*NURSING > NCLEX > MARK KLEMIK: NCLEX SG Lab Values A: abnormal (do nothing, not as important) B: be concerned (assess/ (All)
MARK KLEMIK: NCLEX SG Lab Values A: abnormal (do nothing, not as important) B: be concerned (assess/monitor) C: Critical (priority/Do something) D: Dangerous (Highest priority/Do something NOW)
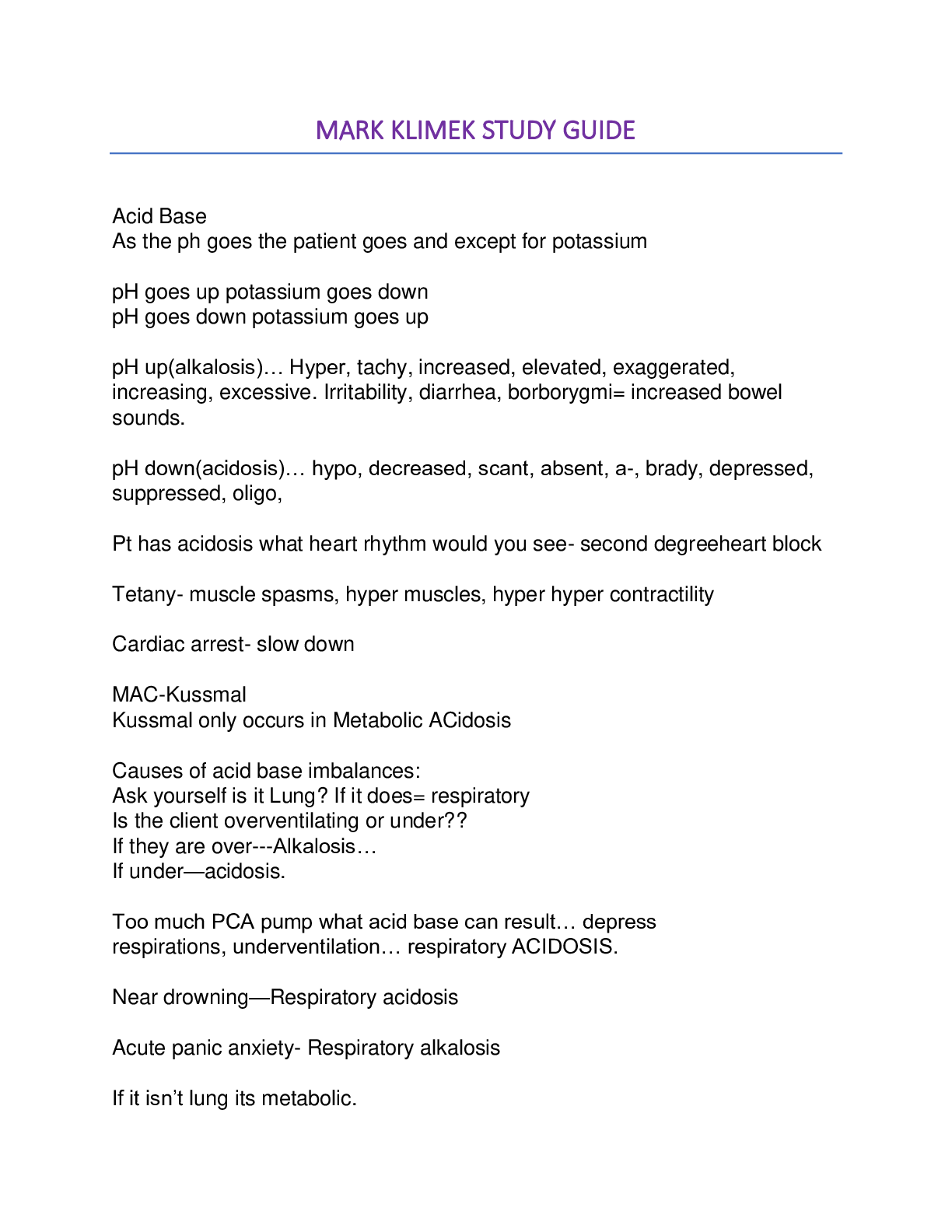
Document Content and Description Below
MARK KLEMIK: NCLEX SG Lab Values A: abnormal (do nothing, not as important) B: be concerned (assess/monitor) C: Critical (priority/Do something) D: Dangerous (Highest priority/Do something NOW) S... erum Creatinine: do nothing Best indicator for what_____? therapeutic range____? Kidney Function (^Serum Cr.=kidney disease) 0.6-1.2 (same as Lithium range) INR (International Normalized Ratio) Monitors what____? Therapeutic range___? Coumadin (Warfarin Therapy) 2 – 3 >4 (Critical priority) o Hold/Stop all warfarin o Assess for bleeding (focused assess.) o Prepare to administer Vit. K (antidote) o Notify/Call HCP Potassium: Therapeutic range___? What to do for K+ <3.5? What to do for K+ >5.3? 3.5 – 5.3 <3.5 (DO SOMETHING) o Assess heart o Prepare to administer K+ o Call HCP 5.4-5.9 (DO SOMETHING) o Hold K+ o Assess heart o Prepare to administer Kayexelate & d5W regular insulin o Call/Notify HCP >6 (DEADLY DANGEROUS/NOW) o Do steps simultaneously (STAT) o Stay with your patient (Deadly patient) pH: Ref. Range___? What What to do for pH <6? 7.35 – 7.45 (drop in pH = patient drops as well) pH in the 6’s (Deadly = severe acidosis) o Assess VS (to make sure they are alive) o Call/notify HCP if VS is bad (call Rapid Response team) o TX the underlying cause (HCP responsibility) BUN (Blood Urea Nitrogen) Ref. Range 8-25 (Bun‟s come in 8/pack) Elevated BUN o Assess for dehydration Blood value goes up b/c concentration. HgB (Hemoglobin) Ref. range 12-18 (people) 8-11 (do nothing) o Assess for anemia/malnutrition (low hgb) <8 (do something) o Assess for bleedingo Prepare to administer blood o Call HCP HCO3 (Bicarb) Ref. range___? 22 – 26 Abnormal not an issue CO2 (Carbon Dioxide) receive it from where__? ref. range___? Arterial Blood Gas 35 – 45 CO2 in 50’s: (Critical / Do something people without COPD) o Assess Respiratory status o Pursed lip breathing (candle blow out) prolonging exhalation = gets out CO2 Effective treatment = breathe easier CO2 in 60‟s: (Respiratory Failure) o Medical emergency/ HIGH PRIORITY o Stay with patient o Assess Respiratory status o If symptomatic call RAPID RESPONSE o Prepare to INTUBATE/ VENTILATE o Call HCP/Respiratory therapist Hct (Hematocrit) ref. range____? 36 – 54% (3x the hgb. ie, 12x3 = 36 & 18x3=54) Elevated Hct o Assess for dehydration PO2: Oxygen level in blood; obtained from ABG. ref. range____? Respiratory Failure range__? 78 – 100 Low PO2 in the 70’s (Critical/Priority) o Assess Respiratory o Provide Oxygen Should correct itself No dyspnea, restlessness, anxiety, tachycardia o Hypoxic patient which rate increases first (HR or RR?) HR and when the heart can no longer compensate the RR will increase. Coronary Care: 2 most common causes of episodic tachycardia in heart patient? o Hypoxia & Dehydration o TX: increase the IV rate & Provide O2 PO2 Low in the 60’s (Emergency/Immediate Care) o Respiratory Failure (O2 & CO2 in 60’s) o Assess Respiratory status o Give O2 o Prepare intubate/ventilate o Call HCP/Respiratory therapist SaO2 Stat ref. range____? What invalidates SaO2 stat? SaO2: 93 – 100% <93% (critical patient) o Assess the patient o Give O2 Pediatric <95% (BAD) Anemic patient invalidates O2 stat because anemia falsely elevates SaO2. Dye-procedure in the last 48 hours because it colors the hand and falsely elevates BNP. BNP (brain natruie peptide) Good indicator for what____? Normal ref. range should be less than what_______? Chronic Heart Failure (CHF) Normal <100 Elevated BNP (HF, pt. not going to die) o Monitor for CHF (chronic condition) Sodium (Na) ref. range 135 – 145 Abnormal: (monitor) o HypOnatremia: Fluid Overload o HypErnatremia: Assess dEhydration o Na abnormal and change in LOC: Critical Safety issues WBC’s Total WBC o ref. range? Absolute Neutrophil Count (ANC) o needs to be above what? CD4 Count (T Cells) Needs to be above what? Defining line for AIDS? Total WBC o 5,000 – 10,000 o WBC <5,000 (Critical) ANC >500 ANC<500 (critical) CD4 count >200 CD4 count <200 o AIDS Assess for Sign of Infection Place on Neutropenic Precautions: Neutropenic Precautions: Strict Handwash Shower BID with antimicrobial soap avoid crowds private room limit # of staff entering the room limit visitors to healthy adults no fresh flowers/ potted plants low bacteria diet o no raw fruits, veggies, salads o no undercooked meat Do not drink water that has been standing longer than 15mins VS (temp) q 4 hours Check WBC (ANC) daily avoid use of indwelling cath. Do not re-use cups (must wash in between) Use disposable plates, cups, straws, plastic knife, fork, spoon Dedicated items in RM: Stethoscope, BP cuff, Thermometer, Gloves Terminology: High WBC count o Leukocytosis Low WBC Count o Leukopenia o Neutropenia o Agranulocytosis o Immunosuppression o Bone Marrow Suppression Platelets (Thrombocyte Clotting cell) o Range? 150,000 – 400,000 <90,000 (Critical) o Assess bleeding o Place Bleeding Precaution o Call HCP <40,000 (Danger/ Immediate care) o Could spontaneously hemorrhage to death o Assess for bleeding o Bleeding Precaution o Prepare for transfusion o Notify HCP Bleeding Precautions: (Thrombocytopenic Protocol) No unnecessary venipuncture-injection or IV Handle patient gently Use electric razor, No toothbrush or flossing No hard foods, Well fitted dentures Blow nose gently No rectal temp, enema, suppository No aspirin, Use stool softener (no straining) No contact sport, No walking in bare feet No tight clothes/shoes Notify HCP of blood in urine, stool RBC 4 – 6 million Abnormal (monitor) KNOW THE 5’Ds: o HIGHEST PRIORITY K+>6 pH<6 CO2: 60’s O2: 60’s Platelet: <40,000 Know what to do for the C’s: INR>4 Hypokalemia Potassium: 5.4 – 5.9 HgB <8 CO2 in 50’s PaO2 in 70’s O2 <93 Abnormal Na WBC <5,000 ANC <500 CD4 <200 Platelet <90,000 Acid/Base Balance Rule of B‟s: pH & the Bicarb (HCO3) Both in same direction = Metabolic. pH↑ = HCO3↑= Metabolic Alkalosis pH↓ = HCO3↓= Metabolic Acidosis (MacKussmaul Respiration) pH↓ = HCO3↑ = Respiratory Acidosis What is the pH value____? 7.35 – 7.45 pH< 7.35 (Acidosis) pH>7.45 (Alkalosis) What is the BiCarb value? 22 – 26 What is the PaCO2 value? 35 – 45 What is the PaO2 value? 80-100 What is the SaO2 value? 95% - 100% S & S’s of Acid-Base Balance As the pH goes, so goes the patient EXCEPT for Potassium (K+ will try to compensate) pH ↓ (Body-Shut’s Down), K+↑ (UP) Acidosis o Hyperkalemia o Acidosis o Bradycardia o Bradypnea o Hyporeflexia (+0, +1) o Constipation o Absent bowel sound o obtunded (more lethargic) o paralytic ileus o COMA o Respiratory Arrest AMBU BAG AT BEDSIDE pH ↑ (Body-Goes UP), K+ ↓ (DOWN) Alkalosis o Hypokalemia o Alkalosis o Tachycardia o Tachypnea o Irritability o Hyperreflexia (+3 & +4) o Borborygme (↑ bowel sound)) o Diarrhea o Spastic o SEIZURE SUCTION MACHIN E AT BEDSIDE (r/f Aspiratio n) Causes of Acid-Base Balance 1. Ask, “Is it Lung”? a. if yes, -> Respiratory 2. Then ask yourself:a. Pt. Under-ventilating or Over-ventilating b. Under-ventilating (ACIDOSIS, pH DOWN) Ventilating= GAS EXCHANGE***not just RR c. Over-ventilating (ALKALOSIS, pH UP) Pay attention to SaO2 3. If it‟s not Lung, It is METABOLIC a. If the patient has prolonged gastric vomiting/suctioning = METABOLIC ALKALOSIS i. Patient is losing acid from suctioning/gastric vomiting = BASIC b. For everything thing else that isn‟t lung, pick METABOLIC ACIDOSIS i. Also, If you don‟t know what to pick choose METABOLIC ACIDOSIS. 1. Pt. had a GI surgery & NG tube to low Intermittent suctioning for 3 days (Metabolic Alkalosis) 2. Pt has hyperemesis gravidarum (Met. alkalosis) 3. Pt with hyperemesis gravidarum and is dehydrated (Met. Acidosis) 4. Infant with diarrhea (Met. Acidosis, Not lung & Vomiting) 5. 3rd degree burn with 60% of body (Metabolic Acidosis) Ventilator Alarms High Pressure Alarm are triggered by what? Triggered by Increase resistance to airflow (machine has to push to hard because there is a resistance) What can cause an increase in High Pressure alarms? Obstructions: 1. Kinked Tube a. NRS Intervention: Unkink it 2. Water in tubing (caused by condensation a. NRS Intervention: Empty/Remove H2O in tubing 3. Mucus in airway a. NRS Intervention: i. Turn patient ii. Cough & Deep breathing iii. Suction (as last resort) 1. Suction as needed Low Pressure Alarms are triggered by what? Triggered by Decrease resistance to airflow What are the causes of Low Pressure alarms? Disconnections in the main tubing: 1. Disconnection in Main Tubing a. NRS Intervention: Reconnect tube 2. Disconnection from Oxygen sensor tubing a. Senses the FiO2 & Reconnect it. Respiratory Acidosis (Under-ventilation) The ventilator setting may be what? Ventilator setting may be too LOW ie:HCP says wean off the vent in A.M. The 6am ABG shows respiratory acidosis. What would you do? a. Follow the Order (pt. is under-ventilated) b. Call Respiratory therapist c. Hold the order/Call MD d. Begin to decrease the setting Respiratory Alkalosis (Over-ventilation) The ventilator setting may be what? Ventilator setting may be too HIGH How do you wean a patient on a ventilator? Gradually & Incrementally decrease with the goal of riding all together. Alcohol/Drug The #1 problem in abusive is what? Denial Refusal to accept the reality of the problem What is the #1 problem psychologically in denial? Alcoholism How do you treat denial? Confrontation Point out what they say and what they do When do you not use confrontation in a patient with denial? Loss & Grief Support the patient What are the stages of GRIEF? DAB-DA Denial (normal for loss/grief ->support pt.) Anger Bargaining Depression Acceptance What is Dependent? Abuser gets the Co-dependency to do things for them/make decisions for them. What is Co-Dependent? Significant other feels positive self esteem from supporting the habit of the abuser. NRS Education:o set limits/enforce them o Teach them to say “NO” What is Manipulation? Abuser gest significant other to do things for the client that is not in the best interest for the significant other. Nature of the act is dangerous & harmful. NRS Intervention: o Set limits/enforce them o Teach them to say “NO” Easier to treat than Dependency because there is no positive self-esteem issue with manipulation What is Neutral? Dependency & Co-dependency has 2 patient. What is Negative? Manipulation has 1 patient. What is Wernicke Korsakoff? Psychosis induced by Vit. B1 (Thiamine) deficiency What is the primary S&S’s of Wernicke Korsakoff? Amnesia (memory loss) with Confabulation What is Confabulation? Making up stories to fill in memory loss (believe as TRUE) What the RN action to a patient with confabulation? Redirect the patient, don’t confront them/present reality What are the Characteristics Of Wernicke’s Korsakoff’s syndrome? 1. Preventable (Take Vit. B1) 2. Arrestable: Can stop from getting worse a. Take Vit. B1 (doesn’t have to stop drinking) 3. Irreversible (70%): Kills brain cells What is Disulfiram (Antabuse)? Aversion Therapy for Alcoholism causes patients to hate drinking and causes ill when taken with Alcohol What is the Onset and Duration of Effectiveness of Disulfiram? 2 weeks It takes the drug 2 weeks to get into the blood system for it to work. They have to be off the drug for 2 weeks before they can drink again. What is the patient teaching for patients taking Disulfiram? Avoid all forms of alcohol to prevent: N/V & Possibly Death What are some products that contain alcohol? Mouth wash, Cologne, Perfume, Aftershave, Vanilla extract, hand sanitizer, INSECT REPELLANT, VINAGARETTES, uncooked icing (contains vanilla extract) OTC liquid medicine that contains the word - ELIXIR (hydroalcoholic liquid) o ie: Robutusin, Dayquil, NyQuil Overdose Vs. Withdrawal Upper (5) Caffeine Cocaine PCP (Phencyclidine) /LSD (acid) (Psychedelic hallucinogens) Methamphetamines (meth, chalk, ice, crystal) Adderall (Attention deficit Drug) Downer (135) EVERYTHING NOT IN UPPER o Heroin o Marijuana o Alcohol o Morphine Sulfate o Fentanyl/Ativano Phenobarbutal What are the S&S’s of Upper Drugs? Euphoria, Tachycardia, Tachypnea, Restlessness, Irritability, Borborygmi, hyperreflexia (+3/+4), Spastic, Seizure (need suction bad at bedside) What are the S&S’s of Downer Drugs? Respiratory Depression, Bradycardia, Bradypnea, Lethargy Overdose/Intoxication 1. “I have too much…” 2. Too much upper: Everything is UP 3. Too much downer: Everything is DOWN Withdrawal 1. “I don’t’ have enough” 2. Too little upper: Everything is DOWN 3. Too little downer: Everything is UP Pt. withdrawing from Cocaine: everything DOWN RR<12 What should you always assume to a baby born to an Addicted mom? Always assume INTOXICATION at BIRTH (first 24 hour) Assume withdrawal after 24 hours. Every alcoholic patient goes through what? Alcohol Withdrawal Syndrome (after 24 hrs) Not dangerous to themselves or others Everything Going UP Only a Minority goes through what? Delirium Tremens What is Delirium Tremens? Severe form of Alcohol Withdrawal Syndrome that can kill you (occurs after 72 hours) AWS Semi-private-anywhere Regular Diet Up Ad Lib (no activity restriction) Do not restrain DT’s Private-near nurse’s station (unstable) Clear liquids or NPO (↓ r/f seizure) Restricted bedrest (NO BA privileges) Should be restrained (dangerous) o 2 extremity restricted BOTH Anti-hypertensives going up b/c w/drawal Tranquilizer going up b/c downer B1 multi-vitamin o to prevent dementia Aminoglycosides What are Aminoglycosides? “A mean old Mycin” Powerful Antibiotics to treat SEVERE, LIFETHREATENING, RESISTANT INFECTION. TB, Septic peritonitis, Septic Shock, Aminoglycosides ends in what? -mycin (not all drugs that end in mycin are aminoglycosides. What are the 3 drugs that end in “-mycin” are not Aminoglycosides? Azithromycin, Clarithromycin, Erythromycin If it ends in “-thromycin”, throw it out (less severe) What are some examples of -mycin? Streptomycin, Tobramycin, Gentamicin, Vancomycin, Cleomycin What are the toxic effects of -mycin? When you see mycin, think MICE. 1. The world‟s most famous mouse (Ears) Ototoxicity o hearing, tinnitus, balance, dizziness 2. The human “Ear” is shaped like a kidney. Nephrotoxicity o Monitor: Creatinine (0.6-1.2) o best indicator: Kidney function o 24 hour creatinine clearance would be better than Serum creatinine3. The #8 drawn inside of the ear reminds you of: Toxic to Cranial nerve 8 (ear) Freq. of administration: q 8 hours What are the Route of Administration for -mycin? IM or IV Why is -mycin not given through the PO route? The drug is not absorbed through the PO and it will excrete. If it is not absorbed, it‟s not in the systemic (treatment not effective). What are the 2 cases -mycin is given through PO? Hepatic encephalopathy & Pre-op Bowel Surgery What is Hepatic encephalopathy? Hepatic/Liver Coma (increased ammonia in brain) What is the goal and treatment of Hepatic encephalopathy? Reduce the Ammonia in the Encephalopathy PO “-mycin” will go into the gut, & will kill gram – in the gut and sterilize the bowel. Why would you give an Oral “-mycin” before a Sx? To sterilize the bowel. What 2 PO “-mycin” is used to help sterilize the bowel? NEOmycin & KANmycin Who Can sterilize my bowel? NEO KAN What does Trough level mean? When the drug is at the lowest end. What does the Peak level mean? When the drug is at the highest What is the order of Trough level and Peak Level? TAP (Draw Trough, Administer Med, Draw Peak) What is the reason for drawing TAP levels? Narrow Therapeutic range EX: Digoxin 0.125 - .25 (narrow range> TAP req.) EX: Lasix 10-80mg (wide range>TAP not req.) Route Trough (lowest) Peak (highest) Sublingual 30 mins before next dose 5-10 mins After drug dissolves IV 30 mins before next dose 15-30 mins After drug FINISHED IM 30 mins before next dose 30 – 60 mins After drug given SQ 30 mins before next dose See Diabetes lecture “INSULIN” PO 30 mins before next dose FORGET ABOUT IT Calcium Channel BLOCKER are like Valium for your Heart What does Ca+ channel blocker do to your heart? Relax/Rest your heart (Tachycardia, Tachyarrhythmia) Name the 3 actions of Ca+ channel blocker? NEG: Inotropic, Chronotropic, Dromotropic What do the positive actions do? Cardiac stimulants (atropine, epi/norepinephrine) What do the negative actions do? Cardiac depressant (Ca+ channel blocker/B-blocker) Action Definition Positive (↑-excites) Negative (↓-depress) Inotropic Strength of Heartbeat Strong Weak Chronotropic Rate of Heartbeat Fast Slow Dromotropic Conductivity Excitable Blocks/Slow conduction What do Ca+ Channel Blockers (CCB) treat? Know what Letter it Starts with: A 1. Antihypertensives (bring BP down for HTN pt) 2. Antianginal (relaxes-decreasing O2 demand) 3. Anti-Atrial Arrythmia treats “Atrial” cardiac problems doesn‟t treat ventricular arrythmias Does CCB treat SupraVentricular arrhythmia? Yes, because atrial is above the ventricular. What are the side effects of CCB? Headache: Vasodilation in the brain (migrane) Hypotension: relaxes the heart & blood vessel Bradycardia What names end in CCB? -DIPine (dip in the calcium channel) o amlodipine, nifedipine Verapamil/Diltiazem (Cardiazem) Which CCB can be given through Conti. IV drip? Diltiazem (Cardizem) What VS needs to be measured before giving CCB? Blood pressure o SE: hypotension What is the guideline to hold CCB? HOLD, if Systolic is <100 monitor BP intermittently What would you do with the drip if the systolic was 98? Titrate it down, measure BP Cardiac Arrhythmias What is a Normal Sinus Rhythm? Peaks of p waves are evenly distanced** P wave for every QRS P wave with inverted QRS What is Atrial Flutter? Rapid-p wave depolarizations (saw tooth) What is Atrial Fibrillation & TX? No clear, Chaotic (fib) P wave (atrial) atrial has multiple rapid impulses TX: decrease HR, Decrease BP What is a Ventricular Fibrillation & TX? Chaotic (fib) QRS (ventricular) depolarization, no pattern TX: CPR & immediate De-FIB What is a Ventricular Tachycardia & TX? Wide, Sharp, Peak QRS, there is a pattern Bizarre (tachycardia) QRS (ventricular) TX: o Pulse is present= Cardioversion o No pulse= De-FIB What is Asystole & TX? A lack of QRS depolarization (flat line) TX: High quality CPR If the question says QRS depolarization, what is it talking about? Ventricular If the questions say‟s P wave, what is it referring to? Atrial What is premature ventricular contractions (PVC)? Periodic (PVC) wide, Bizarre QRS Gen. low to mod. priority, unless everyone else has a normal rhythm When should you be concerned with a PCV pt? 1. More than 6/min 2. 6 in a row 3. PVC falls of T-wave of previous beat What are 2 lethal arrhythmias (highest priority)? Asystole & V-Fib (no pulse) What do asystole and V-Fib have in common? No Cardiac Output (no brain perfusion=dead in 8min) What is a potentially life-threatening arrhythmia? Ventricular Tachycardia (has Cardiac Output) What is the Treatment for V-Tach & PVC’s (VENTRICLES)? Lidocaine (V looks like L shape) & Amiodarone Ventricular use Lidocaine (last longer)What should the RN prepare to assist with a pt. whose rhythm changed from normal to Supraventricular Tachycardia? Vagal Stimulation to temp. convert the pts. heart rate to normal sinus rhythm SE: Bradydysrhythmias, ventricular dysrhythmias, or asystole What is the TX for SupraVentricular arrhythmias (ATRIAL ARRYTHMIA)? ABCD: Adeno, Beta, Calcium, Dig A: Adenocard (adenosine) o Push in less than 8 sec (fast IV push) o Pt. goes into Asystole, but its okay they come out of it in 30sec. o When it comes to IV push, When you don‟t know go slow. B: Beta Blockers (end in “LOL”) o Similar to CCB‟s o Same: TX: Antihypertensive Antianginal Anti-Atrial Arrythmia o Same SE: Headache, Hypotension C: CCB D: Digoxin/Digitalis (Lanoxin) What is the Treatment for Ventricular Fibrillation? Defibrillation (shock) What is the Treatment for Asystole? Epinephrine, then Atropine (if Epi doesn’t work) Chest Tube What is the purpose of Chest tube? Re-establish NEGATIVE pressure in the pleural space by suctioning, so lung expands when the chest wall moves (effective gas exchange). Pneumothorax in the chest tube removes what? “Pneumo” (air) thorax in the chest tube removes Air/Gas because of the positive pressure Hemothorax in the chest tube removes what? Hemothorax removes blood Pneumohemothorax chest tube removes what? Pneumohemothorax removes both the air & blood When should you notify the HCP if you observe what to a pt. with chest tubes in for a hemothorax? When the chest tube is not draining. Notify the HCP if you observe what to a pt. with chest tubes in for a Pneumothorax? Chest tube is not “Bubbling” and if there is drainage. What are the 2 locations of chest tubes? Apical (High) & Basilar (base of lung) What does Apical remove? Removes Air (pneumothorax) (expect bubbling) What does Basilar remove? Removes Blood (hemothorax) (expected drainage) How many chest tubes are placed for a unilateral pneumohemothorax? Where is it located? 2 chest tubes will be placed. Apical & Basilar How many chest tubes for a bilateral pneumothorax? 2 chest tubes will be placed Both will be Apical (right and left) How many chest tubes for post-op chest surgery? 2 chest tubes (Unilateral) Apical (air) & Basilar (Blood) always assume chest trauma & sx is unilateral Pt with a post-op pneumonectomy, how many chest tubes? None because the lungs are removed (no pleural space) What is the RN‟s intervention if you kick over the collection bottle? Not a big deal, just sit it right back up and have the patient take a couple deep breath What are the RN‟s intervention if the water seal breaks? Positive pressure can get in the pleural space 1. Clamp chest tube (nothing gets in)-PRIORITY 2. Cut the tube away from the device 3. Submerge the open end chest tube into sterile water until system can be replaced- BEST 4. Unclamp it (air can‟t go in and stuff comes out) What should you do if the chest tube dislodges? First: Cover the hole with gloved hand BEST: cover it with Vaseline gauze dressing, taped on 3 sides Ask yourself if there is a bubbling in the chest tube? Ask: When and Where In the Water seal chamber what do you expect to see? Intermitted bubbling (good & document) *SEALED: there should not be continuous bubbling In the water seal chamber what are you not expected to see? Continuous bubbling (bad because of LEAK) 1. Start at the chest & find & locate the air leak. Tighten connection or replace drainage system. Keep connection taped securely. In the Suction control chamber what do you expect to see? Continuous bubbling (good & document) *Suction-Continuous (opposite of Water sealed) In the suction control chamber what do you not expect to see? Intermitted bubbling (BAD because the suction is too low and you want to turn it UP) Chest tubes should not be clamped for longer than what? 15 secs without a HCP order What should you use to clamp? Rubber tip (it won‟t puncture) double clamps (safety) Congenital Heart Defects: Every Congenital Heart Defect cause what? TRouBLe or No Trouble All CHD will have what and need what done? Heart murmur (shunt of blood) & echocardiogram Troubled CHD needs what? Surgery to live, delayed growth & development, shorter life expectancy, financial difficulties, exercise intolerance, Pediatric cardiologist Troubled CHD shunts blood from which direction? Right to Left (TRouBLe) No-Trouble CHD defect is shunting blood from which direction? Left to Right: What type of shunts are cyanotic (BLUE)? Right to left (TRouBLe) What type of shunts are acyanotic? Left to Right What kind of Troubled heart defects starts with the letter T? Tetralogy of Fallot What are the 4 defects of Tetralogy of Fallot? VarieD PictureS Of A RancH or V-Days Pick Some One A Red Heart Ventricular Defect Pulmonary Stenosis Overriding Aorta Right HypertrophyInfections Disease & Transmission Based Precautions: What are the 4 levels of Precaution Standards? Standard/Universal Precautions (Tier One) Contact, Droplet, Airborne What disease are considered a Contact precautions? Anything Enteric (fecal/oral) o C-diff o Hep A o Herpes simplex o MRSA o Staph infections o Rotavirus What are the Nursing Interventions for Contact precautions? Private room preferred & may be in the same room who has infection with same organism. Gloves & Gown (visitors & staff) Disposal of infectious dressing material into nonporous bag What disease are considered Droplet precautions? Prevent the transmission of pathogens the spread within 3 feet with mucous membranes or respiratory secretions Meningitis Haemophilus influenzae (causes epiglottitis) Streptococcal pharyngitis Scarlet fever Mumps, Rubella, Pertussis Pneumonia What are the Nursing Interventions for Droplet precautions? Private room preferred & may be in same room who has infection with same organism Gloves, Mask (within 3 ft of the pt.) Keep door closed What disease are considered Airborne Precautions? Disease transmitted by air for infectious agent smaller than 5mcg. Measles Varicella (Chicken pox) Herpes Zoster (shingles) TB What are the Nursing Interventions for Airborne precautions? Private room preferred & may be in same room who has infection with same organism Negative airflow (air exchange & air discharge through HEPA filter) Keep door closed Mask (RN must FIT tested for N95 respirator) Surgical mask if pt is leaving the room When would you use the N95 respirator mask? Known or suspected TB patient Order to put ON the Personal Protective Equipment? Gown, Mask, Goggles/face shield, Gloves What is the order to take OFF the PPE? Always take it off in alphabetical order: Gloves Goggles Gown Mask Crutches/Canes/Walkers How do you measure the length of the crutch? 2-3 finger widths Below the anterior axillary fold to a point lateral to and slightly in front of the foot No landmarks on the foot or axilla***(rule out) What do you measure next? The hand grip (adjusted up/down) How do you know if the hand grip is properly placed? The angle of elbow flexion is about 30 degree‟s Crutches: Non-weight bearing (ATI) 1. Begin in tripod position, maintain weight on “Unaffected”. 2. Advance both crutches and the affected extremity. 3. Move the unaffected weight-bearing foot/leg forward. 4. Advance both crutches, and then the affected extremity Crutches: Weight bearing (ATI) 1. Move crutches forward about 1 step‟s length 2. Move “affected” leg forward: level with crutch tip3. Move the “unaffected” leg forward 4. Continue sequence making steps of equal length How do you crutch a 2-point gait? (even) Move a crutch and the opposite foot together Mild Bilateral weakness o Early stage rheumatoid arthritis o Bilateral total knee replacement (3-wk) How do you crutch a 3-point gait? (odd) Move 2 crutches and the bad leg together One leg is affected o first day Right total knee replacement ATI: Unaffected leg bears wt. Wt-bearing indicated with solid foot & crutch tips. How do you crutch a 4-point gait? (even) Left crutch followed by Right foot, Right crutch followed by Left foot Severe Bilateral weakness o Advanced ALS o Bilateral total knee replaced (wt. allowed) How do you teach a “swing-through” gait? Used for non-weight bearing (amputations) right hip post-op non-weightbearing Can you bear weight for an amputation with prosthetic? Yes, you can bear-weight Patient teaching for going up the stairs with crutches. Go up with your good (lead with your foot), then your crutches. (crutches move with bad legs). Hold onto tail with one hand & cutches with the other hand Push down the stair rail & the crutches Step up with the unaffected leg If allowed to place weight on affected leg, hop up with the unaffected leg Bring the affected leg and the crutches up beside the unaffected leg Remember, Good leg goes up first and the crutches move with the Bad leg. Walking down the stair: (ATI) Place the affected leg & the crutches down on the step below; support weight by leaning on the crutches and the stair rail Bring the unaffected leg down Remember, bad leg goes down first and the crutches move the bad leg. Which side should you hold the cane? Stronger side of your body How do you measure cane for a patient? Measure from the greater trochanter to the floor.How many inches should the cane move forward? Move can forward 6-10 in, then move the weaker leg forward and advance with stronger leg past the cane. How do you measure the correct size for walker? Pts. wrist are even with hand grips on the walker when arms are dangling downward. How many inches should you advance the walker? 12in, and advance with bad leg, then move good leg forward. If the patient wants to tie something to the walker, where should they tie it? On the side and not the front because of tipping over. Rolling walker should be avoided with what disease? Parkinson‟s disease due to shuffling gait Mental Health: Nonpsychotic Vs. Psychosis What is important to know for a mental health quest.? Ask yourself: If patient is psychotic or Non-psychotic What is seen in a non-psychotic patient? Has insight: know they are sick & it‟s messing their life. good therapeutic communication (normal pt.) What are seen in psychotic patient? Doesn‟t think they are sick & no insight Blame everyone else S&Ss: Delusions, Hallucinations, Illusions What is delusion? False fixed (don‟t change) idea of belief No sensory component (no hearing, sensor) What are 3 types of delusions? Paranoia, Grandiose, Somatic What is a Paranoia delusion? Fixed belief people are out to harm you (distrust) What is a Grandiose delusion? Fixed belief you are superior (you are Christ, best..) What is a Somatic delusion? False fixed belief about you body part (invisible, xray) What is a hallucination? False fixed Sensory experience What are the types of hallucination? Think about 5 senses: Auditory (voices telling you to harm yourself) Visual (seeing things not there) Tactile (Feeling things not there) Gustatory (tasting) Olfactory (smelling)What is an Illusion? Misinterpretation of reality (sensory experience) What is the difference b/t hallucination & illusion? Illusion there is a referent in reality What is a referent? There is actually something there and they are misinterpreting it. (ie: pt overhears and misinterprets) What are the 3 types of psychosis? Functional, Dementia (Alzheimer’s), Delirium What is functional psychotics? They can function (live alone, job, family) What are the 4 types of functional psychotics? 1. Schizophrenic 2. Schizo-affective Disorder 3. Major depression 4. Manic-Bipolar What is Dementia? Progression brain disease (senile/Alzheimer‟s) What is Delirium? Temp. sudden dramatic secondary loss of reality usually d/t chemical imbalance in the body How to answer these questions: 1. Ask yourself, are they psychotic or non-psychotic? 2. If non-psychotic, pick the best therapeutic communication response. 3. If psychotic, decide which 3 categories that person falls in. Functional (potential to learn reality) 1. Acknowledge their “feeling” 2. Present “REALITY” 3. Set limit (“topic is off limits”) 4. Enforce the limit Abnormal: Antisocial, Borderline, Narcissistic: treat like functional Dementia (brain damage, can‟t learn) 1. Acknowledge their feelings 2. REDIRECT them a. Don‟t‟ present reality b. Don‟t change subject c. Reorient them 3. S&Ss: Rapid Delirium (remove the underlying cause) 1. Acknowledge their feelings 2. REASSURE them a. patient safety 3. S&Ss: Slow Narrow self-concept: Functional psychotic refuses to leave their room or change their clothes. Flight of ideas: thought to thought Word salad: Random words Idea of Reference: Pt. thinks everyone is talking about them. Diabetes What is Diabetes? An error in glucose metabolism lack of insulin or resistance to insulin What is “Diabetes” Insipidus? DI: polyuria, polydipsia leading to dehydration d/t low Antidiuretic hormone. fluid volume deficit because of polyuria (DM) USG<1.01 What is Syndrome Inappropriate Anti-diuretic hormone? S&S‟s opposite of Diabetes Insipidus: Low urine output (oliguria) Not thirsty Wt. gain High Specific gravity >1.03 What is the relation of amount of urine and specific gravity? Less the urine output=higher the specific gravity (vice-versa) What is Type 1 DM? Insulin dependent, Juvenile onset, Ketosis prone What is the S&S‟s of Type 1 DM? Polyuria, Polydipsia, Polyphagia What are the treatment for Type 1 DM? DIE: Diet, Insulin (most important), Exercise What is Type 2 DM? Non-insulin dependent, Non-ketosis prone What are the treatment for Type 2 DM? DOA: Diet(most important), Oral hypoglycemia, Activity What is the primary diet modification is what? 1. Calorie restriction (1,600 calories/day) (BEST)2. 6 small feedings/day (1,600/6): keeps peak level What does insulin do to the glucose level? Lowers the blood glucose Short acting: Regular insulin A. Onset? B. Peak? C. Duration? Clear solution (IV drip), Rapid & Run, Take before meal A. Onset: 30-60 mins (1 hr) B. Peak: 1-5 hours (2 hrs) C. Duration: 6-10 hours (4hr) Intermediate: NPH (SQ) A. Onset? B. Peak? C. Duration? Cloudy (Never IV), Not so fast & Not in bag, After meal A. Onset: 1 - 2 hour (2) B. Peak: 6 -14 hour (6) C. Duration: 16-24 hour If you give N at 7 when would you check Rapid-acting: Lispro/Humalog A. Onset? B. Peak? C. Duration? Give with meal A. Onset: 15 – 30 mins B. Peak: 30-2.5 hour C. Duration: 3-6 hour Long-acting: Glargine/Lantus A. Onset? B. Peak? C. Duration? Slowly absorbed: little – no risk for hypoglycemia Safe to give at bedtime*** A. Onset: 70min B. Peak: None C. Duration: 24 hour What action invalidates the bottle expiration date? After you open the bottle, New exp: 30 days What should you teach your patients? Refrigerate their insulin at home. Exercise can cause what? Exercise is like another shot of insulin, they have to eat. What happens to the blood glucose level if Diabetic patient gets sick? Hyperglycemia & Dehydration. They have to take their insulin even if they are not eating. Stay active as possible. Take sips of water (r/f dehydration) What is the cause of Hypoglycemia? Too much insulin/meds: Not enough food, too much exercise What are the S&S’s of Hypoglycemia? “DRUNK + Shock”: Drunk: staggering gait, slurred speech, impaired judgment, delayed reaction time, labile (emotion all over the place) Shock: Low BP, High HR, tachypnea, Cold, Pale, Clammy, mottled, patchy skin, diaphoresis What is the treatment for hypoglycemia? “Rapidly metabolized carbs” (Sugars): Juice, Soda, Candy, ½ skim milk, OJ/apple juice (sugar) & crackers/turkey(starch) What is a ratio that you want? One sugar & one starch; one sugar & one protein What is the treatment for hypoglycemia if the pt. is unconscious? Glucagon (IM): if at home setting D10W/D50 IV: IV in ER setting What is the cause of Hyperglycemia in Type 1- DKA? Diabetic Coma or Diabetic „Ketoacidosis” Acute viral upper resp. infection within last 2 wks too much food, not enough meds or exercise What are the S&S‟s of DKA? Dehydrated (hot, flushed, dry skin -“car”) Ketones in BLOOD Kussmaul (hyperventilate) hyperKalemia, Acidotic Acetone breath (fruity breath) Anorexia d/t nausea *use Insulin, more priority than HHS What are the causes of Hyperglycemia in Type2-HHS HHS: Hyperglycemic “hyperosmolar” syndrome (Fatal) Causes: DEHYDRATION (hot, flushed, dry) USG<1.01 What is the treatment for HHS? IV fluids (rehydration) What are the chronic complications of DM? Poor tissue perfusion & peripheral Neuropathy Which lab test is the best indicator of long-term blood glucose control? HbA1C (glycosylated hemoglobin) What is a good number for HbA1C? Good: <6% What number needs evaluation? 7 -Maybe What number is out of control for HbA1C? >8% What is the order for mixing NPH & Regular insulin? Clear to cloudy: NRRN Inject air into the NPH, then inject air into the Regular, Draw up the Regular, Lastly, Draw NPH Endocrine glands: When you hear “Hyperthyroidism”, turn it into what? Hyper-Metabolism (↑T3 & T4, ↓TSH) What disease is hyperthyroidism? Graves Disease “Run yourself into the Grave” What are the S&Ss of hyperthyroidism? Wt. loss, High HR, Low BP, irritable/hyper, heat intolerance, cold tolerance, heat Intolerance, exophthalmos What 3 treatments are available for hyperthyroidism? Radioactive Iodine, PTU, Thyroidectomy What are the precau. for pt. with radioactive Iodine thx? Stay away from preg., immunocompromised pts. Limited contact to less than 1 hr Flush toilet 3x If the pt. spill urine, call HAZMAT team What is Prophylthiouracil (PTU)? PTU: Puts Thyroid Under (↓ thyroid production) What should you RN monitor for pt. taking PTU? Monitor WBC (immunosuppression – cancer dx) What is thyroidectomy? Surgical removal of the thyroid Total thyroidectomy needs what? Lifelong hormonal replacement R/F hypocalcemia (parathyroid taken out) o Paresthesia(1st sign), tetany, tremor, spasm, irritability, tachycardia, HTN What two signs are present for total thyroidectomy? Positive Chvostek‟s & Trousseau‟s signWhat is a positive Chvostek‟s sign? twitching of the facial muscles in response to tapping over the area of a facial nerve (hypocalcemia) What is a positive Trousseau‟s sign? Temporarily occlude arterial blood flow (with BP cuff inflated) above the normal systolic pressure and spasm of the wrist & hand occurs (hypocalcemia) What‟s priority for tx Chvostek & Trousseau‟s sign? IV calcium gluconate or calcium chloride Subtotal thyroidectomy does not need life-long hormonal replacement why? Remaining thyroid tissue usually supplies enough thyroid hormone for normal function Subtotal thyroidectomy are at risk for what? Thyroid storm/crisis (MEDICAL EMERGENCY) o large amounts of thyroid hormones in bloodstream causing greater increase in body metabolism What are the S&S‟s of Thyroid storm/crisis? Hyperthermia - Increase temp >105 Extreme High BP >210/180 (stoke category) Severe Tachycardia (180‟s) Psychotic delirium- brain damage What are the treatments for Thyroid storm/crisis? Maintain patent airway & administer O2 @ 10L Provide ice pack or cooling blanket Administer acetaminophen (↓temp) - ATI What are the Post-op R/F? AIRWAY*** (edema), Hemorrhage Never pick infection in the first 72 hours*** What are the Post-op Total R/F for 12-48hr? Tetany (muscle spasm) d/t Low Calcium and can cut off your airway at the larynx. What are the Post-op Subtotal R/F for 12-48? Storm What is Hypothyroidism & TX? Low metabolism (↑TSH, ↓T3 & T4): TX: levothyroxine What are the S&S‟s of hypothyroidism? Wt. gain, fatigue/weakness, cold Intolerance, heat tolerance (can‟t tolerate what you are), bradycardia, hypotension Hypothyroidism are at risk for what? Myxedema coma o d/t uncontrolled/untreated hypothyroidism and the patient is hypothermic with changes in mental function from depression to unconsciousness. What is the r/f for myxedema coma? Resp depression & cardiovascular collapse d/t severely depressed metabolism Patient in Myxedema Coma needs to avoid what drug? Sedatives (ambian & anesthetic agents) Adrenal Cortex Disease: All starts with A & C What are some examples of Adrenal Cortex disease? Addison‟s, Cushing‟s, Conn‟s What is Addison‟s Disease? Under secretion of adrenal cortex hormone (steroids) What are the S&S‟s of Addison‟s disease? Doesn‟t adapt to stress ↓Steroid, ↓Sugar, ↓Sodium, Skin (hyperpigmented) What happens if the patient with Addison‟s disease experience stress? Decrease in BS & decrease in BP = SHOCK What is the treatment for Addison‟s disease? Give what the patient is low on: Steroids Prednisone, Cortisone, Hydrocortisone What is Addisonian crisis (adrenal crisis)? Signs of shock:Hypotension, tachycardia, tachypnea, pallor d/t stress What is the treatment for Addisonian Crisis? Iv fluid replacement and IV steroids (maybe resp. thx) What is Cushing‟s syndrome? Over production of glucocorticoid What are the S&S‟s of Cushing syndrome /SE steroid? ↑Steroid, ↑Sugar, ↑Sodium, Skin (thin, fragile, striae) Moon face, buffalo hump, hirsutism, truncal/central obesity (apple body), gynecomastia (breast), immunosuppressed. retaining NA & H20, losing K+, What does patient with Cushing‟s syndrome say? I am mad. I have infection: irritable, immunosuppression What is the treatment for hypersecretory gland? Unilateral or bilateral adrenalectomy What should you monitor for post-op adrenalectomy? Adrenal insufficiency (Addison‟s disease) Children Toys What are 3 things to consider when selecting toys? Is it safe? Is it age-appropriate? Is it feasible? (easy) What are 3 safety consideration? No small toys for children <4yr old No metal/ “die-cast” toys if O2 is in use (sparks) Beware of fomites (nonliving object that harbors microorganisms-stuffed animals) What are age- appropriate toys for 0-6months? musical mobile, snake rattles, (sensory/motor) Soft-large Play pat-a-cake, chewing on teething toys What are age-appropriate toys for 6-9 months? Working on object permanence Cover/uncover toy, peek a boo, jack in the box Large plastic/wood/metal What is the worst toy for 6-9months? Musical mobile, they can strangulate because now they can sit up. What are age-appropriate toys for 9-12 months? Learning to speak speaking toys, talking books What words should you not pick if the child is <9 Build, stack, sort, stack, make, construct because kid ismonth? not purposeful until 9months. What are age-appropriate toys for toddlers (1-3)? Work on gross motor skills, parallel play Push/pull toy, running/jumping What should you not pick for toddlers? Anything with finger dexterity Cutting, using pencils What are age-appropriate toys for preschoolers (3-6)? Finger dexterity/ working on balance, associate play with some cooperation Tricycles, tumbling/dance class, coloring, pretend play & “dress up”, imaginary friends, What are age-appropriate toys for school age (6-12)? Characterized by TRIPLE C‟s Create/Craft: blank paper, colored pencils) Collective: (Pokemon card, Digimon, beanie babies) Competitive: Play is competitive/cooperative What are age-appropriate toys for adolescent (12-20)? Peer group association Nonviolent video games, sports, caring for a pet, When should you not let an adolescent hang out? Fresh out of postop (<12hrs) Contagious disease Immunosuppressed Laminectomy/Spinal cord What is laminectomy? Removal of vertebral spinal process winged ends of vertebrae Why is laminectomy performed? Relieve nerve root compression What are the S&S‟s of nerve root compression? 3 P‟s: Pain: Paresthesia: numbness/tingling Paresis: muscle weakness What is important to pay attention when determining prognosis, treatment, & symptoms? LOCATION: Cervical Thoracic Lumbar What is the most important assessment for Cervical? Airway (innervates diaphragm) Function of arms/hand What is the most important assessment for Thoracic? Cough (contraction of abdomen)-how well the pt coughs Bowel mechanism What is the most important assessment for Lumbar? Bladder (bladder distention or empty) Leg function What is the #1 postop for spinal or laminectomy? Log roll*** What should you not do with patient after postop? Don‟t dangle the patient‟s leg Don‟t‟ sit longer than >30mins What is the postop complication for cervical? Pneumonia because they don‟t breathe well What is the postop complication for thoracic? Pneumonia & Paralytic ileus (bowels not working) What is the postop complication for lumbar? Urinary retention followed by leg problems What is Anterior thoracic? From the front through the chest to the spine Will have chest tube (pneumohemothorax) What is laminectomy with “infusion”? Bone graft from the iliac crest How many incisions are present with laminectomy with infusion? 2 incisions, one on the hip & one of the spine Which one is more painful? Hip has the most pain, bleeding, draining What are the temporary discharge teaching (restrictions 6wks)? Sit longer than 30mins, lie flat & log roll, no driving, do not life more than 5lb (gallon of milk) What are 3 Permanent restrictions? Never lift objects by bending at the waist o Lift with legs Cervical laminectomy‟s not allowed to lift anything over their head No jerking, horseback riding, 6 flags Drug toxicity DRUG THERAPEUTIC LEV. TOXIC LEVEL S&S’s/ContraindcationDumping Syndrome VS. Hiatal Hernia What is Hiatal Hernia? (ticket for going wrong way) Regurgitation of acid into your esophagus because the upper part of stomach herniates upwards through the Lithium 1. Anti-mania, not depression 0.6 – 1.2 ≥2.0 GI distress, polyuria, fine hand tremor, renal tox. NSAID ↑ lithium level Lanoxin (Digoxin) 1. CHD 2. Atrial arrhythmias 1-2 ≥2.0 Thiazide/loop diuretic ↑r/f hypokalemia & dig. toxicity Dig. Toxicity: Abd. pain, fatigue, blurred vision, halo Antidote: Digoxin immune FAB Amino/Theophylline 1. Airway antispasmodic 2. Relaxes muscle spasm 10-20 ≥20 Irritability/restlessness toxic effect: Tachycardia, tachypnea, seizure Antidote: activated charcoal ↓absorption Dilantin (phenytoin) [CCB] 1. antiseizure 10-20 ≥20 Constipation, reflex tachycardia, peripheral edema NO grapefruit juice pts w/ HF, bradycardia Bilirubin (Waste product from breakdown of RBC) *know NB’s level Adult: <1 “Elevated level” 10-20 ≥20 Kernicterus: o (Bilirubin in the brain) o Bilirubin >20 & causes anemia & brain damage. What position is the pt with Kernicterus display? Opisthotonos How does the opisthotonos position looks like? Hyperextend d/t irritation of the meninges. What position should you place the patient in? On their side What is jaundice? Bilirubin in the skin, thus causing yellow skin What is Pathological jaundice Yellow skin at birth, Bilirubin high at birth What is Physiological jaundice Bilirubin normal at birth, in 2-3 days turn yellowdiaphragm (2 stomachs) What is the problem with Hiatal Hernia? It is moving in the wrong direction at the right rate What are the S&S‟s of Hiatal Hernia? GERD (heartburn/indigestion) ONLY after you lay down right after you eat What is the treatment for Hiatal hernia? “In Hi-atal hernia, everything needs to be high, except protein” You want stomach to empty FAST because if it‟s empty it won‟t reflux Fowler position HOB (gravity empties it faster) HIGH fluid (liquid), High Carb (carb empty fast) LOW PROTEIN What is Dumping syndrome? Occurs after gastric surgery Why does Dumping syndrome occur? (speed ticket) It is moving fast but at the right direction What are the S&S‟s for dumping syndrome? DRUNK: staggering gait, slurred speech, impaired, labile (emotions) SHOCK: hypotensive, tachycardia, cold (vasoconstriction), pallor, clammy skin Acute abdominal distress: Borborygmic (bowel sound), cramp, bloating, distention, tenderness, pain What is the S&S‟s of hypoglycemia? DRUNK & SHOCK DRUNK + SHOCK + Acute abd. distress is what syndrome? Dumping syndrome What is the treatment for dumping syndrome? “when everything is low, stomach empty slow, except protein” You want the stomach to empty SLOWER Low position, HOB flat Turn to side with head down Low fluids (1-2hr before or after meals) FLUIDS NOT WITH MEALS LOW CARB (empty slow) HIGH PROTEIN If carb is low, Protein is what? OPPOSITE Electrolytes:KALEMIAS (K+) do the SAME as the prefix (hyper/hypo) EXCEPT for heart rate & urine output Calcium (Ca+) do the OPPOSITE as the prefix (hyper/hypo), Exceptions What are S&S‟s of Hyperkalemia? (Increase except HR, U.O) BRAIN: everything UP (agitation, restlessness, clonus) LUNG: tachypnea Bowel: diarrhea, borborygmic, Muscle: spasticity, increased tone, reflex >+3 HEART: LOW HR, but T-waves peaked U.O: Low urine output (oliguria) What are S&S‟s of Hypokalemia? (decrease, except HR, U.O) BRAIN: everything DOWN (confusion, coma, lethargy) LUNG: dyspnea (shallow breathing) Bowel: Constipation, abd. distention, paralytic ileus Muscle: weakness, decreased reflex, flaccidity HEART: tachycardia, ST depression, U-wave U.O: Increase urine output (polyuria) What are the treatments for Potassium? Never give K+ Route: IM, SQ and IV Push (bolus) Not >40/L IV Fluid (call & clarify HCP) Why is Potassium bad? STOPS your heart (cardiac arrest) What is the fastest way to lower potassium? Give D5W with Regula insulin (fast & temp) Drive potassium into the cell, and out of blood***(Potassium in blood will KILL YOU) Why is Kayexalate used? Kayexalate is full of Na and it trades Na for K+. (oral, enema) K+ comes out and now blood has hypernatremia. What do you give after Kayexalate? “Dehydration” and now correct with IV FLUID If you see Kay-exalate, what should you remember? K+ exists slow & late in kayexalate, D5W & Insulin K+ enters early What are the S&S‟s of Hypercalcemia? “Everything goes low” Bradycardia, bradypnea, flaccid muscle, lethargy, constipation, hypoactive reflex What are the S&S‟s of Hypocalcemia? “everything goes high” Tachycardia, tachypnea, agitation, irritability, clonus, +4 reflex, seizure, diarrhea What are the 2 signs present in hypocalcemia? Chvostek‟s Sign: tap the cheek & face spasm Trousseau‟s Sign: hand spasm when you put a BP cuff Chvostek‟s sign is an indication of what? Sign of neuro muscle irritability associated with low calciumMagnesium do the OPPOSITE. IN a TIE b/t Calcium & Magnesium, don‟t pick Magnesium. If it‟s about nerve/skeletal pick calcium, heart pick potassium. What are the S&S‟s of Hypermagnesium? Bradycardia, bradypnea, flaccid muscles, hypoactive reflex, constipation What are the S&S‟s of Hypomagnesium? Tachycardia, agitation, irritability, tachypnea, diarrhea, borborygmic, spastic muscle, hyperreflexia, seizure Sodium: HypErnatremia “E” Dehydration HypOnatremia “O” Overload What are the S&S‟s of HypErnatremia? Hot, flushed, dry skin Increased USG, dark urine weak, thread pulse Poor skin turgor What disease has hypernatremia? DKA (dehydration), DI, HHS, What are the S&S‟s of HypOnatremia? Increased wt. & edema hyponatremia pt. is placed on what restriction? Fluid restriction, Placed on Lasix What disease has hyponatremia? SIADH What is the earliest sign of any electrolyte disorder? Numbness/tingling (Paresthesia) Circumoral paresthesia (in the mouth) The universal S&S of electrolyte imbalance? Muscle weakness (paresis)Psychotropic Drug All psycho drugs cause what? Hypotension (↓BP) & Wt. gain Phenothiazines is what kind of class of drug? Typical antipsychotics (1st generation-Old) All Typical antipsychotics ends with what? “Zines” ZzZzZz (sedative) What is the action of Typical antipsychotics drug? Reduce symptoms (no cure) If you see ZzZzines (large doses) think what? Zaney ->Psychotics (crazy) Small doses of zines are used for what? Antiemetics (nausea) Phenothiazines are MAJOR what? Tranquilizers What are the Side-Effects of major tranquilizers? ABCDEFG: A: anticholinergic (dry mouth) B: blurred vision C: Constipation D: Drowsiness E: EPS (parkinsonism- Benztropine/Diphenhydramine) F: Fotosensitivity G: aGranulocytosis (low WBC, immunosuppressed) What is the nrsing action if the pt. displays SE? Pt. continues to take the drug, teach the pt and notify HCP. What is the nrsing action if the pt. displays Toxic effects? Stop the Drug, & Notify HCP What is the #1 nrsg DX if the patient is on a tranquilizer? Risk for Injury/Safety issues What is the definition of Decanoate? Long-term treatment IM injection for non-compliance pt. When do you see Decanoate? Decanoate is usually seen after the name of the drug What is a Tricyclic Antidepressant? NSSRI’s: Non-Selective Serotonin Reuptake Inhibitors What is Tricyclic Antidepressant used for? Mood elevators to treat depression (happy pill) What are some examples of Tricyclic antidepressant dx? Imipramine (Trofanil), Amitriptyline (Elavil) What are the side effects of this dx: A: Anticholinergic (dry mouth) B: Blurred vision C: Constipation D: Drowsiness E: Euphoria (way too happy) What is important to teach to pts taking Tricyclic Antidepressant? IT takes 2-4weeks before you see effects of the medication. Continue to take it. (long-term) What is Benzodiazepines? Minor Tranquilizers (minor) Benzodiazepine drugs can be classified by what? They always have “ZEP” in their name What are Benzodiazepine drugs? Lorazepam, Temazepam, Diazepam (alcohol w/drawal) Benzodiazepine can be used for what besides minor tranquilizer? A: Anesthesia (pre-op) B: Muscle relaxant C: Alcohol withdrawal D: Seizures E: Help when pt. is fighting the ventilator to calm down What is important to teach pt. taking benzodiazepines? They work quickly & Do not take greater than 2-4 wks (Used for short-term therapy) What are the SE of benzodiazepine? ABCD:A: Anticholinergic (dry mouth) B: Blurred vision C: Constipation D: Drowsiness What is MAOI’s? Monoamine Oxidase Inhibitors What is MAOI’s used for? Treat antidepressant How do you distinguish MAOI’s from other drugs? Drug name rhymes: Marplan (ISOCARBOXAZID) Nardil (PHENELZINE) Parnate (TRANYCYPROMINE) What is the pt. teaching for a pt taking MAOI? Prevent hypertensive crisis What should be avoided when taking MAOI? Avoid food containing tyramine What food contains Tyramine? Fruit/Veggies: Salad BAR o No Banana, Avocados (guacamole), Raisins (dry fruit) Meats: o No Organ, preserved (smoke, dried, cured, pickled), hot dogs/cheeseburger & lunch meats Dairy: o CAN EAT MOZZARELLA/COTTAGE CHEESE o No yogurt, No chocolate, No alcohol Should not take OTC meds What is Lithium used for? Bipolar disorder: Decrease Mania, Not depression What are the SE of Lithium? 3P’s: Peeing, Pooping, Paresthesia What does the patient have SE of Paresthesia? First sign of all electrolyte imbalance: numbness/tingling What are the Toxic effects of Lithium? Tremors, metallic tastes, Severe diarrhea What is the #1 Nrsg Intervention is what? Increase fluids (give Gatorade/Powerade b/c electrolyte) What should you monitor for? Dehydration & Na levels Why should you monitor for Na level? Low Sodium = Makes Lithium Toxic High Sodium = Ineffective Lithium Toxic What is Fluoxetine (Prozac)? SSRI: Selective Serotonin Reuptake Inhibitor What are the SE of Fluoxetine? ABCDE: A: Anticholinergic (dry mouth) B: Blurred vision C: Constipation D: Drowsiness E: Euphoria When should you give & not give Fluoxetine? Give: Before Noon Don’t Give: At bedtime Why should you give Fluoxetine before NOON? It causes Insomnia Monitor what when changing doses in adolescent? Increased Suicidal Risk/Ideation What is Haldol? Schizophrenia: Typical Antipsychotic (1st generation) (long term: Decanoate) What are the SE of Haldol? ABCDEFG: A: anticholinergic (dry mouth) B: blurred visionC: Constipation D: Drowsiness E: EPS (parkinsonism- Benztropine/Diphenhydramine) F: Fotosensitivity G: aGranulocytosis (low WBC) What are the S&Ss of EPSs? Acute dystonia: severe spasms of tongue, neck, face/back EPSs: Dystonia, Pseudoparkinsonism, Akathisia (unable to stay still), Tardive dyskinesia (involuntary movement: lip smacking-late EPS) What is the treatment for EPSs? Benzotropine or diphenhyramine What is Neuroleptic Malignant Syndrome?*** Haldol Overdose (MEDICAL EMERGENCY) Who are at risk for NMS? Young white & elderly pt schizophrenic What is clinical present for a pt with NMS? Fatal hyperpyrexia (high fever) >105-108 altered LOC, dysrhythmias, BP fluctuates, Muscle rigidity How do you tell the difference between EPS & NMS? Take a temperature*** b/c NMS has High FEVER What should be the dose for elderly patient? Half the adult dose What is the RN action for pt. showing sign of NMS? STOP medication, monitor VS, apply cooling blanket, Give antipyretics (aspirin, acetaminophen) What is CloZapine? Atypical antipsychotic drug –“Zapine” - NEW CloZapine is used to treat what? Severe Schizophrenia What is the advantage of Clozapine? No SE: ABCDEF What is the Severe SE of Clozapine? “G” SE: aGranulocytosis (immunosuppression) What should the pt. monitor when on CloZapine? Monitor WBC (decreases WBC) What is Ziprasidone (Geodon)? Atypical antipsychotic dx (BLACK BOX WARNING) What is the SE of Ziprasidone? Prolongs QT interval & cause sudden Cardiac arrest Ziprasidone should not be given to pts with what? Don’t give to pts with heart conditions What is Sertraline (Zoloft)? SSRI: Selective Serotonin Reuptake Inhibitor (can be given at bedtime even though it cause insomnia) Why is Sertraline dangerous? Sertraline prevents other drugs from metabolizing, thus causing toxicity in other drugs. You need to lower the other Drug. Sertraline is contraindicated with what? St. John’s Wort, Warfarin Sertraline and St. John’s Wort taken together can cause what? Serotonin Syndrome What are the S&S’s of Serotonin Syndrome? Life-threatening: SAD-HEAD S: Sweating A: Apprehension/(appending sense of doom) D: Dizziness HEADache What should you do with a pt. on Sertraline & Warfarin? Reduce warfarin because pt. can bleed outMaternal/NB overview: How do you calculate the Delivery Date: Nagele’s Rule? First date of the last menstrual cycle, add 7 days and subtract 3 months. First date of last menstrual period: June 10th June 10th + 7 days , -3 months = March 17th What is the McDonald’s rule? The fundal height measurement should be approximate to the gestational age between 28- 32weeks What is the total average weight gain during a pregnancy? 28lbs (+/-2-3lbs) First trimester, how many wt (lbs) should the pt. gain? 1 lb/month How long is the first trimester? 3 months (1-12wks) (pt. should gain 3lbs total) Second trimester, how many wt (lbs) should the pt. gain? 1 lb/wk How do you calculate a women ideal wt. gain? EX: women in 28wk, she gained 22lbs, what is your impression? 19lbs should have gained (+3lb): ASSESS ideal wt. gain = Gestation week – 9lbs What is Fundus? It’s the top part of the uterus At what gestational stage should you not palpate the Fundus? First trimester: Fundus is not palpable until week 12 In the first trimester, If the pt. has palpable fundus or gains 10lbs what does it mean? Hydatiform mole (cancerous) What is Hydatiform mole/Molar pregnancy? Abnormal growth of chorionic villi. Grape like clusters that may develop into choriocarinoma What are the S&S’s of Hydatiform mole? Anemia, vaginal bleeding (brown), rapid uterine growth (increased fundal height), extreme nausea. What is the Diagnostic testing for Hydatiform mole? U/S & persistent, high hCG level In the 2nd trimester (12-27) Fundus is located where? Fundus is at umbilicus or below it. (mom-priority) At what week is the Fundus located at the umbilicus? 20-22weeks (end of the 2nd trimester) In 3rd trimester (28-40wks) Fundus is located where? Above the umbilicus (baby is priority) 3 Different questions in answering OB Questions When would you “First” auscultate the FHR? 8wks (earliest)/Quickening 16 When would you “Most Likely” auscultate the FHR? 10wks (mid-point)/ Quickening 18 When “Should” you by auscultate the FHR? 12wks (end range)/ Quickening By 20 What are the 4 signs of positive pregnancy? (related to presence of fetus) 1. Fetal Skeleton on X-Ray 2. Fetal presence on U/S 3. Auscultation of FHR a. (doppler with rate of 140) 8-12wks What are the Presumptive/Probable sign of Pregnancy? (subjective/objective sign) 1. All urine & blood test a. Positive Prg. Test = Probable (only hormone) 2. Signs: (alphabetical order) a. Chadwick Sign4. Examiner Palpates fetal movement b. Godel’s Sign c. Hegar’s Sign What is a Chadwick Sign? Cervical color change to cyanosis (bluish) What is Godel’s Sign? Softening of the cervical What is Hegar’s Sign? Softening of the Uterus What should be included in the patient teaching? Come in once a month until 28th week (q 4 weeks) What gestational stage should the pt. come in q 2 weeks? 28 weeks q 2 weeks until 36 weeks What gestation stage should the pt. come in q week? 36 weeks until delivery date or until week 42 What happens at week 42? C-section or induction What will happen to the patients hemoglobin? 1st trimester: Hgb 11 What will be the Hgb level in the 2nd trimester? 2nd trimester: Hgb 10.5 (normal) What will be the Hbg level in the 3rd trimester? 3rd trimester: Hgb 10 What are the discomforts of pregnancy? Morning sickness What is the nrsing action for treating morning sickness? (1st trimester) Eat “Dry carbohydrates” before getting out of bed dry crackers, ginger, raspberry Treatment Urinary incontinence treatment in 2nd trimester? Void every 2 hours until 16 weeks after delivery What is the treatment for difficulty breathing? (2nd / 3rd trimester? Tripod position: Sitting propped or sitting up and leaning over the table Treatment for Back pain (2nd/3rd trimester)? Pelvic/tilt exercise: Women tilts the pelvic forward What is TRUE LABOR? Regular, Progressive contractions What is Dilation? Opening of the Cervix (0-10cm (4in) (fully dilated)) What is Effacement? Thinning of the Cervix (thick to 100%effaced) What is Station? Relationship of the fetal presenting part to mom’s ischial spines. What is the Ischial Spine? Narrowest part of the pelvis which the baby has to fit to be born vaginal. What is neg. station? (negative news-babe not move down) Baby’s head (presenting part) is above the ischial spine What is a positive station? (positive news) Baby’s head (presenting part) is below the ischial spine What is engagement? Station is 0 (presenting part is at ischial spine) What is Lie Relationship between the spine of the mom and the spine of the baby What is Vertical lie? GOOD & compatible with vaginal birth Parallel What is Transverse Lie? (Trouble) BAD What is Presentation? Part of the baby that enters the birth canal firstWhat is the best position for birth? ROA or LOA What are the 4 stages of Labor? Stage 1: Labor phases LAT: Latent, Active, Transition Stage 2: Delivery of the Baby Stage 3: Delivery of the Placenta Stage 4: Recovery (2 hrs) What is the purpose of uterine contraction in the 1 stage? Dilate & effacement of Cervix What is the purpose of uterine contraction in the 2 stage? Push the baby out What is the purpose of uterine contraction in the 3 stage? Push placenta out What is the purpose of uterine contraction in the 4 stage? Stop bleeding & contract the uterus When does Post-partum begin? 2 hours after delivery of the placenta What is the #1 priority in the 2 phase of labor? Pain management What is the #1 priority in the 2 stage of labor? Assist with pushing/ breathing, comfort and providing cares to NB What is the #1 priority in the 3rd phase of labor? Pain management, dilation What is the #1 priority in the 3rd stage of labor? Assess VS, bleeding, fundus, Infection control How many phases are in the Labor? Latent, Active and Transitional Latent Phase Dilation: 0-4 cm Contraction: 5-30mins Duration: 15-30sec Intensity: mild Active Phase Dilation: 5-7 cm Contraction: 3-5min Duration: 30-60 Intensity: Moderate L<-(REMEMBER THIS ONLY)->T Transition Phase Dilation: 8-10cm Contraction: 2-3 min Duration: 60-90 Intensity: Strong NOTE**Contractions should not be longer than 90 seconds or closer than q 2 minutes Sign of Uterine Tetany What is Uterine Hyperstimulation? Contractions should not be longer than 90 seconds or closer than q 2 minutes When should you stop Pitocin? Contractions should not be longer than 90 seconds or closer than q 2 minutes What is Frequency? Beginning of one contraction to the beginning of the next. What is Duration? Beginning to end of one contraction What is Intensity? Strength of Contraction What should you teach? Teach to palpate with one hand over the fundus with the pads of the fingers (finger tips). How many complications of Labor are present? 18 complications & 3 protocols Painful back labor usually occurs in what labor? Occiput posterior (OP-Oh pain) labor What is Occiput posterior labor? Baby’s spine & head are pressed closer to the mom’s spine and sacrum What is the intervention for Occiput posterior? Position & PushWhat position would you place the patient in? 1. Knee-chest position (on hands and knees with rear end up in the air, brings the baby off the sacrum by gravity. 2. Push into the pt’s sacrum, provide counter pressure & relieving some pain What happens in Prolapsed cord? Medical emergency: cord comes out (presenting) because it presses on the cord & baby dies d/t lack of blood flow MONITOR: Variable Deceleration What is the nrsg intervention for prolapsed cord? 1. Push the head back up using a sterile-gloved hand, insert 2 fingers into the vaginal/birth canal & apply finger pressure to elevate fetal presenting head off the cord 2. Position in a knee-chest position What is the TX: All other complications in labor & birth: uterine tetany, uterine atony, uterine hypertension/hypotension, vena cava syndrome, eclampsia, toxemia, uterine rupture LION: 1. Left side position 2. Increase IV Fluid 3. Oxygenate pt (8-10L/min via nonbreather) 4. Noticy HCP In OB crisis, if the Pitocin/Oxytocin is running what should you do? STOP the Pitocin/Oxytocin & LION When should you not administer pain med to a woman in labor? If the baby is likely to be born when the med peaks EX: Primagravida pt is at 5cm asking for her IV push pain med. IV Push Pain meds peak in 15-30min after administration. GIVE MED EX: Multigravida pt at 8cm asking for IM pain med. IM peaks at 30-60min. DON”T GIVE MED. What is Low Fetal Heart Rate? FHR<110/min What is the action for Low FHR? BAD: Stop the Oxytocin if running, & LION Give tocolytics to inhibit contractions. cuased by Cord prolapse/cord compression, maternal hypoglycemia, Congenital heart block. What is High Fetal Heart Rate? GOOD: FHR>160 What is the action for the High FHR? Nothing is wrong: Take mom’s temp & if high give tylenol. What is low baseline Variability? BAD: Fetal heart rate stays the same (doesn’t change) What is the action for low baseline Variability? LION What is High baseline Variability? GOOD: FHR always changing (Document) What is late Decelerations? BAD: FHR slows down near the end or after a contractionWhat is the action for late decelerations? LION & prepare for vaginal birth/C-section What is Early decelerations? NORMAL: FHR slows down before or at the beginning of a contraction What is the action for Early decelerations? Document & Continue to monitor What is Variable decelerations? VERY BAD: Abrupt slowing of FHR <110/min This occurs with prolapsed cord What is the action of the Variable decelerations? LION Variable Cord Compression Move Pt. Early Decele Head Compression Identify labor program Acceleration Ok No action needed Late Decele Placental insufficiency Execute actions immediately 2nd stage (delivery of the baby) what is NRSG Action: 1. Deliver the head 2. Suction mouth, then nose 3. Check for nuchalc (neck) cord 4. Deliver the shoulders & the body What should the baby have before leaving the delivery area? MUST HAVE ID BAND 3rd stage (delivery of Placenta) what is NRSG Action? Make sure all of the placenta is there Check for 3-vessel cord (2 arteries/1 vein) AVA 4th stage (Recovery stage) what is NRSG Action? First 2 hours after delivery of placenta: 4 things to do 4 times an hour (q 15mins) in 4th stage. VS & assessing for S&S shock (tachycardia/hypotension-pale, cold, clammy) Check Fundus o Boggy -massage it o Displaced- void/catheterize Check the perineals pad o Excessive bleeding is saturating (98%) full pad q 15 (NOT BAD): o Saturated: BAD o Change the pad each time you check Roll her over o Check for bleeding underneath b/c pad displacement could mean pads are not the best indicator for bleeding How many times do you assess postpartum pt? Every 4-8hours depending on the woman’s stability What do you assess in Postpartum pt? BUBBLE-Head What does the B stand for? Breast (not important) What does U stand for and assess for what? Uterine***(important) Firm o If boggy: massage At midline o Not at the midline: void/catheterize Fundal height = the day of the postpartum What does the Fundal Height tell you? The day of the postpartumHow do you tell the location of the Fundal height? 1 hour post-birth: Fundus is at the umbilicus at midline. After 1 hour, it goes down by 1 cm or finger breadth a day. -3,-2,-1,(0-midlin), 1,2,3 What does BB stand for? Bowel & Bladder (not important) What does L stand for? Lochia *** What are the 3 colors in Lochia? Rubra, Serosa, Alba What is the color of Rubra? Red (Ruby) What is the color of SeROSA? Pink What is the color of Alba? White (Albino) When is considered in bad in the Rubra? Saturation (bad) What does the 1st E stand for? Episiotomy What does the Episiotomy stand for? Surgical cut made b/t the opening of the vagina and the perineum. What does 2nd stand for? Extremities*** What should you check for in the Extremities? Check for Thrombophlebitis How should you check for thrombophlebitis? Best: Bilateral calf circumference measurents What is Homan’s sign? Discomfort behind the knee on forced dorsiflexion of the foot (not the best) What does the E stand for? Emotional status What does A stand for? Affect What does D stand for? Discomfort What are the 3 big things to know for postpartum? Fundus, Lochia & Extremities (thrombophlebitis) What are some normal variations for NB? Erythema toxicum neontorum (rash) Caput Succidanum (symmetrical) o Crosses Suture, Symmetrical/Bruise Cephalohematoma Hyperbilirubinemia o Physiologic jaundice appear after 24 hrsOB MEDICATIONS: What is the action of Tocolytics? Stop the labor (threatening premature labor) What are some Tocolytic medications? Terbutaline & Magnesium Sulfate What is the SE of Terbutaline? Stops the labor & maternal tachycardia (increase HR) What is the action of Mg. Sulfate? Stops the muscle contraction (stop labor) What is the SE of Mg. Sulfate (Hypermagnesium)? ↑Mg Sulfate = ↓everything Everything goes down bradycardia hypotension (↓BP) respiratory depression absent deep tendon reflex What should the RN monitor for pt. on Mg. Sulfate? Respiration (>12) & Reflexes +2 When should you slow down the Mg. Sulfate? RR <11 & Reflex <+1 What is the action of Oxytocic? (opposite of tocolytics) Stimulate & strengthen labor What is the SE of Oxytocin/Pitocin? It can cause Uterine hyperstimulation What is uterine hyperstimulation? Contractions >90 seconds & Closer than 2 mins What is the SE of Methergine/ergometerine? Causes Hypertension (↑BP) What are the meds. to help mature the fetal lungs? Betamethasone & Survanta (Synthetic Surfactant) What is the action of Betamethasone & Survanta? Help mature the NB’s lung Betamethasone is given to who? (mom or baby?) MOM What is the route of administration for Betamethasone? IM (90 ) When is Betamethasone given? (before birth or after) Before Survanta is given to which pt? mom or baby? Baby What is the route of administration for Survanta? Trans-trachial (blown through the trachea) When is Survanta given? (before birth or after) After birthMedication Help & Hints What is Humulin 70/30? Mix of Insulin of Regular & NPH The 70% is which Insulin? NPH (intermediate acting) The 30% is which Insulin? Regular (short-acting) Examples: If you gave 50 units of 70/30 how many units N would there be? 50* 70% = 35 NPH 50* 30%= 15 Regular Can you use the same syringe to draw up 2 insulins? Yes What is the step for mixing insulins? NRRN: Inject Air into the NPH (pressurized NPH vial) Inject Air into the Regular Draw up Regular Draw up the NPH What needle should you use for an IM injection? Gauge and needle IM (I looks similar to #1) 21 G, 1 inch. What needle should you use for an SQ injection? SQ (S looks like #5) 25 G, 5/8 inch. HeParin (exoparin) IV or SQ Works immediately Short term use (cannot be use >3weeks) o Except for Lovenox (can be used longterm) Antidote: Protamine Sulfate Lab test to Monitor: PTT ( o (partial thromboplastin) Safe for Pregnant Woman Warfarin (Coumadin) PO only Takes few days to a week to start showing effect Can take it forever Antidote: Vit. K (phytonadione) Lab test to Monitor: PT & INR o Partial thrombin o INR (derived from PT) Not safe for Preg. woman What major antipsychotic can be given to preg. pt? Haldol Any diuretic ending in the letter “X” (-semides), exes out what? Wastes K+ plus hydrochlorothiazide (hear the X sound) If it doesn’t end in X and its not hydrochlorothiazide, what does it do? Spare or water Potassium? Spares K+ What is the action of Baclofen? Muscle relaxants What are the 2 side effects of Muscle relaxants? Fatigue, Drowsiness & Muscle weakness What are the 3 teachings for Baclofen? Don’t drink, drive & operate heavy machinery that requires alertness. What is the action of Flexeril? Muscle Relaxant (FLEX)Pediatric Teaching: How many stages are there in Piaget’s Theory of Cog. development? “know how to teach a teaching by using Piaget” Sensorimotor Stage Pre-Operational Stage Operational Stage Concrete Stage What is the age for the Sensorimotor Stage? 0-2months What is important to focus on WHEN providing teaching? Teach at the MOMENT when and while they do it because they are Totally present oriented (no past or future) WHAT should you teach them? Teach them what you are doing (Present) HOW should you teach a patient in the Sensorimotor stage? Teach verbally. While we do it, we will tell him what we are doing. MOSTLY teaching parent** What is the age for the Pre-Operational Stage? 3-6 years (Pre-schooler) What is important to focus on WHEN providing teaching? Imaginative, Fantasy-oriented, Illogical, CANNOT REASON with them WHAT should you teach them? They understand the past & future Pick the answer (“2 hours before”, “the morning of”, “the day of”) They understand the past & future WHAT should you teach a patient in the PreOperational stage? What you are going to do now (Future) HOW should you teach them? Play, (stories or dolls) What is the age for the Concrete-Operational Stage? 7-11 years old What is important to focus on WHEN providing teaching? They are RULE-ORIENTED They live & Die by RULES. NO ABSTRACT. Only one way to do things and other things are wrong. Cannot manage their own cares because it involves decision making and won’t seek help) WHAT should you teach them? Teach them days ahead of time. If you explain “this is what will happen” then that’s exactly how it’s going to happen and they won’t imagine anything else. WHAT should you teach a patient in the ConcreteOperational stage? What you are going to do, plus skills (will do exactly how you teach them) HOW should you teach them? Use age-appropriate reading & demonstration What is the age for the Formal-Operational Stage? 12-15years old What is important to focus on WHEN providing teaching? Teach them like an adult. Abstract thinking Think Cause & Effect Able to Manage their own Cares (seek help)Psych Questions: What are the 7 Principles to follow when answering Psych Questions? 1. Phases of therapeutic Relationship 2. Gift-Giving (Don’t except gifts from Psych pt) 3. Don’t give advice (know pt’s feeling) 4. Don’t give guarantee 5. Immediacy (keep the patient talking) 6. Concreteness (Don’t use slang) 7. Empathy a. nurse accepts the pt’s feelings as being valid, real, and worthy of action What are the 4 step process for empathy questions? 1. Recognize that its an empathy question a. usually have a quote in the questions b. each answer option is a quote as well 2. Put yourself in the pts shoes 3. ask yourself how you would feeling 4. Choose the answer that reflects that feeling or anything close. a. Do not chose the answer that reflects their words. Think about feeling.Prioritization, Delegation & Staff Management: When prioritizing what are you looking for? Sickest or the healthiest What 4 parts are included in a prioritization question? Age, Gender, Diagnosis & Modifying phrase What is most important to focus on prioritization question? Diagnosis & “Modifying phrase” What are the 4 rules in prioritization? 1. Acute beats Chronic 2. Fresh Post-OP (12hrs) beats medical/other Sx 3. Unstable beats Stable Stable Patient “Stable” Chronic Illness Post-op >12 Local or Regional Anesthesia Level A or B labs Discharge patients Admitted longer than 24 hrs Unchanged assessments Experiencing the typical & Expected S&Ss of the disease Unstable Patients Unstable Acute illness Post-op<12 Gen. Anesthesia Lab abnormalities C or D o D: Highest priority K+>6 pH<6 CO2: 60’s O2: 60’s Platelet<40,000 o Lab level in C: Priority INR>4 K 5.4-5.9 Hgb<8 CO2: 50’s PaO2: 70’s O2<93 Abnormal Na WBC<5,000 ANC<500 CD4<200 Platelet<90,000 Not ready for discharge Newly admitted or Admitted <24hours Newly diagnosed Changing or Changed Assessments Experiencing unexpected S&Ss What are some things that are unstable whether its expected or not? Hemorrhage (Bleeding-check if its expected) High fever >105 (r/f seizure) Hypoglycemia (brain & tissue damage) No pulse, no breathing. When Triaging at an unwitnessed disaster/response scene, When is a patient has:who will you Black Tag? no pulse no breathing fixed/dilated pupils What is the order of organ vitality? 1. Brain 2. Lung 3. Heart 4. Liver 5. Kidney 6. Pancreas Delegations: DON” T DELEGATE TO LPN NO IV’s: o Can’t START IV o Can’t Hang or mix IV meds o Can’t Push IV meds They can maintain IVs/Doc. flow NO Blood Products NO Central line care NO Planning care NO performing/developing teaching o They can Reinforce teaching NO Unstable Patients NO INITIAL PERFORMANCE/TASK o they can reinforce teaching DON”T DELEGATE TO UAP Charting o except for what they did (bed bath given, side rails up; but not about pt less anxious) Meds o except OTC topical barrier creams Assessments/evaluating o except VS Treatments TASKS to DELEGATE TO LPN Monitoring findings (as input to RN’s ongoing assessment) Reinforce pt. teaching from standard care plan Perform tracheostomy care Suctioning Checking NG tube patency Administering enteral feeding Inserting Urinary catheter Administer Medications (except IV meds) TASKS to DELEGATE TO UAP ADLs but not the INITIAL Specimen collection Intake/Output (stable patients) Bathing, Bed-making, Grooming, Dressing Toileting (bed pan) Ambulating Feeding (w/o swallowing precautions) Positioning Routine tasks Bed-making Specimen collectionStaff Management: When you get a staff, question ask yourself what? Is what they are doing illegal? If yes: Tell the Supervisor If what they are doing is not illegal, ask yourself what? Is anyone in immediate danger? If Yes: Confront immediately and take over If what they are doing is illegal/harmful what should you do? Confront first, tell supervisor later Is the behavior legal & not harmful, but inappropriate? If Yes: talk to them at a later date What are the 5 rights of Delegation? 1. Right Task a. repetitive & req. little supervision & invasive 2. Right Circumstance a. assess health status (stable) 3. Right Person a. task w/in scope of practice b. have necessary training/competence 4. Right Direction/Communication a. Date, method/Time and report findings, task to be performed an expected results 5. Right Supervision/Evaluation a. clear direction b. expectations to be performed c. provide feedback d. intervene if necessary (unsafe skill) e. evaluate task/identify improvementClick & POINT: What are the locations of the organ in the abdomens RUQ: Gallbladder, Bile duct, Ascending colon LUQ: Stomach, spleen, Duodenum, Pancreas, Descending colon RLQ: Appendix, Cecum (AC) LLQ: Anus, Rectum, Small Intestine (ARS) What are the valves of the Heart? APE-To-Man 1. Aortic 2. Pulmonic 3. Erb’s point 4. Tricuspid 5. Mitral (apical pulse) Where is the Aortic valve located? 2nd intercostal space at the Right sternal border Where is the Pulmonary valve located? 2nd intercostal space @ Left sternal border Where is the Erb’s valve located? 3rd intercostal space @ Left sternal border Where is the Tricuspid valve located? 4th intercostal space @ Left sternal border Where is the Mitral (apical) valve located? 5th intercostal space in Midclavicular lineHow to Guess: If you don’t know the answer after In psych, the best guess is what? 1. Nurse will examine their own feelings 2. “Establish a trusting relationship” In Nutrition, if you don’t know pick this? 1. In a tie, PICK GRILLED CHICKEN 2. CHICKEN’s unavailable, PICK FISH (not shellfish: lobster b/c high in LDL) 3. Neve pick Casseroles for children 4. Never mix medication in children’s food 5. Finger food for toddlers/mania patient 6. Preschoolers don’t need to eat as nearly as much In Pharmacology, If you know how the Dx works, but don’t know the SE? Pick side effect in the same body system as where the drug is working. If you’ve never heard of a drug o see if its PO, & pick GI side effect Never tell a child the Medicine is Candy In OB, If you don’t know what to pick? If it’s a TIE, Pick ASSESS FHR In Med Surg, what is the 1st thing you assess? Assess LOC In Med Surg, what is the 1st thing you do? Establish Airway In Peds (growth & development), if you don’t know pick these? Give the PED. MORE TIME to grow and develop. 1. When in doubt, call it “Normal” (peds) 2. When in doubt, pick the “Older age” 3. When in doubt, pick the “easier task” General guessing skills to know. 1. Rule out absolutes (never/always)*** 2. If 2 answers say the same thing, neither is right 3. If 2 answers are OPPOSITE, one of them is prob. right 4. Umbrella answer (answer that covers all the other’s without saying it does) 5. If the question gives you 4 right answers, & ask’s for Highest priority, then ask yourself if I don’t do this what is the worse outcome, Then pick the WORSE outcome. If you don’t know a question, Such as the “DX”, what should you do? Take the Name of the DX (something that you don’t know) and read the question again without reading what you don’t know and then use common sense. DO NOT EXPECT 75 Q’s, DO NOT EXPECT TO KNOW EVERYTHING, DO NOT EXPECT EVERYTHING TO GO RIGHT [Show More]
Last updated: 1 year ago
Preview 1 out of 47 pages
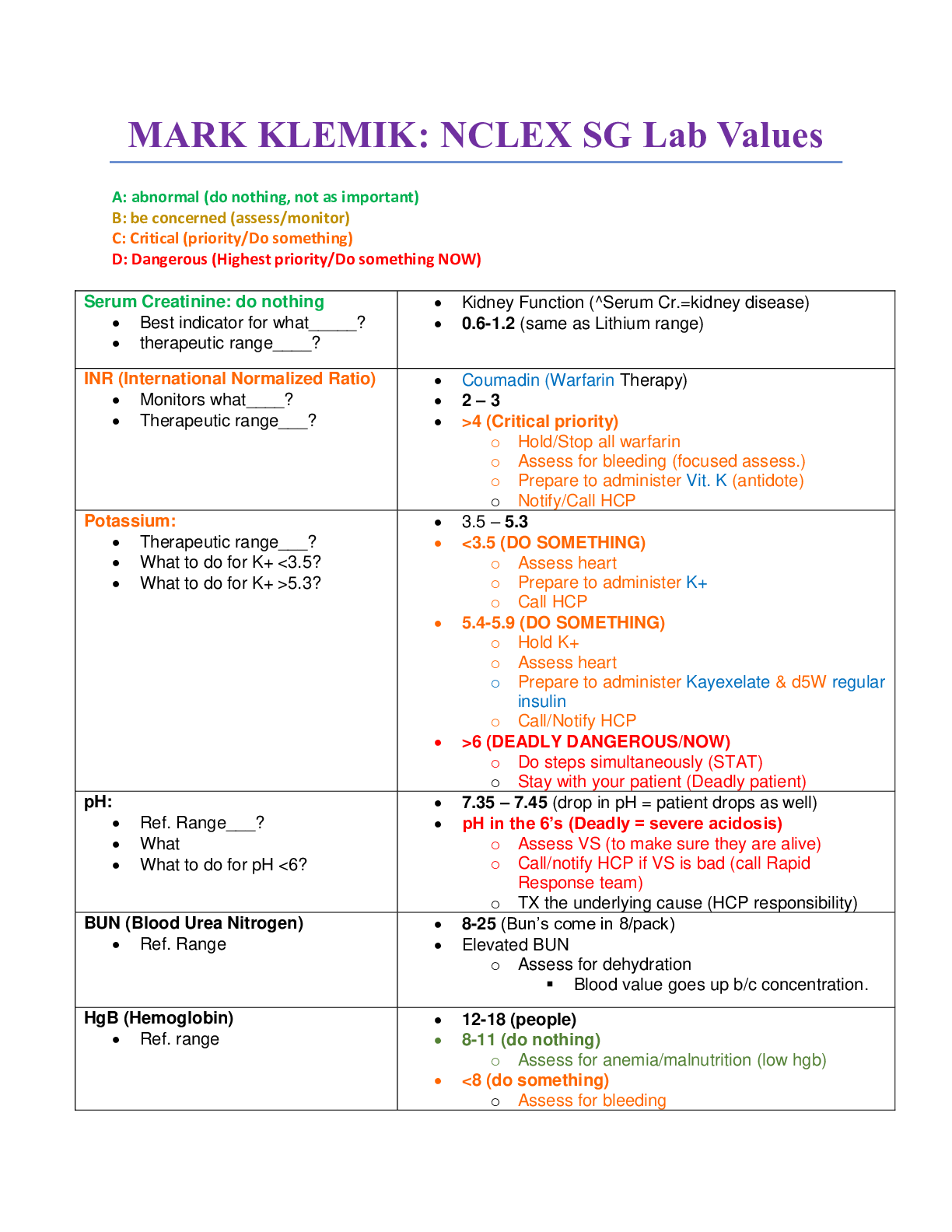
Reviews( 0 )
Recommended For You
*NURSING> NCLEX > Mark Klimek Blue Book. With over 400 Questions and Answers.Best Rated 2021. (All)
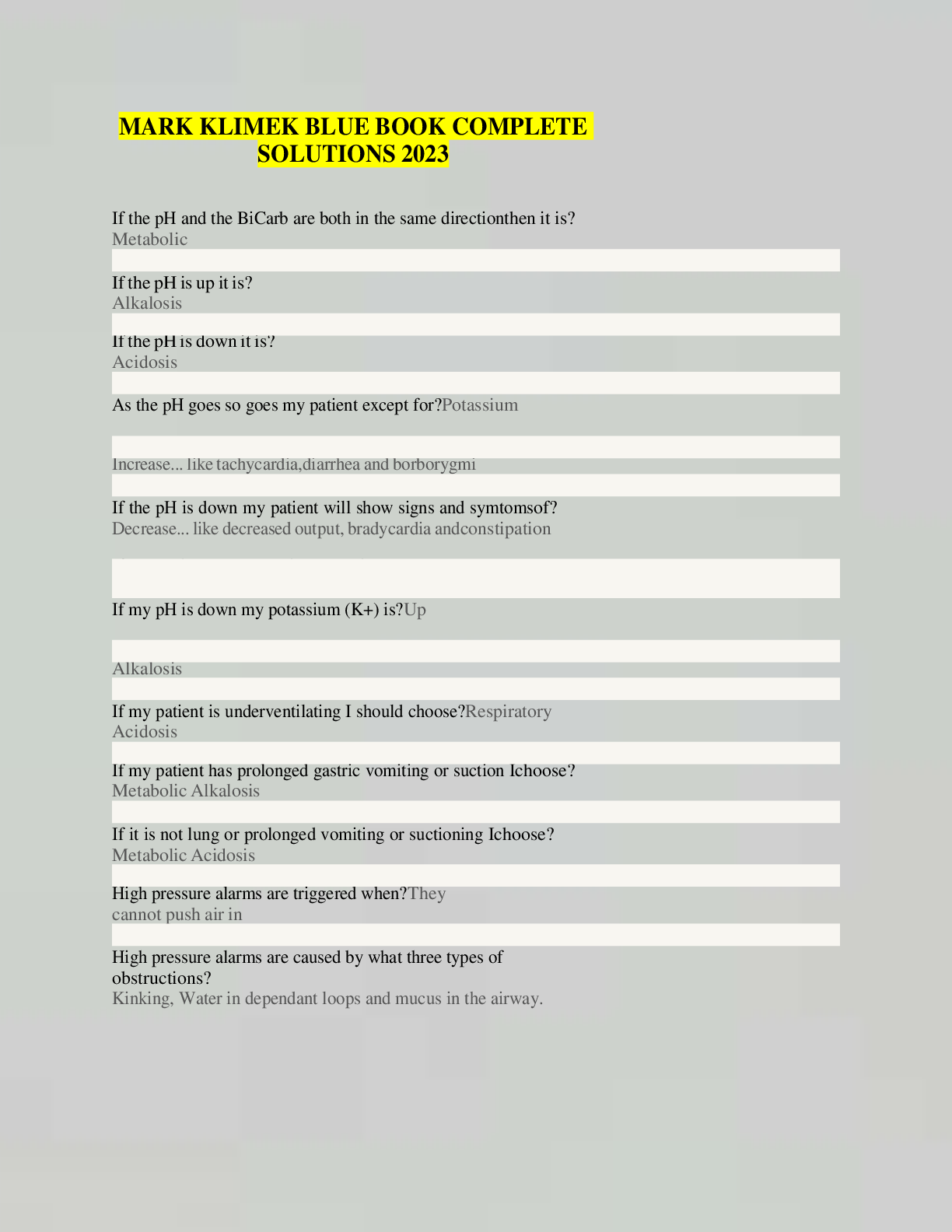
Mark Klimek Blue Book. With over 400 Questions and Answers.Best Rated 2021.
If the pH and the BiCarb are both in the same direction then it is? Metabolic If the pH is up it is? Alkalosis If the pH is down it is? Acidosis As the pH goes so goes my patient except for? P otassiu...
By Hannington , Uploaded: May 03, 2021
$10
*NURSING> NCLEX > NGN NCLEX QUESTIONS FOR 2024 EXAM (All)
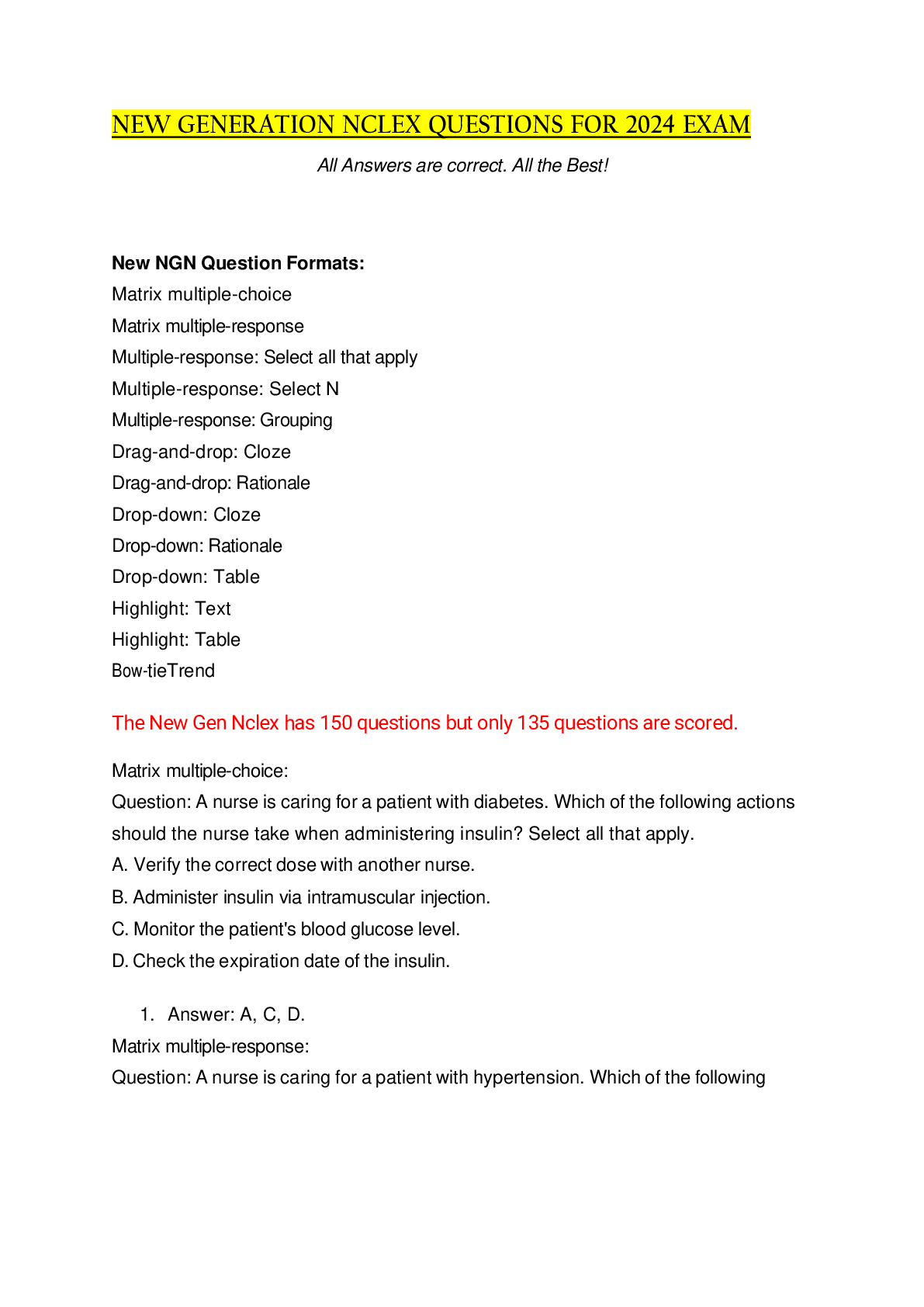
NGN NCLEX QUESTIONS FOR 2024 EXAM
New NGN Question Formats: Matrix multiple-choice Matrix multiple-response Multiple-response: Select all that apply Multiple-response: Select N Multiple-response: Grouping Drag-and-drop: Cloze Drag...
By Rixx Dennis , Uploaded: May 29, 2023
$50.5
*NURSING> NCLEX > Mark Klimek Blue Book. With over 400 Questions and Answers. (All)
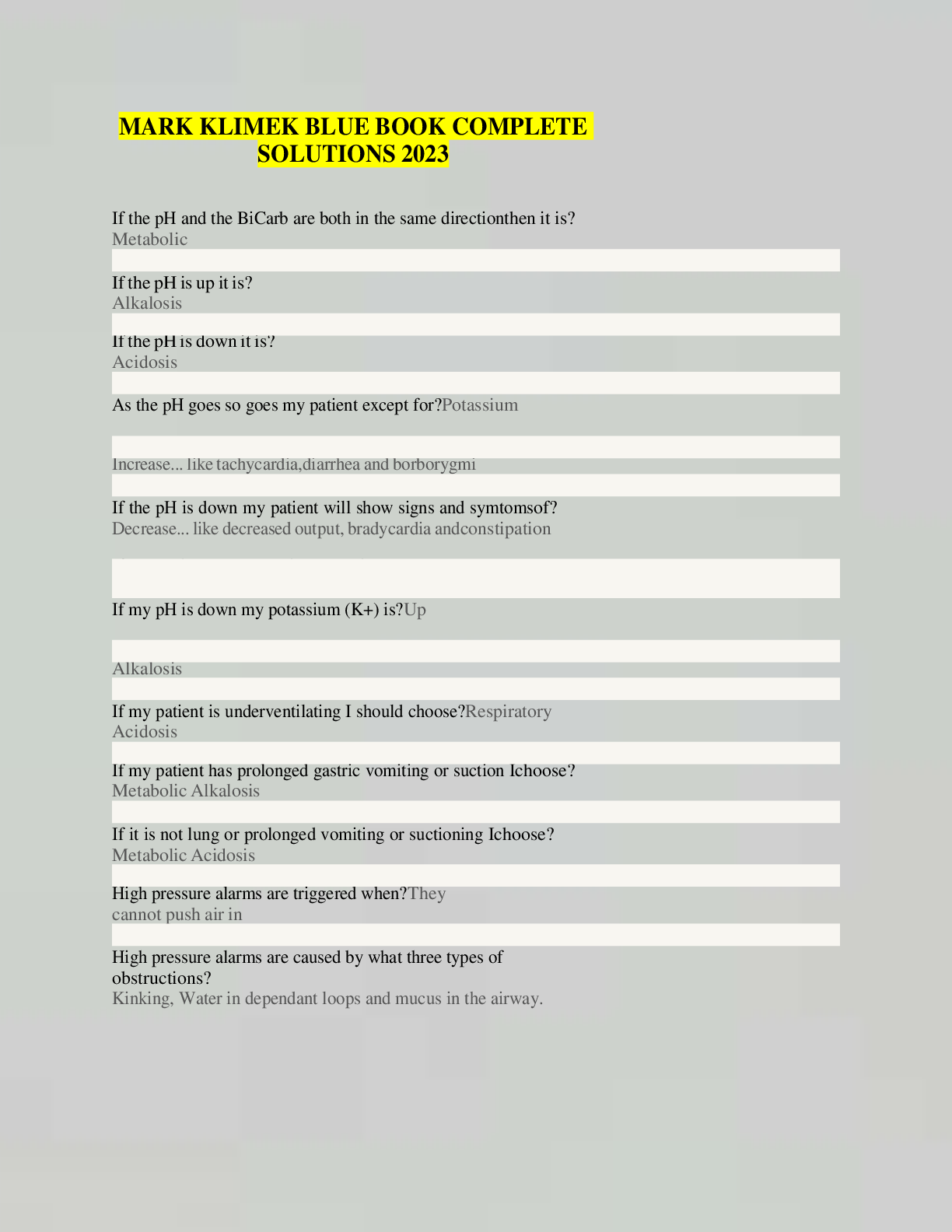
Mark Klimek Blue Book. With over 400 Questions and Answers.
If the pH and the BiCarb are both in the same direction then it is? Metabolic If the pH is up it is? Alkalosis If the pH is down it is? Acidosis As the pH goes so goes my patient except for? P...
By SuperSolutions© , Uploaded: Feb 02, 2021
$12.5
*NURSING> NCLEX > KEEP CALM and PASS NCLEX with MARK KLIMEK Review. Comprehensive Information and content for revisions and last minute reading. (All)
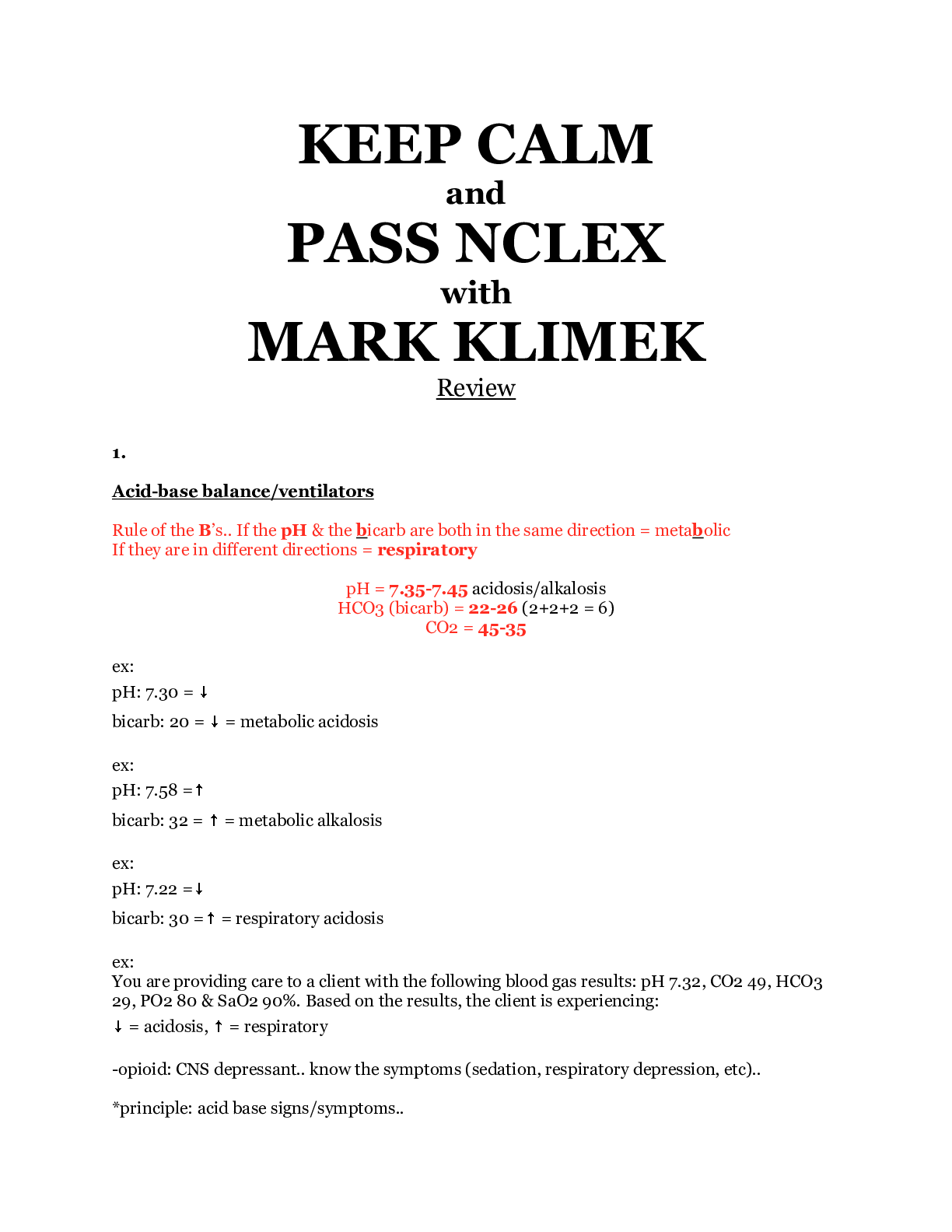
KEEP CALM and PASS NCLEX with MARK KLIMEK Review. Comprehensive Information and content for revisions and last minute reading.
1. Acid-base balance/ventilators Rule of the B’s.. If the pH & the bicarb are both in the same direction = metabolic If they are in different directions = respiratory pH = 7.35-7.45 acidosis/alkal...
By SuperSolutions© , Uploaded: Oct 19, 2020
$9
*NURSING> NCLEX > NCLEX Exam NCLEX-PN TEST BANK. National Council Licensure Examination (NCLEX-PN) Version: 5.0. All 725 Questions and Answers. verified (All)
NCLEX Exam NCLEX-PN TEST BANK. National Council Licensure Examination (NCLEX-PN) Version: 5.0. All 725 Questions and Answers. verified
NCLEX Exam NCLEX-PN TEST BANK. National Council Licensure Examination (NCLEX-PN) Version: 5.0. Teaching the client with gonorrhea how to prevent reinfection and further spread is an example of: Whic...
By EXCLLENTLEC , Uploaded: Jun 14, 2023
$14.5
*NURSING> NCLEX > NURSING Med Surg 2 SAUNDERS COMPREHENSIVE REVIEW FOR NCLEX FOUR. Contains 1141 NCLEX Commonly Tested Q&A With Rationale. (All)
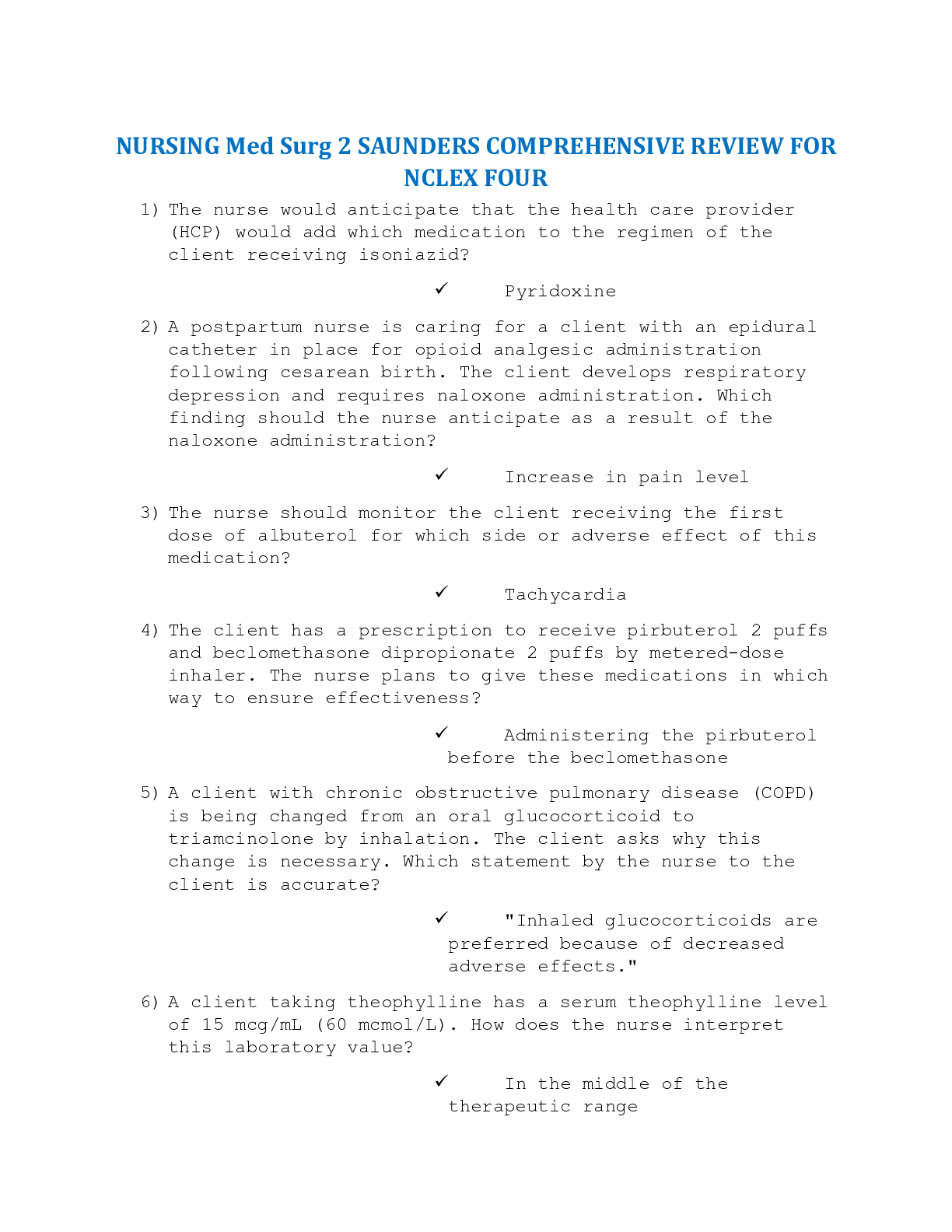
NURSING Med Surg 2 SAUNDERS COMPREHENSIVE REVIEW FOR NCLEX FOUR. Contains 1141 NCLEX Commonly Tested Q&A With Rationale.
NURSING Med Surg 2 SAUNDERS COMPREHENSIVE REVIEW FOR NCLEX FOUR 1) The nurse would anticipate that the health care provider (HCP) would add which medication to the regimen of the client receiving iso...
By SuperSolutions© , Uploaded: Nov 28, 2020
$25
*NURSING> NCLEX > [NGN] NEW GENERATION NCLEX RN EXAM 2023 POST TEST EXAM TOP RATED EXAM (GENUINE AND COMPLETE) (All)
[NGN] NEW GENERATION NCLEX RN EXAM 2023 POST TEST EXAM TOP RATED EXAM (GENUINE AND COMPLETE)
NEW GENERATION NCLEX RN EXAM 2023 POST TEST EXAM TOP RATED EXAM (GENUINE AND COMPLETE)
By Rixx Dennis , Uploaded: Jul 12, 2023
$30.5
*NURSING> NCLEX > NGN NCLEX EXAM NCLEX-PN 2023 (All)
NGN NCLEX EXAM NCLEX-PN 2023
NGN NCLEX EXAM NCLEX-PN 2023
By Rixx Dennis , Uploaded: Aug 08, 2023
$30.5
NCLEX RN> NCLEX > Saunders 2022-2023 Clinical Judgment and Test-Taking Strategies by R.N. Silvestri, Linda Anne, Ph.D., R.N.; Silvestri, Angela E., Ph.D.; Gray, Eileen H. (All)
Saunders 2022-2023 Clinical Judgment and Test-Taking Strategies by R.N. Silvestri, Linda Anne, Ph.D., R.N.; Silvestri, Angela E., Ph.D.; Gray, Eileen H.
Welcome to Saunders Pyramid to Success! Saunders 2022-2023 Clinical Judgment and Test-Taking Strategies: Passing Nursing School and the NCLEX® Exam is one in a series of products designed to assist...
By TopRankProf , Uploaded: Jun 04, 2023
$22
*NURSING> NCLEX > NCLEX RN Exam Prep Compilation in 406 Pages. (See Areas Covered Below) (All)
NCLEX RN Exam Prep Compilation in 406 Pages. (See Areas Covered Below)
NCLEX RN. Latest Exam Prep Comilation in 406 Pages.IT COVERS: 1. BASIC NURSING CARE-171 2. MANAGEMENT AND PRACTICE DIRECTIVES-115 3. PREVENTING RISKS AND COMPLICATIONS-81 4. CARING FOR ACUTE OR CH...
By CHRIS , Uploaded: Jul 01, 2020
$30
Document information
Connected school, study & course
About the document
Uploaded On
Feb 02, 2021
Number of pages
47
Written in
Additional information
This document has been written for:
Uploaded
Feb 02, 2021
Downloads
1
Views
417