*NURSING > Manual > Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking Stud (All)
Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking Answers Listed From Page 125
Document Content and Description Below
Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking Student Laboratory Manual for Bates’ Nursing Guide to Physical Learning Objectives The student w... ill: 1. Def ne health and health assessment. 2. Identify the health indicators and purpose of Healthy People 2020. 3. Explain the components of the health assessment. 4. Clarify the nurse’s role in assessment. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Health is def ned as a state of complete , , and well-being. Introduction to Health Assessment B. Healthy People 2020 is a framework that identif es factors, issues, and of concern in the United States. C. The nursing health assessment entails both a comprehensive and a complete examination. D. prevention focuses on improving overall wellness and protecting from or . E. The nurse’s initial role in health assessment is to . 2. List the facets of health. A. B. C. D. E. F . 2 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 3. Match the level of prevention with its def nition. Activity C SHORT ANSWER 5. The ability to maintain health includes integrating a variety of components. List these components. 6. Referring to www.healthypeople.gov, list the leading health indicators for Healthy People 2020. 4. Match the examples of prevention with their corresponding level of prevention. (Level of prevention may be used more than once.) Level of Prevention Def nition Primary A. Decreasing the effects of a disease or disability by pre venting complications and additional loss that happens when a defect is permanent Secondary B. Improving the overall wellness and protection from disease or disability Tertiary C. Early detection and treatment of a disease when it is curable or has few complications or disabilities Example Level of Prevention Communicable disease control A. Primary Health education B. Secondary Periodic selective examinations C. Tertiary Sheltered communities Provision of adequate housing Provision of hospital and community facilities Reducing risk factors Early treatment of diseases Self-examination Rehabilitation programs 7. The authors state that health assessment is similar to a puzzle. Explain why this is an appropriate metaphor. 8. The nursing health assessment enables nurses to detect areas of patients’ lives that may benef t from change. Explain the potential benef ts of such change. CHAPTER 1 INTRODUCTION TO HEALTH ASSESSMENT 3 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 9. Describe three ways in which nurses are able to inf uence the health of the patient. Activity D NCLEX STYLE QUESTIONS 10. When doing an overall assessment of a patient, the nurse is able to utilize f ndings and do what? a. Identify what level of prevention the patient is at b. Identify in what areas the patient can educate his or her family c. Identify in what areas the patient needs the most care d. Identify the patient’s medical diagnosis 11. What is paramount in health promotion? (Mark all that apply.) a. Working with the individual patient b. Demonstrating authority c. Emphasizing the risks of poor health practices d. Developing the nursing care plan e. Limiting the involvements of the patient’s friends and family 12. What is the primary function of the health care team? a. To work together to obtain maximum coverage b. To decide the best overall care c. To guide the patient’s care throughout times of crisis d. To develop an individual focus for each member 13. What are nurses able to detect through the health assessment? a. Areas that need continuous care b. Areas that need in-hospital care c. Areas that need referral to a specialist d. Areas in need of health adjustments 14. Using both verbal and nonverbal clues given by the patient, what is the nurse constantly doing? a. Diagnosing b. Intervening where necessary c. Formulating a discharge plan d. Assessing 15. When assisting a patient with health promotion, what must the nurse also nurture? a. A healthy environment b. Knowledge of the Healthy People 2020 indicators c. Family communication d. School/work attendance 16. As a nurse becomes more prof cient and comfortable in his or her role, what increases? a. Conf dence and knowledge base b. Time management and conf dence c. Knowledge base and expertise d. Expertise and time management 17. What is the foundation of nursing practice? a. Planning b. Assessment c. Evaluation d. Intervention 18. How does a nurse best facilitate the nursing health assessment? a. Maintaining privacy b. Asking the appropriate questions c. Formulating a nursing diagnosis d. Creating a nursing care plan 19. Why is the nurse always reassessing the patient for changes? a. To never make a mistake when providing care b. To always have the best nursing care plan c. To achieve the best results d. To update the nursing diagnosis 4 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION III: CASE STUDY Activity E A graduate nurse is meeting her f rst patient on the medical-surgical unit. The patient is a 52-year-old woman of African American descent who is being admitted with an exacerbation of her multiple sclerosis. The patient currently lacks health insurance and has a low income. a. Refer to the leading health indicators listed at www.healthypeople.gov. What Healthy People 2020 health indicator would apply most directly to this patient? b. What are some of the abilities that the nurse would use when performing the nursing health assessment? 5 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the components of the nursing process. 2. Identify appropriate subjective questions based on the health assessment. 3. Categorize patient problems into a priority list. 4. Formulate a nursing diagnosis. 5. Develop a plan of care for a patient. 6. Evaluate and revise a care plan based on an individual patient. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. data are the basis for symptoms; data are considered to be signs. B. The is the broad systematic framework that supplies a methodical base applicable to the practice of nursing. Critical Thinking in Health Assessment C. When f ndings, be as specif c as your data allow, but bear in mind that you may have to settle for a , such as the chest, or a body system, such as the musculoskeletal system. D. Problems may relate to events in the patient’s life. E. Involvement of body may help you to cluster the clinical data. F. Almost all clinical information is subject to . 2. List the steps in clinical reasoning. A. B. C. D. E. F. C H A P T E R 2 6 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 3. Match the term with its def nition. Answer Term Def nition Assessment A. The performance of nursing interventions Diagnosis B. A continuing process that determines if the goals/outcomes have been attained Planning C. Subjective and objective data gathered ini tially during the health history and physical examination and the additional information collected on a daily basis Implementation D. Charting the best course to achieve the patient’s optimal wellness and comfort Evaluation E. Has a nursing focus and is based on real or potential health problems or human responses 4. Match the part of the nursing process with its action. Answer Part of Nursing Process Action Assessment A. Use your inferences about the structures and processes involved Diagnosis B. Nursing interventions that help to achieve the goals stated Planning C. Continue to monitor Implementation/interventions D. Collect the most specif c and critical f nd ings to support your problem list Evaluation E. Develop goals 5. Match the term with its corresponding meaning. Answer Term Meaning Onset A. How long the sign or symptom has been going on Location B. What else is going on when the patient experiences the sign or symptom Duration C. What the symptom feels like Characteristic symptoms D. Anything the patient has tried to make it go away Associated manifestations E. Nursing interventions that are recommended Relieving factors F. Where the sign or symptom is Treatments G. When the sign or symptom began CHAPTER 2 CRITICAL THINKING IN HEALTH ASSESSMENT 7 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity C SHORT ANSWER 6. The process of diagnosis has unique characteristics within nursing practice. What are some characteristics of this process that differentiate it from other health disciplines? 7. The f nal step in the process of clinical reasoning involves the direct input of the patient. What is this step and how is the patient’s input integrated? 8. Describe methods nurses use to ensure the quality of patient data. 9. Discuss the principles that nurses use to appraise the value of diagnostic tests because of their inherent imperfection. 10. Explain the characteristics of a correctly written progress note. Activity D NCLEX STYLE QUESTIONS 11. In what area do nurses use formalized screening and assessment tools? a. Vital signs b. Skin breakdown c. Hand hygiene d. Kidney failure 12. How does an experienced nurse improve his or her eff ciency and enhance the relevance and value of the data he or she collects? a. By conducting the assessment as rapidly as possible b. By utilizing an information source other than the patient c. By correlating medical diagnoses and nursing diagnoses d. By generating plans early 13. When constructing a nursing care plan, what should you reference? (Mark all that apply.) a. Therapy b. Healthy People 2020 health indicators c. Patient education d. Input from the patient’s physician e. Diagnosis 14. When documenting clinical data after an assessment of the patient’s neck, what might you write in the physical assessment? a. Thyroid isthmus barely palpable, lobes not felt b. Apical impulse indiscrete and tapping c. Thorax symmetric without equal excursion d. Extraocular movements full and equal on exam 15. You are the off ce nurse admitting a new patient to the clinic. You have gained your patient’s trust, gathered a detailed history, and f nished your portion of the physical examination. What is your next step in caring for this patient? a. Formulate nursing diagnoses b. Order the appropriate laboratory tests c. Identify the patient’s problems d. Notify the physician of your f ndings 16. What is pivotal to determining how to move from each patient problem to its goals? a. Your clinical reasoning process b. Your positive interpretation of the patient’s history c. Your process in collecting physical data d. Your evaluation as an accurate historian of the patient 8 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 17. As the nurse caring for a patient you have completed the collection of the subjective data. On what do you base your decision to do an entire head-to-toe physical assessment or a systems-specif c assessment? a. The patient’s answers b. Observable signs and symptoms c. Your knowledge base and expertise d. The patient’s chief complaint 18. For each patient problem you identify you develop and record a plan. What must your plan do? (Mark all that apply.) a. Begin discharge planning b. Include referral to dietician c. Flow logically from identif ed diagnoses d. Specify which steps are needed next e. Identify timing of family involvement 19. Your patient tells you that his chief complaint is “fatigue.” When obtaining the patient history, what additional information might you want to elicit to try and pinpoint the patient’s “real problem”? a. More information regarding family history b. More information regarding cognition c. More information from the patient’s peers d. More information regarding psychosocial issues 20. Your patient has been directly admitted from the doctor’s off ce. The only paperwork he has brought with him is his admission orders. You are gathering your admission data when ordered lab work is collected. When documenting your history, physical examination, assessment, and plan, what would you write under the heading “Laboratory Data”? a. Not recommended. b. None currently. c. Not relevant to patient’s care. d. Nothing. Enter as a late entry. SECTION III: CASE STUDY Activity E Kris Brown is a 28-year-old Caucasian male who presents to the emergency department with a swollen and tender left ankle. He tells the nurse that he was playing baseball and was sliding into second base when the injury occurred. a. Using critical thinking, what subjective data would be important for the nurse to gather? b. Using clinical reasoning, what objective data would be important for the nurse to gather? 9 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Utilize therapeutic communication techniques during the patient interview. 2. Interview patients using a broad to narrow questioning technique. 3. Describe the phases of the nurse–patient interview. 4. Describe the appropriate environment to promote a successful interview. 5. Become more comfortable interviewing patients on sensitive subjects. 6. Discuss strategies for handling diff cult patients. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The primary goal of the nurse–patient interview is to improve the - of the patient. Interviewing and Communication B. The interviewing process that actually generates the pieces of health information is much more f uid and demands effective and skills. C. Being consistently and to individual differences is one of the clinician’s challenges. D. Remember that background and inf uence preferences about interpersonal space. E. Learning about the effects of the illness gives the nurse and the patient the opportunity to create a and picture of the problem. 2. List the phases of the interviewing process. A. B. C. D. C H A P T E R 3 10 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 3. Match the technique of skilled interviewing with its def nition. Answer Term Def nition Active listening A. Communication that occurs continu ously and provides important clues to feelings and emotions Guided questioning B. Acknowledging the legitimacy of the patient’s emotional experience Nonverbal communication C. Telling the patient when you are chang ing directions during the interview Empathic responses D. Closely attending to what the patient is communicating Validation E. Reinforcing the patient’s primary respon sibility for his or her health Reassurance F. Providing a general overview of what the patient has said Partnering G. Options for expanding and clarifying the patient’s story Summarization H. Must be realistic. Avoid assuring the patient that “everything will be all right.” Transitions I. Identify the patient’s feelings and then communicate understanding and acceptance Empowering the patient J. Making the relationship collaborative 7. Discuss phase 1 of the interview process. 8. Explain and discuss the attributes of a symptom. 9. Discuss what the nurse should assess when obtaining the patient’s perspective on his or her illness. Activity C SHORT ANSWER 4. Describe the guidelines for working with an interpreter. 5. Explain how you would facilitate communication with a hearing-impaired patient. 6. Describe how the health history format differs from the interviewing process. CHAPTER 3 INTERVIEWING AND COMMUNICATION 11 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity D NCLEX STYLE QUESTIONS 10. Learning about the effects of the illness does what for the nurse and the patient? a. Gives them the basis to establish a trusting relationship b. Gives them each a better understanding of the other c. Gives them the ability to communicate better d. Gives them the opportunity to create a complete and congruent picture of the problem 11. What occurs during the termination phase of an interview? a. Planning for follow-up care b. Addressing topics that have not yet been addressed c. Assessing the patient’s mental status d. Letting the patient know you understood all he or she has told you 12. How would the nursing instructor explain the goal of guided questioning to his or her students? a. Providing the most plausible answer to the patient b. Facilitating the patient’s fullest communication c. Developing a basis for accurate health promotion activities d. Creating an opportunity for the early generation of a plan 13. “How many steps can you climb before you get short of breath?” is an example of what kind of question? a. A question that offers multiple choices for answers b. A question that is qualitative in focus c. A question that elicits a graded response d. A question that demands an imprecise response 14. While interviewing a new patient, you notice that he is mirroring your position. What can this signify? a. An increasing sense of connectedness b. A desire to be on an equal power level c. A desire for increased rapport d. The patient does not take you seriously 15. Your new patient becomes visibly anxious during the nursing interview. You respond by telling her, “Don’t worry, everything will be okay.” What might this premature reassurance cause? a. A feeling of closeness between the patient and the nurse b. The nurse to shorten the interview process c. The blockage of further disclosures by the patient d. A noticeable lessening of the patient’s anxiety 16. What techniques encourage patient disclosures while minimizing the risk for distorting the patient’s ideas or missing signif cant details? (Mark all that apply.) a. Asking a series of questions, one at a time b. Using ref ection c. Asking only open-ended questions d. Encouraging with repetition e. Offering multiple choices for answers 17. A student nurse is conducting her f rst patient interview. The student suddenly draws a blank on what to ask the patient next. What is a useful interview technique for the student to use at this point? a. Transition b. Summarization c. Reassurance d. Termination 18. During one of your clinical placements you encounter a patient who becomes silent during the nursing interview. What would be appropriate for you to do? (Mark all that apply.) a. Appear attentive b. Give brief encouragement to the patient c. Change the subject you are asking about d. Ask your question again e. Watch the patient closely for nonverbal cues 19. The principle of conf dentiality is of paramount importance in the nurse–patient relationship. When should you inform the patient of with whom his or her information will be shared? a. When the patient asks b. At the beginning of the interview c. At the end of the interview d. Whenever it seems appropriate 12 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 20. When interacting with a patient, what conveys the extent of interest, attention, acceptance, and understanding of the nurse? (Mark all that apply.) a. Cultural reassurance b. Eye contact c. Gestures d. Posture e. Restatement SECTION III: CASE STUDY Activity E Nailah Shadid, a 22-year-old immigrant from Egypt, comes to the clinic for the f rst time because of a gynecologic problem. Her husband accompanies her. a. Discuss what aspects of Nailah’s culture you should consider when conducting your nursing interview. 13 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Explain the four types of histories and when they are used. 2. Describe the components of a comprehensive health history. 3. Obtain a comprehensive health history from a patient. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The of should reveal the patient’s responses to his or her symptoms and what effect the illness has had on the patient’s . B. Inquire about past of a symptom and ask what treatments were and their results. C. Risk factors and other pertinent information related to the symptom are frequently , such as risk factors for coronary artery disease in a patient with chest pain, or current that may have side effects similar to the . The Health History D. The Health Pattern section provides a guide for gathering or history from the patient and daily that may inf uence health and illness. E. of behaviors or elements in the health history will only with learning about the patient. F. How much history to gather varies by the of the patient encounter. 2. List the clues to physical abuse. A. B. C. D. E. 3. List the eight main components of a comprehensive health history. A. B. C. D. E. F. G. H. C H A P T E R 4 14 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 4. Match the type of assessment with the description (assessments will have multiple descriptions). Answer Description Type of Assessment A systematic prioritization of need in an urgent context A. Comprehensive assessment Having a problem or treatment plan evaluated B. Focused assessment Strengthens the nurse–patient relationship due to its broad scope C. Follow-up history Assesses symptoms restricted to a specif c body system D. Emergency history Addresses specif c concerns or symptoms Gathering data to evaluate the outcomes of the plan of care Immediate priorities are the ABCs of airway, breathing, and circulation Provides fundamental and personalized knowledge about the patient Appropriate for established patients Data collection is focused on the patient’s emergent problem Creates platform for health promotion through education and counseling Carried out by a second-shift nurse who is addressing a problem identif ed by an earlier nurse 5. Match the component of the health history with the information obtained. Answer Component of the Health History Information Obtained Identifying Data A. Includes patient’s thoughts and feelings about the illness Reliability B. Risk factors Chief Complaint(s) C. May include a genogram Present Illness D. Establishes source of referral Past History E. Documents personal/social history and daily living routines Family History F. One or more major symptoms or concerns Review of Systems G. Systemic documentation of presence or absence of common symptoms Health Patterns H. Varies according to the patient’s memory, trust, and mood CHAPTER 4 THE HEALTH HISTORY 15 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the system to its corresponding data. Answer System Data General A. Goiter Skin B. Paroxysmal nocturnal dyspnea HEENT C. Flank pain Neck D. Trouble swallowing Breasts E. Arthritis Respiratory F. Weakness, fatigue, or fever Cardiovascular G. Dentures Gastrointestinal H. Changes in hair or nails Peripheral vascular I. HPV Urinary J. Depressed mood Reproductive K. Unilateral weakness Musculoskeletal L. Hemoptysis Psychiatric M. Easy bruising Neurologic N. Change in glove or shoe size Hematologic O. Swelling with redness or tenderness Endocrine P. Abnormal nipple discharge 10. Discuss what the nurse should address in each of the different components of the health history. Activity D NCLEX STYLE QUESTIONS 11. What information aids the nurse in assessing possible biases in the data collected in the health history? a. Ethnicity of patient b. Gender of patient c. Source of information d. Socioeconomic status of the patient 12. What is a key element of the history of present illness? a. Initiating a problem list b. Obtaining an accurate history c. Developing accurate nursing diagnoses d. Self-treatment Activity C SHORT ANSWER 7. Explain why it is important to investigate a patient’s health patterns when taking a health history. 8. Discuss what students/nurses can do to become more comfortable gathering patient data on sensitive topics. 9. Compare and contrast the four types of health histories. 16 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 13. You are collecting data for a comprehensive health history on a patient new to your clinic. Under what component of the health history would you place data on a chronic childhood illness? a. Past history b. Health maintenance c. General information d. Risk factors 14. A nurse at the local free clinic is collecting data on a 16-year-old boy who has come to the clinic. Under what component of the health history would the nurse place data on whether the teen routinely uses seat belts when in a vehicle? a. General information b. Health maintenance c. Risk factors d. Initial information 15. As a nursing student you learn that mastering all the components of the comprehensive history provides what? a. Empathy b. Avocacy c. Prof ciency d. Authority 16. Which of the following are aspects of the comprehensive health history? (Mark all that apply.) a. Strengthens the nurse–patient relationship b. Provides baselines for future assessments c. Creates platform for health promotion through education and counseling d. Obtains data to evaluate the outcomes of the plan of care e. Is appropriate for established patients 17. When collecting data on the history of the present illness, it is appropriate to include what? a. Chronic childhood illnesses b. Treatment recommendations c. Reliability of information source d. Current medications 18. A patient states that the reason he has come into the clinic is for a routine annual physical. In what section of the health history would you document this information? a. Initial information b. History of present illness c. Health maintenance d. Chief complaint 19. Your patient has two aff rmative answers to the CAGE Questionnaire. What other questions should you ask? (Mark all that apply.) a. What OTC medications do you take? b. Do you experience blackouts when drinking? c. How would you describe your level of nutrition? d. Do you have seizures while drinking? e. Do you have any legal problems? 20. While gathering data for the family history portion of the health history, what would you ask about? a. Coronary artery disease b. Low bone density c. Liver disease d. Injuries SECTION III: CASE STUDY Activity E Geri Christianson, a 67-year-old white woman, has been brought to the emergency room with chest pain. Vital signs are T 37°C; pulse 115; respirations 33; BP 152/83. She states that her chest pain began while she was shoveling snow from the sidewalk outside her home and describes her pain as “signif cant” but describes it as “pressure more than actual pain.” She localizes her pain to her left shoulder and scapular region and rates it at 7 out of 10. Mrs. Christianson states that at this point nothing makes her pain worse or more tolerable. She states that she has a history of “clogged arteries” and takes ASA daily on the advice of her physician. During the interview, she states that her father died of a myocardial infarction and that her mother suffers from angina. a. Compile a basic health history for this patient. CHAPTER 4 THE HEALTH HISTORY 17 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE COMPREHENSIVE ADULT HEALTH HISTORY Patient Name __________________________________________________ Date/Time ____________________________ Overview. _____________________________________________________________________________________________ Identifying Data ________________________________________________________________________________________ Source and Reliability ___________________________________________________________________________________ Chief Complaint(s) _____________________________________________________________________________________ History of Present Illness Onset _______________________________________________________________________________________________ Location _____________________________________________________________________________________________ Duration ____________________________________________________________________________________________ Characteristic symptoms ______________________________________________________________________________ Associated manifestations _____________________________________________________________________________ Relieving/exacerbating factors_________________________________________________________________________ Treatment ___________________________________________________________________________________________ Past History Allergies _____________________________________________________________________________________________ Medications _________________________________________________________________________________________ Childhood illnesses ___________________________________________________________________________________ Adult illnesses Medical ____________________________________________________________________________________________ Surgical ____________________________________________________________________________________________ Psychiatric ________________________________________________________________________________________ Health Maintenance Immunizations _______________________________________________________________________________________ Screening tests _______________________________________________________________________________________ Safety measures _______________________________________________________________________________________ Risk Factors Tobacco ______________________________________________________________________________________________ Alcohol/drugs ________________________________________________________________________________________ Family History _________________________________________________________________________________________ Review of Systems General ______________________________________________________________________________________________ Skin _________________________________________________________________________________________________ HEENT ______________________________________________________________________________________________ Head ________________________________________________________________________________________________ Eyes _________________________________________________________________________________________________ Ears _________________________________________________________________________________________________ Nose and sinuses _____________________________________________________________________________________ Throat (or mouth and pharynx) _______________________________________________________________________ Neck ________________________________________________________________________________________________ Breasts ______________________________________________________________________________________________ Respiratory __________________________________________________________________________________________ Cardiovascular _______________________________________________________________________________________ Gastrointestinal ______________________________________________________________________________________ Urinary ______________________________________________________________________________________________ Reproductive _________________________________________________________________________________________ Peripheral vascular ___________________________________________________________________________________ Musculoskeletal ______________________________________________________________________________________ Psychiatric ___________________________________________________________________________________________ 18 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Neurologic ___________________________________________________________________________________________ Hematologic _________________________________________________________________________________________ Endocrine ____________________________________________________________________________________________ Health Patterns _________________________________________________________________________________________ Self-perception–self-concept ___________________________________________________________________________ Value-belief __________________________________________________________________________________________ Activity-exercise ______________________________________________________________________________________ Sleep-rest _____________________________________________________________________________________________ Nutrition _____________________________________________________________________________________________ Role-relationship _____________________________________________________________________________________ Coping-stress tolerance ________________________________________________________________________________ 19 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Explain why culture is important in the health assessment process. 2. Def ne cultural competency and cultural humility. 3. Demonstrate behaviors that show sensitivity to a patient’s culture during the assessment process. 4. Explain the difference between spirituality and religion. 5. Explain why the patient’s spiritual needs should be assessed. 6. Utilize a spiritual assessment tool to assess a patient’s spiritual needs. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Nursing has long recognized and practiced care of the patient and attention to is a part of caring for the whole patient. B. You must evaluate each patient with pain as an , being aware of your reaction to the patient’s style. Cultural and Spiritual Assessment C. Knowledge of the or groups in your practice region will help you better and the patient’s needs. D. It can be disconcerting working with a person whose culture nodding the head for and shaking the head for . E. There are , which are “illnesses” def ned by a particular culture but that have no illness in Western medicine. F. ____________ distress may be a response to ____________ or _____________ issues. 2. List several of the aspects of culture relevant to health assessment. A. B. C. D. E. F. G. H. I. C H A P T E R 5 20 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity C SHORT ANSWER 6. Def ne nursing presence and explain what it involves. 7. Discuss Stoll’s guidelines for spiritual assessment. 3. List the stages of grief as characterized by Kubler-Ross. A. B. C. D. E. Activity B MATCHING 4. Match the dimension of cultural humility with its component. Answer Component Def nition Self-awareness A. Communication based on trust, respect, and a willingness to re-examine assumptions Respectful communication B. Intuitively knowing members of one’s own group Collaborative partnerships C. Maintaining an open and inquiring attitude 5. Match the concept with the statement about the concept. Answer Concept Statement Spirituality A. Involves a sincere connection and sharing of human experience Religion B. What do you think is going to happen to you? Spiritual care C. Has being sick (or what has happened to you) made any difference in your practice of praying? Nursing presence D. A system of beliefs or a practice of worship Relation between spiritual beliefs and health E. Being present during unpleasant experiences, listening to the patient, providing opportuni ties for the patient to practice religious rituals, or referring the patient to a religious leader of the patient’s choice. Dying patients F. Involves a two-tiered approach Religious practices G. Culture specif c Spiritual assessment H. May not wish to conf de in everyone they meet CHAPTER 5 CULTURAL AND SPIRITUAL ASSESSMENT 21 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 8. Discuss some of the major priorities in the nursing care of the dying patient. 9. Explain the statement “Patients do not live in isolation . . .” and how this affects nursing care. 10. Identify and discuss Campinha-Bacote’s model of cultural competence. Activity D NCLEX STYLE QUESTIONS 11. When culture is def ned as a system, what components would be included? (Mark all that apply.) a. Cognitive ability of the patient b. How we view the world c. How we experience the world physically d. How we behave in relation to other people e. Shared ideas, rules, and meanings 12. What concept is an approach to caring for patients from culturally diverse backgrounds? a. Cultural humility b. Ethnic sensitivity c. Spiritual awareness d. Cultural values 13. You are caring for a 70-year-old Serbian woman who is in the United States visiting her family. What must occur before this patient is willing to teach you about her culture? a. The patient’s family must allow it b. You need to hide your biases c. You need to establish rapport and trust d. You need to establish a value-based partnership 14. As a novice nurse caring for a patient from a different culture, what may you f nd confusing or upsetting? a. Patient’s level of motivation b. Patient’s nonverbal communication c. Patient’s family members d. Patient’s ethnicity 15. You are attending a seminar on transcultural nursing at a nursing conference. What aspects of culture relevant to health assessment would you expect to be discussed? (Mark all that apply.) a. Nutrition b. High-risk behaviors c. Wound care d. Educational goals e. Health care practitioners 16. The “evil eye” is an example of what? a. A spiritually def ned illness b. A psychosocial condition c. A cultural-bound syndrome d. An ethnic belief 17. An elderly Chinese man is touring the United States and has a heart attack. When admitting this patient to the coronary care unit, what would be important to note in the family history? a. Chronic childhood illnesses b. Quality of family relationships c. Reliability of information source d. The decision makers for the family 18. What is an important part of being present with a patient? a. Listening b. Understanding c. Spiritual awareness d. Cultural knowledge 19. You are discussing hospice care with a dying patient who will be going home from the hospital tomorrow. What would be important to tell this patient about hospice care? a. It teaches CPR b. It provides all medicine and treatment c. It is palliative d. It makes end-of-life decisions easier 22 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 20. When studying Campinha-Bacote’s model of cultural competency in the delivery of health care, you learn that cultural desire is viewed as the motivation for the nurse to want to do what? (Mark all that apply.) a. Become culturally skillful b. Seek cultural compassion c. Become culturally knowledgeable d. Seek cultural encounters e. Become ethnically expert SECTION III: CASE STUDY Activity E A 55-year-old Amish man is trampled by a horse. He is unable to move his legs when admitted to the ICU from the emergency department. a. Using Stoll’s Guidelines for Spiritual Assessment, what data would be important to obtain from the patient. Why? 23 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the components of the physical examination. 2. Recognize the best approach for each physical examination based on individual patient needs. 3. Utilize lighting and the environment to ensure an accurate physical examination. 4. Describe the equipment for performing a physical examination. 5. Demonstrate a head-to-toe physical examination. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The physical examination is a to obtain data through patient assessment. Physical Examination B. Before beginning the physical examination, the measures that promote the patient’s and make any adjustments needed in the lighting and surrounding environment. C. The skillful nurse is thorough without time, systematic without being , gentle yet not afraid to cause should this be required. D. The of the nurse is to one area of the at a time. E. The strength of a is used to central and peripheral nervous system disorders. F. As the nurse develops his or her own sequence of examination, an important is to how often you ask the patient to change . 2. List the elements of standard precautions. A. B. C. D. E. C H A P T E R 6 24 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 3. Match the component of assessment with the appropriate position of the patient. Each position will be used more than once. Activity D SHORT ANSWER 5. Describe the four cardinal techniques of examination and provide examples of when each would be applied. 6. Discuss the decision process used to decide between performing a complete or a focused physical examination. Answer Component of Assessment Patient Position Assessment of cranial nerve function A. Standing Inspection for varicose veins B. Sitting Palpation of femoral and popliteal pulses C. Supine Cardiac auscultation Range of motion of the patient’s spine Ref exes Romberg test Inspection, auscultation, and percussion of the abdomen Palpation of the breasts Activity C SEQUENCING 4. Show the suggested sequence of the following components of the physical examination. A. General survey B. Back C. Abdomen D. Peripheral vascular system E. Vital signs F. Breasts, axillae, and epitrochlear nodes G. Nervous system H. Neck I. Anterior thorax and lungs J. HEENT K. Skin L. Lower extremities M. Posterior thorax and lungs CHAPTER 6 PHYSICAL EXAMINATION 25 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 7. Explain what you would do when preparing to perform a physical examination on a patient and why. 8. Describe the attributes of an assessment that is thorough, eff cient, and respectful of the patient’s comfort. Activity E NCLEX STYLE QUESTIONS 9. You are performing a physical examination on a new patient. What would you be assessing if you were testing the patient’s sense of smell? a. Cranial nerves b. Nose c. Upper neuron function d. Strength of nerve functioning 10. When inspecting structures such as the jugular venous pulse, what would be the best lighting to use? a. Direct lighting b. Tangential lighting c. Diffuse lighting d. Back lighting 11. You have f nished the physical examination. What do you do immediately after f nishing? (Mark all that apply.) a. Identify needed laboratory tests b. Share f ndings with physician c. Give your general impressions d. Tell patient what to expect next e. Perform interventions 12. Which of the following is a component of the general survey? a. Patient’s blood pressure b. Patient’s state of hygiene c. Patient’s breath sounds d. Patient’s oral temperature 13. Equipment used in conducting a physical examination includes a 2 × 2 gauze pad. What is this used for? a. Testing facial sensation b. Invoking the blink ref ex c. Inverting the eyelid d. Examining the tongue 14. What is used to gauge central and peripheral nervous system disorders? a. Strength of a ref ex b. Gait c. Tuning fork d. Heat and cold 15. What general goals do you organize your comprehensive or focused examination around? (Mark all that apply.) a. Identifying the patient’s medical diagnosis b. Ensuring the patient’s compliance with treatment c. Avoiding unnecessary changes in position d. Enhancing clinical eff ciency e. Maximizing the patient’s comfort 16. Your lab instructor explains that physical examination relies on what cardinal assessment technique? a. Assessment b. Percussion c. Organization d. Communication 17. Universal precautions are primarily designed to protect the health care worker from what? a. STDs b. Musculoskeletal injuries c. Blood-borne pathogens d. Respiratory diseases 18. During the physical examination of your patient you auscultate the sound of the patient’s breathing. What area of the patient are you assessing? a. Abdomen b. Neck c. Lungs d. Back 26 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION III: CASE STUDY Activity F Mr. Boudroux, 68 years old, is HIV positive. He is admitted to your unit following knee replacement surgery. He is now 24 hours postop and you are caring for him for the f rst time. a. What cardinal assessment techniques would you use when conducting a focused assessment on Mr. Boudroux? Why? All members of the health care team will implement universal precautions in Mr. Boudroux’s care. b. What are universal precautions and how would they be used with Mr. Boudroux? Patient’s Name ___________________________________________________ Date/Time __________________________ General survey __________________________________________________________________________________________ Vital signs ______________________________________________________________________________________________ Skin: upper torso, anterior and posterior __________________________________________________________________ Head and neck, including thyroid and lymph nodes _______________________________________________________ Nervous system (mental status; cranial nerves; upper extremity motor strength, bulk, tone; cerebellar function) ___________________________________________________________ Thorax and lungs Anterior _____________________________________________________________________________________________ Posterior _____________________________________________________________________________________________ Breasts _________________________________________________________________________________________________ Musculoskeletal as indicated: upper extremities ___________________________________________________________ Cardiovascular JVP, carotid upstrokes and bruits, PMI, etc. ______________________________________________________________ S3 and murmur of mitral stenosis ______________________________________________________________________ Murmur of aortic insuff ciency _________________________________________________________________________ Breasts and axillae _______________________________________________________________________________________ Abdomen _______________________________________________________________________________________________ Peripheral vascular; skin—lower torso and extremities ______________________________________________________ Nervous system: lower extremity motor strength, bulk, tone, sensation; ref exes ______________________________ Skin, anterior and posterior (may prefer in this position) ___________________________________________________ Nervous system, including gait ___________________________________________________________________________ Musculoskeletal, comprehensive _________________________________________________________________________ SECTION IV: DOCUMENTATION FORM TO BE USED IN PRACTICE 27 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the components of the general survey. 2. Identify appropriate subjective questions based on initial observations. 3. Demonstrate how to measure blood pressure, pulse, respiration, and temperature. 4. Discuss variations in vital signs and the possible causes. 5. Describe the different types of pain. 6. Perform and document a pain assessment utilizing information from the health history and the physical examination. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. is a nonspecif c sense of weariness with many causes. B. Decreased eye contact may be , or may suggest , , or . Beginning the Physical Examination: General Survey, Vital Signs, and Pain C. Blood pressure should be verif ed in the arm. D. Never assume that on a patient’s breath explains changes in status or f ndings. E. When you cannot hear sounds at all, you may be able to estimate the pressure by palpation. F. temperature measurements are more variable than or measurements. G. Thermometers used to measure fevers will not detect as thermometers only measure temperature and the core may still be . 2. List the four A’s of monitoring patient outcomes during the management of pain. A. B. C. D. C H A P T E R 7 28 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the areas that the nurse should assess during the general survey. A. B. C. D. E. F. G. H. I. J. Activity B MATCHING 4. Match the description of the blood pressure cuff error with the type of error (type of error will have multiple descriptions). Answer Description of Error Type of Error Cuff too small (narrow) A. False low readings Cuff too large (wide) B. False high readings Pressing stethoscope too tightly against pulse Inf ating or def ating cuff too slowly Cuff too loose or uneven Repeating assessments too quickly Def ating cuff too quickly 5. Match the problem obtaining an accurate blood pressure with the most likely solution or explanation for the problem. Answer Problem Possible Solution or Explanation Radial pulse is diff cult to f nd or there is an irregularity A. Doppler ultrasound stethoscope Weak or inaudible Korotkoff sounds B. Important to use a wide cuff of 15 cm Frequent premature contractions or atrial f brillation C. Apical pulse should be taken The patient has an obese arm D. Patient may have “white coat hyper tension” Palpation of an irregularly irregular rhythm E. Consider that there may be technical problems with equipment Weak pulse F. Determine the average of several observations and note that your measurements are approximate Patient’s blood pressure is higher in off ce setting than when taken in private G. Patient may have atrial f brillation CHAPTER 7 BEGINNING THE PHYSICAL EXAMINATION: GENERAL SURVEY, VITAL SIGNS, AND PAIN 29 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the def nition to its corresponding description. Answer Def nition Description Night sweats A. Can be used with unconscious patients Sweating B. Measures core body temperature Axillary temperatures C. Accompanies a rising temperature Feeling cold D. Usually blue Tympanic membrane temperature E. Usually red Rectal thermometer F. Accompanies a falling temperature Oral thermometer G. Occur in tuberculosis and malignancy c. Genetic composition d. Geographic location e. Cultural norms 12. Mr. Smith presents to the clinic stating, “My face looks funny.” You note that his face is asymmetric. What might you suspect is the patient’s problem? a. Myocardial infarction b. Parafacial macrosomia c. Muscular dystrophy d. Palsy 13. Mrs. Helms is admitted to your unit with an exacerbation of COPD. When you enter her room to do your initial assessment, you note that she is sitting on the side of the bed, leaning forward, with her arms on the bedside table. What would this indicate to you? a. Respiratory distress b. A relaxed attitude c. Depression d. Peripheral edema 14. A patient admitted to your unit from the emergency room is noted to have “grownout” nail polish. What might this indicate? a. Inability to give accurate history b. Depression c. Length of an illness d. Integumentary problems Activity C SHORT ANSWER 7. List the various techniques that the nurse can use to measure the severity of pain. 8. Discuss some of the health disparities that have been shown to inhibit the effective management of pain. 9. Compare and contrast the different types of pain. 10. In addition to pain assessment, list the vital signs that should be assessed during the general survey. Activity D NCLEX STYLE QUESTIONS 11. What factors contribute to the patient’s individual makeup? (Mark all that apply.) a. Ethnicity of patient b. Nutrition 30 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 15. As a nursing student you learn that the normal range for an adult pulse is what? a. 80–120 bpm b. 70–110 bpm c. 60–100 bpm d. 50–90 bpm 16. Fatigue is considered a common symptom of what? (Mark all that apply.) a. Infections b. Panhypopituitarism c. Mild anemia d. Depression e. Hyperthyroidism 17. You are educating your patient on taking blood pressure at home. What would be important to include in your patient education? a. Monthly replacement of batteries b. Routine recalibration of the device c. Application of a thigh cuff d. Use of a wrist cuff 18. Ideally, when taking a blood pressure, the patient should be instructed to what? a. Avoid smoking for 30 minutes prior to the assessment b. Sit quietly for at least 10 minutes in a chair, rather than on the examining table, with feet f at on the f oor and legs uncrossed c. Abstain from drinking caffeine for 45 minutes prior to the assessment d. Take several deep breaths to help relax prior to the assessment 19. The nurse should know that some disease processes affect facial expression. What are they? (Mark all that apply.) a. Diabetes mellitus b. Depression c. Multiple sclerosis d. Parkinsonism e. Hyperthyroidism 20. When counting the patient’s pulse, what beats may be diff cult to detect peripherally? a. Split beats b. Early beats c. Irregular beats d. Late beats SECTION III: CASE STUDY Activity E Ms. Cox has come to the clinic with a chief complaint of “severe sore throat.” She is 27 years old, is married, and has one child. She is dressed in jeans and a light sweater. Ms. Cox states that she generally enjoys good health and that this sore throat is a rare exception to this. She is appropriately interactive when conversing with you and ambulated steadily when she entered the room. You note a faint smell of tobacco smoke on Ms. Cox’s clothes and she does not appear to be in any distress. Her vital signs are unremarkable apart from a slightly elevated oral temperature. a. Document a general survey for this patient. 31 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Assess the nutritional status of an individual through a nutrition history and physical examination. 2. Identify persons at risk for malnutrition or overnutrition. 3. Differentiate between normal and abnormal nutrition assessment f ndings. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The MyPyramid Tracker provides information on quality and activity status. B. status is related to f uid intake and output and is critical to a patient’s health. C. Changes in result from changes in body or body f uid. D. In addition to the __________ history, the nurse should collect a sample intake record. E. Do not use a to measure height for children or unstable elderly; instead, use a attached to the wall. Nutrition F. Body fat consists primarily of adipose in the form of and is stored in , , and fat deposits that are diff cult to measure directly. 2. List the key messages for promoting patient nutrition. A. B. C. D. E. F. G. H. I. 3. List the assessment areas of a nutrition history. A. B. C. D. E. F. G. H. C H A P T E R 8 32 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 4. Match the assessment with the component of the general assessment during which it occurs. Answer Assessment Component of the General Assessment Nutrition A. ROS Weight changes B. Health patterns Exercise patterns Allergies Fatigue 5. Match the assessment area of the nutrition history with the question used to obtain the data. Answer Assessment Area Question Food pattern A. Are there any foods the client feels are harmful or benef cial? Personal food preferences B. How many meals are eaten outside the home? Food preparation C. Does the client take nutritional sup plements or vitamins? What type? Finances D. Is there transportation to the market? Accessibility E. Are there any eating disorders, heart disease, osteoporosis, diabetes, obe sity, or gastrointestinal disorders? Client health F. Is mealtime a social time? Family health G. Is any supplementary f nancial pro gram used? Family dietary patterns H. Who does the cooking? E. The patient should stand facing away from the scale with a straight back and the heels, hips, shoulders, and occiput aligned. Activity D SHORT ANSWER 7. Discuss the causes of weight loss. Activity C SEQUENCING 6. Show the suggested sequence for measuring height. A. Have the patient step off the scale or away from the wall. B. Raise the horizontal bar above the patient’s head and lower it until it just touches the crown of the head. C. On a balance beam scale read the height at the point where the top of the measuring slide comes out of the lower portion of the measuring slide. D. Have the patient remove shoes and hat. CHAPTER 8 NUTRITION 33 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 8. When taking a nutrition history, why is it also necessary to assess the gastrointestinal system? 9. List some of the signs or symptoms elicited during a nutritional assessment that would potentially signal health problems. 10. Name the sources for the following nutrients: calcium, iron, folate and vitamin D. Activity E NCLEX STYLE QUESTIONS 11. Which of the following are causes of weight loss? (Mark all that apply.) a. Hypothyroidism b. Chronic heart failure c. Chronic renal failure d. Chronic infections e. Adrenal insuff ciency 12. What can cause edema in a patient with a weak heart? a. Hyponatremia b. Dehydration c. Hyperproteinemia d. Overhydration 13. You note that your patient has developed mental status changes and paresthesias. What would you know to assess as a possible cause for these changes? a. Patient’s hydration status b. Patient’s intake of protein c. Patient’s vitamin intake d. Patient’s BMI 14. You are caring for a patient with hypertension. What dietary change would be appropriate to recommend? a. Eat fewer plantains b. Drink less orange juice c. Eat more spinach d. Drink more apple juice 15. As a nursing student you learn that obesityrelated risk factors include what? (Mark all that apply.) a. Infertility b. Hypermenorrhea c. Polycystic ovarian syndrome d. Type 1 diabetes e. Androgenicity 16. You are caring for a 16-year-old female patient diagnosed with anorexia nervosa. What biologic complication would you know to assess for? a. Severe cognitive disorder b. Increased corticotropin-releasing factor c. Diabetes mellitus d. Decreased BUN 17. You are teaching a health class. What would you tell older adults is necessary when they are exposed to heat stress or when they perform sustained vigorous physical activity? a. Fluid limitation b. Purposeful drinking c. 8–10 glasses of water daily d. 64 oz of nonsweetened f uid 18. You are counseling a 44-year-old woman about ways to maintain her weight, which is within normal range for her height. What should you suggest for her? a. 15 minutes per day of physical activity at a moderate intensity b. 30 minutes per day of physical activity at a moderate intensity c. 45 minutes per day of physical activity at a moderate intensity d. 60 minutes per day of physical activity at a moderate intensity 34 UNIT 1 FOUNDA TIONS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 19. A student asks the school nurse what the recommended daily allowance for sodium is. What should the school nurse reply? a. 2400 mg/day b. 1800 mg/day c. 1200 mg/day d. 600 mg/day 20. When teaching a nutrition class, what would you recommend for adults older than the age of 50? a. Increase foods rich in vitamin B6 and saturated fats b. Increase foods rich in vitamin E and folic acid c. Increase foods rich in vitamin B12 and calcium d. Increase foods rich in vitamin B6 and vitamin D SECTION III: CASE STUDY Activity F Penny Sandusky, 53 years old, comes to the clinic with a chief complaint of unintended weight loss of 10 pounds over an 8-week period. She is 5'4" tall and had a BMI of 24.88 when she started losing weight. a. Describe the areas of a physical examination you would look at to assess for nutritional def ciencies. b. When assessing Mrs. Sandusky’s weight loss, what questions should you ask her? 35 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the structures of the skin, nails, and hair. 2. Explain the functions of the integumentary system. 3. Identify risk factors for pressure ulcers. 4. Identify risk factors for skin cancer. 5. Obtain an accurate history of the integumentary system. 6. Appropriately prepare and position the client for the integumentary examination. 7. Describe the equipment necessary to perform an integumentary examination. 8. Correctly perform an integumentary examination. 9. Accurately describe primary, secondary, and vascular lesions. 10. Discuss risk reduction and health promotion strategies to reduce skin cancer. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The skin contains layers: the , the , and the tissues. The Integumentary System B. An increase in blood f ow through the to the causes a of the skin, whereas the opposite change usually produces . C. Adults have two types of hair: , which is short, f ne, inconspicuous, and relatively unpigmented; and , which is coarser, thicker, more conspicuous, and usually pigmented. D. The f rm, rectangular, and usually curving plate gets its pink color from the to which the plate is f rmly attached. E. The glands are widely distributed, open directly onto the surface, and by their production help to control . F. Remember to your f ndings with observations of the mucous , especially when assessing skin , because may appear in both areas. G. result when compression arteriolar and capillary blood f ow to the . C H A P T E R 9 36 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. H. The is a ratio of the number of minutes for treated versus untreated skin to with exposure to . I. Early detection of , when mm or less, signif cantly improves . J. Inspect the scalp for , , and by separating the hair at inch intervals. 2. List the functions of the skin. A. B. C. Activity B MATCHING 4. Match the type of skin cancer with the description (skin cancers will have multiple descriptions). Answer Description Type of Skin Cancer Most rapidly increasing U.S. malignancy A. Basal cell carcinoma Often crusted and scaly B. Squamous cell carcinoma Pearly white and translucent C. Melanoma Accounts for approximately 16% of skin cancers Can spread rapidly to the lymph system and internal organs Rarely metastasizes 5. Match the type of skin lesion with its description. Answer Type of Skin Lesion Description Primary skin lesions (primary presentation) A. Comedones, papules, pustules, and alcohol Secondary skin lesions B. Pitting and scars Secondary skin lesions—depressed C. Ecchymosis Acne vulgaris—primary lesion D. Dry skin Acne vulgaris—secondary lesion E. Cherry angioma Vascular lesion F. Café-au-lait spot Purpuric lesion G. Excoriation D. E. F. G. H. 3. List the characteristics of the skin assessed in a physical examination. A. B. C. D. E. F. G. CHAPTER 9 THE INTEGUMENTARY SYSTEM 37 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity C SEQUENCING 6. Put the following actions in the correct sequence for skin self-examination: A. Examine the right and left sides with arms raised. B. Look at the backs of your legs and feet, the spaces between your toes, and the sole. C. Examine the back of your neck and scalp with a hand mirror. D. Check your back and buttocks with a hand mirror. E. Examine your body front and back in the mirror F. Bend elbows and look carefully at forearms, upper underarms, and palms. Activity D SHORT ANSWER 7. Describe how the eight major functions of the skin contribute to homeostasis. 8. Discuss the purpose of the integumentary history. 9. Explain the difference between pitting and nonpitting edema and how each is assessed. 10. When assessing a lesion, explain the different characteristics that you would examine and document. Activity E NCLEX STYLE QUESTIONS 11. You are using the Braden Scale to measure risk factors for pressure sores. What risk factors will you assess? a. Admitting diagnosis b. Moisture c. Age d. Activity e. Nutrition 12. When assessing your new patient, you note that he has no hair on his legs. What might this indicate about the patient? a. He has a hormonal imbalance b. He has hyperthyroidism c. He has peripheral artery disease d. He has hypothyroidism 13. When educating a patient about the risks of malignant melanoma, what would you know to include? (Mark all that apply.) a. Red or light hair b. Freckles c. Immunosuppression d. Female gender e. Age older than 60 14. A 16-year-old African-American girl shows the school nurse a rash that has developed on the back of her left hand. You assess the rash as a depigmented macular area. What might the nurse suspect? a. Addison disease b. Vitiligo c. Tinea versicolor d. Dermatomyositis 15. A golden yellow pigment that is heavily keratinized and is found in subcutaneous fat is called what? a. Oxyhemoglobin b. Deoxyhemoglobin c. Carotene d. Melanin 38 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 16. The student nurse learns that examining the skin can do what? a. Reveal overhydration b. Allow early identif cation of neurologic def cits c. Rule out physical abuse d. Allow early identif cation of risk factors for dehydration 17. Which of the following scores on the Braden Scale signif es that the patient is not at risk for a pressure sore? a. 9 or lower b. 10 to 12 c. 13 to 18 d. 19 to 23 18. A 67-year-old male patient tells the clinic nurse that his feet and lower legs turn a blue color. On assessment, the nurse notes that the patient’s oxygenation level is within normal levels. The nurse knows that the blue color the patient described is caused by what? a. Reynaud disease b. Central cyanosis c. Neurof bromatosis d. Peripheral cyanosis 19. The apocrine glands are stimulated by what? a. Emotional stress b. Temperature c. Physical stress d. Overhydration 20. In what age group does the American Cancer Society recommend yearly skin examination as part of a routine cancer-related check-up? a. 30 or older b. 40 or older c. 50 or older d. 60 or older SECTION III: CASE STUDY Activity F Belinda Mitchell, a 53-year-old Caucasian female, has been referred to the dermatology clinic because of a suspicious lesion on the inside of her left thigh. A biopsy of the lesion is negative for cancer. a. Develop a teaching plan for this patient covering the risks for malignant melanoma. b. Explain what you would teach the patient about the technique for self-examining moles for malignant melanoma. CHAPTER 9 THE INTEGUMENTARY SYSTEM 39 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. INTEGUMENTARY SYSTEM ASSESSMENT Patient Name ____________________________________________________ Date/Time _________________________________ Overview. ___________________________________________________________________________________________________ Identifying Data ______________________________________________________________________________________________ Source and Reliability __________________________________________________________________________________________ Common or Concerning Symptoms ____________________________________________________________________________ Onset ______________________________________________________________________________________________________ Location ___________________________________________________________________________________________________ Duration ___________________________________________________________________________________________________ Characteristic symptoms ____________________________________________________________________________________ Associated manifestations ___________________________________________________________________________________ Relieving/exacerbating factors _______________________________________________________________________________ Treatment __________________________________________________________________________________________________ Past History __________________________________________________________________________________________________ Skin diseases _______________________________________________________________________________________________ Diabetes or peripheral vascular disease ________________________________________________________________________ Allergies or food sensitivities _________________________________________________________________________________ Burns (including sunburns) __________________________________________________________________________________ Medications ________________________________________________________________________________________________ Corticosteroids ___________________________________________________________________________________________ OTCs ____________________________________________________________________________________________________ Family History _______________________________________________________________________________________________ Same or similar symptoms ___________________________________________________________________________________ Melanoma, eczema, or psoriasis or skin biopsies _______________________________________________________________ Allergies ____________________________________________________________________________________________________ Health Maintenance __________________________________________________________________________________________ Immunizations _____________________________________________________________________________________________ Screening tests ______________________________________________________________________________________________ Lifestyle and Personal Habits ___________________________________________________________________________________ Bathing and shampooing routines ___________________________________________________________________________ Changed brands ____________________________________________________________________________________________ False nails or wigs ___________________________________________________________________________________________ Nail salon or gym ___________________________________________________________________________________________ Daily sun exposure __________________________________________________________________________________________ Sunscreen use ______________________________________________________________________________________________ SPF ______________________________________________________________________________________________________ Skin self-examinations ______________________________________________________________________________________ Chemicals or radiation exposure _____________________________________________________________________________ Hobbies ____________________________________________________________________________________________________ Typical day’s diet ___________________________________________________________________________________________ Physical Examination _________________________________________________________________________________________ Skin _______________________________________________________________________________________________________ Color ____________________________________________________________________________________________________ Moisture _________________________________________________________________________________________________ T emperature _____________________________________________________________________________________________ T exture __________________________________________________________________________________________________ Mobility and Turgor _______________________________________________________________________________________ Edema ___________________________________________________________________________________________________ Lesions __________________________________________________________________________________________________ Hair _______________________________________________________________________________________________________ Nails _______________________________________________________________________________________________________ Health Promotion ____________________________________________________________________________________________ Patient Instructions for the Skin Self-Examination _______________________________________________________________ SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE 40 C H A P T E R 10 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the structures of the head and neck and the purpose of each. 2. Perform an accurate health history of the head and neck. 3. Perform the physical examination techniques to evaluate the head and neck. 4. Document the physical examination results. 5. Determine the measures for prevention of traumatic brain injury. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Every warrants careful evaluation for life-threatening causes such as meningitis, or ___________ , or tumor. B. An , with neurologic symptoms, may a headache. C. The function of the system is to detect and eliminate substances. D. Deep to the sternomastoids run the of the neck: the artery and the internal . The Head and Neck E. is an anomaly characterized by a small in proportion to the and an underdeveloped . F. The nodes lie in the angle between the and the sternomastoid. G. Tracheal may also signify important problems in the thorax, such as a mediastinal , , or a large . H. The cartilage, the cartilage, and the gland all rise with swallowing and then fall to their resting positions. 2. List the “red f ags” that suggest secondary causes to headaches. A. B. C. D. E. F. G. H. I. J. K. L. CHAPTER 10 THE HEAD AND NECK 41 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the steps for palpating the thyroid gland using the posterior approach. A. B. C. D. E. Activity B MATCHING 4. Match the description of head pain with the type of head pain. Answer Description of Head Pain Type of Head Pain Around the eyes A. Sinus headache Most often the temporal, but also the occipital B. Subarachnoid hemorrhage Cheek, jaws, lips, or gums C. Brain tumor Nausea, vomiting, possibly loss of consciousness, neck pain D. Meningitis Mental and physical exertion E. Trigeminal neuralgia Occurs after medication is discon tinued F. Acute glaucoma In and around one eye G. Posttraumatic headache Generalized, fever, stiff neck H. Giant cell arteritis Often intermittent but progressive I. Headaches from eye disorders Usually above the eyes J. Analgesic rebound 5. Match the facies with their description. Answer Facies Description Parkinson disease A. The head is elongated, with bony promi nence of the forehead, nose, and lower jaw. Myxedema B. Chronic bilateral asymptomatic swellings anterior to the ear lobes Cushing syndrome C. Swelling usually appears f rst around the eyes and in the morning. Acromegaly D. A mask-like face may result, with decreased blinking and a characteristic stare. Parotid gland enlargement E. A dull, puffy facies Nephrotic syndrome F. A round or “moon” face with red cheeks 42 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity C SEQUENCING 6. Put the palpation of lymph nodes in the correct sequence. A. Occipital B. Submandibular C. Posterior auricular D. Superf cial cervical E. Deep cervical chain F. Preauricular G. Submental H. Supraclavicular I. Posterior cervical J. Tonsillar Activity D SHORT ANSWER 7. List and explain the educational topics you would address when teaching a patient to prevent falls. 8. Explain the process for assessing the trachea and thyroid gland. 9. List the assessment parameters that are applicable to a patient with migraines. 10. Name and explain the four major common or concerning symptoms of the head. Activity E NCLEX STYLE QUESTIONS 11. What activity is known to aggravate a tension headache? a. Listening to music b. Exercise c. Driving d. Prolonged sleep 12. A 16-year-old white female is brought to the clinic by her mother with a chief complaint of a severe headache lasting more than 24 hours. The mother states, “Just before the headache started my daughter was craving food. I couldn’t feed her enough.” What is this called? a. Aura b. Prodrome c. Neurologic onset d. Aberrant sign 13. What are associated manifestations of a headache caused by a traumatic head injury? (Mark all that apply.) a. Attention span def cit b. Changes in appetite c. Gait changes d. Seizures e. Apathy 14. The nursing instructor is discussing assessment of the head and neck with the class. What identifying characteristic would the instructor use for the thyroid cartilage? a. Its position just below the mandible b. The curve on its inferior edge c. Its relation to the cricoid cartilage d. The notch on its superior edge 15. During your physical examination of the patient you note an enlarged tender tonsillar lymph node. What would you do? a. Assess for meningitis b. Look for involvement of other regions of the body c. Look for a source such as infection in the area that it drains d. Assess for dietary changes CHAPTER 10 THE HEAD AND NECK 43 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 16. What are the bordering landmarks of the anterior triangle of the neck? (Mark all that apply.) a. The sternomastoid b. The mandible c. The midline of the neck d. The omohyoid muscle e. The clavicle 17. A 43-year-old Asian female presents at the clinic for a routine check-up. The nurse notes that she is dressed in warm clothing even though the temperature outside is 73°F. The nurse also notes that the patient has gained 10 pounds since her last visit 9 months ago. What might the nurse suspect? a. Effects of age-related changes b. Brain tumor c. Hyperthyroidism d. Hypothyroidism 18. A 72-year-old male arrives in the emergency department by ambulance after falling down his front steps. You note two soft lumps, approximately 3 cm in diameter, on the side of his head. What would you identify these as? a. Pilar cysts b. Pigmented nevi c. Signs of abuse d. Edema from fall 19. When assessing your patient’s head and neck, what would you assess the face for? (Mark all that apply.) a. Hair color b. Asymmetry c. Affect d. Edema e. Involuntary movements 20. When assessing a patient with Graves disease, how would you expect the thyroid gland to be? a. Soft b. Firm c. Nodular d. Tender SECTION III: CASE STUDY Activity F Brian Miller is brought to the emergency room by his parents after being knocked unconscious in a high school football game. Vital signs include BP 105/ 80; HR 80; respirations 16; T 38°C; eyes PERRLA. a. When completing an assessment on this patient, what would you focus on? b. Explain why a CT scan of the head and neck would be an important assessment tool. 44 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE HEAD AND NECK ASSESSMENT Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms of the Head Common or Concerning Symptoms of the Neck History of Present Illness Onset Location Duration Characteristic symptoms Associated manifestations Relieving/exacerbating factors Treatment Past History Allergies Medications Past head trauma Thyroid problems Health Maintenance Immunizations Screening tests Risk Factors Tobacco Alcohol/drugs Family History Headaches Thyroid disease Brain tumors Review of Systems General Hair Scalp Skull Face Skin Neck Lymph nodes Trachea and the thyroid gland Carotid arteries and jugular veins Health Promotion, Disease Prevention, and Education: Head Prevention of traumatic brain injury Fall prevention Prevention of head injuries in motor vehicle accidents Prevention of injuries from being hit by an object 45 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the components of the eye and the function of each. 2. Perform an accurate health history of the eye. 3. Describe the physical examination techniques performed to evaluate the eye. 4. Demonstrate how to use the ophthalmoscope. 5. Determine the measures for prevention or early detection of eye disease, infections, or vision loss. 6. Perform and document a complete eye assessment utilizing information from the health history and physical examination. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. A f lm of protects the and from drying, inhibits , and gives a optical to the cornea. B. A is the entire area seen by an eye when it looks at a . C. A light beam shining onto one causes pupillary both in that eye, termed the The Eyes reaction, and in the opposite eye, the ____________ reaction. D. can occur and the eye if contact lenses are not taken care of . E. , also known as “lazy eye,” is a of vision due to lack of use, and is eye misalignment; these are found most frequently in and children up to years old. F. Vision is a critical sense for experiencing the world around us, and areas of importance are and . 2. List the posterior structures of the eye seen through an ophthalmoscope, beginning with the retina. A. B. C. D. E. F. 3. List the cardinal directions of gaze. A. B. C. D. E. F. C H A P T E R 11 46 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity B MATCHING 4. Match the pupillary abnormality with its description. Answer Description Pupillary Abnormality Unequal pupils A. Tonic pupil Does not cause anisocoria as long as the sympathetic and parasympathetic innervation to both irises is normal B. Horner syndrome Reaction to light is severely reduced and slowed, or even absent C. Oculomotor nerve (CN III) paralysis Pupils that accommodate but do not react to light D. Anisocoria The dilated pupil is f xed to light and near effort. Ptosis of the upper eyelid and lateral deviation of the eye are almost always present E. Presence of equal pupils and one blind eye The affected pupil, though small, reacts briskly to light and near effort. Ptosis of the eyelid is present, perhaps with loss of sweating on the forehead F. Small, irregular pupils (Argyll Robertson pupils) 5. Match the lump or swelling in and around the eye with its description. Answer Lump or Swelling Description Pinguecula A. A localized ocular redness from inf ammation of the episcleral vessels Hordeolum B. A swelling between the lower eyelid and nose Xanthelasma C. A subacute, nontender, and usually painless nodule involving a meibo mian gland Episcleritis D. A painful, tender red infection in a gland at the margin of the eyelid Chalazion E. Yellowish triangular nodule in the bulbar conjunctiva on either side of the iris Dacryocystitis F. Slightly raised, yellowish, well circumscribed plaques that appear along the nasal portions of one or both eyelids CHAPTER 11 THE EYES 47 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity C SHORT ANSWER 6. Explain the differences between a nuclear and a peripheral cataract. 7. Compare and contrast two or more of the following types of red eyes: conjunctivitis, subconjunctival hemorrhage, corneal injury or infection, acute iritis, and glaucoma. 8. Explain the visual pathway, beginning with light entering the pupil and ending with a signal in the visual cortex. 9. Discuss the processes for testing distal vision, near vision, and peripheral f elds. Activity D NCLEX STYLE QUESTIONS 10. What is a characteristic symptom of Graves hyperthyroidism? a. Pterygium b. Exophthalmos c. Pinguecula d. Episcleritis 11. What is the primary purpose of the health history in relation to the eyes? a. To identify a family history of ocular disease b. To identify if problems are unilateral or bilateral c. To test the acuity of central vision d. To identify changes 12. A patient in the clinic where you work is considered legally blind. You know that this means the vision in his better eye, corrected by glasses, is what? a. 20/100 or less b. 20/200 or less c. 20/300 or less d. 20/400 or less 13. You are assessing visual f elds on a patient newly admitted for eye surgery. The patient’s left eye repeatedly does not see your f ngers until they have crossed the line of gaze. You would document that the patient has what? a. A left temporal hemianopsia b. A homonymous hemianopsia c. A bitemporal hemianopsia d. A quadrantic defect 14. What are you testing when you ask the patient to follow your f nger or pencil as you move it in toward the bridge of the nose? a. Accommodation b. EOM c. Convergence d. Visual f elds 15. What systemic diseases may cause nodular episcleritis? (Mark all that apply.) a. Systemic lupus erythematosus b. Multiple sclerosis c. Fibromyalgia d. Muscular dystrophy e. Rheumatoid arthritis 16. When examining the eye with an ophthalmoscope, where would you look to visualize the optic disc? a. Medially toward the nose b. Laterally toward the ear c. Upward toward the forehead d. Downward toward the chin 48 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 17. You note anterior bulging of the physiologic cup when performing a funduscopic examination of your patient’s eyes. What would you document? a. Positive axoplasmic sign b. Arteriovenous crossings c. Papilledema d. Hyperopia 18. What are the glands that are located on the tarsal plates and open on the lid margins? a. Levator glands b. Chalazion glands c. Pterygium glands d. Meibomian glands 19. What is vital in maintaining vision and a healthy outlook for clients? a. Health education b. Monthly eye exams c. Emotional support d. Physical exercise SECTION III: CASE STUDY Activity E Bud Thygeson, a 57-year-old cabinet maker, presents at the clinic with a chief complaint of left eye pain. He states, “I got something in my eye at work.” a. Describe how you would examine Mr. Thygeson’s upper palpebral conjunctiva for the presence of a foreign body. b. What would you include in a teaching plan for Mr. Thygeson? SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE EYE EXAMINATION Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Eye History Do you have any past history of eye problems or eye disease? Do you have a history of: Premature birth? Trauma or injury to the eye? Eye surgery? Related to injury, congenital causes, or cosmetic reasons? Eye infections? Strabismus? Cataracts? Glaucoma? Diabetes? Retinal detachment? Macular degeneration? Blindness? When was your last eye examination? Test for color blindness? CHAPTER 11 THE EYES 49 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Do you wear glasses or contact lenses? When did you begin to wear them? Are they corrective or cosmetic? How do you care for your contacts? Do you share contacts? How long are the contacts in your eye? Day hours? Night hours? Family History Do you have a family history of congenital eye diseases, cataracts, glaucoma, macular degeneration, or diabetes? Lifestyle Habits Do you smoke? Do you use contacts? Do you use goggles or protective eyewear? When? Are you on any medications/drugs that dry out the eye? Physical Examination Vision tests Distal Near Peripheral Inspection of the eye Eyebrows Lids Conjunctiva Sclera Cornea Lens Iris Pupils Inspection and palpation of the lacrimal apparatus Extraocular movements Assessment of cardinal f elds Convergence Corneal light test Cover–uncover test Inspection of the fundi Optic disc and cup Retina Retinal vessels 50 C H A P T E R 12 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the structures of the ear, nose, mouth, and throat and the purpose of each. 2. Perform an accurate health history of the ear, nose, mouth, and throat. 3. Describe the physical examination techniques performed to evaluate the ear, nose, mouth, and throat. 4. Demonstrate how to use the otoscope. 5. Determine the measures for prevention or early detection of ear, sinus, and throat infections; hearing loss; change in balance; and maintenance of oral health. 6. Perform and document a complete ear, nose, mouth, and throat assessment utilizing information from the health history and the physical examination. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The nurse’s role is to detect changes and work with the health care team to prevent or loss . Ears, Nose, Mouth, and Throat B. The nurse assesses the patient for and to maintain sensory organs. C. The lowest portion of the temporal bone, the , is palpable behind the . D. The second part of the hearing pathway, involving the and the nerve, is called the phase; a disorder here causes hearing loss. E. Air enters the nasal cavity by way of the on either side, then passes into a widened area known as the and on through the narrow nasal passage to the . F. The paranasal sinuses are air f lled and make the skull and add to speech . G. Nasal sprays, if overused, can contribute to the , causing and . H. A midline mucosal fold, called a , connects each lip with the . I. At the base of the tongue the of the gland pass and . J. Each duct opens onto the mucosa near the upper second molar. CHAPTER 12 EARS, NOSE, MOUTH, AND THROAT 51 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 2. List the most common or concerning symptoms of the mouth and throat. A. B. C. D. E. F. G. 3. A nurse is preparing to conduct a physical assessment of a patient’s mouth and throat. What equipment will the nurse require? A. B. C. D. Activity B MATCHING 4. Match the term for dizziness with its description. Answer Term Description Vertigo A. Causes include anxiety, panic disorder, hyper ventilation, depression, somatization disorder, and alcohol and substance abuse Presyncope B. Unsteadiness or imbalance when walking Dysequilibrium C. A spinning sensation accompanied by nystagmus and ataxia Psychiatric D. A near faint from “feeling faint or lightheaded” 5. Match the abnormality of the eardrum with its description. Answer Abnormalities of the Eardrum Description Perforation of the drum A. Viral infection characterized by painful hemor rhagic vesicles that appear on the tympanic membrane, the ear canal, or both Tympanosclerosis B. Caused by bacterial infection Serous effusion C. Holes in the eardrum that usually result from purulent infections of the middle ear Bullous myringitis D. A deposition of hyaline material within the layers of the tympanic membrane that sometimes follows a severe episode of otitis media Acute otitis media with purulent effusion E. Usually caused by viral upper respiratory infections or by sudden changes in atmospheric pressure as from f ying or diving 52 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the oral abnormality to its corresponding description. Answer Abnormality Description Geographic tongue A. Painful, round or oval ulcer Fissured tongue B. Small purplish or blue-black round swellings under the tongue Candidiasis C. The undersurface of the tongue appears painted white Hairy tongue D. Slightly raised, oval, and covered by a grayish membrane Smooth tongue E. Rounded bony growths Hairy leukoplakia F. Thick white coating Varicose veins G. Sometimes termed scrotal tongue Mucous patch of syphilis H. A map-like pattern that changes over time Tori mandibulares I. Medially, note the reddened area of mucosa, called erythro plakia, suggesting possible malignancy Aphthous ulcer J. Yellowish to brown or black elongated papillae on the tongue’s dorsum Leukoplakia K. Whitish raised areas with a feathery or corrugated pattern Carcinoma, f oor of the mouth L. Suggests a def ciency in ribof avin, niacin, folic acid, vitamin B12, pyridoxine, or iron, or treatment with chemotherapy 10. Explain the technique for the physical examination of the tongue and the f oor of the mouth. Activity D NCLEX STYLE QUESTIONS 11. When providing patient education on hearing, patients should be reminded to utilize ear plugs when they are what? (Mark all that apply.) a. At train stations b. Cleaning their homes c. Using lawnmowers d. Working with children e. At concerts 12. Functionally, the most important range for hearing is the range of human speech. What is the range of human speech? a. 150 Hz to 1500 Hz b. 200 Hz to 2000 Hz c. 250 Hz to 2500 Hz d. 300 Hz to 3000 Hz Activity C SHORT ANSWER 7. Explain the anatomy and physiology of the pathway of hearing. 8. Def ne tinnitus and list the most common causes, characteristics, and manifestations. 9. Relate the anatomy and physiology of the nose to its functions in maintaining homeostasis. CHAPTER 12 EARS, NOSE, MOUTH, AND THROAT 53 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 13. When assessing a patient you note that the tonsils are touching the uvula. How would you document the tonsils? a. Tonsils are T4 b. Tonsils are T3 c. Tonsils are T2 d. Tonsils are T1 14. What is the average age of signif cant hearing loss detected if the infant is not assessed prior to leaving the hospital at birth? a. 10 months b. 14 months c. 19 months d. 24 months 15. You are teaching a health class on a college campus. What would you teach the students to use during oral sex to help reduce the transmission of STDs? a. Oral barriers b. Dental prophylactic c. Dental dams d. Oral condoms 16. What structure in the inner ear senses the position and movements of the head and helps to maintain balance? a. The cochlea b. The labyrinth c. The umbo d. The ossicle 17. An alternate pathway that bypasses the external and middle ear is called what? a. Bone conduction b. Sensory conduction c. Neuro conduction d. Air conduction 18. A patient presents at the clinic with a chief complaint of right ear pain. You note a rash in the right ear canal. What should you know is a possible cause of these symptoms? a. Acute ossiculo-mastitis b. Chronic otosclerosis c. Acute mastoiditis d. Chronic otitis media 19. Your patient is complaining of nasal stuff - ness. What drugs should you ask if she is taking? (Mark all that apply.) a. Guaifenesin b. Oral contraceptives c. Nicotine d. Alcohol e. Guanethidine 20. What lines the cheeks? a. Lingual mucosa b. Alveolar mucosa c. Buccal mucosa d. Labial mucosa SECTION III: CASE STUDY Activity E Marcus Merriweather, a 55-year-old white male, presents at the clinic complaining of decreased hearing for the past 6 weeks. He works in a bowling alley. a. Describe an appropriate physical examination for this patient. b. Develop a teaching plan for this patient. 54 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE EARS, NOSE, MOUTH, AND THROAT Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms of the Ears History of Present Illness Onset Location Duration Characteristic symptoms Associated manifestations Relieving/exacerbating factors Treatment Past History Congenital hearing loss Removal of cerumen Ear surgery Trauma or injury to ear(s) Exposure to hazardous noise levels (work, home, war) History of syphilis, rubella, meningitis Family History Hearing loss Otitis media Allergies Smoking or exposure to cigarette smoke Lifestyle Habits Are you exposed to loud noises? What is your occupation? Hobbies (e.g., hunting)? Do you attend concerts? Bars? Loud places? Do you use headphones or earbuds to listen to music? Do you use an iPod? How often? On what level? Do you use a lawnmower? Power tools? Firearms? Do you live near a busy road or train tracks? Have you ever used ear plugs/protectors? Currently? Have you ever used hearing aid(s)? Which ear? Currently? At all times? Brand? Have you used medications or drugs that interfere with how you hear or cause dizziness? Any medications that cause ototoxicity (e.g., large doses of antibiotics infused rapidly)? Common or Concerning Symptoms of the Nose and Sinuses History of Present Illness Onset Location Duration Characteristic symptoms Associated manifestations Relieving/exacerbating factors Treatment CHAPTER 12 EARS, NOSE, MOUTH, AND THROAT 55 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Past History Sinus infections Upper respiratory infections Allergies Trauma or injury Nasal or sinus surgery Polyps Dental history Family History Allergies Asthma Cancer of the nose or sinus Lifestyle Habits Air quality: at home and work, how often f lters are changed, age of home and work or school site, rugs Pets: What kind? How many? Are they in the house or outside? Do they sleep in bed with the patient? Alcohol: What kind? How much? Tobacco use: What kind? How often? How many? Recreational drugs: What kind? Route? How often? Common or Concerning Symptoms of the Mouth and Throat History of Present Illness Onset Location Duration Characteristic symptoms Associated manifestations Relieving/exacerbating factors Treatment Past History Sore throats Loss of voice Dental, mouth, or throat surgery Trauma or injury to teeth, mouth, or throat Exposure to hazardous noise levels (work, home, war) History of infections Oral cancer STDs Family History Allergies Smoking or exposure to cigarette smoke Stroke Tuberculosis Lifestyle Habits Do you see a dentist? When was your last exam? What were the results? How many times a day do you brush your teeth? Do you f oss? How often? Do you use tobacco? Cigarettes, cigars, a pipe, or chewing tobacco? How many per day? Since when? Do you smoke marijuana? Crack? Inhale any other product? Do you drink alcohol? What? How many ounces per day? 56 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. What is your occupation? Do you attend concerts? Bars? Loud places? Do you use dental dams? Physical Examination of the Ears The auricle Ear canal and drum Auditory acuity Air and bone conduction Physical Examination of the Nose Inspect the anterior and inferior surfaces of the nose Inspect the inside of the nose Physical Examination of the Mouth and Throat The lips The oral mucosa The gums and teeth The roof of the mouth The tongue and the f oor of the mouth The pharynx Health Promotion, Disease Prevention, and Education: Ears Hearing screening Ear protection Health Promotion, Disease Prevention, and Education: Mouth and Throat Oral and dental screening Cancer prevention 57 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Describe the structure and functions of the airways, alveoli, lungs, and pleura. 2. Identify the locations of each lung lobe using landmarks on the thorax. 3. Describe the mechanics of breathing. 4. Identify the percussion and auscultation sites for assessment of the lungs. 5. Describe the normal lung sounds and their location. 6. Describe adventitious sounds and voice sounds and their origin. 7. Obtain an accurate history of the respiratory system. 8. Appropriately prepare and position the client for the respiratory examination. 9. Describe the equipment necessary to perform a respiratory examination. 10. Correctly inspect, palpate, percuss, and auscultate the anterior and posterior thorax. 11. Discuss risk factors for respiratory disease. 12. Discuss risk reduction and health promotion strategies to reduce respiratory disease. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. In a woman, to f nd the spaces, either the __________ The Respiratory System laterally or closer to the sternum. B. As you percuss down the chest on the left, the of normal lung usually changes to the of the gastric air bubble. C. sets the chest wall and underlying tissues in motion, producing and palpable . D. refers to the palpable vibrations transmitted through the to the as the patient is . E. When examining the posterior thorax, try to visualize the , and compare one side with the other, so that the serves as his or her own . F. Cough is typically a to stimuli that irritate receptors in the , , or . 2. List the groups for whom the CDC recommends the pneumococcal vaccine. A. B. C. D. E. F. C H A P T E R 13 58 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the anatomic sources of chest pain. A. B. C. D. E. F. G. H. Activity B MATCHING 4. Match the type of breath sound with its most accurate description (breath sounds may have multiple descriptions). Answer Description Type of Breath Sound Musical, prolonged A. Crackles (or rales) Discontinuous B. Wheezes and rhonchi Soft, high pitched, very brief C. Fine crackles Continuous D. Course crackles Like dots in time E. Wheezes Relatively high pitched with hissing or shrill quality F. Rhonchi Somewhat louder, lower in pitch, brief (20–30 msec) Relatively low pitched with snoring Like dashes in time Intermittent, nonmusical, and brief 5. Match the respiratory term with its description. Answer Term Description Dyspnea A. Inspiratory and expiratory sounds about equal in length Wheezes B. Fade away about one third of the way through expiration Cough C. Suggest partial airway obstruction from secretions, tissue inf ammation, or a foreign body Bronchovesicular sounds D. Have a short silence between inspiratory and expiratory sounds Vesicular sounds E. May be caused by inf ammation of the respiratory mucosa or tension in the air passages from a tumor or enlarged peribronchial lymph nodes Bronchial sounds F. Shortness of breath CHAPTER 13 THE RESPIRATORY SYSTEM 59 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the disease process to its corresponding location of chest pain. Answer Disease Process Corresponding Location of Chest Tracheobronchitis A. Retrosternal or across the anterior chest Pericarditis B. Precordial, below the left breast, or across the anterior chest Dissecting aortic aneurysm C. Retrosternal, may radiate to the back Ref ex esophagitis D. Often below the left breast Diffuse esophageal spasm E. Sometimes radiating to the shoulders, arms, neck, lower jaw, or upper abdomen Costochondritis F. Upper sternal or on either side of the sternum Pleuritic pain G. Retrosternal, may radiate to the back, arms, and jaw Anxiety H. Anterior chest, radiating to the neck, back, or abdomen Angina pectoris I. Precordial, may radiate to the tip of the shoulder and to the neck Myocardial infarction J. Chest wall overlying the process Activity D NCLEX STYLE QUESTIONS 11. What is the best guide to make vertical locations on the chest? a. Midclavicular line b. Sternal angle c. Angle of Henri d. 5th intercostal space 12. When assessing the posterior chest, what is a starting point for counting ribs and interspaces? a. 6th rib b. 8th rib c. 10th rib d. 12th rib 13. Which ribs are considered “f oating ribs”? a. 11th and 12th b. 10th and 11th c. 9th and 10th d. 8th and 9th 14. When assessing posteriorly, where would the trachea bifurcate into its mainstem bronchi? a. Sternal angle b. T4 spinous process c. Suprasternal notch d. Midaxillary line Activity C SHORT ANSWER 7. Explain how to use chest landmarks for respiratory assessment. 8. Discuss adventitious breath sounds and their causes. 9. Describe the physical f ndings that characterize two or more chest disorders and contrast these with normal f ndings. 10. Describe the technique for conducting the initial survey of respiration and the thorax. 60 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 15. Dyspnea, an uncomfortable awareness of breathing that is inappropriate to the level of exertion, is what? a. Audible breathing b. Painful breathing c. Air hunger d. Prolonged inspiration 16. A 25-year-old male patient is brought to the emergency department by ambulance after being involved in a motor vehicle accident. You f nd that he has decreased breath sounds over the left lung f elds. What might you suspect is the cause? a. Pneumothorax b. Atelectasis c. Muscular weakness d. Asthma 17. When assessing the breath sounds of a newly admitted patient, the nurse notes increased transmission of voice sounds over the right lung. What would this indicate to the nurse? a. The lung is full of f uid b. The lung has an embolus c. The lung is overinf ated d. The lung has become airless 18. What replaces resonance when f uid or solid tissue replaces air-containing lung or occupies the plural space? a. Hyperresonance b. Dullness c. Tympany d. Chief complaint 19. What associated symptoms might a patient with a history of chronic bronchitis have? (Mark all that apply.) a. Orthopnea b. Chronic productive cough c. Paroxysmal nocturnal dyspnea d. Recurrent respiratory infections e. Wheezing 20. You are caring for an 80-year-old Hispanic woman who is 48 hours postop from the repair of a fractured hip. She has a sudden onset of dyspnea without pain. What disease process would you suspect? a. Left ventricular failure b. Asthma c. Pulmonary embolism d. Chronic lung disease SECTION III: CASE STUDY Activity E Stan Conner, 62 years old, presents at the clinic with a chief complaint of malaise. He tells the nurse, “I just don’t feel good.” Vital signs are T 37°C; respirations 25 and shallow; HR 100 bpm; BP 125/85. Past history indicates Mr. Conner has been a pack-a-day smoker for 30 years. Family history is positive for paternal COPD and lung cancer. a. What characteristics of Mr. Conner’s case should you prioritize when planning a focused respiratory assessment? Mr. Conner is being evaluated for COPD. b. Develop a teaching plan for Mr. Conner. CHAPTER 13 THE RESPIRATORY SYSTEM 61 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE RESPIRATORY SYSTEM Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms History of Present Illness Onset Location Duration Characteristic symptoms Associated manifestations Relieving/exacerbating factors Treatment Past History Have you had any prior respiratory problems? Have you had thoracic surgery, biopsy, or trauma to your chest? Do you have any allergies that affect your breathing or respiratory system? Have you had tuberculosis skin testing (purif ed protein derivative [PPD]) or a chest x-ray? When? What were the results? Have you had any other pulmonary testing? When? What were the results? Have you had an inf uenza immunization? When? Have you had the Tdap version of the tetanus immunization? If the client is over 65 years of age, inquire whether he or she had pneumococcal or varicella zoster immunizations. Have you traveled outside the United States within the past 6 months? If yes, where? Have you been in contact with anyone with severe acute respiratory syndrome (SARS) or suspected of having SARS? Health Maintenance Immunizations Screening tests Safety measures Family History Does anyone in your family currently have a respiratory infection or disease? Has anyone had lung cancer, asthma, or cystic f brosis? Did anyone smoke in your home when you were growing up? Lifestyle and Personal Habits Do you smoke or have you ever smoked tobacco or marijuana? How many cigarettes or packs per day do you smoke? When did you start? How long have you smoked/did you smoke? Do you use or have you ever used snuff? Do you chew or have you ever chewed tobacco? Are you exposed to second-hand smoke? How many hours per day? For how many years? Are you exposed to any environmental conditions at home or work that affect your breathing (e.g., mold, sawdust, asbestos, coal dust, insecticides, radon, paint, or pollution)? 62 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Are you taking any prescription, herbal, or over-the-counter (OTC) medications for breathing or respiratory problems? Do you use oxygen or other treatments for breathing problems (e.g., nebulizer treatments)? Physical Examination Overview Initial survey of respiration and the thorax Examination of the posterior chest Deformities or asymmetry Abnormal retraction of the intercostal spaces during inspiration Impaired respiratory movement on one or both sides or a unilateral lag (or delay) in movement Palpation Identify tender areas. Assess any observed abnormalities. T est chest expansion. Feel for tactile fremitus. Palpate and compare symmetric areas. Percussion Auscultation Breath sounds Adventitious sounds T ransmitted voice sounds Examination of the anterior chest Inspection Deformities or asymmetry W ork of breathing Local lag or impairment in respiratory Movement Palpation Identify tender areas. Assess any observed abnormalities. T est chest expansion. Feel for tactile fremitus. Palpate and compare symmetric areas. Percussion Auscultation Breath sounds Adventitious sounds T ransmitted voice sounds Health Promotion and Counseling Tobacco cessation Immunizations (adults) 63 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Describe the structure and functions of the heart and great vessels. 2. Identify the landmarks and key auscultation sites of the precordium. 3. Describe the electrical conduction system of the heart. 4. Explain the normal electrocardiogram waveform pattern. 5. Describe the two phases of the mechanical heart cycle. 6. Describe the normal heart sounds and their origin. 7. Describe extra heart sounds and their origin. 8. Obtain an accurate history of the cardiovascular system. 9. Appropriately prepare and position the client for the cardiovascular examination. 10. Describe the equipment necessary to perform a cardiovascular examination. 11. Inspect, palpate, and auscultate the jugular veins and carotid arteries of the neck. 12. Inspect, palpate, and auscultate the precordium to evaluate cardiovascular status. 13. Discuss risk factors for coronary heart disease. 14. Discuss risk reduction and health promotion strategies to reduce coronary heart disease. The Cardiovascular System SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The area of the exterior chest that the heart and great vessels is called the . B. To reduce the risk for , counsel patients to pursue exercise, or exercise that increases uptake, for at least minutes on most days of the week. C. of heart sounds and murmurs is an important skill of physical examination that leads directly to several clinical diagnoses. D. If an impulse or heave is , assess its , , and . E. To assess duration, listen to the impulse as you feel the , or watch the movement of your stethoscope as you at the . F. Carefully the anterior chest for the of the apical impulse or of or heaves over the precordium, which indicate increased movement. C H A P T E R 14 64 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. G. Note the anatomic location of sounds in terms of and their distance from the or lines. H. The provides valuable information about the patient’s status and function. 2. List the lifestyle modif cations to prevent cardiovascular disease and stroke. A. B. C. D. E. F. G. H. 3. List the f ve broad components that make up a complete cardiovascular examination. A. B. C. D. E. Activity B MATCHING 4. Match the heart rhythm with its usual resting rate. Answer Heart Rhythm Usual Resting Rate Ventricular tachycardia A. <60 Second-degree AV block B. 100–175 Complete heart block C. 100–180 Atrial f utter with a regular ventricular response D. 60–100 Sinus tachycardia E. <40 Sinus bradycardia F. 150–250 Normal sinus rhythm G. 110–250 Supraventricular (atrial or nodal) tachycardia H. 60–90 5. Match the description with the correct gradation of murmur. Answer Gradation of Murmur Description Grade 1 A. Loud, with palpable thrill Grade 2 B. Very loud, with thrill; may be heard when the stethoscope is partly off the chest Grade 3 C. Very loud, with thrill; may be heard with stethoscope entirely off the chest Grade 4 D. Quiet, but heard immediately after placing the stethoscope on the chest Grade 5 E. Very faint; heard only after listener has “tuned in” Grade 6 F. Moderately loud CHAPTER 14 THE CARDIOVASCULAR SYSTEM 65 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Put the steps of the cardiac examination in the correct sequence. A. Listen at the 2nd right and left intercostal spaces. B. Listen at the right sternal border. C. Inspect and palpate the precordium. D. Palpate the apical impulse. Activity C SHORT ANSWER 7. Describe the basic sequence of the cardiac examination with reference to the cardinal assessment techniques. 8. Explain the circulation of blood through the heart beginning with the vena cavae and ending with the aorta. 9. Describe the characteristics of the different layers of the heart wall. 10. Describe the path of the cardiac electrical impulse. Activity D NCLEX STYLE QUESTIONS 11. What is located at the right and left 2nd intercostal spaces next to the sternum? a. Base of the heart b. Apex of the heart c. Pulmonary vein d. Aortic valve 12. When a patient is obese or has a thick chest wall, what is diff cult to palpate? a. JVP b. Apical impulse c. Grade 4 murmur d. Sternal angle 13. What is the normal peak pressure of the left ventricle? a. 90 mm Hg b. 100 mm Hg c. 110 mm Hg d. 120 mm Hg 14. A 78-year-old male Hispanic patient is noted to have a pathologic change in ventricular compliance. What information from the cardiac assessment would indicate this? a. A split S2 b. An S3 gallop c. A delayed S3 d. A weak S4 15. What are the components of S1? (Mark all that apply.) a. An earlier aortic sound b. An earlier mitral sound c. A later pulmonic sound d. A later tricuspid sound e. An earlier tricuspid sound 16. Your patient asks you what the small P wave on her ECG indicates. What would you answer? a. Atrial depolarization b. Ventricular depolarization c. Atrial repolarization d. Ventricular repolarization 17. What term is used to describe the degree of vascular resistance to ventricular contraction? a. Contractile overload b. Volume overload c. Preload d. Afterload 66 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 18. When, in the cardiac cycle, does blood pressure peak? a. Preload b. Systole c. Diastole d. Afterload 19. Over a 24-hour period there is a striking variation in blood pressure levels. What can cause these variations? (Mark all that apply.) a. Time of day b. Sugar ingestion c. Size of meals d. Noise e. Environmental temperature 20. What do the oscillations in the internal jugular veins ref ect? a. Changing pressures within the right atrium b. Changing pressures within the left atrium c. Changing pressures within the right ventricle d. Changing pressures within the left ventricle SECTION III: CASE STUDY Activity E Sam Simmons, age 57, is an African American man who works for the post off ce. He is 6′ tall and weighs 182 pounds. Vital signs are T 37°C; HR 95; BP 138/88; pain level 0. He presents at the clinic with a chief complaint of “just not feeling well.” a. How would you assess Mr. Simmons for hypertensive risks? On auscultation you hear a heart murmur. b. How would you identify Mr. Simmons’ heart murmur? CHAPTER 14 THE CARDIOVASCULAR SYSTEM 67 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE THE CARDIOVASCULAR SYSTEM Name Date/Time Overview. Identifying Data Common or Concerning Symptoms Chest pain Pain or discomfort radiating to the neck, left shoulder or arm, and back Nausea Diaphoresis Arrhythmias: skipped beats, palpitations Dyspnea Orthopnea or paroxysmal nocturnal dyspnea Cough Edema Nocturia Fatigue Cyanosis or pallor Cardiac History Do you have any past history of heart problems or heart disease? Do you have a history of: Heart murmur? Congenital heart disease? Rheumatic fever? Hypertension? Elevated cholesterol or triglycerides? Peripheral arterial disease? Cerebral arterial disease? Diabetes? When were your last ECG, cholesterol measurement, and other heart tests? What were the results? Family History Is there any family history of coronary artery disease, hypertension, sudden death at younger than 60 years of age, stroke, diabetes, or obesity? Lifestyle Habits Nutrition Smoking Alcohol Exercise: Describe your daily or weekly exercise: type and amount Medications/drugs Physical Examination Blood pressure and heart rate Face Great vessels of the neck Inspection and palpation of the precordium Auscultation of normal and extra heart sounds Peripheral edema 68 C H A P T E R 15 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the locations of the peripheral pulses. 2. Obtain an accurate history of the peripheral vascular system. 3. Describe the structure and functions of arteries, veins, and lymph vessels and nodes. 4. Appropriately prepare and position the client for the peripheral vascular examination. 5. Describe the equipment necessary to perform a peripheral vascular examination. 6. Evaluate and interpret variations in pulse rhythm, rate, and amplitude. 7. Discuss risk factors for peripheral artery disease, chronic venous stasis, and thromboembolic disease. 8. Discuss risk reduction and health promotion strategies to reduce peripheral vascular disease. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Chronic venous is caused by incompetent secondary to The Peripheral Vascular System and Lymphatic System deep vein thrombosis or prolonged increased venous pressure as seen in prolonged or . B. An is a fatty in the walls of arteries. C. and early of DVT are critical nursing tasks, especially in the care of hospitalized patients and patients with reduced . D. Capillaries have an endothelial cell lining but no , facilitating rapid of and . E. The aorta and its immediate branches are or highly arteries, such as the , common , and arteries. F. Dislodgement of a produces an that can travel to the , causing and . CHAPTER 15 THE PERIPHERAL VASCULAR SYSTEM AND LYMPHATIC SYSTEM 69 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 2. List the important topics for health promotion and counseling for arterial disease. A. B. C. D. E. F. G. H. 3. List the most common or concerning symptoms regarding the peripheral vascular system. A. B. C. D. E. Activity B MATCHING 4. Match the type of peripheral vascular disorder with the location of the pain it causes. Answer Peripheral Vascular Disorder Location of Pain Acute arterial occlusion A. Diffuse aching of the leg(s) Intermittent claudication B. Tight, bursting pain, if present, usually in the calf; may be painless Compartment syndrome C. An arm or a leg Chronic venous insuff ciency (deep) D. Pain in the arch of the foot Atherosclerosis—rest pain E. Pain in a local area along the course of a superf cial vein Raynaud disease and phe nomenon F. Distal pain, usually involving the foot and leg Superf cial thrombophlebitis G. Distal pain, in the toes or forefoot Deep venous thrombosis (DVT) H. Usually calf muscles Thromboangiitis obliterans (Buerger disease) I. Distal portions of one or more f ngers Acute lymphangitis J. Tight, bursting pain in calf muscles, usually in the anterior tibial com partment 5. Match the score of the ankle–brachial Index with the interpretation of the score (with a range of 0.90 to 1.30). Answer Interpretation of Score Score Normal lower extremity blood f ow A. <0.39 Mild PAD B. <0.59 to >0.40 Moderate PAD C. >0.90 Severe PAD D. <0.89 to >0.60 70 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the type of ulcer to its corresponding characteristic. Answer Ulcer Type Characteristic Chronic venous insuff ciency ulcer A. Develops in pressure points of areas with dimin ished sensation Arterial insuff ciency ulcer B. Usually appears over the medial and sometimes the lateral malleolus Neuropathic ulcer C. Occurs in the toes, feet, or possibly areas of trauma c. Amputation d. Diabetes mellitus 13. The nurse is testing the valvular competency of the saphenous system. What test is the nurse performing on the patient? a. Trendelenburg test b. Ankle–brachial index test c. Allen test d. Venous occlusion test 14. You are studying the peripheral vascular system so you would know that the vasa vasorum is found where? a. Inferior vena cava b. Superior vena cava c. Venous intima d. Adventitia of the artery 15. The nursing instructor is discussing the great and small saphenous veins. What would the instructor say connects these two veins? a. Bridging veins b. Communicating veins c. Anastomotic veins d. High-pressure veins 16. Your patient has a difference between the highest and lowest systolic pressure of 12 mm Hg. What does this indicate? (Mark all that apply.) a. Obstructive airway disease b. Pericardial tamponade c. Possible constrictive pericarditis d. Peripheral arterial disease e. Complex atheroma 17. What is a function of the lymph system? a. Produce antibodies b. Clean the blood c. Drain lymph f uid from the vascular bed d. Transport nutrients to the tissues Activity C SHORT ANSWER 7. Explain how to perform an assessment of a patient’s ankle–brachial index. 8. List the different types of edema and the characteristics and causes of each. 9. Describe the clinical characteristics of chronic arterial insuff ciency. 10. Describe the clinical characteristics of chronic venous insuff ciency. Activity D NCLEX STYLE QUESTIONS 11. What is the Virchow triad? (Mark all that apply.) a. Arterial stasis b. Hypercoagulability c. Vessel wall damage d. High fat content in blood e. Venous stasis 12. What is a long-term complication of peripheral vascular disease? a. Metabolic changes b. Thickened skin CHAPTER 15 THE PERIPHERAL VASCULAR SYSTEM AND LYMPHATIC SYSTEM 71 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 18. You are preparing a class presentation on edema. What mechanisms would you cite as producing edema? (Mark all that apply.) a. Arterial insuff ciency b. Low plasma protein levels c. Capillary leak syndrome d. Increased capillary blood pressure e. Hyperglycemia 19. The nurse is assessing a patient with Raynaud disease. When assessing the wrist pulses, what would the nurse expect to f nd? a. Normal wrist pulses b. Decreased wrist pulses c. Bounding wrist pulses d. Absent wrist pulses 20. While assessing the legs of your patient you note that the legs and feet are cool to the touch. What would you know is most often the cause of bilateral coolness? a. Inadequate arterial circulation b. Embolism c. Anxiety d. DVT SECTION III: CASE STUDY Activity E Mitchell Olson, a 75-year-old white man, is admitted to the unit you are working on. He has a documented history of peripheral vascular disease. While you are conducting Mr. Olson’s admission assessment he states, “I can’t walk but a couple of blocks without getting pain in my legs.” a. What signs, symptoms, or additional problems would you assess this patient for? b. You decide to assess the arterial supply to Mr. Olson’s legs. How would you perform this assessment? SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE THE PERIPHERAL VASCULAR SYSTEM AND LYMPHATIC SYSTEM Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Onset Location Duration Characteristic symptoms Associated manifestations Relieving/exacerbating factors Treatment Current Health Status Medications, especially oral contraceptives or hormone replacement therapy Pregnancy or recent childbirth Inf ammatory diseases such as lupus, rheumatoid arthritis, or irritable bowel disease Active cancer 72 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Risk factors Obesity Smoking Hyperlipidemia Constrictive clothing Central venous lines Past History Coronary artery disease (CAD) Heart attack Congestive heart failure Stroke (cerebral arterial disease) Clotting disorders Hypertension Diabetes Problems in circulation, such as blood clots, leg ulcers, swelling, or poor healing of wounds Major surgery or fracture of a long bone in the past 4 weeks Family History Peripheral vascular disease Varicose veins Abdominal aortic aneurysm CAD Sudden death younger than 60 years of age Diabetes Lifestyle or Health Patterns Job requiring prolonged standing or sitting Sedentary lifestyle Decreased mobility such as paralysis or cast Physical Examination Important Areas of Examination Arms Inspection Palpation Legs Health Promotion and Counseling Arterial disease Smoking cessation W eight control Exer cise program Hypertension control Hyperlipidemia control Diabetes management Limiting alcohol intake Foot care Venous disease Avoidance of prolonged sitting and standing Avoidance of constrictive clothing, including girdles and tight hose Exer cise program W eight control Foot care Dehydration prevention 73 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the landmarks of the abdominal wall and pelvis. 2. Identify the four quadrants and the organs in each quadrant. 3. Perform an accurate health history of the gastrointestinal and renal systems. 4. Describe the physical examination techniques and the order performed to evaluate the gastrointestinal and renal systems. 5. Determine the health promotion and counseling measures related to alcohol abuse, hepatitis, colorectal cancer, and urinary incontinence. 6. Perform and document a complete gastrointestinal and renal system assessment utilizing information from the health history and the physical examination. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Dyspepsia is def ned as or discomfort or pain centered in the . The Gastrointestinal and Renal Systems B. Some acute pain, especially in the suprapubic area or from the f ank, originates in the . C. Brownish or blackish with a “ ” appearance suggests altered by acid. D. Patients may complain of fullness after light or moderate meals, or early , the inability to eat a full meal. E. pain is felt in the perineum and occasionally in the rectum. F. refers to a increase in 24-hour urine volume, roughly def ned as exceeding . G. pain, fever, and occur in pyelonephritis. H. A protuberant abdomen with suggests the possibility of . 2. List the screening guidelines for colorectal cancer for people at average risk. A. B. C. D. E. C H A P T E R 16 74 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the risk factors for abdominal aortic aneurysm. A. B. C. D. Activity B MATCHING 4. Match the information with the correct variety of hepatitis (varieties of hepatitis may have multiple information data). Answer Information Variety of Hepatitis 95% of infections in healthy adults are self limited A. Hepatitis A Transmitted by repeated percutaneous exposure to blood B. Hepatitis B Persons with chronic liver disease C. Hepatitis C Sexual contacts Transmission is fecal–oral People with percutaneous (through the skin) or mucosal exposure to blood Transfusion with clotting factors before 1987 Undiagnosed liver disease Contamination of water and foods Immune serum globulin can be administered before and within 2 weeks of contact 5. Match the description with the type of incontinence it is describing. Answer Description Type of Incontinence Detrusor contractions are insuff cient to over come urethral resistance. A. Stress incontinence An inability to get to the toilet in time B. Urge incontinence Detrusor contractions are stronger than normal and overcome the normal urethral resistance. C. Overf ow inconti nence May contribute to any type of incontinence D. Functional incontinence The urethral sphincter is weakened so that tran sient increases in intra-abdominal pressure raise the bladder pressure to levels that exceed ure thral resistance. E. Incontinence secondary to medications CHAPTER 16 THE GASTROINTESTINAL AND RENAL SYSTEMS 75 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the cause of a protuberant abdomen to its corresponding characteristic. Answer Cause of Protuberant Abdomen Characteristic Fat A. Air-f lled bowel is displaced to the periphery Gas B. Bulging f anks that are dull to percussion Tumor C. Causes a tympanitic percussion note Pregnancy D. Most common cause of a protuberant abdomen Ascitic f uid E. Common cause of a pelvic “mass” 12. Which type of incontinence occurs when excessive bladder volume exceeds urethral pressure? a. Urge incontinence b. Functional incontinence c. Stress incontinence d. Overf ow incontinence 13. You are admitting a patient who is in hypertensive crisis. The doctor’s notes indicate that bruits that are both systolic and diastolic have been noted and renal artery stenosis is suspected as the cause of the hypertension. Where would you auscultate the patient’s abdomen to hear these bruits? (Mark all that apply.) a. Right upper quadrant b. Femoral arteries c. Iliac arteries d. Epigastrium e. Costovertebral angles 14. A 55-year-old African American man presents at the clinic with a chief complaint of “indigestion.” The patient tells the nurse, “It usually happens after I do things like mowing the lawn or doing other yard work.” What should the nurse suspect? a. Angina b. Ulcer disease c. Aortic aneurysm d. Gallbladder disease Activity C SHORT ANSWER 7. Describe the potential causes of a localized bulge in the patient’s abdominal wall. 8. Explain the process for palpating the abdomen, including which organs can be felt and where they can be felt. 9. Explain the types, patterns, and mechanisms of visceral pain. 10. Describe the different types of jaundice and the etiology of each. Activity D NCLEX STYLE QUESTIONS 11. Your patient has a bladder disorder. Where would you expect the pain to be? a. Upper abdomen b. Suprapubic c. Back d. Perineal 76 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 15. Mrs. Wells presents at the clinic with a chief complaint of pain in her upper abdomen. On assessment the nurse notes that Mrs. Wells has recurrent pain, more than two times weekly, in her upper abdomen, and that this recurrent pain started 2 months ago. What term should the nurse use for this type of pain? a. Discomfort b. Dysphagia c. Dyspepsia d. Odynophagia 16. What can cause bladder distention? (Mark all that apply.) a. Medications b. Stroke c. Multiple sclerosis d. Perineal f ssure e. Rectal abscess 17. You are assessing a patient for acute cholecystitis. What sign would you assess for? a. Psoas sign b. Obstipation sign c. Murphy sign d. Cutaneous hyperesthesia 18. Your patient has epigastric pain that is poorly localized and radiates to the back. What would be an important diagnosis to assess for? a. Acute pancreatitis b. Biliary colic c. Acute cholecystitis d. Acute diverticulitis 19. When assessing for an appendicitis, what signs might you look for? (Mark all that apply.) a. Murphy sign b. Psoas sign c. Obfuscator sign d. Rovsing sign e. Cutaneous hyperesthesia 20. Your patient describes her stool as soft, light yellow to gray, mushy, greasy, foul-smelling, and usually f oats in the toilet. What would you suspect is wrong with your patient? a. Malabsorption syndrome b. Lactose intolerance c. Crohn disease d. Ulcerative colitis SECTION III: CASE STUDY Activity E Tiffany Christus, 25 years old, presents at the emergency department with complaints of nausea, vomiting, and acute abdominal pain of rapid onset. a. Using the comprehensive health history and the focused GI assessment as frameworks, outline an appropriate assessment of this patient. b. Describe specif c assessments you would make to conf rm or rule out acute appendicitis. CHAPTER 16 THE GASTROINTESTINAL AND RENAL SYSTEMS 77 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE COMPREHENSIVE ADULT HEALTH HISTORY Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Gastrointestinal Abdominal pain, acute and chronic Indigestion, nausea, vomiting including blood, loss of appetite, early satiety Dysphagia and/or odynophagia Change in bowel function Diarrhea, constipation Jaundice Urinary and Renal Suprapubic pain Dysuria, urgency, or frequency Hesitancy, decreased stream in males Polyuria or nocturia Urinar y incontinence Hematuria Kidney or f ank pain Ureteral colic Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment Past History Allergies Medications Childhood illnesses Adult illnesses Medical Surgical Psychiatric Risk Factors Tobacco Alcohol/drugs Family History Gastrointestinal disease Urinary tract disease Review of Systems General Inspection Skin Scars 78 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Striae Dilated veins Rashes and lesions Contour of the abdomen Peristalsis Pulsations Auscultation Bowel sounds Abdominal bruits and friction rub Percussion Palpation Liver Spleen Kidneys Bladder Aorta Health Promotion Screening for alcohol abuse Risk factors for hepatitis A, B, and C Screening for colon cancer 79 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the structures and function of the breasts and axillae. 2. Perform an accurate health history of the breasts and axillae. 3. Describe the physical examination techniques performed to evaluate the breasts and axillae. 4. Demonstrate how to perform a clinical breast examination. 5. Document a complete breast and axilla assessment utilizing information from the health history and the physical examination. 6. Determine the measures for prevention or early detection of breast cancer. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. The breast is sensitive , responsive to the changes of cycles and . B. Lacking and stimulation, ductal branching and development of lobules are . C. All women should be __________ with the and of their breasts to any changes. The Breasts and Axillae D. Long-standing is usually a normal of no clinical consequence, except for possible when . E. Dimpling or retraction of the breasts may be associated with such as or . F. is best performed when the breast tissue is f attened. G. Although the may be examined with the patient , a position is preferable. H. Clear, serous, green, black, or nonbloody discharges that are usually require only . I. Masses, nodularity, and change in color or inf ammation, especially in the , suggest of . J. breast density has been identif ed as “the most and risk factor” in studies of breast cancer. 2. List the risk factors for breast cancer. A. B. C. D. E. F. G. H. C H A P T E R 17 80 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the common types of breast masses. A. B. C. D. Activity B MATCHING 4. Match the descriptive information with the correct type of breast lump (type of breast lump will have multiple information data). Answer Information Type of Breast Lump Usually single, although may coexist with other nodules A. Fibroadenoma 30–50, regress after menopause except with estrogen therapy B. Cysts Well delineated C. Cancer 30–90, most common over age 50 Very mobile 15–25, usually puberty and young adulthood, but up to age 55 Often tender Round, disc-like, or lobular Firm or hard 5. Match the description with the lymph nodes it is describing. Answer Description Nodes Drain the posterior chest wall and a portion of the arm A. Pectoral nodes Drain most of the arm B. Subscapular nodes Drain the anterior chest wall and much of the breast C. Central nodes Palpable most frequently D. Lateral nodes CHAPTER 17 THE BREASTS AND AXILLAE 81 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the visible sign of breast cancer to its corresponding description. Answer Visible Sign Description Skin dimpling A. Flattened or pulled inward Abnormal contours B. Produced by lymphatic Nipple retraction C. Usually starts as a scaly, eczema-like lesion that may weep, crust, or erode; breast mass may be present Peau d’orange (orange peel) sign D. Look for this sign with the patient’s arm at rest, during special positioning, and on moving or compressing the breast Edema of the skin E. Any variation in the normal convexity of each breast Paget disease F. Appears as thickened skin with enlarged pores 12. The nursing instructor explains to the students that malignant cells from a breast cancer may spread directly to what nodes? a. Medial nodes b. Lateral nodes c. Supraclavicular nodes d. Infraclavicular nodes 13. When examining a breast, what would you consider a common or concerning symptom? (Mark all that apply.) a. Rash b. Unusual nipple discharge c. Breast discomfort d. Change in shape e. Edema 14. What is an accurate description of scaling? a. Small indents of the breast tissue b. Thin f akes of keratinized epithelium c. Red, rough patch of skin d. Silvery patches of itchy skin 15. When is the best time for examination of the breast? a. 3 to 5 days after the onset of menstruation b. 3 to 5 days before the onset of menstruation c. 5 to 7 days after the onset of menstruation d. 5 to 7 days before the onset of menstruation Activity C SHORT ANSWER 7. Discuss the challenges of communicating risks and benef ts about breast cancer screening and potential approaches to these communication challenges. 8. Explain the process for breast self-examination. 9. Describe the anatomy and physiology of the male breast. 10. Describe the anatomy of the female breast. Activity D NCLEX STYLE QUESTIONS 11. The nursing student is learning to palpate the axillary nodes during a breast examination. Which nodes is he or she most likely to palpate? a. Central nodes b. Pectoral nodes c. Subscapular nodes d. Lateral nodes 82 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 16. Your patient is noted to have thickening of the skin and unusually prominent pores on her right breast. What might you suspect? a. Lymphatic obstruction b. Inf ammation c. Cyst d. Fibrocystic disease 17. You instruct your patient to lean forward so you can inspect the breasts. What might this position reveal that is not visible in another position? a. Retraction of the nipple and areola b. Posttraumatic fat necrosis c. Asymmetry of the breast or nipple d. Mammary duct ectasia 18. What pattern of palpation is currently the best validated technique for detecting breast masses? a. Circular pattern b. Vertical strip pattern c. Wedge pattern d. Supra to infra pattern 19. When palpating a breast, what must you examine the breast tissue carefully for? (Mark all that apply.) a. Dimples b. Nodules c. Tenderness d. Consistency e. Rash 20. You palpate a mobile mass that becomes f xed when your patient’s arm relaxes. What would this tell you about the mass? a. It is attached to the ribs and intercostal muscles b. It is attached to the pectoral fascia. c. It is attached to the scapular fascia. d. It is attached to the pectoral and scapular muscles. SECTION III: CASE STUDY Activity E Letitia Gibbson, a 65-year-old African American woman, has come to the clinic for her annual check-up. She is 3 years post–right mastectomy for a cancerous tumor in the tail of Spence. a. How would Mrs. Gibbson’s breast exam differ from the breast exam of someone who had never had breast cancer? b. When teaching Mrs. Gibbson about breast self-examination, what would you teach her about standing for part of the exam? CHAPTER 17 THE BREASTS AND AXILLAE 83 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE THE BREASTS AND AXILLAE HEALTH HISTORY Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Breast lump or mass Breast pain or discomfort Change in shape Nipple discharge Edema Dimpling Rash Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Pregnancies Menstrual history Previous history of breast cancer and/or reproductive cancer Previous breast biopsy Breast self-examination (BSE) Clinical breast examination (CBE) Mammogram or MRI Family History Breast cancer Genetic testing Reproductive cancer BRCA testing Lifestyle Habits Alcohol Physical activity Physical Examination THE FEMALE BREAST Inspection Arms at sides Arms over head Hands pressed against hips Leaning forward 84 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Palpation Right breast THE AXILLAE Inspection Palpation Assessment of Spontaneous Nipple Discharge Examination of the Mastectomy or Breast Augmentation Patient Breast Awareness and Self-Examination Instructions Health Promotion and Counseling Palpable masses of the breast Assessing risk of breast cancer Breast cancer screening Right nipple Left breast Left nipple THE MALE BREAST Inspection Nipple and areola Palpation Nipple and areola 85 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Describe the structure and functions of the bones, muscles, and joints. 2. Identify the key landmarks of each joint. 3. Obtain an accurate history of the musculoskeletal system. 4. Appropriately prepare and position the client for the musculoskeletal examination. 5. Describe the equipment necessary to perform a musculoskeletal examination. 6. Inspect and palpate the joints, bones, and muscles. 7. Describe the range of motion of the major joints. 8. Assess muscle strength using the muscle strength grading scale. 9. Correctly document the f ndings of the musculoskeletal assessment. 10. Discuss risk factors for osteoporosis. 11. Discuss risk factors for falls. 12. Discuss risk reduction and health promotion strategies to reduce musculoskeletal injuries and disease. The Musculoskeletal System SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Articular disease typically involves and of the entire joint and limits both and range of motion. B. Many of the joints examined are , or movable, joints. C. Generalized “ ” are called if they occur in muscles, and if there is pain in a but no evidence of arthritis. D. is the second most common reason for off ce visits. E. Regular exercise that includes - and can increase bone and muscle but has not yet been shown to reduce risk. F. For the older person, increased intake reduces age-related and increases of newly formed bone. C H A P T E R 18 86 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. G. A percent drop in bone , equivalent to 1.0 , is associated with a percent increase in risk for . H. percent of patients with hip fractures within 1 year. I. Each has its own specif c vulnerabilities to and . J. Observe the gait for the of the , the of the , and of the . 2. List the risk factors for falls. A. B. C. D. E. F. G. H. I. J. K. L. 3. List the types of movement of the hip. A. B. C. D. Activity B MATCHING 4. Match the test with what is being tested. Answer Test What Is Being Tested Flex the patient’s forearm to 90° at the elbow and pronate the patient’s wrist. Pro vide resistance when the patient supinates the forearm. A. Infraspinatus strength Ask the patient to place arms at the side and f ex the elbows to 90° with the thumbs turned up. Provide resistance as the patient presses the forearms outward. B. Supraspinatus strength Adduct the patient’s arm across the chest. C. “Drop-arm” sign Elevate the arms to 90° and internally rotate the arms with the thumbs pointing down, as if emptying a can. Ask the patient to resist as you place downward pressure on the arms. D. “Crossover test” Ask the patient to fully abduct the arm to shoulder level (or up to 90°) and lower it slowly. E. Forearm supination CHAPTER 18 THE MUSCULOSKELETAL SYSTEM 87 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 5. Match the description with the foot abnormality it is describing. Answer Abnormality Description Neuropathic ulcer A. A painful conical thickening of skin that results from recur rent pressure on normally thin skin Callus B. Symptoms include hyperesthesia, numbness, aching, and burning from the metatarsal heads into the 3rd and 4th toes. Plantar wart C. Characterized by hyperextension at the metatarsophalangeal joint with f exion at the proximal interphalangeal joint Corn D. The head of the f rst metatarsal may enlarge on its medial side, and a bursa may form at the pressure point. Hammer toe E. May develop at pressure points on the feet Hallux valgus F. An area of greatly thickened skin that develops in a region of recurrent pressure Morton neuroma G. It may look like a callus or even be covered by one. 6. Match the musculoskeletal entity to its corresponding description. Answer Musculoskeletal Entity Description Ankle A. Include the anterior tibial muscle and the toe extensors Transverse tarsal joint B. A hinge joint formed by the tibia, the f bula, and the talus Tibiotalar joint C. Fans out from the inferior surface of the medial malleo lus to the talus and proximal tarsal bones Deltoid ligament D. Powered by the gastrocnemius, the posterior tibial mus cle, and the toe f exors Knee joint E. Stabilizes the heel and inverts and everts the forefoot Plantar f exion F. Dorsif ex and plantar f ex the foot at the ankle Dorsif exors G. The largest joint in the body 9. Discuss what is involved in assessing muscle bulk. 10. Describe some of the assessment techniques that facilitate an accurate and eff cient musculoskeletal assessment. Activity C SHORT ANSWER 7. Discuss the risk factors for osteoporosis. 8. Explain what basic elements of musculoskeletal health are assessed during the general survey. 88 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity D NCLEX STYLE QUESTIONS 11. You are testing your patient for extension of the wrist and note weakness on the right side. This assessment f nding is consistent with what disease of the nervous system? a. Fibromyalgia b. Multiple sclerosis c. Gillian-Barré d. Lyme disease 12. How would you document normal muscle strength? a. 1:1 b. 2 & 2 c. 4+ d. 5/5 13. When examining a patient’s musculoskeletal system, you f nd acute involvement of only one joint. What would this suggest to you? (Mark all that apply.) a. Gout b. Duchenne muscular dystrophy c. Septic arthritis d. Trauma e. Rheumatoid arthritis 14. What is increased muscle tone in both directions that is not rate dependent? a. Rigidity b. Spasticity c. Atrophy d. Atony 15. What are the principal muscles used in opening the mouth? a. Temporalis b. Masseter c. External pterygoids d. Internal pterygoids 16. You are the school nurse in the local high school. You note that a 15-year-old girl carries her left shoulder higher than her right shoulder. You should recognize the likely presence of what health problem? a. Torn rotator cuff b. Dislocated shoulder c. Broken clavicle d. Scoliosis 17. The pitcher of the high school baseball team, 16 years old, is brought to the clinic by his mother with a complaint of pain in his right elbow. Where would you expect to locate his tenderness? a. Distal to the right lateral epicondyle b. Distal to the right medial epicondyle c. Over the right olecranon process d. Proximal to the right olecranon bursa 18. Birthmarks, port-wine stains, hairy patches, and lipomas often overlie what? a. Bony defects b. Muscular defects c. Missing bursa d. Malformed ligaments 19. A patient presents at the clinic with a history of cerebral palsy. When examining the patient you note increased resistance that is rate dependent and increases with rapid movement. What would you chart about this patient? a. Patient has rigidity b. Patient demonstrates spasticity c. Patient has muscular atrophy d. Patient demonstrates muscular atony 20. You note that your patient has decreased muscle tone. You know that this can be caused by what? (Mark all that apply.) a. Brain stem injury b. Cerebral disease c. Acute stages of spinal cord injury d. Cerebellar disease e. Disease of the peripheral nervous system SECTION III: CASE STUDY Activity E Ryne Nordstrom, 16 years old, is injured during a high school basketball game. He is brought to the emergency department by ambulance with a long leg air splint on his left leg. EMTs report that vital signs are HR 130; BP 128/82; RR 21; T 38°C; and pain 10/10. CHAPTER 18 THE MUSCULOSKELETAL SYSTEM 89 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. HEALTH HISTORY OF THE MUSCULOSKELETAL SYSTEM Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Joint pain Joint pain associated with systemic symptoms, such as fever, chills, rash, weakness, and weight loss Low back pain Neck pain Bone pain Muscle pain or cramps Muscle weakness Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Muscle or bone disease (present) Muscle or bone disease (past) Family History Muscle or bone disease Diabetes Genetic testing Lifestyle Habits Alcohol Physical activity Physical Examination Overview Muscle bulk Muscle tone Muscle strength TEMPOROMANDIBULAR JOINT Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma a. What musculoskeletal assessments would be made on this patient? b. What diagnostic tests could be used in the assessment of this patient? SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE 90 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE SHOULDER Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE ELBOW Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE WRIST AND HANDS Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE SPINE Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE HIP Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE KNEE Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength THE ANKLE AND FOOT Inspection for joint symmetry, alignment, bony deformities Inspection and palpation of surrounding tissues for skin changes, nodules, muscle atrophy, crepitus Range of motion and maneuvers to test joint function and stability, and integrity of ligaments, tendons, bursae, especially if pain or trauma Assessment of inf ammation or arthritis, especially swelling, warmth, tenderness, redness Assessment of muscle strength Health Promotion Topics Nutrition, exercise, and weight Low back: lifting and biomechanics Falls: prevention Osteoporosis: screening and prevention 91 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Describe the multiple areas assessed in the mental status examination. 2. Determine the symptoms and behaviors for mental health screening. 3. Obtain an accurate mental status history for a patient. 4. Perform a mini-mental status examination. 5. Identify the screening and health promotion and counseling tools for depression, suicide, and dementia. 6. Correctly document the f ndings of the mental status assessment. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Despite the prevalence of , detection is diff cult and and rates are low. B. Alcohol, tobacco, and illicit drugs account for more , , and than any other condition. C. The U.S. Preventive Services Task Force recommends in clinical settings that can provide accurate , , and . Mental Status D. The burden of that mental disorders impose is . E. and , when observed clinically, provide a rough of a person’s . F. Note whether and are based on reality or, for example, on , fulf llment, or disordered content. G. Inquire about perceptions in a manner similar to that used for content. H. Watch for in expression with under . I. nurses may feel to perform mental status examinations, wondering if it will patients or invade . J. Two thirds of patients with present with complaints, and half report unexplained or symptoms. 2. List the f ve broad components of a mental status examination. A. B. C. D. E. C H A P T E R 19 92 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the patient identif ers for selective mental health screening. A. B. C. D. Activity B MATCHING 4. Match the term to its corresponding description. Answer Term Description Level of consciousness A. Awareness of personal identity, place, and time Attention B. What the patient thinks about Memory C. Awareness that symptoms or disturbed behaviors are normal or abnormal Orientation D. The ability to focus or concentrate over time on one task or activity Perceptions E. Alertness or state of awareness of the environment Thought processes F. Assessed by vocabulary, fund of information, abstract thinking, calcu lations, and construction of objects that have two or three dimensions Thought content G. The process of registering or recording information Insight H. A more sustained emotion that may color a person’s view of the world Judgment I. A complex symbolic system for expressing, receiving, and compre hending words Affect J. The logic and coherence of the patient’s thoughts Mood K. An observable, usually episodic, feeling or tone expressed through voice, facial expression, and demeanor Language L. Process of comparing and evaluating alternatives when deciding on a course of action Higher cognitive functions M. Sensory awareness of objects in the environment and their inter relationships E. F. G. H. I. J. 6. Explain the relationship between health and human behavior and describe some of the clinical implications of this relationship. 7. Discuss some of the characteristics and implications of unexplained symptoms. Activity C SHORT ANSWER 5. Explain some of the clinical guidelines for distinguishing between physical, psychological, unexplained, and somatoform symptoms. CHAPTER 19 MENT AL STATUS 93 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 8. Discuss what aspects of mental health are assessed during the general survey. 9. Discuss the incidence and risk factors for suicide. Activity D NCLEX STYLE QUESTIONS 10. What percent of the population identif ed as drug abusers abuse marijuana? a. 60% b. 50% c. 40% d. 30% 11. The outcome and costs of care of what diseases improve when depression is treated? (Mark all that apply.) a. HIV/AIDS b. Dementia c. Pneumonia d. Diabetes e. Tuberculosis 12. When depression goes undiagnosed, what consequences occur eight times more frequently than in the general population? a. Polyhedonia b. Comorbidity c. Death d. Bankruptcy 13. Which patients are most at risk for depressive symptoms? (Mark all that apply.) a. Married patients b. Divorced patients c. Females d. Males e. Chronically ill patients 14. In light of the low incidence of suicide, nurses are encouraged to perform what type of screening? a. General b. Targeted c. Focal d. Mini 15. As a nurse, when do you screen for alcohol and drug use? a. Every patient/every patient history b. Every patient/every interaction c. At-risk patient/every patient history d. At-risk patient/initial assessment 16. When assessing your patient you note that he is delusional. You would know that delusional thinking can lead to what? a. Insight b. Suicide c. Flight of ideas d. Comorbidity 17. Mr. Hanks, 77 years old, is brought to the clinic by his son, who states, “My father just doesn’t seem to be able to function as well as he used to.” When assessing this patient the nurse is aware that she will be a what? a. Patient advocate b. Diagnostician c. Surrogate decision maker d. Family liaison 18. You are admitting a patient to your unit for surgery the next morning. You note that the patient speaks at an accelerated pace and jumps from topic to topic, none of which progresses to sensible conversation. What would you document about this patient? a. Patient demonstrates confabulation b. Patient is depressed c. Patient demonstrates f ight of ideas d. Patient demonstrates schizophrenia 19. You are assessing a patient with a history of Korsakoff syndrome. What would you expect this patient might demonstrate? a. Psychotic tendencies b. Incoherence c. Flight of ideas d. Confabulation 94 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION III: CASE STUDY Activity E Belinda McGuire, 33 years old, presents at the clinic with vague complaints of aching joints, headache, and chronic fatigue. Vital signs are: temperature 36.9°C; BP 120/80; pulse 75; respirations 16; and pain 5/10. All objective physical f ndings are normal. She is tearful and responds only when spoken to. Demographics: 45 year old, married, lives in townhouse with wife. Plumber, self-employed. Scenario: Referred by family physician for assessment after being arrested for DWI for the second time in 12 months. Past medical history: 20-year history of alcohol use. No chronic illnesses. Family history: Grandfather, father, and one sister “have drinking problem.” No other signif cant family history. Behavior during interview: Anxious, does not want to discuss alcohol use. Denies having a problem; states, “I only drink beer. I don’t touch the hard stuff.” Presenting information: Appears well groomed. Physical f ndings during assessment: Temperature 36.6°C tympanic; pulse 118; R 20; BP 108/66. Skin warm, pink, dry. Odor of alcohol on breath. Using the information from the role play, write an assessment note including nursing diagnosis. Nursing diagnosis or problem: Signature Date SECTION V: DOCUMENTATION FORM FOR USE IN PRACTICE MENTAL HEALTH HISTORY Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Changes in attention, mood, or speech Changes in insight, orientation, or memory Delirium or dementia Onset Location Duration Characteristic Symptoms a. In light of Ms. McGuire’s presentation, how would you assess this patient? b. What potential nursing diagnoses may be relevant to this patient? SECTION IV: ROLE PLAY CHAPTER 19 MENT AL STATUS 95 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Chronic Illness Mental/emotional disease (present) Mental/emotional disease (past) Family History Mental/emotional disease Chronic illness Genetic testing Lifestyle Habits Alcohol Tobacco Drugs Physical activity Physical Examination Overview APPEARANCE AND BEHAVIOR Level of consciousness Posture and motor behavior Dress, grooming, and personal hygiene Facial expression Manner, affect, and relationship to people and things SPEECH AND LANGUAGE Quantity Rate Loudness Articulation of words Fluency MOOD THOUGHT AND PERCEPTIONS Thought processes Thought content Per ceptions Insight and judgment COGNITIVE FUNCTIONS Orientation Attention Remote memory Recent memory New learning ability HIGHER COGNITIVE FUNCTIONS Information and Vocabulary Calculating Ability Abstract Thinking Constructional Ability Health Promotion Topics Screening for depression Screening for suicide Screening for alcohol and substance abuse Screening for dementia 96 C H A P T E R 20 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Describe the structure and function of the nervous system. 2. Obtain an accurate history of the neurologic system. 3. Identify the cranial nerves and the motor and sensory functions. 4. Perform a screening neurologic examination. 5. Assess level of consciousness utilizing the Glasgow Coma Scale. 6. Document the f ndings of the nervous system examination. 7. Discuss risk reduction and health promotion strategies to reduce strokes. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Often the patient’s mental status offers clues about , disorders, and other conditions. B. Deep in the brain lies the basal , which affects , and the thalamus and the , structures in the . The Nervous System C. The , which lies at the base of the brain, coordinates all and helps maintain the body in space. D. The , which connects the upper part of the brain with the , has three sections: the , the , and the . E. The spinal cord is divided into f ve segments: , , , , and . F. Three kinds of impinge on the anterior horn cells: the tract, the system, and the system. G. Sudden brain damage involving the tract may produce a , which early in its course is . H. refers to a defect in the muscular control of the speech . I. Generalized begin with body movements, impairment of , or . J. Observe the for the of the base, the shift of the , and of the knee. CHAPTER 20 THE NERVOUS SYSTEM 97 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 2. List the cranial nerves. A. B. C. D. E. F. G. H. I. J. K. L. 3. List the warning signs of stroke. A. B. C. D. E. Activity B MATCHING 4. Match the level of consciousness with the def nition. Answer Level of Consciousness Def nition Alertness A. Arouses from sleep only after painful stimuli. Verbal responses are slow or even absent. Lethargy B. Opens the eyes and looks at you, but responds slowly and is somewhat confused Obtundation C. Unarousable with eyes closed Stupor D. Opens the eyes, looks at you, and responds fully and appropriately Coma E. Appears drowsy but opens the eyes and looks at you, responds to questions, and then falls asleep 5. Match the disorder of muscle tone with the location of the lesion. Answer Disorder of Muscle Tone Location of Lesion Spasticity A. Lower motor neuron system at any point from the anterior horn cell to the peripheral nerves Rigidity B. Both hemispheres, usually in the frontal lobes Flaccidity C. Upper motor neuron of the corticospinal tract at any point from the cortex to the spinal cord Paratonia D. Basal ganglia system 98 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the gait/posture to its description. Answer Gait/posture Description Spastic hemiparesis A. Patients appear to be walking through water. Steppage gait B. Gait is unsteady and wide based. Patients throw their feet for ward and outward and bring them down, f rst on the heels and then on the toes, with a double tapping sound. Parkinsonian gait C. Gait is staggering, unsteady, and wide based, with exaggerated diff culty on turns. Scissors gait D. Poor control of f exor muscles during swing phase Cerebellar ataxia E. Posture is stooped, with f exion of head, arms, hips, and knees. Patients are slow getting started. Sensory ataxia F. Patients either drag the feet or lift them high, with knees f exed, and bring them down with a slap onto the f oor, thus appearing to be walking up stairs. Activity D NCLEX STYLE QUESTIONS 11. Which of the following are types of diabetic neuropathies? (Mark all that apply.) a. Diabetic amyotrophy b. Autonomic dysfunction c. Mononeuritis multiplex d. Orthostatic hypotension e. Gastroparesis 12. Which cranial nerve controls pupillary constriction? a. Optic b. Oculomotor c. Trochlear d. Trigeminal 13. Where do the cell bodies of the lower motor neurons lie? a. Anterior roots b. Neuromuscular junction c. Motor strip d. Spinal cord 14. When assessing your patient you note bradykinesia. You would know that this abnormality is caused by damage to what? a. Basal ganglia system b. Medulla c. Cerebellar system d. Brainstem Activity C SHORT ANSWER 7. Def ne nystagmus and list the most common causes. 8. List the most common speech disorders and the pathophysiological processes that cause each. 9. Describe the distribution and functions of the peripheral nerves. 10. Describe the anatomy and physiology of the spinal cord. CHAPTER 20 THE NERVOUS SYSTEM 99 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 15. What functions are attributed to sensory impulses? (Mark all that apply.) a. Cessation of cough ref ex b. Stimulation of sneezing c. Regulation of internal autonomic functions d. Body position in space e. Conscious sensation 16. Mr. Clyde presents at the clinic with a complaint of weakness that is made worse with repeated effort and improves with rest. Mr. Clyde’s complaint is consistent with what health problem? a. Ischemic stroke b. Lyme disease c. Myasthenia gravis d. Parkinson disease 17. You are admitting a patient new to the clinic who states, “My face feels funny.” When you assess the patient you f nd isolated facial sensory loss to pain and no neurologic def cits in his extremities. What would you expect this patient to be diagnosed with? a. Stroke b. Horner syndrome c. Bell palsy d. Trigeminal neuralgia 18. You are assessing your patient’s coordination and you f nd that her movements are clumsy, unsteady, and inappropriately varying in their speed, force, and direction. You note the patient has dysmetria. What would you know this patient has? a. Cerebellar disease b. Cerebral disease c. Brainstem disease d. Basal ganglia disease 19. Your patient is diagnosed with a peripheral neuropathy. You know that often the f rst sensation lost in a peripheral neuropathy is what? a. Light touch b. Pain c. Vibration d. Temperature 20. What important questions guide the approach to this challenging clinical area? (Mark all that apply.) a. Where does the lesion lie? b. Is the central nervous system intact? c. Is the mental status intact? d. Is the peripheral nervous system intact? e. Are right-sided and left-sided examination f ndings symmetric? SECTION III: CASE STUDY Activity E Margaret Blankenship, 76 years old, has fallen down her front steps. She is brought to the emergency department by ambulance with a large bruise on her right temple. EMTs report that vital signs are: HR 120; BP 109/77; RR 16; T 37.5°C; and pain 4/10. a. List the major domains of assessment that you would address during a neurologic examination. b. What diagnostic tests would be completed on this patient? 100 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE THE NEUROLOGIC SYSTEM Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Headache Dizziness or vertigo Generalized, proximal, or distal weakness Numbness, abnormal or loss of sensations Loss of consciousness, syncope, or near syncope Seizures Tremors or involuntary movements Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Neurologic disease (present) Neurologic disease (past) Family History Neurologic disease Genetic testing Lifestyle Habits Alcohol Tobacco Physical activity Physical Examination Mental Status Exam Level of alertness Appropriateness of responses Orientation to date and place Cranial Nerves V isual acuity Pupillar y light ref ex Eye movements Hearing Facial strength—smile, eye closure Motor System Strength—shoulder abduction, elbow extension, wrist extension, f nger abduction, hip f exion, knee f exion, ankle dorsif exion Gait—casual, tandem Coordination—f ne f nger movements, f nger-to-nose Sensory System One modality at toes—can be light touch, pain/temperature, or proprioception Ref exes Deep tendon ref exes—biceps, patellar, Achilles Plantar responses Health Promotion Topics Preventing stroke or transient ischemic attack (TIA) Reducing risk of peripheral neuropathy 101 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Describe the anatomy and physiology of the female and male reproductive systems. 2. Conduct a focused interview to obtain patient history pertinent to the reproductive system. 3. Explain appropriate technique in inspecting and palpating external reproductive structures. 4. Discuss factors related to developmental, psychosocial, cultural, and environmental areas that affect the reproductive systems. 5. Differentiate between normal and abnormal f ndings in the reproductive system. 6. Accurately document subjective and objective data f ndings related to the reproductive system using the appropriate terminology. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. When detected early, testicular has a/an prognosis. B. Hernia pain and are more likely to occur when abdominal increases. C. The openings of glands are located on either side of the opening but are not usually visible. Reproductive Systems D. The junction migrates toward the , creating the zone. E. Increased secretions during stimulate the development of secondary including the and . F. Lymph from the vulva and drains into the . G. Questions about , , and often give the nurse an opportunity to explore the and attitude toward her body. H. Obstetricians commonly record the history using the “ ” system. I. Patients with - or preferences may be or during clinical encounters. J. The woman’s to the pelvic examination may reveal about her feelings about the and her . 2. List the symptoms of prostate disorders. A. B. C. D. E. F. C H A P T E R 21 102 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the phases of a woman’s reproductive health over the lifespan. A. B. Activity B MATCHING 4. Match the male reproductive term with its description. Answer Term Description Scrotal hernia A. A congenital displacement of the urethral meatus to the superior surface of the penis Hydrocele B. Seen in congestive heart failure or nephrotic syndrome Carcinoma of the penis C. Comes through the external inguinal ring, so the examining f ngers cannot get above it within the scrotum Hypospadias D. May manifest as an indurated nodule or ulcer that is usually nontender Epispadias E. It transilluminates, and the examining f ngers can get above the mass within the scrotum Primary syphilis F. Small scattered or grouped vesicles, 1–3 mm in size, on glans or shaft of penis Genital herpes simplex G. A chancre, or painless erosion up to 2 cm in diameter Chancroid H. Single or multiple papules or plaques of variable shapes Scrotal edema I. A congenital displacement of the urethral meatus to the inferior surface of the penis Genital warts J. A painful deep ulcer with ragged nonindurated margins 5. Match the female reproductive term with its description. Answer Term Description Epidermoid cyst A. A protozoan; often but not always acquired sexually Syphilitic chancre B. Appears as a tense, hot, very tender abscess Genital herpes C. Unpleasant f shy or musty genital odor Venereal wart D. Shallow, small, painful ulcers on red bases Bartholin gland infection E. Most commonly caused by trauma during childbirth, in particular multiple or diff cult births Trichomonal vaginitis F. A small, f rm, round nodule in the labia that is yellowish in color Candidal vaginitis G. Most develop internally; they often go undetected Bacterial vaginosis H. Result from infection with human papillomavirus Uterine prolapse I. White and curdy discharge C. D. E. CHAPTER 21 REPRODUCTIVE SYSTEMS 103 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the abnormality of the male reproductive system to its description. Answer Abnormality Description Cryptorchidism A. Seen in mumps and other viral infections; usually unilateral Varicocele of the spermatic cord B. A painless, movable cystic mass just above the testis Acute orchitis C. Feels like a soft “bag of worms” separate from the testis, and slowly collapses when the scrotum is elevated in the supine patient Tumor of the testis D. Coexisting urinary tract infection or prostatitis supports the diagnosis Torsion of the spermatic cord E. The testis is atrophied and may lie in the inguinal canal or the abdo men, resulting in an unf lled scrotum Spermatocele and cyst of the epididymis F. Most common in adolescents Acute epididymitis G. Usually appears as a painless nodule 12. You are taking a sexual history on a new patient. What action is considered appropriate at this time? (Mark all that apply.) a. Explain to the patient what is considered to be normal sexual behavior b. Aff rm that your conversation is conf dential c. Note that you realize this information is highly personal d. Explain why you are taking the sexual history e. Relate that you gather this history on only high-risk patients 13. A 35-year-old female has come to the clinic for her yearly check-up. During the history the patient tells you that she does not “feel anything” during sex with her husband. You know that the most common cause of this type of problem is what? a. A situational factor b. A physical factor c. A medical factor d. A social factor 14. A rape victim is being examined in the emergency department. A special rape kit must be used to ensure what? a. Anonymity of care b. Diagnostic imaging is performed c. A chain of custody for evidence d. Only licensed personnel do the examination Activity C SHORT ANSWER 7. Explain the patient instructions for testicular self-examination. 8. Discuss the risk factors for prostate cancer. 9. Describe the types and causes of dysmenorrhea. 10. Describe the onset, causes, signs, and symptoms of menopause. Activity D NCLEX STYLE QUESTIONS 11. What is a lay term for the spontaneous loss of pregnancy? a. Missed abortion b. Missed pregnancy c. Abortion d. Miscarriage 104 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 15. What are the indications for a pelvic examination during adolescence? (Mark all that apply.) a. Onset of menarche at age 13 b. Minimal bleeding during menses c. Dysmenorrhea d. Prescription of contraceptives e. Vaginal discharge 16. Mrs. Janis brings her 11- and 13-year-old daughters to the clinic to receive the HPV vaccine. Mrs. Janis wants to know how long her daughters will have immunity once they are vaccinated. What would be the correct response? a. Length of immunity is 5 years b. Length of immunity is 25 years c. Length of immunity is lifetime d. Length of immunity is undetermined 17. Donovan Graham, a 45-year-old black male, tells the nurse that he has little or no interest in sex. He says he is concerned and he knows his wife is unhappy with his lack of libido. What can you tell Mr. Graham often causes lack of libido? a. Manic episodes b. Mental illness c. Side effects of medications d. Testosterone hypersecretion 18. You are presenting patient education on STDs to a high school health class. What infection would you tell the students can be transmitted by oral–penile transmission? a. Cervical cancer b. Chlamydia c. Prostatitis d. Urethritis 19. Your patient states that she does not enjoy sex because she does not attain adequate vaginal lubrication. You should be aware of what potential causes of sexual dysfunction? (Mark all that apply.) a. Psychiatric conditions b. Medical illness c. Excessive testosterone d. Amenorrhea e. Lack of estrogen 20. What ethnic group has a signif cantly higher incidence rate of prostate cancer? a. Native American b. African American c. Caucasian d. Asian SECTION III: CASE STUDY Activity E Sixty-seven-year-old Ernest Rand, a Dutch national, is touring the United States when he comes to an acute care clinic complaining of severe pain on urination. a. Describe a physical examination of this patient’s penis. b. What diagnostic tests would be completed on this patient? CHAPTER 21 REPRODUCTIVE SYSTEMS 105 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE THE REPRODUCTIVE SYSTEM Patient Name Date/Time Overview. Identifying Data Source and Reliability Female Reproductive Tract Common or Concerning Symptoms Menarche, menstruation, menopause, postmenopausal bleeding Dysmenorrhea Pregnancy Sexual abuse Vulvovaginal symptoms Sexual preference and sexual response Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Reproductive disorders (present) Reproductive disorders (past) Family History Reproductive disorders Genetic testing Lifestyle Habits Alcohol Tobacco Sexual preference Sexual partners (#) Menarche, menstruation, menopause Obstetric history Pregnancy Contraception V ulvovaginal symptoms Sexual preference and sexual response Sexually transmitted diseases Physical Examination External Examination Mons pubis Labia majora and minora Urethral meatus, clitoris V aginal introitus Perineum 106 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Internal Examination V isual V agina and cervix V aginal muscle tone Color , ulcerations, inf ammation, discharge, or masses Bimanual examination Cer vix and uterus Ovaries Health Promotion Topics Anatomy and physiology of the reproductive system and its changes from puberty to menopause Cervical cancer screening: Pap smear and human papilloma virus (HPV) infection Early prenatal care Options for family planning Sexually transmitted diseases and HIV Male Reproductive Tract Common or Concerning Symptoms Sexual preference and sexual response Penile discharge or lesions Scrotal pain, swelling, or lesions Problems with urination Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Reproductive disorders (present) Reproductive disorders (past) Family History Reproductive disorders Genetic testing Lifestyle Habits Alcohol Tobacco Sexual preference Sexual partners (#) Physical Examination The Penis Inspection The Scrotum and its contents Inspection Hernias Inspection Important Topics for Health Promotion and Counseling Prevention of STDs and HIV Testicular self-examination Screening for prostate cancer 107 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Identify the components of the physical examination. 2. Identify the best approach for the physical examination based on individual patient needs. 3. Utilize lighting and the environment to ensure an accurate physical examination. 4. Demonstrate a head-to-toe physical examination. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Generally, a ___________ assessment is performed on or to a health care facility. B. Generally, a is performed in a - - sequence comparing to for symmetry. C. Determining the most format for you to perform the physical examination is the step. D. During the , remember to consider the patient’s . Putting It All Together E. As a practitioner, your examination of the patient should take less than from start to f nish. F. If an __________ is missed, it may be at another place in the exam. G. It is recommended that acuity be inserted at the or at the of the examination to alleviate the patient another time. H. The integration of the and data guides the nurse in preparing the best nursing of for the patient. 2. List the equipment needed to perform a comprehensive physical examination. A. B. C. D. E. F. G. H. I. J. K. L. M. N. C H A P T E R 22 108 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. O. P. Q. R. S. T. U. V. Activity B MATCHING 3. Match each assessment with the most appropriate patient position. Answer Assessment Patient Position Range of motion of the spine A. Patient lying down Cardiac auscultation B. Patient seated Deep tendon ref exes C. Patient standing Breast examination Romberg test Strength and range of motion of the arms Cranial nerve function Abdominal palpation Inspection of the eyes Activity C SHORT ANSWER 4. Explain the examination of the nose and sinuses. 5. Discuss the peripheral vascular examination. 6. List some of the guidelines and tips for conducting an eff cient and accurate health assessment. 7. Describe how you would assess the posterior thorax. Activity D NCLEX STYLE QUESTIONS 8. You have a hand-held Snellen. When in the sequence of assessment should you assess visual acuity? a. General assessment b. Eye assessment c. Beginning of exam d. End of exam 9. It is important to apprise the patient of what you are doing and what you f nd as it does what? a. Causes assessment f ndings to be more accurate b. Speeds up the pace of the assessment c. Opens up teaching/learning moments d. Instills a friendly feeling toward you in the patient 10. You are preparing to enter your patient’s room. Before doing so, you should assess your own: a. Demeanor b. Skill set c. Personal history d. Breathing CHAPTER 22 PUTTING IT ALL TOGETHER 109 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 11. At the beginning of the exam you would perform a general survey. What would you assess at this time? a. Hearing acuity b. Pedal pulses c. Oxygen saturation d. Safety 12. When inspecting the face for facial symmetry, what would you have the patient do? (Mark all that apply.) a. Raise eyebrows b. Frown c. Grin d. Stick out tongue e. Close eyes Demographics: 19 year old, single, lives in dormitory. College freshman. Scenario: Comes to the student clinic for a physical assessment before playing college volleyball. Past medical history: No chronic illness; childhood illness (mumps, measles, whooping cough). No disabilities. Family history: None signif cant. Behavior during interview: Calm, relaxed, communicative. Presenting information: Appears well groomed. Physical f ndings during assessment: Temperature 37°C tympanic, pulse 120, R 16, BP 100/62. Using the information from the role play, write an assessment note for a comprehensive physical examination for this patient. Nursing diagnosis or problem: Signature Date SECTION III: CASE STUDY Activity E Lucy Linquist, a 27-year-old elementary school teacher, comes to the emergency department after being in a motor vehicle accident. She complains of pain in the abdomen. Vital signs are as follows: T 36.9°C; pulse 125; BP 80/50; R 26; and pain 9/10. a. What physical assessment would be indicated for this patient? The patient is found to have a ruptured kidney. b. What laboratory tests would you expect to be run on this patient? SECTION IV: ROLE PLAY 110 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. COMPREHENSIVE ASSESSMENT Patient Name Date/Time Overview. Identifying Data Source and Reliability Common or Concerning Symptoms Onset Location Duration Characteristic symptoms Associated manifestations Relieving factors Treatment History Medications (current) Medications (past) Surgeries Illnesses Family History Cancer Diabetes Other Chronic Illnesses Genetic Testing Lifestyle Habits Alcohol Tobacco Sexual preference Sexual partners (#) Overview Age—stated age versus apparent age Emotional state—compare verbal description and nonverbal indicators Developmental stage—compare with behavior Cultural background Health requirements and learning needs Mental Status a. Level of consciousness b. Facial expressions c. Speech d. Thought processes and perception e. Mood f. Grooming and hygiene g. Posture, gait, and body movements *If changes are noted, then a mini-mental status examination should be performed. Vital Signs a. Temperature b. Pulse c. Respirations d. Blood pressure—arm at heart level e. Pain SECTION V: DOCUMENTATION FORM FOR USE IN PRACTICE CHAPTER 22 PUTTING IT ALL TOGETHER 111 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Body Measurements a. Height b. Weight c. Body mass index and ideal body weight Integument—assess throughout examination as you examine each part of the body. a. Inspect for color, lesions, scars, rashes, or any changes in the skin. b. Palpate for moisture, temperature, and texture. c. Palpate for skin turgor. d. Inspect the hair for color, distribution, and texture. e. Inspect and palpate the nails for size, shape, color, texture, angle, ref ll, and any changes. Head a. Inspect the skull for size and shape. b. Inspect the scalp for tenderness, lesions, and bumps. Face a. Inspect facial features for symmetry. Cranial nerve VII, facial: symmetry of face—raise eyebrows, frown, close eyes, smile, puff out cheeks. b. Palpate temporal and masseter strength. c. Assess temporomandibular joint for pain, crepitus, and swelling. d. Assess sensation to sharp and light on face—forehead, cheeks, and chin. (Continue assessing arms and feet for sharp and light touch.) Cranial nerve V, trigeminal. Eyes a. Inspect eyelids. b. Inspect eyelashes. c. Inspect eyebrows. d. Inspect lacrimal apparatus. e. Inspect conjunctiva. f. Inspect sclera. g. Inspect cornea. h. Inspect lens. i. Inspect pupils. Cranial nerve II, optic; cranial nerve III, occulomotor - Direct light reaction; consensual light reaction j. Test confrontation. Cranial nerve II, optic k. Test six cardinal directions of gaze. Cranial nerve III, occulomotor; cranial nerve IV, trochlear; cranial nerve VI, abducens; -Convergence; -Near reaction (accommodation); - Cover–uncover test l. Ophthalmoscopic examination—check optic disc for color, size, and shape. Ears a. Inspect auricle, lobe, and tragus for position, shape, ulcers, lesions, or discharge. b. Palpate auricle and tragus for tenderness or lumps. c. Palpate mastoid f rmly for tenderness. d. Otoscopic examination—inspect inner canal, tympanic membrane, and cone of light. e. Hearing acuity - Cranial nerve VIII, acoustic; - Whisper test; - Weber (518 Hz on top of head); -Rinne (518 Hz on mastoid bone and compare to air conduction) Nose and Sinuses a. Inspect for symmetry, alignment, and deformity. b. Palpate for tenderness and patency. c. Palpate frontal and maxillary sinuses. d. Inspect mucous membrane, septum, and turbinates for inf ammation, polyps, ulcers, and deviation. e. Sense of smell—have patient identify two different scents with eyes closed. Cranial nerve I, olfactory Mouth and Pharynx a. Inspect lips, oral mucosa, gums, roof of mouth, and f oor of mouth for color, lesions, and moisture. b. Inspect dentition for condition, number, and placement. c. Tongue - Inspect for size, shape, color, moisture, lesions, and texture. 112 UNIT 2 BODY SYSTEMS Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. - Articulation of words; Cranial nerve XII, hypoglossal; - Range of motion—assess at-rest, raised, sticking out, and side-to-side movements; – Taste; Cranial nerve VII, facial; cranial nerve IX, glossopharyngeal; d. Pharynx—inspect rise of palate and uvula; cranial nerve IX, glossopharyngeal; cranial nerve X, vagus Neck a. Inspect anteriorly for symmetry, masses, enlarged glands, or deviation. b. Inspect trachea position. c. Inspect thyroid. d. Palpate thyroid. e. Palpate lymph nodes (preauricular, posterior auricular, occipital, tonsillar, submandibular, submental, superf cial cervical, posterior cervical, deep cervical chain, supraclavicular). f. Test sternomastoid and upper trapezius muscle strength; cranial nerve XI, spinal accessory g. Test head and neck range of motion (f exion, extension, rotation, and lateral bends). Posterior Thorax a. Inspect shape, deformities, retractions, symmetry, and skin integrity. b. Palpate for - Tenderness - Tactile fremitus - Respiratory expansion c. Percuss lung sounds and diaphragmatic excursion. d. Auscultate lung sounds. Anterior Thorax (can also be performed with patient lying down if preferred) a. Inspect for shape, deformities, retractions, symmetry, and skin integrity. b. Palpate for - Tenderness - Tactile fremitus - Respiratory expansion c. Percuss sounds and diaphragmatic excursion. d. Auscultate lung sounds. Cardiovascular (can also be performed with patient lying down if preferred) a. Inspect carotid arteries for pulsations. b. Palpate carotid arteries. c. Auscultate carotids with the Bell while patient holds breath. d. Inspect external jugular vein. e. Inspect precordium. f. Auscultate heart with the diaphragm at the right sternal border 2nd intercostal space (ICS), left sternal border 2nd ICS, left sternal border 3rd ICS, left sternal border 4th ICS, left sternal border 5th ICS, and left midclavicular line (MCL) 5th ICS. g. Auscultate heart with the Bell at the right sternal border 2nd ICS, left sternal border 2nd ICS, left sternal border 3rd ICS, left sternal border 4th ICS, left sternal border 5th ICS, and left MCL 5th ICS. h. Auscultate with the Bell at the apical impulse while in the left lateral decubitus position (listening for mitral murmur, S3, S4). Breasts a. Inspect with - Arms at side - Hands pressed into hips - Arms raised over head Axillary Nodes a. Palpate axillary nodes (central, lateral, pectoral, subscapular). Patient Lying Down Breast Examination a. Place the arm that is on the side of the breast being examined under the head. Abdomen a. Inspect for contour, pulsations, bulges, and skin integrity. b. Auscultate for bowel sounds and aortic pulsation. c. Abdominal ref ex—lightly stroke inward in all quadrants. CHAPTER 22 PUTTING IT ALL TOGETHER 113 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. d. Lightly palpate all four quadrants noting masses, tenderness, and patient’s expression. e. Palpate for the liver, kidneys, and spleen. Peripheral Vascular a. Inspect arms and legs for color, swelling, hair distribution, and nail bed color. b. Palpate - Carotid - Radial - Brachial - Femoral - At this time palpate the remaining lymph nodes: inguinal lymph nodes (vertical then horizontal groups). - Posterior tibial - Dorsalis pedis c. Palpate for pitting edema in feet and legs. Musculoskeletal a. Inspect for deformity, swelling, nodules, redness, and muscle bulk. b. Palpate for tenderness, crepitus, swelling, and increased warmth. c. Palpate strength and range of motion - Hips (f exion, extension, abduction, adduction, internal and external rotation) - Knees (f exion and extension) - Ankles (dorsif exion, plantarf exion, inversion, eversion) - Toes (f exion, extension, abduction, adduction) Patient Seated Neurologic—Motor a. Inspect body position, noting tremors. b. Deep tendon ref exes - Biceps - Triceps - Brachioradialis - Patellar - Achilles Neurologic—Sensory (if not incorporated previously then complete now) a. Pain and light touch—if the patient is unable to feel pain and light touch, then assess for vibration and temperature. Musculoskeletal a. Inspect for deformity, swelling, nodules, redness, and muscle bulk. b. Palpate for tenderness, crepitus, swelling, and increased warmth. c. Palpate strength and range of motion - Shoulders (f exion, extension, abduction, adduction, internal and external rotation) - Elbows (f exion, extension, pronation, supination) - Wrists (f exion, extension, radial and ulnar deviation) - Fingers (grip and f exion, extension, adduction, abduction) - Thumb (f exion, extension, opposition, abduction, adduction) Patient Standing Musculoskeletal—Spine a. Inspect for deformity, symmetry, and skin integrity. b. Palpate spinous processes. c. Assess range of motion (f exion, extension, lateral bends, rotation). Neurologic a. Perform Romberg, gait, balance, and other appropriate neurologic screenings. 114 C H A P T E R 23 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Gather a history on an infant, child, and adolescent. 2. Perform a developmental assessment on infants, children, and adolescents. 3. Utilize age-appropriate techniques to perform a physical examination on infants, children, and adolescents. 4. Analyze f ndings against age-appropriate norms and standards. 5. Identify education topics for anticipatory guidance, health promotion, and risk reduction. 6. Correctly document infant, child, and adolescent assessment f ndings. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. When examining and , the sequence should vary according to the child’s and level. Assessing Children: Infancy through Adolescence B. With , as with adults, the point at which the sounds disappear constitutes the pressure. C. Causes of sustained in childhood include renal or , of the aorta, and primary . D. For young children, the of the wall for 30-second intervals or minute, preferably before them. E. are the most common health problem in children. F. Adolescence is the of from to . G. Adolescence is a tumultuous time, marked by the transition from to and . H. Adolescents are more likely to when the interview focuses on rather than on their . I. Your goal is to help adolescents bring their or to their . CHAPTER 23 ASSESSING CHILDREN: INFANCY THROUGH ADOLESCENCE 115 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. J. The size of the approaches the size as the teen progresses through , and is related to the adolescent’s overall . 2. List the general principles of child development. A. B. C. D. 3. List the developmental tasks during middle childhood. A. B. C. D. E. F. G. Activity B MATCHING 4. Match the common childhood lesions with their description. Answer Common Childhood Lesions Description Insect bites A. Annular lesion that has central clearing and papules along the border Urticaria (hives) B. Scaling, crusting, and hair loss Tinea corporis C. Intensely pruritic, red, distinct papules Tinea capitis D. Pruritic, allergic sensitivity reaction that changes shape quickly 5. Match the developmental task of adolescence with its characteristic (tasks will have more than one characteristic dependent on the stage of adolescence). Answer Characteristic Task Peers increasingly important A. Physical Females more comfortable, males awkward B. Cognitive “Formal operational” C. Identity Def ning sexuality D. Independence Separation from family Adult appearance Concern with global issues Bodily changes of puberty Ambivalence Limit testing Transition; many ideas “Concrete operational” 116 UNIT 3 SPECIAL LIFESPAN Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 6. Match the primitive ref ex to its description. Answer Primitive Ref ex Description Palmar grasp ref ex A. The arm/leg on side to which head is turned extends while the opposite arm/leg f exes. Plantar grasp ref ex B. The mouth will open and baby will turn the head toward the stimulated side and suck. Moro ref ex C. The toes curl Asymmetric tonic neck ref ex D. The spine will curve toward the stimulated side. Positive support ref ex E. The hip and knee of that foot will f ex and the other foot will step forward. Alternate stepping will occur. Rooting ref ex F. The arms and legs will extend in a protective fashion. Galant ref ex G. The hips, knees, and ankles extend; the baby stands up, partially bearing weight, and sags after 20–30 seconds. Placing and stepping ref exes H. The head will lift up, and the spine will straighten. Landau ref ex I. The arms abduct and extend, hands open, and legs f ex. Baby may cry. Parachute ref ex J. The baby will f ex all f ngers to grasp your f ngers Activity D NCLEX STYLE QUESTIONS 11. What does laxity of the soft-tissue structures of the foot cause in young children? a. Pronation b. Pes planus c. Metatarsus adductus d. Talipes calcaneovalgus 12. After the age of 2 years, how much do toddlers grow per year? a. About 3 cm b. About 5 cm c. About 7 cm d. About 9 cm 13. You are examining a 3-year-old girl who becomes very distressed during the examination. What should you tell the parents? a. “This behavior shows a lack of discipline.” b. “This behavior shows inability to adjust.” c. “This behavior is developmentally appropriate.” d. “This behavior is socially inappropriate.” Activity C SHORT ANSWER 7. Discuss the test for scoliosis in the adolescent. 8. Discuss four major principles of child development and relate them to the technique for conducting a health assessment. 9. Discuss social and emotional development during middle childhood. 10. Discuss tips for examining 1- to 4-year-olds. CHAPTER 23 ASSESSING CHILDREN: INFANCY THROUGH ADOLESCENCE 117 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 14. You are speaking to a local PTO about childhood obesity. What would you cite as the consequences of childhood obesity? (Mark all that apply.) a. Hepatic disease b. Hypertension c. Metabolic syndrome d. Poor self-esteem e. Pulmonary disease 15. When examining visual acuity on a 30-monthold child, you should assess for what? a. Fixation preference b. “Lazy eye” c. Hyperopia d. Myopia 16. While performing cardiac auscultation of a young child, you detect a pulmonary f ow murmur that is accompanied by a f xed splitsecond heart sound. What does this suggest? a. Aortic insuff ciency b. Tricuspid valve prolapse c. Left-heart volume load d. Right-heart volume load 17. Your patient is a 15-year-old male. His testes and scrotum are enlarged and the scrotal skin is darkened. His pubic hair is coarse and curly but does not extend to the thighs. What Tanner stage would you assign to this patient? a. Stage 2 b. Stage 3 c. Stage 4 d. Stage 5 18. Mrs. Mendellson has brought 14-year-old Lucretia to the clinic because of her weight. When weighed, Lucretia falls below the 5th percentile for her height. The nurse notes that Lucretia is so thin that her bony skeleton is readily observable. She has delayed sexual development. What would the nurse f rst suspect? a. Bulimia nervosa b. Anorexia nervosa c. Cystic f brosis d. AIDS 19. What is helpful in measuring older children, especially if the child is suspected of having endocrine disorders? a. Age:weight comparison b. WHO child growth standards c. Symphysiofundal height growth curve d. Velocity growth curves 20. Elevated blood pressure readings in children are most often attributable to what? a. Obesity b. An improperly performed examination c. Diabetes d. An improperly calibrated sphygmomanometer SECTION III: CASE STUDY Activity E Sixteen-year-old George Kristus comes to the clinic for a sports physical. a. Describe a physical examination of this patient. b. Describe the priority focuses during this assessment and the rationale for each. 118 UNIT 3 SPECIAL LIFESPAN Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE PEDIATRIC HEALTH HISTORY AND PHYSICAL EXAMINATION Patient Name Date/Time Overview Referral Source and Reliability Chief Complaint Present Illness Medications Past History Pregnancy Newborn period Illnesses Accidents Preventive Care Family history Developmental history Personal and social history Environmental exposures Review of Systems General Skin Head, eyes, ears, nose, and throat (HEENT) Head Eyes Ears Nose Mouth Neck Respiratory Cardiovascular Gastrointestinal Urinary Genital Musculoskeletal Neurologic Psychiatric Physical Examination Vital signs Skin HEENT Head Eyes Ears Nose Mouth CHAPTER 23 ASSESSING CHILDREN: INFANCY THROUGH ADOLESCENCE 119 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Neck Lymph nodes Lungs Cardiovascular Breasts Abdomen Genitalia Musculoskeletal Neurologic Mental status Developmental (DDST) Cranial nerves Cerebellar Deep tendon ref exes (DTRs) Sensor y 120 C H A P T E R 24 SECTION I: LEARNING OBJECTIVES Learning Objectives The student will: 1. Determine how to best facilitate the health history and physical examination of the older adult. 2. Identify areas of focus during the health history specif c to the older adult. 3. Recognize normal physiologic changes in the older adult. 4. Address areas of health promotion and counseling specif c to the older adult. 5. Utilize screening tools in the assessment of older adults. 6. Perform a health history and physical assessment on an older adult. 7. Document the older adult assessment f ndings. SECTION II: STUDY GUIDE Activity A FILL IN THE BLANK 1. Complete the following statements: A. Over the past years, actually have become more and less . B. Self-neglect is a growing and represents more than of adult referrals. C. Depressed men older than have the of suicide and require careful and . Assessing Older Adults D. Loss of from fear of and anxiety further impair . E. Cancer screening can be because of supporting its use for adults older than to years. F. In general, decisions should be based on each older person’s , rather than alone. G. the abdomen for , , or artery bruits. H. may occur with poor hygiene or or caries. I. Investigators have identif ed vast in how people and have distinguished “ ” aging, with its complex of diseases and impairments, from “ ” aging. J. Because their eyes produce fewer , aging patients may complain of . 2. List the home safety and fall prevention tips for older adults. A. B. C. D. E. F. CHAPTER 24 ASSESSING OLDER ADULTS 121 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 3. List the important topics for health promotion and counseling in the older adult. A. B. C. D. E. F. G. H. I. J. K. Activity B MATCHING 4. Match the problem with its relevant assessment technique or f nding. Answer Problem Assessment Technique or Finding Vision loss A. Unable to complete movement task in 15 seconds Hearing loss B. Weight <100 lbs Leg immobility C. “Do you often feel sad or depressed?” Urinary incontinence D. Unable to remember all three items after 1 minute Malnutrition E. Inability to hear 1,000 or 2,000 Hz in both ears or either of these frequencies in one ear Memory impairment F. “Are you able to go shopping for groceries or clothes?” Depression G. “Do you have diff culty driving or watching television? Physical disability H. “Have you lost urine on at least six separate dates?” 5. Match the characteristic with the type of pain. (Type of pain will have more than one characteristic.) Answer Characteristic Type of Pain Can f uctuate in character and intensity over time A. Acute Obvious pathology B. Persistent Distinct onset Lasts more than 3 months Short duration Common causes: arthritis, cancer, claudication, leg cramps, neuropathy, radiculopathy 122 UNIT 3 SPECIAL LIFESPAN Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. Activity C SHORT ANSWER 6. Describe the role of advance directives and the guidelines surrounding their appropriate use. 7. Def ne dementia and describe the etiology and clinical characteristics of this health problem. 8. List the immunizations that should be made available to older adults and the rationale for each. 9. Discuss the use of medications in the older population and relate this to the relevant nursing responsibilities. 10. Compare and contrast delirium and dementia. Activity D NCLEX STYLE QUESTIONS 11. When discussing palliative care with a patient, what would you say are the goals? (Mark all that apply.) a. Improvement in the quality of life b. Providing bereavement support c. Management of family values d. Relieving suffering e. Communication among family members 12. You are assessing an older adult patient for a closed head injury after a motor vehicle accident. What ref ex would you assess for? a. The pig ref ex b. The grasp ref ex c. The snout ref ex d. The spinal ref ex 13. A 75-year-old female patient tells you that she is sexually active but that it causes her pain when she has intercourse. What would you suggest to alleviate this pain? a. Taking warm baths b. Exclusive use of a side-lying position c. Cold application d. Having sex in the morning 14. What would be important to assess when detecting alcohol use disorders in older adults? a. Increased appetite b. Increased proprioception c. Blood sugar control problems d. Diff culty managing Levoxyl dosing 15. You are providing an educational event for the families of elderly patients. What would you tell them that ER visits and fatalities frequently involve? (Mark all that apply.) a. Exercise injuries b. Hair dryers and nonf ammable clothing c. Ladders and stepstools d. Bathroom injuries e. Yard and garden equipment 16. The nurse is assessing a new patient, age 68 years, for orthostatic hypotension. The nurse would know that this means a drop in systolic blood pressure of ≥20 mm Hg or diastolic blood pressure of ≥10 mm Hg within how many minutes of standing? a. 4 minutes b. 3 minutes c. 2 minutes d. 1 minute CHAPTER 24 ASSESSING OLDER ADULTS 123 Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. 17. Grady O’Bannion, a 70-year-old black male, is brought to the clinic by his daughter, who tells the nurse that she is concerned because her father appears to be losing weight and she doesn’t know why. What would the nurse know is a cause of undernutrition? a. Poor time management b. Obsessive/compulsive disorder c. Acute organ failure d. Poverty 18. When assessing the eyes of an older adult, impairment of what gaze may be a result of age-related changes? a. Downward gaze b. Upward gaze c. Conjugate gaze d. Consensual gaze 19. You are counseling an elderly patient and her family. Why would you recommend regular aerobic exercise? (Mark all that apply.) a. Maintain high blood sugar levels b. Slow onset of disability c. Improve energy level d. Maintain social interaction e. Improve strength 20. You tell your patient that you are going to listen to his abdomen for sounds of blood rushing through the blood vessels. He wants to know why you are specif cally listening for this. How would you answer him? a. “Bruits over the aorta or renal or femoral artery are found in cardiovascular disease.” b. “Bruits over the aorta or renal or femoral artery are found in atherosclerotic disease.” c. “Bruits over the aorta or renal or femoral artery are found in chronic pulmonary disease.” d. “Bruits over the aorta or renal or femoral artery are found in rheumatoid arthritis disease.” SECTION III: CASE STUDY Activity E Eighty-one-year-old Phillip Lister has come to the clinic for a routine check-up. a. Document Mr. Lister’s check-up using The Siebens Domain Management Model. b. What would you include in patient education for Mr. Lister and his family? 124 UNIT 3 SPECIAL LIFESPAN Copyright © 2012. Wolters Kluwer Health | Lippincott Williams & Wilkins. Student Laboratory Manual for Bates’ Nursing Guide to Physical Examination and History Taking. SECTION IV: DOCUMENTATION FORM FOR USE IN PRACTICE ASSESSMENT OF THE OLDER ADULT Patient Name Date/Time Overview Identifying Data Source and Reliability Vital Signs Ht (without shoes) Wt (dressed) Body mass index (BMI) BP: right arm supine, left arm supine Heart rate (HR) Respiratory rate (RR) Temperature (oral) 10-Minute Geriatric Screener Vision Hearing Leg mobility Urinary incontinence Nutrition Memory Depression Physical disability Physical Examination Skin Head, eyes, ears, nose, throat (HEENT) Neck Lymph nodes Thorax and lungs Cardiovascular Abdomen Genitourinary Rectal Extremities Peripheral vascular Musculoskeletal Neurologic 125 Answers D. Primary prevention focuses on improving overall wellness and protecting from disease or disability. E. The nurse’s initial role in health assessment is to collect data. 2. List the facets of health. A. Physical health B. Emotional health C. Social well-being D. Culture E. Spiritual inf uences F. Developmental level [Show More]
Last updated: 1 year ago
Preview 1 out of 207 pages
Reviews( 0 )
Recommended For You
Anatomy and Physiology - A&P 1> Manual > LABORATORY MANUAL FOR HUMAN ANATOMY & PHYSIOLOGY 4TH EDITION BY TERRY R. MARTIN CYNTHIA PRENTICE-CRAVER (All)
LABORATORY MANUAL FOR HUMAN ANATOMY & PHYSIOLOGY 4TH EDITION BY TERRY R. MARTIN CYNTHIA PRENTICE-CRAVER
LABORATORY MANUAL FOR HUMAN ANATOMY & PHYSIOLOGY 4TH EDITION BY TERRY R. MARTIN CLABORATORY MANUAL FOR HUMAN ANATOMY & PHYSIOLOGY 4TH EDITION BY TERRY R. MARTIN CYNTHIA PRENTICE-CRAVERLABORATORY MANUA...
By Quiz Merchant , Uploaded: Jan 17, 2023
$25
Anatomy> Manual > Laboratory Manual for Hole's Human Anatomy & Physiology 16th Edition by Phillip Snider & Terry Martin - Complete, Elaborated and Latest Test Bank. ALL Chapters (1-64) Included and Updated for 2023 (All)
Laboratory Manual for Hole's Human Anatomy & Physiology 16th Edition by Phillip Snider & Terry Martin - Complete, Elaborated and Latest Test Bank. ALL Chapters (1-64) Included and Updated for 2023
Laboratory Manual for Hole's Human Anatomy & Physiology 16th Edition by Phillip Snider & Terry Martin - Complete, Elaborated and Latest Test Bank. ALL Chapters (1-64) Included and Updated for 2023...
By ProfXams , Uploaded: Jan 24, 2024
$28.5
*NURSING> Manual > NURS 6003 Academic and Professional Success Plan Template, Filled and Graded. Walden University (All)
NURS 6003 Academic and Professional Success Plan Template, Filled and Graded. Walden University
Week 1 | Part 1: My Academic and Professional Network Why I selected this individual and/or team and how they will support my success in the MSN program and as a practicing nurse: Week 2 | Part 2: A...
By Kirsch , Uploaded: Jun 08, 2020
$10
Operations Management> Manual > Complete Test Bank for Operations Management 14th Edition Stevenson All Chapters 1 - 19! RATED A+ (All)
Complete Test Bank for Operations Management 14th Edition Stevenson All Chapters 1 - 19! RATED A+
Complete Test Bank for Operations Management 14th Edition Stevenson All Chapters 1 - 19! RATED A+
By ACADEMICTUTORIAL , Uploaded: Oct 25, 2023
$7.5
Art> Manual > Sun Tzu on The Art of War: THE OLDEST MILITARY TREATISE IN THE WORLD Translated from the Chinese By LIONEL GILES, M.A. (1910) (All)
Sun Tzu on The Art of War: THE OLDEST MILITARY TREATISE IN THE WORLD Translated from the Chinese By LIONEL GILES, M.A. (1910)
Laying out plan Waging war Attack by Stratagem Tactical Dispositions Energy Weak points and strong Maneuvering Variation in Tactics The army on the march Terrain The nine situations The atta...
By QuizMaster , Uploaded: Sep 22, 2019
$9.5
> Manual > MARKETING STRATEGY & COMPETITIVE POSITIONING (All)
MARKETING STRATEGY & COMPETITIVE POSITIONING
PArt 1 MARKETING STRATEGY 3 1 MARKET-LED STRATEGIC MANAGEMENT 4 2 STRATEGIC MARKETING PLANNING 28 PArt 2 COMPETITIvE MARKET ANALYSIS 53 3 THE CHANGING MARKET ENvIRONMENT 54 4 CUSTOMER ANALYSIS 88...
By QuizMaster , Uploaded: Sep 02, 2019
$0
Health Care> Manual > BASIC CLEANLINESS AND PROTECTION (All)
BASIC CLEANLINESS AND PROTECTION
BASIC CLEANLINESS AND PROTECTION To prevent the spread of germs, always wash your hands with soap and water before and after giving first aid. When a person is hurt, the most important thing is to...
By Passmark , Uploaded: Sep 20, 2022
$5
*NURSING> Manual > NCLEX-RN Cram Sheet by 2019 Update: This NCLEX-RN cram sheet or cheat sheet can help you prepare as it contains condensed facts about the nurse licensure exam itself and key nursing information: (All)
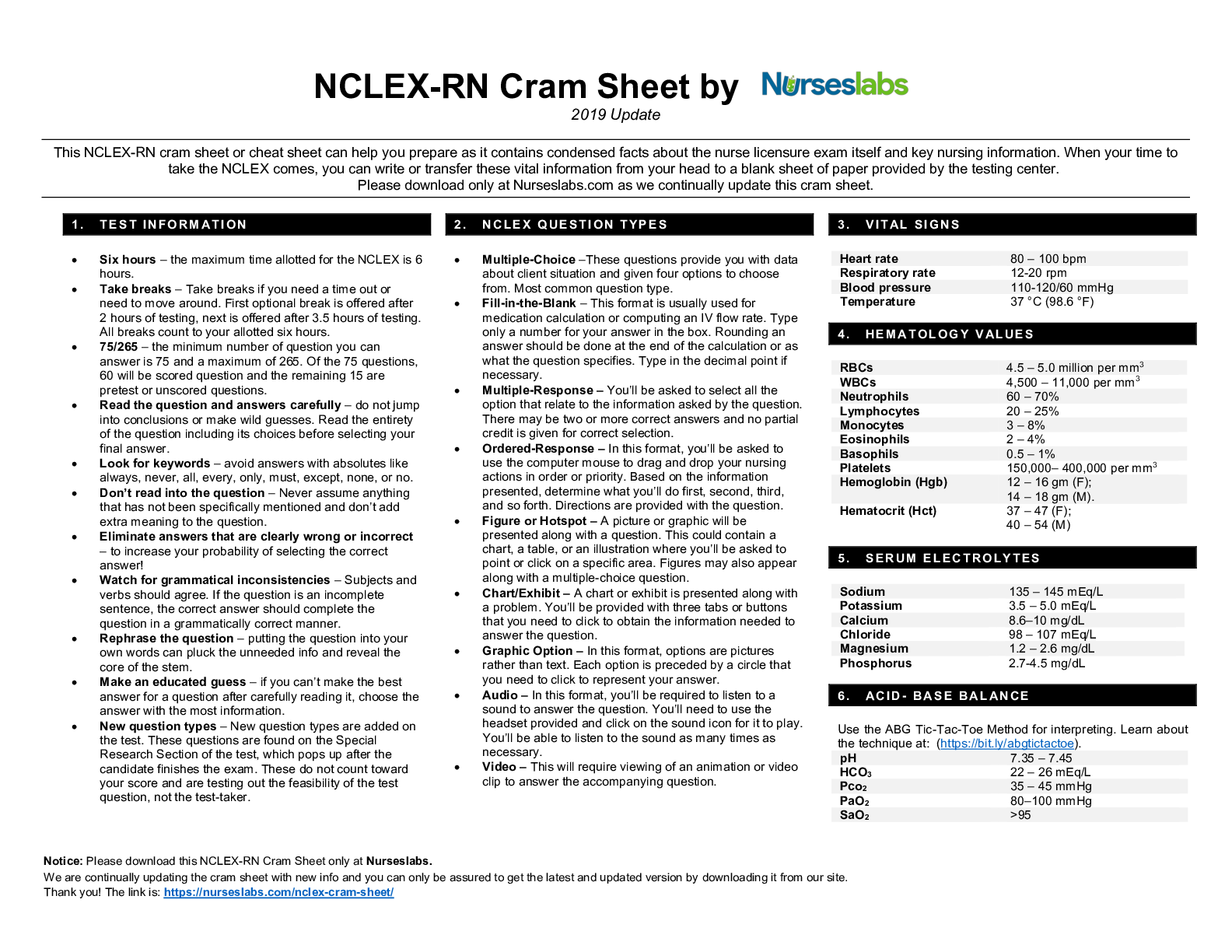
NCLEX-RN Cram Sheet by 2019 Update: This NCLEX-RN cram sheet or cheat sheet can help you prepare as it contains condensed facts about the nurse licensure exam itself and key nursing information:
We are continually updating the cram sheet with new info and you can only be assured to get the latest and updated version by downloading it from our site. This NCLEX-RN cram sheet or cheat sheet...
By Kirsch , Uploaded: Jun 05, 2020
$5
*NURSING> Manual > AB 1432 – California Educator Mandated Reporter Training (All)
AB 1432 – California Educator Mandated Reporter Training
The Child Abuse Mandated Reporter Training California website team worked with the California Department of Social Services and the California Department of Education to develop a new online trainin...
By Kirsch , Uploaded: May 02, 2020
$9
Finance> Manual > ISACA CISA Review Manual 27th Edition (All)

ISACA CISA Review Manual 27th Edition
Chapter 1: Information System Auditing Process Overview Domain 1 Exam Content Outline Learning Objectives/Task Statements Suggested Resources for Further Study Self-assessment Questions Answers to...
By Stuvia , Uploaded: Aug 01, 2022
$13.5
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2020
Number of pages
207
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2020
Downloads
0
Views
404






