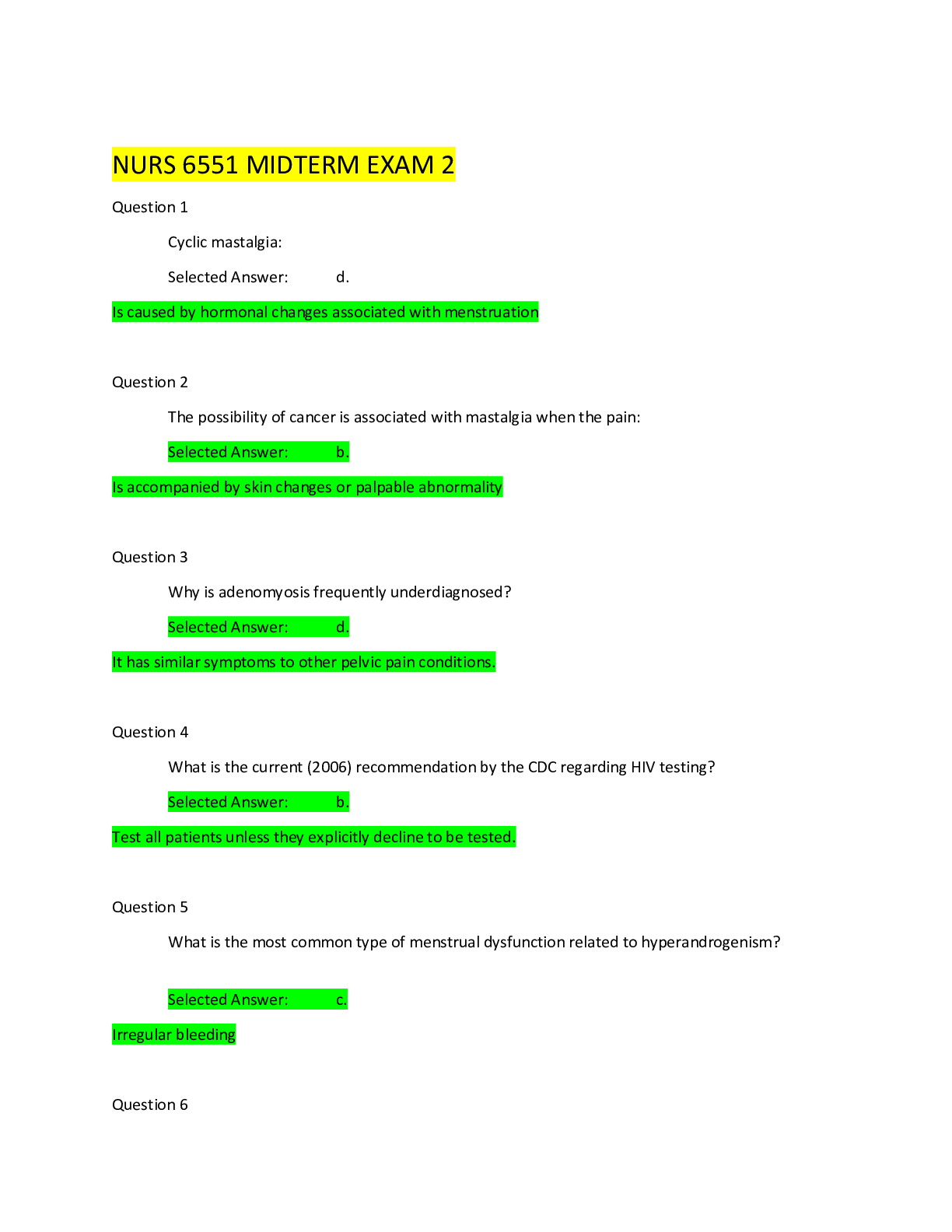
NR 304 Final Worksheet Questions And Answers
Document Content and Description Below
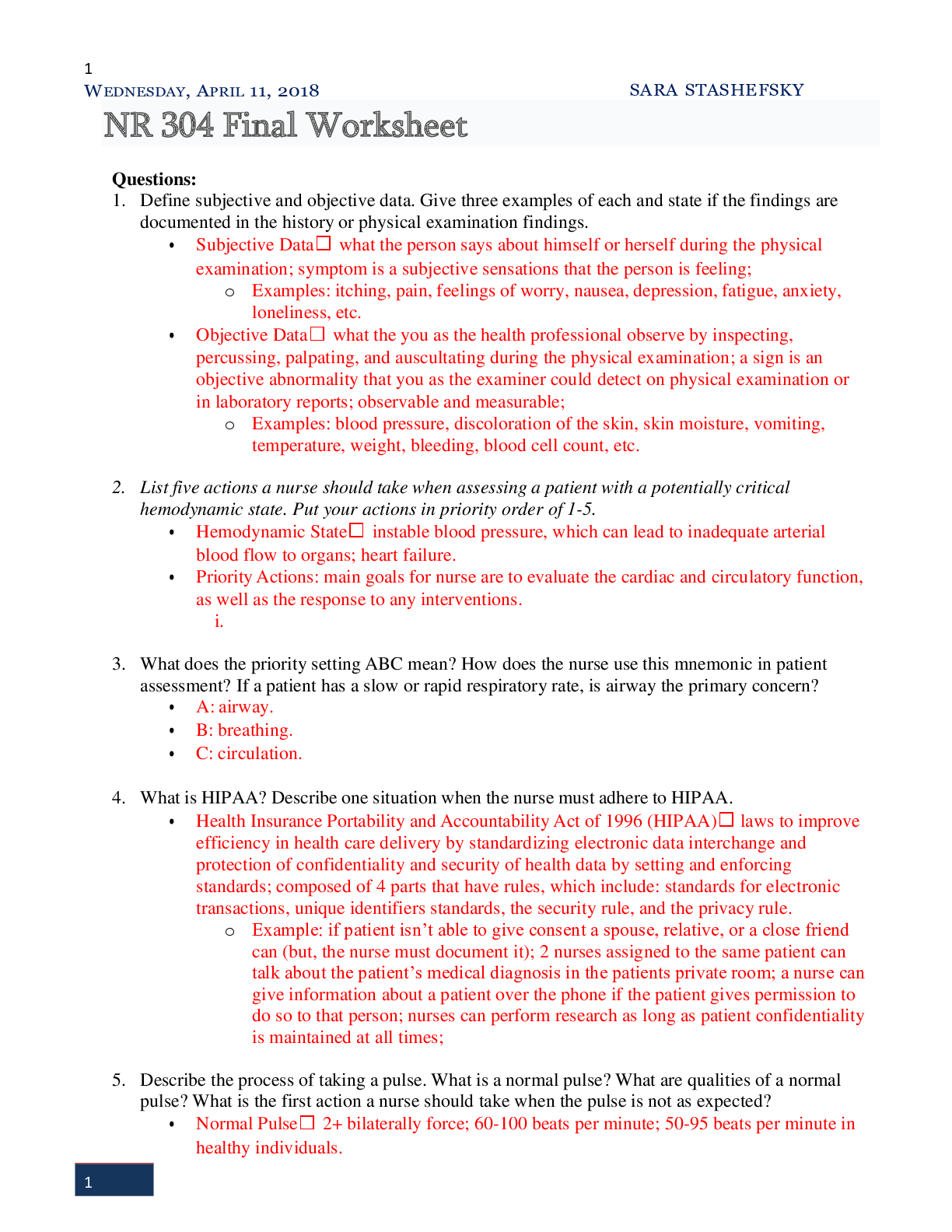
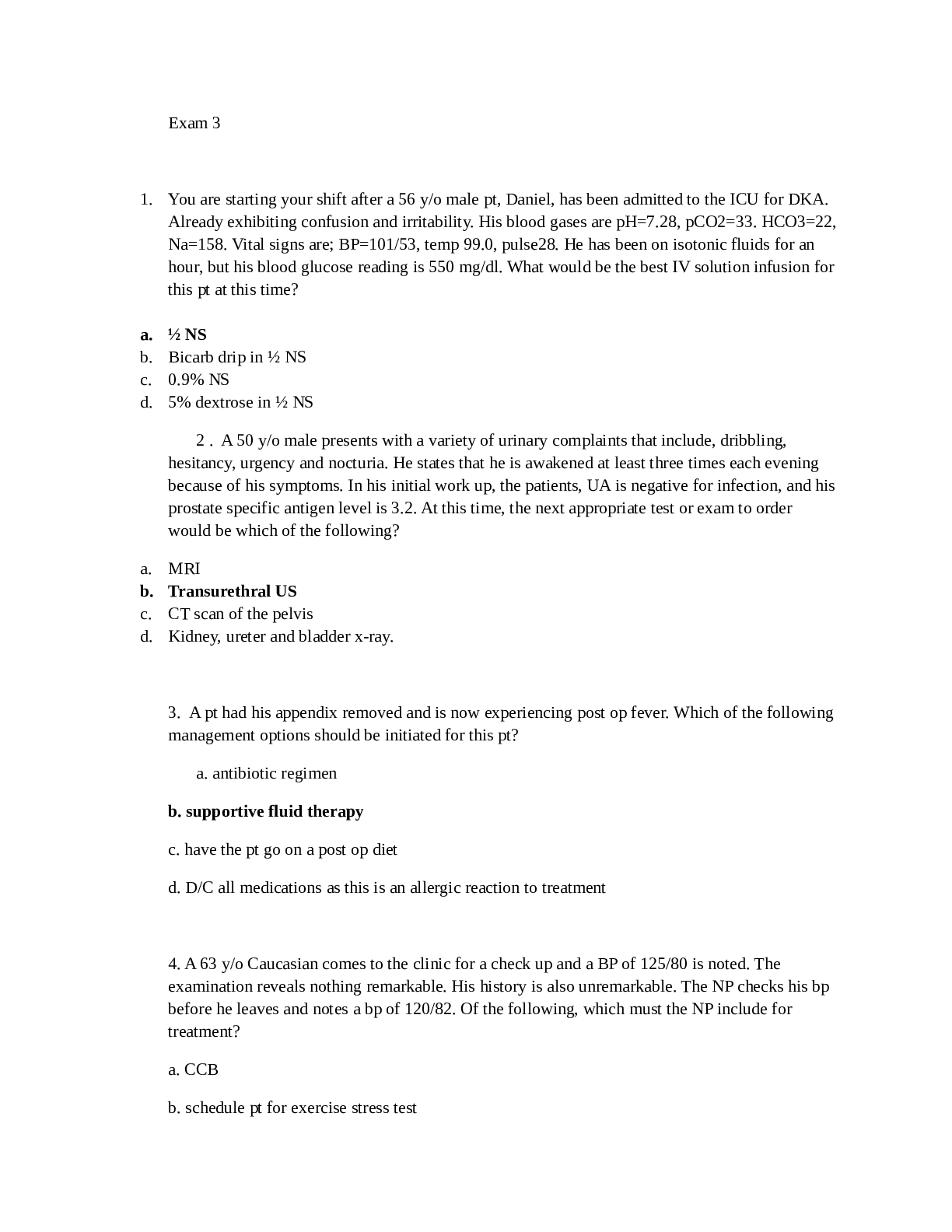
NR 304 Final Worksheet Questions: 1. Define subjective and objective data. Give three examples of each and state if the findings are documented in the history or physical examination findings. �... � Subjective Data what the person says about himself or herself during the physical examination; symptom is a subjective sensations that the person is feeling; o Examples: itching, pain, feelings of worry, nausea, depression, fatigue, anxiety, loneliness, etc. • Objective Data what the you as the health professional observe by inspecting, percussing, palpating, and auscultating during the physical examination; a sign is an objective abnormality that you as the examiner could detect on physical examination or in laboratory reports; observable and measurable; o Examples: blood pressure, discoloration of the skin, skin moisture, vomiting, temperature, weight, bleeding, blood cell count, etc. 2. List five actions a nurse should take when assessing a patient with a potentially critical hemodynamic state. Put your actions in priority order of 1-5. • Hemodynamic State instable blood pressure, which can lead to inadequate arterial blood flow to organs; heart failure. • Priority Actions: main goals for nurse are to evaluate the cardiac and circulatory function, as well as the response to any interventions. i. 3. What does the priority setting ABC mean? How does the nurse use this mnemonic in patient assessment? If a patient has a slow or rapid respiratory rate, is airway the primary concern? • A: airway. • B: breathing. • C: circulation. 4. What is HIPAA? Describe one situation when the nurse must adhere to HIPAA. • Health Insurance Portability and Accountability Act of 1996 (HIPAA) laws to improve efficiency in health care delivery by standardizing electronic data interchange and protection of confidentiality and security of health data by setting and enforcing standards; composed of 4 parts that have rules, which include: standards for electronic transactions, unique identifiers standards, the security rule, and the privacy rule. o Example: if patient isn’t able to give consent a spouse, relative, or a close friend can (but, the nurse must document it); 2 nurses assigned to the same patient can talk about the patient’s medical diagnosis in the patients private room; a nurse can give information about a patient over the phone if the patient gives permission to do so to that person; nurses can perform research as long as patient confidentiality is maintained at all times; 5. Describe the process of taking a pulse. What is a normal pulse? What are qualities of a normal pulse? What is the first action a nurse should take when the pulse is not as expected? • Normal Pulse 2+ bilaterally force; 60-100 beats per minute; 50-95 beats per minute in healthy individuals. o Qualities of A Normal Pulse rhythm should be regular, even tempo; symmetrical 2+ bilateral force; • Process of Taking A Pulse using the pads of your 1st 3 fingers, palpate the radial pulse @ the flexor aspect of the wrist laterally along the radius bone; if rhythm is regular, count the # of beats in 30 seconds and multiply by 2; if it’s irregular than count for a full minute; • 1ST Action if Pulse Is Not Expected 6. What is dehydration? List three subjective and three objective findings of dehydration. List the expected vital signs of a patient who is dehydrated. • Dehydration osmolar fluid loss of water, with no loss of electrolytes. o Subjective Findings: thirst, dizziness, syncope, confusion, weakness, fatigue, nausea, o Objective Findings: dry, furrowed tongue, vomiting, weight loss, oliguria ( output of urine), distended bladder, sunken eyes, diminished capillary refill, diaphoresis, cool clammy skin, flattened neck veins, urine specific gravity, osmolality, blood urea nitrogen (BUN), electrolytes, glucose, serum sodium. • Expected Vital Signs of Dehydrations tachycardia, weak, thread pulse; hypotension, orthostatic hypotension, central venous pressure; tachypnea ( respirations), hypoxia; hyperthermia 7. How is fluid volume deficit related to dehydration? How would concentrations of some solutes (solids) change with dehydration? Why? • Fluid Volume in dehydration, it is osmolar fluid loss, in which there is only a loss of water and there’s no loss of electrolytes. 8. What is an undesirable response of the body to a fever? • It can reset the thermostat of the brain @ a higher level, resulting in heat production and conservation. Why is this undesirable? What effect does it have? • It can result in an increased internal thermostat, which will mean that next time the tolerance of a fever will be higher and result in an increased heat production and increased heat conservation. 9. What is the most serious skin cancer? What is one risk factor for this cancer and one teaching item to address with your patient? Describe this most serious skin cancer below. • Most Serious Skin Cancer melanoma. o Risk Factors: fair skin, history of sunburn, excessive UV exposure, living closure to equator or @ a higher elevation, have many or unusual moles, family history of melanoma, weakened immune, etc. o Teaching Items To Address: protect your skin, limit your exposure to the sun, wear a heat or protective gear, wear sunscreen, check an unusual moles and always check on your moles to be able to note any differences, etc. 10. In dark skinned client, where is the best area to assess for jaundice (not skin or sclera)? Best place to assess for pallor? Best place to assess for cyanosis? • On Dark Skinned PT’s Where Would You Check For: o Jaundice best noted in the junction of hard and soft palate of the hands or feet, o Pallor: oral mucous membranes and the conjunctiva of the eye. o Cyanosis: oral mucous membranes and the conjunctiva of the eye. 11. To document pitting edema, the nurse measures the following depths of pitting. What is the corresponding scale (1+, 2+, 3+, 4+ ) for: • 2mm deep = 1+ • 4mm deep = 2+ • 6mm deep = 3+ • 8mm deep = 4+ 12. What is a body system complication for the client who is a chronic heavy drinker? Name 3 possible associated findings associated with this complication. • Body System Complication(s) for Heavy Drinkers liver disease, alcoholic liver disease, fatty liver, hepatitis, cirrhosis, pancreatitis, cancer, ulcer and gastrointestinal problems, immune system dysfunction, neurological damages, vitamin deficiencies, etc. • Possible Findings Associated With This Complication stomach ulcers, acid reflex, heartburn, gastritis, weakens your immune system and causes a decreased in WBCs, difficulty processing information BC it interferes with the brain receptors and neurotransmitters, as well as their cognitive function, malnourishment, anemia, tiredness, weakness, memory loss, etc. 13. It is important to encourage the elderly client to continue to be as active as possible. List five complications associated with the inability to move independently. • Complications Associated With Elderly Being Unable To Move Independently: a. Urinary System retention, stasis, renal calculi, incontinence, as well as UTI’s. b. Gastrointestinal Systemconstipation, impaction, and difficulty evacuating. c. Musculoskeletal System disuse osteoporosis, hypercalcemia, and fractures; joints can become stiff, painful, along w/impaired range of motion and contractures that include foot drop, which is a plantar flexion contracture; muscles can be weak and atrophy can result. d. Respiratory System thickening of respiratory secretions, the pooling of respiratory secretions, and an inability of the client to mobilize and expectorate these secretions, all of which can lead to atelectasis, hypostatic pneumonia, and respiratory tract infections; can also lead to shallow, ineffective respirations, movement, and a in terms of the client’s vital capacity. e. Circulatory System venous stasis, venous dilation, BP, edema, embolus formation, thrombophlebitis, and orthostatic hypotension, which is a risk factor also often associated w/client falls. f. Metabolic System rate of metabolism, which can lead to unintended weight gain, a negative calcium balance secondary to the loss of calcium from the bones during immobilization, a negative nitrogen balance secondary to an in terms of catabolic protein breakdown, and anorexia. g. Integumentary System skin breakdown, pressure ulcers, and poor skin turgor. h. Psychological Alterations apathy, isolation, frustration ,a lowered mood, as well as depression. 14. Describe fluid volume overload. List a possible cause of FVO. List three signs/symptoms of FVO. • Fluid Volume Overload (FVO) also known as hypervolemia, is a medical condition where there is too much fluid in the blood; the excess fluid is primarily salt and water, which builds up throughout the body resulting in weight gain; it’s expansion of the extracellular fluid volume, including the intravascular or interstitial space; • Possible Cause of FVO may be the product of compromised mechanisms for regulating water and sodium, as seen in congestive heart failure, hepatic failure, and renal failure; liver malfunction; inaccurate sodium and water retention include low protein sources, use of corticosteroids, glomerulonephritis, nephritic syndrome, nephropathy, hyperaldosteronism, and liver cirrhosis; too much intake of sodium and fluids; fluid shift into the intravascular space that may occur in response to fluid remobilization during burn therapy, as a result of giving albumin, and from mannitol or any hypertonic fluid administration. o S/S: SOB, respiratory rate, both due to in RBC’s, pulses w/ bounding character stemmed from circulatory overload and concomitant elevation of cardiac contractility, labored breathing and difficulty of breathing caused by an 15. Describe fluid volume deficit. List a possible cause of FVD. List three signs/symptoms of FVD. • Fluid Volume Deficit (FVD) this refers to dehydration, water loss alone WITHOUT a change in the amount of sodium; intravascular, interstitial, and/or intracellular fluid. • Possible Cause of FVD severe diarrhea, vomiting, fever, heat exposure, too much exercise, or work-related activity, urination due to infection, diseases such as diabetes o S/S: not peeing or having very dark yellow pee, very dry skin, feeling dizzy, rapid heartbeat, rapid breathing, sunken eyes, sleepiness, lack of energy, confusion or irritability, fainting, etc. 16. Differentiate between oral candidiasis and leukoplakia. List one possible cause of each. • Oral Candidiasis a white, cheesy, curd-like patch on the buccal mucosa and tongue; it scrapes off, leaving a raw, red surface that bleeds easily; termed ‘Thrush’ in newborn; o Possible Causes: it is an opportunistic infection that occurs after the use of antibiotics and corticosteroids, as well as in immunosuppressed people. • Leukoplakia chalky white, thick, raised patch with well-defined borders; the lesion is firmly attached an does not scrape off; it may occur on the lateral edges of the tongue. o Possible Causes: due to chronic irritation and occurs w/heavy smoking and alcohol use; lesions are precancerous; must refer to specialist. 17. What is a common manifestation that an elderly client has an acute problem such as infection or stroke? • Elderly client’s tend to present with severe confusion when faced with certain problems, and it is important to be prepared to know the symptoms that may present. 18. What are crackles? • Crackles are an abnormal breath sound that is heard via stethoscope during a physical exam and usually reflects a buildup of fluid, mucous, or pus in the small airways. How would you describe the sound crackles? • Sound of Crackles often described as fine, medium, and coarse; abnormal advantageous breath sounds that are characterized by discontinuous clicking or rattling sounds; you can simulate this sound by rolling a strand of hair b/w your fingers near your ear oy by moistening your thumb and by separating them near your hear Describe two pathological conditions when the nurse would expect crackles on auscultation. a. Crackles that do NOT clear after a cough may indicate pulmonary edema or fluid in the alveoli due to heart failure, pulmonary fibrosis, or acute respiratory distress syndrome. b. Crackles that partially clear or change after coughing may indicate bronchiectasis. 19. What are wheezes? • Wheezes (rhonchi) continuous musical sounds heard mainly over expiration; How would you describe the sound of wheezes? • Sound of Wheezes a whiny, whistle sound; a high-pitches continuous musical sound, which may occur during inspiration and/or expiration, due to an obstructive process. Describe two pathological conditions when the nurse would expect wheezes on auscultation. a. Asthma referred to as a ‘sibilant wheeze’ and is heard as a high-pitched whistle- like sound heard during expiration, as air moves through a narrow or obstructed airway. b. Rhonchi referred to as a ‘sonorous wheeze’ and is heard as a deep, low-pitched rumbling or coarse sound as air moves through tracheal-bronchial passages in the presence of mucous or respiratory secretions. 20. What is the significance of a syncopal episode in the elderly client? • Significance Of A Syncopal Episode In The Elderly syncope is the formal medical term for fainting, describing a temporary loss of consciousness due to a sudden decline in blood flow to the brain and can be caused by numerous things; the most common causes of syncope in the older adults are orthostatic hypotension, carotid sinus hypersensitivity, neuro-mediated syncope and cardiac arrhythmias; accounts for almost 70% of hospitalization in the North America. 21. Describe the subjective and objective findings of a client with a pneumothorax. • Pneumothorax when free air in the pleural space causes partial or complete lung collapse; air in pleural space neutralizes the usual negative pressure present; thus, the lung collapses; o Subjective Findings: can be acute and sudden and sharp; lateral region of the chest is usually affected, but can have referred pain to shoulder; acute dyspnea; difficulty breathing; sharp pain that can lead to feelings of tightness in the chest; o Objective Findings: shortness of breath; rapid heart rate; rapid breathing; cough; fatigue; 22. Describe the subjective and objective findings of a client with a pulmonary embolus. • Pulmonary Embolus a condition in which one or more arteries in the lungs become blocked by a blood clot. o Subjective Findings: shortness of breath; chest pain; lightheadedness or dizziness; clammy or discolored skin; leg pain; o Objective Findings: cough; excessive sweating, rapid or irregular heartbeat; fever; cyanosis; swelling, along with leg pain that is usually in the calf. 23. Describe the subjective and objective findings of a client with pneumonia. • Pneumonia an infection that inflames the air sacs in one or both lungs; the air sacs fill with fluid or pus (purulent material), causing cough with phlegm or puss, fever, chills, and difficulty breathing; can be caused by a variety of organisms, including bacteria, viruses and fungi, etc. o Subjective Findings: loss of appetite; chills; clammy skin or sweating; fatigue; sharp pain in the chest; dehydration; malaise; o Objective Findings: fever; shortness of breath, coughing, fast heart rate; rapid breathing; 24. Describe the subjective and objective findings of a client with emphysema. • Emphysema is a chronic obstructive pulmonary disease; a group of lung diseases that block airflow and make it difficult to breathe; it is a long-term, progressive disease of the lungs that primarily causes SOB due to over-inflation of the alveoli (air sacs in the lung); the lung tissue involved in the exchange of gases (oxygen and carbon dioxide) is impaired or destroyed. o Subjective Findings: chest tightness; fatigue or inability to exercise; chronic cough; shortness of breath; o Objective Findings: cough, that can be either dry or with phlegm; wheezing; frequent respiratory infections; 25. Describe the subjective and objective findings of a client with a myocardial infarction. • Myocardial Infarction a blockage of blood flow to the heart muscle; o Subjective Findings: tightness or pain in the chest, neck, or arms, as well as fatigue, lightheadedness, abnormal heartbeat, anxiety; discomfort or tightness; dizziness; fatigue; pain can be like a clenched fist in the chest; pain in the area between the shoulder blades, arm, chest, jaw, left arm, or upper abdomen; pain can occur while at rest, too; feelings of impending doom, palpations, shoulder discomfort. o Objective Findings: indigestion, nausea, vomiting, cold sweat or sweating; shortness of breath; palpations; 26. Describe the subjective and objective findings of a client with congestive heart failure. • Congestive Heart Failure a chronic condition in which the heart does not pump blood, as well as it should. o Subjective Findings: dizziness; fatigue; pain in the chest; shortness of breath while lying down or exercising; o Objective Findings: shortness of breath on lying down; excessive urination at night; cough with phlegm or that is dry; water retention or bloating; swollen legs; weight gain; palpations; 27. Describe the subjective and objective findings of a client with a suspected stroke or TIA. List at least three assessments a nurse will perform for a suspected stroke or TIA. • Transient Ischemic Attack (TIA) it is like a stroke and produces similar symptoms, but usually lasts only a few minutes and does not cause permeant damage; often is referred to as a ‘mini stroke’ o Subjective Findings: numbness in the right arm; disturbed sensory perception; tactile inadequate oxygen supply to the brain; o Objective Findings: • Nursing Assessment Performed For Suspected TIA: you should assess and monitor vital signs, oxygenation, neuro-checks, and for signs and symptoms of bleeding; notify the physician of changes; 28. What is a murmur? What does a murmur indicate? How does the nurse describe the sound of a murmur? What are the subjective findings of a patient with a murmur? How does the nurse assess for a murmur? • Murmur an abnormal sound heard on listening to the heart, usually through a stethoscope, produced by the blood passing through deformed cardiac valves. o Subjective Findings: o Objective Findings: • Sound Of A Murmur a heart murmur usually is an unusual sound heart between heartbeats; they sometimes sound like a whooshing or swishing noise; o What A Murmur Indicates: murmur indicates turbulent blood in or near your heart; • Nursing Assessment For A Murmur as a nurse you will need to assess and document the murmur timing, description, quality, and supplemental deatials, too. 29. Describe PAD. List three subjective and three objective findings of the client with PAD. • Peripheral Arterial Disease (PAD) a common circulatory problem, in which narrowed arteries blood flow to your limbs; your extremities (usually your legs), do not receive enough blood flow to keep up w/demand, which causes the notably leg pain when walking; o Subjective Findings: leg pain, particularly when walking; most common symptom is in the lower extremities: painful muscle cramping in the hips, thighs or calves when walking, climbing stairs or exercising; tingling in the legs; o Objective Findings: foot wounds that do not heal; plagues of arteries outside of the heart and/or the brain; 30. Describe PVD. List three subjective and three objective findings of the client PVD. • Peripheral Vascular Disease (PVD) circulation of blood to a body part (other than the brain or the heart) that is caused by a narrowed or blocked vessel; the main cause is atherosclerosis; o Subjective Findings: leg pain, particularly when walking; pain in the buttocks; pain that can occur in the leg and improve with rest or while exercising. o Objective Findings: edema; ulcers; thinning of the skin on the legs; cool skin; loss of hair on the legs; 31. Describe DVT. List three subjective and three objective findings of the client with DVT. • Deep Venous Thrombosis (DVT) occurs when a blood clot (thrombus) forms in 1 or more of the deep veins in the body, usually in the legs; sometimes it can present without an symptoms; o Subjective Findings: swelling, pain, tenderness that is often in the legs; o Objective Findings: swelling, redness; warmth of skin; 32. List three subjective and three objective findings of the client with an infection of the hand from a dog bite. • Dog Bite Infection On The Hand any infected laceration on the arm due to an animal bite should always be monitored for any changes, unusual discharge, or drainage. o Subjective Findings: pain, unable to move arm easily, stiffness, sore; painful joints. o Objective Findings: osteomyelitis; puss; fever; contaminated wounds; edema; 33. Describe the sequence of abdominal assessment (and why this is different from the normal sequence of assessment techniques). • Abdominal Assessment: i. Inspection. ii. Auscultate. iii. Percussion. iv. Palpation. • Reason It’s Performed In This Order B/C the percussion and palpation can lead to a change in the bowel sounds and make them hyperactive, which would lead to an inaccurate assessment. 34. Describe at least two different descriptions of emesis of the client with bleeding gastric ulcer. • E [Show More]
Last updated: 1 year ago
Preview 1 out of 14 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$12.00
Document information
Connected school, study & course
About the document
Uploaded On
Mar 28, 2021
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Mar 28, 2021
Downloads
0
Views
47



.png)