Summary NR 509 Week 1 Health History SOAP Note
Document Content and Description Below
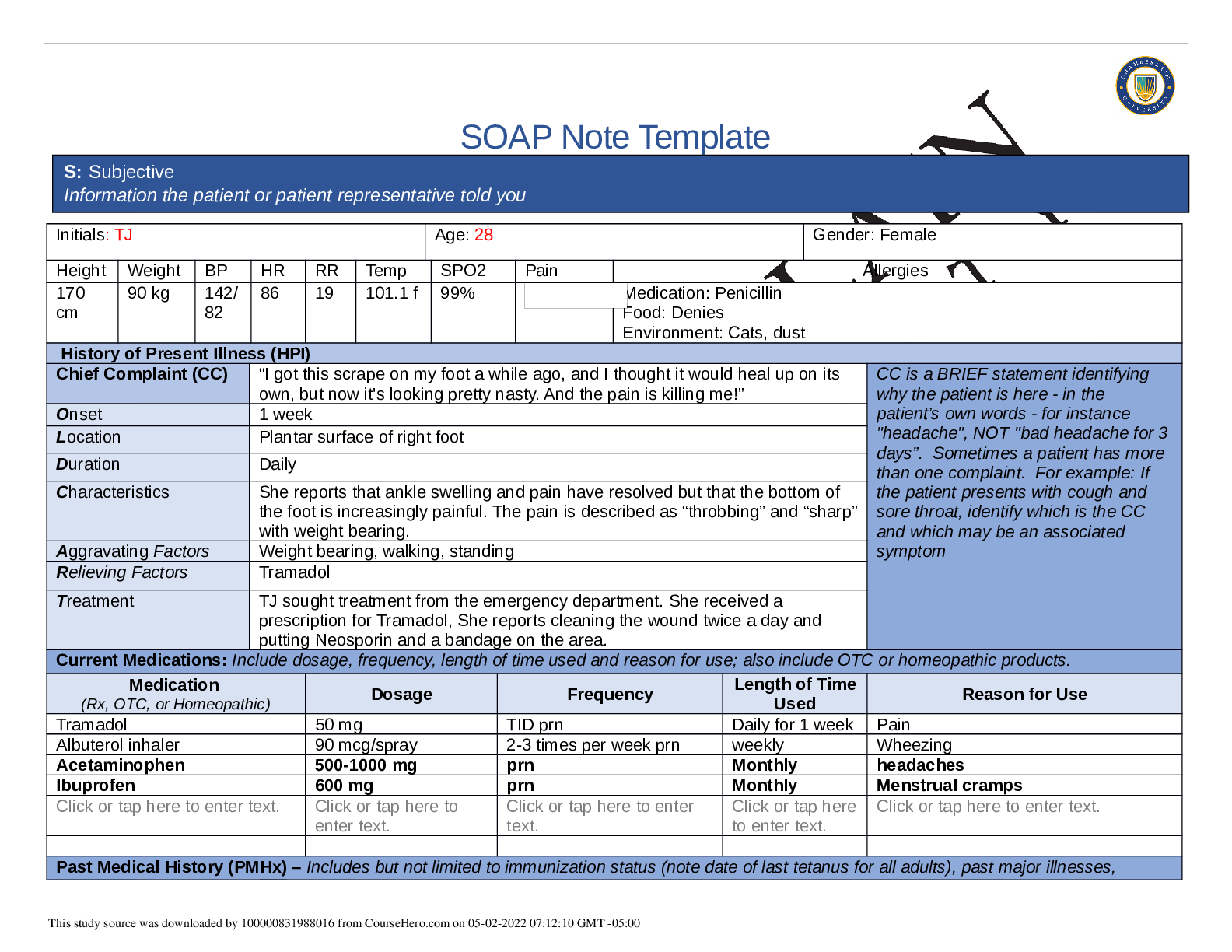
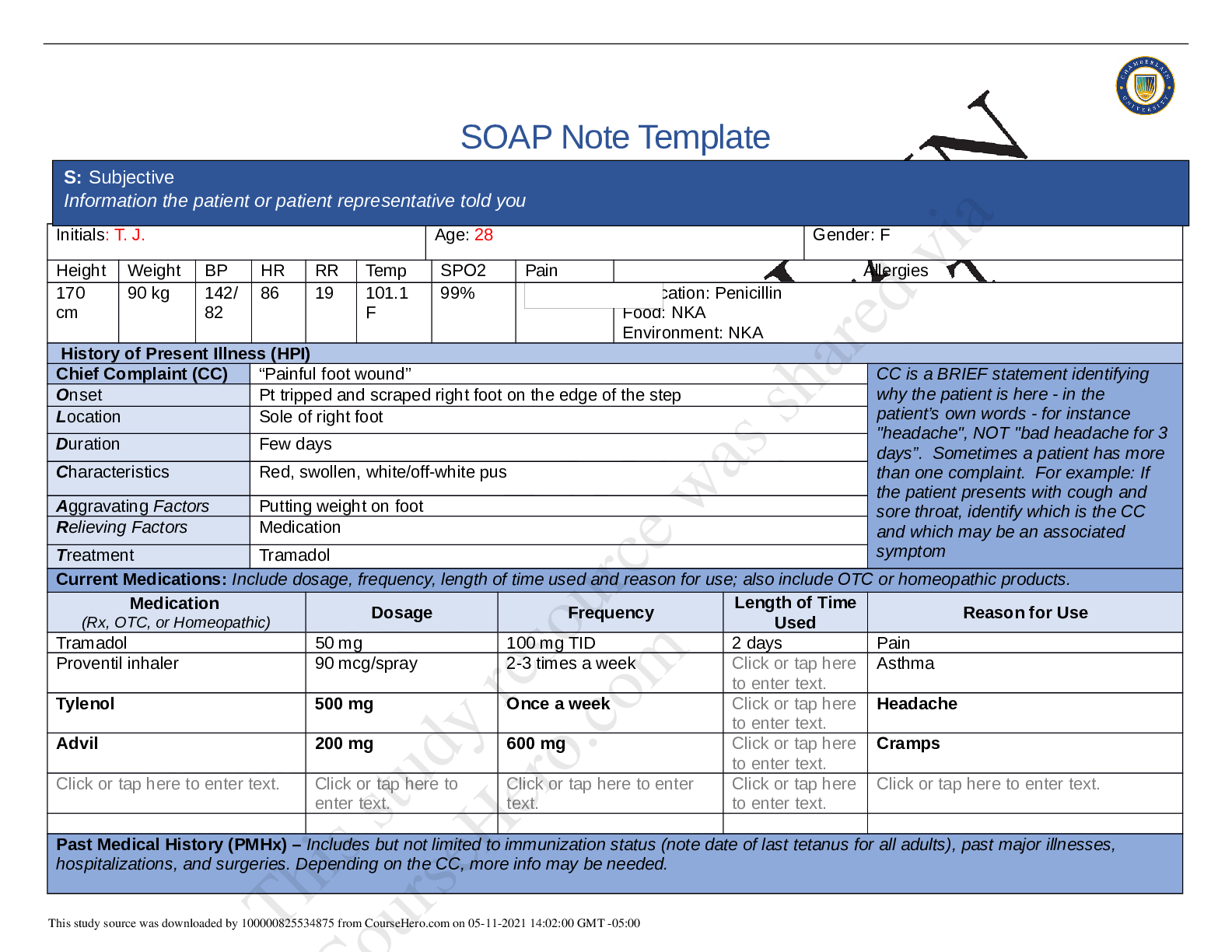
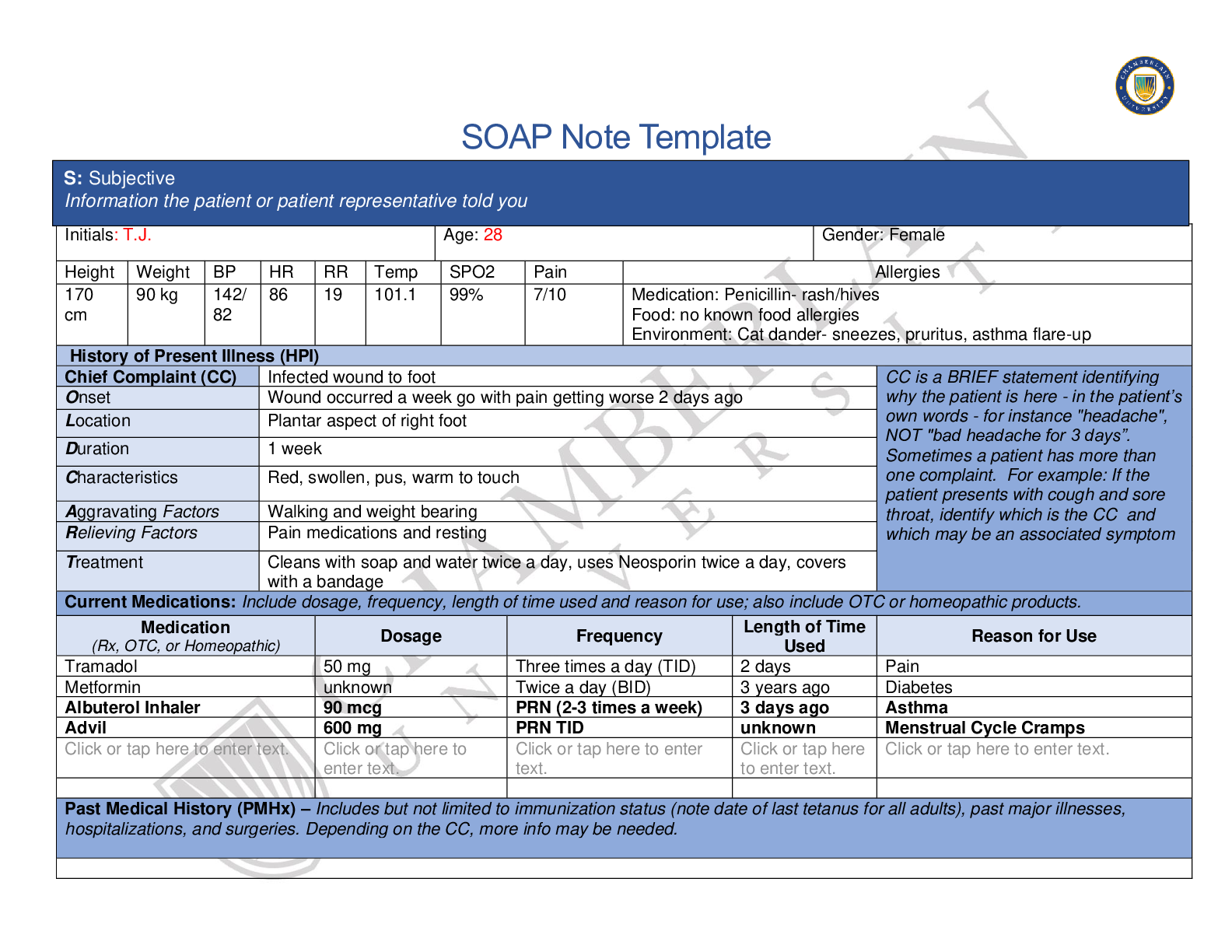
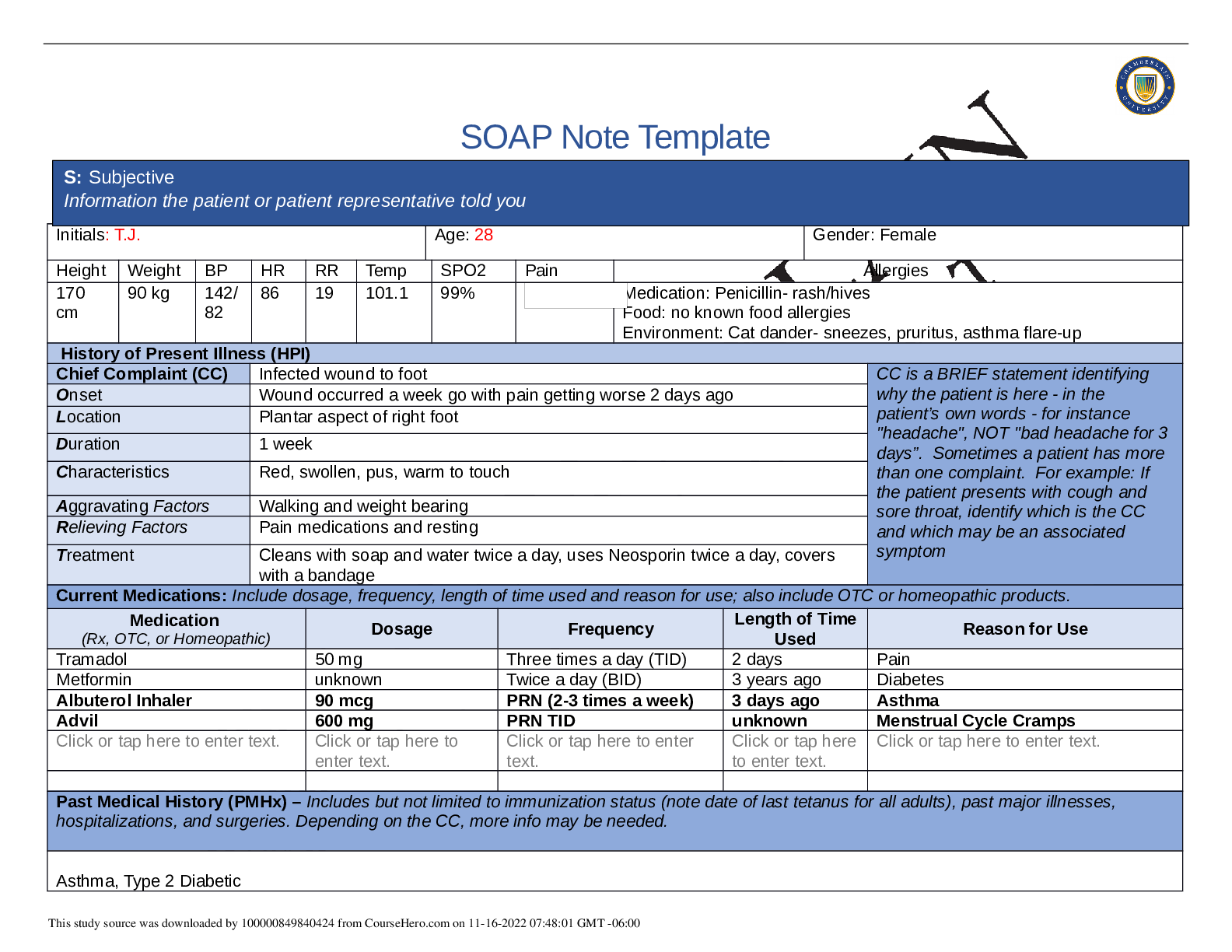
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 90 kg 142/ 82 86 19 101.1 f 99% Medication: Penicillin Food: Denies Environment: ... Cats, dust History of Present Illness (HPI) Chief Complaint (CC) “I got this scrape on my foot a while ago, and I thought it would heal up on its own, but now it's looking pretty nasty. And the pain is killing me!” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset 1 week Location Plantar surface of right foot Duration Daily Characteristics She reports that ankle swelling and pain have resolved but that the bottom of the foot is increasingly painful. The pain is described as “throbbing” and “sharp” with weight bearing. Aggravating Factors Weight bearing, walking, standing Relieving Factors Tramadol Treatment TJ sought treatment from the emergency department. She received a prescription for Tramadol, She reports cleaning the wound twice a day and putting Neosporin and a bandage on the area. Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Tramadol 50 mg TID prn Daily for 1 week Pain Albuterol inhaler 90 mcg/spray 2-3 times per week prn weekly Wheezing Acetaminophen 500-1000 mg prn Monthly headaches Ibuprofen 600 mg prn Monthly Menstrual cramps Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, S: Subjective Information the patient or patient representative told you This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:12:10 GMT -05:00 hospitalizations, and surgeries. Depending on the CC, more info may be needed. Asthma diagnosed at age 2.5, last hospitalized “in high school”, never intubated. Diabetes Mellitus type two, diagnosed age 24. Denies taking medication for Diabetes, denies keeping track of her glucose. Denies surgies. Immunizations: tetanus: within the past year, Influenza: denies, Human paoillomavirus: denies, reports all of her childhood shots are up to date abd she received all shots needed for college. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Never married. No Children. Moved out after high school. Currently lives with mother and sister. Moved back in after father died to help mother. Works at Mid-American Copy and Shipping as a supervisor. 32 hours a week. She is a part time college student; she has 2 semesters left in order to earn her bachelor's degree in accounting. She plans to get a job at an accounting firm after graduation. She has a car and a cell phone. She has health insurance through work but is unsure of what it covers. She likes to go to bar and clubs with her friends. She like to watch tv, spend time with friends, attend bible study, volunteer at church, and dance. She has a strong support system. She generally gets stressed when she has too much to do but currently reports no stressors. Reports smoking marijuana at age 15 until age 21. Denies any other drug use. Reports occasional alcohol consumption 2-3 times per month. Reports only a "few" drinks when she goes out. She denies driving while intoxicated. Reports drinking 4 diet sodas a day. Denies foreign travel. Denies pets. Denies current relationship. Last relationship 2 years ago. Future plans to live independently, have a relationship, family, and job growth. Safety: Has smoke detectors in the house, wears a seat belt, does not ride a bike, occasionally wears sunscreen, gun lucked up in mothers’ room. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. • Mother: age 50, hypertension, elevated cholesterol • Father: deceased in car accident one year ago at age 58, hypertension, high cholesterol, and type 2 diabetes • Brother (Michael, 25): overweight • Sister (Britney, 14): asthma • Maternal grandmother: died at age 73 of a stroke, history of hypertension, high cholesterol • Maternal grandfather: died at age 78 of a stroke, history of hypertension, high cholesterol • Paternal grandmother: still living, age 82, hypertension • Paternal grandfather: died at age 65 of colon cancer, history of type 2 diabetes • Paternal uncle: alcoholism • Negative for mental illness, other cancers, sudden death, kidney disease, sickle cell anemia, thyroid problems Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:12:10 GMT -05:00 Constitutional Skin HEENT ☒Fatigue Click or tap here to enter text. ☐Weakness Click or tap here to enter text. ☒Fever/Chills Click or tap here to enter text. ☐Weight Gain Click or tap here to enter text. ☒Weight Loss 10 pound weight lose ☐Trouble Sleeping Click or tap here to enter text. ☐Night Sweats Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Itching Click or tap here to enter text. ☐Rashes Click or tap here to enter text. ☐Nail Changes Click or tap here to enter text. ☒Skin Color Changes Darkness around neck, facial hair ☐Other: Click or tap here to enter text. ☐Diplopia Click or tap here to enter text. ☐Eye Pain Click or tap here to enter text. ☐Eye redness Click or tap here to enter text. ☒Vision changes Blurred vision ☐Photophobia Click or tap here to enter text. ☐Eye discharge Click or tap here to enter text. ☐Earache Click or tap here to enter text. ☐Tinnitus Click or tap here to enter text. ☐Epistaxis Click or tap here to enter text. ☐Vertigo Click or tap here to enter text. ☐Hearing Changes Click or tap here to enter text. ☐Hoarseness Click or tap here to enter text. ☐Oral Ulcers Click or tap here to enter text. ☐Sore Throat Click or tap here to enter text. ☐Congestion Click or tap here to enter text. ☐Rhinorrhea Click or tap here to enter text. ☐Other: Click or tap here to enter text. Respiratory Neuro Cardiovascular ☒Cough When around cats or dust ☐Hemoptysis Click or tap here to enter text. ☐Dyspnea Click or tap here to enter text. ☒Wheezing When around cats or dust ☐Pain on Inspiration Click or tap here to enter text. ☐Sputum Production ☐Other: Click or tap here to enter text. ☐Syncope or Lightheadedness Click or tap here to enter text. ☐Headache Click or tap here to enter text. ☐Numbness Click or tap here to enter text. ☐Tingling Click or tap here to enter text. ☐Sensation Changes ☐Speech Deficits Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Chest pain Click or tap here to enter text. ☐SOB Click or tap here to enter text. ☒Exercise Intolerance Foot pain ☐Orthopnea Click or tap here to enter text. ☒Edema Right foot ☐Murmurs Click or tap here to enter text. ☐Palpitations Click or tap here to enter text. ☐Faintness Click or tap here to enter text. ☐OC Changes Click or tap here to enter text. ☐Claudications Click or tap here to enter text. ☐PND Click or tap here to enter text. ☐Other: Click or tap here to enter text. This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:12:10 GMT -05:00 MSK GI GU PSYCH ☒Pain Right foot 7/10 ☐Stiffness Click or tap here to enter text. ☐Crepitus Click or tap here to enter text. ☒Swelling Right foot ☒Limited ROM ☒Redness Right foot ☐Misalignment Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Nausea/Vomiting Click or tap here to enter text. ☐Dysphasia Click or tap here to enter text. ☐Diarrhea Click or tap here to enter text. ☒Appetite Change Increased appetite ☐Heartburn Click or tap here to enter text. ☐Blood in Stool Click or tap here to enter text. ☐Abdominal Pain Click or tap here to enter text. ☐Excessive Flatus Click or tap here to enter text. ☐Food Intolerance Click or tap here to enter text. ☐Rectal Bleeding Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Urgency Click or tap here to enter text. ☐Dysuria Click or tap here to enter text. ☐Burning Click or tap here to enter text. ☐Hematuria Click or tap here to enter text. ☐Polyuria Click or tap here to enter text. ☐Nocturia Click or tap here to enter text. ☐Incontinence Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☒Stress School, family ☐Anxiety Click or tap here to enter text. ☐Depression Click or tap here to enter text. ☐Suicidal/Homicidal Ideation Click or tap here to enter text. ☐Memory Deficits Click or tap here to enter text. ☐Mood Changes Click or tap here to enter text. ☐Trouble Concentrating Click or tap here to enter text. ☐Other: Click or tap here to enter text. GYN ☐Rash Click or tap here to enter text. ☒Discharge Right foot ☐Itching Click or tap here to enter text. ☒Irregular Menses Always had, every 6-8 weeks ☒Dysmenorrhea Pain, heavy flow ☐Foul Odor Click or tap here to enter text. ☐Amenorrhea Click or tap here to enter text. ☒LMP: 3 weeks ago ☒Contraception Denies ☐Other:Click or tap here to enter text. O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings. This study source was downloaded by 100000831988016 from CourseHero.com on 05-02-2022 07:12:10 GMT -05:00 Body System Positive Findings Negative Findings General Ms. Jones is alert and oriented, seated upright on the examination table, and is in no apparent distress. She is wellnourished, well-developed, and dressed appropriately with good hygiene. Wound: 2 cm x 1.5 cm, 2.5 mm deep wound, red wound edges, right ball of foot, serosanguinous drainage. Mild erythema surrounding wound, no edema, no tracking Skin Warm, dry, color appropriate, good turgor, no rash noted, no bruising Acanthosis nigricans, facial hair HEENT Head: Normocephalic, atraumatic, no visible or palpable masses, depressions, or scaring. Eyes: conjunctiva clear, sclera non-icteric, EOM [Show More]
Last updated: 1 year ago
Preview 1 out of 8 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > NR-509 Week 7 Comprehensive Health History SOAP Note (All)
NR-509 Week 7 Comprehensive Health History SOAP Note
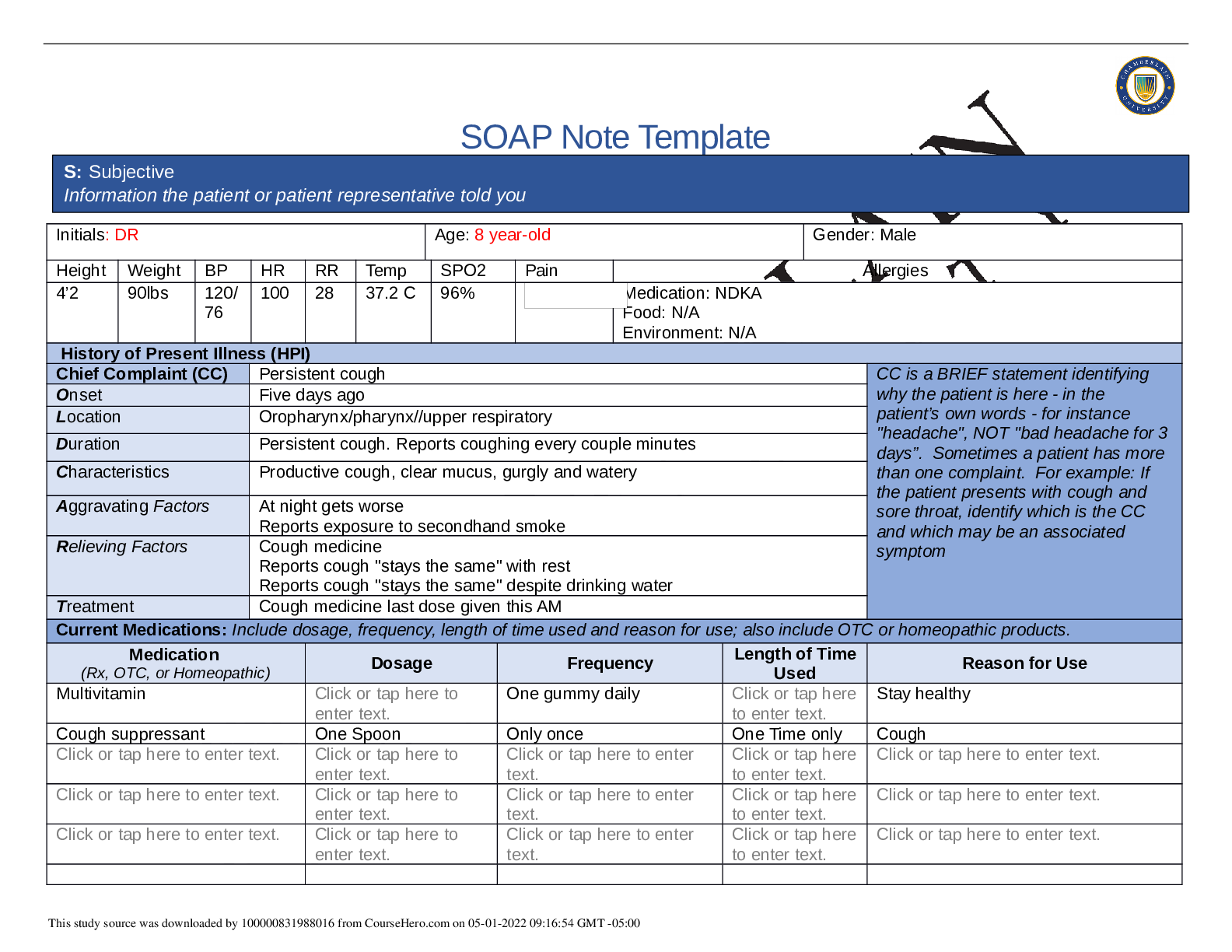
SOAP Note Template Initials: DR Age: 8 year-old Gender: Male Height Weight BP HR RR Temp SPO2 Pain Allergies 4’2 90lbs 120/ 76 100 28 37.2 C 96% Medication: NDKA Food: N/A Environment: N/A Hi...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
NR 509 Week 1 Health History SOAP Note
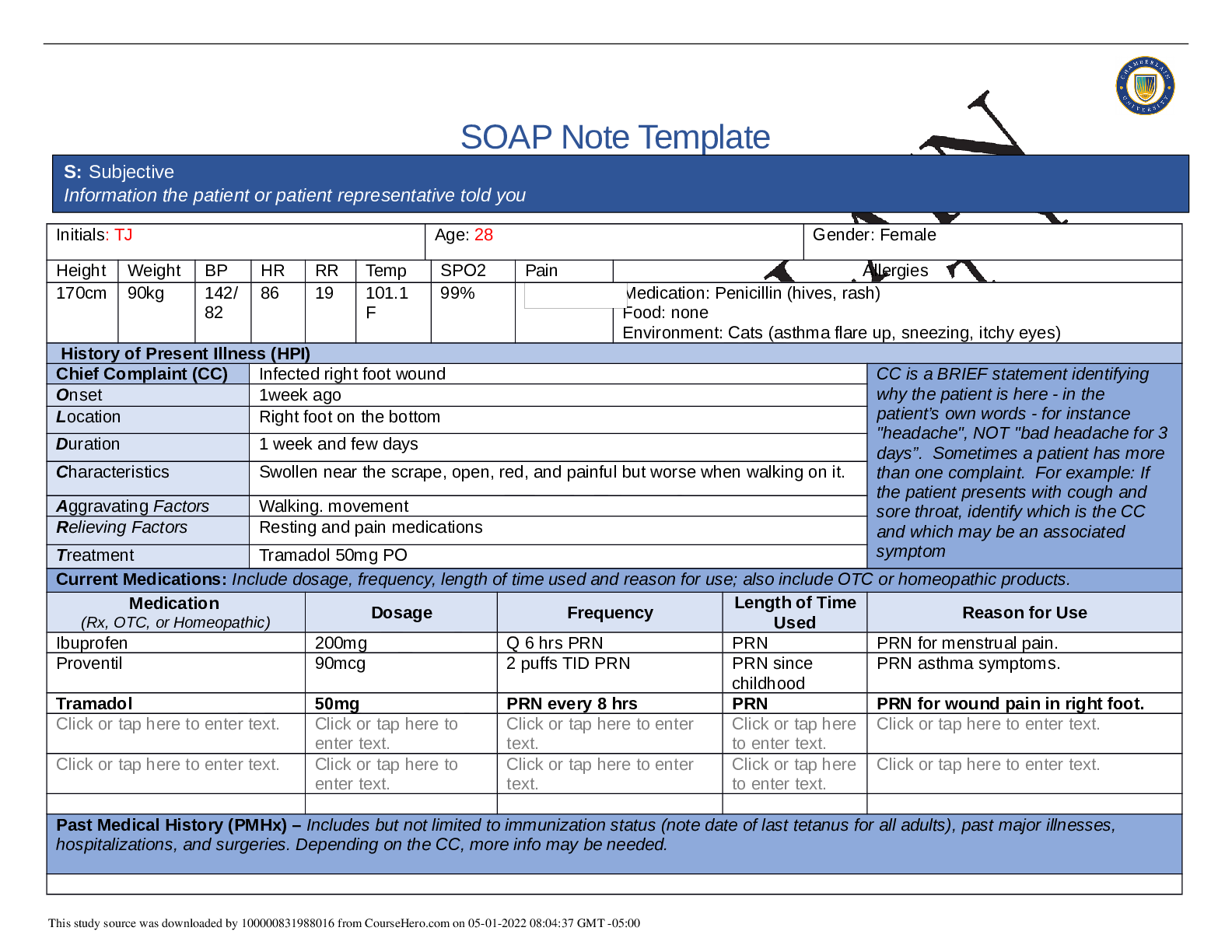
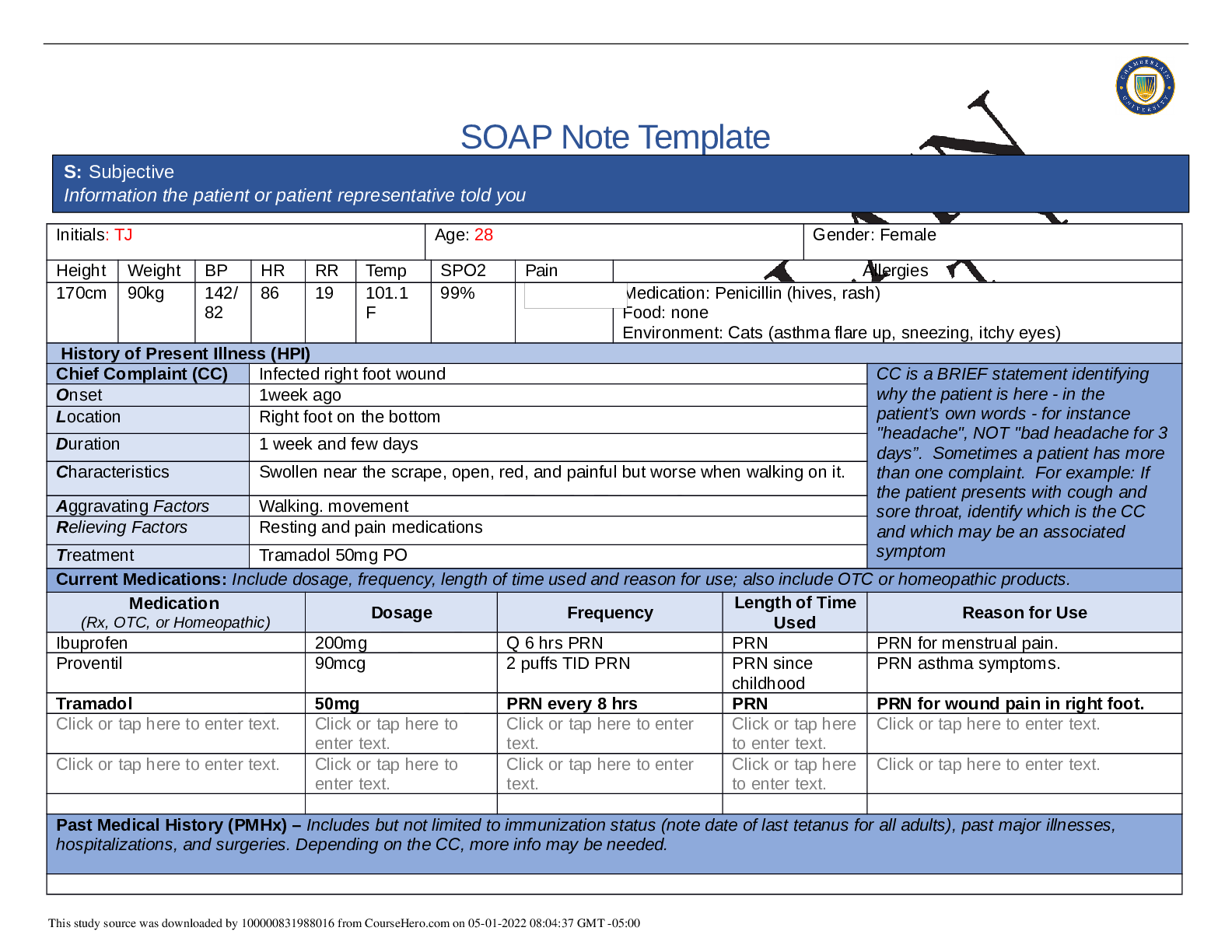
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 90kg 142/ 82 86 19 101.1 F 99% Medication: Penicillin (hives, rash) Food: none Env...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR509 Week 1 SOAP Note – Chamberlain College of Nursing | NR 509 Week 1 SOAP Note – Grade A (All)
NR509 Week 1 SOAP Note – Chamberlain College of Nursing | NR 509 Week 1 SOAP Note – Grade A
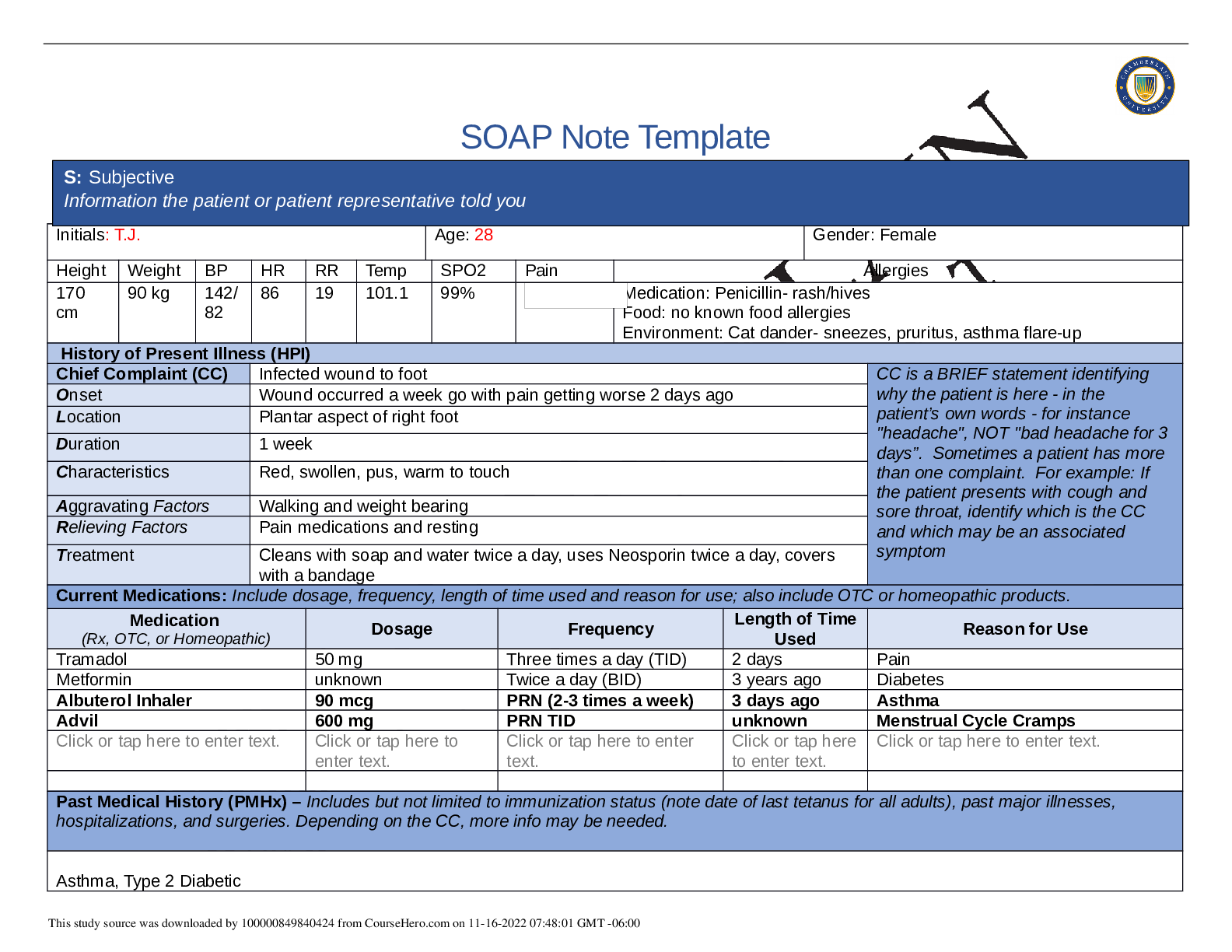
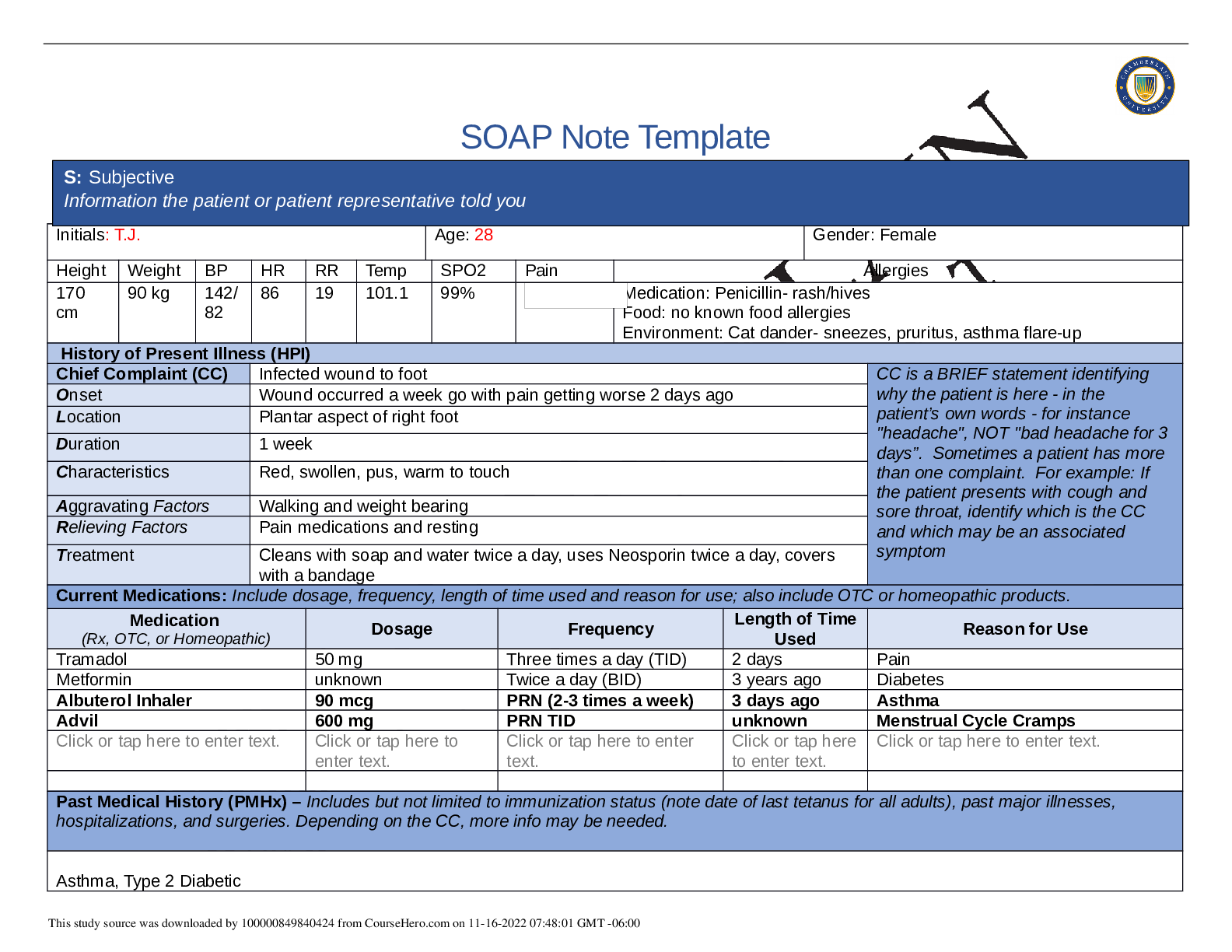
SOAP Note Template Initials: T.J. Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 90 kg 142/ 82 86 19 101.1 99% Medication: Penicillin- rash/hives Food: no known...
By Nutmegs , Uploaded: Apr 11, 2022
$12
Health Care> SOAP NOTE > TINA JONES SOAP Note NR 509 Week 1 Health History S: Subjective – Information the patient or patient representative told you (All)
TINA JONES SOAP Note NR 509 Week 1 Health History S: Subjective – Information the patient or patient representative told you
TINA JONES SOAP Note NR 509 Week 1 Health History S: Subjective – Information the patient or patient representative told youTINA JONES SOAP Note NR 509 Week 1 Health History S: Subjective – Informat...
By STUDY-GUIDENOTES , Uploaded: Apr 29, 2021
$5
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
NR 509 Week 1 Health History SOAP Note
NR 509 SOAP Notes/NR 509 Advanced Physical Assessment/NR 509 SOAP Notes/NR 509 Advanced Physical Assessment/NR 509 SOAP Notes/NR 509 Advanced Physical Assessment/NR 509 SOAP Notes/NR 509 Advanced Phys...
By LAVIE , Uploaded: Apr 18, 2021
$13
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (All)
NR 509 Week 1 Health History SOAP Note
NR 509 Week 1 Health History SOAP Note
By PROF , Uploaded: Feb 19, 2021
$17
*NURSING> SOAP NOTE > NR-509 Week 7 Comprehensive Health History SOAP Note (All)
NR-509 Week 7 Comprehensive Health History SOAP Note
NR-509 Week 7 Comprehensive Health History SOAP Note
By PROF , Uploaded: Feb 19, 2021
$15
*NURSING> SOAP NOTE > NR 509 Coursework Week 1 – 8 - NR 509 Week 1 SOAP NoteS (All)
NR 509 Coursework Week 1 – 8 - NR 509 Week 1 SOAP NoteS
NR 509 Coursework Week 1 – 8 - NR 509 Week 1 SOAP NoteS
By PROF , Uploaded: Feb 01, 2021
$6.5
*NURSING> SOAP NOTE > Summary NR 509 Week 1 Health History SOAP Note (All)

Summary NR 509 Week 1 Health History SOAP Note
NR 509 Week 1 Health History SOAP Note S: Subjective – Information the patient or patient representative told you O: Objective – Information gathered during the physical examination by inspection, pal...
By Quality Suppliers , Uploaded: Nov 04, 2020
$9
*NURSING> SOAP NOTE > NR 509 Week 1 Health History SOAP Note (GRADED A) (All)
NR 509 Week 1 Health History SOAP Note (GRADED A)
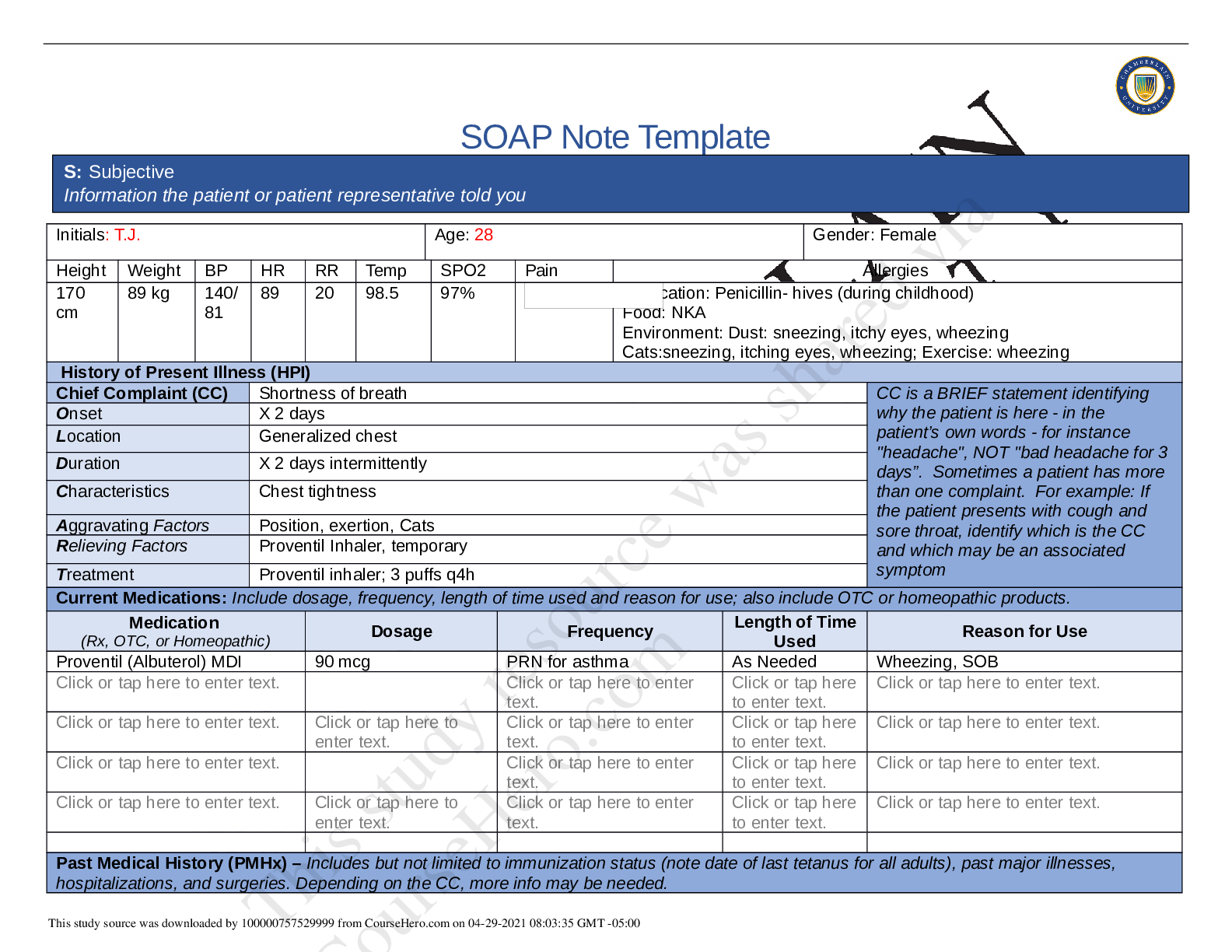
SOAP Note Template S: Subjective Information the patient or patient representative told you Initials: T.J. Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 90 kg 142...
By A+ Solutions , Uploaded: Nov 16, 2022
$12
Document information
Connected school, study & course
About the document
Uploaded On
May 02, 2022
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
May 02, 2022
Downloads
0
Views
86






