*NURSING > EXAM > NURSE Dilemma Student Burnout STUDENT Worksheet _mavis anderson 84 years old / NUR 1022C clinicals.. (All)
NURSE Dilemma Student Burnout STUDENT Worksheet _mavis anderson 84 years old / NUR 1022C clinicals...
Document Content and Description Below
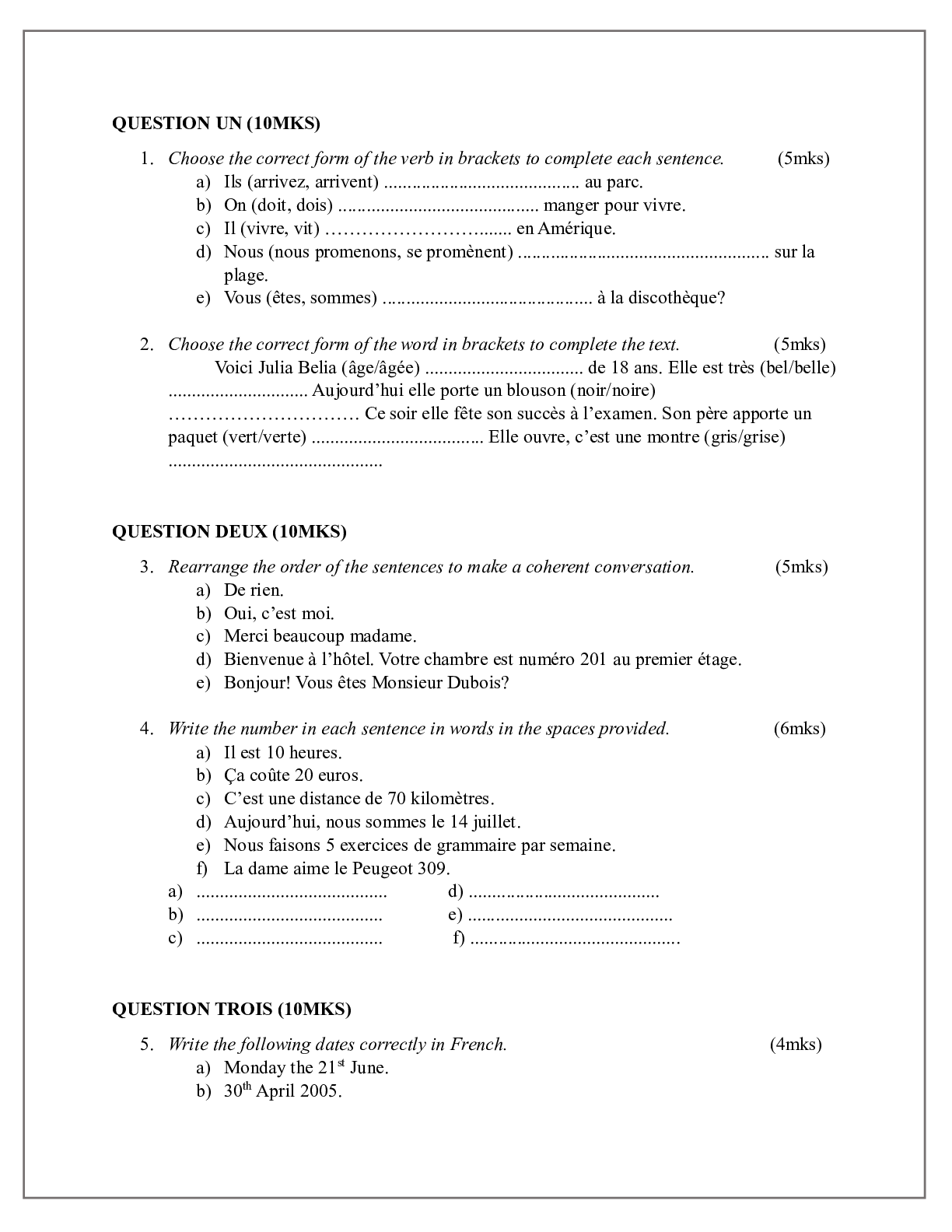
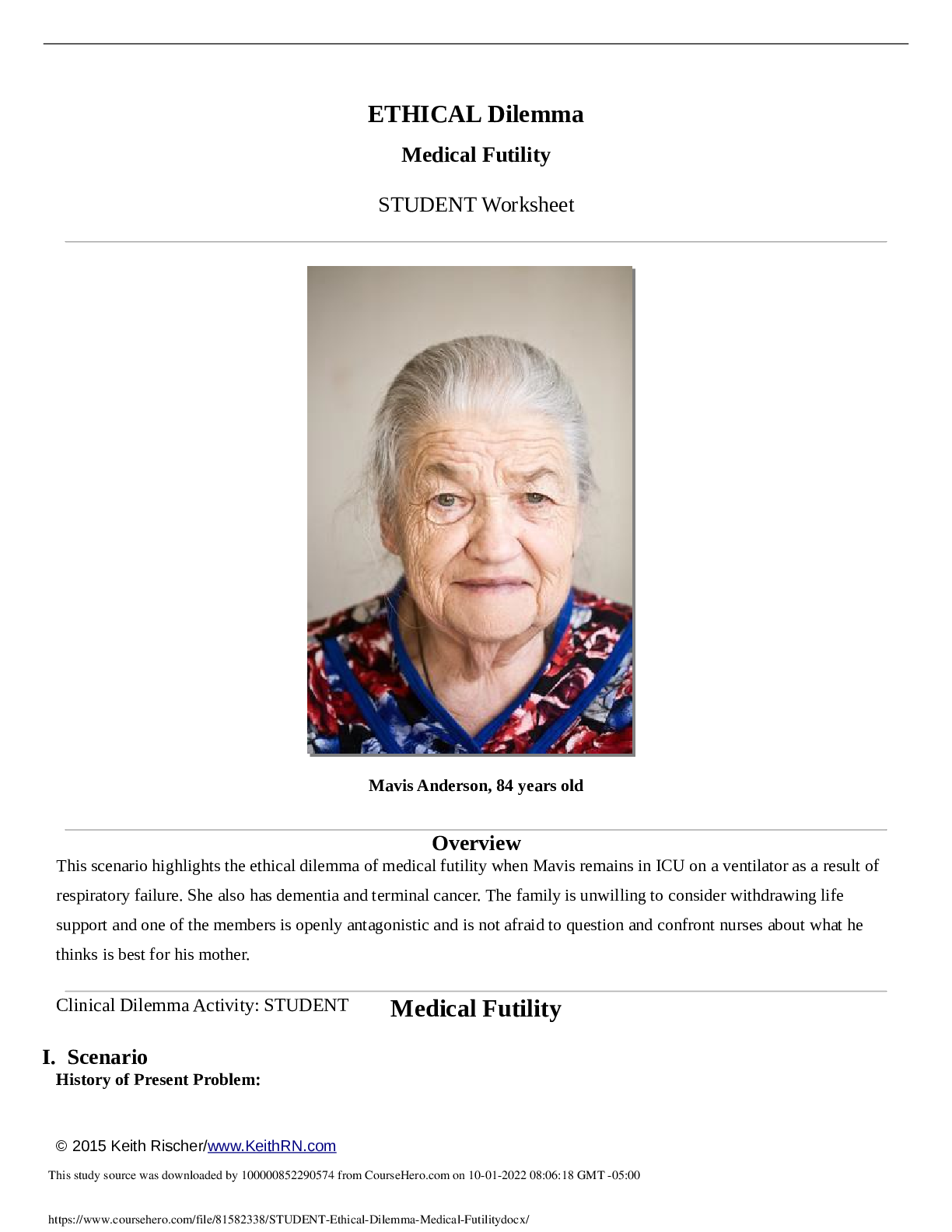
ETHICAL Dilemma Medical Futility STUDENT Worksheet Mavis Anderson, 84 years old Overview This scenario highlights the ethical dilemma of medical futility when Mavis remains in ICU on a ... ventilator as a result of respiratory failure. She also has dementia and terminal cancer. The family is unwilling to consider withdrawing life support and one of the members is openly antagonistic and is not afraid to question and confront nurses about what he thinks is best for his mother. Clinical Dilemma Activity: STUDENT I. Scenario History of Present Problem: Medical Futility Mavis Anderson is a frail, 84-year-old woman who was admitted to your medical unit six days ago after falling at home. She has a large hematoma on her right lateral hip. She is on warfarin daily for chronic atrial fibrillation. She has a history of stage IV breast cancer with metastasis to the liver, dementia, and COPD. Despite having only months to live, she is currently a full code. Mavis does not have a living will, but according to her son, who has the power of attorney (POA), she would want to live and wants everything done to support her. Ten days ago Mavis developed progressive SOB with respiratory failure that required intubation and mechanical ventilation. CXR confirmed bilateral infiltrates consistent with aspiration pneumonia. She continues to require ventilator support with vent settings of AC: 12, TV: 500, PEEP: +5, FiO2: 60%. Bipap weans have lasted only 15 minutes before she becomes tachypneic with RR >30 and O2 sat that drops to <90%. Personal/Social History: Mavis lives in a skilled long-term care facility and is widowed. She has six children who are actively involved in her care and live in the area. The oldest son, Tom, is POA. What data from the histories is important & RELEVANT; therefore it has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: No living will. Son power of attorney (POA). Bilateral infiltrates consistent with aspiration pneumonia. Bipap weans lasted only 15 min. before she become tachypneic with RR >30 and O2 drops to <90% Requires ventilator support. Because patient does not have a living will, the son holds the power to make medical decisions on behalf of Mavis. Son will oversee medical decisions. Air spaces in the lung are filled with fluid. Patient not able to tolerate weans due to Patient is unable to breath on her. Related to respiratory complications. RELEVANT Data from Social History: Clinical Significance: Has six children who are actively involved in her care. Patient has a lot of support when it comes to her care but it could also make decision making difficult when so many people are involved. II. The Dilemma Begins… Current Concern: Palliative care was consulted and the physician documented the following: • Mavis is critically and terminally ill with no chance of recovery to return to her prior living arrangement. She would require ventilatory support at a long term-care-acute-care (LTAC) facility with 24/7 nursing care. Despite this assessment, the son Tom who is POA continues to insist that full ICU support be continued that includes ventilator, vasopressors (neosynephrine), and parenteral tube feedings. • Mavis and her family are Catholic, and have faith and hope for a miraculous recovery which cannot happen unless Mavis is maximally supported in ICU. The son believes that removal of the ventilator support is akin to directly causing the death of his mother. • Palliative Plan: Care conference with all family members, medical providers and nursing. The current grim prognosis and recommendations of medical team will be presented. Tom is angry that his viewpoint does not seem to be considered by the medical providers. He openly shares his frustration and distrust of hospital staff including nursing. He has “fired” physicians who he does not feel are supportive of his wishes and current plan of care. He remains at his mother’s bedside most of the day. He intently watches everything that is done, writes in a notebook as care is provided, and questions nurses in a confrontational tone of voice. What data from the current concern is important & RELEVANT; therefore it has clinical significance to the nurse? RELEVANT Data from Current Concern: Clinical Significance: Son continues to insist that full ICU support be continued. Family is Catholic. Care conference with all family member and medical staff. Son is angry that his viewpoint does not seem to be considered. Religious background has a strong effect on the son’s decision to continue ICU support. It is not allowing the son to see the situation in the doctor’s perspective. Nurses and medical staff still need to respect the son’s decision even if they do not agree. Allowing the family and all staff assigned to this case keep everyone on one accord and it also keeps the family involved and up to date. III. Resolving the Dilemma 1. Identifying data that is RELEVANT, what is the essence of this current dilemma? Deciding whether to continue with the family’s wishes to continue ICU support or to allow a natural death since the patient is terminal. 2. What additional information is needed by the nurse that would help clarify the current dilemma? Medical staff could question if the son is making a decision based off of his own personal feelings because he does not want to see his mother pass or if this is a decision that his mother would want. 3. What additional members of the healthcare team could be used in this situation? Why? Social worker. A social worker provides conflict mediation, provides education on coping skills, participates in interdisciplinary team meetings, care planning, and ethics consultations. Ethics committees in health care institutions. (n.d.). Retrieved February 13, 2021, from https://www.ama-assn.org/delivering-care/ethics/ethics-committees-health-care- institutions 4. What is the nursing priority? Continue ICU support until a decision made. Continue to keep the family involved and updated. Work on building a trusting relationship with the family so that they will feel reassured about the situation. Support spiritual and emotional needs of the family. 5. What nursing interventions and/or principles can the nurse use to successfully resolve this clinical dilemma? Sit down with the family and get a better understanding on their feelings and viewpoint pertaining to the current situation. Educate with honesty. The family may not have a full understanding of the prognosis. Once the family has been educated sufficiently, the family will be able to come to terms peacefully and will do what is best for the patient. Be sure to show empathy and support towards the family and be sensitive with their concerns. What is the expected response of the family that indicate the nursing interventions were effective? Family will come to terms and allow staff to discontinue ICU support. 6. What response by the family would indicate that a change in the plan of care and nursing interventions are needed? The family ignoring and going against doctor’s recommendations. 7. What is the patient or family likely experiencing/feeling right now in this situation? Anger, frustration, family may be scared or fearful of losing their mother. I am sure they are not ready to let go. Family may feel betrayed by medical by going against their wishes of continuing ICU care. 8. What can I do to engage myself with this patient’s experience, and show that she matters to me as a person? Speak calmly to the patient. Use gentle touch to comfort the patient. Provide comfort. Communicate with the patient throughout procedures and let the patient know what you are going to do before doing it. Ensure patient’s dignity. 9. Does this scenario warrant a review by the medical ethics committee of the hospital? Why or why not? Yes, because the ethics committee could assist in addressing the issue and help facilitate a sound decision that respects the family’s values, concerns, and interests. They provide support and guidance. The ethics committee serves as advisor and educators. Ethics committees in health care institutions. (n.d.). Retrieved February 13, 2021, from https://www.ama-assn.org/delivering-care/ethics/ethics-committees-health- care-institutions 10. What was learned from this case study that you will incorporate into your practice? I got a better understanding on how to handle this ethical dilemma and what steps I need to take to help support the family come to a conclusion. How to show support towards the family and their decisions and who to get involved to help resolve the dilemma. [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 06, 2021
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Aug 06, 2021
Downloads
0
Views
47



 (1).png)
 (1).png)
 (1).png)