*NURSING > SOAP NOTE > Tina jones (T.J). SOAP Note Template. Contains Subjective informations; History of Present Illness (All)
Tina jones (T.J). SOAP Note Template. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS);
Document Content and Description Below
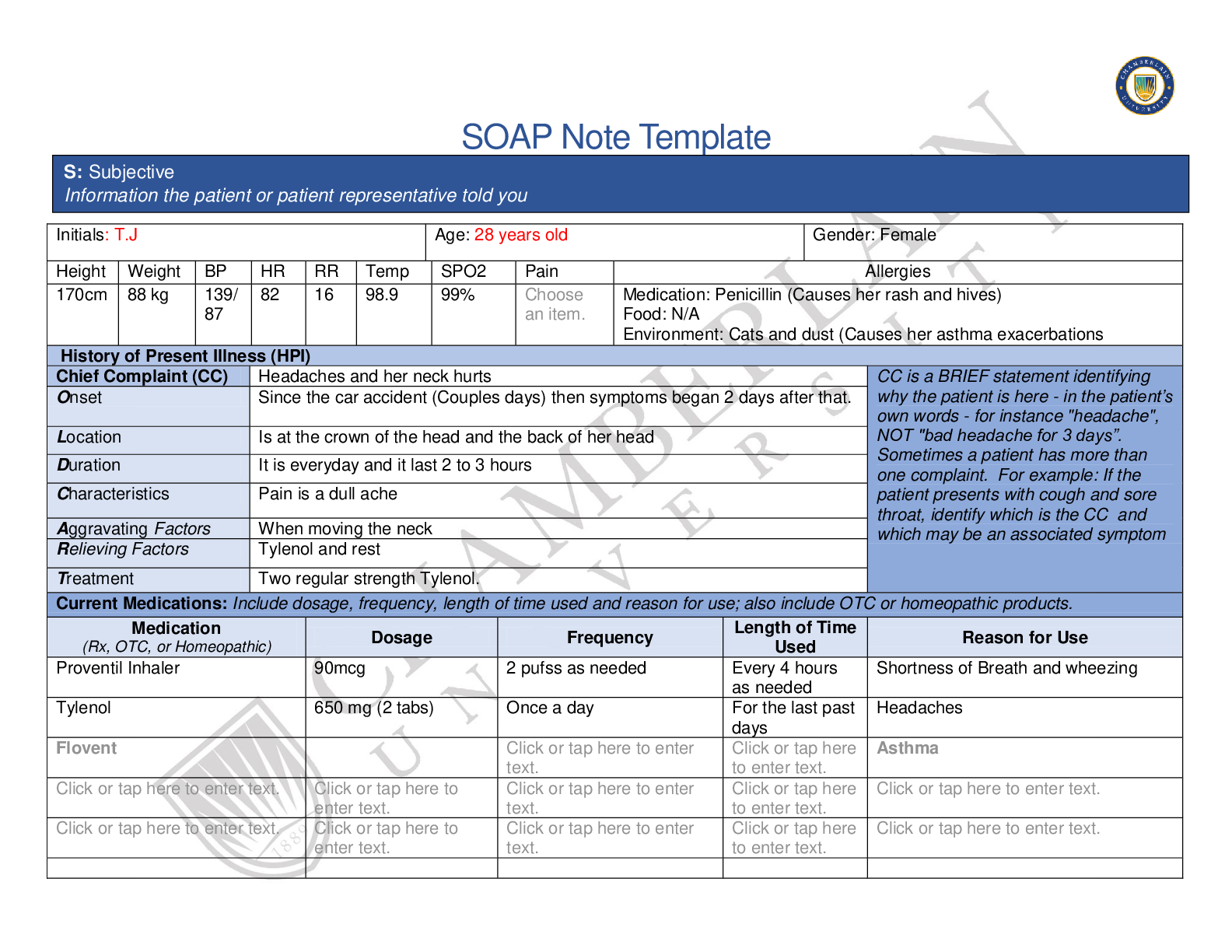
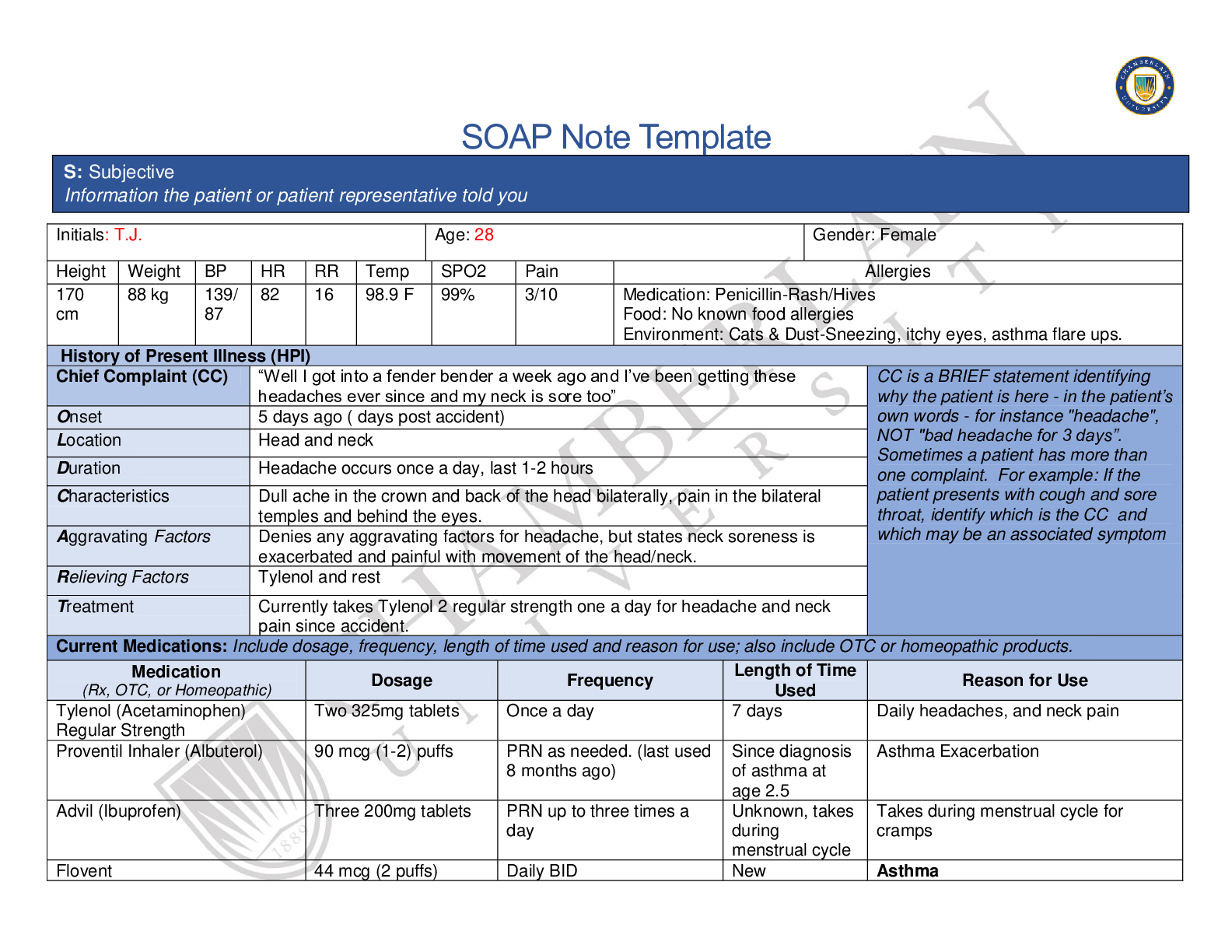
SOAP Note Template Initials: T.J Age: 28 years old Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 88 kg 139/ 87 82 16 98.9 99% Choose an item. Medication: Penicillin (Caus... es her rash and hives) Food: N/A Environment: Cats and dust (Causes her asthma exacerbations History of Present Illness (HPI) Chief Complaint (CC) Headaches and her neck hurts CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset Since the car accident (Couples days) then symptoms began 2 days after that. Location Is at the crown of the head and the back of her head Duration It is everyday and it last 2 to 3 hours Characteristics Pain is a dull ache Aggravating Factors When moving the neck Relieving Factors Tylenol and rest Treatment Two regular strength Tylenol. Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Proventil Inhaler 90mcg 2 pufss as needed Every 4 hours as needed Shortness of Breath and wheezing Tylenol 650 mg (2 tabs) Once a day For the last past days Headaches O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If unable to assess a body system, write “Unable to assess”. Document pertinent positive and negative assessment findings A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis. P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. Crain Ian, Hoskin Justin, Al-Hasan Yazan, Zieman Glynnis, Cardenas Javie (Dec 2018) Early prophylactic treatment reduces development of chronic post traumatic headache after concussion. (23 Supplement 1) S29; DOI: 10.1212/01.wnl.0000550646.79759.e1 Defrin R. (2014). Chronic post-traumatic headache: clinical findings and possible mechanisms. The Journal of manual & manipulative therapy, 22(1), 36–44. doi:10.1179/2042618613Y.0000000053 [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Recommended For You
*NURSING> SOAP NOTE > Tina jones (T.J) Neurology. SOAP Note Template. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS). (All)
Tina jones (T.J) Neurology. SOAP Note Template. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS).
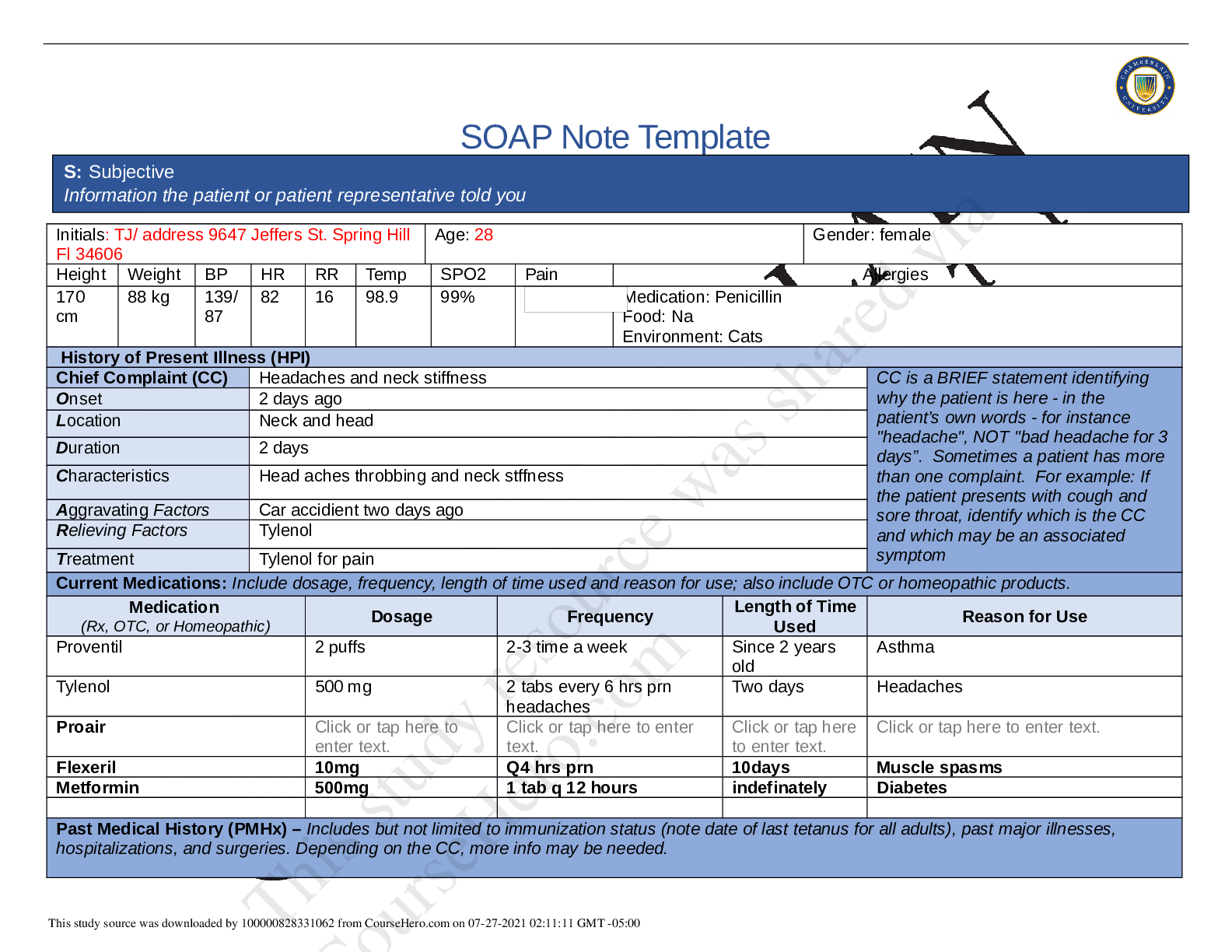
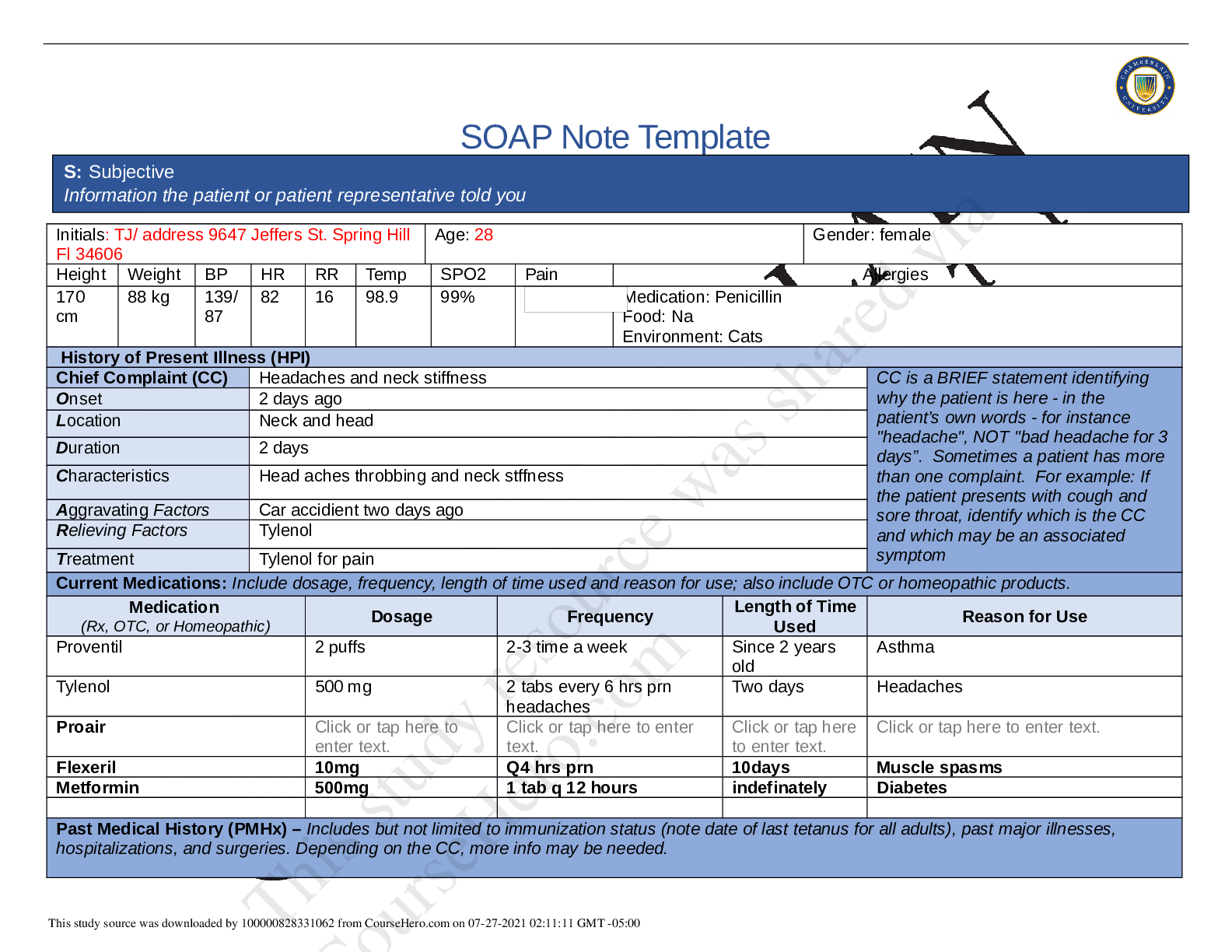
SOAP Note Template Initials: TJ/ address 9647 Jeffers St. Spring Hill Fl 34606 Age: 28 Gender: female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 88 kg 139/ 87 82 16 98.9 99% 3/10...
By QuizMaster , Uploaded: Aug 18, 2020
$8.5
*NURSING> SOAP NOTE > Tina jones (T.J) . SOAP Note week 2. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS). (All)
Tina jones (T.J) . SOAP Note week 2. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS).
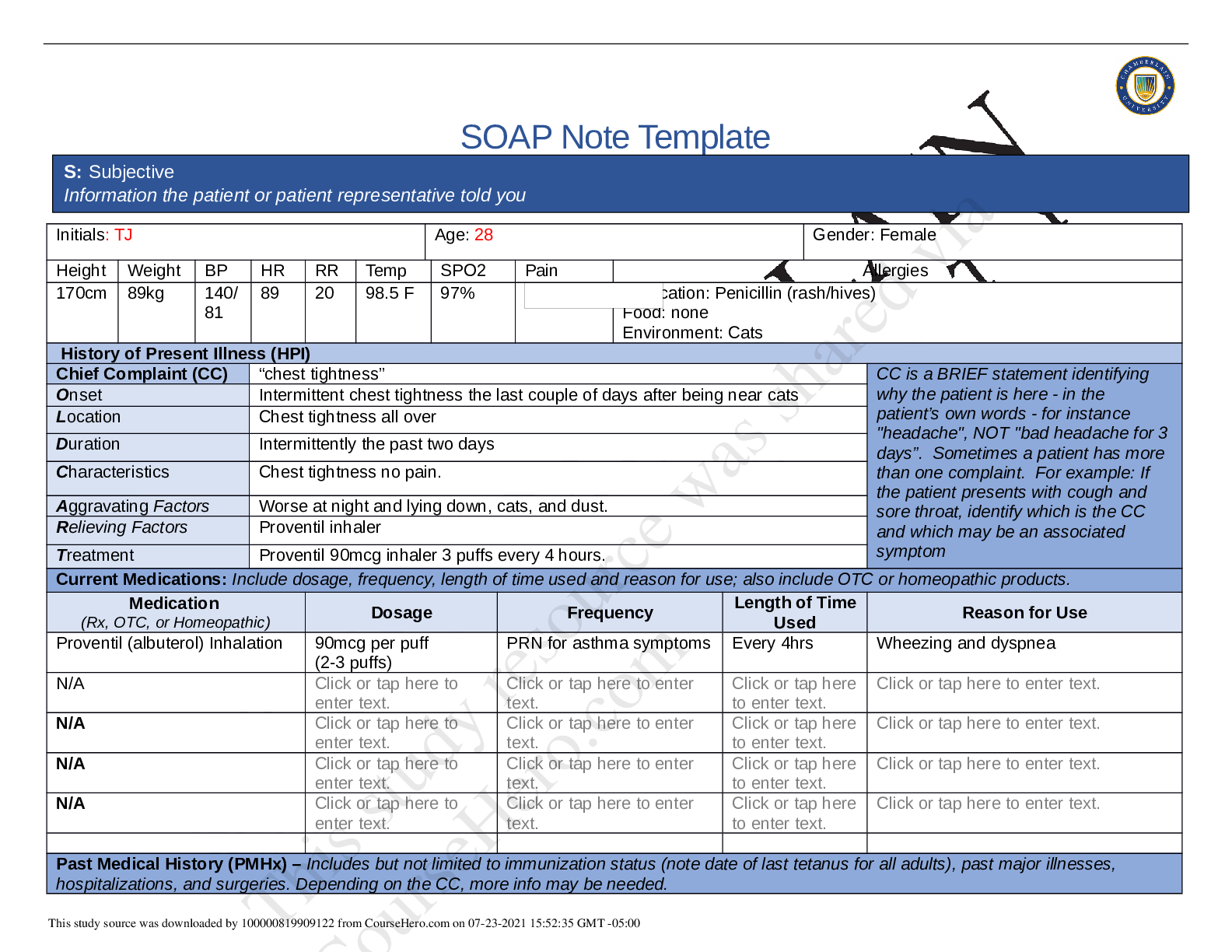
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170cm 89kg 140/ 81 89 20 98.5 F 97% Choose an item. Medication: Penicillin (rash/hives) F...
By QuizMaster , Uploaded: Aug 18, 2020
$7.5
*NURSING> SOAP NOTE > Tina jones (T.J) . SOAP Note week 3 Neuro. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS). (All)
Tina jones (T.J) . SOAP Note week 3 Neuro. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS).
Tina jones (T.J) . SOAP Note week 3 Neuro. Contains Subjective informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Syst...
By PROF , Uploaded: Jan 23, 2021
$7
*NURSING> SOAP NOTE > Chamberlain University_Tina jones -T.J- . SOAP Note Template Week 3 Neuro. Subjective Informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS). (All)
Chamberlain University_Tina jones -T.J- . SOAP Note Template Week 3 Neuro. Subjective Informations; History of Present Illness (HPI); Current Medications; Past Medical History (PMHx); Family History (Fam Hx); Review of Systems (ROS).
SOAP Note Template Initials: T.J. Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 88 kg 139/ 87 82 16 98.9 F 99% 3/10 Medication: Penicillin-Rash/Hives Food: No k nown fo...
By QuizMaster , Uploaded: Mar 11, 2023
$9
*NURSING> SOAP NOTE > NRP 531Tom Walker, Episodic SOAP Note: Already graded A. (All)
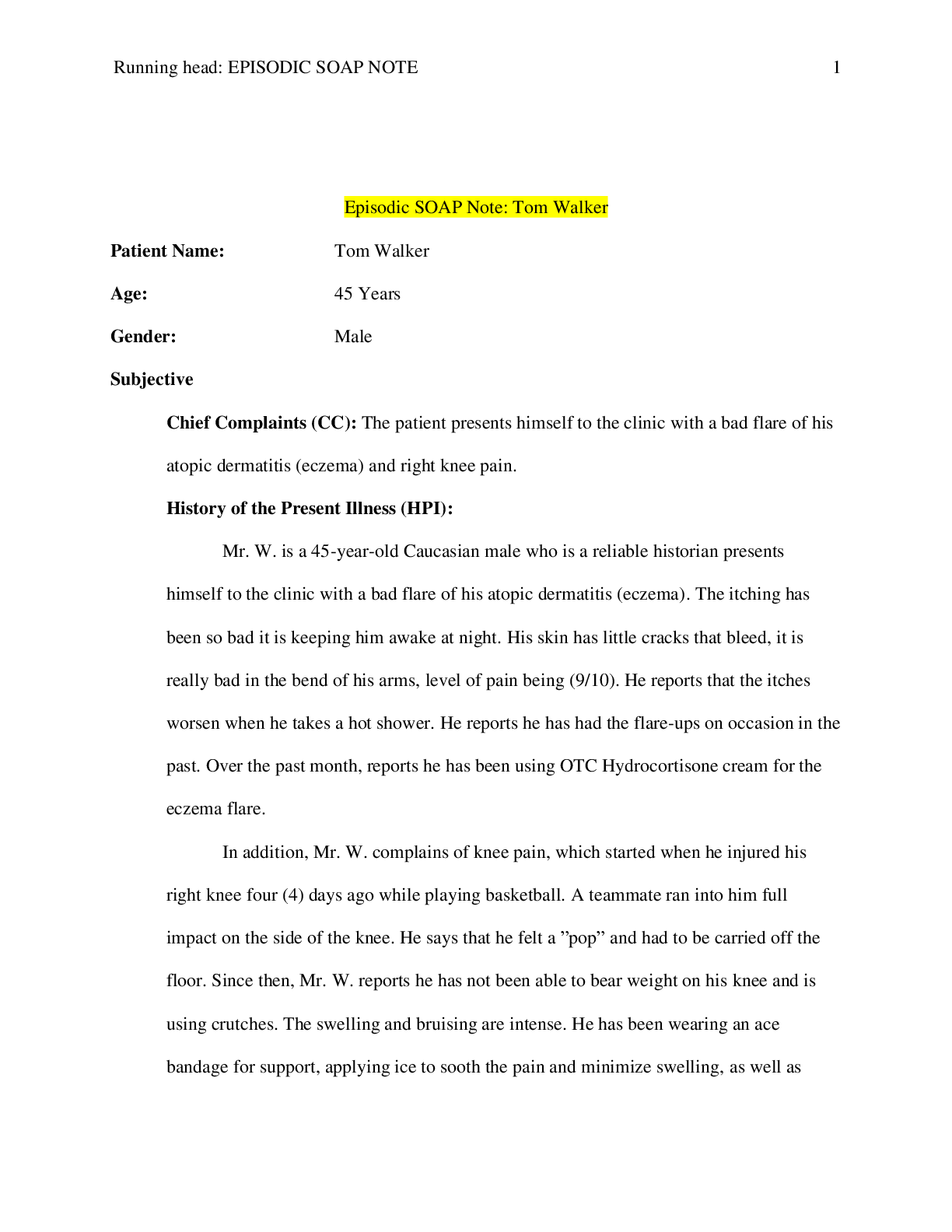
NRP 531Tom Walker, Episodic SOAP Note: Already graded A.
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A.
By Expert1 , Uploaded: Jul 18, 2020
$10
*NURSING> SOAP NOTE > NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A (All)
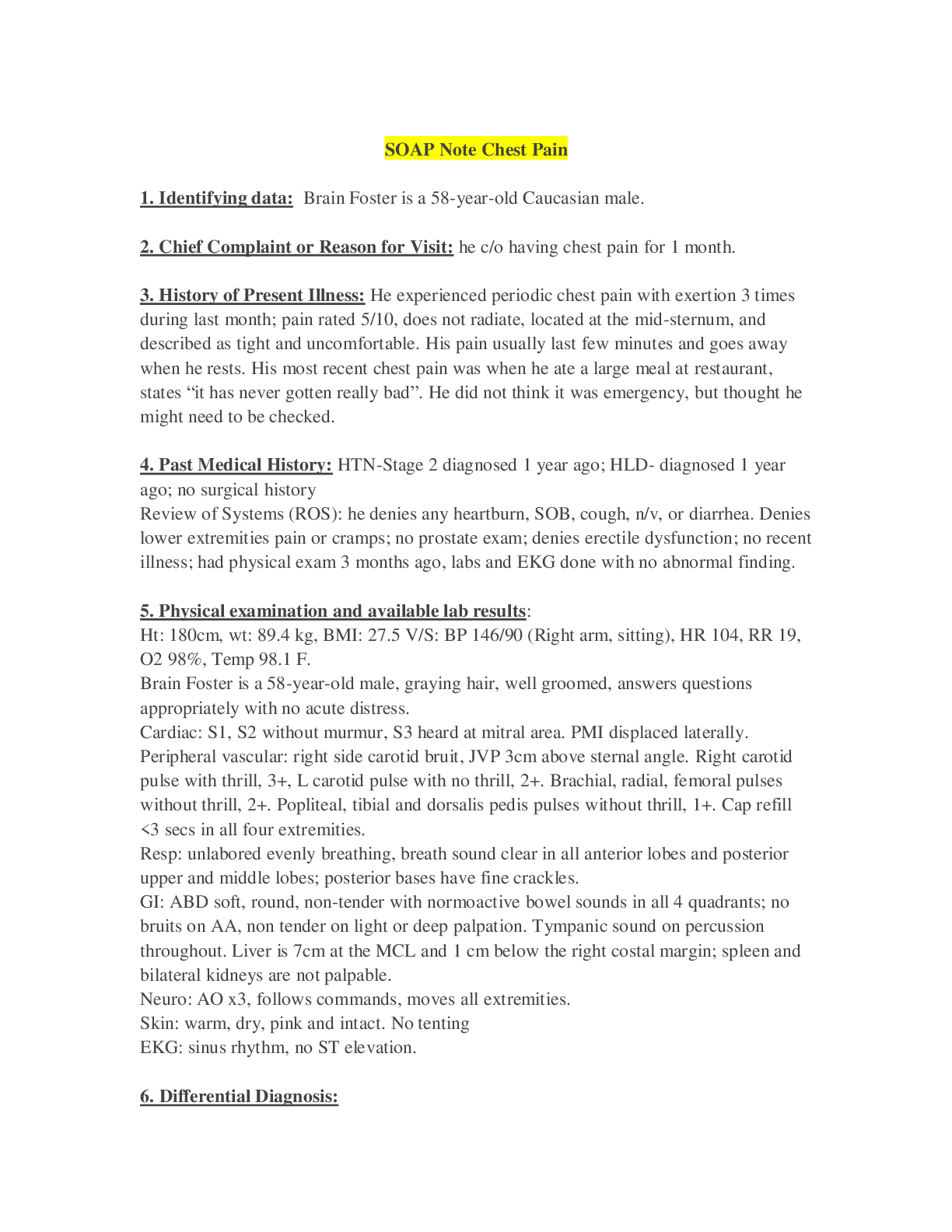
NURS 112 SOAP Note Chest Pain Pennsylvania State University -Download To Score An A
SOAP Note Chest Pain 1. Identifying data: Brain Foster is a 58-year-old Caucasian male. 2. Chief Complaint or Reason for Visit: he c/o having chest pain for 1 month. 3. History...
By Succeed , Uploaded: Aug 03, 2020
$9.5
Health Care> SOAP NOTE > SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions” (All)
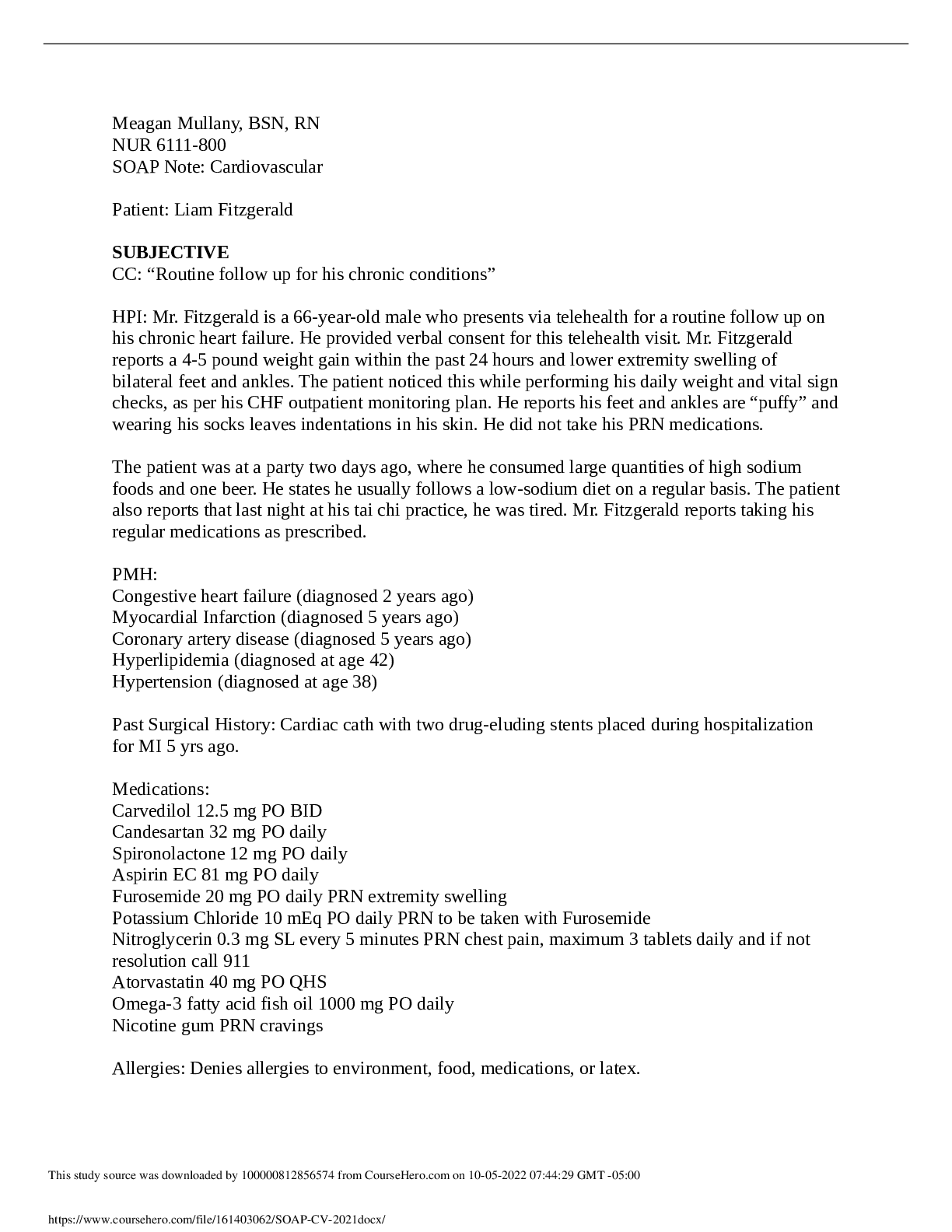
SOAP Note: Cardiovascular Patient: Liam Fitzgerald SUBJECTIVE CC: “Routine follow up for his chronic conditions”
HPI: Mr. Fitzgerald is a 66-year-old male who presents via telehealth for a routine follow up on his chronic heart failure. He provided verbal consent for this telehealth visit. Mr. Fitzgerald repor...
By STUDY-GUIDENOTES , Uploaded: Oct 05, 2022
$7
Health Care> SOAP NOTE > Caroline Casey SOAP (All)
Caroline Casey SOAP
Caroline Casey SOAP
By Ellen Ronald , Uploaded: Jul 29, 2022
$8
Health Care> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2019/ 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By MARKALLAN , Uploaded: Jul 20, 2022
$9
*NURSING> SOAP NOTE > Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A (All)
Episodic SOAP Note: Tom Walker|NRP 531,Latest 2020 complete, Already graded A
Running head: EPISODIC SOAP NOTE: TOM WALKER 1 Episodic SOAP Note: Tom Walker NRP 531 2021 Professor Sandra Brown EPISODIC SOAP NOTE: TOM WALKER 2 DOS: 4/15/2019 ID: Tom Walker (M) DOB: 6/28/73 (45) C...
By Prof.Pierro , Uploaded: Jul 20, 2022
$9
Document information
Connected school, study & course
About the document
Uploaded On
Aug 18, 2020
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Aug 18, 2020
Downloads
1
Views
301






