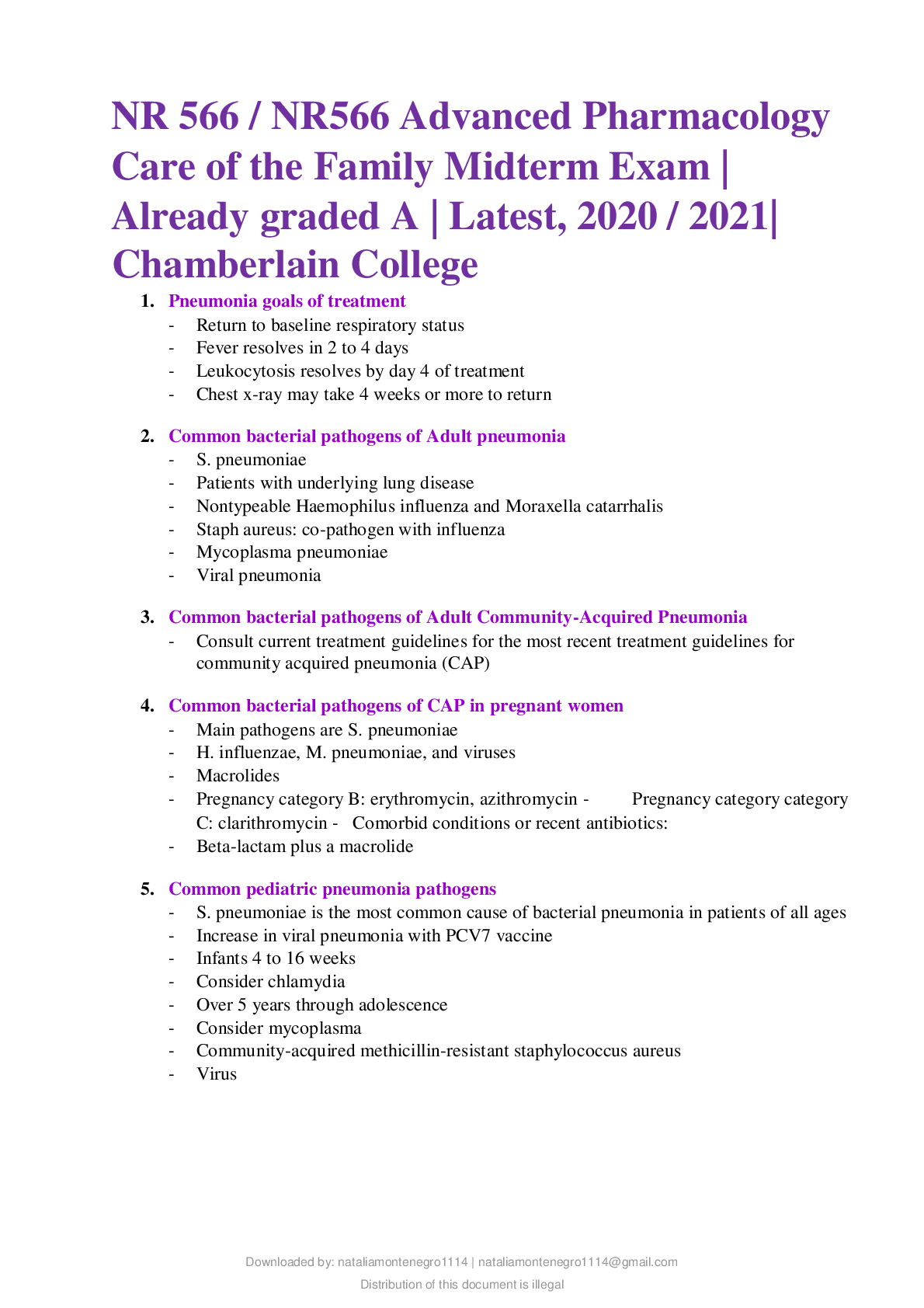
*NURSING > EXAM > NR 566 / NR566 Advanced Pharmacology Care of the Family Midterm Exam | Rated A | Chamberlain College (All)
NR 566 / NR566 Advanced Pharmacology Care of the Family Midterm Exam | Rated A | Chamberlain College
Document Content and Description Below
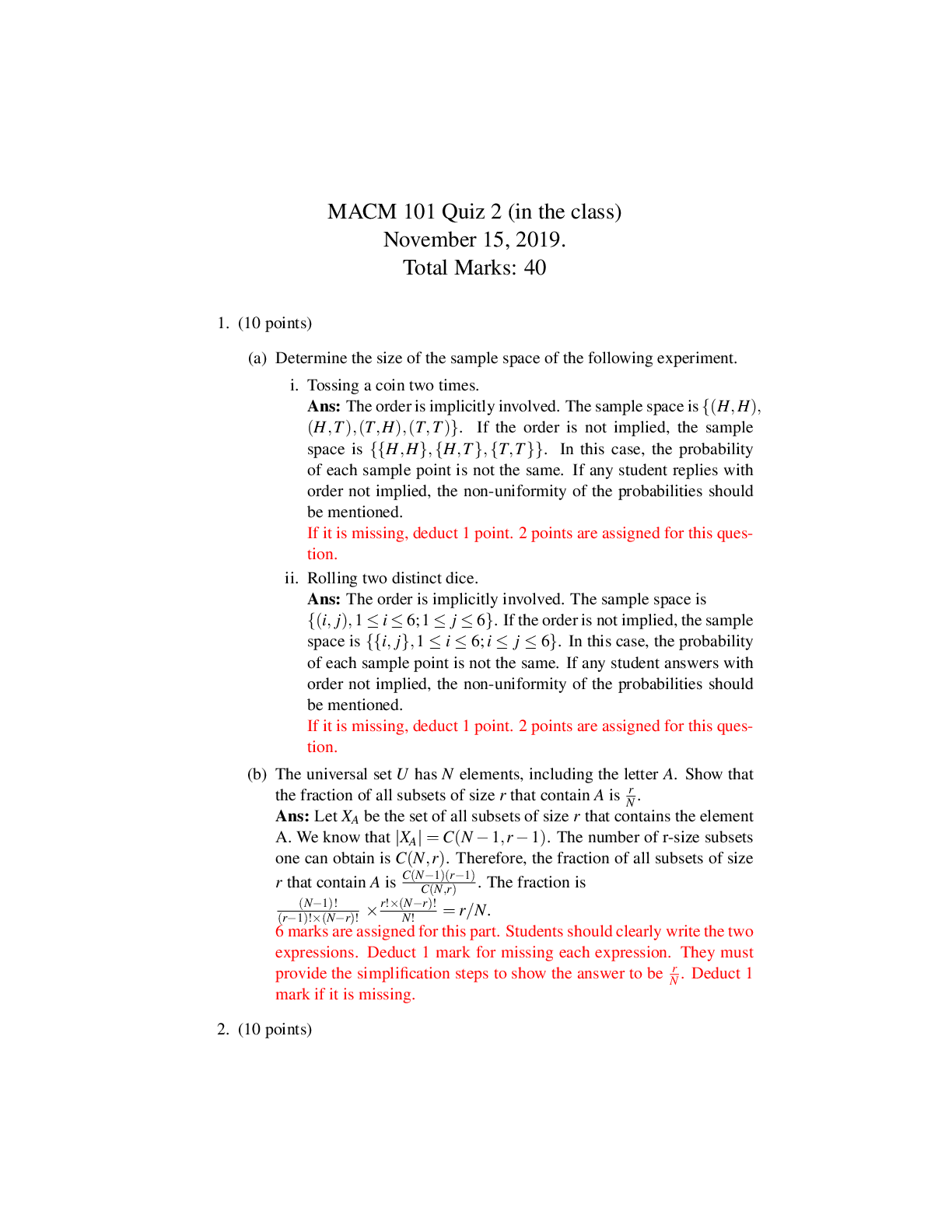
NR 566 / NR566 Advanced Pharmacology Care of the Family Midterm Exam | Rated A | Chamberlain College NR 566 / NR566 Advanced Pharmacology Care of the Family Midterm Exam | Already graded A | La... test, 2020 / 2021| Chamberlain College 1. Pneumonia goals of treatment - Return to baseline respiratory status - Fever resolves in 2 to 4 days - Leukocytosis resolves by day 4 of treatment - Chest x-ray may take 4 weeks or more to return 2. Common bacterial pathogens of Adult pneumonia - S. pneumoniae - Patients with underlying lung disease - Nontypeable Haemophilus influenza and Moraxella catarrhalis - Staph aureus: co-pathogen with influenza - Mycoplasma pneumoniae - Viral pneumonia 3. Common bacterial pathogens of Adult Community-Acquired Pneumonia - Consult current treatment guidelines for the most recent treatment guidelines for community acquired pneumonia (CAP) 4. Common bacterial pathogens of CAP in pregnant women - Main pathogens are S. pneumoniae - H. influenzae, M. pneumoniae, and viruses - Macrolides - Pregnancy category B: erythromycin, azithromycin - Pregnancy category category C: clarithromycin - Comorbid conditions or recent antibiotics: - Beta-lactam plus a macrolide 5. Common pediatric pneumonia pathogens - S. pneumoniae is the most common cause of bacterial pneumonia in patients of all ages - Increase in viral pneumonia with PCV7 vaccine - Infants 4 to 16 weeks - Consider chlamydia - Over 5 years through adolescence - Consider mycoplasma - Community-acquired methicillin-resistant staphylococcus aureus- Virus 6. Clinical practice guidelines for treatment of CAP - Children under age 5 years - Bacterial pneumonia (S. pneumoniae) - Amoxicillin: 80 to 90 mg/kg/day - Ceftriaxone: 50 mg/kg/day until able to take oral antibiotics - Penicillin allergy: clindamycin or a macrolide - Infant with suspected chlamydial pneumonia - Azithromycin 20 mg/kg/day for 3 days OR erythromycin (EryPed) 50 mg/kg for 14 days - Children 5 Years or Older - Mycoplasma or other atypical most likely - Azithromycin: 10 mg/kg on day 1 and 5 mg/kg on days 2 through 5 - Clarithromycin: 15 mg/kg per day in two divided doses (maximum 1 g/day) - Erythromycin: 40 to 50 mg/kg/day 7. CAP treatment in pregnancy - abx treatment: - 1st choice: Erythromycin or azithromycin cat B. or Clarythromycin cat C. 8. Radiologic findings during CAP treatment - assist in confirming the dx of pneumonia vs other resp disorders such as lung abscess or tuberculosis 9. Treatment of chlamydial pneumonia - he standard treatment for infants is erythomycin 10. Nicotine patch teaching - Advise patients to dispose of used nicotine patches out of the reach of children or animals. Enough nicotine is left in a used patch to lead to toxic levels in a child or small animal. - The transdermal nicotine system, or "patch," provides a slow, cutaneous absorption of nicotine over many hours. The patch is applied to clean, nonhairy skin on the upper body or upper arm when the patient wakes up. Peak nicotine levels occur in 2 to 6 hours (brand-dependent) and then gradually decrease. Once the patch is removed, nicotine levels in the blood reach a nondetectable level in 10 to 12 hours in nonsmokers. 11. Nicotine gum patient teaching - Patients complain about the taste of the nicotine gum. Suggest that the patient try the flavored variety, which patients seem to tolerate better. - The patient should not eat or drink for 15 minutes before or while the lozenge is dissolving in the mouth. There may be a tingling sensation in the mouth as the lozenge dissolves. - Chewing too quickly causes an excess amount of nicotine to be released into the bloodstream, producing nausea, throat irritation, and hiccoughs. The patient should avoidsmoking while chewing nicotine gum because toxicity symptoms may occur (nausea, vomiting, and headache). 12. Common side effects associated with smoking cessation therapy - Constipation. 13. Contraindications for smoking cessation therapy. - Hypersensitivity to nicotine. - Myocardial infarction. - Life-threatening arrhythmias. - Severe or worsening angina pectoris. - Bupropion is contraindicated in patients with seizure disorders, bulimia, and anorexia nervosa and within 14 days of MAOIs. 14. Tuberculosis Etiology - Infectious disease caused by M. tuberculosis· Inhaled into the alveolus and spreads from lungs· M. tuberculosis grows slowly· Infection is spread almost exclusively by aerosolization of contaminated lung secretions 15. Rational drug selection for pregnancy for tuberculosis - INH and RIF. EMB should be included unless INH resistance is unlikely. 6 month therapy. Pyridoxine (vit b6) 25 mg/d should be added to the regimen to decrease incidence of peripheral neuropathy assoc with INH. 16. Rational drug selection for children for tuberculosis - INH and RIF are used for asymptomatic infection for 6-9 months. Multidrug regimens (INH RIF PZA EMB) are used for progressive disease. EMB may be used if risk of drugresistant organisms is present. DOT should be used for all children. 17. Criteria for resistant TB diagnosis - Primary resistance risk factors: exposure to a patient with drug-resistant TB, immigration from a country with a high prevalence of d-r TB, and greater than 4% incidence of d-r RB in the community. - Acquired/Secondary risk factors: poorly or inadequately treated TB. - DRUG RESISTANCE CAN ONLY BE PROVEN BY SUSCEPTIBILITY TESTING. - Second-line treatment usually requires injectable medications, which complicates the treatment regimen. Fluoroquinolones such as levofloxacin, moxifloxacin, and gatifloxacin are all active against M. tuberculosis. Based on the evidence so far, levofloxacin is the preferred oral fluoroquinolone for treating drug-resistant TB or when first-line agents cannot be used because of intolerance 18. Risk factors for fatal hepatitis with INH use - Pregnant and postpartum patients. Patients 50-64 years of age. Daily alcohol use, chronic liver disease, IV drug use. Black and hispanic women.INH has a black-box warning regarding the development of severe/fatal hepatitis, even after months of treatment.19. Prophylactic TB treatment for high risk patients - INH or via DOT with weekly INH/RPT. Standard anti-TB drugs ING and RIF used for asymptomatic infection for 6-9 months. 20. ACEIS and ARBS benefits in other conditions - CAD, Post MI, heart failure. - Clinical pearl: If you hear an abdominal bruit in a patient known to have vascular disease, give captopril, a short-acting ACEI, and measure serum creatinine prior to the dose and within 1 or 2 days after the dose. A rapid rise in the creatinine level suggests renal artery stenosis. A slower rise probably indicates a problem with poor hydration that can be corrected by rehydrating the patient and discontinuing or lowering the dose of any diuretics the patient is taking. 21. Management of ACEI side effects - Education concerning hypotensive reactions. - For ACEI-related cough, no effective treatment - may change to another ACEI or ARB. - Change in taste resolves on its own within 8-12 weeks. 22. Amiodarone monitoring - Cxray, PFT every 3-6 mo. - TSH, free T4 every 6 mo. - Opthalmic exam (slit lamp and fundoscopy) every 6 mo. 23. Flecainide monitoring - ECG, liver function studies, serum drug levels. - Watch for sinus node problems and AV block. - Keep trough <1 mcg/mL. 24. Mexiletine monitoring - Liver function studies, Aspartate aminotransferase (AST) elevations >3 times upper limit of normal have been observed. 25. Procainamide monitoring - CBC and Antinuclear antibody (ANA) titer. - At initiation of therapy for blood dyscrasias; at initiation for indication of lupus-like symptoms. 26. Propafenone monitoring - Liver function studies, CBC, renal and liver function studies 27. Sotalol monitoring - Fasting blood glucose 28. Cardiac glycosides monitoring - In general, testing should be done when any of the following occurs: o The patient is taking other drugs that may alter the pharmacokinetics of digoxin.o Steady state has been achieved (4 to 5 half-lives or 1 to 2 weeks) after starting a new dose. o Toxicity is suspected. o Confirmation of adequacy of maintenance dose is needed in situations of poor therapeutic response or patient adherence. o A reference point is needed in adjusting a dose. o The patient has progressive renal function decline. 29. Myocardial oxygen supply - Supply is reduced by the following: o Hemodynamic factors such as increased resistance in coronary vessels, hypotension, and decreased blood volume. ACE inhibitors, beta blockers, direct renin inhibitors, and the dihydropyridine CCBs decrease peripheral resistance through their vasodilatory actions. o Cardiac factors such as decreases in diastolic filling time, increases in heart rate, and valvular incompetence. Beta blockers and non-dihydropyridine CCBs decrease heart rate. The beta blockers have the further advantage of preventing the recurrence of MIs. o Hematological factors such as the oxygen content of the blood, the acid-base status of the blood, and anemia. o Systemic disorders, such as shock, which reduce blood flow or the availability of oxygen. 30. Myocardial oxygen demand - High systolic blood pressure, which increases the work the heart has to do to move blood from the left ventricle to the systemic circulation. One focus of anginal management is control of blood pressure. ACE inhibitors, beta blockers, direct renin inhibitors, and both types of CCBs decrease blood pressure. o Increased ventricular volume, which increases the work the heart has to do because the left ventricle must move more blood. ACE inhibitors reduce sodium and water retention. o Increased thickness of the myocardium (ventricular hypertrophy). The same mechanism that facilitated growth of the vessel walls in atherosclerosis also increases the thickness of the myocardium. ACE inhibitors play a major role here to decrease the remodeling. Beta blockers can assist in prevention of ventricular hypertrophy but play a smaller role. o Increased heart rate resulting from exercise, stress, hyperthyroidism, fever, anemia, hyperviscosity of the blood, or negative feedback systems' response to decreased cardiac output. Beta blockers can assist in decreasing heart rate resulting from conditions such as hyperthyroidism and from negative feedback patterns secondary to decreased cardiac output. [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 21, 2022
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Nov 21, 2022
Downloads
0
Views
31



.png)