*NURSING > STUDY GUIDE > NR 511 Week 3 Case Study Discussion Part One 2020 (All)
NR 511 Week 3 Case Study Discussion Part One 2020
Document Content and Description Below
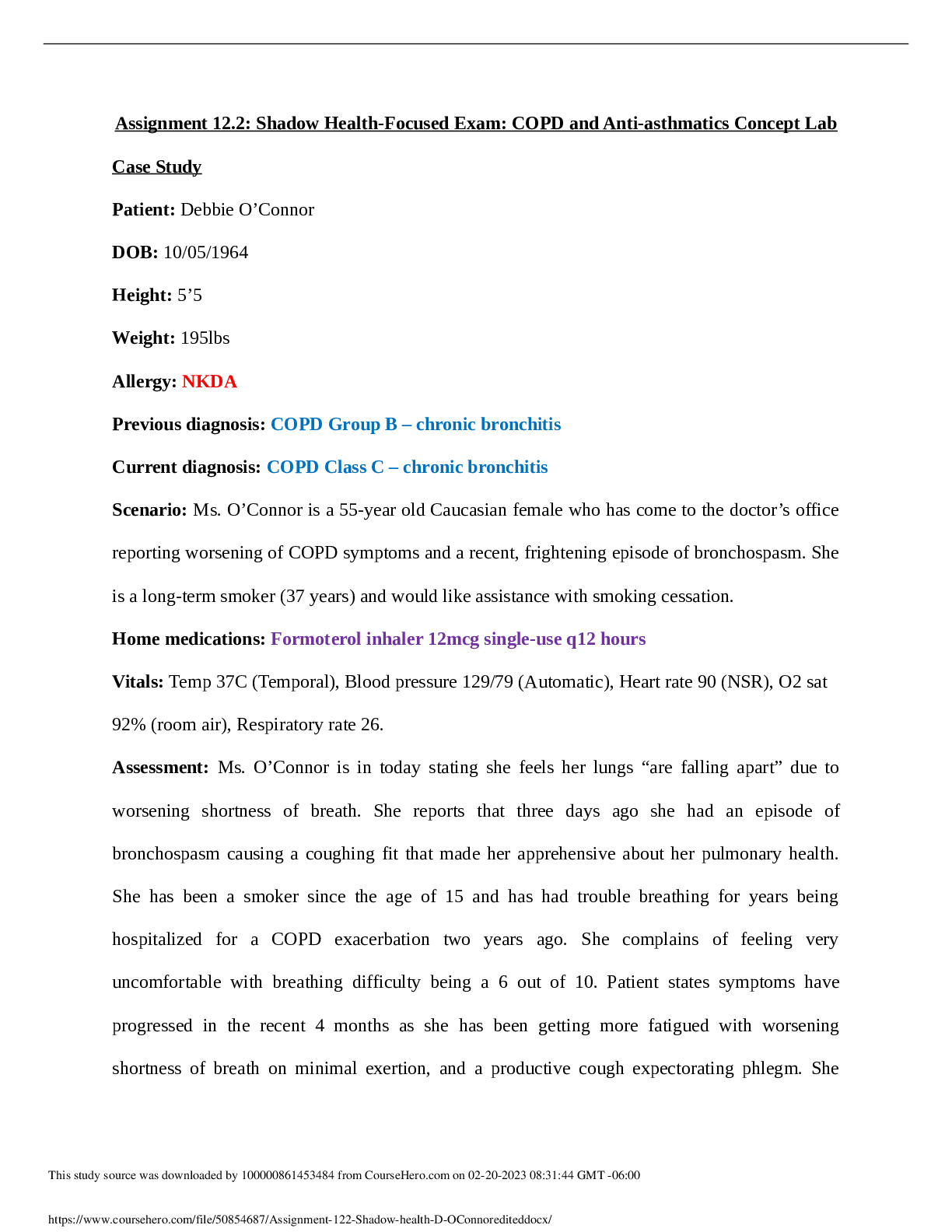
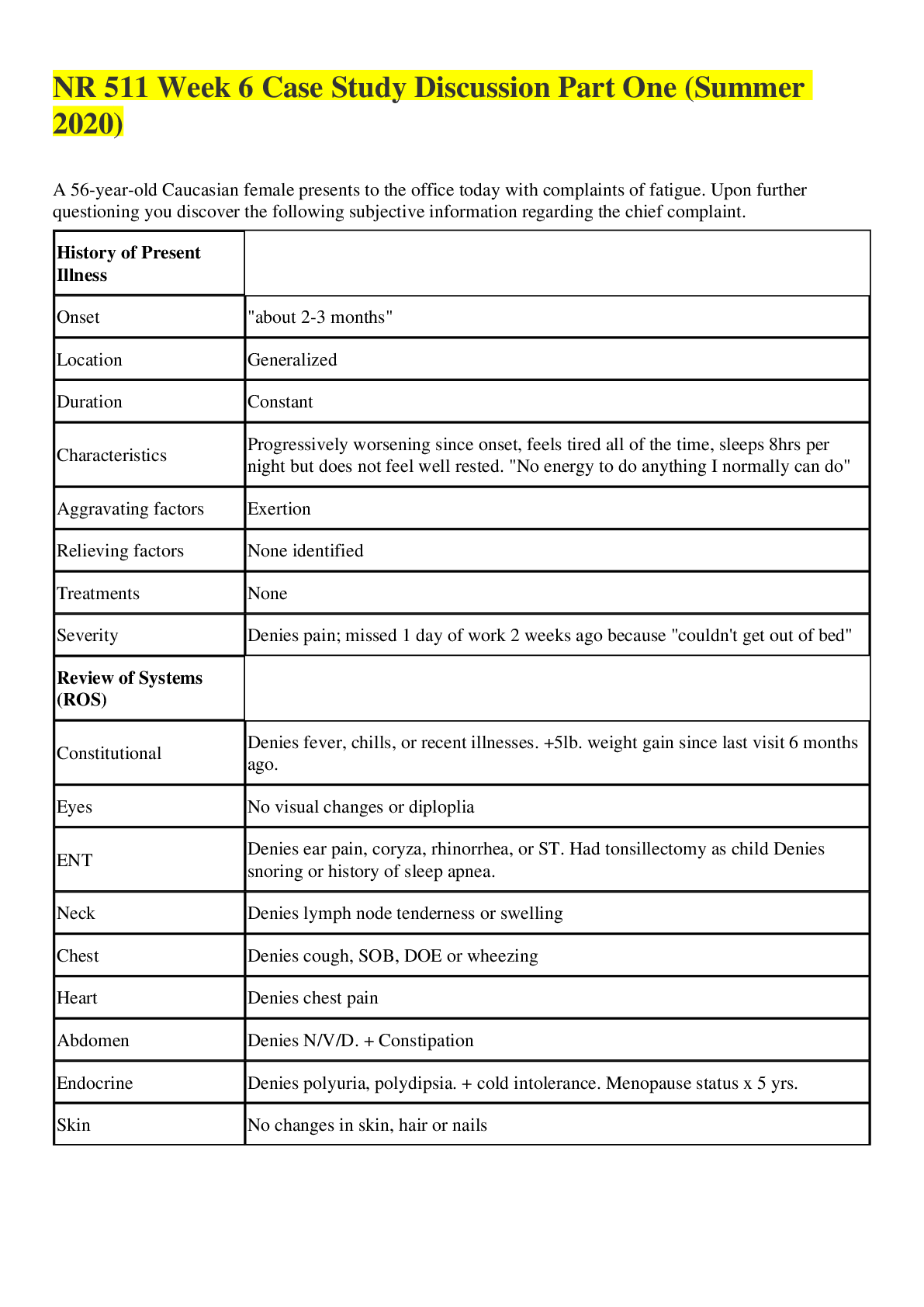
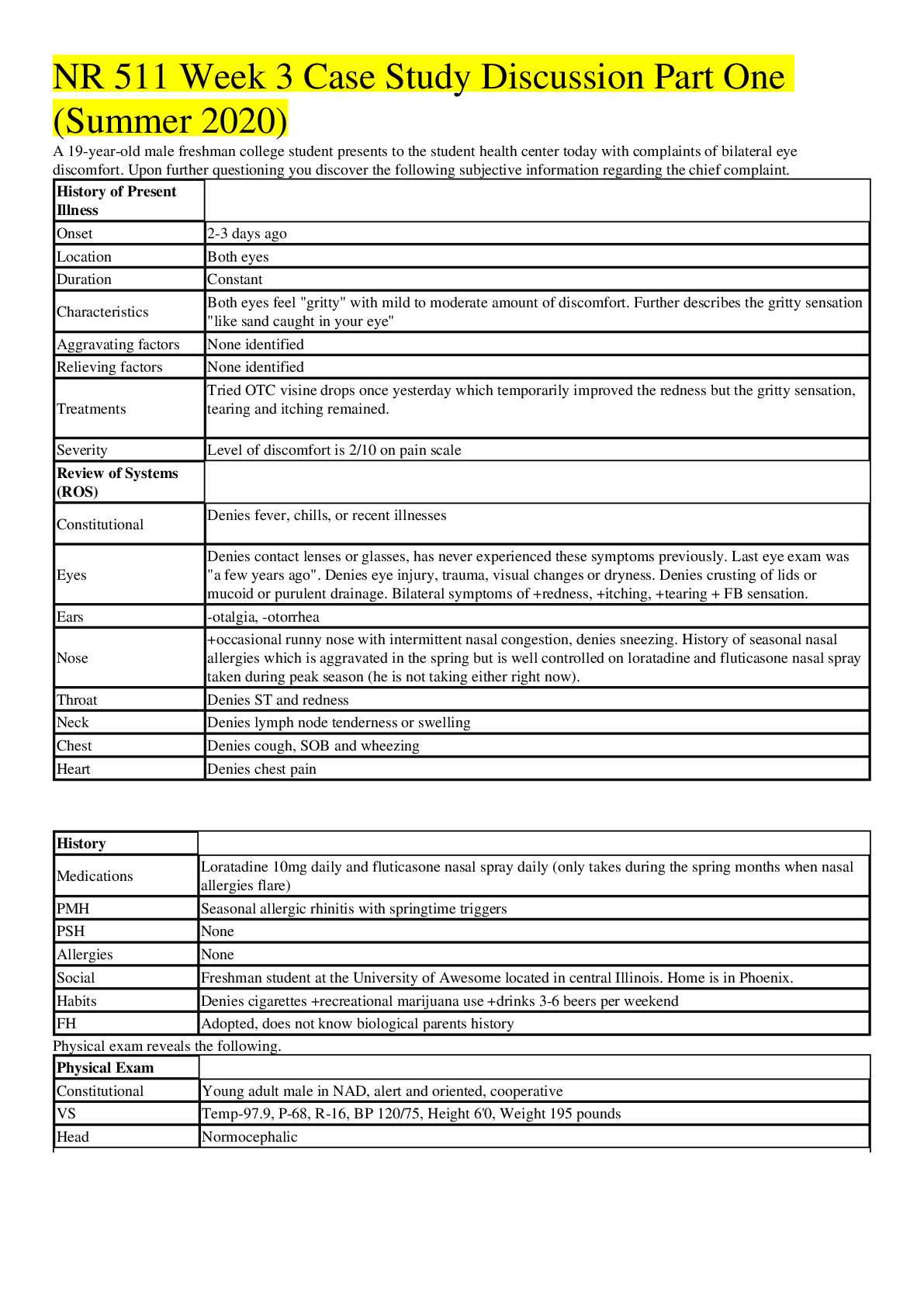
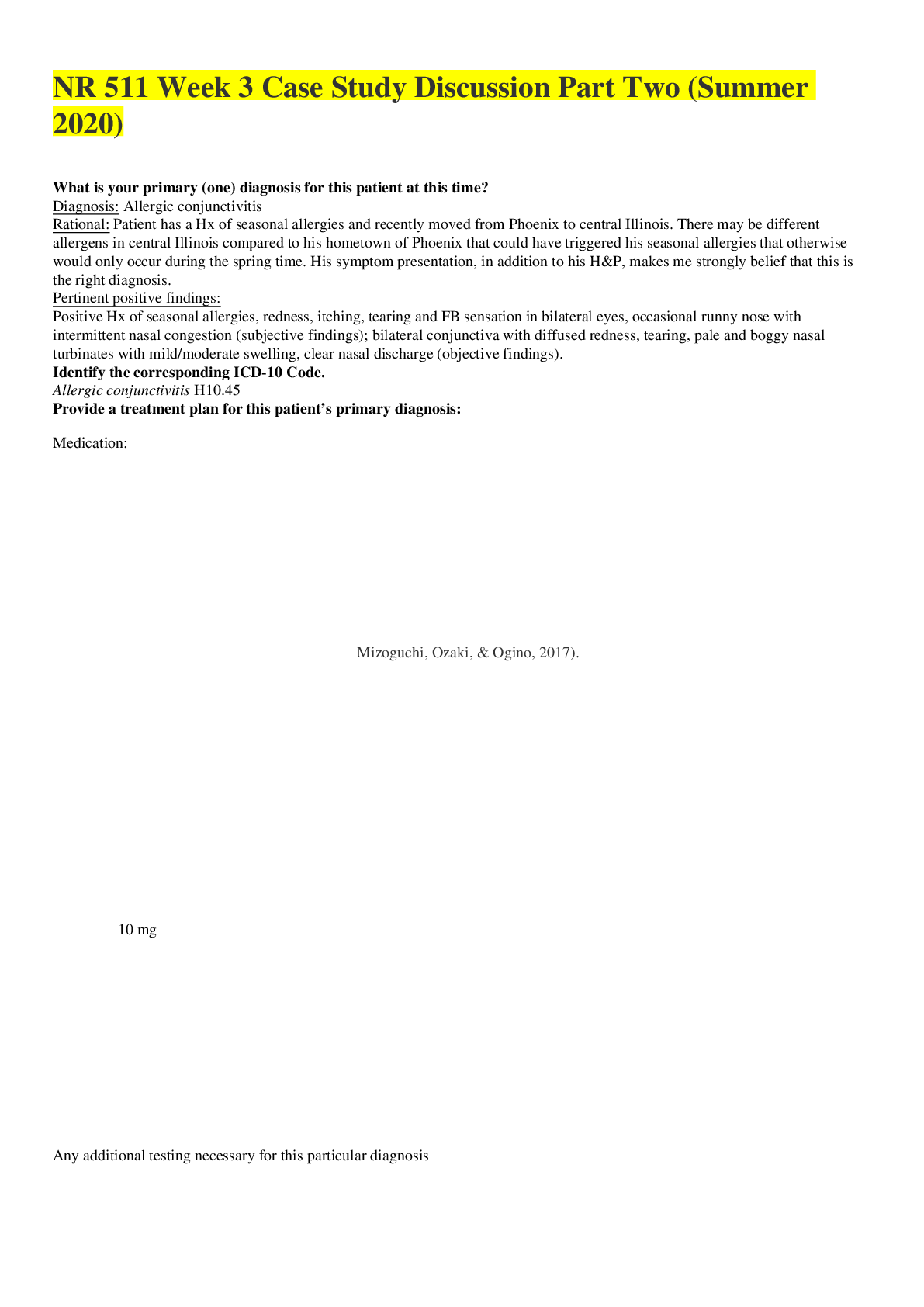
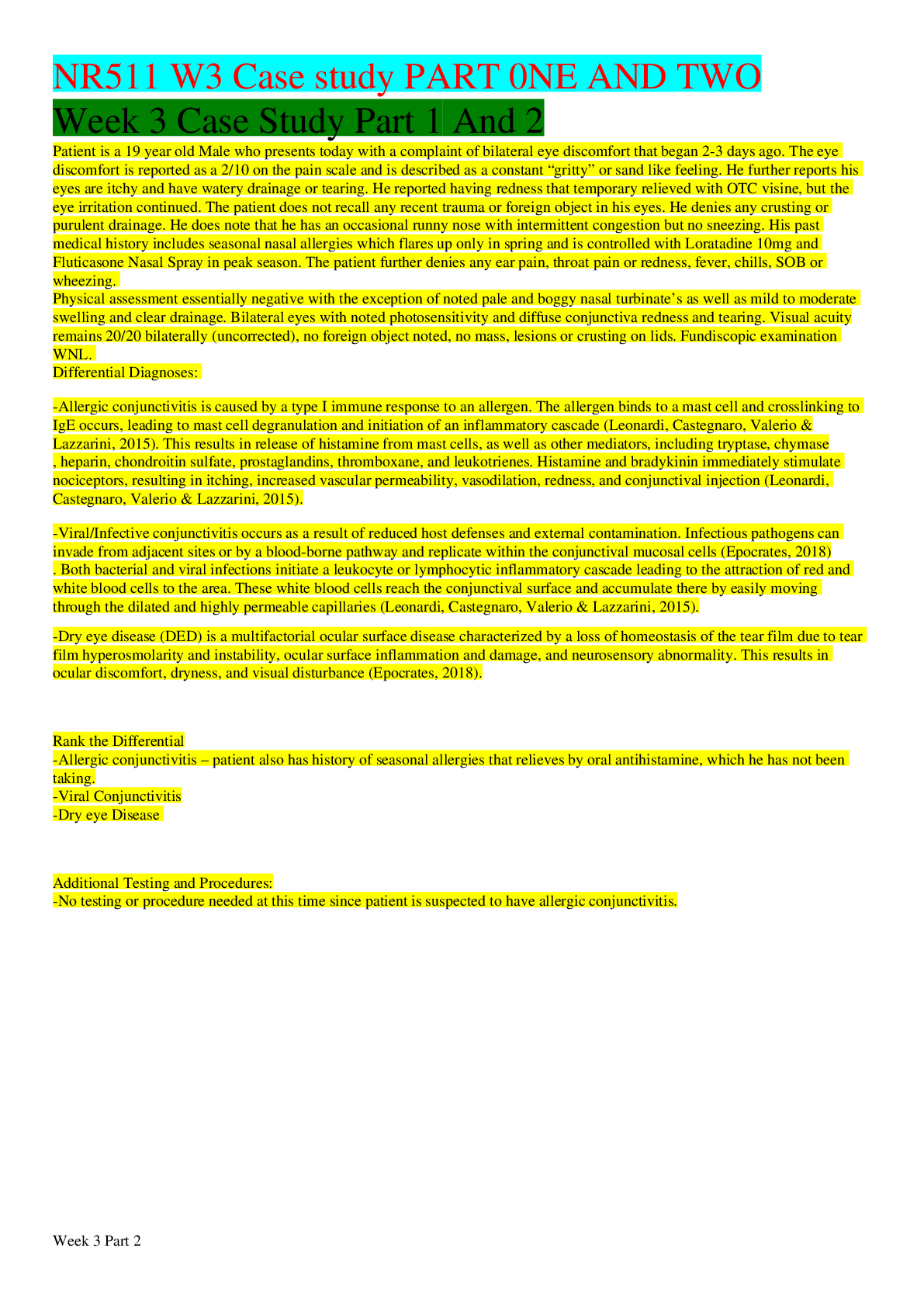
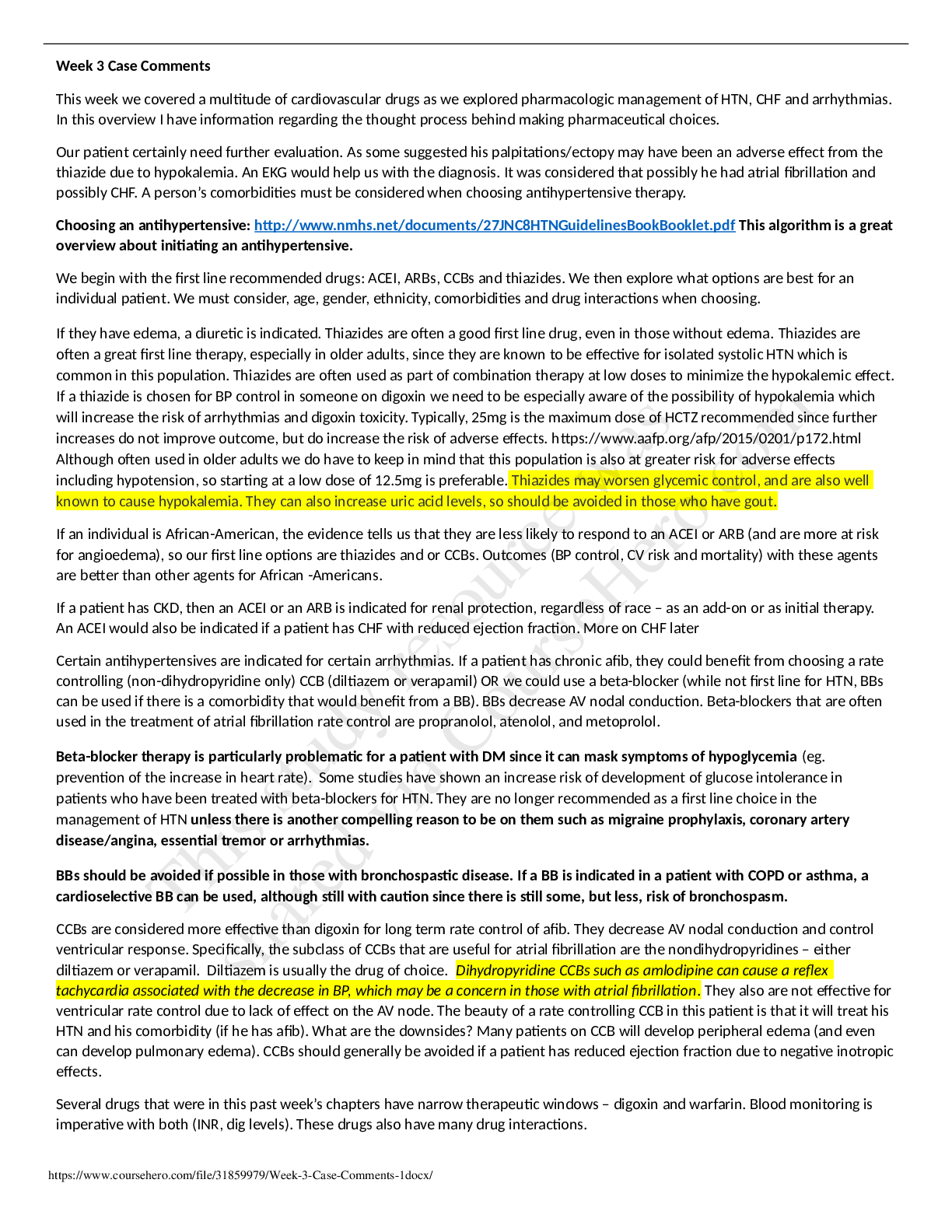
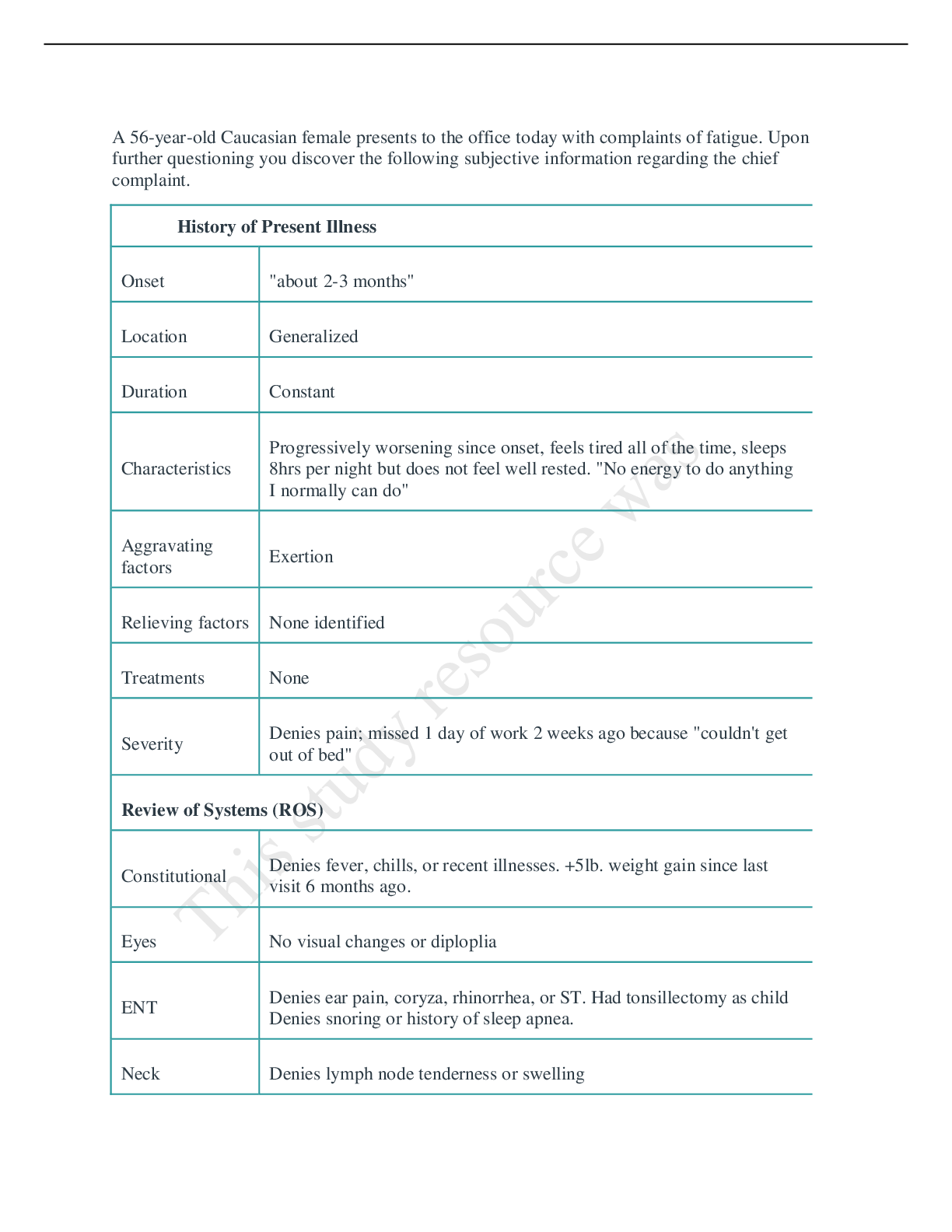
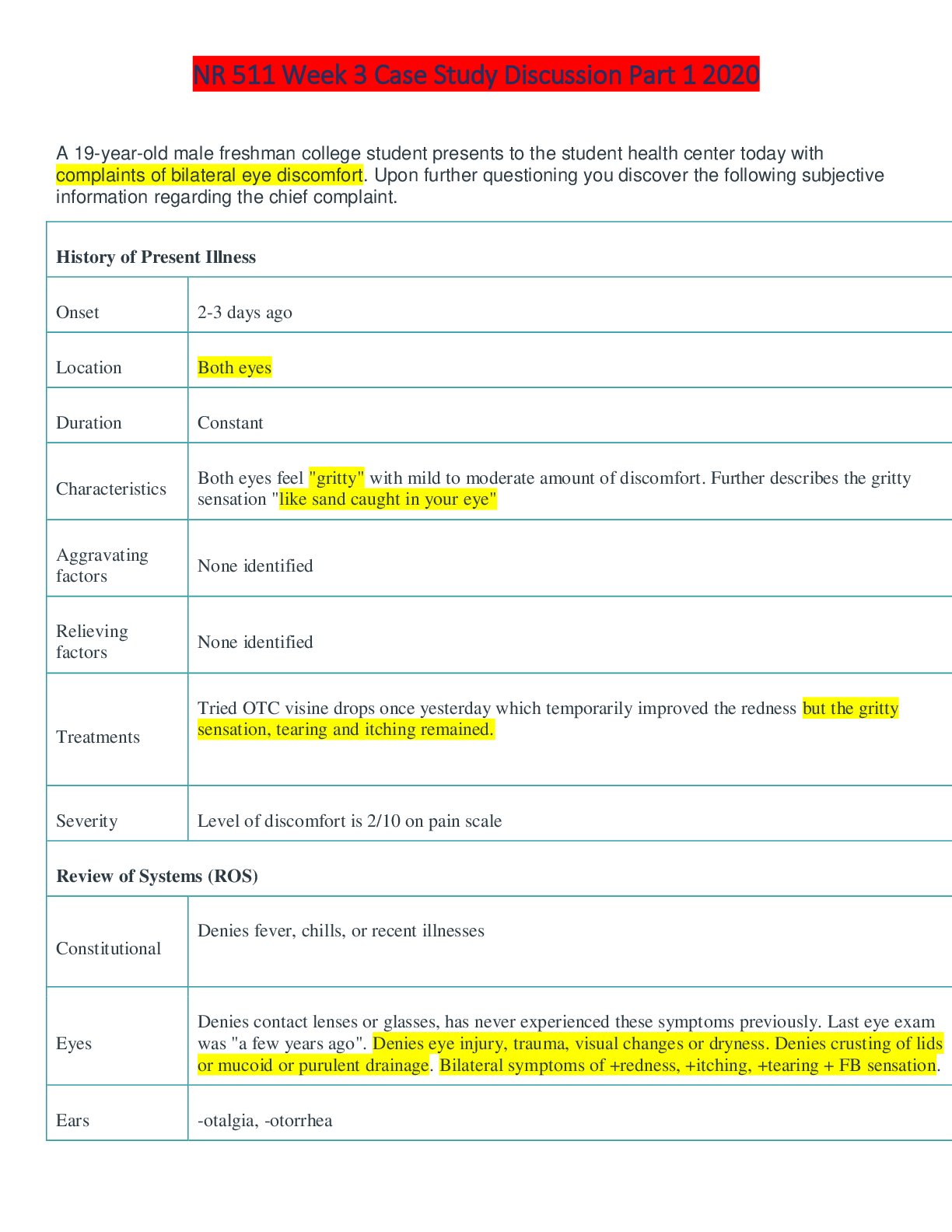
NR 511 Week 3 Case Study Discussion Part One r 2020 GRADED A NR 511 Week 3 Case Study Discussion Part One (Summer 2020) A 19-year-old male freshman college student presents to the student health cent... er today with complaints of bilateral eye discomfort. Upon further questioning you discover the following subjective information regarding the chief complaint. History of Present Illness Onset 2-3 days ago Location Both eyes Duration Constant Characteristics Both eyes feel "gritty" with mild to moderate amount of discomfort. Further describes the gritty sensation "like sand caught in your eye" Aggravating factors None identified Relieving factors None identified Treatments Tried OTC visine drops once yesterday which temporarily improved the redness but the gritty sensation, tearing and itching remained. Severity Level of discomfort is 2/10 on pain scale Review of Systems (ROS) Constitutional Denies fever, chills, or recent illnesses Eyes Denies contact lenses or glasses, has never experienced these symptoms previously. Last eye exam was "a few years ago". Denies eye injury, trauma, visual changes or dryness. Denies crusting of lids or mucoid or purulent drainage. Bilateral symptoms of redness, itching, tearing FB sensation. Ears -otalgia, -otorrhea Nose occasional runny nose with intermittent nasal congestion, denies sneezing. History of seasonal nasal allergies which is aggravated in the spring but is well controlled on loratadine and fluticasone nasal spray taken during peak season (he is not taking either right now). Throat Denies ST and redness Neck Denies lymph node tenderness or swelling Chest Denies cough, SOB and wheezing Heart Denies chest pain History Medications Loratadine 10mg daily and fluticasone nasal spray daily (only takes during the spring months when nasal allergies flare) PMH Seasonal allergic rhinitis with springtime triggers PSH None Allergies None Social Freshman student at the University of Awesome located in central Illinois. Home is in Phoenix. Habits Denies cigarettes recreational marijuana use drinks 3-6 beers per weekend FH Adopted, does not know biological parents history Physical exam reveals the following. Physical Exam Constitutional Young adult male in NAD, alert and oriented, cooperative VS Temp-97.9, P-68, R-16, BP 120/75, Height 6'0, Weight 195 pounds Head Normocephalic Eyes Visual Acuity 20/20 (uncorrected) OU. PERRL with white sclera bilaterally. Slight light sensitivity noted bilaterally. No crusting, lesions or masses on lids noted. Bilateral conjunctiva with diffuse redness and tearing but no mucoid or purulent drainage noted.e No visible FBs under lids or on cornea to gross examination. Fundiscopic examination: Discs flat with sharp margins. Vessels present in all quadrants without crossing defects. Retinal background has even color, no hemorrhages noted. Macula has even color. Ears Tympanic membranes gray and intact with light reflex noted. Pinna and tragus nontender. Nose Nares patent. Nasal turbinates are pale and boggy with mild to moderate swelling. Nasal drainage is clear. Throat Oropharynx moist, no lesions or exudate. Tonsils ¼ bilaterally. Teeth in good repair, no cavities noted. Neck Neck supple. No lymphadenopathy. Thyroid midline, small and firm without palpable masses. Cardiopulmonary Heart S1 and S2 noted, no murmurs, noted. Lungs clear to auscultation bilaterally. Respirations unlabored. 1. Briefly and concisely summarize the history and physical (H&P) findings as if you were presenting it to your preceptor using the pertinent facts from the case. Use shorthand where possible and approved medical abbreviations. Avoid redundancy and irrelevant information. M.J is a 19 yo male with a CC of both eye discomfort x 2 to 3 days. He describes his discomfort as foreign body sensation in his eyes. He c/o grittiness, epiphora (tearing), redness, and ocular pruritis on both eyes which did not resolve from one-time usage of OTC visine. He is also positive for occasional rhinorrhea (runny nose) with intermittent nasal congestion which are subsided with loratadine and fluticasone nasal spray during spring season. Physical exam confirms that the patient is positive for bilateral OU photophobia (light sensitivity), conjunctival hyperemia and epiphora. He is also positive for nasal turbinate hypertrophy and rhinorrhea which is clear. 2. Provide a differential diagnosis (minimum of 3) which might explain the patient's chief complaint along with a brief statement of pathophysiology for each. 1) Allergic conjunctivitis (AC) Allergic conjunctivitis (AS) is mainly due to IgE-mediated hypersensitivity reaction. (La Rosa et al., 2013). Akil, Celik, Ulas, & Kara (2015) also mentioned from their citation that AC is caused by activation of T-cells as well as increased inflammatory cytokines which are epidermal growth factor, interleukin 1 (IL 1), and IL 8, affect goblet cells and conjunctival epithelial. Berger, Granet, & Kabat (2017) cited that allergic conjunctivitis occurs when conjunctival tissue responses to allergens such as animal dander, pollen, and other environmental allergens. They also cited that antigen exposure initiates mast cell degranulation and histamine release which triggers whole body inflammatory response (Berger et al., 2017). Furthermore, Akil et al., (2015) cited that these mechanism results in decreased mucin which causes decreased tear formation. 2) Allergic rhinitis (AR) AR is the most common form of noninfectious rhinitis which is associated with an IgE-mediated immune response against allergens, such as dust mites, grass pollen tree pollen, weed pollens, cat, dog, and molds (Gentile, Bartholow, Valovirta, Scadding, & Skoner, 2013). Gentile et al. (2013) cited that IgE antibodies are created from previous exposure to allergen and stays on the surface of mast cells which triggers mast cell degranulation with re-exposure to allergen. They also cited that this mechanism results in release of histamine which activates H1 receptor that can cause smooth muscle contraction, bronchospasm, increased endothelial permeability, and stimulation of cough, sneezing, itching, rhinorrhea (Gentile et al., 2013). 3) Bacterial conjunctivitis (BC) BC can be resulted due to direct contact with bacteria, such as staphylococcus pneumoniae and haemophilus influenza (Azari & Barney, 2013). But in children, H influenza, S pneumonia, and Moraxella catarrhalis are very common cause of BC (Azari & Barney, 2013). Azari & Barney (2013) mentioned that the most common signs and symptoms of BC are red eye, purulent or mucopurulent discharge and chemosis. 3. Analyze the differential by using the pertinent findings from the history and physical to argue for or against a diagnosis. Rank the differential in order of most likely to least likely. Diagnosis #1 –Allergic conjunctivitis (AC) Allergic conjunctivitis (AC) is at the top of my differential. It is necessary to differentiate AC from other ocular infections to make sure providing proper treatment. Careful history taking is very important to guide the direction of care. If ocular itching does not present, AC can be deleted from diagnosis (Berger et al., 2017). • Pertinent positive findings: Bilateral eye involvement, itching, redness, tearing, FB sensation, occasional runny nose with intermittent nasal congestion (subjective findings); bilateral light sensitivity, bilateral conjunctive with diffuse redness and tearing (objective findings) • Pertinent negative findings: no visual changes or dryness (subjective findings),No chemosis, no eyelid abonomality, - crusting or lids or mucoid or purulent drainage, no visible FBs under lids or cornea (objective findings) Diagnosis #2- Allergic rhinitis (AR) Gentile et al. (2013) found from their study that about 60 to 70 % of AR cases were provoked by spring and fall and the most frequent symptoms of AR are mainly related to nasal inflammation which includes nasal congestion, runny nose, and postnasal drip. Also added some nasal symptoms such as conjunctivitis, rhinosinusitis, hyposmia, middle ear problems, throat and laryngeal effects (Scadding et al., 2017). • Pertinent positive findings: occasional runny nose with intermittent nasal congestion, Hx of nasal allergies, redness of eye, itching, (subjective findings); pale and boggy nasal turbinates with mild to moderate swelling, clear nasal drainage (objective findings) • Pertinent negative findings: - sneezing, denies ST and redness (subjective data); oropharynx moist, no lesions or exudate, tonsils with no s/s of infection, no nares blockage (objective findings) Diagnosis #3- Bacterial conjunctivitis According to Azari & Barney (2013) the most common signs and symptoms of BC includes red eye, purulent or mucopurulent discharge and chemosis. Azari & Barney (2013) mentioned from their citation that lack of itching, adherence of eyelids, and no history of conjunctivitis can provide a very strong evidence for BC. The symptoms of bacterial conjunctivitis includes bilateral/unilateral red eye, thin or thick muco-purulent discharge, tearing, light sensitivity, fluctuating or decreased vision, chemosis, lid erythema, bulbar conjucntival injection. • Pertinent positive findings: FB sensation, redness on bilateral eyes, tearing(subjective findings); light sensitivity, bilateral conjunctive with diffuse redness (objective findings) • Pertinent negative findings: - vision change, denies contact lenses or glasses, - crusting or mucoid or purulent drainage (subjective findings);- eye lid swelling (objective findings) 4. Identify any additional tests and/or procedures that you feel is necessary or needed to help you narrow your differential. All testing decisions must be supported with an evidence-based medicine (EBM) argument as to why it is necessary or pertinent in this case. If no testing is indicated or needed, you must also support this decision with EBM evidence. At primary care office, the resources to diagnose the eye condition are limited, so I would perform in-office rapid antigen test since this test has very high sensitivity (89%) and specificity (94%) on viral conjunctivitis due to adenoviruses which does not require antibiotics for treatment regimen (Azari & Barney, 2013). Again, due to limited resources at the primary care office, I would refer patient for skin testing for specific allergens done by allergist. This type of test will assist with finding of different cause of the allergic reaction which will be very helpful in guiding future treatment (Azari & Barney, 2013). Besides above mentioned tests, a thorough history taking and physical assessment is very important in differentiating AC from any other conditions since the symptoms can be very similar. [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 17, 2020
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Nov 17, 2020
Downloads
0
Views
35