*NURSING > QUESTIONS & ANSWERS > NUR 3463 (exam 2) ADULT HEALTH ACUTE CARE | GRADED A | QUESTIONS AND ANSWER KEY PROVIDED (All)
NUR 3463 (exam 2) ADULT HEALTH ACUTE CARE | GRADED A | QUESTIONS AND ANSWER KEY PROVIDED
Document Content and Description Below
NUR 3463 (exam 2) ADULT HEALTH ACUTE CARE | GRADED A | QUESTIONS AND ANSWER KEY PROVIDED Chapter 21 cancer development. 1. The nurse is giving a group presentation on cancer prevention and reco... gnition. Which statement by an older adult client indicates understanding of the nurse's instructions? A "Cigarette smoking always causes lung cancer." B "Taking multivitamins will prevent me from developing cancer." C "If I have only one shot of whiskey a day, I probably will not develop cancer." D "I need to report the pain going down my legs to my health care provider." ANS: D Pain in the back of the legs could indicate prostate cancer in an older man. Cigarette smoking is implicated in causing lung cancer and other types of cancer, but it does not always cause cancer. Investigation is ongoing about the efficacy of vitamins A and C in cancer prevention. Limiting alcohol to one drink per day is only one preventive measure. 2. The nurse is teaching a 47-year-old woman about recommended screening practices for breast cancer. Which statement by the client indicates understanding of the nurse's instructions? A "My mother and grandmother had breast cancer, so I am at risk." B "I get a mammogram every 2 years since I turned 30." C "A clinical breast examination is performed every month since I turned 40." D "A computed tomography (CT) scan will be done every year after I turn 50." ANS: A A strong family history of breast cancer indicates a risk for breast cancer. Annual rather than biannual screening may be indicated for a strong family history. An annual mammogram is performed after age 40 or in younger clients with a strong family history. The client may perform a self-breast examination monthly; a clinical examination by a health care provider is indicated annually. Annual CT breast scans after age 50 are not a current recommendation. 3. A 72-year-old client recovering from lung cancer surgery asks the nurse to explain how she developed cancer when she has never smoked. Which factor may explain the possible cause? A A diagnosis of diabetes treated with insulin and diet B An exercise regimen of jogging 3 miles four times a week C A history of cardiac disease D Advancing age ANS: D Advancing age is the single most important risk factor for cancer. As a person ages, immune protection decreases. Diabetes is not known to cause lung cancer. Regular exercise is not a risk factor for lung cancer, nor does having cardiac disease predispose a person to lung cancer. 4. The nurse reviews the chart of a client admitted with a diagnosis of glioblastoma with a T1NXM0 classification. Which explanation does the nurse offer when the client asks what the terminology means? A "Two lymph nodes are involved in this tumor of the glial cells, and another tumor is present." B "The brain tumor measures about 1 to 2 cm and shows no regional lymph nodes and no distant metastasis." C "This type of tumor in the brain is small with some lymph node involvement; another tumor is present somewhere else in your body." D "Glioma means this tumor is benign, so I will have to ask your health care provider the reason for the chemotherapy and radiation." ANS: B T1 means that the tumor is increasing in size to about 2 cm, and that no regional lymph nodes are present in the brain. M0 means that no distant metastasis has occurred. NX means that no regional lymph nodes can be assessed. A glioma is a benign tumor of the brain, but the client is diagnosed with a glioblastoma, which means a malignant tumor of the glial cells of the brain. 5. The nurse manager in a long-term care facility is developing a plan for primary and secondary prevention of colorectal cancer. Which tasks associated with the screening plan will be delegated to nursing assistants within the facility? A Testing of stool specimens for occult blood B Teaching about the importance of dietary fiber C Referring clients for colonoscopy procedures D Giving vitamin and mineral supplements ANS: A Testing of stool specimens for occult blood is done according to a standardized protocol and can be delegated to nursing assistants. Client education is within the scope of practice of the RN, not of the LPN or nursing assistant. Referral for further care is best performed by the RN. Administration of medications is beyond the nursing assistant's scope of practice and should be done by licensed nursing personnel. 6. The nurse presents a cancer prevention program to teens. Which instruction will have the greatest impact in cancer prevention? A Avoid asbestos. B Wear sunscreen. C Get the human papilloma virus (HPV) vaccine. D Do not smoke cigarettes. ANS: D All of these actions are part of cancer prevention; however, tobacco is the single most important source of preventable carcinogenesis. Asbestos may be found in older homes and buildings. Most schools have been through an asbestos abatement program so should not pose a risk. It would be important to share with teens who may be involved in the construction industry during the summer to be aware of asbestos risks. Although asbestos may present a risk for lung cancer, it is not a likely exposure for teens. Lifetime exposure to the sun and the use of tanning beds will increase the risk for cancer, but not as much as tobacco use. The HPV vaccine will decrease the risk for cervical cancer, but will not have as much of an impact on cancer prevention as avoiding tobacco. 7. The nurse suspects metastasis from left breast cancer to the thoracic spine when the client has which symptom? A Vomiting B Back pain C Frequent urination D Cyanosis of the toes ANS: B Typical sites of breast cancer metastasis include bone (manifested by back pain), lung, liver, and brain. Signs of metastasis to the spine may include numbness, pain, paresthesias and tingling, and loss of bowel and bladder control, but not vomiting. Although frequent urination may be a sign of bladder cancer, incontinence is more indicative of spinal metastasis. Cyanosis of the toes indicates decreased tissue perfusion, often related to atherosclerotic disease. 8. The nurse explains to a client that which risk factor of those listed most likely contributed to the client's primary liver carcinoma? A Infection with hepatitis B virus B Consuming a diet high in animal fat C Exposure to radon D Familial polyposis ANS: A Hepatitis B and C are risk factors for primary liver cancer. Alcohol abuse is also a risk factor for the development of liver cancer. Consuming a diet high in animal fat may predispose a person to colon or breast cancer. Exposure to radon is a risk factor for lung cancer. Familial polyposis is a risk factor for colorectal cancer. 9. Which type of cancer has been associated with Down syndrome? A Breast cancer B Colorectal cancer C Malignant melanoma D Leukemia ANS: D Leukemia is associated with Down syndrome and Turner syndrome. Breast cancer is often found clustered in families, not in association with Down syndrome. Colorectal cancer is associated with familial polyposis. Malignant melanoma is associated with familial clustering and sun exposure. 10. The nurse is assessing a client with lung cancer. Which symptom does the nurse anticipate finding? A Easy bruising B Dyspnea C Night sweats D Chest wound ANS: B Dyspnea is a sign of lung cancer, as are cough, hoarseness, shortness of breath, bloody sputum, arm or chest pain, and dysphagia. Easy bruising is a nonspecific finding. Night sweats is a symptom of the lymphomas. A chest wound is not specific to lung cancer. 11. Which activity performed by the community health nurse best reflects primary prevention of cancer? A Assisting women to obtain free mammograms B Teaching a class on cancer prevention C Encouraging long-term smokers to get a chest x-ray D Encouraging sexually active women to get annual Papanicolaou (Pap) smears ANS: B Primary prevention involves avoiding exposure to known causes of cancer; education assists clients with this strategy. Mammography is part of a secondary level of prevention, defined as screening for early detection. Chest x-ray is a method of detecting a cancer that is present—secondary prevention and early detection. A Pap smear is a means of detecting cervical cancer early—secondary prevention. 12. A 52-year-old client relates to the nurse that she has never had a mammogram because she is terrified that she will have cancer. Which response by the nurse is therapeutic? A "Don't worry, most lumps are discovered by women during breast self-examination." B "Does anyone in your family have breast cancer?" C "Finding a cancer in the early stages increases the chance for cure." D "Have you noticed a lump or thickening in your breast?" ANS: C Providing truthful information addresses the client's concerns. Mammography can detect lumps smaller than those discovered by palpation. Asking about family history or symptoms is not therapeutic because it does not address the client's fear of cancer. 13. Which information must the organ transplant nurse emphasize before a client is discharged? A "Taking immunosuppressant medications increases your risk for cancer and the need for screenings." B "You are at increased risk for cancer when you reach 60 years of age." C "Immunosuppressant medications will decrease your risk for developing cancers." D "After 6 months, you may stop immunosuppressant medications, and your risk for cancer will be the same as that of the general population." ANS: A Use of immunosuppressant medications to prevent organ rejection increases the risk for cancer. Advanced age is a risk factor for all people, not just for organ transplant recipients. Immunosuppressant medications must be taken for the life of the organ; the risk for developing cancer remains. 14. The home health nurse is caring for a client who has a history of a kidney transplant and takes cyclosporine (Sandimmune) and prednisone (Deltasone) to prevent rejection. Which assessment finding is most important to communicate to the transplant team? A Temperature of 96.6° F B Reports of joint pain C Pink and dry oral mucosa D Palpable lump in the client's axilla ANS: D Clients taking immunosuppressive drugs to prevent rejection are at increased risk for the development of cancer; any lump should be reported to the physician. Fever should be reported to the physician, but this client's temperature is normal. It is not necessary to report joint pain to the transplant team; it is not a sign of rejection and is not a complication of transplant. A pink and dry oral mucosa may be a sign of dehydration, but it is not necessary to report this to the transplant team. 15. A client who is scheduled to undergo radiation for prostate cancer is admitted to the hospital by the nurse. Which statement by the client is most important to communicate to the health care provider? A "I am allergic to iodine." B "My urinary stream is very weak." C "My legs are numb and weak." D "I am incontinent when I cough." ANS: C Numbness and weakness should be reported to the physician because paralysis caused by spinal cord compression can occur. Prostate cancer may frequently metastasize to the bone, specifically the spine. Allergy to iodine should be reported when contrast media will be used, but dye is not used in radiation therapy. A weak urinary stream and incontinence are common clinical manifestations of prostate cancer. Incontinence associated with coughing is typical of stress incontinence and is not a complication of cancer. 16. When the nurse is counseling a 60-year-old African-American male client with all of these risk factors for lung cancer, teaching should focus most on which risk factor? A Tobacco use B Ethnicity C Gender D Increased age ANS: A Although all of these are risk factors for lung cancer, the client's tobacco use is the only factor that he can change. Ethnicity, gender, and increasing age are associated with lung cancer, but they are not modifiable risks. 17. Which statement about the process of malignant transformation is correct? A Mutation of genes is an irreversible event that always leads to cancer development in the initiation phase. B Insulin and estrogen enhance the division of an initiated cell during the promotion phase. C Tumors form when carcinogens invade the gene structure of the cell in the latency phase. D Nutrition of cancer cells is provided by tumor angiogenesis factor (TAF) in the promotion stage. ANS: D The promotion phase consists of progression when the blood supply changes from diffusion to TAF.Insulin and estrogen increase cell division. If cell division is halted, mutation of genes does not lead to cancer development in the initiation phase. In the initiation phase, carcinogens invade the DNA of the nucleus of a single cell. A 1-cm tumor consists of 1 billion cells. The latency phase occurs between initiation and tumor formation. 18. A client has a glioblastoma. The nurse begins to plan care for this client with which type of cancer? A Liver B Smooth muscle C Fatty tissue D Brain ANS: D The prefix "glio-" is used when cancers of the brain are named. The prefix "hepato-" is included when cancers of the liver are named. The prefix "leiomyo-" is included when cancers of smooth muscle are named. The prefix "lipo-" is included when cancers of fat or adipose tissue are named. 19. A client has a diagnosis of lung cancer. To which areas does the nurse anticipate that this client's tumor may metastasize? (Select all that apply.) A Brain B Bone C Lymph nodes D Kidneys E Liver ANS: A, B, C, E Typical sites of metastasis of lung cancer include the brain, bone, liver, lymph nodes, and pancreas. Kidneys are not a typical site of lung cancer metastasis. 20. The nurse is conducting a community health education class on diet and cancer risk reduction. What should be included in the discussion? (Select all that apply.) A Limit sodium intake. B Avoid beef and processed meats. C Increase consumption of whole grains. D Eat "colorful fruits and vegetables," including greens. E Avoid gas-producing vegetables such as cabbage. ANS: B, C, D Consuming bran and whole grains and avoiding red meat and processed foods such as lunchmeats can reduce cancer risk. Consuming foods high in vitamin A, including apricots, carrots, and leafy green and yellow vegetables, can also reduce cancer risk. Reducing sodium is helpful in the treatment of hypertension and heart and kidney failure; no evidence suggests that lowering of sodium intake decreases the incidence of cancer. Eating cruciferous vegetables such as broccoli, cauliflower, Brussels sprouts, and cabbage may actually reduce cancer risk. 21. What are the common cancers related to tobacco use? (Select all that apply.) A Cardiac cancer B Lung cancer C Cancer of the tongue D Skin cancer E Cancer of the larynx ANS: B, C, E Organs exposed to the carcinogens in tobacco (lungs, tongue, larynx) are the most likely to develop cancer. Oral cancer is also a risk with "smokeless" tobacco. The heart does not contain cells that divide; therefore, cardiac cancer is unlikely. Skin cancer generally is related to repeated sun and other ultraviolet exposure, such as that found with tanning beds. 22. The nurse includes which factors in teaching regarding the typical warning signs of cancer? (Select all that apply.) A Persistent constipation B Scab present for 6 months C Curdlike vaginal discharge D Axillary swelling E Headache ANS: A, B, D Change in bowel habits, a sore that does not heal, and a lump or thickening in the breast or elsewhere are all potential warning signs of cancer. Curdlike vaginal discharge represents a yeast infection. Headache is not a warning sign, but may be present with multiple problems. Chapter 25: pt’s with skin problem A nurse teaches a client who has very dry skin. Which statement should the nurse include in this client's education? a. "Use lots of moisturizer several times a day to minimize dryness." b. "Take a cold shower instead of soaking in the bathtub." c. "Use antimicrobial soap to avoid infection of cracked skin." d. "After you bathe, put lotion on before your skin is totally dry." ANS: D The client should bathe in warm water for at least 20 minutes and then apply lotion immediately because this will keep the moisture in the skin. Just using moisturizer will not be as helpful because the moisturizer is not what rehydrates the skin; it is the water. Bathing in warm water will rehydrate skin more effectively than a cold shower, and antimicrobial soaps are actually more drying than other kinds of soap. A nurse assesses clients on a medical-surgical unit. Which client is at greatest risk for pressure ulcer development? a.A 44-year-old prescribed IV antibiotics for pneumonia b.A 26-year-old who is bedridden with a fractured leg c.A 65-year-old with hemi-paralysis and incontinence d.A 78-year-old requiring assistance to ambulate with a walker ANS: C Being immobile and being incontinent are two significant risk factors for the development of pressure ulcers. The client with pneumonia does not have specific risk factors. The young client who has a fractured leg and the client who needs assistance with ambulation might be at moderate risk if they do not move about much, but having two risk factors makes the 65-year-old the person at highest risk. When transferring a client into a chair, a nurse notices that the pressure-relieving mattress overlay has deep imprints of the client's buttocks, heels, and scapulae. Which action should the nurse take next? a.Turn the mattress overlay to the opposite side. b.Do nothing because this is an expected occurrence. c.Apply a different pressure-relieving device. d.Reinforce the overlay with extra cushions. ANS: C "Bottoming out," as evidenced by deep imprints in the mattress overlay, indicates that this device is not appropriate for this client, and a different device or strategy should be implemented to prevent pressure ulcer formation. A nurse cares for a client who has a deep wound that is being treated with a wet-to- damp dressing. Which intervention should the nurse include in this client's plan of care? a.Change the dressing every 6 hours. b.Assess the wound bed once a day. c.Change the dressing when it is saturated. d.Contact the provider when the dressing leaks ANS: A Wet-to-damp dressings are changed every 4 to 6 hours to provide maximum débridement. The wound should be assessed each time the dressing is changed. Dry gauze dressings should be changed when the outer layer becomes saturated. Synthetic dressings can be left in place for extended periods of time but need to be changed if the seal breaks and the exudate leaks. A nurse is caring for a client who has a pressure ulcer on the right ankle. Which action should the nurse take first? a.Draw blood for albumin, prealbumin, and total protein. b.Prepare for and assist with obtaining a wound culture. c.Place the client in bed and instruct the client to elevate the foot. d.Assess the right leg for pulses, skin color, and temperature. ANS: D A client with an ulcer on the foot should be assessed for interruption in arterial flow to the area. This begins with the assessment of pulses and color and temperature of the skin. The nurse can also assess for pulses noninvasively with a Doppler flowmeter if unable to palpate with his or her fingers. Tests to determine nutritional status and risk assessment would be completed after the initial assessment is done. Wound cultures are done after it has been determined that drainage, odor, and other risks for infection are present. Elevation of the foot would impair the ability of arterial blood to flow to the area. After educating a caregiver of a home care client, a nurse assesses the caregiver's understanding. Which statement indicates that the caregiver needs additional education? a. "I can help him shift his position every hour when he sits in the chair." b. "If his tailbone is red and tender in the morning, I will massage it with baby oil." c."Applying lotion to his arms and legs every evening will decrease dryness." d."Drinking a nutritional supplement between meals will help maintain his weight." ANS: B Massage of reddened areas over bony prominences such as the coccyx, or tailbone, is contraindicated because the pressure of the massage can cause damage to the skin and subcutaneous tissue layers. The other statements are appropriate for the care of a client at home After teaching a client who is at risk for the formation of pressure ulcers, a nurse assesses the client's understanding. Which dietary choice by the client indicates a good understanding of the teaching? a.Low-fat diet with whole grains and cereals and vitamin supplements b.High-protein diet with vitamins and mineral supplements c.Vegetarian diet with nutritional supplements and fish oil capsules d.Low-fat, low-cholesterol, high-fiber, low-carbohydrate diet ANS: B The preferred diet is high in protein to assist in wound healing and prevention of new wounds. Fat is also needed to ensure formation of cell membranes, so any of the options with low fat would not be good choices. A vegetarian diet would not provide fat and high levels of protein. A nurse assesses clients on a medical-surgical unit. Which client should the nurse evaluate for a wound infection? a.Client with blood cultures pending b.Client who has thin, serous wound drainage c.Client with a white blood cell count of 23,000/mm3 d.Client whose wound has decreased in size ANS: C A client with an elevated white blood cell count should be evaluated for sources of infection. Pending cultures, thin drainage, and a decrease in wound size are not indications that the client may have an infection. A nurse who manages client placements prepares to place four clients on a medical- surgical unit. Which client should be placed in isolation awaiting possible diagnosis of infection with methicillin-resistant Staphylococcus aureus(MRSA)? a.Client admitted from a nursing home with furuncles and folliculitisb. b. Client with a leg cut and other trauma from a motorcycle crash c.Client with a rash noticed after participating in sporting events d.Client transferred from intensive care with an elevated white blood cell count ANS: A The client in long-term care and other communal environments is at high risk for MRSA. The presence of furuncles and folliculitis is also an indication that MRSA may be present. A client with an open wound from a motorcycle crash would have the potential to develop MRSA, but no signs are visible at present. The rash following participation in a sporting event could be caused by several different things. A client with an elevated white blood cell count has the potential for infection but should be at lower risk for MRSA than the client admitted from the communal environment. After teaching a client how to care for a furuncle in the axilla, a nurse assesses the client's understanding. Which statement indicates the client correctly understands the teaching? a. "I'll apply cortisone cream to reduce the inflammation." b. "I'll apply a clean dressing after squeezing out the pus." c. "I'll keep my arm down at my side to prevent spread." d. "I'll cleanse the area prior to applying antibiotic cream." ANS: D Cleansing and topical antibiotics can eliminate the infection. Warm compresses enhance comfort and open the lesion, allowing better penetration of the topical antibiotic. Cortisone cream reduces the inflammatory response but increases the infectious process. Squeezing the lesion may introduce infection to deeper tissues and cause cellulitis. Keeping the arm down increases moisture in the area and promotes bacterial growth. A nurse assesses an older client who is scratching and rubbing white ridges on the skin between the fingers and on the wrists. Which action should the nurse take? a.Place the client in a single room. b.Administer an antihistamine. c.Assess the client's airway. d.Apply gloves to minimize friction. ANS: A The client's presentation is most likely to be scabies, a contagious mite infestation. The client needs to be admitted to a single room and treated for the infestation. Secondary interventions may include medication to decrease the itching. This is not an allergic manifestation; therefore, antihistamine and airway assessments are not indicated. Gloves may decrease skin breakdown but would not address the client's infectious disorder A nurse assesses a client who has a chronic wound. The client states, "I do not clean the wound and change the dressing every day because it costs too much for supplies." How should the nurse respond? a. "You can use tap water instead of sterile saline to clean your wound." b. "If you don't clean the wound properly, you could end up in the hospital." c. "Sterile procedure is necessary to keep this wound from getting infected." d. "Good hand hygiene is the only thing that really matters with wound care." ANS: A For chronic wounds in the home, clean tap water and nonsterile supplies are acceptable and serve as cheaper alternatives to sterile supplies. Of course, if the wound becomes grossly infected, the client may end up in the hospital, but this response does not provide any helpful information. Good handwashing is important, but it is not the only consideration. After teaching a client who has psoriasis, a nurse assesses the client's understanding. Which statement indicates the client needs additional teaching? a. "At the next family reunion, I'm going to ask my relatives if they have psoriasis." b. "I have to make sure I keep my lesions covered, so I do not spread this to others." c. "I expect that these patches will get smaller when I lie out in the sun." d. "I should continue to use the cortisone ointment as the patches shrink and dry out." ANS: B Psoriasis is not a contagious disorder. The client does not have to worry about spreading the condition to others. It is a condition that has hereditary links, the patches will decrease in size with ultraviolet light exposure, and cortisone ointment should be applied directly to lesions to suppress cell division. A nurse performs a skin screening for a client who has numerous skin lesions. Which lesion does the nurse evaluate first? a.Beige freckles on the backs of both hands b.Irregular blue mole with white specks on the lower leg c.Large cluster of pustules in the right axilla d.Thick, reddened papules covered by white scales ANS: B This mole fits two of the criteria for being cancerous or precancerous: variation of color within one lesion, and an indistinct or irregular border. Melanoma is an invasive malignant disease with the potential for a fatal outcome. Freckles are a benign condition. Pustules could mean an infection, but it is more important to take care of the potentially cancerous lesion first. Psoriasis vulgaris manifests as thick reddened papules covered by white scales. This is a chronic disorder and is not the priority. A nurse cares for a client who is prescribed vancomycin (Vancocin) 500 mg IV every 6 hours for a methicillin-resistant Staphylococcus aureus (MRSA) infection. Which action should the nurse take? a.Administer it over 30 minutes using an IV pump. b.Give the client diphenhydramine (Benadryl) before the drug. c.Assess the IV site at least every 2 hours for thrombophlebitis. d.Ensure that the client has increased oral intake during therapy. ANS: C Vancomycin is very irritating to the veins and can easily cause thrombophlebitis. This drug is given over at least 60 minutes; although it can cause histamine release (leading to "red man syndrome"), it is not customary to administer diphenhydramine before starting the infusion. Increasing oral intake is not specific to vancomycin therapy. A nurse assesses a young female client who is prescribed isotretinoin (Accutane). Which question should the nurse ask prior to starting this therapy? a. "Do you spend a great deal of time in the sun?" b. "Have you or any family members ever had skin cancer?" c. "Which method of contraception are you using?" d. "Do you drink alcoholic beverages?" ANS: C Isotretinoin has many side effects. It is a known teratogen and can cause severe birth defects. A pregnancy test is required before therapy is initiated, and strict birth control measures must be used during therapy. Sun exposure, alcohol ingestion, and family history of cancer are contraindications for isotretinoin. A nurse cares for clients who have various skin infections. Which infection is paired with the correct pharmacologic treatment? a.Viral infection - Clindamycin (Cleocin) b.Bacterial infection - Acyclovir (Zovirax) c.Yeast infection - Linezolid (Zyvox) d.Fungal infection - Ketoconazole (Nizoral) ANS: D Ketoconazole is an antifungal. Clindamycin and linezolid are antibiotics. Acyclovir is an antiviral drug. A nurse prepares to discharge a client who has a wound and is prescribed home health care. Which information should the nurse include in the hand-off report to the home health nurse? a.Recent wound assessment, including size and appearance b.Insurance information for billing and coding purposes c.Complete health history and physical assessment findings d.Resources available to the client for wound care supplies ANS: A The hospital nurse should provide details about the wound, including size and appearance and any special wound needs, in a hand-off report to the home health nurse. Insurance information is important to the home health agency and manager, but this is not appropriate during this hand-off report. The nurse should report focused assessment findings instead of a complete health history and physical assessment. The home health nurse should work with the client to identify community resources. A nurse assesses a client who has psoriasis. Which action should the nurse take first? a.Don gloves and an isolation gown. b.Shake the client's hand and introduce self. c.Assess for signs and symptoms of infections. d.Ask the client if she might be pregnant. ANS: B Clients with psoriatic lesions are often self-conscious of their skin. The nurse should first provide direct contact and touch without gloves to establish a good report with the client. Psoriasis is not an infectious disease, nor is it contagious. The nurse would not need to wear gloves or an isolation gown. Obtaining a health history and assessing for an infection and pregnancy should be completed after establishing a report with the client. A nurse assesses a wife who is caring for her husband. She has a Braden Scale score of 9. Which question should the nurse include in this assessment? a. "Do you have a bedpan at home?" b. "How are you coping with providing this care?" c. "What are you doing to prevent pediculosis?" d. "Are you sharing a bed with your husband?" ANS: B A client with a Braden Scale score of 9 is at high risk for skin breakdown and requires moderate to maximum assistance to prevent further breakdown. Family members who care for clients at home may experience a disruption in family routines and added stress. The nurse should assess the wife's feelings and provide support for coping with changes. Asking about the client's toileting practices, prevention of pediculosis, and sleeping arrangements do not provide information about the caregiver's support and coping mechanisms and ability to continue to care for her husband. A nurse assesses a client who has a lesion on the skin that is suspicious for skin cancer, as shown below: Which diagnostic test should the nurse anticipate being ordered for this client? a.Punch skin biopsy b.Viral cultures c.Wood's lamp examination d.Diascopy ANS: A This lesion is suspicious for skin cancer and a biopsy is needed. A viral culture would not be appropriate. A Wood's lamp examination is used to determine if skin lesions have characteristic color changes. Diascopy eliminates erythema, making skin lesions easier to examine. A nurse evaluates the following data in a client's chart: 66-year-old male with a health history of a cerebral vascular accident and left-side paralysis White blood cell count: 8000/mm3 Prealbumin: 15.2 mg/dL Albumin: 4.2 mg/dL Lymphocyte count: 2000/mm3 Sacral ulcer - 4 cm ´ 2 cm ´ 1.5 cm Based on this information, which action should the nurse take? a.Perform a neuromuscular assessment. b.Request a dietary consult. c.Initiate Contact Precautions. d.Assess the client's vital signs. ANS: B The white blood cell count is not directly related to nutritional status. Albumin, prealbumin, and lymphocyte counts all give information related to nutritional status. The prealbumin count is a more specific indicator of nutritional status than is the albumin count. The albumin and lymphocyte counts given are normal, but the prealbumin count is low. This puts the client at risk for inadequate wound healing, so the nurse should request a dietary consult. The other interventions do not address the information provided. A nurse evaluates the following data in a client's chart: 78-year-old male with a past medical history of atrial fibrillation is admitted with a chronic leg wound Warfarin sodium (Coumadin) Sotalol (Betapace) Vacuum-assisted wound closure (VAC) treatment to leg wound Based on this information, which action should the nurse take first? a.Assess the client's vital signs and initiate continuous telemetry monitoring. b.Contact the provider and express concerns related to the wound treatment prescribed. c.Consult the wound care nurse to apply the VAC device. d.Obtain a prescription for a low-fat, high-protein diet with vitamin supplements. ANS: B A client on anticoagulants is not a candidate for VAC because of the incidence of bleeding complications. The health care provider needs this information quickly to plan other therapy for the client's wound. The nurse should contact the wound care nurse after alternative orders for wound care are prescribed. Vital signs and telemetry monitoring is appropriate for a client who has a history of atrial fibrillation and should be implemented as routine care for this client. A low-fat, high-protein diet with vitamin supplements will provide the client with necessary nutrients for wound healing but can be implemented after wound care, vital signs, and telemetry monitoring. A nurse manages wound care for clients on a medical-surgical unit. Which client wounds are paired with the appropriate treatments? (Select all that apply.) a.Client with a left heel ulcer with slight necrosis - Whirlpool treatments b.Client with an eschar-covered sacral ulcer - Surgical débridement c.Client with a sunburn and erythema - Soaking in warm water for 20 minutes d.Client with urticaria - Wet-to-dry dressing changes every 6 hours e.Client with a sacral ulcer with purulent drainage - Transparent film dressing ANS: A, B Necrotic tissue should be removed so that healing can take place. Whirlpool treatment can gently remove the necrosis. A wound covered with eschar most likely needs surgical débridement. Warm water would not be recommended for a client with erythema. A wet-to-dry dressing and a transparent film dressing are not appropriate for urticaria or pressure ulcers, respectively. A nurse plans care for a client who is immobile. Which interventions should the nurse include in this client's plan of care to prevent pressure sores? (Select all that apply.) a.Place a small pillow between bony surfaces. b.Elevate the head of the bed to 45 degrees. c.Limit fluids and proteins in the diet. d.Use a lift sheet to assist with re-positioning. e.Re-position the client who is in a chair every 2 hours. f.Keep the client's heels off the bed surfaces. g.Use a rubber ring to decrease sacral pressure when up in the chair. ANS: A, D, F A small pillow decreases the risk for pressure between bony prominences, a lift sheet decreases friction and shear, and heels have poor circulation and are at high risk for pressure sores, so they should be kept off hard surfaces. Head-of-the-bed elevation greater than 30 degrees increases pressure on pelvic soft tissues. Fluids and proteins are important for maintaining tissue integrity. Clients should be repositioned every hour while sitting in a chair. A rubber ring impairs capillary blood flow, increasing the risk for a pressure sore. A nurse prepares to admit a client who has herpes zoster. Which actions should the nurse take? (Select all that apply.) a.Prepare a room for reverse isolation. b.Assess staff for a history of or vaccination for chickenpox. c.Check the admission orders for analgesia. d.Choose a roommate who also is immune suppressed. e.Ensure that gloves are available in the room. ANS: B, C, E Herpes zoster (shingles) is caused by reactivation of the same virus, varicella zoster, in clients who have previously had chickenpox. Anyone who has not had the disease or has not been vaccinated for it is at high risk for getting chickenpox. Herpes zoster is very painful and requires analgesia. Use of gloves and good handwashing are sufficient to prevent spread. It is best to put this client in a private room. Herpes zoster is a disease of immune suppression, so no one who is immune-suppressed should be in the same room. A nurse cares for older adult clients in a long-term acute care facility. Which interventions should the nurse implement to prevent skin breakdown in these clients? (Select all that apply.) a.Use a lift sheet when moving the client in bed. b.Avoid tape when applying dressings. c.Avoid whirlpool therapy. d.Use loose dressing on all wounds. e.Implement pressure-relieving devices. ANS: A, B, E Using a lift sheet will prevent shearing forces from tearing skin. Tape should be avoided so that the skin won't tear. Using pressure-relieving devices for clients who are at risk for pressure ulcer formation, including older adults, is a proactive approach to prevent skin breakdown. No contraindication to using whirlpool therapy for the older client is known. Dressings should be applied as prescribed, not so loose that they do not provide required treatment, and not so tight that they decrease blood flow to tissues. A nurse assesses a client who presents with an increase in psoriatic lesions. Which questions should the nurse ask to identify a possible trigger for worsening of this client's psoriatic lesions? (Select all that apply.) a. "Have you eaten a large amount of chocolate lately?" b. "Have you been under a lot of stress lately?" c. "Have you recently used a public shower?" d. "Have you been out of the country recently?" e. "Have you recently had any other health problems?" f. "Have you changed any medications recently?" ANS: B, E, F Systemic factors, hormonal changes, psychological stress, medications, and general health factors can aggravate psoriasis. Psoriatic lesions are not triggered by chocolate, public showers, or international travel. A nurse delegates care for a client who has open skin lesions. Which statements should the nurse include when delegating this client's hygiene care to an unlicensed assistive personnel (UAP)? (Select all that apply.) a. "Wash your hands before touching the client." b. "Wear gloves when bathing the client." c. "Assess skin for breakdown during the bath." d. "Apply lotion to lesions while the skin is wet." e. "Use a damp cloth to scrub the lesions" ANS: A, B All health care providers should follow Standard Precautions when caring for clients who have any open skin areas. This includes hand hygiene and wearing gloves when in contact with the lesions. The UAP is not qualified to assess the client's skin. The other statements are not appropriate for the care of open skin lesions. A nurse cares for a client who reports pain related to eczematous dermatitis. Which nonpharmacologic comfort measures should the nurse implement? (Select all that apply.) a.Cool, moist compresses b.Topical corticosteroids c.Heating pad d.Tepid bath with cornstarch e.Back rub with baby oil ANS: A, D For a client with eczematous dermatitis, the goal of comfort measures is to decrease inflammation and help débride crusts and scales. The nurse should implement cool, moist compresses and tepid baths with additives such as cornstarch. Topical corticosteroids are a pharmacologic intervention. A heating pad and a back rub with baby oil are not appropriate for this client and could increase inflammation and discomfort. Chapeter 20 A nurse works in an allergy clinic. What task performed by the nurse takes priority? a. Checking emergency equipment each morning b. Ensuring informed consent is obtained as needed c. Providing educational materials in several languages d. Teaching clients how to manage their allergies ANS: A All actions are appropriate for this nurse; however, client safety is the priority. The nurse should ensure that emergency equipment is available and in good working order and that sufficient supplies of emergency medications are on hand as the priority responsibility. When it is appropriate for a client to give informed consent, the nurse ensures the signed forms are on the chart. Providing educational materials in several languages is consistent with holistic care. Teaching is always a major responsibility of all nurses. A client is in the preoperative holding area prior to surgery. The nurse notes that the client has allergies to avocados and strawberries. What action by the nurse is best? a. Assess that the client has been NPO as directed. b. Communicate this information with dietary staff. c. Document the information in the client's chart. d. Ensure the information is relayed to the surgical team. ANS: D A client with allergies to avocados, strawberries, bananas, or nuts has a higher risk of latex allergy. The nurse should ensure that the surgical staff is aware of this so they can provide a latex-free environment. Ensuring the client's NPO status is important for a client having surgery but is not directly related to the risk of latex allergy. Dietary allergies will be communicated when a diet order is placed. Documentation should be thorough but does not take priority. The nurse is caring for clients on the medical-surgical unit. What action by the nurse will help prevent a client from having a type II hypersensitivity reaction? a. Administering steroids for severe serum sickness b. Correctly identifying the client prior to a blood transfusion c. Keeping the client free of the offending agent d. Providing a latex-free environment for the client ANS: B A classic example of a type II hypersensitivity reaction is a blood transfusion reaction. These can be prevented by correctly identifying the client and cross-checking the unit of blood to be administered. Serum sickness is a type III reaction. Avoidance therapy is the cornerstone of treatment for a type IV hypersensitivity. Latex allergies are a type I hypersensitivity A nurse suspects a client has serum sickness. What laboratory result would the nurse correlate with this condition? a. Blood urea nitrogen: 12 mg/dL b. Creatinine: 3.2 mg/dL c. Hemoglobin: 8.2 mg/dL d. White blood cell count: 12,000/mm3 ANS: B The creatinine is high, possibly indicating the client has serum sickness nephritis. Blood urea nitrogen and white blood cell count are both normal. Hemoglobin is not related. A client calls the clinic to report exposure to poison ivy and an itchy rash that is not helped with over-the-counter antihistamines. What response by the nurse is most appropriate? a. "Antihistamines do not help poison ivy." b. "There are different antihistamines to try." c. "You should be seen in the clinic right away." d. "You will need to take some IV steroids." ANS: A Since histamine is not the mediator of a type IV reaction such as with poison ivy, antihistamines will not provide relief. The nurse should educate the client about this. The client does not need to be seen right away. The client may or may not need steroids; they may be given either IV or orally A client with Sjögren's syndrome reports dry skin, eyes, mouth, and vagina. What nonpharmacologic comfort measure does the nurse suggest? a. Frequent eyedrops b. Home humidifier c. Strong moisturizer d. Tear duct plugs ANS: B A humidifier will help relieve many of the client's Sjögren's syndrome symptoms. Eyedrops and tear duct plugs only affect the eyes, and moisturizer will only help the skin. A client is receiving plasmapheresis as treatment for Goodpasture's syndrome. When planning care, the nurse places highest priority on interventions for which client problem? a. Reduced physical activity related to the disease's effects on the lungs b. Inadequate family coping related to the client's hospitalization c. Inadequate knowledge related to the plasmapheresis process d. Potential for infection related to the site for organism invasion ANS: D Physical diagnoses take priority over psychosocial diagnoses, so inadequate family coping and inadequate knowledge are not the priority. The client has a potential for infection because plasmapheresis is an invasive procedure. Reduced activity is manifested by changes in vital signs, oxygenation, or electrocardiogram, and/or reports of chest pain or shortness of breath. There is no information in the question to indicate that the client is experiencing reduced physical activity. A nurse has educated a client on an epinephrine auto-injector (EpiPen). What statement by the client indicates additional instruction is needed? a. "I don't need to go to the hospital after using it." b. "I must carry two EpiPens with me at all times." c. "I will write the expiration date on my calendar." d. "This can be injected right through my clothes." ANS: A Clients should be instructed to call 911 and go to the hospital for monitoring after using the EpiPen. The other statements show good understanding of this treatment. A client having severe allergy symptoms has received several doses of IV antihistamines. What action by the nurse is most important? a. Assess the client's bedside glucose reading. b. Instruct the client not to get up without help. c. Monitor the client frequently for tachycardia. d. Record the client's intake, output, and weight. ANS: B Antihistamines can cause drowsiness, so for the client's safety, he or she should be instructed to call for assistance prior to trying to get up. Hyperglycemia and tachycardia are side effects of sympathomimetics. Fluid and sodium retention are side effects of corticosteroids. A client is in the hospital and receiving IV antibiotics. When the nurse answers the client's call light, the client presents an appearance as shown below: What action by the nurse takes priority? a. Administer epinephrine 1:1000, 0.3 mg IV push immediately. b. Apply oxygen by facemask at 100% and a pulse oximeter. c. Ensure a patent airway while calling the Rapid Response Team. d. Reassure the client that these manifestations will go away ANS: C The nurse should ensure the client's airway is patent and either call the Rapid Response Team or delegate this to someone else. Epinephrine needs to be administered right away, but not without a prescription by the physician unless standing orders exist. The client may need oxygen, but a patent airway comes first. Reassurance is important, but airway and calling the Rapid Response Team are the priorities. A client suffered an episode of anaphylaxis and has been stabilized in the intensive care unit. When assessing the client's lungs, the nurse hears the following sounds. What medication does the nurse prepare to administer? (Click the media button to hear the audio clip.) a. Albuterol (Proventil) via nebulizer b. Diphenhydramine (Benadryl) IM c. Epinephrine 1:10,000 5 mg IV push d. Methylprednisolone (Solu-Medrol) IV push ANS: A The nurse has auscultated wheezing in the client's lungs and prepares to administer albuterol, which is a bronchodilator, or assists respiratory therapy with administration. Diphenhydramine is an antihistamine. Epinephrine is given during an acute crisis in a concentration of 1:1000. Methylprednisolone is a corticosteroid. The nursing student is studying hypersensitivity reactions. Which reactions are correctly matched with their hypersensitivity types? (Select all that apply.) a. Type I - Examples include hay fever and anaphylaxis b. Type II - Mediated by action of immunoglobulin M (IgM) c. Type III - Immune complex deposits in blood vessel walls d. Type IV - Examples are poison ivy and transplant rejection e. Type V - Examples include a positive tuberculosis test and sarcoidosis ANS: A, C, D Type I reactions are mediated by immunoglobulin E (IgE) and include hay fever, anaphylaxis, and allergic asthma. Type III reactions consist of immune complexes that form and deposit in the walls of blood vessels. Type IV reactions include responses to poison ivy exposure, positive tuberculosis tests, and graft rejection. Type II reactions are mediated by immunoglobulin G, not IgM. Type V reactions include Graves' disease and B-cell gammopathies. A client in the family practice clinic reports a 2-week history of an "allergy to something." The nurse obtains the following assessment and laboratory data: Physical Assessment Data Laboratory Results Reports sore throat, runny nose, headache Posterior pharynx is reddened Nasal discharge is seen in the back of the throat Nasal discharge is creamy yellow in color Temperature 100.2° F (37.9° C) Red, watery eyes White blood cell count: 13,400/mm3 Eosinophil count: 11.5% Neutrophil count: 82% About what medications and interventions does the nurse plan to teach this client? (Select all that apply.) a. Elimination of any pets b. Chlorpheniramine (Chlor-Trimaton) c. Future allergy scratch testing d. Proper use of decongestant nose sprays e. Taking the full dose of antibiotics ANS: B, C, D, E This client has manifestations of both allergic rhinitis and an overlying infection (probably sinus, as evidenced by purulent nasal drainage, high white blood cells, and high neutrophils). The client needs education on antihistamines such as chlorpheniramine, future allergy testing, the proper way to use decongestant nasal sprays, and ensuring that the full dose of antibiotics is taken. Since the nurse does not yet know what the client is allergic to, advising him or her to get rid of pets is premature Chapter 29: non infectious upper respiratory problems 1. A nurse is assessing a client who has suffered a nasal fracture. Which assessment should the nurse perform first? a. Facial pain b. Vital signs c. Bone displacement d. Airway patency ANS: D A patent airway is the priority. The nurse first should make sure that the airway is patent and then should determine whether the client is in pain and whether bone displacement or blood loss has occurred. 2. A nurse assesses a client who has a nasal fracture. The client reports constant nasal drainage, a headache, and difficulty with vision. Which action should the nurse take next? a. Collect the nasal drainage on a piece of filter paper. b. Encourage the client to blow his or her nose. c. Perform a test focused on a neurologic examination. d. Palpate the nose, face, and neck. ANS: A The client with nasal drainage after facial trauma could have a skull fracture that has resulted in leakage of cerebrospinal fluid (CSF). CSF can be differentiated from regular drainage by the fact that it forms a halo when dripped on filter paper. The other actions would be appropriate but are not as high a priority as assessing for CSF. A CSF leak would increase the client's risk for infection. 3. A nurse assesses a client who reports waking up feeling very tired, even after 8 hours of good sleep. Which action should the nurse take first? a. Contact the provider for a prescription for sleep medication. b. Tell the client not to drink beverages with caffeine before bed. c. Educate the client to sleep upright in a reclining chair. d. Ask the client if he or she has ever been evaluated for sleep apnea. ANS: D Clients are usually unaware that they have sleep apnea, but it should be suspected in people who have persistent daytime sleepiness and report waking up tired. Causes of the problem should be assessed before the client is offered suggestions for treatment. 4. A nurse teaches a client who has open vocal cord paralysis. Which technique should the nurse teach the client to prevent aspiration? a. Tilt the head back as far as possible when swallowing. b. Tuck the chin down when swallowing. c. Breathe slowly and deeply while swallowing. d. Keep the head very still and straight while swallowing. ANS: B The client with open vocal cord paralysis may aspirate. The nurse should teach the client to tuck in his or her chin during swallowing to prevent aspiration. Tilting the head back would increase the chance of aspiration. Breathing slowly would not decrease the risk of aspiration, but holding the breath would. Keeping the head still and straight would not decrease the risk for aspiration. 5. A nurse assesses clients on the medical-surgical unit. Which client is at greatest risk for development of obstructive sleep apnea? a. A 26-year-old woman who is 8 months pregnant b. A 42-year-old man with gastroesophageal reflux disease c. A 55-year-old woman who is 50 pounds overweight d. A 73-year-old man with type 2 diabetes mellitus ANS: C The client at highest risk would be the one who is extremely overweight. None of the other clients have risk factors for sleep apnea. 6. After teaching a client who is prescribed "voice rest" therapy for vocal cord polyps, a nurse assesses the client's understanding. Which statement indicates the client needs further teaching? a. "I will stay away from smokers to minimize inhalation of secondhand smoke." b. "When I speak, I will whisper rather than use a normal tone of voice." c. "For the next several weeks, I will not lift more than 10 pounds." d. "I will drink at least three quarts of water each day to stay hydrated." ANS: B Treatment for vocal cord polyps includes no speaking, no lifting, and no smoking. The client has to be educated not to even whisper when resting the voice. It is also appropriate for the client to stay out of rooms where people are smoking, to stay hydrated, and to use stool softeners. 7. A nurse cares for a client who is experiencing epistaxis. Which action should the nurse take first? a. Initiate Standard Precautions. b. Apply direct pressure. c. Sit the client upright. d. Loosely pack the nares with gauze. ANS: A The nurse should implement Standard Precautions and don gloves prior to completing the other actions. 8. A nurse cares for a client after radiation therapy for lung cancer. The client reports a sore throat. Which action should the nurse take first? a. Ask the client to gargle with mouthwash containing lidocaine. b. Administer prescribed intravenous pain medications. c. Explain that soreness is normal and will improve in a couple days. d. Assess the client's neck for redness and swelling. ANS: A Mouthwashes and throat sprays containing a local anesthetic agent such as lidocaine or diphenhydramine can provide relief from a sore throat after radiation therapy. Intravenous pain medications may be used if local anesthetics are unsuccessful. The nurse should explain to the client that this is normal and assess the client's neck, but these options do not decrease the client's discomfort. 9. A nurse cares for a client who had a partial laryngectomy 10 days ago. The client states that all food tastes bland. How should the nurse respond? a. "I will consult the speech therapist to ensure you are swallowing properly." b. "This is normal after surgery. What types of food do you like to eat?" c. "I will ask the dietitian to change the consistency of the food in your diet." d. "Replacement of protein, calories, and water is very important after surgery." ANS: B Many clients experience changes in taste after surgery. The nurse should identify foods that the client wants to eat to ensure the client maintains necessary nutrition. Although the nurse should collaborate with the speech therapist and dietitian to ensure appropriate replacement of protein, calories, and water, the other responses do not address the client's concerns. 10. A nurse cares for a client who is scheduled for a total laryngectomy. Which action should the nurse take prior to surgery? a. Assess airway patency, breathing, and circulation. b. Administer prescribed intravenous pain medication. c. Assist the client to choose a communication method. d. Ambulate the client in the hallway to assess gait. ANS: C The client will not be able to speak after surgery. The nurse should assist the client to choose a communication method that he or she would like to use after surgery. Assessing the client's airway and administering IV pain medication are done after the procedure. Although ambulation promotes health and decreases the complications of any surgery, this client's gait should not be impacted by a total laryngectomy and therefore is not a priority. 11. While assessing a client who has facial trauma, the nurse auscultates stridor. The client is anxious and restless. Which action should the nurse take first? a. Contact the provider and prepare for intubation. b. Administer prescribed albuterol nebulizer therapy. c. Place the client in high-Fowler's position. d. Ask the client to perform deep-breathing exercises. ANS: A Facial and neck tissue edema can occur in clients with facial trauma. Airway patency is the highest priority. Clients who experience stridor and hypoxia, manifested by anxiety and restlessness, should be immediately intubated to ensure airway patency. Albuterol decreases bronchi and bronchiole inflammation, not facial and neck edema. Although putting the client in high-Fowler's position and asking the client to perform breathing exercises may temporarily improve the client's comfort, these actions will not decrease the underlying problem or improve airway patency. 12. A nurse is caring for a client who has sleep apnea and is prescribed modafinil (Provigil). The client asks, "How will this medication help me?" How should the nurse respond? a. "This medication will treat your sleep apnea." b. "This sedative will help you to sleep at night." c. "This medication will promote daytime wakefulness." d. "This analgesic will increase comfort while you sleep." ANS: C Modafinil is helpful for clients who have narcolepsy (uncontrollable daytime sleep) related to sleep apnea. This medication promotes daytime wakefulness. 13. A nurse cares for a client who has packing inserted for posterior nasal bleeding. Which action should the nurse take first? a. Assess the client's pain level. b. Keep the client's head elevated. c. Teach the client about the causes of nasal bleeding. d. Make sure the string is taped to the client's cheek. ANS: D The string should be attached to the client's cheek to hold the packing in place. The nurse needs to make sure that this does not move because it can occlude the client's airway. The other options are good interventions, but ensuring that the airway is patent is the priority objective. 14. A nurse teaches a client to use a room humidifier after a laryngectomy. Which statement should the nurse include in this client's teaching? a. "Add peppermint oil to the humidifier to relax the airway." b. "Make sure you clean the humidifier to prevent infection." c. "Keep the humidifier filled with water at all times." d. "Use the humidifier when you sleep, even during daytime naps." ANS: B Priority teaching related to the use of a room humidifier focuses on infection control. Clients should be taught to meticulously clean the humidifier to prevent the spread of mold or other sources of infection. Peppermint oil should not be added to a humidifier. The humidifier should be refilled with water as needed and should be used while awake and asleep. 1. A nurse assesses a client who is 6 hours post-surgery for a nasal fracture and has nasal packing in place. Which actions should the nurse take? (Select all that apply.) a. Observe for clear drainage. b. Assess for signs of bleeding. c. Watch the client for frequent swallowing. d. Ask the client to open his or her mouth. e. Administer a nasal steroid to decrease edema. f. Change the nasal packing. ANS: A, B, C, D The nurse should observe for clear drainage because of the risk for cerebrospinal fluid leakage. The nurse should assess for signs of bleeding by asking the client to open his or her mouth and observing the back of the throat for bleeding. The nurse should also note whether the client is swallowing frequently because this could indicate postnasal bleeding. A nasal steroid would increase the risk for infection. It is too soon to change the packing, which should be changed by the surgeon the first time. 2. A nurse assesses a client who has developed epistaxis. Which conditions in the client's history should the nurse identify as potential contributors to this problem? (Select all that apply.) a. Diabetes mellitus b. Hypertension c. Leukemia d. Cocaine use e. Migraine f. Elevated platelets ANS: B, C, D Frequent causes of nosebleeds include trauma, hypertension, leukemia and other blood dyscrasias, inflammation, tumor, dry air, blowing or picking the nose, cocaine use, and intranasal procedures. Diabetes, migraines, and elevated platelets and cholesterol levels do not cause epistaxis. 3. A nurse assesses a client who has facial trauma. Which assessment findings require immediate intervention? (Select all that apply.) a. Stridor b. Nasal stuffiness c. Edema of the cheek d. Ecchymosis behind the ear e. Eye pain f. Swollen chin ANS: A, D Stridor is a sign of airway obstruction and requires immediate intervention. Ecchymosis, or bruising, behind the ear is called "battle sign" and indicates basilar skull fracture. Nasal stuffiness, edema of the cheek or chin, and eye pain do not interfere with respirations or neurologic function, and therefore are not priorities for immediate intervention. 4. A registered nurse (RN) cares for clients on a surgical unit. Which clients should the RN delegate to a licensed practical nurse (LPN)? (Select all that apply.) a. A 32-year-old who had a radical neck dissection 6 hours ago b. A 43-year-old diagnosed with cancer after a lung biopsy 2 days ago c. A 55-year-old who needs discharge teaching after a laryngectomy d. A 67-year-old who is awaiting preoperative teaching for laryngeal cancer e. An 88-year-old with esophageal cancer who is awaiting gastric tube placement ANS: B, E The nurse can delegate stable clients to the LPN. The client who had a biopsy 2 days ago and the client who is awaiting gastric tube placement are stable. The client who is 6 hours post-surgery is not yet stable. The RN is the only one who can perform discharge and preoperative teaching; teaching cannot be delegated. 5. A nurse teaches a client who is being discharged after a fixed centric occlusion for a mandibular fracture. Which statements should the nurse include in this client's teaching? (Select all that apply.) a. "You will need to cut the wires if you start vomiting." b. "Eat six soft or liquid meals each day while recovering." c. "Irrigate your mouth every 2 hours to prevent infection." d. "Sleep in a semi-Fowler's position after the surgery." e. "Gargle with mouthwash that contains Benadryl once a day." ANS: A, B, C, D The client needs to know how to cut the wires in case of emergency. If the client vomits, he or she may aspirate. The client should also be taught to eat soft or liquid meals multiple times a day, irrigate the mouth with a Waterpik to prevent infection, and sleep in a semi-Fowler's position to assist in avoiding aspiration. Mouthwash with Benadryl is used for clients who have mouth pain after radiation treatment; it is not used to treat pain in a client with a mandibular fracture. 6. A nurse is assessing clients on a rehabilitation unit. Which clients are at greatest risk for asphyxiation related to inspissated oral and nasopharyngeal secretions? (Select all that apply.) a. A 24-year-old with a traumatic brain injury b. A 36-year-old who fractured his left femur c. A 58-year-old at risk for aspiration following radiation therapy d. A 66-year-old who is a quadriplegic and has a sacral ulcer e. An 80-year-old who is aphasic after a cerebral vascular accident ANS: A, C, D, E Risk for asphyxiation related to inspissated oral and nasopharyngeal secretions is caused by poor oral hygiene. Clients at risk include those with altered mental status and level of consciousness (traumatic brain injury), dehydration, an inability to communicate (aphasic) and cough effectively (quadriplegic), and a risk of aspiration (aspiration precautions). The client with a fractured femur is at risk for a pulmonary embolism. Chapter 7 1. A nurse cares for a dying client. Which manifestation of dying should the nurse treat first? a. Anorexia b. Pain c. Nausea d. Hair loss B Rationale: Only symptoms that cause distress for a dying client should be treated. Such symptoms include pain, nausea and vomiting, dyspnea, and agitation. These problems interfere with the client's comfort. Even when symptoms, such as anorexia or hair loss, disturb the family, they should be treated only if the client is distressed by their presence. The nurse should treat the client's pain first. 2. A nurse plans care for a client who is nearing end of life. Which question should the nurse ask when developing this client's plan of care? a. "Is your advance directive up to date and notarized?" b. "Do you want to be at home at the end of your life?" c. "Would you like a physical therapist to assist you with range-of-motion activities?" d. "Have your children discussed resuscitation with your health care provider?" B Rationale: When developing a plan of care for a dying client, consideration should be given for where the client wants to die. Advance directives do not need to be notarized. A physical therapist would not be involved in end-of-life care. The client should discuss resuscitation with the health care provider and children; do-not-resuscitate status should be the client's decision, not the family's decision. 3. A nurse is caring for a client who has lung cancer and is dying. Which prescription should the nurse question? a. Morphine 10 mg sublingual every 6 hours PRN for pain level greater than 5 b. Albuterol (Proventil) metered dose inhaler every 4 hours PRN for wheezes c. Atropine solution 1% sublingual every 4 hours PRN for excessive oral secretions d. Sodium biphosphate (Fleet) enema once a day PRN for impacted stool A Rationale: Pain medications should be scheduled around the clock to maintain comfort and prevent reoccurrence of pain. The other medications are appropriate for this client. 4. A client tells the nurse that, even though it has been 4 months since her sister's death, she frequently finds herself crying uncontrollably. How should the nurse respond? a. "Most people move on within a few months. You should see a grief counselor." b. "Whenever you start to cry, distract yourself from thoughts of your sister." c. "You should try not to cry. I'm sure your sister is in a better place now." d. "Your feelings are completely normal and may continue for a long time." D Rationale: Frequent crying is not an abnormal response. The nurse should let the client know that this is normal and okay. Although the client may benefit from talking with a grief counselor, it is not unusual for her to still be grieving after a few months. The other responses are not as therapeutic because they justify or minimize the client's response. 5. After teaching a client about advance directives, a nurse assesses the client's understanding. Which statement indicates the client correctly understands the teaching? a. "An advance directive will keep my children from selling my home when I'm old." b. "An advance directive will be completed as soon as I'm incapacitated and can't think for myself." c. "An advance directive will specify what I want done when I can no longer make decisions about health care." d. "An advance directive will allow me to keep my money out of the reach of my family." C Rationale: An advance directive is a written document prepared by a competent individual that specifies what, if any, extraordinary actions a person would want taken when he or she can no longer make decisions about personal health care. It does not address issues such as the client's residence or financial matters. 6. A nurse teaches a client who is considering being admitted to hospice. Which statement should the nurse include in this client's teaching? a. "Hospice admission has specific criteria. You may not be a viable candidate, so we will look at alternative plans for your discharge." b. "Hospice care focuses on a holistic approach to health care. It is designed not to hasten death, but rather to relieve symptoms." c. "Hospice care will not help with your symptoms of depression. I will refer you to the facility's counseling services instead." d. "You seem to be experiencing some difficulty with this stage of the grieving process. Let's talk about your feelings." B Rationale: As both a philosophy and a system of care, hospice care uses an interdisciplinary approach to assess and address the holistic needs of clients and families to facilitate quality of life and a peaceful death. This holistic approach neither hastens nor postpones death but provides relief of symptoms experienced by the dying client. 7. A nurse is caring for a dying client. The client's spouse states, "I think he is choking to death." How should the nurse respond? a. "Do not worry. The choking sound is normal during the dying process." b. "I will administer more morphine to keep your husband comfortable." c. "I can ask the respiratory therapist to suction secretions out through his nose." d. "I will have another nurse assist me to turn your husband on his side." D Rationale: The choking sound or "death rattle" is common in dying clients. The nurse should acknowledge the spouse's concerns and provide interventions that will reduce the choking sounds. Repositioning the client onto one side with a towel under the mouth to collect secretions is the best intervention. The nurse should not minimize the spouse's concerns. Morphine will assist with comfort but will not decrease the choking sounds. Nasotracheal suctioning is not appropriate in a dying client. 8. The nurse is teaching a family member about various types of complementary therapies that might be effective for relieving the dying client's anxiety and restlessness. Which statement made by the family member indicates understanding of the nurse's teaching? a. "Maybe we should just hire an around-the-clock sitter to stay with Grandmother." b. "I have some of her favorite hymns on a CD that I could bring for music therapy." c. "I don't think that she'll need pain medication along with her herbal treatments." d. "I will burn therapeutic incense in the room so we can stop the anxiety pills." B Rationale: Music therapy is a complementary therapy that may produce relaxation by quieting the mind and removing a client's inner restlessness. Hiring an around-the-clock sitter does not demonstrate that the client's family understands complementary therapies. Complementary therapies are used in conjunction with traditional therapy. Complementary therapy would not replace pain or anxiety medication but may help decrease the need for these medications. 9. A nurse is caring for a terminally ill client who has just died in a hospital setting with family members at the bedside. Which action should the nurse take first? a. Call for emergency assistance so that resuscitation procedures can begin. b. Ask family members if they would like to spend time alone with the client. c. Ensure that a death certificate has been completed by the physician. d. Request family members to prepare the client's body for the funeral home. B Rationale: Before moving the client's body to the funeral home, the nurse should ask family members if they would like to be alone with the client. Emergency assistance will not be necessary. Although it is important to ensure that a death certificate has been completed before the client is moved to the mortuary, the nurse first should ask family members if they would like to be alone with the client. The client's family should not be expected to prepare the body for the funeral home. 10.A A nurse assesses a client who is dying. Which manifestation of a dying client should the nurse assess to determine whether the client is near death? a. Level of consciousness b. Respiratory rate c. Bowel sounds d. Pain level on a 0-to-10 scale B Rationale: Although all of these assessments should be performed during the dying process, periods of apnea and Cheyne-Strokes respirations indicate death is near. As peripheral circulation decreases, the client's level of consciousness and bowel sounds decrease, and the client would be unable to provide a numeric number on a pain scale. Even with these other symptoms, the nurse should continue to assess respiratory rate throughout the dying process. As the rate drops significantly and breathing becomes agonal, death is near. 11.A A nurse is caring for a client who is terminally ill. The client's spouse states, "I am concerned because he does not want to eat." How should the nurse respond? a. "Let him know that food is available if he wants it, but do not insist that he eat." b. "A feeding tube can be placed in the nose to provide important nutrients." c. "Force him to eat even if he does not feel hungry, or he will die sooner." d. "He is getting all the nutrients he needs through his intravenous catheter." A Rationale: When family members understand that the client is not suffering from hunger and is not "starving to death," they may allow the client to determine when, what, or if to eat. Often, as death approaches, metabolic needs decrease and clients do not feel the sensation of hunger. Forcing them to eat frustrates the client and the family. 12.A A nurse discusses inpatient hospice with a client and the client's family. A family member expresses concern that her loved one will receive only custodial care. How should the nurse respond? a. "The goal of palliative care is to provide the greatest degree of comfort possible and help the dying person enjoy whatever time is left." b. "Palliative care will release you from the burden of having to care for someone in the home. It does not mean that curative treatment will stop." c. "A palliative care facility is like a nursing home and costs less than a hospital because only pain medications are given." d. "Your relative is unaware of her surroundings and will not notice the difference between her home and a palliative care facility." A Rationale: Palliative care provides an increased level of personal care designed to manage symptom distress. The focus is on pain control and helping the relative die with dignity. 13. An intensive care nurse discusses withdrawal of care with a client's family. The family expresses concerns related to discontinuation of therapy. How should the nurse respond? a. "I understand your concerns, but in this state, discontinuation of care is not a form of active euthanasia." b. "You will need to talk to the provider because I am not legally allowed to participate in the withdrawal of life support." c. "I realize this is a difficult decision. Discontinuation of therapy will allow the client to die a natural death." d. "There is no need to worry. Most religious organizations support the client's decision to stop medical treatment." C Rationale: The nurse should validate the family's concerns and provide accurate information about the discontinuation of therapy. The other statements address specific issues related to the withdrawal of care but do not provide appropriate information about their purpose. If the client's family asks for specific information about euthanasia, legal, or religious issues, the nurse should provide unbiased information about these topics. 14.A A hospice nurse is caring for a variety of clients who are dying. Which end-of-life and death ritual is paired with the correct religion? a. Roman Catholic - Autopsies are not allowed except under special circumstances. b. Christian - Upon death, a religious leader should perform rituals of bathing and wrapping the body in cloth. c. Judaism - A person who is extremely ill and dying should not be left alone. d. Islam - An ill or dying person should receive the Sacrament of the Sick. C Rationale: According to Jewish law, a person who is extremely ill or dying should not be left alone. Orthodox Jews do not allow autopsies except under special circumstances. The Islamic faith requires a religious leader to perform rituals of bathing and wrapping the body in cloth upon death. A Catholic priest performs the Sacrament of the Sick for ill or dying people. 15.A A hospice nurse is caring for a dying client and her family members. Which interventions should the nurse implement? (Select all that apply.) a. Teach family members about physical signs of impending death. b. Encourage the management of adverse symptoms. c. Assist family members by offering an explanation for their loss. d. Encourage reminiscence by both client and family members. A,B,D e. Avoid spirituality because the client's and the nurse's beliefs may not be congruent. Rationale: The nurse should teach family members about the physical signs of death, because family members often become upset when they see physiologic changes in their loved one. Palliative care includes management of symptoms so that the peaceful death of the client is facilitated. Reminiscence will help both the client and family members cope with the dying process. The nurse is not expected to explain why this is happening to the family's loved one. The nurse can encourage spirituality if the client is agreeable, regardless of whether the client's religion is the same. 16.A A nurse admits an older adult client to the hospital. Which criterion should the nurse use to determine if the client can make his own medical decisions? (Select all that apply.) a. Can communicate his treatment preferences b. Is able to read and write at an eighth-grade level c. Is oriented enough to understand information provided d. Can evaluate and deliberate information e. Has completed an advance directive A,C,D Rationale: To have decision-making ability, a person must be able to perform three tasks: receive information (but not necessarily oriented ´ 4); evaluate, deliberate, and mentally manipulate information; and communicate a treatment preference. The client does not have to read or write at a specific level. Education can be provided at the client's level so that he can make the necessary decisions. The client does not need to complete an advance directive to make his own medical decisions. An advance directive will be necessary if he wants to designate someone to make medical decisions when he is unable to. 17.A A hospice nurse plans care for a client who is experiencing pain. Which complementary therapies should the nurse incorporate in this client's pain management plan? (Select all that apply.) a. Play music that the client enjoys. b. Massage tissue that is tender from radiation therapy. c. Rub lavender lotion on the client's feet. d. Ambulate the client in the hall twice a day. e. Administer intravenous morphine. A,C Rationale: Complementary therapies for pain management include massage therapy, music therapy, Therapeutic Touch, and aromatherapy. Nurses should not massage over sites of tissue damage from radiation therapy. Ambulation and intravenous morphine are not complementary therapies for pain management. 18. A nurse teaches a client's family members about signs and symptoms of approaching death. Which manifestations should the nurse include in this teaching? (Select all that apply.) D,E a. Warm and flushed extremities b. Long periods of insomnia c. Increased respiratory rate d. Decreased appetite e. Congestion and gurgling Rationale: Common physical signs and symptoms of approaching death including coolness of extremities, increased sleeping, irregular and slowed breathing rate, a decrease in fluid and food intake, congestion and gurgling, incontinence, disorientation, and restlessness. Chapter 34 A nurse assesses a client's electrocardiograph tracing and observes that not all QRS complexes are preceded by a P wave. How should the nurse interpret this observation? a. The client has hyperkalemia causing irregular QRS complexes. b. Ventricular tachycardia is overriding the normal atrial rhythm. c. The client's chest leads are not making sufficient contact with the skin. d. Ventricular and atrial depolarizations are initiated from different sites. ANS: D Normal rhythm shows one P wave preceding each QRS complex, indicating that all depolarization is initiated at the sinoatrial node. QRS complexes without a P wave indicate a different source of initiation of depolarization. This finding on an electrocardiograph tracing is not an indication of hyperkalemia, ventricular tachycardia, or disconnection of leads. A nurse cares for a client who has a heart rate averaging 56 beats/min with no adverse symptoms. Which activity modification should the nurse suggest to avoid further slowing of the heart rate? a. "Make certain that your bath water is warm." b. "Avoid straining while having a bowel movement." c. "Limit your intake of caffeinated drinks to one a day." d. "Avoid strenuous exercise such as running." ANS: B Bearing down strenuously during a bowel movement is one type of Valsalva maneuver, which stimulates the vagus nerve and results in slowing of the heart rate. Such a response is not desirable in a person who has bradycardia. The other instructions are not appropriate for this condition. A nurse is assessing clients on a medical-surgical unit. Which client should the nurse identify as being at greatest risk for atrial fibrillation? a. A 45-year-old who takes an aspirin daily b. A 50-year-old who is post coronary artery bypass graft surgery c. A 78-year-old who had a carotid endarterectomy d. An 80-year-old with chronic obstructive pulmonary disease ANS: B Atrial fibrillation occurs commonly in clients with cardiac disease and is a common occurrence after coronary artery bypass graft surgery. The other conditions do not place these clients at higher risk for atrial fibrillation. A nurse assesses a client with atrial fibrillation. Which manifestation should alert the nurse to the possibility of a serious complication from this condition? a. Sinus tachycardia b. Speech alterations c. Fatigue d. Dyspnea with activity ANS: B Clients with atrial fibrillation are at risk for embolic stroke. Evidence of embolic events includes changes in mentation, speech, sensory function, and motor function. Clients with atrial fibrillation often have a rapid ventricular response as a result. Fatigue is a nonspecific complaint. Clients with atrial fibrillation often have dyspnea as a result of the decreased cardiac output caused by the rhythm disturbance. A nurse evaluates prescriptions for a client with chronic atrial fibrillation. Which medication should the nurse expect to find on this client's medication administration record to prevent a common complication of this condition? a. Sotalol (Betapace) b. Warfarin (Coumadin) c. Atropine (Sal-Tropine) d. Lidocaine (Xylocaine) ANS: B Atrial fibrillation puts clients at risk for developing emboli. Clients at risk for emboli are treated with anticoagulants, such as heparin, enoxaparin, or warfarin. Sotalol, atropine, and lidocaine are not appropriate for this complication. A nurse administers prescribed adenosine (Adenocard) to a client. Which response should the nurse assess for as the expected therapeutic response? a. Decreased intraocular pressure b. Increased heart rate c. Short period of asystole d. Hypertensive crisis ANS: C Clients usually respond to adenosine with a short period of asystole, bradycardia, hypotension, dyspnea, and chest pain. Adenosine has no conclusive impact on intraocular pressure. A telemetry nurse assesses a client with third-degree heart block who has wide QRS complexes and a heart rate of 35 beats/min on the cardiac monitor. Which assessment should the nurse complete next? a. Pulmonary auscultation b. Pulse strength and amplitude c. Level of consciousness d. Mobility and gait stability ANS: C A heart rate of 40 beats/min or less with widened QRS complexes could have hemodynamic consequences. The client is at risk for inadequate cerebral perfusion. The nurse should assess for level of consciousness, light-headedness, confusion, syncope, and seizure activity. Although the other assessments should be completed, the client's level of consciousness is the priority. A nurse cares for a client with an intravenous temporary pacemaker for bradycardia. The nurse observes the presence of a pacing spike but no QRS complex on the client's electrocardiogram. Which action should the nurse take next? a. Administer intravenous diltiazem (Cardizem). b. Assess vital signs and level of consciousness. c. Administer sublingual nitroglycerin. d. Assess capillary refill and temperature. ANS: B In temporary pacing, the wires are threaded onto the epicardial surface of the heart and exit through the chest wall. The pacemaker spike should be followed immediately by a QRS complex. Pacing spikes seen without subsequent QRS complexes imply loss of capture. If there is no capture, then there is no ventricular depolarization and contraction. The nurse should assess for cardiac output via vital signs and level of consciousness. The other interventions would not determine if the client is tolerating the loss of capture. A nurse prepares to defibrillate a client who is in ventricular fibrillation. Which priority intervention should the nurse perform prior to defibrillating this client? a. Make sure the defibrillator is set to the synchronous mode. b. Administer 1 mg of intravenous epinephrine. c. Test the equipment by delivering a smaller shock at 100 joules. d. Ensure that everyone is clear of contact with the client and the bed. ANS: D To avoid injury, the rescuer commands that all personnel clear contact with the client or the bed and ensures their compliance before delivery of the shock. A precordial thump can be delivered when no defibrillator is available. Defibrillation is done in asynchronous mode. Equipment should not be tested before a client is defibrillated because this is an emergency procedure; equipment should be checked on a routine basis. Epinephrine should be administered after defibrillation. After teaching a client who has an implantable cardioverter-defibrillator (ICD), a nurse assesses the client's understanding. Which statement by the client indicates a correct understanding of the teaching? a. "I should wear a snug-fitting shirt over the ICD." b. "I will avoid sources of strong electromagnetic fields." c. "I should participate in a strenuous exercise program." d. "Now I can discontinue my antidysrhythmic medication." ANS: B The client being discharged with an ICD is instructed to avoid strong sources of electromagnetic fields. Clients should avoid tight clothing, which could cause irritation over the ICD generator. The client should be encouraged to exercise but should not engage in strenuous activities that cause the heart rate to meet or exceed the ICD cutoff point because the ICD can discharge inappropriately. The client should continue all prescribed medications. A nurse cares for a client with atrial fibrillation who reports fatigue when completing activities of daily living. What interventions should the nurse implement to address this client's concerns? a. Administer oxygen therapy at 2 liters per nasal cannula. b. Provide the client with a sleeping pill to stimulate rest. c. Schedule periods of exercise and rest during the day. d. Ask unlicensed assistive personnel to help bathe the client. ANS: C Clients who have atrial fibrillation are at risk for decreased cardiac output and fatigue when completing activities of daily living. The nurse should schedule periods of exercise and rest during the day to decrease fatigue. The other interventions will not assist the client with self-care activities. A nurse assists with the cardioversion of a client experiencing acute atrial fibrillation. Which action should the nurse take prior to the initiation of cardioversion? a. Administer intravenous adenosine. b. Turn off oxygen therapy. c. Ensure a tongue blade is available. d. Position the client on the left side. ANS: B For safety during cardioversion, the nurse should turn off any oxygen therapy to prevent fire. The other interventions are not appropriate for a cardioversion. The client should be placed in a supine position. A nurse prepares to discharge a client with cardiac dysrhythmia who is prescribed home health care services. Which priority information should be communicated to the home health nurse upon discharge? a. Medication reconciliation b. Immunization history c. Religious beliefs d. Nutrition preferences ANS: A The home health nurse needs to know current medications the client is taking to ensure assessment, evaluation, and further education related to these medications. The other information will not assist the nurse to develop a plan of care for the client. A nurse assesses a client with tachycardia. Which clinical manifestation requires immediate intervention by the nurse? a. Mid-sternal chest pain b. Increased urine output c. Mild orthostatic hypotension d. P wave touching the T wave ANS: A Chest pain, possibly angina, indicates that tachycardia may be increasing the client's myocardial workload and oxygen demand to such an extent that normal oxygen delivery cannot keep pace. This results in myocardial hypoxia and pain. Increased urinary output and mild orthostatic hypotension are not life-threatening conditions and therefore do not require immediate intervention. The P wave touching the T wave indicates significant tachycardia and should be assessed to determine the underlying rhythm and cause; this is an important assessment but is not as critical as chest pain, which indicates cardiac cell death. A nurse teaches a client who experiences occasional premature atrial contractions (PACs) accompanied by palpitations that resolve spontaneously without treatment. Which statement should the nurse include in this client's teaching? a. "Minimize or abstain from caffeine." b. "Lie on your side until the attack subsides." c. "Use your oxygen when you experience PACs." d. "Take amiodarone (Cordarone) daily to prevent PACs." ANS: A PACs usually have no hemodynamic consequences. For a client experiencing infrequent PACs, the nurse should explore possible lifestyle causes, such as excessive caffeine intake and stress. Lying on the side will not prevent or resolve PACs. Oxygen is not necessary. Although medications may be needed to control symptomatic dysrhythmias, for infrequent PACs, the client first should try lifestyle changes to control them. The nurse asks a client who has experienced ventricular dysrhythmias about substance abuse. The client asks, "Why do you want to know if I use cocaine?" How should the nurse respond? a. "Substance abuse puts clients at risk for many health issues." b. "The hospital requires that I ask you about cocaine use." c. "Clients who use cocaine are at risk for fatal dysrhythmias." d. "We can provide services for cessation of substance abuse." ANS: C Clients who use cocaine or illicit inhalants are particularly at risk for potentially fatal dysrhythmias. The other responses do not adequately address the client's question. A nurse supervises an unlicensed assistive personnel (UAP) applying electrocardiographic monitoring. Which statement should the nurse provide to the UAP related to this procedure? a. "Clean the skin and clip hairs if needed." b. "Add gel to the electrodes prior to applying them." c. "Place the electrodes on the posterior chest." d. "Turn off oxygen prior to monitoring the client." ANS: A To ensure the best signal transmission, the skin should be clean and hairs clipped. Electrodes should be placed on the anterior chest, and no additional gel is needed. Oxygen has no impact on electrocardiographic monitoring. A nurse assesses a client's electrocardiogram (ECG) and observes the reading shown below: How should the nurse document this client's ECG strip? a. Ventricular tachycardia b. Ventricular fibrillation c. Sinus rhythm with premature atrial contractions (PACs) d. Sinus rhythm with premature ventricular contractions (PVCs) ANS: D Sinus rhythm with PVCs has an underlying regular sinus rhythm with ventricular depolarization that sometimes precede atrial depolarization. Ventricular tachycardia and ventricular fibrillation rhythms would not have sinus beats present. Premature atrial contractions are atrial contractions initiated from another region of the atria before the sinus node initiates atrial depolarization. A nurse cares for a client who is on a cardiac monitor. The monitor displayed the rhythm shown below: Which action should the nurse take first? a. Assess airway, breathing, and level of consciousness. b. Administer an amiodarone bolus followed by a drip. c. Cardiovert the client with a biphasic defibrillator. d. Begin cardiopulmonary resuscitation (CPR). ANS: A Ventricular tachycardia occurs with repetitive firing of an irritable ventricular ectopic focus, usually at a rate of 140 to 180 beats/min or more. Ventricular tachycardia is a lethal dysrhythmia. The nurse should first assess if the client is alert and breathing. Then the nurse should call a Code Blue and begin CPR. If this client is pulseless, the treatment of choice is defibrillation. Amiodarone is the antidysrhythmic of choice, but it is not the first action. A nurse performs an admission assessment on a 75-year-old client with multiple chronic diseases. The client's blood pressure is 135/75 mm Hg and oxygen saturation is 94% on 2 liters per nasal cannula. The nurse assesses the client's rhythm on the cardiac monitor and observes the reading shown below: Which action should the nurse take first? a. Begin external temporary pacing. b. Assess peripheral pulse strength. c. Ask the client what medications he or she takes. d. Administer 1 mg of atropine. ANS: C This client is stable and therefore does not require any intervention except to determine the cause of the bradycardia. Bradycardia is often caused by medications. Clients who have multiple chronic diseases are often on multiple medications that can interact with each other. The nurse should assess the client's current medications first. The nurse is caring for a client on the medical-surgical unit who suddenly becomes unresponsive and has no pulse. The cardiac monitor shows the rhythm below: After calling for assistance and a defibrillator, which action should the nurse take next? a. Perform a pericardial thump. b. Initiate cardiopulmonary resuscitation (CPR). c. Start an 18-gauge intravenous line. d. Ask the client's family about code status. ANS: B The client's rhythm is ventricular fibrillation. This is a lethal rhythm that is best treated with immediate defibrillation. While the nurse is waiting for the defibrillator to arrive, the nurse should start CPR. A pericardial thump is not a treatment for ventricular fibrillation. If the client does not already have an IV, other members of the team can insert one after defibrillation. The client's code status should already be known by the nurse prior to this event. After assessing a client who is receiving an amiodarone intravenous infusion for unstable ventricular tachycardia, the nurse documents the findings and compares these with the previous assessment findings: Vital Signs Nursing Assessment Time: 0800 Temperature: 98° F Heart rate: 68 beats/min Blood pressure: 135/60 mm Hg Respiratory rate: 14 breaths/min Oxygen saturation: 96% Oxygen therapy: 2 L nasal cannula Time: 1000 Temperature: 98.2° F Heart rate: 50 beats/min Blood pressure: 132/57 mm Hg Respiratory rate: 16 breaths/min Oxygen saturation: 95% Oxygen therapy: 2 L nasal cannula Time: 0800 Client alert and oriented. Cardiac rhythm: normal sinus rhythm. Skin: warm, dry, and appropriate for race. Respirations equal and unlabored. Client denies shortness of breath and chest pain. Time: 1000 Client alert and oriented. Cardiac rhythm: sinus bradycardia. Skin: warm, dry, and appropriate for race. Respirations equal and unlabored. Client denies shortness of breath and chest pain. Client voids 420 mL of clear yellow urine. Based on the assessments, which action should the nurse take? a. Stop the infusion and flush the IV. b. Slow the amiodarone infusion rate. c. Administer IV normal saline. d. Ask the client to cough and deep breathe. ANS: B IV administration of amiodarone may cause bradycardia and atrioventricular (AV) block. The correct action for the nurse to take at this time is to slow the infusion, because the client is asymptomatic and no evidence reveals AV block that might require pacing. Abruptly ceasing the medication could allow fatal dysrhythmias to occur. The administration of IV fluids and encouragement of coughing and deep breathing exercises are not indicated, and will not increase the client's heart rate. A nurse cares for a client with congestive heart failure who has a regular cardiac rhythm of 128 beats/min. For which physiologic alterations should the nurse assess? (Select all that apply.) a. Decrease in cardiac output b. Increase in cardiac output c. Decrease in blood pressure d. Increase in blood pressure e. Decrease in urine output f. Increase in urine output ANS: A, D, E Elevated heart rates in a healthy client initially cause blood pressure and cardiac output to increase. However, in a client who has congestive heart failure or a client with long- term tachycardia, ventricular filling time, cardiac output, and blood pressure eventually decrease. As cardiac output and blood pressure decrease, urine output will fall A nurse teaches a client with a new permanent pacemaker. Which instructions should the nurse include in this client's teaching? (Select all that apply.) a. "Until your incision is healed, do not submerge your pacemaker. Only take showers." b. "Report any pulse rates lower than your pacemaker settings." c. "If you feel weak, apply pressure over your generator." d. "Have your pacemaker turned off before having magnetic resonance imaging (MRI)." e. "Do not lift your left arm above the level of your shoulder for 8 weeks." ANS: A, B, E The client should not submerge in water until the site has healed; after the incision is healed, the client may take showers or baths without concern for the pacemaker. The client should be instructed to report changes in heart rate or rhythm, such as rates lower than the pacemaker setting or greater than 100 beats/min. The client should be advised of restrictions on physical activity for 8 weeks to allow the pacemaker to settle in place. The client should never apply pressure over the generator and should avoid tight clothing. The client should never have MRI because, whether turned on or off, the pacemaker contains metal. The client should be advised to inform all health care providers that he or she has a pacemaker. A nurse is teaching a client with premature ectopic beats. Which education should the nurse include in this client's teaching? (Select all that apply.) a. Smoking cessation b. Stress reduction and management c. Avoiding vagal stimulation d. Adverse effects of medications e. Foods high in potassium Chapter 35: Care of Patients With Cardiac Problems A nurse assesses clients on a cardiac unit. Which client should the nurse identify as being at greatest risk for the development of left-sided heart failure? a. A 36-year-old woman with aortic stenosis b. A 42-year-old man with pulmonary hypertension c. A 59-year-old woman who smokes cigarettes daily d. A 70-year-old man who had a cerebral vascular accident ANS: A Although most people with heart failure will have failure that progresses from left to right, it is possible to have left-sided failure alone for a short period. It is also possible to have heart failure that progresses from right to left. Causes of left ventricular failure include mitral or aortic valve disease, coronary artery disease, and hypertension. Pulmonary hypertension and chronic cigarette smoking are risk factors for right ventricular failure. A cerebral vascular accident does not increase the risk of heart failure. A nurse assesses a client in an outpatient clinic. Which statement alerts the nurse to the possibility of left-sided heart failure? a. "I have been drinking more water than usual." b. "I am awakened by the need to urinate at night." c. "I must stop halfway up the stairs to catch my breath." d. "I have experienced blurred vision on several occasions." ANS: C Clients with left-sided heart failure report weakness or fatigue while performing normal activities of daily living, as well as difficulty breathing, or "catching their breath." This occurs as fluid moves into the alveoli. Nocturia is often seen with right-sided heart failure. Thirst and blurred vision are not related to heart failure. A nurse assesses a client admitted to the cardiac unit. Which statement by the client alerts the nurse to the possibility of right-sided heart failure? a. "I sleep with four pillows at night." b. "My shoes fit really tight lately." c. "I wake up coughing every night." d. "I have trouble catching my breath." ANS: B Signs of systemic congestion occur with right-sided heart failure. Fluid is retained, pressure builds in the venous system, and peripheral edema develops. Left-sided heart failure symptoms include respiratory symptoms. Orthopnea, coughing, and difficulty breathing all could be results of left-sided heart failure. While assessing a client on a cardiac unit, a nurse identifies the presence of an S3 gallop. Which action should the nurse take next? a. Assess for symptoms of left-sided heart failure. b. Document this as a normal finding. c. Call the health care provider immediately. d. Transfer the client to the intensive care unit. ANS: A The presence of an S3 gallop is an early diastolic filling sound indicative of increasing left ventricular pressure and left ventricular failure. The other actions are not warranted. A nurse cares for a client with right-sided heart failure. The client asks, "Why do I need to weigh myself every day?" How should the nurse respond? a. "Weight is the best indication that you are gaining or losing fluid." b. "Daily weights will help us make sure that you're eating properly." c. "The hospital requires that all inpatients be weighed daily." d. "You need to lose weight to decrease the incidence of heart failure." ANS: A Daily weights are needed to document fluid retention or fluid loss. One liter of fluid equals 2.2 pounds. The other responses do not address the importance of monitoring fluid retention or loss. A nurse is teaching a client with heart failure who has been prescribed enalapril (Vasotec). Which statement should the nurse include in this client's teaching? a. "Avoid using salt substitutes." b. "Take your medication with food." c. "Avoid using aspirin-containing products." d. "Check your pulse daily." ANS: A Angiotensin-converting enzyme (ACE) inhibitors such as enalapril inhibit the excretion of potassium. Hyperkalemia can be a life-threatening side effect, and clients should be taught to limit potassium intake. Salt substitutes are composed of potassium chloride. ACE inhibitors do not need to be taken with food and have no impact on the client's pulse rate. Aspirin is often prescribed in conjunction with ACE inhibitors and is not contraindicated. After administering newly prescribed captopril (Capoten) to a client with heart failure, the nurse implements interventions to decrease complications. Which priority intervention should the nurse implement for this client? a. Provide food to decrease nausea and aid in absorption. b. Instruct the client to ask for assistance when rising from bed. c. Collaborate with unlicensed assistive personnel to bathe the client. d. Monitor potassium levels and check for symptoms of hypokalemia. ANS: B Administration of the first dose of angiotensin-converting enzyme (ACE) inhibitors is often associated with hypotension, usually termed first-dose effect. The nurse should instruct the client to seek assistance before arising from bed to prevent injury from postural hypotension. ACE inhibitors do not need to be taken with food. Collaboration with unlicensed assistive personnel to provide hygiene is not a priority. The client should be encouraged to complete activities of daily living as independently as possible. The nurse should monitor for hyperkalemia, not hypokalemia, especially if the client has renal insufficiency secondary to heart failure. A nurse assesses a client after administering isosorbide mononitrate (Imdur). The client reports a headache. Which action should the nurse take? a. Initiate oxygen therapy. b. Hold the next dose of Imdur. c. Instruct the client to drink water. d. Administer PRN acetaminophen. ANS: D The vasodilating effects of isosorbide mononitrate frequently cause clients to have headaches during the initial period of therapy. Clients should be told about this side effect and encouraged to take the medication with food. Some clients obtain relief with mild analgesics, such as acetaminophen. The client's headache is not related to hypoxia or dehydration; therefore, these interventions would not help. The client needs to take the medication as prescribed to prevent angina; the medication should not be held. A nurse teaches a client who is prescribed digoxin (Lanoxin) therapy. Which statement should the nurse include in this client's teaching? a. "Avoid taking aspirin or aspirin-containing products." b. "Increase your intake of foods that are high in potassium." c. "Hold this medication if your pulse rate is below 80 beats/min." d. "Do not take this medication within 1 hour of taking an antacid." ANS: D Gastrointestinal absorption of digoxin is erratic. Many medications, especially antacids, interfere with its absorption. Clients are taught to hold their digoxin for bradycardia; a heart rate of 80 beats/min is too high for this cutoff. Potassium and aspirin have no impact on digoxin absorption, nor do these statements decrease complications of digoxin therapy. A nurse teaches a client who has a history of heart failure. Which statement should the nurse include in this client's discharge teaching? a. "Avoid drinking more than 3 quarts of liquids each day." b. "Eat six small meals daily instead of three larger meals." c. "When you feel short of breath, take an additional diuretic." d. "Weigh yourself daily while wearing the same amount of clothing." ANS: D Clients with heart failure are instructed to weigh themselves daily to detect worsening heart failure early, and thus avoid complications. Other signs of worsening heart failure include increasing dyspnea, exercise intolerance, cold symptoms, and nocturia. Fluid overload increases symptoms of heart failure. The client should be taught to eat a heart- healthy diet, balance intake and output to prevent dehydration and overload, and take medications as prescribed. The most important discharge teaching is daily weights as this provides the best data related to fluid retention. A nurse admits a client who is experiencing an exacerbation of heart failure. Which action should the nurse take first? a. Assess the client's respiratory status. b. Draw blood to assess the client's serum electrolytes. c. Administer intravenous furosemide (Lasix). d. Ask the client about current medications. ANS: A Assessment of respiratory and oxygenation status is the priority nursing intervention for the prevention of complications. Monitoring electrolytes, administering diuretics, and asking about current medications are important but do not take priority over assessing respiratory status. A nurse assesses a client with mitral valve stenosis. What clinical manifestation should alert the nurse to the possibility that the client's stenosis has progressed? a. Oxygen saturation of 92% b. Dyspnea on exertion c. Muted systolic murmur d. Upper extremity weakness ANS: B Dyspnea on exertion develops as the mitral valvular orifice narrows and pressure in the lungs increases. The other manifestations do not relate to the progression of mitral valve stenosis. A nurse cares for a client recovering from prosthetic valve replacement surgery. The client asks, "Why will I need to take anticoagulants for the rest of my life?" How should the nurse respond? a. "The prosthetic valve places you at greater risk for a heart attack." b. "Blood clots form more easily in artificial replacement valves." c. "The vein taken from your leg reduces circulation in the leg." d. "The surgery left a lot of small clots in your heart and lungs." ANS: B Synthetic valve prostheses and scar tissue provide surfaces on which platelets can aggregate easily and initiate the formation of blood clots. The other responses are inaccurate. After teaching a client who is being discharged home after mitral valve replacement surgery, the nurse assesses the client's understanding. Which client statement indicates a need for additional teaching? a. "I'll be able to carry heavy loads after 6 months of rest." b. "I will have my teeth cleaned by my dentist in 2 weeks." c. "I must avoid eating foods high in vitamin K, like spinach." d. "I must use an electric razor instead of a straight razor to shave." ANS: B Clients who have defective or repaired valves are at high risk for endocarditis. The client who has had valve surgery should avoid dental procedures for 6 months because of the risk for endocarditis. When undergoing a mitral valve replacement surgery, the client needs to be placed on anticoagulant therapy to prevent vegetation forming on the new valve. Clients on anticoagulant therapy should be instructed on bleeding precautions, including using an electric razor. If the client is prescribed warfarin, the client should avoid foods high in vitamin K. Clients recovering from open heart valve replacements should not carry anything heavy for 6 months while the chest incision and muscle heal. A nurse cares for a client with infective endocarditis. Which infection control precautions should the nurse use? a. Standard Precautions b. Bleeding precautions c. Reverse isolation d. Contact isolation ANS: A The client with infective endocarditis does not pose any specific threat of transmitting the causative organism. Standard Precautions should be used. Bleeding precautions or reverse or contact isolation is not necessary. A nurse assesses a client with pericarditis. Which assessment finding should the nurse expect to find? a. Heart rate that speeds up and slows down b. Friction rub at the left lower sternal border c. Presence of a regular gallop rhythm d. Coarse crackles in bilateral lung bases ANS: B The client with pericarditis may present with a pericardial friction rub at the left lower sternal border. This sound is the result of friction from inflamed pericardial layers when they rub together. The other assessments are not related. After teaching a client who is recovering from a heart transplant to change positions slowly, the client asks, "Why is this important?" How should the nurse respond? a. "Rapid position changes can create shear and friction forces, which can tear out your internal vascular sutures." b. "Your new vascular connections are more sensitive to position changes, leading to increased intravascular pressure and dizziness." c. "Your new heart is not connected to the nervous system and is unable to respond to decreases in blood pressure caused by position changes." d. "While your heart is recovering, blood flow is diverted away from the brain, increasing the risk for stroke when you stand up." ANS: C Because the new heart is denervated, the baroreceptor and other mechanisms that compensate for blood pressure drops caused by position changes do not function. This allows orthostatic hypotension to persist in the postoperative period. The other options are false statements and do not correctly address the client's question. A nurse teaches a client recovering from a heart transplant who is prescribed cyclosporine (Sandimmune). Which statement should the nurse include in this client's discharge teaching? a. "Use a soft-bristled toothbrush and avoid flossing." b. "Avoid large crowds and people who are sick." c. "Change positions slowly to avoid hypotension." d. "Check your heart rate before taking the medication." ANS: B These agents cause immune suppression, leaving the client more vulnerable to infection. The medication does not place the client at risk for bleeding, orthostatic hypotension, or a change in heart rate. A nurse cares for a client with end-stage heart failure who is awaiting a transplant. The client appears depressed and states, "I know a transplant is my last chance, but I don't want to become a vegetable." How should the nurse respond? a. "Would you like to speak with a priest or chaplain?" b. "I will arrange for a psychiatrist to speak with you." c. "Do you want to come off the transplant list?" d. "Would you like information about advance directives?" ANS: D The client is verbalizing a real concern or fear about negative outcomes of the surgery. This anxiety itself can have a negative effect on the outcome of the surgery because of sympathetic stimulation. The best action is to allow the client to verbalize the concern and work toward a positive outcome without making the client feel as though he or she is crazy. The client needs to feel that he or she has some control over the future. The nurse personally provides care to address the client's concerns instead of pushing the client's issues off on a chaplain or psychiatrist. The nurse should not jump to conclusions and suggest taking the client off the transplant list, which is the best treatment option. A nurse assesses a client who has a history of heart failure. Which question should the nurse ask to assess the extent of the client's heart failure? a. "Do you have trouble breathing or chest pain?" b. "Are you able to walk upstairs without fatigue?" c. "Do you awake with breathlessness during the night?" d. "Do you have new-onset heaviness in your legs?" ANS: B Clients with a history of heart failure generally have negative findings, such as shortness of breath. The nurse needs to determine whether the client's activity is the same or worse, or whether the client identifies a decrease in activity level. Trouble breathing, chest pain, breathlessness at night, and peripheral edema are symptoms of heart failure, but do not provide data that can determine the extent of the client's heart failure. A nurse cares for an older adult client with heart failure. The client states, "I don't know what to do. I don't want to be a burden to my daughter, but I can't do it alone. Maybe I should die." How should the nurse respond? a. "Would you like to talk more about this?" b. "You are lucky to have such a devoted daughter." c. "It is normal to feel as though you are a burden." d. "Would you like to meet with the chaplain?" ANS: A Depression can occur in clients with heart failure, especially older adults. Having the client talk about his or her feelings will help the nurse focus on the actual problem. Open-ended statements allow the client to respond safely and honestly. The other options minimize the client's concerns and do not allow the nurse to obtain more information to provide client-centered care. A nurse teaches a client with heart failure about energy conservation. Which statement should the nurse include in this client's teaching? a. "Walk until you become short of breath, and then walk back home." b. "Gather everything you need for a chore before you begin." c. "Pull rather than push or carry items heavier than 5 pounds." d. "Take a walk after dinner every day to build up your strength." ANS: B A client who has heart failure should be taught to conserve energy. Gathering all supplies needed for a chore at one time decreases the amount of energy needed. The client should not walk until becoming short of breath because he or she may not make it back home. Pushing a cart takes less energy than pulling or lifting. Although walking after dinner may help the client, the nurse should teach the client to complete activities when he or she has the most energy. This is usually in the morning. A nurse is caring for a client with acute pericarditis who reports substernal precordial pain that radiates to the left side of the neck. Which nonpharmacologic comfort measure should the nurse implement? a. Apply an ice pack to the client's chest. b. Provide a neck rub, especially on the left side. c. Allow the client to lie in bed with the lights down. d. Sit the client up with a pillow to lean forward on. ANS: D Pain from acute pericarditis may worsen when the client lays supine. The nurse should position the client in a comfortable position, which usually is upright and leaning slightly forward. Pain is decreased by using gravity to take pressure off the heart muscle. An ice pack and neck rub will not relieve this pain. A nurse assesses a client who has mitral valve regurgitation. For which cardiac dysrhythmia should the nurse assess? a. Preventricular contractions b. Atrial fibrillation c. Symptomatic bradycardia d. Sinus tachycardia ANS: B Atrial fibrillation is a clinical manifestation of mitral valve regurgitation and stenosis. Preventricular contractions and bradycardia are not associated with valvular problems. These are usually identified in clients with electrolyte imbalances, myocardial infarction, and sinus node problems. Sinus tachycardia is a manifestation of aortic regurgitation due to a decrease in cardiac output. A nurse is assessing a client with left-sided heart failure. For which clinical manifestations should the nurse assess? (Select all that apply.) a. Pulmonary crackles b. Confusion, restlessness c. Pulmonary hypertension d. Dependent edema e. Cough that worsens at night ANS: A, B, E Left-sided heart failure occurs with a decrease in contractility of the heart or an increase in afterload. Most of the signs will be noted in the respiratory system. Right-sided heart failure occurs with problems from the pulmonary vasculature onward including pulmonary hypertension. Signs will be noted before the right atrium or ventricle including dependent edema. A nurse evaluates laboratory results for a client with heart failure. Which results should the nurse expect? (Select all that apply.) a. Hematocrit: 32.8% b. Serum sodium: 130 mEq/L c. Serum potassium: 4.0 mEq/L d. Serum creatinine: 1.0 mg/dL e. Proteinuria f. Microalbuminuria ANS: A, B, E, F A hematocrit of 32.8% is low (should be 42.6%), indicating a dilutional ratio of red blood cells to fluid. A serum sodium of 130 mEq/L is low because of hemodilution. Microalbuminuria and proteinuria are present, indicating a decrease in renal filtration. These are early warning signs of decreased compliance of the heart. The potassium level is on the high side of normal and the serum creatinine level is normal. A nurse assesses clients on a cardiac unit. Which clients should the nurse identify as at greatest risk for the development of acute pericarditis? (Select all that apply.) a. A 36-year-old woman with systemic lupus erythematosus (SLE) b. A 42-year-old man recovering from coronary artery bypass graft surgery c. A 59-year-old woman recovering from a hysterectomy d. An 80-year-old man with a bacterial infection of the respiratory tract e. An 88-year-old woman with a stage III sacral ulcer ANS: A, B, D Acute pericarditis is most commonly associated acute exacerbations of systemic connective tissue disease, including SLE; with Dressler's syndrome, or inflammation of the cardiac sac after cardiac surgery or a myocardial infarction; and with infective organisms, including bacterial, viral, and fungal infections. Abdominal and reproductive surgeries and pressure ulcers do not increase clients' risk for acute pericarditis. After teaching a client with congestive heart failure (CHF), the nurse assesses the client's understanding. Which client statements indicate a correct understanding of the teaching related to nutritional intake? (Select all that apply.) a. "I'll read the nutritional labels on food items for salt content." b. "I will drink at least 3 liters of water each day." c. "Using salt in moderation will reduce the workload of my heart." d. "I will eat oatmeal for breakfast instead of ham and eggs." e. "Substituting fresh vegetables for canned ones will lower my salt intake." ANS: A, D, E Nutritional therapy for a client with CHF is focused on decreasing sodium and water retention to decrease the workload of the heart. The client should be taught to read nutritional labels on all food items, omit table salt and foods high in sodium (e.g., ham and canned foods), and limit water intake to a normal 2 L/day. A nurse collaborates with an unlicensed assistive personnel (UAP) to provide care for a client with congestive heart failure. Which instructions should the nurse provide to the UAP when delegating care for this client? (Select all that apply.) a. "Reposition the client every 2 hours." b. "Teach the client to perform deep-breathing exercises." c. "Accurately record intake and output." d. "Use the same scale to weigh the client each morning." e. "Place the client on oxygen if the client becomes short of breath." ANS: A, C, D The UAP should reposition the client every 2 hours to improve oxygenation and prevent atelectasis. The UAP can also accurately record intake and output, and use the same scale to weigh the client each morning before breakfast. UAPs are not qualified to teach clients or assess the need for and provide oxygen therapy. A nurse prepares to discharge a client who has heart failure. Based on the Heart Failure Core Measure Set, which actions should the nurse complete prior to discharging this client? (Select all that apply.) a. Teach the client about dietary restrictions. b. Ensure the client is prescribed an angiotensin-converting enzyme (ACE) inhibitor. c. Encourage the client to take a baby aspirin each day. d. Confirm that an echocardiogram has been completed. e. Consult a social worker for additional resources. ANS: A, B, D The Heart Failure Core Measure Set includes discharge instructions on diet, activity, medications, weight monitoring and plan for worsening symptoms, evaluation of left ventricular systolic function (usually with an echocardiogram), and prescribing an ACE inhibitor or angiotensin receptor blocker. Aspirin is not part of the Heart Failure Core Measure Set and is usually prescribed for clients who experience a myocardial infarction. Although the nurse may consult the social worker or case manager for additional resources, this is not part of the Core Measures. A nurse prepares to discharge a client who has heart failure. Which questions should the nurse ask to ensure this client's safety prior to discharging home? (Select all that apply.) a. "Are your bedroom and bathroom on the first floor?" b. "What social support do you have at home?" c. "Will you be able to afford your oxygen therapy?" d. "What spiritual beliefs may impact your recovery?" e. "Are you able to accurately weigh yourself at home?" ANS: A, B, D To ensure safety upon discharge, the nurse should assess for structural barriers to functional ability, such as stairs. The nurse should also assess the client's available social support, which may include family, friends, and home health services. The client's ability to adhere to medication and treatments, including daily weights, should also be reviewed. The other questions do not address the client's safety upon discharge. A nurse assesses a client who is recovering from a heart transplant. Which assessment findings should alert the nurse to the possibility of heart transplant rejection? (Select all that apply.) a. Shortness of breath b. Abdominal bloating c. New-onset bradycardia d. Increased ejection fraction e. Hypertension ANS: A, B, C Clinical manifestations of heart transplant rejection include shortness of breath, fatigue, fluid gain, abdominal bloating, new-onset bradycardia, hypotension, atrial fibrillation or flutter, decreased activity tolerance, and decreased ejection fraction. A nurse assesses a client who is diagnosed with infective endocarditis. Which assessment findings should the nurse expect? (Select all that apply.) a. Weight gain b. Night sweats c. Cardiac murmur d. Abdominal bloating e. Osler's nodes ANS: B, C, E Clinical manifestations of infective endocarditis include fever with chills, night sweats, malaise and fatigue, anorexia and weight loss, cardiac murmur, and Osler's nodes on palms of the hands and soles of the feet. Abdominal bloating is a manifestation of heart transplantation rejection. After receiving change-of-shift report about these four clients, which client should the nurse assess first? a. A 46-year-old with aortic stenosis who takes digoxin (Lanoxin) and has new-onset frequent premature ventricular contractions b. A 55-year-old admitted with pulmonary edema who received furosemide (Lasix) and whose current O2 saturation is 94% c. A 68-year-old with pericarditis who is reporting sharp, stabbing chest pain when taking deep breaths d. A 79-year-old admitted for possible rejection of a heart transplant who has sinus tachycardia, heart rate 104 beats/min a The 46-year-old's premature ventricular contractions may be indicative of digoxin toxicity; further assessment for clinical manifestations of digoxin toxicity should be done and the health care provider notified about the dysrhythmia. The 55-year-old is stable and can be assessed after the client with aortic stenosis. The 68-year-old may be assessed after the client with aortic stenosis; this type of pain is expected in pericarditis. Tachycardia is expected in the 79-year-old because rejection will cause signs of decreased cardiac output, including tachycardia; this client may be seen after the client with aortic stenosis. Which client is best to assign to an LPN/LVN working on the telemetry unit? A. Client with heart failure who is receiving dobutamine (Dobutrex) B. Client with dilated cardiomyopathy who uses oxygen for exertional dyspnea C. Client with pericarditis who has a paradoxical pulse and distended jugular veins D. Client with rheumatic fever who has a new systolic murmur B. The client with dilated cardiomyopathy who needs oxygen only with exertion is the most stable; administration of oxygen to a stable client is within the scope of LPN/LVN practice. The client with heart failure is receiving an intravenous inotropic agent, which requires monitoring by the RN. The client with pericarditis is displaying signs of cardiac tamponade and requires immediate lifesaving intervention. The client with a new-onset murmur requires assessment and notification of the provider, which is within the scope of practice of the RN. Chapter 36 A student nurse is assessing the peripheral vascular system of an older adult. What action by the student would cause the faculty member to intervene? a. Assessing blood pressure in both upper extremities b. Auscultating the carotid arteries for any bruits c. Classifying capillary refill of 4 seconds as normal d. Palpating both carotid arteries at the same time ANS: D The student should not compress both carotid arteries at the same time to avoid brain ischemia. Blood pressure should be taken and compared in both arms. Prolonged capillary refill is considered to be greater than 5 seconds in an older adult, so classifying refill of 4 seconds as normal would not require intervention. Bruits should be auscultated. The nurse is reviewing the lipid panel of a male client who has atherosclerosis. Which finding is most concerning? a. Cholesterol: 126 mg/dL b. High-density lipoprotein cholesterol (HDL-C): 48 mg/dL c. Low-density lipoprotein cholesterol (LDL-C): 122 mg/dL d. Triglycerides: 198 mg/dL ANS: D Triglycerides in men should be below 160 mg/dL. The other values are appropriate for adult males. The nurse is evaluating a 3-day diet history with a client who has an elevated lipid panel. What meal selection indicates the client is managing this condition well with diet? a. A 4-ounce steak, French fries, iceberg lettuce b. Baked chicken breast, broccoli, tomatoes c. Fried catfish, cornbread, peas d. Spaghetti with meat sauce, garlic bread ANS: B The diet recommended for this client would be low in saturated fats and red meat, high in vegetables and whole grains (fiber), low in salt, and low in trans fat. The best choice is the chicken with broccoli and tomatoes. The French fries have too much fat and the iceberg lettuce has little fiber. The catfish is fried. The spaghetti dinner has too much red meat and no vegetables. A nurse is working with a client who takes atorvastatin (Lipitor). The client's recent laboratory results include a blood urea nitrogen (BUN) of 33 mg/dL and creatinine of 2.8 mg/dL. What action by the nurse is best? a. Ask if the client eats grapefruit. b. Assess the client for dehydration. c. Facilitate admission to the hospital. d. Obtain a random urinalysis. ANS: A There is a drug-food interaction between statins and grapefruit that can lead to acute kidney failure. This client has elevated renal laboratory results, indicating some degree of kidney involvement. The nurse should assess if the client eats grapefruit or drinks grapefruit juice. Dehydration can cause the BUN to be elevated, but the elevation in creatinine is more specific for a kidney injury. The client does not necessarily need to be admitted. A urinalysis may or may not be ordered. A client has been diagnosed with hypertension but does not take the antihypertensive medications because of a lack of symptoms. What response by the nurse is best? a. "Do you have trouble affording your medications?" b. "Most people with hypertension do not have symptoms." c. "You are lucky; most people get severe morning headaches." d. "You need to take your medicine or you will get kidney failure. ANS: B Most people with hypertension are asymptomatic, although a small percentage do have symptoms such as headache. The nurse should explain this to the client. Asking about paying for medications is not related because the client has already admitted nonadherence. Threatening the client with possible complications will not increase compliance. A student nurse asks what "essential hypertension" is. What response by the registered nurse is best? a. "It means it is caused by another disease." b. "It means it is 'essential' that it be treated." c. "It is hypertension with no specific cause." d. "It refers to severe and life-threatening hypertension." ANS: C Essential hypertension is the most common type of hypertension and has no specific cause such as an underlying disease process. Hypertension that is due to another disease process is called secondary hypertension. A severe, life-threatening form of hypertension is malignant hypertension. A nurse is interested in providing community education and screening on hypertension. In order to reach a priority population, to what target audience should the nurse provide this service? a. African-American churches b. Asian-American groceries c. High school sports camps d. Women's health clinics ANS: A African Americans in the United States have one of the highest rates of hypertension in the world. The nurse has the potential to reach this priority population by providing services at African-American churches. Although hypertension education and screening are important for all groups, African Americans are the priority population for this intervention. A client has hypertension and high risk factors for cardiovascular disease. The client is overwhelmed with the recommended lifestyle changes. What action by the nurse is best? a. Assess the client's support system. b. Assist in finding one change the client can control. c. Determine what stressors the client faces in daily life. d. Inquire about delegating some of the client's obligations. ANS: B All opti ons are appropriate when assessing stress and responses to stress. However, this client feels overwhelmed by the suggested lifestyle changes. Instead of looking at all the needed changes, the nurse should assist the client in choosing one the client feels optimistic about controlling. Once the client has mastered that change, he or she can move forward with another change. Determining support systems, daily stressors, and delegation opportunities does not directly impact the client's feelings of control. The nurse is caring for four hypertensive clients. Which drug-laboratory value combination should the nurse report immediately to the health care provider? a. Furosemide (Lasix)/potassium: 2.1 mEq/L b. Hydrochlorothiazide (Hydrodiuril)/potassium: 4.2 mEq/L c. Spironolactone (Aldactone)/potassium: 5.1 mEq/L d. Torsemide (Demadex)/sodium: 142 mEq/L ANS: A Lasix is a loop diuretic and can cause hypokalemia. A potassium level of 2.1 mEq/L is quite low and should be reported immediately. Spironolactone is a potassium-sparing diuretic that can cause hyperkalemia. A potassium level of 5.1 mEq/L is on the high side, but it is not as critical as the low potassium with furosemide. The other two laboratory values are normal. A nurse is assessing a client with peripheral artery disease (PAD). The client states walking five blocks is possible without pain. What question asked next by the nurse will give the best information? a. "Could you walk further than that a few months ago?" b. "Do you walk mostly uphill, downhill, or on flat surfaces?" c. "Have you ever considered swimming instead of walking?" d. "How much pain medication do you take each day?" ANS: A As PAD progresses, it takes less oxygen demand to cause pain. Needing to cut down on activity to be pain free indicates the client's disease is worsening. The other questions are useful, but not as important. An older client with peripheral vascular disease (PVD) is explaining the daily foot care regimen to the family practice clinic nurse. What statement by the client may indicate a barrier to proper foot care? a. "I nearly always wear comfy sweatpants and house shoes." b. "I'm glad I get energy assistance so my house isn't so cold." c. "My daughter makes sure I have plenty of lotion for my feet." d. "My hands shake when I try to do things requiring coordination." ANS: D Clients with PVD need to pay special attention to their feet. Toenails need to be kept short and cut straight across. The client whose hands shake may cause injury when trimming toenails. The nurse should refer this client to a podiatrist. Comfy sweatpants and house shoes are generally loose and not restrictive, which is important for clients with PVD. Keeping the house at a comfortable temperature makes it less likely the client will use alternative heat sources, such as heating pads, to stay warm. The client should keep the feet moist and soft with lotion. A client is taking warfarin (Coumadin) and asks the nurse if taking St. John's wort is acceptable. What response by the nurse is best? a. "No, it may interfere with the warfarin." b. "There isn't any information about that." c. "Why would you want to take that?" d. "Yes, it is a good supplement for you." ANS: A Many foods and drugs interfere with warfarin, St. John's wort being one of them. The nurse should advise the client against taking it. The other answers are not accurate. A nurse is teaching a larger female client about alcohol intake and how it affects hypertension. The client asks if drinking two beers a night is an acceptable intake. What answer by the nurse is best? a. "No, women should only have one beer a day as a general rule." b. "No, you should not drink any alcohol with hypertension." c. "Yes, since you are larger, you can have more alcohol." d. "Yes, two beers per day is an acceptable amount of alcohol." ANS: A Alcohol intake should be limited to two drinks a day for men and one drink a day for women. A "drink" is classified as one beer, 1.5 ounces of hard liquor, or 5 ounces of wine. Limited alcohol intake is acceptable with hypertension. The woman's size does not matter. A nurse is caring for four clients. Which one should the nurse see first? a. Client who needs a beta blocker, and has a blood pressure of 92/58 mm Hg b. Client who had a first dose of captopril (Capoten) and needs to use the bathroom c. Hypertensive client with a blood pressure of 188/92 mm Hg d. Client who needs pain medication prior to a dressing change of a surgical wound ANS: B Angiotensin-converting enzyme inhibitors such as captopril can cause hypotension, especially after the first dose. The nurse should see this client first to prevent falling if the client decides to get up without assistance. The two blood pressure readings are abnormal but not critical. The nurse should check on the client with higher blood pressure next to assess for problems related to the reading. The nurse can administer the beta blocker as standards state to hold it if the systolic blood pressure is below 90 mm Hg. The client who needs pain medication prior to the dressing change is not a priority over client safety and assisting the other client to the bathroom. A client had a percutaneous transluminal coronary angioplasty for peripheral arterial disease. What assessment finding by the nurse indicates a priority outcome for this client has been met? a. Pain rated as 2/10 after medication b. Distal pulse on affected extremity 2+/4+ c. Remains on bedrest as directed d. Verbalizes understanding of procedure ANS: B Assessing circulation distal to the puncture site is a critical nursing action. A pulse of 2+/4+ indicates good perfusion. Pain control, remaining on bedrest as directed after the procedure, and understanding are all important, but do not take priority over perfusion. A client is 4 hours postoperative after a femoropopliteal bypass. The client reports throbbing leg pain on the affected side, rated as 7/10. What action by the nurse takes priority? a. Administer pain medication as ordered. b. Assess distal pulses and skin color. c. Document the findings in the client's chart. d. Notify the surgeon immediately. ANS: B Once perfusion has been restored or improved to an extremity, clients can often feel a throbbing pain due to the increased blood flow. However, it is important to differentiate this pain from ischemia. The nurse should assess for other signs of perfusion, such as distal pulses and skin color/temperature. Administering pain medication is done once the nurse determines the client's perfusion status is normal. Documentation needs to be thorough. Notifying the surgeon is not necessary. A client had a femoropopliteal bypass graft with a synthetic graft. What action by the nurse is most important to prevent wound infection? a. Appropriate hand hygiene before giving care b. Assessing the client's temperature every 4 hours c. Clean technique when changing dressings d. Monitoring the client's daily white blood cell count ANS: A Hand hygiene is the best way to prevent infections in hospitalized clients. Dressing changes should be done with sterile technique. Assessing vital signs and white blood cell count will not prevent infection. A client is receiving an infusion of alteplase (Activase) for an intra-arterial clot. The client begins to mumble and is disoriented. What action by the nurse takes priority? a. Assess the client's neurologic status. b. Notify the Rapid Response Team. c. Prepare to administer vitamin K. d. Turn down the infusion rate. ANS: B Clients on fibrinolytic therapy are at high risk of bleeding. The sudden onset of neurologic signs may indicate the client is having a hemorrhagic stroke. The nurse does need to complete a thorough neurological examination, but should first call the Rapid Response Team based on the client's manifestations. The nurse notifies the Rapid Response Team first. Vitamin K is not the antidote for this drug. Turning down the infusion rate will not be helpful if the client is still receiving any of the drug. A nursing student is caring for a client with an abdominal aneurysm. What action by the student requires the registered nurse to intervene? a. Assesses the client for back pain b. Auscultates over abdominal bruit c. Measures the abdominal girth d. Palpates the abdomen in four quadrants ANS: D Abdominal aneurysms should never be palpated as this increases the risk of rupture. The registered nurse should intervene when the student attempts to do this. The other actions are appropriate. A nurse is caring for a client with a deep vein thrombosis (DVT). What nursing assessment indicates a priority outcome has been met? a. Ambulates with assistance b. Oxygen saturation of 98% c. Pain of 2/10 after medication d. Verbalizing risk factors ANS: B A critical complication of DVT is pulmonary embolism. A normal oxygen saturation indicates that this has not occurred. The other assessments are also positive, but not the priority. A client has a deep vein thrombosis (DVT). What comfort measure does the nurse delegate to the unlicensed assistive personnel (UAP)? a. Ambulate the client. b. Apply a warm moist pack. c. Massage the client's leg. d. Provide an ice pack. ANS: B Warm moist packs will help with the pain of a DVT. Ambulation is not a comfort measure. Massaging the client's legs is contraindicated to prevent complications such as pulmonary embolism. Ice packs are not recommended for DVT. A nurse is assessing an obese client in the clinic for follow-up after an episode of deep vein thrombosis. The client has lost 20 pounds since the last visit. What action by the nurse is best? a. Ask if the weight loss was intended. b. Encourage a high-protein, high-fiber diet. c. Measure for new compression stockings. d. Review a 3-day food recall diary. ANS: C Compression stockings must fit correctly in order to work. After losing a significant amount of weight, the client should be re-measured and new stockings ordered if needed. The other options are appropriate, but not the most important. A nurse wants to provide community service that helps meet the goals of Healthy People 2020 (HP2020) related to cardiovascular disease and stroke. What activity would best meet this goal? a. Teach high school students heart-healthy living. b. Participate in blood pressure screenings at the mall. c. Provide pamphlets on heart disease at the grocery store. d. Set up an "Ask the nurse" booth at the pet store. ANS: B An important goal of HP2020 is to increase the proportion of adults who have had their blood pressure measured within the preceding 2 years and can state whether their blood pressure was normal or high. Participating in blood pressure screening in a public spot will best help meet that goal. The other options are all appropriate but do not specifically help meet a goal. A client has been diagnosed with a deep vein thrombosis and is to be discharged on warfarin (Coumadin). The client is adamant about refusing the drug because "it's dangerous." What action by the nurse is best? a. Assess the reason behind the client's fear. b. Remind the client about laboratory monitoring. c. Tell the client drugs are safer today than before. d. Warn the client about consequences of noncompliance. ANS: A The first step is to assess the reason behind the client's fear, which may be related to the experience of someone the client knows who took warfarin. If the nurse cannot address the specific rationale, teaching will likely be unsuccessful. Laboratory monitoring once every few weeks may not make the client perceive the drug to be safe. General statements like "drugs are safer today" do not address the root cause of the problem. Warning the client about possible consequences of not taking the drug is not therapeutic and is likely to lead to an adversarial relationship. A client with a history of heart failure and hypertension is in the clinic for a follow-up visit. The client is on lisinopril (Prinivil) and warfarin (Coumadin). The client reports new- onset cough. What action by the nurse is most appropriate? a. Assess the client's lung sounds and oxygenation. b. Instruct the client on another antihypertensive. c. Obtain a set of vital signs and document them. d. Remind the client that cough is a side effect of Prinivil. ANS: A This client could be having an exacerbation of heart failure or be experiencing a side effect of lisinopril (and other angiotensin-converting enzyme inhibitors). The nurse should assess the client's lung sounds and other signs of oxygenation first. The client may or may not need to switch antihypertensive medications. Vital signs and documentation are important, but the nurse should assess the respiratory system first. If the cough turns out to be a side effect, reminding the client is appropriate, but then more action needs to be taken. A nurse is caring for a client with a nonhealing arterial lower leg ulcer. What action by the nurse is best? a. Consult with the Wound Ostomy Care Nurse. b. Give pain medication prior to dressing changes. c. Maintain sterile technique for dressing changes. d. Prepare the client for eventual amputation. ANS: A A nonhealing wound needs the expertise of the Wound Ostomy Care Nurse (or Wound Ostomy Continence Nurse). Premedicating prior to painful procedures and maintaining sterile technique are helpful, but if the wound is not healing, more needs to be done. The client may need an amputation, but other options need to be tried first. A client has peripheral arterial disease (PAD). What statement by the client indicates misunderstanding about self-management activities? a. "I can use a heating pad on my legs if it's set on low." b. "I should not cross my legs when sitting or lying down." c. "I will go out and buy some warm, heavy socks to wear." d. "It's going to be really hard but I will stop smoking." ANS: A Clients with PAD should never use heating pads as skin sensitivity is diminished and burns can result. The other statements show good understanding of self-management. A client presents to the emergency department with a severely lacerated artery. What is the priority action for the nurse? a. Administer oxygen via non-rebreather mask. b. Ensure the client has a patent airway. c. Prepare to assist with suturing the artery. d. Start two large-bore IVs with normal saline. ANS: B Airway always takes priority, followed by breathing and circulation. The nurse ensures the client has a patent airway prior to providing any other care measures. The nurse is assessing a client on admission to the hospital. The client's leg appears as shown below: What action by the nurse is best? a. Assess the client's ankle-brachial index. b. Elevate the client's leg above the heart. c. Obtain an ice pack to provide comfort. d. Prepare to teach about heparin sodium. ANS: A This client has dependent rubor, a classic finding in peripheral arterial disease. The nurse should measure the client's ankle-brachial index. Elevating the leg above the heart will further impede arterial blood flow. Ice will cause vasoconstriction, also impeding circulation and perhaps causing tissue injury. Heparin sodium is not the drug of choice for this condition. What nonpharmacologic comfort measures should the nurse include in the plan of care for a client with severe varicose veins? (Select all that apply.) a. Administering mild analgesics for pain b. Applying elastic compression stockings c. Elevating the legs when sitting or lying d. Reminding the client to do leg exercises e. Teaching the client about surgical options ANS: B, C, D The three E's of care for varicose veins include elastic compression hose, exercise, and elevation. Mild analgesics are not a nonpharmacologic measure. Teaching about surgical options is not a comfort measure. A nurse is preparing a client for a femoropopliteal bypass operation. What actions does the nurse delegate to the unlicensed assistive personnel (UAP)? (Select all that apply.) a. Administering preoperative medication b. Ensuring the consent is signed c. Marking pulses with a pen d. Raising the siderails on the bed e. Recording baseline vital signs ANS: D, E The UAP can raise the siderails of the bed for client safety and take and record the vital signs. Administering medications, ensuring a consent is on the chart, and marking the pulses for later comparison should be done by the registered nurse. This is also often done by the postanesthesia care nurse and is part of the hand-off report. A client has been bedridden for several days after major abdominal surgery. What action does the nurse delegate to the unlicensed assistive personnel (UAP) for deep vein thrombosis (DVT) prevention? (Select all that apply.) a. Apply compression stockings. b. Assist with ambulation. c. Encourage coughing and deep breathing. d. Offer fluids frequently. e. Teach leg exercises. ANS: A, B, D The UAP can apply compression stockings, assist with ambulation, and offer fluids frequently to help prevent DVT. The UAP can also encourage the client to do pulmonary exercises, but these do not decrease the risk of DVT. Teaching is a nursing function. A nurse is caring for a client on IV infusion of heparin. What actions does this nurse include in the client's plan of care? (Select all that apply.) a. Assess the client for bleeding. b. Monitor the daily activated partial thromboplastin time (aPTT) results. c. Stop the IV for aPTT above baseline. d. Use an IV pump for the infusion. e. Weigh the client daily on the same scale ANS: A, B, D Assessing for bleeding, monitoring aPTT, and using an IV pump for the infusion are all important safety measures for heparin to prevent injury from bleeding. The aPTT needs to be 1.5 to 2 times normal in order to demonstrate that the heparin is therapeutic. Weighing the client is not related. A client is being discharged on warfarin (Coumadin) therapy. What discharge instructions is the nurse required to provide? (Select all that apply.) a. Dietary restrictions b. Driving restrictions c. Follow-up laboratory monitoring d. Possible drug-drug interactions e. Reason to take medication ANS: A, C, D, E The Joint Commission's Core Measures state that clients being discharged on warfarin need instruction on follow-up monitoring, dietary restrictions, drug-drug interactions, and reason for compliance. Driving is typically not restricted. Which statements by the client indicate good understanding of foot care in peripheral vascular disease? (Select all that apply.) a. "A good abrasive pumice stone will keep my feet soft." b. "I'll always wear shoes if I can buy cheap flip-flops." c. "I will keep my feet dry, especially between the toes." d. "Lotion is important to keep my feet smooth and soft." e. "Washing my feet in room-temperature water is best." ANS: C, D, E Good foot care includes appropriate hygiene and injury prevention. Keeping the feet dry; wearing good, comfortable shoes; using lotion; washing the feet in room- temperature water; and cutting the nails straight across are all important measures. Abrasive material such as pumice stones should not be used. Cheap flip-flops may not fit well and won't offer much protection against injury. A nurse is caring for a client with a nonhealing arterial ulcer. The physician has informed the client about possibly needing to amputate the client's leg. The client is crying and upset. What actions by the nurse are best? (Select all that apply.) a. Ask the client to describe his or her current emotions. b. Assess the client for support systems and family. c. Offer to stay with the client if he or she desires. d. Relate how smoking contributed to this situation. e. Tell the client that many people have amputations. ANS: A, B, C When a client is upset, the nurse should offer self by remaining with the client if desired. Other helpful measures include determining what and whom the client has for support systems and asking the client to describe what he or she is feeling. Telling the client how smoking has led to this situation will only upset the client further and will damage the therapeutic relationship. Telling the client that many people have amputations belittles the client's feelings. The nurse working in the emergency department knows that which factors are commonly related to aneurysm formation? (Select all that apply.) a. Atherosclerosis b. Down syndrome c. Frequent heartburn d. History of hypertension e. History of smoking ANS: A, D, E Atherosclerosis, hypertension, hyperlipidemia, and smoking are the most common related factors. Down syndrome and heartburn have no relation to aneurysm formation. A client with a known abdominal aortic aneurysm reports dizziness and severe abdominal pain. The nurse assesses the client's blood pressure at 82/40 mm Hg. What actions by the nurse are most important? (Select all that apply.) a. Administer pain medication. b. Assess distal pulses every 10 minutes. c. Have the client sign a surgical consent. d. Notify the Rapid Response Team. e. Take vital signs every 10 minutes. ANS: B, D, E This client may have a ruptured/rupturing aneurysm. The nurse should notify the Rapid Response team and perform frequent client assessments. Giving pain medication will lower the client's blood pressure even further. The nurse cannot have the client sign a consent until the physician has explained the procedure. A nurse is caring for a client who weighs 220 pounds and is started on enoxaparin (Lovenox). How much enoxaparin does the nurse anticipate administering? (Record your answer using a whole number.) mg ANS: 90 mg The dose of enoxaparin is 1 mg/kg body weight, not to exceed 90 mg. This client weighs 220 pounds (110 kg), and so will get the maximal dose. Chapter 40 The nurse is caring for a client with sickle cell disease. Which action is most effective in reducing the potential for sepsis in this client? a) Administering prophylactic drug therapy b) Frequent and thorough handwashing c) Monitoring laboratory values to look for abnormalities d) Taking vital signs every 4 hours, day and night Correct Answer: b Prevention and early detection strategies are used to protect the client in sickle cell crisis from infection. Frequent and thorough handwashing is of the utmost importance. Drug therapy is a major defense against infections that develop in the client with sickle cell disease, but is not the most effective way that the nurse can reduce the potential for sepsis. Continually assessing the client for infection and monitoring the daily complete blood count with differential white blood cell count is early detection, not prevention. Taking vital signs every 4 hours will help with early detection of infection, but is not prevention. Which intervention most effectively protects a client with thrombocytopenia? a) Avoiding the use of dentures b) Encouraging the use of an electric shaver c) Taking rectal temperatures d) Using warm compresses on trauma sites Correct Answer: b The client with thrombocytopenia should be advised to use an electric shaver instead of a razor. Any small cuts or nicks can cause problems because of the prolonged clotting time. Dentures may be used by clients with thrombocytopenia as long as they fit properly and do not rub. To prevent rectal trauma, rectal thermometers should not be used. Oral or tympanic temperatures should be taken. Ice (not heat) should be applied to areas of trauma. A client with leukemia is being discharged from the hospital. After hearing the nurse's instructions to keep regularly scheduled follow-up provider appointments, the client says, "I don't have transportation." How does the nurse respond? a) "A pharmaceutical company might be able to help." b) "I might be able to take you." c) "The local American Cancer Society may be able to help." d) "You can take the bus." Correct Answer: c Many local units of the American Cancer Society offer free transportation to clients with cancer, including those with leukemia. Suggesting a pharmaceutical company is not the best answer; drug companies typically do not provide this type of service. Although the nurse offering to take the client is compassionate, it is not appropriate for the nurse to offer the client transportation. Telling the client to take the bus is dismissive and does not take into consideration the client's situation (e.g., the client may live nowhere near a bus route). Which client statement indicates that stem cell transplantation that is scheduled to take place in his home is not a viable option? a) "I don't feel strong enough, but my wife said she would help." b) "I was a nurse, so I can take care of myself." c) "I will have lots of medicine to take." d) "We live 5 miles from the hospital." Correct Answer: b Stem cell transplantation in the home setting requires support, assistance, and coordination from others. The client cannot manage this type of care on his own. The client must be emotionally stable to be a candidate for this type of care. It is acceptable for the client's spouse to support the client undergoing this procedure. It is not unexpected for the client to be taking several prescriptions. Five miles is an acceptable distance from the hospital, in case of emergency. The nurse is to administer packed red blood cells to a client. How does the nurse ensure proper client identification? a) Asks the client's name b) Checks the client's armband c) Reviews all information with another registered nurse d) Verifies the client's room number Correct Answer: c With another registered nurse, verify the client by name and number, check blood compatibility, and note expiration time. Human error is the most common cause of ABO incompatibility reactions, even for experienced nurses. Asking the client's name and checking the client's armband are not adequate for identifying the client before transfusion therapy. Using the room number to verify client identification is never appropriate. What is the most important environmental risk for developing leukemia? a) Direct contact with others with leukemia b) Family history c) Living near high-voltage power lines d) Smoking cigarettes Correct Answer: d According to the American Cancer Society (ACS), the only proven lifestyle-related risk factor for leukemia is cigarette smoking. Leukemia is not contagious. Genetics is a strong indicator, but it is not an environmental risk factor. According to the ACS, living near high-voltage power lines is not a proven risk factor for leukemia. A client who has been newly diagnosed with leukemia is admitted to the hospital. Avoiding which potential problem takes priority in the client's nursing care plan? a) Fluid overload (overhydration) b) Hemorrhage c) Hypoxia d) Infection Correct Answer: d The main objective in caring for a newly diagnosed client with leukemia is protection from infection. Fluid overload, hemorrhage, and hypoxia are not priority problems for the client with leukemia. The nurse is assessing the endurance level of a client in a long-term care facility. What question does the nurse ask to get this information? a) "Are your feet or hands cold, even when you are in bed?" b) "Do you feel more tired after you get up and go to the bathroom?" c) "How much exercise do you get?" d) "What is your endurance level?" Correct Answer: b Asking about feeling tired after using the bathroom is pertinent to the client's activity and provides a comparison. The specific activity helps the client relate to the question and provide needed answers. Asking about cold feet or hands does not address the client's endurance. The hospitalized client typically does not get much exercise; this would be a difficult assessment for a client in long-term care facility to make. Asking the client about his or her endurance level is too vague; the client may not know how to answer this question. The nurse is teaching a client with vitamin B12 deficiency anemia about dietary intake. Which type of food does the nurse encourage the client to eat? a) Dairy products b) Grains c) Leafy vegetables d) Starchy vegetables Correct Answer: a Dairy products such as milk, cheese, and eggs will provide the vitamin B12 that the client needs. Grains, leafy vegetables, and starchy vegetables are not a source of vitamin B12. A client with thrombocytopenia is being discharged. What information does the nurse incorporate into the teaching plan for this client? a) "Avoid large crowds." b) "Drink at least 2 liters of fluid per day." c) "Elevate your lower extremities when sitting." d) "Use a soft-bristled toothbrush." Correct Answer: d Using a soft-bristled toothbrush reduces the risk for bleeding in the client with thrombocytopenia. Avoiding large crowds reduces the risk for infection, but is not specific to the client with thrombocytopenia. Increased fluid intake reduces the risk for dehydration, but is not specific to the client with thrombocytopenia. Elevating extremities reduces the risk for dependent edema, but is not specific to the client with thrombocytopenia. The nurse is teaching a client about induction therapy for acute leukemia. Which client statement indicates a need for additional education? a) "After this therapy, I will not need to have any more." b) "I will need to avoid people with a cold or flu." c) "I will probably lose my hair during this therapy." d) "The goal of this therapy is to put me in remission." Correct Answer: a Induction therapy is not a cure for leukemia, it is a treatment; therefore, the client needs more education to understand this. Because of infection risk, clients with leukemia should avoid people with a cold or flu. Induction therapy will most likely cause the client with leukemia to lose his or her hair. The goal of induction therapy is to force leukemia into remission. A client with multiple myeloma reports bone pain that is unrelieved by analgesics. How does the nurse respond to this client's problem? a) "Ask your doctor to prescribe more medication." b) "It is too soon for additional medication to be given." c) "I'll turn on some soothing classical music for you." d) "Would you like to try some relaxation techniques?" Correct Answer: d Because most clients with multiple myeloma have local or generalized bone pain, analgesics and alternative approaches for pain management, such as relaxation techniques, are used for pain relief. This also offers the client a choice. Before prescribing additional medication, other avenues should be explored to relieve this client's pain. Even if it is too soon to give additional medication, telling that to the client is not helpful because it dismisses the client's pain concerns. Although music therapy can be helpful, this response does not give the client a choice. The nurse is reinforcing information about genetic counseling to a client with sickle cell disease who has a healthy spouse. What information does the nurse include? a) "Sickle cell disease will be inherited by your children." b) "The sickle cell trait will be inherited by your children." c) "Your children will have the disease, but your grandchildren will not." d) "Your children will not have the disease, but your grandchildren could." Correct Answer: b The children of the client with sickle cell disease will inherit the sickle cell trait, but may not inherit the disease. If both parents have the sickle cell trait, their children could get the disease. The nurse is caring for a client who is in sickle cell crisis. What action does the nurse perform first? a) Apply cool compresses to the client's forehead. b) Encourage the client's use of two methods of birth control. c) Increase food sources of iron in the client's diet. d) Provide pain medications as needed. Correct Answer: d Analgesics are needed to treat sickle cell pain. Warm soaks or compresses can help reduce pain perception. Cool compresses do not help the client in sickle cell crisis. Birth control is not the priority for this client. Increasing iron in the diet is not pertinent for the client in sickle cell crisis. The nurse is caring for a client with neutropenia. Which clinical manifestation indicates that an infection is present or should be ruled out? a) Coughing and deep breathing b) Evidence of pus c) Fever of 102° F or higher d) Wheezes or crackles Correct Answer: d Wheezes or crackles in the neutropenic client may be the first symptom of infection in the lungs. Coughing and deep breathing are not indications of infection, but can help prevent it. The client with leukopenia, not neutropenia, may have a severe infection without pus or with only a low-grade fever. The nurse is caring for a client with neutropenia who has a suspected infection. Which intervention does the nurse implement first? a) Hydrate the client with 1000 mL of IV normal saline. b) Initiate the administration of prescribed antibiotics. c) Obtain requested cultures. d) Place the client on Bleeding Precautions. Correct Answer: c Obtaining cultures to identify the infectious agent correctly is the priority for this client. Hydrating the client is not the priority. Administering antibiotics is important, but antibiotics should always be started after cultures are obtained. Placing the client on Bleeding Precautions is unnecessary. The nurse is assessing a newly admitted client with thrombocytopenia. Which factor needs immediate intervention? a) Nosebleed b) Reports of pain c) Decreased urine output d) Increased temperature Correct Answer: a The client with thrombocytopenia has a high risk for bleeding. The nosebleed should be attended to immediately. The client's report of pain, decreased urine output, and increased temperature are not the highest priority. A client who is receiving a blood transfusion suddenly exclaims to the nurse, "I don't feel right!" What does the nurse do next? a) Call the Rapid Response Team. b) Obtain vital signs and continue to monitor. c) Slow the infusion rate of the transfusion. d) Stop the transfusion. Correct Answer: d The client may be experiencing a transfusion reaction; the nurse should stop the transfusion immediately. Calling the Rapid Response Team or obtaining vital signs is not the first thing that should be done. The nurse should not slow the infusion rate, but should stop it altogether. Which client is at greatest risk for having a hemolytic transfusion reaction? a) A 34-year-old client with type O blood b) A 42-year-old client with allergies c) A 58-year-old immune-suppressed client d) A 78-year-old client Correct Answer: a Hemolytic transfusion reactions are caused by blood type or Rh incompatibility. When blood that contains antigens different from the client's own antigens is infused, antigen- antibody complexes are formed in the client's blood. Type O is considered the universal donor, but not the universal recipient. The client with allergies would be most susceptible to an allergic transfusion reaction. The immune-suppressed client would be most susceptible to a transfusion-associated graft-versus-host disease. The older adult client would be most susceptible to circulatory overload. The nurse is educating a group of young women who have sickle cell disease (SCD). Which comment from a class member requires correction? a) "Frequent handwashing is an important habit for me to develop." b) "Getting an annual 'flu shot' would be dangerous for me." c) "I must take my penicillin pills as prescribed, all the time." d) "The pneumonia vaccine is protection that I need." Correct Answer: b The client with SCD should receive annual influenza and pneumonia vaccinations; this helps prevent the development of these infections, which could cause a sickle cell crisis. Handwashing is a very important habit for the client with SCD to develop because it reduces the risk for infection. Prophylactic penicillin is given to clients with SCD orally twice a day to prevent the development of infection. The nurse is transfusing 2 units of packed red blood cells to a postoperative client. What post-transfusion electrolyte imbalance does the nurse want to rule out? a) Hypercalcemia b) Hyperkalemia c) Hypomagnesemia d) Hyponatremia Correct Answer: b During transfusion, some cells are damaged. These cells release potassium, thus raising the client's serum potassium level (hyperkalemia). This complication is especially common with packed cells and whole-blood products. High serum calcium levels, low magnesium levels, or low sodium levels are not expected with blood transfusions. The nurse is infusing platelets to a client who is scheduled for a hematopoietic stem cell transplant. What procedure does the nurse follow? a) Administer intravenous corticosteroids before starting the transfusion. b) Allow the platelets to stabilize at the client's bedside for 30 minutes. c) Infuse the transfusion over a 15- to 30-minute period. d) Set up the infusion with the standard transfusion Y tubing. Correct Answer: c The volume of platelets—200 or 300 mL (standard amount)—needs to be infused rapidly over a 15- to 30-minute period. Administering steroids is not standard practice in administering platelets. Platelets must be administered immediately after they are received; they are considered to be quite fragile. A special transfusion set with a smaller filter and shorter tubing is used to get the platelets into the client quickly and efficiently. The nurse is mentoring a recent graduate RN about administering blood and blood products. What does the nurse include in the data? a) Obtain the client's initial set of vital signs (VS) within the first 10 minutes of the infusion. b) Remain with the client who is receiving the blood for the first 5 minutes of the infusion. c) Use a 22-gauge needle to obtain venous access when starting the infusion. d) Verify with another RN all of the data on blood products. Correct Answer: d All data are checked by two RNs. Human error is the most common cause of ABO incompatibilities in administering blood and blood products. Initial VS should be recorded before the start of infusion of blood, not after it has begun. The nurse remains with the client for the first 15 to 30 minutes (not 5) of the infusion. This is the period when any transfusion reactions are likely to happen. A 20-gauge needle (or a central line catheter) is used; the 22-gauge needle is too small. An RN from pediatrics has "floated" to the medical-surgical unit. Which client is assigned to the float nurse? a) A 42-year-old with sickle cell disease receiving a transfusion of packed red blood cells b) A 50-year-old with pancytopenia needing assessment of risk factors for aplastic anemia c) A 55-year-old with folic acid deficiency anemia caused by alcohol abuse who needs counseling d) A 60-year-old with newly diagnosed polycythemia vera who needs teaching about the disease Correct Answer: a Because sickle cell disease is commonly diagnosed during childhood, the pediatric nurse will be familiar with the disease and with red blood cell transfusion; therefore, he or she should be assigned to the client with sickle cell disease. Aplastic anemia, folic acid deficiency, and polycythemia vera are problems more commonly seen in adult clients who should be cared for by nurses who are more experienced in caring for adults. Which would be an appropriate task to delegate to unlicensed assistive personnel (UAP) working on a medical-surgical unit? a) Administering erythropoietin to a client with myelodysplastic syndrome b) Assessing skin integrity on an anemic client who fell during ambulation c) Assisting a client with folic acid deficiency in making diet choices d) Obtaining vital signs on a client receiving a blood transfusion Correct Answer: d Obtaining vital signs on a client is within the scope of practice for UAP. Administering medication, assessing clients, and assisting with prescribed diet choices are complex actions that should be done by licensed nurses. A hematology unit is staffed by RNs, LPN/LVNs, and unlicensed assistive personnel (UAP). When the nurse manager is reviewing documentation of staff members, which entry indicates that the staff member needs education about his or her appropriate level of responsibility and client care? a) "Abdominal pain relieved by morphine 4 mg IV; client resting comfortably and denies problems. B.C., RN" b) "Ambulated in hallway for 40 feet and denies shortness of breath at rest or with ambulation. T.Y., LPN" c) "Client reporting increased shortness of breath; oxygen increased to 4 L by nasal cannula. M.N., UAP" d) "Vital signs 37.0° C, heart rate 60, respiratory rate 20, blood pressure 110/68, and oximetry 98% on room air. L.D., UAP" Correct Answer: c Determination of the need for oxygen and administration of oxygen should be done by licensed nurses who have the education and scope of practice required to administer it. All other documentation entries reflect appropriate delegation and assignment of care. The nurse assesses the client with which hematologic problem first? a) A 32-year-old with pernicious anemia who needs a vitamin B12 injection b) A 40-year-old with iron deficiency anemia who needs a Z-track iron injection c) A 67-year-old with acute myelocytic leukemia with petechiae on both legs d) An 81-year-old with thrombocytopenia and an increase in abdominal girth Correct Answer: d An increase in abdominal girth in a client with thrombocytopenia indicates possible hemorrhage; this warrants further assessment immediately. The 32-year-old with pernicious anemia, the 40-year-old with iron deficiency anemia, and the 67-year-old with acute myelocytic leukemia do not indicate any acute complications, so the nurse can assess them after assessing the client with thrombocytopenia. The nurse assesses multiple clients who are receiving transfusions of blood components. Which assessment indicates the need for the nurse's immediate action? a) A partial thromboplastin time (PTT) that is 1.2 times normal in a client who received a transfusion of fresh-frozen plasma (FFP) b) Respiratory rate of 36 breaths/min in a client receiving red blood cells c) Sleepiness in a client who received diphenhydramine (Benadryl) as a premedication d) Temperature of 99.1° F (37.3° C) for a client with a platelet transfusion Correct Answer: b An increased respiratory rate indicates a possible hemolytic transfusion reaction; the nurse should quickly stop the transfusion and assess the client further. Because FFP is not usually given until the PTT is 1.5 times above normal, a PTT that is 1.2 times normal indicates that the FFP has had the desired response. Sleepiness is expected when Benadryl is administered. Temperature elevations are not an indication of an allergic reaction to a platelet transfusion, although the nurse may administer acetaminophen (Tylenol) to decrease the fever. Which client does the nurse assign as a roommate for the client with aplastic anemia? a) A 23-year-old with sickle cell disease who has two draining leg ulcers b) A 28-year-old with glucose-6-phosphate dehydrogenase (G6PD) deficiency anemia who is receiving mannitol (Osmitrol) c) A 30-year-old with leukemia who is receiving induction chemotherapy d) A 34-year-old with idiopathic thrombocytopenia who is taking steroids Correct Answer: b Because clients with aplastic anemia usually have low white blood cell counts that place them at high risk for infection, roommates such as the client with G6PD deficiency anemia should be free from infection or infection risk. The client with sickle cell disease has two draining leg ulcer infections that would threaten the diminished immune system of the client with aplastic anemia. The client with leukemia who is receiving induction chemotherapy and the client with idiopathic thrombocytopenia who is taking steroids are at risk for development of infection, which places the client with aplastic anemia at risk, too. The nurse is transfusing a unit of whole blood to a client when the health care provider requests the following: "Furosemide (Lasix) 20 mg IV push." What does the nurse do? a) Add furosemide to the normal saline that is infusing with the blood. b) Administer furosemide to the client intramuscularly (IM). c) Piggyback furosemide into the infusing blood. d) Wait until the transfusion has been completed to administer furosemide. Correct Answer: d Completing the transfusion before administering furosemide is the best course of action in this scenario. Drugs are not to be administered with infusing blood products; they can interact with the blood, causing risks for the client. Stopping the infusing blood to administer the drug and then restarting it is also not the best decision. Changing the admission route is not a nursing decision. A 56-year-old client admitted with a diagnosis of acute myelogenous leukemia is prescribed IV cytosine arabinoside for 7 days and an infusion of daunorubicin for the first 3 days. What is the major side effect of this therapy? a) Bone marrow suppression b) Liver toxicity c) Nausea d) Stomatitis Correct Answer: a Intravenous cytosine arabinoside and daunorubicin are a commonly prescribed course of aggressive chemotherapy, and bone marrow suppression is a major side effect. The client is even more at risk for infection than before treatment began. Liver toxicity, nausea, and stomatitis are not the major problems with this therapy. A 56-year-old client admitted with a diagnosis of acute myelogenous leukemia (AML) is prescribed IV cytosine arabinoside for 7 days and an infusion of daunorubicin for the first 3 days. An infection develops. What knowledge does the nurse use to determine that the appropriate antibiotic has been prescribed for this client? a) Evaluating the client's liver function tests (LFTs) and serum creatinine levels b) Evaluating the client's white blood cell (WBC) count level c) Checking the culture and sensitivity test results to be certain that the requested antibiotic is effective against the organism causing the infection d) Recognizing that vancomycin (Vancocin) is the drug of choice used to treat all infections in clients with AML Correct Answer: c Checking the culture and sensitivity test results to be certain that the requested antibiotic is effective against the organism causing the infection is the best action to take. Drug therapy is the main defense against infections that develop in clients undergoing therapy for AML. Agents used depend on the client's sensitivity to various antibiotics for the organism causing the infection. Although LFTs and kidney function tests may be influenced by antibiotics, these tests do not determine the effectiveness of the antibiotic. Although the WBC count is elevated in infection, this test does not influence which antibiotic will be effective in fighting the infection. Vancomycin may not be effective in all infections; culturing of the infection site and determining the organism's sensitivity to a cohort of drugs are needed, which will provide data on drugs that are capable of eradicating the infection in this client. A 32-year-old client is recovering from a sickle cell crisis. His discomfort is controlled with pain medications and he is to be discharged. What medication does the nurse expect to be prescribed for him before his discharge? a) Heparin (Heparin) b) Hydroxyurea (Droxia) c) Tissue plasminogen activator (t-PA) d) Warfarin (Coumadin) Correct Answer: b Hydroxyurea (Droxia) has been used successfully to reduce sickling of cells and pain episodes associated with sickle cell disease (SCD). Clients with SCD are not prescribed anticoagulants such as heparin or warfarin (Coumadin). t-PA is used as a "clot buster" in clients who have had ischemic strokes. A 32-year-old client recovering from a sickle cell crisis is to be discharged. The nurse says, "You and all clients with sickle cell disease are at risk for infection because of your decreased spleen function. For this reason, you will most likely be prescribed an antibiotic before discharge." Which drug does the nurse anticipate the health care provider will request? a) Cefaclor (Ceclor) b) Gentamicin (Garamycin) c) Penicillin V (Pen-V K) d) Vancomycin (Vancocin) Correct Answer: c Prophylactic therapy with twice-daily oral penicillin reduces the incidence of pneumonia and other streptococcal infections and is the correct drug to use. It is a standard protocol for long-term prophylactic use in clients with sickle cell disease. Cefaclor (Ceclor) and vancomycin (Vancocin) are antibiotics more specific for short-term use and would be inappropriate for this client. Gentamicin (Garamycin) is a drug that can cause liver and kidney damage with long-term use. A recently admitted client who is in sickle cell crisis requests "something for pain." What does the nurse administer? a) Intramuscular (IM) morphine sulfate b) Intravenous (IV) hydromorphone (Dilaudid) c) Oral ibuprofen (Motrin) d) Oral morphine sulfate (MS-Contin) Correct Answer: b The client needs IV pain relief, and it should be administered on a routine schedule (i.e., before the client has to request it). Morphine is not administered intramuscularly (IM) to clients with sickle cell disease (SCD). In fact, all IM injections are avoided because absorption is impaired by poor perfusion and sclerosed skin. Nonsteroidal anti- inflammatory drugs may be used for clients with SCD for pain relief once their pain is under control; however, in a crisis, this choice of analgesic is not strong enough. Moderate pain may be treated with oral opioids, but this client is in a sickle cell crisis; IV analgesics should be used until his or her condition stabilizes. A distant family member arrives to visit a female client recently diagnosed with leukemia. The family member asks the nurse, "What should I say to her?" Which responses does the nurse suggest? (Select all that apply.) a) "Ask her how she is feeling." b) "Ask her if she needs anything." c) "Tell her to be brave and to not cry." d) "Talk to her as you normally would when you haven't seen her for a long time." e) "Tell her what you know about leukemia." Correct Answers: a, b, d Asking the client how she is feeling is a broad general opening and would be nonthreatening to the client. Asking if she needs anything is a therapeutic communication of offering self and would be considered to be therapeutic and helpful to the client. The family member should talk to her as she normally would when she hasn't seen her in a long time. There is no need to act differently with the client. If she wants to offer her feelings, keeping a normal atmosphere facilitates that option. Acting as if things are "different" because she has cancer takes the control of the situation from the client. Telling her to be brave and not to cry is callous and unfeeling; if the client is feeling vulnerable and depressed, telling her to "be brave" shuts off any opportunity for her to express her feelings. There is no need to inform the client about her disease, unless she asks about it. Opening the conversation with discussion about leukemia should be the client's prerogative. What are the typical clinical manifestations of anemia? (Select all that apply.) a) Decreased breath sounds b) Dyspnea on exertion c) Elevated temperature d) Fatigue e) Pallor f) Tachycardia Correct Answers: b, d, e, f Difficulty breathing—especially with activity—is common with anemia. Lower levels of hemoglobin carry less O2 to the cells of the body. Fatigue is a classic symptom of anemia; lowered O2 levels contribute to a faster pulse (i.e., cardiac rate) and tend to "wear out" a client's energy. Lowered O2 levels deliver less oxygen to all cells, making clients with anemia pale—especially their ears, nail beds, palms, and conjunctivae and around the mouth. Respiratory problems with anemia do not include changes in breath sounds; dyspnea and decreased oxygen saturation levels are present. Skin is cool to the touch, and an intolerance to cold is noted; elevated temperature would signify something additional, such as infection. What are the risk factors for the development of leukemia? (Select all that apply.) a) Bone marrow hypoplasia b) Chemical exposure c) Down syndrome d) Ionizing radiation e) Multiple blood transfusions f) Prematurity at birth Correct Answers: a, b, c, d Reduced production of blood cells in the bone marrow is one of the risk factors for developing leukemia. Exposure to chemicals through medical need or by environmental events can also contribute. Certain genetic factors contribute to the development of leukemia; Down syndrome is one such condition. Radiation therapy for cancer or other exposure to radiation, perhaps through the environment, also contributes. There is no indication that multiple blood transfusions are connected to clients who have leukemia. Although some genetic factors may influence the incidence of leukemia, prematurity at birth is not one of them. The nurse is teaching a client with newly diagnosed anemia about conserving energy. What does the nurse tell the client? (Select all that apply.) a) "Allow others to perform your care during periods of extreme fatigue." b) "Drink small quantities of protein shakes and nutritional supplements daily." c) "Perform a complete bath daily to reduce your chance of getting an infection." d) "Provide yourself with four to six small, easy-to-eat meals daily." e) "Perform your care activities in groups to conserve your energy." f) "Stop activity when shortness of breath or palpitations are present." Correct Answers: a, b, d, f It is critical to have others help the anemic client who is extremely tired. Although it may be difficult for him or her to ask for help, this practice should be stressed to the client. Drinking small protein or nutritional supplements will help rebuild the client's nutritional status. Having four to six small meals daily is preferred over three large meals; this practice conserves the body's expenditure of energy used in digestion and assimilation of nutrients. Stopping activities when strain on the cardiac or respiratory system is noted is critical. A complete bath should be performed only every other day; on days in between, the client can be taught to take a "mini" sponge bath, which will conserve energy and still be safe in preventing the risks for infection. Care activities should be spaced every hour or so rather than in groups to conserve energy; the time just before and after meals should be avoided. An 82-year-old client with anemia is requested to receive 2 units of whole blood. Which assessment findings cause the nurse to discontinue the transfusion because it is unsafe for the client? (Select all that apply.) a) Capillary refill less than 3 seconds b) Decreased pallor c) Flattened superficial veins d) Hypertension e) Hypotension f) Rapid, bounding pulse Correct Answers: d, e, f In an older adult receiving a transfusion, hypertension is a sign of overload, low blood pressure is a sign of a transfusion reaction, and a rapid and bounding pulse is a sign of fluid overload. In this scenario, 2 units, or about a liter of fluid, could be problematic. Capillary refill time that is less than 3 seconds is considered to be normal and would not pose a problem. Increased (not decreased) pallor and cyanosis are signs of a transfusion reaction, while swollen (not flattened) superficial veins are present in fluid overload in older adult clients receiving transfusions. What are serious side effects of antiviral agents prescribed for a client with acute myelogenous leukemia? (Select all that apply.) a) Cardiomyopathy b) Nephrotoxicity c) Ototoxicity d) Stroke e) Diarrhea Correct Answers: b, c Antiviral agents, although helpful in combating severe infection, have serious side effects, especially nephrotoxicity and ototoxicity. Cardiomyopathy and stroke are not serious side effects of antiviral agents. Diarrhea is a mild side effect associated with antibiotic therapy. 42 A nurse is teaching a client who experiences migraine headaches and is prescribed a beta blocker. Which statement should the nurse include in this client's teaching? a. "Take this drug only when you have prodromal symptoms indicating the onset of a migraine headache." b. "Take this drug as ordered, even when feeling well, to prevent vascular changes associated with migraine headaches." c. "This drug will relieve the pain during the aura phase soon after a headache has started." d. "This medication will have no effect on your heart rate or blood pressure because you are taking it for migraines." ANS: B Beta blockers are prescribed as prophylactic treatment to prevent the vascular changes that initiate migraine headaches. Heart rate and blood pressure will also be affected, and the client should monitor these side effects. The other responses do not discuss appropriate uses of the medication. A nurse assesses a client who has a history of migraines. Which clinical manifestation should the nurse identify as an early sign of a migraine with aura? a. Vertigo b. Lethargy c. Visual disturbances d. Numbness of the tongue ANS: C Early warning of impending migraine with aura usually consists of visual changes, flashing lights, or diplopia. The other manifestations are not associated with an impending migraine with aura. A nurse obtains a health history on a client prior to administering prescribed sumatriptan succinate (Imitrex) for migraine headaches. Which condition should alert the nurse to hold the medication and contact the health care provider? a. Bronchial asthma b. Prinzmetal's angina c. Diabetes mellitus d. Chronic kidney disease ANS: B Sumatriptan succinate effectively reduces pain and other associated symptoms of migraine headache by binding to serotonin receptors and triggering cranial vasoconstriction. Vasoconstrictive effects are not confined to the cranium and can cause coronary vasospasm in clients with Prinzmetal's angina. The other conditions would not affect the client's treatment. A nurse assesses a client with a history of epilepsy who experiences stiffening of the muscles of the arms and legs, followed by an immediate loss of consciousness and jerking of all extremities. How should the nurse document this activity? a. Atonic seizure b. Tonic-clonic seizure c. Myoclonic seizure d. Absence seizure ANS: B Seizure activity that begins with stiffening of the arms and legs, followed by loss of consciousness and jerking of all extremities, is characteristic of a tonic-clonic seizure. An atonic seizure presents as a sudden loss of muscle tone followed by postictal confusion. A myoclonic seizure presents with a brief jerking or stiffening of extremities that may occur singly or in groups. Absence seizures present with automatisms, and the client is unaware of his or her environment. A nurse witnesses a client begin to experience a tonic-clonic seizure and loss of consciousness. Which action should the nurse take? a. Start fluids via a large-bore catheter. b. Turn the client's head to the side. c. Administer IV push diazepam. d. Prepare to intubate the client. ANS: B The nurse should turn the client's head to the side to prevent aspiration and allow drainage of secretions. Anticonvulsants are administered on a routine basis if a seizure is sustained. If the seizure is sustained (status epilepticus), the client must be intubated and should be administered oxygen, 0.9% sodium chloride, and IV push lorazepam or diazepam. A nurse cares for a client who is experiencing status epilepticus. Which prescribed medication should the nurse prepare to administer? a. Atenolol (Tenormin) b. Lorazepam (Ativan) c. Phenytoin (Dilantin) d. Lisinopril (Prinivil) ANS: B Initially, intravenous lorazepam is administered to stop motor movements. This is followed by the administration of phenytoin. Atenolol, a beta blocker, and lisinopril, an angiotensin-converting enzyme inhibitor, are not administered for seizure activity. These medications are typically administered for hypertension and heart failure. After teaching a client who is diagnosed with new-onset status epilepticus and prescribed phenytoin (Dilantin), the nurse assesses the client's understanding. Which statement by the client indicates a correct understanding of the teaching? a. "To prevent complications, I will drink at least 2 liters of water daily." b. "This medication will stop me from getting an aura before a seizure." c. "I will not drive a motor vehicle while taking this medication." d. "Even when my seizures stop, I will continue to take this drug." ANS: D Discontinuing antiepileptic drugs can lead to the recurrence of seizures or status epilepticus. The client does not need to drink more water and can drive while taking this medication. The medication will not stop an aura before a seizure. After teaching a client newly diagnosed with epilepsy, the nurse assesses the client's understanding. Which statement by the client indicates a need for additional teaching? a. "I will wear my medical alert bracelet at all times." b. "While taking my epilepsy medications, I will not drink any alcoholic beverages." c. "I will tell my doctor about my prescription and over-the-counter medications." d. "If I am nauseated, I will not take my epilepsy medication." ANS: D The nurse must emphasize that antiepileptic drugs must be taken even if the client is nauseous. Discontinuing the medication can predispose the client to seizure activity and status epilepticus. The client should not drink alcohol while taking seizure medications. The client should wear a medical alert bracelet and should make the doctor aware of all medications to prevent complications of polypharmacy. A nurse obtains a focused health history for a client who is suspected of having bacterial meningitis. Which question should the nurse ask? a. "Do you live in a crowded residence?" b. "When was your last tetanus vaccination?" c. "Have you had any viral infections recently?" d. "Have you traveled out of the country in the last month?" ANS: A Meningococcal meningitis tends to occur in multiple outbreaks. It is most likely to occur in areas of high-density population, such as college dormitories, prisons, and military barracks. A tetanus vaccination would not place the client at increased risk for meningitis or protect the client from meningitis. A viral infection would not lead to bacterial meningitis but could lead to viral meningitis. Simply knowing if the client traveled out of the country does not provide enough information. The nurse should ask about travel to specific countries in which the disease is common, for example, sub- Saharan Africa. After teaching the wife of a client who has Parkinson disease, the nurse assesses the wife's understanding. Which statement by the client's wife indicates she correctly understands changes associated with this disease? a. "His masklike face makes it difficult to communicate, so I will use a white board." b. "He should not socialize outside of the house due to uncontrollable drooling." c. "This disease is associated with anxiety causing increased perspiration." d. "He may have trouble chewing, so I will offer bite-sized portions." ANS: D Because chewing and swallowing can be problematic, small frequent meals and a supplement are better for meeting the client's nutritional needs. A masklike face and drooling are common in clients with Parkinson disease. The client should be encouraged to continue to socialize and communicate as normally as possible. The wife should understand that the client's masklike face can be misinterpreted and additional time may be needed for the client to communicate with her or others. Excessive perspiration is also common in clients with Parkinson disease and is associated with the autonomic nervous system's response. A nurse plans care for a client with Parkinson disease. Which intervention should the nurse include in this client's plan of care? a. Ambulate the client in the hallway twice a day. b. Ensure a fluid intake of at least 3 liters per day. c. Teach the client pursed-lip breathing techniques. d. Keep the head of the bed at 30 degrees or greater. ANS: D Elevation of the head of the bed will help prevent aspiration. The other options will not prevent aspiration, which is the greatest respiratory complication of Parkinson disease, nor do these interventions address any of the complications of Parkinson disease. Ambulation in the hallway is usually implemented to prevent venous thrombosis. Increased fluid intake flushes out toxins from the client's blood. Pursed-lip breathing increases exhalation of carbon dioxide. A nurse is teaching the daughter of a client who has Alzheimer's disease. The daughter asks, "Will the medication my mother is taking improve her dementia?" How should the nurse respond? a. "It will allow your mother to live independently for several more years." b. "It is used to halt the advancement of Alzheimer's disease but will not cure it." c. "It will not improve her dementia but can help control emotional responses." d. "It is used to improve short-term memory but will not improve problem solving." ANS: C Drug therapy is not effective for treating dementia or halting the advancement of Alzheimer's disease. However, certain drugs may help suppress emotional disturbances and psychiatric manifestations. Medication therapy may not allow the client to safely live independently. A nurse assesses a client with Alzheimer's disease who is recently admitted to the hospital. Which psychosocial assessment should the nurse complete? a. Assess religious and spiritual needs while in the hospital. b. Identify the client's ability to perform self-care activities. c. Evaluate the client's reaction to a change of environment. d. Ask the client about relationships with family members. ANS: C As Alzheimer's disease progresses, the client experiences changes in emotional and behavioral affect. The nurse should be alert to the client's reaction to a change in environment, such as being hospitalized, because the client may exhibit an exaggerated response, such as aggression, to the event. The other assessments should be completed but are not as important as assessing the client's reaction to environmental change. A nurse witnesses a client with late-stage Alzheimer's disease eat breakfast. Afterward the client states, "I am hungry and want breakfast." How should the nurse respond? a. "I see you are still hungry. I will get you some toast." b. "You ate your breakfast 30 minutes ago." c. "It appears you are confused this morning." d. "Your family will be here soon. Let's get you dressed." ANS: A Use of validation therapy with clients who have Alzheimer's disease involves acknowledgment of the client's feelings and concerns. This technique has proved more effective in later stages of the disease, when using reality orientation only increases agitation. Telling the client that he or she already ate breakfast may agitate the client. The other statements do not validate the client's concerns. A nurse assesses a client after administering prescribed levetiracetam (Keppra). Which laboratory tests should the nurse monitor for potential adverse effects of this medication? a. Serum electrolyte levels b. Kidney function tests c. Complete blood cell count d. Antinuclear antibodies ANS: B Adverse effects of levetiracetam include coordination problems and renal toxicity. The other laboratory tests are not affected by levetiracetam. A nurse cares for a client with advanced Alzheimer's disease. The client's caregiver states, "She is always wandering off. What can I do to manage this restless behavior?" How should the nurse respond? a. "This is a sign of fatigue. The client would benefit from a daily nap." b. "Engage the client in scheduled activities throughout the day." c. "It sounds like this is difficult for you. I will consult the social worker." d. "The provider can prescribe a mild sedative for restlessness." ANS: B Several strategies may be used to cope with restlessness and wandering. One strategy is to engage the client in structured activities. Another is to take the client for frequent walks. Daily naps and a mild sedative will not be as effective in the management of restless behavior. Consulting the social worker does not address the caregiver's concern. A nurse prepares to discharge a client with Alzheimer's disease. Which statement should the nurse include in the discharge teaching for this client's caregiver? a. "Allow the client to rest most of the day." b. "Place a padded throw rug at the bedside." c. "Install deadbolt locks on all outside doors." d. "Provide a high-calorie and high-protein diet." ANS: C Clients with Alzheimer's disease have a tendency to wander, especially at night. If possible, alarms should be installed on all outside doors to alert family members if the client leaves. At a minimum, all outside doors should have deadbolt locks installed to prevent the client from going outdoors unsupervised. The client should be allowed to exercise within his or her limits. Throw rugs are a slip and fall hazard and should be removed. The client should eat a well-balanced diet. There is no need for a high-calorie or high-protein diet. A nurse assesses a client with Huntington disease. Which motor changes should the nurse monitor for in this client? a. Shuffling gait b. Jerky hand movements c. Continuous chewing motions d. Tremors of the hands ANS: B An imbalance between excitatory and inhibitory neurotransmitters leads to uninhibited motor movements, such as brisk, jerky, purposeless movements of the hands, face, tongue, and legs. Shuffling gait, continuous chewing motions, and tremors are associated with Parkinson disease. A nurse cares for a client who has been diagnosed with the Huntington gene but has no symptoms. The client asks for options related to family planning. What is the nurse's best response? a. "Most clients with the Huntington gene do not pass on Huntington disease to their children." b. "I understand that they can diagnose this disease in embryos. Therefore, you could select a healthy embryo from your fertilized eggs for implantation to avoid passing on Huntington disease." c. "The need for family planning is limited because one of the hallmarks of Huntington disease is infertility." d. "Tell me more specifically what information you need about family planning so that I can direct you to the right information or health care provider." ANS: D The presence of the Huntington gene means that the trait will be passed on to all offspring of the affected person. Understanding options for contraception and conception (e.g., surrogacy options) and implications for children may require the expertise of a genetic counselor or a reproductive specialist. The other statements are not accurate. A nurse is teaching a client with chronic migraine headaches. Which statement related to complementary therapy should the nurse include in this client's teaching? a. "Place a warm compress on your forehead at the onset of the headache." b. "Wear dark sunglasses when you are in brightly lit spaces." c. "Lie down in a darkened room when you experience a headache." d. "Set your alarm to ensure you do not sleep longer than 6 hours at one time." ANS: C At the onset of a migraine attack, the client may be able to alleviate pain by lying down and darkening the room. He or she may want both eyes covered and a cool cloth on the forehead. If the client falls asleep, he or she should remain undisturbed until awakening. The other options are not recognized therapies for migraines. A nurse delegates care for a client with Parkinson disease to an unlicensed assistive personnel (UAP). Which statement should the nurse include when delegating this client's care? a. "Allow the client to be as independent as possible with activities." b. "Assist the client with frequent and meticulous oral care." c. "Assess the client's ability to eat and swallow before each meal." d. "Schedule appointments early in the morning to ensure rest in the afternoon." ANS: A Clients with Parkinson disease do not move as quickly and can have functional problems. The client should be encouraged to be as independent as possible and provided time to perform activities without rushing. Although oral care is important for all clients, instructing the UAP to provide frequent and meticulous oral is not a priority for this client. This statement would be a priority if the client was immune-compromised or NPO. The nurse should assess the client's ability to eat and swallow; this should not be delegated. Appointments and activities should not be scheduled early in the morning because this may cause the client to be rushed and discourage the client from wanting to participate in activities of daily living. A nurse delegates care for a client with early-stage Alzheimer's disease to an unlicensed assistive personnel (UAP). Which statement should the nurse include when delegating this client's care? a. "If she is confused, play along and pretend that everything is okay." b. "Remove the clock from her room so that she doesn't get confused." c. "Reorient the client to the day, time, and environment with each contact." d. "Use validation therapy to recognize and acknowledge the client's concerns." ANS: C Clients who have early-stage Alzheimer's disease should be reoriented frequently to person, place, and time. The UAP should reorient the client and not encourage the client's delusions. The room should have a clock and white board with the current date written on it. Validation therapy is used with late-stage Alzheimer's disease. A nurse plans care for a client with epilepsy who is admitted to the hospital. Which interventions should the nurse include in this client's plan of care? (Select all that apply.) a. Have suction equipment at the bedside. b. Place a padded tongue blade at the bedside. c. Permit only clear oral fluids. d. Keep bed rails up at all times. e. Maintain the client on strict bedrest. f. Ensure that the client has IV access. ANS: A, D, F Oxygen and suctioning equipment with an airway must be readily available. The bed rails should be up at all times while the client is in the bed to prevent injury from a fall if the client has a seizure. If the client does not have an IV access, insert a saline lock, especially for those clients who are at significant risk for generalized tonic-clonic seizures. The saline lock provides ready access if IV drug therapy must be given to stop the seizure. Padded tongue blades may pose a danger to the client during a seizure and should not be used. Dietary restrictions and strict bedrest are not interventions associated with epilepsy. The client should be encouraged to eat a well-balanced diet and ambulate while in the hospital. A nurse is teaching a client who has chronic headaches. Which statements about headache triggers should the nurse include in this client's plan of care? (Select all that apply.) a. "Increase your intake of caffeinated beverages." b. "Incorporate physical exercise into your daily routine." c. "Avoid all alcoholic beverages." d. "Participate in a smoking cessation program." e. "Increase your intake of fruits and vegetables." ANS: B, D, E Triggers for headaches include caffeine, smoking, and ingestion of pickled foods, so these factors should be avoided. Clients are taught to eat a balanced diet and to get adequate exercise and rest. Alcohol does not trigger chronic headaches but can enhance headaches during the headache period. A nurse evaluates the results of diagnostic tests on a client's cerebrospinal fluid (CSF). Which fluid results alerts the nurse to possible viral meningitis? (Select all that apply.) a. Clear b. Cloudy c. Increased protein level d. Normal glucose level e. Bacterial organisms present f. Increased white blood cells ANS: A, C, D In viral meningitis, CSF fluid is clear, protein levels are slightly increased, and glucose levels are normal. Viral meningitis does not cause cloudiness or increased turbidity of CSF. In bacterial meningitis, the presence of bacteria and white blood cells causes the fluid to be cloudy. A nurse assesses a client who is experiencing a cluster headache. Which clinical manifestations should the nurse expect to find? (Select all that apply.) a. Ipsilateral tearing of the eye b. Miosis c. Abrupt loss of consciousness d. Neck and shoulder tenderness e. Nasal congestion f. Exophthalmos ANS: A, B, E Cluster headache is usually accompanied by ipsilateral tearing, miosis, rhinorrhea or nasal congestion, ptosis, eyelid edema, and facial sweating. Abrupt loss of consciousness, neck and shoulder tenderness, and exophthalmos are not associated with cluster headaches. A nurse assesses a client who is experiencing an absence seizure. For which clinical manifestations should the nurse assess? (Select all that apply.) a. Intermittent rigidity b. Lip smacking c. Sudden loss of muscle tone d. Brief jerking of the extremities e. Picking at clothing f. Patting of the hand on the leg ANS: B, E, F Automatisms are characteristic of absence seizures. These behaviors consist of lip smacking, picking at clothing, and patting. Rigidity of muscles is associated with the tonic phase of a seizure, and jerking of the extremities is associated with the clonic phase of a seizure. Loss of muscle tone occurs with atonic seizures. A nurse prepares to provide perineal care to a client with meningococcal meningitis. Which personal protective equipment should the nurse wear? (Select all that apply.) a. Particulate respirator b. Isolation gown c. Shoe covers d. Surgical mask e. Gloves ANS: D, E Meningeal meningitis is spread via saliva and droplets, and Droplet Precautions are necessary. Caregivers should wear a surgical mask when within 6 feet of the client and should continue to use Standard Precautions, including gloves. A particulate respirator, an isolation gown, and shoe covers are not necessary for Droplet Precautions. A nurse assesses clients on a medical-surgical unit. Which clients should the nurse identify as at risk for secondary seizures? (Select all that apply.) a. A 26-year-old woman with a left temporal brain tumor b. A 38-year-old male client in an alcohol withdrawal program c. A 42-year-old football player with a traumatic brain injury d. A 66-year-old female client with multiple sclerosis e. A 72-year-old man with chronic obstructive pulmonary disease ANS: A, B, C Clients at risk for secondary seizures include those with a brain lesion from a tumor or trauma, and those who are experiencing a metabolic disorder, acute alcohol withdrawal, electrolyte disturbances, and high fever. Clients with a history of stroke, heart disease, and substance abuse are also at risk. Clients with multiple sclerosis or chronic obstructive pulmonary disease are not at risk for secondary seizures. A nurse assesses a client who is recovering from the implantation of a vagal nerve stimulation device. For which clinical manifestations should the nurse assess as common complications of this procedure? (Select all that apply.) a. Bleeding b. Infection c. Hoarseness d. Dysphagia e. Seizures ANS: C, D Complications of surgery to implant a vagal nerve stimulation device include hoarseness (most common), dyspnea, neck pain, and dysphagia. The device is tunneled under the skin with an electrode connected to the vagus nerve to control simple or complex partial seizures. Bleeding is not a common complication of this procedure, and infection would not occur during the recovery period. A nurse is caring for a client with meningitis. Which laboratory values should the nurse monitor to identify potential complications of this disorder? (Select all that apply.) a. Sodium level b. Liver enzymes c. Clotting factors d. Cardiac enzymes e. Creatinine level ANS: A, C Inflammation associated with meningitis can stimulate the hypothalamus and result in excessive production of antidiuretic hormone. The nurse should monitor sodium levels for early identification of syndrome of inappropriate antidiuretic hormone. A systemic inflammatory response (SIR) can also occur with meningitis. A SIR can result in a coagulopathy that leads to disseminated intravascular coagulation. The nurse should monitor clotting factors to identify this complication. The other laboratory values are not specific to complications of meningitis. A nurse assesses a client who has encephalitis. Which manifestations should the nurse recognize as signs of increased intracranial pressure (ICP), a complication of encephalitis? (Select all that apply.) a. Photophobia b. Dilated pupils c. Headache d. Widened pulse pressure e. Bradycardia ANS: B, D, E Increased ICP is a complication of encephalitis. The nurse should monitor for signs of increased ICP, including dilated pupils, widened pulse pressure, bradycardia, irregular respirations, and less responsive pupils. Photophobia and headache are not related to increased ICP. 43 the spinal cord A nurse promotes the prevention of lower back pain by teaching clients at a community center. Which instruction should the nurse include in this education? a. "Participate in an exercise program to strengthen muscles." b. "Purchase a mattress that allows you to adjust the firmness." c. "Wear flat instead of high-heeled shoes to work each day." d. "Keep your weight within 20% of your ideal body weight." ANS: A Exercise can strengthen back muscles, reducing the incidence of low back pain. The other options will not prevent low back pain. A nurse plans care for a client with lower back pain from a work-related injury. Which intervention should the nurse include in this client's plan of care? a. Encourage the client to stretch the back by reaching toward the toes. b. Massage the affected area with ice twice a day. c. Apply a heating pad for 20 minutes at least four times daily. d. Advise the client to avoid warm baths or showers. ANS: C Heat increases blood flow to the affected area and promotes healing of injured nerves. Stretching and ice will not promote healing, and there is no need to avoid warm baths or showers. A nurse assesses a client who is recovering from a diskectomy 6 hours ago. Which assessment finding should the nurse address first? a. Sleepy but arouses to voice b. Dry and cracked oral mucosa c. Pain present in lower back d. Bladder palpated above pubis ANS: D A distended bladder may indicate damage to the sacral spinal nerves. The other findings require the nurse to provide care but are not the priority or a complication of the procedure. A nurse assesses clients at a community center. Which client is at greatest risk for lower back pain? a. A 24-year-old female who is 25 weeks pregnant b. A 36-year-old male who uses ergonomic techniques c. A 45-year-old male with osteoarthritis d. A 53-year-old female who uses a walker ANS: C Osteoarthritis causes changes to support structures, increasing the client's risk for low back pain. The other clients are not at high risk. A nurse teaches a client who is recovering from a spinal fusion. Which statement should the nurse include in this client's postoperative instructions? a. "Only lift items that are 10 pounds or less." b. "Wear your brace whenever you are out of bed." c. "You must remain in bed for 3 weeks after surgery." d. "You are prescribed medications to prevent rejection." ANS: B Clients who undergo spinal fusion are fitted with a brace that they must wear throughout the healing process (usually 3 to 6 months) whenever they are out of bed. The client should not lift anything. The client does not need to remain in bed. Medications for rejection prevention are not necessary for this procedure. A nurse assesses a client who is recovering from anterior cervical diskectomy and fusion. Which complication should alert the nurse to urgently communicate with the health care provider? a. Auscultated stridor b. Weak pedal pulses c. Difficulty swallowing d. Inability to shrug shoulders ANS: A Postoperative swelling can narrow the trachea, cause a partial airway obstruction, and manifest as stridor. The client may also have trouble swallowing, but maintaining an airway takes priority. Weak pedal pulses and an inability to shrug the shoulders are not complications of this surgery. A nurse assesses a client with a spinal cord injury at level T5. The client's blood pressure is 184/95 mm Hg, and the client presents with a flushed face and blurred vision. Which action should the nurse take first? a. Initiate oxygen via a nasal cannula. b. Place the client in a supine position. c. Palpate the bladder for distention. d. Administer a prescribed beta blocker. ANS: C The client is manifesting symptoms of autonomic dysreflexia. Common causes include bladder distention, tight clothing, increased room temperature, and fecal impaction. If persistent, the client could experience neurologic injury. Precipitating conditions should be eliminated and the physician notified. The other actions would not be appropriate. An emergency room nurse initiates care for a client with a cervical spinal cord injury who arrives via emergency medical services. Which action should the nurse take first? a. Assess level of consciousness. b. Obtain vital signs. c. Administer oxygen therapy. d. Evaluate respiratory status. ANS: D The first priority for a client with a spinal cord injury is assessment of respiratory status and airway patency. Clients with cervical spine injuries are particularly prone to respiratory compromise and may even require intubation. The other assessments should be performed after airway and breathing are assessed. An emergency department nurse cares for a client who experienced a spinal cord injury 1 hour ago. Which prescribed medication should the nurse prepare to administer? a. Intrathecal baclofen (Lioresal) b. Methylprednisolone (Medrol) c. Atropine sulfate d. Epinephrine (Adrenalin) ANS: B Methylprednisolone (Medrol) should be given within 8 hours of the injury. Clients who receive this therapy usually show improvement in motor and sensory function. The other medications are inappropriate for this client. A nurse teaches a client with a lower motor neuron lesion who wants to achieve bladder control. Which statement should the nurse include in this client's teaching? a. "Stroke the inner aspect of your thigh to initiate voiding." b. "Use a clean technique for intermittent catheterization." c. "Implement digital anal stimulation when your bladder is full." d. "Tighten your abdominal muscles to stimulate urine flow." ANS: D In clients with lower motor neuron problems such as spinal cord injury, performing a Valsalva maneuver or tightening the abdominal muscles are interventions that can initiate voiding. Stroking the inner aspect of the thigh may initiate voiding in a client who has an upper motor neuron problem. Intermittent catheterization and digital anal stimulation do not initiate voiding or bladder control. A nurse is caring for a client with paraplegia who is scheduled to participate in a rehabilitation program. The client states, "I do not understand the need for rehabilitation; the paralysis will not go away and it will not get better." How should the nurse respond? a. "If you don't want to participate in the rehabilitation program, I'll let the provider know." b. "Rehabilitation programs have helped many clients with your injury. You should give it a chance." c. "The rehabilitation program will teach you how to maintain the functional ability you have and prevent further disability." d. "When new discoveries are made regarding paraplegia, people in rehabilitation programs will benefit first." ANS: C Participation in rehabilitation programs has many purposes, including prevention of disability, maintenance of functional ability, and restoration of function. The other responses do not meet this client's needs. After teaching a client with a spinal cord injury, the nurse assesses the client's understanding. Which client statement indicates a correct understanding of how to prevent respiratory problems at home? a. "I'll use my incentive spirometer every 2 hours while I'm awake." b. "I'll drink thinned fluids to prevent choking." c. "I'll take cough medicine to prevent excessive coughing." d. "I'll position myself on my right side so I don't aspirate." ANS: A Often, the person with a spinal cord injury will have weak intercostal muscles and is at higher risk for developing atelectasis and stasis pneumonia. Using an incentive spirometer every 2 hours helps the client expand the lungs more fully and prevents atelectasis. Clients should drink fluids that they can tolerate; usually thick fluids are easier to tolerate. The client should be encouraged to cough and clear secretions. Clients should be placed in high-Fowler's position to prevent aspiration. A nurse assesses a client with early-onset multiple sclerosis (MS). Which clinical manifestation should the nurse expect to find? a. Hyperresponsive reflexes b. Excessive somnolence c. Nystagmus d. Heat intolerance ANS: C Early signs and symptoms of MS include changes in motor skills, vision, and sensation. Hyperresponsive reflexes, excessive somnolence, and heat intolerance are later manifestations of MS. A nurse cares for a client who presents with an acute exacerbation of multiple sclerosis (MS). Which prescribed medication should the nurse prepare to administer? a. Baclofen (Lioresal) b. Interferon beta-1b (Betaseron) c. Dantrolene sodium (Dantrium) d. Methylprednisolone (Medrol) ANS: D Methylprednisolone is the drug of choice for acute exacerbations of the disease. The other drugs are not used to treat acute exacerbations of MS. Interferon beta-1b is used to treat and control MS, decrease specific symptoms, and slow the progression of the disease. Baclofen and dantrolene sodium are prescribed to lessen muscle spasticity associated with MS. A nurse assesses a client with multiple sclerosis after administering prescribed fingolimod (Gilenya). For which adverse effect should the nurse monitor? a. Peripheral edema b. Black tarry stools c. Bradycardia d. Nausea and vomiting ANS: C Fingolimod (Gilenya) is an antineoplastic agent that can cause bradycardia, especially within the first 6 hours after administration. Peripheral edema, black and tarry stools, and nausea and vomiting are not adverse effects of fingolimod. A nurse is teaching a client with multiple sclerosis who is prescribed cyclophosphamide (Cytoxan) and methylprednisolone (Medrol). Which statement should the nurse include in this client's discharge teaching? a. "Take warm baths to promote muscle relaxation." b. "Avoid crowds and people with colds." c. "Relying on a walker will weaken your gait." d. "Take prescribed medications when symptoms occur." ANS: B The client should be taught to avoid people with any type of upper respiratory illness because these medications are immunosuppressive. Warm baths will exacerbate the client's symptoms. Assistive devices may be required for safe ambulation. Medication should be taken at all times and should not be stopped. A nurse assesses a client with a neurologic disorder. Which assessment finding should the nurse identify as a late manifestation of amyotrophic lateral sclerosis (ALS)? a. Dysarthria b. Dysphagia c. Muscle weakness d. Impairment of respiratory muscles ANS: D In ALS, progressive muscle atrophy occurs until a flaccid quadriplegia develops. Eventually, the respiratory muscles are involved, which leads to respiratory compromise. Dysarthria, dysphagia, and muscle weakness are early clinical manifestations of ALS. A nurse cares for several clients on a neurologic unit. Which prescription for a client should direct the nurse to ensure that an informed consent has been obtained before the test or procedure? a. Sensation measurement via the pinprick method b. Computed tomography of the cranial vault c. Lumbar puncture for cerebrospinal fluid sampling d. Venipuncture for autoantibody analysis ANS: C A lumbar puncture is an invasive procedure with many potentially serious complications. The other assessments or tests are considered noninvasive and do not require an informed consent. A nurse prepares a client for prescribed magnetic resonance imaging (MRI). Which action should the nurse implement prior to the test? a. Implement nothing by mouth (NPO) status for 8 hours. b. Withhold all daily medications until after the examination. c. Administer morphine sulfate to prevent claustrophobia during the test. d. Place the client in a gown that has cloth ties instead of metal snaps. ANS: D Metal objects are a hazard because of the magnetic field used in the MRI procedure. Morphine sulfate is not administered to prevent claustrophobia; lorazepam (Ativan) or diazepam (Valium) may be used instead. The client does not need to be NPO, and daily medications do not need to be withheld prior to MRI. A nurse cares for a client with a spinal cord injury. With which interdisciplinary team member should the nurse consult to assist the client with activities of daily living? a. Social worker b. Physical therapist c. Occupational therapist d. Case manager ANS: C The occupational therapist instructs the client in the correct use of all adaptive equipment. In collaboration with the therapist, the nurse instructs family members or the caregiver about transfer skills, feeding, bathing, dressing, positioning, and skin care. The other team members are consulted to assist the client with unrelated issues. A nurse cares for a client with amyotrophic lateral sclerosis (ALS). The client states, "I do not want to be placed on a mechanical ventilator." How should the nurse respond? a. "You should discuss this with your family and health care provider." b. "Why are you afraid of being placed on a breathing machine?" c. "Using the incentive spirometer each hour will delay the need for a ventilator." d. "What would you like to be done if you begin to have difficulty breathing?" ANS: D ALS is an adult-onset upper and lower motor neuron disease characterized by progressive weakness, muscle wasting, and spasticity, eventually leading to paralysis. Once muscles of breathing are involved, the client must indicate in the advance directive what is to be done when breathing is no longer possible without intervention. The other statements do not address the client's needs. A nurse assesses the health history of a client who is prescribed ziconotide (Prialt) for chronic back pain. Which assessment question should the nurse ask? a. "Are you taking a nonsteroidal anti-inflammatory drug?" b. "Do you have a mental health disorder?" c. "Are you able to swallow medications?" d. "Do you smoke cigarettes or any illegal drugs?" ANS: B Clients who have a mental health or behavioral health problem should not take ziconotide. The other questions do not identify a contraindication for this medication. A nurse assesses a client who recently experienced a traumatic spinal cord injury. Which assessment data should the nurse obtain to assess the client's coping strategies? (Select all that apply.) a. Spiritual beliefs b. Level of pain c. Family support d. Level of independence e. Annual income f. Previous coping strategies ANS: A, C, D, F Information about the client's preinjury psychosocial status, usual methods of coping with illness, difficult situations, and disappointments should be obtained. Determine the client's level of independence or dependence and his or her comfort level in discussing feelings and emotions with family members or close friends. Clients who are emotionally secure and have a positive self-image, a supportive family, and financial and job security often adapt to their injury. Information about the client's spiritual and religious beliefs or cultural background also assists the nurse in developing the plan of care. The other options do not supply as much information about coping. After teaching a client with a spinal cord tumor, the nurse assesses the client's understanding. Which statements by the client indicate a correct understanding of the teaching? (Select all that apply.) a. "Even though turning hurts, I will remind you to turn me every 2 hours." b. "Radiation therapy can shrink the tumor but also can cause more problems." c. "Surgery will be scheduled to remove the tumor and reverse my symptoms." d. "I put my affairs in order because this type of cancer is almost always fatal." e. "My family is moving my bedroom downstairs for when I am discharged home." ANS: A, B, E Although surgery may relieve symptoms by reducing pressure on the spine and debulking the tumor, some motor and sensory deficits may remain. Spinal tumors usually cause disability but are not usually fatal. Radiation therapy is often used to shrink spinal tumors but can cause progressive spinal cord degeneration and neurologic deficits. The client should be turned every 2 hours to prevent skin breakdown and arrangements should be made at home so that the client can complete activities of daily living without needing to go up and down stairs. After teaching a male client with a spinal cord injury at the T4 level, the nurse assesses the client's understanding. Which client statements indicate a correct understanding of the teaching related to sexual effects of this injury? (Select all that apply.) a. "I will explore other ways besides intercourse to please my partner." b. "I will not be able to have an erection because of my injury." c. "Ejaculation may not be as predictable as before." d. "I may urinate with ejaculation but this will not cause infection." e. "I should be able to have an erection with stimulation." ANS: C, D, E Men with injuries above T6 often are able to have erections by stimulating reflex activity. For example, stroking the penis will cause an erection. Ejaculation is less predictable and may be mixed with urine. However, urine is sterile, so the client's partner will not get an infection. A nurse cares for a client with a lower motor neuron injury who is experiencing a flaccid bowel elimination pattern. Which actions should the nurse take to assist in relieving this client's constipation? (Select all that apply.) a. Pour warm water over the perineum. b. Provide a diet high in fluids and fiber. c. Administer daily tap water enemas. d. Implement a consistent daily time for elimination. e. Massage the abdomen from left to right. f. Perform manual disimpaction. ANS: B, D, F For the client with a lower motor neuron injury, the resulting flaccid bowel may require a bowel program for the client that includes stool softeners, increased fluid intake, a high-fiber diet, and a consistent elimination time. If the client becomes impacted, the nurse would need to perform manual disimpaction. Pouring warm water over the perineum, administering daily enemas, and massaging the abdomen would not assist this client. A nurse assesses a client who is recovering from a lumbar laminectomy. Which complications should alert the nurse to urgently communicate with the health care provider? (Select all that apply.) a. Surgical discomfort b. Redness and itching at the incision site c. Incisional bulging d. Clear drainage on the dressing e. Sudden and severe headache ANS: C, D, E Bulging at the incision site or clear fluid on the dressing after a laminectomy strongly suggests a cerebrospinal fluid leak, which constitutes an emergency. Loss of cerebral spinal fluid may cause a sudden and severe headache, which is also an emergency situation. Pain, redness, and itching at the site are normal. A nurse assesses a client with paraplegia from a spinal cord injury and notes reddened areas over the client's hips and sacrum. Which actions should the nurse take? (Select all that apply.) a. Apply a barrier cream to protect the skin from excoriation. b. Perform range-of-motion (ROM) exercises for the hip joint. c. Re-position the client off of the reddened areas. d. Get the client out of bed and into a chair once a day. e. Obtain a low-air-loss mattress to minimize pressure. ANS: C, E Appropriate interventions to relieve pressure on these areas include frequent re-positioning and a low-air-loss mattress. Reddened areas should not be rubbed because this action could cause more extensive damage to the already fragile capillary system. Barrier cream will not protect the skin from pressure wounds. ROM exercises are used to prevent contractures. Sitting the client in a chair once a day will decrease the client's risk of respiratory complications but will not decrease pressure on the client's hips and sacrum. A nurse assesses a client who experienced a spinal cord injury at the T5 level 12 hours ago. Which manifestations should the nurse correlate with neurogenic shock? (Select all that apply.) a. Heart rate of 34 beats/min b. Blood pressure of 185/65 mm Hg c. Urine output less than 30 mL/hr d. Decreased level of consciousness e. Increased oxygen saturation ANS: A, C, D Neurogenic shock with acute spinal cord injury manifests with decreased oxygen saturation, symptomatic bradycardia, decreased level of consciousness, decreased urine output, and hypotension. A nurse plans care for a client with a halo fixator. Which interventions should the nurse include in this client's plan of care? (Select all that apply.) a. Tape a halo wrench to the client's vest. b. Assess the pin sites for signs of infection. c. Loosen the pins when sleeping. d. Decrease the client's oral fluid intake. e. Assess the chest and back for skin breakdown. ANS: A, B, E A special halo wrench should be taped to the client's vest in case of a cardiopulmonary emergency. The nurse should assess the pin sites for signs of infection or loose pins and for complications from the halo. The nurse should also increase fluids and fiber to decrease bowel straining and assess the client's chest and back for skin breakdown from the halo vest. 47 care of patients with vision problem A client has a corneal ulcer. What information provided by the client most indicates a potential barrier to home care? a. Chronic use of sleeping pills b. Impaired near vision c. Slightly shaking hands d. Use of contact lenses ANS: A Antibiotic eyedrops are often needed every hour for the first 24 hours for corneal ulceration. The client who uses sleeping pills may not wake up each hour or may awaken unable to perform this task. This client might need someone else to instill the eyedrops hourly. Impaired near vision and shaking hands can both make administration of eyedrops more difficult but are not the most likely barriers. Contact lenses should be discarded. DIF: Analyzing/Analysis REF: 980 KEY: Visual system| visual disorders| medication administration MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Health Promotion and Maintenance An older client has decided to give up driving due to cataracts. What assessment information is most important to collect? a. Family history of visual problems b. Feelings related to loss of driving c. Knowledge about surgical options d. Presence of family support ANS: B Loss of driving is often associated with loss of independence, as is decreasing vision. The nurse should assess how the client feels about this decision and what its impact will be. Family history and knowledge about surgical options are not related as the client has made a decision to decline surgery. Family support is also useful information, but it is most important to get the client's perspective on this change. DIF: Applying/Application REF: 983 KEY: Visual system| visual disorders| cataracts| older adult| coping| psychosocial response MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Psychosocial Integrity A client is in the preoperative holding area waiting for cataract surgery. The client says "Oh, yeah, I forgot to tell you that I take clopidogrel, or Plavix." What action by the nurse is most important? a. Ask the client when the last dose was. b. Check results of the prothrombin time (PT) and international normalized ratio (INR). c. Document the information in the chart. d. Notify the surgeon immediately. ANS: D Clopidogrel is an antiplatelet aggregate and could increase bleeding. The surgeon should be notified immediately. The nurse should find out when the last dose of the drug was, but the priority is to notify the provider. This drug is not monitored with PT and INR. Documentation should occur but is not the priority. DIF: Applying/Application REF: 983 KEY: Visual system| visual disorders| cataracts| preoperative nursing| communication MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Physiological Integrity: Reduction of Risk Potential A client does not understand why vision loss due to glaucoma is irreversible. What explanation by the nurse is best? a. "Because eye pressure was too high, the tissue died." b. "Glaucoma always leads to permanent blindness." c. "The traumatic damage to your eye was too great." d. "The infection occurs so quickly it can't be treated." ANS: A Glaucoma is caused when the intraocular pressure becomes too high and stays high long enough to cause tissue ischemia and death. At that point, vision loss is permanent. Glaucoma does not have to cause blindness. Trauma can cause glaucoma but is not the most common cause. Glaucoma is not an infection. DIF: Understanding/Comprehension REF: 985 KEY: Visual system| visual disorders| glaucoma| patient education| pathophysiology MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client's intraocular pressure (IOP) is 28 mm Hg. What action by the nurse is best? a. Educate the client on corneal transplantation. b. Facilitate scheduling the eye surgery. c. Plan to teach about drugs for glaucoma. d. Refer the client to local Braille classes. ANS: C This increased IOP indicates glaucoma. The nurse's main responsibility is teaching the client about drug therapy. Corneal transplantation is not used in glaucoma. Eye surgery is not indicated at this time. Braille classes are also not indicated at this time. DIF: Applying/Application REF: 985 KEY: Visual system| visual disorders| glaucoma| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client had a retinal detachment and has undergone surgical correction. What discharge instruction is most important? a. "Avoid reading, writing, or close work such as sewing." b. "Dim the lights in your house for at least a week." c. "Keep the follow-up appointment with the ophthalmologist." d. "Remove your eye patch every hour for eyedrops." ANS: A After surgery for retinal detachment, the client is advised to avoid reading, writing, and close work because they cause rapid eye movements. Dim lights are not indicated. Keeping a postoperative appointment is important for any surgical client. The eye patch is not removed for eyedrops. DIF: Understanding/Comprehension REF: 990 KEY: Visual system| visual disorders| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Reduction of Risk Potential A client has been taught about retinitis pigmentosa (RP). What statement by the client indicates a need for further teaching? a. "Beta carotene, lutein, and zeaxanthin are good supplements." b. "I might qualify for a retinal transplant one day soon." c. "Since I'm going blind, sunglasses are not needed anymore." d. "Vitamin A has been shown to slow progression of RP." ANS: C Sunglasses are needed to prevent the development of cataracts in addition to the RP. The other statements are accurate. DIF: Evaluating/Synthesis REF: 990 KEY: Visual system| visual disorders| patient education MSC: Integrated Process: Nursing Process: Evaluation NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client has a foreign body in the eye. What action by the nurse takes priority? a. Administering ordered antibiotics b. Assessing the client's visual acuity c. Obtaining consent for enucleation d. Removing the object immediately ANS: A To prevent infection, antibiotics are provided. Visual acuity in the affected eye cannot be assessed. The client may or may not need enucleation. The object is only removed by the ophthalmologist. DIF: Applying/Application REF: 992 KEY: Visual system| visual disorders| antibiotics MSC: Integrated Process: Nursing Process: Implementation NOT: Client Needs Category: Safe and Effective Care Environment: Safety and Infection Control A client who is near blind is admitted to the hospital. What action by the nurse is most important? a. Allow the client to feel his or her way around. b. Let the client arrange objects on the bedside table. c. Orient the client to the room using a focal point. d. Speak loudly and slowing when talking to the client. ANS: C Using a focal point, orient the client to the room by giving descriptions of items as they relate to the focal point. Letting the client arrange the bedside table is a good idea, but not as important as orienting the client to the room for safety. Allowing the client to just feel around may cause injury. Unless the client is also hearing impaired, use a normal tone of voice. DIF: Remembering/Knowledge REF: 993 KEY: Visual system| visual disorders| patient safety MSC: Integrated Process: Nursing Process: Implementation NOT: Client Needs Category: Safe and Effective Care Environment: Safety and Infection Control A client had proxymetacaine (Ocu-Caine) instilled in one eye in the emergency department. What discharge instruction is most important? a. Do not touch or rub the eye until it is no longer numb. b. Monitor the eye for any bleeding for the next day. c. Rinse the eye with warm saline solution at home. d. Use all the eyedrops as prescribed until they are gone. ANS: A This drug is an ophthalmic anesthetic. The client can injure the numb eye by touching or rubbing it. Bleeding is not associated with this drug. The client should not be told to rinse the eye. This medication was given in the emergency department and is not prescribed for home use. DIF: Understanding/Comprehension REF: 979 KEY: Visual system| visual disorders| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Pharmacological and Parenteral Therapies A client is taking timolol (Timoptic) eyedrops. The nurse assesses the client's pulse at 48 beats/min. What action by the nurse is the priority? a. Ask the client about excessive salivation. b. Assess the client for shortness of breath. c. Give the drops using punctal occlusion. d. Hold the eyedrops and notify the provider. ANS: D The nurse should hold the eyedrops and notify the provider because beta blockers can slow the heart rate. Excessive salivation can occur with cholinergic agonists. Shortness of breath is not related. If the drops are given, the nurse uses punctal occlusion to avoid systemic absorption. DIF: Applying/Application REF: 988 KEY: Visual system| visual disorders| beta blockers MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Physiological Integrity: Pharmacological and Parenteral Therapies A client has been prescribed brinzolamide (Azopt). What assessment by the nurse requires consultation with the provider? a. Allergy to eggs b. Allergy to sulfonamides c. Use of contact lenses d. Use of beta blockers ANS: B Brinzolamide is similar to sulfonamides, so an allergic reaction could occur. The other assessment findings are not related to brinzolamide. DIF: Applying/Application REF: 988 KEY: Visual system| visual disorders| nursing assessment| antibiotics MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Physiological Integrity: Pharmacological and Parenteral Therapies A client is brought to the emergency department after a car crash. The client has a large piece of glass in the left eye. What action by the nurse takes priority? a. Administer a tetanus booster shot. b. Ensure the client has a patent airway. c. Prepare to irrigate the client's eye. d. Turn the client on the unaffected side. ANS: B Airway always comes first. After ensuring a patent airway and providing cervical spine precautions (do not turn the client to the side), the nurse provides other care that may include administering a tetanus shot. The client's eye may or may not be irrigated. DIF: Applying/Application REF: 992 KEY: Visual system| visual disturbances| primary survey MSC: Integrated Process: Nursing Process: Implementation NOT: Client Needs Category: Safe and Effective Care Environment: Management of Care A nurse is seeing clients in the ophthalmology clinic. Which client should the nurse see first? a. Client with intraocular pressure reading of 24 mm Hg b. Client who has had cataract surgery and has worsening vision c. Client whose red reflex is absent on ophthalmologic examination d. Client with a tearing, reddened eye with exudate ANS: B After cataract surgery, worsening vision indicates an infection or other complication. The nurse should see this client first. The intraocular pressure is slightly elevated. An absent red reflex may indicate cataracts. The client who has the tearing eye may have an infection. DIF: Applying/Application REF: 984 KEY: Visual system| visual disorders MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Safe and Effective Care Environment: Management of Care The nurse working in the ophthalmology clinic sees clients with eyelid and eye problems. What information should the nurse understand about these disorders? (Select all that apply.) a. A chalazion is an inflammation of an eyelid sebaceous gland. b. An ectropion is the eyelid turning inward. c. An entropion is the eyelid turning outward. d. A hordeolum is an infection of the eyelid sweat gland. e. Keratoconjunctivitis sicca is caused by drugs or diseases. ANS: A, D, E A chalazion is an inflammation of one of the sebaceous glands in the eyelid. A hordeolum is an infection of a sweat gland in the eyelid. Keratoconjunctivitis sicca can be caused by drugs or diseases. An ectropion is an outward turning and sagging eyelid, while an entropion is an inward turning of the eyelid. DIF: Remembering/Knowledge REF: 977 KEY: Visual system| visual disorders MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client is seen in the ophthalmology clinic with bacterial conjunctivitis. Which statements by the client indicate a good understanding of home management of this condition? (Select all that apply.) a. "As long as I don't wipe my eyes, I can share my towel." b. "Eye irrigations should be done with warm saline or water." c. "I will throw away all my eye makeup when I get home." d. "I won't touch the tip of the eyedrop bottle to my eye." e. "When the infection is gone, I can use my contacts again." ANS: C, D Bacterial conjunctivitis is very contagious, and re-infection or cross-contamination between the client's eyes is possible. The client should discard all eye makeup being used at the time the infection started. When instilling eyedrops, the client must be careful not to contaminate the bottle by touching the tip to the eye or face. The client should be instructed not to share towels. Eye irrigations are not needed. Contacts being used when the infection first manifests also need to be discarded. DIF: Evaluating/Synthesis REF: 979 KEY: Visual system| visual disorders MSC: Integrated Process: Nursing Process: Evaluation NOT: Client Needs Category: Health Promotion and Maintenance A client had cataract surgery. What instructions should the nurse provide? (Select all that apply.) a. Call the doctor for increased pain. b. Do not bend over from the waist. c. Do not lift more than 10 pounds. d. Sexual intercourse is allowed. e. Use stool softeners to avoid constipation ANS: A, B, C, E The client should be taught to call the physician for increased pain as this might indicate infection or other complication. To avoid increasing intraocular pressure, clients are taught to not lift more than 10 pounds, to avoid bending at the waist, to avoid straining at stool, and to avoid sexual intercourse for a time after surgery. DIF: Understanding/Comprehension REF: 982 KEY: Visual system| visual disorders| cataracts MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Reduction of Risk Potential A nurse has delegated applying a warm compress to a client's eye. What actions by the unlicensed assistive personnel (UAP) warrant intervention by the nurse? (Select all that apply.) a. Heating the wet washcloth in the microwave b. Holding the cloth on the client using an Ace wrap c. Turning the cloth so it remains warm on the client d. Using a clean washcloth for the compress e. Washing the hands on entering the client's room ANS: A, B The washcloth should be warmed under running warm water. Microwaving it can lead to burns. Gentle pressure is used to hold the compress in place. The other actions are correct. DIF: Applying/Application REF: 980 KEY: Visual system| visual disorders| nonpharmacologic comfort measures| unlicensed assistive personnel (UAP) MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Physiological Integrity: Basic Care and Comfort 48 care of patients with ear and hearing problems A nurse is teaching a client about ear hygiene and health. What client statement indicates a need for further teaching? a. "A soft cotton swab is alright to clean my ears with." b. "I make sure my ears are dry after I go swimming." c. "I use good earplugs when I practice with the band." d. "Keeping my diabetes under control helps my ears." ANS: A Clients should be taught not to put anything larger than their fingertip into their ears. Using a cotton swab, although soft, can cause damage to the ears and cerumen buildup. The other statements are accurate. DIF: Evaluating/Synthesis REF: 1005 KEY: Auditory system| auditory assessment MSC: Integrated Process: Nursing Process: Evaluation NOT: Client Needs Category: Health Promotion and Maintenance The student nurse is performing a Weber tuning fork test. What technique is most appropriate? a. Holding the vibrating tuning fork 10 to 12 inches from the client's ear b. Placing the vibrating fork in the middle of the client's head c. Starting by placing the vibrating fork on the mastoid process d. Tapping the vibrating tuning fork against the bridge of the nose ANS: B The Weber tuning fork test includes placing the vibrating tuning fork in the middle of the client's head and asking in which ear the client hears the vibrations louder. The other techniques are incorrect. DIF: Applying/Application REF: 1001 KEY: Auditory system| auditory assessment MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Physiological Integrity: Reduction of Risk Potential The client's chart indicates a sensorineural hearing loss. What assessment question does the nurse ask to determine the possible cause? a. "Do you feel like something is in your ear?" b. "Do you have frequent ear infections?" c. "Have you been exposed to loud noises?" d. "Have you been told your ear bones don't move?" ANS: C Sensorineural hearing loss can occur from damage to the cochlea, the eighth cranial nerve, or the brain. Exposure to loud music is one etiology. The other questions relate to conductive hearing loss. DIF: Remembering/Knowledge REF: 1001 KEY: Auditory system| auditory assessment| auditory disorders MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Physiological Integrity: Reduction of Risk Potential The nurse works with clients who have hearing problems. Which action by a client best indicates goals for an important diagnosis have been met? a. Babysitting the grandchildren several times a week b. Having an adaptive hearing device for the television c. Being active in community events and volunteer work d. Responding agreeably to suggestions for adaptive devices ANS: C Clients with hearing problems can become frustrated and withdrawn. The client who is actively engaged in the community shows the best evidence of psychosocial adjustment to hearing loss. Babysitting the grandchildren is a positive sign but does not indicate involvement outside the home. Having an adaptive device is not the same as using it, and watching TV without evidence of other activities can also indicate social isolation. Responding agreeably does not indicate the client will actually follow through. DIF: Evaluating/Synthesis REF: 1002 KEY: Auditory system| auditory disorders| psychosocial response| coping MSC: Integrated Process: Nursing Process: Evaluation NOT: Client Needs Category: Psychosocial Integrity A client has external otitis. On what comfort measure does the nurse instruct the client? a. Applying ice four times a day b. Instilling vinegar-and-water drops c. Use of a heating pad to the ear d. Using a home humidifier ANS: C A heating pad on low or a warm moist pack can provide comfort to the client with otitis externa. The other options are not warranted. DIF: Remembering/Knowledge REF: 1004 KEY: Auditory system| auditory disorders| comfort measures MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Basic Care and Comfort An older adult in the family practice clinic reports a decrease in hearing over a week. What action by the nurse is most appropriate? a. Assess for cerumen buildup. b. Facilitate audiological testing. c. Perform tuning fork tests. d. Review the medication list. ANS: A All options are possible actions for the client with hearing loss. The first action the nurse should take is to look for cerumen buildup, which can decrease hearing in the older adult. If this is normal, medications should be assessed for ototoxicity. Further auditory testing may be needed for this client. DIF: Applying/Application REF: 1004 KEY: Auditory system| auditory assessment| auditory disorders| nursing assessment MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Physiological Integrity: Reduction of Risk Potential A client had a myringotomy. The nurse provides which discharge teaching? a. Buy dry shampoo to use for a week. b. Drink liquids through a straw. c. Flying is not allowed for 1 month. d. Hot water showers will help the pain. ANS: A The client cannot shower or get the head wet for 1 week after surgery, so using dry shampoo is a good suggestion. The other instructions are incorrect: straws are not allowed for 2 to 3 weeks, flying is not allowed for 2 to 3 weeks, and the client should not shower. DIF: Applying/Application REF: 1007 KEY: Auditory system| auditory disorders| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client is going on a cruise but has had motion sickness in the past. What suggestion does the nurse make to this client? a. Avoid alcohol on the cruise ship. b. Change positions slowly on the ship. c. Change your travel plans. d. Try scopolamine (Transderm Scop). ANS: D Scopolamine can successfully treat the vertigo and dizziness associated with motion sickness. Avoiding alcohol and changing positions slowly are not effective. Telling the client to change travel plans is not a caring suggestion. DIF: Applying/Application REF: 1008 KEY: Auditory system| auditory disorders MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Pharmacological and Parenteral Therapies A nurse is teaching a community group about noise-induced hearing loss. Which client who does not use ear protection should the nurse refer to an audiologist as the priority? a. Client with an hour car commute on the freeway each day b. Client who rides a motorcycle to work 20 minutes each way c. Client who sat in the back row at a rock concert recently d. Client who is a tree-trimmer and uses a chainsaw 6 to 7 hours a day ANS: D A chainsaw becomes dangerous to hearing after 2 hours of exposure without hearing protection. This client needs to be referred as the priority. Normal car traffic is safe for more than 8 hours. Motorcycle noise is safe for about 8 hours. The safe exposure time for a front-row rock concert seat is 3 minutes, but this client was in the back, and so had less exposure. In addition, a one-time exposure is less damaging than chronic exposure. DIF: Remembering/Knowledge REF: 1002 KEY: Auditory system| auditory disorders| referrals MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Safe and Effective Care Environment: Management of Care A nursing student is instructed to remove a client's ear packing and instill eardrops. What action by the student requires intervention by the registered nurse? a. Assessing the eardrum with an otoscope b. Inserting a cotton ball in the ear after the drops c. Warming the eardrops in water for 5 minutes d. Washing the hands and removing the packing ANS: D The student should wash his or her hands, don gloves, and then remove the packing. The other actions are correct. DIF: Applying/Application REF: 1004 KEY: Auditory system| auditory disorders MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Safe and Effective Care Environment: Safety and Infection Control A nurse is irrigating a client's ear when the client becomes nauseated. What action by the nurse is most appropriate for client comfort? a. Have the client tilt the head back. b. Re-position the client on the other side. c. Slow the rate of the irrigation. d. Stop the irrigation immediately. ANS: D During ear irrigation, if the client becomes nauseated, stop the procedure. The other options are not helpful. DIF: Remembering/Knowledge REF: 1005 KEY: Auditory system| auditory disorders MSC: Integrated Process: Nursing Process: Implementation NOT: Client Needs Category: Physiological Integrity: Basic Care and Comfort A client hospitalized for a wound infection has a blood urea nitrogen of 45 mg/dL and creatinine of 4.2 mg/dL. What action by the nurse is best? a. Assess the ordered antibiotics for ototoxicity. b. Explain how kidney damage causes hearing loss. c. Use ibuprofen (Motrin) for pain control. d. Teach that hearing loss is temporary. ANS: A Some medications are known to be ototoxic. Diminished kidney function slows the excretion of drugs from the body, worsening the ototoxic effects. The nurse should assess the antibiotics the client is receiving for ototoxicity. The other options are not warranted. DIF: Analyzing/Analysis REF: 1000 KEY: Auditory system| auditory disorders| adverse effects MSC: Integrated Process: Nursing Process: Assessment NOT: Client Needs Category: Physiological Integrity: Pharmacological and Parenteral Therapies A nurse is teaching a community group about preventing hearing loss. What instruction is best? a. Always wear a bicycle helmet. b. Avoid swimming in ponds or lakes. c. Don't go to fireworks displays. d. Use a soft cotton swab to clean ears. ANS: A Avoiding head trauma is a practical way to help prevent hearing loss. Swimming can lead to hearing loss if the client has repeated infections. Fireworks displays are loud, but usually brief and only occasional. Nothing smaller than the client's fingertip should be placed in the ear canal. DIF: Applying/Application REF: 1007 KEY: Auditory system| auditory disorders| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Health Promotion and Maintenance A client has severe tinnitus that cannot be treated adequately. What action by the nurse is best? a. Advise the client to take antianxiety medication. b. Educate the client on nerve cutting procedures. c. Refer the client to online or local support groups. d. Teach the client side effects of furosemide (Lasix). ANS: C If the client's tinnitus cannot be treated, he or she will have to learn to cope with it. Referring the client to tinnitus support groups can be helpful. The other options are not warranted. DIF: Applying/Application REF: 1008 KEY: Auditory system| auditory disorders| referrals| coping MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Safe and Effective Care Environment: Management of Care A client has labyrinthitis and is prescribed antibiotics. What instruction by the nurse is most important for this client? a. Immediately report headache or stiff neck. b. Keep all follow-up appointments. c. Take the antibiotics with a full glass of water. d. Take the antibiotic on an empty stomach. ANS: A Meningitis is a complication of labyrinthitis. The client should be taught to take all antibiotics as prescribed and to report manifestations of meningitis such as fever, headache, or stiff neck. Keeping follow-up appointments is important for all clients. Without knowing what antibiotic was prescribed, the nurse cannot instruct the client on how to take it. DIF: Applying/Application REF: 1008 KEY: Auditory system| auditory disorders| patient education| infection control MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client with Ménière's disease is in the hospital when the client has an attack of this disorder. What action by the nurse takes priority? a. Assess vital signs every 15 minutes. b. Dim or turn off lights in the client's room. c. Place the client in bed with the upper siderails up. d. Provide a cool, wet cloth for the client's face. ANS: C Clients with Ménière's disease can have vertigo so severe that they can fall. The nurse should assist the client into bed and put the siderails up to keep the client from falling out of bed due to the intense whirling feeling. The other actions are not warranted for clients with Ménière's disease. DIF: Applying/Application REF: 1008 KEY: Auditory system| auditory disorders| patient safety MSC: Integrated Process: Nursing Process: Implementation NOT: Client Needs Category: Safe and Effective Care Environment: Safety and Infection Control A client is scheduled to have a tumor of the middle ear removed. What teaching topic is most important for the nurse to cover? a. Expecting hearing loss in the affected ear b. Managing postoperative pain c. Maintaining NPO status prior to surgery d. Understanding which medications are allowed the day of surgery ANS: A Removal of an inner ear tumor will likely destroy hearing in the affected ear. The other teaching topics are appropriate for any surgical client. DIF: Remembering/Knowledge REF: 1007 KEY: Auditory disorders| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A nursing student studying the auditory system learns about the structures of the inner ear. What structures does this include? (Select all that apply.) a. Cochlea b. Epitympanum c. Organ of Corti d. Semicircular canals e. Vestibule ANS: A, C, D, E The cochlea, organ of Corti, semicircular canals, and vestibule are all part of the inner ear. The epitympanum is in the middle ear. DIF: Remembering/Knowledge REF: 997 KEY: Auditory system| auditory assessment MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client has Ménière's disease with frequent attacks. About what drugs does the nurse plan to teach the client? (Select all that apply.) a. Broad-spectrum antibiotics b. Chlorpromazine hydrochloride (Thorazine) c. Diphenhydramine (Benadryl) d. Meclizine (Antivert) e. Nonsteroidal anti-inflammatory drugs (NSAIDs) ANS: B, C, D Drugs such as chlorpromazine, diphenhydramine, and meclizine can all be used to treat Ménière's disease. Antibiotics and NSAIDs are not used. DIF: Remembering/Knowledge REF: 1008 KEY: Auditory system| auditory disorders| patient education MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Physiological Integrity: Pharmacological and Parenteral Therapies A client is scheduled for a tympanoplasty. What actions by the nurse are most appropriate? (Select all that apply.) a. Administer preoperative antibiotics. b. Assess for allergies to local anesthetics. c. Ensure that informed consent is on the chart. d. Give ordered antivertigo medications. e. Teach that hearing improves immediately. ANS: A, C Preoperatively, the nurse administers antibiotics and ensures that informed consent is on the chart. Local anesthetics can be used, but general anesthesia is used more often. Antivertigo medications are not used. Hearing will be decreased immediately after the operation until the ear packing is removed. DIF: Applying/Application REF: 1012 KEY: Auditory system| auditory disorders| preoperative nursing| informed consent MSC: Integrated Process: Nursing Process: Implementation NOT: Client Needs Category: Safe and Effective Care Environment: Management of Care A client has a hearing aid. What care instructions does the nurse provide the unlicensed assistive personnel (UAP) in the care of this client? (Select all that apply.) a. Be careful not to drop the hearing aid when handling. b. Soak the hearing aid in hot water for 20 minutes. c. Turn the hearing aid off when the client goes to bed. d. Use a toothpick to clean debris from the device. e. Wash the device with soap and a small amount of warm water. ANS: A, C, D, E All these actions except soaking the hearing aid are proper instructions for the nurse to give to the UAP. While some water is used to clean the hearing aid, excessive wetting should be avoided. DIF: Remembering/Knowledge REF: 1011 KEY: Auditory system| auditory disorders| assistive devices| unlicensed assistive personnel (UAP) MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Physiological Integrity: Basic Care and Comfort A hospitalized client has Ménière's disease. What menu selections demonstrate good knowledge of the recommended diet for this disorder? (Select all that apply.) a. Chinese stir fry with vegetables b. Broiled chicken breast c. Chocolate espresso cookies d. Deli turkey sandwich and chips e. Green herbal tea with meals ANS: B, E The diet recommendations for Ménière's disease include low-sodium, caffeine-free foods and fluids distributed evenly throughout the day. Plenty of water is also needed. The broiled chicken breast and herbal tea are the best selections. The stir fry is high in sodium and possibly monosodium glutamate (MSG, also not recommended). The cookies have caffeine, and the sandwich and chips are high in sodium. DIF: Evaluating/Synthesis REF: 1011 KEY: Auditory system| auditory disorders| nursing evaluation MSC: Integrated Process: Nursing Process: Evaluation NOT: Client Needs Category: Physiological Integrity: Physiological Adaptation A client is scheduled for a stapedectomy in 2 weeks. What teaching instructions are most appropriate? (Select all that apply.) a. Avoid alcohol use before surgery. b. Blow the nose gently if needed. c. Clean the telephone often. d. Sneeze with the mouth open. e. Wash the external ear daily. ANS: B, C, D, E It is imperative that the client having a stapedectomy is free from ear infection. Teaching includes ways to prevent such infections, such as blowing the nose gently, cleaning objects that come into contact with the ear, sneezing with the mouth open, and washing the external ear daily. Avoiding alcohol will not help prevent ear infections. DIF: Applying/Application REF: 1008 KEY: Auditory system| auditory disorders| patient education| infection control MSC: Integrated Process: Teaching/Learning NOT: Client Needs Category: Safe and Effective Care Environment: Safety and Infection Control A client is admitted to the nursing unit after having a tympanoplasty. What activities does the nurse delegate to the unlicensed assistive personnel (UAP)? (Select all that apply.) a. Administer prescribed antibiotics. b. Keep the head of the client's bed flat. c. Remind the client to lie on the operative side. d. Remove the iodoform gauze in 8 hours. e. Take and record postoperative vital signs. ANS: B, E The UAP can keep the head of the client's bed flat and take/record vital signs. The nurse administers medications. The client should lie flat with the head turned so the operative side is up. The nurse or surgeon removes the gauze packing. DIF: Applying/Application REF: 1013 KEY: Auditory system| auditory disorders| delegation| postoperative nursing| unlicensed assistive personnel (UAP) MSC: Integrated Process: Communication and Documentation NOT: Client Needs Category: Safe and Effective Care Environment: Management of Care 50 A client has a bone density score of -2.8. What action by the nurse is best? a. Asking the client to complete a food diary b. Planning to teach about bisphosphonates c. Scheduling another scan in 2 years d. Scheduling another scan in 6 months ANS: B A T-score from a bone density scan at or lower than -2.5 indicates osteoporosis. The nurse should plan to teach about medications used to treat this disease. One class of such medications is bisphosphonates. A food diary is helpful to determine if the client gets adequate calcium and vitamin D, but at this point, dietary changes will not prevent the disease. Simply scheduling another scan will not help treat the disease either. A nurse is assessing an older client and discovers back pain with tenderness along T2 and T3. What action by the nurse is best? a. Consult with the provider about an x-ray. b. Encourage the client to use ibuprofen (Motrin). c. Have the client perform hip range of motion. d. Place the client in a rigid cervical collar. ANS: A Back pain with tenderness is indicative of a spinal compression fracture, which is the most common type of osteoporotic fracture. The nurse should consult the provider about an x-ray. Motrin may be indicated but not until there is a diagnosis. Range of motion of the hips is not related, although limited spinal range of motion may be found with a vertebral compression fracture. Since the defect is in the thoracic spine, a cervical collar is not needed. A client has been advised to perform weight-bearing exercises to help minimize osteoporosis. The client admits to not doing the prescribed exercises. What action by the nurse is best? a. Ask the client about fear of falling. b. Instruct the client to increase calcium. c. Suggest other exercises the client can do. d. Tell the client to try weight lifting. ANS: A Fear of falling can limit participation in activity. The nurse should first assess if the client has this fear and then offer suggestions for dealing with it. The client may or may not need extra calcium, other exercises, or weight lifting. The nurse sees several clients with osteoporosis. For which client would bisphosphonates not be a good option? a. Client with diabetes who has a serum creatinine of 0.8 mg/dL b. Client who recently fell and has vertebral compression fractures c. Hypertensive client who takes calcium channel blockers d. Client with a spinal cord injury who cannot tolerate sitting up ANS: D Clients on bisphosphonates must be able to sit upright for 30 to 60 minutes after taking them. The client who cannot tolerate sitting up is not a good candidate for this class of drug. Poor renal function also makes clients bad candidates for this drug, but the client with a creatinine of 0.8 mg/dL is within normal range. Diabetes and hypertension are not related unless the client also has renal disease. The client who recently fell and sustained fractures is a good candidate for this drug if the fractures are related to osteoporosis. A client has been prescribed denosumab (Prolia). What instruction about this drug is most appropriate? a. "Drink at least 8 ounces of water with it." b. "Make appointments to come get your shot." c. "Sit upright for 30 to 60 minutes after taking it." d. "Take the drug on an empty stomach." ANS: B Denosumab is given by subcutaneous injection twice a year. The client does not need to drink 8 ounces of water with this medication as it is not taken orally. The client does not need to remain upright for 30 to 60 minutes after taking this medication, nor does the client need to take the drug on an empty stomach. A client in a nursing home refuses to take medications. She is at high risk for osteomalacia. What action by the nurse is best? a. Ensure the client gets 15 minutes of sun exposure daily. b. Give the client daily vitamin D injections. c. Hide vitamin D supplements in favorite foods. d. Plan to serve foods naturally high in vitamin D. ANS: A Sunlight is a good source of vitamin D, and the nursing staff can ensure some sun exposure each day. Vitamin D is not given by injection. Hiding the supplement in food is unethical. Very few foods are naturally high in vitamin D, but some are supplemented. A client is in the internal medicine clinic reporting bone pain. The client's alkaline phosphatase level is 180 units/L. What action by the nurse is most appropriate? a. Assess the client for leg bowing. b. Facilitate an oncology workup. c. Instruct the client on fluid restrictions. d. Teach the client about ibuprofen (Motrin). ANS: A This client has manifestations of Paget's disease. The nurse should assess for other manifestations such as bowing of the legs. Other care measures can be instituted once the client has a confirmed diagnosis. An older client with diabetes is admitted with a heavily draining leg wound. The client's white blood cell count is 38,000/mm3 but the client is afebrile. What action does the nurse take first? a. Administer acetaminophen (Tylenol). b. Educate the client on amputation. c. Place the client on contact isolation. d. Refer the client to the wound care nurse. ANS: C In the presence of a heavily draining wound, the nurse should place the client on contact isolation. If the client has discomfort, acetaminophen can be used, but this client has not reported pain and is afebrile. The client may or may not need an amputation in the future. The wound care nurse may be consulted, but not as the first action. A nurse is caring for four clients. After the hand-off report, which client does the nurse see first? a. Client with osteoporosis and a white blood cell count of 27,000/mm3 b. Client with osteoporosis and a bone fracture who requests pain medication c. Post-microvascular bone transfer client whose distal leg is cool and pale d. Client with suspected bone tumor who just returned from having a spinal CT ANS: C This client is the priority because the assessment findings indicate a critical lack of perfusion. A high white blood cell count is an expected finding for the client with osteoporosis. The client requesting pain medication should be seen second. The client who just returned from a CT scan is stable and needs no specific postprocedure care. A client has a metastatic bone tumor. What action by the nurse takes priority? a. Administer pain medication as prescribed. b. Elevate the extremity and apply moist heat. c. Handle the affected extremity with caution. d. Place the client on protective precautions. ANS: C Bones invaded by tumors are very fragile and fracture easily. For client safety, the nurse handles the affected extremity with great care. Pain medication should be given to control pain. Elevation and heat may or may not be helpful. Protective precautions are not needed for this client. A hospitalized client is being treated for Ewing's sarcoma. What action by the nurse is most important? a. Assessing and treating the client for pain as needed b. Educating the client on the disease and its treatment c. Handling and disposing of chemotherapeutic agents per policy d. Providing emotional support for the client and family ANS: C All actions are appropriate for this client. However, for safety, the nurse should place priority on proper handling and disposal of chemotherapeutic agents. A client with bone cancer is hospitalized for a limb salvage procedure. How can the nurse best address the client's psychosocial needs? a. Assess the client's coping skills and support systems. b. Explain that the surgery leads to a longer life expectancy. c. Refer the client to the social worker or hospital chaplain. d. Reinforce physical therapy to aid with ambulating normally. ANS: A The first step in the nursing process is assessment. The nurse should assess coping skills and possible support systems that will be helpful in this client's treatment. Explaining that a limb salvage procedure will extend life does not address the client's psychosocial needs. Referrals may be necessary, but the nurse should assess first. Reinforcing physical therapy is also helpful but again does not address the psychosocial needs of the client. A client had a bunionectomy with osteotomy. The client asks why healing may take up to 3 months. What explanation by the nurse is best? a. "Your feet have less blood flow, so healing is slower." b. "The bones in your feet are hard to operate on." c. "The surrounding bones and tissue are damaged." d. "Your feet bear weight so they never really heal." ANS: A The feet are the most distal to the heart and receive less blood flow than other organs and tissues, prolonging the healing time after surgery. The other explanations are not correct. A client has scoliosis with a 65-degree curve to the spine. What action by the nurse takes priority? a. Allow the client to rest in a position of comfort. b. Assess the client's cardiac and respiratory systems. c. Assist the client with ambulating and position changes. d. Position the client on one side propped with pillows. ANS: B This degree of curvature of the spine affects cardiac and respiratory function. The nurse's priority is to assess those systems. Positioning is up to the client. The client may or may not need assistance with movement. A nurse sees clients in an osteoporosis clinic. Which client should the nurse see first? a. Client taking calcium with vitamin D (Os-Cal) who reports flank pain 2 weeks ago b. Client taking ibandronate (Boniva) who cannot remember when the last dose was c. Client taking raloxifene (Evista) who reports unilateral calf swelling d. Client taking risedronate (Actonel) who reports occasional dyspepsia ANS: C The client on raloxifene needs to be seen first because of the manifestations of deep vein thrombosis, which is an adverse effect of raloxifene. The client with flank pain may have had a kidney stone but is not acutely ill now. The client who cannot remember taking the last dose of ibandronate can be seen last. The client on risedronate may need to change medications. What information does the nurse teach a women's group about osteoporosis? a. "For 5 years after menopause you lose 2% of bone mass yearly." b. "Men actually have higher rates of the disease but are underdiagnosed." c. "There is no way to prevent or slow osteoporosis after menopause." d. "Women and men have an equal chance of getting osteoporosis." ANS: A For the first 5 years after menopause, women lose about 2% of their bone mass each year. Men have a slower loss of bone after the age of 75. Many treatments are now available for women to slow osteoporosis after menopause. A client with osteoporosis is going home, where the client lives alone. What action by the nurse is best? a. Arrange a home safety evaluation. b. Ensure the client has a walker at home. c. Help the client look into assisted living. d. Refer the client to Meals on Wheels. ANS: A This client has several risk factors that place him or her at a high risk for falling. The nurse should consult social work or home health care to conduct a home safety evaluation. The other options may or may not be needed based upon the client's condition at discharge. A client is scheduled for a bone biopsy. What action by the nurse takes priority? a. Administering the preoperative medications b. Answering any questions about the procedure c. Ensuring that informed consent is on the chart d. Showing the client's family where to wait ANS: C The priority is to ensure that informed consent is on the chart. The preoperative medications should not be administered until the nurse is confident the procedure will occur and the client has already signed the consent, if the medications include anxiolytics or sedatives or opioids. The provider should answer questions about the procedure. The nurse does show the family where to wait, but this is not the priority and could be delegated. A client is admitted with a large draining wound on the leg. What action does the nurse take first? a. Administer ordered antibiotics. b. Insert an intravenous line. c. Give pain medications if needed. d. Obtain cultures of the leg wound. ANS: D The nurse first obtains wound cultures prior to administering broad-spectrum antibiotics. The nurse would need to start the IV prior to giving the antibiotics as they will most likely be parenteral. Pain should be treated but that is not the priority. A client has an ingrown toenail. About what self-management measure does the nurse teach the client? a. Long-term antibiotic use b. Shoe padding c. Toenail trimming d. Warm moist soaks ANS: D Treatment of an ingrown toenail includes a podiatrist clipping away the ingrown part of the nail, warm moist soaks, and antibiotic ointment if needed. Antibiotics are not used long-term. Padding the shoes will not treat or prevent ingrown toenails. Clients should not attempt to trim ingrown nails themselves. A nurse is assessing a community group for dietary factors that contribute to osteoporosis. In addition to inquiring about calcium, the nurse also assesses for which other dietary components? (Select all that apply.) a. Alcohol b. Caffeine c. Fat d. Carbonated beverages e. Vitamin D ANS: A, B, D, E Dietary components that affect the development of osteoporosis include alcohol, caffeine, high phosphorus intake, carbonated beverages, and vitamin D. Tobacco is also a contributing lifestyle factor. Fat intake does not contribute to osteoporosis. A nurse is providing education to a community women's group about lifestyle changes helpful in preventing osteoporosis. What topics does the nurse cover? (Select all that apply.) a. Cut down on tobacco product use. b. Limit alcohol to two drinks a day. c. Strengthening exercises are important. d. Take recommended calcium and vitamin D. e. Walk 30 minutes at least 3 times a week. ANS: C, D, E Lifestyle changes can be made to decrease the occurrence of osteoporosis and include strengthening and weight-bearing exercises and getting the recommended amounts of both calcium and vitamin D. Tobacco should be totally avoided. Women should not have more than one drink per day. A client with Paget's disease is hospitalized for an unrelated issue. The client reports pain and it is not yet time for more medication. What comfort measures can the nurse delegate to the unlicensed assistive personnel (UAP)? (Select all that apply.) a. Administering ibuprofen (Motrin) b. Applying a heating pad c. Providing a massage d. Referring the client to a support group e. Using a bed cradle to lift sheets off the feet ANS: B, C Comfort measures for Paget's disease include heat and massage. Administering medications and referrals are done by the nurse. A bed cradle is not necessary. A client with chronic osteomyelitis is being discharged from the hospital. What information is important for the nurse to teach this client and family? (Select all that apply.) a. Adherence to the antibiotic regimen b. Correct intramuscular injection technique c. Eating high-protein and high-carbohydrate foods d. Keeping daily follow-up appointments e. Proper use of the intravenous equipment ANS: A, C, E The client going home with chronic osteomyelitis will need long-term antibiotic therapy— first intravenous, then oral. The client needs education on how to properly administer IV antibiotics, care for the IV line, adhere to the regimen, and eat a healthy diet to encourage wound healing. The antibiotics are not given by IM injection. The client does not need daily follow-up. A client is admitted with a bone tumor. The nurse finds the client weak and lethargic with decreased deep tendon reflexes. What actions by the nurse are best? (Select all that apply.) a. Assess the daily serum calcium level. b. Consult the provider about a loop diuretic. c. Institute seizure precautions for the client. d. Instruct the client to call for help out of bed. e. Place the client on a 1500-mL fluid restriction. ANS: A, B, D The client is exhibiting manifestations of possible hypercalcemia. This disorder is treated with increased fluids and loop diuretics. The nurse should assess the calcium level, consult with the provider, and instruct the client to call for help getting out of bed due to possible fractures and weakness. The client does not need seizure precautions or fluid restrictions. The nurse is assessing a client for chronic osteomyelitis. Which features distinguish this from the acute form of the disease? (Select all that apply.) a. Draining sinus tracts b. High fevers c. Presence of foot ulcers d. Swelling and redness e. Tenderness or pain ANS: A, C Draining sinus tracts and foot ulcers are seen in chronic osteomyelitis. High fever, swelling, and redness are more often seen in acute osteomyelitis. Pain or tenderness can be in either case. The nurse studying osteoporosis learns that which drugs can cause this disorder? (Select all that apply.) a. Antianxiety agents b. Antibiotics c. Barbiturates d. Corticosteroids e. Loop diuretics ANS: C, D, E Several classes of drugs can cause secondary osteoporosis, including barbiturates, corticosteroids, and loop diuretics. Antianxiety agents and antibiotics are not associated with the formation of osteoporosis. A client is suspected to have muscular dystrophy. About what diagnostic testing does the nurse educate the client? (Select all that apply.) a. Electromyography b. Muscle biopsy c. Nerve conduction studies d. Serum aldolase e. Serum creatinine kinase ANS: A, B, D, E Diagnostic testing for muscular dystrophy includes electromyography, muscle biopsy, serum aldolase and creatinine kinase levels. Nerve conduction is not related to this disorder. [Show More]
Last updated: 1 year ago
Preview 1 out of 117 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:
Reviews( 0 )
$14.50
Document information
Connected school, study & course
About the document
Uploaded On
Jun 22, 2021
Number of pages
117
Written in
Additional information
This document has been written for:
Uploaded
Jun 22, 2021
Downloads
0
Views
250

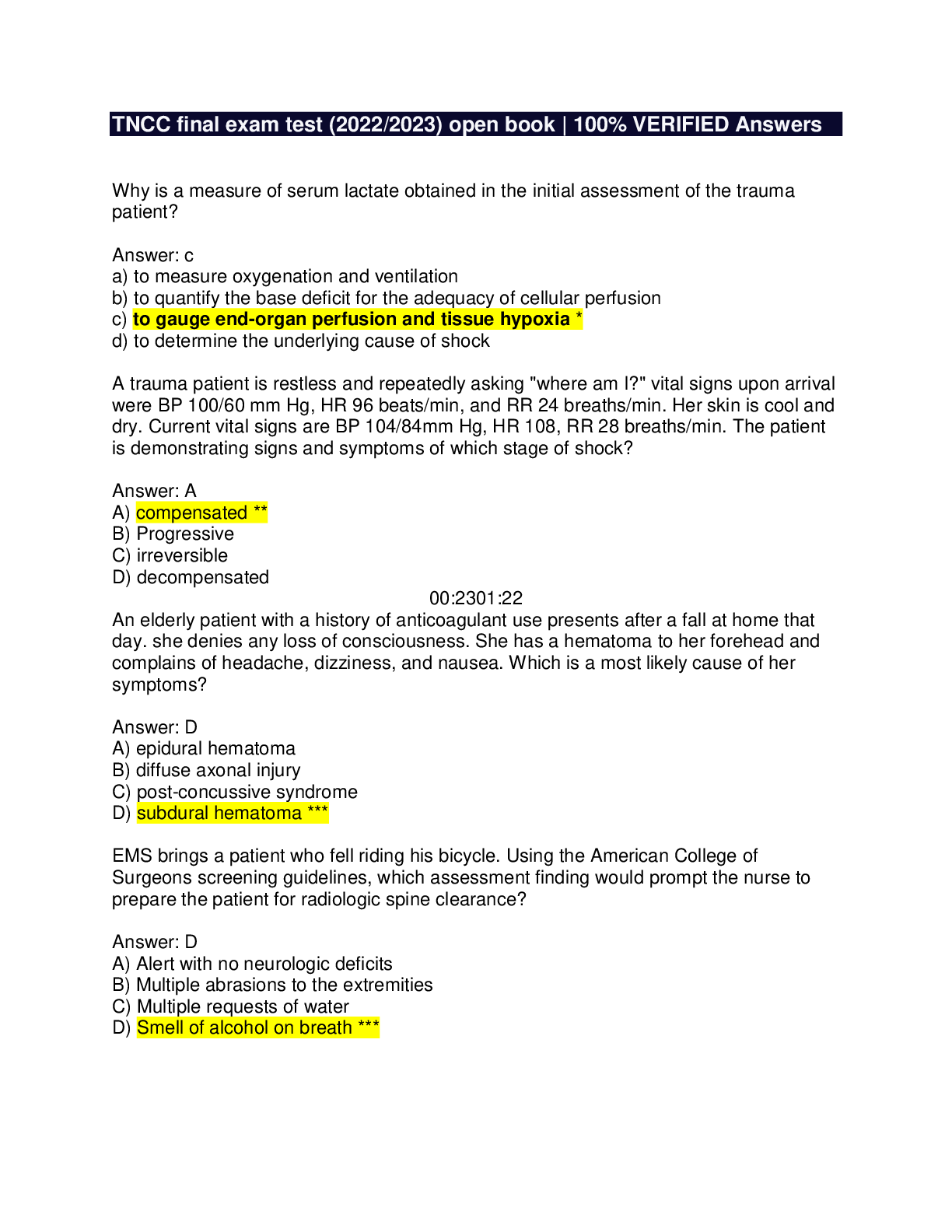
 And LETRS Unit 8 Final Assessment Test.png)
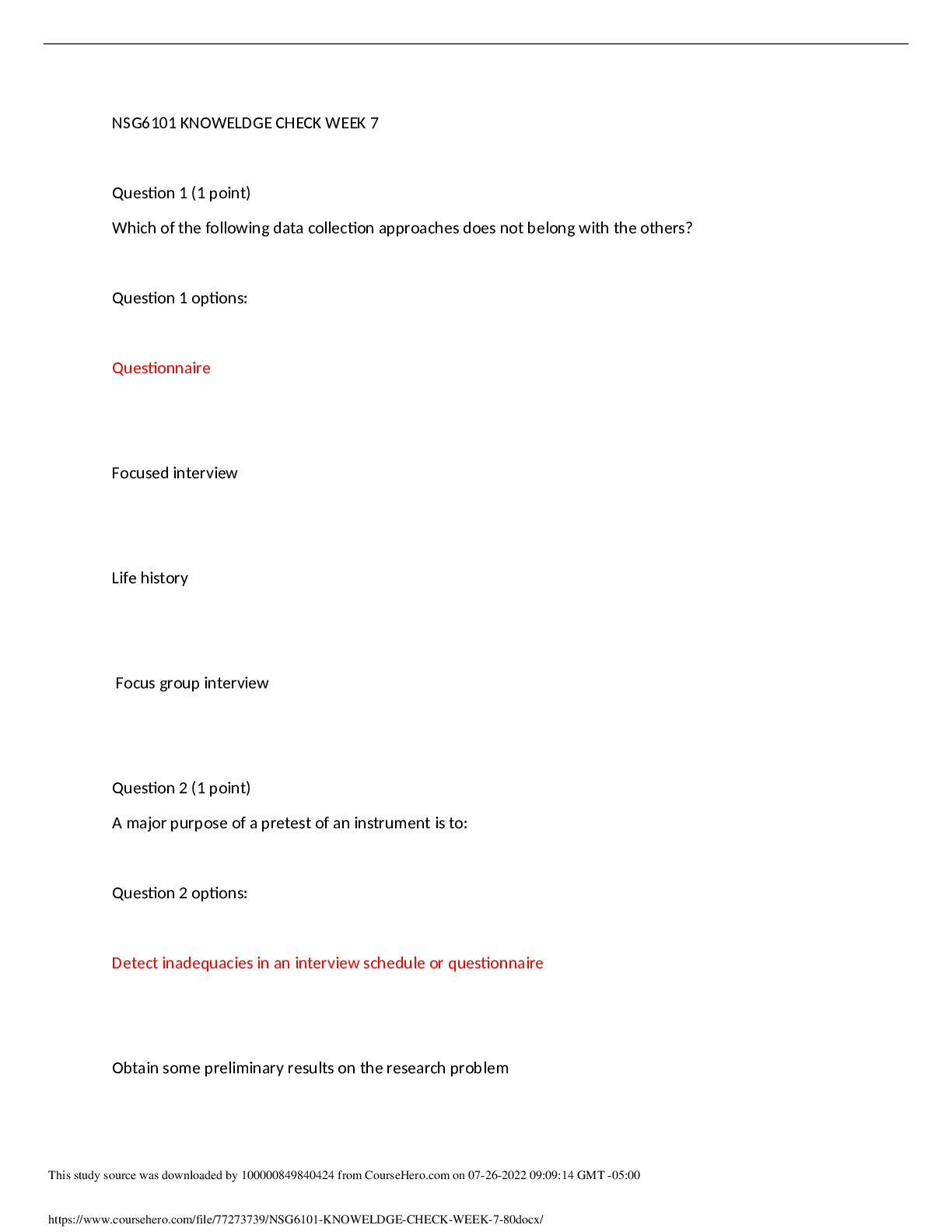
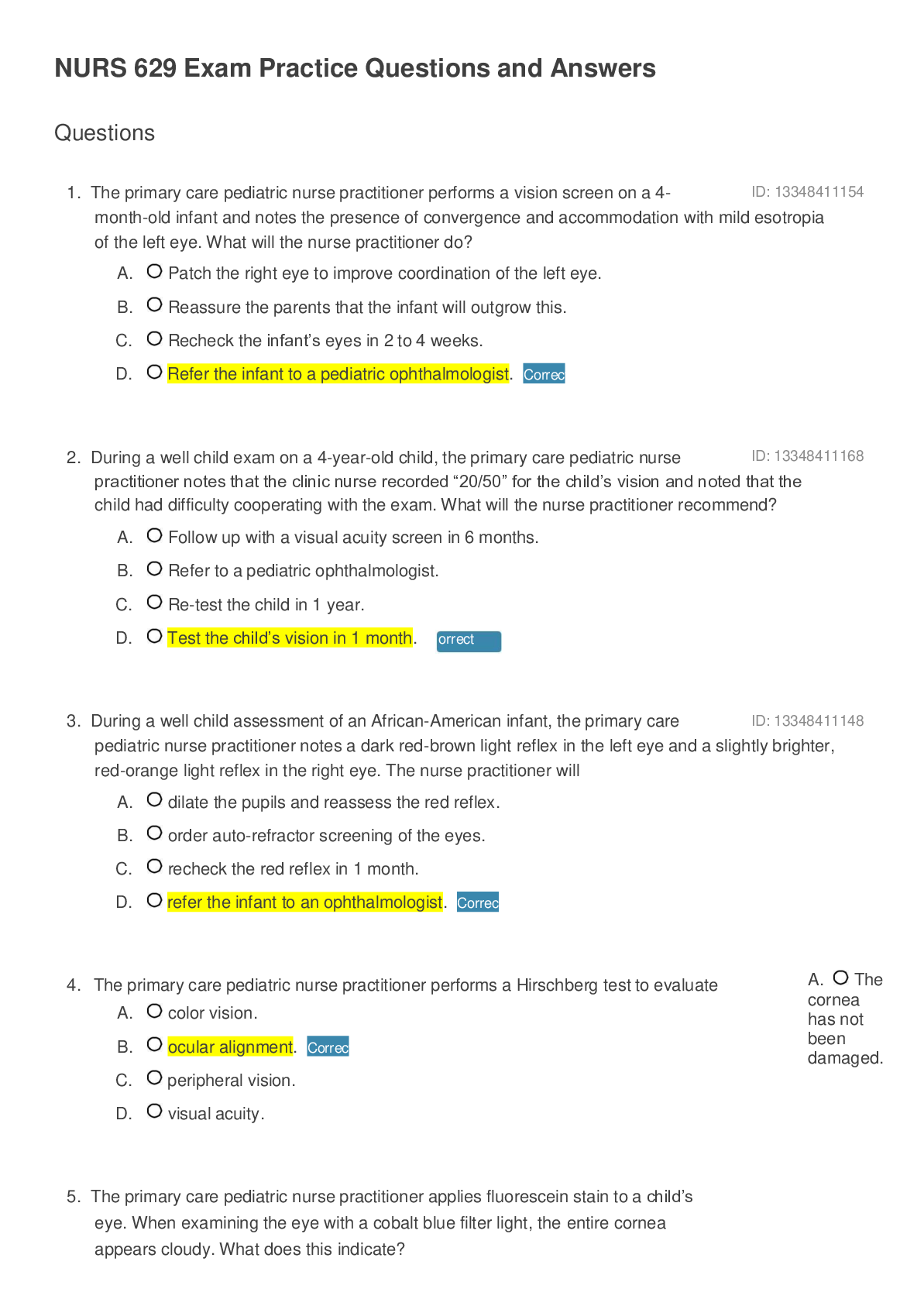
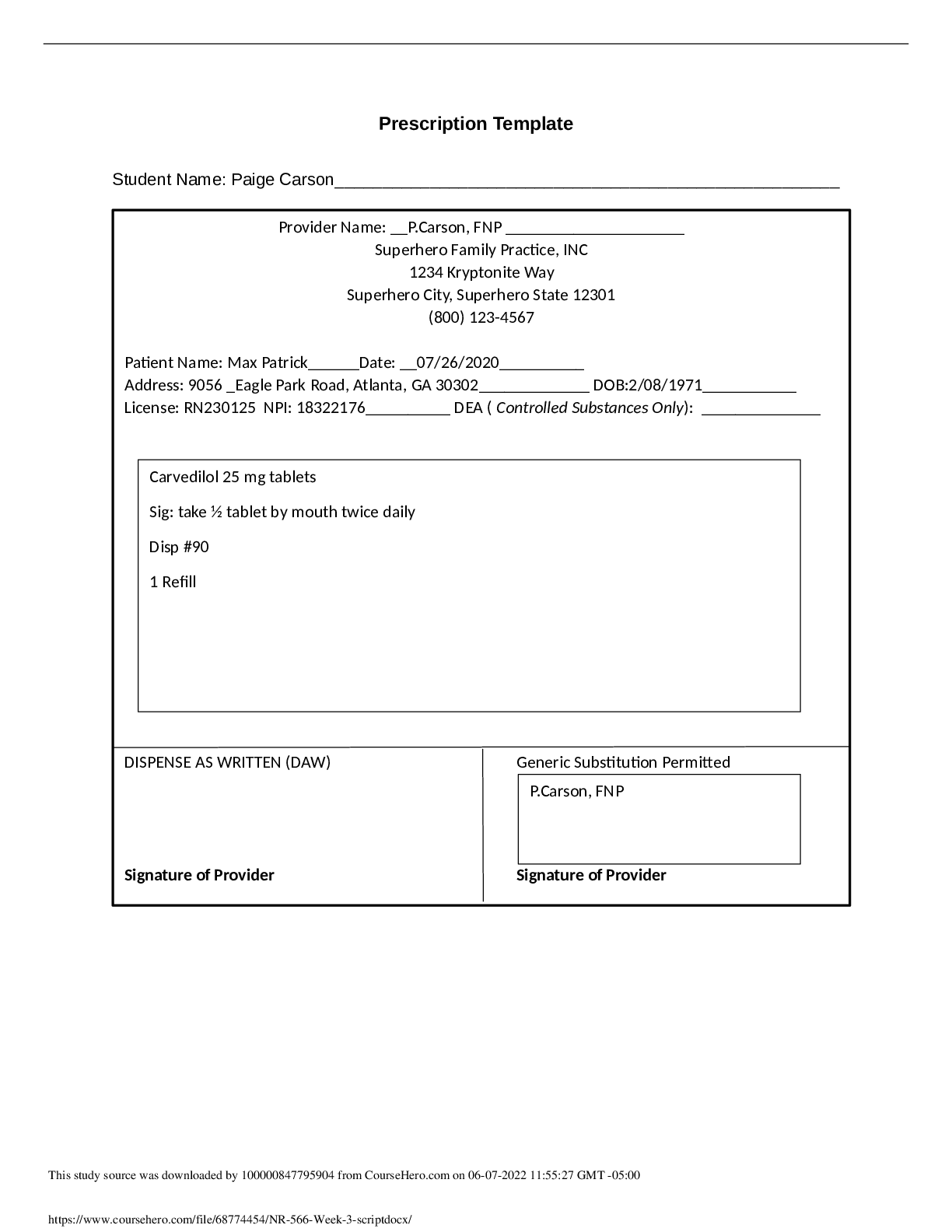
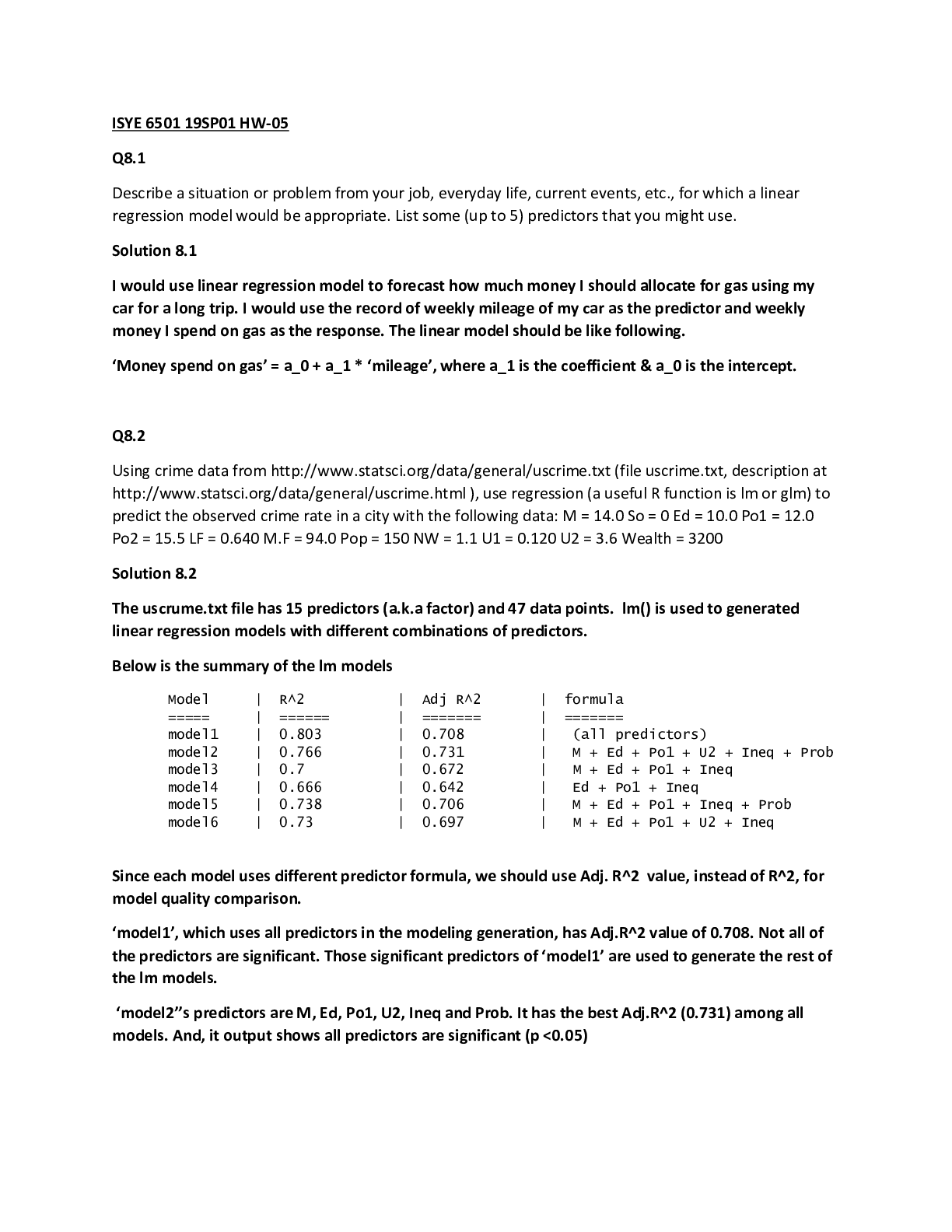
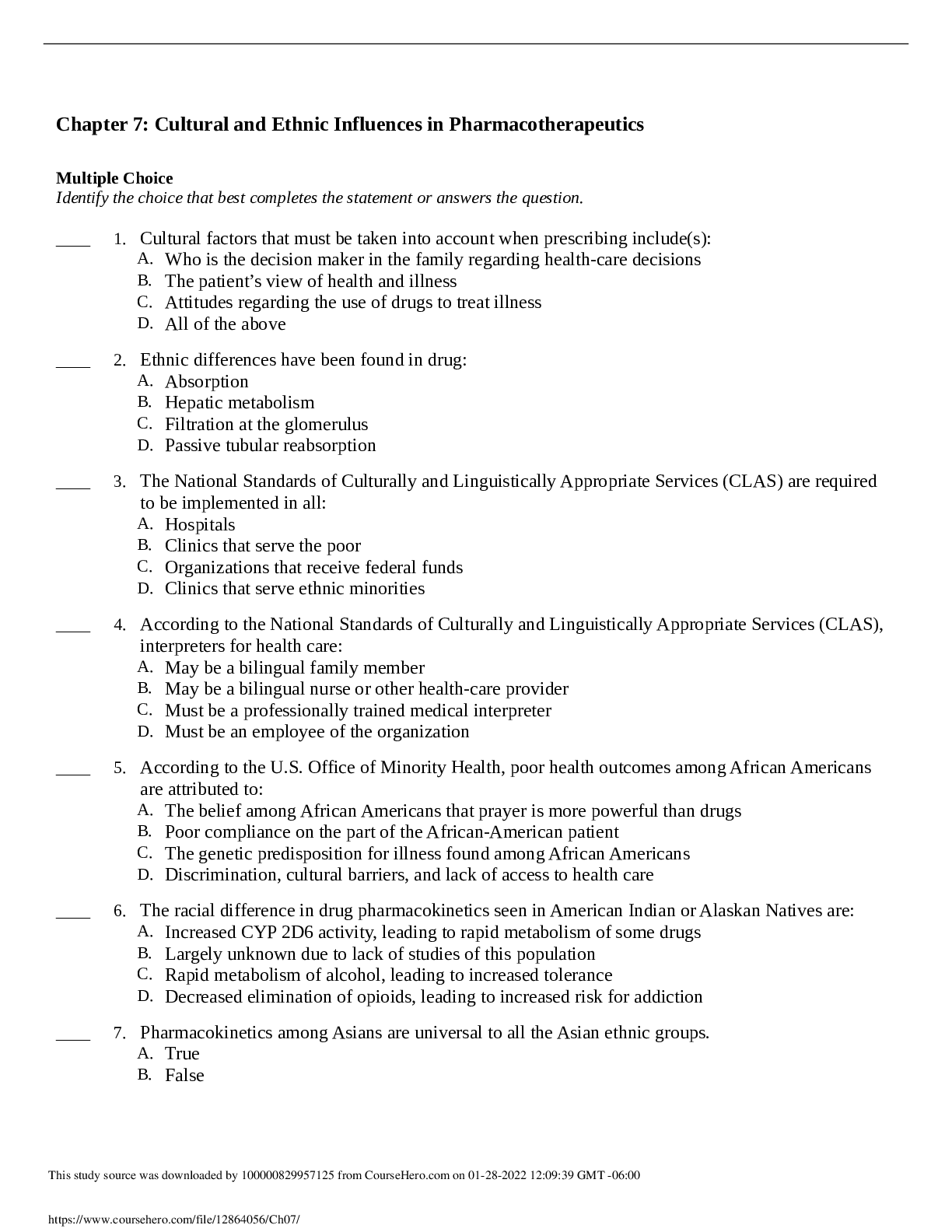

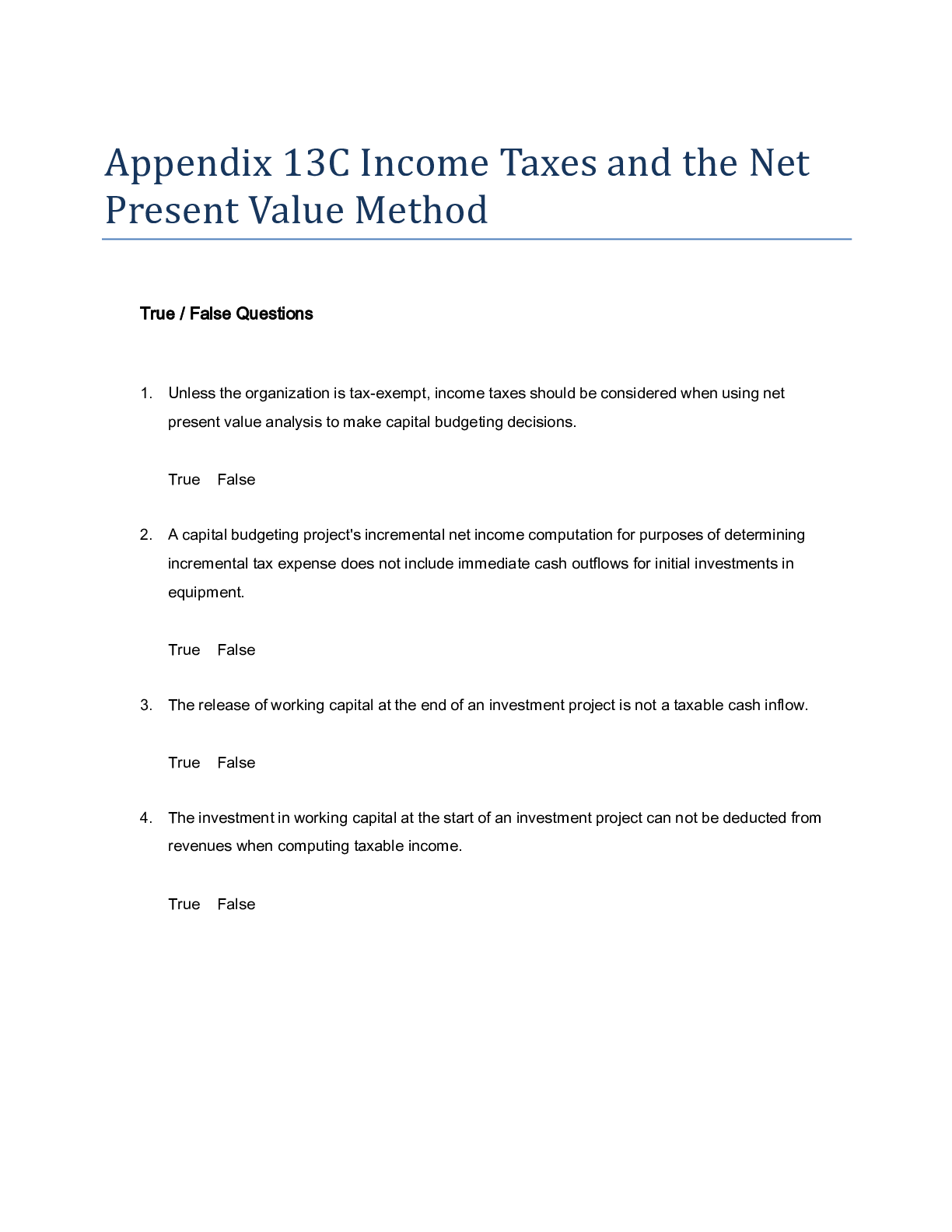
 (2).png)
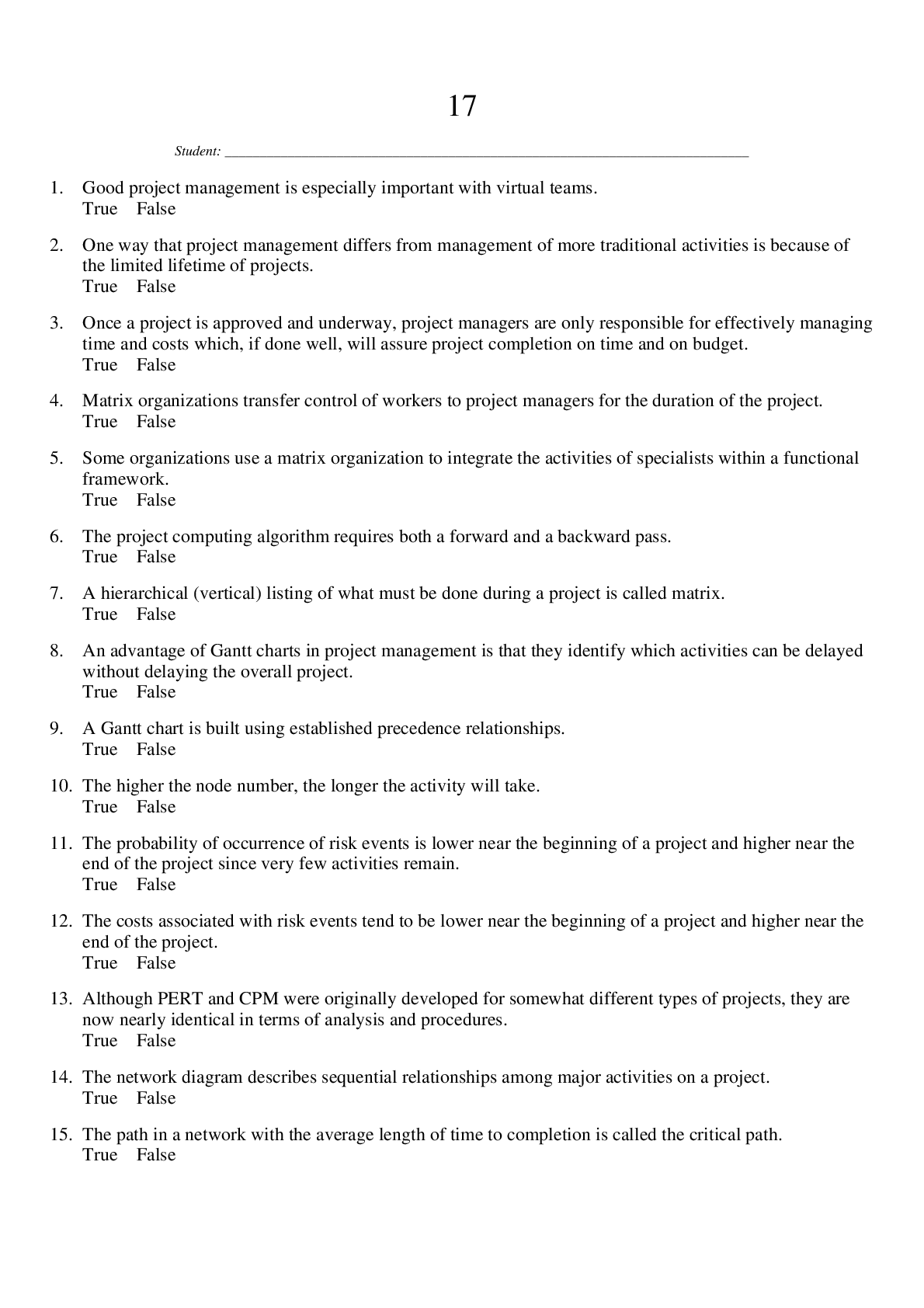
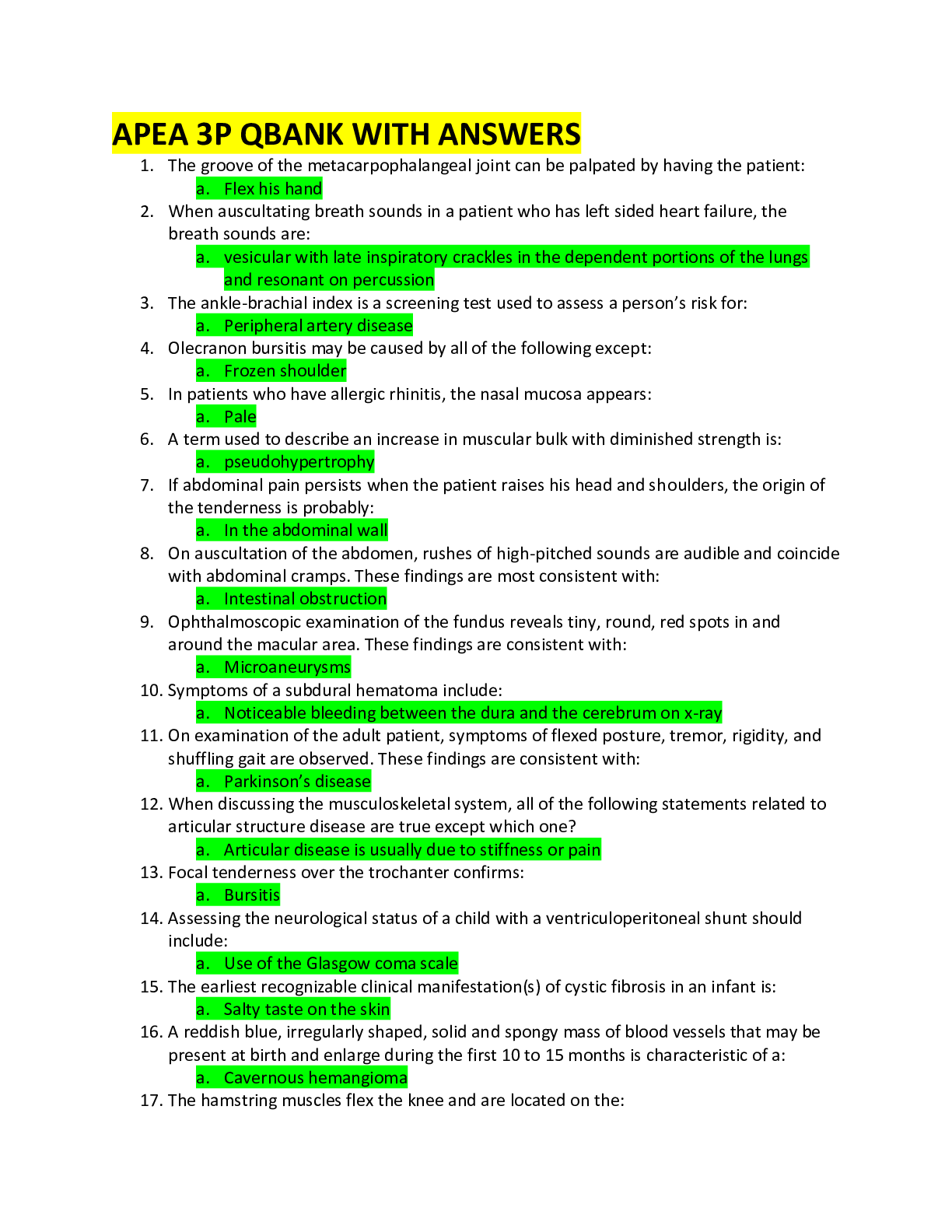
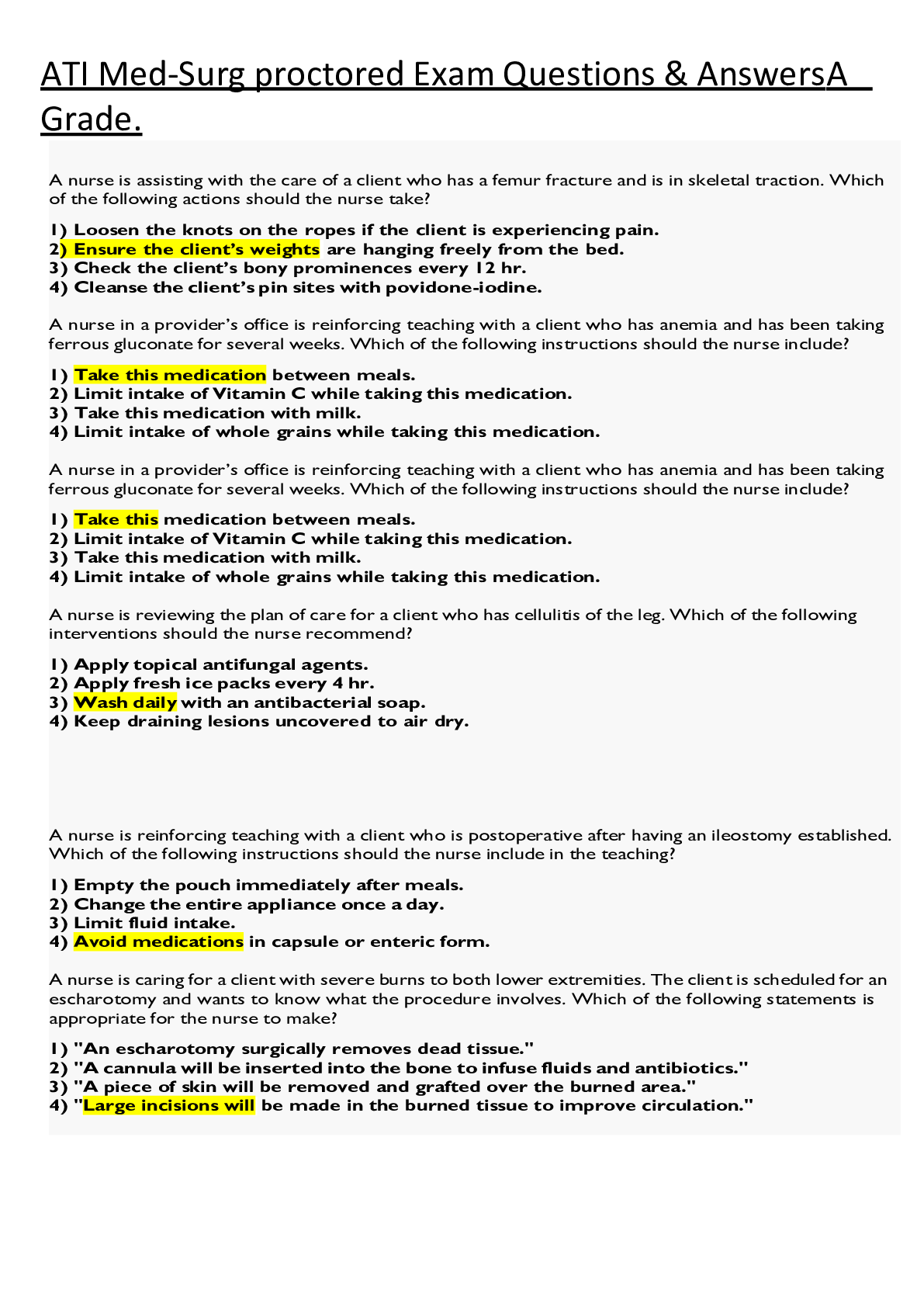
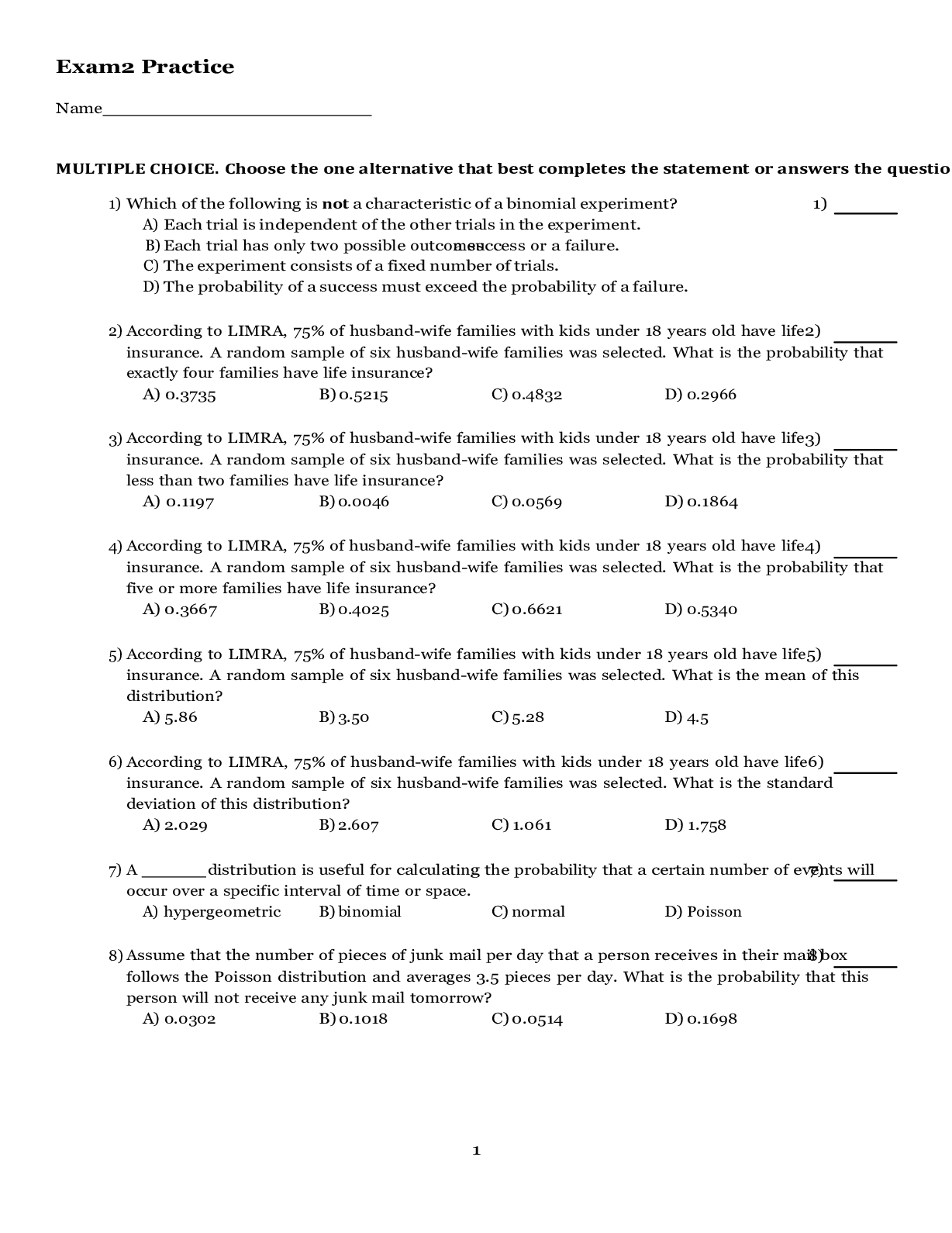
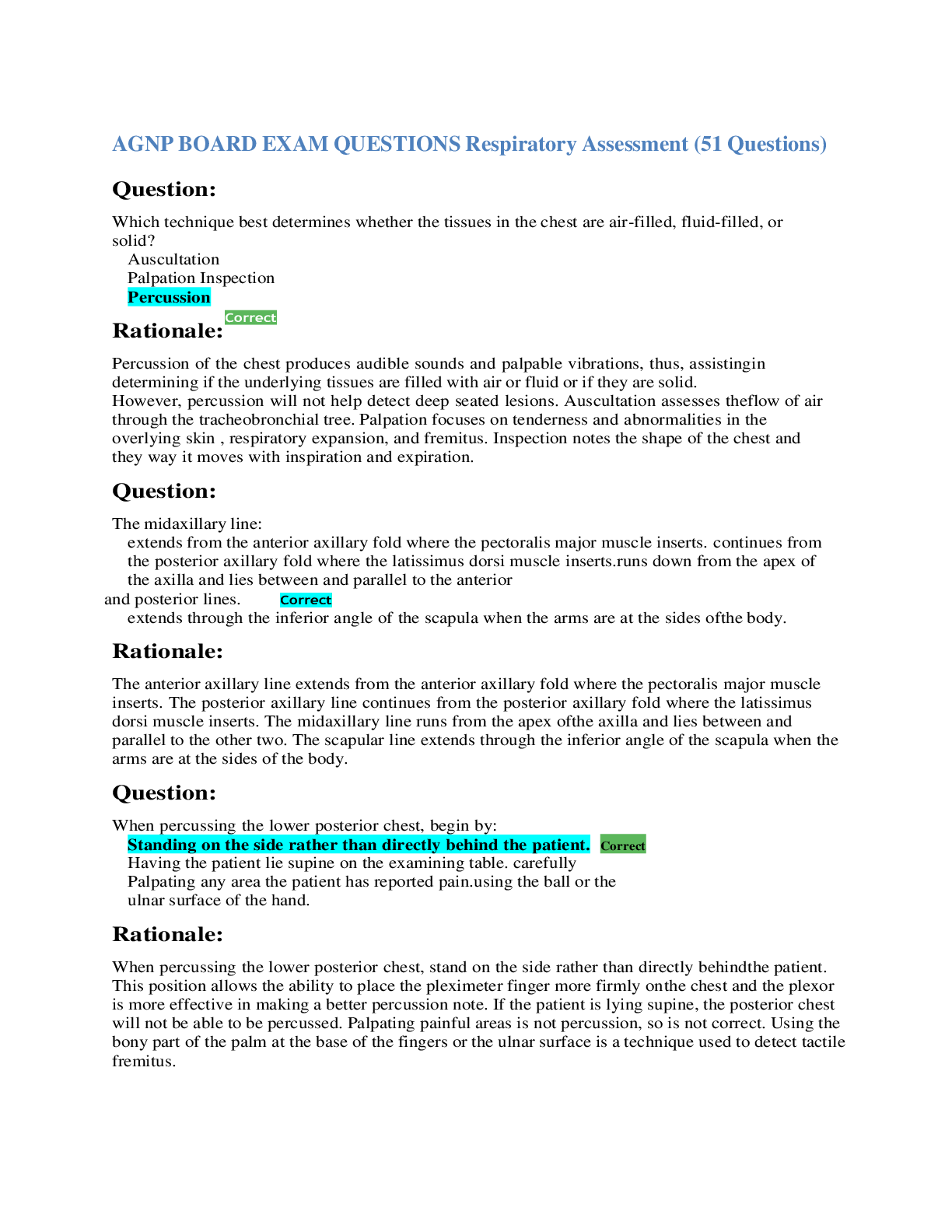
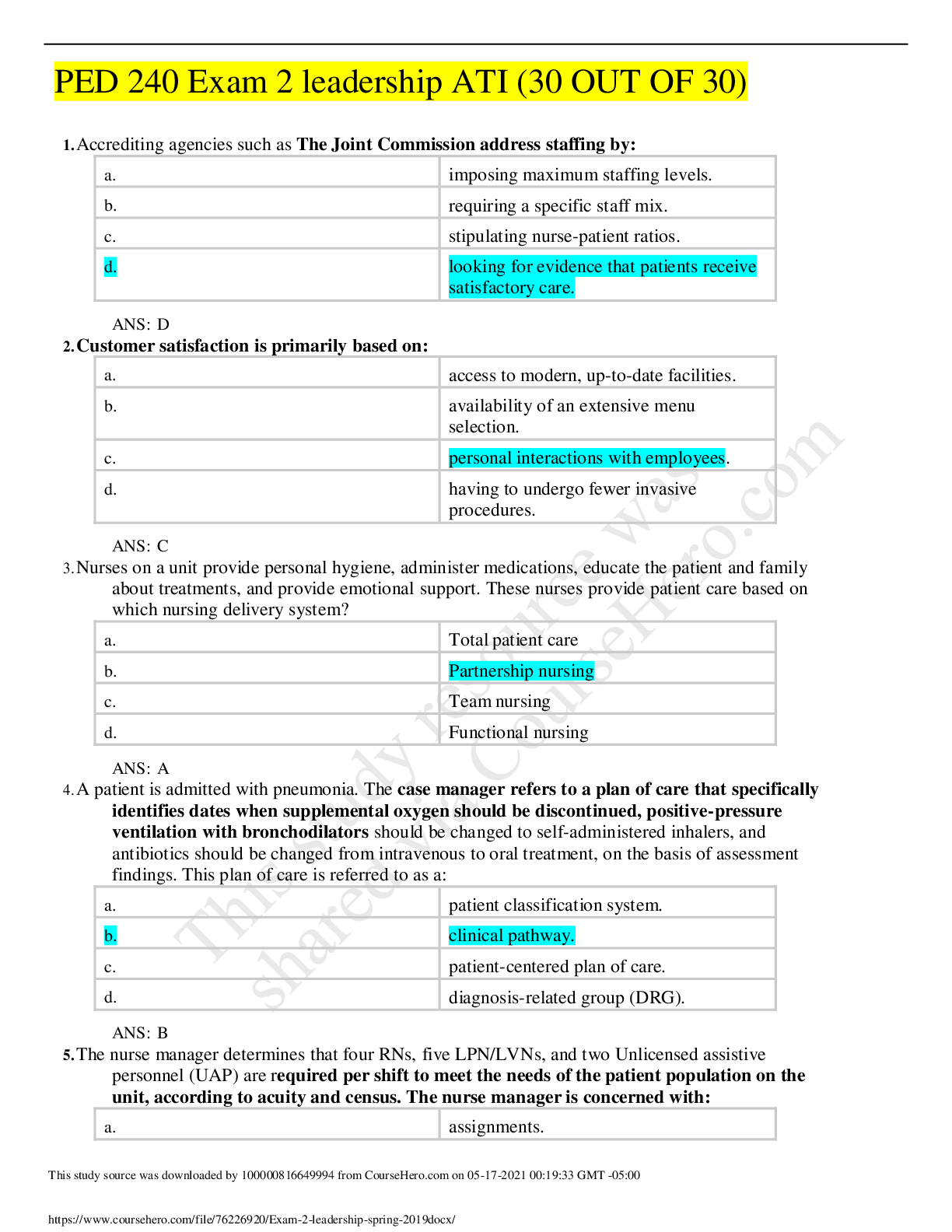
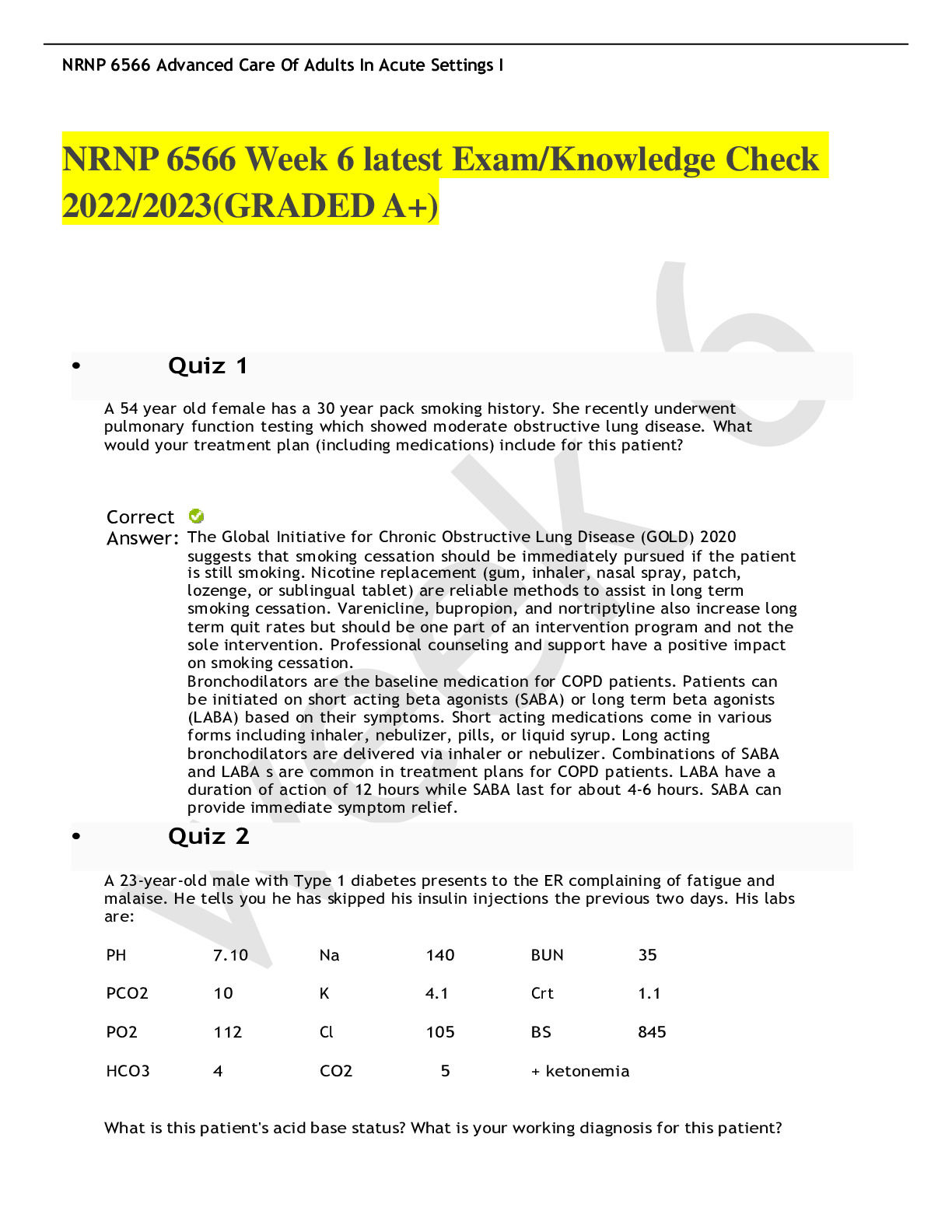
 (1).png)