Health Care > QUESTIONS & ANSWERS > HE 380 exam 5 complete solutions with correct answers 2021 (All)
HE 380 exam 5 complete solutions with correct answers 2021
Document Content and Description Below
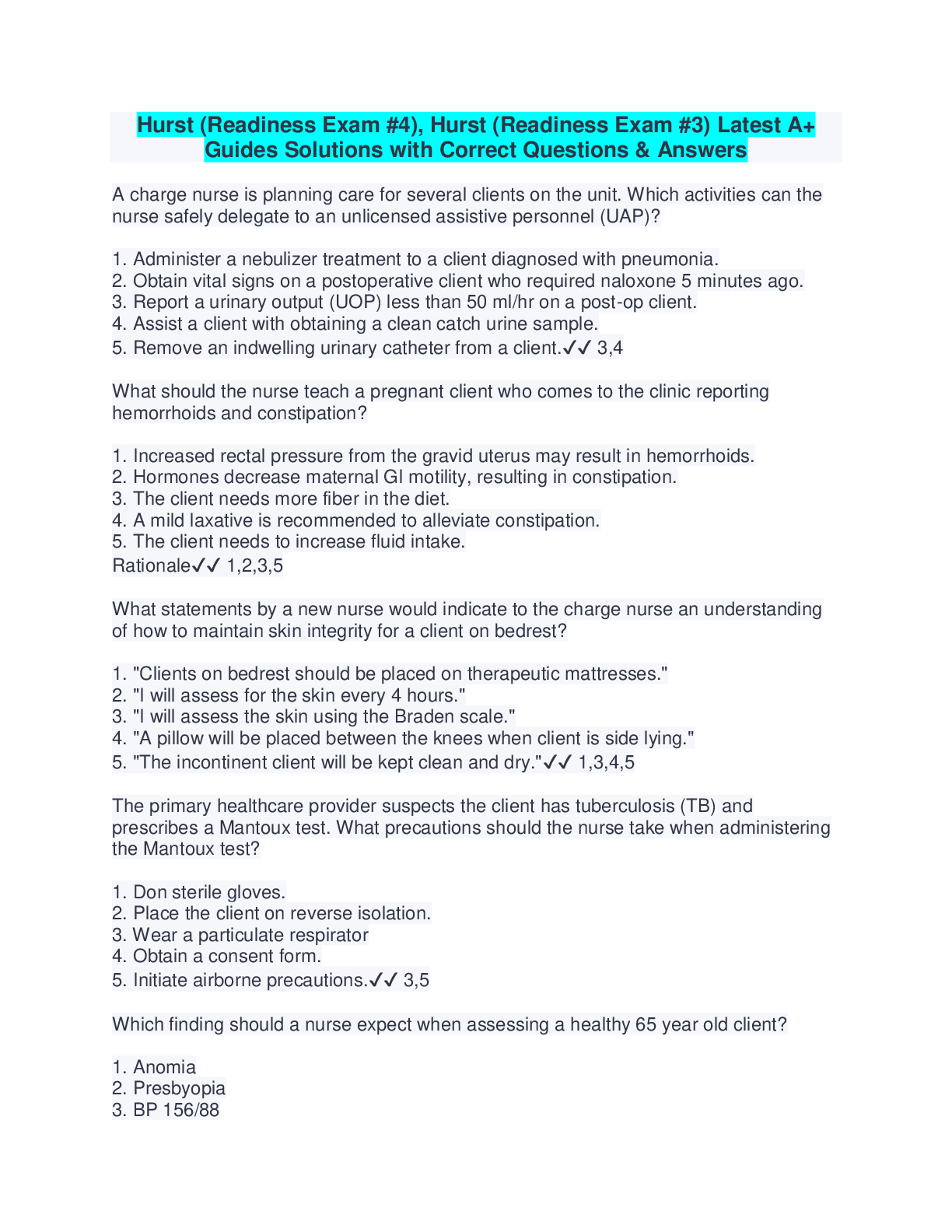
HE 380 exam 5 complete solutions with correct answers 2021 Part 1 of 2 - 95.0/ 100.0 Points Question 1 of 40 5.0/ 5.0 Points Physician pay for performance programs usually look at the performanc... e of groups of physicians because: • A. there are usually only a small number of measures that any individual physician may be able to report. • B. it is cheaper to look at groups. • C. it is more patient driven. • D. it is more cost effective. Question 2 of 40 5.0/ 5.0 Points One major provision of the ACA with Medicare reform was the creation of __________, now called the Innovation Center. • A. DHHS • B. CMI • C. WHO • D. CMS Question 3 of 40 5.0/ 5.0 Points The following are examples of non-risked based physician payment EXCEPT: • A. fee for service. • B. UCR fee allowances. • C. fee schedule. • D. HMO. Question 4 of 40 5.0/ 5.0 Points __________ benefits are usually administered, not through a payer’s usual claims system, but rather through a PBM. • A. Prescription drug • B. Vision • C. Dental • D. Physical therapy Question 5 of 40 5.0/ 5.0 Points Which of the following is NOT required to submit documentation that demonstrates compliance with the adopted standards and operating rules? • A. Eligibility for a health plan • B. Paper remittance advice (PRA) transactions • C. Healthcare claim status • D. Healthcare electronic funds transfer (EFT) Question 6 of 40 5.0/ 5.0 Points A __________ based provider payment is where the provider shares some portion of financial risk for overall costs, such that higher than budgeted costs can result in payment reductions while lower than budgeted costs can result in higher payment. • A. non-risk • B. HMO • C. risk • D. PPO Question 7 of 40 5.0/ 5.0 Points When we think of provider payment as reimbursement: • A. it reduces our awareness of how payment affects personal and organizational behavior. • B. the services rendered are diminished. • C. procedure costs increase. • D. it increases awareness and services rendered are diminished. Question 8 of 40 5.0/ 5.0 Points __________ refers to financial incentives aligned with the practice of evidence-based clinical care and is based on incentives rather than being risk-based. • A. Capitation • B. Fee for service • C. Pay for performance • D. Fee schedule Question 9 of 40 5.0/ 5.0 Points When a hospital, that runs the clinics or offices used by their employed physicians, bills the payer a separate fee, it is called a/an __________ facility fee. • A. add-on • B. auxiliary • C. maintenance • D. electronic Question 10 of 40 5.0/ 5.0 Points A single payment that includes all professional services delivered in a defined episode of care is/are: • A. case rates. • B. price transparency. • C. capitation. • D. electronic visits. Question 11 of 40 5.0/ 5.0 Points For pharmaceutical payment the usual method of paying combines what two concepts? • A. Quality and quantity • B. Coding and pharmacology • C. Fill fee and ingredient cost • D. Cost of bottles and the color of pills Question 12 of 40 5.0/ 5.0 Points __________ means HMO payment of a single entity for all medical services. • A. Global capitation • B. Pay for performance • C. DRG • D. TRICARE Question 13 of 40 0.0/ 5.0 Points Which type of provider payment is a common method of provider payment? • A. Non-risk based • B. HMO based • C. Risk based • D. PPO based Question 14 of 40 5.0/ 5.0 Points Transactions other than pharmacy claims are subject to __________ standards developed by the American National Standards Institute (ANSI). • A. 823 • B. X12 • C. D35 • D. Ph3 Question 15 of 40 5.0/ 5.0 Points All of the following are examples of risk-based physician payment used by HMOs EXCEPT: • A. capitation. • B. case rates. • C. variation factors. • D. at risk FFS. Question 16 of 40 5.0/ 5.0 Points HIPAA mandated that all covered entities use the same type of: • A. electronic transaction standards. • B. reimbursement standards. • C. eligibility benefits standards. • D. none of the above. Question 17 of 40 5.0/ 5.0 Points Which concept refers to an individual’s wages or salary, or any type of work-related bonus? • A. Reimbursement • B. Payment • C. Services • D. Fee schedule Question 18 of 40 5.0/ 5.0 Points What concept refers to being made whole for actual out-of-pocket expenses on a dollar-for-dollar basis? • A. Reimbursement • B. Payment • C. Services • D. Salary Question 19 of 40 5.0/ 5.0 Points Which of the following is NOT considered a factor that affects payment methods of physicians? • A. The type of health plan or payer • B. Physician location • C. Number of payers the provider contracts with • D. Negotiating strength of either party Question 20 of 40 5.0/ 5.0 Points When reviewing CMS’s RBRVS, all of the following are the different RVUs that are added together to make up the overall value EXCEPT the: • A. amount of work and the amount of resources invested by the physician in training • B. cost of the practice, including the cost of personnel, supplies • C. cost of malpractice insurance • D. cost of housing for physician Part 2 of 2 - 95.0/ 100.0 Points Question 21 of 40 5.0/ 5.0 Points Prevention is aimed at: • A. preventing certain diseases or conditions. • B. making money for providers. • C. trying out new procedures. • D. helping meet patients’ deductible. Question 22 of 40 5.0/ 5.0 Points Which is NOT a category of Quality Management (QM) activities? • A. Structure • B. Process • C. Outcome • D. Utilization Question 23 of 40 5.0/ 5.0 Points Examples of outcomes in a payer quality management program do NOT include which of the following? • A. Hospital readmission • B. Return to intensive care unit • C. Death • D. Deductible Question 24 of 40 5.0/ 5.0 Points The primary source involving medical necessity coverage decisions are typically made by the: • A. patient. • B. treating physician. • C. family of patient. • D. secretary in the office of the provider. Question 25 of 40 5.0/ 5.0 Points The most popular demand management method is: • A. transportation to providers. • B. a round-the-clock nurse advise line. • C. prescription delivery. • D. exercise programs. Question 26 of 40 5.0/ 5.0 Points Which is NOT a form of preventive care? • A. Pap smears • B. Wellness programs • C. Mammograms • D. Ultrasounds Question 27 of 40 5.0/ 5.0 Points Which is NOT an example of structure measures in a typical quality management (QM) program? • A. Cleanliness of a physician’s office • B. Credentialing criteria • C. Physical location of a physician’s office • D. Number of asleep patients waiting in lobby Question 28 of 40 5.0/ 5.0 Points Medical necessity typically describes types of services that are excluded from coverage because they are not considered to be medically necessary. Which is NOT an example of the type of services that may be excluded? • A. Services that are primarily for the convenience of the patient or physician • B. Custodial care or care that is essentially assisting with acts of daily living • C. Experimental or investigational care • D. Services outside of the country Question 29 of 40 5.0/ 5.0 Points Peer review committees are made up of: • A. plan physicians. • B. retired teachers. • C. patients. • D. hospital administrators. Question 30 of 40 5.0/ 5.0 Points Managed healthcare plans: • A. provide healthcare. • B. prevent healthcare from being provided. • C. make coverage decisions. • D. prevent members from seeking healthcare. Question 31 of 40 5.0/ 5.0 Points Concurrent utilization management refers to care used primarily for: • A. out-patient care. • B. urgent care. • C. hospital inpatient care. • D. emergency rooms. Question 32 of 40 5.0/ 5.0 Points Prospective review management addresses utilization: • A. after it occurs. • B. while it occurs. • C. before it occurs. • D. a year after it occurs. Question 33 of 40 5.0/ 5.0 Points Referral management is sometimes called: • A. medical necessity. • B. preauthorization. • C. capitation. • D. evaluation. Question 34 of 40 5.0/ 5.0 Points In quality management which is NOT true about Process? • A. It focuses on receiving payment. • B. It focuses on what is being done and how it is being done. • C. It must be defined beforehand. • D. It focuses on the way in which medical services are provided. Question 35 of 40 5.0/ 5.0 Points __________ refers to the routine functions used to manage the cost of most widely used medical services. • A. Medical necessity • B. Utilization management • C. Benefit Coverage • D. Clinical trials Question 36 of 40 5.0/ 5.0 Points Which term does NOT describe medical necessity? • A. Reasonable • B. Necessary • C. Appropriate • D. Expensive Question 37 of 40 0.0/ 5.0 Points __________ is a set of standardized measures that look at plan performance across a variety of important dimensions, such as delivery of preventive health services, member satisfaction, and treatment efficacy for various illnesses. • A. CVO • B. UM • C. CAHPS • D. HEDIS Question 38 of 40 5.0/ 5.0 Points Average length of stay (ALOS) is the average: • A. amount of time a patient spends in the waiting room. • B. length of time for inpatient hospital stays. • C. time in the ER. • D. amount of time visitors are allowed to stay. Question 39 of 40 5.0/ 5.0 Points Prospective utilization management does NOT include: • A. referral management. • B. demand management. • C. precertification. • D. clinical trials. Question 40 of 40 5.0/ 5.0 Points Which is NOT true of a health plan accreditation? • A. It is a “seal of approval.” • B. It is a form of oversight. • C. It determines if industry standards are met. • D. It is not relied on by employers and consumers. [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$18.00
Document information
Connected school, study & course
About the document
Uploaded On
Jan 17, 2021
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Jan 17, 2021
Downloads
0
Views
34