis: with history, finger-prick glucose + ketones; venous blood gas; urine dip for ketones/glucose. o Formal investigations: Weigh; FBC; U&E; glucose; Ca2+; PO43–; blood gas; ECG monitoring (look for peaked T-waves of hyperkalaemia), lab urine. o Use clinical signs to assess dehydration; Now calculate the volume of fluid to be replaced (fluid requirement): i.e. maintenance fluid plus the dehydration deficit minus any fluid already given as resuscitation fluid. It should be given at a constant steady rate over the 1st 48h. o Start IV fluids: Start with 0.9% saline + 20mmol KCl/500mL. When blood glucose falls to 14mmol/L use 0.9% saline + 5% glucose + 20mmol KCl /500mL. After 12h, if plasma sodium is stable, change to 0.45% saline + 5% glucose + 20mmol KCl/500mL. o Start IV insulin only after 1h of IV fluids: Cerebral oedema may be more likely if insulin is started early. There is no need for an initial bolus of insulin. Use a 1 unit/mL solution of fast acting insulin (eg Actrapid®). Run at 0.1 units/kg/h Ensure there is glucose in the IV fluids when venous glucose is <14mmol/L. DO NOT stop insulin at this stage, it is still required to switch off ketogenesis. Once pH >7.3 and glucose is <14mmol/L consider reducing insulin to 0.05units/kg/h o Stop IV insulin: When blood ketone levels are <1.0mmol/L, and patient is able to tolerate food, give a dose of subcutaneous insulin; feed the patient. Stop infusion 10–60mins after subcutaneous insulin injection Avoid bicarbonate in DKA: it can increase the risk of cerebral oedema. If acidosis persists, consider dose of insulin (more glucose may be needed in the IV fluids). Hypoglycaemic coma: • Get IV access. Get help. Intra-oral GlucoGel® has a role if IV access fails. • Give glucose 5mL/kg of 10% dextrose IVI, or by rectal tube if no IV access, with glucagon 0.5–1mg IM or slowly IV (0.5mg if <25kg). • Expect quick return to consciousness o If not, recheck glucose; if low, give IV dexamethasone; o If normal, ask yourself is this is a post-ictal state after a hypoglycaemic fit? Here, giving more glucose worsens cerebral oedema. Hypothyroidism Thyroid hormone is necessary for growth and neurologic development. Dysfunction may occur in the neonate, infant or during childhood. Congenital: Thyroid scans divide these into 3 groups: athyreosis (complete absence); thyroid dysgenesis (ectopic or underdeveloped); dyshormonogenesis (problem with synthesis). Also remember maternal antithyroid drugs (eg propylthiouracil). Acquired: Prematurity; Hashimoto’s thyroiditis; hypopituitarism; X-rays; Down’s syndrome. • Signs: May be none at birth—or prolonged neonatal jaundice, widely opened posterior fontanelle, poor feeding, hypotonia, and dry skin are common. Inactivity, sleepiness, slow feeding, little crying, and constipation may occur. o Look for coarse dry hair, a flat nasal bridge, a protruding tongue, hypotonia, umbilical hernia, slowly relaxing reflexes, pulse, and poor growth and mental development (cretinism). o Other later signs: IQ, delayed puberty (occasionally precocious), short stature, delayed dentition. • Universal neonatal screening: Cord blood or filter paper spots (at ~7 days, from heel prick) allow early diagnosis (the ‘Guthrie card). They do prevent serious sequelae. Act on high and low TSHs (may indicate pituitary failure). • Tests: reduced T4, increased TSH (but undetectable in secondary hypothyroidism), decreased Iodine uptake, reduced Hb. Paediatrics: Page 23 of 78 o Bone age < chronological age; left wrist and hand have a large number of ossification centres. Each passes through a number of morphological stages, and using comparisons with key diagrams from ‘normal’ populations. • Levothyroxine (LT4): Start neonates with ~15μg/kg/day; adult doses are reached by 12yrs. Adjust according to growth and clinical state. Avoid high TSH levels. Those with athyreosis need the highest doses of T4 and the closest monitoring early on. Those with dysgenesis and dyshormonogenesis need more attention later. Hyperthyroidism Typical child: Pubertal girl. Signs/ lab features: Same as adult; palpitations, tremor, hypertonia, restlessness, weight loss, graves disease • Fine-needle cytology of goitres may show juvenile autoimmune thyroiditis. Carbimazole starting dose: ~250μg/kg/8h. Adjust according to response. Propylthiouracil: 2.5mg/kg/8h (/12h in neonates) PO until euthyroid—then ad- just dose; expect remission in ~67%. • Higher doses may be needed. Typical maintenance dose: 1⁄3–2⁄3 of remission-inducing dose. Inborn errors of metabolism These are often diagnosed by a urine metabolic screen (eg amino acids, organic acids, carbohydrates, mucopolysaccharides—in deciding which tests to do, get help; interest the lab in your problem). Typical signs: diarrhoea, lethargy, respiratory distress, metabolic acidosis (± odd body smells), jaundice, hypoglycaemia, U&E imbalance, fits, and coma. Features may be intermittent, and provoked by crises (eg infection; dehydration). In addition, signs in box to right: Newborn screening test to detect hypothyroidism and phenylketonuria (PKU). The tests are done on a spot of blood from a heel-prick collected onto a filter paper. Rhe screening programme has been extended to include cystic fibrosis, haemoglobinopathies and the metabolic disorder MCADD. Emergency management of IEM involves: • Stopping feeds • Promote anabolism with 10% dextrose + appropriate electrolytes additives for imbalances • Eliminate toxic metabolites: o Drugs, e.g. Sodium benzoate (for ammonia), carnitine (for organic acids) o Dialysis – extremes of ammonia, organic acids, MSUD, lactate Amino acid disorders: Phenylketonuria is due to a deficiency of the enzyme phenylalanine hydroxylase (classical PKU, alothough there is a rarer type involving the synthesis of biopterin cofactor for this enzyme) • Clinical features: o Developmental delay at 6–12 months of age o Fair haired, blue-eyed (may develop eczema o There may be a musty odour PKU (phenylalanine ketonuria) • Cause: Mutation of phenylalanine hydroxylase (PAH) gene (chromosome 1—autosomal recessive) leading to absent or reduced activity of phenylalanine hydroxylase. Classic PKU leads to gradual mental impairment. The defect leads to reduced CNS dopamine, reduced protein synthesis, and demyelination. Milder forms of hyperphenylalanaemia can occur with different mutations to the same gene, or mutations to co-factor tetrahydrobiopetrin (BH4). • Clinical features: Fair hair and blue eyes (lack of tyrosine), fits, eczema, musty urine. The chief manifestations is reduced IQ (eg dyscalculia ± poor spelling ± cognition) • Tests: Hyperphenylalaninaemia (reference interval: 50–120μmol/L). Treatment instigated in infants with levels >360μmol/L—to avoid reduced IQ which may start with levels of >394μmol/L. • Treatment: Get expert help. • Diet: protein substitute that lacks phenylalanine but is enriched in tyrosine. Aim to keep phenylalanine levels to <360μmol/L570 by prescribing artificial food substitutes (amino acid drinks) to give <300mg–8g of natural protein/day (depending on age and severity of phenylalanine hydroxylase deficiency). o Hypomyelination may be proportional to degree of phenylketonaemia, but some studies fail to show stricter diets are associated with higher IQs. o Despite treatment, children are more prone to depression, anxiety, phobic tendencies, isolation, and a less ‘masculine’ self- image. o Adherence to the diet may be poor (it’s unpalatable). May cause changes of questionable significance in levels of selenium, zinc, iron, retinol, and polyunsaturated fatty acids. • Prevention of manifestations: Screen blood at 1 week (using a heel-prick and filter paper impregnation—the Guthrie test). Paediatrics: Page 24 of 78 • Maternal phenylketonuria: Preconception counselling is vital as baby can be born with: facial dysmorphism, microcephaly, growth retardation, IQ Homocystinuria This is due to cystathionine synthetase deficiency. • Clinical features: Developmental delay, subluxation of the ocular lens (ectopia lentis), progressive learning difficulty, psychiatric disorders and convulsions, skeletal manifestations resemble Marfan syndrome, complexion is usually fair with brittle hair, Thromboembolic episodes may occur at any age. • Treatment: Almost half respond to large doses of the Vitamin B6 (coenzyme pyridoxine). Those who do not respond are treated with a low-methionine diet and the re-methylating agent betaine Disorders of carbohydrate metabolism: Diagnosis is with a ‘metabolic screen’ in addition to the standard investigations for unwell infants. The ‘metabolic screen’ varies between laboratories and should be discussed with the specialist laboratory before collecting samples. The urgency should also be indicated. Both blood and urine samples will be needed. In patients with acidosis, beside ketone testing and calculation of the anion gap can be helpful. Values >25 mmol/L (normal 12–16 mmol/L) are usually secondary to an organic acidaemia. Galactosaemia is a rare, recessively inherited disorder results from deficiency of the enzyme galactose-1-phosphate uridyltransferase, which is essential for galactose metabolism. • When lactose-containing milk feeds such as breast or infant formula are introduced, affected infants feed poorly, vomit and develop jaundice and hepatomegaly and hepatic failure – death by liver failure or E.Coli sepsis. • Improvement when given intravenous fluids but relapse if milk feeds are restarted is characteristic of classical galactosaemia. • Chronic liver disease, cataracts within a few days and developmental delay are inevitable if the condition is untreated. • Management is with a lactose- and galactose-free diet for life. • Even if treated early, there are usually moderate learning difficulties (adult IQ 60–80) • Treatment: o Restriction of lactose and galactose o Neonate: Acutely management (10% dextrose/supportive treatment) followed by soya feeds o Older children: Beware of hidden sources of lactose/galatose e.g. milk powder additives, drugs in tablets, toothpaste, sausage fillers Feeding Importance of adequate nutrition Nutrition requirements at different ages Benefits of Breastfeeding Awareness of different formula's available for different medical conditions The Spectrum of Clinical Conditions ◦ Feeding difficulties ◦ Failure to thrive/ faltering growth ◦ Malnutrition ◦ Deficiency ◦ Obesity Breastfeeding Health Benefits for Baby Reduced: • GI and respiratory infections • Necrotizing enterocolitis • UTI • Urine infections • Allergic diseases (eczema, asthma and wheezing) • Type 1 and 2 diabetes • Obesity Principles of breastfeeding Positioning – CHIN: Close Head free In line Nose to nipple Paediatric Nutrition Background knowledge Assessing nutritional status ◦ Plot height and weight on growth charts (determine trend and centiles) • Childhood leakaemia • SIDS Health benefits for mother Reduced: • Breast cancer • Ovarian cancer • Hip fracture and osteoporosis • Cardiovascular disease Nutrient Neonate/Infant Children 2-12 years Adolescent Energy kcal/kg/day 80-100 60-80 30-40 Protein g/kg/day 1.2-1.8 1 0.8 Fluid ml/kg/day 100 for 1st 10 kg, 50 for 2nd 10kg, 20 for remainder Paediatrics: Page 25 of 78 ◦ History and examination ◦ Bloods: haemoglobin, electrolytes (including Mg, PO, Ca), LFTs (including albumin), haematinics (B12, folate, ferritin) ◦ Normal requirements Matching requirements ◦ Most formulas contain 0.6-1 kcal/ml and are nutritionally complete ◦ The volume of formula required must be calculated by working out their requirements ◦ Daily volume required (ml) = daily requirement (kcal) / formula concentration (kcal/ml) Age progression ◦ Breast milk is ideal for most infants ◦ Weaning on to solids should occur at 6 months o Initially baby rice, fruit and vegetables, then progress tastes and textures o Finger food from 7 months ◦ Complimentary breast or formula milk should continue until 1 year, then full fat cow’s milk should be main drink (semi-skimmed from 2 years) ◦ Supplemental vitamins A, C and D until 5 years ◦ Older children: whole-grain cereals; 5-a-day vegetables/fruit; 2 servings of meat or alternatives per day; 1 starchy food at each meal time; 3-4 portions of dairy product per day Formulas Standard milk-based o Examples: aptamil, SMA first, Enfamil, cow & gate, babynet, alpro, hollie Protein variations (for dietary protein intolerances) Relatively high incidence of adverse reactions to food proteins in infancy • Immaturity of immune system • Increased gut permeability to large molecules • IgA deficiency involved in immune defense mucosal surfaces • CMPI most common, range of estimates • 5-15% show symptoms of CMPI Soy formulas o Still whole protein but different type o Not first line because up to half of babies with cow’s milk protein intolerance are also intolerant to soy protein o Examples: infasoy, wysoy Partially-hydrolysed o Available over the counter o Examples: aptamil comfort, cow & gate comfort, SMA comfort Extensively-hydrolysed o 1st line for dietary protein intolerances o Examples: nutramigen 1, pepti junior, aptamil pepti, infatrini peptisorb Elemental (amino-acid based) o 2nd line for dietary protein intolerances o Very expensive o Examples: neocate LCP, nutramigen AA Carbohydrate variations (for carbohydrate intolerances) Lactose-free o Examples: enfamil o-lac, SMA LF Fat variations (for fat absorption disorders) Medium chain triglyceriedes (MCT) o Examples: portagen powder Light chain triglyceriedes (LCT) Viscosity variations (for reflux) Thickened o Examples: SMA stay down, enfamil AR (anti-reflux), aptamil AR High energy variations (for catch up growth) High energy o Examples: infatrini, SMA high energy Enteric feeds When oral feeds cannot sustain adequate growth and the gut is functioning, formula milk, expressed breast milk or enteral feeds can be administered via tubes... Administration methods • Fine bore-nasogastric (NG) tube – default • Nasojejunal (NJ) tube – if problems with gastric reflux or delayed gastric emptying • Percutaneous gastrostomy/jejunostomy tube – for longer term feeding i.e. >4-6 weeks or if mechanical swallowing obstruction Administration Paediatrics: Page 26 of 78 • Boluses – more physiological but can cause ‘dumping syndrome’ (fluid shift into the gut lumen with plasma volume contraction and acute intestinal distention) • Intermittent infusion – most commonly used (e.g. 10 hours on, 2 hours off) • Continuous infusion – used for very ill patients Drugs down enteric tubes • Use solutions where possible • Some tablets can be crushed and some capsules may be opened (check with pharmacist) • Tablets which cannot be crushed: modified release tablets; enteric coated tablets Parenteral nutrition Parenteral nutrition may be required in intestinal failure (acute or chronic) and is given via central venous access • ‘Parenteric nutrition’ (PN) – if also feeding patient by other methods • ‘Total parenteric nutrition’ (TPN) – only IV feeding Re-feeding syndrome • Insulin surge and re-switching on of cellular membrane pumps in response to feeding causes electrolyte abnormalities (especially K+, PO43-, Mg2+) which can lead to arrhythmias and death • Check K+, PO43-, Mg2+ • Prevent by starting feed slowly in at risk patients • Management o Continue low level of feed o Daily bloods minimum initially o Replace all electrolytes – see common prescriptions Causes of faltering growth Low intake cases) Food loss Not enough food offered or taken (95% of Psychological Structural Neurological GORD Pyloric stenosis Dysmotility Increased requirements Cystic fibrosis Congenital heart disease Malignancy Malabsorption - Digestive Carbohydrate ‘intolerance’ (lack of enzymes mean undigested disaccharides increase osmotic load causing flatulence, bloating, diarrhoea and cramps after eating carbohydrate) o Lactose intolerance Congenital lactase deficiency (rare) Secondary to enterocyte damage after gastroenteritis (transient) o Maltose intolerance o Sucrose intolerance Pancreatic o Cystic fibrosis o Chronic pancreatitis o Cholestasis Malabsorption - Mucosal • Dietary protein ‘intolerance’ (allergy to certain proteins) o Investigations: Skin prick testing (SPT), Radioallergosorbent test (RAST), Specific IgE Cow’s milk protein allergy (presents in first few months after being fed with formula) Soya bean protein allergy Egg protein allergy • Coeliac disease (presents any time after weaning with bloating, diarrhoea, failure to thrive) • Inflammatory bowel disease • Abetalipoproteinemia (autosomal recessive mutation in microsomal triglyceride transfer protein resulting in interference with fat and fat soluble vitamin absorption) • Intestinal venous/lymphatic obstruction (e.g. cardiac failure, lymphangiectasia) Failure to thrive • is a description, not a diagnosis • weights of infants are only helpful if accurate and plotted on a centile chart • is present if an infant’s weight falls across two centile lines Paediatrics: Page 27 of 78 • is likely to be present the further the weight is below the 2nd centile • is mostly due to inadequate food intake • is accompanied by abnormal symptoms or signs if there is organic disease • most affected infants and toddlers do not require any investigations and are managed in primary care by increasing energy intake by dietary and behavioural modification and monitoring growth. Gastroenterology Important Presenting Symptoms and Signs in Gastrointestinal You should be able to list the 3-4 commonest causes of these symptoms/signs at various ages and be able to differentiate these (by features and investigations): Abdominal pain Diarrhoea Constipation Vomiting The Spectrum of Clinical Conditions in Gastrointestinal You should be able to describe - aetiology, presentation, natural history, signs, diagnosis and basic management of an infant/toddler/older child with: ◦ Gastro-oesophageal reflux ◦ Pyloric stenosis ◦ Coeliac disease ◦ Milk intolerance ◦ Infective diarrhoeas (rotavirus, giardia lamblia, shigella, salmonella etc) ◦ Constipation/Encopresis ◦ Feeding problems ◦ Faltering growth ◦ Inflammatory bowel disease ◦ Food allergy and intolerance You should also have knowledge of Oral rehydration therapy Practical skills ◦ Abdominal examination ◦ Assess for dehydration Acute abdominal pain Exclude medical causes, in particular: o Lower lobe pneumonia, diabetic ketoacidosis, hepatitis, pyelonephritis/UTI o Check for strangulated inguinal hernia or torsion of the testis in boys o On palpating the abdomen in children with acute appendicitis, guarding and rebound tenderness are often absent or unimpressive, but pain from peritoneal inflammation may be demonstrated on coughing, walking or jumping o To distinguish between acute appendicitis and non-specific abdominal pain may require close monitoring and repeated evaluation in hospital. Acute appendicitis is the commonest cause of abdominal pain requiring surgery and important to catch early due to immature omentum allowing for early perforation • Clinical features: o Central, colicky abdo pain that eventually localizes to right iliac fossa (local peritoneal inflam.) Made worse by movement Paediatrics: Page 28 of 78 o Flushed face with oral fetor o McBurney’s point • Investigations: o No specific lab tests can consistently help, child requires regular clinical review o USS can aid diagnosis (thickened, non-compressible appendix with increased blood flow) May also reveal complications: abscess, perforation, appendix mass o Laproscopy may be available to visualize inflamed appendix • Management: o Uncomplicated appendicitis – Appendectomy o Complicated (abscess, perf’, etc.) – fluid resuss, IV ABx before appendectomy Non-specific abdominal pain and mesenteric adenitis is abdo pain that is less severe than appendicitis and resolves 24-48hr. • Often accompanied with URTI and cervical lymphadenopathy • Mesenteric adenitis can only be diagnosed in those with large mesenteric nodes and normal appendix at laparoscopy ********************************CONTINUED************************************ [Show More]
Last updated: 1 year ago
Preview 1 out of 78 pages
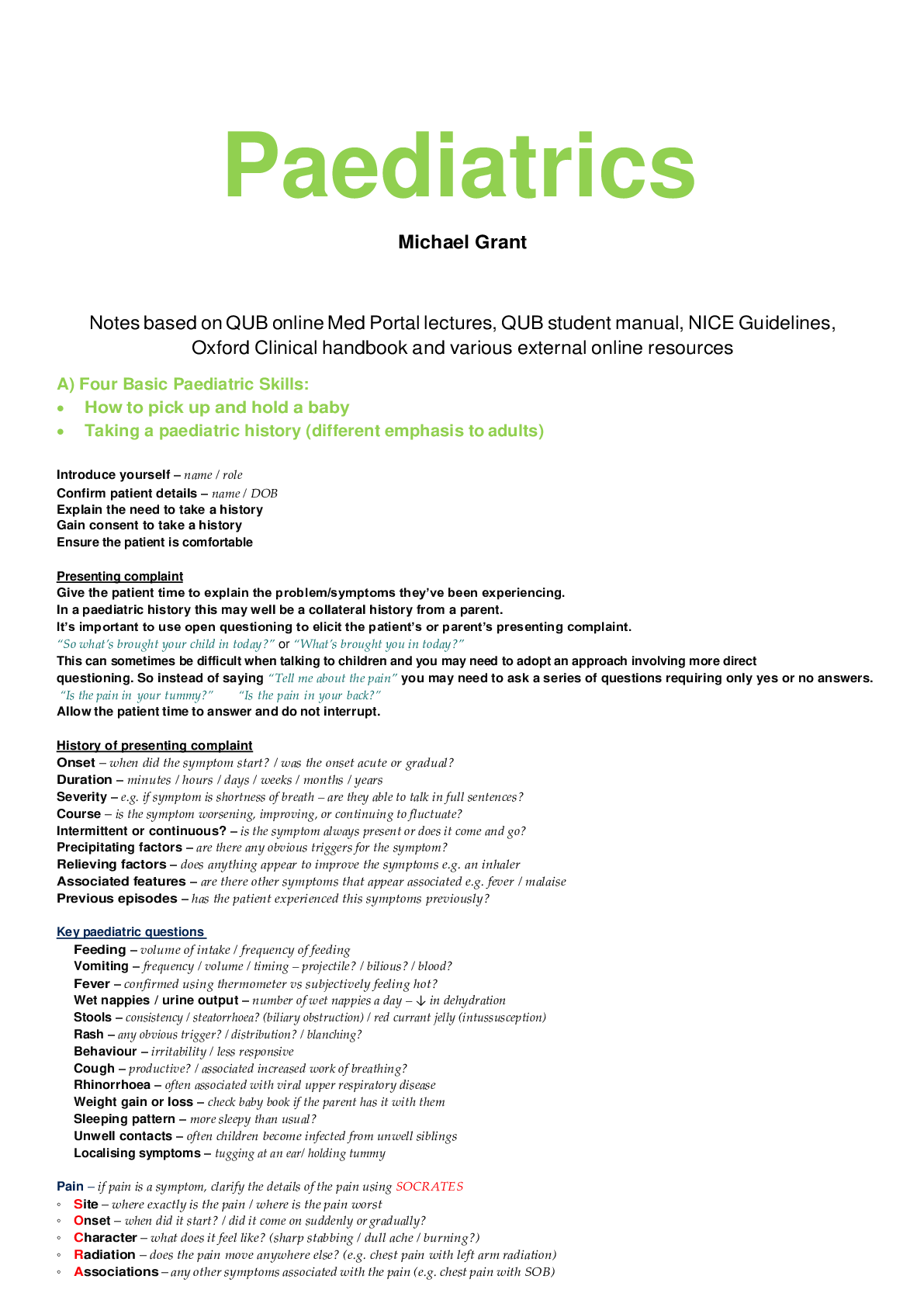
Reviews( 0 )
Recommended For You
Pharmacology> NCLEX-PN > UWorld for Nclex Pharmacology Nursing- Med Surg *Contains main drugs questioned in UWorld and mentioned in MK; Antibiotics, CV drugs, Diuretics, (All)
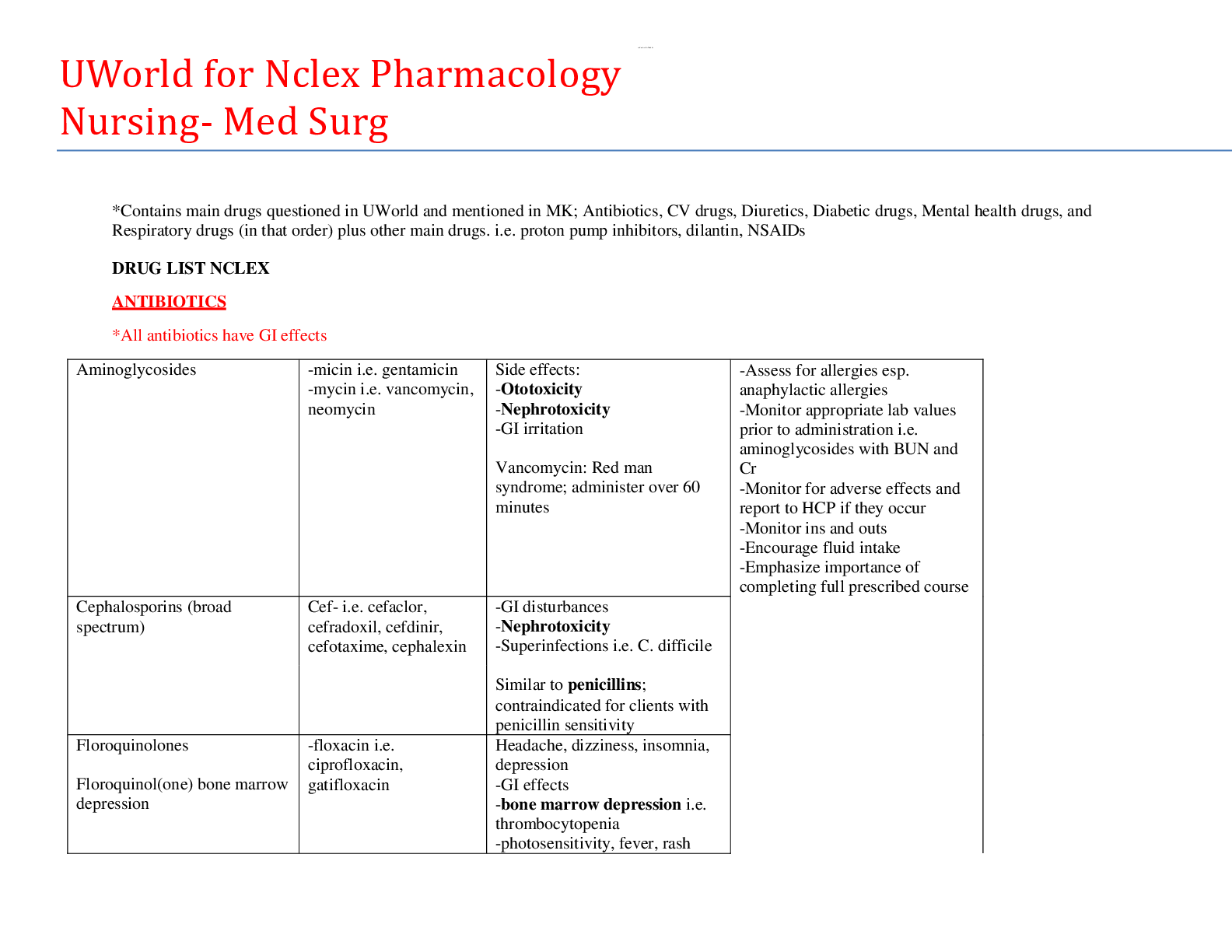
UWorld for Nclex Pharmacology Nursing- Med Surg *Contains main drugs questioned in UWorld and mentioned in MK; Antibiotics, CV drugs, Diuretics,
DRUG LIST NCLEX ANTIBIOTICS *All antibiotics have GI effects CARDIOVASCULAR MEDICATIONS DIURETICS *All diuretics are contraindicated in clients taking lithium! Hyponatremia can induce lithium tox...
By QuizMaster , Uploaded: Sep 02, 2020
$9
*NURSING> NCLEX-PN > NCLEX-PN Test Prep,100% CORRECT (All)
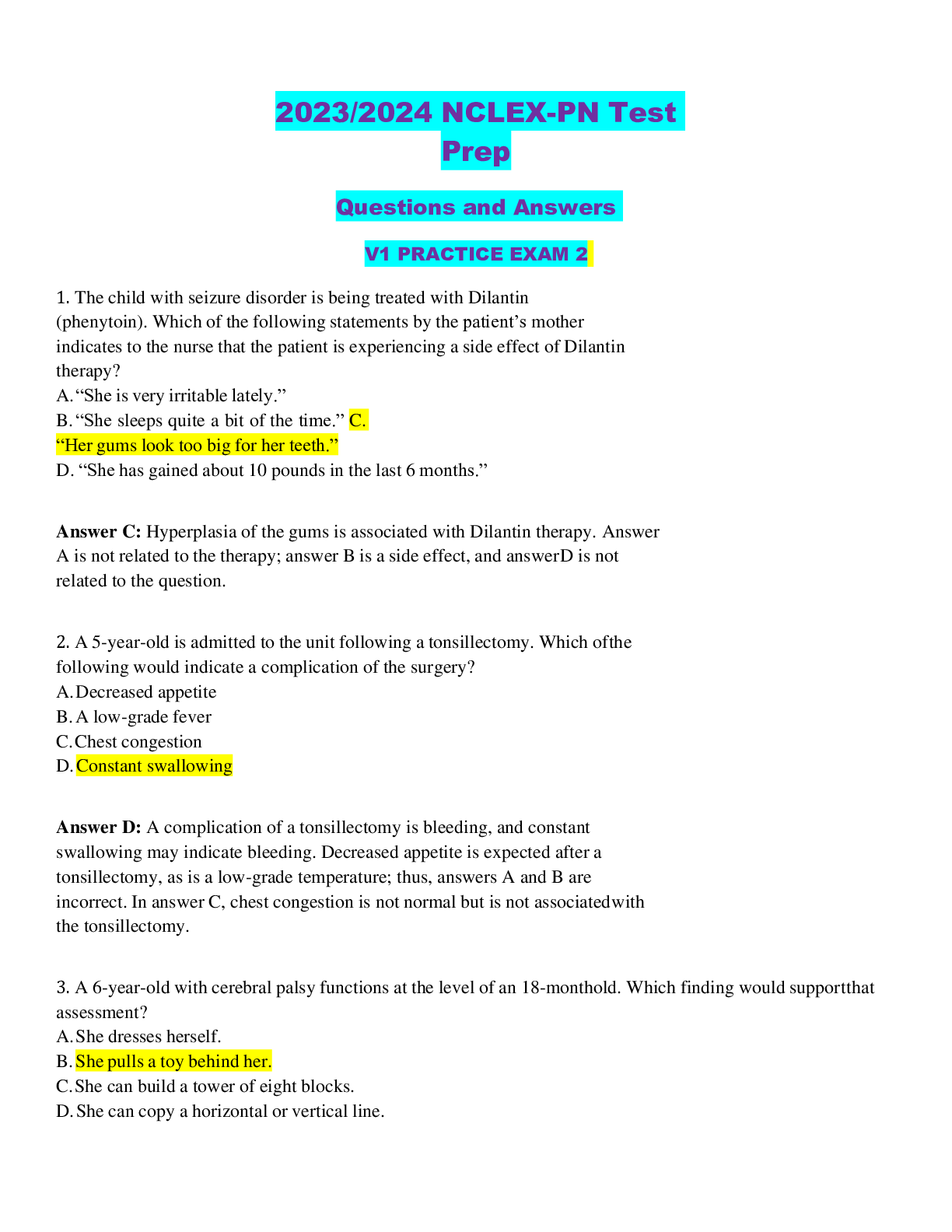
NCLEX-PN Test Prep,100% CORRECT
. The child with seizure disorder is being treated with Dilantin (phenytoin). Which of the following statements by the patient’s mother indicates to the nurse that the patient is experiencing a side...
By securegrades , Uploaded: Sep 03, 2020
$15
*NURSING> NCLEX-PN > SAUNDERS COMPREHENSIVE REVIEW FOR NCLEX FIVE 2020: Best Q&A for Revision and Prefessional Certification Exams. (Contains 1000 Questions and Answers). (All)
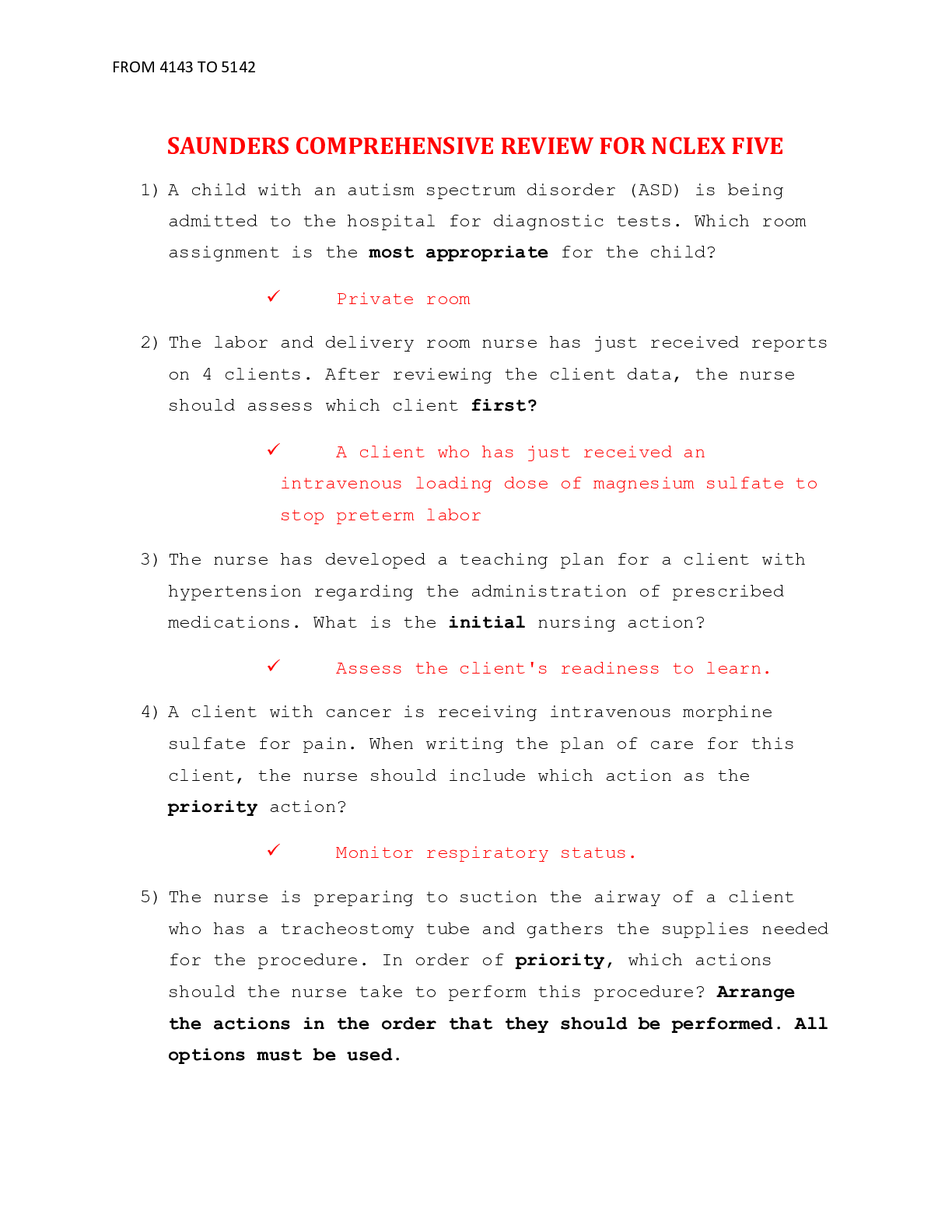
SAUNDERS COMPREHENSIVE REVIEW FOR NCLEX FIVE 2020: Best Q&A for Revision and Prefessional Certification Exams. (Contains 1000 Questions and Answers).
SAUNDERS COMPREHENSIVE REVIEW FOR NCLEX FIVE 1) A child with an autism spectrum disorder (ASD) is being admitted to the hospital for diagnostic tests. Which room assignment is the most appropriate fo...
By QuizMaster , Uploaded: Aug 06, 2020
$9.5
*NURSING> NCLEX-PN > NCLEX-PN Test Prep Questions and Answers with Explanations V4 PRACTICE EXAM 1 (2023/2024) (STUDY MODE) (All)
NCLEX-PN Test Prep Questions and Answers with Explanations V4 PRACTICE EXAM 1 (2023/2024) (STUDY MODE)
2020/2021 NCLEX-PN Test Prep Questions and Answers with Explanations V4 PRACTICE EXAM 1 (STUDY MODE) 1. A client with AIDS asks the nurse why he can’t have a pitcher of water at his bedside so h...
By Bobweiss , Uploaded: Mar 12, 2021
$17
*NURSING> NCLEX-PN > NCLEX-PN Practice Part 1: 25 Questions And Answers Plus Rationales (All)
NCLEX-PN Practice Part 1: 25 Questions And Answers Plus Rationales
NCLEX-PN Practice Part 1: 25 Questions And Answers 1. Question A 4-year old child is brought by her grandmother in the emergency room due to fever, chills, and difficulty walking. The nurse tries to r...
By browseAgrades , Uploaded: Feb 02, 2022
$15
*NURSING> NCLEX-PN > LIPPINCOTT'S FAST FACTS FOR NCLEX-PN (LWW) By LIPPINCOTT WILLIAMS & WILKINS (All)
.png)
LIPPINCOTT'S FAST FACTS FOR NCLEX-PN (LWW) By LIPPINCOTT WILLIAMS & WILKINS
LIPPINCOTT'S FAST FACTS FOR NCLEX-PN (2012, LWW) By LIPPINCOTT WILLIAMS & WILKINS
By Test Bank Store , Uploaded: Oct 26, 2021
$19.5
*NURSING> NCLEX-PN > NCLEX PN Complete Exam- 150 QUESTIONS FROM PREVIOUS ACTUAL EXAMS (All)
NCLEX PN Complete Exam- 150 QUESTIONS FROM PREVIOUS ACTUAL EXAMS
NCLEX PN 2020-QUESTIONS FROM PREVIOUS ACTUAL EXAMSNCLEX PN 2020/2021-QUESTIONS FROM PREVIOUS ACTUAL EXAMS/NCLEX PN 2020/2021-QUESTIONS FROM PREVIOUS ACTUAL EXAMS/NCLEX PN 2020/2021-QUESTIONS FROM PREV...
By CHRIS , Uploaded: Jul 31, 2020
$24.5
*NURSING> NCLEX-PN > NCLEX PN Exam. Contains 205 Highly Tested Comprehensive MCQ for Quick Exam Prep. Rated 100% (All)
NCLEX PN Exam. Contains 205 Highly Tested Comprehensive MCQ for Quick Exam Prep. Rated 100%
NCLEX PN Exam. Contains 205 Highly Tested Comprehensive MCQ for Quick Exam Prep. Rated 100% A 24-year-old female client is scheduled for surgery in the morning. Which of the following is the primar...
By Grade A+ , Uploaded: Jan 25, 2023
$23
*NURSING> NCLEX-PN > PSYCHIATRIC HESI prep - HESI Study guide completed Psychiatric Mental Health Nursing (University of Rhode Island). The Last minute study Materials in 32 pages of information with HESI Hints you MUST know to pass your exam. Below is the content in brief. (All)
PSYCHIATRIC HESI prep - HESI Study guide completed Psychiatric Mental Health Nursing (University of Rhode Island). The Last minute study Materials in 32 pages of information with HESI Hints you MUST know to pass your exam. Below is the content in brief.
Therapeutic Communication A. Purpose of therapeutic interaction w/ pts a. Allow them autonomy to make choices when appropriate B. Keep statements value-free, advice-free, and re-assurance-free C....
By QuizMaster , Uploaded: Sep 01, 2020
$10
*NURSING> NCLEX-PN > NCLEX SATA 1-5. A Complete and Comprehensive Select All That Apply Questions and Answers. (All)
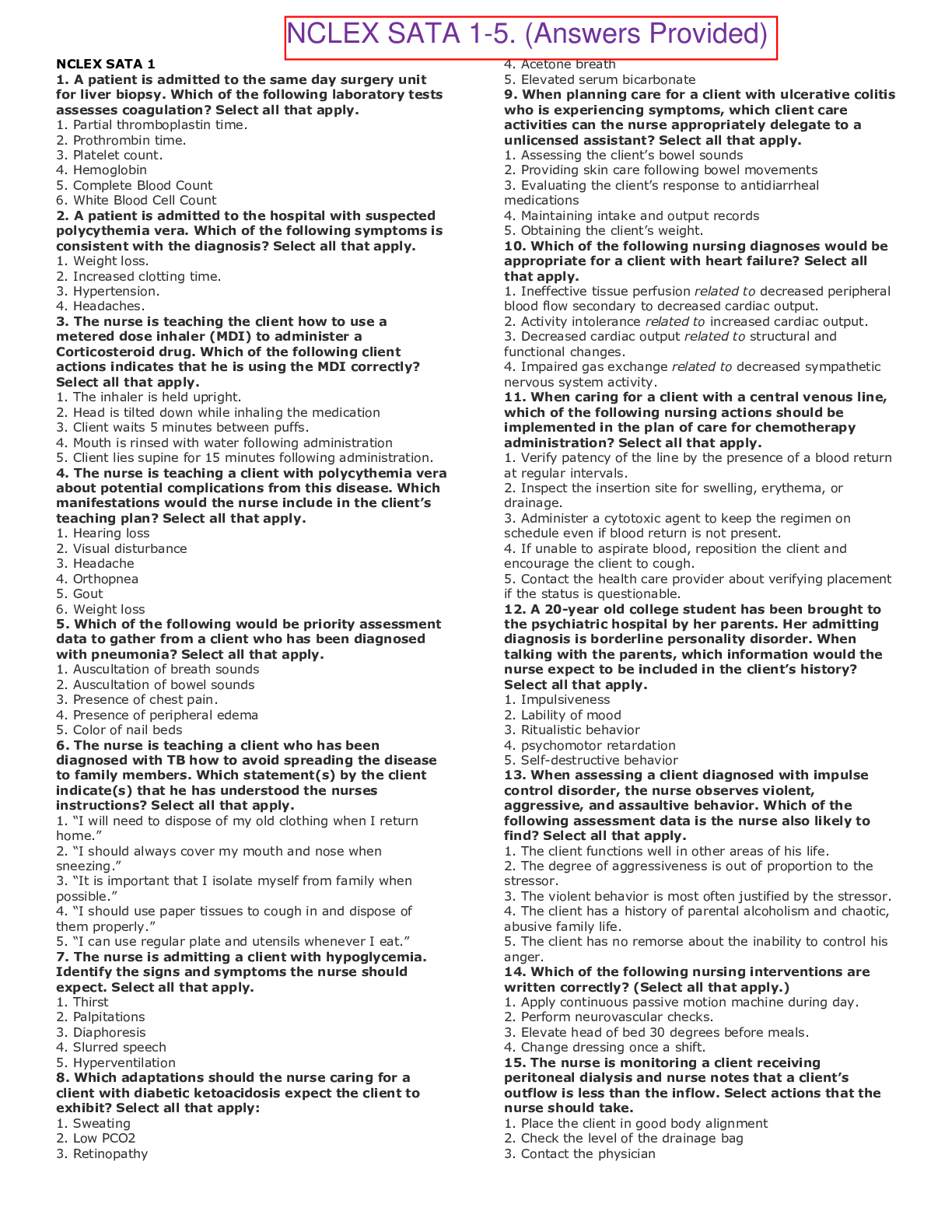
NCLEX SATA 1-5. A Complete and Comprehensive Select All That Apply Questions and Answers.
NCLEX SATA 1-5. A Complete and Comprehensive Select All That Apply Questions and Answers. NCLEX SATA 1 1. A patient is admitted to the same day surgery unit for liver biopsy. Which of the following...
By TESTBANKS , Uploaded: Nov 11, 2021
$11
Document information
Connected school, study & course
About the document
Uploaded On
Sep 03, 2020
Number of pages
78
Written in
Additional information
This document has been written for:
Uploaded
Sep 03, 2020
Downloads
1
Views
328






