*NURSING > EXAM > NSG 6420 QUIZ 1 Questions and Answer Solutions | 100% VERIFIED | ANSWERED and Guaranteed pass | Sout (All)
NSG 6420 QUIZ 1 Questions and Answer Solutions | 100% VERIFIED | ANSWERED and Guaranteed pass | South University, Savannah
Document Content and Description Below
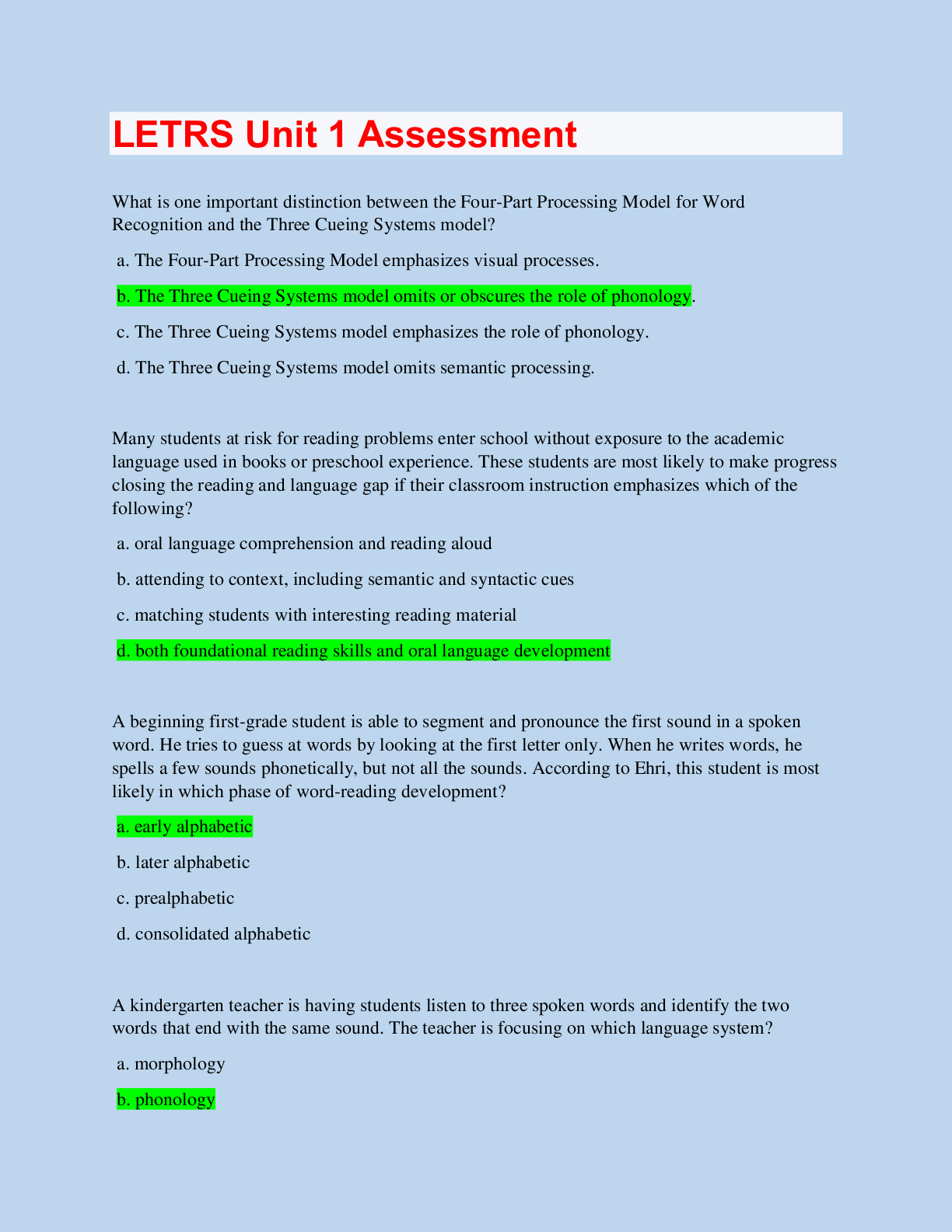
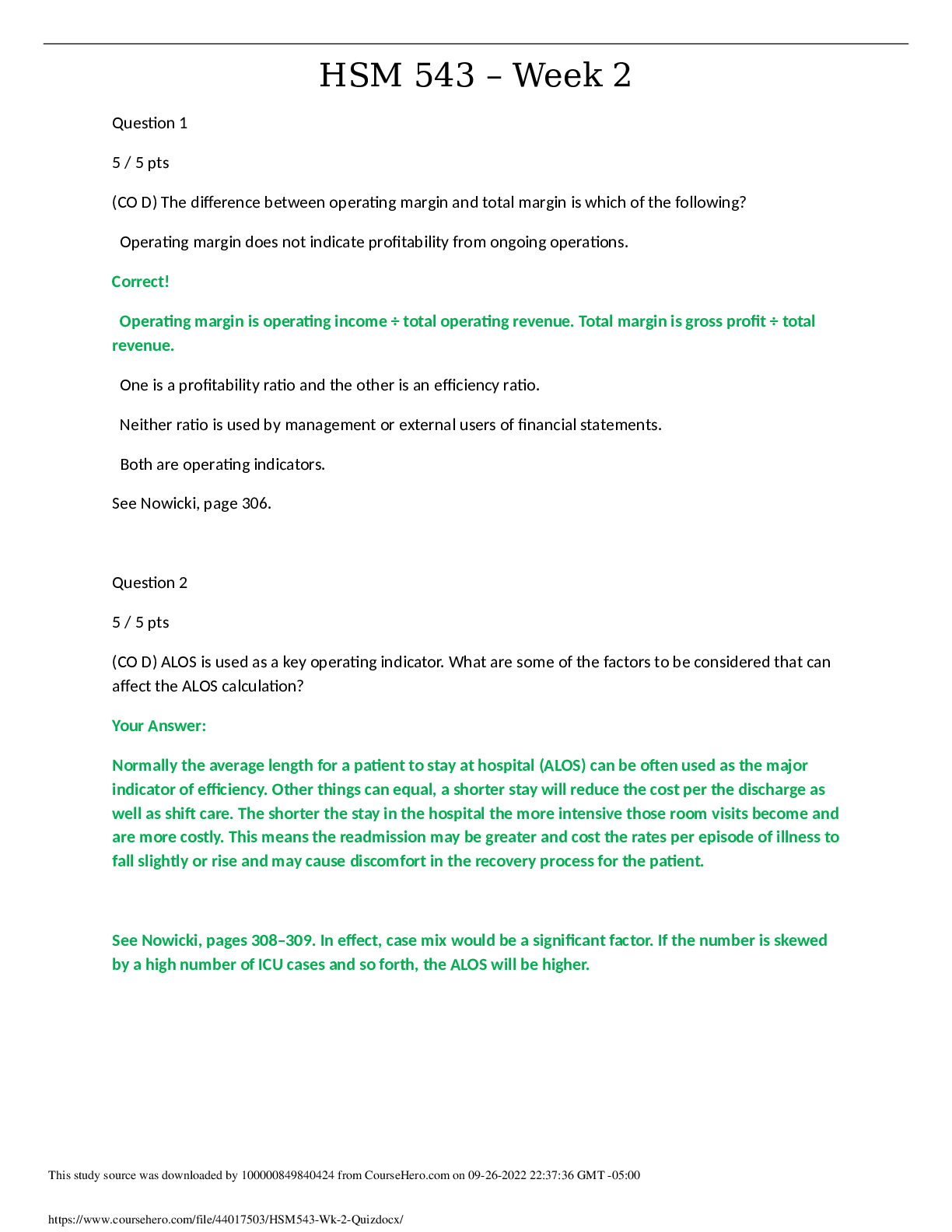
NSG 6420 Quiz 1 . Question : Which of the following is the most important question to ask during cardiovascular health history? Student Answer: Number of offspring Last physical exam S... udden death of a family member Use of caffeine Instructor Explanation: The sudden death of a family member is an important question to ask in the health history because it reveals the cardiovascular disease risk of the patient. Sudden death is usually due to an acute cardiovascular event, such as myocardial infarction, cardiac dysrhythmia, or stroke. Family history is particularly important for cardiac assessment because CVD, HTN, hyperlipidemia, and other vascular diseases often have a familial association that is not easily ameliorated by lifestyle changes. If there are deaths in the family related to CVD, determine the age and exact cause of death, because CVD at a young age in the immediate family carries an increased risk compared with CVD in an elderly family member. Ask about sudden death, which might indicate a congenital disease such as Marfan's syndrome. This is especially important to ask during pre-sports physicals because sudden death in athletes is often related to congenital or familial heart disease. Familial hyperlipidemia is autosomal dominant and often leads to CAD and MI at a young age. Family history of obesity and type 2 diabetes are also secondary risk factors for heart disease because the familial tendency for these is strong. Ask about smoking in the house, as secondhand smoke is a risk factor for respiratory and cardiac disease. (Goolsby 167-168) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 2. Question : A key symptom of ischemic heart disease is chest pain. However, angina equivalents may include exertional dyspnea. Angina equivalents are important because: Student Answer: Women with ischemic heart disease many times do not present with chest pain Some patients may have no symptoms or atypical symptoms; diagnosis may only be made at the time of an actual myocardial infarction Instructor Explanation: Elderly patients have the most severe symptoms A & B only The key symptom of IHD is chest pain, but other common symptoms include arm pain, lower jaw pain, shortness of breath, and diaphoresis. These symptoms are referred to as angina equivalents and can also include fatigue or breathlessness. Some patients may have no symptoms or atypical ones so that CAD may not be diagnosed until they experience a myocardial infarction. (Kennedy-Malone 227) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01- 14. VitalBook file. Question 3. Question : A 55-year-old post-menopausal woman with a history of hypertension complains of jaw pain on heavy exertion. There were no complaints of chest pain. Her ECG indicates normal sinus rhythm without ST segment abnormalities. Your plan may include: Student Answer: Echocardiogram Exercise stress test Cardiac catheterization Myocardial perfusion imaging Instructor Explanation: Once all the results of the initial laboratory and ECG testing are reviewed, a pretest probability of disease can be generated and additional tests can be ordered.2 The probability of CAD can be calculated by considering the chosen noninvasive test's sensitivity and specificity.2 Selection of the proper cardiac test (see Table 115-1) for an individual depends on the person's risk stratification, age, and tolerable level of activity. The most common and least invasive test for diagnosis of CAD is the stress test, also called the exercise tolerance test (ETT) or treadmill exercise. (Buttaro 488) Buttaro, Terry, JoAnn Trybulski, Patricia Bailey, Joanne Sandberg-Cook. Primary Care, 4th Edition. Mosby, 2013. VitalBook file. Question 4. Question : Jenny is a 24 year old graduate student that presents to the clinic today with complaints of fever, midsternal chest pain and generalized fatigue for the past two days. She denies any cough or sputum production. She states that when she takes Ibuprofen and rest that the chest pain does seem to ease off. Upon examination the patient presents looking very ill. She is leaning forward and states that this is the most comfortable position for her. Temp is 102. BP= 100/70. Heart rate is 120/min and regular. Upon auscultation a friction rub is audible. Her lung sounds are clear. With these presenting symptoms your initial diagnosis would be: Student Answer: Mitral Valve Prolapse Referred Pain from Cholecystitis Pericarditis Pulmonary Embolus Instructor Explanation: Pericarditis Pericarditis, inflammation of the pericardium, is usually not a solo disease process but is seen in conjunction with other diseases or conditions. Pericarditis may occur as a complication of MI (Dressler's syndrome) or coronary artery bypass surgery. It is also more commonly seen in patients with connective tissue disorders such as rheumatoid arthritis, systemic lupus erythematosus (SLE), scleroderma, and sarcoidosis. Bacterial, viral, or fungal infections, including HIV, are risk factors for pericarditis. Pericarditis can occur with kidney failure or metastatic neoplasias or as a reaction to medication, particularly phenytoin, hydralazine, and procainamide. Rarely, it is idiopathic and the cause unknown, although a common viral infection is suspected. Cardiac tamponade can occur as a serious complication, and it is an emergency requiring immediate pericardiocentesis. Constrictive pericarditis can occur over time due to scarring of the pericardial sac. Signs and Symptoms Unlike the symptoms associated with ACS, the pain accompanying pericarditis is sharp and stabbing; it may worsen with inspiration or when lying flat or leaning forward. Associated symptoms may include shortness of breath, fever, chills, and malaise. (Goolsby 179) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 5. Question : Which symptom is more characteristic of Non-Cardiac chest pain? Student Answer: arm Pain often radiates to the neck, jaw, epigastrium, shoulder, or Pain tends to occur with movement, stretching or palpation Pain usually lasts less than 10 minutes and is relieved by Instructor Explanation: nitroglycerine Pain is aggravated by exertion or stress Palpate chest wall for tenderness and swelling. Chest pain present in only one body position is usually not cardiac in origin. (MSN 194) MSN, Jill C. C., FNP-BC. Family Practice Guidelines: Third Edition, 3rd Edition. Springer Publishing Company, 2014-02-01. VitalBook file. Question 6. Question : What is the most common valvular heart disease in the older adult? Student Answer: Aortic regurgitation Aortic stenosis Mitral regurgitation Mitral stenosis Instructor Explanation: Age: Present in 2% to 9% of persons over age 65, aortic stenosis is the most clinically significant cardiac valve lesion (Faggiano, 2006). Isolated aortic regurgitation is rarely seen and is usually accompanied by some degree of mitral valve involvement. Mitral regurgitation is more common than mitral stenosis in elderly individuals. Mitral valve disease, commonly caused by rheumatic heart disease, is usually acquired by younger patients; however, the effects may not be seen until they are in their forties or fifties. Mitral valve stenosis has a progressively slow course with latent symptoms over 20 to 40 years followed by rapid acceleration in later life. (Kennedy-Malone 259) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Question 7. Question : Jeff, 48 years old, presents to the clinic complaining of fleeting chest pain, fatigue, palpitations, lightheadedness, and shortness of breath. The pain comes and goes and is not associated with activity or exertion. Food does not exacerbate or relieve the pain. The pain is usually located under the left nipple. Jeff is concerned because his father has cardiac disease and underwent a CABG at age 65. The ANP examines Jeff and hears a mid-systolic click at the 4th ICS mid- clavicular area. The ANP knows that this is a hallmark sign of: Student Answer: Angina Pericarditis Mitral valve prolapse Congestive heart failure Instructor Explanation: Mitral valve prolapse Sharp left anterior chest pain, generally occurring in response to stress or emotional events Chest discomfort lasting seconds to days Palpitations and dyspnea Mitral valve click may be noted in systole at left lower sternal border (Buttaro 529) Buttaro, Terry, JoAnn Trybulski, Patricia Bailey, Joanne Sandberg-Cook. Primary Care, 4th Edition. Mosby, 2013. VitalBook file. MVP, also termed click-murmur syndrome, is a variant of mitral regurgitation and occurs in approximately 10% of young women. MVP generally is hemodynamically insignificant and characterized by normal heart size and dynamics, although the process can progress to hemodynamically significant mitral regurgitation. Characteristically, a portion of the mitral valve balloons into the left atrium, giving rise to a midsystolic click followed by a soft grade I murmur that crescendos up to S2. It is high-pitched and is heard best at the apex or left sternal border. Some patients with MVP have only a murmur and no click, and others have only a click and no murmur. (Goolsby 185) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 8. Question : The aging process causes what normal physiological changes in the heart? Student Answer: Instructor Explanation: The heart valve thickens and becomes rigid, secondary to fibrosis and sclerosis Cardiology occurs along with prolapse of the mitral valve and regurgitation Dilation of the right ventricle occurs with sclerosis of pulmonic and tricuspid valves Hypertrophy of the right ventricle The aging process can also have an adverse effect on the cardiac valves. The valves tend to become thick and stiff secondary to arteriosclerosis and atherosclerotic plaques. (Kennedy-Malone 201) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. During the past three decades, with the successful treatment of streptococcal pharyngitis, the etiology has shifted away from rheumatic to calcific. All such cases share a history of 20 to 30years of repetitive mechanical trauma of the blood against the valve, resulting in fibrosis, calcification, and eventually stenosis. This progress of calcification within the valve cusps is usually seen during the latter decades of life. An inflammatory process similar to that affecting the development of atherosclerotic plaques in coronaries may be a possible cause of the progression of AS. It has been noted that early lesions and calcification in AS are comparable to those found in coronary plaques.4 (Buttaro 602) Buttaro, Terry, JoAnn Trybulski, Patricia Bailey, Joanne Sandberg-Cook. Primary Care, 4th Edition. Mosby, 2013. VitalBook file. Question 9. Question : Dan G., a 65-year-old man, presents to your primary care office for the evaluation of chest pain and left-sided shoulder pain. Pain begins after strenuous activity, including walking. Pain is characterized as dull, aching; 8/10 during activity, otherwise 0/10. Began a few months ago, intermittent, aggravated by exercise, and relieved by rest. Has occasional nausea. Pain is retrosternal, radiating to left shoulder, definitely affects quality of life by limiting activity. Pain is worse today; did not go away after he stopped walking. BP 120/80. Pulse 72 and regular. Normal heart sounds, S1 and S2, no murmurs. Which of the following differential diagnoses would be most likely? Student Answer: Musculoskeletal chest wall syndrome with radiation Esophageal motor disorder with radiation Acute cholecystitis with cholelithiasis Coronary artery disease with angina pectoris Instructor Explanation: With a complaint of chest pain, the most life-threatening diagnosis should be ruled out first. A thorough history identifying the quality and quantity of the pain, alleviating and aggravating factors, and associated symptoms assists in raising or lowering your index of suspicion for a myocardial origin of the pain. Age, gender, weight, vital signs, family history, and medical history also assist in diagnosis. Signs and symptoms that are suspicious for myocardial ischemia include substernal chest pain or discomfort that may radiate into the neck or left arm, diaphoresis, nausea, shortness of breath, and perhaps weakness. Chest discomfort that increases with exertion and resolves with rest or nitroglycerin can indicate myocardial ischemia. Chest discomfort that occurs in the early morning or wakes a patient at night can also be cardiac in origin. Chest discomfort or pain at rest is worrisome because it may signify ACS (unstable angina or an acute MI). Atypical symptoms such as jaw pain, fatigue, indigestion, and upper back pain are more common in women, the elderly, and patients with diabetes. (Goolsby 178- 179) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file Question 1 0. Question : A common auscultatory finding in advanced CHF is: Student Answer: Systolic ejection murmur S3 gallop rhythm Friction rub Bradycardia Instructor Explanation: Pathological S3, also called a ventricular gallop, is heard in adults and is associated with decreased myocardial contractility, HF, and volume overload conditions, as can occur with mitral or tricuspid regurgitation. The sound is the same as a physiological S3 and is heard just after S2 with the patient supine or in the left lateral recumbent position. The sound is very soft and can be difficult to hear. (Goolsby 165) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 1 1. Question : Your 35-year-old female patient complains of feeling palpitations on occasion. The clinician should recognize that palpitations are often a sign of: Student Answer: Anemia Anxiety Hyperthyroidism All of the above Instructor Explanation: Occasional palpitations occur physiologically in the majority of the population or as a result of other noncardiac conditions, such as anxiety, exercise, hyperthyroidism, and anemia. They can also occur with VHD, increased or decreased stroke volume, and arrhythmias. The patient may complain of palpitations or skipped beats, or an arrhythmia may be seen on EKG. Patients are often aware if their heart rate is slower or faster than normal or if it is irregular. With some arrhythmias, patients may complain only of fatigue, shortness of breath, weakness, or syncopal episodes. These are common symptoms in patients who have atrial fibrillation, and, if the ventricular response is slow, the patient may be unaware of the arrhythmia. Ask the patient about the frequency and duration of the palpitations and the presence of associated symptoms, such as loss of consciousness, lightheadedness, chest pain, shortness of breath, nausea, or vomiting. (Goolsby 173) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 1 2. Question : The best way to diagnose structural heart disease/dysfunction non- invasively is: Student Answer: Chest X-ray Instructor Explanation: EKG Echocardiogram Heart catheterization Echocardiography is recommended in patients with ventricular arrhythmias who are suspected of having structural heart disease (Zipes et al., 2006). An echocardiogram is used more commonly than magnetic resonance imaging (MRI) or cardiac computed tomography (CT) because it is inexpensive in comparison. The echocardiogram is a useful tool in assessing for valvular disorders, left ventricular function and wall motion, and the ejection fraction. (Kennedy-Malone 203) Kennedy-Malone, Laurie, Kathleen Fletcher, Lori Martin-Plank. Advanced Practice Nursing in the Care of Older Adults. F.A. Davis Company, 2014-01-14. VitalBook file. Question 1 3. Question : During auscultation of the chest, your exam reveals a loud grating sound at the lower anterolateral lung fields, at full inspiration and early expiration. This finding is consistent with: Student Answer: Pneumonia Pleuritis Pneumothorax A and B Instructor Explanation: Adventitious Sounds Description Significance Crackles Coarse, medium, or fine; early, mid-, or late inspiratory Atelectasis, bronchiectasis, congestive heart failure, pulmonary fibrosis Rhonchi, Wheezes Low- or high-pitched; inspiratory or expiratory COPD, acute and chronic bronchitis, asthma, bronchiectasis, pneumonia Friction Rub Loud, grating; late inspiratory–early expiratory Inflamed pleura; pneumonia, pleuritis, malignancy (Goolsby 211) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 1 4. Question : A 75-year-old patient complains of pain and paresthesias in the right foot that worsens with exercise and is relieved by rest. On physical examination you note pallor of the right foot, capillary refill of 4 seconds in the right foot, +1 dorsalis pedis pulse in the right foot, and +2 pulse in left foot. Which of the following is a likely cause of the signs and symptoms? Student Answer: Arterial insufficiency Femoral vein thrombus Venous insufficiency Peripheral neuropathy Instructor Explanation: Intermittent claudication is pain in the leg or foot that becomes worse with exercise and is relieved by rest. The classic signs of peripheral arterial disease include pain, pallor, weak pulse, paresthesias, and palpable coolness. The signs of venous thrombosis are erythema, ropiness, as well as warmth and tenderness along the course of the vein. Edema of the leg and Homan’s sign of the foot are also common. Note any symptoms of intermittent claudication, such as complaints of cramping, aching, or pain in the ankle, calf, or thigh that occur with exercise and are promptly relieved with rest. (Goolsby 200) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 1 5. Question : Your patient complains of a feeling of heaviness in the lower legs daily. You note varicosities, edema, and dusky color of both ankles and feet. Which of the following is the most likely cause for these symptoms? Student Answer: Femoral vein thrombosis Femoral artery thrombus Venous insufficiency Musculoskeletal injury Instructor Explanation: Chronic venous insufficiency can be a long-term complication of venous thrombosis owing to the destruction of valves in the deep veins. The calf muscle pump that returns blood from the lower legs is damaged, increasing ambulatory pressure in the calf veins. A constellation of symptoms is set up: aching or pain in the lower legs, edema, thinning and hyperpigmentation of the skin, superficial varicosities, venous stasis, and ulceration. Ankle edema is often the earliest sign. Other causes of chronic venous insufficiency include trauma, pelvic neoplasm, and occasionally secondary to superficial venous disease. Prompt treatment of DVT with anticoagulants decreases the risk for chronic venous insufficiency. General measures for symptom management include the following: elevation of the legs intermittently during the day and at night, avoidance of prolonged sitting or standing, and support or compression stockings. Wearing an Unna boot is valuable and successful in the treatment of stasis ulcers. (Goolsby 203-204) Goolsby, Mary J., Laurie Grubbs. Advanced Assessment Interpreting Findings and Formulating Differential Diagnoses, 3rd Edition. F.A. Davis Company, 11/2014. VitalBook file. Question 1 6. Question : Your 54 year old patient, Mr. A, presents to your clinic with a 2 day history of severe shoulder pain. On initial assessment you note that in addition to shoulder findings his blood pressure on the ‘good’ arm is 162/100. You review his history and on his last visit his blood pressure was 120/70. He has a medical history of sleep apnea and has used anabolic steroids when body building as a younger adult. In addition to caring for Mr. A’s chief complaint of shoulder pain, you also: Student Answer: Start a thiazide diuretic, discussing the importance of adherence Discuss with him his new diagnosis of hypertension and the importance of taking medication. Schedule a follow up appointment after pain has subsided to take additional blood pressure readings Start an ACE inhibitor because with his history he may also be diabetic. Instructor Explanation: MedU Card #3 Question 1 7. Question : You decide to order labs today to help with the diagnosis and management of hypertension in Mr. A. Which of the following labs are indicated to assist in the medical management of Mr. A if he meets the diagnostic criteria for hypertension? Student Answer: Instructor Explanation: Serum Sodium Thyroid function tests Fasting serum cholesterol panel Complete liver function enzyme panel MedU Card #14 Question 1 8. Question : Lifestyle modifications reduce blood pressure, enhance antihypertensive medication efficacy, and decrease cardiovascular risks. Which lifestyle change will decrease blood pressure the most? Student Answer: Instructor Explanation: Physical activity Dietary sodium reduction DASH diet Weight reduction MedU Card # 15 Question 1 9. Question : Mr. A returns to your clinic and a diagnosis of hypertension is made. He is started on a diuretic and counseled on lifestyle modifications including increasing activity and smoking cessation. On his next visit you note that his blood pressure remains elevated. Before referring to a specialist you should do all of the following except: Student Answer: Instructor Explanation: Assure medications are at appropriate dose Identify any underlying medical condition that requires treatment Review diet with Mr. A and refer to dietician if it is diet problematic Determine he has ‘white coat’ hypertension because his home readings are also elevated MedU Card #22 Question 2 0. Question : Mr. A has many issues that seem to be interfering with his health outcomes. In order to negotiate and formulate a patient-centered management plan you take the time to gather more information. This can be started by asking the following question: Student Answer: Instructor Explanation: What do you think caused your hypertension and how has it affected your life? I see that you are 20 pounds overweight -- do you exercise? Does you wife help you to manage your diet and medication? Taking your blood pressure everyday is important so that I can see what happens each day. Do you do this? MedU Card #23 [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
 (1).png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 18, 2021
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Oct 18, 2021
Downloads
0
Views
38
 (1).png)

.png)


 (1).png)