*NURSING > STUDY GUIDE > NSG 6020 Week 4 Study Guide with complete solution 2020 (All)
NSG 6020 Week 4 Study Guide with complete solution 2020
Document Content and Description Below
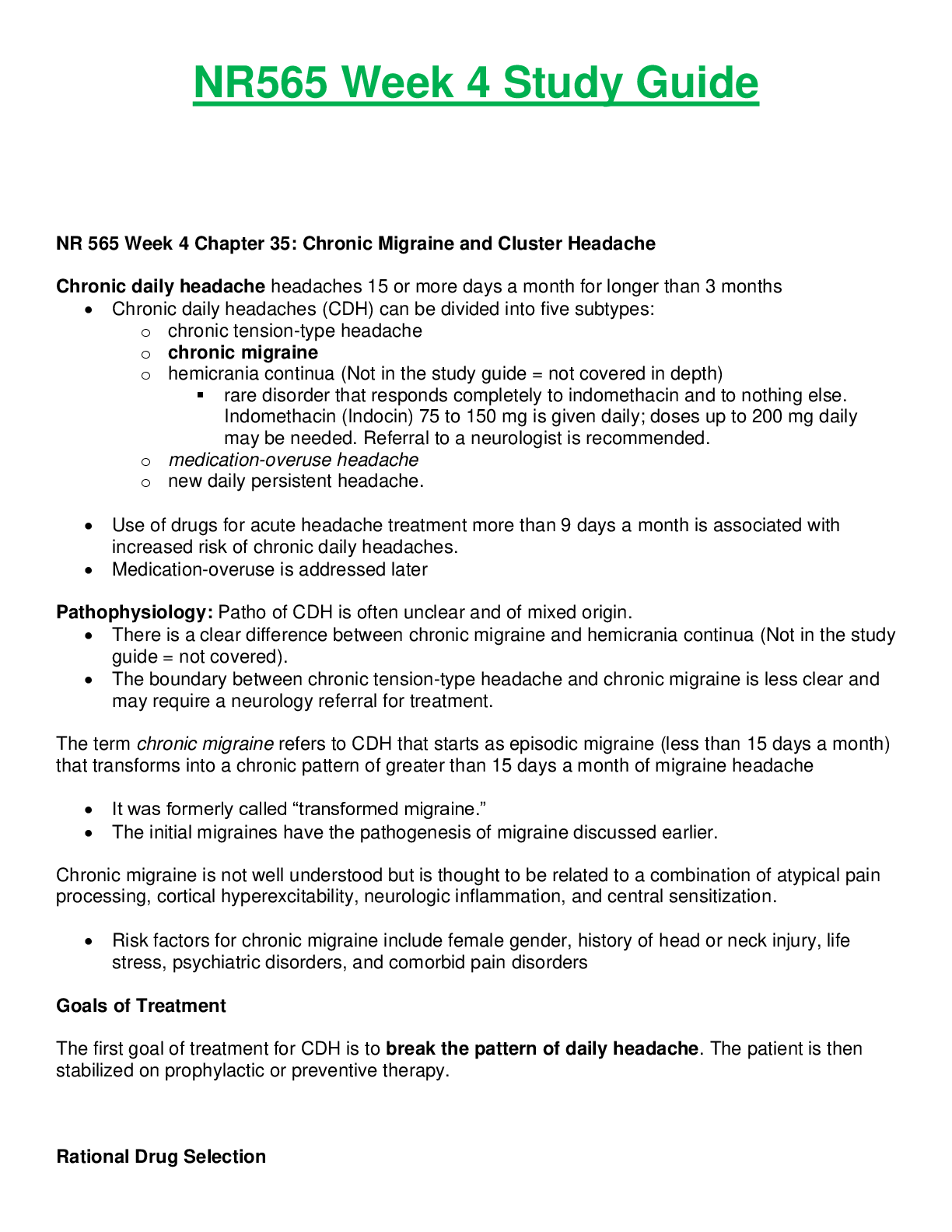
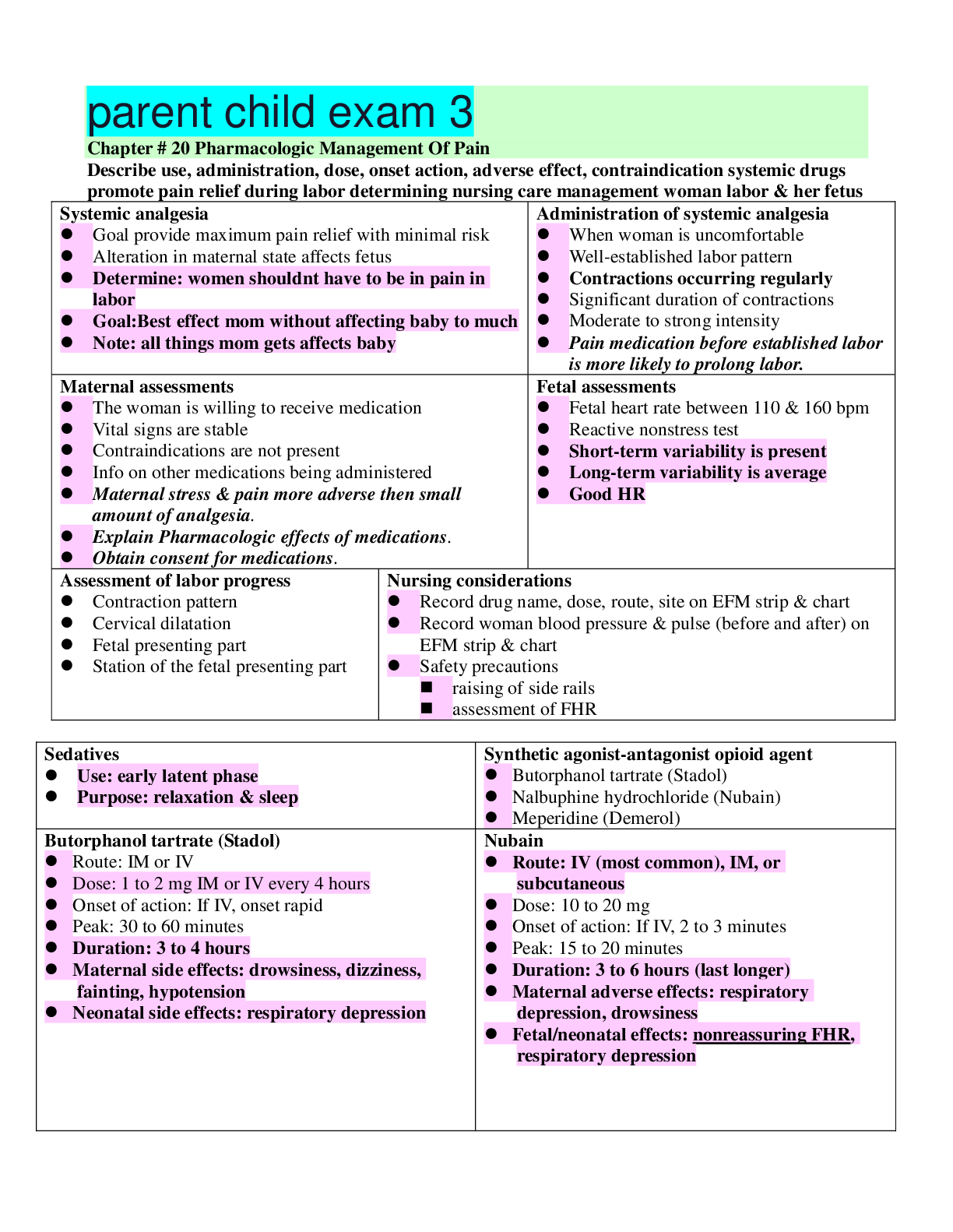
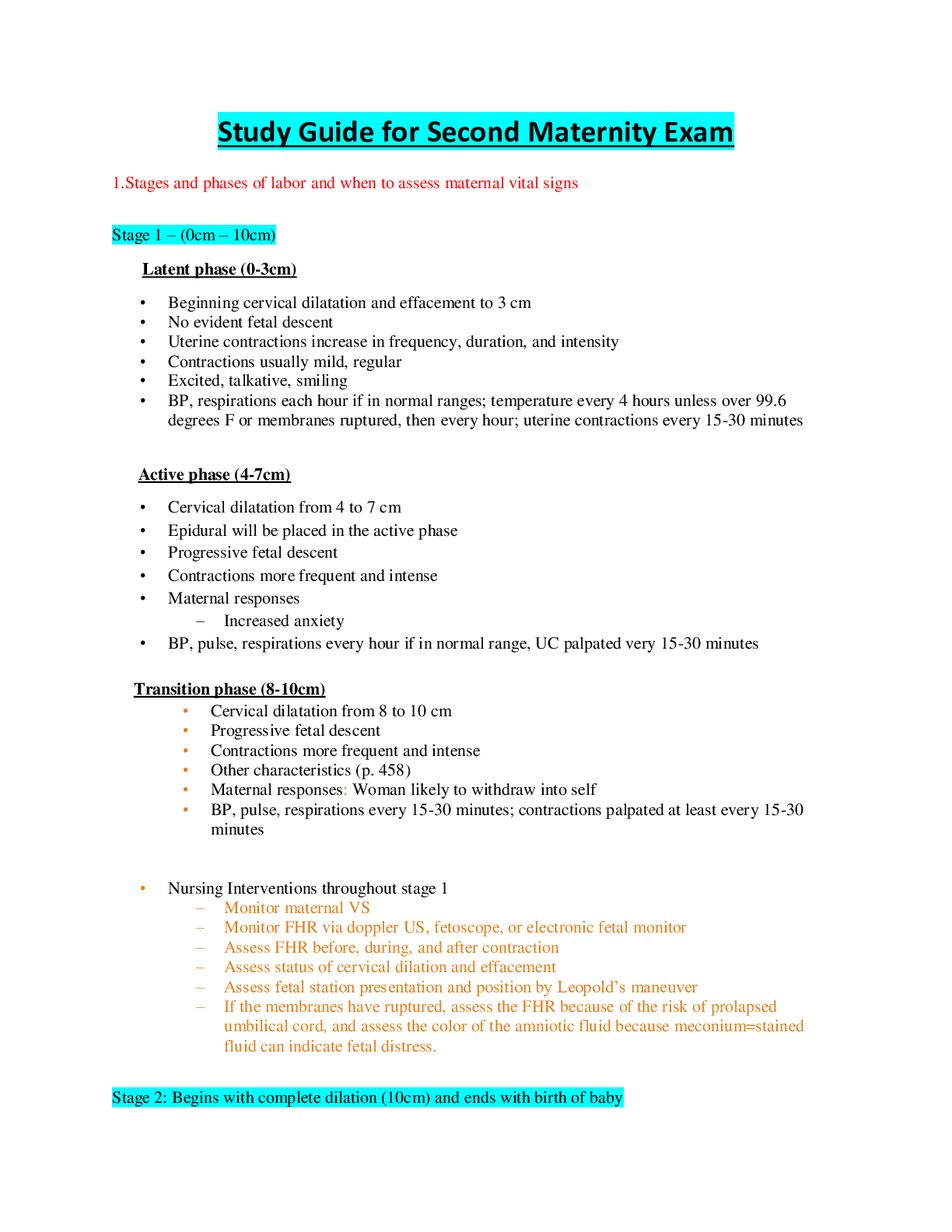
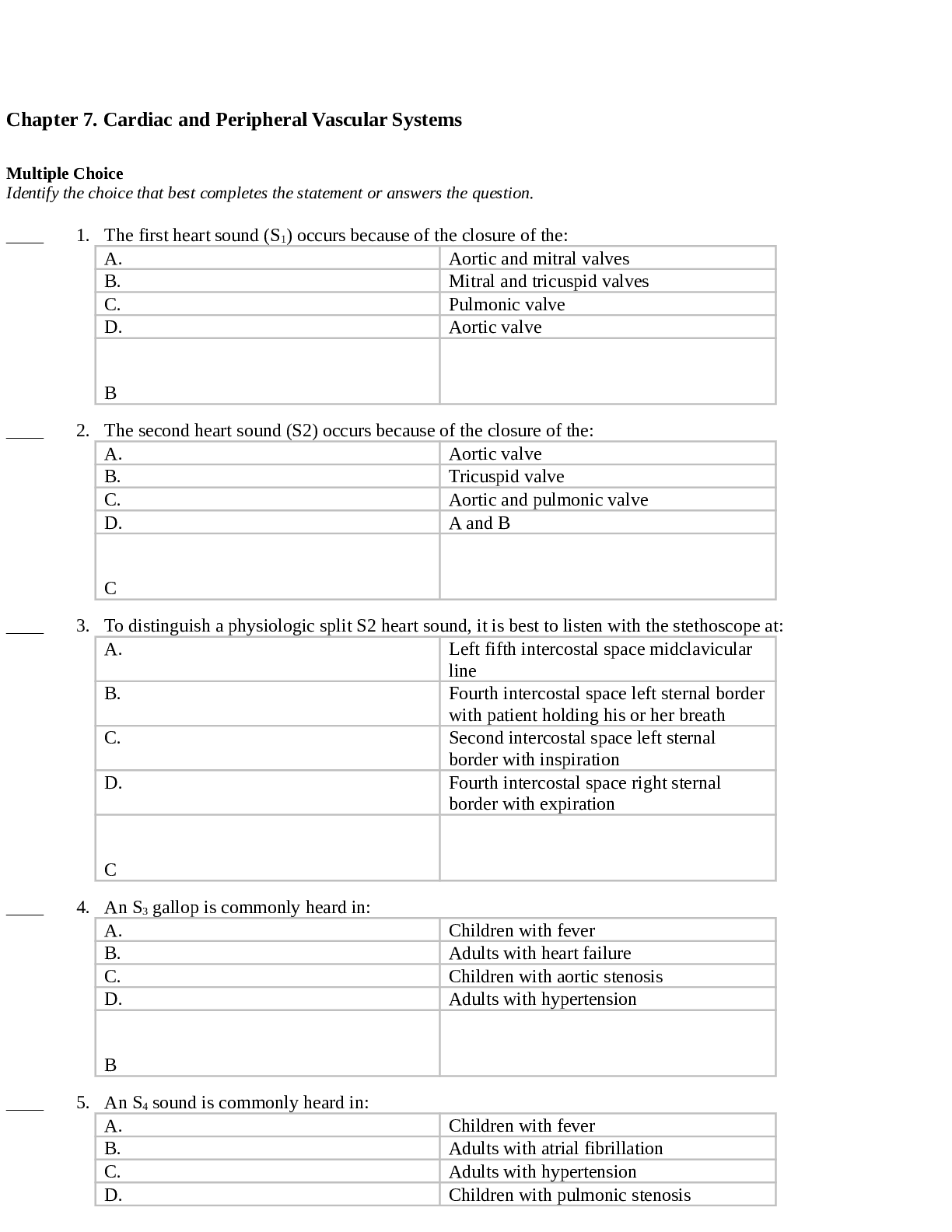
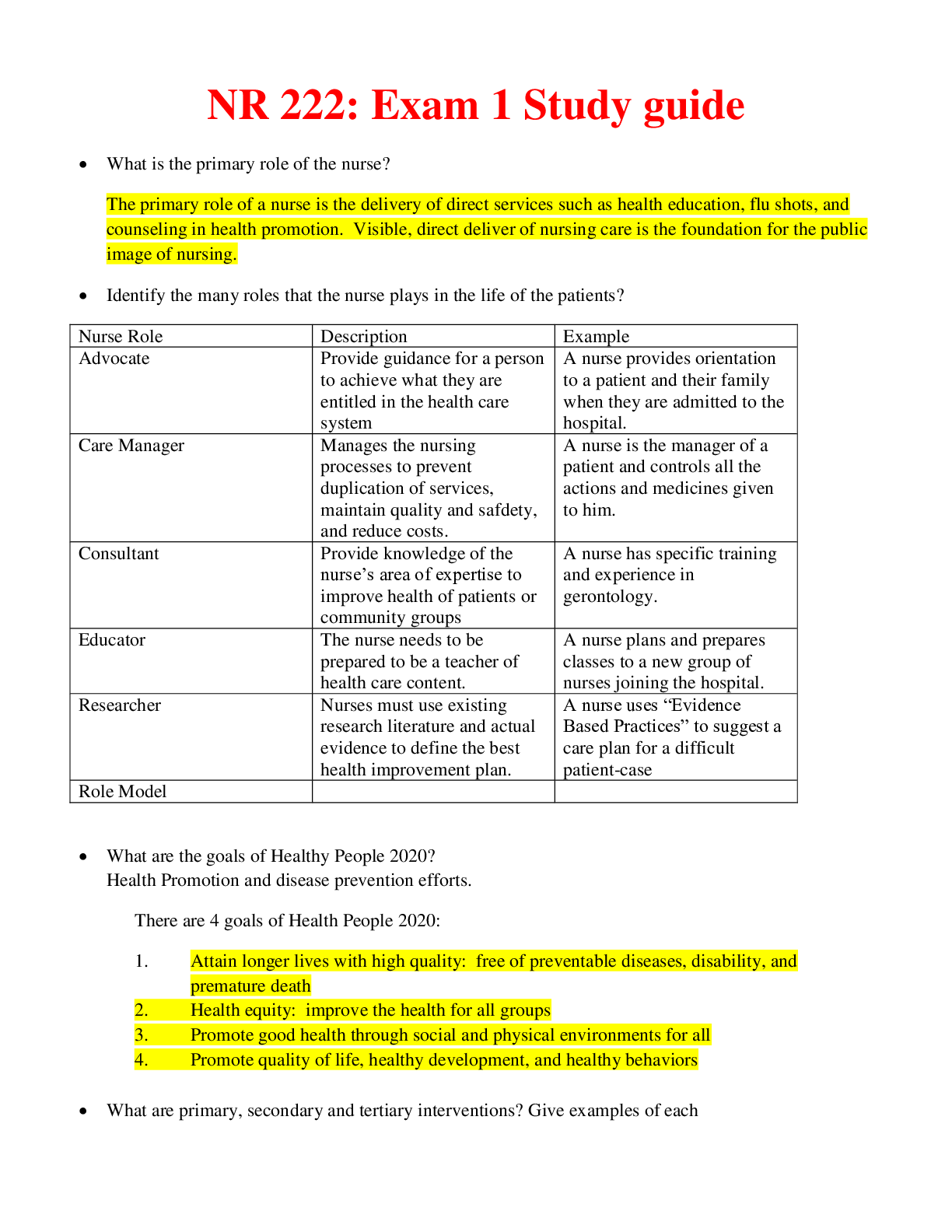
Chapter 7. Cardiac and Peripheral Vascular Systems Multiple Choice Identify the choice that best completes the statement or answers the question. ____ 1. The first heart sound (S1) occurs becau... se of the closure of the: A. Aortic and mitral valves B. Mitral and tricuspid valves C. Pulmonic valve D. Aortic valve ____ 2. The second heart sound (S2) occurs because of the closure of the: A. Aortic valve B. Tricuspid valve C. Aortic and pulmonic valve D. A and B ____ 3. To distinguish a physiologic split S2 heart sound, it is best to listen with the stethoscope at: A. Left fifth intercostal space midclavicular line B. Fourth intercostal space left sternal border with patient holding his or her breath C. Second intercostal space left sternal border with inspiration D. Fourth intercostal space right sternal border with expiration ____ 4. An S3 gallop is commonly heard in: A. Children with fever B. Adults with heart failure C. Children with aortic stenosis D. Adults with hypertension ____ 5. An S4 sound is commonly heard in: A. Children with fever B. Adults with atrial fibrillation C. Adults with hypertension D. Children with pulmonic stenosis ____ 6. Which of the following heart sounds is commonly heard after myocardial infarction? A. Friction rub B. S4 C. S3 D. Opening snap ____ 7. Which of the following is the most important question to ask during cardiovascular health history? A. Number of offspring B. Last physical examination C. Sudden death of a family member D. Use of caffeine ____ 8. Cardiovascular disease risk increase in women after age: A. 30 B. 40 C. 45 D. 55 ____ 9. Which of the following blood pressure measurements is categorized as prehypertension? A. 110/78 B. 129/85 C. 142/80 D. 145/92 ____ 10. Xanthelasma is a skin condition that should alert the clinician to ____ in a patient. A. Familial hyperlipidemia B. Type 2 diabetes C. Congenital heart disease D. Peripheral arterial disease ____ 11. When palpating the chest, you find the point of maximal impulse (PMI) in the left mid-axillary region. This can be indicative of: A. Normal PMI B. Congenital heart disease C. Ventricular hypertrophy D. Hypertension ____ 12. Upon inspecting the patient, you find jugular venous distension. This is a sign of: A. Left ventricular hypertrophy B. Right ventricular failure C. Hypertension D. Valve disease ____ 13. On an electrocardiogram, you see a deepened Q wave that is greater than one-third the height of the QRS complex. This is indicative of: A. Acute myocardial infarction B. Acute myocardial ischemia C. Left ventricular hypertrophy D. Past myocardial infarction ____ 14. Your 35-year-old female patient complains of feeling palpitations on occasion. The clinician should recognize that palpitations are often a sign of: A. Anemia B. Anxiety C. Hyperthyroidism D. All of the above ____ 15. A pulse rate of 56 beats per minute can be normal in: A. Elderly patients B. Newborns C. Athletic individuals D. Hypertensive patients ____ 16. Your patient has a dysrhythmia and has been on a diuretic for 2 months. Which of the following should be suspected? A. Potassium imbalance B. Sodium deficit C. Calcium imbalance D. Insufficient diuretic ____ 17. Your patient has suffered an inferior wall myocardial infarction. This is most commonly due to an obstruction in the: A. Posterior branch of the right coronary artery B. Circumflex branch of the left coronary artery C. Right main coronary artery D. Left main coronary artery ____ 18. Cardiac chest pain is most often described as: A. Stabbing, piercing pain B. Pain with inhalation C. Crushing, squeezing pain D. Burning, gnawing pain ____ 19. On an electrocardiogram (ECG), an anterior wall myocardial infarction is demonstrated on leads: A. II, III, AVR B. II, III, AVF C. V1, V2, V3, V4 D. I, AVL, V5, V6 ____ 20. Which is the most specific and sensitive test for validating a myocardial infarction? A. 12-lead EKG B. Troponin C. CK-MB D. CT scan ____ 21. It is important for clinicians to recognize that individuals with ____ often sustain silent myocardial infarction. A. Diabetes mellitus B. Hypertension C. Valvular disorders D. Congenital heart defects ____ 22. The pain associated with pericarditis is ____. A. Crushing and squeezing B. Constant C. Worse with inspiration D. Only present with fever ____ 23. Pain associated with a dissecting thoracic aortic aneurysm is commonly described as: A. Retrosternal crushing and squeezing B. Chest stabbing and sharp C. Ripping and tearing in the chest or thoracic back D. Worse with inspiration ____ 24. The pain of ____ can frequently be mistaken for cardiac chest pain. A. Gastroesophageal reflux disease (GERD) B. Peptic ulcer disease (PUD) C. Cholecystitis D. All of the above ____ 25. The pain of pancreatitis is described as: A. Abdominal sharp and piercing pain in the left upper quadrant B. Dull and cramping pain in the right upper quadrant C. Severe, epigastric pain radiating straight into the back D. Sharp pain radiating to the shoulder ____ 26. The pain of costochondritis typically ____. A. Mimics cardiac crushing and squeezing pain B. Worsens with movement and full inspiration C. Radiates from epigastrium into the back D. Is a tearing and ripping pain ____ 27. The medical record of your patient lists a grade III systolic murmur. This indicates the patient has a heart murmur that is: A. Soft and after S2 B. Loud and crescendo in quality C. Moderately loud and after S1 D. Loud and after S2 ____ 28. The radiation of a mitral valve murmur is commonly heard in the: A. Carotid arteries B. Left mid-axillary line C. Base of the heart D. Left mid-clavicular line ____ 29. The murmur of aortic stenosis is best heard in the: A. Left second intercostal space left sternal border B. Left fifth intercostal space mid-clavicular line C. Right fourth intercostal space right sternal border D. Right second intercostal space right sternal border ____ 30. The pulmonary valve is best heard over the: A. left second intercostal space left sternal border B. left fifth intercostal space mid-clavicular line C. right fourth intercostal space right sternal border D. right second intercostal space right sternal border ____ 31. The key sign(s) of aortic stenosis are: A. Syncope B. Dyspnea C. Angina D. All of the above ____ 32. Classically in mitral valve prolapse, the clinician can hear a(n) ____. A. Mid-systolic click followed by a grade I murmur that crescendos up to S2 B. Opening snap followed by a grade III holosystolic murmur C. Crescendo-decrescendo grade I diastolic murmur after S2 D. Rough grade III holosystolic murmur that obscures S1 and S2 ____ 33. The best diagnostic test that allows analysis of a heart murmur is: A. CT scan B. Echocardiogram C. MRI D. ECG ____ 34. The most common cause of tricuspid regurgitation is: A. Left ventricular hypertrophy B. Left atrial enlargement C. Aortic stenosis D. Pulmonary hypertension ____ 35. The tricuspid valve is best heard over the: A. Third intercostal space left sternal border B. Fifth intercostal space right sternal border C. Fourth intercostal space left sternal border D. Third intercostal space right sternal border ____ 36. From Erb’s point, all the heart valves can be heard equally. Erb’s point is located over the: A. Third intercostal space left sternal border B. Fifth intercostal space right sternal border C. Fourth intercostal space left sternal border D. Third intercostal space right sternal border ____ 37. Upon examination of a child, an innocent systolic murmur is heard at the second intercostal space left sternal border. This is usually due to: A. Atrial septal defect B. Patent foramen ovale C. Low flow velocity D. High flow turbulence ____ 38. In mitral stenosis, the murmur occurs: A. From S1 through S2 as a holosystolic murmur B. After an opening snap that is heard after S2 during diastole C. As a soft mid-systolic click D. A loud crescendo-decrescendo systolic murmur ____ 39. In mitral stenosis, the murmur can be best heard with the patient in the: A. Squatting position B. Seated position C. Left lateral recumbent D. Supine position ____ 40. Due to increased left atrial pressure, a patient with mitral stenosis often suffers from: A. Pulmonary congestion B. Hepatomegaly C. Jugular venous distension D. Ventricular tachycardia ____ 41. In aortic stenosis, the patient’s point of maximal impulse is commonly located at the: A. Fifth intercostal space mid-clavicular line B. Fifth intercostal space mid-axillary line C. Second intercostal space left sternal border D. Second intercostal space right sternal border ____ 42. Aortic regurgitation occurs after S2 during ____ because there is turbulent flow that refluxes into the left ventricle after the aortic valve closes. A. Early diastole B. Late diastole C. Early systole D. Mid-systole ____ 43. The murmur of a ventricular septal defect (VSD) occurs when the ventricle contracts and blood flows from the left ventricle into the right ventricle. This creates a ____ heart murmur. A. Holodiastolic B. Early diastolic C. Holosystolic D. Late systolic ____ 44. An atrial septal defect (ASD) causes a left to right shunt, which enlarges the right atrium. Because of this effect, which of the following conditions often occur with ASD? A. Asthma B. Jugular venous distension C. Atrial fibrillation D. B & C ___ 45. A patient with hypertension who has hyperlipidemia should aim for LDL measurement to be: A. 130 mg/dL or less B. 40 mg/dL or less C. 100 mg/dL or less D. 60mg/dL or less ____ 46. Your 47-year-old female patient has a waist to hip ratio of 1. In terms of cardiovascular disease risk, this is considered: A. Ideal B. Greater than acceptable limits C. Less than acceptable limits D. Within acceptable limits ____ 47. Which of the following conditions is/are part of metabolic syndrome? A. Hypertension B. Hyperlipidemia C. Insulin resistance D. All of the above ____ 48. The target body mass index for women is: A. 27 kg/m2 B. 25 kg/m2 C. 22 kg/m2 D. 16 kg/m2 ____ 49. Dyspnea, cough, and pulmonary crackles are symptoms that can occur in left ventricular failure and respiratory disorders, such as pneumonia. Which of the blood tests below can be used to differentiate cardiovascular from pulmonary disease? A. B type natriuretic peptide (BNP) B. Pulse oximetry C. Arterial blood gases D. High sensitivity C reactive protein (hs-CRP) ____ 50. When an examiner presses on the liver and elicits hepato-jugular reflux, which of the following conditions is likely? A. Left ventricular failure B. Right ventricular failure C. Hepatomegaly D. Pulmonary edema ____ 51. Your patient has had hypertension for 10 years, a myocardial infarction 5 years ago, and now complains of dyspnea on exertion, cough, and 3-pillow orthopnea. Which of the following conditions is likely? A. Right ventricular failure B. Pulmonary embolism C. Cor pulmonale D. Left ventricular failure ____ 52. Your patient complains of worsening ankle edema and weight gain over the last week. On physical examination, you note jugular venous distension, ascites, hepatomegaly, and esplenomegaly. These conditions are indicative of: A. Left ventricular failure B. Pulmonary embolism C. Right ventricular failure D. Myocardial infarction ____ 53. A 23-year-old patient presents the emergency department with high fever, chills, extreme fatigue, and arthralgias. Your physical examination reveals grade II heart murmur heard loudest over the fourth intercostal space left sternal border. The arms of the patient reveal past intravenous drug abuse. The clinician should recognize these are signs and symptoms of: A. Pulmonary embolism B. Right ventricular failure C. Functional heart murmur D. Bacterial endocarditis ____ 54. A 75-year-old patient complains of pain and paresthesias in the right foot that worsens with exercise and is relieved by rest. On physical examination you note pallor of the right foot, capillary refill of 4 seconds in the right foot, +1 dorsalis pedis pulse in the right foot, and +2 pulse in left foot. Which of the following is a likely cause of the signs and symptoms? A. Arterial insufficiency B. Femoral vein thrombus C. Venous insufficiency D. Peripheral neuropathy ____ 55. Which of the following ankle-brachial index measurements require a referral to a vascular consultant? A. ABI 1.2 B. ABI 1 C. ABI 0.9 D. ABI 0.5 ____ 56. Your patient complains of a feeling of heaviness in the lower legs daily. You note varicosities, edema, and dusky color of both ankles and feet. Which of the following is the most likely cause for these symptoms? A. Femoral vein thrombosis B. Femoral artery thrombus C. Venous insufficiency D. Musculoskeletal injury ____ 57. After multiple pregnancies, the following vascular disorder is common: A. Deep venous thrombosis B. Varicose veins C. Peripheral arterial disease D. Aortic aneurysm Bates’ Guide to Physical Examination and History Taking, 12th Edition Chapter 9 The Cardiovascular System 1. You are performing a thorough cardiac examination. Which of the following chambers of the heart can you assess by palpation? A) Left atrium B) Right atrium C) Right ventricle D) Sinus node 2. What is responsible for the inspiratory splitting of S2? A) Closure of aortic, then pulmonic valves B) Closure of mitral, then tricuspid valves C) Closure of aortic, then tricuspid valves D) Closure of mitral, then pulmonic valves 3. A 25-year-old optical technician comes to your clinic for evaluation of fatigue. As part of your physical examination, you listen to her heart and hear a murmur only at the cardiac apex. Which valve is most likely to be involved, based on the location of the murmur? A) Mitral B) Tricuspid C) Aortic D) Pulmonic 4. A 58-year-old teacher presents to your clinic with a complaint of breathlessness with activity. The patient has no chronic conditions and does not take any medications, herbs, or supplements. Which of the following symptoms is appropriate to ask about in the cardiovascular review of systems? A) Abdominal pain B) Orthopnea C) Hematochezia D) Tenesmus 5. You are screening people at the mall as part of a health fair. The first person who comes for screening has a blood pressure of 132/85. How would you categorize this? A) Normal B) Prehypertension C) Stage 1 hypertension D) Stage 2 hypertension 6. You are participating in a health fair and performing cholesterol screens. One person has a cholesterol of 225. She is concerned about her risk for developing heart disease. Which of the following factors is used to estimate the 10-year risk of developing coronary heart disease? A) Ethnicity B) Alcohol intake C) Gender D) Asthma 7. You are evaluating a 40-year-old banker for coronary heart disease risk factors. He has a history of hypertension, which is well-controlled on his current medications. He does not smoke; he does 45 minutes of aerobic exercise five times weekly. You are calculating his 10-year coronary heart disease risk. Which of the following conditions is considered to be a coronary heart disease risk equivalent? A) Hypertension B) Peripheral arterial disease C) Systemic lupus erythematosus D) Chronic obstructive pulmonary disease (COPD) 8. You are conducting a workshop on the measurement of jugular venous pulsation. As part of your instruction, you tell the students to make sure that they can distinguish between the jugular venous pulsation and the carotid pulse. Which one of the following characteristics is typical of the carotid pulse? A) Palpable B) Soft, rapid, undulating quality C) Pulsation eliminated by light pressure on the vessel D) Level of pulsation changes with changes in position 9. A 68-year-old mechanic presents to the emergency room for shortness of breath. You are concerned about a cardiac cause and measure his jugular venous pressure (JVP). It is elevated. Which one of the following conditions is a potential cause of elevated JVP? A) Left-sided heart failure B) Mitral stenosis C) Constrictive pericarditis D) Aortic aneurysm 10. You are palpating the apical impulse in a patient with heart disease and find that the amplitude is diffuse and increased. Which of the following conditions could be a potential cause of an increase in the amplitude of the impulse? A) Hypothyroidism B) Aortic stenosis, with pressure overload of the left ventricle C) Mitral stenosis, with volume overload of the left atrium D) Cardiomyopathy 11. You are performing a cardiac examination on a patient with shortness of breath and palpitations. You listen to the heart with the patient sitting upright, then have him change to a supine position, and finally have him turn onto his left side in the left lateral decubitus position. Which of the following valvular defects is best heard in this position? A) Aortic B) Pulmonic C) Mitral D) Tricuspid 12. You are concerned that a patient has an aortic regurgitation murmur. Which is the best position to accentuate the murmur? A) Upright B) Upright, but leaning forward C) Supine D) Left lateral decubitus 13. A 68-year-old retired waiter comes to your clinic for evaluation of fatigue. You perform a cardiac examination and find that his pulse rate is less than 60. Which of the following conditions could be responsible for this heart rate? A) Second-degree A-V block B) Atrial flutter C) Sinus arrhythmia D) Atrial fibrillation 14. Where is the point of maximal impulse (PMI) normally located? A) In the left 5th intercostal space, 7 to 9 cm lateral to the sternum B) In the left 5th intercostal space, 10 to 12 cm lateral to the sternum C) In the left 5th intercostal space, in the anterior axillary line D) In the left 5th intercostal space, in the midaxillary line 15. Which of the following events occurs at the start of diastole? A) Closure of the tricuspid valve B) Opening of the pulmonic valve C) Closure of the aortic valve D) Production of the first heart sound (S1) 16. Which is true of a third heart sound (S3)? A) It marks atrial contraction. B) It reflects normal compliance of the left ventricle. C) It is caused by rapid deceleration of blood against the ventricular wall. D) It is not heard in atrial fibrillation. 17. Which is true of splitting of the second heart sound? A) It is best heard over the pulmonic area with the bell of the stethoscope. B) It normally increases with exhalation. C) It is best heard over the apex. D) It does not vary with respiration. 18. Which of the following is true of jugular venous pressure (JVP) measurement? It is measured with the patient at a 45-degree angle. A) B) The vertical height of the blood column in centimeters, plus 5 cm, is the JVP. C) A JVP below 9 cm is abnormal. D) It is measured above the sternal notch. 19. Which of the following regarding jugular venous pulsations is a systolic phenomenon? A) The “y” descent B) The “x” descent C) The upstroke of the “a” wave D) The downstroke of the “v” wave 20. How much does cardiovascular risk increase for each increment of 20 mm Hg systolic and 10 mm Hg diastolic in blood pressure? A) 25% B) 50% C) 75% D) 100% 21. In healthy adults over 20, how often should blood pressure, body mass index, waist circumference, and pulse be assessed, according to American Heart Association guidelines? A) Every 6 months B) Every year C) Every 2 years D) Every 5 years 22. Which of the following is a clinical identifier of metabolic syndrome? A) Waist circumference of 38 inches for a male B) Waist circumference of 34 inches for a female C) BP of 134/88 for a male D) BP of 128/84 for a female 23. Mrs. Adams would like to begin an exercise program and was told to exercise as intensely as necessary to obtain a heart rate 60% or greater of her maximum heart rate. She is 52. What heart rate should she achieve? A) 80 B) 100 C) 120 D) 140 23. In measuring the jugular venous pressure (JVP), which of the following is important? A) Keep the patient's torso at a 45-degree angle. B) Measure the highest visible pressure, usually at end expiration. C) Add the vertical height over the sternal notch to a 5-cm constant. D) Realize that a total value of over 12 cm is abnormal. 24. You find a bounding carotid pulse on a 62-year-old patient. Which murmur should you search out? A) Mitral valve prolapse B) Pulmonic stenosis C) Tricuspid insufficiency D) Aortic insufficiency 25. To hear a soft murmur or bruit, which of the following may be necessary? A) Asking the patient to hold her breath B) Asking the patient in the next bed to turn down the TV C) Checking your stethoscope for air leaks D) All of the above 26. Which of the following may be missed unless the patient is placed in the left lateral decubitus position and auscultated with the bell? A) Mitral stenosis murmur B) Opening snap of the mitral valve C) S3 and S4 gallops D) All of the above 27. How should you determine whether a murmur is systolic or diastolic? A) Palpate the carotid pulse. B) Palpate the radial pulse. C) Judge the relative length of systole and diastole by auscultation. D) Correlate the murmur with a bedside heart monitor. 28. Which of the following correlates with a sustained, high-amplitude PMI? A) Hyperthyroidism B) Anemia C) Fever D) Hypertension 29. You are examining a patient with emphysema in exacerbation and are having difficulty hearing his heart sounds. What should you do to obtain a good examination? A) Listen in the epigastrium. B) Listen to the patient in the left lateral decubitus position. C) Ask the patient to hold his breath for 30 seconds. D) Listen posteriorly. 30. You are listening carefully for S2 splitting. Which of the following will help? A) Using the diaphragm with light pressure over the 2nd right intercostal space B) Using the bell with light pressure over the 2nd left intercostal space C) Using the diaphragm with firm pressure over the apex D) Using the bell with firm pressure over the lower left sternal border 31. Which of the following is true of a grade 4-intensity murmur? A) It is moderately loud. B) It can be heard with the stethoscope off the chest. C) It can be heard with the stethoscope partially off the chest. D) It is associated with a “thrill.” 32. Which valve lesion typically produces a murmur of equal intensity throughout systole? A) Aortic stenosis B) Mitral insufficiency C) Pulmonic stenosis D) Aortic insufficiency 33. You notice a patient has a strong pulse and then a weak pulse. This pattern continues. Which of the following is likely? A) Emphysema B) Asthma exacerbation C) Severe left heart failure D) Cardiac tamponade 34. Suzanne is a 20-year-old college student who complains of chest pain. This is intermittent and is located to the left of her sternum. There are no associated symptoms. On examination, you hear a short, high-pitched sound in systole, followed by a murmur which increases in intensity until S2. This is heard best over the apex. When she squats, this noise moves later in systole along with the murmur. Which of the following is the most likely diagnosis? 35. A) Mitral stenosis B) Mitral insufficiency C) Mitral valve prolapse D) Mitral valve papillary muscle ischemia [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 24, 2020
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Nov 24, 2020
Downloads
0
Views
49

 (2).png)
.png)