*NURSING > STUDY GUIDE > NR 226 Final Exam Study Outline (Download To Score An A) | NEW!!!! (All)
NR 226 Final Exam Study Outline (Download To Score An A) | NEW!!!!
Document Content and Description Below
NR 226 Final Exam Study Outline *****ADPIE for ALL!!**** The Nursing Process o The purpose of the nursing process is to diagnose and treat human responses (e.g., patient symptoms, need for... knowledge) to actual or potential health problems. Use of the process allows nurses to help patients meet agreed-on outcomes for better health. o The nursing process requires a nurse to use the general and specific critical thinking competencies described earlier to focus on a particular patient's unique needs. The format for the nursing process is unique to the discipline of nursing and provides a common language and process for nurses to “think through” patients' clinical problems • 5 Steps of the Nursing Process (ADPIE) o Assessment ▪ Phases of interview/assessment • An interview is an approach for gathering subjective and objective data from a patient through an organized conversation. An initial interview involves collecting a nursing health history and gathering information about a patient's condition • 1. Orientation and Setting an Agenda o Begin an interview by introducing yourself and your position and explaining the purpose of the interview. Explain why you are collecting data and assure patients that all of the information will be confidential. o Your aim is to set an agenda for how you will gather information about a patient's current chief concerns or problems. Remember, the best clinical interview focuses on a patient's goals, preferences, and concerns and not on your agenda. • 2. Working Phase-Collecting Assessment or Nursing Health History o Start an assessment or a nursing health history with open- ended questions that allow patients to describe more clearly their concerns and problems. For example, begin by having a patient explain symptoms or physical concerns and describe what he or she knows about the health problem or ask him or her to describe health care expectations. o Use attentive listening and other therapeutic communication techniques that encourage a patient to tell his or her story. • 3. Terminating an Interview o Termination of an interview requires skill. You summarize your discussion with a patient and check for accuracy of the information collected. Give your patient a clue that the interview is coming to an end. For example, say, “I have just two more questions. We'll be finished in a few more minutes.” o This helps a patient maintain direct attention without being distracted by wondering when the interview will end. ▪ Methods of obtaining data • An assessment is necessary for you to gather information to make accurate judgments about a patient's current condition. Your information comes from: • The patient through interview, observations, and physical examination. • Family members or significant others' reports and response to interviews. • Other members of the health care team. • Medical record information (e.g., patient history, laboratory work, x-ray film results, multidisciplinary consultations). • Scientific and medical literature (evidence about disease conditions, assessment techniques, and standards). ▪ Subjective Data • Subjective data are your patients' verbal descriptions of their health problems. For example, Mr. Lawson's self-report of pain at the area where his incision slightly separated is an example of subjective data. Subjective data include patients' feelings, perceptions, and self-report of symptoms. • Only patients provide subjective data relevant to their health condition. The data often reflect physiological changes, which you further explore through objective review of body systems. ▪ Objective Data • Objective data are observations or measurements of a patient's health status. Inspecting the condition of a surgical incision or wound, describing an observed behavior, and measuring blood pressure are examples of objective data. o Diagnosis • Objective data is measured on the basis of an accepted standard such as the Fahrenheit or Celsius measure on a thermometer, inches or centimeters on a measuring tape, or a rating scale (e.g., pain). • When you collect objective data, apply critical thinking intellectual standards (e.g., clear, precise, and consistent) so you can correctly interpret your findings. ▪ Identify components of the nursing diagnostic statement • The diagnostic reasoning process involves using the assessment data you gather about a patient to logically explain a clinical judgment, in this case a nursing diagnosis. • The diagnostic process flows from the assessment process and includes decision-making steps. These steps include data clustering, identifying patient health problems, and formulating the diagnosis. ▪ Identify assessment findings, goals, interventions, evaluations appropriate to a specific nursing diagnosis. • Be able to recognize the difference between each category. Context clues like “The Patient will…” means it is a goal. o Planning ▪ Components of goal/outcome statement • A patient-centered goal reflects a patient's highest possible level of wellness and independence in function. It is realistic and based on patient needs, abilities, and resources. A patient-centered goal or outcome reflects a patient's specific behavior, not your own goals or interventions. • Goals and expected outcomes direct your nursing care. Once you set a patient-centered goal for a nursing diagnosis, the expected outcomes provide the desired physiological, psychological, social, developmental, or spiritual responses that indicate resolution of the patient's health problems. • Usually you develop several expected outcomes for each nursing diagnosis and goal. For a patient to resolve a goal, several measurable outcomes are needed to ensure that the goal is met. In the case of Mr. Lawson's diagnosis of Risk for Infection, Tonya knows that more than one outcome is needed to ensure that the patient is infection free. • The SMART acronym (Specific, Measurable, Attainable, and Realistic, Timely) is a useful approach for writing goals and outcome statements more effectively. o Implementation ▪ Independent nursing interventions • Nurse-initiated interventions are the independent nursing interventions or actions that a nurse initiates without supervision or direction from others. • Examples include positioning patients to prevent pressure ulcer formation, instructing patients in side effects of medications, or providing skin care to an ostomy site. Independent nursing interventions do not require an order from another health care provider. ▪ Dependent nursing interventions • Health care provider–initiated interventions are dependent nursing interventions, or actions that require an order from a health care provider. The interventions are based on the health care provider's response to treating or managing a medical diagnosis. • Advanced practice nurses who work under collaborative agreements with physicians or who are licensed independently by state practice acts are also able to write dependent interventions. • As a nurse you intervene by carrying out the health care provider's written and/or verbal orders. Administering a medication, implementing an invasive procedure (e.g., inserting a Foley catheter, starting an intravenous [IV] infusion) and preparing a patient for diagnostic tests are examples of health care provider- initiated interventions. ▪ Direct care activities • Direct care interventions are treatments performed through interactions with patients. For example, a patient receives direct intervention in the form of medication administration, insertion of a urinary catheter, discharge instruction, or counseling during a time of grief. ▪ Indirect care activities • Indirect care interventions are treatments performed away from a patient but on behalf of the patient or group of patients (e.g., managing a patient's environment [e.g., safety and infection control]), documentation, and interdisciplinary collaboration. o Evaluation ▪ Elements of the evaluation process • Evaluation, the final step of the nursing process, is crucial to determine whether, after application of the first four steps of the nursing process, a patient's condition or well-being improves. • You conduct evaluative measures to determine if your patients met expected outcomes, not if nursing interventions were completed. The expected outcomes established during planning are the standards against which you judge whether goals have been met and if care is successful. • You examine the results of care by using evaluative measures, which are assessment skills and techniques (e.g., observations, physiological measurements, use of measurement scales, patient interview). • In fact, evaluative measures are the same as assessment measures, but you perform them at the point of care when you make decisions about a patient's status and progress. The intent of assessment is to identify which, if any, problems exist. The intent of evaluation is to determine if the known problems have remained the same, improved, worsened, or otherwise changed. • Professional Practice o Delegation ▪ 5 rights 1. Right task – ones that are repetitive and require little supervision, relatively noninvasive, results that are predictable, minimal risk (ex: specimen collection, ambulating stable pts, prepping room for pt. admit) 2. Right Circumstances – patient setting, available resources 3. Right person – make sure that the tasks match the person’s level of expertise 4. Right Direction / Communication – give clear, concise descriptions of the task including its objective, limits, and expectations 5. Right Supervision/ Evaluation – provide appropriate monitoring, evaluation, intervention when needed, and feedback ▪ supervision o Prioritization of care – organization of vison of desired outcomes for a patient\ ▪ High Priority – immediate threat to patient’s survival or safety (ex: obstructed airway, loss of consciousness, psychological episode of anxiety attack, ABC’s) ▪ Intermediate Priority – non-emergency, nonlife threatening actual or potential needs that a pt. and family members are experiencing (ex: teaching needs of pt. related to a new drug, taking measures to decrease post-operative complications) ▪ Low Priority – actual or potential problems that are not directly related to a patient’s illness or disease. (ex: developmental needs or long-term health care needs such as self-care at home) o Nursing care delivery model 1. Traditional Models ▪ Team nursing – developed in response to severe nursing shortage ▪ Primary nursing – developed to place RNs at the bedside and improve the accountability of nursing for patient outcomes and the professional relationships among staff members ▪ Patient and family centered – mutual partnerships among the patient, family, and health care team are formed to plan, implement and evaluate the nursing and health care delivered • Four core concepts 1. Respect and dignity – ensuring that care provided is given based on a pt.’s and family’s knowledge, values, beliefs, and cultural backgrounds 2. Information sharing – health care providers communicate and share information, so patients and families receive timely, complete, and accurate information to effectively participate in care and decision making 3. Participation – pts and families are encouraged and supported in participating in care and decision making 4. Collaboration – demonstrated by health care leaders collaborating with patients and families in policy and program development, implementation, and evaluation and patients who are fully engaged in their health care o Management of patient care ▪ Organization – combine and utilize effective use of time (doing the right things) and efficient use of time (doing things right), approaches any procedure or situation as well prepared as possible ▪ Time management – involve learning how, where, and when to use your time; remain goal oriented and use it wisely; use pt. goals to identify priorities (ex: priority to do list) ▪ Utilization of resources – resources include all members of the health care team, pt. care occurs more smoothly when staff members work together; more help can ensure a more comfortable and safer procedure/environment for the pt. ▪ Evaluation – ongoing task; compares actual patient outcomes with expected outcomes; reveals the need to continue current therapies for a longer period, revise approaches to care, or introduce new therapies o Leadership ▪ Characteristics of effective leader • Effective communicator • Consistent in managing conflict • Knowledgeable and competent in all aspects of delivery of care • Role model for staff • Uses participatory approach in decision making • Shows appreciate for a job well done • Shows appreciation for a job well done • Delegates work appropriately • Sets objectives and guides staff • Displays caring, understanding, and empathy for others • Motivates and empowers others • Is proactive and flexible • Focuses on team development • Ethics o Code of Ethics a set of guiding principles that all members of a profession accept. It is a collective statement about the group's expectations and standards of behavior. The American Nurses Association (ANA) established the first code of nursing ethics decades ago. The ANA reviews and revises the code periodically; but principles of responsibility, accountability, advocacy, and confidentiality remain constant. o Understand, give examples of terms Advocacy Advocacy refers to the support of a particular cause. As a nurse you advocate for the health, safety, and rights of patients, including their right to privacy and their right to refuse treatment. Responsibility The word responsibility refers to a willingness to respect one's professional obligations and to follow through. An example is following an agency's policies and procedures. Accountability Accountability refers to the ability to answer for one's actions. You ensure that your professional actions are explainable to your patients and your employer. Confidentiality Federal legislation known as the Health Insurance Portability and Accountability Act of 1996 (HIPAA) mandates confidentiality about and protection of patients' personal health information. The legislation defines the rights and privileges of patients for protection of privacy. Social Networking The online presence of social networks presents ethical challenges for nurses. On one hand social networks can be a supportive source of information about patient care or professional nursing activities. Social media can provide you emotional support when you encounter hardships at work with colleagues or patients. On the other hand, the risk to patient privacy is great. Patients need to be confident that their most personal information and their basic dignity will be protected by the nurse. Issues – quality of life, genetic screening, futile care Quality of life represents something deeply personal. Health care researchers use quality-of-life measures to define scientifically the value and benefits of medical interventions. Quality-of-life measures may take into account the age of a patient, the patient's ability to live independently, his or her ability to contribute to society in a gainful way, and other nuanced measures of quality. Futile Care Difficult emotional and spiritual challenges resulting in moral distress can characterize the management of care at the end of life. The term futile refers to something that is hopeless or serves no useful purpose. In health care discussions the term refers to interventions unlikely to produce benefit for a patient. The concept is slippery when applied to clinical situations. If a patient is dying of a condition with little or no hope of recovery, almost any intervention beyond symptom management and comfort measures is seen as futile. In this situation an agreement to label an intervention as futile can help providers, families, and patients turn to palliative care measures as a more constructive approach to the situation. o Guidelines for ethical decision making Deontology proposes a system of ethics that is perhaps most familiar to health care practitioners. Deontology defines actions as right or wrong on the basis of their “right-making characteristics” such as fidelity to promises, truthfulness, and justice. It specifically does not look at consequences of actions to determine right or wrong. Instead, deontology examines a situation for the existence of essential right or wrong. Deontology depends on a mutual understanding of justice, autonomy, and goodness. But it still leaves room for confusion to surface. • Legal issues in nursing o Nurse Practice Acts describe and define the legal boundaries of nursing practice within each state. The Nurse Practice Act of each state defines the scope of nursing practice and expanded nursing roles, sets education requirements for nurses, and distinguishes between nursing and medical practice. o Regulatory law, or administrative law, reflects decisions made by administrative bodies such as State Boards of Nursing when rules and regulations are passed. ▪ An example of a regulatory law is the requirement to report incompetent or unethical nursing conduct to the State 303Board of Nursing. HIPAA o Standards of care are the legal requirements for nursing practice that describe minimum acceptable nursing care. Standards reflect the knowledge and skill ordinarily possessed and used by nurses actively practicing in the profession. o The American Nurses Association (ANA) develops standards for nursing practice, policy statements, and similar resolutions. These standards outline the scope, function, and role of the nurse in practice. o Nursing standards of care are described in the Nurse Practice Act of every state, in the federal and state laws regulating hospitals and other health care agencies, by professional and specialty nursing organizations, and by the policies and procedures established by the health care agency where nurses work o Errors ▪ The best way for nurses to avoid malpractice is to follow standards of care, give competent care, and communicate with other health care providers. You also avoid malpractice by developing a caring rapport with the patient and documenting assessments, interventions, and evaluations fully. ▪ Nurses need to know the current nursing literature in their areas of practice. Know and follow the policies and procedures of the agency where you work. Be sensitive to common sources of patient injury such as falls and medication errors. ▪ Finally, communicate with the patient, explain all tests and treatments, document that you provided specific explanations to him or her, and listen to his or her concerns about treatments. You are accountable for timely reporting of any significant changes in the patient's condition to the health care provider and documenting these changes in the medical record. o ADA ▪ The Americans with Disabilities Act (ADA) of 1990 and as amended in 2008 is a civil rights statute that protects the rights of people with physical or mental disabilities. ▪ The ADA prohibits discrimination and ensures equal opportunities for people with disabilities in employment, state and local government services, public accommodations, commercial facilities, and transportation. ▪ As defined by the statute and the U.S. Supreme Court, a disability is a mental or physical condition that substantially limits a major life activity, including seeing, hearing, speaking, walking, breathing, performing manual tasks, learning, caring for oneself, and/or working. ▪ Under the ADA employers are required to construe the definition of a person's disability to the maximum intent allowed under the ADA. o EMTALA (Emergency Medical Treatment and Active Labor Act) ▪ This act provides that, when a patient comes to the emergency department or the hospital, an appropriate medical screening occurs within the capacity of the hospital. ▪ If an emergency condition exists, staff must evaluate the patient and may not discharge or transfer him or her until the patient's condition stabilizes. ▪ Exceptions to this provision include if a patient requests transfer or discharge in writing after receiving information about the benefits and risks or if a health care provider certifies that the benefits of transfer outweigh the risks. o Living will ▪ Living wills represent written documents that direct treatment in accordance with a patient's wishes in the event of a terminal illness or condition. ▪ With this document a patient is able to declare which medical procedures he or she wants or does not want when terminally ill or in a persistent vegetative state. ▪ Living wills are often difficult to interpret and not clinically specific in unforeseen circumstances. o Durable power of attorney ▪ A health care proxy or durable power of attorney for health care (DPAHC) is a legal document that designates a person or people of one's choosing to make health care decisions when a patient is no longer able to make decisions on his or her own behalf. ▪ This agent makes health care treatment decisions on the basis of the patient's wishes o Health care surrogate ▪ In some instances obtaining informed consent is difficult. For example, if a patient is unconscious, you must obtain consent from a person legally authorized to give it on the patient's behalf. Sometimes a patient has legally designated surrogate decision makers through special power of attorney documents or court guardianship procedures. ▪ In emergencies, if it is impossible to obtain consent from the patient or an authorized person, a health care provider may perform a procedure required to benefit the patient or save a life without liability for failure to obtain consent. o Organ donation ▪ An individual who is at least 18 years of age has the right to make an organ donation (defined as a “donation of all or part of a human body to take effect upon or after death”). ▪ Donors need to make the gift in writing with their signature. In many states adults sign the back of their driver's license, indicating consent to organ donation. o Minor child ▪ Ordinarily minors may not consent to medical treatment without a parent. However, emancipated minors may consent to medical treatment without a parent. ▪ Parents are usually the legal guardians of pediatric patients; therefore they typically are the people who sign consent forms for treatment. ▪ Occasionally a parent or guardian refuses treatment for a child. In these cases the court sometimes intervenes on the child's behalf. Courts generally consider the child's ultimate safety and well-being as the most important factors. o Consent ▪ A patient's signed consent form is necessary for admission to a health care agency, invasive procedures such as intravenous central line insertion, surgery, some treatment programs such as chemotherapy, and participation in research studies. ▪ A patient signs a general consent form for treatment when admitted to a health care agency or other health care facility. A patient or the patient's representative needs to sign separate special consent or treatment forms before the performance of a specialized procedure. State laws designate individuals who are legally able to give consent to medical treatment ▪ Informed consent is a patient's agreement to have a medical procedure after receiving full disclosure of risks, benefits, alternatives, and consequences of refusal. ▪ The person responsible for performing the procedure is responsible for obtaining the informed consent. o Use of restraints ▪ A physical restraint is any manual method, physical or mechanical device, or material or equipment that immobilizes or reduces the ability of a patient to move freely. ▪ The Omnibus Reconciliation Act (1987) includes chemical restraint as a form of restraint. ▪ Restraints can be used (1) only to ensure the physical safety of the patient or other patients, (2) when less restrictive interventions are not successful, and (3) only on the written order of a health care provider ▪ The use of restraints has been associated with serious complications and even death. ▪ You need to know when and how to use and safely apply restraints. • Older Adult o Expected physical changes ▪ With aging, muscle mass decreases, body fat increases, and percentage of body water decreases. This increases the concentration of water-soluble drugs such as morphine given in normal doses. The volume of distribution for fat-soluble drugs such as fentanyl increases. ▪ Older adults frequently eat poorly, resulting in low serum albumin levels. Many drugs are highly protein bound. In the presence of low serum albumin, more free drug (active form) is available, thus increasing the risk for side and/or toxic effects. ▪ A decline of liver and renal function naturally occurs with aging. This results in reduced metabolism and excretion of drugs. Thus older adults often experience a greater peak effect and longer duration of analgesics. ▪ Age-related changes in the skin such as thinning and loss of elasticity affect the absorption rate of topical analgesics. ▪ Aging does not automatically lead to disability and dependence. Most older people remain functionally independent despite the increasing prevalence of chronic disease. Nursing assessment provides valuable clues to the effects of a disease or illness on a patient's functional status. Chronic conditions add to the complexity of assessment and care of the older adult. ▪ Most older people have at least one chronic condition, and many have multiple conditions. The physical and psychosocial aspects of aging are closely related. A reduced ability to respond to stress, the experience of multiple losses, and the physical changes associated with normal aging combine to place people at high risk for illness and functional deterioration. ▪ Although the interaction of these physical and psychosocial factors is often serious, do not assume that all older adults have signs, symptoms, or behaviors representing disease and decline or that these are the only factors you need to assess. You also need to identify an older adult's strengths and abilities during the assessment and encourage independence as an integral part of your plan of care o Expected Cognitive Changes ▪ A common misconception about aging is that cognitive impairments are widespread among older adults. Because of this misconception, older adults often fear that they are, or soon will be, cognitively impaired. ▪ Younger adults often assume that older adults will become confused and no longer able to handle their affairs. Forgetfulness as an expected consequence of aging is a myth. Some structural and physiological changes within the brain are associated with cognitive impairment. Reduction in the number of brain cells, deposition of lipofuscin and amyloid in cells, and changes in neurotransmitter levels occur in older adults both with and without cognitive impairment. ▪ Symptoms of cognitive impairment such as disorientation, loss of language skills, loss of the ability to calculate, and poor judgment are not normal aging changes and require you to further assess patients for underlying causes. There are standard assessment forms for determining a patient's mental status, including the Mini-Mental State Exam-2 (MMSE- 2), the Mini-Cog, and the Clock Drawing Test ▪ The three common conditions affecting cognition are delirium, dementia, and depression. o Goals for care of cognitively impaired older adults ▪ Provide a comprehensive assessment to differentiate between a progressive or reversible etiology. ▪ Institute medical measures to correct underlying physiological alterations (e.g., infection, electrolyte imbalances, pain). ▪ Maximize safe function. Keep a routine, encourage activity and mobility, limit choices (e.g., clothes for dressing, what to eat), allow for rest. ▪ Provide unconditional positive regard. Be respectful and provide positive nonverbal communication. ▪ Use behaviors to gauge activity and stimulation. Watch for nonverbal signs of anxiety. ▪ Teach caregivers to listen to the behaviors that show stress (e.g., verbalizations such as repetition). ▪ Make sure that the environment is safe for mobility and promote way- finding with pictures or cues. Try to identify patients who wander and remove the cause (e.g., pain, thirst, unfamiliar surroundings, and new noises). ▪ Promote social interaction on the basis of abilities. ▪ Compensate for sensory deficits (e.g., hearing aids, glasses, dentures). ▪ Encourage fluid intake (make sure that fluids are accessible) and avoid long periods of giving nothing orally. ▪ Be vigilant for drug reactions or interactions; consider onset of new symptoms as an adverse reaction. ▪ Activate bed and chair alarms. ▪ Provide ongoing assistance to family caregivers; educate them in nursing care techniques and inform them about community resources. o Nursing Process ▪ Nursing assessment takes into account three key points to ensure an age- specific approach: (1) the interrelation between physical and psychosocial aspects of aging, (2) the effects of disease and disability on functional status and, (3) tailoring the nursing assessment to an older person. A comprehensive assessment of an older adult takes more time than the assessment of a younger adult because of the longer life and medical history and the potential complexity of the history. ▪ During the physical examination allow rest periods as needed or conduct the assessment in several sessions if a patient has reduced energy or limited endurance. Remember to review both prescribed and over-the- counter medications carefully with each patient. ▪ A patient's sensory changes also affect data gathering. Your choice of communication techniques depends on an older adult's visual or hearing impairments. If an older adult is unable to understand your visual or auditory cues, your assessment data will likely be inaccurate or misleading, leading you to incorrectly conclude that the older adult is confused. When a person has a hearing impairment, speak directly to the patient in clear, low-pitched tones and move to a quiet area to reduce background noise. ▪ When caring for people with visual impairments, sit or stand at eye level and face them. Always encourage the use of assistive devices such as glasses and hearing aids. ▪ Memory deficits, if present, affect the accuracy and completeness of your assessment. Information contributed by a family member or other caregiver is sometimes necessary to supplement an older adult's recollection of past medical events and information about current self-care habits, medication adherence, and history of allergies and immunizations. ▪ Use tact when involving another person in the assessment interview. The additional person supplements information with the consent of the older adult, but the older adult remains the primary source of the interview. ▪ During all aspects of an assessment, you are responsible for providing culturally competent care. Your ability to recognize and process your own Pain biases related to ageism, social norms, and racism affects your ability to provide culturally competent care. • Assessment of pain: o Patient’s expression of pain o Characteristics of pain o Onset and duration o Location o Intensity o Quality o Pattern o Relief measures o Contributing symptoms o Effects of pain on the patient • Factors affecting/influencing pain perception o Physiological ▪ Age, fatigue, genes, neurological function ▪ Fatigue increases the perception of pain and can cause problems with sleep and rest. o Social ▪ Attention, previous experiences, family and support groups, spiritual ▪ Spirituality includes active searching for meaning in situations, with questions such as “Why am I suffering?” o Psychological ▪ Anxiety ▪ Coping style o Pain tolerance ▪ The level of pain a person is willing to accept o Cultural ▪ Meaning of pain ▪ Ethnicity • Pain scales Wong-Baker FACES Scale • Cultural considerations o The meaning that a person associates with pain affects the experience of pain and how one adapts to it. This is often closely associated with a person's cultural background, including age, education, race, and familial factors. Cultural beliefs and values affect how individuals cope with pain. They learn what is expected and accepted by their culture, including how to react to pain. Health care providers often mistakenly assume that everyone responds to pain in the same way. Different meanings and attitudes are associated with pain across various cultural groups. o Culture affects pain expression. Some people believe that it is natural to be demonstrative about pain. Others tend to be more introverted. When a person moves to another country, it is important to know to what extent the individual has assimilated into his or her new home. For example, if several generations of a Hispanic patient's family have lived in the United States, the influence of the Spanish culture may be limited, whereas newly immigrated patients still often embrace their cultural norms. o As a nurse explore the impact of cultural differences on a patient's pain experience and make adjustments to the plan of care. Ask if the patient has had any previous bad experiences with pain management. Work with a patient and family to learn their cultural beliefs, values, and preferences to adequately assess and manage pain. Pain is a biopsychosocial phenomenon. Culture shapes the experience of pain, including its expression and a patient's behaviors, or coping responses. o For example, an individual from a higher socioeconomic group has more resources for managing pain and is more likely to adapt behaviors that will lessen pain. One research study showed that people in the lowest as compared to the highest socioeconomic class were 2 to 3 times more likely to feel disabled through pain. Culture also affects a person's choice of lay remedies, help-seeking activities, and receptivity to medical treatment. Some health care providers undertreat pain because they do not understand the cultural effects on the perception of pain intensity. • Implications for Patient-Centered Care o Use culturally appropriate assessment tools such as tools written in the patient's native language to assess pain. o Assess the patient's health literacy level because this affects your ability to provide appropriate education about pain management and therapies. o Recognize variations in subjective responses to pain. Some patients are stoic and less expressive, whereas others are emotive and more likely to verbalize pain. o Be sensitive to variations in communication styles. Some cultures believe that nonverbal expression of pain is sufficient to describe the pain experience, whereas others assume that, if pain medication is appropriate, the nurse will bring it; thus asking is inappropriate. o Understand that expression of pain is unacceptable within certain cultures. Some patients believe that asking for help indicates a lack of respect, whereas others believe acknowledging pain is a sign of weakness. o The meaning of pain varies among cultures. Pain is personal and related to religious beliefs. Some cultures consider suffering a part of life to be endured to enter heaven. o Use knowledge of biological variations of pain. Significant differences in drug metabolism, dosing requirements, therapeutic response, and adverse effects occur in cultural groups. A wide range of responses is also possible within this group. Therefore assess each patient's response to pain medication carefully. o Develop a personal awareness of your own values and beliefs that affect your responses to patients' reports of pain. • Tolerance & Addiction o Drug tolerance: A state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more effects of the drug over time o Addiction: A primary, chronic, neurobiological disease with genetic, psychosocial, and environmental factors influencing its development and manifestations • Goals for pain management o Determine with the patient what the pain has prevented the patient from doing. o Then agree on an acceptable level of pain that allows return of function. o For example, for the goal, “The patient will achieve a satisfactory level of pain relief within 24 hours,” possible outcomes are as follows: o Reports that pain is a 3 or less on a scale of 0 to 10 o Identifies factors that intensify pain o Uses pain relief measures safely o Level of discomfort does not interfere with activities of daily living (ADLs). • Patient teaching regarding pain management o Implementation ▪ Pain therapy requires an individualized approach, perhaps more so than any other patient problem. The nurse, patient, and frequently the family are partners in pain management. You are responsible for administering and monitoring therapies ordered by health care providers for pain relief and independently providing measures that complement those prescribed. Generally try the least invasive or safest therapy first along with previously used successful patient remedies. If you question a medical therapy, consult with the health care provider. ▪ Regardless of the therapies chosen, your ability to show compassionate care toward patients has the potential for maximizing their pain control. You can help the patient minimize pain through caring behaviors such as listening, offering a gentle touch, and responding promptly to a pain request. o Health Promotion ▪ When providing pain-relief measures, choose therapies suited to a patient's unique pain experience. Apply guidelines for individualizing pain therapy, including the following: ▪ Use different types of pain-relief measures. ▪ Use measures that patient believes are effective. ▪ Keep an open mind about ways to relieve pain. ▪ Keep trying. When efforts at pain relief fail, do not abandon the patient but reassess the situation. o Maintaining Wellness ▪ Patients are better prepared to handle almost any situation when they understand it. The experience of pain and related therapies are no exception. However, patients with moderate-to-severe pain are not always able to participate in decision making until the pain is controlled at an acceptable level. Once you accomplish this, you can begin teaching. ▪ Health literacy significantly affects a patient's pain experience and understanding of pain-management strategies. Low health literacy poses significant barriers to optimal pain management. In a study of patients with chronic pain, patients with low health literacy were found to have low overall pain medication knowledge and did not know where to find health care professionals to help them with their pain. The patients in the study also lacked knowledge about nonpharmacological approaches to pain management and did not know which nonprescription pain medications could provide pain relief. ▪ Research conducted with patients with chronic back pain and other patient groups provides evidence for why educational materials and approaches must be adapted so they are suited for low–health literacy patients. In addition, combat any cultural norms that may stop patients from talking about pain at all. Stoicism not only potentially obscures dangerous signs about which you should know, but it also denies people the opportunity to use labels as a tool to cope with pain. Help patients who don't have the words to describe their pain find them. Because pain affects physical and mental functioning, holistic health approaches are important interventions for maintaining wellness. Holistic health is an ongoing state of wellness that involves taking care of the whole person: body, mind, spirit, and emotions. To achieve optimal health and well-being, it is necessary to have balance of all of the interdependent elements of the whole person. ▪ Patients actively participate in their own well-being whenever possible. Common holistic health approaches include wellness education, regular exercise, and rest, attention to good hygiene practices and nutrition, and management of interpersonal relationships. When a person develops pain, you can offer nonpharmacological and pharmacological strategies. Several nonpharmacological interventions are nurse initiated. • Non-pharmacologic interventions o Nonpharmacological pain relief interventions ▪ Relaxation, guided imagery ▪ Biofeedback ▪ Distraction, music ▪ Cutaneous stimulation • Massage, transcutaneous electrical nerve stimulation (TENS), heat, cold, acupressure ▪ Herbal Remedies ▪ Reducing pain perception • Evaluation of effectiveness of interventions o Beh aviora l I nd icato rs of Effects of Pain ▪ Vocalizations • Moaning • Crying • Gasping • Grunting ▪ Facial Expressions • Grimace • Clenched teeth • Wrinkled forehead • Tightly closed or widely opened eyes or mouth • Lip biting ▪ Body Movement • Restlessness • Immobilization • Muscle tension • Increased hand and finger movements • Pacing activities • Rhythmic or rubbing motions • Protective movement of body parts • Grabbing or holding a body part ▪ Social Interaction • Avoidance of conversation • Focus only on activities for pain relief • Avoidance of social contacts • Reduced attention span • Reduced interaction with environment • Evaluation of pain is one of many nursing responsibilities that require effective critical thinking. • The patient’s response to pain may not be obvious. • Evaluating the appropriateness of pain medication will require nurses to evaluate patients’ responses after administration. • Patients help decide the best times to attempt pain treatments. Ask patients about tolerance to therapy and the overall amount of relief obtained. If patients state that an intervention is not helpful or even aggravates the discomfort, stop it immediately and seek an alternative. • Pain evaluation includes measuring the changing character of pain, the patient’s response to interventions, and the patient’s perceptions of effectiveness of a therapy Grief - Grief – a normal but bewildering cluster of ordinary human emotions arising in response to a significant loss, intensified and complicated by the relationship to the person or the object loss 1. Normal Grief – common and universal reaction characterized by complex, emotional, cognitive, social, physical, behavioral, and spiritual responses to loss and death o Normal feelings: disbelief, yearning, anger, and depression o Coping mechanisms: hardiness, resilience, personal sense of control, ability to make sense of and identity positive aspects after a loss 2. Anticipatory grief – occurs before the actual loss or death occurs, especially in situations prolonged or predicted loss o Gives people time to prepare or complete tasks related to impending death 3. Disenfranchised Grief – when their relationship to the deceased person is not socially sanctioned, cannot be shared openly, or seems of lesser significance o Ex: former spouse, married love, incarcerated person, terminated pregnancy o Ambiguous loss – type of disenfranchised grief, can occur when the lost person is physically present but not psychologically available ▪ Ex: dementia, brain injury 4. Complicated Grief – person has a prolonged or significantly difficult time moving forward after a loss o Person experiences chronic and disruptive yearning for the deceased, has trouble accepting the loss, feels excessively bitter, emotionally numb, or anxious about the future o Occurs more often in those who had a conflicted relationship with the deceased, multiple stresses or losses, mental health issues, or lack of social support o Chronic grief – normal grief response for prolonged periods of time (Inc. years to decades) o Exaggerated Grief – exhibits self-destructive or maladaptive behaviors, obsession, or psychotic disorders (suicide risk is high for these people) o Delayed Grief – unusually delayed or postponed because the loss is so overwhelming that the person must avoid the full realization of the loss (triggered by second loss not as significant) o Masked Grief – persons behavior interferes with normal functioning and person is unaware that the disruptive behavior is a result of the loss - Mourning – the outward social expression of grief and the behavior associated with loss - Types of loss o Loss of possessions/objects: (theft, deterioration, misplacement, destruction) extent of grieving depends on value of object, sentiment attached, and its usefulness o Loss of known environment: (leaving home, hospitalization, new job, leaving rehab unit) occurs through maturational or situation events or by injury/illness ▪ Can threaten self-esteem, hopefulness, or belonging o Loss of significant other (divorce, loss of friend, trusted caregiver, pet) can hurt self-esteem needs o Loss of an aspect of life (body part, job, psychological, physiological function) result in loss of a valued aspect of self, altering personal identity and self-concept o Loss of life (death of family member, friend, co-worker, one’s own death) grieves those left behind, dying people also feel sadness or fear pain, loss of control, and dependency on others Criteria for hospice care, palliative care (pg. 761) • Palliative Care – holistic method to prevent and reduce symptoms promotes quality of life and whole person wellbeing through care of mind, body, and spirit; focuses on the prevention, relief, and reduction, or soothing of symptoms of disease or disorders throughout the entire course of an illness o Primary goal – to help patients and families achieve the best possible quality of life o Especially important advanced or chronic illness but can be for any age, diagnosis, time, or setting o Appropriate for patients still receiving aggressive treatment with hope of achieving a cure and for patients who have forgone any life-extending treatment o WHO summarization: ▪ Affirms life and regards dying as normal process ▪ Neither hastens or postpones death ▪ Integrates psychological and spiritual aspects of patient care ▪ Offers a support system to help patients live as actively as possible until death ▪ Enhances the quality of life ▪ Uses a team approach to meet the needs of patients and families o Ex: yoga, acupuncture, massage, aromatherapies, music therapy, mindfulness- based stress- reduction techniques • Hospice Care – for the care of terminally ill patients and their families at the end of life; gives priority to managing a patient’s pain and other symptoms, comfort, quality of life, and attention to physical, psychological, social, and spiritual needs o Eligibility: ▪ Approximately 6 months left to live ▪ Family caregiver to provide care when the patient sis no longer able to function alone ▪ Hospice nurses use therapeutic communication, offer psychosocial care, expert symptoms management, promote patient dignity and self-esteem, maintain a comfortable and peaceful environment, provide spiritual comfort and hope, protect against abandonment or isolation, ethical decision making, facilitate mourning o Available in home, hospital, extended care, and nursing home settings o Built on core beliefs and services: ▪ Pt and family are the unit of care ▪ Coordinated home care with access to inpatient and nursing home beds when needed ▪ Symptom management ▪ Physician-directed services ▪ Provision of an interdisciplinary care team ▪ Medical and nursing services available always ▪ Bereavement follow-up after a pts death ▪ Se for trained volunteers for visitation and support Post mortem care, when autopsy required (pg. 765) • Policies and procedures for after death 1. Requesting organ or tissue donation, performing autopsy, verifying and documenting the occurrence of death, providing safe and appropriate postmortem care • Organ donation o Transplant coordinator or social worker request for organ donation upon death o Life support pts pronounced brain dead can stay on life support only to preserve the vital organs o The family gives or denies consent at the time of death if the deceased has not given previous instruction • Autopsy o Family members give consent o Most cases the coroner determines the need for an autopsy; however, the law sometimes require an autopsy to be performed if death is the result of foul play, homicide, suicide, or accidental causes such as MVA’s, falls, ingestion of drugs, death within 24 hours of hospital admission o Typically, physician asks for family’s permission Cultural considerations for death, dying, post-mortem care (pg.767, 755) • African-American: depends on country of origin and degree of American acculturation, o Presence of extended family groups, including church family are common at time of death o Mourning period relatively short o Memorial service and public viewing prior to burial o Organ donation and autopsy allowed • Chinese: death is regarded as a negative life event and there is no concept of an afterlife o Dead are treated with the same respect as the living and may be buried with food and other artifacts o Members of extended family usually stay with deceased up to 8 hours after death o Oldest son or daughter bathes the body under direction from elder o Organ donation and autopsy are uncommon • Hispanic/Latino: honoring family values and roles is essential o Often use special objects such as amulets or rosary beads, alternative healing practices (folk medicine), and prayer o Grief is expressed openly o Religious and spiritual (catholic) are essential at end of life (death is believed to be the will of God) • Native American: o Traditional Navajos – do not touch the body after death ▪ Care includes cleansing the body, painting the deceased’s face, dressing in clothing, and attaching an eagle feather to symbolize a return home ▪ Dead are buried on the deceased’s homeland • Islamic: body is washed, wrapped, cried over, prayed for, and buried as soon as possible after death o Eyes and mouth are closed, face turned toward Mecca o Muslims of the same gender must prepare the body o Bodies are buried, not cremated o Not likely to agree to autopsy (Islamic people believe in quick burials) o Believed that the soul stays with the body until buried o Organ donation is permissible by some Quran interpretations • Buddhist: believe in afterlife in which human’s manifest in different forms o death is preferred at home, and pts state at TOD is important o usually minimize emotional expression and maintain a peaceful, compassionate atmosphere o male family members prepare the body o recommend not touching the body so deceased has a smoother transition to afterlife • Hindu: o Body is placed on the floor with the head facing north o People of the same gender handle the body after death o No general prohibitions against autopsy o Bodies are cremated after death to purify by fire • Jewish: o If Orthodox Judaism determine if members from the Jewish burial society are coming before preparing the body o Family member often stays with the body until burial (usually occurs within 24 hours of death – but not on the Sabbath) some but not all forms of Judaism avoid cremation, autopsy, and embalming Kubler-Ross stages of dying (DABDA pg. 753) • Denial – person cannot accept the fact of the loss; form of psychological protection from a loss that the person cannot yet bear • Anger – person expresses resistance or intense anger at God, other people, or the situation • Bargaining – person cushions and postpones awareness of the loss by trying to prevent it from happening • Depression – the person realizes the full impact of the loss • Acceptance – the person incorporates the loss into life Factors influencing loss and grief (pg.753-756) • Human development: o Toddlers: cannot understand loss or death but often feel anxiety over the loss of objects and separation from parents ▪ Common expressions: changes in eating and sleeping patterns, bowel and bladder disturbances, increased fussiness o School-Aged: understand the concepts of permanence and irreversibility but do not always understand the causes of a loss ▪ Common experiences: some have intense periods of emotional expression and experience changes in eating, sleeping, and level of social engagement o Young Adults: undergo many necessary developmental losses related to their evolving future ▪ Illness or death disrupts the young adult’s future dreams and establishment of an autonomous sense of self o Middle Adults: major life transitions such as caring for aging parents, dealing with changes in marital status, and adapting to new family roles o Older Adults: the aging process leads to necessary and developmental losses ▪ Some experience age discrimination, especially when they become dependent or are near death ▪ Show resilience after a loss because of their prior experiences and developed coping skills • Personal Relationships: the quality and meaning of the lost relationship influence the grief response o Relationships that are very rewarding and well connected tend to cause for difficulty for the survivor o Grief work is hampered by regret and a sense of unfinished business, especially related members that did not have a good relationship • Nature of the loss: will help understand the effect of the loss on the patient’s behavior, health, and well-being o Encouraging patients to share information about the loss will help you better develop appropriate interventions that meet the individualized needs of your patients • Coping Strategies: coping strategies such as talking, journaling, and sharing their emotions with others may be healthy and effective o They may also be unhealthy and ineffective such as increased use of alcohol, drugs, and violence o Nurses provide support by assessing a patient’s coping strategies, educating about new and healthy strategies, and encouraging use of these strategies • Socioeconomic Status: influences a person’s grief response in direct and indirect ways • Culture: patients and families draw on the social and spiritual practices of their culture to find comfort expressions, and meaning in the experience • Spiritual and Religious Beliefs: provide a framework to navigate, understand, and heal from loss, death, and grief o Hope: a multidimensional concept considered to be a component of spirituality, energizes, and provides comfort to individuals experiencing personal challenges ▪ Gives the person the ability to see life as enduring or having meaning or purpose • Nurse’s care for self Communication/care of patient and significant others (761-763) • Provide psychosocial care: patients often experience anxiety, depression, powerlessness, uncertainty, and isolation o Can feel anguish from unknown surroundings, treatment options, health status, and dying process o Worry or fear is also common in pts and often heightens their perception of discomfort and suffering o Can be alleviated by providing information and benefits/burdens of treatment • Promote dignity and self-esteem: includes a person’s positive self-regard, the ability to find meaning in life and feel valued by others, and treatment of caregivers o Nurses promote by respecting him/her person, attending to their physical appearance, allow them to make decisions, keep pt. and family informed • Maintain a comfortable and peaceful environment: comfortable, clean, pleasant environment helps patients relax, promotes good sleep patterns, and minimizes symptom severity o Consider non-pharmacological interventions (allows family members to be more involved) • Promote spiritual comfort and hope: helping pts make connections to their spiritual practice or cultural community can be useful interventions to allow patients assurance that some aspect of their lies will transcend death o Nursing interventions: be present and provide whole person care o Pts perceive the love of family and friends, faith, goal setting, positive relationships with professional caregivers, humor, and uplifting memories as hope promoting • Protect against abandonment and isolation: many pts fears dying alone, and feel more hopeful when others are near to help them o Nurses need to offer reassurance Nursing diagnoses related to grief/death & dying (pg. 757) • Compromised family coping • Death anxiety • Grieving • Complicated grieving • Risk or complicated grieving • Hopelessness • Pain (acute or chronic) • Spiritual distress Steps for Care of the Body after Death (Box 37-11) • 1. Confirm that the health care provider certified the death and documented the time of death and actions taken. • 2. Determine if the health care provider requested an autopsy. An autopsy is required for deaths that occur under certain circumstances. • 3. Validate the status of request for organ or tissue donation. Given the complex and sensitive nature of such requests, only specially trained personnel make the requests. Maintain sensitivity to personal, religious, and cultural beliefs in this process. • 4. Identify the patient using two identifiers (e.g., name and birthday or name and medical record number according to agency policy). • 5. Provide sensitive and dignified nursing care to the patient and family. o a. Elevate the head of the bed as soon as possible after death to prevent discoloration of the face. o b. Collect ordered specimens. o c. Ask if the family wishes to participate in preparation of the body. Offer to make arrangements for supportive company for the family (patient/family religious leader, spiritual care personnel, or bereavement specialist) during body preparation. o d. Ask about family requests for body preparation such as wearing special clothing or religious artifacts. Be aware that personal, religious, or cultural practices determine whether or not to shave male facial hair. Get permission before shaving a beard. o e. Remove all equipment, tubes, and indwelling lines. Note that autopsy or organ donation often poses exceptions to removal; thus consult agency policy in these situations. o f. Cleanse the body thoroughly, maintaining safety standards for body fluids and contamination when indicated. Comb patient's hair or apply personal hairpieces. o g. Cover body with a clean sheet, place head on a pillow, and leave arms outside covers if possible. Close eyes by gently holding them shut; leave dentures in the mouth to maintain facial shape; cover any signs of body trauma. o h. Prepare and clean the environment, deodorize room if needed, and lower the lights. o i. Offer family members the option to view the body and ask if they want you or other support people to accompany them. Honor and respect individual choices. o j. Encourage grievers to say good-bye in their own way: words, touch, singing, religious rituals, or prayers. o k. Provide privacy and an unrushed atmosphere. Assess family members' need or desire for your presence at this time. If you leave, tell them how to reach you. Sleep o l. Determine which personal belongings stay with the body (e.g., wedding ring or religious symbol) and give other personal items to family members. Document time, date, description of the items taken, and who received them. Save any items that are left behind accidentally and contact family for further instructions. o m. Apply identifying name tags and shroud according to agency policy before transporting the body. Follow safety procedures for body fluid precautions or contamination concerns. o n. Complete documentation in the narrative notes section (see Box 37-9). o o. Maintain privacy and dignity when transporting the body to another location; cover the body or stretcher with a clean sheet. • Stages of sleep – definitions & what happens in each stage o Stage 1: NREM ▪ Stage lasts a few minutes. ▪ It includes lightest level of sleep. ▪ Decreased physiological activity begins with gradual fall in vital signs and metabolism. ▪ Sensory stimuli such as noise easily arouse person. ▪ When awakened, person feels as though daydreaming has occurred. o Stage 2: NREM ▪ Stage lasts 10 to 20 minutes. ▪ It is a period of sound sleep. ▪ Relaxation progresses. ▪ Body functions continue to slow. Arousal remains relatively easy. o Stage 3: NREM ▪ Stage lasts 15 to 30 minutes. ▪ It involves initial stages of deep sleep. ▪ Muscles are completely relaxed. ▪ Vital signs decline but remain regular. ▪ Sleeper is difficult to arouse and rarely moves. o Stage 4: NREM ▪ Stage lasts approximately 15 to 30 minutes. ▪ It is the deepest stage of sleep. ▪ If sleep loss has occurred, sleeper spends considerable part of night in this stage. ▪ Vital signs are significantly lower than during waking hours. ▪ Sleepwalking and enuresis (bed-wetting) sometimes occur. ▪ It is very difficult to arouse sleeper. o REM Sleep ▪ Stage usually begins about 90 minutes after sleep has begun. ▪ Duration increases with each sleep cycle and averages 20 minutes. ▪ Vivid, full-color dreaming occurs; less vivid dreaming occurs in other stages. ▪ Stage is typified by rapidly moving eyes, fluctuating heart and respiratory rates, increased or fluctuating blood pressure, loss of skeletal muscle tone, and increase of gastric secretions. ▪ It is very difficult to arouse sleeper. o NREM, Non rapid eye movement; REM, rapid eye movement. • Functions/ Purposes of sleep o The primary function of sleep is unclear. It contributes to physiological and psychological restoration. NREM sleep contributes to body tissue restoration During NREM sleep biological functions slow. A healthy adult's normal heart rate throughout the day averages 70 to 80 beats/min or less if the individual is in excellent physical condition. However, during sleep the heart rate falls to 60 beats/min or less, which benefits cardiac function. Other biological functions decreased during sleep are respirations, blood pressure, and muscle tone. o The body needs sleep to routinely restore biological processes. During deep slow- wave (NREM stage 4) sleep, the body releases human growth hormone for the repair and renewal of epithelial and specialized cells such as brain cells. Protein synthesis and cell division for renewal of tissues such as the skin, bone marrow, gastric mucosa, or brain occur during rest and sleep. NREM sleep is especially important in children, who experience more stage 4 sleep. o Another theory about the purpose of sleep is that the body conserves energy during sleep. The skeletal muscles relax progressively, and the absence of muscular contraction preserves chemical energy for cellular processes. Lowering of the basal metabolic rate further conserves body energy supply. o REM sleep is necessary for brain tissue restoration and appears to be important for cognitive restoration and memory. It is associated with changes in cerebral blood flow, increased cortical activity, increased oxygen consumption, and epinephrine release. This association helps with memory storage and learning. o The benefits of sleep on behavior often go unnoticed until a person develops a problem resulting from sleep deprivation. A loss of REM sleep leads to feelings of confusion and suspicion. Various body functions (e.g., mood, motor performance, memory, and equilibrium) are altered when prolonged sleep loss occurs. Changes in the natural and cellular immune function also occur with moderate-to-severe sleep deprivation. o The annual direct cost of sleep-related problems in this country is 16 billion dollars. An additional 50 to 100 billion dollars are spent on indirect costs related to accidents, litigation, property damage, hospitalization, and death. • Factors that affect sleep o Drugs and substances ▪ Hypnotics, Antidepressants/stimulants, alcohol, caffeine, diuretics, Beta- Adrenergic Blockers, Benzodiazepines, Nicotine, Opiates, & anticonvulsants. • Most alter/decrease REM sleep, cause insomnia, or daytime sleepiness o Lifestyle ▪ A person’s daily routine influences sleep patterns • Examples: Working a rotating shift, heavy work, late night social activities, changing evening mealtime o Usual Sleep Patterns ▪ Consistently getting low hours of sleep a night o Emotional Stress ▪ Personal problems • Example: elderly worrying about retirement, physical impairment, or death of a loved one. o Environment ▪ Good ventilation, bed quality, w/wo a bed partner, reduce noise, and some need a dark room/lighted room. o Exercise and Fatigue ▪ A person who is moderately fatigued achieves restful sleep. ▪ Exercise 2 or more hours before bedtime to cool down/promote relaxation ▪ However excess fatigue can make it difficult to fall asleep o Food and Caloric Intake ▪ Eating a large, heavy, or spicy meal at night interferes with sleep ▪ Caffeine, alcohol, and nicotine produce insomnia o Sleep Disorders ▪ Sleep disorders are conditions that, if untreated, generally cause disturbed nighttime sleep that results in one of three problems: insomnia, abnormal movements or sensation during sleep or when waking up at night, or excessive daytime sleepiness (EDS) o Physical Illness ▪ Any illness that causes pain, physical discomfort, or mood problems such as anxiety or depression often results in sleep problems. People with such alterations frequently have trouble falling or staying asleep. Illnesses also force patients to sleep in unfamiliar positions. For example, it is difficult for a patient with an arm or leg in traction to rest comfortably. ▪ Respiratory disease often interferes with sleep. Patients with chronic lung disease such as emphysema are short of breath and frequently cannot sleep without two or three pillows to raise their heads. Asthma, bronchitis, and allergic rhinitis alter the rhythm of breathing and disturb sleep. A person with a common cold has nasal congestion, sinus drainage, and a sore throat, which impair breathing and the ability to relax. ▪ Connections among heart disease, sleep, and sleep disorders exist. Sleep- related breathing disorders are linked to increased incidence of nocturnal angina (chest pain), increased heart rate, electrocardiogram changes, high blood pressure, and risk of heart diseases and stroke. Hypertension often causes early-morning awakening and fatigue. Research also identifies an increased risk of sudden cardiac death in the first hours after awakening. Sleep disruptions and frequent arousals occur in people with heart failure as a result of the apnea, hypercapnia, and hypoxemia that develops as the disease progresses. Hypothyroidism decreases stage 4 sleep, whereas hyperthyroidism causes people to take more time to fall asleep. ▪ Nocturia, or urination during the night, disrupts sleep and the sleep cycle. After repeated awakenings to urinate, returning to sleep is difficult, and the sleep cycle is not complete. Although this condition is most common in older people with reduced bladder tone or people with cardiac disease, diabetes, urethritis, or prostatic disease, it also occurs in a significant number of younger people. ▪ Many people experience restless legs syndrome (RLS), which occurs before sleep onset. More common in women, older people, and those with iron deficiency anemia, RLS symptoms include recurrent, rhythmical movements of the feet and legs. Patients feel an itching sensation deep in the muscles. Relief comes only from moving the legs, which prevents relaxation and subsequent sleep. RLS is sometimes a relatively benign condition, depending on how severely sleep is disrupted. Primary RLS is a CNS disorder. Researchers associate secondary RLS with lower levels of iron, pregnancy, renal failure, stress, diet, Parkinson's disease, or a side effect of drugs. ▪ People with peptic ulcer disease often awaken in the middle of the night. Studies showing a relationship between gastric acid secretion and stages of sleep are conflicting. One consistent finding is that people with duodenal ulcers fail to suppress acid secretion in the first 2 hours of sleep. Many patients experience gastroesophageal reflux as a result of the acid production, which disrupts sleep. • Factors that promote sleep/Sleep hygiene o Environmental Controls ▪ All patients require a sleeping environment with a comfortable room temperature and proper ventilation, minimal sources of noise, a comfortable bed, and proper lighting o Promoting Bedtime Routines ▪ Bedtime routines relax patients in preparation for sleep ▪ A bedtime routine (e.g., same hour for bedtime, snack, or quiet activity) used consistently helps young children avoid delaying sleep. Parents need to reinforce patterns of preparing for bedtime. Quiet activities such as reading stories, coloring, allowing children to sit in a parent's lap while listening to music or listening to a prayer are routines that are often associated with preparing for bed. ▪ Adults need to avoid excessive mental stimulation just before bedtime. Reading a light novel, watching an enjoyable television program, or listening to music helps a person relax. Relaxation exercises such as slow, deep breathing for 1 or 2 minutes relieve tension and prepare the body for rest o Promoting Safety ▪ For any patient prone to confusion or falls, safety is critical. A small night- light helps a patient orient to the room environment before going to the bathroom. Beds set lower to the floor can lessen the chance of a person falling when first standing. ▪ Instruct patients to remove clutter and throw rugs from the path used to walk from the bed to the bathroom. If a patient needs help to ambulate from a bed to the bathroom, place a small bell at the bedside to call family members. Sleepwalkers are unaware of their surroundings and are slow to react, increasing the risk of falls. Do not startle sleepwalkers but instead gently wake them and lead them back to bed. ▪ Infants' beds need to be safe. To reduce the chance of suffocation, do not place pillows, stuffed toys, or the ends of loose blankets in cribs o Promoting Comfort ▪ People fall asleep only after feeling comfortable and relaxed. Minor irritants often keep patients awake. Soft cotton nightclothes keep infants or small children warm and comfortable. ▪ Instruct patients to wear loose-fitting nightwear. An extra blanket is sometimes all that is necessary to prevent a person from feeling chilled and being unable to fall asleep. Patients need to void before retiring so they are not kept awake by a full bladder. o Establishing Periods of Rest and Sleep ▪ In the home it helps to encourage patients to stay physically active during the day so they are more likely to sleep at night. Increasing daytime activity lessens problems falling asleep. In a home setting you frequently care for patients with chronic debilitating disease. ▪ The nursing care plan includes having patients set aside afternoons for rest to promote optimal health. Help adjust medication schedules, instruct patients to regularly void before rest periods, and suggest silencing the telephone ringer so rest periods are uninterrupted. o Stress Reduction ▪ The inability to sleep because of emotional stress also makes a person feel irritable and tense. When patients are emotionally upset, encourage them to try not to force sleep. Otherwise insomnia frequently develops, and soon bedtime is associated with the inability to relax. ▪ Encourage a patient who has difficulty falling asleep to get up and pursue a relaxing activity such as sewing or reading rather than staying in bed and thinking about sleep. ▪ Preschoolers have bedtime fears (fear of the dark or strange noises), awaken during the night, or have nightmares. After nightmares the parent enters the child's room immediately and talks to him or her briefly about fears to provide a cooling-down period. ▪ One approach is to comfort children and leave them in their own beds so their fears are not used as excuses to delay bedtime. Keeping a light on in the room also helps some children. o Co-Sleeping Habits ▪ Implications for Patient-Centered Care • Complete a thorough sleep assessment of the child and family. • Discuss the risks of co-sleeping with parents. During the discussion remain culturally sensitive and respectful of the parents' views. • Co-sleeping has been linked to increased risk of SIDS under certain conditions such as parental smoking and alcohol or drug use. • Instruct parents who practice co-sleeping to avoid using alcohol or drugs that impair arousal. Decreased arousal prevents the parents from waking if the child is having problems. • Co-sleeping should occur on a firm mattress (never on a water bed, sofa, or couch). • Encourage parents to use light sleeping clothes, keep room temperature comfortable, and not bundle the child tightly or in too many clothes. o Bedtime Snacks ▪ Some people enjoy bedtime snacks, whereas others cannot sleep after eating. A dairy product such as warm milk or cocoa that contains L- tryptophan is often helpful in promoting sleep. A full meal before bedtime often causes gastrointestinal upset or reflux and interferes with the ability to fall asleep. ▪ Warn patients against drinking or eating foods with caffeine before bedtime. Coffee, tea, colas, and chocolate act as stimulants, causing a person to stay awake or to awaken throughout the night. Caffeinated foods and liquids and alcohol act as diuretics and cause a person to awaken in the night to void. ▪ Infants require special measures to minimize nighttime awakenings for feeding. It is common for children to need middle-of-the-night bottle- feeding or breastfeeding. Experts recommend offering the last feeding as late as possible. Tell parents not to give infants bottles in bed. o Example of a Nursing Plan: ▪ Objective • Patient will follow proper sleep-hygiene habits at home. ▪ Teaching Strategies • Instruct patient to try to exercise daily, preferably in the morning or afternoon, and to avoid vigorous exercise in the evening within 2 hours of bedtime. • Caution patient against sleeping long hours during weekends or holidays to prevent disturbance of normal sleep-wake cycle. • Explain that, if possible, patients should not use the bedroom for intensive studying, snacking, television watching, or other non- sleep activity besides sex. • Encourage patients to try to avoid worrisome thinking when going to bed and to use relaxation exercises. • If patient does not fall asleep within 30 minutes of going to bed, advise him or her to get out of bed and do some quiet activity until feeling sleepy enough to go back to bed. • Recommend that patient limit caffeine to morning coffee and limit alcohol intake (more than one to two drinks a day interrupts sleep cycle). • Ask patient to examine environment. Instruct that use of earplugs and eyeshades may be helpful. • Instruct patient to avoid heavy meals 3 hours before bedtime; a light snack may help. ▪ Evaluation • Have patient complete sleep-wake log for 1 week and compare it with previous sleep-wake log. • Ask patient to periodically complete visual analog or sleep-rating scale for perceptions of quality of sleep. • Nursing diagnoses related to sleep o Examples of nursing diagnoses for patients with sleep problems include the following: ▪ Anxiety ▪ Ineffective Breathing Pattern ▪ Acute Confusion ▪ Ineffective Coping ▪ Insomnia ▪ Fatigue ▪ Disturbed Sleep Pattern ▪ Sleep Deprivation ▪ Readiness for Enhanced Sleep • Sleep disorders & related assessment and nursing care o Insomnia ▪ Insomnia is a symptom that patients experience when they have chronic difficulty falling asleep, frequent awakenings from sleep, and/or a short sleep or nonrestorative sleep. ▪ It is the most common sleep-related complaint. People with insomnia experience EDS and insufficient sleep quantity and quality. However, frequently a patient gets more sleep than he or she realizes. Insomnia often signals an underlying physical or psychological disorder. It occurs more frequently in and is the most common sleep problem for women. ▪ Insomnia is often associated with poor sleep hygiene, or practices that a patient associates with sleep. If the condition continues, the fear of not being able to sleep is enough to cause wakefulness. During the day people with chronic insomnia feel sleepy, fatigued, depressed, and anxious. ▪ Treatment is symptomatic, including improved sleep-hygiene measures, biofeedback, cognitive techniques, and relaxation techniques. Behavioral and cognitive therapies have few adverse effects and show evidence of sustained improvement in sleep over time o Sleep Apnea ▪ Sleep apnea is a disorder characterized by the lack of airflow through the nose and mouth for periods of 10 seconds or longer during sleep. There are three types of sleep apnea: central, obstructive, and mixed apnea. The most common form is obstructive sleep apnea (OSA). ▪ Treatment includes therapy for underlying cardiac or respiratory complications and emotional problems that occur as a result of the symptoms of this disorder. ▪ In addition to complaints of EDS, sleep attacks, fatigue, morning headaches, irritability, depression, difficulty concentrating, and decreased sex drive are common. OSA affects quality-of-life issues such as marital relationships and interactions within and outside the family and often is an embarrassment to a patient. • Obstructive Sleep Apnea o The two major risk factors for OSA are obesity and hypertension. Smoking, heart failure, type II diabetes, alcohol, and a positive family history of OSA also greatly increase the risk of developing the problem o OSA occurs when muscles or structures of the oral cavity or throat relax during sleep. The upper airway becomes partially or completely blocked, diminishing nasal airflow (hypopnea) or stopping it (apnea) for as long as 30 seconds o Excessive daytime sleepiness (EDS) and fatigue are the most common complaints of people with OSA. People with severe OSA often report taking daytime naps and experience a disruption in their daily activities because of sleepiness • Central Sleep Apnea o (CSA) involves dysfunction in the respiratory control center of the brain. The impulse to breathe fails temporarily, and nasal airflow and chest wall movement cease. The oxygen saturation of the blood falls. The condition is common in patients with brainstem injury, muscular dystrophy, and encephalitis. Less than 10% of sleep apnea is predominantly central in origin. People with CSA tend to awaken during sleep and therefore complain of insomnia and EDS. Mild and intermittent snoring is also present. • Mixed Sleep Apnea o No data was given about this, but I assume it is both a physical and respiratory control dysfunction. o Narcolepsy ▪ Narcolepsy is a dysfunction of mechanisms that regulate sleep and wake states. Excessive daytime sleepiness is the most common complaint associated with this disorder. During the day a person suddenly feels an overwhelming wave of sleepiness and falls asleep; REM sleep occurs within 15 minutes of falling asleep. ▪ Cataplexy, or sudden muscle weakness during intense emotions such as anger, sadness, or laughter, occurs at any time during the day. If the cataplectic attack is severe, a patient loses voluntary muscle control and falls to the floor. A person with narcolepsy often has vivid dreams that occur as he or she is falling asleep. These dreams are difficult to distinguish from reality. ▪ Sleep paralysis, or the feeling of being unable to move or talk just before waking or falling asleep, is another symptom. Some studies show a genetic link for narcolepsy. ▪ A person with narcolepsy falls asleep uncontrollably at inappropriate times. When individuals do not understand this disorder, a sleep attack is easily mistaken for laziness, lack of interest in activities, or drunkenness. Typically the symptoms first begin to appear in adolescence and are often confused with the EDS that commonly occurs in teens. ▪ Narcoleptic patients are treated with stimulants or wakefulness-promoting agents such as sodium oxybate, modafinil (Provigil) or armodafinil (Nuvigil) that only partially increase wakefulness and reduce sleep attacks. Patients also receive antidepressant medications that suppress cataplexy and the other REM-related symptoms. Brief daytime naps no longer than 20 minutes help reduce subjective feelings of sleepiness. ▪ Other management methods that help are following a regular exercise program, practicing good sleep habits, avoiding shifts in sleep, strategically timing daytime naps if possible, eating light meals high in protein, practicing deep breathing, chewing gum, and taking vitamins. Patients with narcolepsy need to avoid factors that increase drowsiness (e.g., alcohol; heavy meals; exhausting activities; long-distance driving; and long periods of sitting in hot, stuffy rooms). • Conducting Sleep assessment/ Sleep history o Sources for Sleep Assessment. ▪ Usually patients are the best resource for describing sleep problems and how they are a change from their usual sleep and waking patterns. Often the patient knows the cause for sleep problems such as a noisy environment or worry over a relationship. ▪ In addition, bed partners are able to provide information about patients' sleep patterns that help reveal the nature of certain sleep disorders. For example, partners of patients with sleep apnea often complain that the patient's snoring disturbs their sleep. Ask bed partners (if the patient agrees) whether patients have breathing pauses during sleep and how frequently the apneic attacks occur. Some partners mention becoming fearful when patients apparently stop breathing for periods. ▪ When caring for children, seek information about sleep patterns from parents or guardians because they are usually a reliable source of information. Hunger, excessive warmth, and separation anxiety often contribute to an infant's difficulty going to sleep or frequent awakenings during the night. Parents of infants need to keep a 24-hour log of their infant's waking and sleeping behavior for several days to determine the cause of the problem. ▪ They also need to describe the infant's eating pattern and sleeping environment because these influence sleeping behavior. Older children often are able to relate fears or worries that inhibit their ability to fall asleep. If children frequently awaken in the middle of bad dreams, parents are able to identify the problem but perhaps do not understand the meaning of the dreams. Ask parents to describe the typical behavior patterns that foster or impair sleep. ▪ For example, excessive stimulation from active play or visiting friends predictably impairs sleep. With chronic sleep problems, parents need to relate the duration of the problem, its progression, and children's responses. o Tools for Sleep Assessment. ▪ Two effective subjective measures of sleep are the Epworth Sleepiness Scale and the Pittsburgh Sleep Quality Index. The Epworth Sleepiness Scale evaluates the severity of EDS. The Pittsburgh Sleep Quality Index assesses sleep quality and patterns. Another effective, brief method for assessing sleep quality is the use of a visual analog scale. ▪ Draw a straight horizontal line 100 mm (4 inches) long. Opposing statements such as “best night's sleep” and “worst night's sleep” are at opposite ends of the line. Ask patients to place a mark on the horizontal line at the point corresponding to their perceptions of the previous night's sleep. ▪ Measuring the distances of the mark along the line in millimeters offers a numerical value for satisfaction with sleep. Use the scale repeatedly to show change over time. Such a scale is useful to assess an individual patient, not to compare patients. ▪ Another brief subjective method to assess sleep is a numeric scale with a 0-to-10 sleep rating. Ask individuals to separately rate the quantity and quality of their sleep on the scale. Instruct them to indicate with a number between 0 and 10 their sleep quantity and then their quality of sleep, with 0 being the worst sleep and 10 being the best. o Sleep History. ▪ When suspecting a patient has a sleep problem, assess the quality and characteristics of sleep in greater depth by asking the patient to describe the problem. This includes recent changes in sleep pattern, sleep symptoms experienced during waking hours, use of sleep and other prescribed or over-the-counter medications, diet 1001and intake of substances such as caffeine or alcohol that influence sleep, and recent life events that have affected the patient's mental and emotional status. ▪ As an adjunct to the sleep history, have the patient and bed partner keep a sleep-wake log for 1 to 4 weeks. The patient completes the sleep-wake log daily to provide information on day-to-day variations in sleep-wake patterns over extended periods. ▪ Entries in the log often include 24-hour information about various waking and sleeping health behaviors such as physical activities, mealtimes, type and amount of intake (alcohol and caffeine), time and length of daytime naps, evening and bedtime routines, the time the patient tries to fall asleep, nighttime awakenings, and the time of morning awakening. A partner helps record the estimated times the patient falls asleep or awakens. Although the log is helpful, the patient needs to be motivated to participate in its completion. o Description of Sleeping Problems. ▪ Conduct a more detailed history when a patient has a persistent or what appears to be a serious sleep problem. Open-ended questions help a patient describe a problem more fully. A general description of the problem followed by more focused questions usually reveals specific characteristics that are useful in planning therapies. ▪ To begin, you need to understand the nature of the sleep problem, its signs and symptoms, its onset and duration, its severity, any predisposing factors or causes, and the overall effect on the patient. Ask specific questions related to the sleep problem • Sleep requirements based on developmental stage o Neonates. ▪ The neonate up to the age of 3 months averages about 16 hours of sleep a day, sleeping almost constantly during the first week. The sleep cycle is generally 40 to 50 minutes with wakening occurring after one to two sleep cycles. Approximately 50% of this sleep is REM sleep, which stimulates the higher brain centers. This is essential for development because the neonate is not awake long enough for significant external stimulation. o Infants. ▪ Infants usually develop a nighttime pattern of sleep by 3 months of age. The infant normally takes several naps during the day but usually sleeps an average of 8 to 10 hours during the night for a total daily sleep time of 15 hours. About 30% of sleep time is in the REM cycle. Awakening commonly occurs early in the morning, although it is not unusual for an infant to wake up during the night. o Toddlers. ▪ By the age of 2 children usually sleep through the night and take daily naps. Total sleep averages 12 hours a day. After 3 years of age children often give up daytime naps. It is common for toddlers to awaken during the night. The percentage of REM sleep continues to fall. During this period toddlers may be unwilling to go to bed at night because they need autonomy or fear separation from their parents. o Preschoolers. ▪ On average a preschooler sleeps about 12 hours a night (about 20% is REM). By the age of 5 he or she rarely takes daytime naps except in cultures in which a siesta is the custom. The preschooler usually has difficulty relaxing or quieting down after long, active days and has bedtime fears, awakens during the night, or has nightmares. Partial awakening followed by normal return to sleep is frequent. 998In the awake period the child exhibits brief crying, walking around, unintelligible speech, sleepwalking, or bed-wetting. o School-Age Children. ▪ The amount of sleep needed varies during the school years. A 6-year-old averages 11 to 12 hours of sleep nightly, whereas an 11-year-old sleeps about 9 to 10 hours. The 6- or 7-year-old usually goes to bed with some encouragement or by doing quiet activities. The older child often resists sleeping because he or she is unaware of fatigue or has a need to be independent. o Adolescents. ▪ On average the majority of teenagers get about 7 hours or less of sleep per night. The typical adolescent is subject to a number of changes such as school demands, after-school social activities, and part-time jobs, which reduce the time spent sleeping. Adolescents typically have electronic devices such as televisions, computers, smartphones, or video games in their rooms, which further contribute to sleep disruption, poor sleep quality, and decreased amount of sleep. Shortened sleep time often results in EDS, which frequently leads to reduced performance in school, vulnerability to accidents, behavior and mood problems, and increased use of alcohol. o Young Adults. ▪ Most young adults average 6 to image hours of sleep a night. Approximately 20% of sleep time is REM sleep, which remains consistent throughout life. It is common for the stresses of jobs, family relationships, and social activities to frequently lead to insomnia and the use of sleep medication. Daytime sleepiness contributes to an increased number of accidents, decreased productivity, and interpersonal problems in this age- group. ▪ Pregnancy increases the need for sleep and rest. However, a majority of pregnant women describe variations in sleep habits. Increases in estrogen and progesterone during pregnancy affect sleep. Estrogen has been shown to decrease REM sleep. First-trimester sleep disturbances include a reduction in overall sleep time and quality. Daytime drowsiness, insomnia, and nighttime awakenings also increase because of frequent nocturnal voiding. These disturbances level off in the second trimester. Insomnia, periodic limb movements, RLS, and sleep-disordered breathing are common problems during the third trimester of pregnancy. o Middle Adults. ▪ During middle adulthood the total time spent sleeping at night begins to decline. The amount of stage 4 sleep begins to fall, a decline that continues with advancing age. Insomnia is particularly common, probably because of the changes and stresses of middle age. Anxiety, depression, or certain physical illnesses cause sleep disturbances. Women experiencing menopausal symptoms often experience insomnia. o Older Adults. ▪ Complaints of sleeping difficulties increase with age. Older adults experience weakening, desynchronized circadian rhythms that alter the sleep-wake cycle. Episodes of REM sleep tend to shorten. Stages 3 and 4 NREM sleep progressively decrease; some older adults have almost no stage 4, or deep sleep. An older adult awakens more often during the night, and it takes more time for him or her to fall asleep. The tendency to nap seems to increase progressively with age because of the frequent awakenings experienced at night. ▪ The presence of chronic illness often results in sleep disturbances for the older adult. For example, an older adult with arthritis frequently has difficulty sleeping because of painful joints. Changes in sleep pattern are often caused by changes in the CNS that affect the regulation of sleep. Many older adults with insomnia have co-morbid psychiatric illness or medical conditions, take medications that disrupt sleep patterns, or use drugs or alcohol. Sensory impairment reduces an older person's sensitivity to time cues that maintain circadian rhythms. • Symptoms that occur with lack of sleep o Sleep deprivation is a problem many patients experience as a result of dyssomnia. Causes include symptoms (e.g., fever, difficulty breathing, or pain) caused by illnesses, emotional stress, medications, environmental disturbances (e.g., frequent nursing care), and variability in the timing of sleep because of shift work. o Physicians and nurses are particularly prone to sleep deprivation as a result of long work schedules and rotating shifts. Chronic sleep deprivation is associated with development of cardiovascular disease, weight gain, type II diabetes, poor memory, depression, and digestive problems Bowel Elimination • Assessment of bowel function o Assessment for bowel elimination patterns and abnormalities includes a nursing history, physical assessment of the abdomen, inspection of fecal characteristics, and review of relevant test results. In addition, determine the patient's medical history, pattern and types of fluid and food intake, mobility, chewing ability, medications, recent illnesses and/or stressors, and environmental situation. o Patients expect nurses to answer all of their questions regarding diagnostic tests and the preparation for these tests. They are concerned about discomfort and exposure of their perineal area. Bowel problems are often a source of discomfort and embarrassment for the patient and their families. Fecal and urinary incontinence in older people is the second most common reason for admission to a long-term care facility (Long, 2010). Some older patients who fail to recognize their elimination needs need monitoring for elimination patterns so negative consequences do not occur. Remember that each patient has a unique situation and a perception of what is “right” for him or her. o Then perform physical assessment with emphasis on the mouth, abdomen, and rectum. • Causes of diarrhea, constipation o Diarrhea ▪ Diarrhea is an increase in the number of stools and the passage of liquid, unformed feces. It is associated with disorders affecting digestion, absorption, and secretion in the GI tract. Intestinal contents pass through the small and large intestine too quickly to allow for the usual absorption of fluid and nutrients. ▪ Irritation within the colon results in increased mucus secretion. As a result, feces become watery, and the patient often has difficulty controlling the urge to defecate. ▪ Excess loss of colonic fluid results in dehydration with fluid and electrolyte or acid-base imbalances if the fluid is not replaced. Infants and older adults are particularly susceptible to associated complications. Because repeated passage of diarrhea stools exposes the skin of the perineum and buttocks to irritating intestinal contents, meticulous skin care and containment of fecal drainage is necessary to prevent skin breakdown. o Constipation ▪ Constipation is a symptom, not a disease, and there are many possible causes. Improper diet, reduced fluid intake, lack of exercise, and certain medications can cause constipation. For example, patients receiving opiates for pain after surgery often require a stool softener or laxative to prevent constipation. A recent integrative review of the literature revealed that female gender and older age were the highest risk factors for constipation. ▪ Signs of constipation include infrequent bowel movements (less than three per week) and hard, dry stools that are difficult to pass. When intestinal motility slows, the fecal mass becomes exposed to the intestinal walls over time, and most of the fecal water content is absorbed. Little water is left to soften and lubricate the stool. Passage of a dry, hard stool often causes rectal pain. Constipation is a significant source of discomfort. Assess the need for intervention before defecation becomes painful or the stool is impacted. • Nursing diagnoses related to bowel elimination o Examples Include: ▪ Disturbed Body Image ▪ Bowel Incontinence ▪ Constipation ▪ Perceived Constipation ▪ Risk for Constipation ▪ Diarrhea ▪ Nausea ▪ Deficient Knowledge (Nutrition) ▪ Acute Pain ▪ Toileting Self-Care Deficit • Interventions to promote bowel elimination o A number of interventions stimulate the defecation reflex, affect the character of feces, or increase peristalsis to help patients evacuate bowel contents normally and without discomfort. ▪ Sitting Position. • Help patients who have difficulty sitting because of muscular weakness and mobility problems. Place an elevated seat on the toilet or a bedside commode when patients are unable to lower themselves to a sitting position because of pain or weakness. These seats require patients to use less effort to sit or stand. ▪ Positioning on Bedpan. • Patients restricted to bed use bedpans for defecation. Women use bedpans to pass both urine and feces, whereas men use bedpans only for defecation. Sitting on a bedpan is often uncomfortable. Help position patients comfortably. Two types of bedpans are available (Figure 47-9). The regular bedpan, made of plastic, has a curved smooth upper end and a sharper-edged lower end and is about 5 cm (2 inches) deep. The smaller fracture pan, designed for patients with lower-extremity fractures, has a shallow upper end 1163about 2.5 cm (1 inch) deep. The shallow end of the pan fits under the buttocks toward the sacrum; the deeper end, which has a handle, goes just under the upper thighs. The pan needs to be high enough so feces enter it. ▪ When positioning a patient, it is important to prevent muscle strain and discomfort. Never try to lift a patient onto a bedpan. Never place a patient on a bedpan and then leave with the bed flat unless activity restrictions demand it because it forces the patient to hyperextend the back to lift the hips on the pan. The proper position for the patient on a bedpan is with the head of the bed elevated 30 to 45 degrees (Figures 47-10 and 47-11). When patients are immobile or it is unsafe to allow them to raise their hips, it is safest for both caregivers and patients to roll them on to the bedpan (Box 47-9). Always wear gloves when handling a bedpan. o With some acute illnesses the GI system becomes affected. Changes in a patient's fluid status, mobility patterns, nutrition, and sleep cycle affect regular bowel habits. Surgical interventions on the GI tract obviously affect bowel elimination. However, surgery on other systems (e.g., the musculoskeletal and cardiovascular systems) also sometimes affects it. o Some medications initiate and facilitate stool passage. Laxatives and cathartics have the short-term action of emptying the bowel. These agents are also used to cleanse the bowel for patients undergoing GI tests and abdominal surgery. Although the terms laxative and cathartic are often used interchangeably, cathartics generally have a stronger and more rapid effect on the intestines. o Teach patients about the potential harmful effects of overuse of laxatives such as impaired bowel motility and decreased response to sensory stimulus. Make sure patients understand that laxatives are not to be used long term for maintenance of bowel function. • Ostomy assessments, care, teaching o Review of an Ostomy: ▪ The location of an ostomy determines stool consistency. A person with a sigmoid colostomy will have a more formed stool. The output from a transverse colostomy will be thick liquid to soft consistency. These ostomies are the easiest to perform surgically and are done as a temporary means to divert stool from an area of trauma or perianal wounds. They may also be a palliative diversion if obstruction from a tumor is present. With an ileostomy the fecal effluent leaves the body before it enters the colon, creating frequent, liquid stools. ▪ The end colostomy consists of a stoma formed by bringing a piece of intestine out through a surgically created opening in the abdominal wall, turning it down like a turtleneck and suturing it to the abdominal wall. The intestine distal to the stoma is either removed or sewn closed (called Hartmann's pouch) and left in the abdominal cavity. End ostomies are permanent or reversible. The rectum is either left intact or removed. o Ostomy Care ▪ Patients with temporary or permanent bowel diversions have unique elimination needs. An individual with an ostomy wears a pouch to collect effluent or output from the stoma. The pouches are odor proof and have a protective skin barrier surrounding the stoma. Empty the pouch when it is image to image full. Change the pouching system approximately every 3 to 7 days, depending on a patient's individual needs. ▪ Assess the stoma color. It should be pink or red. You observe the skin at each pouch change for signs of irritation or skin breakdown. Skin protection is important because the effluent has digestive enzymes that cause irritant dermatitis if there is leakage on the peristomal skin. ▪ Other peristomal skin problems are fungal rashes, folliculitis, or ulcerations. Refer patients with these problems to an ostomy care nurse o Ostomy Teaching ▪ Objective • Patient/caregiver will demonstrate how to empty and change an ostomy pouch. ▪ Teaching Strategies • Provide a comprehensive list of the products needed to care for the ostomy • Provide patient/caregiver with supplies to last 1 to 2 weeks and the contact number information for a medical supply company • Show patient/caregiver the step-by-step approach for changing an ostomy pouch. • Provide at least one opportunity for patient/caregiver to empty and change the ostomy pouch while patient is in the hospital • Provide detailed instructions for diet, fluids, peristomal skin care, restrictions on lifting, resuming exercise, intimacy, and when to contact the health care provider. • Arrange follow-up with an ostomy nurse if possible. ▪ Evaluation • Observe patient/caregiver change ostomy pouch. • Ask patient/caregiver to teach back instructions given. • Hemoccult testing o The skill of fecal occult blood test (FOBT) can be delegated to nursing assistive personnel (NAP). However, the nurse is responsible for assessing the significance of the findings. You may need to send the specimen to the laboratory. Refer to your agency policies. The nurse instructs the NAP to: ▪ Notify the nurse if frank bleeding occurs after obtaining the sample. • Equipment o Hemoccult test paper, Hemoccult developer, wooden applicator, and clean gloves (Check the expiration dates on the developer and the test paper before using.) o Steps ▪ 1. Identify patient using two identifiers (e.g., name and birthday or name and account number) according to agency policy. ▪ 2. Explain purpose of test and ways patient can help. Patient can collect own specimen if possible. ▪ 3. Perform hand hygiene and apply clean gloves. ▪ 4. Use tip of wooden applicator (see illustration) to obtain a small part of stool specimen. Be sure that specimen is free of toilet paper and not contaminated with urine. ▪ 5. Perform Hemoccult slide test: • a. Open flap of slide and, using a wooden applicator, thinly smear stool in first box of the guaiac paper. Apply a second fecal specimen from a different part of the stool to second box of slide • b. Close slide cover and turn the packet over to reverse side (see illustration). After waiting 3 to 5 minutes, open cardboard flap and apply 2 drops of developing solution on each box of guaiac paper. A blue color indicates a positive guaiac or presence of fecal occult blood. • c. Interpret the color of the guaiac paper after 30 to 60 seconds. • d. After determining if the patient's specimen is positive or negative, apply 1 drop of developer to the quality control section and interpret within 10 seconds. • e. Dispose of test slide in proper receptacle. ▪ 6. Wrap wooden applicator in paper towel, remove gloves, and discard in proper receptacle. ▪ 7. Perform hand hygiene. ▪ 8. Record results of test; note any unusual fecal characteristics. (Submit only one sample per day.) o When your patients are going to have a gFOBT, it is important to instruct them to avoid eating red meat for 3 days before testing. If there are no contraindications and it is approved by the health care provider, instruct your patient to stop taking aspirin, ibuprofen, naproxen, or other nonsteroidal anti-inflammatory drugs for 7 days because these could cause a false-positive test result. Patients also need to avoid vitamin C supplements and citrus fruits and juices for 3 days before the test because they can cause a false-negative result • Enema administration o Enemas are available in commercially packaged, disposable units or with reusable equipment prepared before use. Sterile technique is unnecessary because the colon normally contains bacteria. However, wear gloves to prevent the transmission of fecal microorganisms. o Explain the procedure, including the position to assume, precautions to take to avoid discomfort, and length of time necessary to retain the solution before defecation. If a patient needs to take the enema at home, explain the procedure to a family member. o Giving an enema to a patient who is unable to contract the external sphincter poses difficulties. Give the enema with the patient positioned on the bedpan. Giving the enema with a patient sitting on the toilet is unsafe because the position of the rectal tubing could injure the rectal wall. Skill 47-1 on pp. 1170–1173 outlines the steps for an enema administration. • Bowel training program o A patient with chronic constipation or fecal incontinence secondary to cognitive impairment may benefit from bowel training, also called habit training. The training program involves setting up a daily routine. By attempting to defecate at the same time each day and using measures that promote defecation, a patient may establish a normal defecation pattern. The program requires time, patience, and consistency. A patient with cognitive impairment needs to have a caregiver able to devote the time to the training program. A successful program includes the following: ▪ Assessing the normal elimination pattern and recording times when a patient is incontinent ▪ Incorporating principles of gerontological nursing when providing bowel retraining programs for an older adult. Examples for an older adult include: o Older age is a risk factor for having constipation. o Increase fiber in diet with whole grains, legumes, fruits, and vegetables. o A minimum of 1500 mL of fluid per day reduces the risk of constipation, with increased fluid needs during summer months and for those on diuretics with stable cardiovascular status. o If holding a drinking cup is a problem, consider using a lighter plastic cup and filling half full, refilling frequently. o Encourage regular exercise within the limitations imposed by other conditions. o Patients need to feel at ease during elimination. Lack of privacy leads a patient to ignore the urge to defecate. o Review all medications with a patient's health care provider to substitute medications that are less likely to cause constipation whenever possible. o Behavioral interventions such as timed toileting helps establish a scheduled time for bowel elimination. Try to maintain the same schedule each day for toileting. ▪ Choosing a time based on the patient's pattern to initiate defecation- control measures ▪ Offering a hot drink (hot tea) or fruit juice (prune juice) (or whatever fluids normally stimulate peristalsis for the patient) before the defecation time ▪ Helping the patient to the toilet at the designated time ▪ Providing privacy ▪ Instructing the patient to lean forward at the hips while sitting on the toilet, apply manual pressure with the hands over the abdomen, and bear down but not strain to stimulate colon emptying ▪ An unhurried environment and a nonjudgmental caregiver ▪ Maintaining normal exercise within the patient's physical ability Fluid & Electrolytes, Acid/Base • Know normal serum chemistry levels o • Hypo/hypernatremia, hypo/hyperkalemia o Hyponatremia ▪ Also called water excess or water intoxication, is a hypotonic condition. It arises from gain of relatively more water than salt or loss of relatively more salt than water. The excessively dilute condition of interstitial fluid causes water to enter cells by osmosis, causing the cells to swell. Signs and symptoms of cerebral dysfunction occur when brain cells swell. o Hypernatremia ▪ Also called water deficit, is a hypertonic condition. Two general causes make body fluids too concentrated: loss of relatively more water than salt or gain of relatively more salt than water. Table 42-3 lists specific causes under these categories. When the interstitial fluid becomes hypertonic, water leaves cells by osmosis, and they shrivel. ▪ Signs and symptoms of hypernatremia are those of cerebral dysfunction, which arise when brain cells shrivel. Hypernatremia may occur in combination with ECV deficit; this combined disorder is called clinical dehydration. o Hypokalemia ▪ Abnormally low potassium concentration in the blood. It results from decreased potassium intake and absorption, a shift of potassium from the ECF into cells, 941and an increased potassium output. Common causes of hypokalemia from increased potassium output include diarrhea, repeated vomiting, and use of potassium-wasting diuretics. People who have these conditions need to increase their potassium intake to reduce their risk of hypokalemia. ▪ Hypokalemia causes muscle weakness, which becomes life threatening if it includes respiratory muscles and potentially life-threatening cardiac dysrhythmias. o Hyperkalemia ▪ Hyperkalemia is abnormally high potassium ion concentration in the blood. Its general causes are increased potassium intake and absorption, shift of potassium from cells into the ECF, and decreased potassium output. People who have oliguria (decreased urine output) are at high risk of hyperkalemia from the resultant decreased potassium output unless their potassium intake also decreases substantially. ▪ Understanding this principle helps you remember to check urine output before you administer IV solutions containing potassium. Hyperkalemia can cause muscle weakness, potentially life-threatening cardiac dysrhythmias, and cardiac arrest. • ABGs- o Normal ranges ▪ Given in the above table o Metabolic Acidosis ▪ Metabolic acidosis occurs from an increase of metabolic acid or a decrease of base (bicarbonate). The kidneys are unable to excrete enough metabolic acids, which accumulate in the blood, or bicarbonate is removed from the body directly as with diarrhea (see Table 42-7). In either case the blood image decreases, and the pH falls. With an increase of metabolic acids, blood image decreases because it is used to buffer metabolic acids. Similarly, when patients have conditions that cause the removal of image, the amount of image in the blood decreases. ▪ To help identify the specific cause, health care providers and the laboratory calculate the anion gap, a reflection of unmeasured anions in plasma. You calculate anion gap by subtracting the sum of plasma concentrations of the anions Cl− and image from the plasma concentration of the cation Na+. When reviewing laboratory reports, check the reference values from the laboratory that measured the electrolyte concentrations (Table 42-8). o Metabolic Alkalosis ▪ Metabolic alkalosis occurs from a direct increase of base (image) or a decrease of metabolic acid, which increases blood image by releasing it from its buffering function. Common causes include vomiting and gastric suction (see Table 42-7). The respiratory compensation for metabolic alkalosis is hypoventilation. The decreased rate and depth of respiration allow carbonic acid to increase in the blood, as seen by an increased PaCO2. ▪ The need for oxygen may limit the degree of respiratory compensation for metabolic alkalosis. Because image crosses the blood-brain barrier with difficulty, neurological signs and symptoms are less severe or even absent with metabolic alkalosis. o Respiratory Acidosis ▪ Respiratory acidosis arises from alveolar hypoventilation; the lungs are unable to excrete enough CO2. The PaCO2 rises, creating an excess of carbonic acid in the blood, which decreases pH (Table 42-7). The kidneys compensate by increasing excretion of metabolic acids in the urine, which increases blood bicarbonate. ▪ This compensatory process is slow, often taking 24 hours to show clinical effect and 3 to 5 days to reach steady state. Decreased cerebrospinal fluid (CSF) pH and intracellular pH of brain cells cause decreased level of consciousness. o Respiratory Alkalosis ▪ Respiratory alkalosis arises from alveolar hyperventilation; the lungs excrete too much carbonic acid (CO2 and water). The PaCO2 falls, creating a deficit of carbonic acid in the blood, which increases pH (see Table 42-7). Respiratory alkalosis usually is short lived; thus the kidneys do not have time to compensate. ▪ When the pH of blood, CSF, and ICF increases acutely, cell membrane excitability also increases, which can cause neurological symptoms such • IV therapy as excitement, confusion, and paresthesias. If the pH rises high enough, central nervous system (CNS) depression can occur. o Insertion ▪ After you collect the equipment at the patient's bedside, prepare to insert the IV line by assessing the patient for a venipuncture site. The most common IV sites are on the inner arm. Do not use hand veins on older adults or ambulatory patients. IV insertion in a foot vein is common with children, but avoid these sites in adults because of the increased risk of thrombophlebitis. ▪ As you assess a patient for potential venipuncture sites, consider conditions that exclude certain sites. Venipuncture is contraindicated in a site that has signs of infection, infiltration, or thrombosis. An infected site is red, tender, swollen, and possibly warm to the touch. Exudate may be present. Do not use an infected site because of the danger of introducing bacteria from the skin surface into the bloodstream. Avoid using an extremity with a vascular (dialysis) graft/fistula or on the same side as a mastectomy. Avoid areas of flexion if possible. Choose the most distal appropriate site. Using a distal site first allows for the use of proximal sites later if the patient needs a venipuncture site change. ▪ Venipuncture is a technique in which a vein is punctured through the skin by a sharp rigid stylet (e.g., metal needle). The stylet is partially covered either with a plastic catheter or a needle attached to a syringe. General purposes of venipuncture are to collect a blood specimen, start an IV infusion, provide vascular access for later use, instill a medication, or inject a radiopaque or other tracer for special diagnostic examinations. ▪ It takes practice to become proficient in venipuncture. Only experienced practitioners perform it for patients whose veins are fragile or collapse easily such as older adults. Box 42-7 describes principles to follow for venipuncture in older adults. o Maintenance ▪ After placing an IV line and regulating the flow rate, maintain the IV system. Line maintenance involves (1) keeping the system sterile and intact; (2) changing IV fluid containers, tubing, and contaminated site dressings; (3) helping a patient with self-care activities so as not to disrupt the system; and (4) monitoring for complications of IV therapy. The frequency and options for maintaining the system are identified in agency policies. ▪ An important component of patient care is maintaining the integrity of an IV line to prevent infection. Potential sites for contamination of a VAD are shown in Figure 42-16. Inserting an IV line under appropriate aseptic technique reduces the chances of contamination from the patient's skin. After insertion, prevent infection by the conscientious use of infection control principles such as thorough hand hygiene before and after handling any part of the IV system and maintaining sterility of the system during tubing and fluid container changes. ▪ Always maintain the integrity of an IV system. Never disconnect tubing because it becomes tangled or it might seem more convenient for positioning or moving a patient or applying a gown. If a patient needs more room to maneuver, use aseptic technique to add extension tubing to an IV line. However, keep the use of extension tubing to a minimum because each connection of tubing provides opportunity for contamination. Never let IV tubing touch the floor. Do not use stopcocks for connecting more than one solution to a single IV site because they are sources of contamination. IV tubing contains needleless injection ports through which syringes or other adaptors can be inserted for medication administration. Clean an injection port thoroughly with 2% chlorhexidine (preferred), 70% alcohol, or povidone-iodine solution and let it dry before accessing the system. ▪ Protective devices designed to prevent movement or accidental dislodgement of a VAD are called catheter stabilization devices (Figure 42-17). These devices are available in many hospitals, and nurses decide whether or not to use them when starting an IV line. This is a patient safety issue. Movement of the VAD in a vein can cause phlebitis and infiltration; VAD dislodgement requires using another VAD at a new IV infusion site. INS standards indicate that use of these devices is preferable over taping when feasible. o Complications • IV solutions – examples and when given o Hypotonic ▪ A hypotonic solution is more dilute than the blood o Hypertonic ▪ hypertonic solution is more concentrated than normal blood o Isotonic ▪ A fluid with the same tonicity as normal blood is called isotonic • Blood products Perioperative Nursing • Preoperative phase o Factors that can increase risk for complications in surgery ▪ Smoking, Age, Nutrition, Obesity, Obstructive Sleep Apnea, Immunosuppression, Fluid/electrolyte imbalance, Postop Nausea and Vomiting history, Venous Thromboembolism (DVT) risk. ▪ Surgical history, medications, allergies, smoking habits, alcohol ingestion/substance use and abuse, pregnancy, perception and knowledge regarding surgery, support sources, occupation, pre-op pain, review of emotional health, and cultural and spiritual factors. ▪ Your knowledge of potential surgical risk factors allows you to focus your assessment and screen patients carefully so you can take necessary precautions in planning perioperative care. Consider if any of the risk factors described earlier affect your patient. Collaborate closely with the health care provider when you identify a risk factor that requires therapy. ▪ For example, some patients need to stop taking estrogen-containing oral contraceptives or hormone-replacement therapy 4 weeks before elective surgery to reduce risk of thromboembolism. Carefully screen patients who have signs and symptoms of suspected OSA. Include the patient's sleeping partner as appropriate to assess for signs of OSA such as snoring. Also determine if the patient uses a continuous positive airway pressure (CPAP), noninvasive positive-pressure ventilation (NIPPV), or apnea monitoring at home. ▪ Instruct patients who use CPAP or NIPPV to bring their machine to the hospital or surgery center. Many hospitals are now making OSA screening mandatory using evidence-based tools, such as the STOP-BANG sleep apnea assessment tool o Procedures pre-op ▪ Be culturally sensitive when you assess a patient's physical, psychological, emotional, sociocultural, and spiritual well-being; recognize the degree of surgical risk; coordinate diagnostic tests; identify nursing diagnoses and nursing interventions; and establish outcomes in collaboration with patients and their families. Communicate pertinent data and the plan of care to surgical team members. ▪ Physical preparation • Maintaining normal fluid and electrolyte balance • Reducing risk of surgical site infection • Preventing bladder and bowel incontinence • Promoting rest and comfort ▪ Preparation on day of surgery • Hygiene • Hair and cosmetics • Removal of prostheses • Safeguarding valuables • Preparing the bowel and bladder • Vital signs • Documentation • Other procedures • Administering preoperative medications • Eliminating wrong site and wrong procedure surgery • Intraoperative phase o Role of the nurse ▪ There are two traditional nursing roles in the OR: circulating nurse and scrub nurse. The circulating nurse is an RN who does not scrub in and uses the nursing process in the management of patient care activities in the OR suite. The circulating nurse also manages patient positioning, antimicrobial skin preparation, medications, implants, placement and function of IPC devices, specimens, warming devices, and surgical counts of instruments and dressings. ▪ The scrub nurse is either an RN or surgical technologist who is often certified (CST). The scrub nurse must have a thorough knowledge of each step of a surgical procedure and the ability to anticipate each and every instrument and supply needed by the surgeons. A circulating nurse and scrub nurse partner together to ensure patient safety by minimizing risk of error. The team also works together to ensure cost-efficient use of supplies. ▪ A new role in the OR includes the RN first assistant (RNFA). This is an expanded role that requires formal academic education. The RNFA collaborates with the surgeon by handling and cutting tissue, using instruments and medical devices, providing exposure of the surgical area and hemostasis, and suturing. • Postoperative phase o Prevention of post-op complications ▪ Airway and respiration ▪ Circulation ▪ Temperature control ▪ Malignant hyperthermia ▪ Fluid and electrolyte balance ▪ Neurological functions ▪ Skin integrity and condition of the wound ▪ Metabolism ▪ Genitourinary function ▪ Gastrointestinal function • Paralytic ileus ▪ Comfort o Diet progression post-op ▪ Use patient assessment data to determine how quickly to advance your patient's diet. For example, provide clear liquids such as water, apple juice, broth, or tea after nausea subsides. Ingesting large amounts of fluids leads to distention and vomiting. ▪ If a patient tolerates liquids without nausea, advance the diet as ordered. Patients who had abdominal surgery are usually NPO the first 24 to 48 hours. As flatus and peristalsis return, provide clear liquids, followed by full liquids, a light diet of solid foods, and finally a patient's usual diet. Encourage intake of foods high in protein and vitamin C. • Teaching for each phase o Pre-Op ▪ Patient education is an important aspect of a patient's surgical experience (see Chapter 25). The topics and principles discussed depend on the type of surgery scheduled, whether a procedure is inpatient or outpatient, and the ability of a patient to attend to and learn content provided. Research shows that patient education often reduces patients' preoperative anxiety, which often leads to an increase in postoperative pain, poor outcomes, and prolonged hospital stays. ▪ In addition, education about the surgical experience increases patient satisfaction and knowledge, speeds up the recovery process, and facilitates a return to functioning. Structured teaching throughout the perioperative period influences the following: • Ventilatory function: Teaching improves the ability and willingness to deep breathe and cough effectively. • Physical functional capacity: Teaching increases understanding and willingness to ambulate and resume activities of daily living. • Sense of well-being: Patients who are prepared for surgery have less anxiety and report a greater sense of psychological well-being. • Length of hospital stay: Being informed reduces a patient's length of hospital stay by preventing or minimizing complications. ▪ Anxiety about pain and its management: Patients who learn about pain and ways to relieve it before surgery are less anxious about it, ask for what they need, and require less analgesia after surgery. ▪ The health care provider's office or hospital often provide preoperative information and instructions by telephone calls and home mailings. Instructions are available as preprinted teaching guidelines and checklists or in the form of videotapes or educational websites o Intra-Op ▪ A patient is usually still awake and notices health care providers in their surgical attire and masks when entering the OR. You transfer a patient to the OR bed by being sure that the stretcher and bed are locked in place. Explain to the patient all the activities you are completing. After safely securing the patient on the OR table with safety straps, you apply monitoring devices such as continuous ECG electrodes, a pulse oximeter sensor, and blood pressure cuff. For ECG, place electrodes on the chest and extremities correctly to record electrical activity of the heart accurately. ▪ The anesthesia provider will use the cuff to monitor the patient's blood pressure. An electronic monitor in the OR will display the patient's heart rate, vital signs, and pulse oximetry continuously. Capnography is also used frequently to measure the patient's ongoing end-tidal carbon dioxide values. Apply an electrical cautery grounding pad to the skin so cauterizing instruments can be used safely. If not applied before surgery, now is the time to apply anti-embolism devices. You help insert temperature probes via the bladder, esophagus, or rectum if required to continuously measure a patient's body temperature. o Post-Op ▪ Postoperative Instructions for an Ambulatory Surgical Patient • Objective o Patient will describe signs and symptoms of postoperative problems to report to health care provider. • Teaching Strategies o Give instruction sheet with contact information, including health care provider's telephone number, number of surgery center, and follow-up appointment date and time. Allow patient and family to ask questions. o Explain to family member the signs and symptoms of infection. o Explain name, dose, schedule, and purpose of medications and possible side effects. Provide printed drug information. o Explain activity restrictions, diet progression, wound care guidelines, and the signs of any associated problems. Provide instruction sheet with clear, focused explanations. • Evaluation o Have patient explain when and how to call health care provider with problems. o Have patient recite date for follow-up appointment. o Have patient and family member describe signs and symptoms of infection. o Have patient verbalize name of drug, dose, when to take, and common side effects. o Have patient demonstrate proper activity/movement and wound care. Med Calc – to include simple drop rates o Conversion within metric (grams-milligrams-micrograms) • 1 kg per 1000 grams, 1 gram per 1000 mg, 1 mg per 1000 mcg ▪ Conversion of pounds to kilograms • 2.2 lbs./ 1 Kg ▪ Milliliters in tsp, tbsp., ounce • Tsp= 5 mL, TBSP= 15 mL, & OZ= 30 mL, 1 L = 1000 mL ▪ Dosage calculation for tablets, liquid medication and simple injectable calculations • Tablets: 1200 mg, equals 3 tablets of 400 mg • Liquid medication: gtts must always be rounded to nearest whole #, example 13 gtts/min instead of 13.423 • Simple injectable: Usually round to the nearest tenth once you solve, example 5.2 mL instead of 5.196 ▪ Zero always leads, it NEVER follows! Example 0.9 mg & 90 mg [Show More]
Last updated: 1 year ago
Preview 1 out of 63 pages
Reviews( 0 )
Recommended For You
*NURSING> STUDY GUIDE > NUR2356 / NUR 2356 Multidimensional Care Exam 2 Final Exam Study Guide. Rasmussen College (All)
 Rasmussen College.png)
NUR2356 / NUR 2356 Multidimensional Care Exam 2 Final Exam Study Guide. Rasmussen College
NUR2356 / NUR 2356: Multidimensional Care Exam 2 / MDC 2 Final Exam Study Guide (Fall 2020) Rasmussen College
By Good grade , Uploaded: Sep 18, 2020
$10
*NURSING> STUDY GUIDE > NR599 / NR 599 Nursing Informatics for Advanced Practice - Comprehensive Final Exam Study Guide (Latest 2021 /2022):Chamberlain (All)
NR599 / NR 599 Nursing Informatics for Advanced Practice - Comprehensive Final Exam Study Guide (Latest 2021 /2022):Chamberlain
NR599 Nursing Informatics: Comprehensive Final Exam Study Guide
By quiz_bit , Uploaded: Feb 17, 2021
$10
*NURSING> STUDY GUIDE > NUR 2058 / NUR2058 Dimensions of Nursing Practice Final Exam Study Guide | Rated A |Rasmussen College (All)
NUR 2058 / NUR2058 Dimensions of Nursing Practice Final Exam Study Guide | Rated A |Rasmussen College
NUR 2058 / NUR2058 Dimensions of Nursing Practice Final Exam Study Guide | Rated A |Rasmussen College Nursing is activities that manipulates the environment and helps client achieve the balanced st...
By nurse_steph , Uploaded: Dec 05, 2020
$13.5
*NURSING> STUDY GUIDE > NR602 / NR 602 Primary Care of the Childbearing and Childrearing Family Practicum Final Exam Study Guide | Highly Rated | LATEST| Chamberlain College (All)
NR602 / NR 602 Primary Care of the Childbearing and Childrearing Family Practicum Final Exam Study Guide | Highly Rated | LATEST| Chamberlain College
NR602 / NR 602 Primary Care of the Childbearing and Childrearing Family Practicum Final Exam Study Guide | Highly Rated | LATEST| Chamberlain College Eye Disorders Strabismus- a defect in In oc...
By nurse_steph , Uploaded: Feb 07, 2021
$13
*NURSING> STUDY GUIDE > NR601 / NR 601 Primary Care of the Maturing and Aged Family Practicum Final Exam Study Guide | Week 5-7 | Highly Rated | LATEST | Chamberlain College of Nursing (All)
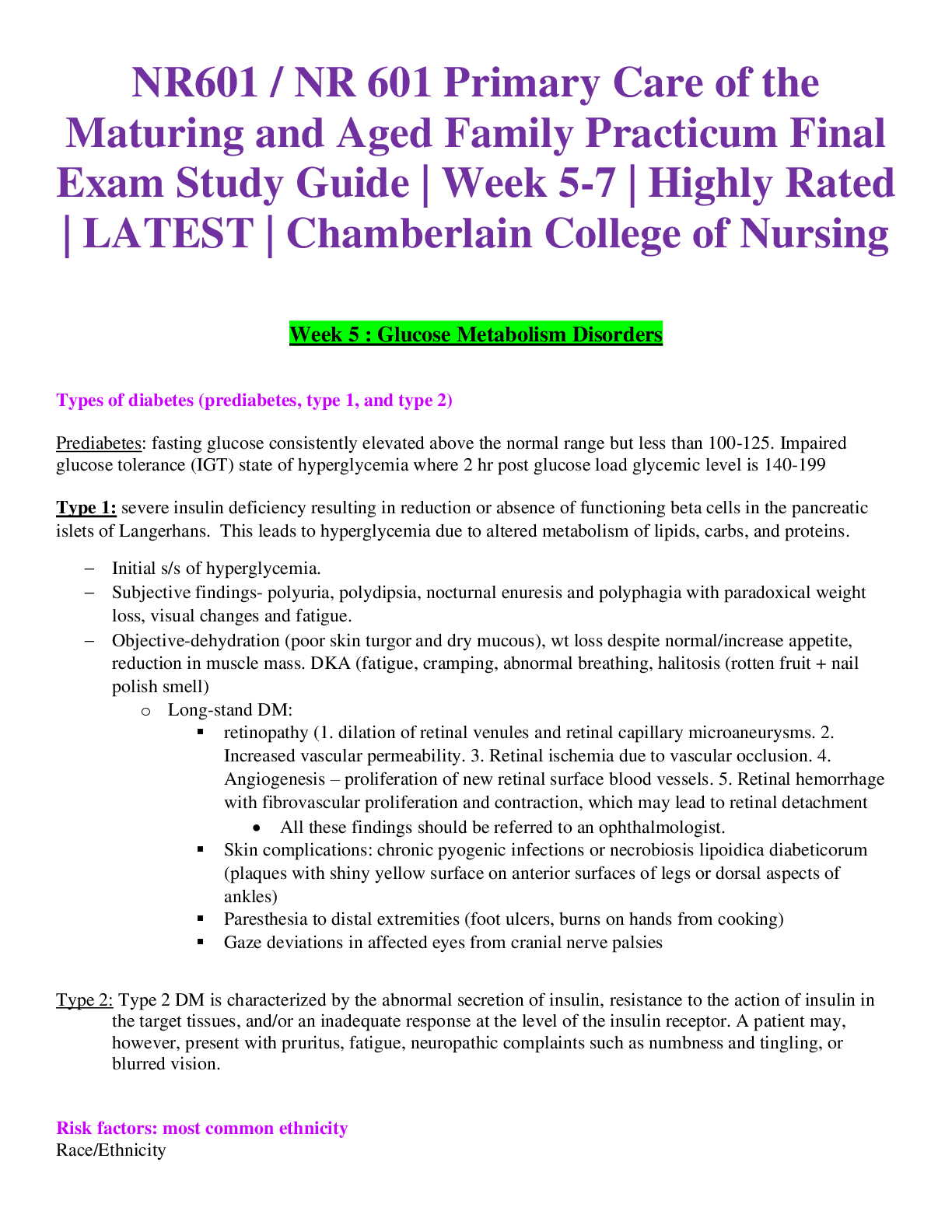
NR601 / NR 601 Primary Care of the Maturing and Aged Family Practicum Final Exam Study Guide | Week 5-7 | Highly Rated | LATEST | Chamberlain College of Nursing
NR601 / NR 601 Primary Care of the Maturing and Aged Family Practicum Final Exam Study Guide | Week 5-7 | Highly Rated | LATEST | Chamberlain College of Nursing Week 5 : Glucose Metabolism Disorders...
By nurse_steph , Uploaded: Feb 07, 2021
$13
*NURSING> STUDY GUIDE > NR511 / NR 511 Differential Diagnosis and Primary Care Practicum Final Exam Study Guide| Highly Rated | Latest | Chamberlain College (All)
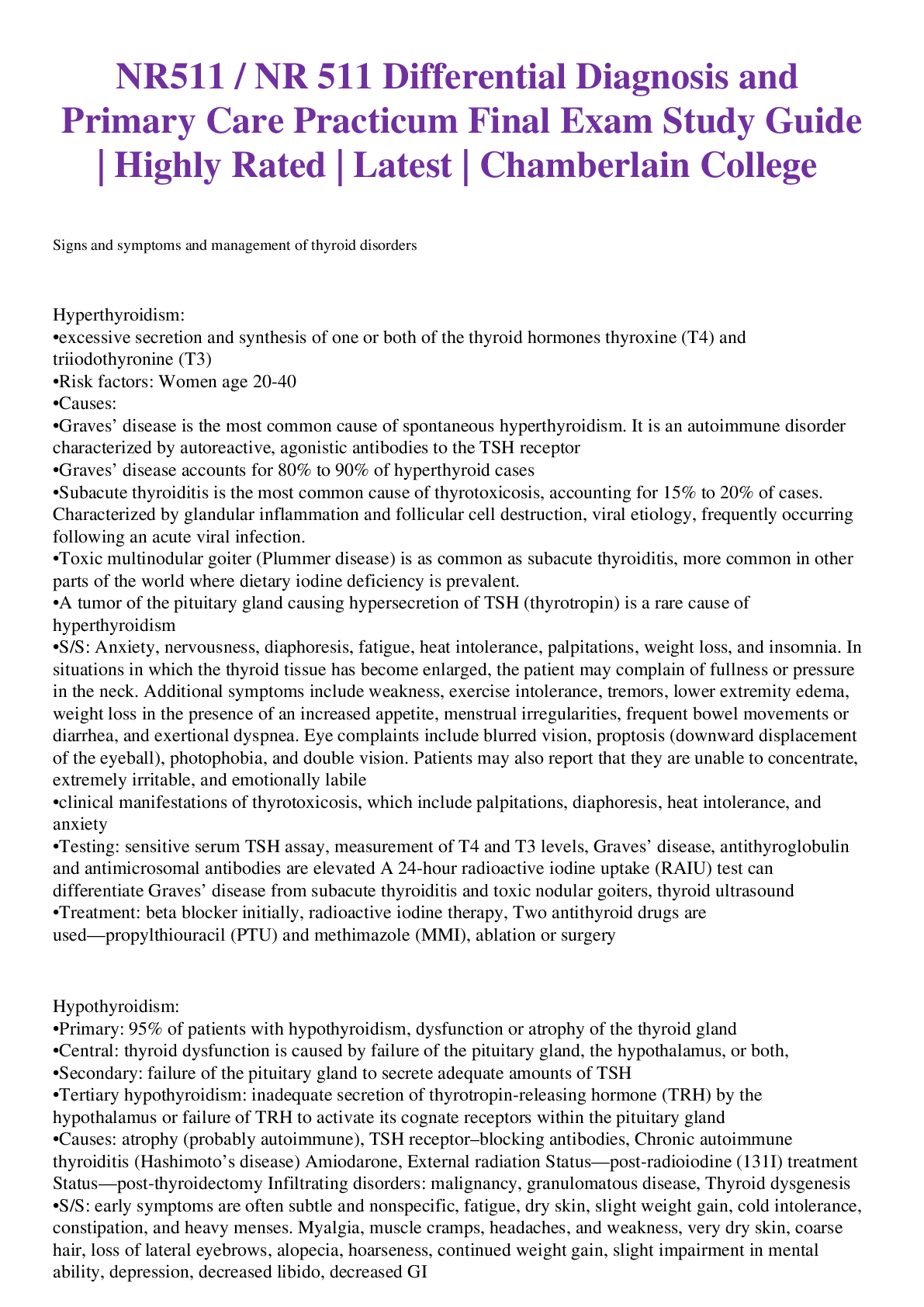
NR511 / NR 511 Differential Diagnosis and Primary Care Practicum Final Exam Study Guide| Highly Rated | Latest | Chamberlain College
NR511 / NR 511 Differential Diagnosis and Primary Care Practicum Final Exam Study Guide| Highly Rated | Latest | Chamberlain College 1. Signs and symptoms and management of thyroid disorders Hy...
By nurse_steph , Uploaded: Mar 02, 2021
$13
*NURSING> STUDY GUIDE > NSG6430 Final Exam South University NSG 6430 Final Exam Study Guide (All)
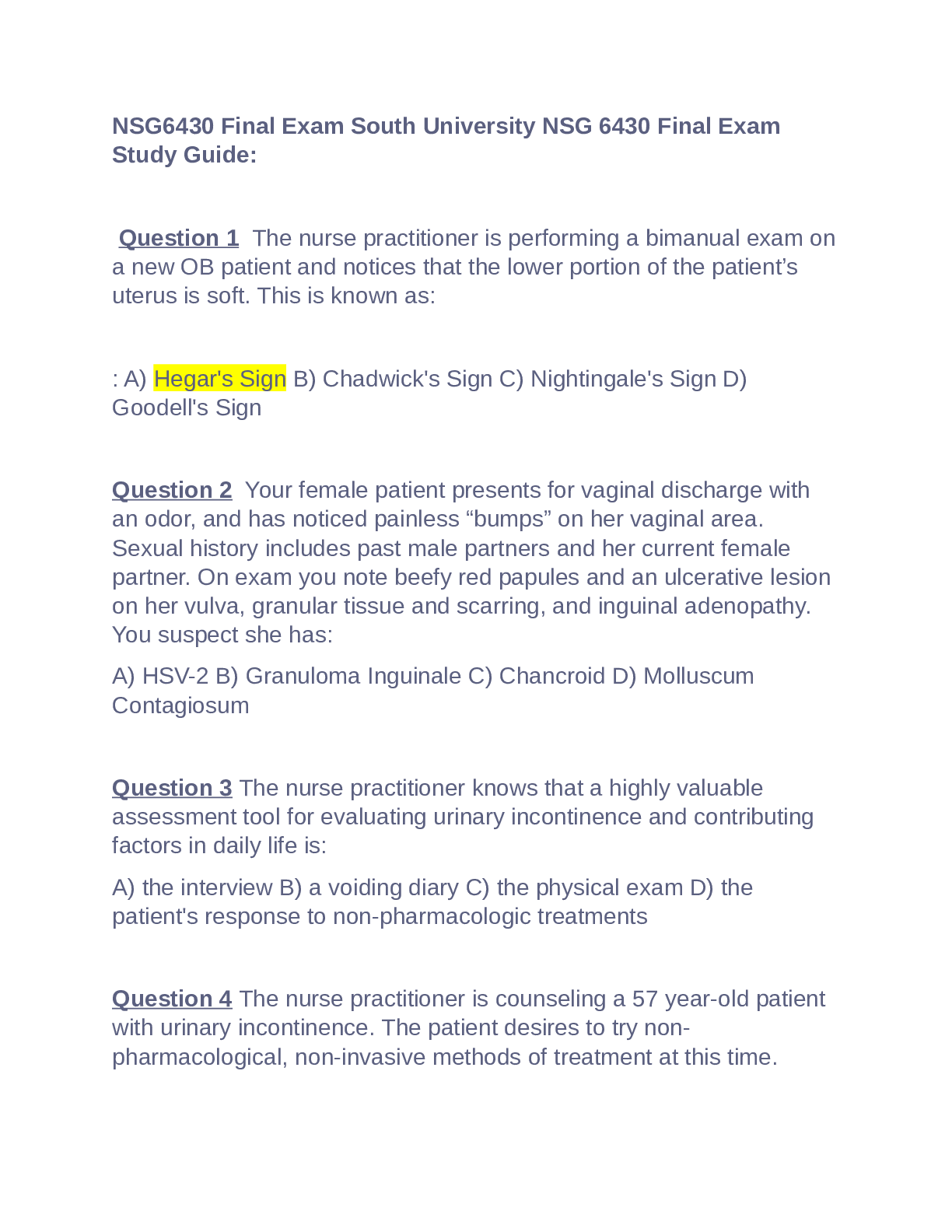
NSG6430 Final Exam South University NSG 6430 Final Exam Study Guide
NSG6430 Final Exam South University NSG 6430 Final ExamStudy Guide
By khalid11 , Uploaded: Sep 29, 2023
$13
*NURSING> STUDY GUIDE > NR 503 Week 8 Final Exam Study Guide; Chapter 2-4, 5-6, 7-8, 9-15, 16-20 (100% Verified Correct Solutions) (All)
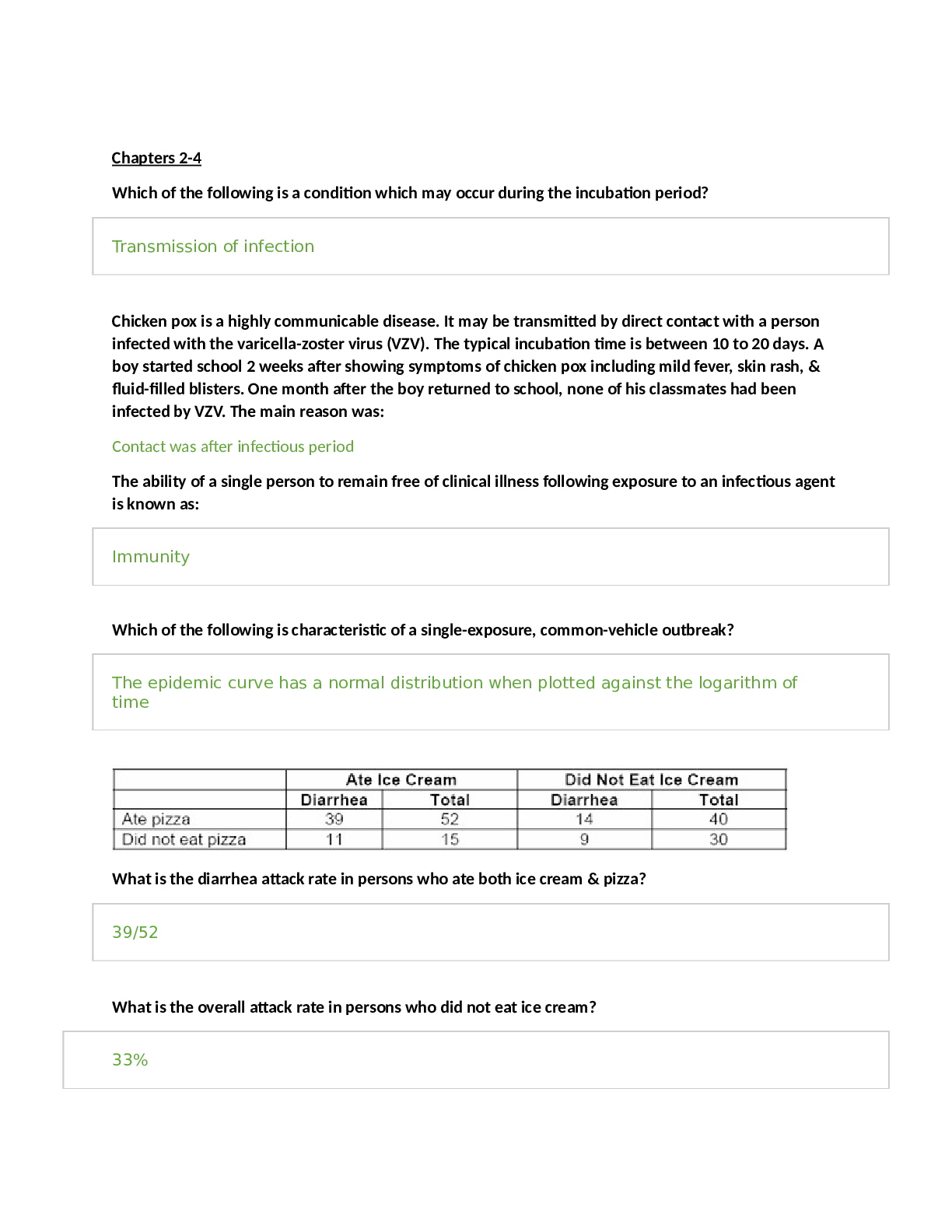
NR 503 Week 8 Final Exam Study Guide; Chapter 2-4, 5-6, 7-8, 9-15, 16-20 (100% Verified Correct Solutions)
NR 503 Week 8 Final Exam Study Guide; Chapter 2-4, 5-6, 7-8, 9-15, 16-20 Chapters 2-4 Which of the following is a condition which may occur during the incubation period? Chicken pox is a hi...
By A+ Solutions , Uploaded: Feb 02, 2022
$16
*NURSING> STUDY GUIDE > NR 503 Week 8 Final Exam Study Guide | Download For best results (All)
NR 503 Week 8 Final Exam Study Guide | Download For best results
NR 503 Week 8 Final Exam Study Guide | Download For best results
By A+ Solutions , Uploaded: Feb 02, 2022
$10
*NURSING> STUDY GUIDE > NR601 / NR-601 Final Exam Study Guide Material (Latest 2022 / 2023): Primary Care of the Maturing & Aged Family Practicum - Chamberlain (All)
NR601 / NR-601 Final Exam Study Guide Material (Latest 2022 / 2023): Primary Care of the Maturing & Aged Family Practicum - Chamberlain
NR601 / NR-601 Final Exam Study Guide Material (Latest 2022 / 2023): Primary Care of the Maturing & Aged Family Practicum - Chamberlain
By kofee , Uploaded: Feb 01, 2022
$16
Document information
Connected school, study & course
About the document
Uploaded On
Sep 21, 2021
Number of pages
63
Written in
Additional information
This document has been written for:
Uploaded
Sep 21, 2021
Downloads
0
Views
39






