NURS 500 Midterm and final Exam practice questions latest update 2021
Document Content and Description Below
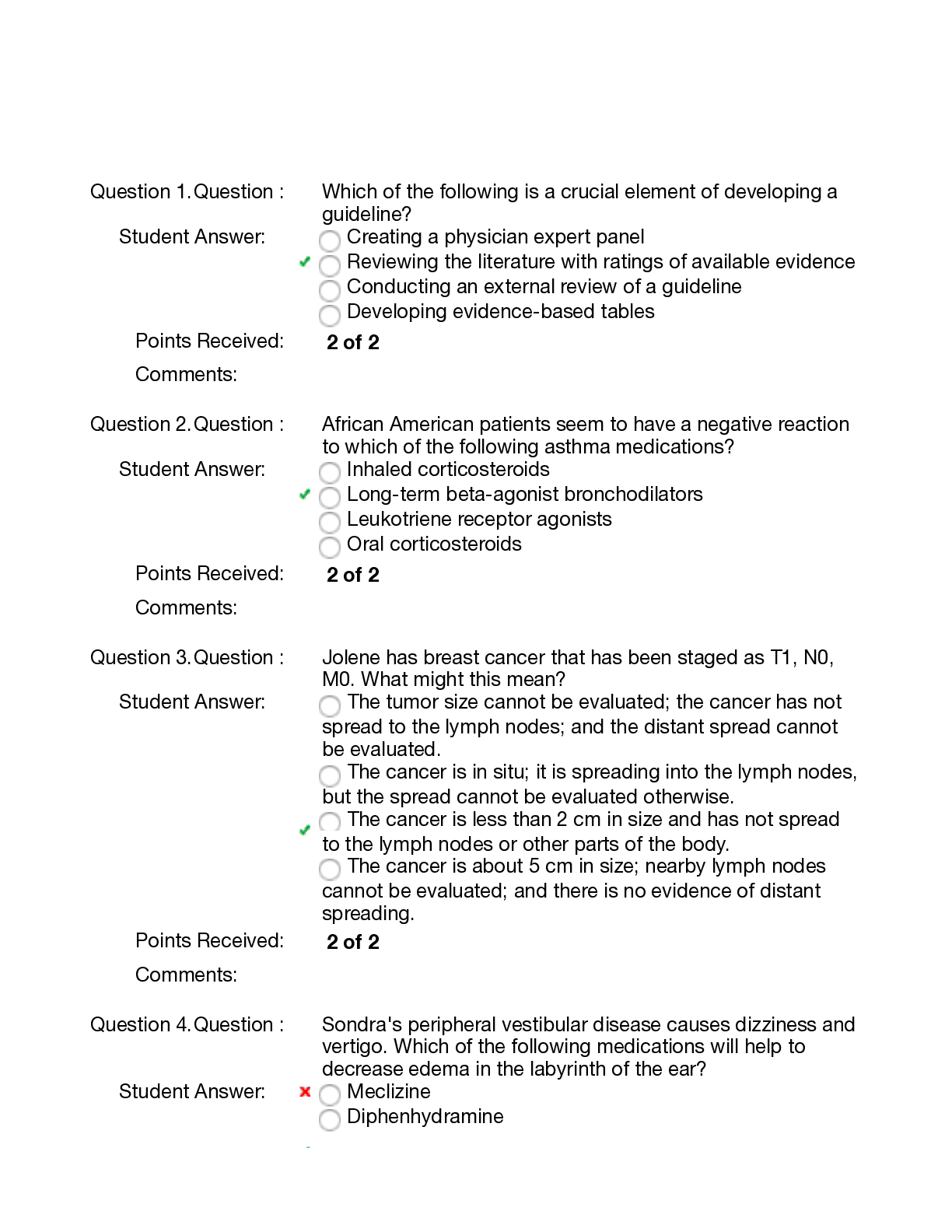
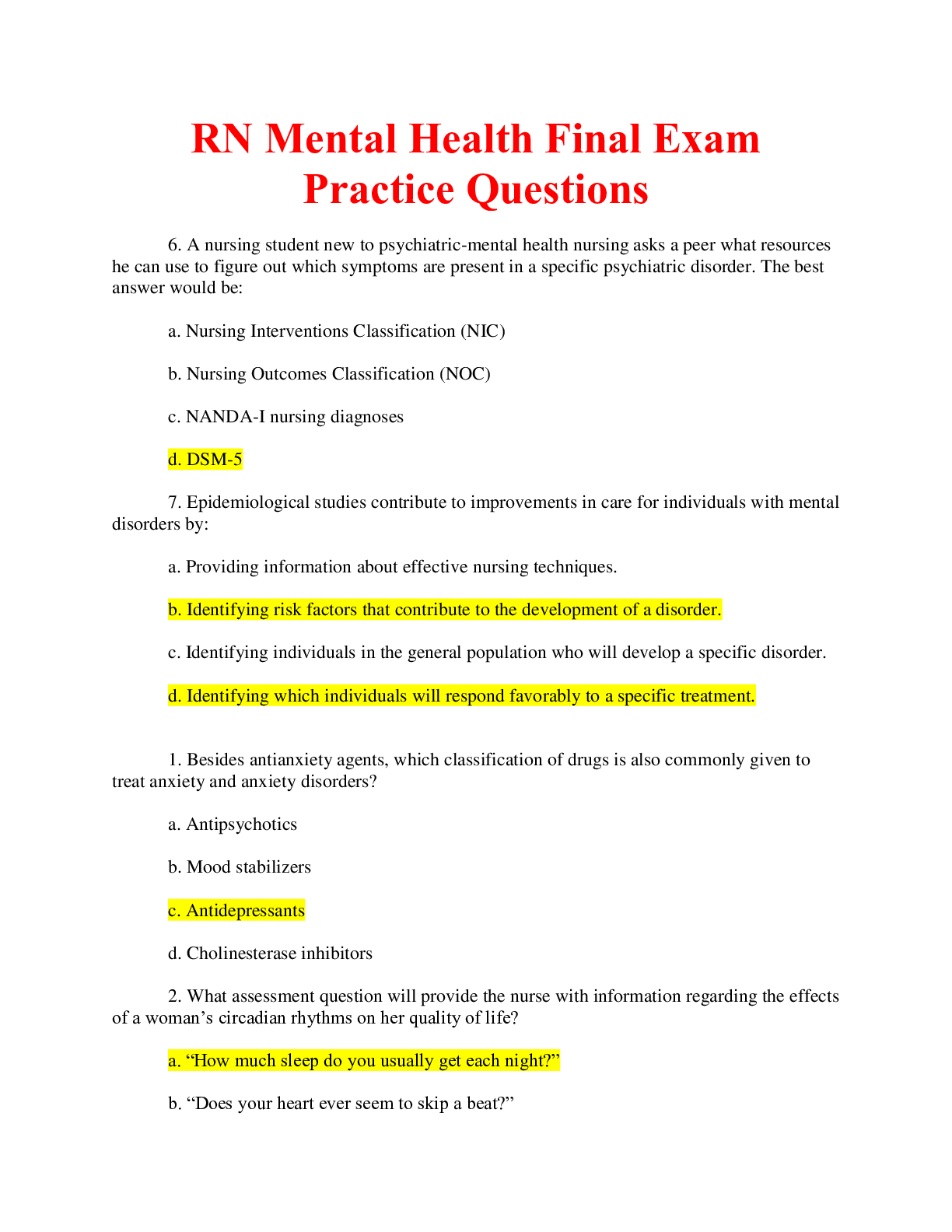
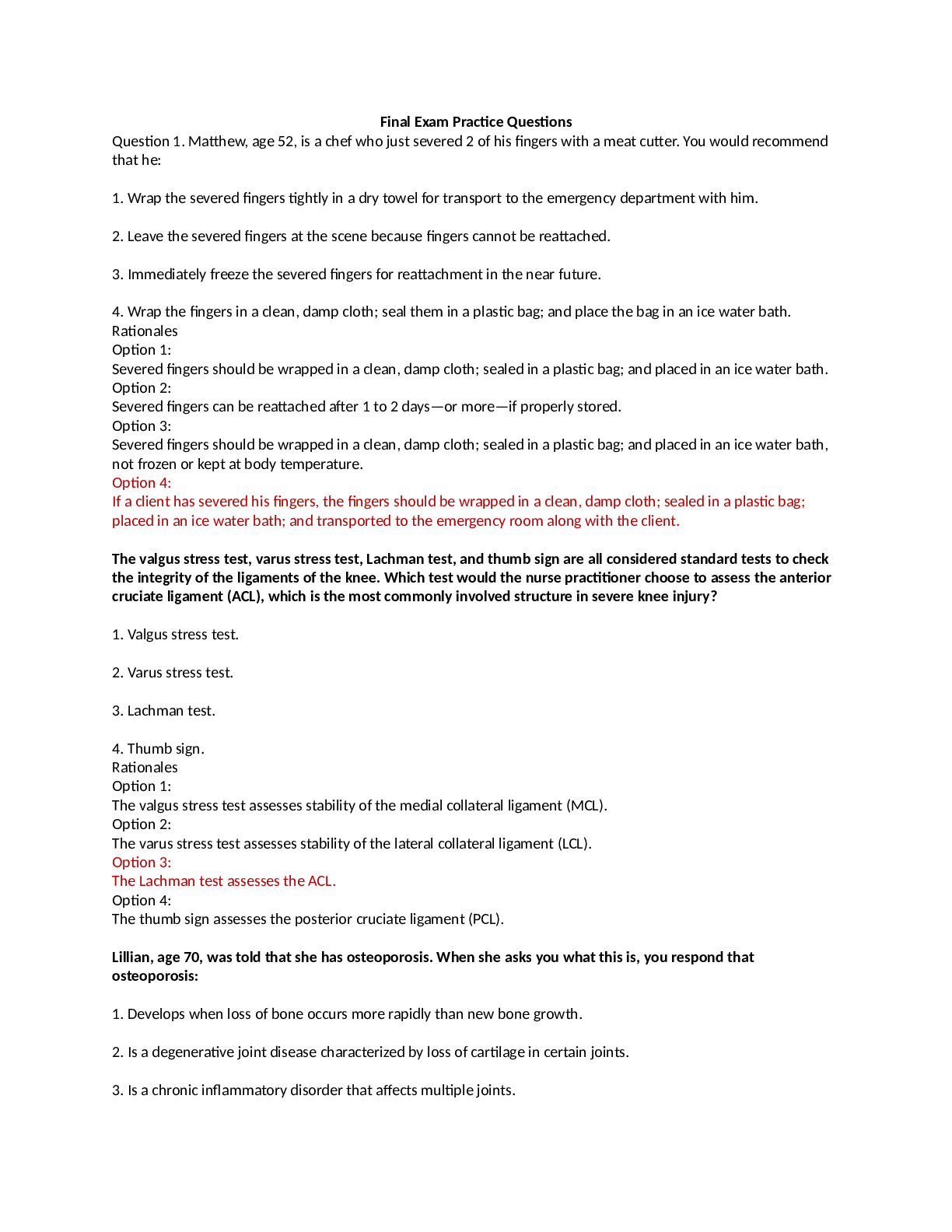
NURS 500 Midterm and final Exam practice questions 1. Why should an elevated PT/aPTT be reported to a physician prior to an invasive procedure? a. All abnormal lab results should be reported to th... e physician. b. The procedure will be cancelled. c. The risk for post-procedure thrombus will increase. d. There is increased risk for bleeding during and after the procedure. 2. The telemetry nurse is differentiating between right- and left-sided heart failure in an assigned patient. For right-sided heart failure, the patient presents with edematous extremities, nausea/vomiting, and: a. anorexia. b. change in level of consciousness. c. diuresis with exertion. d. flat abdomen. 3. A patient has been admitted to the telemetry unit with infective endocarditis. During the nursing assessment, the nurse notes the confirmatory findings of petechiae, splinter hemorrhages, and: a. elevated blood sugar. b. negative/normal blood cultures. c. Osler’s nodes. d. shortness of breath. 4. The most common lethal arrhythmia in the first hour of a myocardial infarction is: a. asystole. b. first-degree atrioventricular (AV) block. c. pulseless ventricular tachycardia. d. ventricular fibrillation. 5. A patient will be discharged following placement of an implantable cardioverter/defibrillator (ICD). The telemetry nurse is completing the patient’s discharge education. The patient demonstrates that he understands the provided instructions when he makes the following statement: a. “I can play football with my team next week.” b. “I will report to my doctor fever, redness, soreness, or drainage at the incision site.” c. “I will wear tight clothing over the ICD device to keep it in place.” d. “If I miss a dose of medication it is okay, because my ICD will take care of any issue.” 6. Which of the following is considered an unreliable sign of heart failure? a. Edema b. Electrolyte imbalance c. Microalbuminuria d. Proportional pulse pressure 7. Prior to administering digoxin (Lanoxin®) to a patient, the nurse assesses the: a. apical pulse for 1 minute. b. radial pulse for 1 minute. c. radial pulse for 2 minutes. d. respiratory rate for 1 minute. 8. Of the brain, heart, kidney, and liver, which can tolerate hypoxia and anoxia for up to 1 hour without permanent damage? a. Brain b. Heart c. Kidney d. Liver 9. Rather than impeding lung blood flow, pulmonary emboli composed of _____________ injure blood vessels and cause acute respiratory distress syndrome (ARDS). a. air b. fat c. foreign objects d. infected blood clots 10. The telemetry nurse is examining a rhythm strip and notices a repeated three-beat pattern, usually occurring as two sequential normal complexes followed by a premature complex and a pause, with the same pattern repeating itself in triplicates. What is the name of this pattern? a. Bigeminy b. Quadrigeminy c. Sinus rhythm d. Trigeminy 11. Your patient was admitted for complications of diabetes mellitus and you note that the lab work revealed hyperlipidemia. You understand that for the patient with diabetes, hyperlipidemia is: a. a genetic predisposition. b. a new finding. c. an expected finding. d. irrelevant. 12. Which lab assessment is the single most important laboratory test in a patient who appears to be intoxicated with ethanol? a. BUN b. Serum creatinine c. Serum ethanol level d. Serum glucose level 13. A patient reports unrelenting, crushing chest pain, nausea, and dyspnea. The nurse suspects an acute myocardial infarction. What change should the nurse expect to see on the patient's ECG? a. P-wave inversion b. ST-segment elevation c. T-wave depression d. T-wave inversion 14. The telemetry nurse is assigned a patient who has congestive heart failure and is receiving enteral nutrition therapy. For which of the following is this patient most at risk? a. Abdominal distention b. Electrolyte imbalance c. Fluid overload d. Nausea and vomiting 15. The telemetry nurse is assigned a patient that is experiencing chest pain resulting from coronary artery spasms while at rest. The nurse quickly realizes that the patient is suffering from: a. new onset angina. b. pre-infarction angina. c. unstable angina. d. variant (Prinzmetal’s) angina. 16. The actions of nitroglycerin in the management of angina include: a. coronary artery constriction and peripheral venous constriction. b. coronary artery constriction and peripheral venous dilation. c. coronary artery dilation and peripheral venous constriction. d. coronary artery dilation and peripheral venous dilation. 17. Which of the following conditions warrants temporary cardiac pacing for a patient? a. bradyarrhythmia secondary to profound hypothermia. b. first-degree AV block without symptoms. c. injury to the sinus node after cardiac surgery d. stable escape rhythm. 18. Which clinical manifestation does a patient with stable angina exhibit? a. Chest pain that is predictable in onset, intensity, and duration b. Chest pain that is unpredictable in onset, intensity, and duration c. Chest pain that is unrelieved by nitroglycerin (Nitrostat®) d. Chest pain that occurs predominantly at rest 19. The telemetry nurse is caring for a patient who has atrial fibrillation. The patient is attempting to understand how this dysrhythmia came to affect him. The nurse educates this patient about his risk factors, including: a. chronic renal disease. b. diabetes mellitus. c. genetic factors. d. hypotension. 20. The most common event reported during coronary artery balloon catheterization is: a. chest pain. b. diarrhea. c. headache. d. leg cramping. 21. Which of the following scales is the most widely used delirium screening instrument in hospitalized older adults? a. CAM b. CIWA c. DRS d. NEECHAM 22. A patient is admitted to the telemetry unit with chest pain. An hour after admission, the patient develops a narrow complex tachycardia with a regular rate of 160. The patient’s vital signs are: BP 100/65, P 160, R 20 and O2 saturation of 95% on room air. What course of action would be most appropriate for this patient? a. 12-lead EKG b. Adenosine (Adenocard®) IV c. Defibrillation d. Wait to determine how long the patient will tolerate the rhythm. 23. The telemetry nurse has a patient that has symptomatic bradycardia. The medication that would be most effective for treatment is: a. adenosine. b. atropine. c. digoxin. d. magnesium sulfate. 24. You are explaining to a new nurse the QT interval on the ECG strip of one of her patients. You confirm that she understands your instructions when she tells you that the QT interval: a. extends from the beginning of QRS complex to the end of the T wave and may result from slow repolarization. b. follows the ST segment and represents ventricular repolarization. c. is measured from the beginning of the P wave to the end of the PR segment. d. represents the total time required for ventricular depolarization and repolarization. 25. A patient is being discharged on cortisol replacement therapy. The nurse knows that education has been completed when the patient states: a. “I do not require a medical alert bracelet.” b. “I will take my medication on an empty stomach.” c. “I will weigh myself daily.” d. “If I miss a dose, I can skip it and double up the next time it is due.” 26. The most common cause of right heart failure is: a. adult respiratory distress syndrome. b. jugular venous distention. c. left heart failure. d. systemic hypertension. 27. The telemetry nurse assessed a 65-year-old female patient that was admitted for an MI and noticed that no ST segment elevation occurred on the ECG during the admission process. The nurse understands that: a. new onset angina will not present with any ST abnormality. b. non-ST elevation during an MI is common in women. c. the ECG results were incorrect and should be discarded; a stat ECG should be ordered. d. this was due to an incorrect lead placement; cardiac enzymes can confirm the MI. 28. You have a patient that is undergoing a sleep study to rule out sleep apnea. The most accurate test to diagnose sleep apnea is: a. blood pressure. b. head MRI. c. polysomnography. d. pulse oximetry. 29. A coronary artery bypass graft (CABG) patient has a chest tube in place. The nurse suspects an air leak, because the collection unit displays: a. bubbling in the suction chamber. b. bubbling in the water seal chamber. c. tidaling in the suction chamber. d. tidaling in the water seal chamber. 30. Following a CABG procedure, a patient can experience changes in level of consciousness. It is important to differentiate transient neurological deficits from signs of a permanent deficit associated with an intraoperative stroke. The primary sign that indicates an intraoperative stroke is: a. easy arousal from anesthesia. b. normal pupillary response. c. presence of intact sensory motor function. d. seizures. 31. A patient has been admitted to the telemetry unit with a diagnosis of pulmonary embolism. The telemetry nurse knows that the primary cardiac assessment findings relevant to pulmonary embolism are distended neck veins, syncope, cyanosis, and: a. elevated BUN and creatinine. b. hypertension. c. hypotension. d. paroxysmal breathing. 32. Which drug is given first to a patient with pulseless electrical activity (PEA)? a. Dopamine b. Epinephrine c. Lidocaine d. Norepinephrine 33. The nurse has a patient that is scheduled to have the next bottle of total parenteral nutrition (TPN) solution hung at 1500; however, there is none available. Until the TPN solution is available, the nurse should administer: a. 10% D/W solution. b. lactated Ringer’s solution. c. normal saline. d. sterile water. 34. EKG changes in leads II, III, and aVF are strongly suggestive of an acute myocardial infarction. What area of the myocardium is affected? a. Anterior b. Inferior c. Lateral d. Posterior 35. A patient is receiving a unit of blood and begins to display signs and symptoms of a transfusion reaction. What primary nursing action should the nurse take? a. Call a rapid response team. b. Change the IV site. c. Decrease the infusion rate. d. Stop the blood transfusion. - The telemetry nurse is differentiating between right- and left-sided heart failure in an assigned patient. For right-sided heart failure, the patient presents with edematous extremities, nausea/vomiting, and: - A patient has been admitted to the telemetry unit with infective endocarditis. During the nursing assessment, the nurse notes the confirmatory findings of petechiae, splinter hemorrhages, and: - Of the brain, heart, kidney, and liver, which can tolerate hypoxia and anoxia for up to 1 hour without permanent damage? - Rather than impeding lung blood flow, pulmonary emboli composed of _____________ injure blood vessels and cause acute respiratory distress syndrome (ARDS). - Which lab assessment is the single most important laboratory test in a patient who appears to be intoxicated with ethanol? - A patient is admitted to the telemetry unit with chest pain. An hour after admission, the patient develops a narrow complex tachycardia with a regular rate of 160. The patient’s vital signs are: BP 100/65, P 160, R 20 and O2 saturation of 95% on room air. What course of action would be most appropriate for this patient? - You are explaining to a new nurse the QT interval on the ECG strip of one of her patients. You confirm that she understands your instructions when she tells you that the QT interval: - The telemetry nurse assessed a 65-year-old female patient that was admitted for an MI and noticed that no ST segment elevation occurred on the ECG during the admission process. The nurse understands that: - Following a CABG procedure, a patient can experience changes in level of consciousness. It is important to differentiate transient neurological deficits from signs of a permanent deficit associated with an intraoperative stroke. The primary sign that indicates an intraoperative stroke is: - A patient has been admitted to the telemetry unit with a diagnosis of pulmonary embolism. The telemetry nurse knows that the primary cardiac assessment findings relevant to pulmonary embolism are distended neck veins, syncope, cyanosis, and: - The nurse has a patient that is scheduled to have the next bottle of total parenteral nutrition (TPN) solution hung at 1500; however, there is none available. Until the TPN solution is available, the nurse should administer: - EKG changes in leads II, III, and aVF are strongly suggestive of an acute myocardial infarction. What area of the myocardium is affected? [Show More]
Last updated: 1 year ago
Preview 1 out of 7 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 19, 2021
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
Jan 19, 2021
Downloads
0
Views
45


.png)

.png)