*NURSING > EXAM > Nursing Management: Lower Gastrointestinal Problems Test Bank | Lower Gastrointestinal Problems Test (All)
Nursing Management: Lower Gastrointestinal Problems Test Bank | Lower Gastrointestinal Problems Test Bank (answered) Spring 2021 > A+
Document Content and Description Below
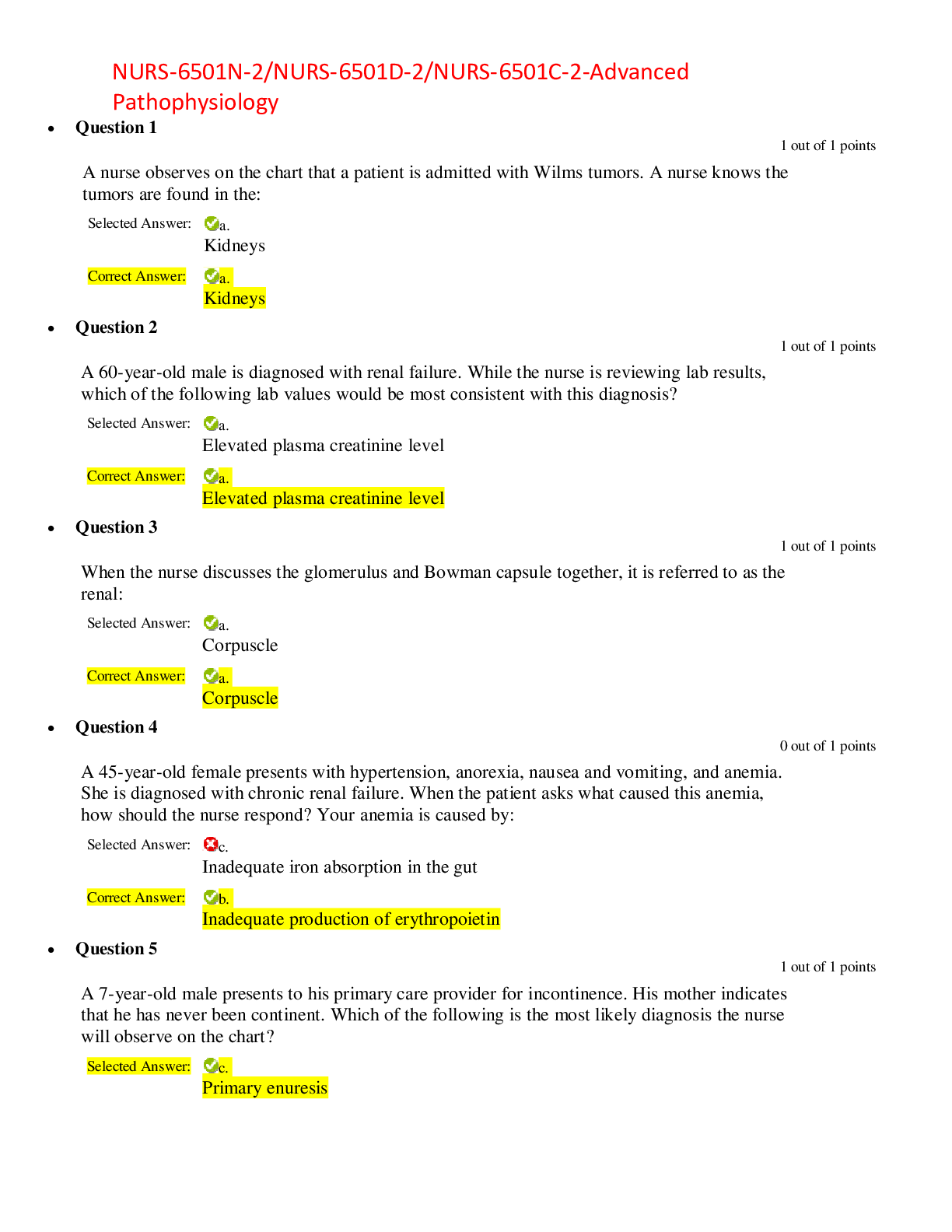
Chapter 43: Nursing Management: Lower Gastrointestinal Problems Test Bank MULTIPLE CHOICE 1. A patient who is hospitalized with watery, incontinent diarrhea is diagnosed with Clostridium difficile. Wh... ich action will the nurse include in the plan of care? a. Order a diet with no dairy products for the patient. b. Place the patient in a private room with contact isolation. c. Teach the patient about why antibiotics are not being used. d. Educate the patient about proper food handling and storage. 2. A 67-year-old patient tells the nurse, “I have problems with constipation now that I am older, so I use a suppository every morning.” Which action should the nurse take first? a. Encourage the patient to increase oral fluid intake. b. Inform the patient that a daily bowel movement is unnecessary. c. Assess the patient about individual risk factors for constipation. d. Suggest that the patient increase dietary intake of high-fiber foods. 3. In teaching a patient who has chronic constipation about the use of psyllium (Metamucil), which information will the nurse include? a. Absorption of fat-soluble vitamins may be reduced by fiber-containing laxatives. b. Dietary sources of fiber should be eliminated to prevent excessive gas formation. c. Use of this type of laxative to prevent constipation does not cause adverse effects. d. Large amounts of fluid should be taken to prevent impaction or bowel obstruction. 4. The nurse is obtaining a history for a 23-year-old woman who is being evaluated for acute lower abdominal pain and vomiting. Which question will be most useful in determining the cause of the patient’s symptoms? a. “Is it possible that you are pregnant?” b. “Can you tell me more about the pain?” c. “What type of foods do you usually eat?” d. “What is your usual elimination pattern?” . 5. Two days after an exploratory laparotomy with a resection of a short segment of small bowel, a patient complains of gas pains and abdominal distention. Which nursing action is best to take at this time? a. Give a return-flow enema. b. Assist the patient to ambulate. c. Administer the ordered IV morphine sulfate. d. Insert the ordered promethazine (Phenergan) suppository. 6. A patient who has blunt abdominal trauma after an automobile accident is complaining of severe pain. A peritoneal lavage returns brown drainage with fecal material. Which action will the nurse plan to take next? a. Auscultate the bowel sounds. b. Prepare the patient for surgery. c. Check the patient’s oral temperature. d. Obtain information about the accident. 7. A patient is admitted to the hospital for evaluation of right lower quadrant abdominal pain with nausea and vomiting. Which action should the nurse take? a. Check for rebound tenderness. b. Assist the patient to cough and deep breathe. c. Apply an ice pack to the right lower quadrant. d. Encourage the patient to take sips of clear liquids. 8. Which nursing action will be included in the plan of care for a patient with bowel irregularity and a new diagnosis of irritable bowel syndrome (IBS)? a. Encourage the patient to express feelings and ask questions about IBS. b. Suggest that the patient increase the intake of milk and other dairy products. c. Educate the patient about the use of alosetron (Lotronex) to reduce symptoms. d. Teach the patient to avoid using nonsteroidal anti-inflammatory drugs (NSAIDs). 9. A patient hospitalized with an acute exacerbation of ulcerative colitis is having 14 to 16 bloody stools a day and crampy abdominal pain associated with the diarrhea. The nurse will plan to a. place the patient on NPO status. b. administer IV metoclopramide (Reglan). c. teach the patient about total colectomy surgery. d. administer cobalamin (vitamin B12) injections. 10. Which nursing action will the nurse include in the plan of care when admitting a patient with an exacerbation of inflammatory bowel disease (IBD)? a. Restrict oral fluid intake. b. Monitor stools for blood. c. Increase dietary fiber intake. d. Ambulate four times daily. 11. After the nurse has finished teaching a patient with ulcerative colitis about sulfasalazine (Azulfidine), which patient statement indicates that the teaching has been effective? a. “I will need to use a sunscreen when I am outdoors.” b. “I will need to avoid contact with people who are sick.” c. “The medication will need to be tapered if I need surgery.” d. “The medication will prevent infections that cause the diarrhea.” 12. A patient who has an exacerbation of ulcerative colitis is having 15 to 20 stools daily and has excoriated perianal skin. Which patient behavior indicates that teaching regarding maintenance of skin integrity has been effective? a. The patient uses incontinence briefs to contain loose stools. b. The patient asks for antidiarrheal medication after each stool. c. The patient uses witch hazel compresses to decrease anal irritation. d. The patient cleans the perianal area with soap and water after each stool. 13. After the nurse has provided patient teaching about recommended dietary choices for a patient with an acute exacerbation of inflammatory bowel disease (IBD), which diet choice by the patient indicates a need for more teaching? a. Scrambled eggs b. White toast and jam c. Oatmeal with cream d. Pancakes with syrup 14. A patient who has had a total proctocolectomy and permanent ileostomy tells the nurse, “I cannot bear to even look at the stoma. I do not think I can manage all these changes.” Which is the best action by the nurse? a. Develop a detailed written plan for ostomy care for the patient. b. Ask the patient more about the concerns with stoma management. c. Reassure the patient that care for the ileostomy will become easier. d. Postpone any patient teaching until the patient adjusts to the ileostomy. 15. When caring for a patient who has a new diagnosis of Crohn’s disease after having frequent diarrhea and a weight loss of 10 pounds (4.5 kg) over 2 months, the nurse will plan to teach the patient about a. medication use. b. fluid restriction. c. enteral nutrition. d. activity restrictions. 16. A patient with Crohn’s disease develops a fever and symptoms of a urinary tract infection (UTI) with tan, fecal-smelling urine. The nurse will teach the patient a. to clean the perianal area carefully after any stools. b. about fistula formation between the bowel and bladder. c. to empty the bladder before and after sexual intercourse. d. about the effects of corticosteroid use on immune function. 17. A patient has a large bowel obstruction that occurred as a result of diverticulosis. When assessing the patient, the nurse will plan to monitor for a. referred back pain. b. metabolic alkalosis. c. projectile vomiting. d. abdominal distention. 18. When preparing for an annual physical exam for a patient who is 50 years old, the nurse will plan to teach the patient about a. endoscopy. b. colonoscopy. c. computerized tomography screening. d. carcinoembryonic antigen (CEA) testing. 19. During preoperative preparation for a patient scheduled for an abdominal-perineal resection, the nurse will a. give IV antibiotics starting 24 hours before surgery to reduce the number of bowel bacteria. b. teach the patient that activities such as sitting at the bedside will be started the first postoperative day. c. instruct the patient that another surgery in 8 to 12 weeks will be used to create an ileal-anal reservoir. d. administer polyethylene glycol lavage solution (GoLYTELY) to ensure that the bowel is empty before the surgery. 20. Before undergoing a colon resection for cancer of the colon, a patient has an elevated carcinoembryonic antigen (CEA) test. The nurse explains that the test is used to a. confirm the diagnosis of colon cancer. b. monitor the tumor status after surgery. c. identify the extent of cancer spread or metastasis. d. determine the need for postoperative chemotherapy. 21. Which nursing action is most important to include in the plan of care for a patient who had an abdominal-perineal resection the previous day? a. Teach about a low-residue diet. b. Monitor output from the stoma. c. Assess the perineal drainage and incision. d. Encourage acceptance of the colostomy stoma. 22. During the initial postoperative assessment of a patient’s stoma formed from a transverse colostomy, the nurse finds it to be deep pink with moderate edema and a small amount of bleeding. The nurse should a. document the stoma assessment. b. monitor the stoma every 30 minutes. c. notify the surgeon about the stoma appearance. d. place an ice pack on the stoma to reduce swelling. 23. A patient who has ulcerative colitis has a proctocolectomy and ileostomy. Which information will the nurse include in patient teaching? a. Restrict fluid intake to prevent constant liquid drainage from the stoma. b. Use care when eating high-fiber foods to avoid obstruction of the ileum. c. Irrigate the ileostomy daily to avoid having to wear a drainage appliance. d. Change the pouch every day to prevent leakage of contents onto the skin. 24. After teaching a patient to irrigate a new colostomy, the nurse will determine that the teaching has been effective if the patient a. hangs the irrigating container about 18 inches above the stoma. b. stops the irrigation and removes the irrigating cone if cramping occurs. c. inserts the irrigation tubing no further than 4 to 6 inches into the stoma. d. fills the irrigating container with 1000 to 2000 mL of lukewarm tap water. 25. The nurse explains to a patient with a new ileostomy that after the bowel adjusts to the ileostomy, the usual drainage will be about a. 1 cup. b. 2 cups. c. 3 cups. d. 1 quart. 26. When implementing the initial plan of care for a patient admitted with acute diverticulitis, the nurse will plan to a. give stool softeners. b. administer IV fluids. c. order a diet high in fiber and fluids. d. prepare the patient for colonoscopy. 27. Which patient education will the nurse provide before discharge for a patient who has had a herniorrhaphy to repair an incarcerated inguinal hernia? a. Encourage the patient to cough. b. Provide sitz baths several times daily. c. Avoid use of acetaminophen (Tylenol) for pain. d. Apply a scrotal support and ice to reduce swelling. 28. After the nurse has completed teaching a patient with newly diagnosed celiac disease, which breakfast choice by the patient indicates good understanding of the information? a. Corn tortilla with eggs b. Bagel with cream cheese c. Oatmeal with non-fat milk d. Whole wheat toast with butter 29. Which instructions will the nurse include in discharge teaching for a patient who has had a hemorrhoidectomy at an outpatient surgical center? a. Maintain a low-residue diet until the surgical area is healed. b. Use ice packs on the perianal area to relieve pain and swelling. c. Take prescribed pain medications before a bowel movement is expected. d. Delay having a bowel movement for several days until healing has occurred. 30. A patient calls the clinic and tells the nurse about a new onset of severe and frequent, diarrhea. The nurse anticipates that the patient will need to a. collect a stool specimen. b. prepare for colonoscopy. c. schedule a barium enema. d. have blood cultures drawn. 31. A patient with Crohn’s disease has megaloblastic anemia. The nurse will anticipate teaching the patient about the ongoing need for a. oral ferrous sulfate tablets. b. regular blood transfusions. c. iron dextran (Imferon) infusion. d. cobalamin (B12) nasal spray or injections. 32. When performing an admission assessment for a patient with abdominal pain, the nurse palpates the left lower quadrant and the patient complains of right lower quadrant pain. The nurse will document this as a. rebound pain. b. Cullen sign. c. Rovsing sign. d. McBurney point. 33. A critically ill patient develops incontinence of watery stools. What action will be best for the nurse to take to prevent complications associated with ongoing incontinence? a. Insert a rectal tube. b. Use incontinence briefs. c. Implement fecal management system. d. Assist the patient to a bedside commode or to the bathroom at frequent intervals. 34. When interviewing a patient with abdominal pain and possible irritable bowel syndrome, which question will be most important for the nurse to ask? a. “Have you been passing a lot of gas?” b. “What foods affect your bowel patterns?” c. “Do you have any abdominal distention?” d. “How long have you had abdominal pain?” 35. Which of these prescribed interventions will the nurse implement first when caring for a patient who has just been diagnosed with peritonitis caused by a ruptured diverticulum? a. Administer morphine sulfate 4 mg IV. b. Infuse metronidazole (Flagyl) 500 mg IV. c. Send the patient for a computerized tomography scan. d. Insert a nasogastric (NG) tube and connect it to intermittent low suction. 36. Which action should the nurse take first when a patient calls the clinic complaining of diarrhea of 24 hours’ duration? a. Ask the patient to describe the character of the stools and any associated symptoms. b. Inform the patient that laboratory testing of blood and stool specimens will be necessary. c. Suggest that the patient drink clear liquid fluids with electrolytes, such as Gatorade or Pedialyte. d. Advise the patient to use over-the-counter loperamide (Imodium) to slow gastrointestinal (GI) motility. 37. A patient is admitted to the emergency department with severe abdominal pain with rebound tenderness. The vital signs include temperature 101° F (38.3° C), pulse 130, respirations 34, and blood pressure (BP) 84/50. Which of the following interventions should the nurse implement first? a. Administer IV ketorolac (Toradol) 15 mg. b. Draw blood for a complete blood count (CBC). c. Obtain a computed tomography (CT) scan of the abdomen. d. Infuse 1000 mL of lactated Ringer’s solution over 30 minutes. 38. Following an exploratory laparotomy and bowel resection, a patient who has a nasogastric tube to suction complains of nausea and stomach distention. The first action by the nurse should be to a. auscultate for hypotonic bowel sounds. b. notify the patient’s health care provider. c. reposition the tube and check for placement. d. remove the tube and replace it with a new one. 39. A patient is brought to the emergency department with a knife impaled in the abdomen following a domestic fight. During the initial assessment of the patient, the nurse should a. assess the BP and pulse. b. remove the knife to assess the wound. c. determine the presence of Rovsing sign. d. insert a urinary catheter and assess for hematuria. 40. Which of these nursing activities included in the care of a patient with a new colostomy should the nurse delegate to nursing assistive personnel (NAP)? a. Document the appearance of the stoma. b. Place the pouching system over the ostomy. c. Drain and measure the output from the ostomy. d. Check the skin around the ostomy for breakdown. 41. The nurse who is interviewing a 40-year-old obtains information about the following patient problems. Which information is most important to communicate to the health care provider? a. The patient had an appendectomy at age 17. b. The patient smokes a pack/day of cigarettes. c. The patient has a history of frequent constipation. d. The patient has recently noticed blood in the stools. 42. The RN and nursing assistive personnel (NAP) are caring for a patient with a paralytic ileus. Which of these nursing activities is appropriate for the nurse to delegate to NAP? a. Auscultation for bowel sounds b. Applying petroleum jelly to the lips c. Irrigation of the nasogastric (NG) tube with saline d. Assessment of the nose for irritation 43. A hospitalized patient who has been taking antibiotics for several days develops watery diarrhea. Which action should the nurse take first? a. Notify the health care provider. b. Obtain a stool specimen for analysis. c. Provide education about handwashing. d. Place the patient on contact precautions. 44. After receiving change-of-shift report, which of the following patients should the nurse assess first? a. A patient whose new ileostomy has drained 800 mL over the previous 8 hours b. A patient with familial adenomatous polyposis who has occult blood in the stool c. A patient with ulcerative colitis who has had six liquid stools in the previous 4 hours d. A patient who has abdominal distention and an apical heart rate of 136 beats/minute 45. A patient with Crohn’s disease who is taking infliximab (Remicade) calls the nurse in the outpatient clinic about all of these symptoms. Which symptom is most important to communicate to the health care provider? a. Nausea b. Joint pain c. Frequent headaches d. Elevated temperature 46. A patient with a gunshot wound to the abdomen undergoes surgery, and a colostomy is formed as illustrated. Which information will be included in patient teaching? a. This type of colostomy is usually temporary. b. Soft, formed stool can be expected as drainage. c. Stool will be expelled from both ostomy stomas. d. Irrigations can regulate drainage from the stomas. [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 05, 2021
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Apr 05, 2021
Downloads
0
Views
31

.png)




.png)
 (1).png)