Oncology > STUDY GUIDE > Rasmussen College NUR201 MDC4 Exam1 ONLY correct answers are provided. (All)
Rasmussen College NUR201 MDC4 Exam1 ONLY correct answers are provided.
Document Content and Description Below
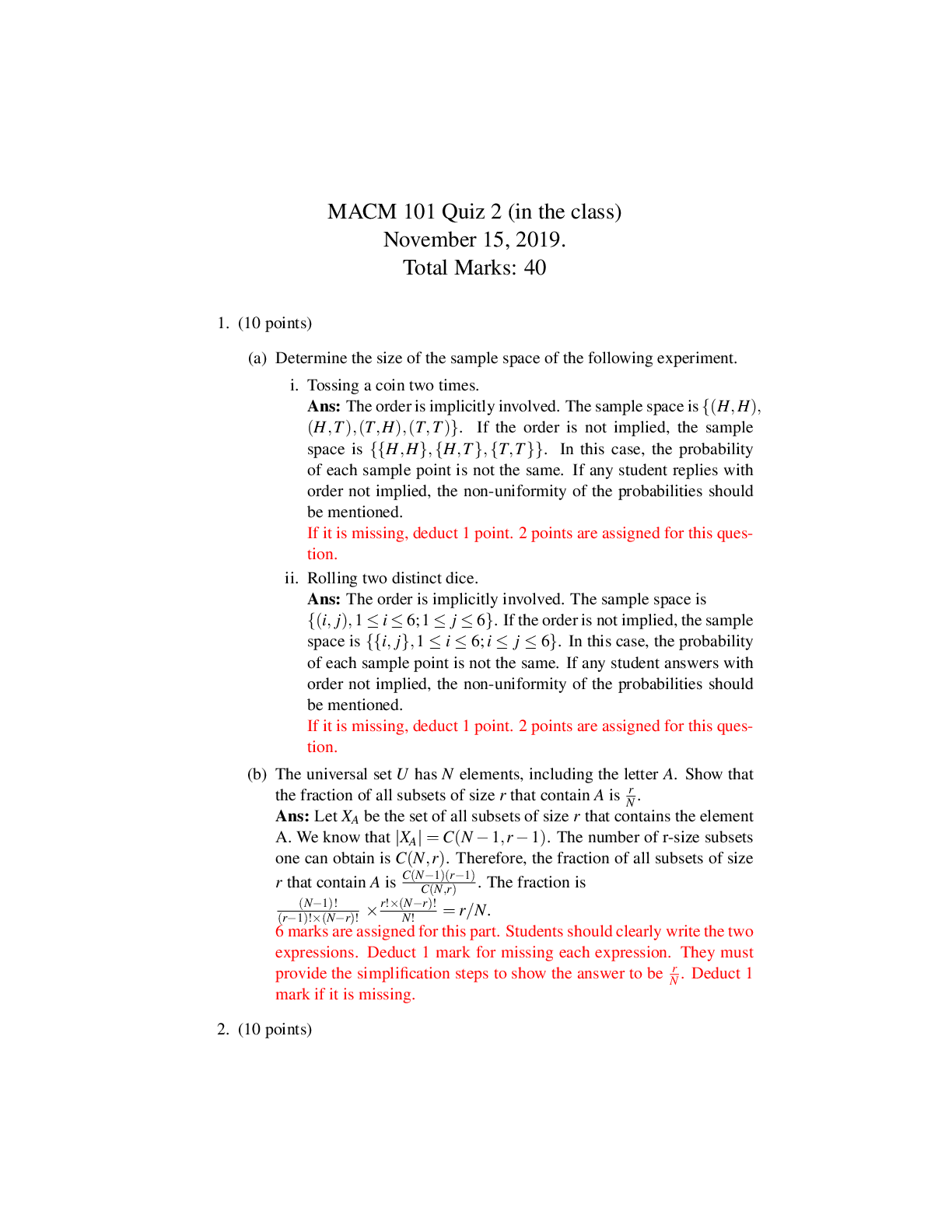
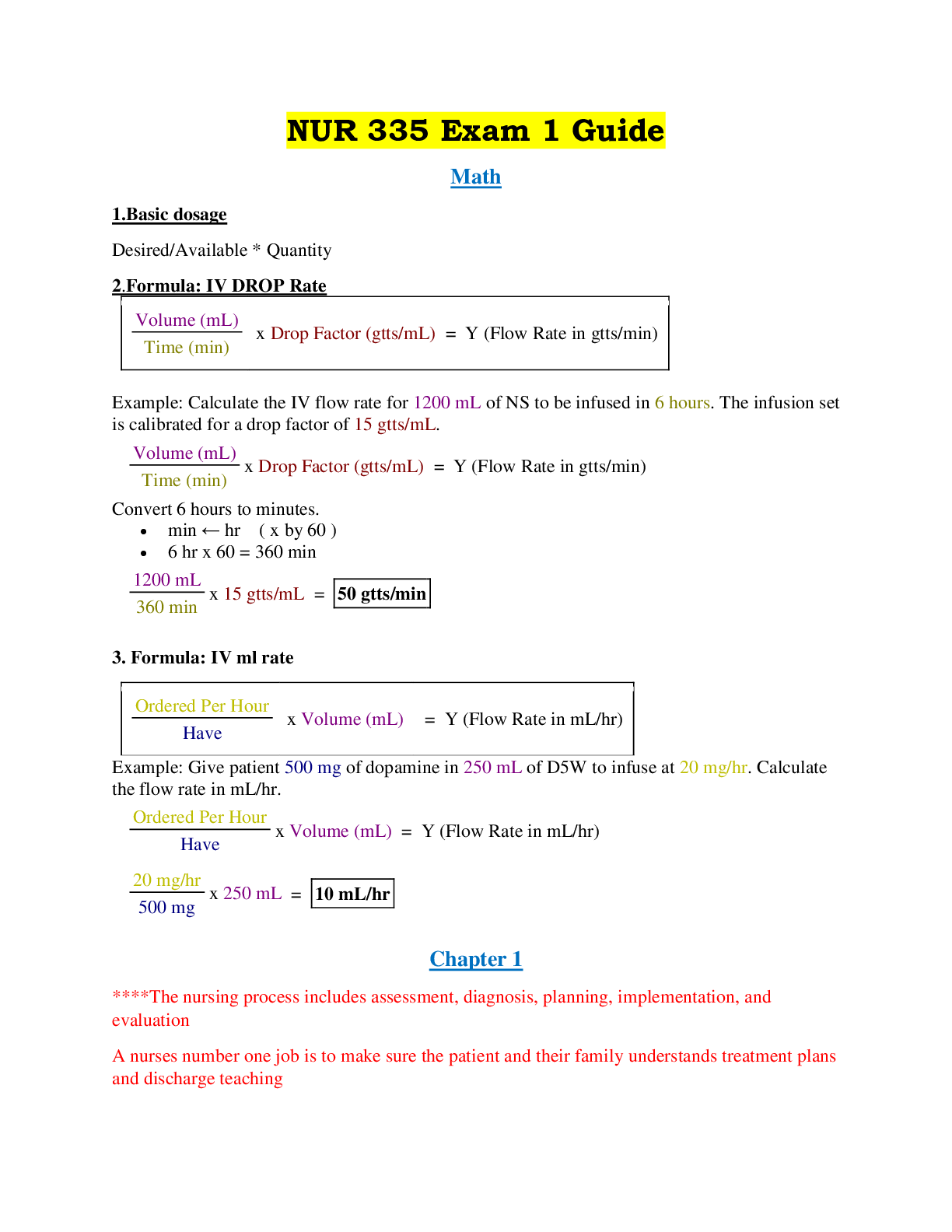
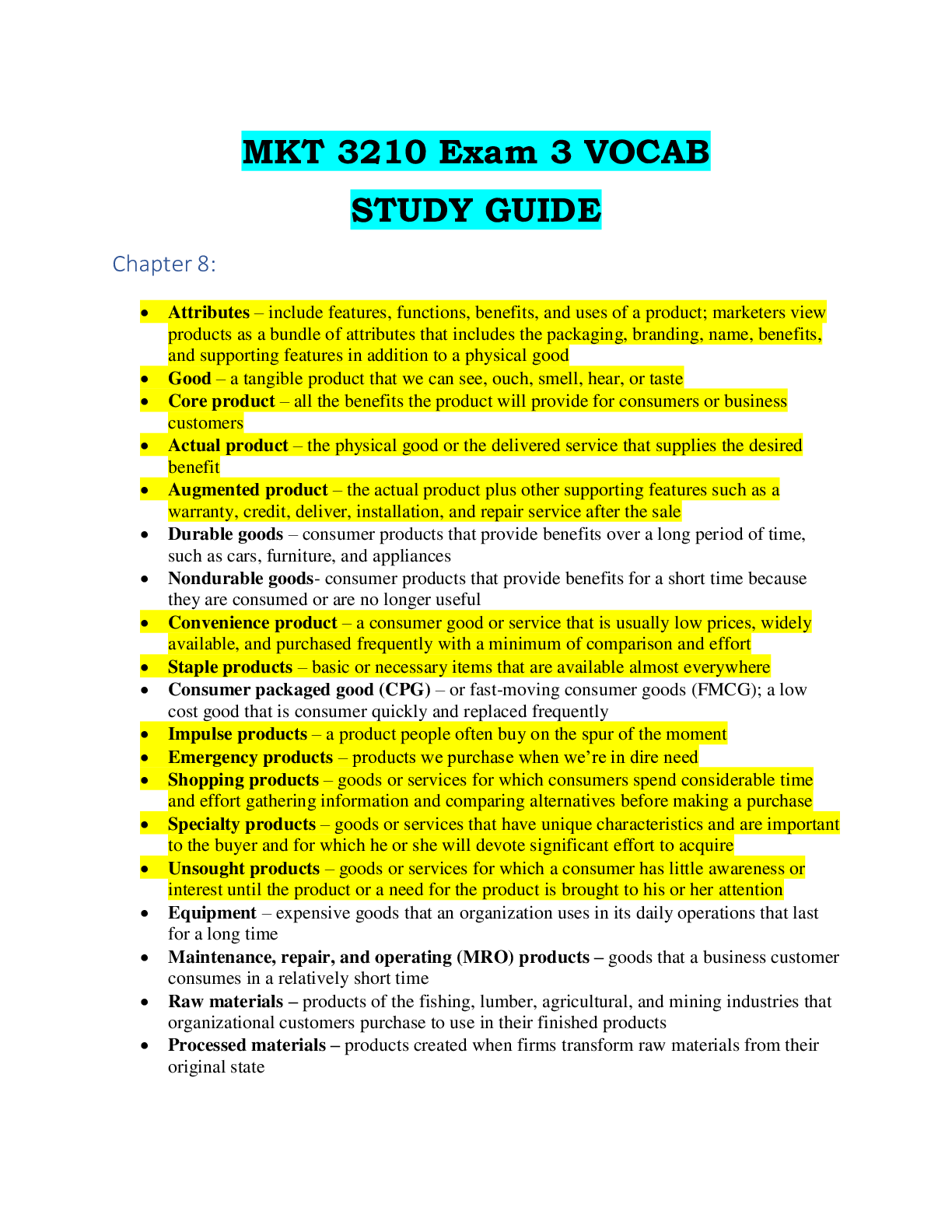
Rasmussen College NUR201 MDC4 Exam1 ONLY correct answers are provided. MDC4 Exam 1 Kahoots! Meaghan Harvley’s Kahoot 1. Alzheimer’s disease is a rapid, reversible brain disease. t/f a. False�... ��slow, progressive, irreversible 2. The patent can eat solid foods for up to 2 hours before their procedure/surgery. t/f a. False—6-8 hours of NPO before a procedure 3. What are the cardinal signs of PD? a. Tremors b. Muscle rigidity c. Shufing gait/postural instability d. Bradykinesia 4. In the severe stages of PD, the pts arms are affected, shufing gate and they have a mask-like face. t/f a. False—in the mild stage this occurs 5. With migraines, if an aura is present, it includes visual changes, flashing lights, colors? t/f a. True 6. Generalized seizures involve both cerebral hemispheres. t/f a. True 7. In the ictal phase of a seizure, what should the nurse do frst? a. Maintain the airway by turning the pt on their side. 8. What is the preferred medicaton to admin during a seizure? a. Lorazepam 9. Status epileptcus is not a life-threatening t/f a. False 10. Viral meningits has a high fatality rate, even with tx, typically within 24-48 hours. T/f a. False—bacterial meningits is highly fatal 11. Progressive relapsing MS (PRMS) includes frequent relapses with only partal recovery. t/f a. True 12. Signs of ALS include: progressive weakness and wastng in the hands and limbs, then upper arms and shoulders. t/f a. True 13. Hyperextension is sudden and extreme movement of the head forward causing extreme flexion of the neck. t/f a. False—hyper reflecton is a sudden and extreme movement of the head forward causing extreme flexion of the neck. b. Hyperextension is an accelerated and then decelerated movement of the head. Associated with motor vehicle accidents from the rear. 14. With incomplete (paresis), the spinal cord has been damaged so at there so no innervaton below the level of injury. t/f a. False—incomplete means the ability of the spinal cord to convey messages to or from the brain is not completely lost. Some sensaton (even if faint) and movement is possible below the level of injury. 15. Autonomic dysreflexia is a sudden, potentally life-threatening occurrence in patents with SCIs. t/f a. TrueMDC4 Exam 1 Kahoots! 16. A CVA affects opposite sides of the body. t/f a. True 17. An ischemic stroke involves bleeding in and around the brain tssue. t/f a. False. A hemorrhagic stoke involves bleeding. 18. With an ischemic stroke, embolic plaques can break loose and occlude vessels. t/f a. True 19. The “thunderclap” headache is common with intracerebral hemorrhage (ICH). t/f a. False—occurs with no hemorrhage. 20. Lef hemisphere stroke, is dominant in most pts, center for language, math, and analysis. T/f a. True 21. Receptve aphasia is referred to as “Broca’s” or motor, aphasia. t/f a. False—receptve aphasia is referred toas Wernicke’s aphasia, able to speak well and use long sentences, but what is said may not make sense. b. Broca’s aphasia or expressive aphasia, partal loss of the ability to produce language (spoken, manual, or writen) 22. Nystagmus involves involuntary movements of the eyes (can be vertcal or horizontal). t/f a. True 23. Interventons for pts experiencing strokes are determined primarily by the type and extent of the stroke. t/f a. True 24. Alteplase (tPA) is primarily given for hemorrhagic stroke. t/f a. False—tPA is a clot buster, therefore it is contraindicated for bleeding disorders. 25. What is the tme for admin tPA? a. Within 3 hours. No longer than 4.5 hours afer onset of symptoms 26. What is the acronym used for quick assessment if a stroke is occurring? a. BEFAST i. B: balance; watch for sudden loss of balance ii. E: eyes; check for vision loss iii. F: face; look for an uneven smile iv. A: arm; check if one arm is weak v. S: speech; listen for slurred speech vi. T: tme; call 911 right away 27. Indirect injury involved a force produced by a blow to the head. t/f a. False—an indirect injury is a gunshot wound 28. With a closed injury, the skull is fractured/pierced by a penetratng object. t/f a. False—this would be an open injury because the skin would be broken 29. The most common secondary injuries are hypotension and hypoxia, intracranial hypertension, and cerebral edema. t/f a. True 30. What is the normal level for ICP? a. 10-15 mmHg—should not exceed 20 mmHg 31. A subdural hematoma results from arterial bleeding into the space between the dura and the inner skull. t/f a. False—this is an epidural hematoma or an extradural hematoma.MDC4 Exam 1 Kahoots! b. A subdural hematoma is venous bleeding into the space beneath the dura and above the arachnoid from a tearing of the bridging veins within the cerebral hemispheres or from a laceraton of brain tssue. 32. Chronic SDH presents within 48 hours afer impact. t/f a. False—An acute SDH presents within 48 hours afer impact; Subacute SDH presents between 48 hours and 2 week; Chronic SDH presents from 2 weeks to several months afer injury 33. Primary tumors originate within the CNS and rarely metastasize (spread) outside this area. t/f a. True 34. Benign tumors require more aggressive interventon, including surgery, radiaton, and/or chemotherapy. t/f a. False-malignant tumors require more aggressive therapy 35. Cerebral tumors involve hearing loss, nystagmus, ataxia, and dysarthria. t/f a. False—brainstem tumors involve the above s/s and more (dysphagia, hoarseness, apnea, bradycardia, hypotension b. Cerebral tumors involve headaches (most common feature), vomitng, seizure, changes in visual acuity and visual felds, diplopia, hemiparesis or hemiplegia, hypokinesia (decreased motor ability), hyperesthesia, paresthesia, decreased tactle discriminaton, aphasia, and changes in personality or behavior. 36. Cushing’s Triad indicated decreasing ICP. t/f a. False—indicates increased ICP 37. What is most important variable to assess with brain injury? a. Level of consciousness 38. As with any critcally injured patent, priority is given to maintaining a patent airway, breathing, and circulaton. t/f a. True 39. What is the frst priority of pre-op nurse? a. Witnessing informed consents—sign the consent as a witness to the signature, not to the fact that the client is informed. 40. Post op nausea and shivering occurs with local/regional anesthesia. t/f a. False—can occur with general anesthesia 41. With malignant hyperthermia, the nurse should immediately admin which medicaton IV? a. Dantrolene 42. Epidural blocks are injected into the CSF. t/f a. False—injected into epidural space 43. What is the frst priority interventon the post-op nurse should implement? a. Airway management 44. The PACU RN is assessing Aldrete scoring, what is an appropriate score for the patent to meet criteria for discharge? a. 8-10MDC4 Exam 1 Kahoots! 45. The operatng room nurse implements a “tme-out” afer the surgery/procedure. t/f a. False-implemented before the procedure to do a safety check to prevent errors 46. Dehiscence occurs when the surgical incision is separatng or splitng. t/f a. True—evisceraton is a wound opening with protrusion of internal organs 47. Phase 3 of post-op occurs immediately afer surgery a. False—phase 1 is immediately afer surgery and includes stabilizing the airway, manage pain, oral intake, and discontnue or adapt IVs Extra Kahoots! 1. All the following foods should be avoided for migraine sufferers except: a. Beef b. Avoid: yogurt, caffeine, and marinated foods 2. The nurse would expect to see improvement in what with the use of levodopa for PD? a. Muscle rigidity 3. Ergotamine tartrate medicatons help in migraine headaches due to dilaton of cerebral blood vessels. t/f a. False—this med helps narrow or constrict already dilated blood vessels. b. This is an abortve medicaton that is taken at the start of the headache in order to stop it from progressing 4. What queston should you ask a patent prior to the patent having a CT scan with contrast? a. “Do you have an allergy to seafood or iodine?” 5. What educaton is important to prevent autonomic dysreflexia for a patent with a comminuted fracture of t6-t7? a. Bowel/bladder training 6. What is the period of rest afer a tonic-clonic seizure? a. Postctal 7. A lumbar puncture should be avoided in a patent with a possible head injury afer a motor vehicle accident. t/f a. True 8. All of the following are a part of Cushing’s Triad except: a. Decreased blood pressure b. Cushing’s Triad include: bradycardia, widened pulse pressure, increased systolic blood pressure 9. If the nurse notces drainage from the head injury from patents nose and ears, what is important to teach the patent? a. You can wipe nose/ears, but do not blow nose or place anything in ear. 10. What is the term for total or partal loss of the ability to recognize familiar objects or people? a. Agnosia 11. IV immune globulin is used to increase producton of acetylcholine antbodies in Myasthenia Gravis. t/f a. False—used for tx of Guillain-Barre Syndrome (GBS) 12. What is the inability to assess the spatal positon of one’s own body? a. Propriocepton 13. All of the following seizure precautons should be used except:MDC4 Exam 1 Kahoots! a. Padded tongue blade available (don’t stck anything in the patent’s mouth) b. Precautons should include: sucton equipment at bedside, keep bed rails up and padded, and ensure patent has IV access. 14. If the nurse notces the patent is experiencing tachycardia, diaphoresis, and rising body temp during surgery… a. He/she should alert the anesthesiologist and surgeon immediately. Signs of malignant hyperthermia. 15. The circulatng nurse is responsible for verifying that the consent form is signed and surgical site is marked. t/f a. True 16. What interventon should the nurse antcipate for a wound evisceraton prior to receiving order from the provider? a. Apply warm, moist normal saline sterile dressing 17. A patent experiencing dyspnea, cyanosis, and tachycardia may be experiencing what complicaton of surgery? a. Pulmonary embolus 18. A fnding f 7 or less on the Glasgow coma scale indicates a coma. a. True. A score of 8 is coma. 19. The nurse would expect to see what effect of the use of baclofen in a patent with MS? a. Reducton of muscular spastcity 20. The nurse must observe for the risk of aspiraton in patent with myasthenia gravis. t/f a. True 21. What interventon can help reduce the risk of increased ICP in a patent with bacterial meningits? a. Elevate head of bead as high as tolerated to reduce the pressure going to the head. 22. A patent with AD is considered in early stages when they exhibit wandering, anger, and visuospatal defcits. t/f a. False. This occurs in the moderate stage of AD. The early stage includes minor memory loss, long term memory and reasoning is typically intact, forget where common items are kept. 23. Progressive proximal to distal muscle weakness and mild diplopia are seen in patent with MS. t/f a. False. These signs are seen in patents with myasthenia gravis. 24. What category of medicatons are typically given to patents actvely experiencing a seizure? a. Benzodiazepines 25. A patent with weakness and tngling in feet and legs and spreads to the upper body is seen in GBS. t/f a. True 26. If the nurse notces a clear drainage from the patent’s nose with a “halo sign,” what should he/she do next? a. Check the presence of glucose in drainage and report to provider. 27. What is the nurse’s role for a patent that is a probable organ donor? a. Maintain perfusion and care for the patent to maintain organs for harvest. 28. Most embolic stroke occur due to blood clots that come from the heart. t/f a. TrueMDC4 Exam 1 Kahoots! 29. Besides tme of onset, what is important to assess in a patent that presents with slurred speech and weakness? a. Blood glucose 30. Phenytoin should only be taken during a seizure. t/f a. False 31. What is another name for CVA? a. Stroke 32. What is the name of the tool used to assess for stroke? a. NIH Stroke Scale 33. Identfy all types of strokes: a. Ischemic b. Transient ischemic atack c. Hemorrhagic 34. Family history, htm, dm, EtOH/illicit drug use, high-fat diet, atherosclerosis, and aneurysm/AVM are risk factors for: a. Stroke 35. Select the ischemic stroke subtypes: a. Embolic stroke and thrombotc stroke 36. Select the subtypes of hemorrhagic stroke: a. Intracerebral and subarachnoid hemorrhage 37. Select the imaging studies used for diagnosis of stroke a. CT with contrast, MRI with Contrast (MRA), and Ultrasound 38. Which is an absolute contraindicaton for tPA? a. Hemorrhagic stroke 39. Changes in LOC, pupils, posturing, seizures, slurred speech, vomitng, and decreased motor functon are s/sx of: a. Increased ICP 40. Acceleraton injury is caused when the head stops moving suddenly. t/f a. False—acceleraton injury is caused by movement of the brain within the unrestrained head. Example whiplash injury 41. What are the TBI risk factors? a. Men, EtOH, and illicit drug use 42. A patent with a TBI has nonreactve dilated pupils. What would the nurse antcipate? a. Brain stem herniaton 43. Which symptom is the earliest indicator of increased ICP in a patent with a head injury? a. Agitaton and confusion 44. A patent has experienced a stroke in the LEFT cerebral hemisphere. What s/sx does the nurse expect? a. Aphasia, agraphia, and acalculia (loss of ability to perform simple arithmetc calculatons) 45. Which food allergy indicates a sensitvity to CT contrast dye? a. Shellfsh 46. When caring for a patent with a potental stroke, what are the important nursing consideratons? a. AirwayMDC4 Exam 1 Kahoots! b. Blood pressure c. Blood sugar 47. How are ergotamine medicatons benefcial in migraine headaches? a. Constrict cerebral blood vessels 48. A priority nursing interventon for seizure management is a. Protect the patent from harm; safety 49. s/sx of PD include the following: a. shufing gait b. mask-like face c. bradykinesia 50. migraine triggers include a. Foods, fastng, nicotne, hormonal changes, and oral contraceptves b. Changes in physical actvity, stress, sleep paterns c. Exposure to polluton, chemical, perfumes, flashing lights 51. All of the following are benefts of patent controlled analgesia: a. Patent is more satsfed and improved pain control b. Faster absorpton and more predictability c. Consistent blood levels are maintained d. Do not let family member assist the patent in using it. 52. What is the difference between quadriplegia and paraplegia? a. It depends where in the spinal cord the injury occurred. Paraplegia cant use their lower extremites. Quadriplegia cannot use any of their extremites. 53. The best interventon for the postctal period is to: a. Allow the patent to rest 54. What is not a component of the Glasgow Coma Scale? a. Pain response b. Components include i. Motor response, verbal response, and eye response. 55. Once you have completed your surgical scrub, what is the next step? a. Hands above waist, dry with sterile towel. 56. What are the treatments for a stroke? a. Surgical tx, IV fluids, rest, and thrombolytc therapy (depending on the type of stroke) 57. You are caring for a pt with dysphasia, what related conditon would you assess for? a. Aspiraton pneumonia 58. Which of these is a complicaton of a lumbar puncture? a. Spinal headache 59. What is a late sign of increased ICP? a. Cushing’s Triad 60. Which symptoms are associated with Cushing’s Triad? a. Widening pulse pressure and bradycardia b. Increased systolic BP, decreased pulse, decreased respiratons i. Symptoms of increased ICP are opposite of shock (decreased bp, increased pulse, and increased respiraton) 61. Who is responsible for explaining and making sure a surgical consent is obtained?MDC4 Exam 1 Kahoots! a. The surgeon 62. When is malignant hyperthermia likely to occur? a. Intraoperatvely 63. Which of these is NOT a sign or symptom of malignant hyperthermia? a. Hypothermia b. s/sx include tachycardia, masseter muscle rigidity, and increased ETCO2 64. Regional anesthesia includes: a. spinal, nerve block, and epidural 65. the types of general anesthesia are: a. Inhalaton and Intravenous 66. An abdominal evisceraton should be managed with: a. A moist, sterile, large bulky dressing 67. Which of the following factors places a client at risk for pulmonary embolism? a. Total hip arthroplasty 68. Baclofen increases and manages what? a. Mobility and muscle spasms 69. Broca’s aphasia means: a. Speech is slow, laborious and lacks fluency 70. Which are true about tonic-clonic seizures? a. There is contracton of all muscles at one, incontnence may occur, and there is loss of consciousness 71. Seizures and epilepsy are the same thing. t/f a. False—epilepsy is a seizure disorder. You can have seizures without having epilepsy but you cannot have epilepsy without having seizures. 72. Potental causes for seizures include all of the following: a. Severe head injury or stroke b. Severe infectons and high fever c. Complicaton caused by diabetes 73. Which system does PD affect? a. Nervous system 74. S/Sx of PS include: a. Shufing gait, mask-like face, and bradykinesia 75. What is Multple Sclerosis? a. Immune system eats the protectve covering of nerves making it difcult for nerves and muscles to communicate 76. Is there a cure for AD? a. No, there are only treatments 77. What is epilepsy a. A disrupton of the brain that interrupts normal actvity 78. what is paraplegia? a. Paralysis from the waist down 79. George has just has a seizure and is now in the postctal period. Which od the following nursing cares are correct? a. Maintain airway, check vital signs, reassure patentMDC4 Exam 1 Kahoots! 80. The Glasgow Coma Scale assesses: a. Eye response, best motor response, and best verbal response 81. Hemiplegia a. Paralysis on one side of the body 82. Lumbar puncture is used to diagnose: a. Encephalits 83. Cushing’s Triad consists of a. Hypertension b. Bradycardia c. Irregular respiratory rate 84. Agnosia is the inability to a. Process sensory input 85. Apraxia is defned as a. Inability to perform familiar movements on demand 86. Aphasia is: a. Inability to understand or produce language 87. Dysphagia is a. Difculty swallowing 88. What is propriocepton a. Awareness of your body’s positon in space 89. Bell’s Palsy symptoms a. Drooping side of face b. Facial paralysis 90. Symptoms of trigeminal neuralgia may include all of the following: a. Extreme, intermitent facial pain in jaw or cheek b. Tingling or numbness on one side of the face c. Pain triggered by contact with the face or facial movements Dr. Fitzgerald Kahoot 1. Triptans and ergotamine preparatons are contraindicated in: a. Coronary disease because these drugs vasoconstrict vessels, and can lead to heart atack or stroke b. These meds are given for migraines 2. Sucton, O2, passed side rails, and a tongue blade are part of seizure precautons. t/f a. False. No tongue blade. Nothing goes in their mouth. They can aspirate by bitng down on the tongue blade. b. Other things we want is IV access, bed in lowest positon. 3. What is it called when a patent comes in with a seizure that lasts for more than 5 min or has multple seizures back-to-back in a 30-minute period? a. Status epileptcus—medical emergency 4. What is the frst drug you MUST administer if your patent is in status epileptcus? a. Lorazepam or other benzodiazepine—goal is to stop the seizure, afer it is stop, give them their antseizure medicaton (Dilantn)MDC4 Exam 1 Kahoots! b. Antseizure medicaton can deactvate birth control—educaton patent of childbearing age 5. Afer the seizure, what positon do we place the patent in? a. On their side (recovery positon) in case they throw up to prevent aspiraton 6. Educaton for patents going home on antseizure medicatons a. Take them on tme b. Take them regularly c. Do not stop them d. Do not drive untl you fnd out the cause of the seizures and seizures are reportable to the DMV because it is a public safety risk. 7. Bradykinesia, muscle rigidity, mask-like face are clinical manifestatons of: a. Parkinson’s Disease i. Chronic disease ii. Some concerns 1. Falls 2. Aspiraton if trouble swallowing iii. Not curable iv. Meds to treat the symptoms, possibly slow progression. 8. Tonic-clonic seizure a. Tensing of muscles, convulsions b. Priority to keep patent safe, get them to the floor. 9. What is it called when the patent knows that they are about to have a seizure? a. An aura. Ex: someone’s aura is that they can smell fresh baked cookies every tme they are about to have a seizure. This is their cue. b. People with migraines also get an aura 10. Period afer the seizure where they may be sleeping, confused, or hard to arouse? a. Postctal phase common in tonic-clonic 11. Multple sclerosis risk factors a. Female, 20-40 years old b. May show up with different signs and symptoms depending on which area is affected c. Could be autoimmune. Can put them on immunosuppressants or cortcosteroids which puts them at risk for infecton. d. Treat symptoms, if they have depression, give antdepressants, if they have incontnence, give them straight cath, or indwelling catheter. If functon incontnence, educate about elastc waist bands. e. Give them support because this is a chronic disease and they need to know how to manage their disease at home. Educate about periods of exacerbaton. Know what can cause these exacerbaton (infecton, weather—being overheated) 12. What is Guillain-Barre Syndrome? a. Ascending paralysis b. Acute inflammatory disease c. Seen afer exposure to viral infectons (about 2-4 weeks) 13. what system worries us the most about GBS?MDC4 Exam 1 Kahoots! a. Respiratory system. May need to be intubated to support their airway as paralysis ascends upward. 14. What medicaton can be used if MS causes muscle spasms? a. Baclofen—antspasmodic 15. Clients with migraines should avoid: a. Foods high in tyramine i. Marinated foods, fermented foods (yogurt), caffeine, red wine, MSG b. Ask patent to keep a food diary/log to help determine the causatve agent of the migraine c. Stay hydrated 16. Highest priority during the postoperatve period is: a. Monitor airway and O2 saturaton 17. What can ambulaton help with postoperatvely? a. Prevent clots, help to pass gas and relieve associated pain 18. If patent comes out of surgery with PCA morphine a. Teaching point: only the client can push the buton! 19. Patent with a t6 fracture develops a sudden headache, what conditon do you suspect? a. Autonomic dysreflexia i. Sudden increase in blood pressure, may feel stuffy or have redness in their face ii. Causes 1. Full bladder 2. Tight clothes 3. Irritaton to the area below injury 4. Constpaton 5. UTI iii. Primary interventon 1. Sit the patent up (to decrease the pressure in the head) and then fnd and fx the cause 20. Reinforcement of postoperatve instructons can be delegate to the UAP. t/f a. False—not within their scope b. LPN can reinforce. c. UAP can: i. Toiletng, bathing, feeding, bathroom needs, feeding if they can swallow and is not a new stroke pt, vitals if stable, emptying catheter, I&O, ADLs, hygiene 21. The Glasgow coma scale evaluate all the following: a. Motor response b. Eye opening c. Verbal response d. Values: i. 3-15 ii. Anything less than 8, the patent is in a coma iii. If there is a change in the patent for the worse, we need to let the provider know. 22. Earliest sign of increased ICP:MDC4 Exam 1 Kahoots! a. Decreased level of consciousness 23. Priority nursing concerns during the intraoperatve period include: a. Safety and infecton control b. Before they go to surgery, it is important to know how long they have been NPO c. Preop: consent and labs will be done d. Postop: wound assessment and dressing changes 24. If patent is going to cath-lab with contrast, be aware of: a. Allergy to shellfsh and iodine b. Know kidney functon and monitor i. BUN and creatnine c. If client is on metormin, try to hold for about 48 hours before and 48 hours afer. 25. Client with a stroke requires a consult from a speech language pathologist. t/f a. True—make sure the patent can swallow, do evaluaton frst to prevent aspiraton. 26. What can patent be allergic to if they are allergic to latex a. Avocados, strawberries, kiwi, bananas 27. If client with latex allergy has to go to surgery, when do we schedule them to go? a. First thing in the morning 28. Nursing diagnoses for preop patent a. Risk for anxiety b. Knowledge defcit 29. What is your concern if patent receives sedatves or any pain medicaton? a. They cannot sign the consent while under the influence of these drugs. b. Always get consent before giving any medicatons that cause sedaton 30. Level of consciousness in preop afer medicatons were given: a. Patent is at risk for falls 31. What are some things that can be done to prevent aspiraton in stroke patents? a. Tuck the chin in, thicken fluids as indicated, sit up right 90 degrees, small bites of foods, give them tme to chew and swallow, ask to double swallow, take distractons away, check mouth for food pockets 32. If patent has lef sided weakness, what side do we give them food? a. Right side, the unaffected side 33. Homonymous hemianopsia a. Can only see half of their visual feld on both sides. 34. Clear drainage from the nose and ears of a head injury client should be tested for WBC. t/f a. False—test blood glucose or halo test. b. Positve glucose is indicatve of CSF c. Halo present is indicatve of CSF 35. If patent had brain injury or surgery, what do we tell them not to do to minimize the risk of IICP? a. Do not cough, blow your nose, or strain (may need stool sofener), no bending over, try not to sneeze, no vagal maneuver, do not bare down b. Positon that is contraindicated for increased ICP i. Supine positon 36. Interventons for a client with increased ICP include: a. Maintain head in neutral positonMDC4 Exam 1 Kahoots! b. Decrease stmuli, want a calm environment c. Sucton only as needed d. Elevate head of bed to about 30 degrees or as tolerated. 37. IICP diagnostc is contraindicated a. Lumbar puncture—can cause herniaton b. Late changes that indicate herniaton of the brain i. Changes in pupils 1. Blown, non-responsive 38. Cushing’s Triad a. Systolic hypotension, bradycardia, irregular respiratons (breath really fast, have periods of apnea, then go back to breathing really fast=Cheyne-stokes respiratons), widened pulse pressure 39. Inability to speak and/or understand language a. Aphasia 40. Agnosia a. Losing the ability to recognize familiar objects or people through sensory stmulaton 41. Propriocepton a. In space b. Patent closes their eyes, we move their hand, and we ask them if we moved it up or down, they should be able to tell. 42. MG is an autoimmune disorder that causes ascending paralysis. t/f a. False—GBS is ascending. Diagnose MG with tensilon test. 43. Bell’s Palsy can sometmes be confused with a. Stroke b. Will have weakness on one side of face, cant close eye, cant wrinkle forehead, unilateral involvement c. Diagnostc to rule out a stroke: CT without contrast (get it one fast. No tme for IV access) looking for blood (hemorrhagic or ischemic). If not hemorrhagic patent is a candidate for thrombolytc therapy. For TPA, consider tme of onset. 44. Clinical manifestatons of trigeminal neuralgia a. Sharp, extreme pain, unilateral 45. A client with conscious/moderate sedaton must have a breathing tube in place. t/f a. False—the patent can maintain their away, pt is reactve b. This sedaton can be used for endoscopy, bronchoscopy at bed side. c. General anesthesia requires intubaton d. Drugs needed for anesthesia: propofol (if allergic to eggs, soy, and peanuts, you may be allergic to propofol) i. Anesthetc (inhaled or injected), paralytc, and analgesic e. Client needs airway protected f. Complicaton that can happen with general anesthesia i. Malignant hyperthermia 1. High temp, hyperkalemia, acidosis, diaphoresis, medical emergency 2. Medicaton: dantrolene! 3. Ice to pack the patentMDC4 Exam 1 Kahoots! 46. Timeout will be called by the circulatng nurse. This nurse is not sterile. This nurse is responsible for making sure pt is safe, making sure we do the tmeout procedure, the equipment is working, and controls movement in and out of OR. 47. Scrub nurse is sterile. Can touch the sterile feld and pass instruments to the surgeon. 48. What are some things that we will do postop to prevent complicatons afer surgery? a. IS to prevent atelectasis b. SCD, ted hose, lovonox to prevent DVT and PE c. Early ambulaton d. Check gag reflex before you feed so they do not develop aspiraton e. Vital signs f. I&O g. Monitor wound for drainage 49. What 2 conditons are referred to as VTE a. Venous thromboembolism i. PE and DVT b. What signs are present with PE i. Chest pain, SOB, low O2 sat, tachycardic, low bp, feeling of impending doom. 50. TPA can be administered to a patent with a hemorrhagic stroke. t/f a. False—this is a contraindicaton b. If patent is bleeding, do not give thrombolytcs 51. If pt has an ischemic stroke, and we are going to give alteplase or tPA, what vital sign are we needing to keep a close eye on? a. Blood pressure 52. Modifable risk factors for stroke a. Diet, smoking, exercise, weight, actvity level, sedentary lifestyle, obesity, HTN, Diabetes, and hyperlipidemia, CAD 53. Clients with what heart conditon can develop an ischemic stroke? a. Atrial fbrillaton 54. What type of stroke (ischemic or hemorrhagic) do patents come in complaining of the worst headache of their life? a. Hemorrhagic 55. What can patents develop before they have an ischemic stroke (may occur weeks or months before the stroke)? a. TIA i. Neurological defcits that may last for seconds up to 24 hours and is a sign that they may have an ischemic stroke in the future. 56. Clients with Alzheimer’s Disease can present with: a. Wandering—occurs in the moderate stage. Puts them at risk for safety concerns b. Clients do not die of Alzheimer’s. They die WITH Alzheimer’s. c. Alzheimer’s is not curable. Meds are used to manage the symptoms. i. May slow down the progression but cannot reverse. d. May become very angry, have periods of incontnence. 57. Clinical manifestatons for meningits a. Nuchal rigidity, headache, photosensitvity,MDC4 Exam 1 Kahoots! b. Droplet precautons as soon as patent presents with these symptoms. c. If bacterial, start on abx as soon as possible. 58. What can a client develop with meningits? a. Increased ICP (also a complicaton of strokes) 59. What type of shock is a patent with spinal cord injury at risk for? a. Neurogenic shock i. S/s: low bp and slow heartrate b. Spinal shock i. S/s: lose reflexes at or below the injury c. Autonomic dysreflexia is complicaton i. Make sure bowel and bladder are empty 60. What are you worried about if your client has a cervical injury? a. Respiratory problems. [Show More]
Last updated: 1 year ago
Preview 1 out of 15 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 21, 2022
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Nov 21, 2022
Downloads
0
Views
43

 (4).png)
.png)