*NURSING > EXAM > NR 511 Davis Edge- Musculoskeletal Disorders Week 5 Q & A (Download To Score) (All)
NR 511 Davis Edge- Musculoskeletal Disorders Week 5 Q & A (Download To Score)
Document Content and Description Below
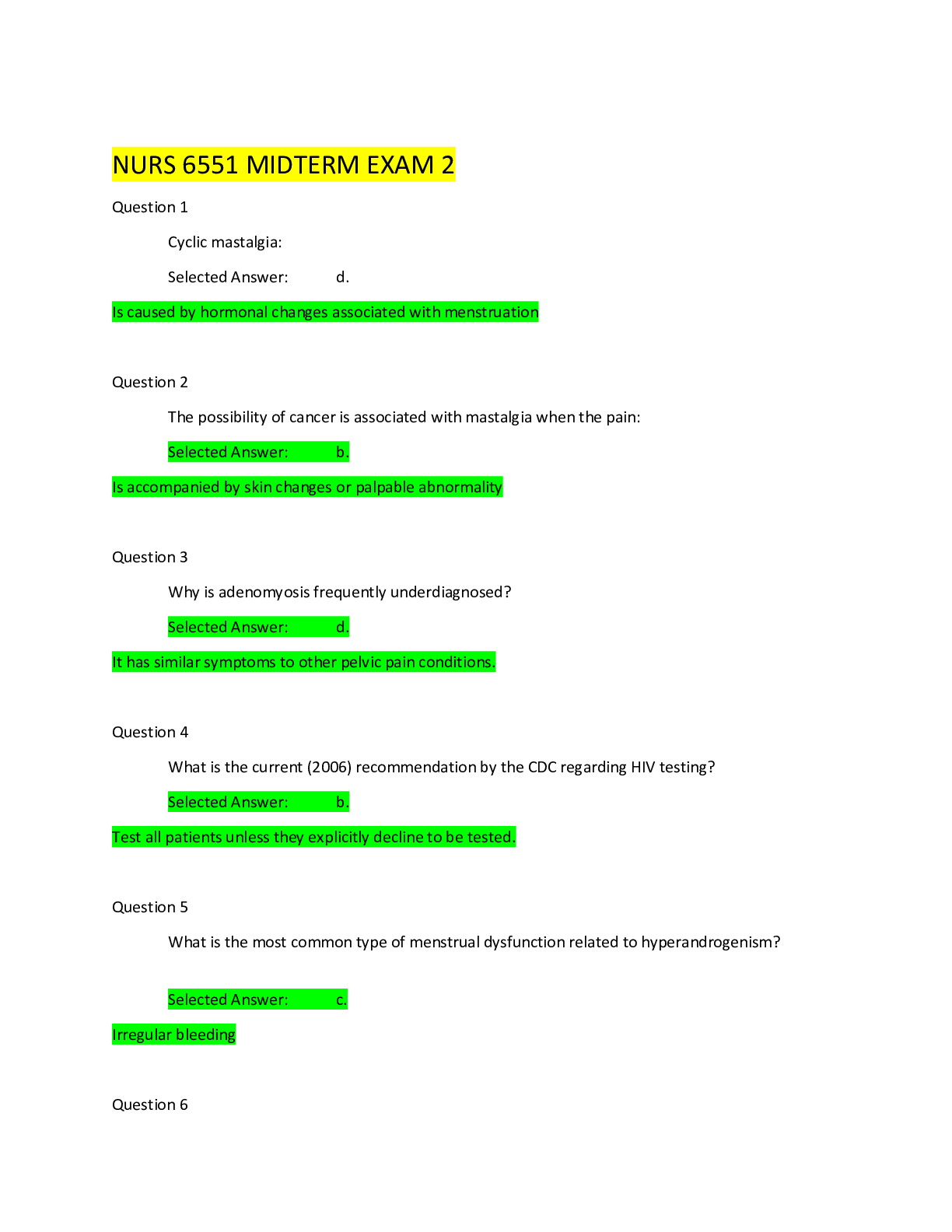
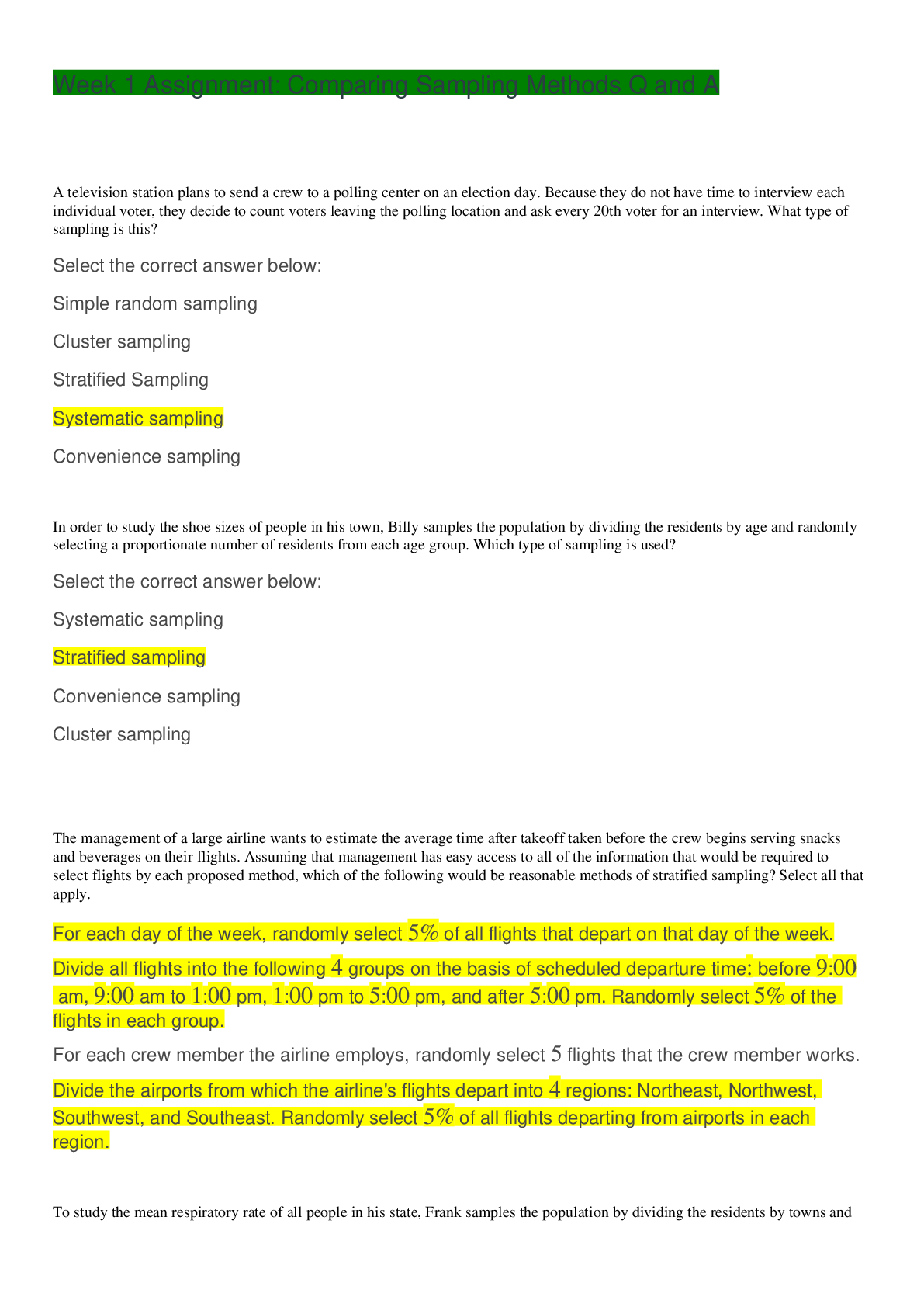
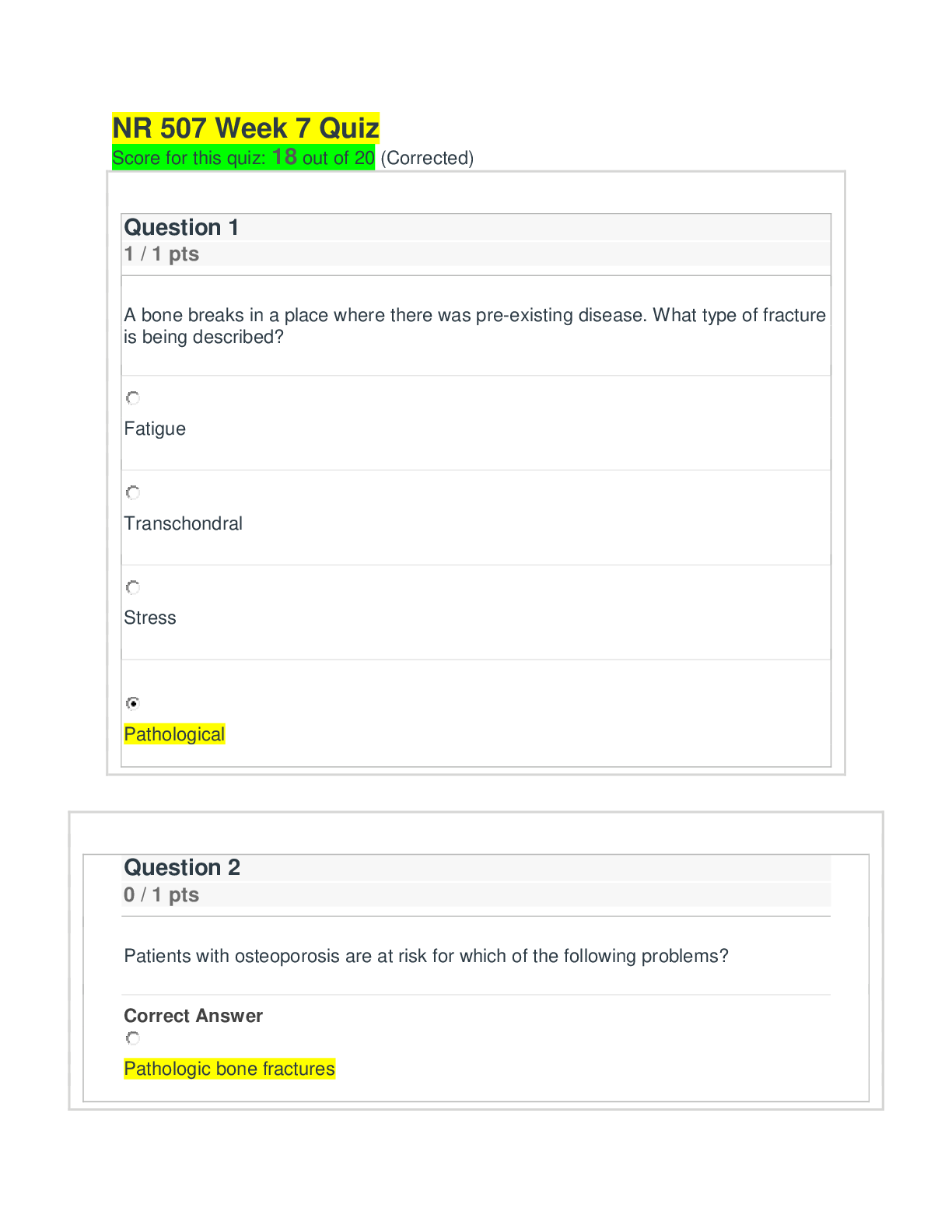
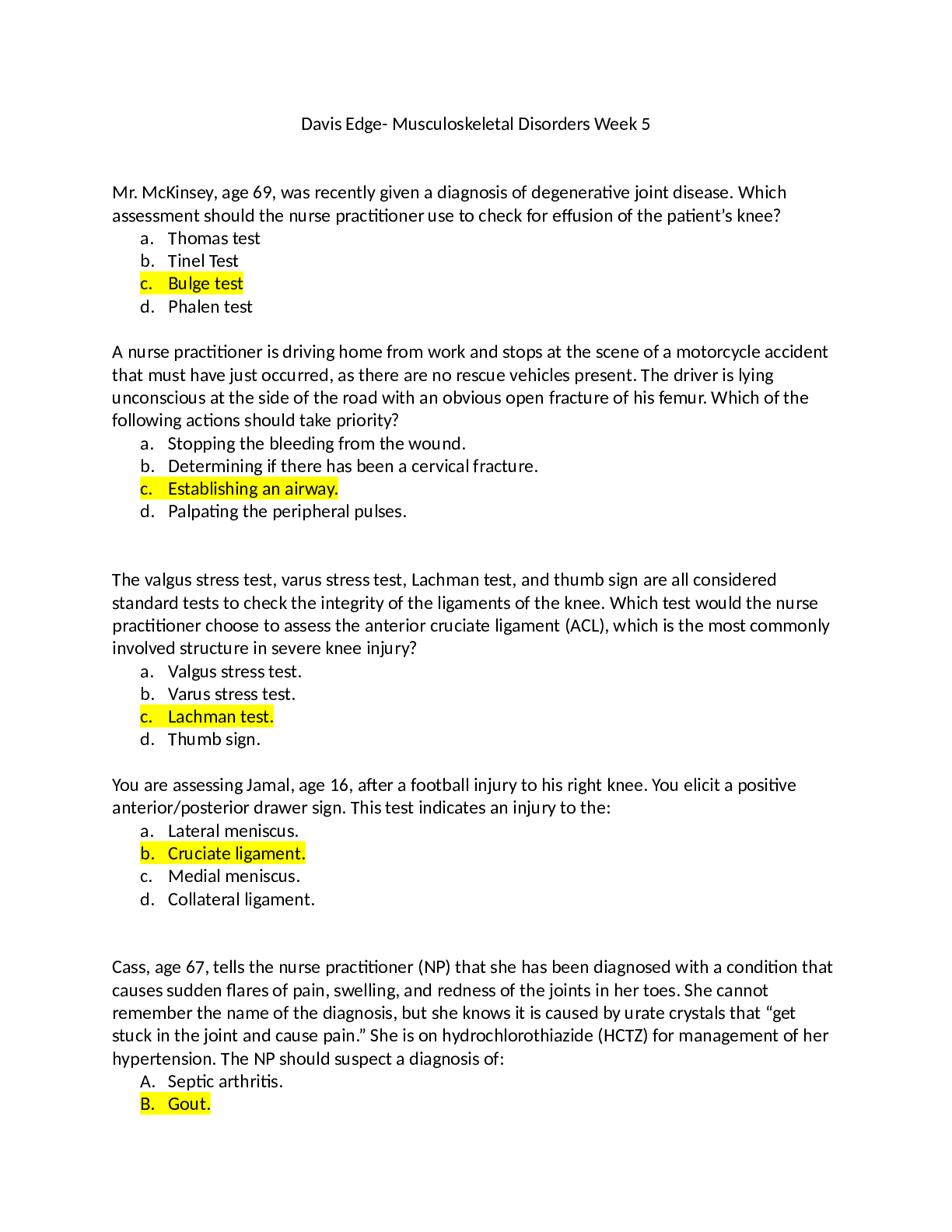
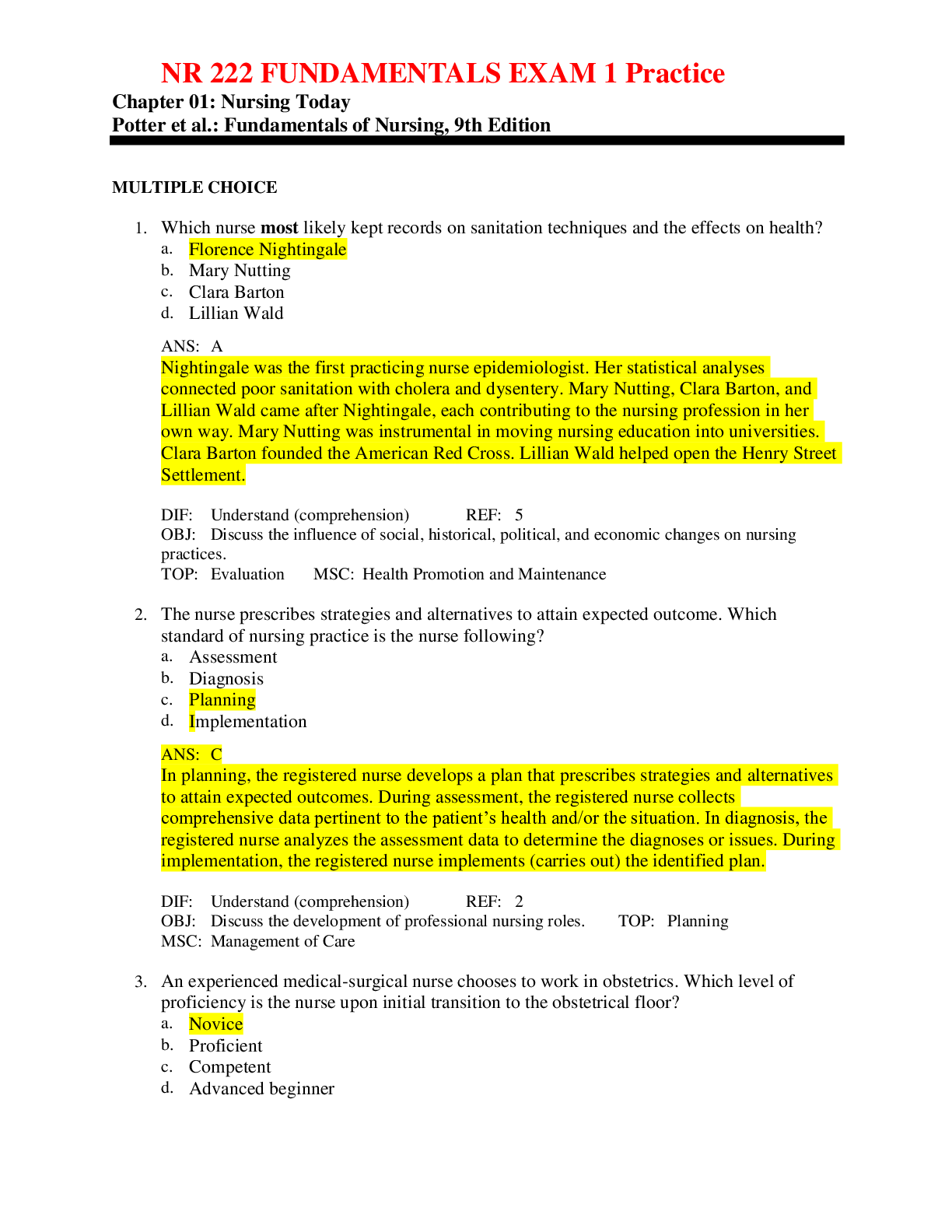
Davis Edge- Musculoskeletal Disorders Week 5 Mr. McKinsey, age 69, was recently given a diagnosis of degenerative joint disease. Which assessment should the nurse practitioner use to check for ef... fusion of the patient’s knee? a. Thomas test b. Tinel Test c. Bulge test d. Phalen test A nurse practitioner is driving home from work and stops at the scene of a motorcycle accident that must have just occurred, as there are no rescue vehicles present. The driver is lying unconscious at the side of the road with an obvious open fracture of his femur. Which of the following actions should take priority? a. Stopping the bleeding from the wound. b. Determining if there has been a cervical fracture. c. Establishing an airway. d. Palpating the peripheral pulses. The valgus stress test, varus stress test, Lachman test, and thumb sign are all considered standard tests to check the integrity of the ligaments of the knee. Which test would the nurse practitioner choose to assess the anterior cruciate ligament (ACL), which is the most commonly involved structure in severe knee injury? a. Valgus stress test. b. Varus stress test. c. Lachman test. d. Thumb sign. You are assessing Jamal, age 16, after a football injury to his right knee. You elicit a positive anterior/posterior drawer sign. This test indicates an injury to the: a. Lateral meniscus. b. Cruciate ligament. c. Medial meniscus. d. Collateral ligament. Cass, age 67, tells the nurse practitioner (NP) that she has been diagnosed with a condition that causes sudden flares of pain, swelling, and redness of the joints in her toes. She cannot remember the name of the diagnosis, but she knows it is caused by urate crystals that “get stuck in the joint and cause pain.” She is on hydrochlorothiazide (HCTZ) for management of her hypertension. The NP should suspect a diagnosis of: A. Septic arthritis. B. Gout. C. Rheumatoid arthritis. D. Charcot neuro-osteoarthropathy. Ethan, age 10, jumped off a 2-foot wall, twisting his foot and ankle upon landing. His ankle x-ray demonstrates a fracture of the distal tibia, over the articular surface, through the epiphysis and physis. Based on the Salter-Harris classification of growth plate injuries, you know this is a: a. Salter-Harris II fracture. b. Salter-Harris III fracture. c. Salter-Harris IV fracture. d. Salter-Harris V fracture. Mrs. Kelly, age 80, has a curvature of the spine. This is likely to indicate which age-related change? a. Lordosis. b. Dorsal kyphosis. c. Scoliosis. d. Kyphoscoliosis. Upon assessment, the nurse practitioner notes unilateral back pain of acute onset that increases when standing and bending. A straight leg raise test is negative. The most likely diagnosis is: a. Herniated nucleus pulposus. b. Muscle strain. c. Osteoarthritis. d. Spondylolisthesis. Joyce, age 87, broke her wrist after falling off a curb. She just had a plaster cast applied to her wrist. In instructing Joyce and her family on allowing the cast to dry properly, tell them to: a. Continuously elevate Joyce’s arm on a pillow. b. Change the position of Joyce’s arm every hour. c. Position a fan near Joyce during the night to ensure even drying of the cast. d. Put a blanket over the cast to absorb the dampness. Anne, age 67, sustained a fall on an outstretched hand. She presents holding her arm against her chest with her elbow flexed. Based on the specific location of her pain, you suspect a radial head fracture. The best initial strategy to assess for a radial head fracture would be: a. To palpate for tenderness, swelling, and crepitus just distal to the lateral epicondyle. b. To palpate for tenderness, swelling, and crepitus along the radial wrist. c. To palpate for tenderness in the “anatomical snuffbox.” d. To order an x-ray of the wrist. Lillian, age 70, was told that she has osteoporosis. When she asks you what this is, you respond that osteoporosis: a. Develops when loss of bone occurs more rapidly than new bone growth. b. Is a degenerative joint disease characterized by loss of cartilage in certain joints. c. Is a chronic inflammatory disorder that affects multiple joints. d. Is a bone disorder that has to do with inadequate mineralization of the bones. Jeffrey, age 16, was involved in a motor vehicle accident. He walks in to the office with an obvious facial fracture and then collapses. What should the first action of the nurse practitioner be? a. Calling his parents for permission to treat. b. Assessing for an adequate airway. c. Obtaining a head and maxillofacial computed tomography (CT). d. Assessing for a septal hematoma. Marsha, age 34, presents with symptoms resembling both fibromyalgia and chronic fatigue syndrome, which have many similarities. Which of the following is more characteristic of fibromyalgia than of chronic fatigue syndrome? a. Musculoskeletal pain. b. Difficulty sleeping. c. Depression. d. Fatigue. The nurse practitioner (NP) is assessing Maya, a 69-year-old Asian woman, for the first time. When trying to differentiate between scoliosis and kyphosis, the NP recalls that kyphosis involves: a. Asymmetry of the shoulders, scapulae, and waist creases. b. A lateral curvature and vertebral rotation on posteroanterior x-rays. c. One leg appearing shorter than the other. d. A posterior rounding at the thoracic level. Alexander, age 12, sprained his ankle playing ice hockey. He is confused as to whether he should apply heat or cold. What should the nurse practitioner tell him? a. “Use continuous heat for the first 12 hours and then use heat or cold to your own preference.” b. “Use continuous cold for the first 12 hours and then use heat or cold to your own preference.” c. “Apply cold for 20 minutes, then remove it for 30 to 45 minutes; repeat this for the first 24 to 48 hours while awake.” d. “Alternate between cold and heat for 20 minutes each for the first 24 to 48 hours.” The nurse practitioner (NP) suspects a herniated disk in a 72-year-old patient. The NP elevates the patient’s affected leg when she is in the supine position, and it elicits back and sciatic nerve pain, which indicates a positive test. This is known as which test or sign? a. Femoral stretch test. b. Crossed straight leg raise test. c. Doorbell sign. d. Straight leg raise test. June, age 67, presents with back pain with no precipitating event. The pain is located over her lower back muscles and spine, without sciatica, and it is aggravated by sitting, standing, and certain movements. It is alleviated with rest. Palpation localizes the pain, and muscle spasms are felt. There was an insidious onset with progressive improvement. What is the most likely diagnosis? a. Ankylosing spondylitis. b. Musculoskeletal strain. c. Spondylolisthesis. d. Herniated disk. Hilda, age 73, presents with a complaint of low back pain. Red flags in her history of a minor fall, osteopenia, and prolonged steroid use for systemic lupus erythematosus suggest the possibility of which of the following serious underlying conditions as the cause of her low back pain? a. Cancer. b. Cauda equina syndrome. c. Neurologic compromise. d. Spinal fracture. Mickey, age 18, is on a chemotherapeutic antibiotic for a musculoskeletal neoplasm. Which drug do you think he is taking? a. Cyclophosphamide (Cytoxan). b. Doxorubicin (Adriamycin). c. Methotrexate (Rheumatrex). d. Cisplatin (Platinol). A nurse practitioner is trying to distinguish between an articular and a nonarticular musculoskeletal complaint in a 26-year-old patient complaining of pain in the elbow area. Which of the following would characterize nonarticular bursitis? a. Deep or diffuse pain. b. Limited range of motion (ROM) on active and passive movement. c. Point or focal tenderness. d. Swelling and instability. The nurse practitioner suspects adolescent idiopathic scoliosis in Victoria, age 15, who is in her “growth spurt.” An Adams forward bend test is performed, and it is noted that the patient has a right-sided rib hump. What is this indicative of? a. Right lumbar shifting. b. Right thoracic curvature. c. Right truncal shift. d. Spondylolysis Paul has a malignant fibrosarcoma of the femur. He recently had surgery and is now on radiation therapy. You want to order a test to determine the extent of the tumor invasion of the surrounding tissues and the response of the bone tumor to the radiation. Which of the following tests should you order? A. An x-ray. B. A magnetic resonance imaging (MRI) scan. C. A computed tomography (CT) scan. D. A needle biopsy. When teaching Alice, age 77, to use a cane because of osteoarthritis of her left knee, an important point to stress is: a. Carrying the cane in the ipsilateral hand. b. Advancing the cane with the ipsilateral leg. c. Making sure the cane length equals the height of the iliac crest. d. Using the cane to aid in joint protection and safety. Anne Marie states she has a maternal history of rheumatoid disease, but she has never been affected. Today she presents with complaints of dryness of the eyes and mouth. What is the most likely diagnosis? a. Rheumatoid arthritis (RA). b. Systemic lupus erythematosus (SLE). c. Sjögren syndrome. d. Rosacea. Greg, age 26, runs marathons and frequently complains of painful contractions of his calf muscles after running. You attribute this to: a. Hypercalcemia. b. Hyponatremia. c. Heat exhaustion. d. Dehydration. The nurse practitioner is considering a diagnosis of calcium pyrophosphate deposition disease (CPPD), or pseudogout, in a 72-year-old man who presents with complaints of pain and stiffness in his wrists and knees. The most useful diagnostic tests to assist in confirming this diagnosis would be: A. Synovial fluid analysis and x-ray. B. Bacterial cultures. C. Bone scan and magnetic resonance imaging (MRI). D. Anticitrullinated protein antibodies (ACPA) and rheumatoid factor (RF). Matthew, age 52, is a chef who just severed 2 of his fingers with a meat cutter. You would recommend that he: a. Wrap the severed fingers tightly in a dry towel for transport to the emergency department with him. b. Leave the severed fingers at the scene because fingers cannot be reattached. c. Immediately freeze the severed fingers for reattachment in the near future. d. Wrap the fingers in a clean, damp cloth; seal them in a plastic bag; and place the bag in an ice water bath. Sean, a factory line worker, has osteoarthritis (OA) of the right hand. According to the American College of Rheumatology (ACR), the guidelines for pharmacologic treatment include: a. Acetaminophen, tramadol, and intra-articular corticosteroid injections. b. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), tramadol, and articular corticosteroid injections. c. Acetaminophen, topical capsaicin, and topical nonsteroidal anti-inflammatory drugs (NSAIDs). d. Topical capsaicin, topical nonsteroidal anti-inflammatory drugs (NSAIDs), and oral NSAIDs. The nurse practitioner is considering a diagnosis of calcium pyrophosphate deposition disease (CPPD), or pseudogout, in a 72-year-old man who presents with complaints of pain and stiffness in his wrists and knees. The most useful diagnostic tests to assist in confirming this diagnosis would be: a. Synovial fluid analysis and x-ray. b. Bacterial cultures. c. Bone scan and magnetic resonance imaging (MRI). d. Anticitrullinated protein antibodies (ACPA) and rheumatoid factor (RF). For an adult patient with a knee injury, the nurse practitioner orders a nonsteroidal anti- inflammatory drug (NSAID) to be taken on a routine basis for the next 2 weeks. Patient teaching should include which of the following? a. “You may take this medication on an empty stomach as long as you eat within two to three hours of taking it.” b. “If one pill does not seem to help, you can double the dose for subsequent doses.” c. “If you notice nausea, vomiting, or black or bloody stools, take the next dose with a glass of milk or a full meal.” d. “If you have additional pain, an occasional acetaminophen (Tylenol) is permitted in between the usual doses of the NSAID.” A 13-year-old obese (body mass index [BMI] above the 95th percentile) boy reports low-grade left knee pain for the past 2 months. He denies antecedent trauma but admits to frequent “horseplay” with his friends. The pain has progressively worsened, and he is now unable to bear weight at all on his left leg. His current complaints include left groin, thigh, and medial knee pain and tenderness. His examination demonstrates negative drawer, Lachman, and McMurray tests; left hip with decreased internal rotation and abduction; and external hip rotation with knee flexion. Based on the above scenario, the nurse practitioner should suspect: A. A left meniscal tear. B. A left anterior cruciate ligament (ACL) tear. C. A slipped capital femoral epiphysis (SCFE). D. Osgood-Schlatter disease. During assessment of a client’s foot, the nurse practitioner notes that the foot is in alignment with the long axis of the lower leg and that weight-bearing falls on the middle of the foot from the heel, along the midfoot, to between the second and third toes. These findings best describe: a. A normal foot. b. Hallux valgus. c. Talipes equinovarus. d. Hammertoes. Sam, age 50, presents with Paget disease that has been stable for several years. Recently, his serum alkaline phosphatase level has been steadily rising. The nurse practitioner determines that it is time to start him on pharmacologic management. Which of the following should she initially prescribe? A. Nonsteroidal anti-inflammatory drugs (NSAIDs). B. Corticosteroids. C. Bisphosphonates. D. Calcitonin. You are caring for a patient who has a history of psoriasis and is now showing signs of joint involvement. Seropositivity provides a definitive diagnosis of psoriatic arthritis (PsA). The initial treatment choice for management of the patient is: a. Disease-modifying antirheumatic drugs (DMARDs). b. Nonsteroidal anti-inflammatory drugs (NSAIDs). c. Tumor necrosis factor-alpha (TNF-α) inhibitors. d. Uricosuric medications. A 55-year-old patient presents with complaints of paresthesias in the lower lateral arm, thumb, and middle finger. The nerve roots most commonly related to these symptoms are C6 and C7. The most likely diagnosis would be: a. Brachial plexus neuritis. b. Cervical radiculopathy c. Peripheral polyneuropathy. d. Thoracic outlet syndrome. June, age 67, presents with back pain with no precipitating event. The pain is located over her lower back muscles and spine, without sciatica, and it is aggravated by sitting, standing, and certain movements. It is alleviated with rest. Palpation localizes the pain, and muscle spasms are felt. There was an insidious onset with progressive improvement. What is the most likely diagnosis? a. Ankylosing spondylitis. b. Musculoskeletal strain. c. Spondylolisthesis. d. Herniated disk. Sandra, a computer programmer, has just been given a new diagnosis of carpal tunnel syndrome. The nurse practitioner’s next step is to: a. Refer her to a hand surgeon. b. Take a more complete history. c. Try neutral position wrist splinting and order an oral nonsteroidal anti-inflammatory drug (NSAID). d. Order nerve conduction studies and electromyography (EMG). Janine, age 69, has class III rheumatoid arthritis. According to the American Rheumatism Association, which of the following describes her ability to function? a. Adequate for normal activities despite a handicap of discomfort or limited motion of one or more joints. b. Largely or wholly incapacitated, bedridden, or confined to a wheelchair, permitting little or no self-care. c. Completely able to carry out all usual duties without handicap. d. Adequate to perform only a few or none of the duties of usual occupation or self-care. James, age 17, has been complaining of a painful knob below his right knee that has prevented him from actively participating in sports. He has recently been given a diagnosis of Osgood- Schlatter disease and asks you about his treatment options. The nurse practitioner should tell him that the initial treatment is: a. Relative rest; he could benefit from hamstring, heel cord, and quadriceps stretching exercises. b. Immobilization; a long-leg knee immobilizer is recommended. c. Surgical intervention; removal of the bony fragments is necessary. d. Bed rest for 1 week. Daniel, age 45, is of Northern European ancestry and has a dysfunctional and disfiguring condition affecting the palmar tissue under the skin of the distal palm and fourth and fifth fingers. What do you suspect? a. Hallux valgus. b. De Quervain tenosynovitis. c. Dupuytren contracture. d. Hallux rigidus. 5, age 49, comes in with low back pain. An x-ray of the lumbosacral spine is within normal limits. Which of the following diagnoses do you explore further? a. Scoliosis. b. Osteoarthritis. c. Spinal stenosis. d. Herniated nucleus pulposus. Jill, age 49, has recently begun a rigorous weightlifting regimen. She presents to the primary care office with a shoulder dislocation. Which of the following clinical manifestations leads the nurse practitioner to suspect an anterior shoulder dislocation over a posterior dislocation? A. Inability to shrug the shoulder. B. Absence of pain. C. Inability to rotate the shoulder externally. D. Shortening of the arm. In assessing a patient, you place the tips of your first 2 fingers in front of each ear and ask the patient to open and close his mouth. Then you drop your fingers into the depressed area over the joint and assess for smooth motion of the mandible. With this action, you are checking for: a. Maxillomandibular integrity. b. Well-positioned permanent teeth or well-fitting dentures. c. Temporomandibular joint syndrome. Mastoid inflammation. Hilda, age 73, presents with a complaint of low back pain. Red flags in her history of a minor fall, osteopenia, and prolonged steroid use for systemic lupus erythematosus suggest the possibility of which of the following serious underlying conditions as the cause of her low back pain? a. Cancer. b. Cauda equina syndrome. c. Neurologic compromise. d. Spinal fracture. Karen, who is postmenopausal, is taking 1200 mg of calcium daily but does not understand why she also needs to take vitamin D. You tell her that: a. A deficiency of vitamin D results in inadequate mineralization of bone matrix. b. All vitamins need to be supplemented. c. Vitamin D increases intestinal absorption of dietary calcium and mobilizes calcium from the bone. d. Vitamin D binds with calcium to allow active transport into the cells. Alexander, age 12, sprained his ankle playing ice hockey. He is confused as to whether he should apply heat or cold. What should the nurse practitioner tell him? a. “Use continuous heat for the first 12 hours and then use heat or cold to your own preference.” b. “Use continuous cold for the first 12 hours and then use heat or cold to your own preference.” c. “Apply cold for 20 minutes, then remove it for 30 to 45 minutes; repeat this for the first 24 to 48 hours while awake.” d. “Alternate between cold and heat for 20 minutes each for the first 24 to 48 hours.” Sandy, age 49, presents with loss of anal sphincter tone, impaired micturition, incontinence, and progressive loss of strength in the legs. You suspect cauda equina syndrome. What is your next action? a. Ordering physical therapy. b. Ordering a lumbosacral x-ray. c. Ordering extensive lab work. d. Referring to a neurosurgeon. Lois, age 52, who has just been given a diagnosis of sarcoidosis, has joint symptoms, including arthralgias and arthritis. Your next plan of action would be to: a. Order a bone scan. b. Obtain a tissue biopsy. c. Begin a course of glucocorticoids. d. Order daily doses of vitamin B. A 55-year-old patient is able to complete range of motion (ROM) against gravity with some resistance. The nurse practitioner would assign which of the following numerical grades to this manual muscle testing description? a. 5. b. 4. c. 3. d. 2. Week 5 Question 1 slipped capital femoral epiphysis https://www.youtube.com/watch?v=l0zT2- wDiIQ&feature=youtu.be&fbclid=IwAR1oo2GKohIPPO5pip- RwNcdSeSlrFKvzkJqVhTi2hhjr_IomDgJWQoz5ZY Week 5 question 2 supination vs pronation https://www.youtube.com/watch?v=OU1fxuHSQ38&feature=youtu.be&fbclid=IwAR0i91a2YRI- gRPPQ5Gbfy24E3c773LRFGG0c2akTkhBjMe5nS7KTlCMkzQ week 5 question 3 --- has to do with GOUT, which is not in this weeks reading. "urate crystals get stuck in joint" should cause you to think of the correct answer---gout...... but if you want some info on gout here is a good video https://www.youtube.com/watch? v=bznoU5bke4U&feature=youtu.be&fbclid=IwAR1oo2GKohIPPO5pip- RwNcdSeSlrFKvzkJqVhTi2hhjr_IomDgJWQoz5ZY week 5 question 4---- again not covered in the reading---but first aid basics states that a severed body part is wrapped in damp gauze sealed in plastic and placed on ice. https://www.youtube.com/watch?v=ESx4Z6Eq3PU&feature=youtu.be&fbclid=IwAR14tiN- lf5sfw_0Zt6tad1eDcWF2v3B2oHGcaisIlMKzYg1ivMSvR0NACo week 5 question 5-- again not in week 5 reading--here is what i found in the book-- There appears to be significant overlap between CFS and fibromyalgia syndrome (FMS), another controversial chronic pain syndrome. Most patients with CFS meet criteria for FMS, and at least 70% of patients with FMS meet criteria for CFS. Moreover, both disorders have been widely recognized in persons with comorbid psychiatric illness, because nearly two-thirds of CFS patients and one-third of FMS patients meet criteria for depression, or anxiety disorders. For a diagnosis of FMS to be made, the patient must have widespread muscular pain that has been present for at least 3 months. The pain should be present in at least 11 of 18 tender points on digital palpation with an applied pressure Week 5 Question 6 Lordosis, kyphosis & scoliosis https://www.youtube.com/watch? v=DOi24AH5yiE&feature=youtu.be&fbclid=IwAR2G_AWHBwlWNtevTvzg_BQ3Pk BuS6PB0mMhR9QxGITDb4aFbd_iCxI77WY [Show More]
Last updated: 1 year ago
Preview 1 out of 12 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 11, 2021
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Nov 11, 2021
Downloads
0
Views
57



.png)