NR 341 Chapter 26 QUIZ | VERIFIED SOLUTION
Document Content and Description Below
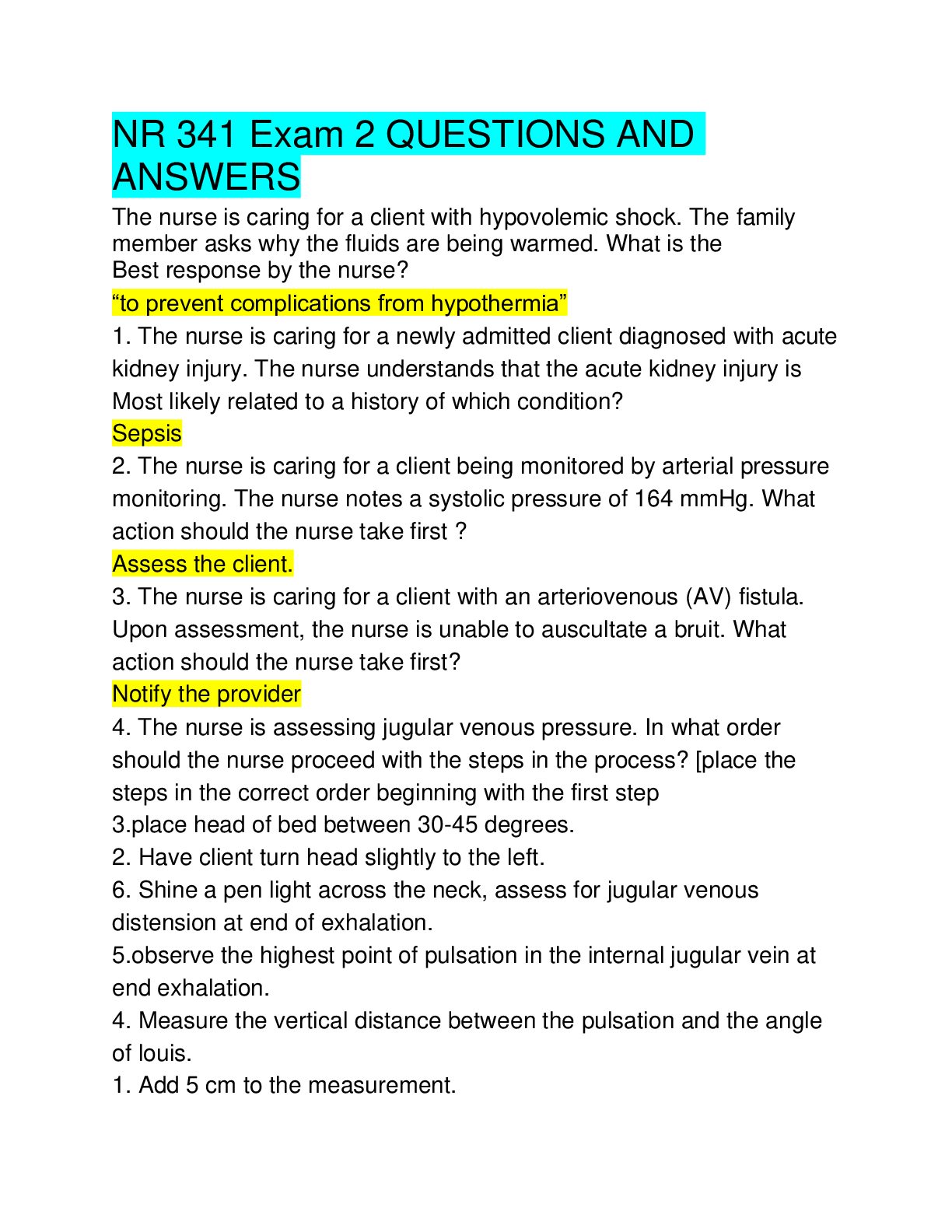
1. The nursing instructor is explaining cardiac function to the senior nursing class. The instructor explains that blood is ejected into circulation as the chambers of the heart become smaller. The in... structor categorizes this action of the heart as what? A) Systole B) Diastole C) Hypertension D) Ejection fraction 2. During a shift assessment, the nurse is assessing the point of maximum impulse (PMI). Where will the nurse best palpate the PMI? A) Left midclavicular line of the chest wall at the seventh intercostal space B) Left midclavicular line of the chest wall at the fifth intercostal space C) Right midclavicular line of the chest wall at the seventh intercostal space D) Right midclavicular line of the chest wall at the fifth intercostal space 3. The instructor is teaching the beginning nursing class how to calculate pulse pressure. If the patient's systolic pressure was 122 mm Hg and the diastolic pressure was 75 mm Hg, what would the pulse pressure be? A) 57 B) 60 C) 54 D) 47 4. The nurse is caring for a patient admitted with unstable angina. The laboratory result for the initial troponin I is elevated in this patient. The nurse recognizes what? A) This is only an accurate indicator of myocardial damage when it reaches its peak in 24 hours. B) Because the entry diagnosis is unstable angina, this is a poor indicator of myocardial injury. C) This is an accurate indicator of myocardial injury. D) It is only an accurate indicator of skeletal muscle injury. 5. You are conducting patient teaching about cholesterol levels in the body. When discussing the patient's elevated LDL and lowered HDL levels, the patient shows an understanding of the significance of these levels by stating what? A) “Increased LDL and decreased HDL increase my risk of coronary artery disease.” B) “Increased LDL and decreased HDL decrease my risk of coronary artery disease.” C) “The decreased HDL level will increase the amount of cholesterol moved away from the artery walls.” D) “The increased LDL will decrease the amount of cholesterol deposited on the artery walls.” 6. The physician has placed a central venous pressure (CVP) monitoring line in your patient so assessments can be made on right ventricular function and venous blood return. The results show a decreased central venous pressure. What does this indicate? A) Possible hypovolemia B) Possible hypervolemia C) Right ventricular failure D) Left ventricular failure 7. The nurse is caring for a patient with heart failure. While auscultating heart sounds of this patient, the nurse hears an extra heart sound immediately after the second heart sound (S2). How would the nurse document this? A) A first heart sound (S1) B) A third heart sound (S3) C) A fourth heart sound (S4) D) A murmur 8. The physical therapist notifies the nurse that a patient with coronary artery disease (CAD) experiences an increase in heart rate during physical therapy at the bedside. The nurse recognizes that an increase in heart rate in a patient with CAD may result in what? A) Increased myocardial perfusion B) Myocardial ischemia C) Formation of a pulmonary embolism D) Electrolyte imbalances 9. The nurse assesses the patient and records the data collected. What would lead the nurse to anticipate that the patient will experience a decrease in cardiac output? A) An order for the patient to receive digoxin B) A heart rate of 54 beats per minute C) A pulse oximetry reading of 98% D) An increase in preload related to ambulation in the hall 10. You are caring for an 82-year-old patient. You know that changes in the cardiac structure and function occur in the heart of an older adult. What is a normal change expected in the aging heart of an older adult? A) Decreased left ventricular ejection time B) Decreased connective tissue in the SA and AV nodes and bundle branches C) Thinning and flaccidity of the cardiac values D) Widening of the aorta 11. You are on triage duty in the emergency department (ED) when a patient presents to the ED with symptoms indicative of a myocardial infarction (MI). The patient informs you that these symptoms have been occurring over the last 4 to 5 days. Which diagnostic study do you expect the physician to order to diagnosis an MI? A) Myoglobin levels B) Creatine kinase (CK) and its isoenzyme CK-MB C) Troponin T and I D) Lactic dehydrogenase and its isoenzymes 12. The critical care nurse is caring for a patient with a central venous pressure (CVP) monitoring system. The nurse notes that the patient's CVP is increasing. What may this be indicative of? A) Hypovolemia B) Hypervolemia C) Hypermagnesemia D) Hypomagnesemia 13. The critical care nurse is caring for a patient with a pulmonary artery pressure monitoring system. The nurse is aware that pulmonary artery pressure monitoring is used to assess left ventricular function (cardiac output.) What else are pulmonary artery pressure monitoring systems used for? A) To assess the patient's response to interventions such as fluid administration and drug administration B) To obtain specimens for arterial blood gas measurements C) They have been determined to not be clinically useful for continuous monitoring of a patient with heart failure D) To diagnose the etiology of chronic obstructive pulmonary disease 14. The student nurses are studying the conduction system of the heart. The instructor explains that the electrical conduction of the heart usually originates in the SA node. Which sequence completes the conduction? A) SA node to Bundle of HIS to AV node to Purkinje fibers B) SA node to AV node to Purkinje fibers to Bundle of HIS C) SA node to bundle of HIS to Purkinje fibers to AV node D) SA node to AV node to bundle of HIS to Purkinje fibers 15. Your patient has had a myocardial infarction and has been diagnosed as having damage to the layer of the heart responsible for the pumping action. You are aware that the damage occurred where? A) Endocardium B) Pericardium C) Myocardium D) Visceral pericardium 16. The nurse working on a cardiac care unit is caring for a patient whose stroke volume has increased. The nurse is aware that afterload influences a patient's stroke volume. The nurse recognizes that afterload is increased when there is what? A) Arterial vasoconstriction B) Venous vasoconstriction C) Arterial vasodilatation D) Venous vasodilatation 17. In preparation for a transesophageal echocardiography, the nurse must A) instruct the patient to drink 1 liter of water before the test. B) heavily sedate the patient. C) inform the patient that blood pressure (BP) and electrocardiogram (ECG) monitoring will occur throughout the test. D) inform the patient that an access line will be initiated in the femoral artery. 18. You are caring for a patient admitted with angina who is scheduled for a cardiac catheterization. The patient is anxious and asks you about the reason for this test. What is your best response? A) “A cardiac catheterization is most commonly done to assess coronary artery patency.” B) “A cardiac catheterization is most commonly done to detect myocardial ischemia.” C) “A cardiac catheterization is most commonly done to evaluate cardiovascular response to stress.” D) “A cardiac catheterization is most commonly done to evaluate cardiac electrical activity.” 19. You are a critical care nurse caring for a patient who has suffered an MI. You know that the most appropriate hemodynamic monitoring procedure to assess the left ventricular function of a patient who has suffered an MI would be what? A) CVP monitoring B) Pulmonary artery pressure monitoring (PAPM) C) Systemic arterial pressure monitoring (SAPM) D) Arterial blood gases (ABG) 20. A critically ill patient is admitted to the ICU. The physician decides to use intra-arterial pressure monitoring. What is the purpose of this? A) To assess left ventricular function B) To assess the pressure of the vena cava C) To assess the pressure in the right atrium D) To measure the patient's BP continually 21. How is hemodynamic monitoring achieved? A) Noninvasive monitoring systems B) Extracorporeal monitoring systems C) Direct pressure monitoring systems D) Partial pressure monitoring systems 22. A patient is brought into the emergency department (ED) by family members who tell the nurse the patient grabbed his chest and complained of substernal chest pain that feels like something is sitting on his chest. The pain radiates to the jaw and the left shoulder. The nurse notes the patient is diaphoretic and short of breath. What is the nurse's priority action? A) Notify the physician of a probable MI B) Take vital signs C) Give sublingual nitroglycerin D) Administer oxygen 23. The nursing instructor is talking to her clinical group about taking an intake assessment on a patient with coronary artery disease. What would be an important determination to make during this intake assessment? A) If the patient and involved family members understand the discharge medications and regimen B) If the patient and involved family members understand nutrition C) If the patient and involved family members are able to recognize symptoms of an acute cardiac problem, such as ACS or HF, and seek timely treatment for these symptoms D) If the patient and involved family members understand the teaching done on exercise and dietary modifications 24. The synchronization of the atrial and ventricular events is the topic of the prenursing physiology class today. What are the physiologic characteristics of the nodal and Purkinje cells that provide this synchronization? (Mark all that apply.) A) Loop connectivity B) Excitability C) Automaticity D) Conductivity E) Independence 25. What is the terminal point in the conduction system of the heart? A) Purkinje fibers B) AV node C) Bundle of HIS D) Nodal cells 26. You are caring for a 77-year-old patient who was admitted to your unit with vital fatigue and shortness of breath. What could be a presumptive diagnosis for this client? A) Acute MI B) Acute coronary syndrome C) Chronic coronary syndrome D) Syncope 27. The nursing students are learning about diagnostic tests for cardiovascular disease (CVD). One blood test related to CVD is a lipid profile. When should a lipid profile be drawn to get accurate results? A) After an 8-hour fast B) After a meal high in fat C) After a 12-hour fast D) After a large meal 28. When hemodynamic monitoring is ordered for a patient, a catheter is inserted into the appropriate blood vessel or heart chamber. It is then connected to a pressure monitoring system that includes what? (Mark all that apply.) A) A transducer B) A flush system C) A leveler D) A pressure bag E) An oscillator 29. The critical care nurse is caring for a client with bradycardia after cardiovascular surgery. The nurse knows that the heart rate is determined by myocardial cells with the fastest inherent firing rate. Under normal circumstances where are these cells located? A) SA node B) AV node C) Bundle of HIS D) Purkinje cells 30. The nurse is doing discharge teaching with a patient with coronary artery disease. The patient asks why he has to take an aspirin every day if he doesn't have a headache. What would be the nurse's best response? A) “Taking an aspirin every day is an easy way to prevent plaque build-up in the arteries.” B) “An aspirin a day is a common nonprescription medication that improves outcomes in patients with CAD.” C) “Taking an aspirin every day really isn't necessary. It just makes some patients feel like they are doing something to help themselves.” D) “An aspirin a day is an easy way to help yourself feel better.” 31. The physician has ordered an hs-CRP drawn on his patient. The results of the test are 1.75 mg/dL. The nurse would know that this patient has what risk for CVD? A) High B) Moderate C) Low D) None 32. The patient has a homocysteine level ordered. What should the nurse know about laboratory results for homocysteine levels? (Mark all that apply.) A) A 12-hour fast is necessary before drawing the blood sample. B) A diet low in vitamin B6 can depress homocysteine levels. C) Genetic factors can elevate homocysteine levels. D) A diet low in folic acid elevates homocysteine levels. E) An 8-hour fast is necessary before drawing the blood sample. 33. What part of an ECG is used to identify the presence of myocardial ischemia or injury? A) ST segments B) QRS complex C) Inverted P wave D) D PVC 34. A critical care nurse is caring for a patient with a hemodynamic monitoring system in place. What complications should the nurse assess for? (Mark all that apply.) A) Pneumothorax B) Infection C) Hemorrhage D) Hemothorax E) Air embolism 35. Your patient has a CVP in place. When you assess your patient, you find that the pressure demonstrated by the CVP is 7 mm Hg. You know that normal pressure in the right atrium is what? A) 2 to 3 mm Hg B) 2 to 4 mm Hg C) 2 to 6 mm Hg D) 2 to 7 mm Hg 36. A critical care nurse is caring for a patient with a pulmonary artery catheter in place. What does this catheter measure that is particularly important in critically ill patients? A) Pulmonary artery systolic pressure B) Right ventricular afterload C) Pulmonary artery pressure D) Left ventricular preload 37. A new nurse on the cardiac unit is taking a class in the anatomy and physiology of the heart. What does the nurse learn is the cardiac action potential? A) The cycle of depolarization and repolarization B) The time it takes from the firing of the SA node to the contraction of the ventricles C) The time between the contraction of the atria and the contraction of the ventricles D) The cycle of the firing of the AV node and the contraction of the myocardium 38. A patient is brought to the emergency department by paramedics for a dysrhythmia. When the patient is placed on the cardiac monitor, the pervading rhythm is a premature ventricular contraction (PVC) every other beat. The nurse knows that a PVC is caused by what? A) Late repolarizations of the atrium of ventricle B) Early depolarizations of the atrium or ventricle C) Early firing of the AV node D) Late firing of the SA node 39. The student nurse is making a teaching plan for a patient being discharged status post MI. What should the student include in the teaching plan? (Mark all that apply.) A) The need for careful monitoring B) The need for exercise C) The need for dietary modifications D) The need for psychological support groups E) The need for daily weight loss 40. You are caring for a patient admitted with a myocardial infarction. While you are doing the admission assessment, the patient asks you for a laxative. The patient tells you he suffers from constipation. What would you teach this patient to do to help his constipation? A) Take a mild laxative every day B) Drink prune juice every day C) Establish a nutritious diet D) Don't strain during defecation [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$14.00
Document information
Connected school, study & course
About the document
Uploaded On
Feb 08, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Feb 08, 2021
Downloads
0
Views
32