*NURSING > STUDY GUIDE > Professional Nursing III Final Exam Concept Guide (complete 2020) solution. (All)
Professional Nursing III Final Exam Concept Guide (complete 2020) solution.
Document Content and Description Below
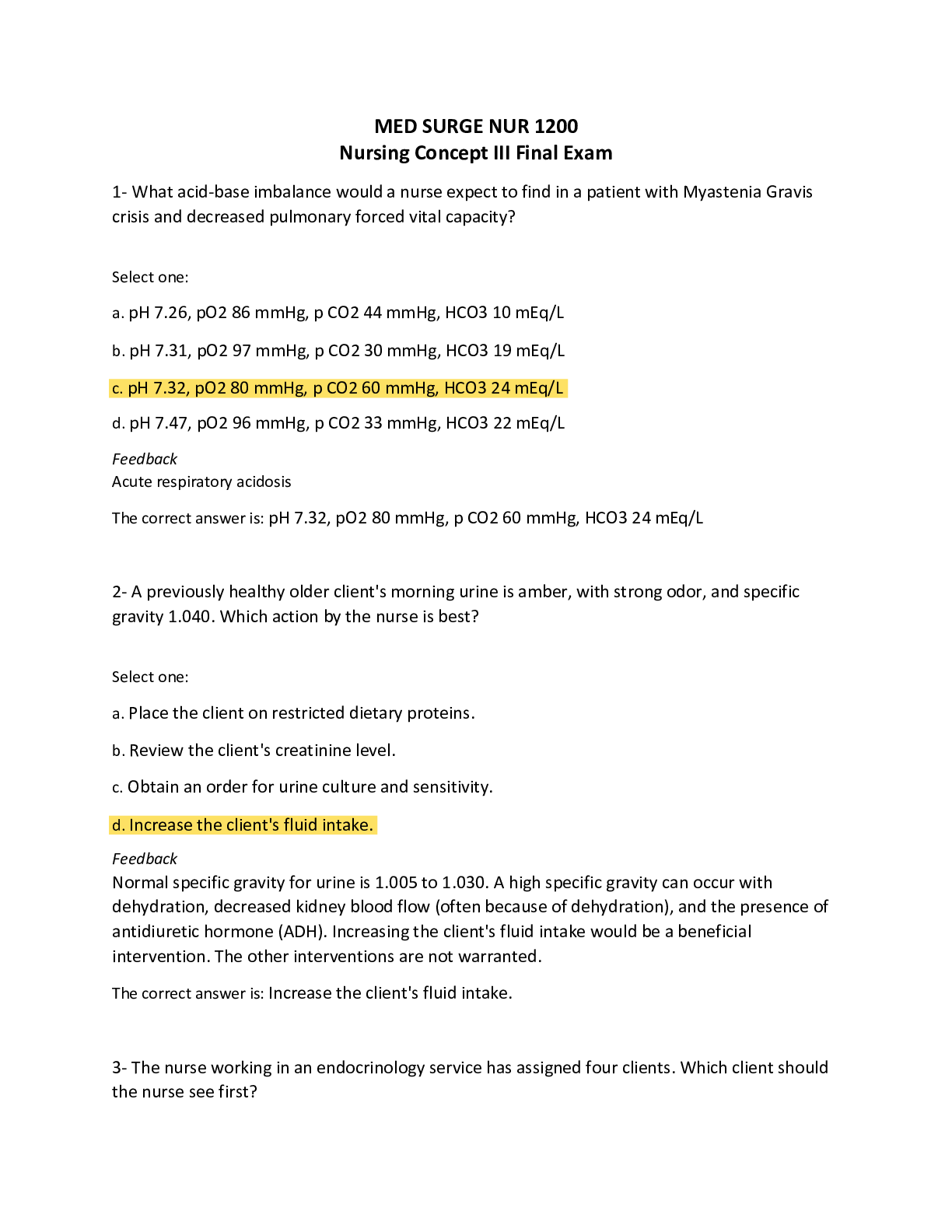
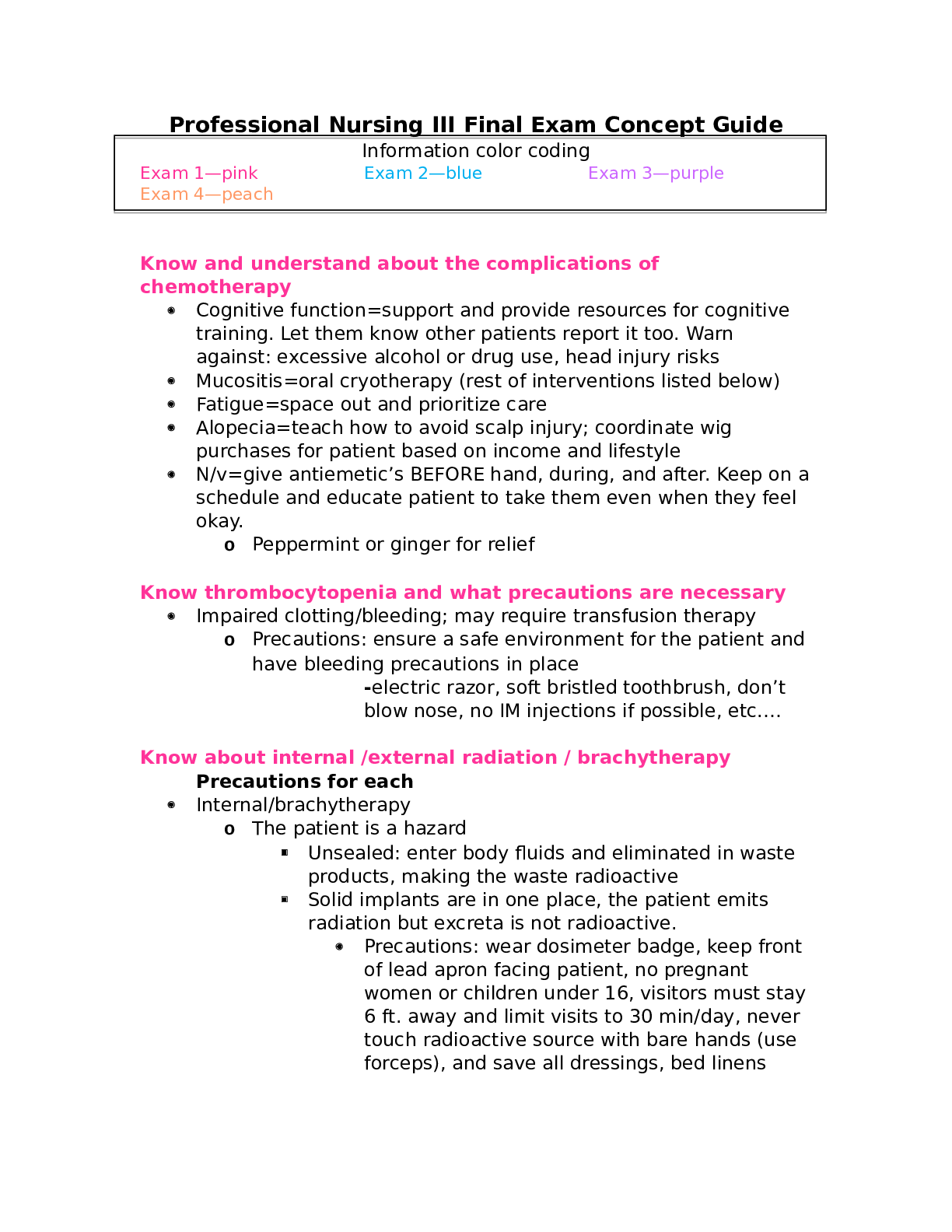
Professional Nursing III Final Exam Concept Guide Information color coding Exam 1—pink Exam 2—blue Exam 3—purple Exam 4—peach Know and understand about the complications of ... chemotherapy • Cognitive function=support and provide resources for cognitive training. Let them know other patients report it too. Warn against: excessive alcohol or drug use, head injury risks • Mucositis=oral cryotherapy (rest of interventions listed below) • Fatigue=space out and prioritize care • Alopecia=teach how to avoid scalp injury; coordinate wig purchases for patient based on income and lifestyle • N/v=give antiemetic’s BEFORE hand, during, and after. Keep on a schedule and educate patient to take them even when they feel okay. o Peppermint or ginger for relief Know thrombocytopenia and what precautions are necessary • Impaired clotting/bleeding; may require transfusion therapy o Precautions: ensure a safe environment for the patient and have bleeding precautions in place -electric razor, soft bristled toothbrush, don’t blow nose, no IM injections if possible, etc.… Know about internal /external radiation / brachytherapy Precautions for each • Internal/brachytherapy o The patient is a hazard Unsealed: enter body fluids and eliminated in waste products, making the waste radioactive Solid implants are in one place, the patient emits radiation but excreta is not radioactive. • Precautions: wear dosimeter badge, keep front of lead apron facing patient, no pregnant women or children under 16, visitors must stay 6 ft. away and limit visits to 30 min/day, never touch radioactive source with bare hands (use forceps), and save all dressings, bed linens until the radioactive source is removed; then dispose as usual. • External/teletherapy o Radiation delivered from a source outside of the patient. The source is external; therefore, the patient is not radioactive, and there is no hazard to others. Know basic labs such as CBC & Electrolytes, Pt, INR, and PTT • CBC o Hemoglobin: 13-17 o Hematocrit: 35%-48% • Electrolytes o K+: 3.5-5 o Na: 135-145 o Mag: 1.5-2.5 o Cal: 9-11 o Phosphorus: 2.5-4.5 • Clotting o Pt: 11-13.5 seconds o INR: 0.8-1.1 o PTT: 25-35 seconds Know how to treat low hemoglobin • Blood transfusion Know the drugs to treat low hemoglobin and platelets when getting chemo • Hgb: Epoetin alfa—can prevent or improve anemia and reduce the need for transfusions • Platelets: Oprelvekin (neumega)—increases platelet production by stimulating bone marrow (biologic response modifier) Know what mucositis is and how to treat during chemo and after chemo • Mouth sores caused by chemo o Tx—oral cryotherapy using ice chips before, during, or after rapid infusions of agents (vasoconstriction) Sodium bi-carb rinses, frequent oral assessments and hygiene • Soft bristled toothbrush, gentle flossing, saline rinse • IV injections of Palifermin—stimulates growth of mucous membranes in the mouth Know your burns • Phases o Resuscitation—onset24/48 hours o Acute—36/48 hours after—wound closure o Rehabilitation—wound closurehighest functioning BSA % ------Rule of 9’s How to differentiate each thickness • Superficial=leaves a good blood supply, pink and moist; blanches; painful • Partial thickness=blisters occur • Full thickness=eschar; not as painful How to treat burns • Monitor airway—assess by looking for drooling, trouble handling secretions, brassy cough, wheezing, or diminished breath sounds • Assess fluid resuscitation—urine output 30 mL/hr. • Assess for hypovolemic shock—monitor degree of edema and cardiac status • Assess for fluid shift hyponatremia and hyperkalemia • Give fluids—LR • Monitor electrolytes • Prevent infection (hand hygiene and standard precautions) • Drug management—morphine • Prevent gastric ulcers (curling’s)—H2 blockers, PPI’s (pantoprazole) Complications • Infection • Immobility contractures • Hypertrophic scarring Interventions • Rapid fluid therapy, oxygen therapy, pain management, antibiotic administration, CAM therapy, quiet environment, wound care management Know the Parkland Formula • 4 mL LR X BSA% X body weight (kg) o First half of solution over 8 hours o Second half over 16 hours Different types of triaging (Disaster & In hospital) What’s your priorities? The ranking system for each TRIAGE UNDER USUAL CONDITIONS TRIAGE UNDER MASS CASUALTY Emergent (immediate threat to life) Emergent—red tag Urgent (major injuries that require immediate treatment) Urgent—yellow tag Non-urgent (minor injuries that do not require immediate treatment) Non-urgent—green tag Does not apply Expected to die—black tag Understand stress debriefing after a mass casualty The different types • Two general types of debriefing occur after a mass casualty incident or disaster. o The first type entails bringing in critical incident stress debriefing (CISD) teams to provide sessions for small groups of staff to promote effective coping strategies. o The second type of debriefing involves an administrative review of staff and system performance during the event to determine whether opportunities for improvement in the emergency management plan exist. Know types of ventilators How to wean off Know high pressure and low-pressure alarms o Pressure cycled: pushes air into the lungs until a preset airway pressure is reached; used for short periods (bi-PAP) o Time-cycled: pushes air into the lungs until a preset time has elapsed o Volume-cycled: pushes air into the lungs until a preset volume is delivered; constant tidal volume is delivered • Weaning—mechanical breaths decrease from 12 to 2 HIGH pressure alarm Secretions or mucus plugs Patient coughs, gags or bites ET tube Wheezing/bronchospasm Tube displacement Pneumothorax Increased PIP Obstruction of tubing LOW pressure alarm Leak in ventilator Patient stops breathing with SIMV or CPAP Cuff leak of the ET Know and understand ARDS What it is • Persistent hypoxia even with oxygenation What are the signs & symptoms? o Refractory hypoxemia o Decreased pulmonary compliance o Dyspnea o Noncardiac-associated bilateral pulmonary edema o Dense pulmonary infiltrates on x-ray (ground-glass appearance) Who’s at risk? Often ARDS occurs after an acute lung injury (ALI) in people who have no pulmonary disease as a result of other conditions such as sepsis, burns, pancreatitis, trauma, and transfusion. Know your labs associated with heparin & Coumadin • HIT or heparin induced thrombocytopenia is a complication of this medication • Labs associated are platelets and aPTT o Therapeutic 1.5-2.5; control value (25-30 seconds 40-70 seconds) How to prevent venous thromboembolism • Anticoagulation therapy, mobilizing, pneumatic compression devices, SCD’s, ted hose, keep feet flat Know and understand Flail chest and how to treat it • Flail chest—fractures of at least 2 neighboring ribs in two or more places causing paradoxical chest wall movements o Tx—oxygen therapy, pain management, deep breathing and positioning, fluid secretion clearance by coughing and tracheal suctioning; possible mechanical ventilation Know what tension pneumothorax is and how to treat it • Life-threatening complication of pneumothorax in which air continues to enter the pleural space during inspiration and does not exit during expiration. As a result, air collects under pressure, completely collapsing the lung and compressing blood vessels, which limits blood return. o Tx— Initial management is an immediate needle thoracostomy, with a large-bore needle inserted into the second intercostal space in the midclavicular line of the affected side. A chest tube then is placed into the fourth intercostal space, and the other end is attached to a water-seal drainage system until the lung re-inflates. Know your rhythm strips and how to treat each rhythm Know what’s stable or unstable Rhythm EKG Treatment Sinus bradycardia If stable, treat underlying cause If not, ATROPINE 0.5 mg IV Sinus tachycardia Bedrest if hypotension or weakness is occurring. Avoid substances that increase the heart rate, such as caffeine Stress management strategies V-tach Cardioversion SVT *chest pain, SOB, palpitations, BP Adenosine Cardioversion V-fib After ensuring that v-fib is real… Cardioversion! A-fib *lightheaded Anticoagulants and calcium channel blockers (diltiazem/Cardizem) A-flutter *saw tooth Antidysrhythmic, anticoagulants, cardioversion, catheter ablation Asystole CPR! Know and understand pacemakers and complication with insertion • Consequences of a pacemaker: Stimulate an arrhythmia Pericardial effusion Infection Hematoma o Prolonged hiccups need immediate attention o Patient education and instruction for pacemakers • Don’t lift more than 10 pounds • Ensure microwave is working properly • No MRI • Let airport security know Know and understand about coronary artery disease • Broad term that includes chronic stable angina & acute coronary syndromes • It affects the arteries that provide blood, oxygen, and nutrients to the myocardium • When blood flow from the coronary arteries is partially of completely occluded it causes ischemia and infarction Treatment Type Typical s/s Treatment Chronic stable angina chest discomfort that occurs with moderate to prolonged exertion in a pattern that is familiar to the patient Nitro and/or rest Unstable: (new onset, variant (after rest), and pre-infarction) Chest pain or discomfort that occurs at rest or with exertion causing severe activity limitation Nitro, aspirin, beta blockers, EKG, PCI Myocardial Infarction (STEMI & NonSTEMI) chest pain, SOB, nausea EKG, MONA, PCI, CABG CABG and complications, patient education • CABG is indicated when patients do not respond to medical management of CAD or when disease progression is evident. o Complications: Fluid and electrolyte imbalance, Hypotension, Hypothermia, Hypertension, Bleeding, Cardiac tamponade, Decreased level of consciousness, Angina pain Patient education: Develop a teaching plan, which usually includes education about the normal anatomy and physiology of the heart, the pathophysiology of angina and MI, risk factor modification, activity and exercise protocols, cardiac drugs, and when to seek medical assistance. Teach ..........................................................................................Continues [Show More]
Last updated: 1 year ago
Preview 1 out of 30 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 25, 2020
Number of pages
30
Written in
Additional information
This document has been written for:
Uploaded
Nov 25, 2020
Downloads
0
Views
78