*NURSING > NCLEX-RN > NCLEX RN & CGFNS Gastrointestinal Disorders Q&A. 200 Most Commonly tested Questions from Week 1 to (All)
NCLEX RN & CGFNS Gastrointestinal Disorders Q&A. 200 Most Commonly tested Questions from Week 1 to 13- NC III
Document Content and Description Below
NCLEX-RN & CGFNS Practice Question » Gastrointestinal Disorders Questions in Power points from Week 1 to 13- NC III Adequate nutrition is required for healing after treatment for recurrent aphth... ous ulcers (RAU). Which client response indicates that nursing teaching has been effective? A. “I've ordered a snack of milk and pretzels.” B. “I‘ll try to drink orange juice twice per day.” C. “I ordered my sandwich on a crusty roll.” D. “I'd like scrambled eggs and a banana for breakfast.” The nurse is caring for four clients. Which is at the highest risk for development of oral cancer? A. 32-year-old client with ankle fracture B. 41-year-old with human papilloma virus (HPV) infection C. 60-year-old who quit smoking 20 years ago D. 83-year-old who lives in a warm climate during the winter A client with a bleeding peptic ulcer develops sudden, severe upper abdominal pain, becomes diaphoretic and draws his knees over his abdomen. Which finding should the nurse report immediately? A. Increased amylase levels. B. A rigid, board-like abdomen. C. Vomiting tar like feces. D. Bowel sounds increased in frequency and pitch. A client with peptic ulcer disease has a nasogastric tube. Suddenly he complains of severe abdominal pain and the nurse notes that his abdomen is rigid. What action should be implemented first? A. Administer the next scheduled dose of intravenous H2 blocker B. Assess the client’s vital signs. C. Irrigate the nasogastric tube with normal saline D. Administer a prescribed PRN antacid A 68-year-old male has been admitted to the hospital with abdominal pain, anemia and melena. He complains of feeling weak and dizzy. He needs to urinate and move his bowels. The nurse should intervene by: A. Helping him to the bed side commode B. Offering him the bedpan and the urinal C. Transferring him to BR in a wheelchair D. Asking a male UAP to transfer him to BR for privacy The healthcare provider prescribes high-protein, high-fat, low-carbohydrate diet with limited fluids during meals for a client recovering from gastric surgery. The client asks the nurse what the purpose is for this type of diet. Which rationale should be included in the nurse's explanation to this client? A. It is quickly digested. B. It does not cause diarrhea. C. It does not dilate the stomach. D. It is slow to leave the stomach. A stressed client, who smokes 13 cigarettes/day, consumes fast-food, and is a strong drinker of coffee, is consulting to the healthcare facility for heartburn, specially after ingesting spicy food. The triage nurse should recommend: A. Avoid spicy food and increase consume of dairy B. Consume Decaf instead of regular coffee C. Schedule an appointment for a physical D. Use over the count omeprazole every day until relief of symptoms The nurse notices that a patient has had a black, tarry stool and recalls that a possible cause would be: a. gallbladder disease. b. overuse of laxatives. c. upper gastrointestinal bleeding. d. localized bleeding around the anus. In a paracentesis 3 liters of fluid are removed. Which assessment parameter is most critical for the nurse to monitor following the procedure? A. Pedal pulses. B. Breath sounds. C. Gag reflex. D. Blood pressure. What finding is a priority in a patient with peptic ulcer disease (PUD)? A. Tarry stools 3 times during the day B. Dizziness when sitting in bed C. Epigastric pain 2 hours after meals D. Loss of 10 pounds of weight since the last month The nurse is teaching a client with advanced COPD who was prescribed theophylline. Which client statement indicates that additional teaching is required? a. I need to avoid caffeinated products b. I need to get my blood drug levels checked periodically c. I need to report anorexia and sleeplessness d. I take cimetidine for my heartburn A client has been on long-term therapy with esomeprazole. What is essential for the nurse to ask the client? a. Are you drinking plenty of water with the medication? b. Are you taking the medication after meals? c. Have you had a bone density test recently? d. Have you had your blood pressure taken regularly? The nurse is preparing a client diagnosed with peptic ulcer disease for a barium study of the stomach and esophagus. Which nursing intervention is the priority for this client? 1. Obtain informed consent from the client for the diagnostic procedure. 2. Discuss the need to increase oral fluid intake after the procedure. 3. Explain to the client that he or she will have to drink a white, chalky substance. 4. Tell the client not to eat or drink anything prior to the procedure. At 0830, the day shift nurse is preparing to administer medications to the client NPO for an endoscopy. Which medication should the nurse question administering? 1. Digoxin 0.125 mg PO every day. 2. Furosemide 40 mg PO bid. 3. Ranitidine 150 mg in 250 mL NS IV continuous infusion every 24 hours. 4. Vancomycin 850 mg IVPB every 24 hours. The client is diagnosed with esophageal bleeding. Which of the following assessment data warrants immediate intervention by the nurse? 1. The client’s hemoglobin/hematocrit is 11.4/32. 2. The client’s abdomen is soft to touch and non-tender. 3. The client’s vital signs are T 99, AP 114, RR 18, B/P 88/60. 4. The client’s nasogastric tube has coffee ground drainage. The client 2 days postoperative from a laparoscopic cholecystectomy tells the office nurse, “My right shoulder hurts so bad I can’t stand it.” Which statement is the nurse’s best response? 1. “This is a result of the carbon dioxide gas used in surgery.” 2. “Call 911 and go to the emergency department immediately.” 3. “Increase the pain medication the surgeon ordered.” 4. “You need to ambulate in the hall to walk off the gas pains.” The male client is 30 minutes post-procedure liver biopsy. Which action by the unlicensed assistive personnel (UAP) requires the nurse to intervene? 1. The UAP offered the client a urinal to void. 2. The UAP gave the client a glass of water. 3. The UAP turned the client on the left side. 4. The UAP took the client’s vital signs. After teaching a client with irritable bowel syndrome (IBS), a nurse assesses the client’s understanding. Which menu selection indicates that the client correctly understands the dietary teaching? a. Ham sandwich on white bread, cup of applesauce, glass of diet cola b. Baked tilapia with brown rice, steamed broccoli, glass of orange juice c. Grilled cheese sandwich, small banana, cup of hot tea with lemon d. Broiled chicken, mashed potatoes, cup of coffee with low-fat milk The emergency department nurse is assessing a client with a known inguinal hernia. Which assessment findings indicate that the hernia may have strangulated? Select all that apply. A. Fever B. Tachycardia C. Abdominal distention D. Nausea and vomiting E. Mild abdominal pain – (no because it is moderate to severe) The nurse is preparing a discharge teaching plan for the client who had an umbilical hernia repair. Which of the following would the nurse include in the plan? 1. Restricting pain medication 2. Maintaining bedrest 3. Avoiding coughing 4. Irrigating the drain The community nurse is talking with a group of individuals about colorectal cancer (CRC) risk factors. Which community participant is at the highest risk for development of CRC? A. 43-year-old facto-vegetarian B. 30-year-old with Crohn's disease C. 69-year-old with no family history of cancer D. 46-year-old with grand parent who died of CRC Three days after a colon resection, the nurse is assessing a client with a nasogastric tube (NGT) to intermittent suction. What assessment is the best to determine proper placement of the NGT? A. Auscultate epigastric sounds while insufflating air through NGT. B. Percuss abdomen for stomach distention. C. Check residual and test the pH. (PH should be acid) D. Review the X-ray report done when NGT was inserted. The nurse administers a tube feeding to a patient with a baseline decreased mental status. Immediately after completing the tube feeding, it is MOST important for the nurse to place the client in which of the following positions? A. Supine with the lower extremities elevated on pillows. B. High Fowler’s or semi-Fowler’s position. C. Supine with the head of the bed elevated 45°. D. On the right side with the head of the bed elevated. The nurse is providing preoperative teaching to a patient who will undergo surgery to create a temporary colostomy. The patient asks the nurse about the difference between colostomies and ileostomies. The best response by the nurse is: A. “A colostomy occurs in the GI tract, and an ileostomy occurs in the urinary tract.” B. “A colostomy is temporary, and an ileostomy is always permanent.” C. “A colostomy is in the large intestine, and an ileostomy is in the small intestine.” D. “Dietary restrictions are required for the patient with an ileostomy but not a colostomy.” The nurse working in the emergency department realizes that which of the following patients with acute abdominal pain is most likely to have acute appendicitis? A. an 8-month-old female B. a 14-year-old male C. an 85-year-old woman D. a 70-year-old male Assessment of the patient’s gag response is a priority nursing intervention following which of the following procedures? A. colon biopsy B. small bowel biopsy C. barium enema D. colonoscopy The nurse intends to participate in a health screening clinic and is preparing teaching materials about colorectal cancer. The nurse should plan to include which of the following in a list of risk factors for colorectal cancer? A. age older than 30 years B. high fiber, low fat diet C. distant relative with colorectal cancer D. personal history of GI polyps The nurse understands that which of the following is a viral pathogen that frequently causes acute diarrhea in young children? A. giardia B. shigella C. rotavirus D. salmonella The nurse knows that acute diarrhea in children is often caused by which of the following? A. celiac disease B. antibiotic therapy C. vitamin deficiency D. protein malnutrition The nurse is caring for a 4-year-old child with celiac disease. The nurse expects to find which of the following manifestations of the disease while assessing the child and obtaining the health history from the patient’s mother? A. anorexia, abdominal distention, steatorrhea B. vomiting, diarrhea, abdominal pain, jaundice C. constipation, abdominal cramping, flatulence D. nausea, vomiting, diarrhea When caring for a child with probable appendicitis, the nurse must be alert to recognize which of the following signs of perforation? A. nausea and vomiting B. anorexia C. sudden relief from pain D. decreased abdominal distention The nurse is caring for a patient with an ileostomy. The nurse anticipates that a normal stoma should appear: A. pale pink. B. reddish pink. C. red with white edges. D. purple. The nurse is planning the care of a client diagnosed with acute gastroenteritis. Which nursing problem is priority? 1. Altered nutrition. 2. Self-care deficit. 3. Impaired body image. 4. Fluid and electrolyte imbalance. The nurse is performing ostomy care for a client who had an abdominal-peritoneal resection with a permanent sigmoid colostomy. Rank the following interventions in order of priority. 1. Cleanse the stomal site with mild soap and water. 2. Assess the stoma for a pink, moist appearance. 3. Attach the ostomy drainage bag to the abdomen. 4. Apply stoma adhesive paste to the skin around the stoma. 5. Monitor the drainage in the ostomy drainage bag. The nurse is transcribing the HCP’s orders for a client who is scheduled for an emergency appendectomy and is being transferred from the emergency department (ED) to the surgical unit. Which order should the nurse implement first? 1. Obtain the client’s informed consent. 2. Administer 2 mg of IV morphine, every 4 hours, PRN. 3. Shave the lower right abdominal quadrant. 4. Administer the on-call IVPB antibiotic. The female client, diagnosed with diverticulosis, called the home healthcare agency and told the nurse, “I am having really bad pain in my left lower stomach and I think I have a fever.” Which action should the nurse take? 1. Recommend the client take an antacid and lie flat in the bed. 2. Instruct one of the nurses to visit the client immediately. 3. Tell the client to have someone drive them to the emergency room. 4. Ask the client what she has had to eat in the last 8 hours. What information in a client's history indicates the highest risk factor for Hepatitis C? A. Homosexuality. B. Intravenous drug abuse. C. Eating contaminated shellfish. D. Recent travel to an underdeveloped country. In a paracentesis 3 liters of fluid are removed. Which assessment parameter is most critical for the nurse to monitor following the procedure? A. Pedal pulses. B. Breath sounds. C. Gag reflex. D. Blood pressure. Which data is the most important in the history of a patient with hepatitis C? A. Frequency and amount of alcohol consume B. Number of sexual partners and use of condoms C. Time since the first time a blood transfusion was received D. Presence of jaundice and dark urine The nurse understands that only one of the following clients needs total parenteral nutrition. Which client has a formal indication of TPN? a. Stroke and dysphagia; history of aspiration pneumonia b. Head trauma, bed sore, and comma c. Anorexia nervosa, BMI 16, chronic diarrhea d. Obstructive esophageal cancer, radiotherapy A nurse is caring for a client who is receiving TPN, but the next bag of solution is not available for administration at this time. Which of the following is an appropriate action by the nurse? a. Administer 10% dextrose in water IV until the next bag is available. b. Slow the infusion rate of the current bag until the solution is available. c. Monitor for hyperglycemia d. Monitor for hyperosmolar diuresis. A client who has begun receiving TPN with lipids develops sudden shaking chills, shortness of breath, and chest pain. The priority action by the nurse is to immediately a. call the physician. b. obtain a 12-lead ECG. c. stop the infusion. d. take a set of vitals. A young adult female client is admitted to a psychiatric facility with a diagnosis of bulimia nervosa. Which nursing intervention has the highest priority? A. Schedule the client for group therapy with other bulimic clients B. Assign an UAP to observe the patient all time, including trips to the bathroom C. Monitor the client carefully for binging activities D. Assess an report the client’s electrolyte status to the healthcare provider An adolescent girl with anorexia nervosa is being discharged from the mental health unit with a prescription for fluoxetine. Which instruction is most important for the nurse to provide the parents? A. Encourage activities that allow the daughter to exhibit control B. Check the daughter mouth to ensure that she swallows the Prozac C. Observe the daughter weigh herself at the same time every day D. Listen for the daughter’s expressions of wanting to harm herself The nurse observes that a male client on a clear liquid diet has a cup of coffee on his breakfast tray. What action should the nurse implement? a. Remind the client that no milk or creamer can be added to the coffee< b. Remove the coffee from the tray c. Determine which member of the staff brought the coffee d. consult with the dietician to learn if the client is allowed to drink coffee Steatorrhea is associated with all of the following EXCEPT: a. pancreatic exocrine insufficiency. b. pancreatic beta-cell insufficiency. c. loss of the proximal small intestine. d. intestinal villous malfunction. Complications of obesity include all of the following EXCEPT: a. arthritis b. coronary artery disease c. gall stones d. obstructive sleep apnea e. type I (insulin dependent) diabetes mellitus The nurse is assessing a child’s weight and height during a clinic visit prior to starting school. The nurse plots the child's weight on the growth chart and notes that the child's weight is in the 95th percentile for the child’s height. What action should the nurse take? A. Recommend a daily intake of at least four glasses of whole milk. B. Encourage giving two additional snacks each day to the child. C. Question the type and quantity of foods eaten in a typical day. D. Assess for signs of poor nutrition, such as a pale appearance. The nurse is planning to conduct nutritional assessments and diet teaching to clients at a family health clinic. Which individual has the greatest nutritional and energy demands? A. A pregnant woman with twins. B. A teenager beginning puberty. C. A 3-month-old infant. D. A school-aged child. The nurse preparing a postoperative teaching plan for a client who had a gastric stapling would include that a. dumping syndrome is a common side effect. b. fluids must be taken in liberal amounts. c. exercise is prohibited after meals. d. small, frequent feedings must become a habit. When working with older adults to promote good nutrition, what actions by the nurse are most appropriate? (Select all that apply.) a. Allow uninterrupted time for eating. b. Assess dentures for appropriate fit. c. Ensure that the patient has glasses on when eating. d. Provide salty foods that the patient can taste. e. Serve high-calorie, high-protein snacks. When assisting a dysphagic client to eat, the nurse should a. have the client slightly flex the neck for swallowing. b. place the client in Sims position for 15 minutes after meals. c. position the client in the semi-Fowler position. d. use the fingers to check the client’s mouth for food. A morbidly obese client is admitted to a community hospital that does not typically care for bariatric-sized patients. The client has past medical history of hypertension and diabetes mellitus. What intervention in planning care by the nurse is most appropriate? a. Assessment of capillary blood sugar every4 hours. b. Ensure adequate assistive device when moving the patient. c. Dietary evaluation for diet low in unsaturated fats d. Non pharmacological management of hypertension A nurse assesses a patient who is recovering from a lumbar laminectomy. Which complications would alert the nurse to urgently communicate with the healthcare provider? (Select all that apply.) a. Surgical discomfort b. Redness and itching at the incision site c. Incisional bulging d. Clear drainage on the dressing e. Sudden and severe headache A client has a herniated disc at S5-L1 and back pain. For greatest comfort, the nurse should position this client: a. In semi Fowler’s with a pillow under ankles b. Supine with knees flexed c. Prone with cold pads on back d. Alternating lateral with knees flexed The nurse notes that no urinary output has occurred in a patient who underwent a laminectomy 2 hours earlier. The nurse should: a. Continue to monitor. b. Inform the charge nurse. c. Perform intermittent catheterizations. d. Turn the patient to the right side. A school nurse is called after a student falls down a flight of stairs. The student is breathing, but unconscious. Which is the most appropriate initial action by the nurse? 1. Extend the neck to open airway. 2. Place the patient on his side to prevent aspiration. 3. Immobilize the neck, securing the head. 4. Assess vital signs and pupil reactions. Which technique of opening the airway in the newly admitted patient with a SCI is the most appropriate? a. Chin lift b. Head tilt c. Jaw thrust d. Neck flexion A client with a spinal cord injury at the T1 level complains of a severe headache and an "anxious feeling." The nurse confirms high blood pressure. Which is the most appropriate initial reaction by the nurse? 1. Try to calm the patient and make the environment soothing. 2. Assess for a full bladder. 3. Notify the healthcare provider. 4. Sit the client. The nurse is caring for a female client with scoliosis who had a posterior spinal fusion and is in a body jacket cast. Which assessment finding indicates to the nurse the client is developing cast syndrome? a. Abdominal distention and vomits b. Hot spot felt on cast. c. Diminished mesenteric pulses. d. Musty, unpleasant odor to cast. The nurse is educating a patient and the family about different types of stabilization devices. Which statement by the patient indicates that the patient understands the benefit of using a halo fixation device instead of Gardner-Wells tongs? 1. "I will have less pain if I use the halo device." 2. "The halo device will allow me to get out of bed." 3. "I am less likely to get an infection with the halo device." 4. "The halo device does not have to stay in place as long." A nurse plans care for a patient with a halo fixator. Which interventions would the nurse include in this patient’s plan of care? (Select all that apply.) a. Tape a halo wrench to the patient’s vest. b. Assess the pin sites for signs of infection. c. Loosen the pins when sleeping. d. Decrease the patient’s oral fluid intake. e. Assess the chest and back for skin breakdown. The patient with a SCI begins to have seizures, and the blood pressure (BP) rises rapidly to 210/160 mm Hg. Which is the third indicator of the dreaded syndrome of autonomic dysreflexia? a. Profuse vomiting b. Hives on face and neck c. Excessive urine output d. Bradycardia A nurse cares for a patient with a spinal cord injury. With which interdisciplinary team member would the nurse consult to assist the patient with activities of daily living? a. Social worker b. Physical therapist c. Occupational therapist d. Case manager You're performing a head-to-toe assessment on a patient with multiple sclerosis. When you ask the patient to move the head and neck downward the patient reports an "electric shock" sensation that travels down the body. You would report your finding to the doctor that the patient is experiencing:* A. Romberg's Sign B. Lhermitte's Sign C. Uhthoff's Sign D. Homan's Sign Which finding below represents a positive Romberg Sign in a patient with multiple sclerosis?* A. The patient report dark spots in the visual fields during the confrontation visual field test. B. When the patient closes the eyes and stands with their feet together they start to lose their balance and sway back and forth. C. The patient's sign and symptoms increase when expose to hot temperatures. D. The patient reports an electric shock feeling when the head and neck are moved downward. During your discharge teaching to a patient with multiple sclerosis, you educate the patient on how to avoid increasing symptoms and relapses. You tell the patient to avoid: A. Hot temperatures B. Infection C. Overexertion D. Salt F. Stress The nurse is evaluating the client with ALS (amyotrophic lateral sclerosis) for indications of requiring ventilatory support. What parameters should the nurse assess? SATA a. Use of accessory respiratory muscles. b. Restlessness c. Bradycardia d. Forced expiratory volume e. Pulse oximetry f. Respiratory alkalosis The home health nurse has four phone messages from clients. Which one should the nurse answer first? a. Client with COPD and chronic cough, who found blood in the expectoration b. Female post radical mastectomy who notices her arm more swollen c. Client with ALS who called to discontinue his home health services d. Male programmed for colonoscopy who wants to know if coffee is allowed before the test. Select all the signs and symptoms below that can present in myasthenia gravis: A. Respiratory failure B. Increased salivation C. Diplopia D. Ptosis E. Slurred speech F. Restlessness G. Mask-like appearance of looking sleepy H. Difficulty swallowing Which medication could help to differentiate a myasthenic from a cholinergic crisis? a. Pyridostigmine b. Neostigmine c. Edrophonium d. Prednisone While assisting with a edrophonium test you will have what antidote on hand? A. Naloxone B. Atropine C. Flumazenil D. Glucagon The nurse is planning care for a client admitted with myasthenia gravis. In what moment of the day should the nurse plan most of the physical activities for this client? a. At least one hour after a dose of narcotic pain killer, when pain is less b. Before lunch, when the client has not eaten, because the slow digestion c. In the morning, soon after getting out of bed d. In the evening, when several doses of cholinergic medication have already been taken. The nurse is teaching a class on the prevention of brain attacks (cerebrovascular accidents). Which of the following risk factors should the nurse identify as the most important factor contributing to all forms of stroke? 1. Diabetes 2. Hypertension 3. Smoking 4. Obesity A patient experienced a period of momentary confusion, dizziness, and slurred speech but recovered in 2 hours. The most helpful assessment in the diagnosis of this episode would be: a. Patient’s complaint of nausea b. Blood pressure (BP) of 140/90 mm Hg c. Patient’s complaint of intense headache d. Auscultation of a bruit over the carotid artery A 65-year-old male recently suffered a cerebral vascular accident. He is now unable to recognize and identify objects by touch because of injury to the sensory cortex. How should the nurse document this finding? a. Hypomimesis b. Agnosia c. Dysphasia d. Echolalia The nurse is planning care for a client who has a right hemispheric stroke and left homonymous hemianopsia. Which nursing diagnosis should the nurse include in the plan of care? a. Impaired physical mobility related to right-sided hemiplegia. b. Impaired verbal communication related to aphasia, agraphia and/or alexia c. Risk for injury related to denial of deficits and impulsiveness. d. Ineffective coping related to depression and distress about disability. The nurse is admitting a client diagnosed to have a cerebrovascular accident involving left brain damage. The nurse evaluates which of the following to be clinical manifestations of a cerebrovascular accident involving left-brain damage? Select all that apply: 1. Paralyzed right side 2. Aphasia 3. L eft-sided neglect 4. Paralyzed left side 5. Depression 6. Denial of deficits A patient has been admitted with a diagnosis of stroke (brain attack). The nurse suspects that the patient has had a right hemisphere stroke because the patient exhibits which symptoms? a. Aphasia and cautiousness b. Impulsiveness and smiling c. Inability to discriminate words d. Quick anger and frustration A nurse assesses a patient recovering from a cerebral angiography via the patient’s right femoral artery. Which assessment would the nurse complete? a. Restrict fluids to prevent brain edema b. Obtain sitting blood pressure for orthostatic hypotension. c. Palpate bilateral lower extremity pulses. d. Assess the gag reflex prior to eating. A day after a CVA, the patient’s family asks the nurse if tissue plasminogen activator (tPA) is a drug therapy option. The nurse’s response is based on the knowledge that this drug must be used within how many hours after the onset of symptoms? a. 3 b. 5 c. 10 d. 24 In caring for an unconscious patient who suffered a stroke 10 days ago, the nurse positions the patient to prevent the limbs from: a. Flexion deformities b. Atrophy c. Paralysis d. Pathologic fracture The client diagnosed with a cerebrovascular accident (CVA) is confined to a wheelchair for most of the waking hours. Which intervention is priority for the nurse to implement? 1. Encourage the client to move the buttocks every 2 hours. 2. Order a high-protein diet to prevent skin breakdown. 3. Get a pressure-relieving cushion to place in the wheelchair. 4. Refer the client to physical therapy for transfer teaching Which basic activity of daily living assistive device can be useful for the post stroke client who is affected with poor fine motor coordination? a. An aphasia aid b. A button hook c. Honey thickened liquids d. A wheelchair The client diagnosed with a cerebrovascular accident (CVA) has residual right-sided hemiparesis and difficulty swallowing, but is scheduled for discharge. Which referral is most appropriate for the case manager to make at this time? 1. Skilled nursing rehabilitation unit. 2. Home healthcare agency. 3. Long-term care facility. 4. Outpatient therapy center. The nurse and unlicensed assistive personnel (UAP) are caring for a client with right-sided paralysis. Which action by the UAP requires the nurse to intervene? 1. The UAP places the gait belt around the client’s waist prior to ambulating. 2. The UAP places the client on the abdomen with the client’s head to the side. 3. The UAP places her hand under both client’s axilla to help the client move up in bed. 4. The UAP praises the client for performing activities of daily living independently. The client diagnosed with a right-sided cerebral vascular accident (CVA), or brain attack, is admitted to the rehabilitation unit. Which interventions should be included in the nursing care plan? Select all that apply. 1. Position the client to prevent shoulder adduction. 2. Refer the client to occupational therapy daily. 3. Encourage the client to move the affected side. 4. Perform quadriceps exercises five times a day. 5. Instruct the client to hold the fingers in a fist. The 69-year-old client post–right cerebral vascular accident (CVA) is on the rehab unit with left leg weakness. What should the nurse instruct the client about use of the quadriplex cane when assisting the client to ambulate? a. Hold the cane with the left hand b. Advance the cane when left leg advances c. Adjust cane height to waist level d. When left leg advances keep cane on floor for support The charge nurse observes the client’s nurse telling the unlicensed assistive personnel (UAP) to feed an elderly client diagnosed with a cerebrovascular accident (CVA). Which question should the charge nurse ask the client’s nurse? 1. “How does the client swallow the medications?” 2. “Did you complete your head to toe assessment?” 3. “Does the client have some Thick-It in the room?” 4. “Why would you delegate feeding to a UAP?” A nurse has applied to work at a hospital that has National Stroke Center designation. The nurse realizes that the hospital adheres to eight Core Measures for ischemic stroke care. What do these Core Measures include? (Select all that apply.) a. Discharging the patient on a statin medication b. Providing the patient with comprehensive therapies c. Meeting goals for nutrition within 1 week d. Providing and charting stroke education e. Preventing venous thromboembolism A male client who sustained a head injury following and automobile collision is admitted to the hospital. The nurse includes the client’s risks for developing increased intracranial pressure (ICP) in the plan of care. Which signs indicate to the nurse that ICP is increased? a. Experiencing the worst headache of his life. b. Bradycardia and systolic hypotension. c. Confusion and papilledema. d. Periorbital ecchymosis (raccoon sign) A patient with a severe head injury begins to assume a posture of flexed upper extremities, with plantar-flexed lower extremities. These assessments indicate: a. Increasing intracranial pressure (ICP) with decorticate posturing b. Decreasing ICP with decerebrate posturing c. Decreasing ICP with decorticate posturing d. Increasing intracranial pressure with decerebrate posturing. The nurse caring for a 80-year-old patient with a closed head injury would immediately report: a. Blood pressure change from 137/72 to 166/70 mm Hg b. Heart rate increases from 64 to 92 beats/min c. Bilateral slow pupillary reaction to light d. Temperature suddenly changes from 100.2° to 97.6° F The earliest assessment indicating that mannitol therapy for cerebral edema is effective in a patient with increased ICP is: a. Increased BP b. Increased urinary output c. Decreased pulse d. Widening pulse pressure Which of the following is a priority when suctioning a client with increased intracranial pressure? 1. Limit the suction passes to 20 seconds 2. Suction the client as needed 3. Suction the client at least every hour 4. Schedule the suctioning with other nursing tasks A nurse is providing community screening for risk factors associated with stroke. Which patient would the nurse identify as being at highest risk for a hemorrhagic stroke? a. A 65-year-old who is taking clopidogrel b. A 30-year-old who drinks every day c. A 40-year-old who uses to lift heavy weights d. A 27-year-old heavy-cocaine user A client is diagnosed with a ruptured brain artery aneurysm. The nurse observed stiff neck, ptosis and right hemiparesis. Which cranial nerve is involved when the patient is experiencing ptosis? a. Abducens (VI) b. Facial (VII) c. Trochlear (VI) d. Oculomotor (III) A patient who has suffered a hemorrhagic stroke is placed on a protocol of 60 mg calcium channel blocker (nimodipine) every 4 hours. The patient’s pulse is 62 beats/min before the administration of the prescribed dose. The nurse should: a. Give the full dose as prescribed, without further assessment. b. Object the drug, recording it is contraindicated in hemorrhages. c. Delay the dose until the pulse is above 70 beats/min. d. Give half of the prescribed dose (30 mg). An older client is admitted with a cerebral vascular accident (CVA). He has facial paralysis and cannot move his left side. When entering the room, the nurse finds the client’s wife trying unsuccessfully to give him a drink of water. What action should the nurse take? a. Assist the wife and carefully give the client small sips of water b. Give the wife a straw to facilitate the client’s drinking c. Obtain thickening powder before providing any more fluids d. Ask the wife to stop and assess the client’s swallowing reflex A 25-year-old male was in an automobile accident. At impact, his forehead struck the windshield. In this situation, a nurse recalls the countercoup injury would occur in the _____ region. a. Frontal b. Temporal c. Parietal d. Occipital A patient has a traumatic brain injury and a positive halo sign. The patient is in the intensive care unit, sedated and on a ventilator, and is in critical but stable condition. What collaborative problem takes priority at this time? a. Inability to communicate b. Risk for increased ICP c. Risk for infection d. Risk for skin breakdown a) b) D) F) Which is the most common benign tumor that arises from the coverings of the brain (the meninges)? a. Meningioma b. Supratentorial c. Pituitary tumors d. Acoustic neuroma Which areas are mostly affected by brain abscesses? a. Cerebellum b. Frontal lobe c. Parietal lobe d. Occipital lobe Which statement about brain abscesses is correct? a. The white blood cell (WBC) count is decreased if a brain abscess is present. b. Magnetic resonance imaging (MRI) cannot detect an abscess in its early stage. c. An electroencephalogram (EEG) shows electro-cerebral silence in the area of abscess. d. The erythrocyte sedimentation rate (ESR) is decreased if a brain abscess is present. A 32-year-old male was injured in a motor vehicle accident and confined to bed for 3 weeks. During this time, the size and strength of muscle fibers decreased, a condition referred to as: a. Myodysplasia b. Ischemic atrophy c. Disuse atrophy d. Deconditioning hypoplasia An important and useful clinical measure in the diagnosis of rhabdomyolysis is measurement of which laboratory value? a. White blood cell count (CBC) b. Antinuclear antibodies (ANA) c. Erythrosedimentation rate (ESR) d. Creatine kinase (CK) While performing an assessment of a 2-month-old, the nurse notes a positive Ortolani click. The nurse would suspect the child has: a. A hip fracture b. Hip dysplasia c. Osteogenesis imperfecta d. Osteomyelitis Duchenne muscular dystrophy (DMD) has a(n) _____ inheritance pattern. a. Autosomal recessive b. X-linked recessive c. Y-linked dominant d. Autosomal dominant A 9-month-old male was diagnosed with osteogenesis imperfecta (OI) following recurrent fractures and findings of osteopenia. This disease is caused by: a. Uterine teratogens b. A genetic defect c. Malnutrition d. Trauma A 1-year-old female was diagnosed with OI. Which of the following is a complication in this patient? a. Seizures b. Liver failure c. Aortic aneurysm d. Pulmonary emboli A 70-year-old female with osteoporosis fractures her leg at a location of preexisting abnormality. She reports that the fracture occurred following a minor fall. Which of the following best describes the fracture? a. Fatigue fracture b. Stress fracture c. Pathologic fracture d. Greenstick fracture A patient has a bone density score of –2.8. What action by the nurse is best? a. Asking the patient to complete a food diary b. Planning to teach about bisphosphonates c. Scheduling another scan in 2 years d. Scheduling another scan in 6 months A nurse sees patients in an osteoporosis clinic. Which patient would the nurse see first? a. Patient taking calcium with vitamin D (Os-Cal) who reports flank pain 2 weeks ago b. Patient taking ibandronate (Boniva) who reports stools with streaks of red bright blood c. Patient taking raloxifene (Evista) who reports unilateral calf swelling d. Patient taking risedronate (Actonel) who reports occasional dyspepsia A 56-year-old male was admitted to the hospital with a diagnosis of osteomalacia. History reveals that he takes anticonvulsants, underwent small bowel resection 3 years earlier, and suffers from chronic pancreatitis. What is the common link between these three factors and the development of osteomalacia? a. Impaired phosphate absorption b. Increased calcium excretion c. Vitamin D deficiency d. Impaired vitamin C metabolism The nurse studying osteoporosis learns that which drugs can cause this disorder? (Select all that apply.) a. Antianxiety agents b. Antibiotics c. Anticonvulsants d. Corticosteroids e. Proton Pump Inhibitors A 35-year-old female presents with impaired motor function and visual disturbances. The diagnosis is Paget disease. What additional symptoms would be expected? (Select all that apply.) a. Skull thickness b. Fractures c. Deafness d. Headache e. Hypertension A 70-year-old male presents with back pain, fever, and weight loss. He reports that he had a recent respiratory infection from which he thought he recovered. Tests revealed increased white blood cell count, and a diagnosis of endogenous osteomyelitis was made. The primary organism causing this condition is: a. Staphylococcus aureus b. Salmonella c. Mycobacterium d. Haemophilus influenza A malignant tumor of striated muscle tissue origin is called: a. Myelogenic tumor b. Myocarcinoma c. Rhabdomyosarcoma d. Rhabdomyoma A school nurse is conducting scoliosis screening. In screening the patient, what technique is most appropriate? a. Bending forward from the hips b. Sitting upright with arms outstretched c. Walking across the room and back d. Walking with both eyes closed The nurse is caring for a female client with scoliosis who had a posterior spinal fusion and is in a body jacket cast. Which assessment finding indicates to the nurse the client is developing cast syndrome? A. Hot spot felt on cast. B. Diminished mesenteric pulses. C. Abdominal distention and vomits D. Musty, unpleasant odor to cast. A 32-year-old obese male begins a jogging routine. A week after beginning, he fractures his leg. This is referred to as a what type of fracture? a. Comminuted b. Greenstick c. Fatigue d. Compound A client with an open reduction and application of an external fixator for open, comminuted fractures of the tibia and fibula begins to complain of severe pain in the affected leg, which is not relieved by analgesics. The client says the toes are numb and tingling, although they appear pink. What action should the nurse implement? A. Notify the healthcare provider. B. Check the client's temperature and apply cool compresses. C. Check pedal pulses before and after loosen the screws on the external fixture pins. D. Neurovascular exam, elevate the extremity and apply warm compresses. On the second day after admission, a client with a fractured pelvis develops chest pain, tachypnea, and tachycardia. Which additional finding should the nurse identify that is most likely related to a fat embolism? A. Hypotension. B. Restlessness and confusion. C. Warm, reddened areas in the leg. D. Petechiae of the anterior chest wall. A nurse assesses an older adult patient who was admitted 2 days ago with a fractured hip. The nurse notes that the patient is confused and restless. The patient’s vital signs are heart rate 98 beats/min, respiratory rate 32 breaths/min, blood pressure 132/78 mm Hg, and SpO2 88%. Which action would the nurse take first? a. Administer oxygen via nasal cannula. b. Re-position to a high-Fowler’s position. c. Increase the intravenous flow rate. d. Assess response to pain medications C) A patient who has had an open reduction and internal fixation (ORIF) of a hip fracture tells the nurse that he is ready to get out of bed for the first time. Which action should the nurse take? a. Use a mechanical lift to transfer the patient from the bed to the chair. b. Check the postoperative orders for the patient’s weight-bearing status. c. Avoid administration of pain medications before getting the patient up. d. Delegate the transfer of the patient to nursing assistive personnel (NAP). A nurse reviews prescriptions for an 82-year-old patient with a fractured left hip. Which prescription would alert the nurse to contact the provider and express concerns for patient safety? a. Meperidine (Demerol) 50 mg IV every 4 hours b. Patient-controlled analgesia (PCA) with morphine sulfate c. Percocet 2 tablets orally every 6 hours PRN for pain d. Ibuprofen elixir every 8 hours for first 2 days A patient arrived at the emergency department after tripping over a rug and falling at home. Which finding is most important for the nurse to communicate to the health care provider? a. There is bruising at the shoulder area. b. The patient reports arm and shoulder pain. c. The right arm appears shorter than the left. d. There is decreased shoulder range of motion A 12-year-old female hurts her ankle while playing basketball. Tests reveal that she tore a ligament. This condition is known as a: a. Sprain b. Strain c. Disunion d. Subluxation A young man arrives in the emergency department with ankle swelling and severe pain after twisting his ankle playing basketball. Which of these prescribed collaborative interventions will the nurse implement first? a. Take the patient to have x-rays. b. Wrap the ankle and apply an ice pack. c. Administer naproxen (Naprosyn) 500 mg PO. d. Give acetaminophen with codeine (Tylenol #3). A 36-year-old male complains of pain and weakness in the elbow. He reports that he is a warehouse worker and lifts boxes daily. MRI reveals inflammation of the tendon where it attaches to bone. This condition is called: a. Periostitis b. Muscle strain c. Bursitis d. Epicondylitis A nurse cares for a client with a deficiency of aldosterone. Which assessment finding should the nurse correlate with this deficiency? a. Increased urine output b. Vasoconstriction c. Blood glucose of 98 mg/dL d. Serum sodium of 144 mEq/L Under what circumstances would a patient’s adrenocorticotropic hormone (ACTH) level most likely increase? a. Malnutrition b. Physiologic stress c. Ingestion of calcium-rich foods d. During estrogen replacement therapy If a patient were experiencing a release of antidiuretic hormone into the blood, which might be happening in the client’s body immediately before the ADH surge? a. Hypotension b. Hypokalemia c. Hypertension d. Volume overload Evidence that a dehydrated patient is compensating by secreting antidiuretic hormone includes: a. Elevated serum sodium level b. Lowering of blood pressure c. Dry mucous membranes d. Reduced urine output A woman with type 1 diabetes has her blood tests done today and has an elevated hemoglobin A1c level. The nurse can conclude that the patient: a. Is noncompliant with her diet b. Has developed resistance to the insulin c. Should have an elevated blood glucose today d. Has had elevated glucose levels over the past 3 months When a patient in the outpatient clinic has an order for blood cortisol testing, which instruction will the nurse provide for the patient? a. “Avoid adding any salt to your foods for 24 hours before the test.” b. “You will need to lie down for 30 minutes before the blood is drawn.” c. “Come to the laboratory to have the blood drawn early in the morning.” d. “Do not have anything to eat or drink before the blood test is obtained.” A patient has a total serum calcium level of 13.3 mg/dL (3.3 mmol/L). The nurse will anticipate the need to teach the patient about testing for a. calcitonin levels. b. catecholamine levels. c. thyroid hormone levels. d. parathyroid hormone levels. A patient is scheduled for a 24-hour urine collection for 17-ketosteroids. The nurse will need to a. keep the specimen on ice and protect from light b. insert a retention catheter. c. have the patient void and save that specimen to start the collection. d. encourage the patient to drink 2 to 3 L of fluid during the 24 hours _________________________________________________________________________ When reviewing the laboratory results for a patient’s total calcium level, which information will the nurse need to consider? a. The blood glucose is elevated. b. The phosphate level is normal. c. The serum albumin level is low. d. The magnesium level is normal. During preoperative teaching for a patient scheduled for trans sphenoidal hypophysectomy for treatment of a pituitary adenoma, the nurse instructs the patient about the need to a. cough and deep breathe every 2 hours postoperatively. b. remain on bed rest for the first 48 hours after the surgery. c. be positioned flat with sandbags at the head postoperatively. d. avoid brushing the teeth for at least 10 days after the surgery. Which nursing action will be included in the postoperative plan of care for a patient who has had a trans sphenoidal resection of a pituitary tumor? a. Monitor urine output every hour. b. Otoscopy exam to detect CSF leak. c. Check glucose hourly for first 12 hours. d. Deep breath and cough to prevent atelectasis. The anti-diuretic hormone is __LOW__ in Diabetes Insipidus and __HIGH__ in SIADH. a. low, low b. absent, absent c. high, low d. low, high What is the priority actions the nurse anticipates been ordered in treating a patient with diabetes insipidus? a. Hypotonic fluids and hormone replacement b. Restrict fluid intake and provide hypertonic solutions c. Low sodium diet and thiazide diuretics d. Restrict refine carbohydrates and start insulin Which patient is most at risk for developing Syndrome of Inappropriate Anti-diuretic Hormone (SIADH)? a. A patient taking Demeclocycline. b. A patient with a tumor on the anterior pituitary gland. c. A patient diagnosed with small cell lung cancer. d. A patient whose kidney tubules are failing to reabsorb water. A 10-year-old child with meningitis is suspected of having diabetes insipidus. In evaluating the child's laboratory values, which finding is sugestive of diabetes insipidus? A. Decreased urine specific gravity. B. Decreased serum osmolarity. C. Decreased hematocrit. D. Decreased serum sodium. What test is usually done to confirm the diagnosis of diabetes insipidus? a. Twenty four hour urine collection b. Urinalysis c. Water restriction test d. Serum sodium D) correct The nurse is caring for a client who had an excision of a malignant pituitary tumor and diabetes insipidus. Which findings should the nurse document that indicate the client is receiving too much treatment? A. Hypernatremia and periorbital edema. B. Muscle spasticity and hypertension. C. Weight gain with low serum sodium. D. Increased urinary output and thirst. Which finding the nurse expects to find in a client with adrenal insufficiency? a. Hyperglycemia b. Hypokalemia c. Tachycardia d. Decreased urinary output Which of the following is not a typical sign and symptom of Cushing’s Syndrome? A. Hyperpigmentation of the skin B. Hirsutism C. Purplish striae D. Moon Face A patient with Addison's disease asks a nurse for nutrition and diet advice. Which of the following diet modification is NOT recommended? A. A diet high in grains B. A diet with adequate caloric intake C. A high protein diet D. A restricted sodium diet The client has decreased adrenal function. What should the nursing care plan for this client include? a. Limit the number of visitors b. Encourage physical activity c. Prevent constipation d. Place the client in reverse isolation Which of the following findings could find the nurse if the treatment of Addisonian crisis is working? a. Decreased blood sugar b. Reduced blood pressure c. Decreasing heart rate d. Increased serum potassium The nurse is planning care of a client with Cushing disease. Which of the following interventions is appropriated to address the diagnosis of risk for injury? a. Request from dietary meals low in refined sugars and potassium. b. Ask the UAP to use a draw sheet to change patient’s position in bed c. Plan to administer pneumococcal vaccine d. Assign a private room for reverse isolation Which statement is incorrect about pheochromocytoma? A. This condition can be trigger by eating foods high in Tyramine such as hamburger meat and spinach. B. Monoamine oxidase inhibitors can trigger signs and symptoms of pheochromocytoma. C. An adrenalectomy is the only surgical treatment for pheochromocytoma. D. Patients with pheochromocytoma are at risk for hypertensive crisis. All of the following are treatments for myxedema coma EXCEPT? A. Corticosteroids B. IV glucose C. IV NaCl 0.45% solution D. IV Synthroid A patient with Graves disease is 6 hours post-opt from a thyroidectomy. The nurse is aware of the need of continuing the exophthalmos care. Which position should the client be better for this purpose? A. Lateral B. Prone C. Trendelenburg D. Semi-Fowler’s A patient is admitted with thyroid storm. Which sign and symptoms are NOT present with this condition-SELECT ALL THAT APPLY? A. Fever B. Tachycardia C. Constipation D. Eye pain E. Intolerance to cold F. Restlessness G. Hypoventilation H. Atrial fibrillation I. High cardiac output heart failure J. Elevated TSH hormone A physician orders the following indications for a client with a thyroid storm. What order should the nurse carry out first? a. Acetaminophen PO b. Propylthiouracil (PTU) PO c. Propranolol IV d. NaCl 0.9%/Dextrose 5% IV Which of the following medication orders should a nurse question if ordered on a patient with thyroid storm? A. Propylthiouracil "PTU" for a 25 year old who is 8 weeks pregnant B. Aspirin as needed for a fever greater than 102.2 'F C. Inderal for a patient who reports having insomnia D. Methimazole for a 30 year old having complaints of a headache A patient taking methimazole reports feeling dizzy, intolerant to cold, and tired. On assessment, you note the patient's heart rate is 55 and blood pressure is 80/60. What is the most likely cause? A. Antithyroid toxicity B. Agranulocytosis C. Thyroid storm D. Bronchospasm Which instruction should the nurse include when teaching a client about the use of PTU? A. "Call the clinic if symptoms do not subside within 24 hours." B. "You will continue taking this medication the rest of your life." C. "Drink this medication with water or fruit juice." D. "Report the onset of a sore throat or fever.“ When the nurse suspects the client with Graves disease is receiving too much PTU? A. Client complains of sore throat or fever B. Client experiences palpitations and the nurse confirms heart rate above 100 bpm C. Client reports weight gain of two pounds in the last week D. CBC shows a neutrophils count of 500 cells x mm3 A patient is recovery from a parathyroidectomy. Which of the following findings causes concern and requires nursing intervention? A. The patient is in lateral position. B. The patient's calcium level is 8.9 mg/dL. C. The patient’s voice is hoarse. D. The patient is drowsy and arouses to name. The nurse should include which of the following in the preoperative teaching plan for a client with hyperparathyroidism who is scheduled to have a portion of his parathyroid gland removed? 1. Force fluids to at least 3000 ml per day 2. Take over-the-counter supplements of vitamin D daily 3. Maintain bed rest as much as possible 4. Adhere strictly to the high-calcium diet A patient hospitalized with hypoparathyroidism is about to order lunch. Which food selection is best for this patient based on their dietary needs at this time? A. Baked chicken, green beans, and baked potatoes B. Broccoli salad, baked salmon, and peaches (food rich in Ca) C. Roast beef, carrots, and pinto beans D. Hamburger, fries, and sorbet A patient is diagnosed with hyperparathyroidism. Which of the following signs and symptoms would you NOT find in this patient? Select all that apply: A. Calcium level 6 mg/dL (hypoparathyroidism) C. Positive Trousseau’s sign (hypoparathyroidism) D. Tingling and numbness of lips and fingers (hypoparathyroidism) B. Bone fracture (hyperparathyroidism) E. Calcium level of 15 mg/dL (hyperparathyroidism) F. Phosphate level 1.2 (hyperparathyroidism) G. Renal calculi (hyperparathyroidism) H. Constipation (hyperparathyroidism) A Type 2 diabetic may have all the following signs or symptoms EXCEPT: a. Blurry vision b. Ketonuria c. Glycosuria d. Poor wound healing A nurse assesses clients who are at risk for type 2 diabetes mellitus. Which client is at greatest risk? a. A 29-year-old Caucasian b. A 30-year-old African-American c. A 14-year-old Hispanic d. A 58-year-old American Indian A 36 year old male is newly diagnosed with Type 2 diabetes. Which of the following treatments do you expect the patient to be started on initially? a. Life style modifications b. Metformin BID by mouth c. Regular insulin subcutaneous d. None, monitoring at this time is sufficient enough Which of the following patient statements about the diabetic diet regime is correct? A. "I'll try to consume about 40% carbs and 60% proteins on a daily basis." B. “Good foods that are high in mono and polyunsaturated fats are avocados, almonds, and cashews." C. "Meats increase the glycemic index; therefore, I should only consume 5% of them on a daily basis." D. "I should completely avoid starchy vegetables like potatoes, rice, and corn." A nurse teaches a client with diabetes mellitus who is experiencing numbness and reduced sensation. Which statement should the nurse include in this client’s teaching to prevent injury? a. “Examine your feet using a mirror every day.” b. “Rotate your insulin injection sites every week.” c. “Check your blood glucose level before each meal.” d. “Use a bath thermometer to test the water temperature.” A nurse reviews laboratory results for a client with type 1 diabetes mellitus who is prescribed an intensified insulin regimen: • Fasting blood glucose: 105 mg/dL • Postprandial blood glucose: 200 mg/dL • Hemoglobin A1c level: 5.5% How should the nurse interpret these laboratory findings? a. Increased risk for developing ketoacidosis b. Good control of blood glucose c. Increased risk for developing hyperglycemia d. Signs of insulin resistance A nurse reviews the laboratory results of a client who is receiving intravenous insulin. Which should alert the nurse to intervene immediately? a. Serum chloride level of 98 mmol/L b. Serum calcium level of 8.5 mg/dL c. Serum sodium level of 132 mmol/L d. Serum potassium level of 2.5 mmol/L A patient who has diabetes is nothing by mouth as prep for surgery. The patient states they feel like their blood sugar is low. You check the glucose and find it to be 52. The next nursing intervention would be to: a. Notify the doctor for further orders b. Continue to monitor the glucose c. Give the patient 6 oz. of orange juice d. None, this is a normal blood glucose reading A nurse assesses a client who has diabetes mellitus and notes the client is awake and alert, but shaky, diaphoretic, and weak. Five minutes after administering a half-cup of orange juice, the client’s clinical manifestations have not changed. Which action should the nurse take next? a. Administer another half-cup of orange juice. b. Administer a half-ampule of dextrose 50% intravenously. c. Administer 10 units of regular insulin subcutaneously. d. Administer 1 mg of glucagon intramuscularly. A patient is scheduled to take 10 units of insulin NPH at 1100. When is the patient most susceptible for hypoglycemia? A. 1900 B. 1300 C. 1600 D. 1500 After teaching a client with diabetes mellitus to inject insulin, the nurse assesses the client’s understanding. Which statement made by the client indicates a need for additional teaching? a. “The lower abdomen is the best location because it is closest to the pancreas.” b. “I can reach my thigh the best, so I will use the different areas of my thighs.” c. “By rotating the sites in one area, my chance of having a reaction is decreased.” d. “Changing injection sites from the thigh to the arm will change absorption rates.” A nurse cares for a client with diabetes mellitus who is visually impaired. The client asks, “Can I ask my niece to prefill my syringes and then store them for later use when I need them?” How should the nurse respond? a. “Yes. Prefilled syringes can be stored for 3 weeks in the refrigerator in a vertical position with the needle pointing up.” b. “Yes. Syringes can be filled with insulin and stored for a month in a location that is protected from light.” c. “Insulin reacts with plastic, so prefilled syringes are okay, but you will need to use glass syringes.” d. “No. Insulin syringes cannot be prefilled and stored for any length of time outside of the container.” After teaching a client with type 2 diabetes mellitus, the nurse assesses the client’s understanding. Which statement made by the client indicates a need for additional teaching? a. “I need to have an annual appointment even if my glucose levels are in good control.” b. “Since my diabetes is controlled with diet and exercise, I must be seen only if I am sick.” c. “I can still develop complications even though I do not have to take insulin at this time.” d. “Because my type of diabetes, if I have surgery or get very ill, I may have to receive insulin injections for a short time.” A client diagnosed with type I diabetes mellitus receives insulin NPH : 15 units at 7 am and 10 units at 5 pm. The client has normal levels of blood glucose along the day but every morning at 7 am presents a glucose average of 200 mg/dl. The nurse suspects and confirms Somogyi phenomenon. What you anticipate will order the physician? a. Increase dose of 7 am insulin b. Increase dose of 5 pm insulin c. Decrease dinner’s carbohydrate content d. Decrease dose of 5 pm insulin A male patient with Type 2 Diabetes is started on the medication glyburide. Which of the following statements by the patient causes concern? A. "I will monitor my blood glucose regularly because I know this medication can cause a low blood sugar." B. "I will consume no more than 7 oz. of alcohol per week." (PT taking this medication can not take alcohol at all) C. "I will continue monitoring my diet and participating in exercise while taking this medication." D. "This medication works by stimulating the beta cells in the pancreas to make insulin." A nurse reviews the medication list of a client recovering from a computed tomography (CT) scan with IV contrast to rule out small bowel obstruction. Which medication should alert the nurse to contact the provider and withhold the prescribed dose? a. Pioglitazone (Actos) b. Glimepiride (Amaryl) c. Glipizide (Glucotrol) d. Metformin (Glucophage) An 8-year-old boy who is recently diagnosed with diabetes mellitus is admitted to the intensive care unit with diabetic ketoacidosis (DKA). Which nursing action has the highest priority? A. Place on cardiac monitor. B. Initiate an intravenous infusion. C. Collect specimen for serum electrolytes. D. Obtain finger stick glucose. The nurse is taking a history of a newly diagnosed Type 2 diabetic who is beginning treatment. Which subjective information is most important for the nurse to note? A. A history of obesity. B. An allergy to sulfa drugs. C. Cessation of smoking three years ago. D. Numbness in the soles of the feet. A nurse cares for a client who is prescribed pioglitazone (Actos). After 6 months of therapy, the client reports that his urine has become darker since starting the medication. Which action should the nurse take? a. Assess for pain or burning with urination. b. Review the client’s liver function study results. c. Instruct the client to increase water intake. d. Test a sample of urine for occult blood. An overweight adolescent girl has been to the school nurse three times in the last two months complaining of vaginal and urinary tract infections. What action should the nurse take first? A. Counsel the girl regarding hygiene. B. Ask if she is going to the bathroom frequently. C. Teach the girl the importance of practicing safe sex. D. Encourage the girl to see the school counselor Which client is at highest risk for chronic kidney disease (CKD) secondary to diabetes mellitus (DM)? a. Type 1 DM and a serum hemoglobin-A1c of 5.5%. b. Type 2 DM and diabetic retinopathy. c. Type 1 DM and hypertension controlled by lisinopril d. Type 2 DM and a history of morbid obesity for 5 years. A client with type 2 diabetes mellitus presents to the emergency room with signs of hyperosmolar hyperglycemic nonketotic syndrome (HHNS). Which of the client’s laboratory values could be expected to require intervention by the nurse? a. Elevated serum phosphate level b. Elevated serum potassium c. Decreased serum potassium d. Positive urinary ketones An older female client with long term type 2 diabetes mellitus is seen in the clinic for a routine health assessment. To determine if the client is experiencing any long term complications of DM, which assessment should the nurse obtain. SATA a. Visual acuity b. Serum creatinine and BUN c. Signs of respiratory tract infection d. Sensations in feet and legs e. Skin condition of lower extremities A client with type 2 diabetes takes metformin (Glucophage) daily. The client is scheduled for major surgery requiring general anesthesia the next day. The nurse anticipates which approach to manage the client's diabetes best while the client is NPO during the perioperative period? a. NPO except for metformin b. NPO except for oral antidiabetic agent c. NPH insulin subcutaneously twice daily d. Regular insulin subcutaneously per sliding scale A patient undergoing treatment for Hyperglycemic Hyperosmolar Nonketotic Syndrome has a blood glucose of 799. The doctor has ordered intravenous fluids and intravenous Regular insulin therapy. Which of the following findings causes concern before starting insulin therapy? a. Regular insulin cannot be given intravenously; therefore, the nurse needs to clarify the doctor's order. b. The patient's potassium level is 3.1. c. The patient is complaining of severe thirst and has dry mucous membranes. d. The patient is confused and drowsy A 45-year-old woman who is seeing her health care provider states that she is tired all the time and has muscle aches and pains. Assessment reveals a heart rate of 56/min and a BP of 96/58. She has non-pitting edema of her face, especially around her eyes, and in her hands and feet. Her health history includes radioactive iodine (RAI) for hyperthyroidism. What diagnosis does the nurse expect for this patient? Rule out hypothyroidism – most cases of hypothyroidism in the U.S. occur as a result of thyroid surgery and radioactive iodine treatment of hyperthyroidism The provider orders laboratory work that includes thyroid function tests. Which results does the nurse expect to see? A. Normal T3 and T4 levels B. Decreased TSH level C. Increased T3 and T4 levels D. Decreased T3 and T4 levels B. Answer: D C. Laboratory findings for hypothyroidism include decreased T3 and T4 levels and increased thyroid-stimulating hormone (TSH) levels with primary hypothyroidism. With secondary hypothyroidism, the TSH level can be close to normal. Which patient statement indicates that further nursing teaching is needed about hypothyroidism? A. “When I go home I should check my heart rate and BP every day.” B. “I will be sure to include fiber in my diet and drink plenty of water.” C. “I will call my provider if I notice any change in level of consciousness.” D. “When I am feeling better in a few months, I will no longer need to take the Synthroid pills.” Answer: D The most important educational need for the patient with hypothyroidism is about hormone replacement therapy and its side effects. The need to take these drugs is life-long. The patient is preparing to go home. What important teaching points should the nurse include in discharge teaching? (Select all that apply.) A. “Your diet should be low-fiber, but with plenty of fluids.” B. “Note how many hours you sleep in a 24-hr period.” C. “Report any difficulty with orientation to time, place, or person.” D. “Be sure that you take your medication every day at the same time.” E. “Call the provider if you develop an unsteady gait or tremors in your hands.” Answer: B, C, D, E The patient's diet should include fiber to prevent constipation. If the patient is constipated, the dose of replacement thyroid hormone may need to be increased. Sleep should be monitored because when the patient has difficulty getting to sleep, the dose may need to be decreased. Changes in orientation, gait, or development of tremors may require an alteration in dose of replacement thyroid hormone. Medication should be taken at the same time daily. A 56-year-old woman is admitted to the ED with a blood pressure of 168/92 and reports of fatigue and muscle weakness. She has bruising on her arms and 2+ swelling in her ankles. Her weight has gone from 150 lb to 185 lb over the past 6 months. Assessment reveals that she has truncal obesity and thin extremities. Which diagnosis does the nurse suspect? A. Hyperpituitarism (acromegaly) B. Hypercortisolism (Cushing’s disease) C. Hyperaldosteronism (Conn’s syndrome) D. Adrenal insufficiency (Addison’s disease) B. Answer: B The patient’s manifestations of elevated blood pressure, fatigue, muscle weakness, bruising, dependent edema, weight gain, and truncal obesity with thin extremities are all key features of hypercortisolism, or Cushing’s disease. Other manifestations of Cushing’s disease include “moon face,” “buffalo hump,” osteoporosis, and thinning skin with striae. The patient is admitted to the acute medical care unit for a workup for Cushing’s disease. When she is assessed, she is found sitting at the bedside crying. She states, “I just don’t know what to do. I feel so confused and down in the dumps.” What is the nurse’s best response? A. “Would you like to speak with a pastor or priest?” B. “Have you experienced this kind of confusion before?” C. “It’s going to be fine. We’ll find out what’s wrong and take care of it.” D. “Have you noticed if your mood goes quickly from happy to sad?” Answer: D Hypercortisolism can result in emotional lability, including mood swings, irritability, confusion, and depression. Asking this question helps in performing a psychosocial assessment of the patient. The next day, a student nurse is caring for the patient, who is scheduled for an MRI of the head. The student nurse asks why a patient with Cushing’s disease needs this test. What is the nurse’s best response? A. “They are looking for brain cancer which may have caused the disease.” B. “The patient may have had headaches and they are looking for the cause.” C. “The most common cause of Cushing’s is a pituitary tumor called an adenoma.” D. “A tumor of the adrenal gland can cause about 15% of Cushing’s disease cases.” Answer: C Pituitary adenoma is the most common cause of Cushing’s disease, and magnetic resonance imaging (MRI) would visualize such a tumor. The student nurse is creating a care plan for the patient. Which priority problems should be the focus of the care plan? (Select all that apply.) A. Fatigue B. Fluid overload C. Sleep deprivation D. Potential for infection E. Predisposition to injury B. Answer: B, D ,E C. Fluid overload, risk for injury, and inadequate nutrition are common problems in patients with Cushing’s disease. Sleep deprivation and fatigue are additional possible focus areas, but not as essential as the other three. During evening shift, the patient’s MRI reveals the presence of a pituitary adenoma. The following day, surgery is performed to remove the tumor. What is the nurse’s priority concern for the patient postoperatively? A. Airway management B. Assessing for systemic infection C. Monitoring for neurologic changes D. Development of transient diabetes mellitus Answer: C Removal of a pituitary adenoma is completed by a transsphenoidal hypophysectomy. Postoperatively, it is essential to monitor the patient for neurologic response, documenting changes in vision, mental status, level of consciousness, or decreased strength in the extremities. Which key interventions should be implemented postoperatively for the patient after undergoing a hypophysectomy? (Select all that apply.) A. Report any postnasal drip. B. Keep the head of the bed elevated. C. Have the patient avoid coughing soon after surgery. D. Monitor for a light-yellow color at the edge of clear drainage. E. Instruct the patient to take thyroid and glucocorticoid replacement for at least 6 months. Answer: A, B, C, D After hypophysectomy, the patient will need thyroid and glucocorticoid replacement for the rest of her life. The nurse is caring for a patient diagnosed with small cell lung cancer. The nurse understands the patient may also present with which endocrine disorder? A. Adrenal crisis B. Cushing’s syndrome C. Diabetes insipidus (DI) D. Syndrome of inappropriate antidiuretic hormone (SIADH) Answer: D Rationale: Cancer (especially lung cancers) increases the risk of the patient developing SIADH. Other risk factors include recent head trauma, cerebrovascular disease, and tuberculosis or other pulmonary disease. A review of past and current medications is also important in searching for the cause of SIADH. Which priority question should the nurse ask a patient with a pituitary tumor? A. “Have you had an unexpected weight loss?” B. “Have you noticed a change in your libido?” C. “Do you have any changes in your visual acuity?” D. “Have you experienced a change in growth of your facial hair? Answer: C Rationale: Changes in vision are frequently the first and most common symptom associated with hypopituitarism as a result of tumor growth. Changes in weight, hair growth patterns, and secondary sex characteristics should also be assessed. The nurse knows which patient with Cushing’s disease is at greatest risk for developing heart failure? A. 60-year-old with pneumonia B. 59-year-old with a history of hypertension C. 32-year-old with a history of hepatitis B infection D. 42-year-old with a serum creatinine level of 3.7 mg/dL Answer: D Rationale: The 42-year-old patient has compromised kidney function evidenced by an elevated serum creatinine level. Preventing fluid overload that may quickly lead to pulmonary edema and heart failure is a primary concern for patients with Cushing’s disease. Any patient with Cushing’s disease is at risk for developing fluid overload, regardless of age. However, the older adult or one who has coexisting cardiac problems, kidney problems, pulmonary problems, or liver problems, is at greater risk. A 23-year-old patient with a history of type 1 diabetes is admitted to the ED with nausea and abdominal pain. His respiratory rate is 34/min with deep breaths and a fruity smell to his breath. He is responsive, but difficult to arouse. 1. What does the nurse suspect is happening with this patient? The manifestations point to diabetic ketoacidosis (DKA). 2. What serum glucose level would the nurse expect to see with this patient? The patient’s glucose level is most likely >300 mg/dL. The student nurse asks why the patient is breathing so rapidly and deeply. What is the nurse’s best response? A. “His serum pH is high, and this is a compensatory mechanism.” B. “His serum pH is low and this is a compensatory mechanism.” C. “His serum potassium is high and this is a compensatory mechanism.” D. “His serum potassium is low and this is a compensatory mechanism.” Answer: B As ketone levels rise, the buffering capacity of the body is exceeded and the pH of the body decreases, leading to metabolic acidosis. Kussmaul respirations (very deep and rapid) cause respiratory alkalosis in an attempt to correct the acidosis by exhaling carbon dioxide. In the ED, the patient is diagnosed with diabetic ketoacidosis (DKA). What is the nurse’s first priority for managing this condition? A. Airway assessment B. Administration of insulin C. Fluid and electrolyte correction D. Administration of IV potassium Answer: A The first priority is airway management, rapidly followed by the administration of insulin, fluids, and correction of any electrolyte imbalances. Twenty minutes later, the patient is admitted to the ICU for DKA management. The patient is receiving IV regular insulin with frequent finger sticks to check his glucose level. His potassium level is 2.5, and IV potassium supplements have been ordered. What assessment must the nurse make before giving the IV potassium? A. Respiratory rate of less than 24/min B. Production of at least 30 mL/hr of urine C. Level of consciousness and orientation D. Finger stick glucose of less than 200 mg/dL Answer: B Hypokalemia is a common cause of death in the treatment of DKA. Before giving IV potassium, make sure the patient produces at least 30 mL/hr of urine. Two days later the patient is recovered and is preparing for discharge. His wife asks about what they can do to prevent this from happening again. What should the nurse teach the patient and his wife? (Select all that apply.) A. Monitor glucose whenever the patient is ill. B. Decrease fluid intake when nausea and vomiting occur. C. Watch for and report any respiratory o urinary infection. D. Check blood glucose levels every 4 to 6 hours if anorexia, nausea, or vomiting is experienced. E. Check urine ketones when blood glucose is greater than 200 mg/dL. Answer: A,C, D, E It is important to teach the patient to reduce the risk of dehydration by maintaining fluid and food intake. Small amounts of fluid may be tolerated even when vomiting is present. The patient should drink at least 3 L of fluid daily and increase this amount when infection is present. A nurse is teaching a group of patients about diabetes, and explains to the group that what percent of the United States population has diabetes? A. 3.2% B. 5.6% C. 8.3% D. 10.1% When caring for a patient having a hypoglycemic episode, the nurse knows which symptom requires immediate intervention? A. Hunger B. Confusion C. Headache D. Tachycardia The nurse is teaching a patient with type 1 diabetes about exercise. The nurse understands the patient should avoid exercise during what time? A. During colder months B. When serum glucose is less than 150 C. When ketones are present in the urine D. When emotional stressors are high for the patient A nurse is developing a plan of care for an older client with diabetic neuropathy of the lower extremities resulting from type 2 diabetes mellitus. Which problem does the nurse recognize as the highest priority for this client? a. Change in body image b. Increased risk for injury c. Increased risk of depression d. Lower level of physical activity The nurse is teaching client with newly diagnosed diabetes mellitus who has been prescribed NPH insulin how to recognize the signs of hypoglycemia. The client states that he must look for certain signs and symptoms in the late afternoon, indicating to the nurse that he has understood the instructions. What are these signs and symptoms? Select all that apply. a. Shakiness b. Confusion c. Blurred vision d. Increased thirst e. Feelings of hunger f. Nausea and vomiting A nurse is reviewing urinalysis results and notices glucose is present in the urine. A nurse realizes glucose will be excreted in the urine when: a. The maximum rate of glucose filtration is achieved b. The maximum rate of glucose tubular reabsorption have reached their maximum c. Glucose is consumed d. The ability of the kidneys to regulate blood glucose is lost When a patient asks what role the kidneys play in vitamin D function, how should the nurse reply? a. Synthesizes vitamin D from cholesterol b. Activates intestinally absorbed vitamin D c. Metabolizes and breaks down vitamin D d. Excretes excess vitamin D A client with a decreased glomerular filtration rate asks how to prevent further damage to the kidneys. Which is the nurse’s best response? a. “The diuretics you are taking will prevent further damage.” b. “Kidney deterioration is inevitable as you age.” c. “Avoid taking NSAIDs.” d. “You will need to follow a low-sodium and high-protein diet.” A client is in the emergency department after experiencing kidney trauma. The abdomen is tender and distended, and blood is visible at the urinary meatus. Which action by the nurse is most important? a. Assess vital signs and abdominal pain every 5 to 15 minutes. b. Consult with the provider before inserting a indwelling catheter. c. Monitor the client’s IV rate of fluids and prepare to give blood. d. Assist with obtaining informed consent for surgery if needed. A confused client is hospitalized for possible pneumonia and is admitted from the emergency department with an indwelling catheter in place. During interdisciplinary rounds the following day, what question by the nurse takes priority? a. “Do you want daily weights on this client?” b. “Do you want postural drainage on this client?” c. “Can we discontinue the in-dwelling catheter?” d. “Can we discontinue droplets isolation?” A 55-year-old female reports an urinary problem to his primary care provider who suspects stress incontinence. Which complain expects the nurse hear from the client? a. Feeling a sudden intense urge to urinate when sneezing b. Unanticipated loss of urine when lifting boxes at her job c. Continuous dribbling of urine after voiding d. Loss of urine before the occupied bathroom is available A client has overflow incontinence. Which initial intervention does the nurse add to this client’s care plan to assist with elimination? a. Stroking the medial aspect of the thigh b. Using intermittent catheterization c. Providing digital anal stimulation d. Using the Valsalva maneuver The nurse is teaching a client about self-catheterization in the home setting. Which instructions are applicable? (Select all that apply.) a. “Wash your hands before and after self-catheterization.” b. “Use a large-lumen catheter for each catheterization.” c. “Use lubricant on the tip of the catheter before insertion.” d. “Self-catheterize every 8 hours.” e. “Use sterile gloves for the procedure.” f. “Maintain a specific schedule for catheterization.” Which laboratory finding, in conjunction with the presenting symptoms, should the nurse expect to find when assessing a child with nephrotic syndrome? A. Decreased urinary albumin B. Low specific gravity C. Decreased hemoglobin D. Decreased serum protein concentration What symptoms is more probable to report the mother of a child with nephrotic syndrome? A. My child had a sore throat 2 weeks ago B. My child’s urine looks like reddish brown C. My child only can use slippers since became sick D. My child face is not swollen in the morning, but swell after noon. D) After recovering from a urosepsis the client has a serum creatinine level of 2 mg/dL and a urine output of 1000 mL/day. How does the nurse categorize the client’s kidney injury? a. Intrarenal b. Nonoliguric c. Prerenal d. Postrenal The nurse is assisting a client on a low-potassium diet to select food items from the menu. Which of the following food items, if selected by the client, would indicate an understanding of this dietary restriction? 1. Cantaloupe 2. Spinach 3. Lima beans 4. Blueberries A 37 year old client with chronic kidney disease (CKD) is being treated with vitamin D, calcium supplements, and phosphate binders. Which nursing diagnosis is most likely to be included in this client’s plan of care? a. High risk for infection related to dialysis catheter b. Hygiene self-care deficit related to uremic frost c. Knowledge deficit related to high-protein diet d. High risk for injury related to renal osteodystrophy A patient with acute renal failure (ARF) will receive hemodialysis. What response demonstrates patient’s understanding? a. “Using the artificial kidney machine soon will help my kidneys to recover and function again” b. “I will be admitted in the long term hemodialysis program” c. “Now that I am in hemodialysis I will need to restrict my protein intake even more” d. “I need to avoid BP measure on the arm where the permanent A-V fistula will be created” The nurse is caring for a patient with a history of systemic lupus erythematosus who has been recently diagnosed with end-stage kidney disease (ESKD). The patient has an elevated phosphorus level and has been prescribed calcium acetate to bind the phosphorus. The nurse should teach the patient to take the prescribed phosphorus-binding medication at what time? a. Only when needed b. Daily at bedtime c. First thing in the morning d. With each meal The healthcare provider prescribes aluminum and magnesium hydroxide (Maalox), 1 tablet PO PRN, for a client with chronic renal failure who is complaining of indigestion. What intervention should the nurse implement? A. Administer 30 minutes before eating. B. Evaluate the effectiveness 1 hour after administration. C. Instruct the client to swallow the tablet whole. D. Question the healthcare provider's prescription. A client with a 16-year history of diabetes mellitus is having renal function tests because of recent fatigue, weakness, elevated blood urea nitrogen, and serum creatinine levels. Which finding should the nurse conclude as an early symptom of renal insufficiency? A. Dyspnea. B. Nocturia. C. Confusion. D. Stomatitis. A client who is admitted to the hospital with a history of kidney disease begins to have difficulty breathing, edema, and very distended neck veins. Vital signs are as follows: blood pressure, 90/70 mm Hg; increased heart rate, difficult to feel peripheral pulses, clear lung sounds. His heart sounds are difficult to hear. Which intervention does the nurse anticipate will be needed? a. Administration of prescribed IV furosemide b. Preparation of pericardiocentesis equipment c. Preparation for emergency hemodialysis d. Administration of insulin with dextrose IV A client with chronic renal failure has completed a hemodialysis treatment. The nurse would use which of the following standard indicators to evaluate the client’s status after dialysis? 1. Potassium level and weight 2. BUN and creatinine levels 3. VS and BUN 4. VS and weight. The nurse is performing an assessment on a client who has returned from the dialysis unit following hemodialysis. The client is complaining of a headache and nausea and is extremely restless. Which of the following is the initial nursing action? 1. Notify the physician 2. Monitor the client 3. Elevate the head of the bed 4. Medicate the client for nausea When providing care for a client receiving peritoneal dialysis, the nurse notices that the effluent is cloudy. Which intervention is most important for the nurse to carry out? a. Irrigate the peritoneal catheter with sterile saline. b. Send a specimen for culture and sensitivity. c. Prepare the client for emergency surgery. d. Clamp the catheter and call the provider. The nurse is providing dietary teaching to a client who was just started on peritoneal dialysis (PD). Which instruction does the nurse provide to this client regarding protein intake? a. “Your protein needs will not change, but you may take more fluids.” b. “You will need more protein now because some protein is lost by dialysis.” c. “Your protein intake will be adjusted according to your predialysis weight.” d. “You no longer need to be on protein restriction.” 2) The nurse is caring for a client receiving Tamoxifen for the treatment of breast cancer. Which action should the nurse include in the client's plan of care? A. Increase fluid intake. B. Decrease sodium chloride intake. C. Assist the client in coping with hot flashes. D. Encourage milk products to increase calcium intake The nurse is caring for a client receiving tamoxifen for the treatment of breast cancer. Which assessment finding requires the nurse immediate follow up? A. Client refers pain during sex B. Client uses Black Cohosh. C. Client states having night hot flashes. D. Client complains of calf tenderness The nurse is conducting a history on a male client to determine the severity of symptoms associated with prostate enlargement. Which finding is cause for prompt action by the nurse? a. Cloudy urine b. Urinary hesitancy c. Post-void dribbling d. Weak urinary stream A client has returned from a transurethral resection of the prostate with a continuous bladder irrigation. Which action by the nurse is a priority if bright red urinary drainage and clots are noted 5 hours after the surgery? a. Review the hemoglobin and hematocrit as ordered. b. Take vital signs and notify the surgeon immediately. c. Release the traction on the three-way catheter. d. Remind the client not to pull on the catheter. A hospitalized patient is placed on Finasteride for prostate cancer. The nurse explains the possible side effects of the medication, which are: a. gynecomastia. b. pruritus. c. constipation. d. tinnitus. An elderly male client reports to the clinic nurse that he is experiencing increasing nocturia with difficulty initiating his urine stream. He reports a weak urine flow and frequent dribbling after voiding. Which nursing action should be implemented? A. Obtain a urine specimen for culture and sensitivity. B. Encourage the client to schedule a digital rectal exam. C. Advise the client to maintain a voiding diary for one week. D. Instruct the client in effective techniques to cleanse the glans penis The nurse is providing care for a patient with continuous bladder irrigation (CBI) following removal of the prostate. The nurse understands that the CBI should be adjusted as needed to result in catheter outflow of which of the following types? A. cloudy yellow B. light pink C. amber with clots D. cherry colored with clots The nurse is caring for a patient following prostate surgery. Upon assessment, the nurse notes that the patient has a urinary catheter that is secured very snugly to the inner thigh. The nurse understands that the catheter: A. is positioned to help prevent hemorrhage. B. may be repositioned if the patient is uncomfortable. C. should be repositioned at least every few hours. D. will normally drain urine with large clots. The nurse is caring for a client after a transurethral resection of the prostate and determines the client's urinary catheter is not draining. What should the nurse implement? A. Change the catheter drainage tubing. B. Increase oral fluids. C. Irrigate the catheter. D. Milk the catheter. A client is diagnosed with metastatic prostate cancer. The client asks the nurse the purpose of his treatment with the luteinizing hormone–releasing hormone (LH-RH) agonist leuprolide (Lupron) and the bisphosphonate alendronate. Which statement by the nurse is most appropriate? a. “The treatment reduces testosterone and prevents bone fractures.” b. “The medications prevent erectile dysfunction and increase libido.” c. “There is less gynecomastia and osteoporosis with this drug regimen.” d. “These medications both inhibit tumor progression by blocking androgens.” The patient who had a prostatectomy 1 year ago now has elevations in serum acid phosphatase, alkaline phosphatase, and calcium levels. The nurse is aware that these are indicators of: a. reduction of cancer risk. b. orchiditis. c. testicular cancer. d. metastasis. A male nurse is speaking on testicular cancer at a high school boys’ gym class. When asked by one of the students why he was talking to their class, because teenagers don’t get cancer, the nurse replies: a. “I’m only speaking to those of you who have a family history of cancer.” b. “There is a link between testicular cancer and sexually transmitted infections.” c. “White men, 18 to 34 years old, are at highest risk for testicular cancer.” d. “This is a condition seen primarily in African-American men with sickle cell anemia. A 34-year-old client comes to the clinic with concerns about an enlarged lump in left testicle and heaviness in his lower abdomen. Which diagnostic test would the nurse expect to be ordered to confirm testicular cancer? a. Alpha-fetoprotein (AFP) b. Prostate-specific antigen (PSA) c. Prostate acid phosphatase (PAP) d. C-reactive protein (CRP) A 25-year-old client has recently been diagnosed with testicular cancer and is scheduled for radiation therapy. Which intervention by the nurse is best? a. Ask the client about his support system of friends and relatives. b. Encourage the client to verbalize his fears about sexual performance. c. Explore with the client the possibility of sperm collection d. Provide privacy to allow time for reflection about the treatment. The nurse takes into account in planning care that acute and chronic bacterial prostatitis are treated with: a. temporary catheter. b. antiseptic swabs. c. sitz baths. d. scrotal support. When conducting an initial assessment on a 65-year-old male patient, the nurse assesses a mass in the left testicle that on transillumination glows red. The nurse notes the presence of: a. phimosis. b. a hydrocele. c. A varicocele. d. a hematocele. A young male is brought to the emergency department by his father. As the patient is being assessed, he cries out and says that he is having intense pain in his genitalia and begins to vomit. Left testicle is swollen and tender. Based on these initial findings, the nurse suspects: a. cryptorchidism. b. testicular torsion. c. varicocele. d. epididymitis. A nurse is assessing a client who presents with a scaly rash over the palms and soles of the feet and the feeling of muscle aches and malaise. The nurse suspects syphilis. Which action by the nurse is appropriate? a. Reassure the client that this stage is not infectious unless she is pregnant. b. Assess the client for hearing loss and generalized weakness. c. Don gloves and further assess the client’s lesions. d. Take a history regarding any cardiovascular symptoms. A male client is diagnosed with primary syphilis. Which question by the nurse is a priority at this time? a. “Have you been using latex condoms?” b. “Are you allergic to any drug?” c. “When was your last sexual encounter?” d. “Do you have a history of sexually transmitted disease?” A 26-year-old client with multiple sexual partners is being assessed for symptoms of dysuria and vaginal discharge. Because the results from the culture of the cervical cells are not available, the client will be treated for both Chlamydia and gonorrhea. Which explanation by the nurse is best? a. “This early treatment will prevent obstruction to the fallopian tubes.” b. “Only azithromycin is prescribed for both diseases.” c. “The treatment will prevent aortic valve disease and aneurysms.” d. “Oral antibiotic treatment for both diseases will prevent meningitis.” Before marriage, a female client has a blood test drawn for syphilis. The test reveals a positive Venereal Disease Research Laboratory (VDRL) serum test. What is the advice that the nurse should give the client? a. “Check with your future husband about his sexual activity.” b. “You must determine if you are pregnant at this time.” c. “Submit to a more specific treponemal test to confirm the infection.” d. “Agree to a benzathine penicillin G injection in multiple doses.” A 23-year-old female has been diagnosed with genital warts. Which action by the nurse is best? a. Encourage the client to have an annual Papanicolaou (Pap) test. b. Recommend self application of podophyllin. c. Report the case to the Centers for Disease Control and Prevention (CDC). d. Discuss popular options for contraception. A patient with syphilis is seen at the clinic and complains of body aches, pustules, fever, and sore throat. The nurse recognizes that these are symptoms of syphilis at which stage? a. Primary b. Secondary c. Latent d. Tertiary (takes years, dementia, paralysis, lesions in joints) When the female patient who is newly diagnosed with gonorrhea screams, “I am going to kill my husband. I mean it.” The nurse’s best response would be: a. “Are you sure it is your husband who gave you gonorrhea?” b. “Yikes! Killing your spouse seems extreme.” You better castrate him! c. “Shall I report your spouse as a sexual contact?” d. “I can understand your anger. How best can you deal with it?” [Show More]
Last updated: 5 months ago
Preview 1 out of 35 pages
Reviews( 0 )
Recommended For You
*NURSING> NCLEX-RN > NCLEX-RN & CGFNS Practice Question » Gastrointestinal Disorders. 200 Most Commonly tested Questions in Power points from Week 1 to 13- NC III (All)
NCLEX-RN & CGFNS Practice Question » Gastrointestinal Disorders. 200 Most Commonly tested Questions in Power points from Week 1 to 13- NC III
NCLEX-RN & CGFNS Practice Question » Gastrointestinal Disorders Questions in Power points from Week 1 to 13- NC III Adequate nutrition is required for healing after treatment for recurrent aphth ous u...
By A-PLUS GUIDENOTES , Uploaded: Aug 26, 2021
$10
*NURSING> NCLEX-RN > CGFNS Practice Question » Gastrointestinal Disorders. 200 Most Commonly tested Questions in Power points from Week 1 to 13- NC III (All)
CGFNS Practice Question » Gastrointestinal Disorders. 200 Most Commonly tested Questions in Power points from Week 1 to 13- NC III
NCLEX-RN & CGFNS Practice Question » Gastrointestinal Disorders Questions in Power points from Week 1 to 13- NC III Adequate nutrition is required for healing after treatment for recurrent aphth ous u...
By STUDY-GUIDENOTES , Uploaded: Aug 26, 2021
$10
*NURSING> NCLEX-RN > Actual tests NCLEX-RN Compilation. (All)
Actual tests NCLEX-RN Compilation.
NCLEX-RN QUESTION 1 A 25-year-old client believes she may be pregnant with her first child. She schedules an obstetric examination with the nurse practitioner to determine the status of her possibl...
By Cheryshev , Uploaded: Sep 12, 2021
$30
*NURSING> NCLEX-RN > TEST BANK NCLEX QUESTIONS AND ANSWERS ALL UPDATED (All)
TEST BANK NCLEX QUESTIONS AND ANSWERS ALL UPDATED
ST BANK NCLEX QUESTIONS AND ANSWERS ALL UPDATED WELL 2021 QUESTIONS 1-15 Ref # 4366 The nurse receives a client from the post anesthesia care unit following a left femoral-popliteal bypass gr aft proc...
By Expert , Uploaded: Mar 14, 2021
$12
*NURSING> NCLEX-RN > NCLEX RN Cardiovascular 150 Q&A. The most commonly tested exam questions. (All)
NCLEX RN Cardiovascular 150 Q&A. The most commonly tested exam questions.
NCLEX RN Cardiovascular 150 Q&As 1. A client admitted to the hospital with chest pain and a history of type 2 diabetes mellitus is scheduled for cardiac catheterization. Which medication would ne...
By QuizMaster , Uploaded: Aug 20, 2020
$10
*NURSING> NCLEX-RN > TEST BANK NCLEX QUESTIONS AND ANSWERS (All)
TEST BANK NCLEX QUESTIONS AND ANSWERS
TEST BANK NCLEX QUESTIONS AND ANSWERS ALL UPDATED WELL 2021 QUESTIONS 1-15 Ref # 4366 The nurse receives a client from the post anesthesia care unit following a left femoral-popliteal bypass gr...
By klaus , Uploaded: Jan 25, 2021
$12
*NURSING> NCLEX-RN > ATI NCLEX RN Comprehensive Predictor 2019 Form A. ATI NCLEX Predictor. Contains 180 Q&A for nursing school personnel and students to Guarantee success on the NCLEX. (All)
ATI NCLEX RN Comprehensive Predictor 2019 Form A. ATI NCLEX Predictor. Contains 180 Q&A for nursing school personnel and students to Guarantee success on the NCLEX.
RN Comprehensive Predictor 2019 Form A 1. A nurse in a pediatric unit is preparing to insert an IV catheter for 7-year-old. Which of the following actions should the nurse take? A. (Unable to re...
By QuizMaster , Uploaded: Aug 16, 2020
$9
*NURSING> NCLEX-RN > SAUNDERS NCLEXRN EXAMINATION REVISON CONTENT. QUESTIONS AND ANSWERS (All)
SAUNDERS NCLEXRN EXAMINATION REVISON CONTENT. QUESTIONS AND ANSWERS
SAUNDERS QUESTIONS AND ANSWERS-NCLEX-RN EXAMINATION 1) The nurse is providing discharge instructions to a Chinese American client regarding prescribed dietary modifications. During th...
By QuizMaster , Uploaded: Aug 05, 2020
$9
*NURSING> NCLEX-RN > NCLEX-RN Cram Sheet: This NCLEX-RN cram sheet or cheat sheet can help you prepare as it contains condensed facts about the nurse licensure exam itself and key nursing information: (All)
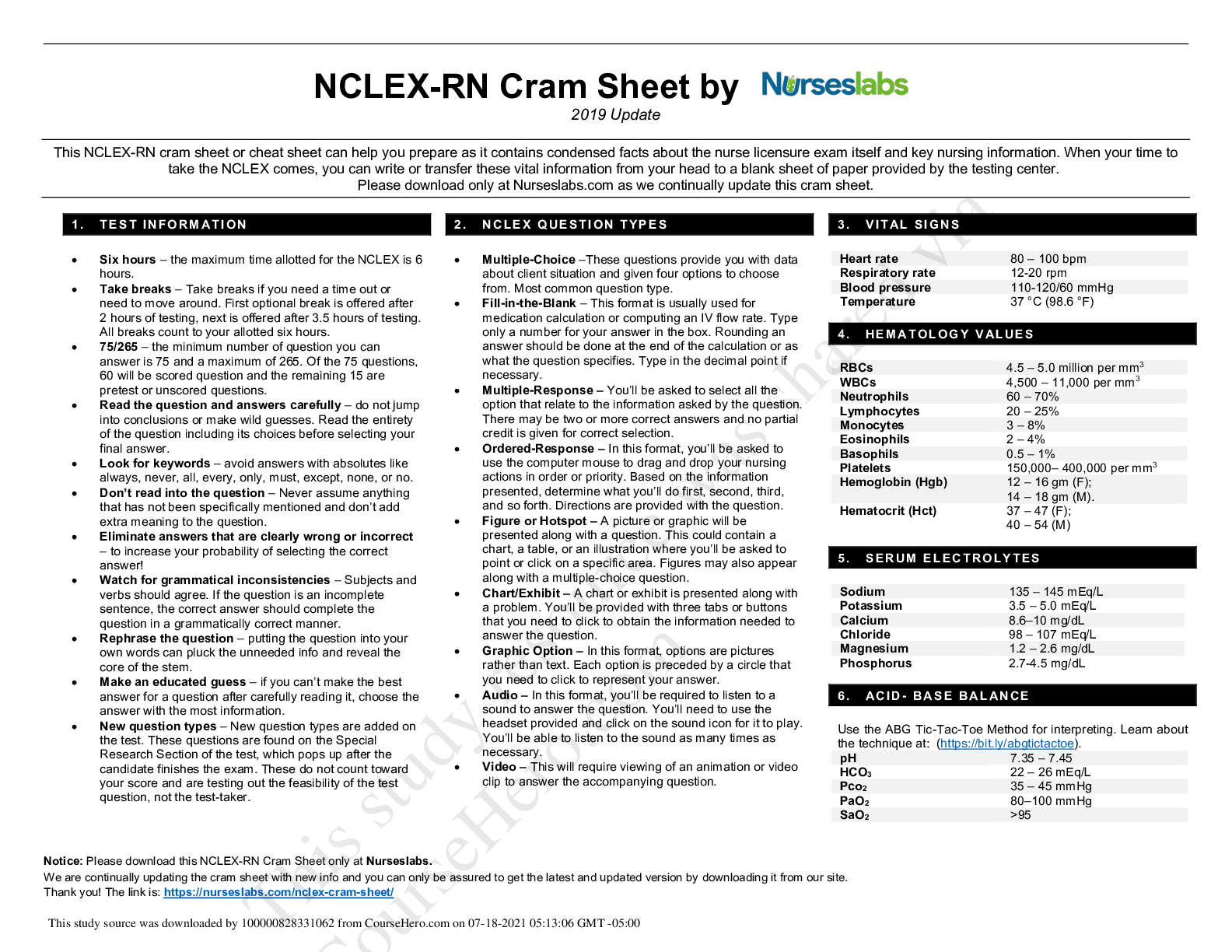
NCLEX-RN Cram Sheet: This NCLEX-RN cram sheet or cheat sheet can help you prepare as it contains condensed facts about the nurse licensure exam itself and key nursing information:
RBCs 4.5 – 5.0 million per mm3 NCLEX-RN Cram Sheet by 2020 Update This NCLEX-RN cram sheet or cheat sheet can help you prepare as it contains condensed facts about the nurse licensure exam itself and...
By Tutor Frankline , Uploaded: Jul 18, 2021
$9.5
*NURSING> NCLEX-RN > NCLEX RN ACTUAL EXAM TEST BANK OF REAL QUESTIONS & ANSWERS NCLEX 2023/2024 (All)
NCLEX RN ACTUAL EXAM TEST BANK OF REAL QUESTIONS & ANSWERS NCLEX 2023/2024
NCLEX RN ACTUAL EXAM TEST BANK OF REAL QUESTIONS & ANSWERS NCLEX 2023/2024
By GradesProff , Uploaded: Jul 19, 2023
$16
Document information
Connected school, study & course
About the document
Uploaded On
Nov 28, 2020
Number of pages
35
Written in
Additional information
This document has been written for:
Uploaded
Nov 28, 2020
Downloads
0
Views
128






