NURS 6541 Pediatric SOAP note
Document Content and Description Below
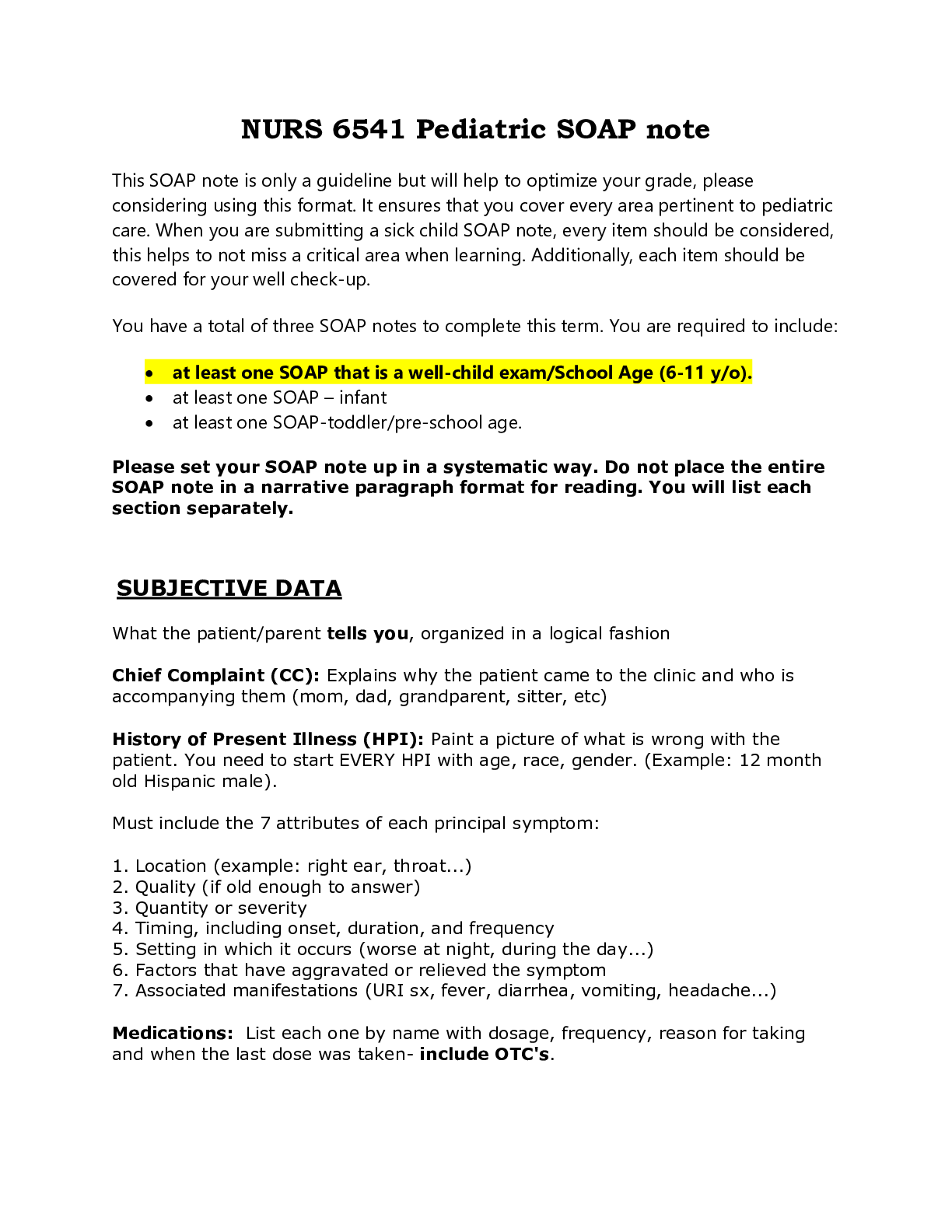
You have a total of three SOAP notes to complete this term. You are required to include: at least one SOAP that is a well-child exam/School Age (6-11 y/o). at least one SOAP – infant ... at least one SOAP-toddler/pre-school age. Please set your SOAP note up in a systematic way. Do not place the entire SOAP note in a narrative paragraph format for reading. You will list each section separately. SUBJECTIVE DATA What the patient/parent tells you, organized in a logical fashion Chief Complaint (CC): Explains why the patient came to the clinic and who is accompanying them (mom, dad, grandparent, sitter, etc) History of Present Illness (HPI): Paint a picture of what is wrong with the patient. You need to start EVERY HPI with age, race, gender. (Example: 12 month old Hispanic male). Must include the 7 attributes of each principal symptom: Review of Systems: Think head to toe. Remember, this is what the patient tells you. (This is not your physical assessment!) For both sick and well-child exams, each area should be addressed. Remember, you are not allowed to use “WNL”. 1. General Health Mom noticed no problems with appetite, sleep, or activity level. Patient denied or mon reports no fevers, bone pain, night sweats, sick contacts, joint pain, rashes. 2. Skin-reports no rashes, bruises, insect bites, or sores 3. HEENT- reports no problems with oral and nasal pharynx 4. Thorax/Chest- Denies chest pain 5. Respiratory-denies SOB 6. Heart- No reported symptoms 7. GI-Denies nausea, vomiting, or diarrhea 8. Genital 9. Musculoskeletal 10. Neuro/Psychiatric 11. Endocrine 12. Hematologic Health Risks: General review. If you are doing a well exam, include them all: pets, tobacco exposure, TB exposure, lead exposure, immunocompromised, cholesterol risk, car seat/booster/seat belt, adequate fluoride, dental exam, firearms in home secured, helmet use, fire alarms, water safety, etc. (The most common health risk behaviors among adolescents are tobacco use, alcohol use, drug use, behaviors that result in injury or violence, sexual behaviors that result in sexually transmitted infections and pregnancy, poor nutrition, and physical inactivity). [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note (All)
NR 509 Week 6 Pediatric SOAP Note
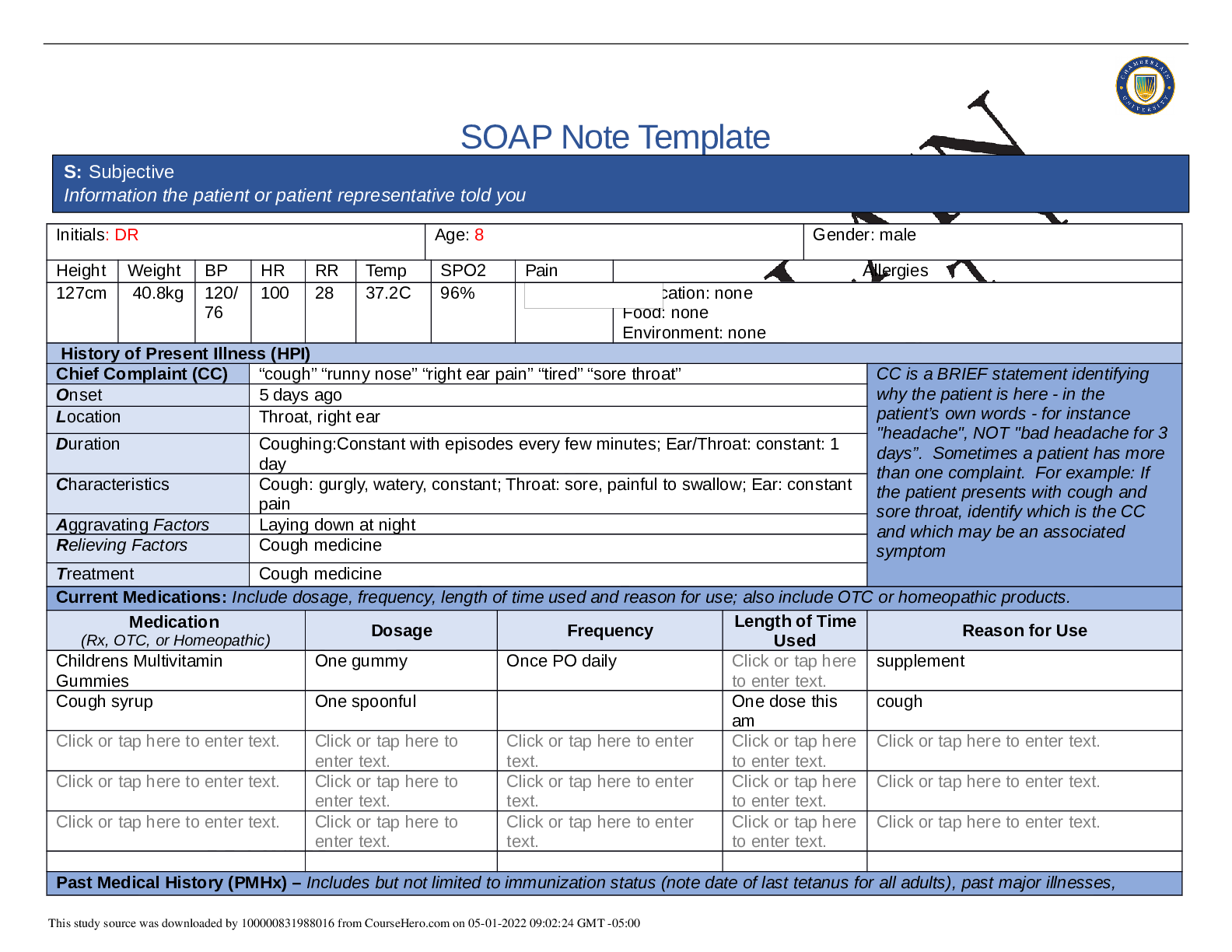
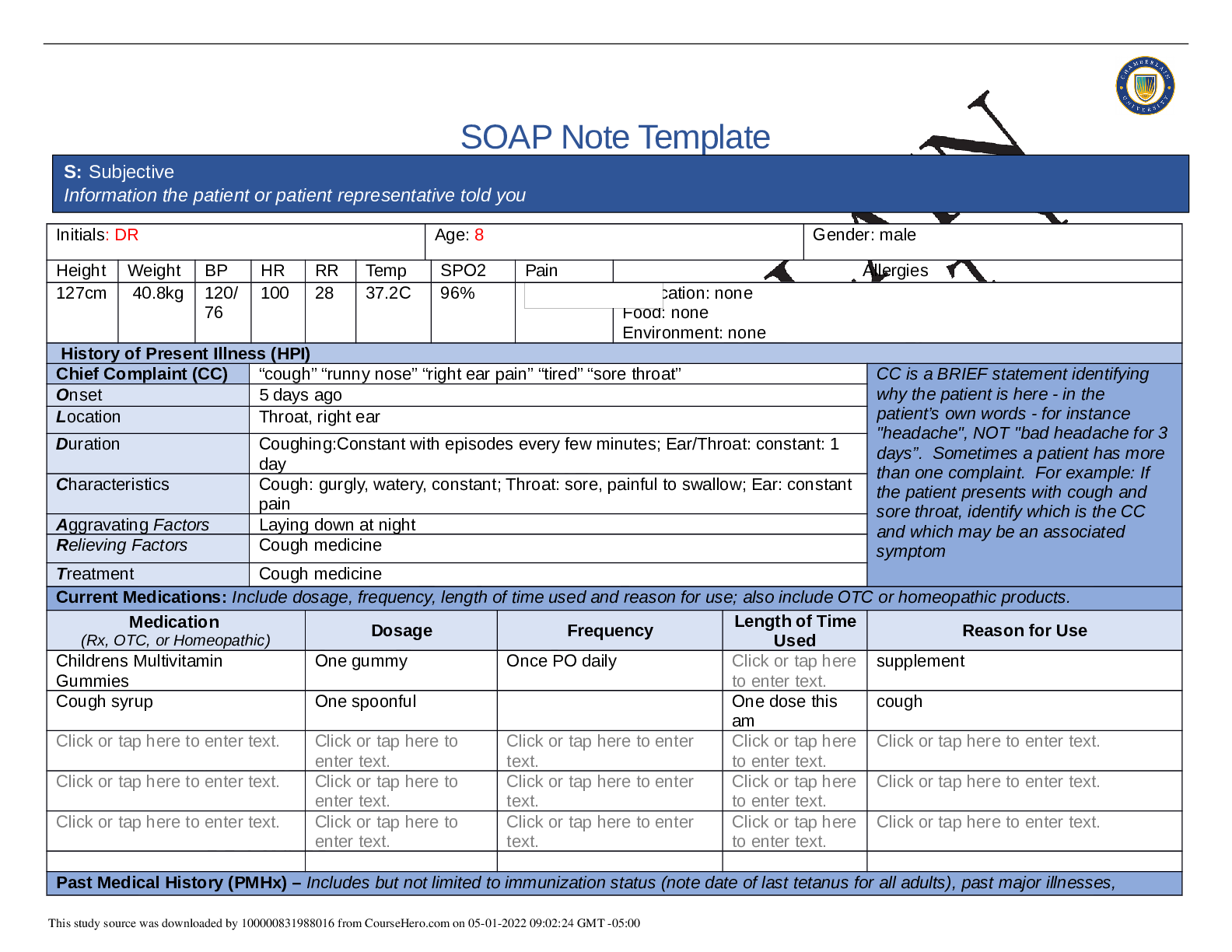
SOAP Note Template Initials: DR Age: 8 Gender: male Height Weight BP HR RR Temp SPO2 Pain Allergies 127cm 40.8kg 120/ 76 100 28 37.2C 96% Medication: none Food: none Environment: none History...
By Nutmegs , Uploaded: May 01, 2022
$9
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution (All)
NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution
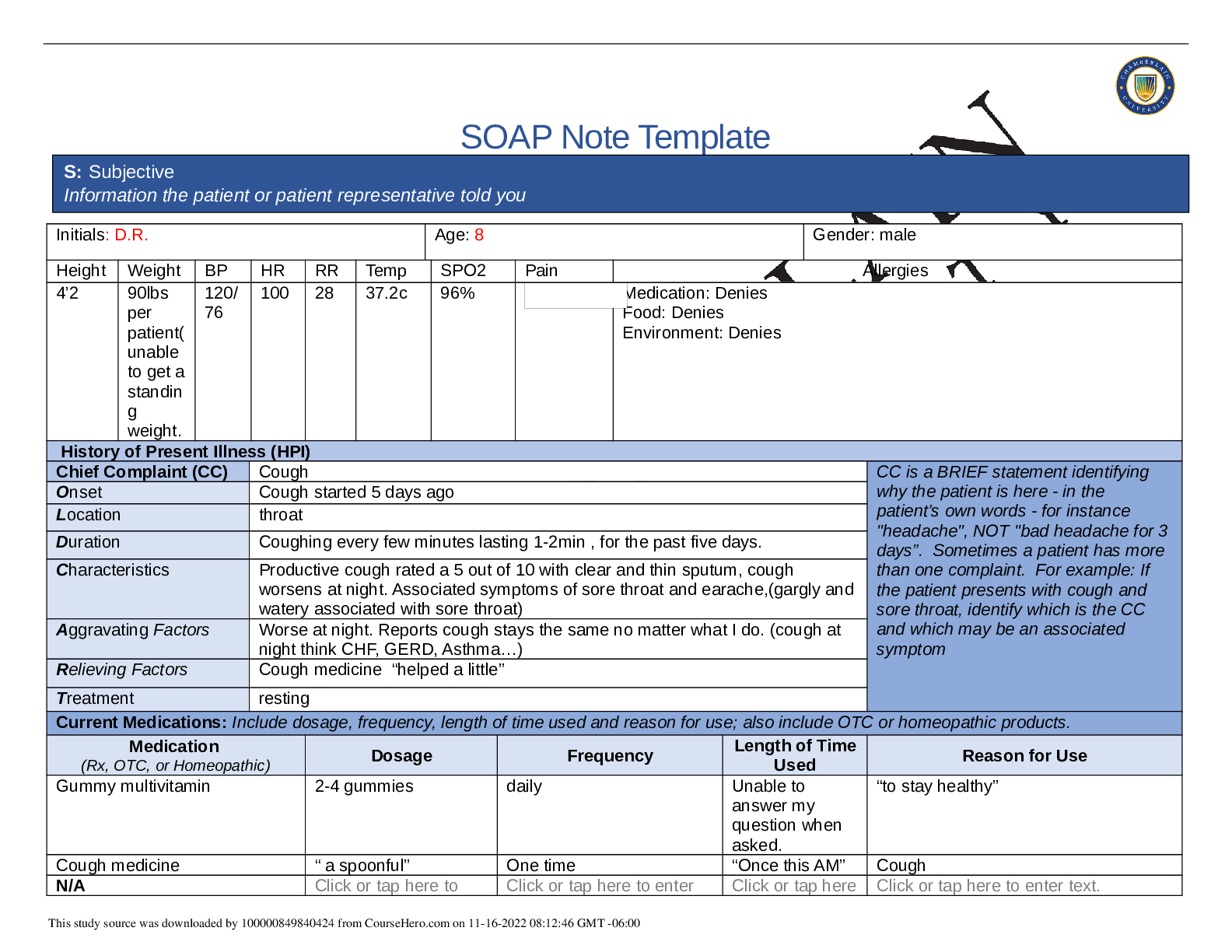
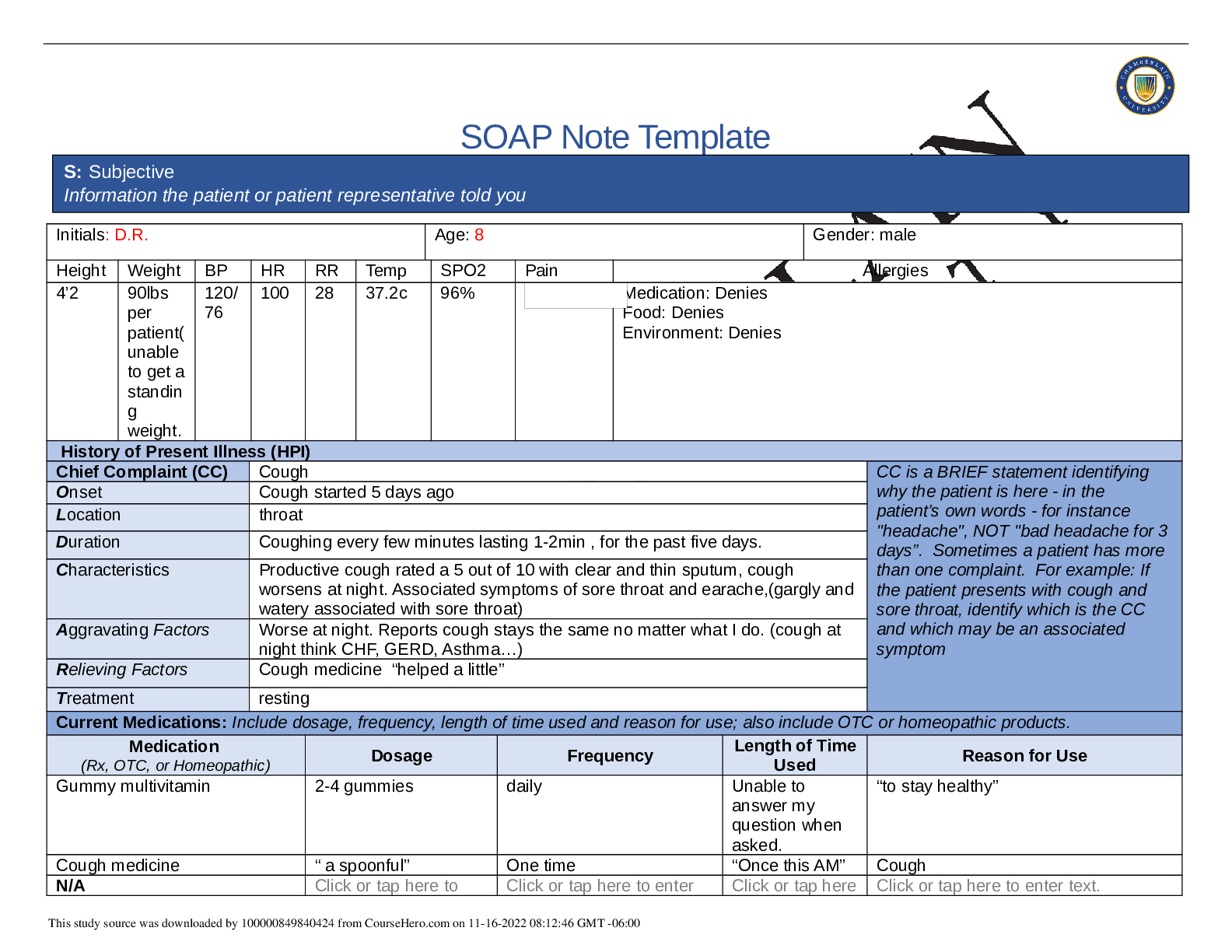
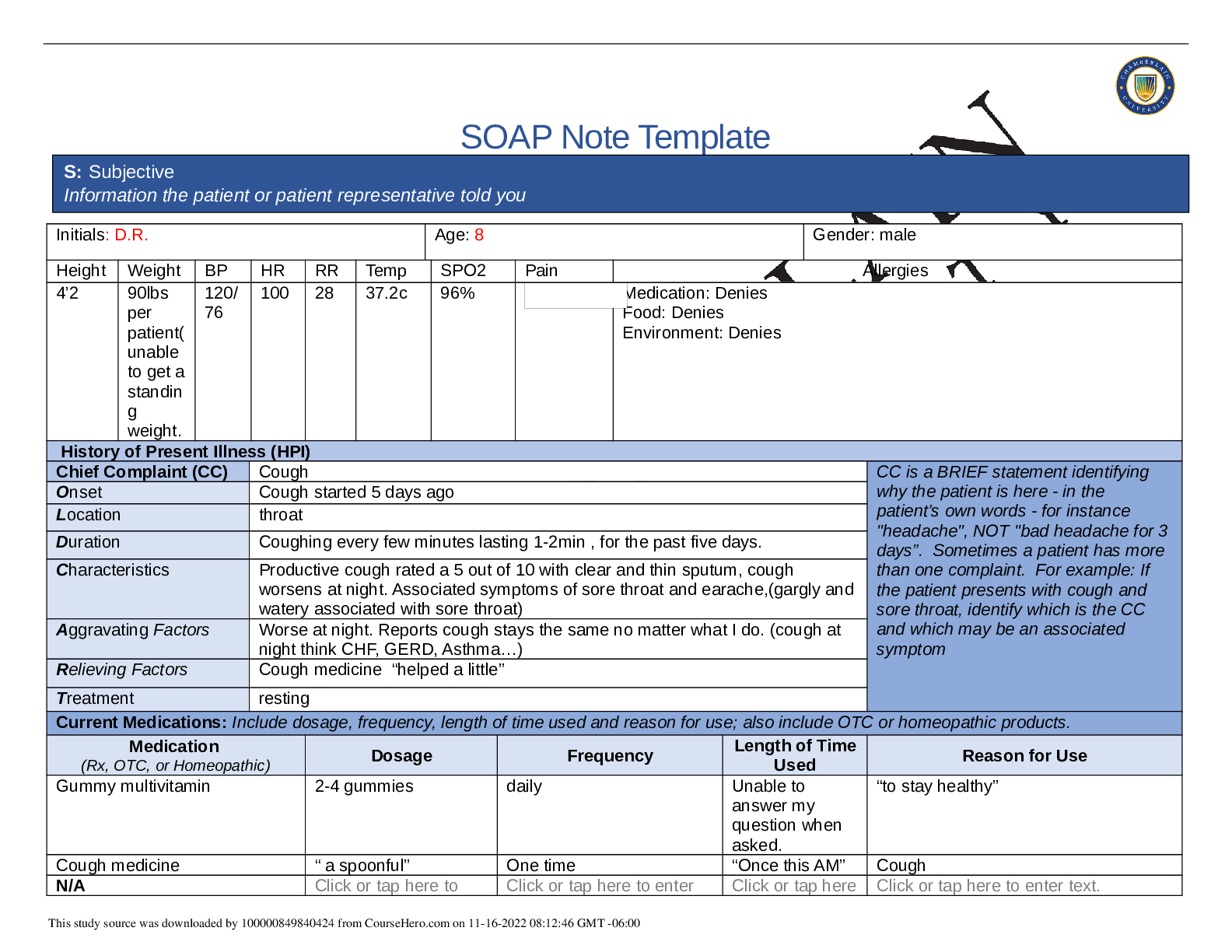
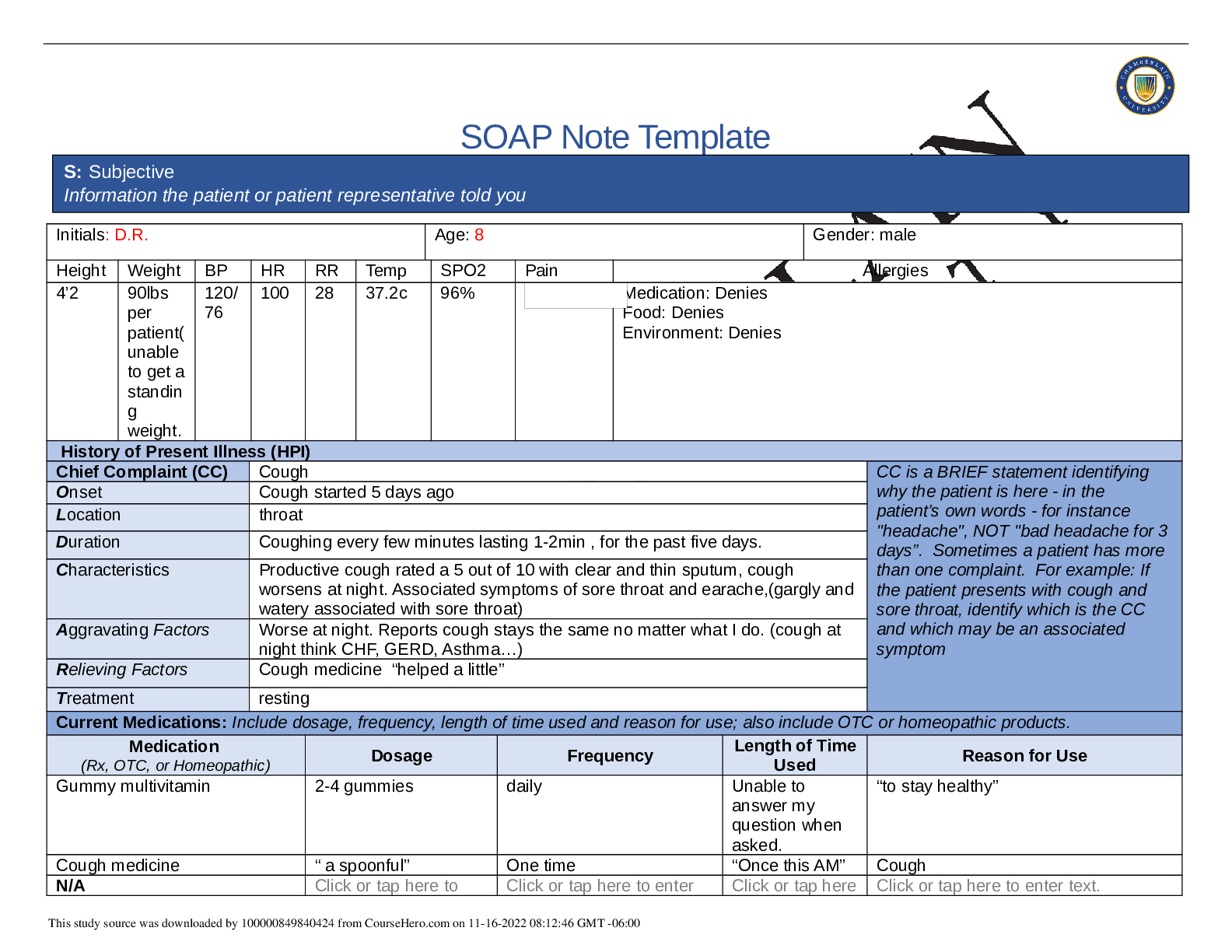
c 96% Medication: Denies Food: Denies Environment: Denies History of Present Illness (HPI) Chief Complaint (CC) Cough CC is a BRIEF statement identifying why the patient is here - in the pat...
By Book Worm, Certified , Uploaded: Jan 10, 2022
$10
*NURSING> SOAP NOTE > NRP571 Health assesment week 4 Pediatric soap notes (ANSWERED) | Graded A. (All)
NRP571 Health assesment week 4 Pediatric soap notes (ANSWERED) | Graded A.
Week 4 Pediatric SOAP Notes NRP571 Phoenix university Pediatric SOAP Note 1 Date: 15 July 2011 Name: C.P (Female) DOB: 15 August 2007 Age: 4 years 11 months CC: Here with father who...
By A+ Solutions , Uploaded: Oct 17, 2021
$11
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Complete latest (Spring 2020) template. (All)
NR 509 Week 6 Pediatric SOAP Note, Complete latest (Spring 2020) template.
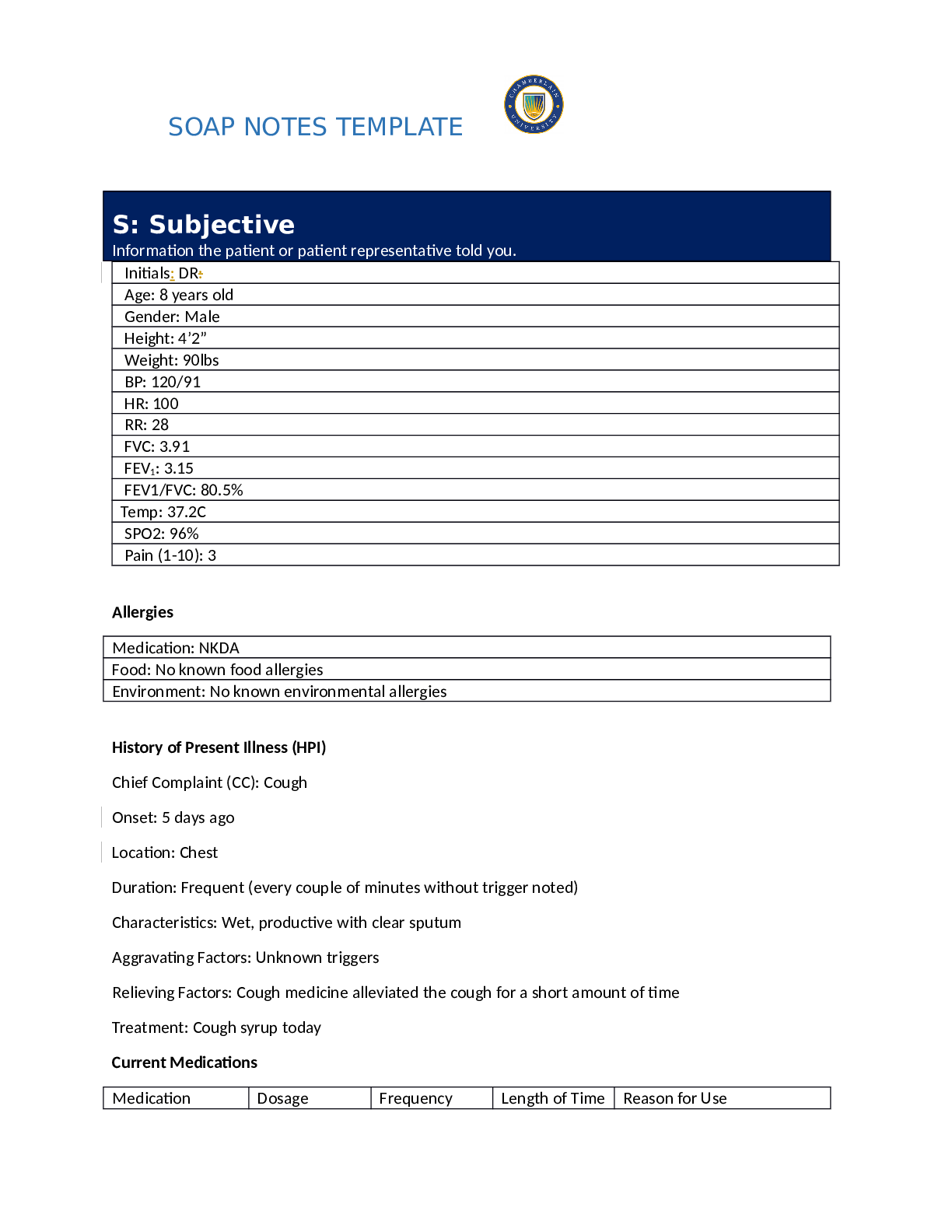
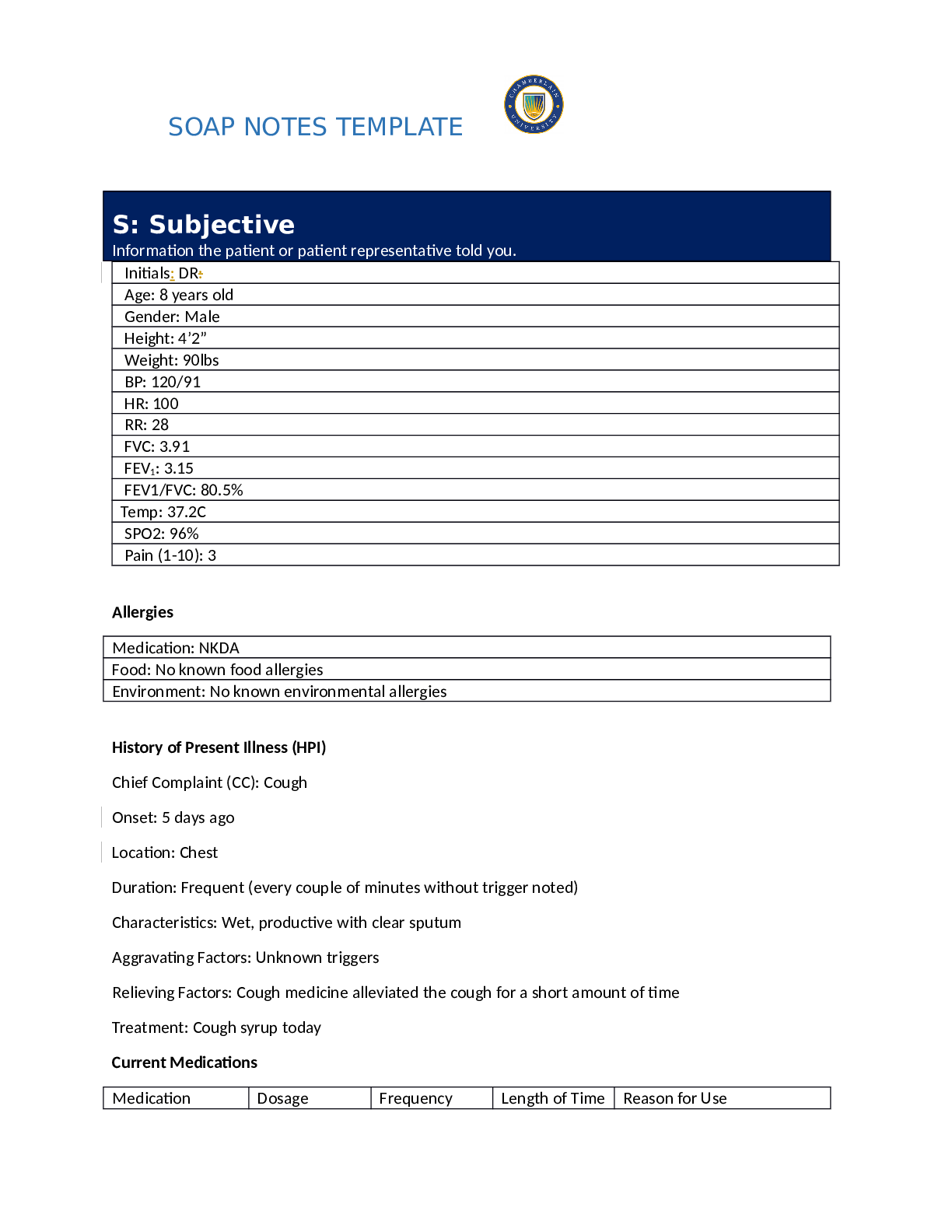
SOAP NOTES TEMPLATE S: Subjective Information the patient or patient representative told you. Initials: DR: Age: 8 years old Gender: Male Height: 4’2” Weight: 90lbs BP: 120/91 HR: 100 RR:...
By Nutmegs , Uploaded: Sep 26, 2021
$13
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Complete latest (Spring 2021) template. (All)
NR 509 Week 6 Pediatric SOAP Note, Complete latest (Spring 2021) template.
History of Present Illness (HPI) Chief Complaint (CC): Cough Onset: 5 days ago Location: Chest Duration: Frequent (every couple of minutes without trigger noted) Characteristics: Wet, productive...
By Dr Medina Reed , Uploaded: Sep 25, 2021
$15
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution (All)
NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution
SOAP Note Template Initials: D.R. Age: 8 Gender: male Height Weight BP HR RR Temp SPO2 Pain Allergies 4’2 90lbs per patient( unable to get a standin g weight. 120/ 76 100 28 37.2c 96% M...
By Nutmegs , Uploaded: Sep 21, 2021
$10
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution (All)
NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution
NR 509 Week 6 Pediatric SOAP Note S: Subjective – Information the patient or patient representative told you O: Objective – Information gathered during the physical examination by inspection, palpatio...
By Muchiri , Uploaded: Sep 13, 2021
$8
*NURSING> SOAP NOTE > NURSING 425_Pediatric SOAP Note on Impetigo (All)

NURSING 425_Pediatric SOAP Note on Impetigo
NURSING 425_Pediatric SOAP Note on Impetigo
By Ebooks , Uploaded: Aug 20, 2021
$9
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note Latest complete solution. (All)
NR 509 Week 6 Pediatric SOAP Note Latest complete solution.
NR 509 Week 6 Pediatric SOAP Note S: Subjective – Information the patient or patient representative told you O: Objective – Information gathered during the physical examination by inspection, palpatio...
By PROF , Uploaded: Apr 09, 2021
$12
*NURSING> SOAP NOTE > NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution A+ Guide (All)
NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution A+ Guide
NR 509 Week 6 Pediatric SOAP Note, Summer 2020 complete solution A+ Guide>NR 509 Week 6 Pediatric SOAP Note S: Subjective – Information the patient or patient representative told you O: Objective – In...
By PROF , Uploaded: Mar 25, 2021
$12
Document information
Connected school, study & course
About the document
Uploaded On
Jan 27, 2021
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Jan 27, 2021
Downloads
0
Views
206






