*NURSING > STUDY GUIDE > Chamberlain College of NursingNR 602 NRNR 602 Final Study Guide.ALL FINAL TOPICS (All)
Chamberlain College of NursingNR 602 NRNR 602 Final Study Guide.ALL FINAL TOPICS
Document Content and Description Below
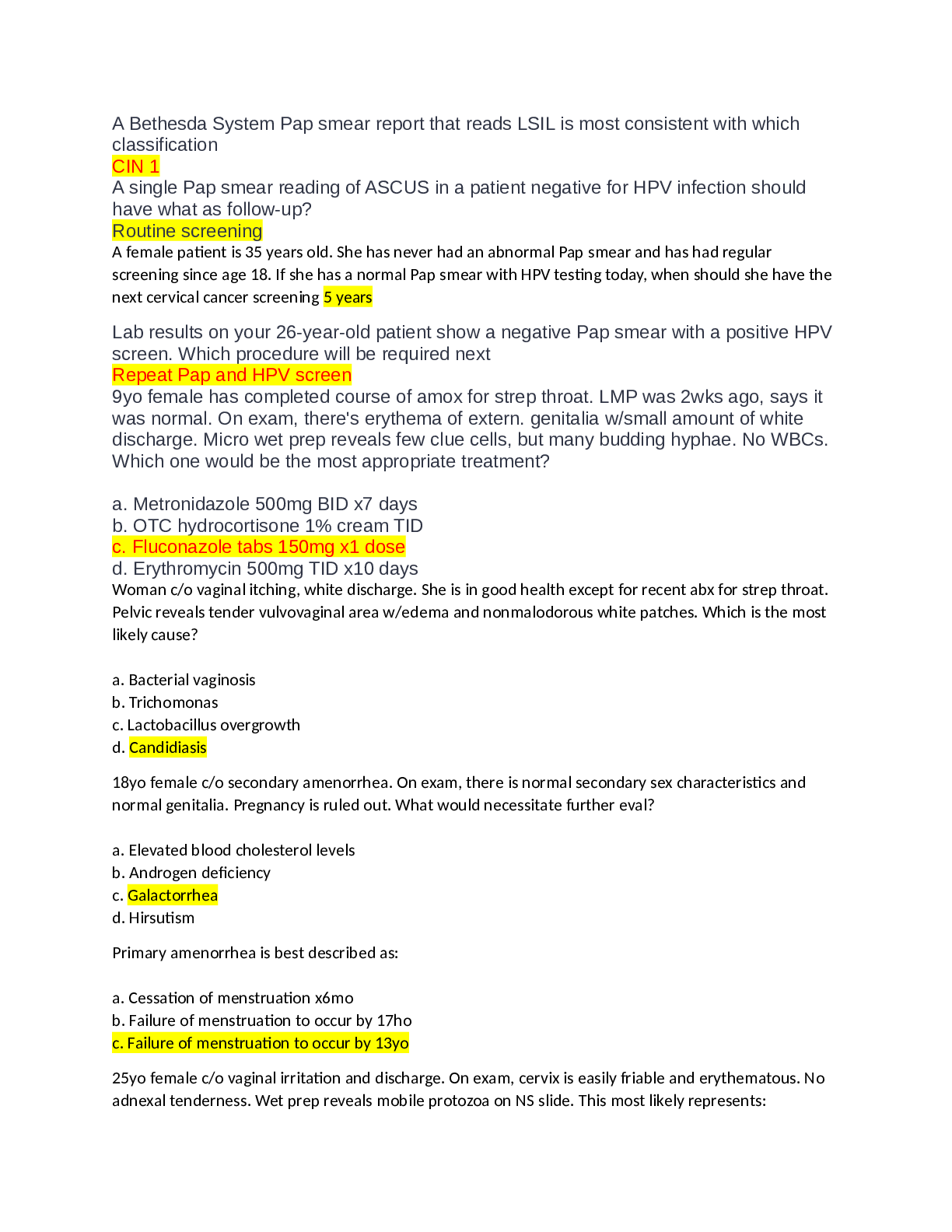
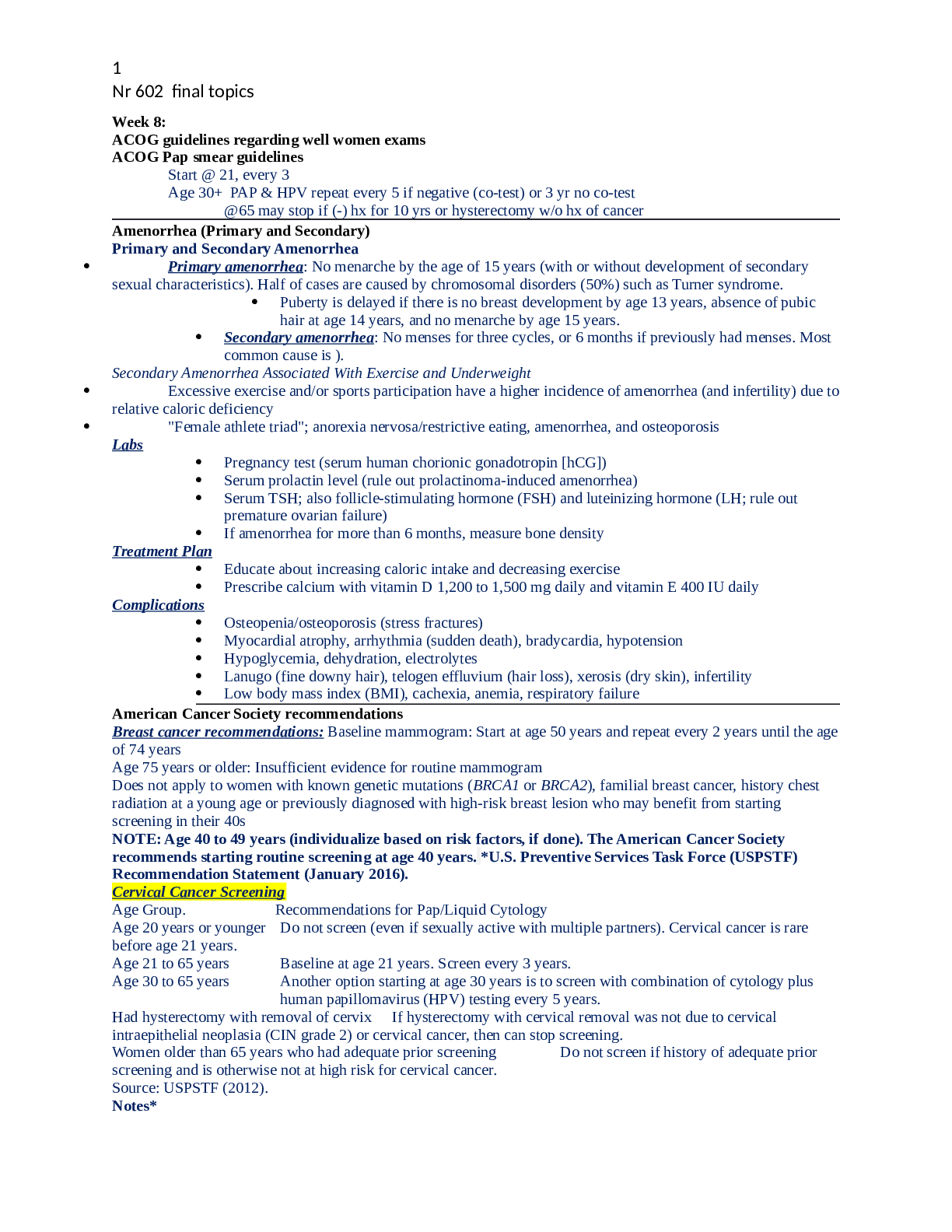
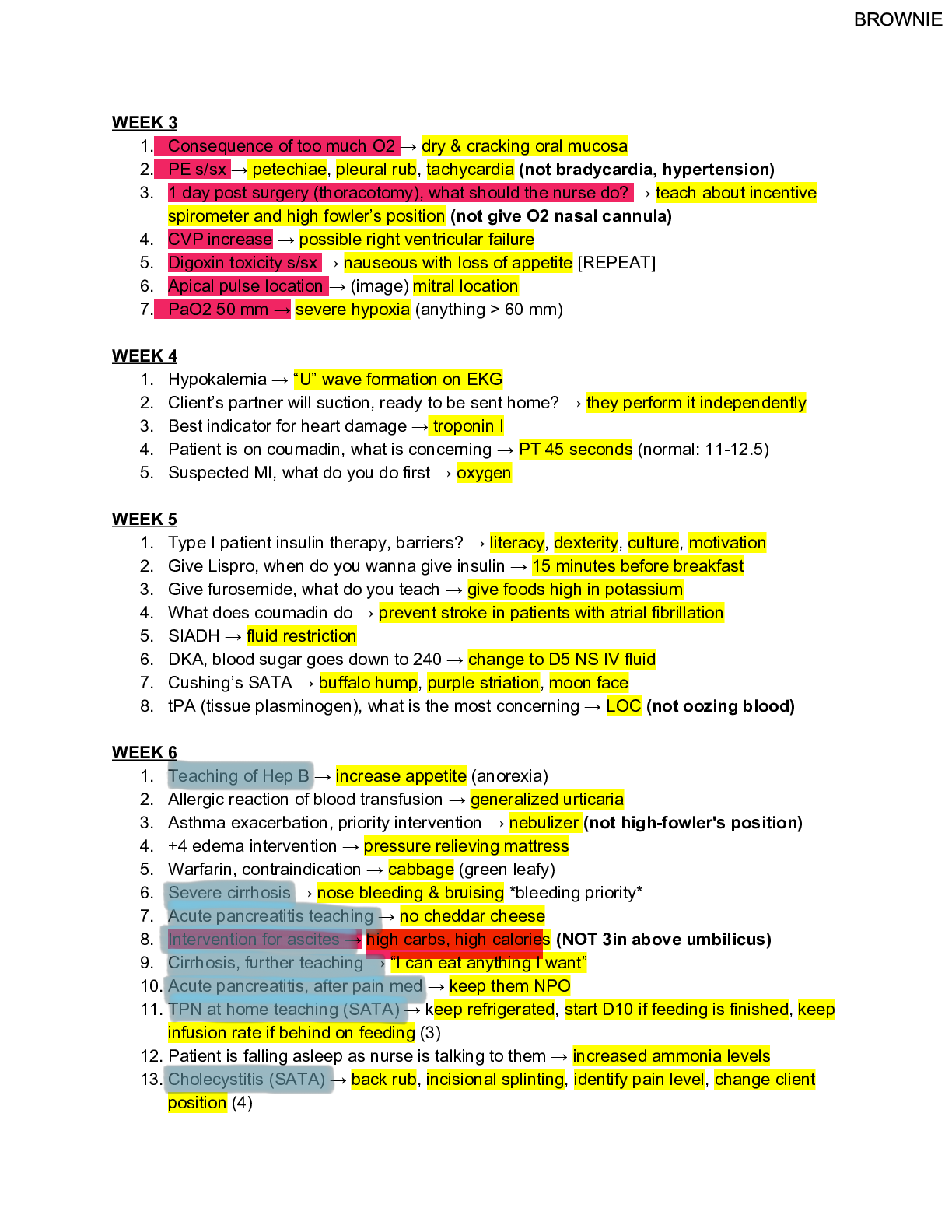
Nr 602 final topics Week 8: ACOG guidelines regarding well women exams ACOG Pap smear guidelines Start @ 21, every 3 Age 30+ PAP & HPV repeat every 5 if negative (co-test) or 3 yr no co-test @65... may stop if (-) hx for 10 yrs or hysterectomy w/o hx of cancer Amenorrhea (Primary and Secondary) Primary and Secondary Amenorrhea Primary amenorrhea: No menarche by the age of 15 years (with or without development of secondary sexual characteristics). Half of cases are caused by chromosomal disorders (50%) such as Turner syndrome. Puberty is delayed if there is no breast development by age 13 years, absence of pubic hair at age 14 years, and no menarche by age 15 years. Secondary amenorrhea: No menses for three cycles, or 6 months if previously had menses. Most common cause is ). Secondary Amenorrhea Associated With Exercise and Underweight Excessive exercise and/or sports participation have a higher incidence of amenorrhea (and infertility) due to relative caloric deficiency "Female athlete triad"; anorexia nervosa/restrictive eating, amenorrhea, and osteoporosis Labs Pregnancy test (serum human chorionic gonadotropin [hCG]) Serum prolactin level (rule out prolactinoma-induced amenorrhea) Serum TSH; also follicle-stimulating hormone (FSH) and luteinizing hormone (LH; rule out premature ovarian failure) If amenorrhea for more than 6 months, measure bone density Treatment Plan Educate about increasing caloric intake and decreasing exercise Prescribe calcium with vitamin D 1,200 to 1,500 mg daily and vitamin E 400 IU daily Complications Osteopenia/osteoporosis (stress fractures) Myocardial atrophy, arrhythmia (sudden death), bradycardia, hypotension Hypoglycemia, dehydration, electrolytes Lanugo (fine downy hair), telogen effluvium (hair loss), xerosis (dry skin), infertility Low body mass index (BMI), cachexia, anemia, respiratory failure American Cancer Society recommendations Breast cancer recommendations: Baseline mammogram: Start at age 50 years and repeat every 2 years until the age of 74 years Age 75 years or older: Insufficient evidence for routine mammogram Does not apply to women with known genetic mutations (BRCA1 or BRCA2), familial breast cancer, history chest radiation at a young age or previously diagnosed with high-risk breast lesion who may benefit from starting screening in their 40s NOTE: Age 40 to 49 years (individualize based on risk factors, if done). The American Cancer Society recommends starting routine screening at age 40 years. *U.S. Preventive Services Task Force (USPSTF) Recommendation Statement (January 2016). Cervical Cancer Screening Age Group. Recommendations for Pap/Liquid Cytology Age 20 years or younger Do not screen (even if sexually active with multiple partners). Cervical cancer is rare before age 21 years. Age 21 to 65 years Baseline at age 21 years. Screen every 3 years. Age 30 to 65 years Another option starting at age 30 years is to screen with combination of cytology plus human papillomavirus (HPV) testing every 5 years. Had hysterectomy with removal of cervix If hysterectomy with cervical removal was not due to cervical intraepithelial neoplasia (CIN grade 2) or cervical cancer, then can stop screening. Women older than 65 years who had adequate prior screening Do not screen if history of adequate prior screening and is otherwise not at high risk for cervical cancer. Source: USPSTF (2012). Notes* 2 Nr 602 final topics These recommendations do not apply to women who are immunocompromised (i.e., Hiv infection), had in utero exposure to diethylstilbestrol (DES), or have a diagnosis of high-grade precancerous cervical lesion or cervical cancer. *USPSTF Screening Recommendations for Cervical Cancer (July 2015). Ovarian cancer- ACS RECOMMENDATIONS - The typical patient is a middle-aged or older woman with vague symptoms of abdominal bloating and discomfort, low-back pain, pelvic pain, and changes in bowel habits. Look for family history of having two or more first- or second-degree relatives with a history of ovarian cancer or a combination of ovarian cancer, especially women of Ashkenazi Jewish ethnicity with a first-degree relative (or second-degree relatives on the same side of the family) with breast or ovarian cancer (American Cancer Society, U.S. Preventive Services Task Force [USPSTF], 2012). Very-high-risk women with suspected BRCA 1/BRCA 2 mutations should be referred for genetic counseling pre- and posttest. The screening starts at age 30 years (or 5 to 10 years before the earliest age of first diagnosis of ovarian cancer in a family member). Androgen insensitivity/resistance syndrome description/features Inability of body to respond properly to male sex hormone, produced during pregnancy Sx- genetic make up is male but physical traits of woman Vagina but no cervix, inguinal hernia w/ testes, normal female breasts, testes in abd or other place of body ASCUS/HSIL results from Paper Test Report (atypical squamous cell undetermined significance) from CDC--- For non-pregnant women between 25 and 65 years of age with ASCUS cytology who have not had HPV co-testing already, HPV testing is the preferred next step (high-risk HPV testing only). With a negative HPV test (either on cotest or after cytology), repeat co-testing every three years is recommended. Normal Pap and Negative HPV Rescreen in 5 years. Normal Pap and Positive HPV Repeat co-test in one year or do HPV DNA typing now (see ASCCP guidelines above). ASCUS Pap, No HPV Test Repeat cytology in one year or do HPV test now (see ASCCP guidelines above). ASCUS Pap and Negative HPV LSIL Pap and Negative HPV Repeat Pap and co-test at interval as per ASCCP guidelines. ASCUS Pap and Positive HPV LSIL Pap and Positive or Unknown HPV ASC-H Pap HSIL Pap Colposcopy and/or referral to gynecologist. Bartholin glands and cysts If a Bartholin duct gets blocked, fluid builds up in the gland. The blocked gland is called a Bartholin gland cyst Bartholin Cyst: common at what locations? 4 and 8 o'clock Bartholin cyst: MC org? E. Coli 3 Nr 602 final topics Bartholin Cyst: txI&D packing, marsupilization Bartholin cyst: tx duration of word catheter placement? 4-6 wks Where are Bartholin's glands and ducts situated? Under the labia minor What do they secrete?- Thin lubricating mucus during sexual excitation How does a cyst form?- If the duct blocks How does an abscess form? If the cyst become infected --> hugely swollen, red labium Investigations- Exclude gonococcus Management- Permanent drainage by marsupialization or by balloon catheter insertion BMI BMI Weight Status Below 18.5 Underweight 18.5 – 24.9 Normal or Healthy Weight 25.0 – 29.9 Overweight 30.0 and Above Obese CDC recommendations regarding STDs and PID CDC FOR STD’s Routine annual screening of all sexually active females aged 25 years or younger for Chlamydia trachomatis and gonorrhea If infected, retest for chlamydia and gonorrhea 3 months after treatment (to check for reinfection, not for test-of-cure) Annual testing for syphilis, chlamydia, and gonorrhea in persons with Hiv infection Minors do not need parental consent if the clinic visit is related to testing or treating STDs and birth control; no state requires parental consent for STD care Men Who Have Sex With Men (MSM) Annual screening for chlamydia and gonorrhea at sites of contact (urethra, rectum) regardless of condom use. Screen every 3 to 6 months if at increased risk. Annual screening recommended for pharyngeal gonorrhea (throat). Screen every 3 to 6 months if at increased risk. Annual testing recommended for Hiv, syphilis, and for HBsAg. Retest more frequently if at risk. Pregnant Women Screen pregnant women for Hiv, chlamydia, gonorrhea, syphilis, and hepatitis B surface antigen (HBsAg) at first prenatal visit. Pregnant women treated for chlamydia and/or gonorrhea should have a test-of-cure within 3 to 4 weeks after treatment. Retest at 3 months for chlamydia and gonorrhea (check for reinfection, not test of cure). CDC FOR PID 72 hr post tx, chlamydia annual screen <25 [PID] – presumptive tx for PID should be given to sexually active women & @ risk women experiencing pelvic/lower abd pain and no cause for illness and one or more of the following: cervical motion tenderness, uterine or adnexal tenderness Criteria to dx PID: endometrial bx, transvag US, laprascopy Tx- Recommended Intramuscular/Oral Regimens Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH* or WITHOUT Metronidazole 500 mg orally twice a day for 14 days. [Show More]
Last updated: 1 year ago
Preview 1 out of 15 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 29, 2021
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Sep 29, 2021
Downloads
0
Views
99

.png)


.png)