Medical Studies > TEST BANK > MCQ for PBS Medical. Document Contains over 5000 Commonly Tested Q&A in 792 Pages (All)
MCQ for PBS Medical. Document Contains over 5000 Commonly Tested Q&A in 792 Pages
Document Content and Description Below
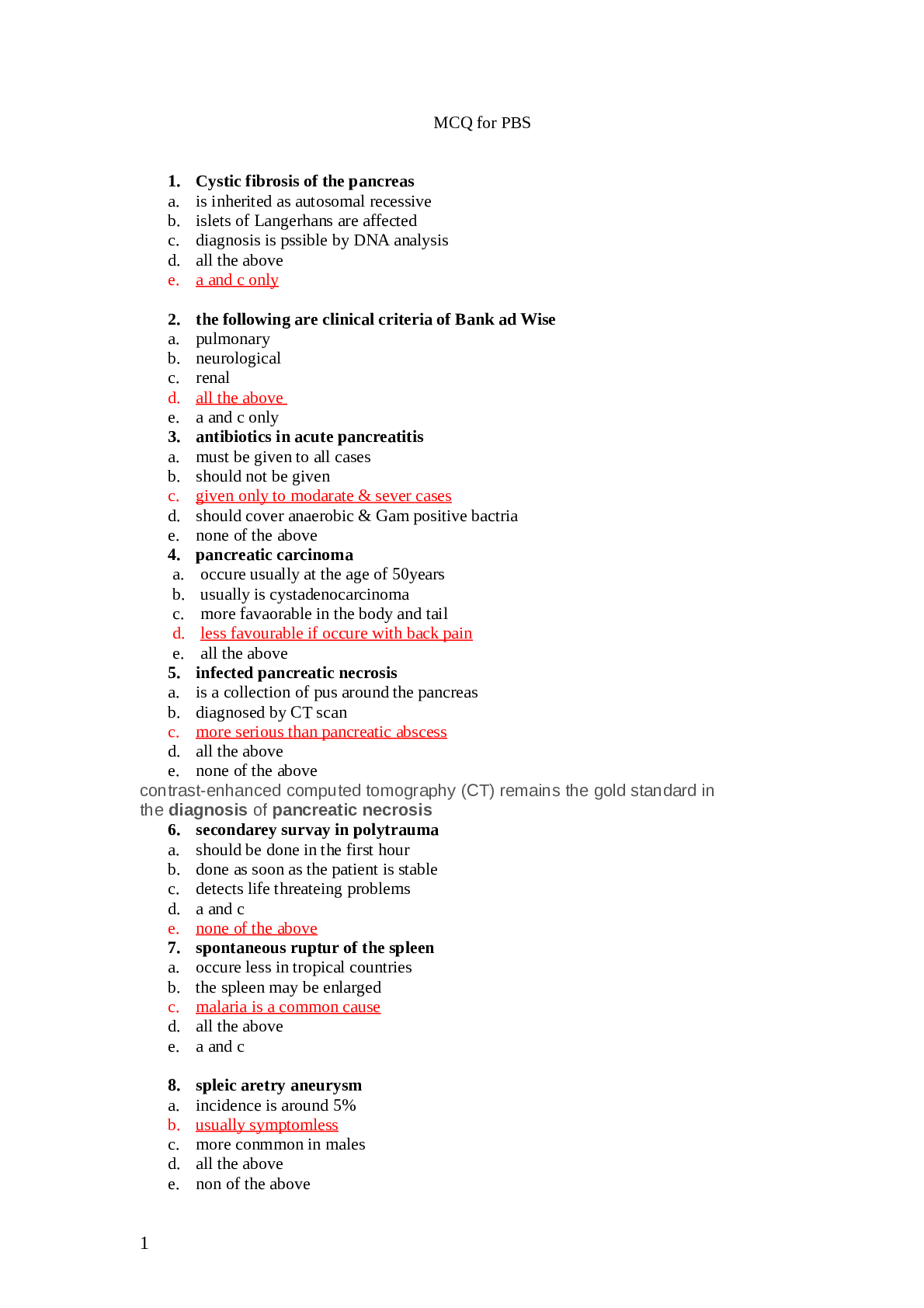
MCQ for PBS 1. Cystic fibrosis of the pancreas a. is inherited as autosomal recessive b. islets of Langerhans are affected c. diagnosis is pssible by DNA analysis d. all the above e. a and c onl... y 2. the following are clinical criteria of Bank ad Wise a. pulmonary b. neurological c. renal d. all the above e. a and c only 3. antibiotics in acute pancreatitis a. must be given to all cases b. should not be given c. given only to modarate & sever cases d. should cover anaerobic & Gam positive bactria e. none of the above 4. pancreatic carcinoma a. occure usually at the age of 50years b. usually is cystadenocarcinoma c. more favaorable in the body and tail d. less favourable if occure with back pain e. all the above 5. infected pancreatic necrosis a. is a collection of pus around the pancreas b. diagnosed by CT scan c. more serious than pancreatic abscess d. all the above e. none of the above contrast-enhanced computed tomography (CT) remains the gold standard in the diagnosis of pancreatic necrosis 6. secondarey survay in polytrauma a. should be done in the first hour b. done as soon as the patient is stable c. detects life threateing problems d. a and c e. none of the above 7. spontaneous ruptur of the spleen a. occure less in tropical countries b. the spleen may be enlarged c. malaria is a common cause d. all the above e. a and c 8. spleic aretry aneurysm a. incidence is around 5% b. usually symptomless c. more conmmon in males d. all the above e. non of the above 1 9. wolf skin graft a. used to cover large area of burn b. success rate is less than split thckness graft c. both thighs are common donor areas d. usually contracts e. none of the above 10 . medullary carcinoma of the thyroid a. is a tumor of the G cells b . may occur in MEN type 1b c. familial in 70% of the cases d. diagosed by low level of calcitonin e. amyloid stroma is charactrestic 11.solitary thyroid nodule a. 70% are follicular adenoma b. 30% are malignant c. more favourable in young males d. all the above e. none of the above 12. rupture of the diaphragm a. is a life threatenig problem b. usually missed c. poly galctan suture is used for repair d. all the above e. noe of the above 13. Varicose ulcer is: a.Usually very painful& shallow b.Deep with much necrotic tissue c.More common with primary varicose vein d.A & C only e.None of the above 14. Complication of vascular graft includes All the following except: a.Infection b.Aneurysm c.Graft failure d.Hemorrhage e.a & c only 15. Adequate urine out put for adult postoperative surgical patient is greater than: a.35 ml per hour regardless of body size b. 50 ml per hour regardless of body size c. o.5 ml per kg. per hour d. 1 ml per kg. per hour e.1.5 ml per kg. per hour 16. Gangrene: a. is necrosis of tissue b. The cause may be venous occlusion c. usually painful d.All the above e.None of the above 2 17. Lynphedema: a. may be Congenital b. should be bilateral c. may be pitting in early stage d.A & C only e. None of the above 18. Suprapubic cystostomy: a. indicated in case of bladder out flow obstruction b. indicated in case of urethral injury c. indicated in case of urethral stricture d. All the above e. B& C only 19.differential diagnosis of Acute scrotal swelling in young adult includes all the follow except: a. Incarcerated inguinal hernia . b. Torsion of testes c. Acute epididymo- orchitis d. Teratoma e.. Seminoma 20. Horizontal spread of infection across the external sphincter can result in which type of anorectal abscess: a. ischiorectal b. perianal c. supralevator d. intersphincteric e. intermuscular 21. All of the following statements are true of diffuse esophageal spasm EXCEPT: a. chest pain is frequently seen b. high amplitude esophageal contraction are present. c. it is best diagnosed with barium esophogram. d. usual surgical treatment is long esohagomyotomy. e. most patients do not have significant coronary artery disease. 22. Gastroesophageal reflux is BEST diagnosed with: a. radiography b. 24-hour pH monitoring of lower esophagus c. esophagoscopy d. documentation of a decrease in esophageal pH after HCI is placed in the stomach . e. acid-clearing swallowing test . . 23. The risk of esophageal cancer increases with all of the following EXCEPT: a. alcohol ingestion. b. smoking . c. chronic ingestion of hot beverages. d. aflatoxin. e. poor oral hygiene. 3 .24. The treatment of an esophageal burn with a caustic agent may include all of the following EXCEPT: a. expeditious administration of an antidote. b. induction of vomiting. c. steroids and antibiotics. d. bougienage. e. gastrectomy. 25. All of the following substances are irritating to the peritoneum EXCEPT: a. bile. b. meconium. c. blood. d. gastric content. e. pus. 26. Complications of truncal vagotomy and pyloroplasty include all of the following EXCEPT: a. dumping syndrome. b. recurrent ulcer. c. diarrhea. d. alkaline reflux gastritis. e. steatorrhea. 27. . Gastric polyps: a. are most commonly adenomatous. b. require gastrotomy and removal if greater than 2 cm and are pedunculated. c. are rarely multiple. d. are clearly premalignant. e. are more frequent in achlorhydric patients. Hyperplastic polyps are among the most commonly observed gastric polyps 28. . Vascular compression of the duodenum resulting in obstruction: a. is present primarily in patients who are overweight. b. should be given a trial of conservative management. c. is common in pediatric patients. d. is best diagnosed by identifying a "double bubble" sign on abdominal x-ray. e. includes as medical therapy lying in the supine position after meals 29. Conditions associated with gastric cancer include all of the following EXCEPT: a. higher socioeconomic groups. b. pernicious anemia. c. chronic atrophic gastritis. d. adenomatous polyps. e. a high intake of dietary nitrates 30. . Patients with morbid obesity have an increased incidence of all of the following EXCEPT: a. gastric carcinoma. b. diabetes. c. stroke d. gallbladder disease. e. joint deterioration. 4 31. All of the following contribute to malabsorption following truncal vagotomy and antrectomy EXCEPT: a. increased rate of gastric emptying. b. poor mixing of pancreatic secretions and bile salts with food. c. increased release of secretions and bile salts with food. d. decreased small intestinal transit time. e. malabsorption of fat and carbohydrates. 32. All of the following statements are true about patients with carcinoid tumors EXCEPT: a. they often have evidence of serotonin production. b. tumor growth is often slow. c. the majority have carcinoid syndrome. d. they have a much better prognosis if the tumors are less than 2 cm. e. the combination of streptozotocin and 5-fluorouracil can often result in objective response. 1. A pregnant woman in her 32nd wk of gestation is given magnesium sulfate for pre-eclampsia. The earliest clinical indication of hypermagnesemia is a. Loss of deep tendon reflexes b. Flaccid paralysis c. Respiratory arrest d. Hypotension 17. The chief surgical risk to which patients with polycythemia vera are exposed is that due to a. Anemic disturbances b. Hemorrhage c. Infection d. Renal dysfunction 28. The surgeon should be particularly concerned about which coagulation function in patients receiving anti-inflammatory or analgesic medications? a. APTT b. PT c. Reptilase time d. Bleeding time 29. The substrate depleted earliest in the postoperative period is d. Glycogen 26. Signs and symptoms of hemolytic transfusion reactions include a. Hypothermia b. Hypertension c. Polyuria d. Abnormal bleeding 5 27. A patient suspected of having a hemolytic transfusion reaction should be managed with b. Fluid restriction d. Steroids e. Fluids and mannitol 53. In a hemolytic reaction caused by an incompatible blood transfusion, the treatment that is most likely to be helpful is e. Stopping the transfusion immediately A 22-months-old child develops maculopapular rash, after 4 days of high fever, associated ?with posterior occipital lymphadenopathy. What might be the diagnosis A. Measles B. Rubella C. Roseola infantum D. Erythema infectiosum ?In which of the following layer of skin are melanocytes located A. Stratum corneum B. Stratum granulosum C. Stratum spinosum D. Stratum basalis :Perinaud syndrome occurs due to lesion in A. Superior colliculi B. Inferior colliculi C. Red nucleus D. Thalamus 33. The enteric fluid with an electrolyte (Na, K, C1-) content similar to that of Ringer’s lactate is a. Saliva b. Contents of small intestine c. Contents of right colon d. Pancreatic secretions Which of the following cerebral lobe is usually spared in Alzheimer disease? A. Frontal lobe B. Temporal lobe C. Parietal lobe D. Occipital lobe Which of the following disease is characterized by rapidly progressive dementia with myoclonus? A. Alzheimer disease B. Pick disease C. Creutzfeldt-Jakob disease D. Vascular dementia 34. Which of the following medications administered for hyperkalemia counteracts the myocardial effects of potassium without reducing the serum potassium level? b. Sodium bicarbonate 6 c. 50% dextrose d. Calcium gluconate e. Insulin 32. Hypocalcemia is associated with a. Acidosis b. Shortened QT interval c. Hypomagnesemia d. Myocardial irritability 36. Which of the following characteristics of this patient might increase the risk of a wound infection? a. History of colon surgery b. Hypertension c. Male sex d. Receipt of chemotherapy 38. A correct statement regarding 5% dextrose in 0.9% saline is which of the following? a. It contains the same concentration of sodium ions as does plasma c. It is isosmotic with plasma d. It has a pH of 7.4 e. It may cause a dilutional acidosis 39. Correct statements regarding lactated Ringer’s solution include which of the following? d. It has a pH of less than 7.0 Isotonic saline solutions contain 154 meq/L of both sodium and chloride ions. Each ion is in a substantially higher concentration than is found in the normal serum (Na=142 meq/L; Cl=103 meq/L). when isotonic solutions are given in large quantities, they overload the kidney’s ability to exerete chloride ion, which results in dilutional acidosis. They also may intensify preexisting acidosis by reducing the base bicarbonate/carbonic acid ration in the body. Isotonic saline solutions are particularly useful in hyponatremic or hypochloremic states and whenever a tendency to metabolic alkalosis is .present, as occurs with significant nasogastric suction losses or vomiting Administration of lactated Ringer’s solution is appropriate for replacing gastronistestinal losses and correcting extracelllular fluid deficits. Containing 130 meq/L sodium, lactated Ringer’s is hyposmolar with respect to sodium and provides approximately 150 mL of free water with each liter given. although ordinarily not a significant “physiological” to enable administration of large amounts without affecting the body’s acid-base balance significantly. It is worth noting that both isotonic saline and lactated Ringer’s are acidic with respect to the plasma: 0.9% NaCl/5%dextrose has a pH of 4.5; lactated .Ringer’s has a pH of 6.5 42. Prophylactic regimens of documented benefit in decreasing the risk of postoperative thromboembolism include 7 a. Early ambulation b. External pneumatic compression devices placed on the upper extremities c. Elastic stockings d. Leg elevation for 24 h postoperatively 43. Signs and symptoms associated with early sepsis include a. Respiratory acidosis b. Decreased cardiac output c. Hypoglycemia e. Cutaneous vasodilation 51. The most common physiologic cause of hypoxemia is a. Hypoventilation b. Incomplete alveolar oxygen diffusion c. Ventilation-perfusion inequality d. Pulmonary shunt flow 52. Generally accepted indications for mechanical ventilatory support include d. Respiratory rate greater than 35 breaths/min 54. Which of the following inhalation anesthetics accumulates in air-filled cavities during general anesthesia? a. Diethyl ether b. Nitrous oxide c. Halothane d. Methoxyflurane 55. Major alterations in pulmonary function associated with adult respiratory distress syndrome (ARDS) include a. Hypoxemia b. Increased pulmonary compliance c. Increased resting lung volume e. Decreased dead space ventilation Adult respiratory distress syndrome (ARDS) has been called “shock lung” or “traumatic wet lung” and occurs under a variety of circumstances. Clinically, its manifestations can range from minimal dysfunction to unrelenting pulmonary failure. Three major physiologic alterations include (1) hypoxemia usually unresponsive to elevations of inspired oxygen concentration; (2) decreased pulmonary compliance, as the lungs become progressively stiffer and harder to ventilate; and (3) decreased functional residual capacity. Progressive alveolar occurs owing to leakage of protein-rich fluid into the interstitium and the alveolar spaces with the subsequent Radiologic picture of diffuse fluffy infiltrates bilaterally. Ventilatory abnormalities develop that result in shunt formation, decreased resting lung volume and increased dead space ventilation. 58. Dopamine is a frequently used drug in critically ill patients because 8 a. At high doses it increases splanchnic flow b. At high doses it increases coronary flow c. At low doses it decreases heart rate d. At low doses it lowers peripheral resistance Dopamine has a variety of pharmacologic characteristics that make it useful in critically ill patients. In low doses [1 to 5 mg/(kg.min)], dopamine affects primarily the dopamonergic receptors. Activation of these receptors causes vasodilation of the renal and mesenteric vasculature and mild vasoconstriction of the peripheral bed, which thereby redirects blood flow to kidneys and bowel. At these low doses, the net effect on the overall vascular resistance may be slight. As the dose rises [2 to 10 mg/(kg.min)], β1-receptor activity predominates and the inotropic effect on the myocardium leads to increased cardiac output and blood pressure. Above 10 mg/(kg.min), α-receptor stimulation causes peripheral vasoconstriction, shifting of blood from extremities to organs, decreased kidney function and hypertension. At all doses, the diastolic blood pressure can be expected to rise; since coronary perfusion is largely a result of the head of pressure at the coronary ostia, .coronary blood flow should be increased 63. If end-diastolic pressure is held constant, increasing which of the following will increase the cardiac index? a. Peripheral vascular resistance b. Pulmonary wedge pressure c. Heart rate d. Systemic diastolic pressure 68. The preoperative characteristics of patients likely to experience postoperative ischemia after non cardiac surgery include a. Angina b. More than three premature ventricular contractions (PVCs) per minute c. Dyspnea on exertion d. Tricuspid regurgitation 70. Compensatory mechanisms during acute hemorrhage include a. Decreased cerebral and coronary blood flow b. Decreased myocardial contractility c. Renal and splanchnic vasodilation d. Increased respiratory rate e. Decreased renal sodium resorption 73. An 18-year-old woman develops urticaria and wheezing after an injection of penicillin. Her blood pressure is 120/60 mm Hg, heart rate is 155 beats/min, and respiratory rate is 30 breaths/min. Immediate therapy should include a. Intubation b. Epinephrine c. Beta blockers e. Fluid challenge 74. During blood transfusion, 9 clotting of transfused blood is associated with a. ABO incompatibility b. Minor blood group incompatibility c. Rh incompatibility d. Transfusion through Ringer’s lactate 75. When an arterial blood gas determination of PCO2 40 kPa is obtained b. Alveolar ventilation is adequate 77. Among patients who require nutritional resuscitation in an intensive care unit, the best evidence that nutritional support is adequate is a. Urinary nitrogen excretion levels b. Total serum protein level c. Serum albumin level d. Serum transferrin levels 78. Paradoxical aciduria (the excretion of acid urine in the presence of metabolic alkalosis) may occur in the presence of a. Release of inappropriate antidiuretic hormone b. Severe crush injury c. Acute tubular necrosis d. Gastric outlet obstruction 79. If a patient suffered a pulmonary arterial air embolism during an open thoracotomy, the anesthesiologist’s most likely observation would be e. Falling end-tidal CO2 A. Unexpected systemic hypertension B. Rising right atrial filling pressures C. Reduced systemic arterial oxygen saturation D. Rising systemic CO2 partial pressures E. Falling end-tidal CO2 A 72-year-old man undergoes resection of an abdominal aneurysm. He arrives in the ICU with a core temperature of 33°C (91.4°F) and shivering. Which of the following is a physiologic consequence of the shivering? Rising mixed venous O2 saturation Increased production of CO2 Decreased consumption of O2 Rising base excess Decreased minute ventilation 10 Shivering is the physiologic effort of the body to generate heat to maintain the core temperature. In healthy persons, shivering increases the metabolic rate by 3 to 5 times and results in increased O2 consumption and CO2 production. In critically ill patients, these metabolic consequences are almost always counterproductive and should be prevented with other means employed to correct systemic hypothermia. In the presence of vigorous shivering, O2 debt in the muscles and lactic acidemia develop. 81. To prepare for operating on a patient with a bleeding history diagnosed as von Willebrand’s disease (recessive), you would give d. Cryoprecipitate von Willebrand disease is similar to true hemophilia in frequently of occurrence. It is being diagnosed more commonly today because of more reliable assays for factor VIII. This autosomal dominant disorder (recessive transmission can occur) is characterized by a diminution in factor VIII:C (procoagulant) activity. The reduction in activity is not as great as in classic hemophilia, and the clinical manifestations are more subtle. These manifestations are often overlooked until an episode of trauma or surgery makes them apparent. Treatment requires correcting the bleeding time and providing factor VIII R:WF (the von Willbrand factor). Only cryoprecipitate is reliably effective. High-purity factor VIII:C concentrates, effective in hemophilia, lack the von Willbrand factor and are consequently underdependable. 83. The accidental aspiration of gastric contents into the tracheobronchial tree should be initially treated by a. Tracheal intubation and suctioning b. Steroids c. Intravenous fluid bolus d. Cricothyroidotomy 84. In performing a tracheostomy, authorities agree that a. The strap muscles should be divided b. The thyroid isthmus should be preserved c. The trachea should be entered at the second or third cartilaginous ring d. Only horizontal incisions should be used Although tracheostomy is occasionally an emergency procedure, it can be more effectively performed in an operating room where hemostasis and antisepsis are readily achieved. Most authorities recommend a horizontal incision; however, limited direct midline incisions have the advantage of not opening any unnecessary tissue planes and perhaps reducing the incidence of bleeding complications. Both approaches have advocates. In either case, the skin incision is made just below the cricoid cartilage, the strap muscles are spared and retracted, the thyroid isthmus is divided if necessary, and the trachea is entered at the second tracheal ring. The second and third tracheal 11 rings are incised vertically, allowing placement of the tracheostomy tube. The .first tracheal ring and the cricoid cartilage must be left intact 85. If malignant hyperthermia is suspected intraoperatively a.Complete the procedure but pretreat with dantrolene prior to future elective surgery b.Administer inhalational anesthetic agents c.Administer succinylcholine d.Hyperventilate with 100% oxygen e.Acidify the urine to prevent myoglobin precipitation in the renal tubules 86. Central venous pressure (CVP) may be decreased by a. Pulmonary embolism b. Hypervolemia c. Positive-pressure ventilation d. Pneumothorax e. Gram-negative sepsis 88. Signs and symptoms of Addison’s disease include a. Hypothermia b. Hypokalemia c. Hyperglycemia d. Hyponatremia e. Hypervolemia 89. The etiologic factor implicated in the development of pulmonary insufficiency following major non thoracic trauma is a. Aspiration b. Atelectasis c. Fat embolism syndrome d. Fluid overload 90. For the severely traumatized patient requiring airway management d. Intubation should be performed in the emergency room if the patient is unstable 91. Treatment for clostridial myonecrosis (gas gangrene) Includes which of the following measures? a. Administration of an antifungal agent b. Administration of antitoxin c. Wide debridement d. Administration of hyperbaric oxygen 12 92. An abnormal ventilatioperfusion ratio (Qs/Qr) in the postoperative patient has been associated with a. Pulmonary thromboembolism b. Lower abdominal surgery d. The upright position e. Increased cardiac output Abnormalities of ventilation-perfusion ratio result from the shunting of blood to a hypoventilated .lung or from the ventilation of hypoperfused regions of lung tissue When this imbalance is extreme, as following massive pulmonary thromboembolism, the effect is life-threatening hypoxemia. Other common predisposing factors in the postoperative patient that contribute to this maldistribution include the assumption of a supine position, thoracic and upper abdominal incisions, obesity, atelectasis, and reduced cardiac output 93. Correct statements concerning drowning or near-drowning include which of the following? d. Renal damage may occur in affected persons as a result of hemoglobinuria 94. Spontaneous retroperitoneal hemorrhage during anticoagulant therapy a. Is best confirmed by bleeding scan b. Is equally likely with parenteral and oral anticoagulants c. May mimic an acute surgical abdomen d. Frequently requires laparotomy for ligation of the bleeding site 96. Indications for surgical intervention to remove smuggled drug packets that have been ingested include e. Signs of toxicity from leaking drug packets Burns 1- When determining the depth of a burn: A. A knowledge of the type of injury is important. B. The presence of blisters is of no clinical significance. C. Impairment of sensibility of the burned area denotes full thickness burn. D. The presence of severe pain denotes a full thickness skin loss. E. A&C only. 2- Estimation of the area of a burn: ( all correct except one) A. Is of very little clinical significance. B. Provides important prognostic information. C. Is an important factor in the estimation of the fluid required. D. Can be based on a formula which states that the adult trunk is 36 per cent of the whole body surface area. E. Should be recorded in each chart of burned patient. 13 3- Patients with major burns: A. Are in a negative nitrogen balance. B. Have normal calorie requirements. C. Do not generally become anaemic. D. Are resistant to septicaemia. E. All of the above. 4- The catabolic response to trauma and infection is characterized by: A. An increase in lean body mass. B. A positive nitrogen balance. C. Gluconeogenesis. D. A falling haemoglobin level. E. A&B only. 5- The catabolic response to trauma: A. Is related to the severity of the trauma. B. Is accompanied by decreased urinary losses of potassium and nitrogen. C. Can be prevented by parenteral nutrition. D. Does not occur in the adrenalectomised patient. E. C&D only. 6- Scalds: A. Are more frequent in children. B. Commonly cause full thickness skin loss. C. Should be skin grafted within 48 hours of the injury. D. Need routine antibiotic treatment. E. All of the above. 7- The dressing of a small burn should be: A. Occlusive. B. Non-absorbtive. C. Non-compressive. D. Changed daily as a routine. E. All of the above 8- A partial thickness burn: A. Usually requires grafting. B. May deteriorate into full thickness skin loss. C. Rarely causes severe physiological derangement of the patient. D. Heals within 7 days in the absence of infection. E. C&D only. 9-Fluid losses in a major burn: A. Are maximal between 12 and 24 hours after the injury. B. Are related to the age of the patient. C. Are not related to the weight of the patient. D. Are related to the area burnt. E. Are not related to the burnt duration. 10- The increased fluid requirements of a patient with a full thickness burn are due to: (all 14 correct except one) A. Increased evaporative water loss. B. Sequestration of fluid in the injured tissues. C. Serum exuding from the burned area. D. Destruction of blood in the skin vessels. E. Vomiting & paralytic ileus occasionally 11- 48 hours after a major burn and with satisfactory fluid therapy a patient: A. Has very few abnormal fluid losses. B. May need a blood transfusion. C. Is often hypornatraemic. D. Usually needs skin grafting. E. C&D only. 12- Major burns are sometimes complicated by: (all correct except one) A. Acute gastric and duodenal ulcers. B. Paralytic ileus. C. Cerebral oedema. D. Mesenteric thrombosis. E. Septicemia. 13- If burned patient, associated pulmonary injury: (all correct except one) A. Should be suspected in head and neck burns. B. Should be suspected when the nasal hairs are burnt. C. Does not appear clinically in the first 24 hours. D. Should be suspected if burns occurred in closed space. E. May require ICU care. 14- Secondary infection of burns: A. Is less common in partial than in full thickness skin loss. B. Is relatively more common in burns of more than 20 per cent body area. C. Is avoided by leaving the burn eschar intact. D. Is avoided by the immediate application of a sterile occlusive dressing. E. All of the above. 15- . The early management of a burn wound may include: A. Early excision. B. Occlusive dressings. C. Exposure treatment. D. Dressings with local antibiotics. E. All of the above. 16- Skin grafting of a burn wound: A. Should usually be with full thickness skin grafts. B. Is more likely to be successful if undertaken in the first week after injury. C. Will be unsuccessful unless the wound surface is sterile. D. Minimizes scar contracture. E. A&C only. 17- The prognosis of a burned patient is: A. Not related to the patient's age. B. Related to the area burnt.?????? C. Generally better below the age of 10 years. 15 D. Very poor in the patient with burns of over 40 per cent surface area. E. C&D only. 2. Anion gap is: A. The difference between measured anions and measured cations B.Is normal in lactic acidosis C.Is high in shock D. Normally is 20 mmol E.High in pancreatic fistula 1. Causes of hypovolaemic shock include all the following Except: A. burn injury. B. low output intestinal fistula C. spinal cord transaction. D. myocardial infarction. E. endotoxaemia. 2. A 53-year-old female has had a high fever with cough productive of yellowish sputum for the past 2 days. Auscultation of the chest reveals a few crackles in both lung bases. A chest radiograph reveals bilateral patchy pulmonary infiltrates. Which of the following inflammatory cell types will be seen in greatly increased numbers in a sputum specimen? A. Macrophages B. Neutrophils C. Mast cells D. Small lymphocytes E. Langhans giant cells 3. The most common breast lesion in women is A. fibroadenoma B. carcinoma of the breast C. fibrocystic disease D. ductal papilloma 4. The liver is held in position in the upper part of the abdominal cavity mainly by: A. Attachment of hepatic vein to inferior vena cava B. Peritoneal ligament C. Tone of Abdominal muscles D. Angular ligament 16 Palestinian Medical Council Final Written Exam (April,2011) Paper ( I ) Candidate’s Name:…………………………………………………………………………………………………………….................. E. Lesser omentum 5. When compared with the late-evening values typically observed in normal subjects, plasma levels of both adrenocorticoiropic hormone and conisol would be expected to be higher in which of the following individuals? A. Normal subjects after waking in the morning B. Normal subjects administered dexamethasone C. Patients with Cushing's syndrome (adrenal adenoma) D. Patients with Addison's disease E. Patients with Conn's syndrome 6. A 23-year-old female receiving chronic corticosteroid therapy for an autoimmune disease underwent minor surgery for incision and drainage of an abscess on her upper outer right arm. The wound healed poorly over the next month. Which of the following aspects of wound healing is most likely to be deficient? A. Re-epithelization B. Fibroblast growth factor elaboration C. Collagen deposition D.Serine proteinase production E.Neutrophil infiltration 7. Regarding the blood supply of the stomach which of the following is not true A. Left gastric artery arise from hepatic artery B. Right gastric artery the lower right part of stomach C. The short gastric artery supply the fundus D. Left gastroepiploic artery arise from splenic artery at the hilum of stomach E. right gastroepiploic artery arise from gasrtoduodenal artery left gastric artery arises from the celiac artery 8. Precipitating physiological events in the metabolic response to injury include: A. haemorrhage. B. pain. C. ischaemia. D. Endotoxaemia E. all the above 9. Psychological stress is often associated with peptic ulcer disease. Which of the following is thought to be a contributing factor in stress-induced ulcer disease? A. Sympathetic stimulation decreases gastric acid secretion B. Sympathetic stimulation increases peristalsis, which decreases the transit time of ingested food C. Psychological stress increases mucous secretion 17 D.Sympathetic stimulation decreases the alkaline mucous secretions of Brunner's glands located in the first few centimeters of the duodenal wall 10. Low molecular weight heparin (LMWH) produces its primary effects because of its inhibition of which factor? A. IIa B. IXa C. Xa D. XIa E. XIIa 11. All of the following are potential outcome in laparoscopic surgery EXCEPT : A. Hypercarbia B. Alkalosis C. Decrease urine out put D. Increase intracranial pressure E. Increased cardiac work 12. Acute Epidural haematoma : A. due to meningeal artery tear B. can be treated conservatively C. classically there is contra lateral, dilated, fixed pupil D. needs operation within 24 hours E. a and c only 13. Which of the following best characterizes the secretions of the small intestine? (A) Hypotonic and slightly acidic (B) Hypotonic and slightly alkaline (C) Isotonic and slightly alkaline (D) Isotonic and slightly acidic 14. Management of hypovolaemic shock involves all except: A. achievement of venous access via peripheral vein catheterisation. B. bladder catheterisation. C. immediate administration of whole blood or red cell concentrate. D. effective analgesia. E. oxygen administration. 15. Concerning the use of a central venous catheter: 18 A. administration of TPN is safe and does not require repetitive haematological and biochemical monitoring. B. its insertion should have mandatory electrocardiographic monitoring. C. it provides a convenient portal for blood sampling and antibiotic administration. D. if tunnelled subcutaneously it has a higher incidence of infection with endogenous staphylococcus. E. if infected it is effectively treated by administration of antibiotics via the offending catheter. 16 .A 16-year old driver, without seat belt, is involved in a rollover head-on accident. Extensive damage to the vehicle . The patient was pulled out of the car, hemodynamically unstable and was transported to a trauma center. During transportation the patient became severely hypotensive , with distended neck veins, unresponsive, with impending respiratory distress. Which of the following is considered an immediate life-threatening injury in this patient? A. pneumothorax secondary to rib fractures B. aortic intimal tear C. diaphragm rupture D. tension pneumothorax E. myocardial contusion 17. Hypochlorhydria is a condition in which acid secretion by the stomach is greatly reduced. How does this condition affect the digestion and absorption of food? (A) Digestion and absorption of all food substances are nearly normal (B) Digestion and absorption of all foods substances are markedly reduced (C) Digestion and absorption of carbohydrates are greatly affected by this condition (D) Digestion and absorption of fats are greatly affected by this condition 18. In chest injury the following are indications of thoracotomy EXCEPT : A. When cardiac tamponade present. B. Massive air leak C. For all transmediastinal wounds D. Flail chest with sever lung contusion E. Clotted hemothorax 19. Which of the following tends to decrease potassium secretion by the cortical collecting tubule? (A) Increased plasma potassium concentration (B) A diuretic that decreases proximal tubule sodium reabsorption (C) A diuretic that inhibits the action of aldostcrone (e.g., spironolactone) (D) Acute alkalosis (E) High sodium intake 19 20.The metabolic response to injury is characterised by a sequence of physiological events aimed at: A. increasing core body temperature. B. conservation of sodium and water. C. mobilising glucose from fat and protein stores. D. maintaining body weight. E. enhancing immune function. 21. A 50 year old man present with haematemsis, Endoscopy shows a bleeding peptic ulcer in the posterior wall of the first part of duodenum. Which artery is involved A. Right gastric artery B. Right gastroepiploic artery C. inferior pancreaticoduodenal artery D. gasrtoduodenal artery E. superior pancreaticoduodenal artery 22. Fasciotomy for extremity compartment syndrome should be performed at a compartment pressure exceeding : A. 20 mmHg B. 30 mmHg C. 40 mmHg D. 50 mmHg E. none of the above 23. All of the following are true about neurogenic shock except: a. there is a decrease in systemic vascular resistance and an increase in venous capacitance. b. tachycardia or bradycardia may be observed, along with hypotension. c. the use of an alpha agonist such as phenylephrine is the mainstay of treatment. d. Severe head injury, spinal cord injury, and high spinal anesthesia may all cause neurogenic shock. 24. The radiographic findings indicating a torn thoracic aorta include all Except : a. Widened mediastinum. b. Presence of an apical “pleural cap.” c. Tracheal deviation to the right. d. right hemothorax.(lt) The most common abnormality noted is a widening of the mediastinal shadow, although only 20% to 40% of patients with a wide mediastinum have aortic injury. In addition to the radiographic signs listed, other findings that may alert the physician to the possibility of an aortic tear include loss of aortic contour, elevation of the left mainstem bronchus, depression of the right mainstem bronchus, shift of the nasogastric tube to the left, and the presence of retrocardiac density. Aortography remains the “gold standard” diagnostic modality and is indicated if aortic injury is suspected on the basis of mechanism of injury and any of these suggested findings. 20 [Show More]
Last updated: 1 year ago
Preview 1 out of 792 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 12, 2022
Number of pages
792
Written in
Additional information
This document has been written for:
Uploaded
Nov 12, 2022
Downloads
0
Views
71