*NURSING > STUDY GUIDE > NSG6006 _ Policies & Practice Standards • State Nurse Practice Act | 5000 (Roles) | AUTHENTIC STUD (All)
NSG6006 _ Policies & Practice Standards • State Nurse Practice Act | 5000 (Roles) | AUTHENTIC STUDY GUIDE | SOUTH UNIVERSITY
Document Content and Description Below
Policies & Practice Standards • State Nurse Practice Act NSG6006 Study Guide 5000 (Roles) • _History and Developmental Aspects of Advanced Practice Nursing • Definition of advanced practice n... urse (APN) - A nurse who has completed an accredited graduate-level education program preparing her or him for the role of certified nurse practitioner, certified registered nurse anesthetist, certified nurse-midwife, or clinical nurse specialist; has passed a national certification examination that measures the APRN role and population-focused competencies; maintains continued competence as evidenced by recertification; and is licensed to practice as an APRN involves advanced nursing knowledge and skills; it is not a medical practice, although APNs perform expanded medical therapeutics in many roles • History of APN movement History and evolution of nursing science Knowledge development APN Roles CNSs have a strong and tumultuous history. Over the past 20 years, the departure from direct patient care as being a main focus to working predominantly in the nursing education and systems improvement domains has created confusion within nursing and the public because non- CNSs (e.g., nurse educators, quality improvement managers) function in the same capacity. However, CNSs are uniquely educated to provide advanced practice and specialist expertise when working directly with complex and vulnerable patients, educating and supporting interdisciplinary staff, and facilitating change and innovation in health care systems that those in other roles in health care cannot. As health care reform continues to gain momentum to improve the health care system, there will be many new opportunities for CNSs. As masters of flexibility and creativity, CNSs can develop new roles to meet the needs of patients and health care systems. For example, in nurse- managed clinics, perhaps NPs could deliver the primary care to patients in the management of hypertension. Once first- or second-line therapies or interventions are found to be ineffective, a referral could be placed to the cardiovascular CNS for specialized pharmacologic and nonpharmacological treatment. Also, the cardiovascular CNS could integrate the latest evidence to create educational materials for patients and other health care professionals. Perhaps a CNM who is caring for a pregnant woman who develops gestational diabetes, preeclampsia, and is in breech position could ask the perinatal CNS to commonage the patient by following the patient and fetus or neonate in the prenatal setting through hospital discharge into the postpartum phase. The perinatal CNS could establish interagency processes to facilitate care delivery across practice settings to provide seamless transitions of care. The possibilities are endless if CNSs understand their role, improve understanding of the importance of this role in advanced practice nursing, and maximize the driving forces and minimize the restraining forces in the health care system. Primary care is the foundation of the evolving U.S. health care system. If access to primary care for all is the goal, while containing costs and focusing on quality outcomes, then NPs will be crucial to achieving these aims. In our current system, there just aren't enough PCPs to meet the need and, with an additional estimated 32 million more people who will be covered and need access to full primary care, based on the PPACA, we will need additional providers more than ever. Physicians are not choosing primary care practice for complex reasons. On the other hand, most NPs choose primary care practice roles (e.g., family, adult, and pediatric NPs) because they enter these programs specifically to provide primary care. Two areas in particular must be addressed before NPs will be able to contribute fully to primary care delivery nationwide: 1. There must be changes in the outdated state scope of practice laws and regulations of nurse practitioners. This is because the variation in state regulations on scope of practice and prescribing authority has been a major barrier to using NPs fully and providing increased access to quality, cost-efficient primary care. 2. There must be substantive changes in health professional education to foster true collaboration and teamwork among physicians, NPs, and other health care disciplines in general to obtain the full benefit of diverse competencies inherent in a team. If both of these are addressed, meeting U.S. primary care needs could be significantly affected in a positive way. Today's NP students and graduates must accept the professional responsibility for being active in the governance of delivery systems and informing and changing policy. There is too much at stake to leave this to a few, or to someone else. The health of the United States population depends on new models of care, on all health care providers practicing to the fullest extent of their education and training, and on strong teams who respect each other and partner with patients. NPs must support their efforts as they take an active role in developing stable health care policy and care delivery systems that allow for patient access to primary care services provided by NPs. The ACNP role provides an opportunity for NPs to have a significant impact on patient outcomes at a dynamic time in the history of health care delivery. As their role continues to evolve, and as health care systems respond to market forces and economic change, opportunities to develop the ACNP role further will arise. Future development of the ACNP role should be based on the evaluation of the need for the role, understanding the scope of the role, assessment of the practice or organization, and the service needs of the patient population. Ensuring that ACNPs practice to the full scope of (2011). Because the ACNP role continues to evolve, participation in national organizations to refine consensus regarding role components, program curriculum, marketing, and role evaluation is necessary. ACNP educators and clinicians must work together to ensure that the preparation and practice of ACNPs is safe, effective, and fully represented as the movement of doctoral APN education evolves. ACNPs must be strong activists in efforts to gain full recognition of their role within their proper scope of practice across acute care settings. In this evolving health care arena, ACNP practice is rapidly expanding and holds unlimited potential. Ongoing challenges include ensuring expansion of the ACNP with a focus on advanced practice nursing, rather than as a physician replacement model of care. Nurse-midwifery practice encompasses a full range of primary health care services for women, from adolescence beyond menopause. These services include the independent provision of primary care, gynecologic and family planning services, preconception care, pregnancy care, childbirth and the postpartum period, care of the normal newborn during the first 28 days of life, and treatment of male partners for sexually transmitted infections. CNMs provide initial and ongoing comprehensive assessment, diagnosis, and treatment. They conduct physical examinations, prescribe medications, including controlled substances and contraceptive methods, admit, manage, and discharge patients from birth centers or hospitals, order and interpret laboratory and diagnostic tests, and order the use of medical devices. CNMs' care also includes health promotion, disease prevention, and individualized wellness education and counseling. CNMs must demonstrate that they meet the core competencies for basic midwifery practice of the ACNM (ACNM, 2008b) and must practice in accordance with the ACNM standards for the practice of midwifery (ACNM, 2011d). With constant changes in health care, CNMs may need to expand their knowledge and skills beyond that of basic CNM practice. Advanced CNM skills, such as level 1 ultrasound or acting as first assistant in surgery, may be incorporated into a CNM's practice as long as the CNM follows the recommendations for acquiring these skills by obtaining formal didactic and clinical training to ensure that the advanced skill is acquired and monitored to ensure patient safety. There have been many recent positive advances in nurse-midwifery and between nurse-midwifery and the broader health care system. The ACNM has been reaching out to professional nursing, midwifery, medical, policy, and public health colleagues nationally and internationally. There has been international recognition of the need for more midwives to reduce maternal and neonatal mortality. In the United States, the IOM report, the Future of Nursing, and passage of the PPACA has placed CNMs and other APRNs in a partnership role in redesigning the health care system for the future. From a midwifery perspective, we hope that this system will honor women and offer them support in realizing the power that comes with the choice of a woman-centered health care system. Nurse anesthesia, the earliest nursing specialty, was also the first nursing specialty to have standardized educational programs, a certification process, mandatory continuing education, and recertification. Nurse anesthetists have been involved in the development of anesthetic techniques along with physicians and engineers. CRNAs have been nursing leaders in obtaining third-party reimbursement for professional services and in coping with challenges such as the prospective payment system, managed care, and physician supervision. Nurse anesthetists provide surgical and nonsurgical anesthesia services in a variety of settings in the United States and other parts of the world. CRNAs work collaboratively with physicians, as do other APNs, and are capable of providing the full spectrum of anesthesia services. Activism at the state and federal legislative and regulatory levels is a recognized CRNA activity. Increasing coalition building among nurse anesthetists, other APNs, and nursing educators is congruent with a shared nursing vision. This vision values health care for all Americans, provided in a safe and cost-effective manner by APNs collaborating with other health care professionals. John F. Garde was a distinguished health care leader who served as AANA Executive Director from 1983 to 2001, and again on an interim basis from February 2009 until his untimely death in July 2009. A statement of his holds true today (Garde, 1998, p. 15): The profession has an optimistic future. I point out with pride the commitment that AANA members have toward the future of their profession—a commitment that encompasses being outstanding anesthesia practitioners who belong to their Association. I am reminded, too, what Dick Davidson, President of the American Hospital Association, said when asked about what will remain in health care 100 years from now: ‘There will always be personal contact and caring. We will always have hands touching patients. Everything we do is about human need. That's the constant over time.’ And, that is the legacy of the nurse anesthesia profession. SCOPE OF PRACTICE scope of practice describes practice limits and sets the parameters within which nurses in the various advanced practice nursing specialties may legally practice. Scope statements define what APRNs can do for and with patients, what they can delegate, and when collaboration with others is required. Scope of practice statements tell APRNs what is actually beyond the limits of their nursing practice (American Nurses Association [ANA], 2003, 2012; Buppert, 2012; Kleinpell, Hudspeth, Scordo, et al., 2012). The scope of practice for each of the four APRN roles differs (see Part III). Scope of practice statements are key to the debate about how the U.S. health care system uses APRNs as health care providers; scope is inextricably linked with barriers to advanced practice nursing. CRNAs, who administer general anesthesia, have a scope of practice markedly different from that of the primary care nurse practitioner (NP), for example, although both have their roots in basic nursing. In addition, it is important to understand that scope of practice differs among states and is based on state laws promulgated by the various state nurse practice acts and rules and regulations for APRNs (Lugo, O'Grady, Hodnicki, et al., 2007, 2009; NCSBN, 2012; Pearson, 2012). On the Internet, scope of practice statements can be found by searching state government websites in the areas of licensing boards, nursing, and advanced practice nursing rules and regulations, or by visiting the NCSBN site (www.ncsbn.org). Recent federal policy initiatives, including the IOM Future of Nursing Report, (2011). the PPACA (HHS, 2011), and the Josiah Macy Foundation (Cronenwett & Dzau, 2010) have all issued recom mendations with important implications for expanding the scope of practice for APRNs. The National Health Policy Forum (http://www.nhpf.org/library/background- papers/BP76_SOP_07-06-2010.pdf) and Citizen Advocacy Center (https://www.ncsbn.org/ReformingScopesofPractice-WhitePaper.pdf) reports state firmly that current scope of practice adjudication is far too technical, subject to political pressure, and therefore not appropriate in the legislative sphere. There must be a more powerful forum so that the public can enter into the dialogue (see Chapter 22). As scope of practice expands, accountability becomes a crucial factor as APRNs obtain more authority over their own practices. First, it is important that scope of practice statements identify the legal parameters of each APRN role. Furthermore, it is crucial that scope of practice statements presented by national certifying entities are carried through in language in state statutes (Buppert, 2012). Our society is highly mobile and APRNs must recognize that their scope of practice will vary among states; in a worst case scenario, one can be an APRN in one state but not meet the criteria in another state. 1. Throughout the century, APNs have been permitted by organized medicine and state legislative bodies to provide care to the underserved poor, particularly in rural areas of the nation. However, when that care competes with physicians' reimbursement for their services, there has been significant resistance from organized medicine, which resulted in interprofessional conflict. 2. Documentation of the outcomes of practice helped establish the earliest nursing specialties and continues to be of critical importance to the survival of APN practice. 3. The efforts of national professional organizations, national certification, and the move toward graduate education as a requirement for advanced practice have been critical to enhancing the credibility of advanced practice nursing. 4. Intraprofessional and interprofessional resistance to expanding the boundaries of the nursing discipline continue to recur. 5. Societal forces, including wars, the economic climate, and health care policy, have influenced APN history. • _Scope of practice cont. The term scope of practice refers to the legal authority granted to a professional to provide and be reimbursed for health care services. The ANA (2010) defined the scope of nursing practice as “The description of the who, what, where, when, why, and how of nursing practice.” This authority for practice emanates from many sources, such as state and federal laws and regulations, the profession's code of ethics, and professional practice standards. For all health care professionals, scope of practice is most closely tied to state statutes; for nursing in the United States, these statutes are the nurse practice acts of the various states. As previously discussed, APN scope of practice is characterized by specialization, expansion of services provided, including diagnosing and prescribing, and autonomy to practice (NCSBN, 2008). The scopes of practice also differ among the various APN roles; various APN organizations have provided detailed and specific descriptions for their particular role. Carving out an adequate scope of APN practice authority has been an historic struggle for most of the advanced practice groups (see Chapter 1) and this continues to be a hotly debated issue among and within the health professions. Significant variability in state practice acts continues, such that APNs can perform certain activities in some states, notably prescribing certain medications and practicing without physician supervision, but may be constrained from performing these same activities in another state (Lugo, O'Grady, Hodnicki, & Hanson, 2007). The Consensus Model's proposed regulatory language can be used by states to achieve consistent scope of practice language and standardized APRN regulation (NCSBN, 2008). A scope of practice is a state-based legal framework (i.e., statutes, codes, and regulations) that defines who is authorized to provide clearly delineated services, to whom and under what circumstances those services can be provided, and who can be reimbursed for those services. All health professions have an autonomous domain of practice and a delegated authority within the medical domain (Lyon, 2004). The autonomous domain of nursing practice “encompasses the diagnosis of health conditions (e.g., nursing diagnoses) that are amenable to nursing interventions [and] therapeutics, the implementation of interventions, and evaluation of the effectiveness of nursing interventions [and] therapeutics” (Lyon, 2004, p. 9). Historically, the medical profession developed a broad, overarching scope of practice that encompassed almost all health care activities (see Chapter 1; Safriet, 2010). As a consequence, other health professionals (e.g., nurses, physical therapists, pharmacists) have had to carve out their scopes of practice out of the medical scope of practice. The ANA's restrictive 1955 definition of nursing reinforced the practice of nursing as having independent functions and being dependent on and delegated to by the profession of medicine. It also prohibited nurses from diagnosing and prescribing. By definition, the term scope of practice describes practice limits and sets the parameters within which nurses in the various advanced practice nursing specialties may legally practice. Scope statements define what APRNs can do for and with patients, what they can delegate, and when collaboration with others is required. Scope of practice statements tell APRNs what is actually beyond the limits of their nursing practice (American Nurses Association [ANA], 2003, 2012; Buppert, 2012; Kleinpell, Hudspeth, Scordo, et al., 2012). The scope of practice for each of the four APRN roles differs (see Part III). Scope of practice statements are key to the debate about how the U.S. health care system uses APRNs as health care providers; scope is inextricably linked with barriers to advanced practice nursing. CRNAs, who administer general anesthesia, have a scope of practice markedly different from that of the primary care nurse practitioner (NP), for example, although both have their roots in basic nursing. In addition, it is important to understand that scope of practice differs among states and is based on state laws promulgated by the various state nurse practice acts and rules and regulations for APRNs (Lugo, O'Grady, Hodnicki, et al., 2007, 2009; NCSBN, 2012; Pearson, 2012). On the Internet, scope of practice statements can be found by searching state government websites in the areas of licensing boards, nursing, and advanced practice nursing rules and regulations, or by visiting the NCSBN site (www.ncsbn.org). Recent federal policy initiatives, including the IOM Future of Nursing Report, (2011). the PPACA (HHS, 2011), and the Josiah Macy Foundation (Cronenwett & Dzau, 2010) have all issued recom mendations with important implications for expanding the scope of practice for APRNs. The National Health Policy Forum (http://www.nhpf.org/library/background-papers/BP76_SOP_07-06-2010.pdf) and Citizen Advocacy Center (https://www.ncsbn.org/ReformingScopesofPractice-WhitePaper.pdf) reports state firmly that current scope of practice adjudication is far too technical, subject to political pressure, and therefore not appropriate in the legislative sphere. There must be a more powerful forum so that the public can enter into the dialogue (see Chapter 22). As scope of practice expands, accountability becomes a crucial factor as APRNs obtain more authority over their own practices. First, it is important that scope of practice statements identify the legal parameters of each APRN role. Furthermore, it is crucial that scope of practice statements presented by national certifying entities are carried through in language in state statutes (Buppert, 2012). Our society is highly mobile and APRNs must recognize that their scope of practice will vary among states; in a worst case scenario, one can be an APRN in one state but not meet the criteria in another state (Minnesota Nursing, 2011; Taylor, 2006) • _Evolution of the APN role CRNA 1945, Mid Wife 1955, PNP 1965, 1979 DN, 1985 NP, 1995 CNS • _Four recognized APN roles o Clinical nurse specialist -1995 Key to their development in the 1940s was the establishment of a formal organization of practicing nurse-midwives, the American Association of Nurse-Midwives (AANM), which incorporated in 1941 under the leadership of Mary Breckinridge. By July 1942, the AANM had a “membership of 71 graduate nurses” who had specialty training in midwifery (News Here and There, 1942, p. 832). Three years later, in 1944, the National Organization of Public Health Nurses established a section for nurse-midwives within their organization. This group prepared a roster of all midwives in the country and defined their practice, making it clear that nurse-midwives would continue to practice under physician authority. By the middle of the 1970s, the ANA officially recognized the CNS role, defining the CNS as an expert practitioner and change agent. Of particular significance, the ANA's definition specified a master's degree as a requirement for the CNS (ANA Congress of Nursing Practice, 1974). As with the other advanced nursing specialties, the development of the CNS role included early evaluation research that served to validate and promote the innovation. Georgopoulos and colleagues (Georgopoulos & Christman, 1970; Georgopoulos & Jackson, 1970; Georgopoulos & Sana, 1971) conducted studies evaluating the effect of CNS practice on nursing process and outcomes in inpatient adult health care settings. These and other evaluative studies (Ayers, 1971; Girouard, 1978; Little & Carnevali, 1967) demonstrated the positive effect of the CNS on improving nursing care and patient outcomes. Moreover, with the increasing demand from society to cure illness using the latest scientific and technologic advances, hospital administrators willingly supported specialization in nursing and hired CNSs, particularly in the revenue-producing ICUs. Box 1-5 presents more information on the growth and development of nursing in the 1970s. this group of health care leaders was charged with evaluating the feasibility of expanding nursing practice (Kalisch & Kalisch, 1986). They concluded that extending the scope of the nurse's role was essential to providing equal access to health care for all Americans. According to an editorial in the AJN, “The kind of health care Lillian Wald began preaching and practicing in 1893 is the kind the people of this country are still crying for” (Schutt, 1971, p. 53). The committee urged the establishment of innovative curricular designs in health science centers and increased financial support for nursing education. It also advocated standardizing nursing licensure and national certification and developed a model nurse practice law suitable for national application. In addition, the committee called for further research related to cost-benefit analyses and attitudinal surveys to assess the impact of the NP role (HEW, 1972). This report resulted in increased federal support for training programs for the preparation of several types of NPs, including family NPs, adult NPs, and emergency department NPs. he 1960s are most often noted as the decade in which clinical nurse specialization took its modern form. Peplau (1965) contended that the development of areas of specialization is preceded by three social forces: (1) an increase in specialty-related information; (2) new technologic advances; and (3) a response to public need and interest. In addition to shaping most nursing specialties, these forces had a particularly strong effect on the development of the psychiatric CNS role in the 1960s. The Community Mental Health Centers Act of 1963, as well as the growing interest in child and adolescent mental health care, directly enhanced the expansion of that role in outpatient mental health care. CNSs have a strong and tumultuous history. Over the past 20 years, the departure from direct patient care as being a main focus to working predominantly in the nursing education and systems improvement domains has created confusion within nursing and the public because non-CNSs (e.g., nurse educators, quality improvement managers) function in the same capacity. However, CNSs are uniquely educated to provide advanced practice and specialist expertise when working directly with complex and vulnerable patients, educating and supporting interdisciplinary staff, and facilitating change and innovation in health care systems that those in other roles in health care cannot. As health care reform continues to gain momentum to improve the health care system, there will be many new opportunities for CNSs. As masters of flexibility and creativity, CNSs can develop new roles to meet the needs of patients and health care systems. For example, in nurse- managed clinics, perhaps NPs could deliver the primary care to patients in the management of hypertension. Once first- or second-line therapies or interventions are found to be ineffective, a referral could be placed to the cardiovascular CNS for specialized pharmacologic and nonpharmacologic treatment. Also, the cardiovascular CNS could integrate the latest evidence to create educational materials for patients and other health care professionals. Perhaps a CNM who is caring for a pregnant woman who develops gestational diabetes, preeclampsia, and is in breech position could ask the perinatal CNS to comanage the patient by following the patient and fetus or neonate in the prenatal setting through hospital discharge into the postpartum phase. The perinatal CNS could establish interagency processes to facilitate care delivery across practice settings to provide seamless transitions of care. The possibilities are endless if CNSs understand their role, improve understanding of the importance of this role in advanced practice nursing, and maximize the driving forces and minimize the restraining forces in the health care system. o Nurse practitioner (primary care; acute care) 1985 The idea of using nurses to provide what we now refer to as primary care services dates to the late nineteenth century. During this period of rapid industrialization and social reform, public health nurses played a major role in providing care for poverty-stricken immigrants in cities throughout the country. In 1893, Lillian Wald, a young graduate nurse from the New York Training School for Nurses, established the Henry Street Settlement (HSS) House on the Lower East Side of Manhattan. Its purpose was to address the needs of the poor, many of whom lived in overcrowded, rat-infested tenements. For several decades, the HSS visiting nurses, like other district nurses, visited thousands of patients with little interference in their work (Wald, 1922). The needs of this disadvantaged community were limitless. According to one account (Duffus, 1938): most NPs choose primary care practice roles (e.g., family, adult, and pediatric NPs) because they enter these programs specifically to provide primary care. As with other advanced practice roles, direct clinical practice is the foundation of the work of the primary care NP, which unfolds around the premise that individuals seek care for a broad range of health care concerns over time and across the life span. Relationships evolve over time, which facilitates a sense of mutual respect and trust. In that relationship, a deep understanding of the patient's life and the meaning of the illness or health issue at hand develops. Knowing patients and their family members, their jobs and careers, and their challenges in raising children and caring for aging parents is part of accompanying patients through the transitions of life it was during the 1960s that the role was first described formally and implemented in outpatient pediatric clinics, originating in part as a response to a shortage of primary care physicians. As the trend toward medical specialization drew increasing numbers of physicians away from primary care, many areas of the country were designated underserved with respect to the numbers of primary care physicians. “Report after report issued by the AMA [American Medical Association] and the Association of American Medical Colleges decried the shortage of physicians in poor rural and urban areas” (Fairman, 2002, p. 163). At the same time, consumers across the nation were demanding accessible, affordable, and sensitive health care while health care delivery costs were increasing at an annual rate of 10% to 14% (Jonas, 1981). o Certified nurse midwife- 1955 Throughout the eighteenth and nineteenth centuries, lay midwives, rather than professional nurses or physicians, assisted women in childbirth. Midwives who were brought to the United States with the slave trade in 1619, and others who arrived later with waves of European immigration, were respected community members. In the late nineteenth and early twentieth centuries however, these untrained midwives would lose respect as scientific, hospital-based deliveries became the norm. Meanwhile, women in isolated communities throughout the country, particularly in rural settings, continued to employ lay midwives for deliveries well into the twentieth century. In the early twentieth century, national concern about high maternal-infant mortality rates led to heated debates surrounding issues of midwife licensing and control; lay midwives would soon be blamed for the high maternal and infant mortality rates that plagued the United States. In 1914, Dr. Frederick Taussig, speaking at the annual meeting of the National Organization of Public Health Nursing (NOPHN) in St. Louis, proposed that the creation of “nurse-midwives” might solve the “midwife question” and suggested that nurse-midwifery schools be established to train graduate nurses (Taussig, 1914). Later in the decade, the Children's Bureau called for efforts to instruct pregnant women in nutrition and recommended that public health nurses teach principles of hygiene and prenatal care to so- called granny midwives (Rooks, 1997) There are many different settings in which a CNM may practice. A CNM may engage in full-scope practice, which can include care of women from adolescence though the postmenopausal period. She or he may also choose one segment of practice—for example, ambulatory care or hospital care—or work exclusively with a population of interest, such as HIV-positive women or young adolescents. Nurse-midwives practice in urban, suburban, and rural areas. Their practice settings can include private practice (nurse-midwife— owned or physician-owned), hospitals, free-standing birth centers, clinics, or homes. Nurse-midwifery practice can be part of a group practice, with any combination of physicians, nurse-practitioners, physician assistants, or other health care providers, or solo practice. The nurse-midwife's actual practice depends on the needs of the population being served, willingness to undertake a variety of functions or roles, particular requests of patients, availability of physicians and nurse-midwife colleagues for backup and coverage and, finally, personal and philosophical beliefs of the individual midwife (Ament, 2007). A nurse-midwife—assisted birth can take place in homes, free-standing birth centers, birth centers in hospitals, or traditional hospital settings (community, regional, or tertiary). For nurse-midwives and the women for whom they provide care, the choice of setting may be a matter of philosophy, comfort, convenience, or degree of medical risk, or a combination of these factors. Each setting has unique advantages and disadvantages. Home births are very family-centered. Risks of iatrogenic and nosocomial infections are minimized. After the birth, the woman can rest or sleep in her own bed, nurse her infant at will, and enjoy the attention and support of her family and friends. A study by Hutton and coworkers (2009) documented the outcomes associated with planned home and planned hospital births in low-risk women attended by midwives in Ontario Canada. The rate of perinatal and neonatal mortality was very low for both groups (0.1%), and no between-group differences in morbidity or mortality were noted. Access to emergency transfer is critical to safe care and good outcomes, as is an integrated maternity care system with excellent communication among providers (Home Birth Consensus Summit, 2011). Analgesia and regional anesthesia are not available in the home setting. The free-standing birth center has a homelike environment, with some select emergency equipment. Most birth centers do not use analgesics or narcotics. Local anesthesia may be used for perineal repair. Disadvantages are similar to those of a home birth in that emergency transport to a hospital may be necessary if the mother or baby develops complications during labor or birth. Most families are discharged within 6 to 12 hours of birth. Current U.S. hospital units for labor and birth tend to be dual-purpose rooms; women labor and give birth in the same room, and almost all rooms are private. The room has a rocking chair, pull-out couch, and private bath, with a tub or shower. Although individual and nicely appointed, these rooms are part of the larger medical environment, with fetal monitoring, operating rooms, anesthesia services, and immediate access to neonatal intensive care. The support people available (nurses, physicians) may not hold the same philosophy of birth as a midwife. Even for a low-risk woman, there is more of a tendency to intervene than support a normal physiologic birth. There is a production pressure to keep things moving and a reliance on technology that is palpable in a busy obstetric unit. The traditional hospital labor, delivery, and maternity units are designed to care for several women at a time, making the units easier for staff to function but not necessarily conducive to the normal labor process. These units are well suited for high-risk women and infants who need special care nurseries. However, midwife-attended births in the United States currently occur mostly in a hospital environment. Therefore, it is incumbent on the midwife to help create an atmosphere of normalcy and trust in the midst of a culture of technology. o Certified registered nurse anesthetist-1945 roots of nurse anesthesia in the United States can be traced to the late nineteenth century. During the 1860s, two key events converged—the widespread use of the newly discovered chloroform anesthesia and the demand for such treatment for wounded soldiers during the American Civil War (1861 to 1865). In 1861, except for Catholic sisters and Lutheran deaconesses, there were few professional nurses in the United States. There were only a handful of nurse training schools1 in the country and, for the most part, laywomen cared for families and friends when they were ill. When the first shots were fired on Fort Sumter and Civil War broke out, thousands of laywomen from the North and South volunteered to nurse. Because of social restrictions, these women actually did little hands- on nursing. Instead, they helped by reading to patients, serving them broths and stimulants such as tea, coffee, and alcohol, and assisting with the preparation of food in diet kitchens. Catholic sisters who nursed were given more freedom to provide direct care; their work included assisting in surgery, particularly with the administration of chloroform. Because the administration of chloroform was a relatively simple procedure in which the anesthetizer poured the drug over a cloth held over the patient's nose and mouth, the nuns quickly mastered this technique, providing the surgeons with invaluable assistance during the war (Jolly, 1927; Wall, 2005). At St. Mary's Hospital in Rochester, Minnesota, Dr. William Worrall Mayo was among the first physicians in the country to recognize and train nurse anesthetists formally. In 1889, Dr. W.W. Mayo hired Edith Granham to be his anesthetist and office nurse. Subsequently, he hired Alice Magaw (later referred to as the “mother of anesthesia”; Keeling, 2007) CRNAs provide services in conjunction with other health care professionals such as surgeons, dentists, podiatrists, and anesthesiologists in diverse clinical settings. These APNs practice in a variety of clinical environments. Nurse anesthetists provide anesthesia services on a solo basis, in groups, and collaboratively. Some CRNAs have independent contracting arrangements with physicians or hospitals. Today, most surgery is performed on a same-day admission or outpatient basis. Anesthesia practices have adapted to this change from a predominantly inpatient model for surgery. A number of mechanisms, ranging from preoperative telephone interviews to preanesthesia clinics, are used to conduct preanesthesia assessment and allow anesthesia providers an opportunity to discuss care options, procedures, and risks with patients. However, detailed physical assessment and establishing a rapport between the anesthesia provider and patient often still occurs on the day of surgery. • Essentials of masters and doctoral education for APNs – Initially, this initiative was aimed at ensuring adequate educational preparation for APNs and was developed in response to the reality of ever-increasing curricular requirements in master's programs throughout the country (Keeling, Kirschgessner & Brodie, 2010). As originally proposed by the AACN, the DNP would standardize practice entry requirements for all APNs by the year 2015, assuring the public that each APN would have had 1000 supervised clinical hours prior to entering the practice setting. (The DNP has also broadened to include nurses with specialties such as informatics, administration, and public health. See Chapter 3 for further discussion of DNP education for non- APNs.) Moreover, the proposed curriculum for DNPs would include competencies deemed essential for nursing practice in the twenty-first century, including the following: (1) scientific underpinnings for practice; (2) organizational and systems leadership; (3) clinical scholarship and analysis for evidence-based practice; (4) information systems technology; (5) health care policy; (6) interprofessional collaboration; and (7) clinical prevention and population health (AACN, 2006). Although it is too early to evaluate this initiative from a historical perspective, the national dialogue to move APN education to a practice doctorate offers significant opportunity for the profession to connect scientific evidence and practice (Magyary, Whitney, & Brown, 2006). Expanded educational preparation could position APNs to be vital players in the translation of research evidence at the point of care, help nursing education achieve parity with physician education, and potentially decrease interprofessional tensions. • Core competencies of practice- 1- Although clinical expertise is a central ingredient of an APN's practice, the direct care practice of APNs is distinguished by six characteristics: (1) use of a holistic perspective; (2) formation of therapeutic partnerships with patients; (3) expert clinical performance; (4) use of reflective practice; (5) use of evidence as a guide to practice; and (6) use of diverse approaches to health and illness management 2-Guidance and coaching 3-Consultation 4-Evidence-based practice 5-Leadership 6- Collaboration 7- Ethical decision making • _ Fenton and Brykczynski’s Expert Practice Domains The seven domains are as follows (Benner, 1984): 1-the helping role, 2-administering and monitoring therapeutic interventions and regimens 3-effective management of rapidly changing situations 4-diagnostic and monitoring function 5-teaching and coaching function 6- monitoring and ensuring the quality of health care practices 7-organizational and work role competencies. • _Practice environments, regulation, reimbursement Later in the decade, with the new requirement that CRNAs have a master's degree, the number of nurse anesthesia education programs declined significantly, largely because of the closure of many small certification programs. However, the new requirement that programs offer a graduate degree did, in fact, promote nurse anesthesia eduction. In 1973, the University of Hawaii opened the first master's degree program for nurse anesthesia, moving the role forward in the evolving criteria of advanced practice nursing. Reimbursement for CRNA practice was not as clear-cut. In fact, third- party payment had its own set of issues. Beginning in 1977, the AANA led a long and complex effort to secure third-party reimbursement under Medicare so that CRNAs could bill for their services. The organization would finally succeed in 1989. Meanwhile, the financial threat posed by CRNAs to physicians was the source of continued interprofessional conflicts with medicine. During the second half of the twentieth century, tensions escalated, particularly in relation to malpractice policies, antitrust, and restraint of trade issues. In 1986, Oltz v. St. Peter's Community Hospital established the right of CRNAs to sue for anticompetitive damages when anesthesiologists conspired to restrict practice privileges. A second case, Bhan v. NME Hospitals, Inc. (1985), established the right of CRNAs to be awarded damages when exclusive contracts were made between hospitals and physician anesthesiologists. Undeniably, CRNAs were winning the legal battles and overcoming practice barriers erected by hospital administrators and physicians. The creation of the National Association of Clinical Nurse Specialists (NACNS), followed by third- party reimbursement for their services, represented two major steps for the CNS. NACNS was formed In 1995, promoting organization of the role at the national level. Soon thereafter, in 1997, the Balanced Budget Act (Public Law 105-33) specifically identified the CNS as eligible for Medicare reimbursement (Safriet, 1998). The law, providing Medicare Part B direct payment to NPs and CNSs, regardless of their geographic area of practice, allowed both types of APNs to be paid 85% of the fee paid to physicians for the same services. Moreover, the law's inclusion and definition of CNSs corrected the previous omission of this group for reimbursement (Safriet, 1998). The possibility of reimbursement for services was an important step in the continuing development of the CNS role because hospital administrators would continue to focus on the cost of having APNs provide patient care. Some CNS roles require prescription of medications and the ability of a CNS to prescribe depends on state regulations. As of January 2012, CNSs have independent prescriptive authority in 11 states and in Washington, DC, no prescribing authority in 15 states, and nonindependent prescriptive authority in the remaining 24 states (National Council of State Boards of Nursing, 2012). NPs worked_ outpatient clinics, health maintenance organizations, health departments, community health centers, rural clinics, schools, occupational health clinics, and private offices • _Dreyfus & Dreyfus: Development of the APN role-novice to expert theory (add theories and models) Acquisition of knowledge and skill occurs in a progressive movement through the stages of performance from novice to expert, as described by Dreyfus and Dreyfus (1986, 2009), who studied diverse groups, including pilots, chess players, and adult learners of second languages. The skill acquisition model has broad applicability and can be used to understand many different skills better, ranging from playing a musical instrument to writing a research grant. The most widely known application of this model is Benner's (1984) observational and interview study of clinical nursing practice situations from the perspective of new nurses and their preceptors in hospital nursing services. Although this study included several APNs, it did not specify a particular education level as a criterion for expertise. As noted in Chapter 3, there has been some confusion about this criterion. The skill acquisition model is a situation-based model, not a trait model. Therefore, the level of expertise is not an individual characteristic of a particular nurse but is a function of the nurse's familiarity with a particular situation in combination with his or her educational background. This model could be used to study the level of expertise required for other aspects of advanced practice, including guidance and coaching, consultation, collaboration, evidence-based practice ethical decision making, and leadership (see Brykczynski [2009] for a detailed discussion of the Dreyfus model). The overall trajectory expected during APN role development is shown in Figure 4-1; however, each APN experiences a unique pattern of role transitions and life transitions concurrently. For example, a professional nurse who functions as a mentor for new graduates may decide to pursue an advanced degree as an APN. As an APN graduate student, she or he will experience the challenges of acquiring a new role, the anxiety associated with learning new skills and practices, and the dependency of being a novice. At the same time, if this nurse continues to work as a registered nurse, his or her functioning in this work role will be at the competent, proficient, or expert level, depending on experience and the situation. On graduation, the new APN may experience a limbo period, during which the nurse is no longer a student and not yet an APN, while searching for a position and meeting certification requirements (see later). Once in a new APN position, this nurse may experience a return to the advanced beginner stage as he or she proceeds through the phases of role implementation. Even after making the transition to an APN role, progression in role implementation is not a linear process. As Figure 4-1 indicates, there are discontinuities, with movement back and forth as the trajectory begins again. Years later, the APN may decide to pursue yet another APN role. The processes of role acquisition, role implementation, and novice to expert skill development will again be experienced—although altered and informed by previous experiences —as the postgraduate student acquires additional skills and knowledge. Role development involves multiple, dynamic, and situational processes, with each new undertaking being characterized by passage through earlier transitional phases and with some movement back and forth, horizontally or vertically, as different career options are pursued. Direct-entry students who are non-nurse college graduates (NNCGs) and APN students with little or no experience as nurses before entry into an APN graduate program would be expected to begin their APN role development at the novice level (see Fig. 4-1). Some evidence indicates that although these inexperienced nurse students may lack the intuitive sense that comes with clinical experience, they avoid the role confusion associated with letting go of the traditional RN role commonly reported with experienced nurse students (Heitz, Steiner, & Burman, 2004). This finding has implications for APN education as the profession moves toward the Doctor of Nursing Practice (DNP) as the preferred educational pathway for APN preparation (American Association of Colleges of Nursing [AACN], 2006). Another significant implication of the Dreyfus model (Dreyfus & Dreyfus, 1986, 2009) for APNs is the observation that the quality of performance may deteriorate when performers are subjected to intense scrutiny, whether their own or that of someone else (Roberts, Tabloski, & Bova, 1997). Novice and Advanced Practice Nurses Participate in professional organizations and become involved in regulatory activities, such as educating lawmakers, providing public comment on APRN issues, writing letters, and being part of campaign activities: •Monitor current APRN legislation and legislation that affects patients. •Offer to participate in test-writing committees for national certification examinations as item writers and/or reviewers. •Respond to offers to review, edit, and provide feedback about circulated draft regulatory policies that directly affect advanced practice nursing education and practice. Experienced and Expert Advanced Practice Nurses • Seek out a gubernatorial appointment to the board of nursing or advanced practice committee that advises the board of nursing in your state. • Seek membership as the APRN or consumer member of the advisory council for the state medical board or state board of pharmacy. • Seek appointment to CMS panels on which Medicare and Medicaid provider issues are decided. • Seek appointment to hospital privileging committees and ensure that privileging materials are appropriate for APRNs. • Seek appointment on advisory committees and task forces that are advising the NCSBN and other regulatory and credentialing bodies. • Provide public comment on draft legislation regarding health care and health care providers. • Offer testimony at state and national hearings at which proposed regulatory changes in advanced practice nursing regulation, prescriptive authority, and reimbursement schemes will be discussed. To accomplish these activities, APRNs need to use research data, a powerful tool for shaping health policy (Hamric, 1998). By actively participating in the regulatory process, APRNs ensure themselves of a strong voice in regulatory and credentialing processes. At the very least, it is incumbent on the practicing APRN to monitor the process carefully through websites and newsletters to stay informed. • _Novice to Expert Skill Acquisition Model • _Role Concepts; Concept Definition Examples 1- Role stress- A situation of increased role performance demand Ex. Returning to school while maintaining work and family responsibilities 2- Role strain- Subjective feeling of frustration, tension, or anxiety in response to role stress Ex. Feeling of decreased self-esteem when performance is below expectations of self or significant others 3- Role stressors- Factors that produce role stress Financial, personal, or academic demands and role expectations that are ambiguous, conflicting, excessive, or unpredictable 4- Role ambiguity- Unclear expectations, diffuse responsibilities, uncertainty about subroles Ex. Some degree of ambiguity in all professional positions because of the evolving nature of roles and expansion of skills and knowledge 5- Role incongruity- A role with incompatibility between skills and abilities and role obligations or between personal values, self-concept, and role obligations Ex. An adult NP in a role requiring pediatric skills and knowledge 7- Role transition -A dynamic process of change over time as new roles are acquired Ex. Changing from a staff nurse role to an APN role 8- Role insufficiency- Feeling inadequate to meet role demands Ex. New APN graduate experiencing the imposter phenomenon (Arena & Page, 1992; Brown & Olshansky, 1998) 9- Role supplementation- Anticipatory socialization Ex. Role-specific educational components in a graduate program 10- Role Implementaion- an example of a situational transition (Schumacher & Meleis, 1994), which has been described as a progressive movement through phases. There is general agreement that significant overlap and fluidity exist among the phases. However, for purposes of discussion, the phases will be considered sequentially. 6-Role conflict- Occurs when role expectations are perceived to be mutually exclusive or contradictory Ex. Role conflict between APNs and other nurses and between APNs and physicians The historical development of APN roles has been fraught with conflict and controversy in nursing education and nursing organizations, particularly for CNMs (Varney, 1987), NPs (Ford, 1982), and CRNAs (Gunn, 1991; see also Chapter 1). Relationships among these APN groups and nursing as a discipline have improved markedly in recent years, but difficulties remain (Fawcett, Newman, & McAllister, 2004). The degree to which APN roles demonstrate a holistic nursing orientation as opposed to a more disease-specific medical orientation remains problematic (see value-added Communication difficulties that underlie intraprofessional role (1) at an organizational level; (2) in educational programs; (3) in the literature; and (4) in direct clinical practice. Kimbro (1978) initially described these communication difficulties in reference to CNMs, but they are relevant for all APN roles. The fact that CNSs, NPs, CNMs, and CRNAs each have specific organizations with different certification requirements, competencies, and curricula creates boundaries and sets up the need for formal lines of communication. Communication gaps occur in education when courses and textbooks are not shared among APN programs, even when more than one specialty is offered in the same school. Specialty- specific journals are another formal communication barrier because APNs may read primarily within their own specialty and not keep abreast of larger APN issues. In clinical settings, some APNs may be more concerned with providing direct clinical care to individual patients, whereas staff nurses and other APNs may be more concerned with 24-hour coverage and smooth functioning of the unit or institution. These differences may set the stage for intraprofessional role conflict. During the 1980s and 1990s, when there was more confusion about the delineation of roles and responsibilities between RNs and NPs, RNs would sometimes demonstrate resistance to NPs by refusing to take vital signs, obtain blood samples, or perform other support functions for patients of NPs (Brykczynski, 1985; Hupcey, 1993; Lurie, 1981), and they were not admonished by their supervisors for these negative behaviors. These behaviors are suggestive of horizontal violence (a form of hostility), which may be more common during nursing shortages (Thomas, 2003). Roberts (1983) first described horizontal violence among nurses as oppressed group behavior wherein nurses who were doubly oppressed as women and as nurses demonstrated hostility toward their own less powerful group, instead of toward the more powerful oppressors. Recognizing that intraprofessional conflict among nurses is similar to oppressed group behavior can be useful in the development of strategies to overcome these difficulties (Bartholomew, 2006; Brykczynski, 1997; Farrell, 2001; Freshwater, 2000; Roberts, 1996; Rounds, 1997; see Chapter 11). According to Rounds (1997), horizontal violence is less common among NPs as a group than among RNs generally. Over the years, as the NP role has become more accepted by nurses, there appear to be fewer cases of these hostile passive- aggressive behaviors, often currently referred to as bullying, toward NPs. However, they are still reported in APN transition literature (Heitz et al., 2004; Kelly & Mathews, 2001). • _Conceptual models for APNs a conceptual model designed to facilitate the evaluation of the acute care nurse practitioner (ACNP) role in acute care settings (Fig. 23-2). Developed in Canada, this model was adapted from a nursing role effectiveness model and is also a derivative of Donabedian's framework, with components focusing on structure (patient, ACNP, and organization), process (ACNP role components, role enactment, and role functions) and outcome (goals and expectations of the ACNP role). A concern with this model is the use of the term goals and expectations for outcome and the focus on quality of care, which is a dimension of care delivery process rather than outcome. (mechanisms) within the ACNP direct care component are expected to achieve patient and cost outcomes: (1) providing comprehensive care; (2) ensuring continuity of care; (3) coordinating services; and (4) providing care in a timely way (Sidani & Irvine, 1999). According to this model, the selection of outcome indicators is guided by the role and functions assumed by the ACNP, how the role is enacted, and the ACNP's particular practice model. Like the models before it, the usefulness of this framework for determining APN impact is limited by its virtual absence of testing in clinical settings. • _Conceptualization barriers Conceptualizations of the Nature of Advanced Practice Nursing The APN role-specific models promulgated by professional organizations naturally lead to the following questions: •What is common across APN roles? •Can an overarching conceptualization of advanced practice nursing be articulated? •How can one distinguish among basic, expert, and advanced levels of nursing practice? Some authors have attempted to discern the nature of advanced practice nursing and address these questions. The extent to which they considered all existing APN roles is not always clear; some authors have considered only the CNS and NP roles. In this section, the focus is on those frameworks that address the nature of advanced practice nursing. The term role is used loosely and variably, sometimes seeming to describe functions (e.g., management, teaching, research, consultation) and sometimes taking a psychological or sociologic perspective on developing social roles in relation to environment. Dictionary definitions add to the confusion by using the terms role, function, occupation, and duties to define one another. For example, role is generally used to refer to titles appearing in legal documents, certification programs, or job descriptions. From this perspective, the CNS, NP, CNM, and CRNA designations represent advanced practice roles. From the present review of a number of frameworks, domain and competency may be the most commonly used concepts in explaining nursing practice and advanced practice nursing. However, meanings are not consistent. Hamric's Model, which uses the terms roles and competencies, is the only one that is integrative— that is, it explicitly considers all four APN roles. Because it is integrative, has remained relatively stable since 1996, has informed the development of the DNP Essentials and CNS competencies, and is widely cited, it will be discussed first, enabling the reader to consider the extent to which important concepts are addressed by other models. Otherwise, the models are discussed in chronologic order. In most cases, new literature on the models discussed here were not found in literature searches in the Cumulative Index to Nursing and Allied Health Literature • _Hamric’s Integrative Model an integrative understanding of the core of advanced practice nursing, based on literature from all APN specialties (Hamric, 1996, 2000, 2005, 2009; see Chapter 3). Hamric proposed a conceptual definition of advanced practice nursing and defining characteristics that included primary criteria (graduate education, certification in the specialty, and a focus on clinical practice with patients) and a set of core competencies (direct clinical practice, collaboration, guidance and coaching, evidence- based practice, ethical decision making, consultation, and leadership). This early model was further refined, together with Hanson and Spross in 2000 and 2005, based on dialogue among the editors. Key components of the model (Fig. 2-4) include the primary criteria for advanced nursing practice, seven advanced practice competencies with direct care as the core competency on which the other competencies depend, and environmental and contextual factors that must be managed for advanced practice nursing to flourish. • _Calkin’s Model of Advanced Practice Nursing The model evolved from the delineation of the domains and competencies of the acute care NP (ACNP) role, conceptualized as a role that “combines the clinical skills of the NP with the systems acumen, educational commitment, and leadership ability of the CNS” (Ackerman et al., 1996, p. 69). The five domains are direct comprehensive patient care, support of systems, education, research, and publication and professional leadership. All domains have direct and indirect activities associated with them. In addition, necessary unifying threads influence each domain, which are illustrated as circular and continuous threads in the figure • _Brown’sFramework for Advanced Practice Nursing developed a conceptual framework for the entire field of advanced practice nursing, including the environments that surround and impact upon practice (Fig. 2-7). Studies were synthesized to propose a conceptual framework that included 4 main and 17 specific concepts (specific concepts are in parentheses): environments (society, health care economy, local conditions, nursing, advanced practice community); role legitimacy (graduate education, certification, licensure); advanced practice nursing (scope, clinical care, competencies, managing health care environments, professional involvement in health care discourse); and profession, individual APN outcomes). The central concept, conceptually and visually, is advanced practice nursing. Brown (1998) proposed a definition of advanced practice nursing: “professional health care activities that (1) focus on clinical services rendered at the nurse-client interface, (2) use a nursing orientation, (3) have a defined but dynamic and evolving scope, and (4) are based on competencies that are acquired through graduate nursing education.” • _Oberle and Allen At the time that they wrote, Oberle and Allen (2001) asserted that conceptualizations of advanced practice nursing were limited; particular gaps were the lack of clear distinctions between the expert practice of experienced nurses and of APNs, as well as the lack of nursing theories to address such levels of practice. The authors noted that, although the literature on expert nursing is mostly focused on expertise as it unfolds in the context of relationships, the literature on advanced practice nursing seems to focus more on expertise as “skills acquisition and critical thinking abilities.” According to Oberle and Allen (2001), any conceptualization of advanced practice nursing should be embedded in a conceptual understanding of nursing, so the authors first proposed a conceptualization of nursing practice. They refer to practice by the term praxis, which captures the values-oriented, reflective, and creative nature of the work of nurses. They conceive of nursing as a dialectic (back and forth) process between the nurse's knowledge and his or her experiences and relationships with patients. In this process, the nurse considers general and particular knowledge, synthesizes this knowledge, and generates options for care that can be offered to the patient. By this, they mean that experiences with patients (and, presumably, reflection on these experiences) extend nurses' knowledge, this new knowledge informs their practice with subsequent patients, and experiences with applying the new knowledge gained from experience and reflection again inform and extend their thinking, a dialectic process that occurs repeatedly. As nurses accumulate experience, this dialectic process that occurs in relationships with patients contributes to developing expertise. Client's meanings, desired outcomes, and acceptable actions—know who. • Dialectic—the process whereby nurses consider general and particular knowledge and synthesize this information to generate options and propose actions to the patient to move the patient toward his or her goals. • Synthesis—know that (a particular action is called for in a specific situation). • Practical wisdom—know when (a particular action ought to be taken). The dialectic process and experience with synthesis, informed by praxis, lead to the development of practical wisdom. • Telos—human flourishing (the object of nursing care, of which health is a part—health is a resource for human flourishing. • Options—possibilities for actions identified by nurse. • _Shuler Model of Nurse Practitioner Practice This model is complex and the review for this edition found no additional reports using this model. Because of its historical importance as an early NP model, the Shuler model (Shuler & Davis, 1993a) is briefly discussed. Readers should refer to the original article to see the full model. Shuler's experience integrating nursing and medical knowledge skills into the NP role led to the development of a conceptual model that would make apparent the unique contributions of NPs, purposefully addressing the need for a model that reflects the acquisition of expertise by the NP in two health care disciplines, nursing and medicine. Shuler's Nurse Practitioner Practice Model is a complex systems model that is holistic and wellness-oriented. It is definitive and detailed in terms of how the NP-patient interaction, patient assessment, intervention, and evaluation should occur (Shuler & Davis, 1993a). It is complex and its value for understanding NP practice may not become clear until one is in practice. Table 2-2 outlines key model constructs and related theories, many of which should be familiar to students. Knowing that these familiar concepts are embedded in this comprehensive model may help readers appreciate its potential usefulness. Shuler's model is intended “to impact the NP domain at four levels: theoretical, clinical, educational, and research” (Shuler & Davis, 1993a). A close review of the model indicates that it addresses important components of a model of advanced practice nursing, such as the following: (1) nursing's metaparadigm (person, health, nursing, and environment); (2) the nursing process; (3) assumptions about patients and nurse practitioners; and (4) theoretical concepts relevant to practice. The model could be characterized as a network or system of frameworks. • _Ball and Cox Theory they were required to be master's-prepared or graduate students preparing for an advanced practice role. The investigators conducted interviews and made observations of the participants over a 3-year period. The theory of legitimate influence emerged from this study (Fig. 2-10). The figure illustrates the range of activities in which APNs engage to “enhance patient stay” and “improve patient outcomes.” This study provided empirical support for many of the competencies described in the models reviewed in this chapter. For example, findings from their work are consistent with the competencies in Hamric's model (Table 2-3). Ball and Cox's work suggests that the activities of APNs, in this case NPs and CNSs, are strategic and focused and that some activities involve direct service to patients, whereas others are aimed at communication and system issues. • _Practice Models for APNs The profession has embraced a wide variety of graduate educational models for preparing APNs, including direct-entry programs for non-nurse college graduates and RN to MSN programs. It is highly unlikely that doctoral preparation for advanced practice nursing will supplant these various master's programs by 2015, as originally proposed by the AACN. Debate on the issue of the DNP continues • _AACN Synergy Model American Association of Critical-Care Nurses Synergy Model. The Synergy Model delineates three levels of outcomes—those derived from the patient, those derived from the nurse, and those derived from the health care system. • _ Dunphy and Winland-Brown Circle of Caring A central premise of Dunphy and Winland-Brown's model (1998) is that the health care needs of individuals, families, and communities are not being met in a health care system that is dominated by medicine and one in which medical language (i.e., the International Classification of Disease Codes [ICD-10-CM]) is the basis for reimbursement. They proposed the “Circle of Caring: A Transformative Model” to foster a more active and visible nursing presence in the health care system and to explain and promote medical-nursing collaboration. Dunphy and Winland-Brown's transformative model, which has been slightly revised since its original publication (Dunphy, Winland-Brown, Porter, et al., 2011; Fig. 2-12) is a synthesized problem-solving approach to advanced practice nursing that builds on nursing and medical models • _Advanced Practice Professional Organizational Perspectives Practice with individual clients or patients is the central work of the field; it is the reason for which nursing was created. The following questions are the kinds of questions a conceptual model of advanced practice nursing should answer: •What is the scope and purpose of advanced practice nursing? •What are the characteristics of advanced practice nursing? •Within what settings does this practice occur? •How do APNs' scopes of practice differ from those of other providers offering similar or related services? •What knowledge and skills are required? •How are these different from other providers? •What patient and institutional outcomes are realized when APNs deliver care? how are these outcomes different from other providers? •When should health care systems employ APNs and what types of patients particularly benefit from APN care? •For what types of pressing health care problems are APNs a solution in terms of improving outcomes, quality of care, and cost- effectiveness? • _APRN Consensus Model for regulation: Licensure, Accreditation, Certification, Education (LACE) An APRN is defined as a nurse who meets the following criteria (APRN Consensus Model, 2008): • Completes an accredited graduate-level education program preparing him or her for one of the four recognized APRN roles and a population focus (see discussion in Chapter 3) • Passes a national certification examination that measures APRN role and population-focused competencies and maintains continued competence by national recertification in the role and population focus • Possesses advanced clinical knowledge and skills preparing him or her to provide direct care to patients; the defining factor for all APRNs is that a significant component of the education and practice focuses on direct care of individuals • Builds on the competencies of RNs by demonstrating greater depth and breadth of knowledge and greater synthesis of data by performing more complex skills and interventions and by possessing greater role autonomy • Is educationally prepared to assume responsibility and accountability for health promotion and/or maintenance, as well as the assessment, diagnosis, and management of patient problems, including the use and prescription of pharmacologic and nonpharmacologic interventions • Has sufficient depth and breadth of clinical experience to reflect the intended license • Obtains a license to practice as an APRN in one of the four APRN roles • _American Nurses Association As the “only full-service professional organization representing the interests of the nation's 3.1 million registered nurses through its constituent and state nurses associations and its organizational affiliates,” the American Nurses Association (ANA) and its constituent organizations have also been active in developing and promulgating documents that address advanced practice nursing. Two of these are particularly important as we consider contemporary conceptualizations of advanced practice nursing. ANA also establishes and promulgates standards of practice and competencies for RNs and APNs. In the second edition of their text, Nursing: Scope and Standards of Practice (ANA, 2010b), six standards of practice and 16 standards of professional performance are described. Of the 22 standards, one standard outlines additional expectations for APNs compared with RNs; Standard 5, “Implementation,” addresses the consultation and prescribing responsibilities of APRNs. Each standard is associated with competencies. It is in the description of the competencies that RN practice is differentiated from APNs and nurses prepared in a specialty at the graduate level. This document is must reading for APN students, practitioners, and others wishing to understand how basic, advanced, and specialized practice differ. In addition to these documents, ANA, together with the American Board of Nursing Specialties (ABNS), convened a task force on CNS competencies. For many reasons, including the recognition that developing psychometrically sound certifications for numerous specialties, especially for clinical nurse specialists (CNSs), would be difficult as the profession moved toward implementing the APRN Consensus Model, the ANA and ABNS convened a group of stakeholders in 2006 to develop and validate a set of core competencies that would be expected of CNSs entering practice (National Association of Clinical Nurse Specialists [NACNS]/National CNS Core Competency Task Force, 2010). This group was charged with identifying core, entry-level competencies that are common in CNS practice, regardless of specialty. This work is discussed later in this chapter in the section on NACNS. ANA continues to make numerous contributions to promoting clarity about all nursing roles, including advanced practice nursing. Its definitions of expansion, specialization, and advanced practice have remained consistent over time. ANA's Nursing: Scope and Standards of Practice (2010), should inform theoretical and empirical work that aims to differentiate nursing roles • _American Association of Colleges of Nursing Over the last decade, the AACN has undertaken two nursing education initiatives aimed at transforming nursing education. In 2006, AACN called for all APN preparation to take place at the doctoral level in practice-based programs (DNP), with master's level education being refocused on generalist preparation for roles such as clinical nurse leaders (CNLs) and staff and clinical educators. CNLs are not APNs (AACN, 2005, 2012a; Spross, Hamric, Hall, et al., 2004) and, therefore, are not included in this discussion of conceptualizations. Through these initiatives, and to the extent that the AACN and Commission on Collegiate Nursing Education (CCNE) influence accreditation, the DNP may become the preferred degree for most APNs, although this goal is controversial. Since the last edition, despite lingering disagreements, DNP education has advanced considerably. In 2006, there were 20 DNP programs; in 2011, there were 182. Similarly, enrollments in and graduation from DNP programs have also risen substantially (AACN, 2012). The DNP Essentials (AACN, 2006) are comprised of eight competencies for DNP graduates (Box 2-2). Graduates are expected to demonstrate the eight essentials on graduation. For APNs, “Essential VIII specifies the foundational practice competencies that cut across specialties and are seen as requisite for DNP practice” (AACN, 2006, p. 16; Box 2-3). Recognizing that DNP programs will prepare nurses for roles other than APN roles, the AACN acknowledged that organizations representing APNs are expected to develop Essential VIII as it relates to specific advanced practice roles and “to develop competency expectations that build upon and complement DNP Essentials 1 through 8” (AACN, 2006, p. 17). These Essentials affirmed that the advanced practice nursing core includes the three Ps (three separate courses)—advanced health and physical assessment, advanced physiology and pathophysiology, and advanced pharmacology—and is specific to APNs. The specialty core must include content and clinical practice experiences that help students acquire the knowledge and skills essential to a specific advanced practice role. These requirements were reconfirmed in the Consensus Model (2008). • _National Organization of Nurse Practitioner Faculties The mission of the NONPF is to provide leadership in promoting quality NP education. Since 1990, NONPF has fulfilled this mission in many ways, including the development, validation, and promulgation of NP competencies. As of 2012, there is only one set of NP core competencies in use (NONPF, 2012); the 2002 and 2006 competencies are available on the website but are no longer active. A brief history of the development of competencies for NPs is presented, in part because their development has influenced other APN models. • _National Association of Clinical Nurse Specialists Three spheres of influence are posited: patient, nurses and nursing practice, and organization or system, each of which requires a unique set of competencies (NACNS, 2004; Fig. 2-2). In addition, the statement outlined expected outcomes of CNS practice for each sphere and competencies that parallel those of the nursing process. Thus, CNSs have sphere-specific competencies of assessment, diagnosis, intervention, and evaluation. • _American Association of Nurse Anesthetists The CRNA's scope of practice was defined in the most recent revision of the AANA's Scope and Standards for Nurse Anesthesia Practice (2010a). The scope is followed by 10 items that can be characterized as clinical competencies or responsibilities (e.g., managing a patient's airway)—the direct clinical practice of CRNAs. CRNAs have seven additional responsibilities that are within the CRNA's scope of practice that can be characterized as leadership behaviors, including participation in research. Eleven standards and an interpretation for each are also listed. The purposes of the standards are as follows: (1) assist the profession in evaluating CRNA care; (2) provide a common foundation on which CRNAs can develop a quality practice; (3) help the public understand what they can expect from CRNAs; and (4) support and preserve the basic rights of patients. • _American College of Nurse-Midwives The scope of practice for CNMs (and certified midwives [CMs] who are not nurses) has been in four ACNM documents: “Definition of midwifery and scope of practice of CNMs and CMs” (ACNM, 2011a), the “Core competencies for basic midwifery practice” (ACNM, 2012a), “Standards for the practice of midwifery” (ACNM, 2011), and a “Code of ethics” (ACNM, 2008). The core competencies are organized into sixteen hallmarks that describe the art and science of midwifery and the components of midwifery care. The components of midwifery care include professional responsibilities, midwifery management processes, fundamentals, primary health care of women, and the childbearing family, within which are prescribed competencies. According to the definition, “CNMs are educated in two disciplines: nursing and midwifery” (ACNM, 2011a). Competencies “describe the fundamental knowledge, skills and behaviors of a new practitioner” (ACNM, 2012a). The hallmarks, components, and associated core competencies are the foundation on which midwifery curricula and practice guidelines are based. • _International Organizations the CNA published Advanced Nursing Practice: A National Framework, which defined advanced nursing practice, described educational preparation and regulation, identified the two APN roles (NP and CNS), and specified competencies in clinical practice, research, and leadership. In addition, they have issued position statements on advanced nursing practice (CNA, 2007), which affirm the key points in the national framework document and defined and described the roles and contributions to health care of nurse practitioners (2009a) and clinical nurse specialists (2009b). Furthermore, leaders have undertaken an evidence-based, patient-centered, coordinated effort (called a decision support synthesis) to develop, implement, and evaluate the APN roles of the CNS and NP in Canada (DiCenso, Martin-Meisener, Bryant-Lukosius, et al., 2010), a process different from the one used to advance APN roles in the United States. This process included a review of 468 published and unpublished articles and interviews conducted with 62 key informants and four focus groups that included a variety of stakeholders. The purpose of this work was to “describe the distinguishing characteristics of CNSs and NPs relevant to Canadian contexts,” identify barriers and facilitators to effective development and use of APN roles, and inform the development of evidence-based recommendations that individuals, organizations, and systems can use to improve the integration of APNs into Canadian health care. • _New innovative roles – educator, administrator, informatics • _Competencies of Advanced Practice Nursing Direct care is the central competency of advanced practice nursing. This competency informs and shapes the execution of the other six competencies. Direct care is essential for a number of reasons. To consult, collaborate, and lead clinical staff and programs effectively, an advanced practice nurse (APN) must have clinical credibility. With the deep clinical and systems understanding that APNs possess, they facilitate the care processes that ensure achievement of outcomes for individuals and groups of patients. Advanced practice occurs within a health care system that is constantly changing—changing delivery models, reimbursement structures, regulatory requirements, population-based management, and even proposed changes in the basic educational requirements for advanced practice nurses through the Doctor of Nursing Practice (DNP) degree. For the purposes of this chapter, the terms direct care and direct clinical practice refer to the activities and functions that APNs perform within the patient-nurse interface. Depending on the focus of an APN's practice, the patient may, and often does, include family members and significant others. The activities that occur in this interface or as direct follow-up are unique because they are interpersonally and physically connected with a particular patient for the purpose of promoting that patient's health or well-being. Many important processes transpire at this point of care, including the following: •The patient-provider therapeutic partnership is established. •Health problems become mutually understood through information gathering and effective communication. •Health, recovery, or palliative goals are expressed by the patient. •Management and treatment options are explored. • Physical acts of diagnosis, monitoring, treatment, and pharmacologic and non-pharmacologic therapy are performed 2- Guidance and coaching is a well-established expectation of the advanced practice nurse (APN). For example, the ability to establish therapeutic relationships and guide patients through transitions is incorporated into the DNP Essentials (American Association of Colleges of Nursing [AACN], 2006). Although there is variability in how this aspect of APN practice is described, standards that specifically address therapeutic relationships and partnerships, coaching, communication, patient- family—centered care, guidance, and/or counseling can be found in competency statements for most APN roles. Definition coaching has long been used in a variety of disciplines and settings. Even as a broad definition of health coaching is evolving, it is important for APNs and other health professionals who coach patients in areas of health, wellness, and illness to represent the nature of their discipline- specific coaching accurately 3- Consultation is an important aspect of advanced practice nursing. As advanced practice nursing has evolved over the years, the consultation competency has received increased attention and is now explicitly addressed as a role expectation. The collective input of others experts in their field to help diagnose and treat a patient. The American Association of Colleges of Nursing (AACN, 2006, 2011) has highlighted consultation as an essential component of master's and Doctor of Nursing Practice (DNP) programs. In defining the essentials of DNP education, the AACN emphasizes the need for exquisite skills in the areas of collaboration and consultation for DNP-prepared advanced practice nurses (APNs). Collaboration is considered in depth in Chapter 12. The complexities of today's health care settings require that all APNs offer and receive consultation and understand, clinically and legally, the differences between consultation and collaboration. 4- Evidence-based practice (EBP) is defined as the conscientious, explicit, and judicious use of (Sackett et al., 1996). It has evolved into a dominant approach for clinical decision making and a core competency for advanced practice nursing (see Chapter 3). Although components tend to overlap, three levels of this core competency can be identified: (1) interpretation and use of EBP principles in individual clinical decision making; (2) interpretation and use of EBP principles to determine policies for patient care; and (3) use of EBP to evaluate clinical practice. Evidence-based practice is based on a four-step process: (1) formulation of a clinical question; (2) identification and retrieval of pertinent research findings based on literature review; (3) extraction and critical appraisal of data from pertinent studies; and (4) clinical decision making based on results of this process. Principles of EBP are used for clinical decision making for individual patients, constructing and applying clinical practice guidelines, and determining policies for delivering care to large groups 5- Leadership is a core competency of advanced practice nursing, but the concept has some unique characteristics in the APN context. Our conceptualization of APN leadership involves three distinct defining characteristics—mentoring, innovation, and activism. Calls for systems redesign and transformation (Institute of Medicine [IOM], 2011, 2001, 2000; Institute for Healthcare Improvement [IHI], 2011; Leape, Berwick, Clancy, et al., 2009), changes in health professional edu cation (American Association of Colleges of Nursing [AACN], 2006), and core interdisciplinary competencies for health professionals (Canadian Interpro fessional Health Collaborative [CIHC], 2010; Greiner & Knebel, 2003; Health Sciences Institute, 2005; Interpro fessional Collaborative Initiative [IPEC], 2011) have important implications for the leadership competency in APN education and practice. To provide leadership in individual patient care situations, APNs must be able to assess the clinical microsystems in which they provide care, understand the macrosystems that influence the smaller systems, determine the need for redesign to improve safety, quality, and reliability, and evaluate the results. In short, systems leaders must be able to identify the need for innovation and change and implement strategies to achieve it. In partnership with others, APNs craft approaches to evaluate, reassess, and implement systems redesign and innovation. (see leadership expanded) 6- Collaboration competency is important in that it is fundamental to successful APN practice. The presence or absence of collaborative relationships affects patient care, including the cost and quality of care. Patients assume that their health care providers communicate and collaborate effectively; thus, patient dissatisfaction with care, unsatisfactory clinical outcomes, and clinician frustration can often be traced to a failure to collaborate with other members of the health care team. Collaboration depends on clinical and interpersonal expertise and an understanding of factors that can promote or impede efforts to establish collegial relationships. The primary focus of this chapter is on collaboration between and among individuals and work groups within organizations and across larger health care delivery systems. Our goal in this chapter is to define collaboration and make more explicit the values, behaviors, structures, and processes that facilitate effective collaboration. Furthermore, the current trends in health care promulgated by the IOM Futures of Nursing report (2011) and the Patient Protection and Affordable Care Act (PPACA; U.S. Department of Health and Human Services [HHS], 2011) and recent education initiatives toward a rebirth of interprofessional collaboration will be described • _Collaboration definition of collaboration as a dynamic, interpersonal process was developed for the first edition of this text (Hanson & Spross, 1996): “Collaboration is a dynamic, interpersonal process in which two or more individuals make a commitment to each other to interact authentically and constructively to solve problems and to learn from each other to accomplish identified goals, purposes, or outcomes. The individuals recognize and articulate the shared values that make this commitment possible.” 7- Ethical decision making is a basic intenet of the central definition of advanced practice nursing (see Chapter 3) that skill in ethical decision making is one of the core competencies of all APNs. In addition, the Doctor of Nursing Practice (DNP) essential competencies emphasize leadership in developing and evaluating strategies to manage ethical dilemmas in patient care and organizational arenas (American Association of Colleges of Nursing [AACN], 2006). This chapter explores the distinctive ethical decision-making competency of advanced practice nursing, the process of developing and evaluating this competency, and barriers to ethical practice that APNs can expect to Ethical principles related to practice and decision making • Principle of respect for autonomy: The duty to respect others' personal liberty and individual values, beliefs, and choices • Principle of non-maleficence: The duty not to inflict harm or evil • Principle of beneficence: The duty to do good and prevent or remove harm • Principle of formal justice: The duty to treat equals equally and treat those who are unequal according to their needs • Rule of veracity: The duty to tell the truth and not to deceive others • Rule of fidelity: The duty to honor commitments • Rule of confidentiality: The duty not to disclose information shared in an intimate and trusted manner • Rule of privacy: The duty to respect limited access to a person o Leadership Expanded o Definition - defined the term transformational leadership as a process whereby “the purposes of the leader and follower become fused, creating unity, wholeness and a collective purpose” (p. 83). Transformational leadership can lead to changes in values, attitudes, perceptions, and/or behaviors on the part of the leader and the follower and lays the groundwork for further positive change. Thus, transformational leadership occurs when people interact in ways that inspire higher levels of motivation and morality among participants. How do leaders do this? Transformational leaders analyze a situation to understand the particular leadership needs and goals; they use this information, together with their interpersonal skills, to motivate, stimulate, share with, conciliate, and satisfy their followers in an interdependent interactional exchange. DePree (1989) has described leadership as an art form that frees (empowers) people “to do what is required of them in the most effective and humane way possible” (p. 1) and contended that contemporary leadership may be viewed simply as a process of moving the self and others toward a shared vision that becomes a shared reality. Successful transformational leadership is relational, driven by a common goal or purpose, and satisfies the needs of leader and follower. It is the leadership style often associated with effective change agents. Schwartz and colleagues (2011) have studied the effects of transformational leadership on the Magnet designation for hospitals. Other authors who have described a transformational approach to leadership include Wang and associates (2012), who studied transformational leadership with Chinese nurses, Heifetz (1994), Secretan (1999, 2003), Senge (2006), and Covey (1989). The term situational leadership is defined as the interaction between an individual's leadership style and the features of the environment or situation in which he or she is operating. Leadership styles are not fixed and may vary based on the environment. Situational leadership depends on particular circumstances, with leaders and followers assuming interchangeable roles according to environmental demands (Fiedler, Chermers, & Mahar, 1976; Lynch, McCormack, & McCance, 2011; Solman, 2010; Stogdill, 1948). The role of follower is important to any discussion about APN leadership because APNs will find themselves in both roles at a given time. Grohar-Murray and DiCroce (1992) and DePree (1989) enlarged on this idea and used the term roving leadership to describe a participatory process that legitimizes the situational leadership of empowered followers through the support and approval of the hierarchical leader. This notion of leadership is relevant because APNs' work in collaborative health care teams requires that the roles of leader and follower be interchangeable to meet the complex needs of the patient. o Characteristics of a leader Defining Characteristic Core Elements (Knowledge and Skills) Mentoring - The responsibility to mentor is central to all the definitions of leadership and change outlined earlier and is a key element of the APN leadership competency. The ability to help others grow and encourage them toward self-actualization requires competent caring leaders who are interested in the success and well-being of their followers.• Shared vision • Seeks mentors and serves as a mentor • Willing to share power • Empowering self and others • Self-reflection Innovation • Knowledge of models of leadership and change • Systems thinking • Systems assessment skills • Flexibility • Risk taking • Expert communication • Credibility • Change agent Activism • Knowledge and understanding of factors driving change in the health care system • Involvement in policy arenas, whether local, regional, national, or global • Advocacy for patients, advanced practice nurses, and the nursing profession Attributes of Nurse Leaders Expert Communication Skills • --Articulate in speech and in writing • Able to get one's point across • Uses excellent listening skills • Desires to hear and understand another's point of view • Stays connected to other people Commitment -Gives of self personally and professionally • Listens to one's inner voice • Balances professional and private life • Plans ahead; makes change happen • Engages in self-reflection Developing One's Own Style - Gets and stays involved • Sets priorities • Manages boundaries • Uses technology • Engages in lifelong learning • Maintains a good sense of humor Risk Taking -Gets involved at any level • Demonstrates self-confidence and assertiveness • Uses creative and big picture thinking • Willing to fail and begin again -Has an astute sense of timing • Copes with change Willingness to Collaborate -Respects cultural diversity • Desires to build teams and alliances • Shares power • Willing to mentor o Leadership styles (list these)- 1. Democratic-Democratic style of leadership in nursing enhances the participation of junior employees in the decision making the procedure of an organization. Although, the final decision is of the leader, s/he collects information, feedback, and ideas from all the staff members before finalizing everything. Democratic leadership style in nursing is quite effective as all the employees feel valued, and due to this, they attempt to give their best. Input of an organization’s employees is of foremost importance when it comes to the growth of the firm. This is one of the best for clinical settings as skills and abilities of all the professionals contribute equally to the success of the organization. Though, this management style in nursing too has some disadvantages as getting everyone’s feedback is really time-consuming process. Also, the confident group of members always come ahead and give suggestions whereas apprehensive employees may never get opportunities to provide their feedback. 2. Affiliative-Affiliative Leadership is not a cup of tea of every other individual. To make this style successful for an organization, the leader must be great at making relationships. This leadership works best when there is a need to fix the bitterness of feelings among a group or when there is workload or stress, as these leaders are the best to motivate other team members. Basically, affiliative leadership is extremely effective when there is a need to team harmony, augment morale or rebuild broken trust. Moreover, it also increases interaction and communication among members. Despite numerous positive aspects about this style of leadership in nursing, there are some disadvantages, first of all, this style cannot be used as the only source, and second, it can lead to poor performance, and that too may go not corrected. 3. Transformational-Transformational leadership style in nursing is also based on the encouragement of the employees to give their best at work and motivation to be positive while performing various tasks instead of being negative. But, all this is done through a common mission and vision. Transformational style results into engaged and productive teams. To make this leadership work in a beneficial way for the organization, there is a requirement of an inspiring and smart nurse leader. This style may fall in a contemptible manner if the one who handles everything lacks in any of the essential traits required to make transformational leadership successful for any health care setting. 4. Authoritarian-Authoritarian or Autocratic leadership style in nursing is the one in which the nurse manager or leader decides everything, give orders and directives to all the team members. Employees just need to follow what they are asked. The manager supervises every staff member and their input is not considered while making decisions. Workers are not even allowed to ask if they have some doubts about the validity of a directive. This kind of leadership style is perfect for the places such as prisons, military, routinized operations, jails because in these kinds of places, lives of patients completely depend on the workers. Thus, it is must for such employees to work step by step as they are directed. Even punishment is given if someone does not enforce the rules properly. Mistakes are completely intolerable, and often individuals are blamed instead of the faulty procedures. The only advantage of this leadership is that it is the most effective in case of emergencies or perplexed situations when there is very less time for discussion. It is completely a bad idea to used this management style in nursing for routine operation as it fails to promote, communication, trust, and teamwork. 5. Coaching-In coaching leadership, leader concentrates on the development of people. They work to make the team members understand their strengths and weaknesses, set targets for development and help them achieve goals. This nurse manager leadership style is great to groom the employees both professionally and personally. If implemented properly it gives long term results. But along with so many pros, it also has some cons such as it can work only if workers are receptive, and it needs time to imply, especially in the start. 6. Transactional-Transactional Leadership style in nursing is the one in which leaders give rewards or punishments to the employees respective of the way in which they complete the tasks. It concentrates on the importance of supervision, leadership, organization and performance of the group. It completely relies on the transactions held between the workers and the nurse manager because it is based on the fact that employees are motivated both by discipline and rewards. Nurse managers who follow this kind of leadership style for nurses do not focus on the performance of the organization in the near future, rather they look for the best that can be done to keep everything perfect in the present. Moreover, these leaders pay special attention to the deviations and faults made by the staff members. Transactional leaders are required when some tasks need to be carried out in a specific manner. 7. Situational-situational leadership is very flexible and transforms according to the existing working requirements and needs of the clinical setting. Management is not based upon the basic skills and abilities of the manager, rather s/he modifies them according to the requirement of the organization. This kind of nurse management style is easy to imply, the leader just needs to analyze the present situation of the organization and imply the best strategy to get the best outcome for the organization. Thus, this style works best only with the right leader. Nurse managers are free to take decisions and modify management styles as per the need. Situational leaders are often seen diverting from the long term goals and strategies of the organization. This is one of the major drawbacks of this style of the various types of leadership styles in nursing. 8. Laissez-faire-In Laissez-faire leadership in nursing, employees are encouraged to undertake a hands-off approach and are allowed to work in a way that they like to, without any kind of supervision or guidance of the nurse managers. Only minimum directions are provided by the leaders and it permits the workers to handle various tasks on their own. Employees are responsible for the decisions made by them, setting their goals and solving all the issues that arise while working. This kind of leadership style in nursing management is successful only in the cases where the staff members are highly skilled, educated, motivated and are ready to give their best for the best results. Using this with the workers who don’t know how to manage time, who are not skilled or unexperienced can result into negative outcome. Laissez-faire nurse managers are mostly new leaders or the ones who are at the end of their careers. 9. Visionary-Visionary leadership is much similar to transformational style. The only difference is that these leaders are much concerned about the future and they guide the followers to stay focused on what they need to achieve in the upcoming years. Nurse manager just motivates the employees to pursue and share a common target and vision by providing proper guidance about where to go and what to do with proper stepwise procedure of how to reach there. A smart, visionary leader interchanges information freely to provide knowledge to the subordinates which they require to be successful. This health care leadership style works best when any clinical facility is new and needs directions to initiate in the field of health care. 10. Servant-To gain success of the organizations, nurse managers often opt this type of leadership style in health care. This leader looks after for those who serve the patients and work hard to gain positive outcomes, i.e., the staff members. They pay special attention to their needs and ask the employees if they want any kind of help. All this is dome for the professional and personal development of the workers. They facilitate engagement and offer a healthy working environment to the subordinate nursing professionals. A good servant leader is an active listener, aware, persuade others, build community, empathetic and is great at conceptualizing everything. It is a caring style of leadership and is often implied to build trust among the employees. o Leadership theories (list these) Leadership theory is a discipline that focuses on finding out what makes successful leaders excel in what they do In other words, leadership style is one of many examples covered with leadership theory. Leadership style focuses specifically on the traits and behaviors of leaders. transformational leadership as a process whereby “the purposes of the leader and follower become fused, creating unity, wholeness and a collective purpose” (p. 83). Transformational leadership can lead to changes in values, attitudes, perceptions, and/or behaviors on the part of the leader and the follower and lays the groundwork for further positive change. Thus, transformational leadership occurs when people interact in ways that inspire higher levels of motivation and morality among participants. How do leaders do this? Transformational leaders analyze a situation to understand the particular leadership needs and goals; they use this information, together with their interpersonal skills, to motivate, stimulate, share with, conciliate, and satisfy their followers in an interdependent interactional exchange. DePree (1989) has described leadership as an art form that frees (empowers) people “to do what is required of them in the most effective and humane way possible” (p. 1) and contended that contemporary leadership may be viewed simply as a process of moving the self and others toward a shared vision that becomes a shared reality. Successful transformational leadership is relational, driven by a common goal or purpose, and satisfies the needs of leader and follower. It is the leadership style often associated with effective change agents. situational leadership is defined as the interaction between an individual's leadership style and the features of the environment or situation in which he or she is operating. Leadership styles are not fixed and may vary based on the environment. Situational leadership depends on particular circumstances, with leaders and followers assuming interchangeable roles according to environmental demands (Fiedler, Chermers, & Mahar, 1976; Lynch, McCormack, & McCance, 2011; Solman, 2010; Stogdill, 1948). The role of follower is important to any discussion about APN leadership because APNs will find themselves in both roles at a given time. Grohar-Murray and DiCroce (1992) and DePree (1989) enlarged on this idea and used the term roving leadership to describe a participatory process that legitimizes the situational leadership of empowered followers through the support and approval of the hierarchical leader. This notion of leadership is relevant because APNs' work in collaborative health care teams requires that the roles of leader and follower be interchangeable to meet the complex needs of the patient. Developing a Leadership Portfolio Developing a Leadership Portfolio Throughout this chapter, definitions, attributes, and components of leadership and key strategies for developing competency in APN leadership have been presented. These approaches will help new APNs acquire leadership skills. Developing a leadership component as part of a marketing portfolio is helpful to novice APNs who desire to individualize continuing development of the leadership competency consistent with their personal vision, goals, timeline, and APN role in the practice setting. An Australian study in 2010 reported increased knowledge, skill sets, and outcomes in clinicians and leaders who used portfolios to enhance their effectiveness (Dadich, 2010). Falter (2003) has suggested the use of a strategy map that includes vision, goals, and objectives that outline steps to achieve a particular strategy. Portfolios are designed to meet the needs of individual APNs and should be consistent with clinical and personal interests and professional goals and provide a timeline that allows for personal and professional balance and boundary setting. Chapter 20 provides the elements of a marketing portfolio. Promoting Collaboration Among Advanced Practice Nursing Groups At different times, each subgroup of APNs has emerged as a leader for the nursing profession. Psychiatric CNSs were among the first entrepreneurial APNs to hang out their shingle, despite the litigious climate in which they could be threatened with lawsuits for “practicing medicine.” CNMs and CRNAs have led the way in using data effectively to justify their practice and attain appropriate scopes of practice. Early in their history, both groups began to record the results of their practices, showing the quality and suitability of their care (see Chapter 1). In the 1990s, NPs, with their flexible, community-based primary care practices, stood at the forefront of the changing health care delivery system. Although these subgroups of APNs have made impressive strides for advanced practice nursing, an obstacle to effective leadership is the tendency for APN specialty groups to separate and establish rigid boundaries that distinguish them from one another, thereby fragmenting APN groups and blocking opportunities for the increased power that unity would bring. The tension and fragmentation created by rigid boundaries require leaders who can transcend APN roles and specialties. APNs must manage and bridge boundaries among other nursing groups and within the ranks of the various APN constituencies. Although the uniqueness of each type of APN must be protected, a professional structure that provides a forum for discussing issues pertinent to all types of APNs also needs to be created. This structure may simply be an annual meeting for APNs or a permanent entity residing within an existing or new professional organization. Consensus groups at the national level have been meeting to discuss policy issues in which the power of the collective numbers of all APN groups speaking with one voice cannot be overemphasized (see Chapters 2, 12, and 21). An excellent example of professional collaboration among nursing leaders is the Consensus Model work (Chapter 21). APN organizations have joined to speak out collaboratively about state regulations regarding reimbursement, prescriptive authority, and managed care empanelment. It is critical that each APN, regardless of specialty, takes on the responsibility of moving toward an integrative and unified understanding of advanced practice nursing. Creating community in the current health care environment is particularly challenging because of the realignment of clinical decision making, scopes of practice for APNs and physicians, and new roles that blur boundaries between nursing and medicine. An understanding of change, effective communication, coalition building, shared vision, and collaborative practice leads to the development of structures on which unity is built. These five building blocks form the foundation of interdisciplinary leadership and practice. Motivating and Empowering Others Motivation and empowerment are core elements of the APN leadership competency. Empowerment was defined earlier as the ability of the leader to give followers the freedom and authority to act. However, truly empowering others requires more than just giving them permission to act on their own. Empowerment is a developmental process; over time, a good leader encourages their constituents' sense of responsibility and competence, thus reinforcing their autonomy and authority to act. Wheatley (2005) has affirmed the importance of motivation and empowerment in developing innovators and has noted that older notions of power and control are things of the past, as has Senge (2006). Today's APN leaders need to use the tools of empowerment and motivation to mentor future leaders who can lead with creativity, innovation, and caring. Networking is an essential technique used by leaders to stay informed and connected regarding APN issues. Networking, formal and informal, is not a new strategy for APN leaders. Formal networks take the form of committees, coalitions, and consortia of people who come together to share information, collaborate, and plan strategy regarding mutual issues. Formal networks open doors to new opportunities and provide shared resources that ensure a competitive edge in the organization (Carroll, 2005; Montgomery, 2011). Informal networking is a behind the scenes strategy that allows for contact with APNs and others who speak the same language, have the same viewpoints, and can offer support and feedback at critical times. The ability of APNs to stay connected to important practice and education issues through networking is key to the leadership competency. The most effective strategy for becoming an insider is networking with colleagues within the circle of APN peers and with other health care providers who have a stake in the outcomes of a particular issue. Montgomery (2011) has suggested that it is important to make your “net” work! Engaging Others in Planning and Implementing Change The skills outlined earlier, “Attributes of Effective Advanced Practice Nurse Leaders,” on personal attributes of successful leaders (p. 281) are integral to leading innovation and change. However, other strategies also assist in the process. It is important to analyze the situation and explore the need for change. If change is warranted, one must craft an implementation plan that involves everyone. Box 11-1 lists leadership strategies that are useful for moving through these transitions. Bonalumi and Fisher (1999) have suggested that an important component of leadership during times of change is the ability to foster and encourage resilience in change recipients. O'Connell (1999) and, more recently, Grafton and associates (2010) have defined resilient people as being positive and self-assured in the face of life's complexities, having a focused, clear vision of what they want to achieve, and having the ability to be organized but flexible and proactive rather than reactive. Helping colleagues and followers develop resilience should be a major focus for advanced practice nursing leaders who seek to facilitate the growth of their followers. The second DNP essential for advanced nursing practice education addresses the provision of sophisticated leadership that “emphasizes practice, ongoing improvement of health outcomes and ensuring patient safety”; to accomplish these goals, APNs will need “expertise in assessing organizations, identifying systems issues and facilitating organization-wide changes in practice delivery” (AACN, 2006, p. 10). Institutional Assessment Regarding Readiness for Change With the emphasis on evidence- based practice and the knowledge that evidence-based guidelines and therapies are underused (IOM, 2001; McGlynn et al., 2003), overused, or misused (IOM, 2001), APNs have an important systems leadership role in improving care. This can be accomplished by leading and collaborating with nurses and interdisciplinary colleagues to ensure the adoption of best practices (Duffy, 2002; Spencer & Jordan, 2001; Spross & Heaney, 2000; Weaver, Salas, & King, 2011). An institutional assessment of specific factors will help the APN identify facilitators of and barriers to change. These data can then be used to design a plan for change in collaboration with others. Box 11-6 lists key . • What is the nature of the change (e.g., policy, procedure, new skill, behavior)? • Is the issue significant? For all stakeholders or just one group? • Is a national policy, guideline, or standard the focus of the change? Is it a mandate with which the agency must be in compliance? • Is the change simple or complex? Will different stakeholders perceive its simplicity or complexity differently? • Do you foresee major problems associated with change, such as an increase in errors or resistance on the part of a group? • Will it be possible to address these major problems? • Are there vested interests—who is likely to gain from the change, who will view the change as a loss (e.g., of power)? • Are there opinion leaders who will promote the change? Do you anticipate strong opposition? • Have you observed a gap between public statements and private actions (e.g., a colleague agrees to serve on a committee but never shows up or participates in the committee's work)? • Are there resource implications? What are the costs (e.g., staffing, materials, lost revenue)? Followship As APNs focus on developing their leadership skills, they cannot ignore the importance of being a good follower. It takes skill to recognize when one should be a follower rather than a leader —when another is more skilled or more appropriate to lead a particular situation, or when it is appropriate to let another who is developing his or her leadership skills take the lead on a project. Successful collaboration and teamwork require not just leadership, but skilled followers as well. Expert followers know how to accept direction, be forthcoming with pertinent information that is valuable to the team, seek clarification, and provide appropriate constructive feedback. o Change theory behavior change un folds through stages Lewin's definition of behavior in this model is "a dynamic balance of forces working in opposing directions." The Change Theory has three major concepts: driving forces, restraining forces, and equilibrium. Driving forces are those that push in a direction that causes change to occur. They facilitate change because they push the patient in a desired direction. They cause a shift in the equilibrium towards change. Restraining forces are those forces that counter the driving forces. They hinder change because they push the patient in the opposite direction. They cause a shift in the equilibrium that opposes change. Equilibrium is a state of being where driving forces equal restraining forces, and no change occurs. It can be raised or lowered by changes that occur between the driving and restraining forces. There are three stages in this nursing theory: unfreezing, change, and refreezing. Unfreezing is the process which involves finding a method of making it possible for people to let go of an old pattern that was somehow counterproductive. It is necessary to overcome the strains of individual resistance and group conformity. There are three methods that can lead to the achievement of unfreezing. The first is to increase the driving forces that direct behavior away from the existing situation or status quo. Second, decrease the restraining forces that negatively affect the movement from the existing equilibrium. Thirdly, finding a combination of the first two methods. The change stage, which is also called "moving to a new level" or "movement," involves a process of change in thoughts, feeling, behavior, or all three, that is in some way more liberating or more productive. The refreezing stage is establishing the change as the new habit, so that it now becomes the "standard operating procedure." Without this final stage, it can be easy for the patient to go back to old habits. • _Evidence-based practice (EBP) Evidence-based nursing is defined as the process that nurses use to make clinical decisions using the best available research evidence, their clinical expertise, and patient preferences (Dicenso, Cullum, & Ciliska, 2002). The explicit inclusion of patient Evidence-based practice involves the generation of a clinically measurable question, identification of pertinent research findings, coding and extraction of essential data, and implementation of findings. Intimate knowledge of this process is critical for the APN to master three core levels of the EBP competency, application to individual clinical decision making, formulating policies for patient care in a local facility, or evaluating evidence in order to establish standards of care via clinical practice guidelines. These competencies are increasingly essential as the APN functions as a team member, leader and decision maker within an interdisciplinary health care team • _Levels of evidence Level I: Interpretation and Use of Evidence-Based Practice in Individual Clinical Decision Making The most basic level of EBP competency is the application of the four steps for clinical decision making in an individual patient. This proficiency requires more than formulation of a clinical question and identification of pertinent studies needed to determine best available evidence. The advanced practice nurse (APN) must combine knowledge of best evidence with an assessment of individual patient factors likely to affect treatment effects, such as the presence of comorbid conditions, psychosocial and cultural factors such as locus of control, preference and impact on quality of life, and cost considerations. Level II: Interpretation and Use of Evidence-Based Practice to Create Policies for Patient Care For many APNs, the growing demand to formulate evidence-based policies and protocols needed to prevent the growing list of “never events” provides an opportunity to master the second level, interpretation and use of EBP to create policies for patient care. Level III: Evaluation of Evidence-Based Practice to Determine Standards of Care Participation in an interdisciplinary team to evaluate and determine standards of care using EBP is the third and most advanced level of the EBP competency for APN practice. Generation of an evidence-based clinical practice guideline requires identification of a number of clinically measurable questions required for establishing and evaluating clinical practice in a broad area of patient care, along with an extensive systematic review of pertinent studies. This often encompasses major assessment strategies related to the management of a particular disorder and first-line and alternative interventions for management. • _Steps of APN core competency EBP Evidence-based practice is based on a four-step process: (1) formulation of a clinical question; (2) identification and retrieval of pertinent research findings based on literature review; (3) extraction and critical appraisal of data from pertinent studies; and (4) clinical decision making based on results of this process. Competency Fundamental Level Expanded Level I: Interpretation and use of research and other evidence in clinical decision making Incorporate evidence-based practice (EBP) principles and processes into individual practice. Incorporate EBP practices and principles on a unit, clinic, department, facility, health care system, national, or international level; function as member of an expert panel on a facility, health care system, national, or global level to create clinical practice guidelines of best practice statements. II: Changing practice Incorporate best practice changes according to EBP principles into own practice. Design and implement a process for changing practice beyond the scope of individual practice on a unit, clinic, facility, health care system, or national basis. III: Evaluation of practice Identify benchmarks for evaluating own practice. Design and implement a process to evaluate pertinent outcomes of practice beyond the scope of individual practice (e.g., generic nursing practice, group APN practice, interdisciplinary team practice, facility- wide or health care system—wide practice • _Appraisal of evidence The third step, evidence appraisal, involves taking the acquired information, and critiquing it by systematically reviewing its relevance, validity and its application to your specific clinical question. In other words, the investigator must ask three essential questions: - What are the results? Are the results valid? Will the results help to answer my clinical question? Step 3: Critical Appraisal of Evidence Step 3 in the EBP process is vital, in that it involves critical appraisal of the evidence obtained from the search process. Although healthcare professionals may view critical appraisal as an exhaustive, time- consuming process, the first steps of critical appraisal can be efficiently accomplished by answering three key questions as part of a rapid critical appraisal process in which studies are evaluated for their validity, reliability, and applicability to answer the posed clinical question (summarized in Box 1.4): 1. Are the results of the study valid? (Validity) That is, are the results as close to the truth as possible? Did the researchers conduct the study using the best research methods possible? For example, in intervention trials, it would be important to determine whether the subjects were randomly assigned to treatment or control groups and whether they were equal on key characteristics prior to the treatment. 2. What are the results? (Reliability) For example, in an intervention trial, this includes (a) whether the intervention worked, (b) how large a treatment effect was obtained, and (c) whether clinicians could expect similar results if they implemented the intervention in their own clinical practice setting (i.e., the preciseness of the intervention effect). In qualitative studies, this includes evaluating whether the research approach fits the purpose of the study, along with evaluating other aspects of the study. 3. Will the results help me in caring for my patients? (Applicability) This third critical appraisal question includes asking whether (a) the subjects in the study are similar to the patients for whom care is being delivered, (b) the benefits are greater than the risks of treatment (i.e., potential for harm), (c) the treatment is feasible to implement in the practice setting, and (d) the patient desires the treatment. The answers to these questions ensure relevance and transferability of the evidence to the specific population for whom the clinician provides care. For example, if a systematic review provided evidence to support the positive effects of using distraction to alleviate pain in postsurgical patients between the ages of 20 and 40 years, those same results may not be relevant for postsurgical patients who are 65 years or older. • _Integrating EBP Step 4: Integrate the Evidence With Clinical Expertise and Patient Preferences to Make the Best Clinical Decision The next key step in EBP is integrating the best evidence found from the literature with the healthcare provider’s expertise and patient preferences and values to implement a decision. Consumers of healthcare services want to participate in the clinical decision-making process, and it is the ethical responsibility of the healthcare provider to involve patients in treatment decisions (Melnyk & Fineout- Overholt, 2006). Even if the evidence from a rigorous search and critical appraisal strongly supports that a certain treatment is beneficial (e.g., HRT to prevent osteoporosis in a very high-risk woman), a discussion with the patient may reveal her intense fear of developing breast cancer while taking HRT or other reasons that the treatment is not acceptable. Moreover, as part of the history-taking process or physical examination, a comorbidity or contraindication may be found that increases the risks of HRT (e.g., prior history of stroke). Therefore, despite compelling evidence to support the benefits of HRT in preventing osteoporosis in high-risk women, a decision against its use may be made after a thorough assessment of the individual patient and a discussion of the risks and benefits of treatment. Similarly, a clinician’s assessment of healthcare resources that are available to implement a treatment decision is a critical part of the EBP decision-making process. For example, on follow-up evaluation, a clinician notes that the first-line treatment of acute otitis media in a 3-year-old patient was not effective. The latest evidence indicates that antibiotic A has greater efficacy than antibiotic B as the second-line treatment of acute otitis media in young children. However, because antibiotic A is far more expensive than antibiotic B and the family of the child does not have prescription insurance coverage, the practitioner and parents together may decide to use the less expensive antibiotic to treat the child’s unresolved ear infection • _Randomized Control Trial –Gold Standard A study in which people are allocated at random (by chance alone) to receive one of several clinical interventions. One of these interventions is the standard of comparison or control. The control may be a standard practice, a placebo ("sugar pill"), or no intervention at all. • _Leadership development plan for practice When considering a leadership development plan, there are formal and informal strategies. Students must have formal and informal opportunities to develop leadership skills in each domain. These can occur in the classroom, clinical practice, student leadership, and health-related service projects. In general, lessons learned in one domain will apply to leadership situations in other domains. Health policy leadership is discussed separately because it has specific features that are somewhat different from the APN's everyday leadership activities. Power resources include many of the attributes described in this chapter, such as education, experience, expert communication, networking, assertiveness, and collaboration and are clearly demonstrated in the studies of leadership discussed in the following sections. Zaccaro (2007) has argued that with increases in conceptual and methodologic resources, combinations of inborn traits and learned attributes are more likely to predict leadership than once was believed. Leadership represents complex patterns of behavior explained in part by multiple leader attributes (Zaccaro, 2007). In this section, we explore leadership traits and attributes that are innate and those that can be learned as APNs develop their leadership competence. • _Key Components of Managing Advanced Practice Environments o Certification requirements for each role –LACE Licensing, Accredidation, Certification, Education Graduation from an approved masters- or doctoral-level APRN program • Licensure and recognition in good standing as an APRN • National certification in an APRN population focus area • Recent pharmacotherapeutics course of at least 3 credit hours (45 contact hours) • Evidence of a collaborative practice arrangement (in some states) • Ongoing CE hours in pharmacotherapeutics to maintain prescribing status (in some states) • State prescribing and national DEA numbers (in some cases) Certifying organizations American Association of Nurse Practitioners (AANP) American Nurses Credentialing Center (ANCC) Credentialing American Nurses Credentialing Center (ANCC) Privileging, and prescriptive Authority DEA, It is critically important that certifying organizations work to clarify the certification credential as appropriate only for currently practicing APNs. Given the centrality of the direct clinical practice component to the definition of advanced practice nursing, certification examinations must establish a significant number of hours of clinical practice as a requirement for maintaining APN certification. Some faculty and nursing leaders who do not maintain a direct clinical practice component in their positions have been allowed to sit for certification examinations and represent themselves as APNs. Statements such as “Once a CNS, always a CNS,” which are heard with NPs and CNMs as well, perpetuate the mistaken notion that an APN title is a professional attribute rather than a practice role. Such a misunderstanding is confusing inside and outside of nursing; by definition, these individuals are no longer APNs. As noted, the Consensus Model focuses regulatory efforts on these broad role and population foci rather than on particular specialties, although some specialties are represented (e.g., neonatal NPs). This decision not to recognize established APN certification examinations in specialties such as oncology or critical care for state licensure purposes has challenged the CNS role more than other APN specialties. The American Nurses' Credentialing Center (ANCC) has become the dominant certifying organization for State Board of Nursing—supported CNS examinations; the number of examination options for CNSs is decreasing as the Consensus Model is being implemented (see the ANCC website for a listing of currently available CNS examinations— www.nursecredentialing.org). Even though APRN regulation is becoming more standardized, a need exists for the continued development of specialty examinations at the advanced practice nursing level, particularly for CNS specialties; as it stands now, many CNSs have to take the broad-based certification examination recognized by their state in addition to an APN-level specialty certification examination necessary for their practice. Another unintended consequence of the limitations set by recognizing only six population foci is that educational programs have closed CNS concentrations given the lack of a sanctioned certification examination in the specialty. Although other factors also influenced these decisions, not recognizing specialty examinations for regulatory purposes is a key factor in these closures. The limited population foci sanctioned at present can be seen as a first step in standardizing regulation; the Consensus Model report notes the expectation that additional population foci will evolve. Even with these transitional issues, the Consensus Model represents an important standardization of APRN regulation and has helped cement the primary criterion of certification as a core regulatory requirement for APRN licensure. o Regulatory and legal requirements At no time has it been more important for APRNs to understand and value the important relationships among groups that control the complex processes and systems that regulate practice. New models of health care and varying configurations of how APRNs practice in interdisciplinary teams have escalated the importance of regulatory considerations. The growth of virtual health care delivery makes the picture even more complex. APRNs will need to provide leadership and clear direction to policymakers to ensure the development of broad-based practice standards that will satisfy state statutes and make sense in all areas of advanced practice nursing. The implementation of the Consensus Model that is currently being implemented across the United States places APRNs in an excellent position of leadership for the future. The need for APRNs to move into key roles as health care providers in the next dec #ade requires careful vigilance with regard to the LACE components of credentialing and regulation o Health policy The health care policy environment is rapidly changing and comprehensive health care reform will be implemented over the next decade, and beyond. APNs must play a larger role in shaping how health care gets delivered because they have a social covenant with the public to serve as patient advocates in the broadest sense. Policymakers are looking for solutions to escalating costs and continued patient safety problems. To be able to do this, APNs must resist the pull of the familiar and overcome invisibility and passivity. Political competency needs to be part of every APN's professional role. Membership in professional organizations that advance issues critical to APN practice and the health of the United States is vital to the continued viability of APNs. The first step to being involved in policy formulation is to be knowledgeable about the policy process and the current and emerging issues relevant to APNs. To be involved, APNs need to understand the details related to funding issues, measures of quality, how they reflect APN practice, and specific programs designed to improve access (Table 22-5). The important lesson for APNs and policy is that a single person, with deep understanding of an issue, along with highly developed political skills, can make a difference. An individual backed by organizational strength, particularly by coalitions of organizations, can make an even more significant difference. o Consulting relationships Common Advanced Practice Nurse Consultation Situations Depending on one's particular advanced practice nursing role, certain consultation situations may be more common than others. APNs are most likely to receive requests for patient- and consultee-centered case consultations. These types of consultations are described here. Experienced APNs may extend their consultative skills into other types of consultations, such as program-centered consultations. The exemplars included here vary in the complexity of consultations and the extent to which aspects of the consultation model are made explicit. The reader is encouraged to examine how the proposed model of advanced practice nursing consultation is applied and consider ways in which it can be applied in his or her own practice. Advanced Practice Nurse Consultation in Practice Within their specialty or setting, APNs may take for granted the available APN consulting resources. They may not think of their interactions regarding patient care as a consultation because they occur as they are engaged in practice, in the hallway, or over coffee. Consultation among APNs may be more or less formal, depending on the culture of the unit or clinic, relationships among the APNs, and specialty populations seen in the facility. Consultations are likely to involve specific patient issues—for example, “Could you look at this rash?” or “I've done everything I can think of to try to make sure this pregnant teen comes to her prenatal visits, and she still misses them. Here's what I've done. … Can you think of anything else I can try before I get the city department of social services involved?” Exemplar 9-1 illustrates a formal consultee-centered consultation between a primary care NP and a CNS-NP specializing in HIV/AIDS; this consultation also led to a plan to comanage the patient. Advanced Practice Nurse—Physician Consultation Consultation and collaboration with the physician and patient care team remain integral components of APN interprofessional development. When consulting with other nurses or physicians, an APN is likely to be far along in the problem-solving process. The need for consultation is often related to the consultee's level of diagnostic uncertainty or complex management issues. Experienced APNs often have a clear definition of the problem and a preliminary plan to address it that they wish to validate or reformulate, depending on the consultant's advice. Truly collaborative relationships between physicians and APNs ensure consultation that is bidirectional. Physicians in primary care often consult APNs regarding issues such as assisting patients in making lifestyle changes or in coping with the effects of chronic illness. Many APNs in primary care have special expertise in women's health care and are sought out by physicians for consultation on such issues. Physicians might then choose to comanage patients with APNs so that patients benefit from the expertise of both professionals. APNs, in turn, might consult a physician regarding a patient in a medically unstable condition, which evolves into comanagement by the physician and APN, with each assuming responsibility for the outcomes of decision making. The ACNM (2011) was deliberate in describing the various types of interactions that CNMs have with physicians. Unfortunately, APN-physician consultative relationships have often been structured by laws and regulations that mandate or imply supervisory oversight, which can reinforce stereotypical nurse-physician relationships. Many organizational cultures reinforce traditional nurse-physician relationships and the behavioral norms associated with them. One of the major challenges facing advanced practice nursing educators is to address students explicitly prior to socialization to nurse-physician relationships that might undermine the full expression of autonomous advanced practice nursing. When a hierarchical relationship exists between an APN and physician, the APN who consults may defer to the physician's decisions, downplaying or ignoring first-hand knowledge of the patient. However, there are successful interactions between physicians and APNs and these practices embrace the collaborative relationships that are key to effective consultation (see Chapter 12). Consultation between APNs and physicians can highlight the strengths of each—that is, the APN's deep appreciation for the human responses related to health and illness and the physician's deep understanding of disease and treatment. When both areas of expertise are available to patients and their families, truly holistic, comprehensive, and individualized care is offered. As APN knowledge evolves and deepens, an emerging issue in relation to APN-physician consultation is the crossing of traditional nurse-physician boundaries. As APNs become more and more specialized, the knowledge embedded in practice may be more closely related to what is generally thought of as medical practice. For example, a CRNA may have highly developed skills in the area of pain management and the requisite skills to perform procedures to address complex pain issues. In women's health practices, APNs may specialize in using complementary therapies for menopausal symptoms. Physicians often refer interested patients to the collaborating women's health APN in the practice for consultation about using naturopathic medications, herbal remedies, and compounded estrogens. Tact and understanding of the long- standing boundaries that are being crossed can elevate the consultation relationship to a new level. Advanced Practice Nurse—Staff Nurse Consultation Early on, as CNSs implemented their consultative roles, it became apparent that the culture of nursing had not adopted consultation as an important strategy in providing patient care (Barron, 1983). Staff nurses were expected to take care of the patients themselves. A novice might consult a head nurse or more senior nurse, but staff members were expected to know how to solve problems and use the policy and procedure manual. An important component of implementing consultation means teaching staff members how and when to consult. During that time, CNSs often engaged in active case finding to identify patients who needed the knowledge and skills they had because CNSs were not actually assigned to patients and staff nurses. By building this type of clinical caseload, they demonstrated to staff how consultation might be helpful. Of note, CNSs tended to carry out direct consultation with patients and to consult with other professionals to assist the staff with problem solving and enhancing patient care. For example, staff nurses might call the medical-surgical CNS regarding a patient with Guillain-Barré syndrome because they had no experience caring for patients with this disorder. The CNS may have had little or no experience as well but could mobilize the resources needed, such as arranging an in service by the neuroscience or rehabilitation CNS, providing articles, being available to staff on all shifts as they implemented unfamiliar assessments, and assisting with care plan development. The APN initiates processes (including additional consultation) and provides knowledge directly. Once relationships are established and staff perceive that the APN consultant is approachable, respectful, and helpful, staff will initiate contact with the consultant when complex clinical issues arise. See Exemplar 9-3 for an example of staff RN to APN consultation. Mechanisms to Facilitate Consultation Mechanisms to facilitate consultation need to be considered by all APNs, regardless of setting. As health care becomes more community-focused and APNs provide care to increasingly diverse and vulnerable populations, the breadth and depth of skill required for these newer roles will be considerable. APN-APN consultation is an important means of developing these evolving skills. The level of enthusiasm for an integrative consultation program at most institutions is very important. A baseline level of trust and collaborative practice on the part of consultees allows the consultant APN, regardless of specialty, the opportunity to make recommendations with confidence. A setting in which the environment is not open to the consultative use of APN services presents barriers and an unwillingness to use APN expertise. The ground work for implementing an APN consultation program would not be productive prior to laying the foundation of openness and willingness of collaboration. It is important to consider new settings and potential sources and beneficiaries of advanced practice nursing consultation. APNs from varying specialties can form networks within organizations or geographic locations and identify specific expertise to be shared through consultation among members of the network. APNs in an agency can develop and initiate an explicit process for consultation so that agency staff is clear about how to request an APN consultation and what to expect reasonably from the consultant. When the APN is involved in collaborative relationships, clarification of the possibilities for consultation could be discussed and negotiated to expand APN consultation opportunities. The consultant's services could be made available to interdisciplinary teams in which the APN is a member. Interdisciplinary teams exist in many settings. In addition to working collaboratively on such teams, APNs can offer valuable consultative services. Staff nurses in these settings may be without the benefit of abundant resources to enhance practice and professional development. APNs could offer such opportunities through consultation. When APNs are the primary providers of care, such as in nursing homes and community health centers, opportunities for consultation may be missed or minimized because the most common interactions are collaborative or comanagerial, or because of time constraints. In these settings, however, the outcome of consultation is often improved patient care. APNs should consider documenting the consultations that they can offer in those settings in somewhat standard and easily retrievable forms, such as computerized databases. If information about these consultations were easier to access, patterns and outcomes of consultation activities would be more apparent and the effectiveness of consultation could be more easily studied. As APNs move into innovative practices, they should determine which consultative services they will market and which types of APNs and other consultants are available and will be needed. Consultation between APNs offers the additional benefit of collegial networking. APNs are establishing private independent practices that require collaboration and consultation for success. As independent practitioners, they are offering their services in primary care, home health (particularly to assist in the respiratory care of patients who require ventilators), pain clinic, and obstetric care settings. Consultation with other APNs and with other health care professionals in those settings, in addition to the direct care they offer, has the potential to enhance the knowledge and practice of APNs and create comanagement and collaborative possibilities for all the APNs involved. o Business practices Through the development of innovative programs and practices grounded in a systems-thinking approach, APNs define, demonstrate, document, and thereby claim their contributions to patient care. Business planning establishes a clear picture of how the APN will function on a daily basis, as well as how midrange and long-term goals are to be met. Knowledge of the processes involved in care delivery increases the sharing of information among APNs and their patients, other health care providers, and colleagues. Reimbursement is identified as the major indirect process of care that has a direct impact on the success of the APN's business planning efforts. Equally important to success is the APN's candid self-evaluation and determination of whether an entrepreneurial or intrapreneurial approach is the most appropriate model under which to deliver patient care. The emergence of clinically focused DNP education for APNs enhances their ability to recognize and implement new practice models and innovate within existing organizations. The recognition that others in the greater health care system (e.g., other APNs, physicians, attorneys, practice managers) have skills and expertise to offer provides the APN with a safety net of advisors who can play an active role in the actualization of advanced practice nursing. Above all, the success of the APN is grounded in the professional recognition of and active participation in the larger system to ensure that the needs of patients are met through the delivery of clinically excellent, holistic health care. o Marketing and negotiation Marketing and contracting can seem overwhelming, especially when first starting out as a new APN or even seasoned APNs who have not considered the long term impact that their skills can have on their careers. Marketing is a critical skill for APNs to develop as they embark on a career or when they decide to start their own practice. The role of the APN has never been more important. It is essential that all APNs realize that marketing is not just about growing a practice or getting a job, but includes promotion for the entire profession. Marketing oneself and one's services is critical to the survival of APNs. As the health care environment changes, clients are becoming more sophisticated about what they need and want in a health care provider. APNs must become familiar with marketing concepts and be flexible enough to meet client's needs. As a result of successful marketing strategies, clients will specifically request APNs and demand their services, recognizing the value they provide in the ever-expanding and complex health care marketplace Theory • _Foundations Foundations of the APN competency are established when nurses learn about therapeutic relationships and communication in their undergraduate and graduate programs, together with growing technical and clinical expertise • _Structure of theory an approach to disciplines based on the writings of Schwab (1962) to provide guidance for development of the discipline. Schwab (1962) and others who worked in the area of disciplinary structure (Shermis, 1962) argued that disciplines comprised two components: a substantive structure and a syntax. The content of the discipline constitutes the substantive structure; it includes concepts, theories, and other knowledge, principles, and ideas that make up the knowledge base of the discipline of nursing Function of theory The function of theory is closely connected to “how good” the theory is. According to Jaccard and Jacoby (2010), a good theory is one that helps us better understand the world. Fawcett and Garity (2009) note that each theory is evaluated in terms of how good it is for guiding research and practice; thus, if we are to judge whether a theory is good, we must evaluate its utility. Shoemaker and colleagues (2004) stated the function of theory in a concise way: Its major purpose, they say, is to “condense and store knowledge . . . and put our discoveries of the nature of the world into statements” (p. 169). To accomplish this goal, the information within the theory must be good. Fawcett (2005b) detailed the functions of theory development as twofold: (1) research inquiry based on theory-testing or theory-generating research and (2) research-supported theory translated into practice. In an article published in 1992, she emphasized that a reciprocal relationship exists between conceptual models and nursing practice (see the Conceptual Models section in this chapter). The conceptual–theoretical–empirical (C-T-E) formalization for theory development has been presented by her in many publications. The C-T-E formalization is a way to analyze research by systematically testing or generating theory; it is sometimes called theoretical substruction, a term still used today by a few scholars and educators (Fawcett, 1999). Within the C-T-E formalization, there are two major C-T-E structures: (1) one C-T-E formalization for theory-testing research (top-down) and (2) one C-T-E formalization for theory-generating research (bottom-up). These functions of theory are noted throughout Fawcett’s discussion of the C-T-E structures. • _Relationship of Theory to practice and research Clinical practice generates research questions and knowledge for theory. Research guides our practice and build knowledge through theory development. Theory guides research and improve practice. In this editorial, I will describe the relationship among the three cornerstones of nursing— Practice, research, and theory—and discuss the theory-practice gap as an impediment to theory-based practice. • _Middle range theories Middle-range nursing theories are narrower in scope than grand nursing theories and offer an effective bridge between grand nursing theories and nursing practice. They present concepts and a lower level of abstraction and guide theory-based research and nursing practice strategies. • _Jean Watson theory of human caring Watson’s goal was to present nursing as a distinct entity, a profession, a discipline and science in its own right, separate from, but complementary to, medicine. In this text, Watson elaborated on the caring occasion, the transpersonal nature of caring, the 10 carative factors, phenomenal fields, the influence of time (past, present, and future), and human growth—all of which are major concepts in the theory. In this theory, all persons are considered to be unique and to have a life history, social norms, and experiences that generate a subjective reality or phenomenal field. A caring occasion occurs whenever the nurse and another person come together with their unique subjective realities, seeking to connect to each other in the present. During this moment, with the carative factors authentically present, the interaction is considered to be transpersonal (unified body, mind, and spirit; collective consciousness; one with the universe). This transpersonal caring relationship conveys deep connections to the spirit of another that transcend time, space, and physicality, ultimately affecting the consciousness field as a whole, generating endless possibilities, facilitating human growth, learning, and development. Thus, both the care provider and the one being cared for evolve from the encounter (Watson, 1985). Later, more spiritual and energy-related aspects of caring were incorporated in the theory, with heightened awareness of the nurse’s intentionality and own personal evolution (Watson, 1999). Likewise, a more sacred dimension of nursing’s work with a philosophical–ethical–moral dimension was presented in Watson’s (2006) book Caring Science as Sacred Science. Moreover, Watson has showcased her evolving views on caring resulting from personal experiences, fresh perspectives on the convergence of transpersonal caring and unitary science theories (Watson & Smith, 2002), and metaphysical orientations. In doing so, Watson has suggested that caring is a foundational framework of caring– healing professions and laid the groundwork for a revised edition of her first book, Nursing: The Philosophy and Science of Caring, Revised Edition (Watson, 2008). In this revised text, Watson first presents caritas nursing as the more mature perspective of nursing and transitioned the 10 carative factors to 10 caritas processes. In 2012, Watson authored Human Caring Science: A Theory of Nursing. This text includes a more expanded worldview of universal cosmology (human connectedness) that affirms human caring science as the “disciplinary foundation for the nursing profession” (Watson, 2012, p. xi). It showcases a more unitary-transformative grand theory of evolving consciousness that includes a global worldview of connectedness to all. In this revision Watson clarifies the 10 caritas processes. Caritas comes from the Greek word meaning “to cherish”; it connotes something that is very precious. Watson’s evolving path to this way of thinking highlights the connections between caring, spirituality, and human love. The connectedness of caring and love allows for deeper transpersonal and healing relationships, enriching for both the patient and the nurse (Watson, 2015). Working within this expanded caring consciousness allows deeper connections between the human condition and universal love. Related to this evolving theoretical stance on caring, Watson (2015) posits that this direction becomes a “converging paradigm for nursing’s future” (p. 325). A major concept in this evolved theory is the caritas field, which is described as a conscious healing presence founded on caring and love that profoundly changes the relational experience for nurses and patients alike (Watson, 2012). Thus, the more evolved clinical caritas processes reflect spirituality and love for others. • _Imogene King Conceptual system human beings are open systems interacting with the environment The central focus of King’s framework is man as a dynamic human being whose perceptions of objects, persons, and events influence his behavior, social interaction, and health (King, 1971). King’s conceptual framework includes three interacting systems with each system having its own distinct group of concepts and characteristics. These systems include personal systems, interpersonal systems, and social systems. King’s basic assumption maintained that nursing is a process that involves caring for human beings with health being the ultimate goal (Torres, 1986). The three systems that constitute King’s conceptual framework provided the basis for the development of her Theory of Goal Attainment. Imogene King was the first nurse theorist to develop a nursing framework and a middle-range theory related to it (Sieloff & Frey, 2007). Born in 1923, King graduated with a diploma in nursing from St. John’s Hospital in St. Louis, Missouri, in 1945, a bachelor’s degree in nursing education from St. Louis University in 1948, a master’s degree in nursing from St. Louis University in 1957, and a doctorate of education from Teachers College, Columbia University, in New York City in 1961. Two decades later, in 1980, she was conferred an honorary doctorate from Southern Illinois University. King began her academic career at St. Louis University, then taught at Loyola University in Chicago, and ultimately moved to the University of South Florida, where, after a distinguished career, she became professor emeritus. In 1964, King was one of the pioneers who urged nursing professionals to focus on the organization of nursing knowledge, arguing that a theoretical body of knowledge was necessary for the advancement of nursing. In her 1968 article titled “A Conceptual Frame of Reference for Nursing,” King presented the concepts of social systems, health, interpersonal relationships, and perceptions as being universal to the discipline of nursing (King, 1968, 1995). In 1971, in her book Toward a Theory for Nursing, she began to refine the conceptual system. She further refined the conceptual system when she introduced the theory of goal attainment as part of her model in A Theory for Nursing: Systems, Concepts, Process (1981a). It is in this book that she presented the concepts of environment and person, suggested that fewer dichotomies exist between health and illness, changed the terminology in her theory from “adaptation” to “adjustment,” and distinguished a person as a human being or individual rather than as “man.” The Philosophy King’s philosophical worldview is a systems and interactional approach, as evidenced by her admonition that her framework should be read “from the perspective of General System Theory and a science of wholeness” (King, 1990, p. 74). King validated her philosophy as driven by Greek philosophy and grounded in the Aristotelian–Thomistic perspective, which includes that of individuals striving for the end goal of happiness and flourishing. Persons must be motivated and guided to understand the necessity of using new and consistent behaviors to facilitate the process of goal attainment. • _King’s Theory of Goal Attainment King’s theory of goal attainment, which was derived from her conceptual framework, focuses on holism and includes nursing as a process that is interactional in nature. These interactions lead to the critical transactions that result in goal attainment (King, 1992; Sieloff Evans, 1991). Emphasis is placed on interpersonal systems and the phenomena of process and outcomes (goals). These goals become criteria for measuring the effectiveness of nursing care Theory of Goal Attainment was developed by Imogene King in the early 1960s. It describes a dynamic, interpersonal relationship in which a patient grows and develops to attain certain life goals. The theory explains that factors which can affect the attainment of goals are roles, stress, space, and time. The model has three interacting systems: personal, interpersonal, and social. Each of these systems has its own set of concepts. The concepts for the personal system are perception, self, growth and development, body image, space, and time. The concepts for the interpersonal system are interaction, communication, transaction, role, and stress. The concepts for the social system are organization, authority, power, status, and decision-making • _King’s Conceptual models The core of King’s conceptual system is the notion that human beings are open systems interacting constantly with the environment (King, 1989). King’s conceptual model incorporates three interacting systems: personal, interpersonal, and social. She discovered these three systems when she began categorizing health issues by way of a systems approach, which was shaped by von Bertalanffy’s (1968) general systems theory and interaction theory. King’s (1989) model reflects the metaparadigm concepts of person, environment, health, and nursing as systems. The concept of person is represented by the three systems (personal system, interpersonal system, and social system); a set of concepts for each system provides a method for nurses to organize their knowledge, skills, and values. Client goals are met through the transaction between the nurse and client. This interaction, which occurs over time, constitutes a transaction, such that eventually the person’s goal is met conceptual model is one part of the structure, or holarchy, of nursing knowledge. This structure consists of metaparadigms (most abstract), philosophies, conceptual models, theories, and empirical indicators (most concrete; Fawcett, 2005). Traditionally, key concepts in the metaparadigm of nursing, which nursing theories are expected to address in their conceptual underpinnings, are humans, the environment, health, and nursing (Fawcett, 2005). Although some theorists have proposed additional or expanded concepts, Fawcett's ideas inform this discussion. At this stage of the evolution, conceptual models of advanced practice nursing remain an appropriate focus. Conceptual model as “a set of relatively abstract and general concepts that address the phenomena of central interest to a discipline, the propositions that broadly describe these concepts, and the propositions that state relatively abstract and general relations between two or more of the concepts” clinical practice, APNs use conceptual models in the delivery of their holistic, comprehensive, and collaborative care • _Grand theories Newman’s theory of health Neuman’s philosophy is based on wholism, reality, and wellness, along with her assumptions about interactions of four metaparadigm concepts—person, environment, health, and nursing. She derived the term wholism from the holistic systems concept introduced by de Chardin (1955), a Catholic priest, scientist, and philosopher who believed in the wholeness of life as being the interconnectedness of the human spirit and mind. Neuman (1996) recognized her systems model as a wholistic conceptual framework for guiding nursing interactions with clients. A focal point in the Neuman model is nurses’ insight and involvement in the response of the client system to actual or potential environmental stressors. Neuman’s notion about reality mirrors gestalt theory in three ways: Emphasis on the perceived Awareness of what is and not what should be Completely understanding the patterns and structures in unity, or the whole situation in a perceptual field Margaret Newman’s Theory of Health as Expanding Consciousness (HEC) posits that “every person in every situation, no matter how disordered and hopeless it may seem, is part of the universal process of expanding consciousness – a process of becoming more of oneself, of finding greater meaning in life, and of reaching new dimensions of connectedness with other people and the world” • _Leininger’s theory of culture care knowing and understanding different cultures with respect to nursing and health-illness caring practices, beliefs and values with the goal to provide meaningful and efficacious nursing care services to people according to their cultural values and health-illness context Cultural care worldview flows into knowledge about individuals, families, groups, communities, and institutions in diverse health care systems. This knowledge provides culturally specific meanings and expressions in relation to care and health. The next focus is on the generic or folk system, professional care system(s), and nursing care. Information about these systems includes the characteristics and the specific care features of each. This information allows for the identification of similarities and differences or cultural care universality and cultural care diversity • _Nola Pender’s Health Promotion Model The Health Promotion Model was designed by Nola J. Pender to be a "complementary counterpart to models of health protection." It defines health as a positive dynamic state rather than simply the absence of disease. Health promotion is directed at increasing a patient's level of well-being. The health promotion model describes the multidimensional nature of persons as they interact within their environment to pursue health. Pender's model focuses on three areas: individual characteristics and experiences, behavior-specific cognitions and affect, and behavioral outcomes. The theory notes that each person has unique personal characteristics and experiences that affect subsequent actions. The set of variables for behavior specific knowledge and affect have important motivational significance. The variables can be modified through nursing actions. Health promoting behavior is the desired behavioral outcome, which makes it the end point in the Health Promotion Model. These behaviors should result in improved health, enhanced functional ability and better quality of life at all stages of development. The final behavioral demand is also influenced by the immediate competing demand and preferences, which can derail intended actions for promoting health. The Health Promotion Model makes four assumptions: 1. Individuals seek to actively regulate their own behavior. 2. Individuals, in all their biopsychosocial complexity, interact with the environment, progressively transforming the environment as well as being transformed over time. 3. Health professionals, such as nurses, constitute a part of the interpersonal environment, which exerts influence on people through their life span. 4. Self-initiated reconfiguration of the person-environment interactive patterns is essential to changing behavior. There are thirteen theoretical statements that come from the model. They provide a basis for investigative work on health behaviors. The statements are: 5. Prior behavior and inherited and acquired characteristics influence beliefs, affect, and enactment of health-promoting behavior. 6. Persons commit to engaging in behaviors from which they anticipate deriving personally valued benefits. 7. Perceived barriers can constrain commitment to action, a mediator of behavior as well as actual behavior. 8. Perceived competence or self-efficacy to execute a given behavior increases the likelihood of commitment to action and actual performance of the behavior. 9. Greater perceived self-efficacy results in fewer perceived barriers to a specific health behavior. 10. Positive affect toward a behavior results in greater perceived self-efficacy, which can in turn, result in increased positive affect. 11. When positive emotions or affect are associated with a behavior, the probability of commitment and action is increased. 12. Persons are more likely to commit to and engage in health-promoting behaviors when significant others model the behavior, expect the behavior to occur, and provide assistance and support to enable the behavior. 13. Families, peers, and health care providers are important sources of interpersonal influence that can increase or decrease commitment to and engagement in health-promoting behavior. 14. Situational influences in the external environment can increase or decrease commitment to or participation in health-promoting behavior. 15. The greater the commitments to a specific plan of action, the more likely health-promoting behaviors are to be maintained over time. 16. Commitment to a plan of action is less likely to result in the desired behavior when competing demands over which persons have little control require immediate attention. 17. Persons can modify cognitions, affect, and the interpersonal and physical environment to create incentives for health actions. The major concepts of the Health Promotion Model are individual characteristics and experiences, prior behavior, and the frequency of the similar behavior in the past. Direct and indirect effects on the likelihood of engaging in health-promoting behaviors. Personal factors are categorized as biological, psychological and socio-cultural. These factors are predictive of a given behavior and shaped by the nature of the target behavior being considered. Biological personal factors include variables such as age gender body mass index pubertal status, aerobic capacity, strength, agility, or balance. Psychological personal factors include variables such as self esteem self motivation personal competence perceived health status and definition of health. Socio-cultural personal factors include variables such as race ethnicity, accuculturation, education and socioeconomic status. Perceived benefits of action are the anticipated positive outcomes that will occur from health behavior. Perceived barriers to action are anticipated, imagined, or real blocks and costs of understanding a given behavior. Perceived self-efficacy is the judgment or personal capability to organize and execute a health-promoting behavior. Perceived self efficacy influences perceived barriers to action so higher efficacy result in lowered perceptions of barriers to the performance of the behavior. Activity-related affect is defined as the subjective positive or negative feeling that occurs based on the stimulus properties of the behavior itself. They influence self-efficacy, which means the more positive the subjective feeling, the greater the feeling of efficacy. In turn, increased feelings of efficacy can generate further positive affect. Interpersonal influences are cognition-concerning behaviors, beliefs, or attitudes of the others. Interpersonal influences include: norms (expectations of significant others), social support (instrumental and emotional encouragement) and modeling (vicarious learning through observing others engaged in a particular behavior). Primary sources of interpersonal influences are families, peers, and healthcare providers. Situational influences are personal perceptions and cognitions that can facilitate or impede behavior. They include perceptions of options available, as well as demand characteristics and aesthetic features of the environment in which given health promoting is proposed to take place. Situational influences may have direct or indirect influences on health behavior. Within the behavioral outcome, there is a commitment to a plan of action, which is the concept of intention and identification of a planned strategy that leads to implementation of health behavior. Competing demands are those alternative behaviors over which individuals have low control because there are environmental contingencies such as work or family care responsibilities. Competing preferences are alternative behavior over which individuals exert relatively high control. Health-promoting behavior is the endpoint or action outcome directed toward attaining a positive health outcome such as optimal well-being, personal fulfillment, and productive living. • _Non-nursing theories Interpersonal relations (Harry Stack Sullivan) • Humanism (Carl Rogers) • Existentialism (Viktor Frankl and Rollo May) • Positive psychology (Martin Seligman and Mihaly Csikszentmihalyi) • Transpersonal psychology (Anthony Sutich) NON-NURSING THEORIES FOCUSED ON INTERPERSONAL RELATIONSHIPS Interpersonal Relations Theory Interpersonal philosophy defines personality as behavior that can be observed within interpersonal relationships. Interpersonal theorists emphasize the socialization of humans throughout their developmental stages. Failure to proceed through these stages satisfactorily lays the foundation for later maladaptive behavior. Supporters believe that unsatisfactory interpersonal relations are the primary cause of maladaptive behaviors. The interpersonal perspective also is concerned with the anxiety-arousing aspects of interpersonal relationships. At present, no systemic view of human nature and behavior is based entirely on interpersonal theory or the social context in which people live and work. The closest approximation may be the viewpoint developed by the neo-Freudian psychologist Harry Stack Sullivan. Several nursing theories also can be classified as interpersonal relations theory (see Table 12-2). Table 12-2 Interpersonal Theories and Theorists Theory/Discipline Theorist Therapeutic Process Interpersonal (Psychiatry) Harry Stack Sullivan The purpose of all behavior is to get needs met through interpersonal interactions, not personality reconstruction as in psychodynamic theories. He coined the terms participant observer and security operations. Nurse–Patient Relationship (Nursing) Hildegard Peplau Influenced by Sullivan’s theory. First nurse theorist to describe the nurse–client relationship as the foundation for the professional practice of psychiatric nursing. Used the technique of process recording to facilitate communication and interpersonal skill building. Synonymous with the concept of the helping relationship as used in counseling. Nursing Process Theory (Nursing) Ida Jean Orlando Study grew out of her dissatisfaction with the possibility that nursing care was governed by organizational rules rather than attention to client needs and her desire to offer nursing students a theory of effective nursing practice. She was also able to link effective nursing care to the nurse’s knowledge of patient needs that are validated by patient response(s). Human-to-Human Relationship Model (Nursing) Joyce Travelbee Focuses on meaning in the nurse–client relationship and the relief of client suffering through the use of communication skills within the phases of the nurse–client relationship. • _Health Related-Quality of life Interest in translating theories into practical actions—such as assessment of health-related experiences and interventions used to promote positive responses to those experiences—has increased dramatically during the last several years in conjunction with an increased emphasis on evidence-based practice. Translational research is a research process used to determine which conditions, costs, and resources are required to progress from theory generation and theory testing to evidence-based practice. The goal of translational research is to decrease the time required for translation of theories into assessment tools and intervention protocols that will improve people’s health-related quality of life. • _Humanistic Learning Theory emphasizes a person-centered approach and stresses the importance of feelings over thoughts. The subjective human experience of each individual is seen as being of value, and human relationships depend on being spontaneous, authentic, and empathetic. The goal is to help individuals express their inner creativity, reach their human potential, and strive for personal growth. Motivation is derived from a person’s needs, feelings about the self, and desire for positive self-development. Learning is facilitated by allowing people freedom and choices, by supporting their expressiveness and efforts at creative problem solving, and by making learning enjoyable. To achieve these goals, teachers, therapists, and health professionals need to engage in a collaborative relationship with students and patients based on authentic behavior, honest dialogue, and genuine therapeutic listening. When learners are encouraged to make wise choices and are free to pursue creative interests, the retention and transfer of information are more likely than in an authoritarian approach to education. Education, therapy, and healing all need to take place within a nurturing context • _Behaviorist Learning Theory According to behaviorist theory (also referred to as behaviorism), since there is no way to know accurately what is going on within a person’s mind, the focus should be on only what is directly observable. What is observable in any learning situation are the stimulus conditions (S) in the environment and the behavior (movements, acts, actions) that is exhibited in response (R) to stimulus conditions (Kazdin, 2013). In this model, learning is relatively simple; it is based on the associations people make between stimuli and responses (termed the S–R model of learning or association learning), and the belief that life is largely a matter of habit that requires little thinking. For example, people learn their health habits, such as their responses to foods, their physical exercise patterns, and their reactions to stress. For better or worse, much behavior is learned in the family through socialization and is passed from generation to generation. According to behaviorists, what is learned can be unlearned by modifying stimulus conditions in the environment or changing the response to stimuli. The route to learning, then, goes through behavior and action—the learning is in the doing— rather than through inner processes such as thinking and feeling. Changes in thinking and feeling, in fact, may come about by first changing behavior; thoughts and emotions then follow. For instance, if nurses who lack self-confidence are given responsibilities where they can perform well, their self- confidence may improve over time. Thus the route to personal change proceeds through behavior and practice. Behaviorist principles are useful for breaking bad habits, designing practice sessions for sports and rehabilitation, and working with people who are more comfortable engaging in actions than reflecting on thoughts and emotions. Behaviorism provides the foundation for behavior modification programs, behavioral medicine, commercial advertising, and some therapies. The principles of the behaviorist model of learning can be applied to animals as well as people. To promote learning, behaviorists change the stimulus–response (S–R) associations the learner makes in the environment and may follow a learner’s response with some kind of reinforcement. To learn, of course, people must be motivated to make a response. Motivation is based on drive reduction—that is, having a drive that needs to be alleviated or satisfied. Primary drives are unlearned, such as the drive for food, warmth, sleep, sex, and avoidance of pain. In contrast, secondary drives are learned, such as the drive for financial security, popularity, or achievement. Culture plays an important role in learning secondary drives. It is difficult to encourage people to learn if there is no drive to be reduced, such as when people are satisfied, complacent, and satiated, or when another drive overpowers the drive to learn. According to behaviorist learning theory, the process of learning proceeds as follows. Once a primary connection is made between the stimulus and the response, learning can be said to have occurred, which is somewhat of an “all or nothing” experience (e.g., not being able to ride a bike, then suddenly being able to steer and ride the bike; not being able to insert an intravenous [IV] line after many tries, then suddenly inserting it correctly). Most initial learning needs to be strengthened with practice. According to behaviorists, memory and retention are helped by repeating S–R connections, although there is a point at which practice becomes redundant and a waste of time. In its early stage, learning tends to be generalized to similar objects, situations, and stimuli. With additional and varied experiences, however, learners begin to make more sophisticated distinctions, called discrimination learning. In a sense, advanced practice nursing education is an exercise in discrimination learning. The goal of most learning is to be able to transfer what is learned to other settings, such as teaching self-care to patients in the hospital—learning that is intended to be transferred to the home and workplace once patients have been discharged from the hospital. Transfer of learning is enhanced when the stimulus conditions and responses in the practice session and in the transfer situation are similar. Thus, working with patients in a hospital or rehabilitation center is necessary, but it may not be sufficient for the transfer of patients’ learning outside the institution. In the behaviorist model, the learner is relatively passive. The teacher or instructor plays a significant role in influencing learning through astute observation of S–R conditions and learners’ reactions. Teachers are also responsible for the selection of motivating and well-chosen experiences to maximize learning, retention, and transfer. Likewise, the effectiveness of teaching depends on identifying appropriate stimulus conditions, reinforcement, practice, and feedback to ensure learning. Two behaviorist perspectives on how learning occurs have had a significant impact on education and promoting behavior change: (1) classical conditioning and (2) operant conditioning. Conditioning is a powerful tool of learning, largely because little, if any, thinking is required in the learning process. • _Cognitive Learning Theory focuses on the perceptions, thinking, reasoning, memory, developmental changes, and processing of information that transpire within the learner (Matlin, 2013; Sawyer, 2006). Taking issue with the behaviorists, researchers advocating this perspective undertook a series of cognitive experiments that demonstrated a number of factors related to learning, such as reward is not necessary to learn, and thinking and reasoning develop in stages over the course of childhood and adolescence. Researchers also documented that learning is an active process in which learners perceive, interpret, and respond to the environment in their own ways, with social factors having a strong influence on each learner’s construction of reality. The introduction of several important subtheories has contributed to the advancement of cognitive theory over more than a century, with cognitive theory currently influencing much of educational practice. Cognitive theory is useful for appreciating the different ways that individuals approach and respond to any learning situation, recognizing the complexity of learning, and prompting instructors to take their cues from learners to be effective. According to the basic principles of cognitive theory, the way individuals approach any learning situation reflects their level of cognitive development, their past experiences, the way they perceive and process information, and the way they think about themselves and respond to instruction. Attention is the key to learning, with each learner incorporating, organizing, and interpreting new information in relation to what he or she already knows. Learners have an awareness of how they acquire knowledge and think—a capacity termed metacognition. The ability to alter his or her thoughts, beliefs, and behavior rests on the learner discovering some kind of insight that causes him or her to reorganize these perceptions and thoughts. Thus a change in one’s perception and thinking may lead to behavior change. In cognitive theory, motivation is based on the learner’s goals and expectations, which create disequilibrium and a tension to act. People without goals or with low expectations for themselves are not motivated to act. Conversely, people whose goals and expectations are too high may be at risk for disappointment and becoming discouraged about education and learning. Research suggests that having realistic goals (goals that stretch accomplishment but are achievable for the person) and taking responsibility for one’s actions (internal locus of control) result in better academic performance, compared to having unrealistic goals (too high or too low) and blaming outside forces for one’s success or failure (external locus of control). In using cognitive theory, the educator’s job is to assess readiness to learn; provide a variety of meaningful, developmentally appropriate experiences; and allow individuals to discover what they learn for themselves. Teachers and other students may provide feedback to correct faulty conceptions. Thus, according to this view, education is a social experience that benefits from human interactions. Sharing different perceptions and ways of thinking enhances learning and fosters an appreciation for the rich diversity in human thought. When operating from a cognitive perspective, instructors need to be organized, with clear goals and expectations and a well-structured approach to presenting information. It may be helpful to provide a framework for understanding (advance organizers) to prepare learners for maneuvering through information on their road to discovery and insight. Creativity and original thought contribute to the excitement of learning and are encouraged. Creativity is engendered by a novel and insightful reorganization of information and experience. Practice for the sake of practice—such as using boring repetition, requiring rote memory, and demanding that thinking conform to instructor expectations and remain “inside the box”—is not helpful. Instead, offering diverse experiences linked to learning is a more beneficial kind of practice. Memory and retention are facilitated by the organization and meaningfulness of the educational material, along with proper pacing and time to reflect on the information. Recognition must be given to the various ways that individuals approach and respond to what is to be learned. Because learning is subject to social and personal influences within a cognitive framework, it is important to determine how information has been perceived, interpreted, and stored. It may be helpful to offer techniques that aid memory and transfer (Matlin, 2013). When a cognitive theoretical approach is used, it is essential to give feedback to learners so they can make adjustments in how they process information. The transfer of learning to future situations is not likely to be total, however, since every experience and situation where learning is to be performed will have its own set of differences and anomalies. Thus, the emphasis is on fortifying learners’ abilities to solve problems by providing a variety of experiences, encouraging flexibility in thinking and creativity, and promoting feelings of competence or self-efficacy. Such training prepares learners to adjust to new cognitive patterns and changing situations—and it explains why clinical experiences need to be carefully selected and structured for nursing students. Having students rotate through different kinds of healthcare facilities broadens their clinical education. • _Conceptual-Theoretical-Empirical empirical indicator as “a very concrete and specific real world proxy for a middle-range theory concept; an actual instrument, experimental condition, or procedure that is used to observe or measure a middle-range theory concept. The information obtained from empirical indicators is typically called data” The C-T-E system is a whole system of nursing knowledge that is implemented for conceptual model- based or theory-based scientific practice. A conceptual model, a theory (or more than one), and empirical indicators are strongly linked to form a C-T-E system for application of a conceptual model or theory to nursing practice, research, and education. Fawcett (2005b) defined the C-T-E system as “service to the society guided by knowledge that is specific to the discipline of nursing, as articulated in conceptual models of nursing and nursing theories” (p. 32). Fawcett described two functions of the C-T-E system: (1) “to provide an intellectual lens” for human beings participating in nursing, their health, and their environment, and (2) “to provide a purposeful and systematic process for practice, that is, a practice methodology” (p. 33). The C-T-E system can be implemented by nursing departments within healthcare institutions, advanced practice nurses and other nurses working in private practice, and nursing educators to guide curriculum development or to teach students this system for practice. This section provides a brief synopsis of the substantive elements of the C-T-E system for practice. Three substantive elements must be considered if the C-T-E system is adopted and used. Referring back to the discussion of the components of nursing knowledge will help clarify this section’s meaning. Figure 5-2 provides an overview of the holarchy translated into practice. • _Application to Nursing practice Along those lines, patterns that reveal potential significance for nursing involvement can be identified. Changes in philosophy, as well as in social context, call for new methods to address pressing issues in nursing. Recognition of the role of culture and social context requires increasing development, application, and evaluation of methods effective at capturing those aspects of existence. These changes also require nurses who understand the philosophy and knowledge development enterprises well enough to articulate the value of differing approaches to inquiry. Advanced practice nurses will provide a critical link in this process through their skill and understanding of both the knowledge development and scientific enterprises, as well as the realm of application in practice. Nursing science work without that critical link to practice is likely to fail in meeting the needs of nurses who apply that science on a daily basis. Nurses at levels prior to advanced practice need leadership and guidance from advanced practice nurses to offer a few problems suitable for inquiry, as well as to help evaluate and apply new information for evidence-based practice. • _Theory analysis and evaluation Theories are formulated to explain, predict, and understand phenomena and, in many cases, to challenge and extend existing knowledge within the limits of critical bounding assumptions. The theoretical framework is the structure that can hold or support a theory of a research study. • _Selecting a theory Selecting a Theory for Nursing Research Before starting to write a proposal, Fawcett (1999) suggests that each investigator become familiar with the research topic and the conceptual model that will guide the study. She reiterates that this is done by an immersion into the literature and a thorough study of the research topic. In addition, a comprehensive literature search should be done several months before making a proposal of the study. This much time must be given to allow the proper amount of time for reading and thinking about both the content of the proposed study and the conceptual model to provide the basis for the study. It is during this time that the most appropriate middle range theory can be decided upon for use in the research. As nurse researchers shift away from using grand nursing theories and begin to consider using middle range theories, the philosophical underpinnings of the theory itself become of decreased importance. The emphasis shifts from the philosophical basis of the nursing theory to how the middle range theory is applied in research and practice. Thus, time previously spent with the philosophy and background of the theorist can now be devoted to ensuring the proper fit between the research questions to be studied and the middle range theory. Each nurse researcher should ask the following questions about the middle range theory proposed for use in his or her research: • Does the theory seem to fit the research that you wish to do? • Is it readily operationalized? • What has been the primary application for this theory in the past? • Where has the theory in question been applied and used before? • How well has the theory performed at describing, predicting, and/or explaining the phenomena that it relates to? • Does the theory relate to and address the research hypothesis in its description and explanation? • Does the hypothesis flow from the research problem? • Does the theory address the primary and secondary research questions? • Are the theory’s assumptions congruent with the assumptions that are made for this research? • Is it oriented to outcomes that are critical to patients and does not describe what nurses perform? • Are tools available to test relationships of the theory or do they need to be developed? The nurse researcher should consider several different middle range theories as possibilities for use. A thorough analysis and evaluation of these theories in question should be done before selecting one. Subsequently, the nurse researcher should become familiar with all aspects of the theory, using the questions provided in the discussion above. It is essential to have a sound understanding and be in total agreement with the theory selected before beginning the study. This is accomplished by becoming immersed in the literature about the middle range theory in question and arriving at a thorough and complete understanding of the theory before using it. The nurse researcher should try to understand the middle range theory by identifying all the major concepts. The definitions of these concepts, in turn, should be studied for this particular theory, to make sure that the meanings have not been changed slightly over time as they are described in the literature. In addition, the major concepts should be examined to determine how they relate to each other. Next, the researcher needs to decide if he or she can accept the premises, rationale, and presuppositions that the nursing theory is based upon before adopting it for use (McKenna, 1997). Finally, it is necessary to determine what means of measurement have been used with previous studies employing this theory. It will be important to know if new measurement tools need to be obtained or if similar tools can be employed for the study at hand. It is evident that to decide upon and use a middle range theory effectively in nursing research, the potential nurse researcher must do a thorough analysis and evaluation of the middle range nursing theory. The following section will provide the guidance for conducting an evaluation of a middle range theory before selecting it for use in a research study. • _PICOT acronym PICOT format to ask a question about the problem, which may be a way to assess people or an intervention. This format takes into account the P= patient population (P), I= an assessment or intervention (I), C=group comparisons (C), O=the desired outcome (O), T= and time (T) • _Johnson’s Behavioral Systems Model Johnson’s Behavioral System Model The goals of nursing in Johnson’s behavioral system model are to maintain or restore behavioral system balance. Her model for nursing presents the patient as a living open system, comprising a collection of behavioral subsystems that interrelate to form a behavioral system. Because the subsystems are linked and open, a disturbance in one subsystem will likely have an effect on the other subsystems (Johnson, 1980). The seven subsystems of behavior proposed by Johnson include the (1) achievement, (2) affiliative, (3) aggressive, (4) dependence, (5) sexual, (6) eliminative, and (7) ingestive subsystems. Subsystems include four structural components: The drive or goal of the subsystem reflects the motivation or reasons for the behaviors of the subsystem. Motivational drives directing the activities or behaviors of the subsystems may vary from strong to weak and are constantly changing because of maturation, experience, and learning. The set is the ordinary or normal behaviors that the patient prefers to use to meet the goal of a subsystem. The choice represents the options that are available to patients to meet their subsystem goals. This structural component is influenced by variables such as gender, age, culture, socioeconomic status, and health status. The action or behavior emanates as a consequence of the previous three structural components. The question of concern in relation to the structural component of behavior is whether the behavior is efficient and effective in relation to subsystem goal attainment. This is the only structural component that can be directly observed (Johnson, 1980). Each of the seven subsystems has a function. The achievement subsystem functions to control or master an aspect of self or environment to achieve a standard. This subsystem encompasses intellectual, physical, creative, mechanical, and social skills. The affiliative or attachment subsystem forms the basis for social organization. Its consequences include social inclusion, intimacy, and the formation and maintenance of strong social bonds. The aggressive or protective subsystem functions to protect and preserve the system. The dependency subsystem promotes helping or nurturing behaviors. Its consequences include approval, recognition, and physical assistance. The sexual subsystem has the function of procreation and gratification and includes development of gender-role identity and gender-role behaviors. The eliminative subsystem addresses “when, how, and under what conditions we eliminate,” whereas the ingestive subsystem “has to do with when, how, what, how much, and under what conditions we eat” (Johnson, 1980, p. 213). Johnson asserted that each of these subsystems, as well as the system as a whole, has certain functional requirements that must be met through the effort of the individual or through outside assistance for continued growth, development, and viability. These functional requirements include (1) protection from noxious influences with which the system cannot cope, (2) nurturing through input of supplies from the environment (examples include food, friendship, and caring), and (3) stimulation by experiences, events, and behavior that would enhance growth and prevent stagnation (Johnson, 1980, p. 212). The nursing process for the behavioral system model is Johnson’s nursing diagnostic and treatment process. The components of this process include determination of the existence of a problem, diagnostic classification of problems, management of nursing problems, and evaluation of behavioral system balance and stability. When nurses use Johnson’s conceptual model as part of advanced practice, the focus of the assessment process is obtaining information to evaluate current behavior in terms of past patterns, determining the effects of the current illness on behavioral patterns, and establishing the maximum level of health. The assessment specifically focuses on gathering information related to the structure and function of the seven behavioral subsystems, as well as the environmental factors that influence the behavioral subsystems (Holaday, 2006). During the assessment phase, APNs obtain data about the nature of the behavioral functioning related to goal attainment—specifically, whether the patient’s behavior is purposeful, orderly, and predictable. APNs need to interview the patient and family also to assess the condition of the subsystem structural components and evaluate the patient’s behavior for behavioral system balance and stability. From the data collected, APNs make inferences and independent judgments related to the organization, interaction, and integration of the subsystems (Fawcett, 2005). Within Johnson’s conceptual model, problems may be classified as internal subsystem problems or intersystem problems. Internal subsystem problems include situations when functional requirements are not met, there is inconsistency or disharmony among components of the subsystem, or behavior is not appropriate for the culture. Intersystem problems include situations when the behavioral system is dominated by one or two subsystems or a conflict exists between two or more subsystems (Fawcett, 2005). The goals of the management of nursing problems for APNs and other nurses are to restore, maintain, or attain the patient’s behavioral system balance and stability and to help the patient achieve an optimal level of balance and functioning. The goals of management could be accomplished through the temporary imposition of external regulatory or control mechanisms, the repair of damaged subsystem structural components, or the fulfillment of subsystem functional requirements (Johnson, 1980). For example, APNs may temporarily impose external regulatory or control mechanisms by setting limits for behavior, inhibiting ineffective behavioral responses, assisting the patient to develop new responses, and reinforcing appropriate behaviors. Repair of damaged structural components includes interventions that modify the drive or motivation, or redirect goals. Interventions can also attempt to alter set behaviors through instruction or counseling and add choices through teaching new skills. In addition, the nurse can intervene to fulfill functional requirements by protecting the patient from overwhelming negative influences that exceed the patient’s coping ability, by nurturing the patient through input of adequate essential supplies, and by providing stimulation to enhance growth and prevent stagnation (Fawcett, 2005; Johnson, 1980). Evaluation is based on the attainment of the goal of balance in the identified subsystems. Evaluation of behavioral system balance and stability is accomplished as the APN compares the patient’s behavior after treatment to indices of behavioral system balance and stability (Health Policy and Health Promotion) Health People 2020 – to improve access to comprehensive, quality, primary care services. Goals: • Increase the quality and years of healthy life • o Eliminate health disparities among Americans • • Health People 2020 - The program is an initiative that develops evidence-based practice objectives designed to improve the health of all Americans. • These objectives are targeted to be followed over a 10-year period 4 foundational healthcare measures 1. General health status 2. Health-related quality of life & well-being • 3. Determinants of Health – aim to create social & physical environments that promote good health for all • Policymaking • Social factors • Health services • Individual behavior • Biology and genetics 4. Reduce Health Disparities • Electronic Medical Record (EMR) – Pros: allows for sharing of health information between healthcare entities & with patients, thereby reducing the cost of care, improving care efficiency, avoiding readmission and decreasing duplicate testing. Cons: the potential for data loss in the event of computer or system failure • Medicaid - a government health insurance program for low-income individuals funded by federal & state entities and administered by the state. * Varies from state-to-state. • Medicare – federally funded health insurance program for those >65yrs, those with severe disability no matter income level, or those with ESRD. Qualifying conditions: US citizen, non US citizens after 5 years of permeant residence in the US, veterans are eligible after 65yrs. requirements: • Are age 65 or older • Have end-stage renal disease (ESRD) • Have amyotrophic lateral sclerosis (ALS) • been on disability for two years A. Medicare Part A covers medically necessary inpatient care and supplies; skilled nursing facility B. Medicare Part B covers nursing home/custodial care (ADL’s), home health services, durable medical equipment, outpatient care & preventative services (i.e. 1 mammogram every 12 months) in women 40 and older. Part B DOES NOT cover eyeglasses or routine dental care. • The Barthel Index is a measurement of ability to perform ADL’s C. Medicare Part C – HMO D. Medicare Part D covers prescriptions • A single payer healthcare system refers to a system where in essence the government runs a nationwide insurance plan that pays for all healthcare costs of its members. • Peer Review / 360 degree Evaluation – employees rate other employees in the same job classification, through the use of established criteria. The system has the potential to offer honest & specific feedback that allows the individual to make improvements or adjustments to meet objectives and performance standards • Fidelity – Loyalty & dedication; keeping a promise • Beneficence – promote good & prevent harm • Non-Maleficence – To do no harm • Justice - right to fair and equitable treatment • Autonomy – The right of patients to make clinical decisions about their medical care, assuming the patient is rational & can make informed decisions about care • Veracity – The duty to be truthful • Utilitarianism – produces the greatest good for the greatest number of people • _Health Promotion "the process of enabling people to increase control over, and to improve, their health. To reach a state of complete physical, mental and social well-being, an individual or group must be able to identify and to realize aspirations, to satisfy needs, and to change or cope with the environment. Health is, therefore, seen as a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities. Therefore, health promotion is not just the responsibility of the health sector, but goes beyond healthy life-styles to well-being". Population-based Health Policy Population health, a field which focuses on the improvement of the health outcomes for a group of individuals, has been described as consisting of three components: "health outcomes, patterns of health determinants, and policies and interventions".[1] Policies and Interventions define the methods in which health outcomes and patterns of health determinants are implemented. Policies which are helpful "improve the conditions under which people live".[2] Interventions encourage healthy behaviors for individuals or populations through "program elements or strategies designed to produce behavior changes or improve health status".[3] Policies and interventions are needed due to the inequalities amongst populations and the inconsistent way care is administered. Policies can include "necessary community and personal social and health services" [2] as well as taxes on alcohol and soft drinks and implement smoking cessation policies. Interventions can include therapeutic or preventative health care and may also include actions taken by the individual or by someone on behalf of the individual. The application of population health is determined by the policies and interventions which can be implemented within an organization, city, state or country. Health policy exists within this larger realm of social policy. Because policy generally is rooted in social values and ideologies, the discussion of health policy begins with the recognition of the values and ideology that shape the organization of the healthcare system. The historic course of American health policy is best described in terms of shifting beliefs about access to care. Sometimes we have stridently pursued health care as a right for all. Sometimes we have treated it as a privilege (Knowles, 1977). These competing values (i.e., a right versus a privilege) are simultaneously and continually at work. • _Legislative and public policy Public policy, the term used to describe government action, is typically divided into three areas: foreign policy, economic policy, and social policy (Lowi & Ginsberg, 1998). The objective of foreign policy is to defend national sovereignty. Economic policy is designed to promote and regulate markets. Although foreign and economic policy seek to promote the political and economic well-being of American society, policies in these areas typically do not have equal impact on all sectors of society. Some groups may benefit, whereas others might suffer undue consequences. The North American Free Trade Agreement benefited the overall economy, but many persons who held manufacturing jobs found themselves unemployed as production moved from the United States to countries with lower production costs. Social policy often becomes the means by which the unintended consequences of policies that seek to better the overall condition of American society are addressed. Government actions are the ways in which the provision of the basic necessities—food, shelter, health care, and education—is ensured (Midgley & Livermore, 2008). Social policy is redistributive by its very nature. Its goal is to achieve greater social equity. • _Epidemiology Epidemiology is the study and analysis of the distribution, patterns and determinants of health and disease conditions in defined populations. It is the cornerstone of public health, and shapes policy decisions and evidence-based practice by identifying risk factors for disease and targets for preventive healthcare. • _Population Focused Health Promotion and Maintenance: Clinical Intervention Population health is the distribution of health outcomes within a population, the determinants that influence distribution, and the policies and interventions that affect the determinants.2,3 These three key components—health outcomes, health determinants, and policies—serve as the foundation for this chapter and those that follow. CDC views population health as an interdisciplinary, customizable approach that allows health departments to connect practice to policy for change to happen locally. This approach utilizes non- traditional partnerships among different sectors of the community – public health, industry, academia, health care, local government entities, etc. – to achieve positive health outcomes. Population health “brings significant health concerns into focus and addresses ways that resources can be allocated to overcome the problems that drive poor health conditions in the populationExternal.” • _Community needs assessment A community needs assessment identifies the strengths and resources available in the community to meet the needs of children, youth, and families. The assessmentfocuses on the capabilities of the community, including its citizens, agencies, and organizations • _Physiologic • _Psychosocial • _Environmental • _Global • _Social • _Developing prevention focused interventions • _Ordering and interpreting screenings • _Vaccinations • _Anticipatory guidance Anticipatory guidance is a nursing intervention used to prepare patients or family members for an anticipated developmental or situational crisis (Rakel, 1992; Thobaben, 1999). When patients know what to expect they can learn the healthy coping strategies needed to help them through a crisis. • _Counseling for health behavior modification • _Primary, secondary, tertiary prevention here are 3 levels of disease prevention Primary Prevention - trying to prevent yourself from getting a disease. Secondary Prevention - trying to detect a disease early and prevent it from getting worse. Tertiary Prevention - trying to improve your quality of life and reduce the symptoms of a disease you already have. • _Population Focused Health Promotion and Maintenance: Program Development- “differences in the incidence, prevalence, mortality, and burden of diseases, as well as other adverse health conditions or outcomes that exist among specific population groups,” and have been well documented in subpopulations based on socioeconomic status, education, age, race and ethnicity, geography, disability, sexual orientation, or special needs.65,66 These subpopulations experience disproportionate burdens of illness as a result of the barriers imposed by discrimination, as well as those from differences in culture, language, beliefs, and values, which lead to considerable social and economic burdens associated with poor quality of care and lack of access to affordable, quality primary care.66–68 Qualities of a Leader • _Advocacy -public support for or recommendation of a particular cause or policy. • _Implementation- the process of putting a decision or plan into effect; execution • _Monitoring-observe and check the progress or quality of (something) over a period of time; keep under systematic review. • _Evaluating effectiveness Measuring the extent to which targets are being met, and detecting the factors that hinder or facilitate their realization. It also involves establishing cause-effect relationships about the extent to which a particular policy (or a set of policies) produces the desired outcome. • _Incorporating Theory and Research Theories are formulated to explain, predict, and understand phenomena and, in many cases, to challenge and extend existing knowledge within the limits of critical bounding assumptions. ... The theoretical framework introduces and describes the theory that explains why the research problem under study exists. • _Hospital classifications What Differentiates the Various Types of Hospitals? In the U.S., you can differentiate hospitals based on a variety of factors that includes functionality, size, location, ownership and specialization. Here they are in more detail: 1. Functionality Functionality refers to whether the hospitals are general-purpose, teaching hospitals, acute care facilities, long-term hospitals, community hospitals, research hospitals or if they provide trauma care for patients. It refers to how the hospitals themselves function within the communities they serve. 2. Size There are three primary classifications when it comes to size: 1 Small hospitals: Fewer than 100 beds 2 Medium hospitals: 100 to 499 beds 3 Large hospitals: 500 or more beds Typically, these sizes are classified by the number of beds they have — although there can be some variation within these groups of hospitals and medical centers. 3. Location You can also classify hospitals by their locations. Rural hospitals aid smaller communities and often have limited access to advanced equipment or specialized procedures and techniques. Since they also face competition, urban hospitals serve larger metropolitan areas and must often offer a wide degree of versatility when it comes to treatment options and patient experience. 4. Ownership Knowing who owns the hospital will also tell you a great deal about how the hospital will operate. Some hospitals are part of larger networks that offer a streamlined approach to management. While some physicians feel this improves efficiency and patient experience, some feel it removes the emphasis from the patient and makes treatment less personal. Private hospitals often offer access to the latest technologies and equipment, but may under-serve community members who need healthcare the most. Government-supported facilities operate via grants and other public funds. They have greater restrictions but also reach out to members of the community who may not otherwise receive healthcare and medical treatment. 5. Specializations Specialized hospitals appeal to physicians who entered the medical field with plans to treat people with a specific condition. Most physicians choose specializations due to personal reasons, an area of intense interest or a desire to provide a comfortable life for themselves and their families. • _Cultural diversity Cultural diversity is the quality of diverse or different cultures, as opposed to monoculture, the global monoculture, or a homogenization of cultures, akin to cultural decay. The phrase cultural diversity can also refer to having different cultures respect each other's differences. The phrase "cultural diversity" is also sometimes used to mean the variety of human societies or cultures in a specific region, or in the world as a whole. Globalization is often said to have a negative effect on the world's cultural diversity. • _Vocational Rehab The Division of Vocational Rehabilitation Services (DVRS) helps people with disabilities achieve their goals for employment and independence. If you have a disability that prevents you from achieving career success or independence in the community of your choice, DVRS can connect you to services and resources to help you meet your goals • _CDC CDC works 24/7 to protect America from health, safety and security threats, both foreign and in the U.S. Whether diseases start at home or abroad, are chronic or acute, curable or preventable, human error or deliberate attack, CDC fights disease and supports communities and citizens to do the same. CDC increases the health security of our nation. As the nation’s health protection agency, CDC saves lives and protects people from health threats. To accomplish our mission, CDC conducts critical science and provides health information that protects our nation against expensive and dangerous health threats, and responds when these arise. • Detecting and responding to new and emerging health threats • Tackling the biggest health problems causing death and disability for Americans • Putting science and advanced technology into action to prevent disease • Promoting healthy and safe behaviors, communities and environment • Developing leaders and training the public health workforce, including disease detectives • Taking the health pulse of our nation ARHQ Agency for Healthcare Research and Quality (AHRQ) is the lead Federal agency charged with improving the safety and quality of America’s health care system. AHRQ develops the knowledge, tools, and data needed to improve the health care system and help Americans, health care professionals, and policymakers make informed health decisions. AHRQ works within the U.S. Department of Health and Human Services (HHS) and with other partners to make sure that the evidence is understood and used in an e ort to achieve the goals of better care, smarter spending of health care dollars, and healthier people. In 1999, an Institute of Medicine report, “To Err Is Human,” documented serious patient safety problems in our health care system. In the intervening years, AHRQ has led the Nation in responding to those issues and improving the safety of health care. Using AHRQ’s research and how-to tools, the U.S. health care system prevented 1.3 million errors, saved 50,000 lives, and avoided $12 billion in wasteful spending from 2010– 2013. But, even with these successes, safety is far from optimal, and AHRQ’s work continues. • _United States Protective and Safety Task Force (USPSTF) The U.S. Preventive Services Task Force is an independent, volunteer panel of national experts in disease prevention and evidence-based medicine. The Task Force works to improve the health of all Americans by making evidence-based recommendations about clinical preventive services. Created in 1984, the U.S. Preventive Services Task Force is an independent, volunteer panel of national experts in prevention and evidence-based medicine. The Task Force works to improve the health of all Americans by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications. All recommendations are published on the Task Force’s Web site and/or in a peer-reviewed journal. Task Force members come from the fields of preventive medicine and primary care, including internal medicine, family medicine, pediatrics, behavioral health, obstetrics and gynecology, and nursing. Their recommendations are based on a rigorous review of existing peer-reviewed evidence and are intended to help primary care clinicians and patients decide together whether a preventive service is right for a patient's needs. The Task Force assigns each recommendation a letter grade (an A, B, C, or D grade or an I statement) based on the strength of the evidence and the balance of benefits and harms of a preventive service. The Task Force does not consider the costs of a preventive service when determining a recommendation grade. The recommendations apply only to people who have no signs or symptoms of the specific disease or condition under evaluation, and the recommendations address only services offered in the primary care setting or services referred by a primary care clinician. Since 1998, the Agency for Healthcare Research and Quality (AHRQ) has been authorized by the U.S. Congress to convene the Task Force and to provide ongoing scientific, administrative, and dissemination support to the Task Force. Each year, the Task Force makes a report to Congress that identifies critical evidence gaps in research related to clinical preventive services and recommends priority areas that deserve further examination. • _The Affordable Care Act The Affordable Care Act (ACA) is changing that landscape. It is a means to fill the gaps that currently exist through the provision of low-cost insurance and high-quality care. It aims to control costs through financial incentives that should improve care coordination and patient outcomes. Although the program met tremendous resistance since it was debated in Congress, it represents an important step to ensure access and quality care for all. The ACA is changing the landscape of the healthcare delivery system in the United States. Designed to fill insurance gaps that currently exist, the legislation’s aim is to provide coverage through low-cost insurance and high-quality care. These problems are broad, and so are their solutions. Success is not guaranteed. It is hard to predict exactly what the impact of the policies will be on the health of Americans and the healthcare delivery system. “Every citizen deserves the right to a healthy and productive life. That’s the politics of health care” (Nickitas, 2013, p. 265). The fact remains that the United Sates is the only developed country without universal access to health care or health insurance. Not every state is participating in Medicaid expansion, and funding has not increased for safety-net services. Approximately 30 million individuals living in the United States are not American citizens and will remain uninsured. The ACA is an amazing accomplishment for the Obama administration. It is a step closer to a cohesive national system. The next administration that proposes health system reform will use Obama’s successes and failures as a guide to achieving the next step. Strong political leadership will be imperative. General Document Guidelines Page numbers are cross-referenced with the APA Publication Manual , 6 th ed. If using another APA 6 th ed. reference source, search for topic in table of contents or index. Margins p. 229 1 ” at the top, bottom, left, and right of every page Spacing p. 229 Double space entire paper—no extra spaces (exception: a heading by itself at the bottom of a page—move heading to next page) Alignment p. 229 Flush left (not justified--right margin should be uneven) Typeface p. 228 12-pt Times New Roman; Always! Paragraphs and Indentations p. 87; 229 • Indent the first line of every paragraph 5-7 spaces (1/2 inch) • Space twice after periods in the body of the paper • Space once after periods on the reference list Title Page Format p. 229 Example: p. 41 Exception: You do NOT need to include an Author Note The title page should include the following items: • Running head: XXX Flush left (at 1” margin), aligns with page number on flush right (1” from right margin). Running head: XXX is used only on title page; starting on page 2 to end of paper, use only running header name in all caps, flush with left margin . Align with page numbers flush with right margin. Running head: RUNNING HEADER NAME (Example): Running head: LEADERSHIP ASSESSMENT Choose 2-3 words from title of paper for running header name Running head and running header name have a maximum of 50 characters including letters, spaces and punctuation; count. Note: Running header name (LEADERSHIP ASSESSMENT) is in all caps Page Numbering begins on Page 1, the title page • Page number flush right--title page is page 1 • CONSULT link below for You Tube Video with specific step-by-step instructions for setting up 5003 (Pathophysiology) AGNP AANP TIPS Action of thiazide diuretics Ocular movement 3,4,6 Definition of sensitivity Erectile disfunction- paxil Tx for anthrax-cipro Cd4<200=aids Webber and rinne test Polymyalgia rheumatica Initial evaluation of pt with acute prostatitis- urine and culture Temperal arteritis Labs for thalassemia and sickle cell- hemoglobin electrophoresis Rainbow flashing lights Av nicking Know your HTN meds Know your anemias 3 questions on murmurs psoriasis serum ferritin level • _Physiology and pathophysiology across the life span • _Geriatric • _Adult • _Pediatric • _Genetics/Genomics • _Normal Physiology vs. Pathologic Changes in Common Health Alterations • _Cellular response • _Physiologic and Psychological Response to Illness • _Etiology, Pathogenesis, and Clinical Manifestations of Common Alterations in Health • _Integumentary • _Neurologic • _Cardiovascular • _Respiratory • _Immunologic/Infectious • _Gastrointestinal • _Genitourinary • _Psychiatric • _Musculoskeletal • _Endocrine • _Hematological • _Reproductive • _Cancer Practice exam 1. Once a practice problem has been identified the next step would be to use the PICOT format to ask a question about the problem. PICOT stands for: P—population, I—intervention, C—comparisons, O—outcome, T—time. 2. The Affordable Care Act has directed the US Department of Health and Human Services and multiple agencies to develop and disseminate initiatives on meeting the care needs of patients with Multiple Chronic Conditions (MCC). What is the primary purpose for the national direction? To protect against high out-of-pocket costs by prohibiting insurers from denying coverage based on pre-existing conditions. 3. After thoroughly researching the topic of interest, what is the next step an APN should ask in selecting a theory/model for use in practice or research? Have several different theories/models been examined? 4. Which three roles represent the accepted advanced practice nursing roles? Certified Nurse Midwives (CNM) Clinical Nurse Specialist (CNS) Certified Registered Nurse Anesthetists (CRNAs) 5. What are the three major categories of Nola Pender’s Health promotion model? Behavior-specific cognitions and affect Characteristics and experiences Behavioral outcomes 6. Which theorist/s identifies carative factors as a value system, faith-hope and sensitivity to self and others? This describes which of the following theories? Jean Watson theory of human caring 7. Which set of components is essential in a scientific theory? Interrelated concepts, definitions, and propositions 8. The term advanced nursing practice (APN) includes nurses who are: Certified APRNs with a minimum of a master’s degree 9. To meet Medicare’s coverage requirements, the Nurse Practitioner’s services must be: Provided subject to state restrictions and supervision requirements 10. A 20-year-old female comes to the primary care clinic with clinical findings consistent with acute bronchitis. She is sexually active with a male partner, although she states prior to this relationship she did have two sexual partners. Her menses occurs every 28 days and is regular. An example of a primary prevention activity for this patient is: Counseling about safer sexual practices 11. Which agency’s initiative establishes national health promotion and prevention efforts and establishes benchmarks for monitoring the progress of health among Americans over a 10-year timeframe? Centers for Disease Control and Prevention (CDC) 12. Development of the first pediatric nurse practitioner program at the University of Colorado in 1965 is credited to which two individuals? Henry Silver, MD Loretta Ford, MD 13. Raynaud phenomenon is classified as a type III hypersensitivity reaction and is due to: Immune complexes that are deposited in capillary beds, blocking circulation 14. The nurse practitioner is caring for a 21-year-old female who presents with a pruritic, erythematous rash matching pattern of her sandal straps. The nurse practitioner advises the patient to avoid scratching the area due to the risk of developing a secondary infection. The NP understands that the most likely etiology of secondary skins infections is caused by which organism? Staphylococcus aureus 15. How can the APN best influence development and passage of a specific health policy agenda? Determine the best fit between legislative agenda, supporting organizations, and health policy issue. 16. Which is the gold standard research design for generating evidence? Randomized Control Trial 17. The APN is examining a client with new onset HTN. The NP recognizes that HTN may result in significant complications associated with which of the following three organs: Kidneys, Eyes, Brain 18. Which organization allows the use of the “BC” credential? American Nurses Credentialing Center (ANCC) 19. Which agency houses the US Protective and Safety Task Force (USPSTF)? Agency for Health, Research and Quality 20. Which 2 organizations administer nurse practitioner certification programs? American Association of Nurse Practitioners (AANP) American Nurses Credentialing Center (ANCC) 21. Transformational leadership is best defined as: A style that is relational, driven by a common goal, and satisfies the leader and the follower 22. A metaparadigm must include which of the following 3 characteristics? Encompass all phenomena of interest Be perspective—neutral Be global in scope 23. Which statement best reflects King’s theory? If nurses with special knowledge and skills communicate appropriate information to clients, mutual goal-setting and goal attainment will occur 24. Which agency will the APN reference when seeking the current evidence based guidelines directing standards of care? Agency for Health Research and Quality 25. A 43-year old woman has a 12-hour history of sudden onset of right upper quadrant abdominal pain with radiation to the shoulder, fever, and chills. She has had similar, milder episodes in the past. Examination reveals marked tenderness to right upper quadrant abdominal palpation. Her most likely diagnosis is: Acute cholecystitis 26. What theory is used to describe the cause of endometriosis? Endometrial tissue passes through the fallopian tubes and into the peritoneal cavity and remains responsive to hormones. 27. Chronic pain, physical disability, social support, age and gender are related to perceived daily stress, which is related to depression. This is an example of which type of theory? Explanatory 28. The leadership core competency of advanced practice nursing includes which three characteristics? Mentoring, Innovation, Activism 29. What initiative specifically focuses on the aging American, under the Affordable Care Act? Multiple Chronic Conditions 30. Which of the following philosophies of work view would characterize human beings as holistic; parts are viewed only in the context of the whole? Reciprocal Interaction 31. A difficult aspect of determining occupational exposure to disease is the: Long latency period between exposure and disease reporting 32. A novice nurse practitioner is experiencing feeling of inferiority toward more experienced clinicians in the practice. She has identified that time constraints for visits and expectations to increase productivity limits her ability to address these non- adherent issues during client visits. Which barrier to ethical practice is influencing practice? Organizational/Environmental 33. Utilizing Johnson’s Behavioral systems model (JBSM), the APN discovers that a patient is not sure who he can depend on because his wife is emotionally distant. This data would be characteristic of which subsystem of the JBSM. Dependency subsystem 34. A purposeful, complex, dynamic, collaborative, and holistic interpersonal process aimed at supporting and facilitating patients and families through health-related experiences and transitions to achieve health-related goals (mutually determined when possible)” defines which APN role? Coach 35. A 60 year old female with a history of emphysema presents to the primary care office with complaints of cough and shortness of breath at rest. During the physical exam, the nurse practitioner recognizes clubbing, barrel chest, and prolonged expiration. The nurse practitioner understands that the patient is exhibiting symptoms resulting from which type of pulmonary disease process? Obstructive 36. Which of the following statements accurately defines Hamric’s conceptual definition of advanced practice nursing? The patient-focused application of an expanded range of competencies to improve health outcomes for patients and populations within a specialized clinical area of the larger discipline of nursing. 37. When caring for a client who presents with pain and swelling to location of the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints. Which diagnostic test is most specific to diagnosis of rheumatoid arthritis? Elevated rheumatoid factor level 38. The Consensus Model for Advanced Practice Registered Nurse Regulations addresses which four areas? Specialty areas Roles and titles to be used Population foci Preparation for emerging APRN roles 39. Which statement best supports primary prevention of burns for geriatric clients? “Avoid smoking in bed” 40. Which of the following three complications are associated with chronic hepatitis B? Continued infectivity Uncompensated cirrhosis Hepatocellular carcinoma 41. The central competency, direct clinical practice, is characterized by which three of the following? Expert clinical performance Formation of a therapeutic partnership with patients Holistic approach 42. Which payment system seeks Medicare reimbursement under the MACRA legislation for providing high quality patient-specific care and improved outcomes? Merit Incentive Based Payment 43. What four components of advanced practice nursing (APN) are specified by the National Council for State Boards of Nursing Consensus Model for APRN regulation? Licensure, Accreditation, Education, Certification 44. Which learning theory would be most applicable as a guide for the development of a program to help families of patients in palliative care? Humanistic Learning Theory 45. What terms indicate appropriate progression associated with the history and evolution of advance practice nursing? Specialist, Expanded Role, Advanced Practice 46. An experienced NP, has two separate but equally important ethical obligations that he is unfortunately unable to carry out. This is an example of which barrier to ethical practice? Moral Dilemma 47. Pre-invasive epithelial tumors of glandular or squamous cell origin describes which of the following? Cancer in situ 48. Which two options are barriers to the conceptualization of Advanced Practice Nursing? Interprofessional education and practice Need to differentiate between advanced practice nursing and medicine 49. The Dreyfus Model of Skill Acquisition includes which four stages of APN performance? Expert, Advanced Beginner, Competent, Proficient 50. The nurse practitioner is caring for a client who has undergone a recent gastrectomy who complains of fatigue, palpitations, shortness of breath, and numbness and tingling to their fingers on both hands. The nurse suspects pernicious anemia related to: Deficiency of intrinsic factor production 51. The analysis of a theory or conceptual model includes examining the origins. Which would not be considered an aspect of origin of the theory/model? The unique focus 52. The clinical manifestations of dyskinetic cerebral palsy include: Jerky uncontrolled and abrupt fine musculoskeletal movements 53. Which core competency incorporates assuming complex collaborative roles with stakeholders and communities? Leadership 54. A critical environmental element that affects the authority of advanced practice nurses to practice to their fullest/maximum scope, according to Hamric’s model, is: Health policy 55. For nursing to considered a discipline, which statement is true? Context has considerable influence on the development of the knowledge base. 56. The APN wants to develop a community educational program for hypertension and stroke prevention. She recognizes that the individual’s lifestyle and pattern of behavior need to be addressed for the program to be successful. Which theory would be most appropriate to guide the program development? Health as Expanding consciousness 57. When considering a theory for use in guiding practice, the APN should examine the Conceptual-Theoretical-Empirical (C-T-E) linkages by for which criteria? Specification adequacy 58. In septic shock, which mediators are anti-inflammatory? Interleukin (IL-4, IL-10, IL13) 59. The link between major depression and cortisol secretion is that individuals with depression: Show that persistently elevated plasma cortisol levels can result in inflammation that is believed to trigger depression. 60. Which three primary criteria for advanced practice nursing are identified in Hamric’s Integrative Model of Advanced Practice Nursing? Guidance, Graduate education, Patient-focused practice, Certification 61. Which advance practice nursing was developed to facilitate delivery of high quality, patient-centered primary care? Certified nurse practitioner (CNP) 62. An adult-gerontology nurse practitioner is employed in a rural practice that is initiating a school-based primary healthcare program. All nurse practitioners in the practice are required to initiate preparations to facilitate conducting patient visits in the new setting. Which role concepts best describes what the adult-gerontology nurse practitioner is experiencing? Role incongruity 63. A MSN student is noting challenges related to attending school while attempting to balance other work, family, and social responsibilities. Which of the following role concepts illustrates the MSN student’s experience? Role stress 64. A 24 year old female presents to the primary care office with complaints of dysuria. Urinalysis lab results indicated positive nitrites. The nurse practitioner plans to initiate antibiotic coverage for the most likely causative organism which is: Escherichia coli 65. Place the following four steps of APN core competency of evidence based practice in order. a. Critically appraise and extract evidence b. Formulate a measurable clinical question c. Review literature for relevant studies d. Implement useful findings in clinical decision making 66. A 12 year old male is diagnosed with Klinefelter syndrome. His karyotype would reveal which of the following? XXY 67. Concerning the MMR vaccine, which of the following is a correct statement? There is no scientific evidence to support MMR use increases autism risk 68. You are seeing a 40 year old patient who has started varenicline (Chantix) 3 weeks ago as a tool for smoking cessation. What is the most important question to ask during the visit? Have you noticed change in your mood? 69. A primary care nurse practitioner (NP) is seeking additional support from ancillary health services for a diabetic client who is noncompliant with nutrition, exercise, and medication. Which barrier to ethical practice is influencing the NP’s practice? Patient-provider 70. Which hospital ownership classification best describes an organization whose excess income is distributed to its shareholders? For profit 71. How has the Quality Chasm Report been used to direct US health care? As a framework for safe, effective, efficient, equitable, timely, and patient centered care. 72. A 12 year old female is newly diagnosed with type 1 DM. When the parents ask what causes this, what is the nurse practitioner’s best response? Immune destruction of the pancreas 73. Which patient below is at most risk for invasive pneumococcal infection? A 32 year old woman who underwent a splenectomy after a motor vehicle accident 74. A Latino patient in your clinic has been perpetually late for his appointment. Which action by the nurse practitioner would be most appropriate? Assess how the patient interprets the appointment time 75. What specific developments have primarily occurred because of the Affordable Care Act (ACA)? Development of patient centered outcomes, use of comparative effectiveness research, quality payment structures that impact APN reimbursement 76. Hamric’s Integrative Model of Advanced Practice Nursing identify the central competency of advance practice nursing that directs the other six core competencies. Direct Clinical Practice 77. A public health nurse is teaching the community about health promotion. When explaining immunity, the APN discusses that innate immunity is: Present at birth 78. According to Madeline Leininger, cultural care/accommodation/negotiation refers to actions/decisions that help a particular culture: Adapt to or negotiate with others for satisfying healthcare outcomes 79. The nurse practitioner is conducting annual physical exam on a 62 year old male. Which of the following risk factors will prompt the nurse practitioner to screen the patient for development of benign prostatic hypertrophy (BPH)? Increased age 80. The family nurse practitioner examines a patient who has sustained a non-work-related injury that interferes with his ability to perform his job. The patient does not qualify for medical disability and has a reasonable chance of engaging in a suitable occupation with proper therapy. What type of services or benefits should the nurse practitioner recommend? Vocational rehabilitation services [Show More]
Last updated: 1 year ago
Preview 1 out of 64 pages

Reviews( 0 )
Recommended For You
*NURSING> STUDY GUIDE > NURSUNG NSG 6430 Women_s health exam study guide | South University, Savannah | ALL CORRECT. (All)
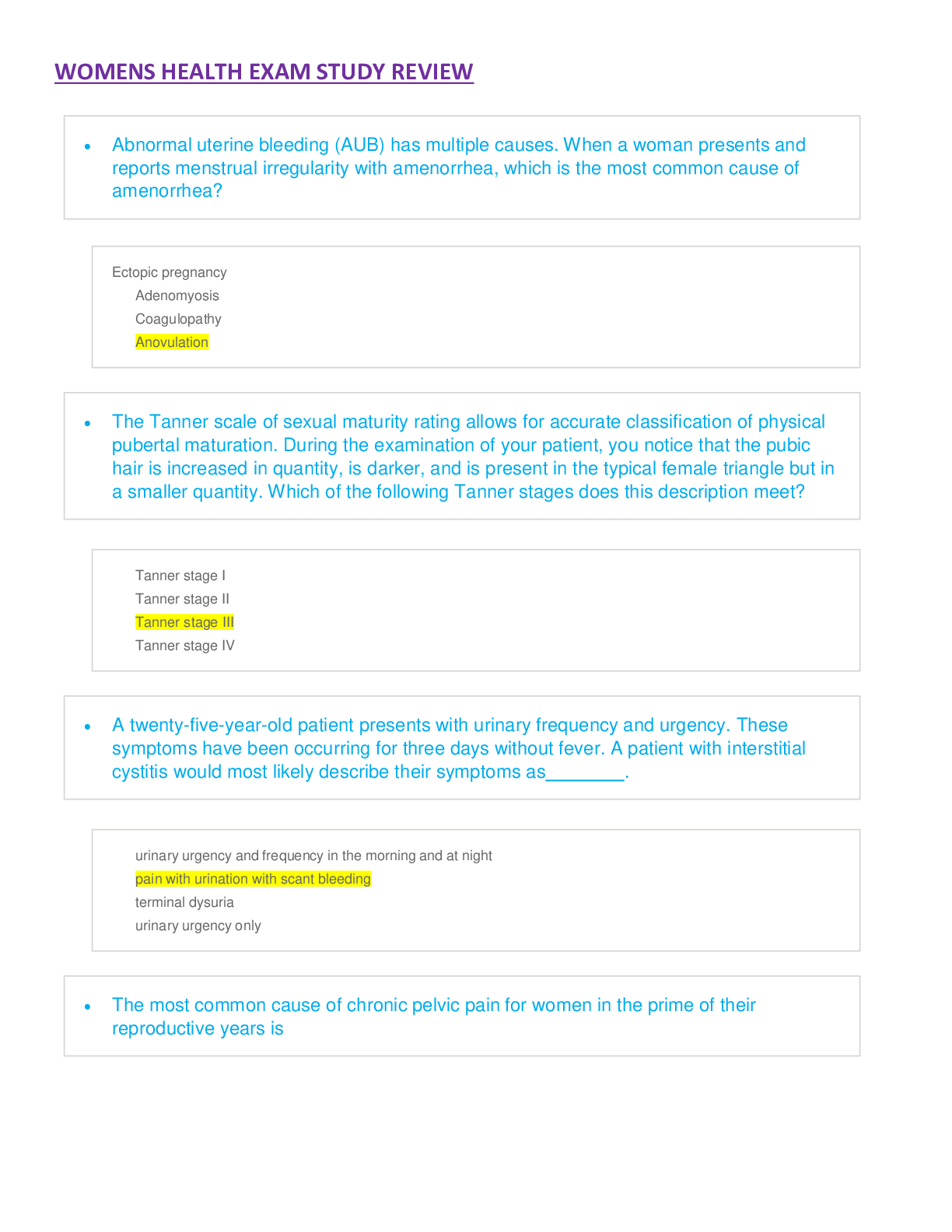
NURSUNG NSG 6430 Women_s health exam study guide | South University, Savannah | ALL CORRECT.
NURSUNG NSG 6430 Women_s health exam study guide NURSUNG NSG 6430 Women_s health exam study guide | South University, Savannah | ALL CORRECT.
By A+ Solutions , Uploaded: Oct 27, 2021
$14
*NURSING> STUDY GUIDE > NSG6006 Study Guide, State Nurse Practice Act (Payne, Kelly) (All)

NSG6006 Study Guide, State Nurse Practice Act (Payne, Kelly)
NSG6006 Study Guide, State Nurse Practice Act (Payne, Kelly) State Nurse Practice Act NSG6006 Study Guide 5000 (Roles) • _History and Developmental Aspects of Advanced Practice Nursing • D...
By VERIFIED A+ , Uploaded: Sep 23, 2021
$15
*NURSING> STUDY GUIDE > NSG6006 Study Guide (Payne, Kelly) | Policies & Practice Standards • State Nurse Practice Act (5000 roles) | South University (All)

NSG6006 Study Guide (Payne, Kelly) | Policies & Practice Standards • State Nurse Practice Act (5000 roles) | South University
Policies & Practice Standards • State Nurse Practice Act NSG6006 Study Guide 5000 (Roles) • _History and Developmental Aspects of Advanced Practice Nursing • Definition of advanced practice nurse (...
By A+ Solutions , Uploaded: May 24, 2021
$12.5
*NURSING> STUDY GUIDE > Policies & Practice Standards • State Nurse Practice Act NSG6006 Study Guide (All)

Policies & Practice Standards • State Nurse Practice Act NSG6006 Study Guide
Policies & Practice Standards • State Nurse Practice Act NSG6006 Study Guide
By Perfectstudy , Uploaded: Nov 02, 2022
$20
*NURSING> STUDY GUIDE > ATI Med-Surg Proctored Exam already Graded A. (All)
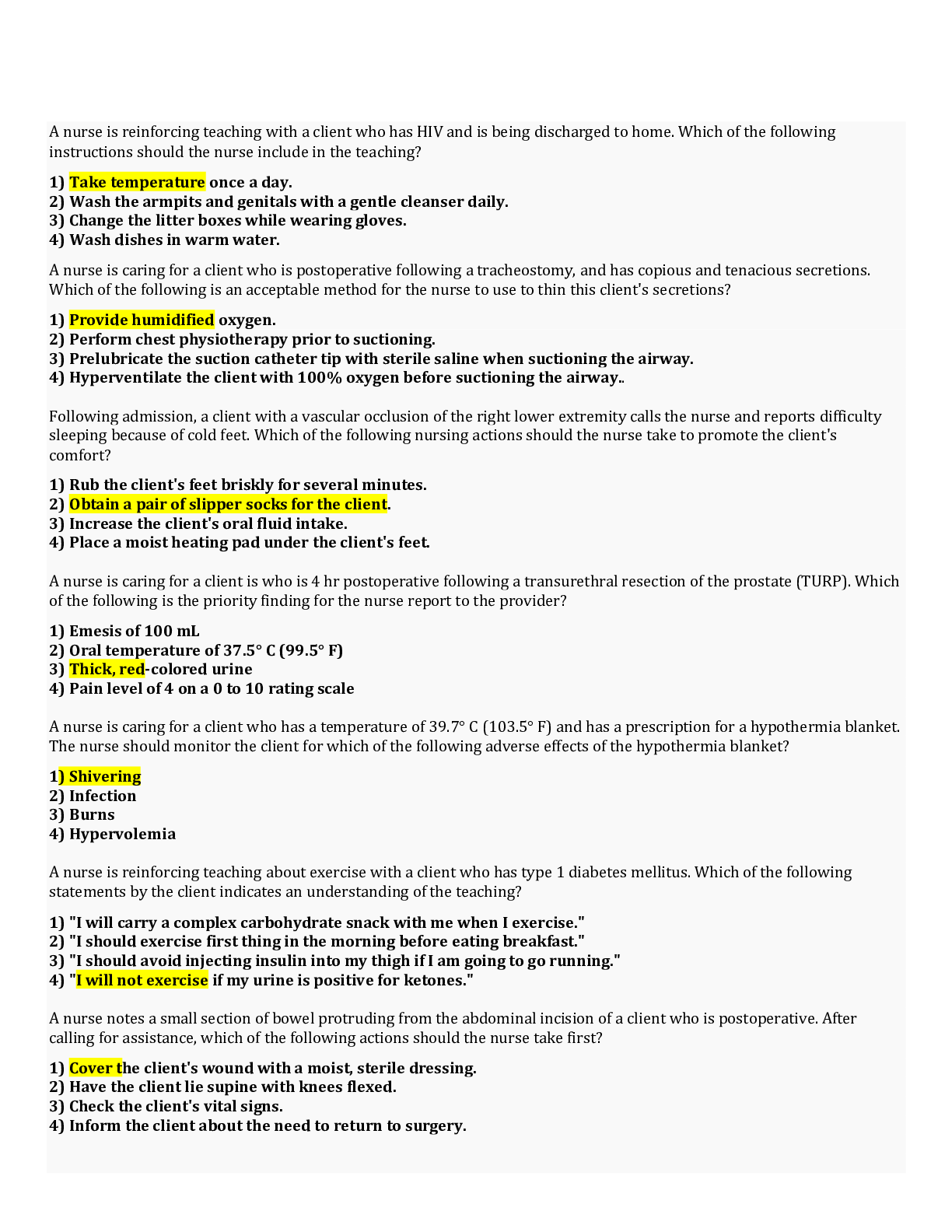
ATI Med-Surg Proctored Exam already Graded A.
A nurse is reinforcing teaching with a client who has HIV and is being discharged to home. Which of the following instructions should the nurse include in the teaching? 1) Take temperature once a da...
By Academia1434 , Uploaded: Jan 15, 2021
$13
*NURSING> STUDY GUIDE > NUR 254 Exam 2 Study Guide (100% Accurate ). (All)
NUR 254 Exam 2 Study Guide (100% Accurate ).
NUR 254 (NUR254 EXAM2 STUDY GUIDE)/NUR 254 - Exam 2 Study Guide (100% Accurate ).
By Solution101 , Uploaded: Mar 11, 2021
$12
*NURSING> STUDY GUIDE > NR 533 Financial Management In Healthcare Organizations, Week 5 Assignment Break-Even Analysis (All)
NR 533 Financial Management In Healthcare Organizations, Week 5 Assignment Break-Even Analysis
NR 533 Financial Management In Healthcare Organizations, NR 533 Week 5 Assignment Break-Even Analysis
By TopScholar , Uploaded: Mar 15, 2021
$8
*NURSING> STUDY GUIDE > NR 511Midterm Exam Study Guide Chamberlain College of Nursing - (All)
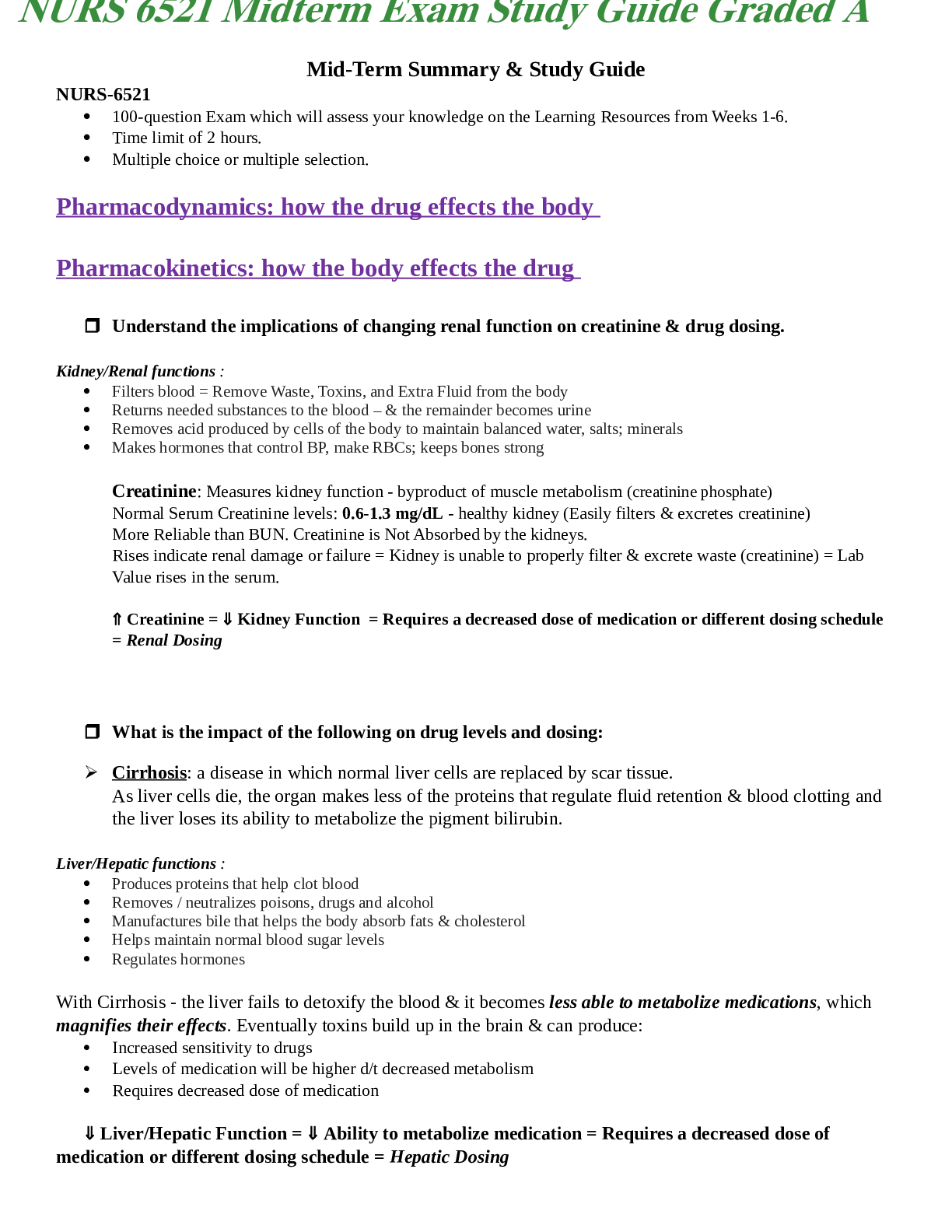
NR 511Midterm Exam Study Guide Chamberlain College of Nursing -
NR511 Midterm Exam Study Guide Week 1 1. Define diagnostic reasoning: type of critical thinking Critical thinking involves the process of questioning one’s thinking to determine if all possible...
By Muchiri , Uploaded: Mar 12, 2021
$11
Finance> STUDY GUIDE > FINANCE 238 Oxford College of Commerce, Lahore - rev test. (All)
FINANCE 238 Oxford College of Commerce, Lahore - rev test.
I recently visited Kennedy's Orbiter Processing Facility to find out how a highly skilled team of shuttle technicians spent the past few months preparing Endeavour for STS-126. (upbeat music) I'm...
By Muchiri , Uploaded: Mar 17, 2021
$7
*NURSING> STUDY GUIDE > NR 222 / NR222 Health and Wellness Exam 1 Review Study Guide Chamberlain College (All)
NR 222 / NR222 Health and Wellness Exam 1 Review Study Guide Chamberlain College
1. Nursing - the protection, promotion, and optimization of health and abilities; - prevention of illness and injury; - alleviation of suffering through the diagnosis and treatment of human resp...
By nurse_steph , Uploaded: Nov 14, 2020
$13
Document information
Connected school, study & course
About the document
Uploaded On
Apr 13, 2021
Number of pages
64
Written in
Additional information
This document has been written for:
Uploaded
Apr 13, 2021
Downloads
0
Views
39






