*NURSING > SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 9 discussion: SOAP NOTE Case Study #3. (All)
Walden University - NURSING: NURS6512 Health Assessment Week 9 discussion: SOAP NOTE Case Study #3. Graded A. SOAP NOTE
Document Content and Description Below
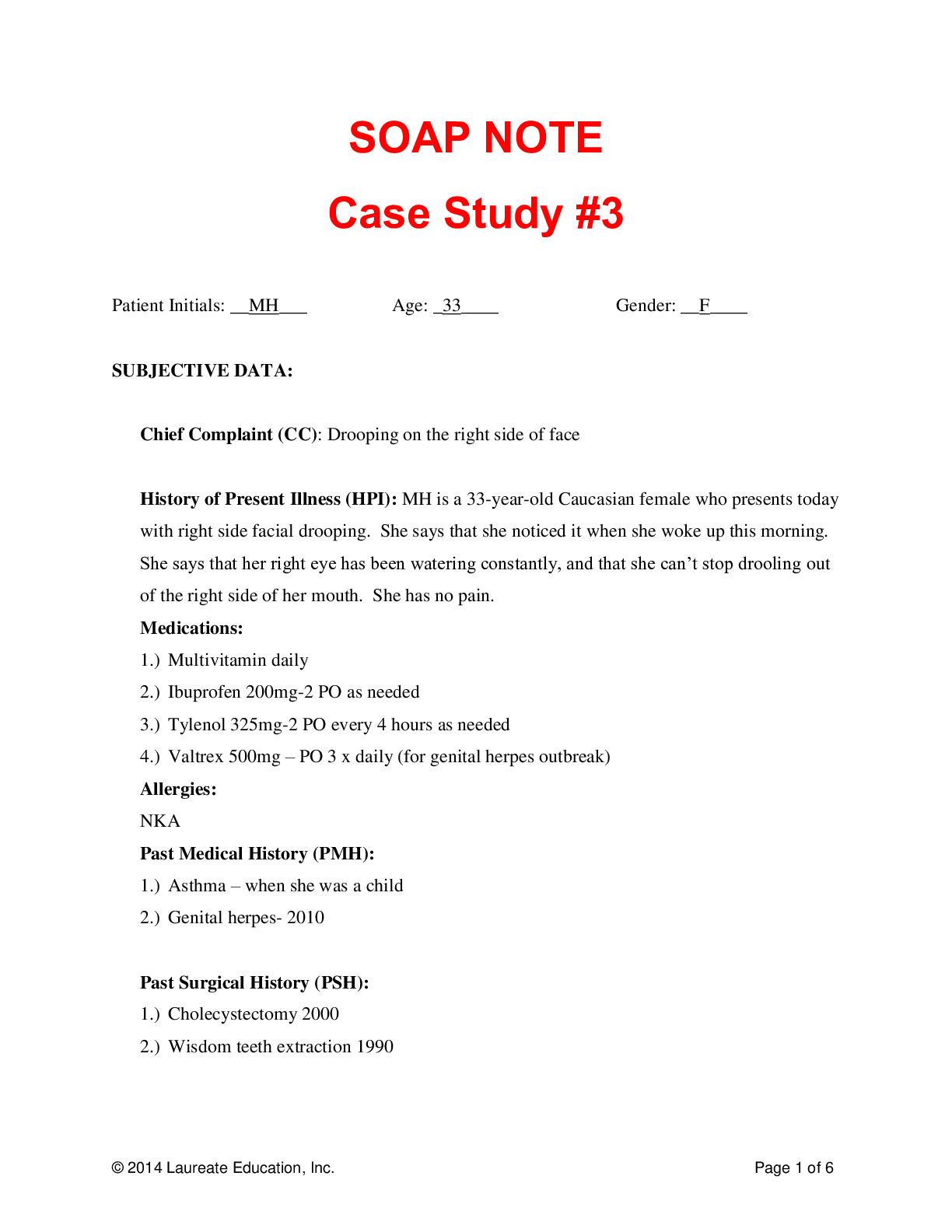
SOAP NOTE Case Study #3 Patient Initials: __MH___ Age: _33____ Gender: __F____ SUBJECTIVE DATA: Chief Complaint (CC): Drooping on the right side of face History of Present Illness (H... PI): MH is a 33-year-old Caucasian female who presents today with right side facial drooping. She says that she noticed it when she woke up this morning. She says that her right eye has been watering constantly, and that she can’t stop drooling out of the right side of her mouth. She has no pain. Medications: 1.) Multivitamin daily 2.) Ibuprofen 200mg-2 PO as needed 3.) Tylenol 325mg-2 PO every 4 hours as needed 4.) Valtrex 500mg – PO 3 x daily (for genital herpes outbreak) Allergies: NKA Past Medical History (PMH): 1.) Asthma – when she was a child 2.) Genital herpes- 2010 Past Surgical History (PSH): 1.) Cholecystectomy 2000 2.) Wisdom teeth extraction 1990 Sexual/Reproductive History: Heterosexual G1P1A0 Menarche age 13, cycles q 28-30, flow: 5-6 days. Mild dysmenorrhea; responds to ibuprofen. Last PAP 2 years ago and normal. Personal/Social History: She drinks occasionally; denied denies smoking or illicit drug use. Immunization History: Her immunizations are up to date. She received the influenza vaccine last October, and had a tetanus shot two years ago when she cut her arm on a piece of metal. Significant Family History: One brothers with hypertension, dx at age 50. She has one son in her 20s, healthy, living at home. Lifestyle: She is divorced and lives alone with her daughter in a nice neighborhood with a low crime rate. She does not exercise daily but says she takes her dog for a short walk daily. She has a primary care nurse practitioner provider and goes for her yearly checkups and when she is sick. She had a PAP smear done two years ago. She has not had a mammogram, but says she does monthly self-exams. She has a healthy diet and eating pattern. She has a good support system composed of family and friends. Review of Systems: [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 10 discussion: SOAP NOTE Case Study #3. Graded A. SOAP NOTE (All)
Walden University - NURSING: NURS6512 Health Assessment Week 10 discussion: SOAP NOTE Case Study #3. Graded A. SOAP NOTE
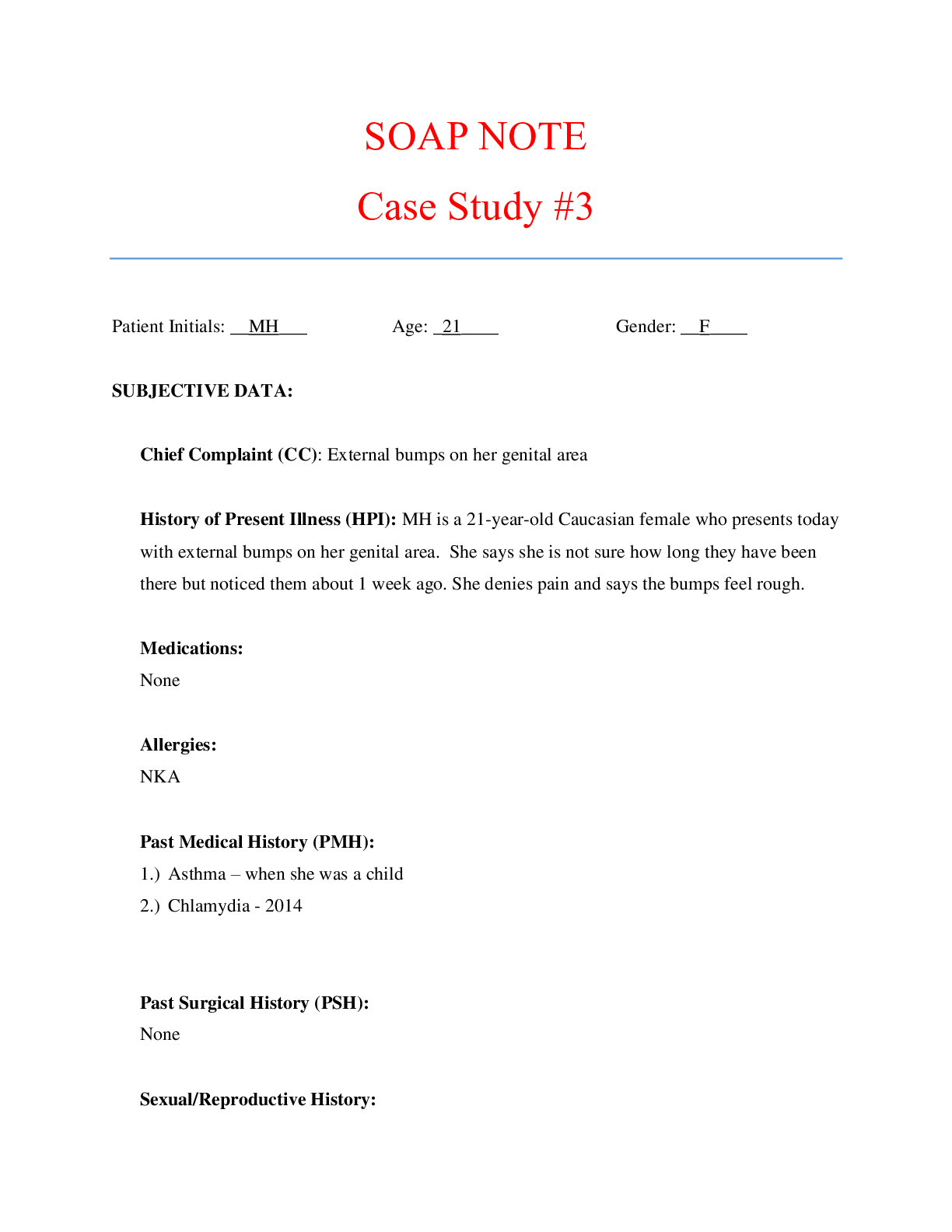
Case Study #3 Patient Initials: __MH___ Age: _21____ Gender: __F____ SUBJECTIVE DATA: Chief Complaint (CC): External bumps on her genital area History of Present Illness (HPI): MH is a...
By QuizMaster , Uploaded: Jul 29, 2020
$9.5
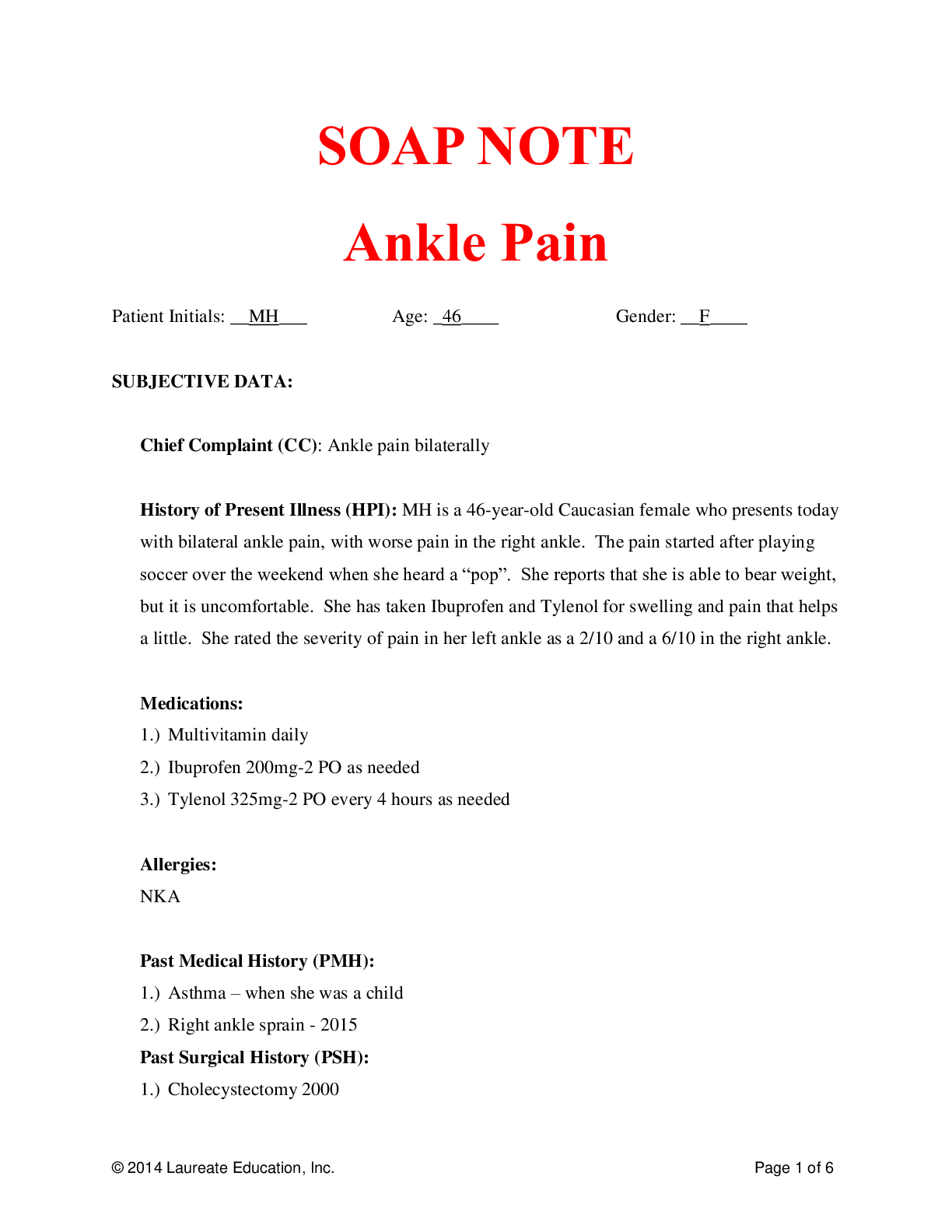
*NURSING> SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 8 discussion: SOAP NOTE Case Study Ankle Pain. Graded A. SOAP NOTE (All)
Walden University - NURSING: NURS6512 Health Assessment Week 8 discussion: SOAP NOTE Case Study Ankle Pain. Graded A. SOAP NOTE
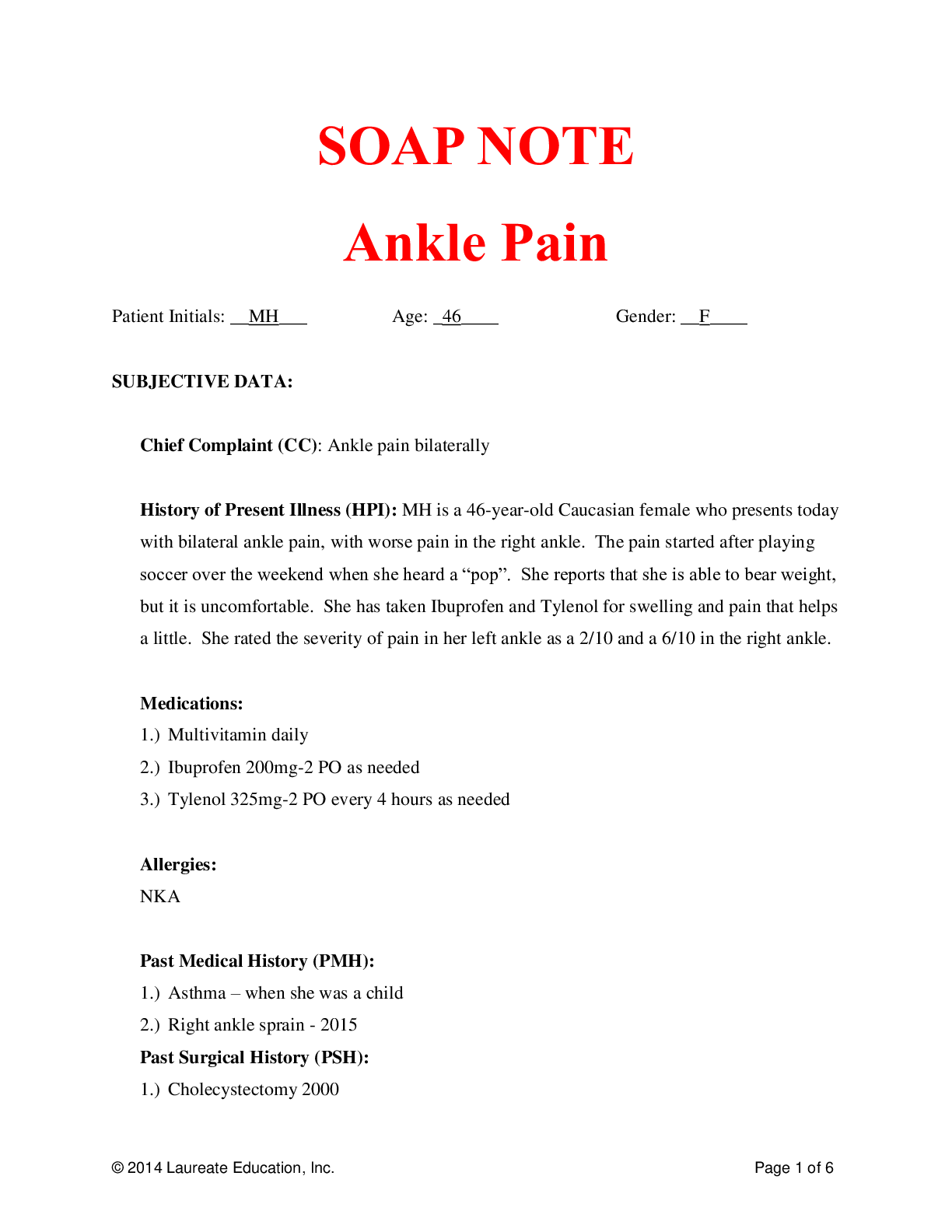
SOAP NOTE Ankle Pain Patient Initials: __MH___ Age: _46____ Gender: __F____ SUBJECTIVE DATA: Chief Complaint (CC): Ankle pain bilaterally History of Present Illness (HPI): MH is a 46-y...
By QuizMaster , Uploaded: Jul 29, 2020
$10.5
*NURSING> SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 7 discussion: Case Study: Vomiting X 3 and nausea over 48 hours. Graded A. SOAP NOTE (All)
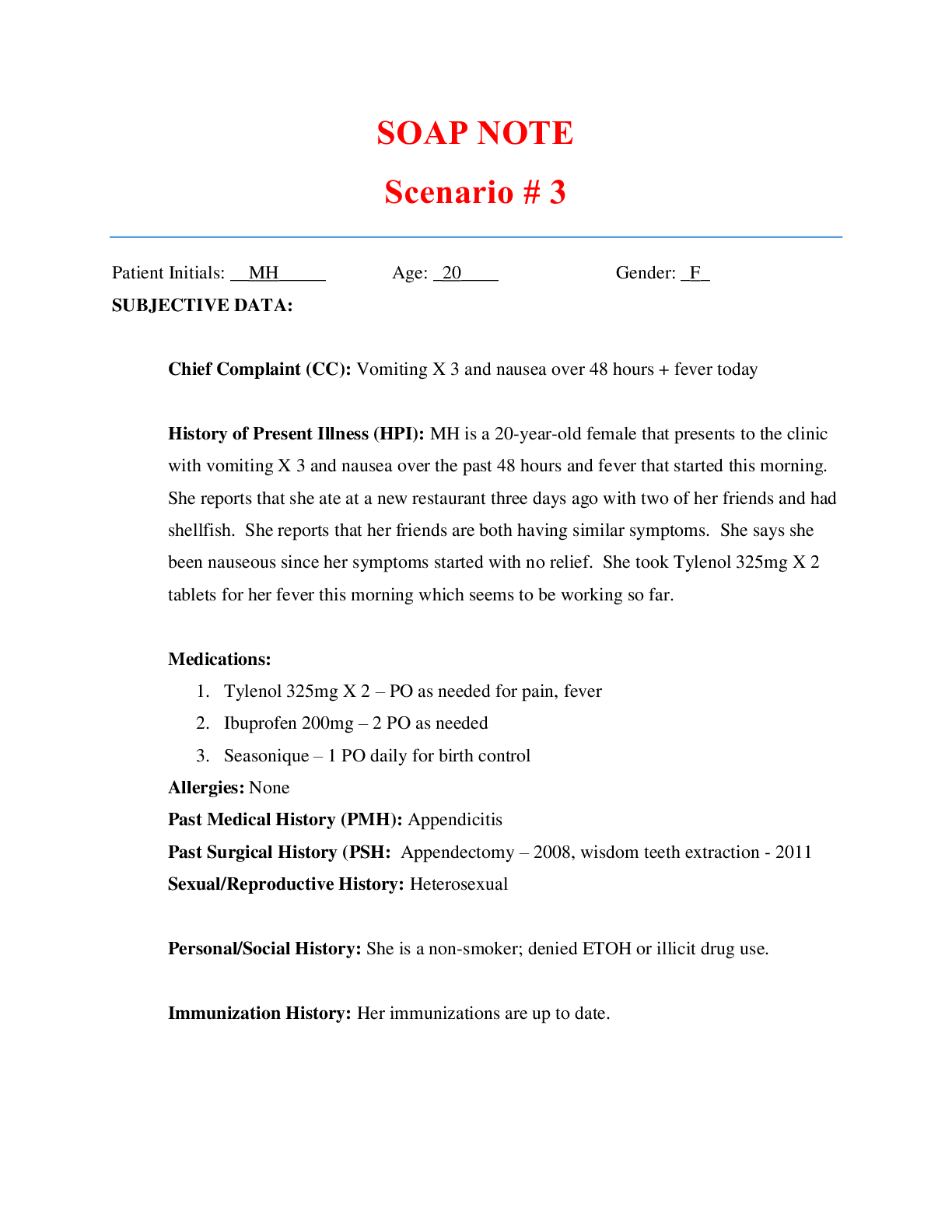
Walden University - NURSING: NURS6512 Health Assessment Week 7 discussion: Case Study: Vomiting X 3 and nausea over 48 hours. Graded A. SOAP NOTE
SOAP NOTE Scenario # 3 Patient Initials: __MH_____ Age: _20____ Gender: _F_ SUBJECTIVE DATA: Chief Complaint (CC): Vomiting X 3 and nausea over 48 hours + fever today History of Present Il...
By QuizMaster , Uploaded: Jul 29, 2020
$9.5
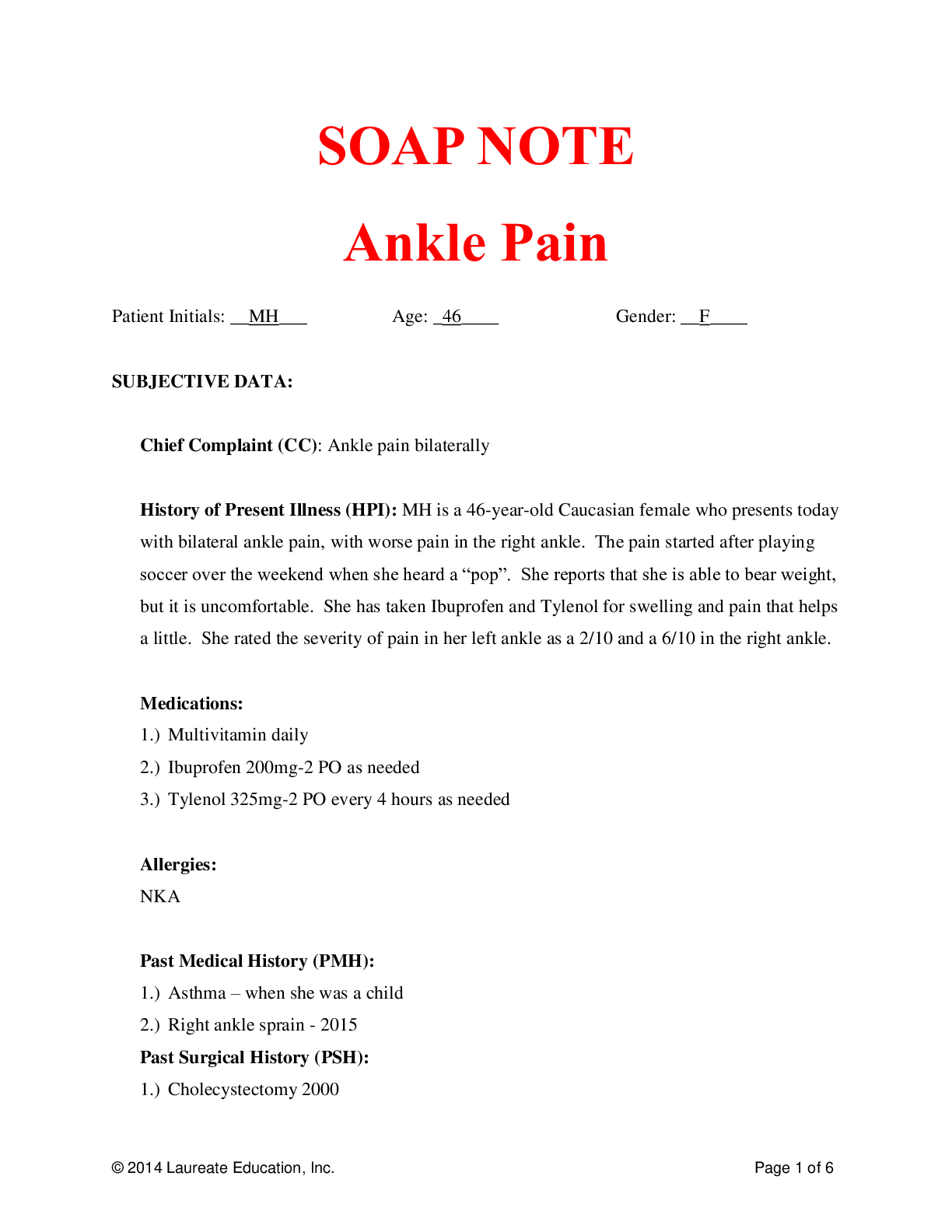
*NURSING> SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 8 discussion: SOAP NOTE Case Study Ankle Pain. Graded A. SOAP NOTE (All)
Walden University - NURSING: NURS6512 Health Assessment Week 8 discussion: SOAP NOTE Case Study Ankle Pain. Graded A. SOAP NOTE
SOAP NOTE Ankle Pain Patient Initials: __MH___ Age: _46____ Gender: __F____ SUBJECTIVE DATA: Chief Complaint (CC): Ankle pain bilaterally History of Present Illness (HPI): MH is a 46-y ear-old Caucasi...
By STUDY-GUIDENOTES , Uploaded: Aug 12, 2021
$8
*NURSING> SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 8 discussion: SOAP NOTE Case Study Ankle Pain. Graded A. SOAP NOTE (All)
Walden University - NURSING: NURS6512 Health Assessment Week 8 discussion: SOAP NOTE Case Study Ankle Pain. Graded A. SOAP NOTE
SOAP NOTE Ankle Pain Patient Initials: __MH___ Age: _46____ Gender: __F____ SUBJECTIVE DATA: Chief Complaint (CC): Ankle pain bilaterally History of Present Illness (HPI): MH is a 46-y ear-old Caucasi...
By A-PLUS GUIDENOTES , Uploaded: Aug 12, 2021
$8
*NURSING> SOAP NOTE > Walden University - NURSING: NURS6512 Health Assessment Week 6 discussion: Case Study: Chest pain, and SOB.. Graded A. SOAP NOTE (All)
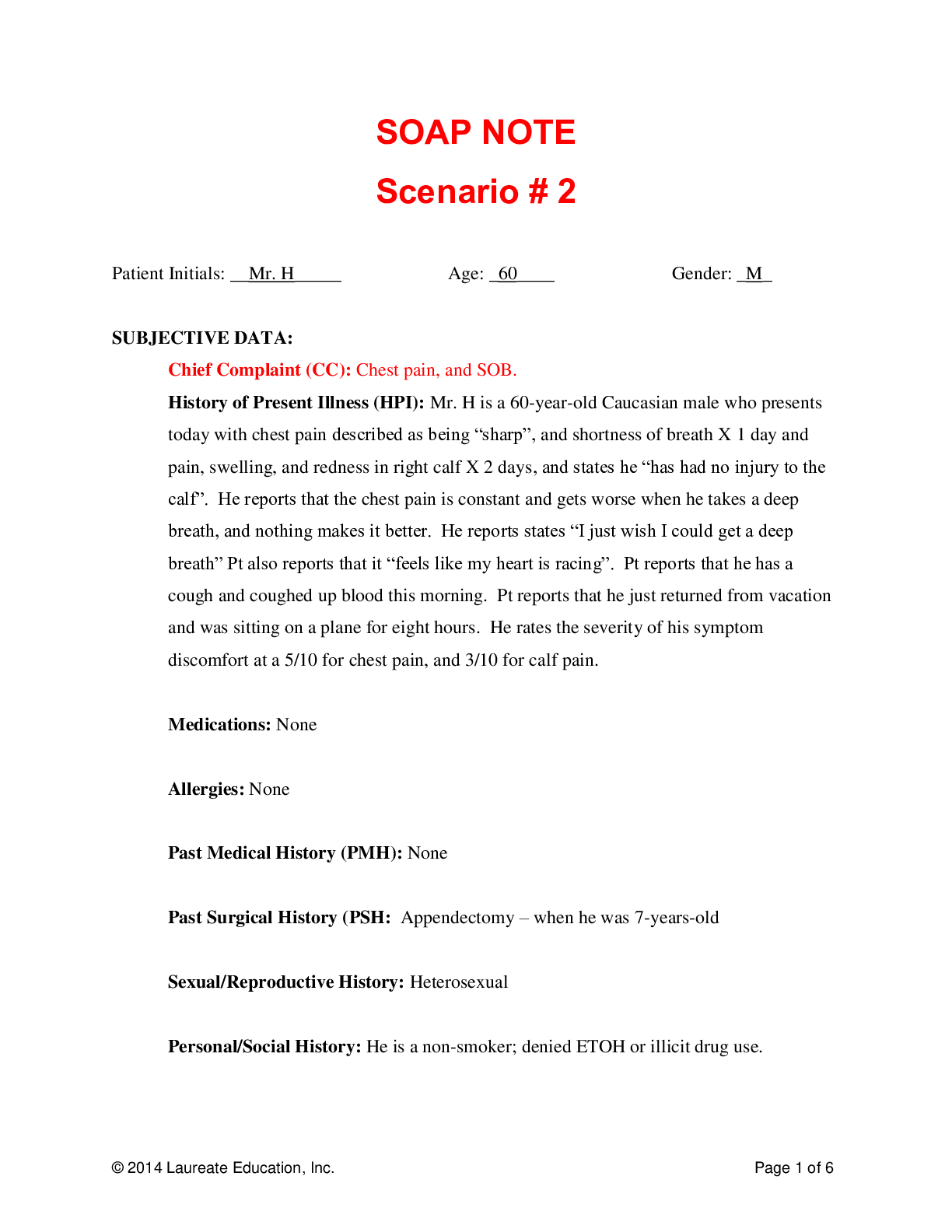
Walden University - NURSING: NURS6512 Health Assessment Week 6 discussion: Case Study: Chest pain, and SOB.. Graded A. SOAP NOTE
SOAP NOTE Scenario # 2 Patient Initials: __Mr. H_____ Age: _60____ Gender: _M_ SUBJECTIVE DATA: Chief Complaint (CC): Chest pain, and SOB. History of Present Illness (HPI): Mr. H is a 60-y...
By QuizMaster , Uploaded: Jul 29, 2020
$7
*NURSING> SOAP NOTE > NRP 531Tom Walker, Episodic SOAP Note: Already graded A. (All)
NRP 531Tom Walker, Episodic SOAP Note: Already graded A.
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A.
By Expert1 , Uploaded: Jul 18, 2020
$10
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
Health Care> SOAP NOTE > SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions” (All)
SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions”
HPI: Mr. Fitzgerald is a 66-year-old male who presents via telehealth for a routine follow up on his chronic heart failure. He provided verbal consent for this telehealth visit. Mr. Fitzgerald repor...
By STUDY-GUIDENOTES , Uploaded: Oct 05, 2022
$7
Health Care> SOAP NOTE > Caroline Casey SOAP (All)
Caroline Casey SOAP
Caroline Casey SOAP
By Ellen Ronald , Uploaded: Jul 29, 2022
$8
Document information
Connected school, study & course
About the document
Uploaded On
Jul 29, 2020
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Jul 29, 2020
Downloads
0
Views
540