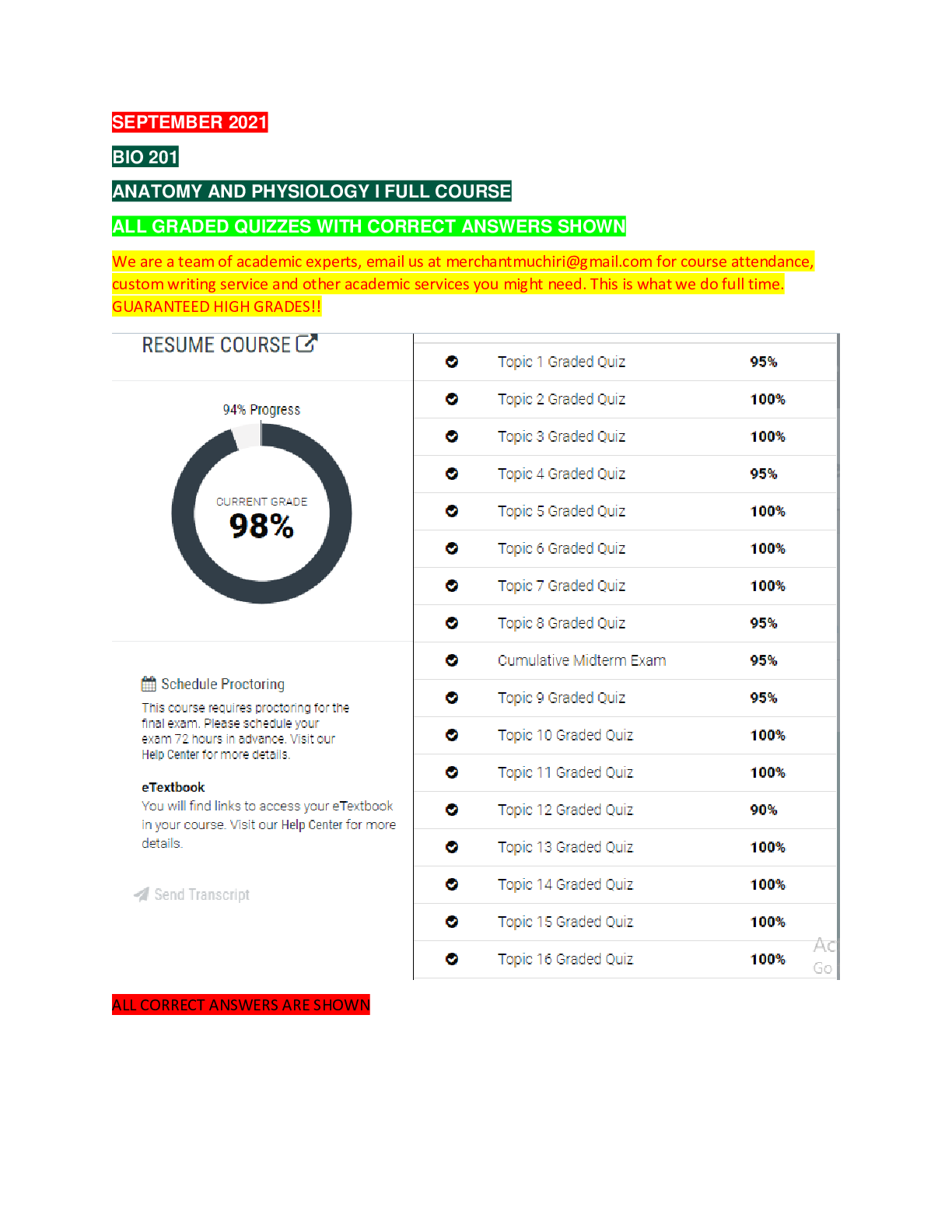
*NURSING > EXAM > Chamberlain College of NursingNR 5082-NR 508 WEEK 4 MIDTERM Exam 2020 (Set-2). (All)
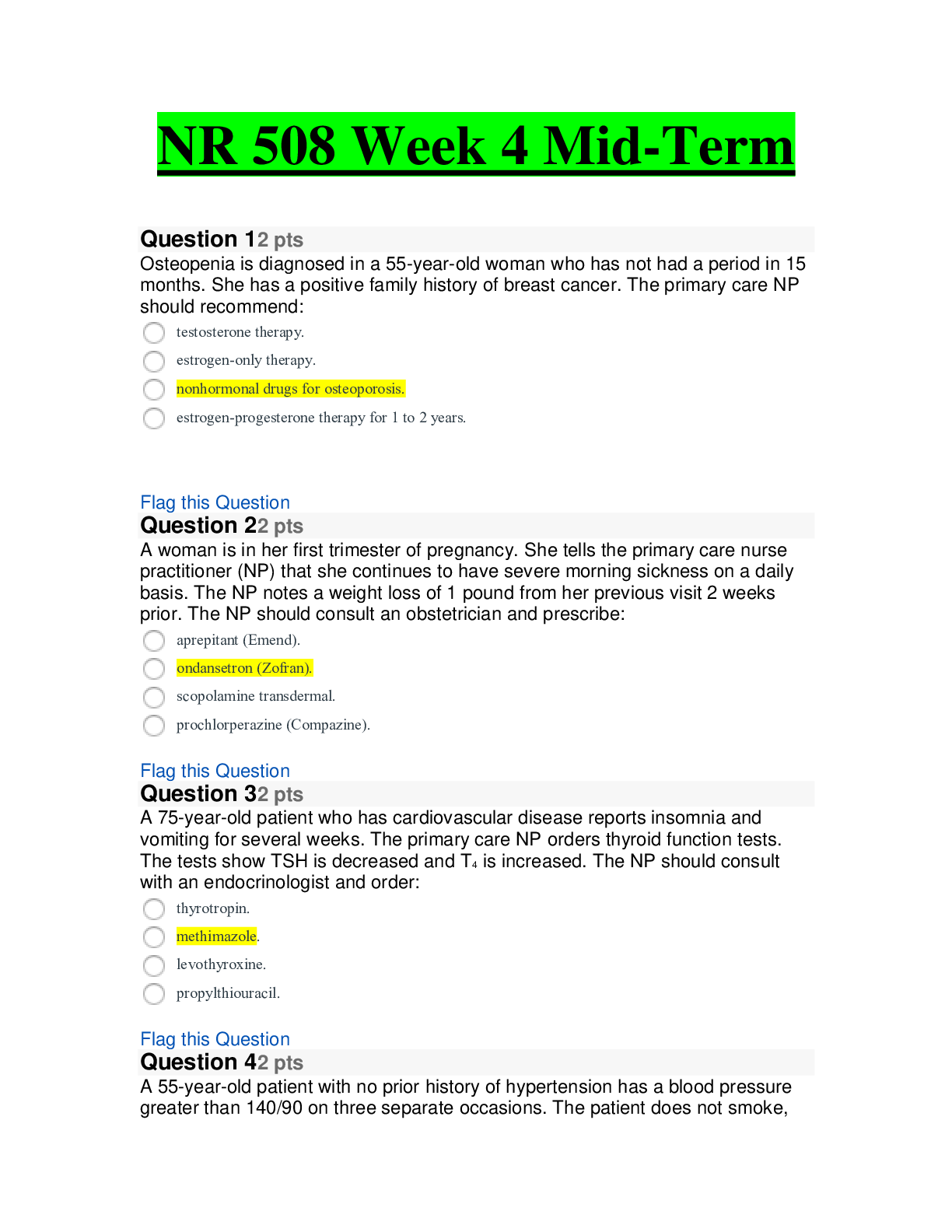
Chamberlain College of NursingNR 5082-NR 508 WEEK 4 MIDTERM Exam 2020 (Set-2).
Document Content and Description Below
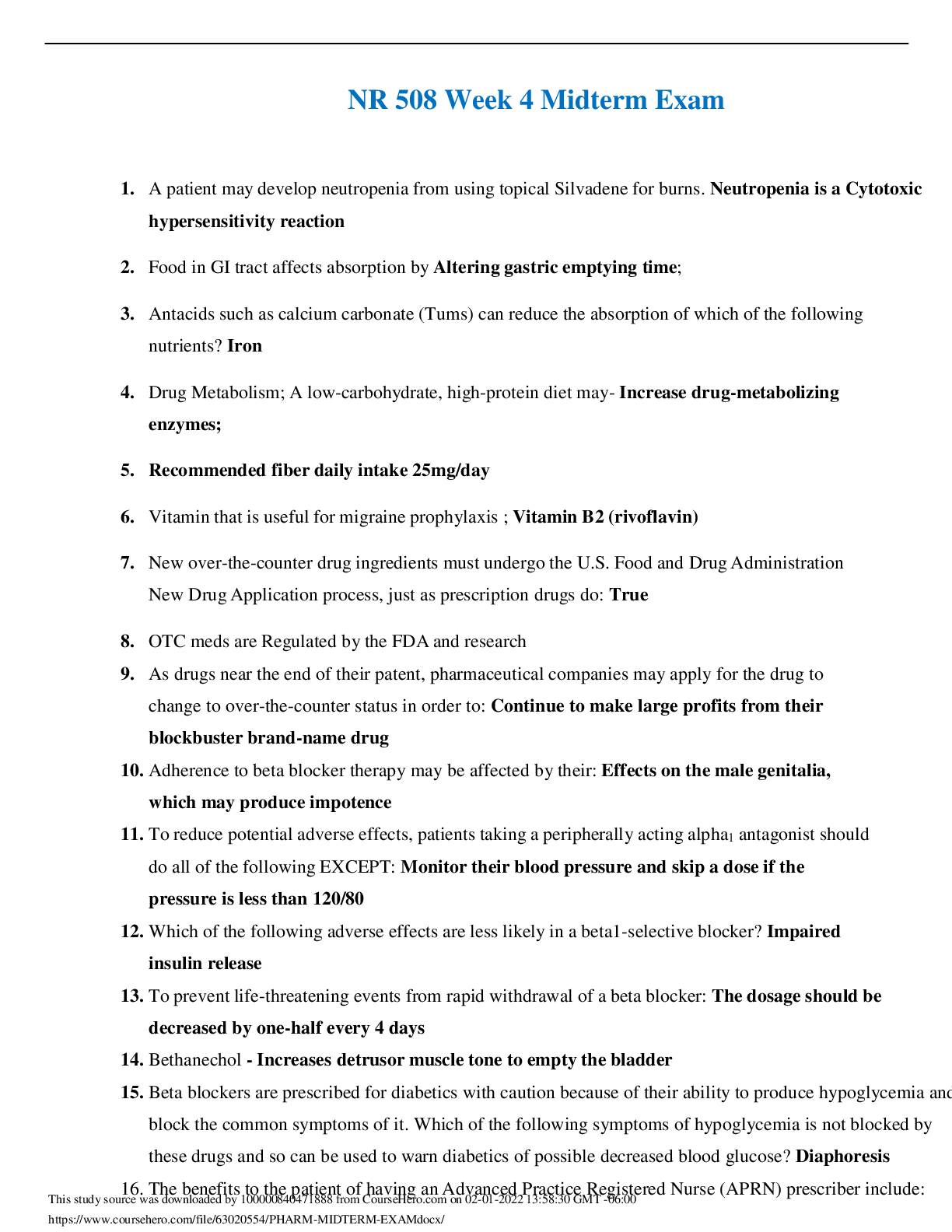
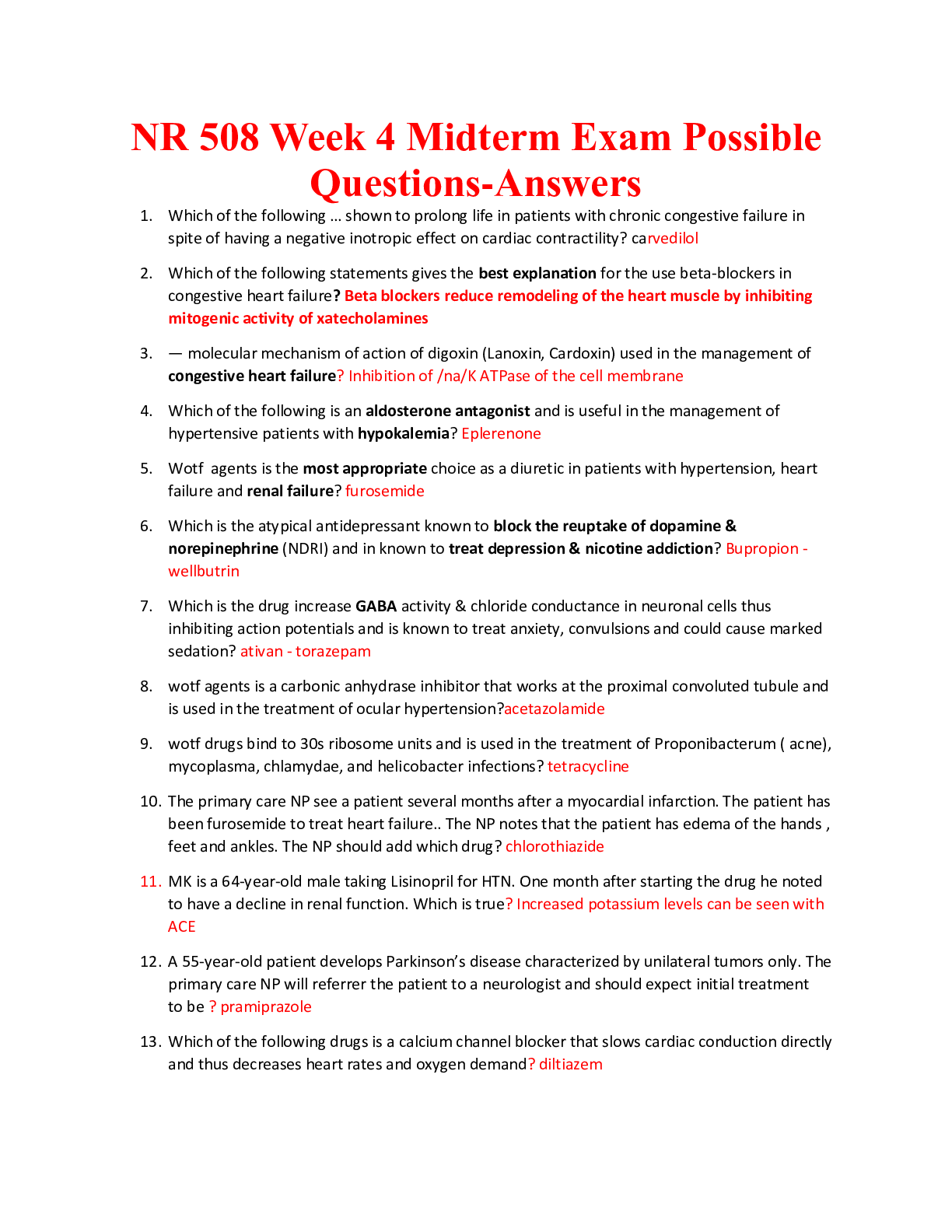
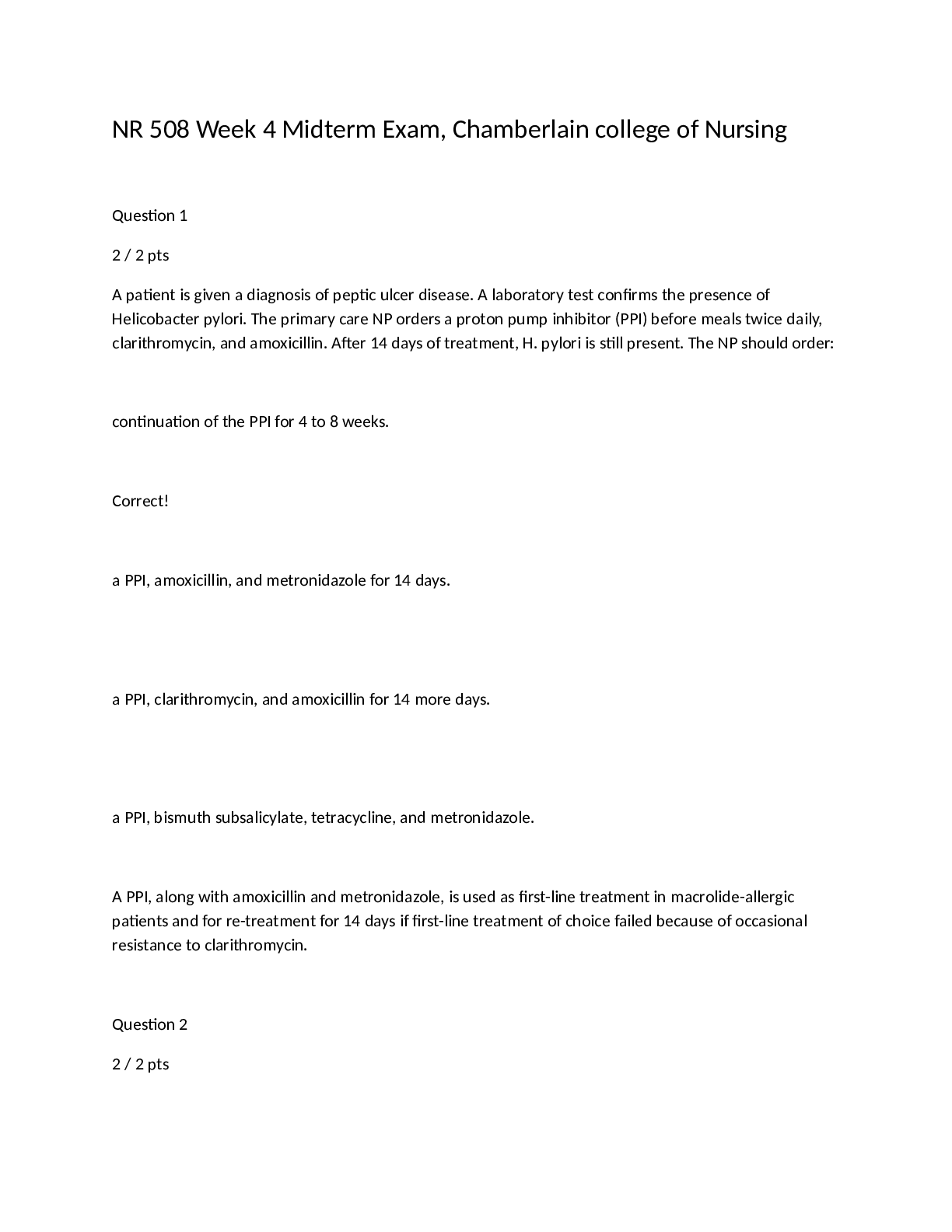
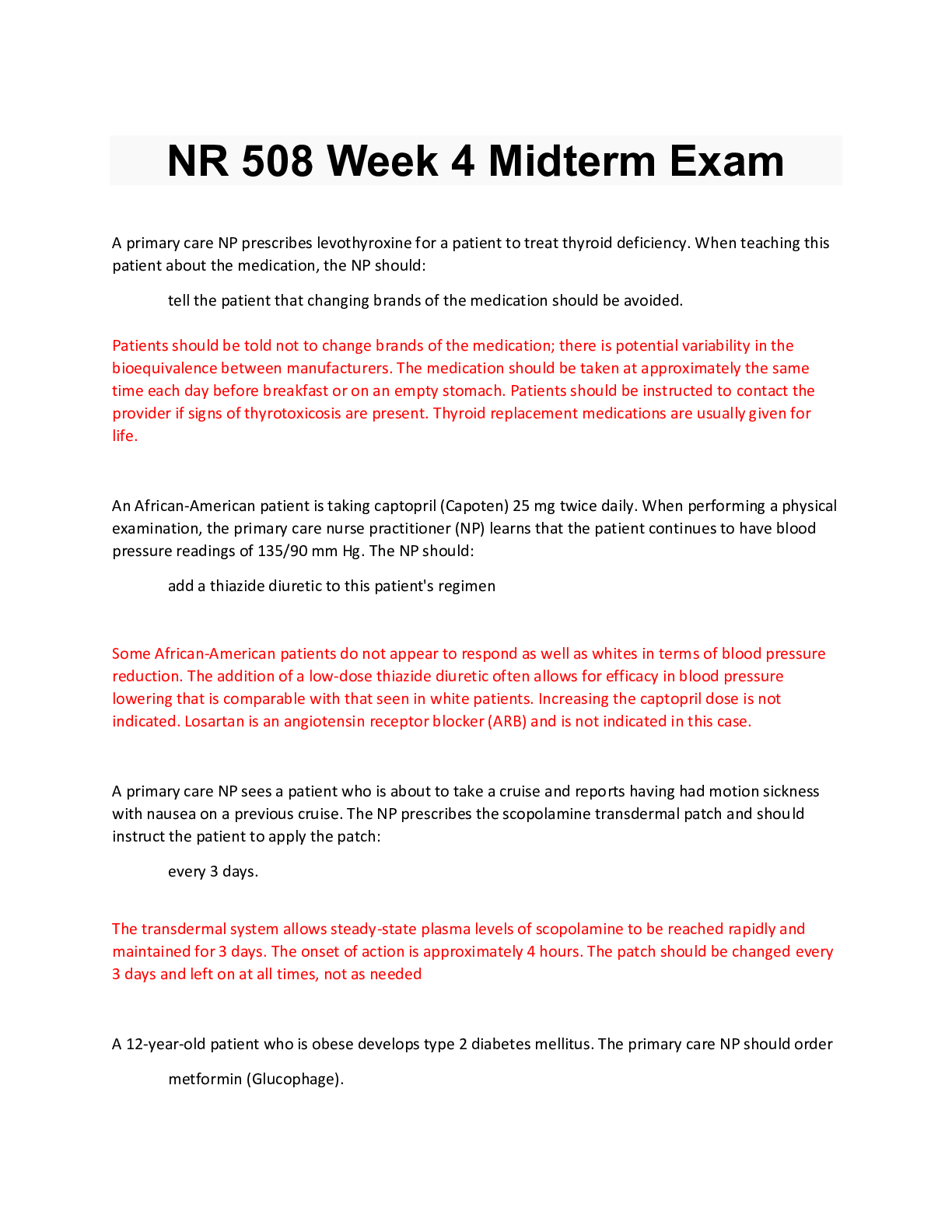
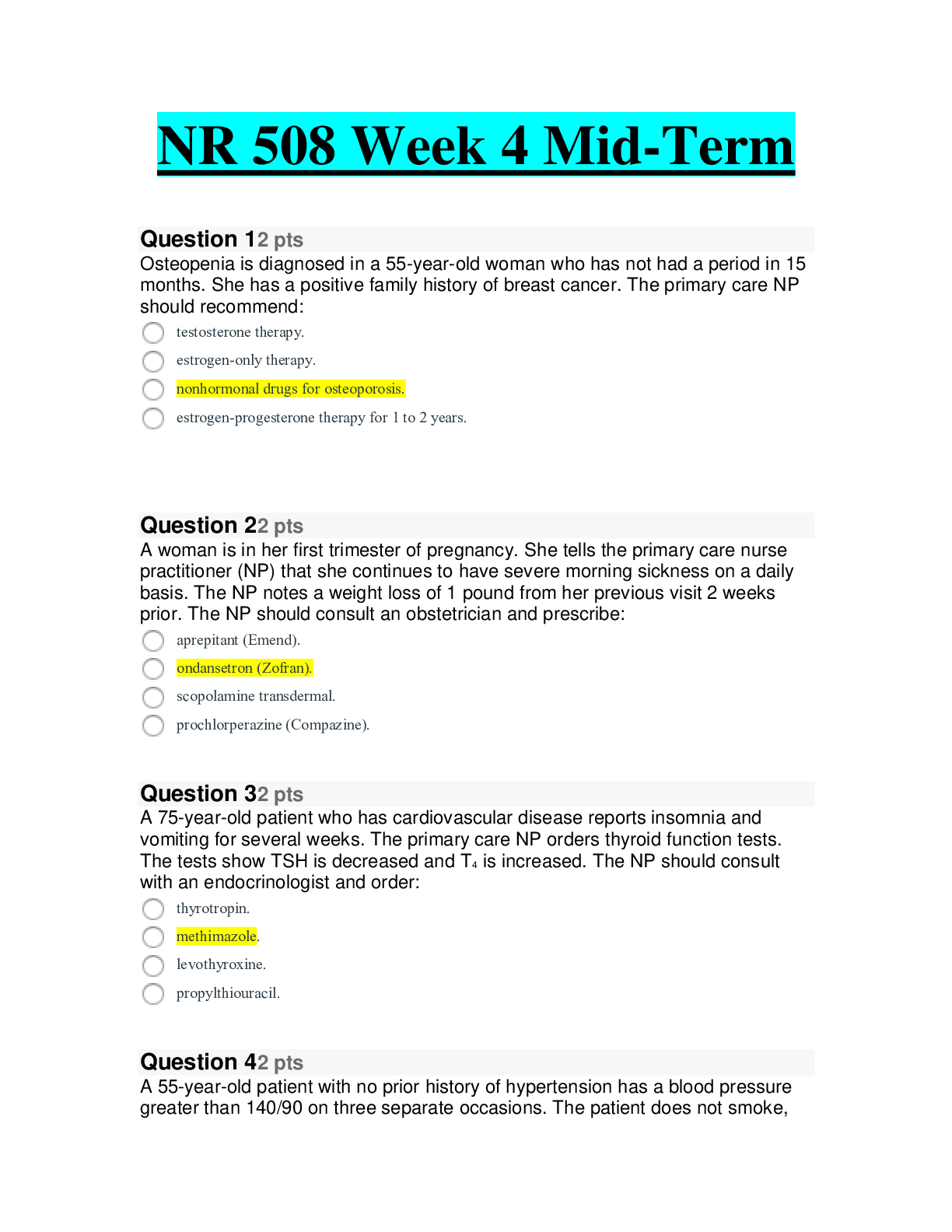
NR 508 Week 4 Midterm Exam, Chamberlain college of Nursing Question 1 2 / 2 pts A patient is given a diagnosis of peptic ulcer disease. A laboratory test confirms the presence of Helicobacter pylo... ri. The primary care NP orders a proton pump inhibitor (PPI) before meals twice daily, clarithromycin, and amoxicillin. After 14 days of treatment, H. pylori is still present. The NP should order: continuation of the PPI for 4 to 8 weeks. Correct! a PPI, amoxicillin, and metronidazole for 14 days. a PPI, clarithromycin, and amoxicillin for 14 more days. a PPI, bismuth subsalicylate, tetracycline, and metronidazole. A PPI, along with amoxicillin and metronidazole, is used as first-line treatment in macrolide-allergic patients and for re-treatment for 14 days if first-line treatment of choice failed because of occasional resistance to clarithromycin. Question 2 2 / 2 ptsA patient is newly diagnosed with type 2 diabetes mellitus. The primary care NP reviews this patient’s laboratory tests and notes normal renal function, increased triglycerides, and deceased HDL levels. The NP should prescribe: nateglinide (Starlix). glyburide (Micronase). colesevelam (Welchol). Correct! metformin (Glucophage). Metformin is recommended as initial pharmacologic treatment for type 2 diabetes. It has been shown to decrease triglycerides and LDLs. Question 3 2 / 2 pts The primary care NP is considering prescribing captopril (Capoten) for a patient. The NP learns that the patient has decreased renal function and has renal artery stenosis in the right kidney. The NP should: Correct! initiate ACE inhibitor therapy at a low dose.consider a different drug class to treat this patient’s symptoms. give the captopril with a thiazide diuretic to improve renal function. orderlisinopril (Zestril) instead of captopril to avoid increased nephropathy. Patients with impaired renal function should use low-dose ACE inhibitors. It is not necessary to avoid ACE inhibitors with unilateral renal stenosis. Question 4 2 / 2 pts A woman who has been taking a COCP for 2 months tells the primary care NP that she has had several headaches, breakthrough bleeding, and nausea. The NP should counsel the woman: to change to a progestin-only pill. to stop taking the COCP immediately. to use a backup form of contraception. Correct!that these effects will likely decrease in another month. Breakthrough bleeding, nausea, and headaches are common during the first 3 months of therapy and should improve without intervention. Progestin-only pills are used for lactating women only. Prolonged bleeding and severe headache would warrant discontinuation of the COCP. Backup contraception is not indicated. Question 5 2 / 2 pts A patient who has hyperlipidemia has been taking atorvastatin (Lipitor) 60 mg daily for 6 months. The patient’s initial lipid profile showed LDL of 180 mg/dL, HDL of 45 mg/dL, and triglycerides of 160 mg/dL. The primary care NP orders a lipid profile today that shows LDL of 105 mg/dL, HDL of 50 mg/dL, and triglycerides of 120 mg/dL. The patient reports muscle pain and weakness. The NP should: order liver function tests (LFTs). Correct! order a creatine kinase-MM (CK-MM) level. change atorvastatin to twice-daily dosing. add gemfibrozil (Lopid) to the patient’s medication regimen. Hepatotoxicity and muscle toxicity are the two primary adverse effects of greatest concern with statin use. Patients who report muscle discomfort or weakness should have a CK-MM level drawn. LFTs areindicated with signs of hepatotoxicity. It is not correct to change the dosing schedule. Gemfibrozil is not indicated. Question 6 2 / 2 pts An 80-year-old patient who has persistent AF takes warfarin (Coumadin) for anticoagulation therapy. The patient has an INR of 3.5. The primary care NP should consider: lowering the dose of warfarin. Correct! rechecking the INR in 1 week. omitting a dose and resuming at a lower dose. omitting a dose and administering 1 mg of vitamin K. This patient’s INR is only minimally prolonged, so no dose reduction is required. The NP should recheck the INR periodically. If the INR becomes more prolonged, lowering the dose of warfarin is recommended. If the INR approaches 5, omitting a dose and resuming at a lower dose is recommended. Vitamin K is used for an INR of 9 or greater. Question 7 2 / 2 ptsPersistent atrial fibrillation (AF) is diagnosed in a patient who has valvular disease, and the cardiologist has prescribed warfarin (Coumadin). The patient is scheduled for electrical cardioversion in 3 weeks. The patient asks the primary care nurse practitioner (NP) why the procedure is necessary. The NP should tell the patient: Correct! this medication prevents clots but does not alter rhythm. if the medication proves effective, the procedure may be canceled. there are no medications that alter the arrhythmia causing AF. to ask the cardiologist if verapamil may be ordered instead of cardioversion. Persistent AF lasts longer than 7 days and episodes fail to terminate on their own, but episodes can be terminated by electrical cardioversion after therapeutic warfarin therapy for 3 weeks. Warfarin does not alter AF. β-Blockers, calcium channel blockers, and digoxin are sometimes given to alter the rate. Verapamil is not an alternative to cardioversion for patients with persistent AF. Question 8 2 / 2 pts A patient who has had a previous myocardial infarction has a blood pressure of 135/82 mm Hg. The patient’s body mass index is 28, and the patient has a fasting plasma glucose of 105 mg/dL. The primary care NP should prescribe: Correct! an angiotensin-converting enzyme inhibitor.a thiazide diuretic. lifestyle modifications. a calcium-channel blocker. This patient has prehypertension but has a compelling reason for treatment. Patients who have had a myocardial infarction should be treated with a β-blocker and angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker (ARB). Question 9 2 / 2 pts An 80-year-old female patient with a history of angina has increased TSH and decreased T4. The primary care NP should prescribe _____ mcg of _____. 25; liothyronine 75; liothyronine Correct! 25; levothyroxine75; levothyroxine Elderly individuals may experience exacerbation of cardiovascular disease and angina with thyroid hormone replacement. It is advisable to start low at 25 mcg and work up as tolerated. Liothyronine is a synthetic T3. Question 10 2 / 2 pts CRNAs in most states: must have a Drug Enforcement Administration (DEA) number to practice. must have prescriptive authority to practice. Correct! order and administer controlled substances but do not have full prescriptive authority. administer medications, including controlled substances, under direct physician supervision. Only five states grant independent prescriptive authority to CRNAs. CRNAs do not require prescriptive authority because they dispense a drug immediately to a patient and do not prescribe. Without prescriptive authority, they do not need a DEA number. Question 112 / 2 pts A patient with primary hypercholesterolemia is taking an HMG-CoA reductase inhibitor. All of the patient’s baseline LFTs were normal. At a 6-month follow-up visit, the patient reports occasional headache. A lipid profile reveals a decrease of 20% in the patient’s LDL cholesterol. The NP should: order LFTs. order CK-MM tests. consider decreasing the dose of the medication. Correct! reassure the patient that this side effect is common. LFTs should be performed at baseline, 12 weeks after initiation of therapy, and only periodically thereafter. Headaches are common side effects, but do not raise concern about hepatotoxicity. CK-MM tests are indicated if patients report muscle pain or weakness. It is not necessary to decrease the medication. Question 12 2 / 2 pts A patient takes an antispasmodic and an occasional antidiarrheal medication to treat IBS. The patient comes to the clinic and reports having dry mouth, difficulty urinating, and more frequent constipation. The primary care NP notes a heart rate of 92 beats per minute. The NP should:prescribe a TCA. discontinue the antidiarrheal medication. encourage the patient to increase water intake. Correct! lower the dose of the antispasmodic medication. Patients taking antispasmodic medications should be monitored for anticholinergic side effects, such as increased heart rate, dry mouth, difficulty urinating, and constipation. The NP should lower the dose if needed. TCAs are used to treat pain long-term. Because the antidiarrheal medication is used as needed, there is no reason to discontinue it. Increasing water intake may improve symptoms associated with side effects but would not treat the underlying cause of these symptoms. Question 13 2 / 2 pts A patient with erosive esophagitis is taking lansoprazole (Prevacid). The primary care NP performs a medication history and learns that the patient also takes digoxin. The NP should recommend: decreasing the dose of digoxin. Correct!obtaining a serum digoxin level. changing the PPI to omeprazole. increasing the dose of lansoprazole. Because PPIs decrease gastric acid, they may interfere with the absorption of drugs that require absorption in an acid stomach, including digoxin. It may be necessary to increase the dose of digoxin but not before obtaining a serum digoxin level. All PPIs have this effect, so changing to another PPI would not solve the problem. Increasing the dose of lansoprazole would decrease the absorption of digoxin. Question 14 2 / 2 pts A patient in the clinic develops sudden shortness of breath and tachycardia. The primary care NP notes thready pulses, poor peripheral perfusion, and a decreased level of consciousness. The NP activates the emergency medical system and should anticipate that this patient will receive: You Answered intravenousalteplase. low-dose aspirin and warfarin. low-molecular-weight heparin (LMWH).Correct Answer unfractionated heparin (UFH) and warfarin. This patient has unstable pulmonary embolism (PE) and should receive thrombolytic therapy. Intravenous alteplase is the preferred agent. UFH and warfarin are recommended for stable PE. LMWH is beneficial in submassive PE and deep vein thrombosis (DVT) but is controversial for treatment of massive PE. Question 15 2 / 2 pts A patient who has gastroesophageal reflux disease (GERD) undergoes an endoscopy, which shows a hiatal hernia. The patient is mildly obese. The patient asks the primary care nurse practitioner (NP) about treatment options. The NP should tell this patient that: a fundoplication will be necessary to correct the cause of GERD. over-the-counter (OTC) antacids can be effective and should be tried first. elevation of the head of the bed at night can relieve most symptoms. Correct! a combination of lifestyle changes, medications, and surgery may be necessary.People with GERD often have hiatal hernia, but this is not the cause of GERD. The approach to treatment of GERD may include lifestyle changes, medications, and surgery. OTC antacids are sometimes used but are rarely used as first-line treatment. Question 16 2 / 2 pts A 40-year-old patient is in the clinic for a routine physical examination. The patient has a body mass index (BMI) of 26. The patient is active and walks a dog daily. A lipid profile reveals low-density lipoprotein (LDL) of 100 mg/dL, high-density lipoprotein (HDL) of 30 mg/dL, and triglycerides of 250 mg/dL. The primary care nurse practitioner (NP) should: Correct! order a fasting plasma glucose level. consider prescribing metformin (Glucophage). suggest dietary changes and increased exercise. obtain serum insulin and hemoglobin A1c levels. Testing for type 2 diabetes should be considered in all adults with a BMI greater than 25 who have risk factors such as HDL less than 35 mg/dL or triglycerides greater than 250 mg/dL. A fasting plasma glucose level greater than 126 mg/dL indicates diabetes. Metformin is not indicated unless testing is positive. Lifestyle changes may be part of the treatment plan. Serum insulin level is not indicated. Question 17 2 / 2 ptsA primary care NP prescribes a COCP for a woman who is taking them for the first time. After teaching, the woman should correctly state the need for using a backup form of contraception if she: Correct! is having vomiting or diarrhea. delays taking a pill by 5 or 6 hours. takes nonsteroidal antiinflammatory drugs several days in a row. has recurrent headaches or insomnia. Vomiting and diarrhea may cause oral contraceptive failure, so women should be advised to use backup contraception if they experience these. The other conditions do not lead to oral contraceptive failure [Show More]
Last updated: 1 year ago
Preview 1 out of 53 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$12.00
Document information
Connected school, study & course
About the document
Uploaded On
Aug 06, 2021
Number of pages
53
Written in
Additional information
This document has been written for:
Uploaded
Aug 06, 2021
Downloads
0
Views
35


.png)
.png)
.png)
 – Strayer University.png)