*NURSING > EXAM > NHA Billing and Coding practice test (CBCS) 2022-2023 Questions and Answers (latest update) (All)
NHA Billing and Coding practice test (CBCS) 2022-2023 Questions and Answers (latest update)
Document Content and Description Below
NHA Billing and Coding practice test (CBCS) 2022-2023 Questions and Answers (latest update) The attending physician -question to the answer-A nurse is reviewing a patients lab results pri... or to discharge and discovers an elevated glucose level. Which of the following health care providers should be altered before the nurse can proceed with discharge planning? The patients condition and the providers information -question to the answer-On the CMS-1500 Claims for, blocks 14 through 33 contain information about which of the following? Problem focused examination -question to the answer-A provider performs an examination of a patient's throat during an office visit. Which of the following describes the level of the examination? Reinstated or recycled code -question to the answer-The symbol "O" in the Current Procedural Terminology reference is used to indicate which of the following? Coinsurance -question to the answer-Which of the following is the portion of the account balance the patient must pay after services are rendered and the annual deductible is met? Place of service -question to the answer-The billing and coding specialist should divide the evaluation and management code by which of the following? Cardiovascular system -question to the answer-The standard medical abbreviation "ECG" refers to a test used to access which of the following body systems? add on codes -question to the answer-In the anesthesia section of the CPT manual, which of the following are considered qualifying circumstances? 12 -question to the answer-As of April 1st 2014, what is the maximum number of diagnosis that can be reported on the CMS-1500 claim form before a further claim is required? Nephrolithiasis -question to the answer-When submitting a clean claim with a diagnosis of kidney stones, which of the following procedure names is correct? Verifying that the medical records and the billing record match -question to the answer-Which of the following is one of the purposes of an internal auditing program in a physician's office? The DOB is entered incorrectly -question to the answer-Patient: Jane Austin; Social Security # 555-22- 1111; Medicare ID: 555-33-2222A; DOB: 05/22/1945. Claim information entered: Austin, Jane; Social Security #.: 555-22-1111; Medicare ID No.: 555-33-2222A; DOB: 052245. Which of the following is a reason this claim was rejected? Operative report -question to the answer-Which of the following options is considered proper supportive documentation for reporting CPT and ICD codes for surgical procedures? Verify the age of the account -question to the answer-Which of the following actions should be taken first when reviewing delinquent claims? Claim control number -question to the answer-Which of the following components of an explanation of benefits expedites the process of a phone appeal? Bloc 24D contains the diagnosis code -question to the answer-A claim can be denied or rejected for which of the following reasons? Privacy officer -question to the answer-To be compliant with HIPAA, which of the following positions should be assigned in each office? encrypted -question to the answer-All e-mail correspondence to a third party payer containing patients' protected health information (PHI) should be patient ledger account -question to the answer-A billing and coding specialist should understand that the financial record source that is generated by a provider's office is called a Coding compliance plan -question to the answer-Which of the following includes procedures and best practices for correct coding? Health care clearinghouses -question to the answer-HIPAA transaction standards apply to which of the following entities? Appeal the decision with a provider's report -question to the answer-Which of the following actions should be taken if an insurance company denies a service as not medically necessary? Accommodate the request and send the records -question to the answer-A patient with a past due balance requests that his records be sent to another provider. Which of the following actions should be taken? $48 -question to the answer-A participating BlueCross/ BlueShield (BC/BS) provider receives an explanation of benefits for a patient account. The charged amount was $100. BC/BS allowed $40 to the patients annual deductible. BC/BS paid the balance at 80%. How much should the patient expect to pay? Deductible -question to the answer-The physician bills $500 to a patient. After submitting the claim to the insurance company, the claim is sent back with no payment. The patient still owes $500 for this year. International Classification of Disease (ICD) -question to the answer-Which of the following is used to code diseases, injuries, impairments, and other health related problems? Ureters -question to the answer-Urine moves from the kidneys to the bladder through which of the following parts of the body? Angioplasty -question to the answer-Threading a catheter with a balloon into a coronary artery and expanding it to repair arteries describes which of the following procedures? To ensure the patient understands his portion of the bill -question to the answer-A patient's portion of the bill should be discussed with the patient before a procedure is performed for which of the following reasons? Performing periodic audits -question to the answer-Which of the following actions by the billing and coding specialists prevents fraud? Name and address of guarantor -question to the answer-Which of the following information is required on a patient account record? Invalid -question to the answer-A claim is submitted with a transposed insurance member ID number and returned to the provider. Which of the following describes the status that should be assigned to the claim by the carrier? CMS-1500 claim form -question to the answer-Which of the following should the billing and coding specialist complete to be reimbursed for the provider's services? The electronic transmission and code set standards require every provider to use the healthcare transactions, code sets, and identifiers. -question to the answer-Which of the following is HIPAA compliance guideline affecting electronic health records? Verification of coverage. -question to the answer-Which of the following is the purpose of precertification The entity to whom the information is to be released -question to the answer-Which of the following should the billing and coding specialist include in an authorization to release information? Report the incident to a supervisor -question to the answer-Which of the following actions should the billing and coding specialist take if he observes a colleague in an unethical situation? Patient's responsibility -question to the answer-When posting payment accurately, which of the following items should the billing and coding specialist include? The parent whose birthdate comes first in the calendar year -question to the answer-A dependent child whose parents both have insurance coverage comes to the clinic. The billing and coding specialist uses the birthday rule to determine which insurance policy is primary. Which of the following describes the birthday rule? Patient access to psychotherapy notes may be restricted -question to the answer-Which of the following statements is true regarding the release of patient records? Denied -question to the answer-A patient's employer has not submitted a premium payment. Which of the following claim statuses should the provider receive from the third-party payer? Clearinghouse -question to the answer-Which of the following do physicians use to electronically submit claims? principal diagnosis -question to the answer-When coding on the UB-04 form, the billing and coding specialist must sequence the diagnosis codes according to the ICD guidelines. Which of the following is the first listed diagnosis code? Block 9 -question to the answer-A patient has AARP as secondary insurance. In which of the following blocks on the CMS-1500 claim form should this information be entered? NPI -question to the answer-According to HIPAA standards, which of the following identifies the rendering provider on the CMS-1500 claim form in Block 24j? Oxygenating blood cells -question to the answer-Which of the following is the function of the respiratory system? Coordination of benefits -question to the answer-Which of the following provisions ensures that an insured's benefits from all insurance companies do not exceed 100% of allowable medical expenses? Consent agreement -question to the answer-Which of the following is the verbal or written agreement that gives approval to some action, situation, or statement, and allows the release of patient information? Fraud -question to the answer-A deductible of $100 is applied to a patient's remittance advice. The provider requests the account personnel write it off. Which of the following terms describes this scenario? Gross examination -question to the answer-A coroner's autopsy is comprised of which of the following examinations? Claims are expedited -question to the answer-Which of the following is the advantage of electronic claim submission? Title 2 -question to the answer-A patient presents to the provider with chest pain and SOB. After an unexpected ECG result, the provider calls a cardiologist and summarizes the patient's symptoms. What portion of HIPAA allows the provider to speak to the cardiologist prior to obtaining the patient's consent? Advanced beneficiary notice -question to the answer-A physician ordered a comprehensive metabolic panel for a 70 year old patient who has Medicare as her primary insurance. Which of the following forms is required so the patient knows she may be responsible for payment? Assignment of benefits -question to the answer-Which of the following does a patient sign to allow payment of claims directly to the provider? Military identification -question to the answer-All dependents 10 year of age or older are required to have which of the following for TRICARE? Private 3rd party payers -question to the answer-Medigap coverage is offered to Medicare beneficiaries by which of the following? Follow up of insurance claims by date -question to the answer-An insurance claims register (aged insurance report) facilitates which of the following? Urethratresia -question to the answer-Which of the following describes an obstruction of the urethra? Admitting clerk -question to the answer-A patient comes to the hospital for an inpatient procedure. Which of the following hospital staff members is responsible for the initial patient interview, obtaining demographic and insurance information, and documenting the chief complaint? The patient demographics -question to the answer-On the CMS-1500 claim form, Blocks 1 through 13 include which of the following Pumping blood in the circulatory system -question to the answer-Which of the following is the primary function of the heart? Submit an appeal to the carrier with the supporting documentation -question to the answer-Which of the following actions should be taken when a claim is billed for a level four office visit and paid at a level three? Delinquent -question to the answer-Which of the following types of claims is 120 days old? Aging report -question to the answer-Which of the following shows outstanding balances? Part D -question to the answer-Which part of Medicare covers prescriptions? Dermatology -question to the answer-In which of the following departments should a patient be seen for psoriasis? Patient information was disclosed to the patient's parent without consent. -question to the answer- Which of the following is an example of a violation of an adult patient's confidentiality? Improper code combinations -question to the answer-Which of the following describes the reason for a claim rejection because of Medicare NCCI edits? History and physical -question to the answer-Which of the following sections of the medical record is used to determine the correct Evaluation and Management code used for billing and coding? Blue shield/ Blue cross -question to the answer-Which of the following is a private insurance carrier? National provider identification number -question to the answer-Which of the following information should the billing and coding specialist input into Block 33a on the CMS-1500 claim form? UB-04 -question to the answer-Which of the following forms should the billing and coding specialist transmit to the insurance carrier for reimbursement of inpatient hospital services? Pulmonary oncologist -question to the answer-A patient who has a primary malignant neoplasm of the lung should be referred to which of the following specialists? They streamline patient billing by summarizing the services rendered for a given date of service - question to the answer-Why does correct claim processing rely on accurately completed encounter forms? Sagittal -question to the answer-Which of the following planes divides the body into left and right? Inform the patient of the reason of the denial -question to the answer-A patient is upset about a bill she received. Her insurance company denied the claim. Which of the following actions is an appropriate way to handle the situation? The claim is overdue for payment -question to the answer-Which of the following describes a delinquent claim? Use Arial size 10 font -question to the answer-When completing a CMS-1500 paper claim form, which of the following is an acceptable action for the billing and coding specialist to take? Pericardium -question to the answer-Which of the following medical terms refers to the sac that encloses the heart? Adjudication -question to the answer-Which of the following is considered the final determination of the issues involving settlement of an insurance claim? Encounter form -question to the answer-A form that contains charges, DOS, CPT codes, ICD codes, fees, and copayment information is called which of the following? Using data encryption software on office workstations -question to the answer-Which of the following privacy measures ensures protected health information (PHI)? It indicates which claims are outstanding -question to the answer-Which of the following is the purpose of running an aging report each month? Billing for services not provided -question to the answer-Which of the following actions by a billing and coding specialist would be considered fraud? Paper claim -question to the answer-Which of the following claims is submitted and then optically scanned by the insurance carrier and converted to an electronic form? Block 12 -question to the answer-Which of the following blocks requires the patient's authorization to release medical information to process a claim? Block 24D -question to the answer-Which of the following blocks should the billing and coding specialist complete on the CMS-1500 claim form for procedures, services, or supplies? Guidelines prior to each section -question to the answer-The unlisted codes can be found in which of the following locations in the CPT manual? $40 -question to the answer-A physician is contracted with an insurance company to accept the allowed amount. The insurance company allows $80 of a $120 billed amount, and $50 of the deductible has been met. How much should the physician write off the patient's account? Provider -question to the answer-On a remittance advice form, which of the following is responsible for writing off the difference between the amount billed and the amount allowed by the agreement? Procedure descriptors -question to the answer-The "><" symbol is used to indicate new and revised text other than which of the following? The claim requires an attachment -question to the answer-Which of the following indicates a claim should be submitted on paper instead of electronically? Coinsurance -question to the answer-Which of the following terms describes when a plan pays 70% of the allowed amount and the patient pays 30%? The number is needed to identify the provider -question to the answer-Claims that are submitted without an NPI number will delay payment to the provider because UB-04 claim form -question to the answer-Ambulatory surgery centers, home health care, and hospice organizations use the Red -question to the answer-Which of the following color formats is acceptable on the CMS-1500 claim form? The deductible is the patient's responsibility -question to the answer-Which of the following statements is correct regarding a deductible? Adjustment column of the credits -question to the answer-A provider charged $500 to a claim that had an allowable amount of $400. In which of the following columns should the billing and coding specialist apply the non-allowed charge? The billing and coding specialist sends the patient's records to the patient's partner. -question to the answer-A patient who is an active member of the military recently returned from overseas and is in need of specialty care. The patient does not have anyone designated with power of attorney. Which of the following is considered a HIPAA violation? Medicaid -question to the answer-A patient's health plan is referred to as the "payer of last resort." The patient is covered by which of the following health plans? Claim adjudication -question to the answer-After a 3rd party payer validates a claim, which of the following takes place next? Health care clearinghouse -question to the answer-HIPAA transaction standards apply to which of the following entities? First report of injury -question to the answer-Which of the following is the initial step in processing a workers' compensation claim? Coordination of benefits -question to the answer-The provision of health insurance policies that specifies which coverage is considered primary or secondary is called which of the following? A provider's office with fewer than 10 full-time employees -question to the answer-Medicare enforces mandatory submission of electronic claims for most providers. Which of the following providers is allowed to submit paper claims to medicare? The 3rd party payer reimburses the patient, and the patient is responsible for reimbursing the provider. -question to the answer-When submitting claims, which of the following is the outcome if block 13 is left blank? accounts receivable -question to the answer-Patient charges that have not been paid will appear in which of the following? Remittance advice -question to the answer-A billing and coding specialist needs to know how much Medicare paid on a claim before billing secondary insurance. To which of the following should the specialist refer? A bilateral procedure -question to the answer-A billing and coding specialist should add modifier -50 to codes when reporting which of the following? CMS -question to the answer-In 1995 and 1997, which of the following introduced documentation guidelines to Medicare carriers to ensure that services paid for have been provided and were medically necessary? Billing using 2 digit CPT modifiers to indicate a procedure as performed differs from its usual 5 digit code -question to the answer-Which of the following is allowed when billing procedural codes? Cold treatment -question to the answer-The destruction of lesions using cryosurgery would use which of the following treatments? Code both acute and chronic sequencing the acute first -question to the answer-When a patient has a condition that is both acute and chronic how should it be reported? An overview of the practice's outstanding claims -question to the answer-Which of the following describes the content of a medical practice aging report? Fraud -question to the answer-After reading a provider's notes about a new patient, a coding specialist decides to code for a longer length of time than the actual office visit. Which of the following describes the specialist's action? The claim will not be re submitted and the patient will be sent a bill -question to the answer-A claim is denied because the service was not covered by the insurance company. Upon confirmation of no errors on the claim, which of the following describes the process that will follow the denial? A billing worksheet from the patient account -question to the answer-A prospective billing account audit prevents fraud by reviewing and comparing a completed claim form with which of the following documents? Encryption -question to the answer-Which of the following security features is required during transmission of protected health information and medical claims to third party payers? HIPAA -question to the answer-Which of the following acts applies to the Administrative Simplification guidelines? Immunizations -question to the answer-Z codes are used to identify which of the following? -53 -question to the answer-Which of the following modifiers should be used to indicate a professional service has been discontinued prior to completion? Complete the information and re transmit according to the 3rd party standards -question to the answer- When an electronic claim is rejected due to incomplete information, which of the following should the medical billing specialist take? Claims submitted via a secure network -question to the answer-Which of the following is an example of electronic claim submission? EEG -question to the answer-Test results indicated that no abnormalities were found in the brain and the brain's electrical activity patterns are normal. Which of the following tests was used to conduct this exam? 9a -question to the answer-When billing a secondary insurance company, which block should the billing and coding specialist fill out on the CMS-1500 claim form? Collect copayment from the patient at the time of service -question to the answer-Which of the following actions should the billing and coding specialist take to effectively manage accounts receivable? 12 -question to the answer-What is the maximum number of ICD codes that can be entered on a CMS- 1500 claim form as of February 2012? Internal monitoring and audting -question to the answer-Which of the following actions should the billing and coding specialist take to prevent fraud and abuse in the medical office? 30 days -question to the answer-For which of the following time periods should the billing and coding specialist track unpaid claims before taking follow up action 0% -question to the answer-A beneficiary of a Medicare/Medicaid crossover claim submitted by a participating provider is responsible for which of the following percentages? Direct data entry -question to the answer-A biller will electronically submit a claim to the carrier via which of the following? Review of systems -question to the answer-When a physician documents a patient's response to symptoms and various body systems, the results are documented as which of the following? 150 00 -question to the answer-Which of the following is a correct entry of a charge of $140 in Block 24F of the CMS-1500 claim form? Services rendered by a physician whose opinion or advice is requested by another physician or agency - question to the answer-Which of the following situations constitutes a consultation? Bones and bone marrow -question to the answer-If a patient has osteomyelitis he has a problem with which of the following areas? An authorization -question to the answer-Which of the following forms must the patient or representative sign to allow the release of protected health information? Referring physician's national provider identifier (NPI) number -question to the answer-Block 17b on the CMS-1500 claim form should list which of the following information? NCCI -question to the answer-Which of the following was developed to reduce Medicare program expenditures by detecting inappropriate codes and eliminating improper coding practices? Denied -question to the answer-Which of the following describes the status of a claim that does not include required preauthorization for a service? Lymphatic system -question to the answer-Which of the following parts of the body system regulates immunity? Clearinghouse -question to the answer-Which of the following is used by providers to remove errors from claims before they are submitted to 3rd party payers? Explanation of benefits -question to the answer-A provider receives reimbursement from a 3rd party payer accompanied by which of the following documents? Claims adjudication -question to the answer-Which of the following is the 3rd stage of the life cycle of a claim? Block 10a -question to the answer-Which of the following blocks on the CMS-1500 claim form is required to indicate a workers' compensation claim? Duplication of services -question to the answer-2 providers from the same practice visit a patient in the emergency department using the same CPT code. The claim may be denied due to which of the following reasons? The patient was out of town during the emergency -question to the answer-A patient has an emergency appendectomy while on vacation. The claim is rejected due to the patient obtaining services out of network. Which of the following information should be included in the claim appeal? Incomplete claim -question to the answer-Which of the following is a type of claim that will be denied by the 3rd party payer? Internal monitoring and auditing -question to the answer-Which of the following steps would be part of a physician's practice compliance program? $120 -question to the answer-A patient has met a Medicare deductible of $150. The patient's coinsurance is 20% and the allowed amount is $600. Which of the following is the patient's out of pocket expense? The age of the account -question to the answer-Which of the following is the primary information used to determine the priority of collection letters to patients? A claim that is delinquent for 60 days -question to the answer-Which of the following claims would appear on an aging report? Preauthorization form -question to the answer-Which of the following is a requirement of some 3rd party payers before a procedure is performed? HCPCS Level 2 manual -question to the answer-Which of the following coding manuals is used primarily to identify products, supplies, and services? Block 23 -question to the answer-A billing and coding specialist should enter the prior authorization number on the CMS-1500 claim form in which of the following blocks? A signed release from the patient -question to the answer-Which of the following documents is required to disclose an adult patient's information? Documenting the patient's chief complaint, history, exam, assessment, and plan for care -question to the answer-Which of the following billing patterns is a best practice action? Communicating with the front desk staff during a team meeting about missing information in patient files -question to the answer-Behavior plays an important part of being a team player in a medical practice. which of the following is an appropriate action for the billing and coding specialist to take? $40 -question to the answer-A physician is contracted with an insurance company to accept the allowed amount. The insurance company allows $80 of a $120 billed amount, and $50 of the deductible has not been met. How much should the physician write off the patient's account? The physician agrees to accept payment under the terms of the payer's program -question to the answer-Accepting assignment on the CMS-1500 claim form indicates which of the following? Any coinsurance, copayments, or deductibles can be collected from the patient -question to the answer- Which of the following statements is true when determining patient financial responsibility by reviewing the remittance advice? Patient account record -question to the answer-In an outpatient setting, which of the following forms is used as a financial report of all services provided to patients? Edema -question to the answer-Which of the following is the appropriate diagnosis for a patient who has an abnormal accumulation of fluid in her lower leg that has resulted in swelling? TRICARE Prime -question to the answer-Which of the following types of health insurance plans best describes a government sponsored benefit program? Recovery Audit Contractor (RAC) -question to the answer-Which of the following organizations identifies improper payments made on CMS claims? The reason Medicare may not pay -question to the answer-Which of the following information is required to include on an Advance Beneficiary Notice (ABN) form? Block 21 -question to the answer-Which of the following blocks on CMS-1500 claim form is used to bill ICD codes? Claim adjustment codes -question to the answer-Which of the following terms is used to communicate why a claim line item was denied or payed differently than it was billed? The name, address, and ZIP code of the facility where services were rendered goes in this block. - question to the answer-Block 32con the CMS form contains what? -question to the answer-A provider's office requests a subpoena requesting medical documentation from a patient's medical record. After confirming the correct authorization, which of the following actions should the billing & coding specialist take? 12 months from the date of service -question to the answer-Which of the following is the deadline for a Medicare for claims submission? CMS-1500 -question to the answer-Which of the following forms does a 3rd party payer require for physician services? Charging excessive fees -question to the answer-Which of the following is an example of Medicare abuse? Adjustment -question to the answer-Which of the following terms refers to the difference between the billed and allowed amounts? Durable medical equipment -question to the answer-Which of the following HMO managed care services requires a referral? Advanced beneficiary notice (ABN) -question to the answer-Which of the following explains why Medicare will deny a particular service or procedure? Delinquent -question to the answer-What type of claim is 120 days old? Photo copy both sides of the card -question to the answer-When reviewing an established patient's insurance card, the billing and specialist notices a minor change from the existing card on file. Which of the following actions should the billing & coding specialist take? The wife's insurance -question to the answer-A husband and wife each have group insurance through their employers. The wife has an appt. with her provider. Which insurance should be used as the primary for this appt? An experimental chemotherapy medication for a patient who has stage 3 renal cancer. -question to the answer-Which of the following would most likely result in a denial on a Medicare claim? Phone number -question to the answer-Which of the following pieces of guarantor information is required when establishing a patient's financial record? Pleurocentesis -question to the answer-A provider surgically punctures through space between the patient's ribs using an aspirating needle to withdraw fluid from the chest cavity. Which of the following is the name of this procedure? Block 9 -question to the answer-A patient has AARP as secondary insurance. Which block on the CMS 1500 claim form should this information be entered? $230 -question to the answer-A medicare non-participating provider's approved payment for $200 for a lobectomy and the deductible was met. Which amounts is the limiting charge for this? add-on codes -question to the answer-In the anesthesia section of the CPT manual, which are considered qualifying circumstances? These codes must correspond to the diagnosis blocker in Block 24E -question to the answer-Which of the following statements is accurate regarding the diagnostic codes in Block 21? Part C -question to the answer-Which of the following parts of Medicare insurance program is managed by private 3rd party insurance providers that have been approved by medicare? Precertification -question to the answer-A billing & coding specialist can ensure appropriate insurance coverage for an outpatient procedure by 1st using which of the following processes? The billing and coding specialist unbundles a code to receive higher reimbursement -question to the answer-Which of the following is considered fraud? Triangle -question to the answer-Which of the following symbols indicates a revised code? Office inspector general (OIG) -question to the answer-Which of the following entities defines the essential elements of a comprehensive compliance program? Prevent multiple insurers from paying benefits covered by other policies -question to the answer-Which of the following is the purpose of coordination of benefits? Clean claim -question to the answer-A billing & coding specialist submitted a claim to Medicare electronically. No errors were found by the billing software or clearinghouse. Which of the following describes the claim? An italicized code used as the first listed diagnosis -question to the answer-Which of the following would result in a claim being denied? HIPAA standard transactions -question to the answer-Which of the following standardized formats are used in the electronic filing of claims? professional component -question to the answer-Which of the following describes a 2 digit CPT code used to indicate that the provider supervised & interpreted a radiology procedure? 837 -question to the answer-Which of the following formats are used to submit electronic claims to a 3rd party payer? Patient eligibility is determined monthly -question to the answer-Which of the following is true regarding Medicaid? 4 -question to the answer-Which of the following is the maximum # of modifiers that the billing & coding specialists can use on a CMS-1500 claim form in Block 24D? Ensure proper payment has been made -question to the answer-When the remittance advice is sent from the 3rd party payer to the provider, which of the following actions should the billing and coding specialists perform first? Incorrectly linked codes -question to the answer-Which of the following would be a reason a claim would be denied? The guidelines define items that are necessary to accurately code -question to the answer-The billing and coding specialists should follow the guidelines in the CPT manual for which of the following reasons? operative report -question to the answer-Which of the following options is considered proper supportive documentation for reporting CPT & ICD codes for surgical procedures? Block 27 -question to the answer-Which of the following blocks on the CMS-1500 claim form is used to accept assignment of benefits? Contractual allowance -question to the answer-Which of the following is an example of a remark code from an explanation of benefits document? When an insurance company transfers data to allow coordination of benefits of a claim -question to the answer-Which of the following describes the term "crossover" as it relates to Medicare? block 24j -question to the answer-Rendering Provider ID Number goes on what block on the CMS-1500 claim form? The date of the last disclosure -question to the answer-Which of the following is included in the release of patient information? History -question to the answer-Which of the following describes a key component of an evaluation & management service? Aging report -question to the answer-Which of the following reports is used to arrange the accounts receivable from the date of service? Medical standard of conduct -question to the answer-Which of the following best describes medical ethics? Arthroscopy -question to the answer-An examination of a patient's knee joint via small incisions & an optical device. Which of the following terms describes this procedure? A product pending FDA approval is indicated as a lightning bolt symbol -question to the answer-Which of the following accurately describes code symbols found in the CPT manual? 3rd party payer -question to the answer-Which of the following describes an insurance carrier that pays the provider who rendered services to a patient? Stark law -question to the answer-Which of the following prohibits a provider from referring Medicare patients to a clinical laboratory service in which the provider has a financial interest? Electronic remittance advice -question to the answer-Which of the following electronic forms is used to post payments? Remittance advice -question to the answer-For non-crossover claims, the billing & coding specialists should prepare an additional claim for the secondary payer & send it with a copy of which of the following? 18% -question to the answer-When coding a front torso burn, which of the following percentages should be coded? block 21 -question to the answer-Which of the following blocks of the CMS-1500 claim form indicates an ICD diagnosis code? Billing provider -question to the answer-Which of the following national provider identifiers (NPIs) is required from block 33A of a CMS-1500 claim form? services require additional information -question to the answer-Which of the following causes a claim to be suspended? Left upper quadrant -question to the answer-Which of the following terms is used to describe the location of the stomach, the spleen, part of the pancreas, part of the liver, & part of the small & large intestines? Attach the remittance advice from the primary insurance along with the Medicaid claim. -question to the answer-Which of the following actions should the billing and coding specialist take when submitting a claim to Medicaid for a patient who has primary & secondary coverage? 17b -question to the answer-National provider # Signed release of information form -question to the answer-When a 3rd party payer requests copies of patient information related to a claim, the billing and coding specialists must make sure which of the following is included in the patient's file? Primary care provider -question to the answer-A patient who has an HMO insurance place needs to see a specialists for a specific problem. From which of the following should the patient obtain the referral? Office inspector general -question to the answer-Which of the following organizations fights waste, fraud, and abuse in medicare and Medicaid? The 3rd party payer reimburses the patient, and the patient is responsible for reimbursing the provider? -question to the answer-When submitting claims, which of the following is the outcome if block 13 is left blank? The provider recieves payment directly from the payer -question to the answer-A billing & coding specialists is reviewing a CMS-1500 claim form. "The assignment of benefits box" has been checked "yes". The checked box indicates which of the following? 0% -question to the answer-A bene [Show More]
Last updated: 1 year ago
Preview 1 out of 25 pages
Reviews( 0 )
Recommended For You
Education> EXAM > MTTC 103 PRACTICE EXAM MULTIPLE QUESTIONS AND ANSWERS,RATED A. (All)
MTTC 103 PRACTICE EXAM MULTIPLE QUESTIONS AND ANSWERS,RATED A.
MTTC 103 PRACTICE EXAM MULTIPLE QUESTIONS AND ANSWERS,RATED A.MTTC 103 PRACTICE EXAM MULTIPLE QUESTIONS AND ANSWERS,RATED A.MTTC 103 PRACTICE EXAM MULTIPLE QUESTIONS AND ANSWERS,RATED A.MTTC 103 PR...
By VERIFIED A+ , Uploaded: Jun 12, 2023
$14
Mathematics> EXAM > ATI TEAS MATHEMATICS PRACTISE TEST QUESTIONS AND ANSWERS LATEST 2023/2024 GRADED A+ (All)
ATI TEAS MATHEMATICS PRACTISE TEST QUESTIONS AND ANSWERS LATEST 2023/2024 GRADED A+
ATI TEAS MATHEMATICS PRACTISE TEST QUESTIONS AND ANSWERS LATEST 2023/2024 GRADED A+
By kelly jane , Uploaded: Jul 04, 2023
$9.5
*NURSING> EXAM > 2023 NCLEX RN NEXT GEN QUESTIONS AND ANSWERS (LATEST VERSION) (All)
2023 NCLEX RN NEXT GEN QUESTIONS AND ANSWERS (LATEST VERSION)
NCLEX RN 2021 LATEST
By Grade A+ , Uploaded: May 31, 2022
$24
Health Care> EXAM > ATI TEAS SCIENCE STUDY PART 1 QUESTIONS AND ANSWERS (All)
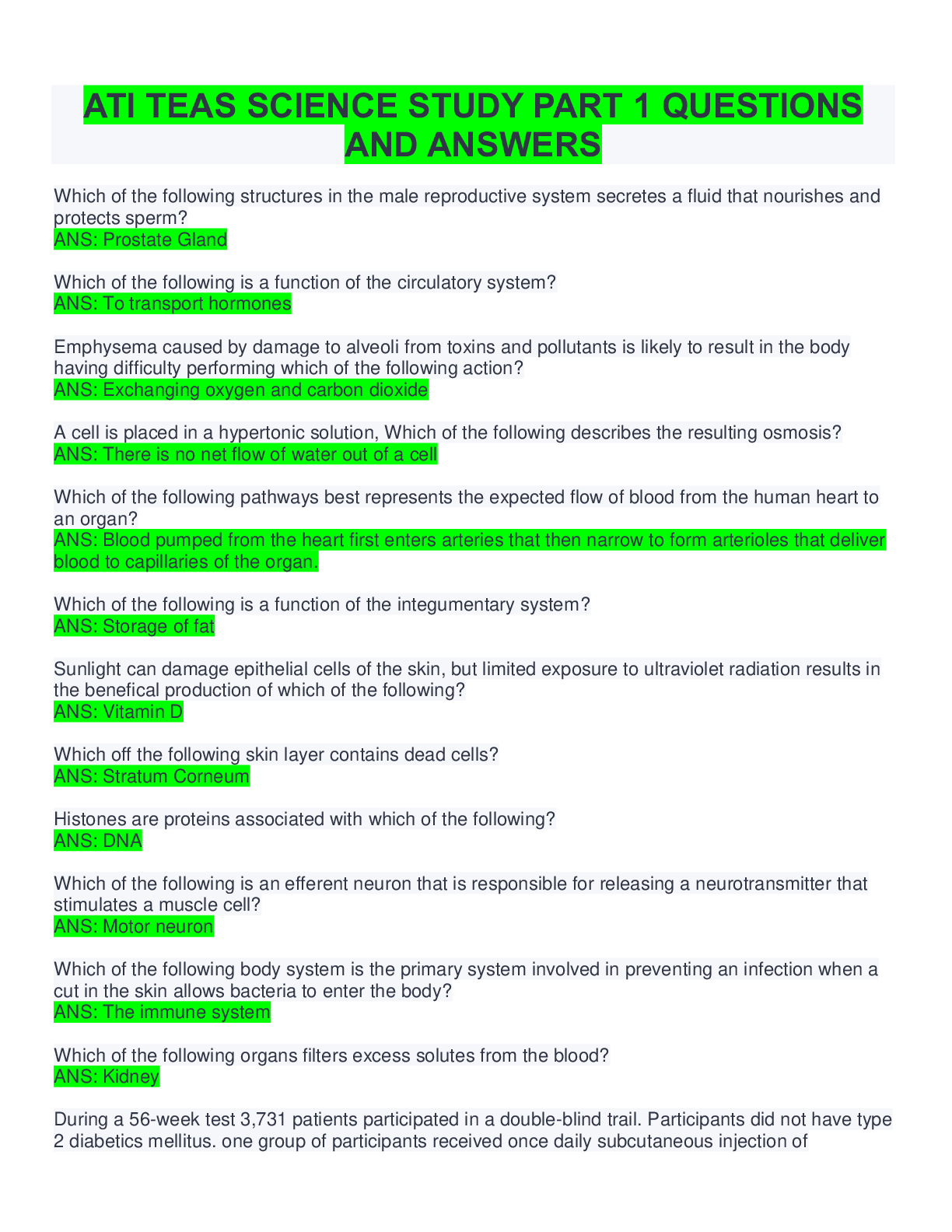
ATI TEAS SCIENCE STUDY PART 1 QUESTIONS AND ANSWERS
Which of the following structures in the male reproductive system secretes a fluid that nourishes and protects sperm? ANS: Prostate Gland Which of the following is a function of the circulatory sy...
By Assignment Help , Uploaded: Oct 06, 2022
$13
LETRS> EXAM > LETRS Unit 8 Assessment Questions and Answers (All)
LETRS Unit 8 Assessment Questions and Answers
LETRS Unit 8 Assessment Questions and Answers
By Tutor Charles , Uploaded: May 28, 2023
$5
*NURSING> EXAM > NUR 2063 Pathophysiology Exam 1 FINAL EXAM Updated 2023/2024 (200+ VERIFIED Q & A) (All questions answered) - Rasmussen (All)
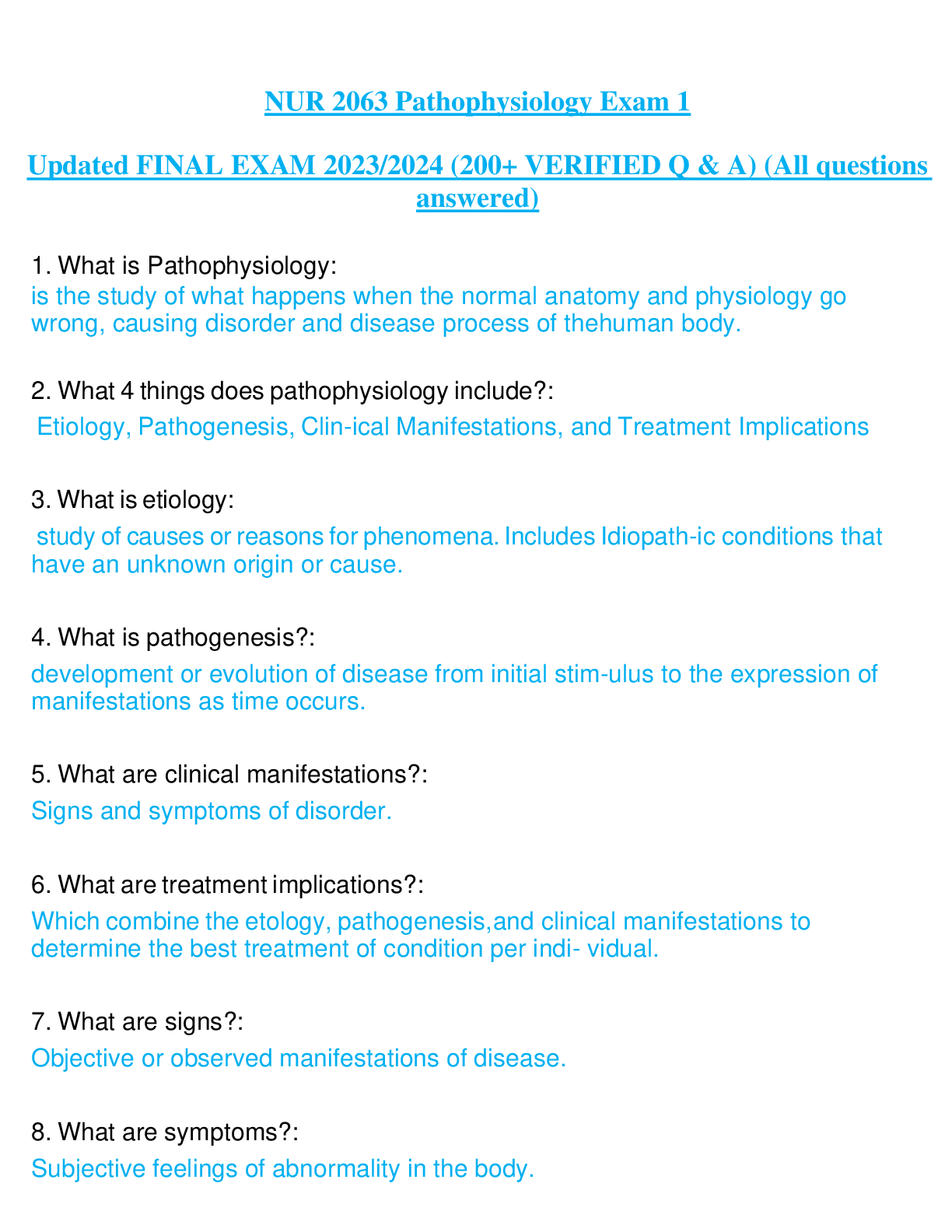
NUR 2063 Pathophysiology Exam 1 FINAL EXAM Updated 2023/2024 (200+ VERIFIED Q & A) (All questions answered) - Rasmussen
NUR 2063 Pathophysiology Exam 1 Updated FINAL EXAM 2023/2024 (200+ VERIFIED Q & A) (All questions answered) - RasmussenNUR 2063 Pathophysiology Exam 1 Updated FINAL EXAM 2023/2024 (200+ VERIFIED Q &...
By ExamNavigator , Uploaded: Apr 30, 2023
$12
Health Care> EXAM > CCMA EXAM QUESTION AND ANSWERS (LATEST 2023) (All)
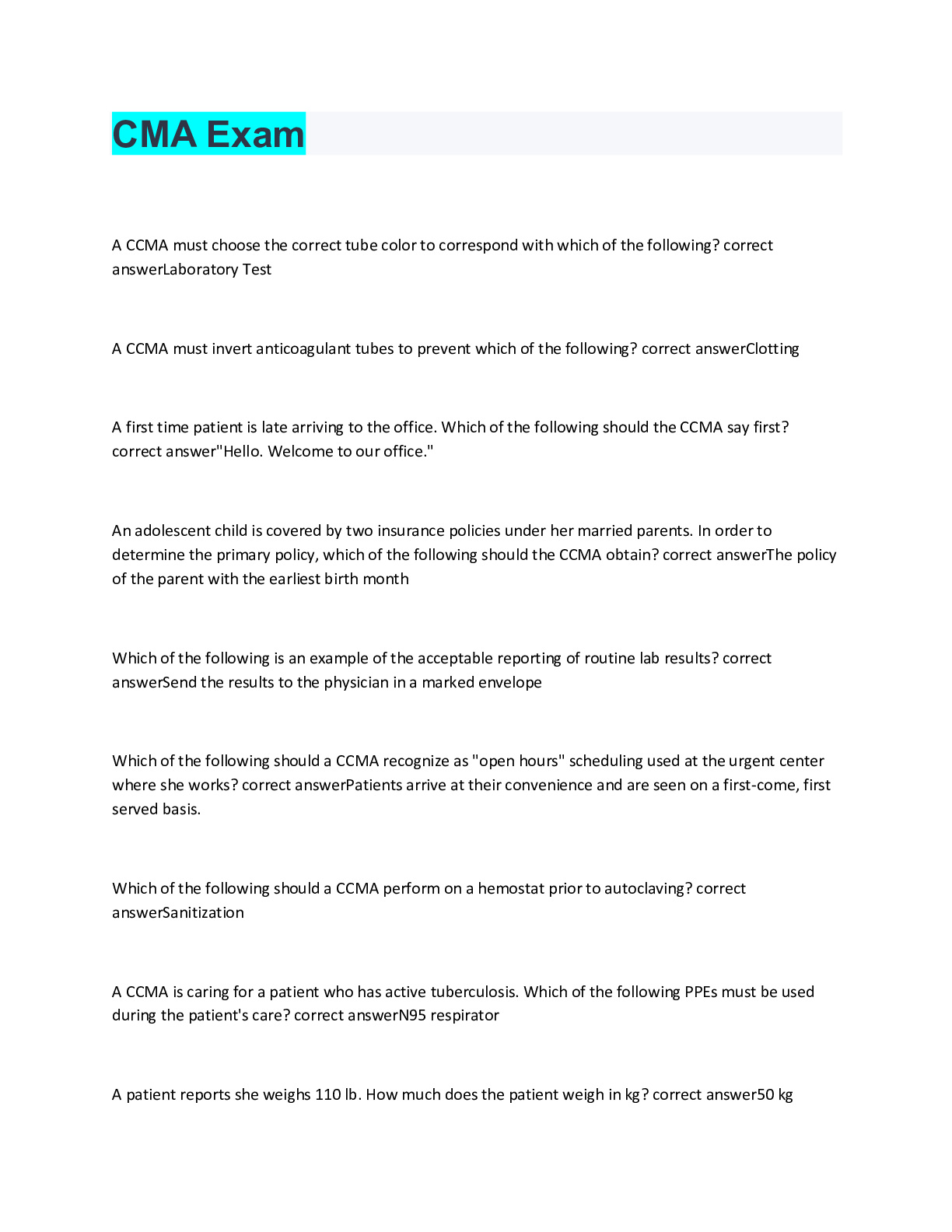
CCMA EXAM QUESTION AND ANSWERS (LATEST 2023)
CCMA EXAM QUESTION AND ANSWERS (LATEST 2023)
By Grade A+ , Uploaded: Mar 27, 2023
$20
Computer Science> EXAM > CEH Practice Questions | 100 Questions with 100% Correct Answers | 34 Pages (All)
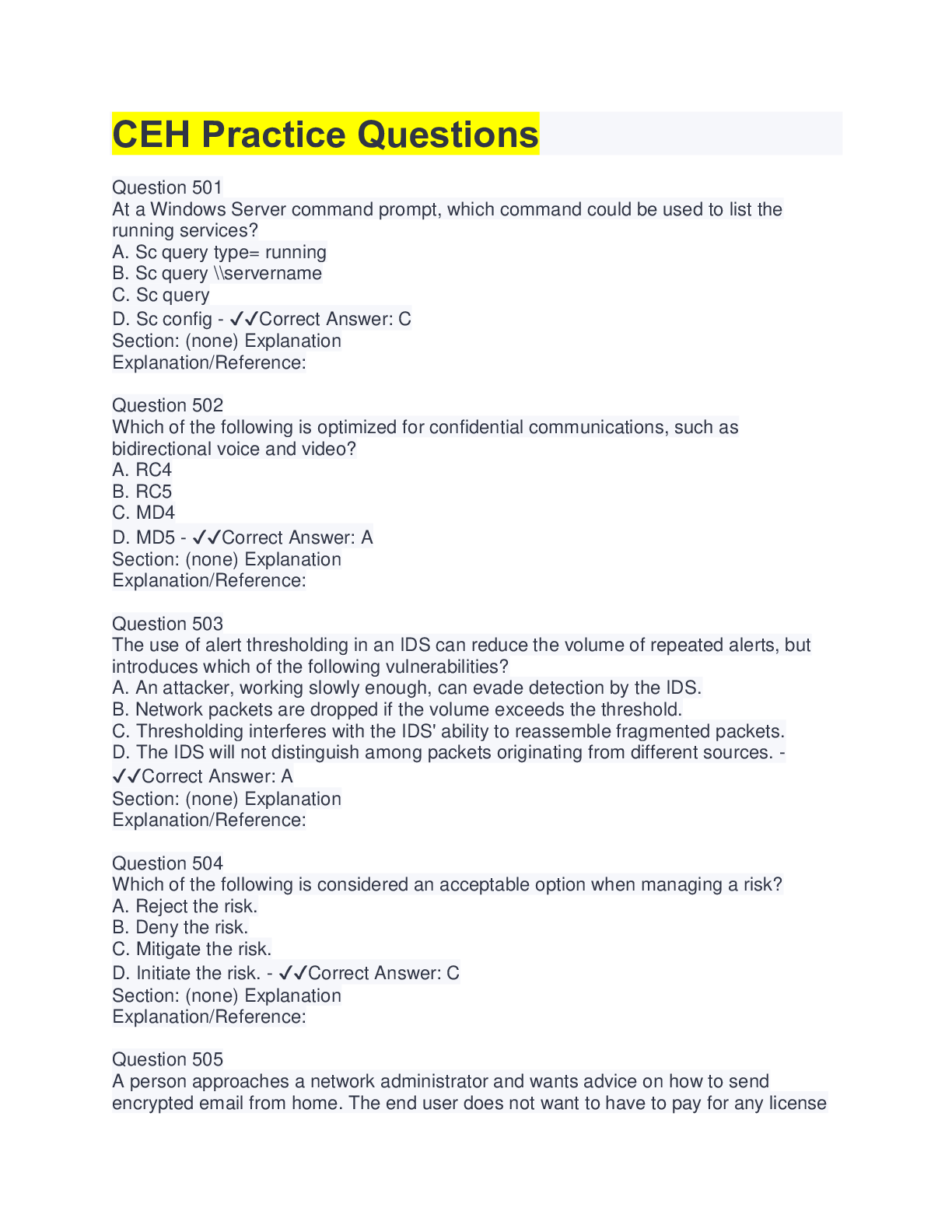
CEH Practice Questions | 100 Questions with 100% Correct Answers | 34 Pages
At a Windows Server command prompt, which command could be used to list the running services? A. Sc query type= running B. Sc query \\servername C. Sc query D. Sc config - ✔✔Correct Answer: C Se...
By Tessa , Uploaded: Aug 12, 2022
$12
*NURSING> EXAM > HESI RN Psychiatric-Mental Health Exit Exam Questions And Answers (Latest 2020/2021 Version) (All)
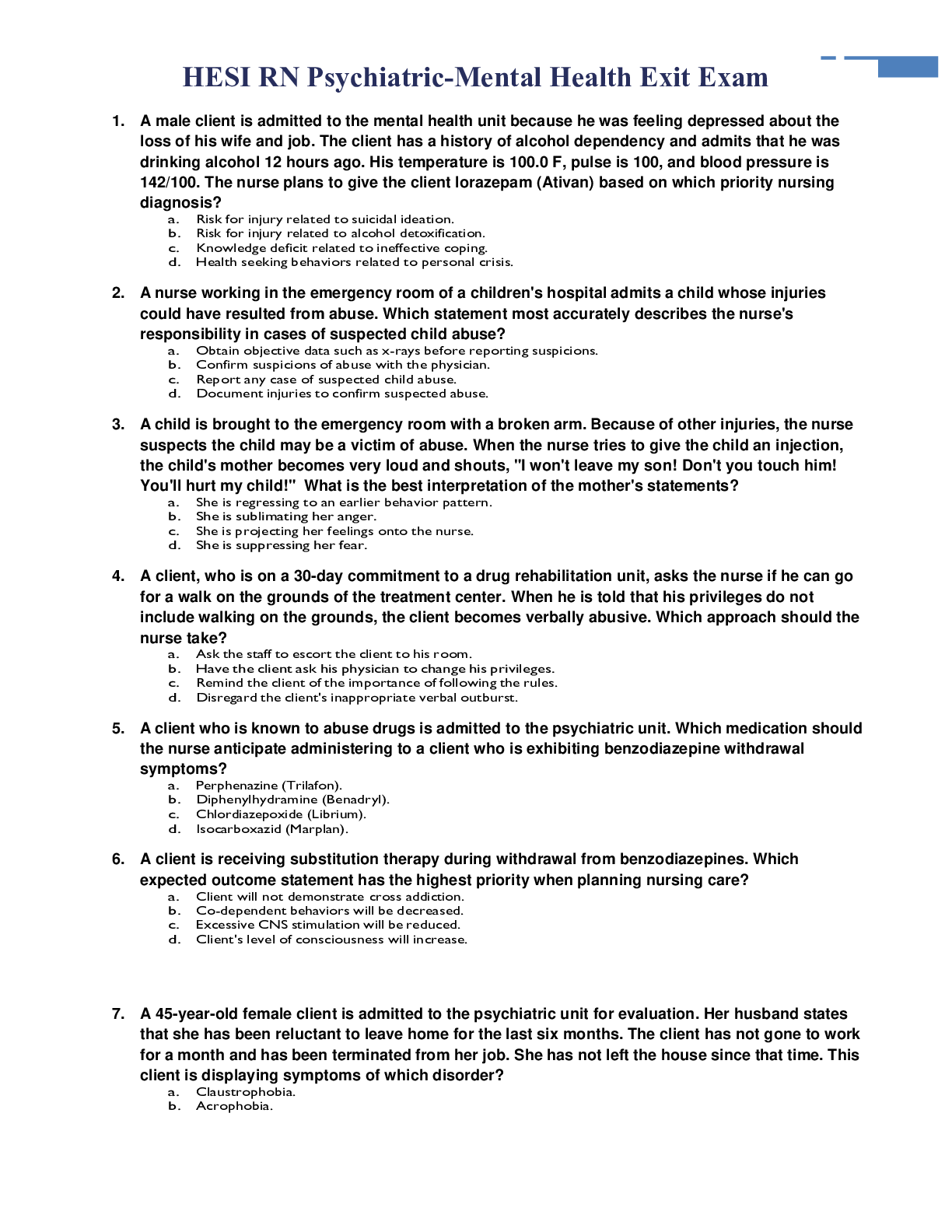
HESI RN Psychiatric-Mental Health Exit Exam Questions And Answers (Latest 2020/2021 Version)
HESI RN Psychiatric-Mental Health Exit Exam 1. A male client is admitted to the mental health unit because he was feeling depressed about the loss of his wife and job. The client has a history of alco...
By merit95 , Uploaded: Apr 26, 2021
$22
*NURSING> EXAM > NUR 4290 HESI EXAM QUESTIONS AND ANSWERS (LATEST 100% ) (All)
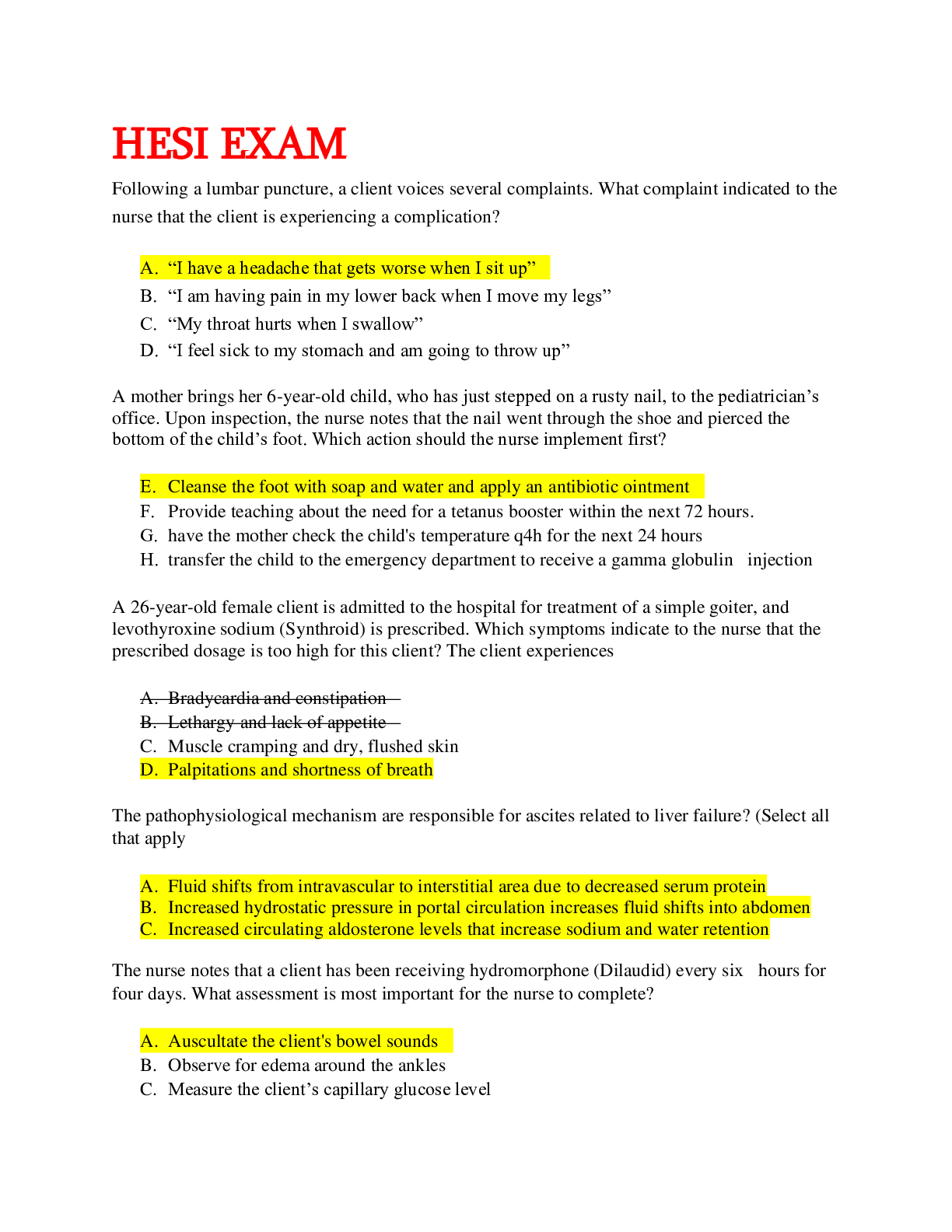
NUR 4290 HESI EXAM QUESTIONS AND ANSWERS (LATEST 100% )
NUR 4290 HESI EXAMNUR 4290 HESI EXAM Following a lumbar puncture, a client voices several complaints. What complaint indicated to the nurse that the client is experiencing a complication? A. “I hav...
By Good grade , Uploaded: Dec 26, 2020
$20
Document information
Connected school, study & course
About the document
Uploaded On
Jan 19, 2023
Number of pages
25
Written in
Additional information
This document has been written for:
Uploaded
Jan 19, 2023
Downloads
0
Views
33






