*NURSING > SHADOW HEALTH > SH Focused Exam Chest Pain Brian Foster (Pro tip, Brian Foster, Shadow Health Chest Pain 113) (All)
SH Focused Exam Chest Pain Brian Foster (Pro tip, Brian Foster, Shadow Health Chest Pain 113)
Document Content and Description Below
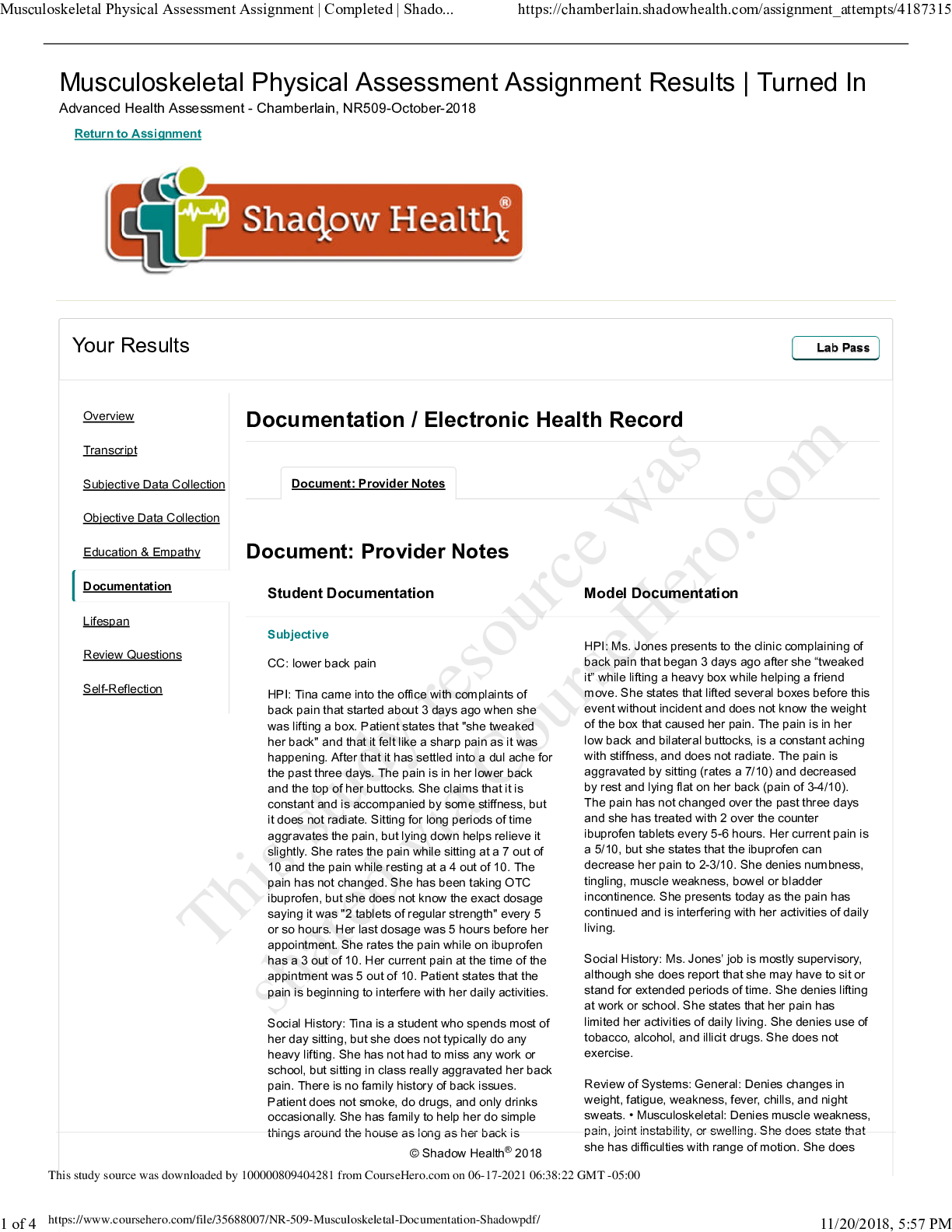
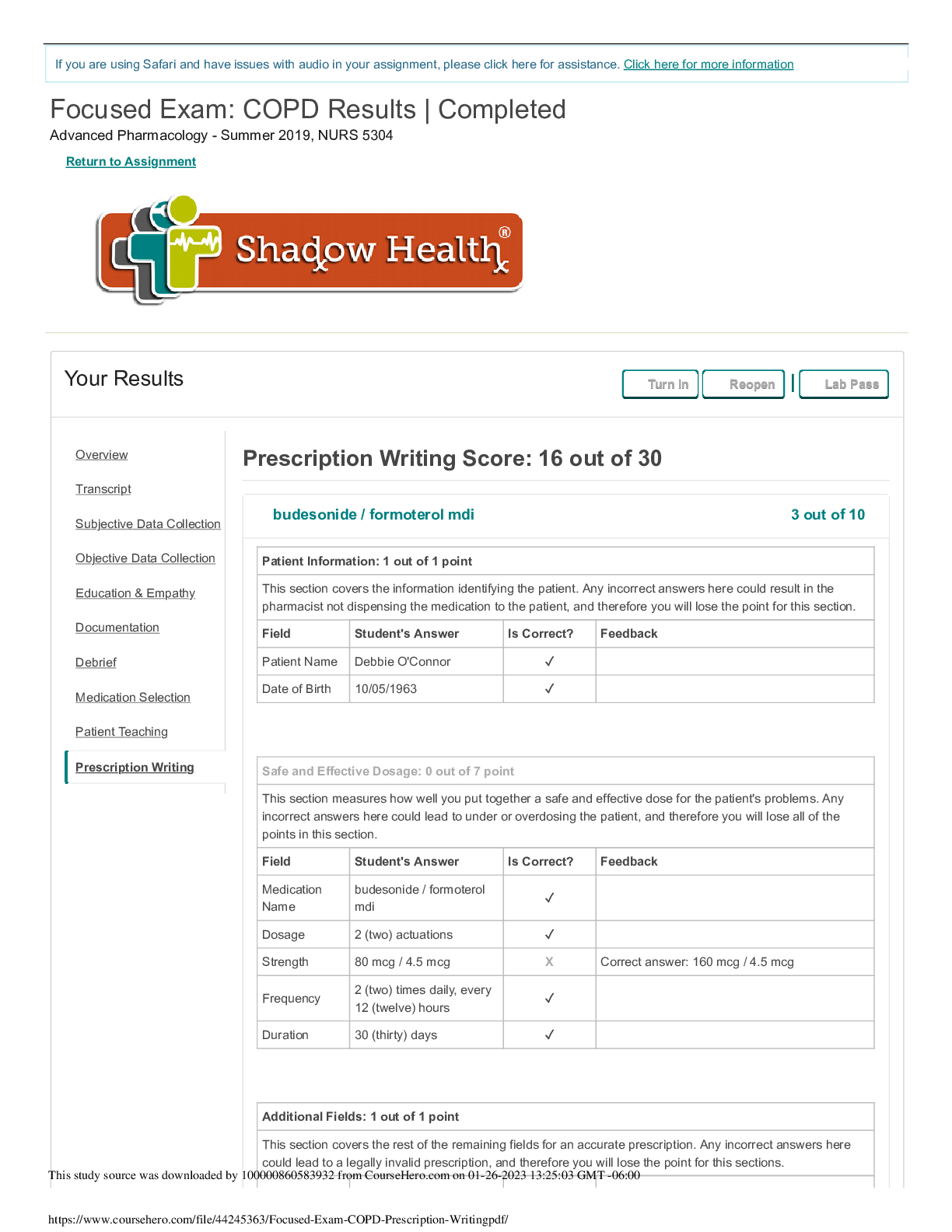
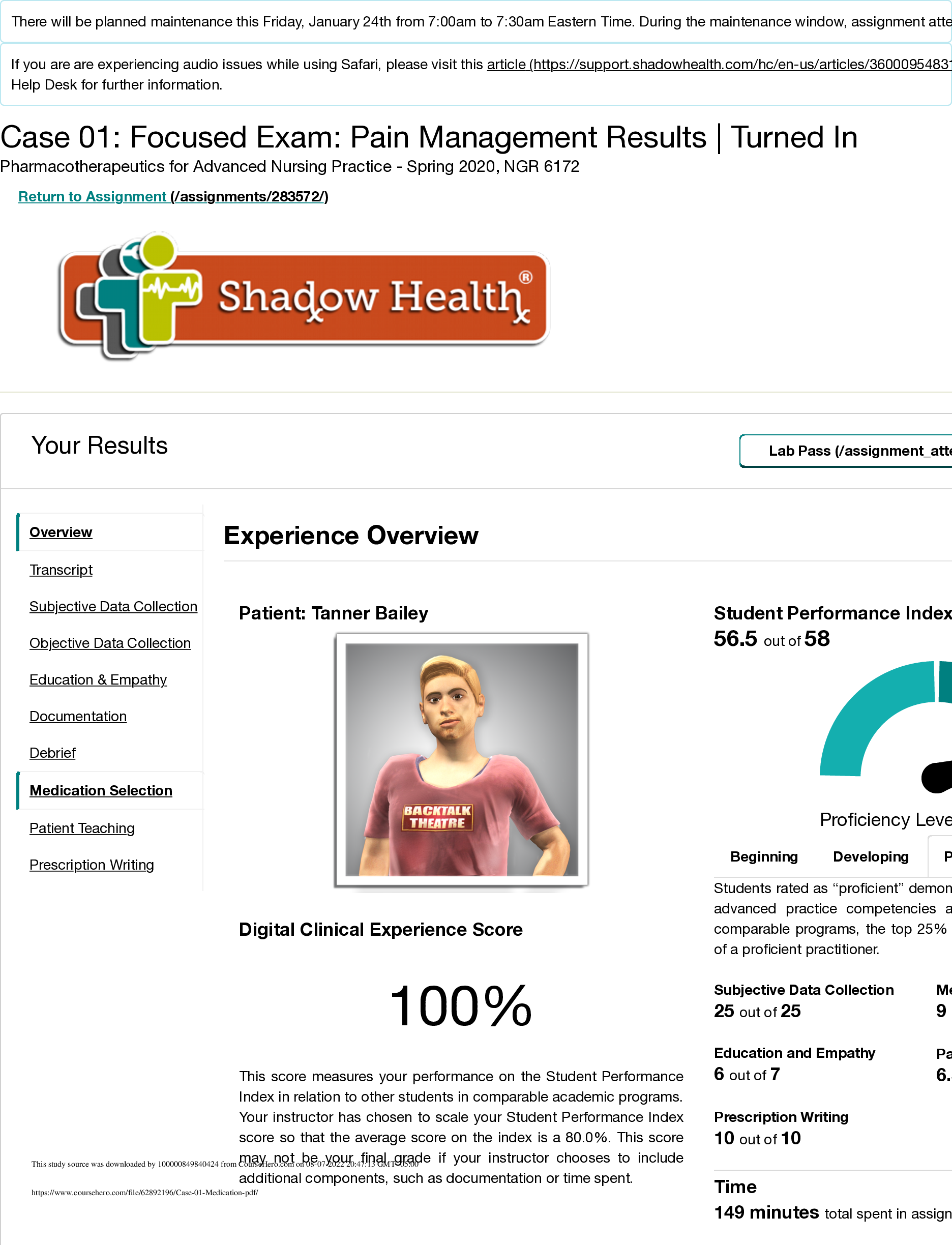
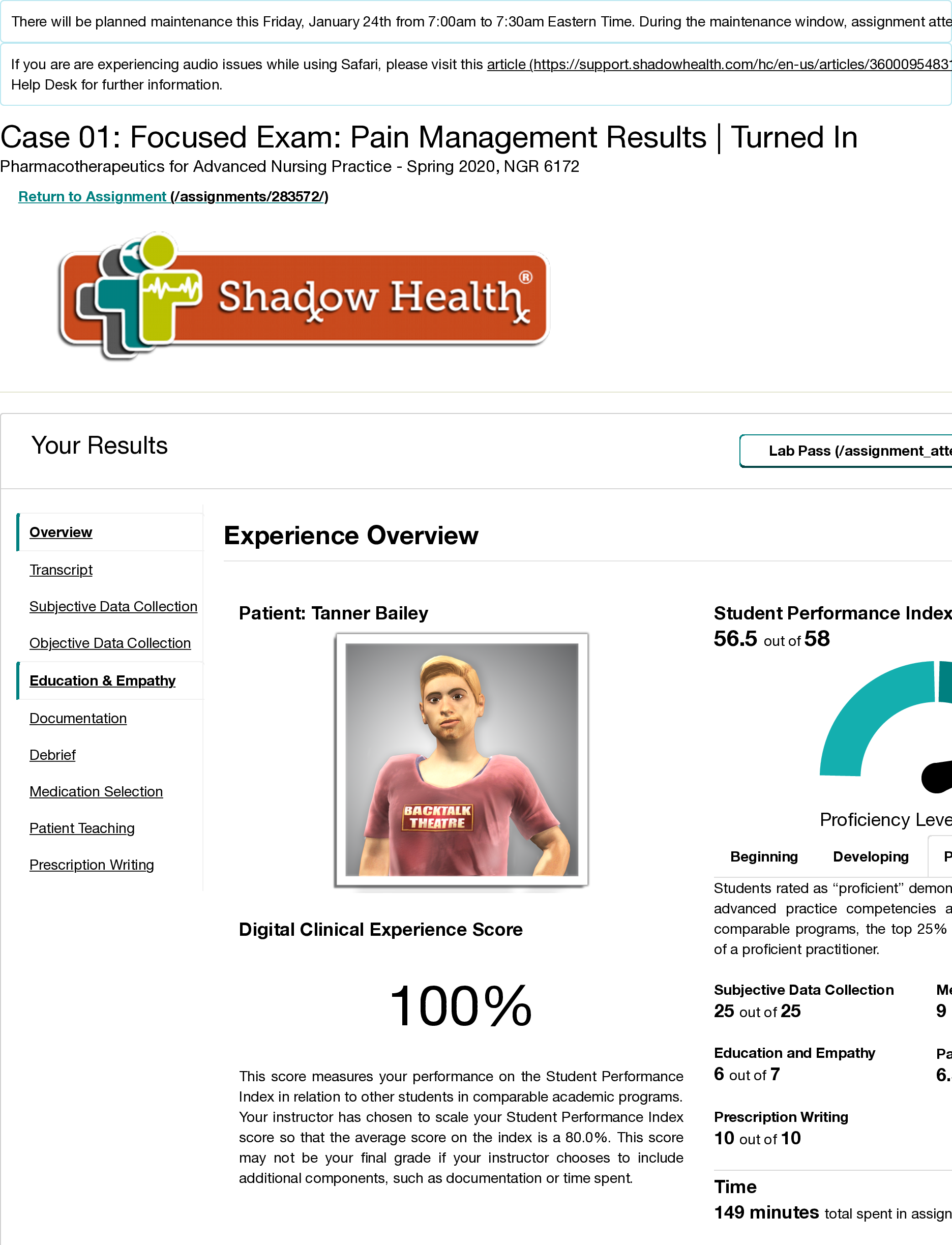
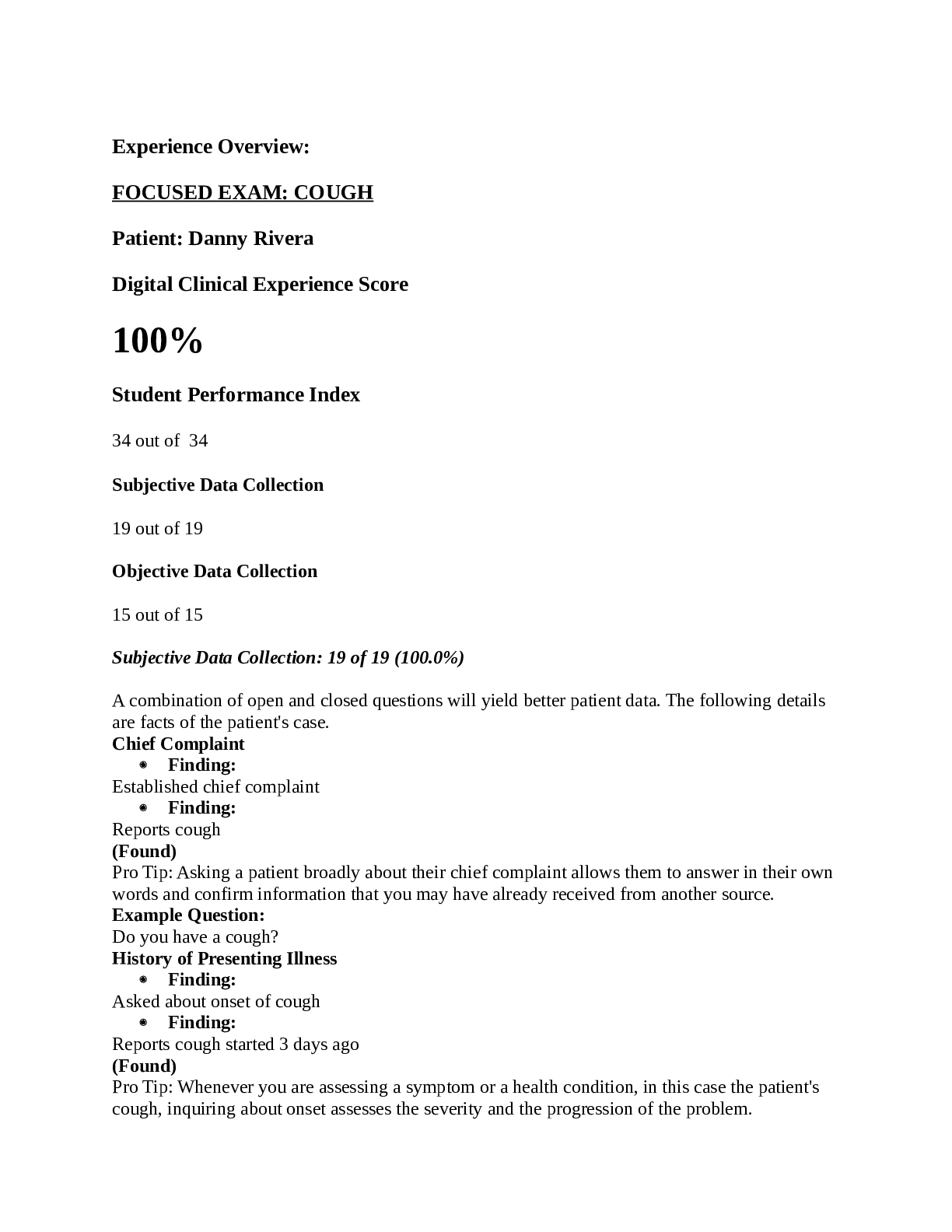
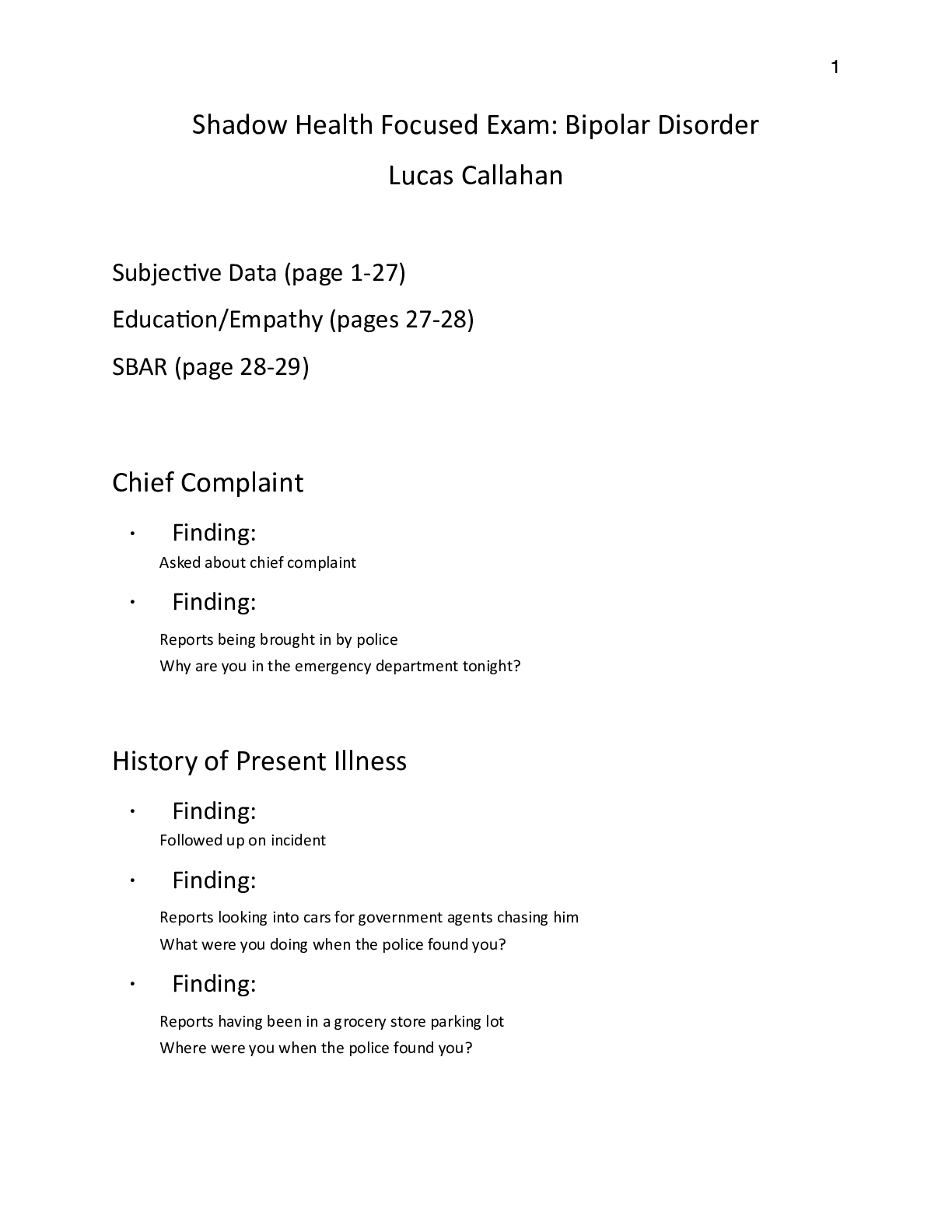
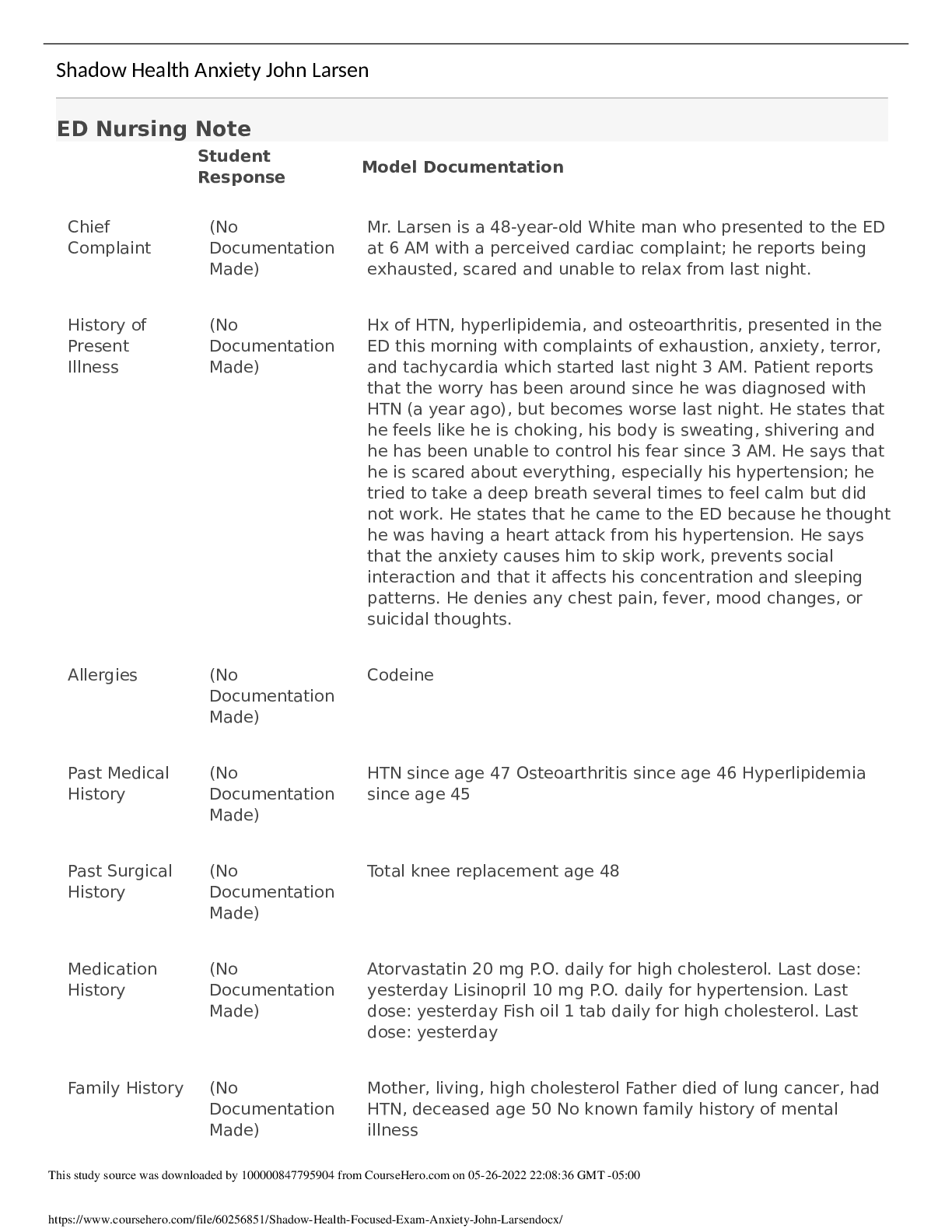
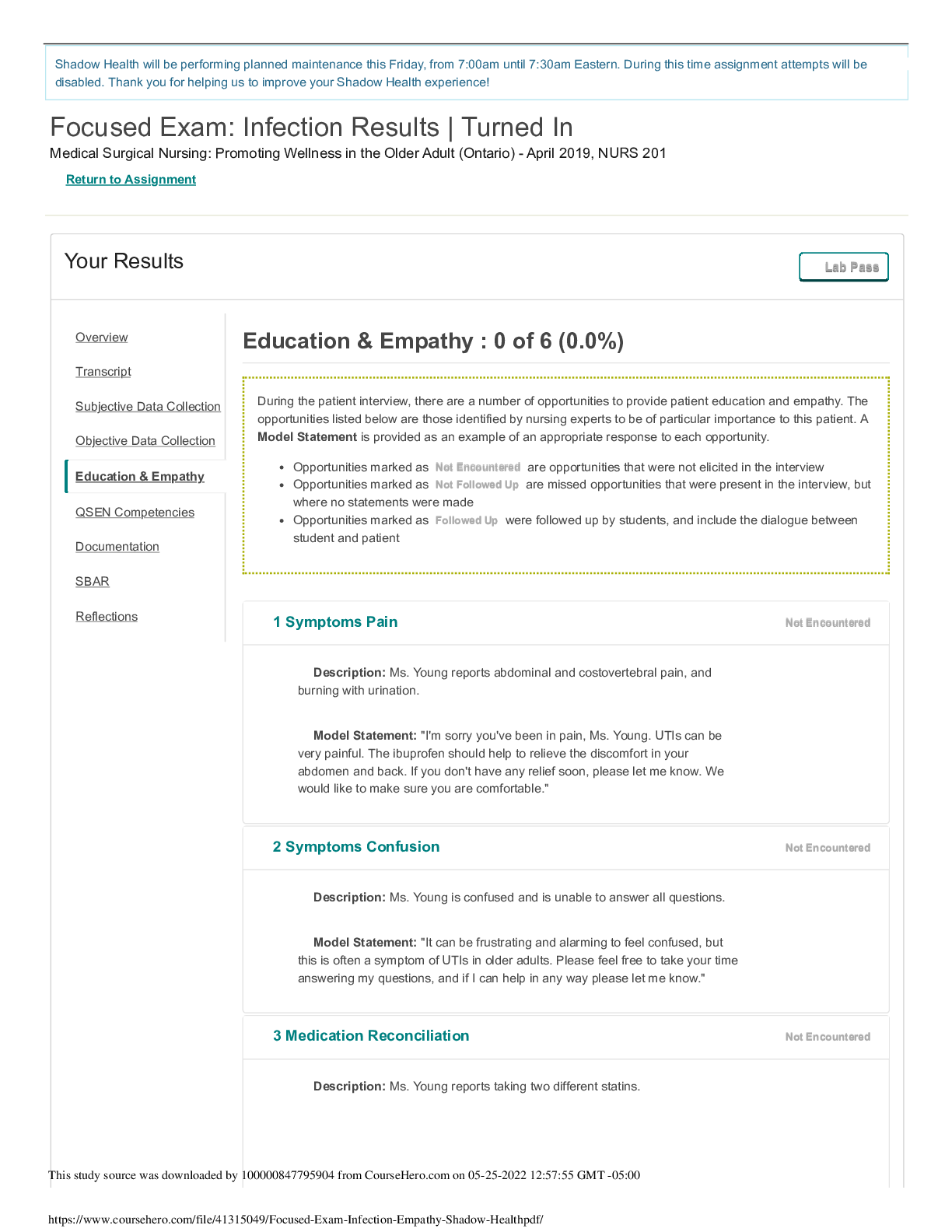
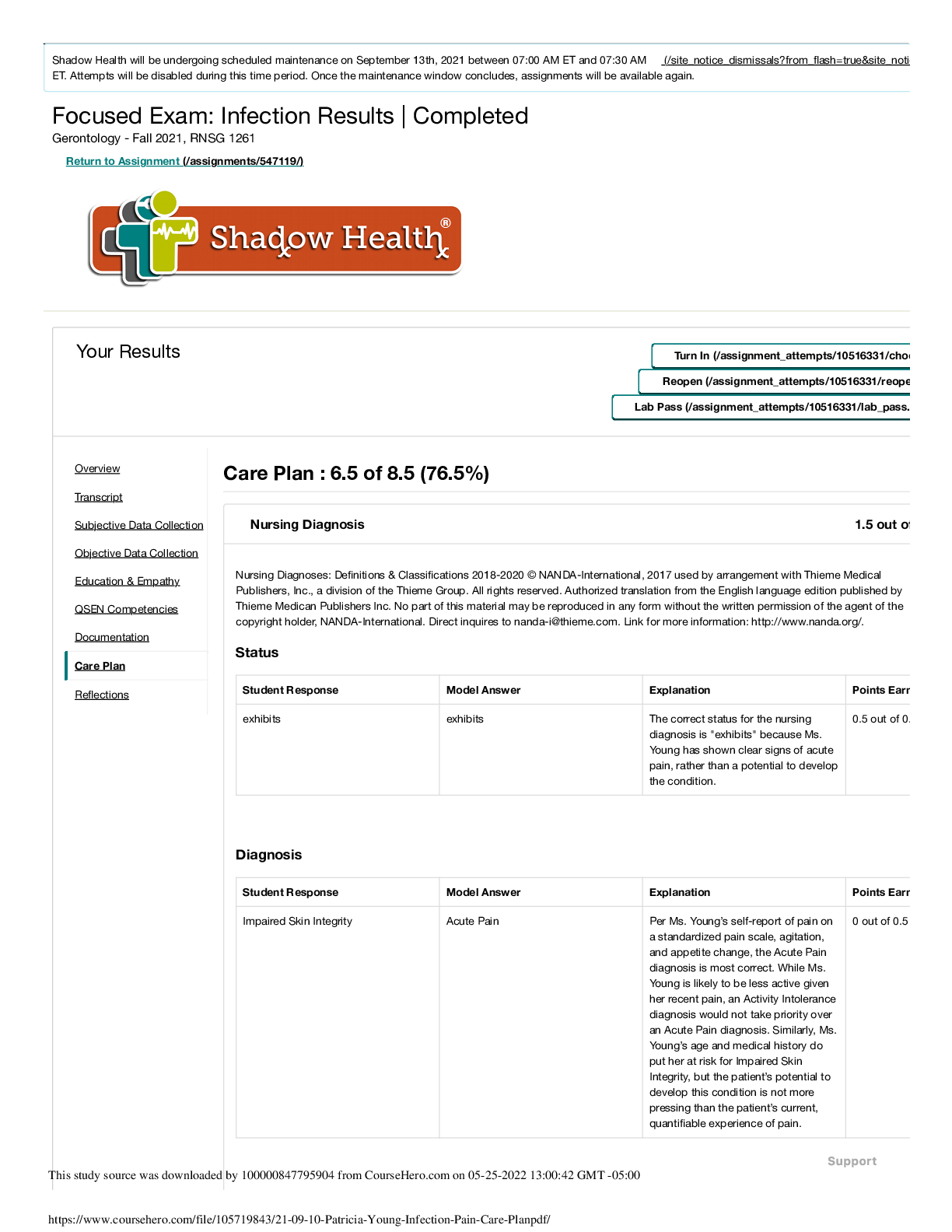
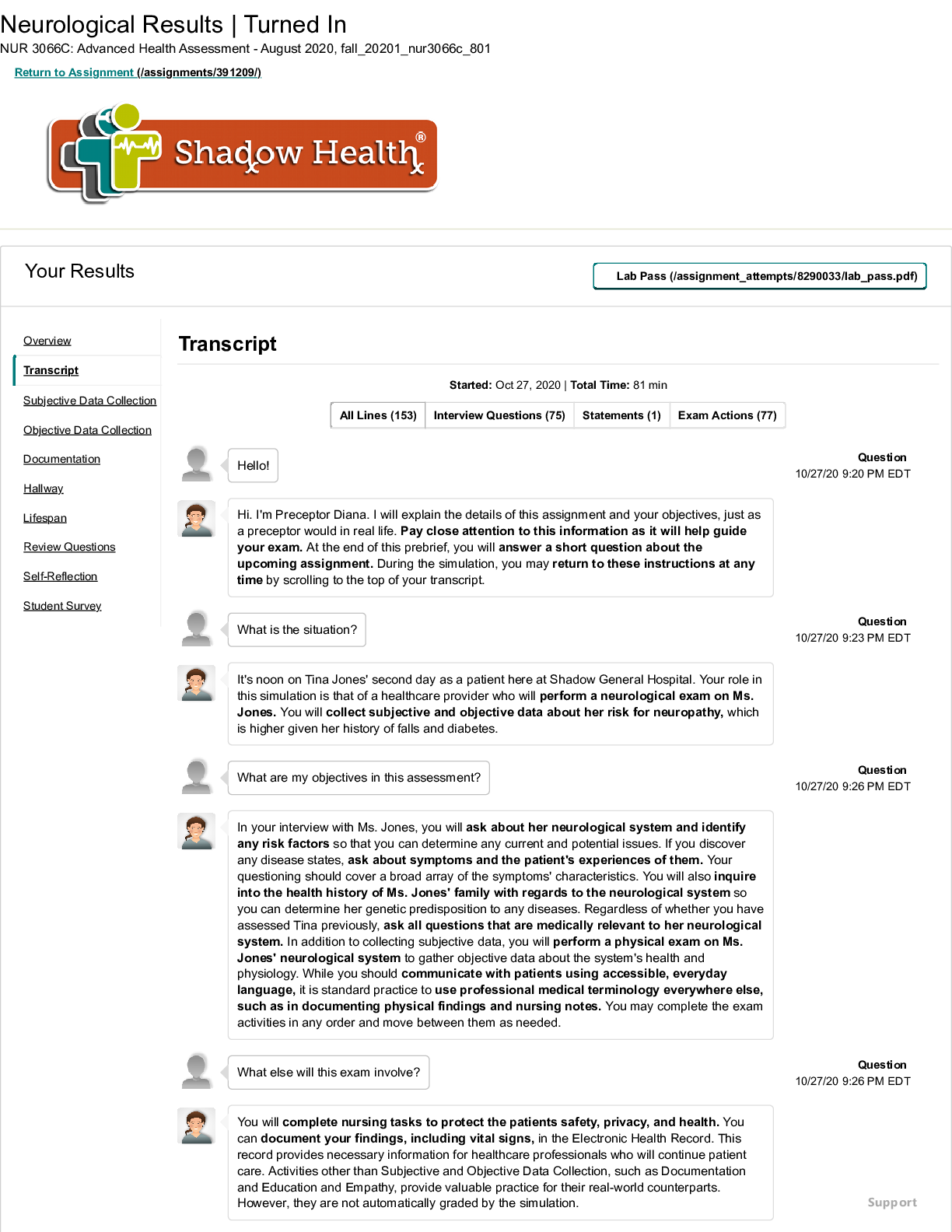
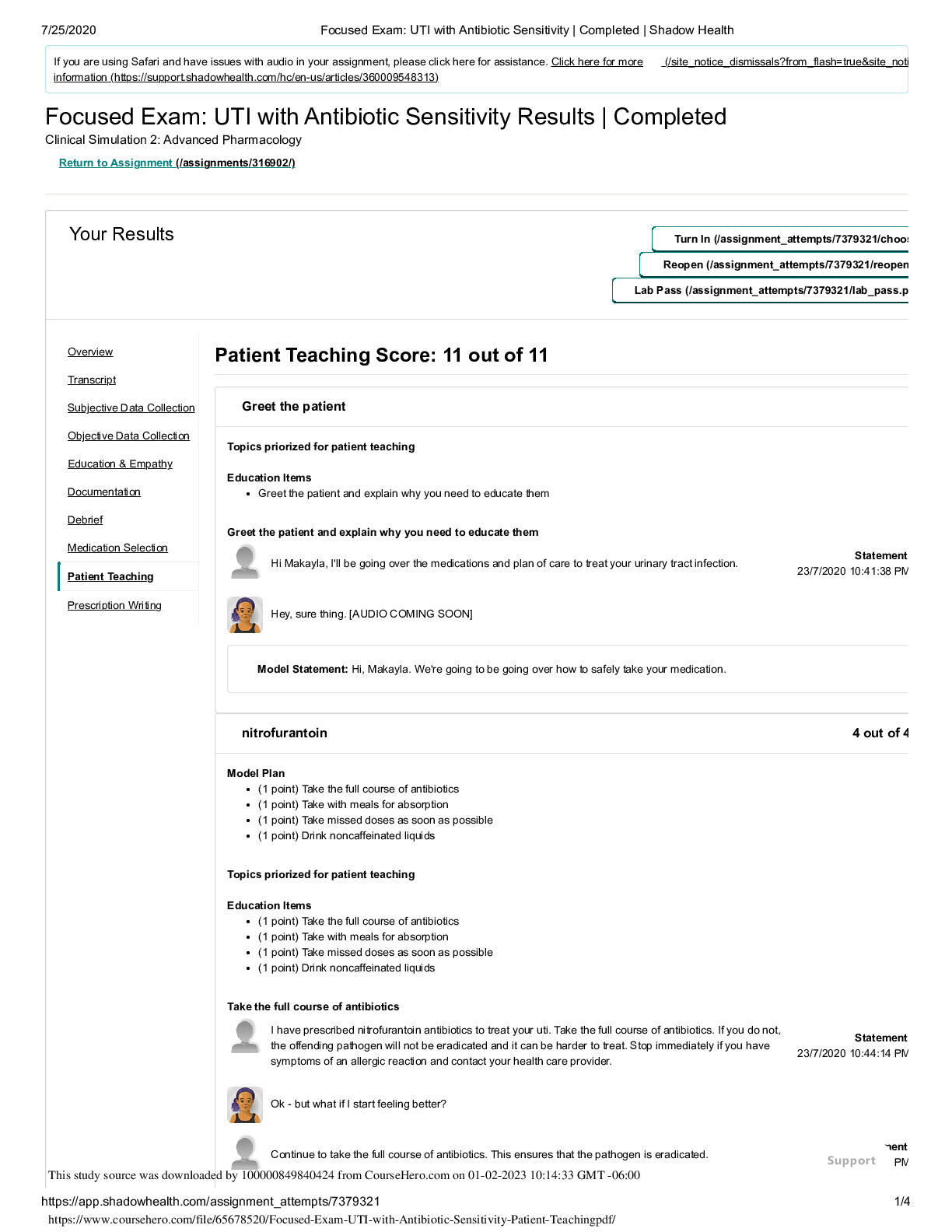
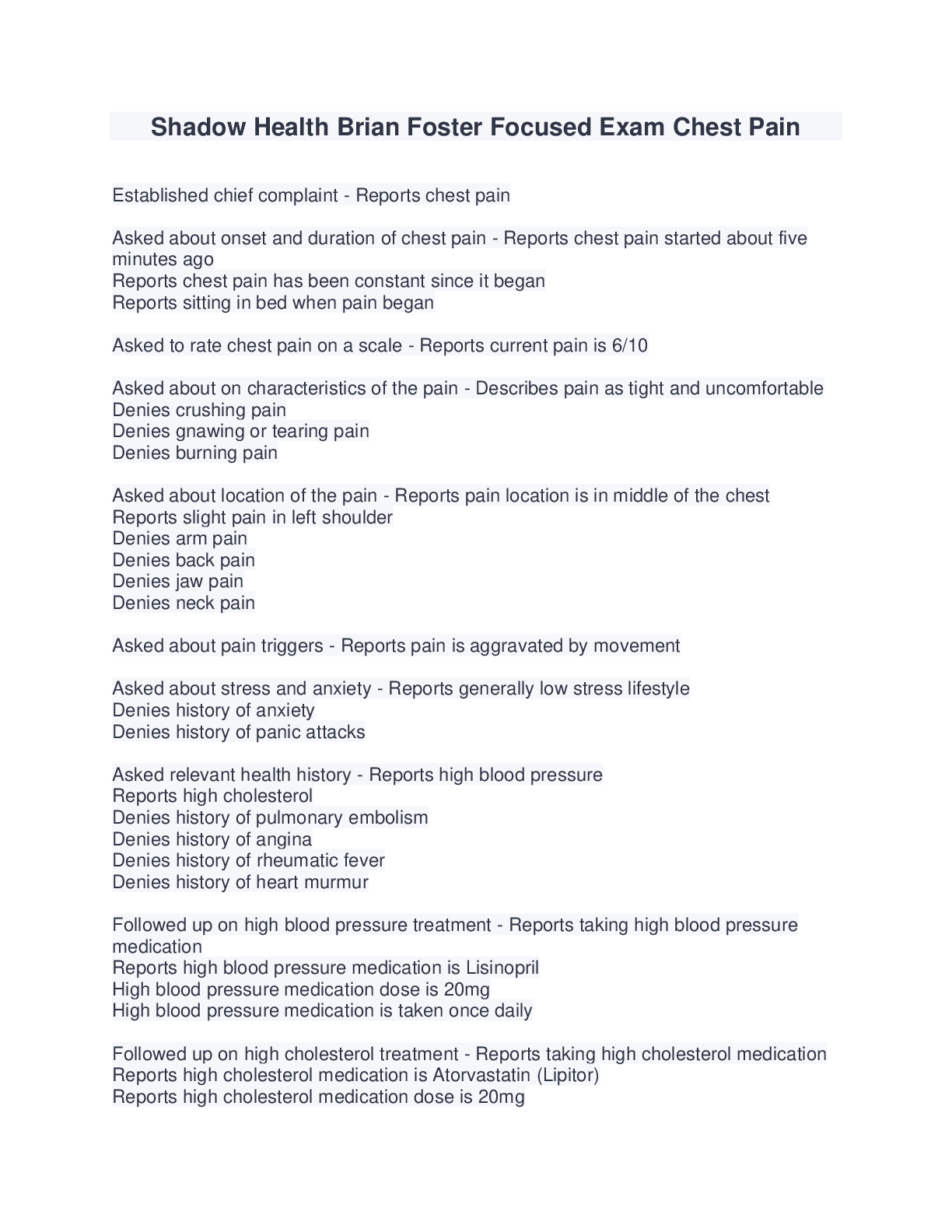
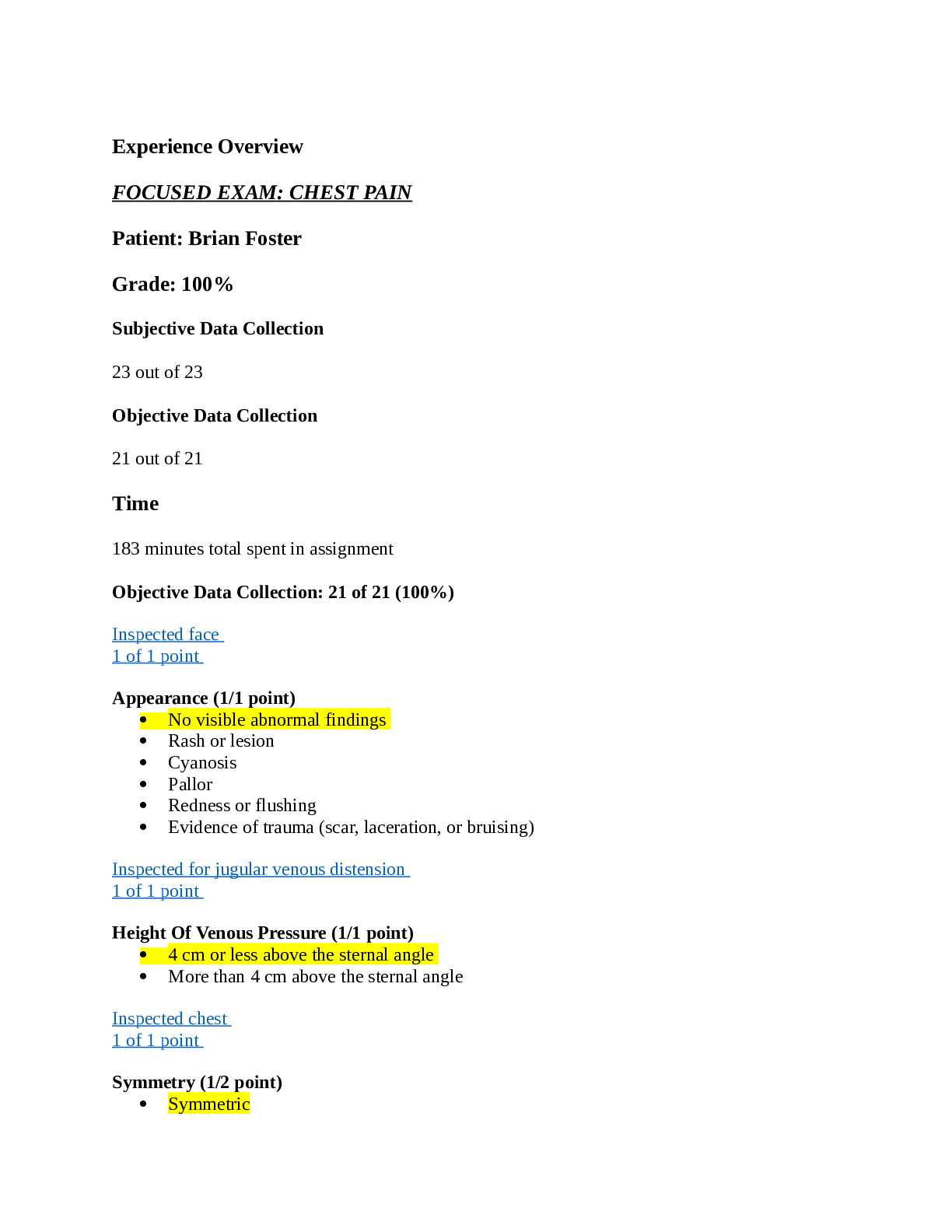
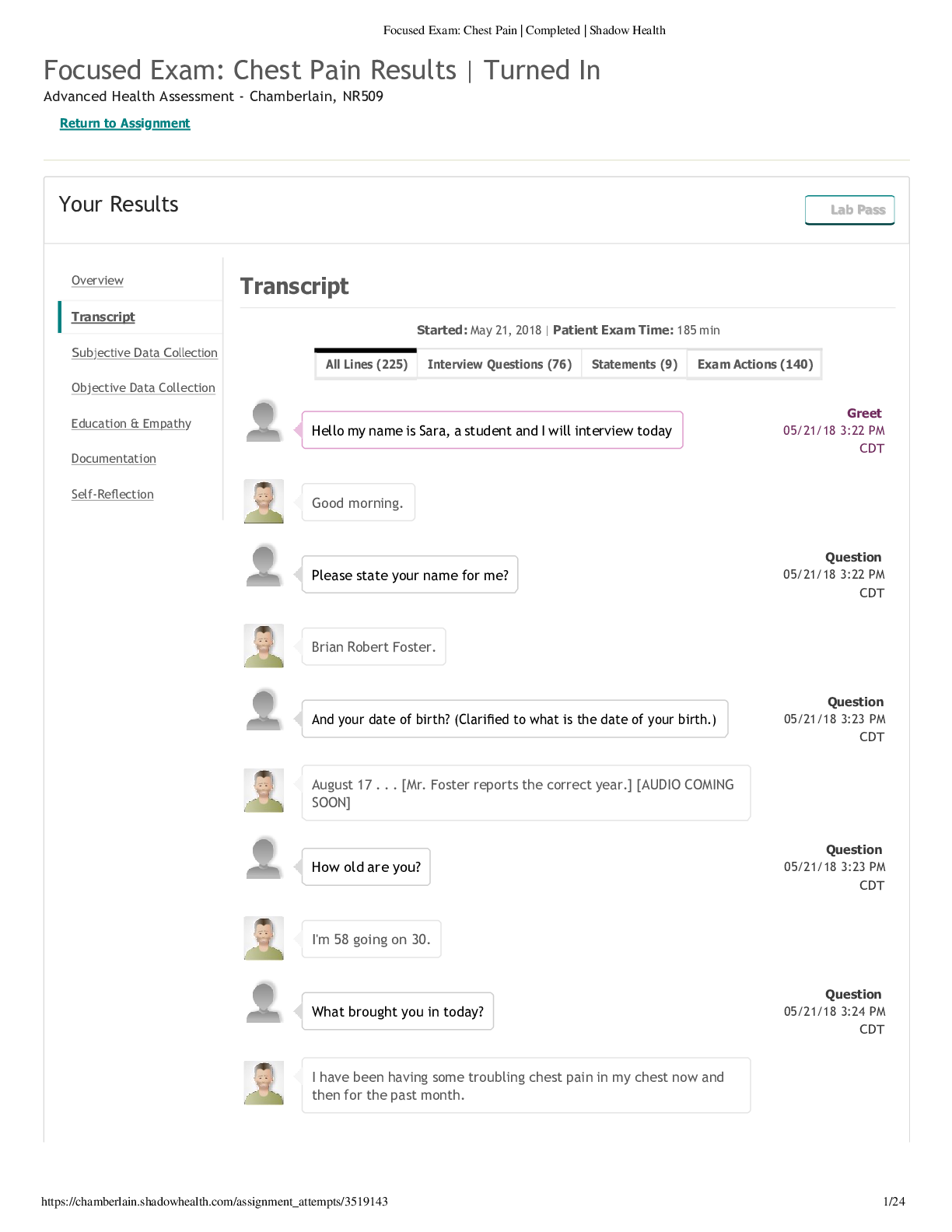
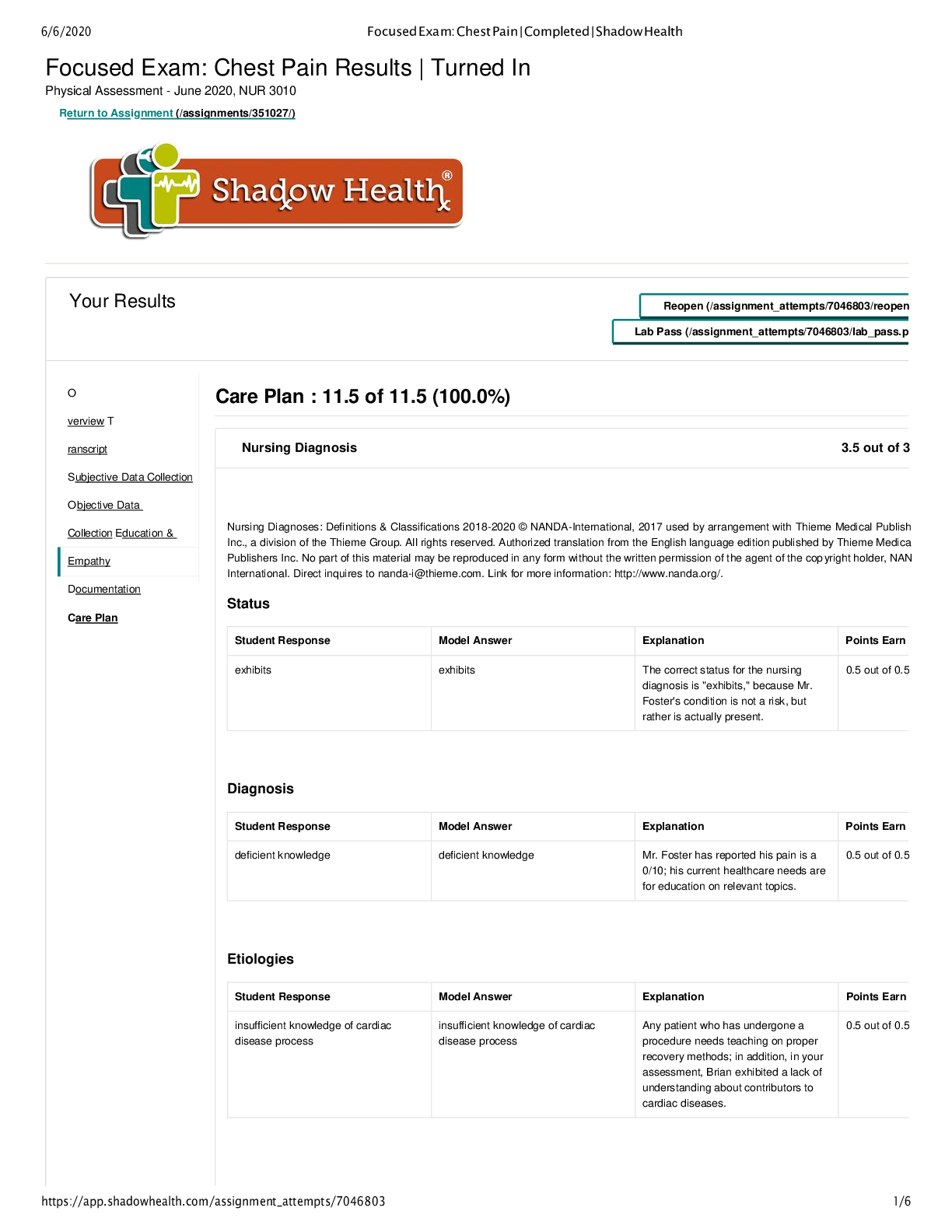
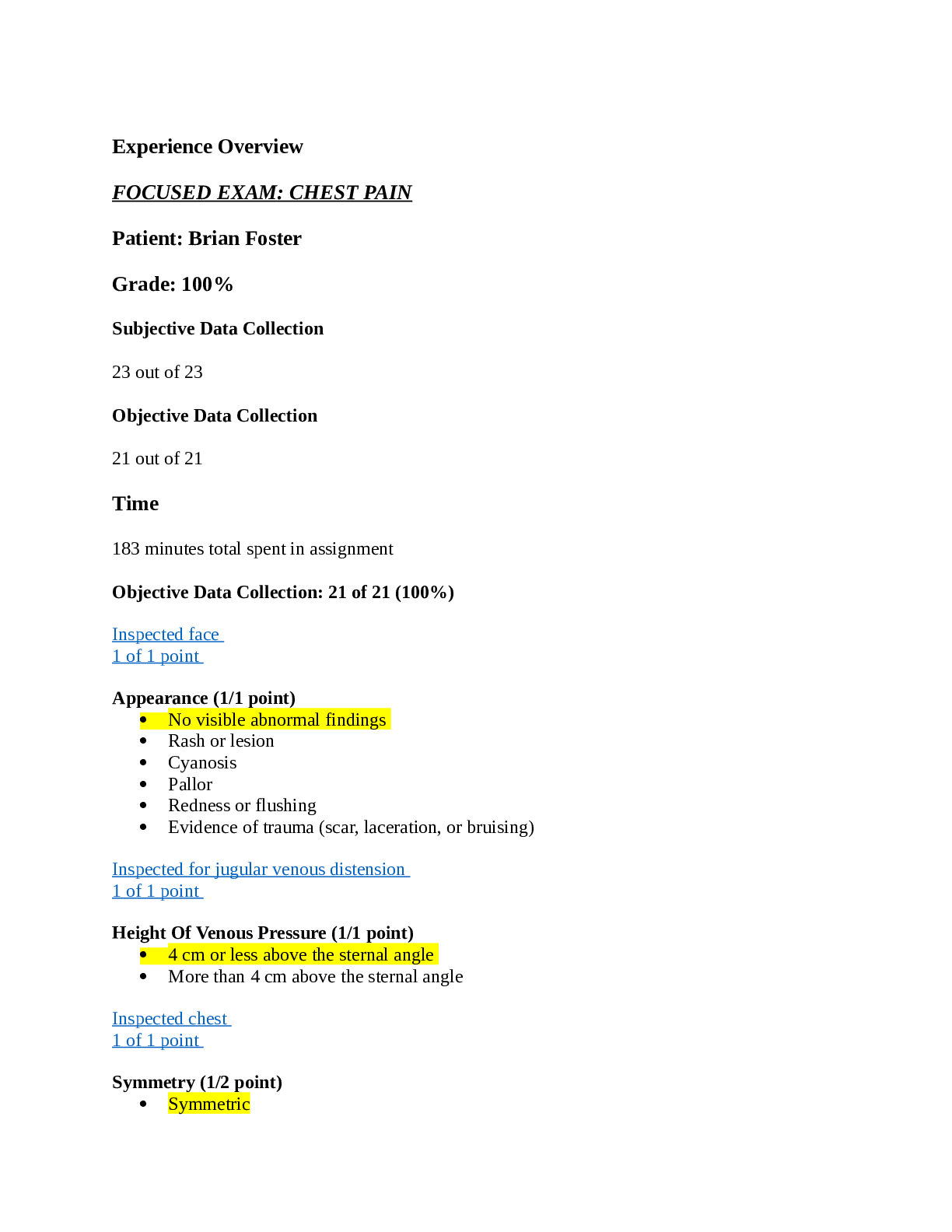
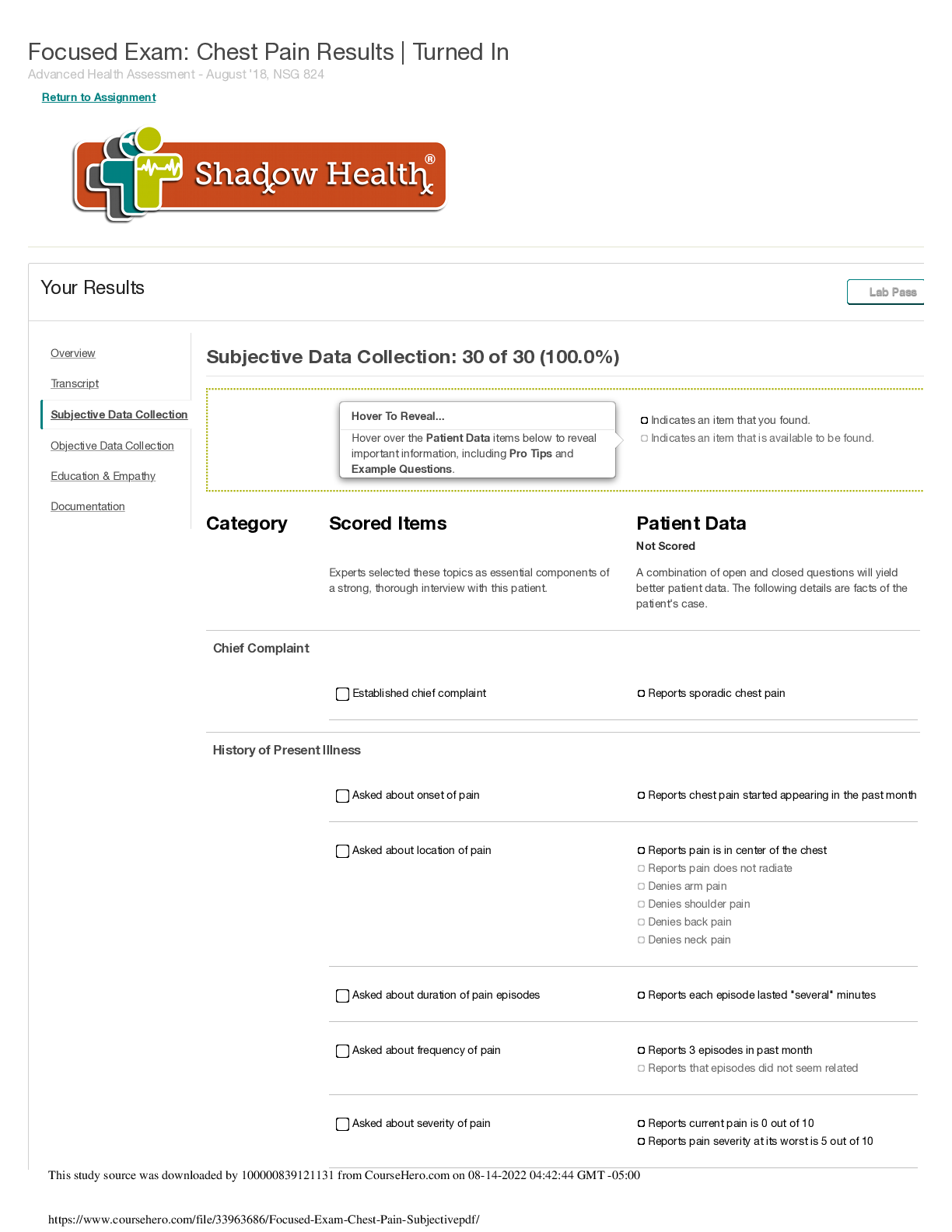
Experience Overview FOCUSED EXAM: CHEST PAIN Patient: Brian Foster Grade: 100% Subjective Data Collection 23 out of 23 Objective Data Collection 21 out of 21 Time 183 minutes tot... al spent in assignment Objective Data Collection: 21 of 21 (100%) Inspected face 1 of 1 point Appearance (1/1 point) • No visible abnormal findings • Rash or lesion • Cyanosis • Pallor • Redness or flushing • Evidence of trauma (scar, laceration, or bruising) Inspected for jugular venous distension 1 of 1 point Height Of Venous Pressure (1/1 point) • 4 cm or less above the sternal angle • More than 4 cm above the sternal angle Inspected chest 1 of 1 point Symmetry (1/2 point) • Symmetric • Asymmetric Appearance (1/2 point) • No visible abnormal findings • Rash or lesion • AP diameter abnormal • Intercostal retraction while breathing • Excessive use of accessory muscles while breathing • Pectus excavatum • Skin growths (freckles or moles) • Evidence of skin trauma (scar, laceration, or bruising) Inspected hands and fingernails 1 of 1 point Right: Appearance (1/4 point) • No visible abnormal findings • Redness • Moles or skin tags • Masses (warts, cysts, or tumors) • Freckles, birthmark, or other discoloration • Excessive dry or flaking skin • Purpura • Scarring • Laceration, lesion, or wound • Bruising • Rash Left: Appearance (1/4 point) • No visible abnormal findings • Redness • Moles or skin tags • Masses (warts, cysts, or tumors) • Freckles, birthmark, or other discoloration • Excessive dry or flaking skin • Purpura • Scarring • Laceration, lesion, or wound • Bruising • Rash Right: Nail Changes (1/4 point) • No visible abnormal findings • Pallor • Cyanosis • Splinter hemorrhages • Clubbing Left: Nail Changes (1/4 point) • No visible abnormal findings • Pallor • Cyanosis • Splinter hemorrhages • Clubbing Inspected lower extremities and toenails 1 of 1 point Right: Appearance (1/4 point) • No visible abnormal findings • Visible distortion or swelling • Brownish pigmentation • Skin thickening • Ulceration • Varicose veins Right: Nail Changes (1/4 point) • No visible abnormal findings • Pallor • Cyanosis • Splinter hemorrhages • Clubbing Left: Appearance (1/4 point) • No visible abnormal findings • Visible distortion or swelling • Brownish pigmentation • Skin thickening • Ulceration • Varicose veins Left: Nail Changes (1/4 point) • No visible abnormal findings • Pallor • Cyanosis • Splinter hemorrhages • Clubbing Inspect lower extremities for edema 1 of 1 point Right: Edema (1/4 point) • No edema • Pitting • Non-pitting Right: Severity Of Edema (1/4 point) • No edema • 1+ Slight pitting • 2+ Deeper pit, disappears in 10 to 15 seconds • 3+ Noticeably deep pit that lasts more than a minute • 4+ Very deep pit that lasts 2 to 5 minutes Left: Edema (1/4 point) • No edema • Pitting • Non-pitting Left: Severity Of Edema (1/4 point) • No edema • 1+ Slight pitting • 2+ Deeper pit, disappears in 10 to 15 seconds • 3+ Noticeably deep pit that lasts more than a minute • 4+ Very deep pit that lasts 2 to 5 minutes Tested capillary refill time 1 of 1 point Fingers (1/2 point) • Less than 3 seconds • Greater than 3 seconds Toes (1/2 point) • Less than 3 seconds • Greater than 3 seconds Palpated carotid arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Palpated PMI 1 of 1 point Location (1/3 point) • Present at midclavicular line and 5th intercostal space • Displaced laterally Diameter (1/3 point) • Less than 3 cm • Greater than 3 cm Amplitude (1/3 point) • Brisk and tapping • Increased amplitude (hyperkinetic) Palpated brachial arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Palpated radial arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Palpated femoral arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Palpated popliteal arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Palpated tibial arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Palpated dorsalis pedis arteries 1 of 1 point Right: Vibration (1/4 point) • No thrill • Thrill Right: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Left: Vibration (1/4 point) • No thrill • Thrill Left: Amplitude (1/4 point) • 0 Absent • 1+ Diminished or barely palpable • 2+ Expected • 3+ Increased • 4+ Bounding pulse Auscultated carotid arteries 1 of 1 point Right (1/2 point) • No bruit • Bruit Left (1/2 point) • No bruit • Bruit Auscultated heart sounds 1 of 1 point Heart Sounds (1/2 point) • S1 and S2 audible • S1, S2, and S3 audible • S1, S2, and S4 audible • S1, S2, S3, and S4 audible Extra Heart Sounds (1/2 point) • No extra sounds • Gallops • Murmur • Friction rub • Valve clicks Auscultated abdominal aorta 1 of 1 point Sounds (1/1 point) • No bruit • Bruit Auscultated abdominal and lower extremity arteries 1 of 1 point Right: Renal (1/6 point) • No bruit • Bruit Right: Iliac (1/6 point) • No bruit • Bruit Right: Femoral (1/6 point) • No bruit • Bruit Left: Renal (1/6 point) • No bruit • Bruit Left: Iliac (1/6 point) • No bruit • Bruit Left: Femoral (1/6 point) • No bruit • Bruit Auscultated breath sounds 1 of 1 point Breath Sounds (1/3 point) • Present in all areas • Diminished in some areas • Absent in some areas Adventitious Sounds (1/3 point) • No adventitious sounds • Wheezing • Fine crackles • Stridor • Rhonchi • Rales Location (1/3 point) • All areas clear • Adventitious sounds in anterior right upper lobe • Adventitious sounds in anterior right middle lobe • Adventitious sounds in anterior right lower lobe • Adventitious sounds in anterior left upper lobe • Adventitious sounds in anterior left lower lobe • Adventitious sounds in posterior right upper lobe • Adventitious sounds in posterior right lower lobe • Adventitious sounds in posterior left upper lobe • Adventitious sounds in posterior left lower lobe Performed EKG 1 of 1 point Sinus Rhythm (1/2 point) • Regular • Irregular St Changes (1/2 point) • No ST elevation • ST elevation present Subjective Data Collection: 23 of 23 (100.0%) A combination of open and closed questions will yield better patient data. The following details are facts of the patient's case. Chief Complaint Finding: Established chief complaint Finding: Reports chest pain (Found) Pro Tip: Asking a patient broadly about their chief complaint allows them to answer in their own words and confirm information that you may have already received from another source. Example Question: Do you have chest pain? History of Presenting Illness Finding: Asked about onset and duration of chest pain Finding: Reports chest pain started about five minutes ago (Found) Pro Tip: Establishing the onset of a patient's chest pain is essential in diagnosing its severity as well as the comfort of the patient. Example Question: When did the chest pain start? Finding: Reports chest pain has been constant since it began (Available) Pro Tip: Knowing the duration of a patient's pain gives you a more complete picture of its severity and potential impact on the patient's health. Example Question: How long does the chest pain last? Finding: Reports sitting in bed when pain began (Found) Pro Tip: A patient's position and posture when their pain began can inform you as to the nature of the pain, as pain upon exertion often has different causes than pain upon resting. Example Question: Were you sitting when the pain began? Finding: Asked to rate chest pain on a scale Finding: Reports current pain is 6/10 (Found) Pro Tip: For many patients, it is difficult to clearly describe pain. Asking Brian to rate his pain on a scale from 0 to 10 develops a consistent measure of pain severity. Example Question: On a scale of 0 to 10 how would you rate the chest pain? Finding: Asked about on characteristics of the pain Finding: Describes pain as tight and uncomfortable (Found) Pro Tip: Asking Brian to describe his pain helps identify the cause and the severity of his discomfort. Patients may not know how to answer, so you may need to suggest words like sharp, dull, crushing, gnawing, or burning. Example Question: Can you describe your pain? Finding: Denies crushing pain (Found) Pro Tip: Asking Brian to describe his pain helps identify the cause and the severity of his discomfort. Patients may not know how to answer, so you may need to suggest words like sharp, dull, crushing, gnawing, or burning. Example Question: Is the pain crushing? Finding: Denies gnawing or tearing pain (Found) Pro Tip: Asking Brian to describe his pain helps identify the cause and the severity of his discomfort. Patients may not know how to answer, so you may need to suggest words like sharp, dull, crushing, gnawing, or burning. Example Question: Is the pain gnawing? Finding: Denies burning pain (Found) Pro Tip: Asking Brian to describe his pain helps identify the cause and the severity of his discomfort. Patients may not know how to answer, so you may need to suggest words like sharp, dull, crushing, gnawing, or burning. Example Question: Is the pain burning? Finding: Asked about location of the pain Finding: Reports pain location is in middle of the chest (Found) Pro Tip: Identifying the location of a patient's pain is essential in determining which body systems are affected, the underlying cause of the pain, and how best to treat it. Example Question: Where is the pain? Finding: Reports slight pain in left shoulder (Found) Pro Tip: Pain radiation is an important symptom that can be helpful in understanding the cause of pain and narrowing the diagnosis. Example Question: Does the pain radiate? Finding: Denies arm pain (Found) Pro Tip: When combined with chest pain, arm pain can be a telling sign that the complaint may be cardiac in nature. Example Question: Do you have arm pain? Finding: Denies back pain (Found) Pro Tip: When combined with chest pain, back pain can be a telling sign that the complaint may be cardiac in nature. Example Question: Do you have back pain? Finding: Denies jaw pain (Found) Pro Tip: When combined with chest pain, jaw pain can be a telling sign that the complaint may be cardiac in nature. Example Question: Do you have jaw pain? Finding: Denies neck pain (Found) Pro Tip: When combined with chest pain, neck pain can be a telling sign that the complaint may be cardiac in nature. Example Question: Do you have neck pain? Finding: Asked about pain triggers Finding: Reports pain is aggravated by movement (Found) Pro Tip: Aggravating factors reveal further information about the nature of the pain and the body systems affected. Example Question: What makes the pain worse? Finding: Asked about stress and anxiety Finding: Reports generally low stress lifestyle (Found) Pro Tip: Stress can have a profound effect on the patient's health and wellness. Asking about stress is an important part of any health assessment. Example Question: What is your usual stress level? Finding: Denies history of anxiety (Available) Pro Tip: Symptoms such as chest pain can be caused or exacerbated by episodes of anxiety. Asking Brian if he's ever suffered from anxiety can point to underlying stressors or triggers. Example Question: Do you have a history of anxiety? Finding: Denies history of panic attacks (Available) Pro Tip: Symptoms such as chest pain can be caused or exacerbated by episodes of anxiety. Asking Brian if he's ever had a panic attack can point to underlying stressors or triggers. Example Question: Have you ever had a panic attack? Past Medical History Finding: Asked relevant health history Finding: Reports high blood pressure (Found) Pro Tip: Hypertension is the most important risk factor for stroke. Soliciting a health history from Brian will allow you to assess his risk of cardiovascular disease. Example Question: Do you have high blood pressure? Finding: Reports high cholesterol (Found) Pro Tip: High cholesterol can lead to cardiovascular disease. Asking Brian whether he's had a history of high cholesterol reveals important details about his cardiovascular health. Example Question: Do you have high cholesterol? Finding: Denies history of pulmonary embolism (Available) Pro Tip: Pulmonary embolism is one of many cardiac risk factors to ask about that can help you form a more complete picture of Brian's cardiovascular health. Example Question: Have you ever had a pulmonary embolism? Finding: Denies history of angina (Available) Pro Tip: A history of angina can weaken the heart and lead to further cardiovascular complications. Asking Brian about angina helps you understand his overall cardiovascular health. Example Question: Do you have a history of angina? Finding: Denies history of rheumatic fever (Available) Pro Tip: Rheumatic fever early in life can cause fibrosis of the heart valves and can weaken the cardiovascular system. Finding out if Brian has a history of rheumatic fever is crucial to understanding his complete heart health. Example Question: Do you have a history of rheumatic fever? Finding: Denies history of heart murmur (Available) Pro Tip: Heart murmurs can be harmless or a sign of ongoing heart disease. Learning if Brian has a heart murmur is an important component of understanding his complete cardiovascular health. Example Question: Do you have a history of heart murmur? Finding: Followed up on high blood pressure treatment Finding: Reports taking high blood pressure medication (Found) Pro Tip: The medication that a patient takes for their high blood pressure will indicate how well controlled their condition is and how well they comply with treatment regimens. Example Question: Do you take medication for high blood pressure? Finding: Reports high blood pressure medication is Lisinopril (Found) Pro Tip: Discovering what specific high blood pressure medication a patient takes helps you assess his health conditions, effectiveness of treatment, and guards against unwanted medication interactions. Example Question: What medication do you take for high blood pressure? Finding: High blood pressure medication dose is 20mg (Available) Pro Tip: The current dose of any patient's high blood pressure medication is important to learn about because it provides useful information about the patient's treatment plan as well as potential medication interactions. Example Question: What dose of medication do you take for high blood pressure? Finding: High blood pressure medication is taken once daily (Available) Pro Tip: The frequency with which a patient takes his high blood pressure medications is an essential element of the complete picture of his medication treatment plan. Example Question: How frequently do you take medication for high blood pressure? Finding: Followed up on high cholesterol treatment Finding: Reports taking high cholesterol medication (Found) Pro Tip: The medication that a patient takes for their high cholesterol will indicate how well controlled their condition is and how well they comply with treatment regimens. Example Question: Do you take medication for cholesterol? Finding: Reports high cholesterol medication is Atorvastatin (Lipitor) (Found) Pro Tip: Discovering what specific high cholesterol medication a patient takes helps you assess his health conditions, effectiveness of treatment, and guards against unwanted medication interactions. Example Question: What medication do you take for cholesterol? Finding: Reports high cholesterol medication dose is 20mg (Available) Pro Tip: The current dose of any patient's high cholesterol medication is important to learn about because it provides useful information about the patient's treatment plan as well as potential medication interactions. Example Question: What dose of medication do you take for cholesterol? Finding: Reports high cholesterol medication is taken once daily (Available) Pro Tip: The frequency with which a patient takes his high cholesterol medications is an essential element of the complete picture of his medication treatment plan. Example Question: How frequently do you take medication for cholesterol? Finding: Asked history of cardiac tests Finding: Reports recent EKG test (Found) Pro Tip: An EKG test checks for electrical problems with the heart. Asking Brian whether he's had an EKG will reveal his recent medical history, cardiac health, and medical literacy. Example Question: Have you recently had an EKG test? Finding: Reports annual stress test (Found) Pro Tip: A stress test can illustrate the amount of stress a patient's heart can handle before developing irregular rhythm. Asking Brian if he's recently had a stress test will indicate a treatment plan, cardiac health, and health literacy. Example Question: Have you recently had a stress test? Finding: Asked about results of cardiac tests Finding: Reports belief that EKG was normal (Available) Pro Tip: An EKG test checks for electrical problems with the heart. Asking Brian whether he's had an EKG will reveal his recent medical history, cardiac health, and medical literacy. Example Question: What were the results of your last EKG? Finding: Reports belief that stress test was normal (Found) Pro Tip: A stress test can illustrate the amount of stress a patient's heart can handle before developing irregular rhythm. Asking Brian if he's recently had a stress test will indicate a treatment plan, cardiac health, and health literacy. Example Question: What were the results of your last stress test? Finding: Asked about substance use Finding: Denies illicit drug use (Found) Pro Tip: Many drugs affect the central nervous system or can cause cardiovascular complications. Asking Brian if he uses illicit drugs will indicate whether drug use puts him at risk for health complications. Example Question: Do you use illicit drugs? Finding: Denies tobacco use (Found) Pro Tip: Tobacco affects the heart by reducing the amount of oxygen the blood is able to carry. Asking Brian if he uses tobacco will allow you to assess whether the condition is caused, in part, by tobacco use. Example Question: Do you use tobacco? Finding: Reports moderate alcohol consumption (Found) Pro Tip: Chronic alcohol use can result in cardiomyopathy. Asking Brian whether he drinks alcohol will allow you to assess whether he has any indicators of alcoholism. Example Question: How much alcohol do you consume? Finding: Followed up on alcohol consumption Finding: Reports drinking only on weekends (Found) Pro Tip: Asking the patient to describe his drinking habits can identify indicators of alcoholism. It may also be helpful to ask about the context and reasons for the patient's alcohol intake. Heavy drinkers will often underestimate their drinking habits. Example Question: How frequently do you drink alcohol? Finding: Reports drinking 2-4 alcoholic drinks per week (Found) Pro Tip: Consumption of alcohol can impact a patient's health and is considered a risk factor for many medical conditions. Asking Brian about his drinking habits will help you determine his risk for disease linked to alcohol consumption. Example Question: How many alcoholic drinks do you have in a week? Finding: Reports 2-3 drinks in a single sitting (Found) Pro Tip: Asking the patient to quantify his drinking is helpful because it elicits objective data on a subject that patients may otherwise downplay. Example Question: How many alcoholic drinks do you consume at a time? Finding: Asked about exercise Finding: Denies having a regular exercise routine (Found) Pro Tip: Activity levels have an important impact on cardiovascular health. Asking Brian about his exercise patterns can help you understand how his lifestyle might affect his health. Example Question: What kind of exercise do you get? Finding: Asked about most recent meal Finding: Reports most recent meal was previous night at 8 p.m. (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Brian about his most recent meal will allow you to assess whether his eating habits put him at risk of cardiovascular disease or other health complications, and can reveal if the food he ate may be affecting his complaint. Example Question: What time was your last meal? Finding: Reports meal consisted of buffalo wings (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Brian about his most recent meal will allow you to assess whether his eating habits put him at risk of cardiovascular disease or other health complications, and can reveal if the food he ate may be affecting his complaint. Example Question: What did you eat last night? Finding: Asked about typical diet Finding: Reports typical breakfast is granola bar and instant breakfast shake (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Brian about his typical breakfast will allow you to assess whether his eating habits put him at risk of cardiovascular disease or other health complications. Example Question: What is a typical breakfast for you? Finding: Reports typical lunch is turkey sub (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Brian about his typical lunch will allow you to assess whether his eating habits put him at risk of cardiovascular disease or other health complications. Example Question: What is a typical lunch for you? Finding: Reports typical dinner is grilled meat and vegetables (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Brian about his typical dinner will allow you to assess whether his eating habits put him at risk of cardiovascular disease or other health complications. Example Question: What is a typical dinner for you? Finding: Denies moderating salt intake (Available) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Salt intake in particular can have a detrimental effect on blood pressure, which is why it is important to ask a patient like Brian, who suffers from hypertension, about his salt consumption. Example Question: Do you moderate your salt intake? Review of Systems Finding: Asked about review of cardiovascular system Finding: Denies palpitations (Found) Pro Tip: Discovering palpitations can be an important clue into the patient's cardiovascular history and current condition. Example Question: Do you have palpitations? Finding: Denies swelling (Found) Pro Tip: Swelling can be a major indicator of cardiovascular and peripheral vascular health. Asking the patient about swelling is an important part of a thorough cardio exam. Example Question: Do you have any swelling? Finding: Denies circulation problems (Found) Pro Tip: Circulation is an important indicator of peripheral vascular and cardiovascular health. Asking Brian about his circulation can help diagnose vascular conditions. Example Question: Do you have any problems with circulation? Finding: Denies blood clots (Found) Pro Tip: Blood clots can be a sign of serious cardiovascular or related illnesses. Asking Brian about blood clots can provide valuable information about the state of his health. Example Question: Have you ever had a blood clot? Finding: Denies easy bleeding (Found) Pro Tip: Bleeding can be a sign of serious cardiovascular or related illnesses. Asking Brian about bleeding can provide valuable information about the state of his cardiovascular health. Example Question: Have you noticed any unusual bleeding? Finding: Denies easy bruising (Found) Pro Tip: Ease of bruising can be a sign of serious cardiovascular or related illnesses. Asking Brian about bruising can provide valuable information about the state of his cardiovascular health. Example Question: Have you noticed any unusual bruising? Finding: Asked about constitutional health Finding: Denies fever (Available) Pro Tip: Fever can signify infection and other complications, so it is important to determine the presence of a fever and treat it if there is. Example Question: Do you have a fever? Finding: Denies chills (Available) Pro Tip: Chills can be a sign of circulation issues, fever, and more. Discovering a patient's chills will reveal more about the cause of his complaint. Example Question: Do you have chills? Finding: Denies fatigue (Available) Pro Tip: Fatigue can be an indicator of serious cardiovascular problems, and it is important to ask the patient about it in order to narrow your diagnosis. Example Question: Do you feel tired? Finding: Denies sleep issues (Available) Pro Tip: Sleep issues can be an indicator of serious cardiovascular problems, and it is important to ask the patient about it in order to narrow your diagnosis. Example Question: Have you had problems sleeping? Finding: Denies recent weight changes (Available) Pro Tip: Weight changes can be an indicator of serious cardiovascular problems, and it is important to ask the patient about it in order to narrow your diagnosis. Example Question: Has your weight changed? Finding: Denies night sweats (Available) Pro Tip: Night sweats can be an indicator of serious cardiovascular problems, and it is important to ask the patient about it in order to narrow your diagnosis. Example Question: Do you have night sweats? Finding: Denies dizziness or lightheadedness (Available) Pro Tip: Patients exhibiting dizziness may be at risk for several conditions as well as a fall risk. It is important to ask about dizziness to keep your patient safe. Example Question: Do you have dizziness? Finding: Asked about review of respiratory system Finding: Denies cough (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the respiratory system. A cough in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have a cough? Finding: Denies shortness of breath while lying down (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the respiratory system. Orthopnea in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have difficulty breathing when lying down? Finding: Denies blue skin (Available) Pro Tip: Cyanosis can be a symptom of troubling cardiovascular illness, though patients may not be aware of its connection to respiratory health. Asking Brian if he has noticed any cyanosis is important in ruling out certain cardiac risk factors. Example Question: Has your skin ever turned blue? Finding: Asked about throat problems Finding: Denies sore throat (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the throat. A sore throat in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have a sore throat? Finding: Denies difficulty swallowing (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the throat. Painful or difficult swallowing in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have difficulty swallowing? Finding: Asked about review of gastrointestinal system Finding: Denies diarrhea (Available) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the gastrointestinal system. Diarrhea in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have diarrhea? Finding: Denies constipation (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the gastrointestinal system. Constipation in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have constipation? Finding: Denies flatus (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the gastrointestinal system. Excessive gas in a patient complaining of chest pain is a symptom worth investigating. Example Question: Do you have flatulence? Finding: Denies bloating (Available) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the gastrointestinal system. A patient complaining of bloating in addition to chest pain is a symptom worth investigating. Example Question: Do you have bloating? Finding: Denies heartburn or GERD (Found) Pro Tip: The cardiovascular system is inextricably balanced with many other body systems, including the gastrointestinal system. Heartburn and GERD are of particular importance to ask about, since their symptoms closely follow the symptoms of cardiac pain. Example Question: Do you have heartburn or GERD? Finding: Reports earlier nausea (Available) Pro Tip: Nausea can be an urgent symptom and sign of distress in more than one body symptom. Assessing and treating a patient's nausea is important in a cardiovascular exam. Example Question: Do you have nausea? Finding: Denies vomiting (Available) Pro Tip: Vomiting can be a major indicator of multiple health problems. Asking the patient about vomiting is an important part of a thorough cardio exam. Example Question: Have you vomited recently? Family History Finding: Asked relevant family history Finding: Reports family history of heart attack (Found) Pro Tip: Family health history is an important genetic indicator of a patient's predisposition to certain medical conditions. Asking Brian if anyone in his family has suffered a heart attack helps you develop a more complete picture of his cardiovascular health. Example Question: Has anyone in your family had a heart attack? Finding: Denies family history of stroke (Available) Pro Tip: Family health history is an important genetic indicator of a patient's predisposition to certain medical conditions. Asking Brian if anyone in his family has suffered a stroke helps you develop a more complete picture of his cardiovascular health. Example Question: Do you have a family history of stroke? Finding: Denies family history of pulmonary embolism (Available) Pro Tip: Family health history is an important genetic indicator of a patient's predisposition to certain medical conditions. Asking Brian if anyone in his family has had a pulmonary embolism helps you develop a more complete picture of his cardiovascular health. Example Question: Do you have a family history of pulmonary embolism? Document: Vitals Vitals 00:00 04:00 08:00 08:05 Blood Pressure 115/62 126/70 122/78 98/60 O2 Sat 98 98 98 98 Pulse 74 78 82 104 Resp. Rate 16 18 18 26 Temperature 37.1 36.9 37.3 37.0 Document: Nursing Notes Student Documentation Model Documentation Subjective Patient complains of constant pressure chest pain near sternum. Started 5 minutes before assessment. Pain level is a 6 out of 10. Lying Mr. Foster is post-op day 3 for a TURP (Transurethral resection of the prostate). He is complaining of chest pain that began 5 minutes ago. He rates his pain at 6/10. He reports the pain is localized to the sub-sternal region and still slightly relieves the pain. Movement causes describes it as “squeezing pressure.” He reports more pain. Complains of slight left shoulder pain. Denies any level of stress or anxiety. States high blood pressure, takes Lisinopril. States high cholesterol, takes Atorvastatin. Denies having a regular exercise routine. the pain is constant and increasing in severity. He denies radiation but reports some pressure in the left shoulder as well. He reports the pain was accompanied by nausea at the onset, but denies emesis. The patient reports becoming increasingly anxious. He denies SOB and palpitations. He denies tenderness, redness, or Student Documentation Model Documentation changes in surgical site. Objective BP has dropped to 98/60 and pulse is raised to 104 at 8:05 within 5 minutes of chest pain beginning. • General Survey: Alert, but uncomfortable appearing middle-aged male supine in hospital bed, pale and mildly diaphoretic. Elevated respiratory rate and evident distress. • Cardiovascular: No JVD, HR between 100-115, S1 & S2, + S4. No murmur, no rub. Occasional PVCs appreciated. BP range 92-109/57-68. No carotid bruit or thrill. • Peripheral Vascular: Capillary refill <3 seconds on bilateral fingers and toes, radial pulses 2+, posterior tibial and dorsalis pedis pulses +1. No lower extremity edema. No varicosities, no areas of focal induration or erythema. • Respiratory: Respirations quiet and unlabored, able to speak in full sentences. Lungs CTA. RR 24-26/m, O2 saturation 97-99%. • Neuro: Alert and oriented x3, follows commands, moves all extremities. • Skin: Slight pallor and diaphoresis. No redness, induration, or purulence noted. • EKG (interpretation): Sinus tachycardia with occasional PVCs. No ST segment elevation. 1. Situation Patient came in for knee surgery. He is stable, complains of chest pain. BP has dropped and pulse is elevated. Model Note Brian Foster is a 58-year-old man currently experiencing chest pain. He rates the pain at 6/10 and described it as a constant squeezing pressure. He reports pressure in his left shoulder and a brief spell of nausea upon onset of the chest pain, but denies other accompanying symptoms. 2. Background the pt had a bp drop, he has chest pain, last meal was buffalo wings? Model Note Mr. Foster is post-op day 3 for a TURP (Transurethral resection of the prostate). His post- operative course was normal until the chest pain this morning. He has a history of hypertension, hyperlipidemia, and family history of cardiac disease. He does not smoke. 3. Assessment the patient is stable Model Note The physical exam revealed an elevated heart rate, between 100-115 beats per minute, and an audible S4 on auscultation. EKG displays sinus tachycardia and occasional PVCs. No ST segment elevation. His respiratory rate is also elevated and he appears in acute distress. 4. Recommendation monitor his bp and consult a cardiologist Model Note I recommend immediate emergency intervention per hospital guidelines. Mr. Foster’s wife is nearby and I will notify her of her husband’s condition. What brings you in today? Question 11/26/18 3:45 PM CST I'm having a really uncomfortable pressure in my chest right now. When did the pain in your chest begin? Only about five minutes ago. [AUDIO COMING SOON] what were you doing when the pain started? I was just sitting here. Is the pain constant? It's hard to say...I've never had a feeling like this before...it seems pretty constant. Can you rate your chest pain on a scale from 0-10? I'd say maybe a...6? It's just really uncomfortable...like there's nothing I can do about it, and it feels like it is getting worse. Can you describe the pain? Well, it mostly feels like pressure. Like a heavy, squeezing pressure right in the middle of my chest. Any burning pain? (Clarified to Would you describe the pain as burning?.) Well, it mostly feels like pressure. Like a heavy, squeezing pressure right in the middle of my chest. (Clarified to if the pain is burning.) Do you know what triggered the chest pain? (Clarified to What do you think triggered your pain?.) I have no idea! (Clarified to what seemed to trigger the pain.) What can you do to alleviate your pain? I'm not sure. I think lying still seems to help a little. Any arm pain? My left shoulder is hurting a tiny bit. [AUDIO COMING SOON] any back pain? No, I wouldn't say so. any neck pain? No. any jaw pain? Nope. does movement make the pain worse? I don't really know, I only noticed it a few minutes ago. I tried to get up and walk around the room a little but I think that made it worse. Do you experience any stress or anxiety? Honestly, my life is pretty low stress. My job rarely stresses me out, my home life is great, and my kids generally behave. My only stress right now is this chest pain. Do you have any history of health issues? Well, let's see...besides this prostate situation, the doctors told me I have a little bit of high blood pressure and cholesterol. I take meds for those but that's it. What medications do you take for your blood pressure? (Clarified to What do you take for your blood pressure?.) Lisinopril. (Clarified to what I take for my blood pressure.) what do you take for your cholesterol? I take Atorvastatin. Have you had any cardiac tests? Just the EKG and stress tests. Unless you count bloodwork. I've had that done too. Were there any abnormal results to the cardiac tests? (No matching questions found.) Were there any abnormal results? (No matching questions found.) What were the results of your stress tests? I'm not sure, all the doctor ever tells me is, "everything looks good." Have you ever used drugs? I tried a few of the usual suspects back in my youth, but I haven't touched any of that stuff in over 30 years. Do you use tobacco products? No. Do you drink alcohol? Sure, but never more than two or three beers on a weekend. How many drinks per week do you consume? Maybe 2 or 3 tops. Just on the weekends. How many alcoholic drinks do you consume in one sitting? Not too much. Maybe a few beers on the weekend, that's about all. Do you exercise? Well I used to ride my bike a lot but it got stolen a couple years ago. I guess I haven't had much regular exercise since then...I want to get a new bike after I recover from this surgery. What did you eat last? My wife brought me some buffalo wings last night around eight. What is your typical diet? I think my diet's alright. My wife says I should do better but I'm a meat man, what can I say. [AUDIO COMING SOON] What do you eat for breakfast? Um let's see...For breakfast I usually eat a granola bar and drink an instant breakfast shake. I've been doing that a while since it saves time in the morning. Most days for lunch I get a sandwich from the sub shop near work. That's usually a turkey sub, but sometimes I get a spicy Italian sub. My wife and I grill a lot, and usually have some grilled meat with veggies for dinner. HOw is your cardiovascular system? I don't know--I thought fine, but my chest is hurting, so. . . [AUDIO COMING SOON] any swelling? I haven't noticed any swelling. any palpitations? I don't think so. I haven't noticed any. any circulation issues? Nope, I haven't noticed anything. do you bleed easy? No, I sure don't think so. Any blood clots? Not that I know of. Do you bruise easily? No, nothing out of the ordinary. How is respiratory system? My breathing's fine. Any throat problems? Nope. any coughing? I don't have a cough. Any shortness of breath? (Clarified to Do you currently have shortness of breath?.) No, I can breathe just fine. (Clarified to if I have shortness of breath right now.) any gastrointestinal issues? No, not at all. any constipation? Nope. any Denies flatus? (No matching questions found.) any flatus? No, I wish this was only gas but it feels different. Any gerd? No, I've never had problems with heartburn. I sure hope that's all this is, but it's pretty intense if it's heartburn. Any family history of cardiac issues? Well, my mom's dad died of a heart attack. He was pretty young too. Scares the bejeezus out of me. [AUDIO COMING SOON] Any relevant family history? No. [Show More]
Last updated: 1 year ago
Preview 1 out of 48 pages
Also available in bundle (1)
SHADOW HEALTH FOCUSED EXAMS BUNDLE. 100% VERIFIED.
SHADOW HEALTH FOCUSED EXAMS BUNDLE. 100% VERIFIED.
By A+ Solutions 2 years ago
$14.5
59
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 04, 2021
Number of pages
48
Written in
Additional information
This document has been written for:
Uploaded
Oct 04, 2021
Downloads
0
Views
191