*NURSING > TEST BANK > Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edi (All)
Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition
Document Content and Description Below
Chapter 01: Mental Health and Mental Illness Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. A staff nurse complet... es orientation to a psychiatric unit. This nurse may expect an advanced practice nurse to perform which additional intervention? a. Conduct mental health assessments. b. Prescribe psychotropic medication. c. Establish therapeutic relationships. d. Individualize nursing care plans. ANS: B In most states, prescriptive privileges are granted to master’s-prepared nurse practitioners and clinical nurse specialists who have taken special courses on prescribing medication. The nurse prepared at the basic level is permitted to perform mental health assessments, establish relationships, and provide individualized care planning. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-23 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 2. A nursing student expresses concerns that mental health nurses “lose all their clinical nursing skills.” Select the best response by the mental health nurse. a. “Psychiatric nurses practice in safer environments than other specialties. Nurse-to-patient ratios must be better because of the nature of the patients’ problems.” b. “Psychiatric nurses use complex communication skills as well as critical thinking to solve multidimensional problems. I am challenged by those situations.” c. “That’s a misconception. Psychiatric nurses frequently use high technology monitoring equipment and manage complex intravenous therapies.” d. “Psychiatric nurses do not have to deal with as much pain and suffering as medical–surgical nurses do. That appeals to me.” ANS: B The practice of psychiatric nursing requires a different set of skills than medical–surgical nursing, though there is substantial overlap. Psychiatric nurses must be able to help patients with medical as well as mental health problems, reflecting the holistic perspective these nurses must have. Nurse–patient ratios and workloads in psychiatric settings have increased, just like other specialties. Psychiatric nursing involves clinical practice, not just documentation. Psychosocial pain and suffering are as real as physical pain and suffering. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-2, 21 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 3. When a new bill introduced in Congress reduces funding for care of persons diagnosed with mental illness, a group of nurses write letters to their elected representatives in opposition to the legislation. Which role have the nurses fulfilled? a. Recovery b. Attending c. Advocacy d. Evidence-based practice ANS: C An advocate defends or asserts another’s cause, particularly when the other person lacks the ability to do that for self. Examples of individual advocacy include helping patients understand their rights or make decisions. On a community scale, advocacy includes political activity, public speaking, and publication in the interest of improving the human condition. Since funding is necessary to deliver quality programming for persons with mental illness, the letter-writing campaign advocates for that cause on behalf of patients who are unable to articulate their own needs. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-26 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 4. A family has a long history of conflicted relationships among the members. Which family member’s comment best reflects a mentally healthy perspective? a. “I’ve made mistakes but everyone else in this family has also.” b. “I remember joy and mutual respect from our early years together.” c. “I will make some changes in my behavior for the good of the family.” d. “It’s best for me to move away from my family. Things will never change.” ANS: C The correct response demonstrates the best evidence of a healthy recognition of the importance of relationships. Mental health includes rational thinking, communication skills, learning, emotional growth, resilience, and self-esteem. Recalling joy from earlier in life may be healthy, but the correct response shows a higher level of mental health. The other incorrect responses show blaming and avoidance. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 1-2, 3, 32 (Figure 1-1) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment 5. Which assessment finding most clearly indicates that a patient may be experiencing a mental illness? The patient a. reports occasional sleeplessness and anxiety. b. reports a consistently sad, discouraged, and hopeless mood. c. is able to describe the difference between “as if” and “for real.” d. perceives difficulty making a decision about whether to change jobs. ANS: B The correct response describes a mood alteration, which reflects mental illness. The distracters describe behaviors that are mentally healthy or within the usual scope of human experience. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-2 to 4 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 6. Which finding best indicates that the goal “Demonstrate mentally healthy behavior” was achieved for an adult patient? The patient a. sees self as capable of achieving ideals and meeting demands. b. behaves without considering the consequences of personal actions. c. aggressively meets own needs without considering the rights of others. d. seeks help from others when assuming responsibility for major areas of own life. ANS: A The correct response describes an adaptive, healthy behavior. The distracters describe maladaptive behaviors. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-2 to 4 TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 7. A nurse encounters an unfamiliar psychiatric disorder on a new patient’s admission form. Which resource should the nurse consult to determine criteria used to establish this diagnosis? a. International Statistical Classification of Diseases and Related Health Problems (ICD-10) b. The ANA’s Psychiatric-Mental Health Nursing Scope and Standards of Practice c. Diagnostic and Statistical Manual of Mental Disorders (DSM-V) d. A behavioral health reference manual ANS: C The DSM-V gives the criteria used to diagnose each mental disorder. It is the official guideline for diagnosing psychiatric disorders. The distracters may not contain diagnostic criteria for a psychiatric illness. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-18, 19 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 8. A nurse wants to find a description of diagnostic criteria for anxiety disorders. Which resource would have the most complete information? a. Nursing Outcomes Classification (NOC) b. DSM-V c. The ANA’s Psychiatric-Mental Health Nursing Scope and Standards of Practice d. ICD-10 ANS: B The DSM-V details the diagnostic criteria for psychiatric clinical conditions. It is the official guideline for diagnosing psychiatric disorders. The other references are good resources but do not define the diagnostic criteria. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 1-18, 19 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 9. Which individual is demonstrating the highest level of resilience? One who a. is able to repress stressors. b. becomes depressed after the death of a spouse. c. lives in a shelter for 2 years after the home is destroyed by fire. d. takes a temporary job to maintain financial stability after loss of a permanent job. ANS: D Resilience is closely associated with the process of adapting and helps people facing tragedies, loss, trauma, and severe stress. It is the ability and capacity for people to secure the resources they need to support their well-being. Repression and depression are unhealthy. Living in a shelter for 2 years shows a failure to move forward after a tragedy. See related audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-5, 6 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 10. Complete this analogy. NANDA: clinical judgment: NIC: a. patient outcomes. b. nursing actions. c. diagnosis. d. symptoms. ANS: B Analogies show parallel relationships. NANDA, the North American Nursing Diagnosis Association, identifies diagnostic statements regarding human responses to actual or potential health problems. These statements represent clinical judgments. NIC (Nursing Interventions Classification) identifies actions provided by nurses that enhance patient outcomes. Nursing care activities may be direct or indirect. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 1-21, 22 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 11. An adult says, “Most of the time I’m happy and feel good about myself. I have learned that what I get out of something is proportional to the effort I put into it.” Which number on this mental health continuum should the nurse select? Mental Illness 1 2 Mental Health 3 4 5 a. 1 b. 2 c. 3 d. 4 e. 5 ANS: E The adult is generally happy and has an adequate self-concept. The statement indicates the adult is reality-oriented, works effectively, and has control over own behavior. Mental health does not mean that a person is always happy. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-2, 3, 32 (Figure 1-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 12. Which disorder is an example of a culture-bound syndrome? a. Epilepsy b. Schizophrenia c. Running amok d. Major depressive disorder ANS: C Culture-bound syndromes occur in specific sociocultural contexts and are easily recognized by people in those cultures. A syndrome recognized in parts of Southeast Asia is running amok, in which a person (usually a male) runs around engaging in furious, almost indiscriminate violent behavior. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-7 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 13. The DSM-V classifies: a. deviant behaviors. b. present disability or distress. c. people with mental disorders. d. mental disorders people have. ANS: D The DSM-V classifies disorders people have rather than people themselves. The terminology of the tool reflects this distinction by referring to individuals with a disorder rather than as a “schizophrenic” or “alcoholic,” for example. Deviant behavior is not generally considered a mental disorder. Present disability or distress is only one aspect of the diagnosis. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 1-18, 19 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 14. A citizen at a community health fair asks the nurse, “What is the most prevalent mental disorder in the United States?” Select the nurse’s correct response. a. Schizophrenia b. Bipolar disorder c. Dissociative fugue d. Alzheimer’s disease ANS: D The 12-month prevalence for Alzheimer’s disease is 10% for persons older than 65% and 50% for persons older than 85. The prevalence of schizophrenia is 1.1% per year. The prevalence of bipolar disorder is 2.6%. Dissociative fugue is a rare disorder. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-33 (Table 1-1) TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 15. In the majority culture of the United States, which individual has the greatest risk to be labeled mentally ill? One who a. describes hearing God’s voice speaking. b. is usually pessimistic but strives to meet personal goals. c. is wealthy and gives away $20 bills to needy individuals. d. always has an optimistic viewpoint about life and having own needs met. ANS: A The question asks about risk. Hearing voices is generally associated with mental illness, but in charismatic religious groups, hearing the voice of God or a prophet is a desirable event. Cultural norms vary, which makes it more difficult to make an accurate diagnosis. The individuals described in the other options are less likely to be labeled mentally ill. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 1-3, 4 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 16. A patient’s relationships are intense and unstable. The patient initially idealizes the significant other and then devalues him or her, resulting in frequent feelings of emptiness. This patient will benefit from interventions to develop which aspect of mental health? a. Effectiveness in work b. Communication skills c. Productive activities d. Fulfilling relationships ANS: D The information given centers on relationships with others that are described as intense and unstable. The relationships of mentally healthy individuals are stable, satisfying, and socially integrated. Data are not present to describe work effectiveness, communication skills, or activities. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-32 (Figure 1-1) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Planning 17. Which belief will best support a nurse’s efforts to provide patient advocacy during a multidisciplinary patient care planning session? a. All mental illnesses are culturally determined. b. Schizophrenia and bipolar disorder are cross-cultural disorders. c. Symptoms of mental disorders are unchanged from culture to culture. d. Assessment findings in mental illness reflect a person’s cultural patterns. ANS: D Symptoms must be understood in terms of a person’s cultural background. A nurse who understands that a patient’s symptoms are influenced by culture will be able to advocate for the patient to a greater degree than a nurse who believes that culture is of little relevance. The distracters are untrue statements. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-27 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 18. A nurse is part of a multidisciplinary team working with groups of depressed patients. One group of patients receives supportive interventions and antidepressant medication. The other group receives only medication. The team measures outcomes for each group. Which type of study is evident? a. Incidence b. Prevalence c. Comorbidity d. Clinical epidemiology ANS: D Clinical epidemiology is a broad field that addresses studies of the natural history (or what happens if there is no treatment and the problem is left to run its course) of an illness, studies of diagnostic screening tests, and observational and experimental studies of interventions used to treat people with the illness or symptoms. Prevalence refers to numbers of new cases. Comorbidity refers to having more than one mental disorder at a time. Incidence refers to the number of new cases of mental disorders in a healthy population within a given period. See related audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-17 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 19. The spouse of a patient diagnosed with schizophrenia says, “I don’t understand how events from childhood have anything to do with this disabling illness.” Which response by the nurse will best help the spouse understand the cause of this disorder? a. “Psychological stress is the basis of most mental disorders.” b. “This illness results from developmental factors rather than stress.” c. “Research shows that this condition more likely has a biological basis.” d. “It must be frustrating for you that your spouse is sick so much of the time.” ANS: C Many of the most prevalent and disabling mental disorders have strong biological influences. Genetics are only one part of biological factors. Empathy does not address increasing the spouse’s level of knowledge about the cause of the disorder. The other distracters are not established facts. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-5, 6 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 20. A category 5 tornado occurred in a community of 400 people. Many homes and businesses were destroyed. In the 2 years following the disaster, 140 individuals were diagnosed with posttraumatic stress disorder (PTSD). Which term best applies to these newly diagnosed cases? a. Prevalence b. Comorbidity c. Incidence d. Parity ANS: C Incidence refers to the number of new cases of mental disorders in a healthy population within a given period of time. Prevalence describes the total number of cases, new and existing, in a given population during a specific period of time, regardless of when they became ill. Parity refers to equivalence, and legislation required insurers that provide mental health coverage to offer annual and lifetime benefits at the same level provided for medical–surgical coverage. Comorbidity refers to having more than one mental disorder at a time. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-16 TOP: Nursing Process: Planning/Outcomes Identification MSC: Client Needs: Safe, Effective Care Environment 21. Which component of treatment of mental illness is specifically recognized by Quality and Safety Education for Nurses (QSEN)? a. All genomes are unique. b. Care is centered on the patient. c. Healthy development is vital to mental health. d. Recovery occurs on a continuum from illness to health. ANS: B The key areas of care promoted by QSEN are patient-centered care, teamwork and collaboration, evidence-based practice, quality improvement, safety, and informatics. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 1-14 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 22. Select the best response for the nurse to a question from another health professional regarding the difference between a diagnosis in DSM-V and a nursing diagnosis. a. “There is no functional difference between the two. Both identify human disorders.” b. “The DSM-V diagnosis disregards culture, whereas the nursing diagnosis takes culture into account.” c. “The DSM-V diagnosis describes causes of disorders whereas a nursing diagnosis does not explore etiology.” d. “The DSM-V diagnosis guides medical treatment, whereas the nursing diagnosis offers a framework for identifying interventions for issues a patient is experiencing.” ANS: D The medical diagnosis is concerned with the patient’s disease state, causes, and cures, whereas the nursing diagnosis focuses on the patient’s response to stress and possible caring interventions. Both tools consider culture. The DSM-V is multiaxial. Nursing diagnoses also consider potential problems. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 1-21 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 23. Which nursing intervention below is part of the scope of an advanced practice psychiatric/mental health nurse rather than a basic level registered nurse? a. Coordination of care b. Health teaching c. Milieu therapy d. Psychotherapy ANS: D Psychotherapy is part of the scope of practice of an advanced practice nurse. The distracters are within a basic level registered nurse’s scope of practice. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 1-23, 35 (Table 1-2) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment MULTIPLE RESPONSE 1. An experienced nurse says to a new graduate, “When you’ve practiced as long as I have, you automatically know how to take care of patients experiencing psychosis.” Which factors should the new graduate consider when analyzing this comment? (Select all that apply.) a. The experienced nurse may have lost sight of patients’ individuality, which may compromise the integrity of practice. b. New research findings should be integrated continuously into a nurse’s practice to provide the most effective care. c. Experience provides mental health nurses with the essential tools and skills needed for effective professional practice. d. Experienced psychiatric nurses have learned the best ways to care for mentally ill patients through trial and error. e. An intuitive sense of patients’ needs guides effective psychiatric nurses. ANS: A, B Evidence-based practice involves using research findings and standards of care to provide the most effective nursing care. Evidence is continuously emerging, so nurses cannot rely solely on experience. The effective nurse also maintains respect for each patient as an individual. Overgeneralization compromises that perspective. Intuition and trial and error are unsystematic approaches to care. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 1-14 TOP: Nursing Process: Diagnosis/Analysis MSC: Client Needs: Safe, Effective Care Environment 2. Which findings are signs of a person who is mentally healthy? (Select all that apply.) a. Says, “I have some weaknesses, but I feel I’m important to my family and friends.” b. Adheres strictly to religious beliefs of parents and family of origin. c. Spends all holidays alone watching old movies on television. d. Considers past experiences when deciding about the future. e. Experiences feelings of conflict related to changing jobs. ANS: A, D, E Mental health is a state of well-being in which each individual is able to realize his or her own potential, cope with the normal stresses of life, work productively, and make a contribution to the community. Mental health provides people with the capacity for rational thinking, communication skills, learning, emotional growth, resilience, and self-esteem. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-2, 3, 32 (Figure 1-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 3. A patient in the emergency department says, “Voices say someone is stalking me. They want to kill me because I developed a cure for cancer. I have a knife and will stab anyone who is a threat.” Which aspects of the patient’s mental health have the greatest and most immediate concern to the nurse? (Select all that apply.) a. Happiness b. Appraisal of reality c. Control over behavior d. Effectiveness in work e. Healthy self-concept ANS: B, C, E The aspects of mental health of greatest concern are the patient’s appraisal of and control over behavior. The appraisal of reality is inaccurate. There are auditory hallucinations, delusions of persecution, and delusions of grandeur. In addition, the patient’s control over behavior is tenuous, as evidenced by the plan to stab anyone who seems threatening. A healthy self-concept is lacking, as evidenced by the delusion of grandeur. Data are not present to suggest that the other aspects of mental health (happiness and effectiveness in work) are of immediate concern. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 1-3, 4 TOP: Nursing Process: Assessment Chapter 02: Theories and Therapies Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. A parent says, “My 2-year-old child refuses toilet training and shouts ‘No!’ when given directions. What do you think is wrong?” Select the nurse’s best reply. a. “Your child needs firmer control. It is important to set limits now.” b. “This is normal for your child’s age. The child is striving for independence.” c. “There may be developmental problems. Most children are toilet trained by age 2.” d. “Some undesirable attitudes are developing. A child psychologist can help you develop a plan.” ANS: B This behavior is conventional of a child around the age of 2 years, whose developmental task is to develop autonomy. The distracters indicate the child’s behavior is abnormal. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 2-52 (Table 2-6) TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 2. A nurse wants to find information on current evidence-based research, programs, and practices regarding mental illness and addictions. Which resource should the nurse consult? a. American Psychiatric Association b. American Psychological Association (APA) c. Clinician’s Quick Guide to Interpersonal Psychotherapy d. Substance Abuse and Mental Health Services Administration (SAMHSA) ANS: D The SAMHSA maintains a National Registry of Evidence-based Practices and Programs. New therapies are entered into the database on a regular basis. The incorrect responses are resources but do not focus on evidence-based information. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 2-32 TOP: Nursing Process: Planning MSC: Client Needs: Management of Care 3. A 26-month-old displays negative behavior, refuses toilet training, and often says, “No!” Which psychosocial crisis is evident? a. Trust versus mistrust b. Initiative versus guilt c. Industry versus inferiority d. Autonomy versus shame and doubt ANS: D The crisis of autonomy versus shame and doubt relates to the developmental task of gaining control of self and environment, as exemplified by toilet training. This psychosocial crisis occurs during the period of early childhood. Trust versus mistrust is the crisis of the infant. Initiative versus guilt is the crisis of the preschool and early-school-aged child. Industry versus inferiority is the crisis of the 6- to 12-year-old child. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 2-52 (Table 2-6) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 4. A 4-year-old grabs toys from other children and says, “I want that now!” From a psychoanalytic perspective, this behavior is a product of impulses originating in which system of the personality? a. Id b. Ego c. Superego d. Preconscious ANS: A The id operates on the pleasure principle, seeking immediate gratification of impulses. The ego acts as a mediator of behavior and weighs the consequences of the action, perhaps determining that taking the toy is not worth the mother’s wrath. The superego would oppose the impulsive behavior as “not nice.” The preconscious is a level of awareness rather than an aspect of personality. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-4, 5 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 5. The parent of a 4-year-old rewards and praises the child for helping a sibling, being polite, and using good manners. These qualities are likely to be internalized and become part of which system of the personality? a. Id b. Ego c. Superego d. Preconscious ANS: C The superego contains the “shoulds,” or moral standards internalized from interactions with significant others. Praise fosters internalization of desirable behaviors. The id is the center of basic instinctual drives, and the ego is the mediator. The ego is the problem-solving and reality-testing portion of the personality that negotiates solutions with the outside world. The preconscious is a level of awareness from which material can be retrieved easily with conscious effort. This item relates to an audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-4, 5 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 6. A nurse supports a parent for praising a child who behaves in helpful ways to others. When this child behaves with politeness and helpfulness in adulthood, which feeling will most likely result? a. Guilt b. Anxiety c. Humility d. Self-esteem ANS: D The individual will be living up to the ego ideal, which will result in positive feelings about self. The other options are incorrect because each represents a negative feeling. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-4, 5 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 7. An adult says, “I never know the answers,” and “My opinion does not count.” Which psychosocial crisis was unsuccessfully resolved for this adult? a. Initiative versus guilt b. Trust versus mistrust c. Autonomy versus shame and doubt d. Generativity versus self-absorption ANS: C These statements show severe self-doubt, indicating that the crisis of gaining control over the environment was not met successfully. Unsuccessful resolution of the crisis of initiative versus guilt results in feelings of guilt. Unsuccessful resolution of the crisis of trust versus mistrust results in poor interpersonal relationships and suspicion of others. Unsuccessful resolution of the crisis of generativity versus self-absorption results in self-absorption that limits the ability to grow as a person. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 2-52 (Table 2-6) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 8. Which statement by a patient would lead the nurse to suspect unsuccessful completion of the psychosocial developmental task of infancy? a. “I know how to do things right, so I prefer jobs where I work alone rather than on a team.” b. “I do not allow other people to truly get to know me.” c. “I depend on frequent praise from others to feel good about myself.” d. “I usually need to do things several times before I get them right.” ANS: B According to Erikson, the developmental task of infancy is the development of trust. The correct response is the only statement clearly showing lack of ability to trust others. An inability to work with others, coupled with a sense of superiority, suggests unsuccessful completion of the task of intimacy versus isolation. Relying on praise from others suggests unsuccessful completion of the task of identity versus role confusion. Shame suggests failure to resolve the crisis of initiative versus guilt. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 2-28, 29, 52 (Table 2-6) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 9. A patient is suspicious and frequently manipulates others. To which psychosexual stage do these traits relate? a. Oral b. Anal c. Phallic d. Genital ANS: A The behaviors in the stem develop as the result of attitudes formed during the oral stage, when an infant first learns to relate to the environment. Anal-stage traits include stinginess, stubbornness, orderliness, or their opposites. Phallic-stage traits include flirtatiousness, pride, vanity, difficulty with authority figures, and difficulties with sexual identity. Genital-stage traits include the ability to form satisfying sexual and emotional relationships with members of the opposite sex, emancipation from parents, a strong sense of personal identity, or the opposites of these traits. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-4, 5, 40 (Table 2-1) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 10. A patient expresses a desire to be cared for by others and often behaves in a helpless fashion. Which stage of psychosexual development is most relevant to the patient’s needs? a. Latency b. Phallic c. Anal d. Oral ANS: D Fixation at the oral stage sometimes produces dependent infantile behaviors in adults. Latency fixations often result in difficulty identifying with others and developing social skills, resulting in a sense of inadequacy and inferiority. Phallic fixations result in having difficulty with authority figures and poor sexual identity. Anal fixation sometimes results in retentiveness, rigidity, messiness, destructiveness, and cruelty. This item relates to an audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 2-40 (Table 2-1) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 11. A nurse listens to a group of recent retirees. One says, “I volunteer with Meals on Wheels, coach teen sports, and do church visitation.” Another laughs and says, “I’m too busy taking care of myself to volunteer to help others.” Which psychosocial developmental task do these statements contrast? a. Trust and mistrust b. Intimacy and isolation c. Industry and inferiority d. Generativity and self-absorption ANS: D Both retirees are in middle adulthood, when the developmental crisis to be resolved is generativity versus self-absorption. One exemplifies generativity; the other embodies self-absorption. This developmental crisis would show a contrast between relating to others in a trusting fashion and being suspicious and lacking trust. Failure to negotiate this developmental crisis would result in a sense of inferiority or difficulty learning and working as opposed to the ability to work competently. Behaviors that would be contrasted would be emotional isolation and the ability to love and commit oneself. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 2-52 (Table 2-6) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 12. An adult dies in a tragic accident. Afterward, the siblings plan a funeral service. Which statement by a sibling best indicates a sense of self-actualization? a. “Of all of us, I am the most experienced with planning these types of events.” b. “Funerals are supposed to be conducted quietly, respectfully, and according to a social protocol.” c. “This death was unfair but I hope we can plan a service that everyone feels is a celebration of life.” d. “This death was probably the consequence of years of selfish and inconsiderate behavior by our sibling.” ANS: C The correct response shows an accurate perception of reality as well as a focus on solving the problem in a way that involves others. These factors are characteristic of self-actualization. The incorrect responses demonstrate self-centeredness, rigidity, and blaming which are characteristic of a failure to achieve self-actualization. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-24, 62 (Box 2-1) TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 13. A student nurse says, “I don’t need to interact with my patients. I learn what I need to know by observation.” An instructor can best interpret the nursing implications of Sullivan’s theory to this student by responding: a. “Interactions are required in order to help you develop therapeutic communication skills.” b. “Nurses cannot be isolated. We must interact to provide patients with opportunities to practice interpersonal skills.” c. “Observing patient interactions will help you formulate priority nursing diagnoses and appropriate interventions.” d. “It is important to pay attention to patients’ behavioral changes, because these signify adjustments in personality.” ANS: B The nurse’s role includes educating patients and assisting them in developing effective interpersonal relationships. Mutuality, respect for the patient, unconditional acceptance, and empathy are cornerstones of Sullivan’s theory. The nurse who does not interact with the patient cannot demonstrate these cornerstones. Observations provide only objective data. Priority nursing diagnoses usually cannot be accurately established without subjective data from the patient. The other distracters relate to Maslow and behavioral theory. This item relates to an audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-8 to 10 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 14. A nurse consistently encourages patient to do his or her own activities of daily living. If the patient is unable to complete an activity, the nurse helps until the patient is once again independent. This nurse’s practice is most influenced by which theorist? a. Betty Neuman b. Patricia Benner c. Dorothea Orem d. Joyce Travelbee ANS: C Orem emphasizes the role of the nurse in promoting self-care activities of the patient; this has relevance to the seriously and persistently mentally ill patient. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 2-44 (Table 2-2) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Evaluation 15. A nurse uses Maslow’s hierarchy of needs to plan care for a patient diagnosed with mental illness. Which problem will receive priority? The patient a. refuses to eat or bathe. b. reports feelings of alienation from family. c. is reluctant to participate in unit social activities. d. is unaware of medication action and side effects. ANS: A The need for food and hygiene are physiological and therefore take priority over psychological or meta-needs in care planning. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 2-23, 24, 39 (Figure 2-5) TOP: Nursing Process: Planning/Outcomes Identification MSC: Client Needs: Safe, Effective Care Environment 16. Operant conditioning is part of the treatment plan to encourage speech in a child who is nearly mute. Which technique applies? a. Encourage the child to observe others talking. b. Include the child in small group activities. c. Give the child a small treat for speaking. d. Teach the child relaxation techniques. ANS: C Operant conditioning involves giving positive reinforcement for a desired behavior. Treats are rewards and reinforce speech through positive reinforcement. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-12, 13, 23 (Figure 2-3) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 17. The parent of a child diagnosed with schizophrenia tearfully asks the nurse, “What could I have done differently to prevent this illness?” Select the nurse’s best response. a. “Although schizophrenia results from impaired family relationships, try not to feel guilty. No one can predict how a child will respond to parental guidance.” b. “Schizophrenia is a biological illness resulting from changes in how the brain and nervous system function. You are not to blame for your child’s illness.” c. “There is still hope. Changing your parenting style can help your child learn to cope effectively with the environment.” d. “Most mental illnesses result from genetic inheritance. Your genes are more at fault than your parenting.” ANS: B The parent’s comment suggests feelings of guilt or inadequacy. The nurse’s response should address these feelings as well as provide information. Patients and families need reassurance that the major mental disorders are biological in origin and are not the “fault” of parents. One distracter places the burden of having faulty genes on the shoulders of the parents. The other distracters are neither wholly accurate nor reassuring. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-25 to 27 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 18. A nurse influenced by Peplau’s interpersonal theory works with an anxious, withdrawn patient. Interventions should focus on a. rewarding desired behaviors. b. use of assertive communication. c. changing the patient’s self-concept. d. administering medications to relieve anxiety. ANS: B The nurse–patient relationship is structured to provide a model for adaptive interpersonal relationships that can be generalized to others. Helping the patient learn to use assertive communication will improve the patient’s interpersonal relationships. The distracters apply to theories of cognitive, behavioral, and biological therapy. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-10, 11 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 19. A patient participated in psychotherapy weekly for 5 months. The therapist used free association, dream analysis, and facilitated transference to help the patient understand conflicts and foster change. Select the term that applies to this method. a. Rational-emotive behavior therapy b. Psychodynamic psychotherapy c. Cognitive-behavioral therapy d. Operant conditioning ANS: B The techniques are aspects of psychodynamic psychotherapy. The distracters use other techniques. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-7, 8, 49 (Table 2-4) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 20. Consider this comment from a therapist: “The patient is homosexual but has kept this preference secret. Severe anxiety and depression occur when the patient anticipates family reactions to this sexual orientation.” Which perspective is evident in the speaker? a. Theory of interpersonal relationships b. Classical conditioning theory c. Psychosexual theory d. Behaviorism theory ANS: A The theory of interpersonal relationships recognizes the anxiety and depression as resulting from unmet interpersonal security needs. Behaviorism and classical conditioning theories do not apply. A psychosexual formulation would focus on uncovering unconscious material that relates to the patient problem. PTS: 1 DIF: REF: Page 2-49 (Table 2-4) Cognitive Level: Apply (Application) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 21. A psychotherapist works with an anxious, dependent patient. Which strategy is most consistent with psychoanalytic psychotherapy? a. Identifying the patient’s strengths and assets b. Praising the patient for describing feelings of isolation c. Focusing on feelings developed by the patient toward the therapist d. Providing psychoeducation and emphasizing medication adherence ANS: C Positive or negative feelings of the patient toward the therapist indicate transference. Transference is a psychoanalytic concept that can be used to explore previously unresolved conflicts. The distracters relate to biological therapy and supportive psychotherapy. Use of psychoeducational materials is a common “homework” assignment used in cognitive therapy. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-7, 8, 49 (Table 2-4) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 22. A person says, “I was the only survivor in a small plane crash. Three business associates died. I got depressed and saw a counselor twice a week for 4 weeks. We talked about my feelings related to being a survivor, and I’m better now.” Which type of therapy was used? a. Systematic desensitization b. Psychoanalysis c. Behavior modification d. Interpersonal psychotherapy ANS: D Interpersonal psychotherapy returned the patient to his former level of functioning by helping him come to terms with the loss of friends and guilt over being a survivor. Systematic desensitization is a type of therapy aimed at extinguishing a specific behavior, such as the fear of flying. Psychoanalysis would call for a long period of exploration of unconscious material. Behavior modification would focus on changing a behavior rather than helping the patient understand what is going on in his life. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-8, 9, 49 (Table 2-4) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 23. Which technique is most applicable to aversion therapy? a. Punishment b. Desensitization c. Role modeling d. Positive reinforcement ANS: A Aversion therapy is akin to punishment. Aversive techniques include pairing of a maladaptive behavior with a noxious stimulus, punishment, and avoidance training. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-16, 17 MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Planning 24. A patient says to the nurse, “My father has been dead for over 10 years, but talking to you is almost as comforting as the talks he and I had when I was a child.” Which term applies to the patient’s comment? a. Superego b. Transference c. Reality testing d. Counter-transference ANS: B Transference refers to feelings a patient has toward the health care workers that were originally held toward significant others in his or her life. Counter-transference refers to unconscious feelings that the health care worker has toward the patient. The superego represents the moral component of personality; it seeks perfection. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-7, 49 (Table 2-4) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 25. A college student received an invitation to attend the wedding of a close friend who lives across the country. The student is afraid of flying. Which type of therapy would be most helpful for this patient? a. Psychoanalysis b. Aversion therapy c. Systematic desensitization d. Short-term dynamic therapy ANS: C Systematic desensitization is a type of therapy aimed at extinguishing a specific behavior, such as the fear of flying. Psychoanalysis and short-term dynamic therapy seek to uncover conflicts. Aversion therapy involves use of a noxious stimulus, punishment, and avoidance. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-15, 16 TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 26. A patient repeatedly stated, “I’m stupid.” Which statement by that patient would show progress resulting from cognitive-behavioral therapy? a. “Sometimes I do stupid things.” b. “Things always go wrong for me.” c. “I always fail when I try new things.” d. “I’m disappointed in my lack of ability.” ANS: A “I’m stupid” is a cognitive distortion. A more rational thought is “Sometimes I do stupid things.” The latter thinking promotes emotional self-control. The distracters reflect irrational or distorted thinking. This item relates to an audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-20 to 22, 46 (Table 2-3) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 27. A patient says, “All my life I’ve been surrounded by stupidity. Everything I buy breaks because the entire American workforce is incompetent.” This patient is experiencing a a. self-esteem deficit. b. cognitive distortion. c. deficit in motivation. d. deficit in love and belonging. ANS: B Automatic thoughts, or cognitive distortions, are irrational and lead to false assumptions and misinterpretations. See related audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-20 to 22, 46 (Table 2-3) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 28. A patient is fearful of riding on elevators. The therapist first rides an escalator with the patient. The therapist and patient then stand in an elevator with the door open for 5 minutes and later with the elevator door closed for 5 minutes. Which technique has the therapist used? a. Classic psychoanalytic therapy b. Systematic desensitization c. Rational emotive therapy d. Biofeedback ANS: B Systematic desensitization is a form of behavior modification therapy that involves the development of behavior tasks customized to the patient’s specific fears. These tasks are presented to the patient while using learned relaxation techniques. The patient is incrementally exposed to the fear. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-15, 16 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 29. A patient says, “I always feel good when I wear a size 2 petite.” Which type of cognitive distortion is evident? a. Disqualifying the positive b. Overgeneralization c. Catastrophizing d. Personalization ANS: B Automatic thoughts, or cognitive distortions, are irrational and lead to false assumptions and misinterpretations. The stem offers an example of overgeneralization. See related audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-20 to 22, 46 (Table 2-3) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 30. Which comment best indicates a patient is self-actualized? a. “I have succeeded despite a world filled with evil.” b. “I have a plan for my life. If I follow it, everything will be fine.” c. “I’m successful because I work hard. No one has ever given me anything.” d. “My favorite leisure is walking on the beach, hearing soft sounds of rolling waves.” ANS: D The self-actualized personality is associated with high productivity and enjoyment of life. Self-actualized persons experience pleasure in being alone and an ability to reflect on events. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-24, 62 (Box 2-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 31. A nurse presents a community education program about mental illness. Which comment by a participant best demonstrates a correct understanding of mental illness from a biological perspective? a. “Some people experience life events so traumatic that they cannot be overcome.” b. “Disturbed and conflicted family relationships are usually a starting place for mental illness.” c. “My friend has had bipolar disorder for years and many problems have resulted. It’s not her fault.” d. “Mental illness is the result of developmental complications that cause a person not to grow to their full potential.” ANS: C The correct response demonstrates an understanding that mental illness is physical in origin. The physical origins of mental illness are aspects of the biological model. The incorrect responses assign the origins of mental illness to interpersonal relationships and traumatic events. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 2 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 32. Which patient is the best candidate for brief psychodynamic therapy? a. An accountant with a loving family and successful career who was involved in a short extramarital affair b. An adult with a long history of major depression who was charged with driving under the influence c. A woman with a history of borderline personality disorder who recently cut both wrists d. An adult male recently diagnosed with anorexia nervosa ANS: A The best candidates for psychodynamic therapy are relatively healthy and well-functioning individuals, sometimes referred to as the “worried well,” who have a clearly circumscribed area of difficulty and are intelligent, psychologically minded, and well-motivated for change. Patients with psychosis, severe depression, borderline personality disorders, and severe character disorders are not appropriate candidates for this type of treatment. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-7, 8 TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity MULTIPLE RESPONSE 1. A patient states, “I’m starting cognitive-behavioral therapy. What can I expect from the sessions?” Which responses by the nurse would be appropriate? (Select all that apply.) a. “The therapist will be active and questioning.” b. “You will be given some homework assignments.” c. “The therapist will ask you to describe your dreams.” d. “The therapist will help you look at your ideas and beliefs about yourself.” e. “The goal is to increase subjectivity about thoughts that govern your behavior.” ANS: A, B, D Cognitive therapists are active rather than passive during therapy sessions because they help patient’s reality-test their thinking. Homework assignments are given and completed outside the therapy sessions. Homework is usually discussed at the next therapy session. The goal of cognitive therapy is to assist the patient in identifying inaccurate cognitions and in reality-testing and formulating new, accurate cognitions. One distracter applies to psychoanalysis. Increasing subjectivity is not desirable. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-19 to 21, 9 (Table 2-4) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 2. Which comments by an elderly person best indicate successful completion of the individual’s psychosocial developmental task? (Select all that apply.) a. “I am proud of my children’s successes in life.” b. “I should have given to community charities more often.” c. “My relationship with my father made life more difficult for me.” d. “My experiences in the war helped me appreciate the meaning of life.” e. “I often wonder what would have happened if I had chosen a different career.” ANS: A, D The developmental crisis for an elderly person relates to integrity versus despair. Pride in one’s offspring indicates a sense of fulfillment. Recognition of the wisdom gained from difficult experiences (such as being in a war) indicates a sense of integrity. Blaming and regret indicate despair and unsuccessful resolution of the crisis. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-28, 29, 52 (Table 2-6) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 3. Which comments by an adult best indicate self-actualization? (Select all that apply.) a. “I am content with a good book.” b. “I often wonder if I chose the right career.” c. “Sometimes I think about how my parents would have handled problems.” d. “It’s important for our country to provide basic health care services for everyone.” e. “When I was lost at sea for 2 days, I gained an understanding of what is important.” ANS: A, D, E Self-actualized persons enjoy privacy, have a sense of democracy, and show positive outcomes associated with peak experiences. Self-doubt, defensiveness, and blaming are not consistent with self-actualization. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-24, 62 (Box 2-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 4. Which activities represent the art of nursing? (Select all that apply.) a. Administering medications on time to a group of patients b. Listening to a new widow grieve her husband’s death c. Helping a patient obtain groceries from a food bank d. Teaching a patient about a new medication e. Holding the hand of a frightened patient ANS: B, C, E Peplau described the science and art of professional nursing practice. The art component of nursing consists of the care, compassion, and advocacy nurses provide to enhance patient comfort and well-being. The science component of nursing involves the application of knowledge to understand a broad range of human problems and psychosocial phenomena, intervening to relieve patients’ suffering and promote growth. See related audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 2-10, 11 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 5. Which therapies involve electrical brain stimulation for treatment of mental illness? (Select all that apply.) a. Aversion therapy b. Operant conditioning c. Systematic desensitization d. Electroconvulsive therapy (ECT) e. Transcranial magnetic stimulation (TMS) ANS: D, E ECT and TMS are therapies that use electrical stimulation of the brain as a form of treatment for mental illness. The incorrect responses are therapies that are interpersonal in nature. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 2-26, 51 (Table 2-5) TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity Chapter 03: Psychobiology and Psychopharmacology Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. A patient asks, “What are neurotransmitters? My doctor said mine are imbalanced.” Select the nurse’s best response. a. “How do you feel about having imbalanced neurotransmitters?” b. “Neurotransmitters protect us from harmful effects of free radicals.” c. “Neurotransmitters are substances we consume that influence memory and mood.” d. “Neurotransmitters are natural chemicals that pass messages between brain cells.” ANS: D The patient asked for information, and the correct response is most accurate. Neurotransmitters are chemical substances that function as messengers in the central nervous system. They are released from the axon terminal, diffuse across the synapse, and attach to specialized receptors on the postsynaptic neuron. The distracters either do not answer the patient’s question or provide untrue, misleading information. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 3-9 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. The parent of an adolescent diagnosed with schizophrenia asks the nurse, “My child’s doctor ordered a PET. What kind of test is that?” Select the nurse’s best reply. a. “This test uses a magnetic field and gamma waves to identify problem areas in the brain. Does your teenager have any metal implants?” b. “PET means positron-emission tomography. It is a special type of scan that shows blood flow and activity in the brain.” c. “A PET scan passes an electrical current through the brain and shows brain-wave activity. It can help diagnose seizures.” d. “It’s a special x-ray that shows structures of the brain and whether there has ever been a brain injury.” ANS: B The parent is seeking information about PET scans. It is important to use terms the parent can understand, so the nurse should identify what the initials mean. The correct response is the only option that provides information relevant to PET scans. The distracters describe magnetic resonance image (MRI), computed tomography (CT) scans, and EEG. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-13, 58 (Table 3-2) TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. A patient with a long history of hypertension and diabetes now develops confusion. The health care provider wants to make a differential diagnosis between Alzheimer’s disease and multiple infarcts. Which diagnostic procedure should the nurse expect to prepare the patient for first? a. Skull x-rays b. CT scan c. PET d. Single photon emission computed tomography (SPECT) ANS: B A CT scan shows the presence or absence of structural changes, including cortical atrophy, ventricular enlargement, and areas of infarct, information that would be helpful to the health care provider. PET and SPECT show brain activity rather than structure and may occur later. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-13, 58 (Table 3-2) TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 4. A patient’s history shows drinking 4 to 6 L of fluid and eating more than 6,000 calories per day. Which part of the central nervous system is most likely dysfunctional for this patient? a. Amygdala b. Parietal lobe c. Hippocampus d. Hypothalamus ANS: D The hypothalamus, a small area in the ventral superior portion of the brainstem, plays a vital role in such basic drives as hunger, thirst, and sex. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-10, 11 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. The nurse prepares to assess a patient diagnosed with major depressive disorder for disturbances in circadian rhythms. Which question should the nurse ask this patient? a. “Have you ever seen or heard things that others do not?” b. “What are your worst and best times of the day?” c. “How would you describe your thinking?” d. “Do you think your memory is failing?” ANS: B Mood changes throughout the day may be related to circadian rhythm disturbances. Questions about sleep pattern are also relevant to circadian rhythms. The distracters apply to assessment for illusions and hallucinations, thought processes, and memory. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 3-7 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 6. The nurse administers a medication that potentiates the action of ã-aminobutyric acid (GABA). Which effect would be expected? a. Reduced anxiety b. Improved memory c. More organized thinking d. Fewer sensory perceptual alterations ANS: A Increased levels of GABA reduce anxiety. Acetylcholine and substance P are associated with memory enhancement. Thought disorganization is associated with dopamine. GABA is not associated with sensory perceptual alterations. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-15, 16, 20, 53 (Table 3-1) TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 7. A nurse would anticipate that treatment for a patient with memory difficulties might include medications designed to a. inhibit GABA. b. prevent destruction of acetylcholine. c. reduce serotonin metabolism. d. increase dopamine activity. ANS: B Increased acetylcholine plays a role in learning and memory. Preventing destruction of acetylcholine by acetylcholinesterase would result in higher levels of acetylcholine, with the potential for improved memory. GABA affects anxiety rather than memory. Increased dopamine would cause symptoms associated with schizophrenia or mania rather than improve memory. Decreasing dopamine at receptor sites is associated with Parkinson’s disease rather than improving memory. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-37, 43, 53 (Table 3-1) TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 8. A patient has disorganized thinking associated with schizophrenia. Neuroimaging would likely show dysfunction in which part of the brain? a. Hippocampus b. Frontal lobe c. Cerebellum d. Brainstem ANS: B The frontal lobe is responsible for intellectual functioning. The hippocampus is involved in emotions and learning. The cerebellum regulates skeletal muscle coordination and equilibrium. The brainstem regulates internal organs. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-13, 50 (Figure 3-5) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 9. The nurse should assess a patient taking a drug with anticholinergic properties for inhibited function of the a. parasympathetic nervous system. b. sympathetic nervous system. c. reticular activating system. d. medulla oblongata. ANS: A Acetylcholine is the neurotransmitter found in high concentration in the parasympathetic nervous system. When anticholinergic drugs inhibit acetylcholine action, blurred vision, dry mouth, constipation, and urinary retention commonly occur. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 3-50 (Figure 3-1) | Page 3-53 (Table 3-1) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 10. The therapeutic action of neurotransmitter inhibitors that block reuptake cause a. decreased concentration of the blocked neurotransmitter in the central nervous system. b. increased concentration of the blocked neurotransmitter in the synaptic gap. c. destruction of receptor sites specific to the blocked neurotransmitter. d. limbic system stimulation. ANS: B If the reuptake of a substance is inhibited, it accumulates in the synaptic gap, and its concentration increases, permitting ease of transmission of impulses across the synaptic gap. Normal transmission of impulses across synaptic gaps is consistent with normal rather than depressed mood. The other options are not associated with blocking neurotransmitter reuptake. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-10, 24, 64 (Box 3-2) TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 11. A patient taking medication for mental illness develops restlessness and an uncontrollable need to be in motion. Which drug action causes these symptoms to develop? a. Anticholinergic effects b. Dopamine-blocking effects c. Endocrine-stimulating effects d. Ability to stimulate spinal nerves ANS: B Medication that blocks dopamine often produces disturbances of movement, such as akathisia, because dopamine affects neurons involved in both thought processes and movement regulation. Anticholinergic effects include dry mouth, blurred vision, urinary retention, and constipation. Akathisia is not caused by endocrine stimulation or spinal nerve stimulation. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-28, 36, 52 (Figure 3-20) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 12. A fearful patient has an increased heart rate and blood pressure. The nurse suspects increased activity of which neurotransmitter? a. GABA b. Norepinephrine c. Acetylcholine d. Histamine ANS: B Norepinephrine is the neurotransmitter associated with sympathetic nervous system stimulation, preparing the individual for “fight or flight.” GABA is a mediator of anxiety level. A high concentration of histamine is associated with an inflammatory response. A high concentration of acetylcholine is associated with parasympathetic nervous system stimulation. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 3-30 (Figure 3-1) | Page 3-53 (Table 3-1) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. A patient has acute anxiety related to an automobile accident 2 hours ago. The nurse should teach the patient about medication from which group? a. Tricyclic antidepressants b. Antipsychotic drugs c. Mood stabilizers d. Benzodiazepines ANS: D Benzodiazepines provide anxiety relief. Tricyclic antidepressants are used to treat symptoms of depression. Mood stabilizers are used to treat bipolar disorder. Antipsychotic drugs are used to treat psychosis. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: MSC: Pages 3-20, 21, 51 (Figure 3-12) TOP: Nursing Process: Planning Client Needs: Physiological Integrity 14. A patient is hospitalized for severe major depressive disorder. Of the medications listed below, the nurse can expect to provide the patient with teaching about a. chlordiazepoxide. b. clozapine. c. sertraline. d. tacrine. ANS: C Sertraline (Zoloft) is an selective serotonin reuptake inhibitor (SSRI). This antidepressant blocks the reuptake of serotonin, with few anticholinergic and sedating side effects. Clozapine is an antipsychotic. Chlordiazepoxide is an anxiolytic. Tacrine treats Alzheimer’s disease. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 3-25 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 15. A patient diagnosed with bipolar disorder displays aggressiveness, agitation, talkativeness, and irritability. The nurse expects the health care provider to prescribe a medication from which group? a. Psychostimulants b. Mood stabilizers c. Anticholinergics d. Antidepressants ANS: B The symptoms describe mania, which is effectively treated by mood stabilizers, such as lithium, and selected anticonvulsants (carbamazepine, valproic acid, and lamotrigine). Drugs from the other classifications listed are not effective in the treatment of mania. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-32, 33 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 16. A drug causes muscarinic receptor blockade. The nurse will assess the patient for a. dry mouth. b. gynecomastia. c. pseudoparkinsonism. d. orthostatic hypotension. ANS: A Muscarinic receptor blockade includes atropine-like side effects, such as dry mouth, blurred vision, and constipation. Gynecomastia is associated with decreased prolactin levels. Movement defects are associated with dopamine blockade. Orthostatic hypotension is associated with á1 antagonism. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 3-25, 30, 35 to 37 TOP: Nursing Process: Assessment Client Needs: Physiological Integrity 17. A patient begins therapy with a phenothiazine medication. What teaching should the nurse provide related to the drug’s strong dopaminergic effect? a. Chew sugarless gum. b. Increase dietary fiber. c. Arise slowly from bed. d. Report changes in muscle movement. ANS: D Phenothiazines block dopamine receptors in both the limbic system and basal ganglia. Movement disorders and motor abnormalities (extrapyramidal side effects), such as parkinsonism, akinesia, akathisia, dyskinesia, and tardive dyskinesia, are likely to occur early in the course of treatment. They are often heralded by sensations of muscle stiffness. Early intervention with antiparkinsonism medication can increase the patient’s comfort and prevent dystonic reactions. The distracters are related to anticholinergic effects. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-28, 36, 37, 52 (Figure 3-20) TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 18. A patient tells the nurse, “My doctor prescribed paroxetine for my depression. I assume I’ll have side effects like I had when I was taking imipramine.” The nurse’s reply should be based on the knowledge that paroxetine is a(n) a. selective norepinephrine reuptake inhibitor. b. tricyclic antidepressant. c. monoamine oxidase (MAO) inhibitor. d. SSRI. ANS: D Paroxetine is an SSRI and will not produce the same side effects as imipramine, a tricyclic antidepressant. The patient will probably not experience dry mouth, constipation, or orthostatic hypotension. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 3-25 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 19. A nurse can anticipate anticholinergic side effects are likely when a patient takes a. lithium. b. buspirone. c. imipramine. d. risperidone. ANS: C Imipramine (Tofranil) is a tricyclic antidepressant with strong anticholinergic properties, resulting in dry mouth, blurred vision, constipation, and urinary retention. Lithium therapy is more often associated with fluid-balance problems, including polydipsia, polyuria, and edema. Risperidone therapy is more often associated with movement disorders, orthostatic hypotension, and sedation. Buspirone is associated with anxiety reduction without major side effects. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-29, 30, 52 (Figure 3-17) TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 20. Which instruction has priority when teaching a patient about clozapine? a. “Avoid unprotected sex.” b. “Report sore throat and fever immediately.” c. “Reduce foods high in polyunsaturated fats.” d. “Use over-the-counter preparations for rashes.” ANS: B Clozapine therapy may produce agranulocytosis; therefore, signs of infection should be immediately reported to the health care provider. In addition, the patient should have white blood cell levels measured weekly. The other options are not relevant to clozapine. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-38, 39 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 21. A nurse cares for a group of patients receiving various medications, including haloperidol, carbamazepine, trazodone, and phenalgine. The nurse will order a special diet for the patient who takes a. carbamazepine. b. haloperidol. c. phenelzine. d. trazodone. ANS: C Patients taking phenelzine, an MAO inhibitor, must be on a low tyramine diet to prevent hypertensive crisis. There are no specific dietary precautions associated with the distracters. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 3-31 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 22. A nurse instructs a patient taking a drug that inhibits MAO to avoid certain foods and drugs because of the risk of a. cardiac dysrhythmia. b. hypotensive shock. c. hypertensive crisis. d. hypoglycemia. ANS: C Patients taking MAO-inhibiting drugs must be on a low tyramine diet to prevent hypertensive crisis. In the presence of MAO inhibitors, tyramine is not destroyed by the liver and in high levels produces intense vasoconstriction, resulting in elevated blood pressure. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 3-31 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 23. A nurse caring for a patient taking a SSRI will develop outcome criteria related to a. coherent thought processes. b. improvement in depression. c. reduced levels of motor activity. d. decreased extrapyramidal symptoms. SSRIs affect mood, relieving depression in many cases. SSRIs do not act to reduce thought disorders. SSRIs reduce depression but have little effect on motor hyperactivity. SSRIs do not produce extrapyramidal symptoms. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-24, 25 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 24. By which mechanism do SSRI medications improve depression? a. Destroying increased amounts of serotonin b. Making more serotonin available at the synaptic gap c. Increasing production of acetylcholine and dopamine d. Blocking muscarinic and á1 norepinephrine receptors ANS: B Depression is thought to be related to lowered availability of the neurotransmitter serotonin. SSRIs act by blocking reuptake of serotonin, leaving a higher concentration available at the synaptic cleft. SSRIs prevent destruction of serotonin. SSRIs have little or no effect on acetylcholine and dopamine production. SSRIs do not produce muscarinic or á1 norepinephrine blockade. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-24, 25 TOP: MSC: Client Needs: Physiological Integrity Nursing Process: Implementation 25. The laboratory report for a patient taking clozapine (Clozaril) shows a white blood cell count of 3000 mm3. Select the nurse’s best action. a. Report the results to the health care provider immediately. b. Administer the next dose as prescribed. c. Give aspirin and force fluids. d. Repeat the laboratory test. ANS: A These laboratory values indicate the possibility of agranulocytosis, a serious side effect of clozapine therapy. These results must be immediately reported to the health care provider, and the drug should be withheld. The health care provider may repeat the test, but in the meantime, the drug should be withheld. (Note: This question requires students to apply previous learning regarding normal and abnormal values of white blood cell counts.) PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 3-38, 39 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 26. A drug blocks the attachment of norepinephrine to 1 receptors. The patient may experience a. hypertensive crisis. b. orthostatic hypotension. c. severe appetite disturbance. d. an increase in psychotic symptoms. Sympathetic-mediated vasoconstriction is essential for maintaining normal blood pressure in the upright position. Blockage of 1 receptors leads to vasodilation and orthostatic hypotension. Orthostatic hypotension may cause fainting and falls. Teach patients ways of minimizing this phenomenon. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-28, 41, 42 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 27. A nurse cares for four patients who are receiving clozapine, lithium, fluoxetine, and venlafaxine, respectively. With which patient should the nurse be most alert for problems associated with fluid and electrolyte imbalance? The patient receiving a. lithium. b. clozapine. c. fluoxetine. d. venlafaxine. ANS: A Lithium is a salt and known to alter fluid and electrolyte balance, producing polyuria, edema, and other symptoms of imbalance. Patients receiving clozapine should be monitored for agranulocytosis. Patients receiving fluoxetine should be monitored for acetylcholine block. Patients receiving venlafaxine should be monitored for heightened feelings of anxiety. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-33, 62 (Table 3-3) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 28. An obese patient has a diagnosis of schizophrenia. Medications that block which receptors would contribute to further weight gain? a. H1 b. 5 HT2 c. Acetylcholine d. GABA ANS: A H1 receptor blockade results in weight gain, which is undesirable for an obese patient. Blocking of the other receptors would have little or no effect on the patient’s weight. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-37, 38, 40 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 29. An individual hiking in the forest encounters a large poisonous snake on the path. Which change in this individual’s vital signs is most likely? a. Pulse rate changes from 90 to 72. b. Respiratory rate changes from 22 to 18. c. Complaints of intestinal cramping begin. d. Blood pressure changes from 114/62 to 136/78. ANS: D This frightening experience would stimulate the sympathetic nervous system, causing a release of norepinephrine, an excitatory neurotransmitter. It prepares the body for fight or flight. Increased blood pressure, pupil size, respiratory rate, and pulse rate signify release of norepinephrine. Intestinal cramping would be associated with stimulation of the parasympathetic nervous system. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-5, 50 (Figure 3-1) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 30. Consider these medications: carbamazepine, lamotrigine, gabapentin. Which medication below also belongs to this group? a. Galantamine b. Valproate c. Buspirone d. Tacrine ANS: B The medications listed in the stem are mood stabilizers, anticonvulsant types. Valproate (Depakote) is also a member of this group. The distracters are drugs for treatment of Alzheimer’s disease and anxiety. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-33, 34 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 31. A professional football player is seen in the emergency department after losing consciousness from an illegal block. Prior to discharge, the nurse assists the patient to schedule an outpatient computed tomography (CT) scan for the next day. Which strategy should the nurse use to ensure the patient remembers the appointment? a. Write the appointment day, time, and location on a piece of paper and give it to the player. b. Log the appointment day, time, and location into the player’s cell phone calendar feature. c. Ask the health care provider to admit the patient to the hospital overnight. d. Verbally inform the patient of the appointment day, time, and location. ANS: B This player may have suffered repeated head injuries with damage to the hippocampus. The hippocampus has significant role in maintaining memory. Logging the appointment into the player’s cell phone calendar will remind him of the appointment the next day. Paper will be lost, and the patient is unlikely to remember verbal instruction. Hospitalization is unnecessary. See relationship to audience response question. Caution: This question requires students to apply previous learning regarding central nervous system anatomy and physiology. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Page 3-12 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment MULTIPLE RESPONSE 1. A nurse prepares to administer a second-generation antipsychotic medication to a patient diagnosed with schizophrenia. Additional monitoring for adverse effects will be most important if the patient has which co-morbid health problems? (Select all that apply.) a. Parkinson’s disease b. Grave’s disease c. Hyperlipidemia d. Osteoarthritis e. Diabetes ANS: A, C, E Antipsychotic medications may produce weight gain, which would complicate care of a patient with diabetes, and increase serum triglycerides, which would complicate care of a patient with hyperlipidemia. Parkinson’s disease involves changes in transmission of dopamine and acetylcholine, so these drugs would also complicate care of this patient. Osteoarthritis and Grave’s disease should have no synergistic effect with this medication. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 3-37, 38, 40 TOP: MSC: Client Needs: Physiological Integrity Nursing Process: Planning 2. Questions the nurse could ask that would be nonjudgmental when obtaining information about a patient’s use of complementary and herbal remedies include (Select all that apply) a. “You don’t regularly take herbal remedies, do you?” b. “What herbal medicines have you used to relieve your symptoms?” c. “What over-the-counter medicines, vitamins, and nutritional supplements do you use?” d. “What differences in your symptoms do you notice when you take herbal supplements?” e. “Have you experienced problems from using herbal and prescription drugs at the same time?” ANS: B, C, D, E The correct responses are neutral in tone and do not express bias for or against the use of complementary or herbal medicines. The distracter, worded in a negative way, makes the nurse’s bias evident. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 3-45 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 3. An individual is experiencing problems with memory. Which of these structures are most likely to be involved in this deficit? (Select all that apply.) a. Amygdala b. Hippocampus c. Occipital lobe d. Temporal lobe e. Basal ganglia ANS: A, B, D The frontal and temporal lobes of the cerebrum play a key role in the storage and processing of memories. The amygdala and hippocampus also play roles in memory. The occipital lobe is predominantly involved with vision. The basal ganglia influence integration of physical movement, as well as some thoughts and emotions. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 3-7, 12, 16, 50 (Figure 3-5) TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 4. A patient’s sibling says, “My brother has a mental illness, but the doctor ordered a functional magnetic resonance image (fMRI) test. That test is too expensive and will just increase the hospital bill.” Select the nurse’s best responses. (Select all that apply.) a. “Sometimes there are physical causes for psychiatric symptoms. This test will help us understand whether that is the situation.” b. “Some mental illnesses are evident on fMRIs. This test will give information to help us plan the best care for your brother.” c. “This test will indicate whether your brother has been taking his psychotropic medications as prescribed.” d. “It sounds like you do not truly believe your brother had a mental illness.” e. “It would be better for you to discuss your concerns with the health care provider.” ANS: A, B The correct responses provide information to the sibling. Modern imaging techniques are important tools in assessing molecular changes in mental disease and marking the receptor sites of drug action, which can help in treatment planning. Psychiatric symptoms can be caused by anatomical or physiologic abnormalities. There is no evidence of denial in the sibling’s comment. The nurse can answer this question rather than referring it to the physician/health care provider. An fMRI does not demonstrate adherence to the medication regime. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 3-13, 58 (Table 3-2) TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity Chapter 04: Treatment Settings Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. Inpatient hospitalization for persons with mental illness is generally reserved for patients who a. present a clear danger to self or others. b. are noncompliant with medication at home. c. have limited support systems in the community. d. develop new symptoms during the course of an illness. ANS: A Hospitalization is justified when the patient is a danger to self or others, has dangerously decompensated, or needs intensive medical treatment. The distracters do not necessarily describe patients who require inpatient treatment. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-18 to 20 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 2. A patient was hospitalized for 24 hours after a reaction to a psychotropic medication. While planning discharge, the case manager learned that the patient received a notice of eviction immediately prior to admission. Select the case manager’s most appropriate action. a. Postpone the patient’s discharge from the hospital. b. Contact the landlord who evicted the patient to further discuss the situation. c. Arrange a temporary place for the patient to stay until new housing can be arranged. d. Determine whether the adverse medication reaction was genuine because the patient had nowhere to live. ANS: C The case manager should intervene by arranging temporary shelter for the patient until an apartment can be found. This activity is part of the coordination and delivery of services that falls under the case manager role. None of the other options is a viable alternative. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 4-10, 40 (Table 4-1) TOP: Nursing Process: Implementation Client Needs: Safe, Effective Care Environment 3. Select the example of tertiary prevention. a. Helping a person diagnosed with a serious mental illness learn to manage money b. Restraining an agitated patient who has become aggressive and assaultive c. Teaching school-age children about the dangers of drugs and alcohol d. Genetic counseling with a young couple expecting their first child ANS: A Tertiary prevention involves services that address residual impairments, with a goal of improved independent functioning. Restraint is a secondary prevention. Genetic counseling and teaching school-age children about substance abuse and dependence are examples of primary prevention. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-16, 17 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 4. A patient diagnosed with schizophrenia had an exacerbation related to medication non-adherence and was hospitalized for 5 days. The patient’s thoughts are now more organized and discharge is planned. The patient’s family says, “It’s too soon for discharge. We will just go through all this again.” The nurse should a. ask the case manager to arrange a transfer to a long-term care facility. b. notify hospital security to handle the disturbance and escort the family off the unit. c. explain that the patient will continue to improve if the medication is taken regularly. d. contact the health care provider to meet with the family and explain the discharge rationale. ANS: C Patients do not stay in a hospital until every symptom disappears. The nurse must assume responsibility to advocate for the patient’s right to the least restrictive setting as soon as the symptoms are under control and for the right of citizens to control health care costs. The health care provider will use the same rationale. Shifting blame will not change the discharge. Security is unnecessary. The nurse can handle this matter. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-18, 40 (Table 4-1), 48 (Box 4-2) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 5. A nurse inspects an inpatient psychiatric unit and finds that exits are free of obstructions, no one is smoking, and the janitor’s closet is locked. These observations relate to a. coordinating care of patients. b. management of milieu safety. c. management of the interpersonal climate. d. use of therapeutic intervention strategies. ANS: B Nursing staff are responsible for all aspects of milieu management. The observations mentioned in this question directly relate to the safety of the unit. The other options, although part of the nurse’s concerns, are unrelated to the observations cited. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-23, 24 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 6. The patients below were evaluated in the emergency department. The psychiatric unit has one bed available. Which patient should be admitted? The patient a. feeling anxiety and a sad mood after separation from a spouse of 10 years. b. who self-inflicted a superficial cut on the forearm after a family argument. c. experiencing dry mouth and tremor related to taking antipsychotic medication. d. who is a new parent and hears voices saying, “Smother your baby.” ANS: D Admission to the hospital would be justified by the risk of patient danger to self or others. The other patients have issues that can be handled with less restrictive alternatives than hospitalization. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Page 4-20 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 7. A suspicious, socially isolated patient lives alone, eats one meal a day at a local shelter, and spends the remaining daily food allowance on cigarettes. Select a community psychiatric nurse’s best initial action. a. Explore ways to help the patient stop smoking. b. Report the situation to the manager of the shelter. c. Assess the patient’s weight; determine foods and amounts eaten. d. Arrange hospitalization for the patient in order to formulate a new treatment plan. ANS: C Assessment of biopsychosocial needs and general ability to live in the community is called for before any other action is taken. Both nutritional status and income adequacy are critical assessment parameters. A patient may be able to maintain adequate nutrition while eating only one meal a day. The rule is to assess before taking action. Hospitalization may not be necessary. Smoking cessation strategies can be pursued later. PTS: 1 DIF: REF: Pages 4-9, 17, 18 Cognitive Level: Apply (Application) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 8. A nurse surveys medical records. Which finding signals a violation of patients’ rights? a. A patient was not allowed to have visitors. b. A patient’s belongings were searched at admission. c. A patient with suicidal ideation was placed on continuous observation. d. Physical restraint was used after a patient was assaultive toward a staff member. ANS: A The patient has the right to have visitors. Inspecting patients’ belongings is a safety measure. Patients have the right to a safe environment, including the right to be protected against impulses to harm self. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-21, 48 (Box 4-2) TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 9. Which principle has the highest priority when addressing a behavioral crisis in an inpatient setting? a. Resolve the crisis with the least restrictive intervention possible. b. Swift intervention is justified to maintain the integrity of a therapeutic milieu. c. Rights of an individual patient are superseded by the rights of the majority of patients. d. Patients should have opportunities to regain control without intervention if the safety of others is not compromised. ANS: A The rule of using the least restrictive treatment or intervention possible to achieve the desired outcome is the patient’s legal right. Planned interventions are nearly always preferable. Intervention may be necessary when the patient threatens harm to self. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-21, 23, 24, 48 (Box 4-2) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 10. Clinical pathways are used in managed care settings to a. stabilize aggressive patients. b. identify obstacles to effective care. c. relieve nurses of planning responsibilities. d. streamline the care process and reduce costs. ANS: D Clinical pathways provide guidelines for assessments, interventions, treatments, and outcomes as well as a designated timeline for accomplishment. Deviations from the timeline must be reported and investigated. Clinical pathways streamline the care process and save money. Care pathways do not identify obstacles or stabilize aggressive patients. Staff are responsible for the necessary interventions. Care pathways do not relieve nurses of the responsibility of planning; pathways may, however, make the task easier. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 4-23 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 11. A nurse receives these three phone calls regarding a newly admitted patient. The psychiatrist wants to complete an initial assessment. An internist wants to perform a physical examination. The patient’s attorney wants an appointment with the patient. The nurse schedules the activities for the patient. Which role has the nurse fulfilled? a. Advocate b. Case manager c. Milieu manager d. Provider of care ANS: B Nurses on psychiatric units routinely coordinate patient services, serving as case managers as described in this scenario. The role of advocate would require the nurse to speak out on the patient’s behalf. The role of milieu manager refers to maintaining a therapeutic environment. Provider of care refers to giving direct care to the patient. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-10, 13, 49 (Box 4-3) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 12. Which aspect of direct care is an experienced, inpatient psychiatric nurse most likely to provide for a patient? a. Hygiene assistance b. Diversional activities c. Assistance with job hunting d. Building assertiveness skills ANS: D Assertiveness training relies on the counseling and psychoeducational skills of the nurse. Assistance with personal hygiene would usually be accomplished by a psychiatric technician or nursing assistant. Diversional activities are usually the province of recreational therapists. The patient would probably be assisted in job hunting by a social worker or vocational therapist. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-10, 11, 49 (Box 4-3) TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 13. Which characteristic would be more applicable to a community mental health nurse than to a nurse working in an operating room? a. Kindness b. Autonomy c. Compassion d. Professionalism ANS: B A community mental health nurse often works autonomously. Kindness, compassion, and professionalism apply to both nurses. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 4-17 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 14. Which patient would be most appropriate to refer for assertive community treatment (ACT)? A patient diagnosed with a. a phobic fear of crowded places. b. a single episode of major depressive disorder. c. a catastrophic reaction to a tornado in the community. d. schizophrenia and four hospitalizations in the past year. ANS: D ACT provides intensive case management for persons with serious persistent mental illness who live in the community. Repeated hospitalization is a frequent reason for this intervention. The distracters identify mental health problems of a more episodic nature. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-12, 13 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 15. The unit secretary receives a phone call from the health insurer for a hospitalized patient. The caller seeks information about the patient’s projected length of stay. How should the nurse instruct the unit secretary to handle the request? a. Obtain the information from the patient’s medical record and relay it to the caller. b. Inform the caller that all information about patients is confidential. c. Refer the request for information to the patient’s case manager. d. Refer the request to the health care provider. ANS: C The case manager usually confers with insurers and provides the treatment team with information about available resources. The unit secretary should be mindful of patient confidentiality and should neither confirm that the patient is an inpatient nor disclose other information. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-10, 13, 49 (Box 4-3) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 16. Select the example of primary prevention. a. Assisting a person diagnosed with a serious mental illness to fill a pill-minder b. Helping school-age children identify and describe normal emotions c. Leading a psychoeducational group in a community care home d. Medicating an acutely ill patient who assaulted a staff person ANS: B Primary preventions are directed at healthy populations with a goal of preventing health problems from occurring. Helping school-age children describe normal emotions people experience promotes coping, a skill that is needed throughout life. Assisting a person with serious and persistent mental illness to fill a pill-minder is an example of tertiary prevention. Medicating an acutely ill patient who assaulted a staff person is a secondary prevention. Leading a psychoeducational group in a community care home is an example of tertiary prevention. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 4-16, 17 TOP: Nursing Process: Implementation Client Needs: Health Promotion and Maintenance 17. Which level of prevention activities would a nurse in an emergency department employ most often? a. Primary b. Secondary c. Tertiary ANS: B An emergency department nurse would generally see patients in crisis or with acute illness, so secondary prevention is used. Primary prevention involves preventing a health problem from developing, and tertiary prevention applies to rehabilitative activities. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-16, 17 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 18. The nurse assigned to ACT should explain the program’s treatment goal as a. assisting patients to maintain abstinence from alcohol and other substances of abuse. b. providing structure and a therapeutic milieu for mentally ill patients whose symptoms require stabilization. c. maintaining medications and stable psychiatric status for incarcerated inmates who have a history of mental illness. d. providing services for mentally ill individuals who require intensive treatment to continue to live in the community. ANS: D An ACT program provides intensive community services to persons with serious, persistent mental illness who live in the community but require aggressive services to prevent repeated hospitalizations. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-12, 13 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 19. Which scenario best depicts a behavioral crisis? A patient is a. waving fists, cursing, and shouting threats at a nurse. b. curled up in a corner of the bathroom, wrapped in a towel. c. crying hysterically after receiving a phone call from a family member. d. performing push-ups in the middle of the hall, forcing others to walk around. ANS: A This behavior constitutes a behavioral crisis because the patient is threatening harm to another individual. Intervention is called for to defuse the situation. The other options speak of behaviors that may require intervention of a less urgent nature because the patients in question are not threatening harm to self or others. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 4-23, 24 TOP: Nursing Process: Assessment Client Needs: Psychosocial Integrity 20. The case manager plans to discuss the treatment plan with a patient’s family. Select the case manager’s first action. a. Determine an appropriate location for the conference. b. Support the discussion with examples of the patient’s behavior. c. Obtain the patient’s permission for the exchange of information. d. Determine which family members should participate in the conference. ANS: C The case manager must respect the patient’s right to privacy, which extends to discussions with family. Talking to family members is part of the case manager’s role. Actions identified in the distracters occur after the patient has given permission. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 4-10, 13, 49 (Box 4-3) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 21. A patient usually watches television all day, seldom going out in the community or socializing with others. The patient says, “I don’t know what to do with my free time.” Which member of the treatment team would be most helpful to this patient? a. Psychologist b. Social worker c. Recreational therapist d. Occupational therapist ANS: C Recreational therapists help patients use leisure time to benefit their mental health. Occupational therapists assist with a broad range of skills, including those for employment. Psychologists conduct testing and provide other patient services. Social workers focus on the patient’s support system. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 4-49 (Box 4-3) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Planning 22. A patient diagnosed with schizophrenia has been stable for 2 months. Today the patient’s spouse calls the nurse to report the patient has not taken prescribed medication and is having disorganized thinking. The patient forgot to refill the prescription. The nurse arranges a refill. Select the best outcome to add to the plan of care. a. The patient’s spouse will mark dates for prescription refills on the family calendar. b. The nurse will obtain prescription refills every 90 days and deliver to the patient. c. The patient will call the nurse weekly to discuss medication-related issues. d. The patient will report to the clinic for medication follow-up every week. ANS: A The nurse should use the patient’s support system to meet patient needs whenever possible. Delivery of medication by the nurse should be unnecessary for the nurse to do if patient or a significant other can be responsible. The patient may not need more intensive follow-up as long as medication is taken as prescribed. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-17, 40 (Table 4-1) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 23. A community mental health nurse has worked for months to establish a relationship with a delusional, suspicious patient. The patient recently lost employment and could no longer afford prescribed medications. The patient says, “Only a traitor would make me go to the hospital.” Select the nurse’s best initial intervention. a. With the patient’s consent, contact resources to provide medications without charge temporarily. b. Arrange a bed in a local homeless shelter with nightly on-site supervision. c. Hospitalize the patient until the symptoms have stabilized. d. Ask the patient, “Do you feel like I am a traitor?” ANS: A Hospitalization may damage the nurse–patient relationship, even if it provides an opportunity for rapid stabilization. If medication is restarted, the patient may possibly be stabilized in the home setting, even if it takes a little longer. Programs are available to help patients who are unable to afford their medications. A homeless shelter is inappropriate and unnecessary. Hospitalization may be necessary later, but a less restrictive solution should be tried first, since the patient is not dangerous. A yes/no question is non-therapeutic communication. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 71 | Pages 4-17, 18, 40 (Table 4-1) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 24. Which activity is appropriate for a nurse engaged exclusively in community-based primary prevention? a. Medication follow-up b. Teaching parenting skills c. Substance abuse counseling d. Making a referral for family therapy ANS: B Primary prevention activities are directed to healthy populations to provide information for developing skills that promote mental health. The distracters represent secondary or tertiary prevention activities. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-10, 11, 16, 17, 49 (Box 4-3) TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 25. A health care provider prescribed long acting antipsychotic medication injections every 3 weeks at the clinic for a patient with a history of medication nonadherence. For this plan to be successful, which factor will be of critical importance? a. The attitude of significant others toward the patient b. Nutrition services in the patient’s neighborhood c. The level of trust between the patient and nurse d. The availability of transportation to the clinic ANS: D The ability of the patient to get to the clinic is of paramount importance to the success of the plan. The long acting antipsychotic medication injections relieve the patient of the necessity to take medication daily, but if he or she does not receive the injection at 3-week intervals, non-adherence will again be the issue. Attitude toward the patient, trusting relationships, and nutrition are important but not fundamental to this particular problem. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 4-17, 18 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 26. Which assessment finding for a patient diagnosed with serious and persistent mental illness and living in the community merits priority intervention by the psychiatric nurse? The patient a. receives social security disability income plus a small check from a trust fund every month. b. was absent from two of six planned Alcoholics Anonymous meetings in the past 2 weeks. c. lives in an apartment with two patients who attend partial hospitalization programs. d. has a sibling who was recently diagnosed with a mental illness. ANS: B Patients who use alcohol or illegal substances often become medication non-adherent. Medication non-adherence, along with the disorganizing influence of substances on cellular brain function, promotes relapse. The distracters do not suggest problems. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 4-5, 10 TOP: Nursing Process: Planning MSC: Client Needs: Health Promotion and Maintenance 27. The nurse should refer which of the following patients to a partial hospitalization program? A patient who a. has a therapeutic lithium level and reports regularly for blood tests and clinic follow-up. b. needs psychoeducation for relaxation therapy related to agoraphobia and panic episodes. c. spent yesterday in a supervised crisis care center and continues to have active suicidal ideation. d. states, “I’m not sure I can avoid using alcohol when my spouse goes to work every morning.” ANS: D This patient could profit from the structure and supervision provided by spending the day at the partial hospitalization program. During the evening, at night, and on weekends, the spouse could assume responsibility for supervision. A suicidal patient needs inpatient hospitalization. The other patients can be served in the community or with individual visits. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-13, 14 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 28. After a Category 5 tornado hits a community and destroys many homes and businesses, a community mental health nurse encourages victims to describe their memories and feelings about the event. This action by the nurse best demonstrates a. triage. b. primary prevention. c. psychosocial rehabilitation. d. psychiatric case management. ANS: B Tornado victims are at risk for psychiatric problems as a consequence of stress and trauma. Primary prevention occurs before any problem is manifested and seeks to reduce the incidence, or rate of new cases. Primary prevention may prevent or delay the onset of symptoms in predisposed individuals. Coping strategies and psychosocial support for vulnerable people are effective interventions in prevention. Disaster victims benefit from telling their story. Triage refers to the process of sorting out victims based on the immediacy of their needs for treatment. Psychosocial rehabilitation programs are designed to assist persons diagnosed with serious mental illness to develop living skills. Psychiatric case management refers to services to assist patients in finding housing or obtaining entitlements. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 4-16 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 29. A nurse makes an initial visit to a homebound patient diagnosed with a serious mental illness. A family member offers the nurse a cup of coffee. Select the nurse’s best response. a. “Thank you. I would enjoy having a cup of coffee with you.” b. “Thank you, but I would prefer to proceed with the assessment.” c. “No, but thank you. I never accept drinks from patients or families.” d. “Our agency policy prohibits me from eating or drinking in patients’ homes.” ANS: A Accepting refreshments or chatting informally with the patient and family represent therapeutic use of self and help to establish rapport. The distracters fail to help establish rapport. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-12, 17, 18 MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Implementation 30. A nurse performed these actions while caring for patients in an inpatient psychiatric setting. Which action violated patients’ rights? a. Prohibited a patient from using the telephone b. In patient’s presence, opened a package mailed to patient c. Remained within arm’s length of patient with homicidal ideation d. Permitted a patient with psychosis to refuse oral psychotropic medication ANS: A The patient has a right to use the telephone. The patient should be protected against possible harm to self or others. Patients have rights to send and receive mail and be present during package inspection. Patients have rights to refuse treatment. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-21, 48 (Box 4-2) TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment MULTIPLE RESPONSE 1. A nurse can best address factors of critical importance to successful community treatment by including making assessments relative to (Select all that apply) a. housing adequacy. b. family and support systems. c. income adequacy and stability. d. early psychosocial development. e. substance abuse history and current use. ANS: A, B, C, E Early psychosocial developmental history is less relevant to successful outcomes in the community than the assessments listed in the other options. If a patient is homeless or fears homelessness, focusing on other treatment issues is impossible. Sufficient income for basic needs and medication is necessary. Adequate support is a requisite to community placement. Substance abuse undermines medication effectiveness and interferes with community adjustment. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-17, 18 TOP: MSC: Client Needs: Psychosocial Integrity Nursing Process: Assessment 2. The health care team at an inpatient psychiatric facility drafts these criteria for admission. Which criteria should be included in the final version of the admission policy? (Select all that apply) a. Clear risk of danger to self or others b. Adjustment needed for doses of psychotropic medication c. Detoxification from long-term heavy alcohol consumption needed d. Respite for caregivers of persons with serious and persistent mental illness e. Failure of community-based treatment, demonstrating need for intensive treatment ANS: A, C, E Medication doses can be adjusted on an outpatient basis. The goal of caregiver respite can be accomplished without hospitalizing the patient. The other options are acceptable, evidence-based criteria for admission of a patient to an inpatient service. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Page 4-20 TOP: Nursing Process: Implementation Client Needs: Safe, Effective Care Environment 3. A psychiatric nurse discusses rules of the therapeutic milieu and patients’ rights with a newly admitted patient. Which rights should be included? The right to (Select all that apply) a. have visitors. b. confidentiality. c. a private room. d. complain about inadequate care. e. select the nurse assigned to their care. ANS: A, B, D Patients’ rights should be discussed shortly after admission. Patients have rights related to receiving/refusing visitors, privacy, filing complaints about inadequate care, and accepting/refusing treatments (including medications). Patients do not have a right to a private room or selecting which nurse will provide care. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 4-21, 48 (Box 4-2) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 4. Which statements by patients diagnosed with a serious mental illness best demonstrate that the case manager has established an effective long-term relationship? “My case manager (Select all that apply) a. talks in language I can understand.” b. helps me keep track of my medication.” c. gives me little gifts from time to time.” d. looks at me as a whole person with many needs.” e. let me do whatever I choose without interfering.” ANS: A, B, D Each correct answer is an example of appropriate nursing foci: communicating at a level understandable to the patient, providing medication supervision, and using holistic principles to guide care. The distracters violate relationship boundaries or suggest a laissez faire attitude on the part of the nurse. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-10, 13, 49 (Box 4-3) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Evaluation 5. Which statements most clearly reflect the stigma of mental illness? (Select all that apply.) a. “Many mental illnesses are hereditary.” b. “Mental illness can be evidence of a brain disorder.” c. “People claim mental illness so they can get disability checks.” d. “Mental illness results from the breakdown of American families.” e. “If people with mental illness went to church, their symptoms would disappear.” ANS: C, D, E Stigma is represented by judgmental remarks that discount the reality and validity of mental illness. Many mental illnesses are genetically transmitted. Neuroimaging can show changes associated with some mental illnesses. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-2 to 4 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 6. A person in the community asks, “People with mental illnesses went to state hospitals in earlier times. Why has that changed?” Select the nurse’s accurate responses. (Select all that apply.) a. “Science has made significant improvements in drugs for mental illness, so now many persons may live in their communities.” b. “There’s now a better selection of less restrictive treatment options available in communities to care for people with mental illness.” c. “National rates of mental illness have declined significantly. There actually is not a need for state institutions anymore.” d. “Most psychiatric institutions were closed because of serious violations of patients’ rights and unsafe conditions.” e. “Federal legislation and payment for treatment of mental illness has shifted the focus to community rather than institutional settings.” ANS: A, B, E The community is a less restrictive alternative than hospitals for treatment of persons with mental illness. Funding for treatment of mental illness remains largely inadequate but now focuses on community rather than institutional care. Antipsychotic medications improve more symptoms of mental illness; hence, management of psychiatric disorders has improved. Rates of mental illness have increased, not decreased. Hospitals were closed because funding shifted to the community. Conditions in institutions have improved. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-19, 21, 47 (Box 4-1), 48 (Box 4-2) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 7. A patient diagnosed with schizophrenia lives in the community. On a home visit, the community psychiatric nurse case manager learns that the patient: wants to attend an activity group at the mental health outreach center. is worried about being able to pay for the therapy. does not know how to get from home to the outreach center. has an appointment to have blood work at the same time an activity group meets. wants to attend services at a church that is a half-mile from the patient’s home. Which tasks are part of the role of a community mental health nurse? (Select all that apply.) a. Rearranging conflicting care appointments b. Negotiating the cost of therapy for the patient c. Arranging transportation to the outreach center d. Accompanying the patient to church services weekly e. Monitoring to ensure the patient’s basic needs are met ANS: A, C, E The correct answers reflect the coordinating role of the community psychiatric nurse case manager. Negotiating the cost of therapy and accompanying the patient to church services are interventions the nurse would not be expected to undertake. The patient can walk to the church services; the nurse can provide encouragement. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 4-10, 13, 49 (Box 4-3) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment Chapter 05: Cultural Implications Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. Which Western cultural feature may result in establishing unrealistic outcomes for patients of other cultural groups? a. Interdependence b. Present orientation c. Flexible perception of time d. Direct confrontation to solve problems ANS: D Directly confronting problems is a highly valued approach in the American culture but not part of many other cultures in which harmony and restraint are valued. American nurses sometimes mistakenly think that all patients should take direct action. Patients with other values will be unable to meet this culturally inappropriate outcome. Present orientation, interdependence, and a flexible perception of time are not valued in Western culture. These views are more predominant in other cultures. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 5-33 (Table 5-4) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Planning 2. A psychiatric nurse leads a medication education group for Hispanic patients. This nurse holds a Western worldview and uses pamphlets as teaching tools. Groups are short and concise. After the group, the patients are most likely to believe a. the nurse was uncaring. b. the session was effective. c. the teaching was efficient. d. they were treated respectfully. ANS: A Hispanic individuals usually value relationship behaviors. Their needs are for learning through verbal communication rather than reading and for having time to chat before approaching the task. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-29 (Table 5-2) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 3. To provide culturally competent care, the nurse should a. accurately interpret the thinking of individual patients. b. predict how a patient may perceive treatment interventions. c. formulate interventions to reduce the patient’s ethnocentrism. d. identify strategies that fit within the cultural context of the patient. ANS: D The correct answer is the most global response. Cultural competence requires ongoing effort. Culture is dynamic, diversified, and changing. The nurse must be prepared to gain cultural knowledge and determine nursing care measures that patients find acceptable and helpful. Interpreting the thinking of individual patients does not ensure culturally competent care. Reducing a patient’s ethnocentrism may not be a desired outcome. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-11 TOP: Nursing Process: Planning/Outcomes Identification MSC: Client Needs: Psychosocial Integrity 4. A black patient, originally from Haiti, has a diagnosis of major depressive disorder. A colleague tells the nurse, “This patient often looks down and is reluctant to share feelings. However, I’ve observed the patient spontaneously interacting with other black patients.” Select the nurse’s best response. a. “Black patients depend on the church for support. Have you consulted the patient’s pastor?” b. “Encourage the patient to talk in a group setting. It will be less intimidating than one-to-one interaction.” c. “Don’t take it personally. Black patients often have a resentful attitude that takes a long time to overcome.” d. “The patient may have difficulty communicating in English. Have you considered using a cultural broker?” ANS: D Society expects a culturally diverse patient to accommodate and use English. Feelings are abstract, which requires a greater command of the language. This may be especially difficult during episodes of high stress or mental illness. Cultural brokers can be helpful with language and helping the nurse to understand the Haitian worldview and cultural nuances. PTS: 1 REF: Page 5-8 DIF: TOP: Cognitive Level: Apply (Application) Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 5. A Haitian patient diagnosed with major depressive disorder tells the nurse, “There’s nothing you can do. This is a punishment. The only thing I can do is see a healer.” The culturally aware nurse assesses that the patient a. has delusions of persecution. b. has likely been misdiagnosed with depression. c. may believe the distress is the result of a curse or spell. d. feels hopeless and helpless related to an unidentified cause. ANS: C Individuals of African American or Caribbean cultures who have a fatalistic attitude about illness may believe they are being punished for wrongdoing or are victims of witchcraft or voodoo. They may be reticent to share information about curses with therapists. No data are present in the scenario to support delusions. Misdiagnosis more often labels a patient with depression as having schizophrenia. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-29 (Table 5-2) | Page 5-33 (Table 5-4) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 6. A group activity on an inpatient psychiatric unit is scheduled to begin at 1000. A patient, who was recently discharged from U.S. Marine Corps, arrives at 0945. Which analysis best explains this behavior? a. The patient wants to lead the group and give directions to others. b. The patient wants to secure a chair that will be close to the group leader. c. The military culture values timeliness. The patient does not want to be late. d. The behavior indicates feelings of self-importance that the patient wants others to appreciate. ANS: C Culture is more than ethnicity and social norms; it includes religious, geographic, socioeconomic, occupational, ability- or disability-related, and sexual orientation-related beliefs and behaviors. In this instance, the patient’s military experience represents an aspect of the patient’s behavior. The military culture values timeliness. The distracters represent misinterpretation of the patient’s behavior and have no bearing on the situation. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 5-6, 33 (Table 5-4), 37 (Box 5-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 7. A nurse in the clinic has a full appointment schedule. A Hispanic American patient arrives at 1230 for a 1000 appointment. A Native American patient does not keep an appointment at all. What understanding will improve the nurse’s planning? These patients are a. members of cultural groups that have a different view of time. b. immature and irresponsible in health care matters. c. acting-out feelings of anger toward the system. d. displaying passive-aggressive tendencies. ANS: A Hispanic Americans and Native Americans traditionally treat time in a way unlike the Western culture. They tend to be present-oriented; that is, they value the current interaction more than what is to be done in the future. If engaged in an activity, for example, they may simply continue the activity and appear later for an appointment. Understanding this, the nurse can avoid feelings of frustration and anger when the nurse’s future orientation comes into conflict with the patient’s present orientation. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 5-6, 29 (Table 5-2) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 8. The sibling of an Asian American patient tells the nurse, “My sister needs help for pain. She cries from the hurt.” Which understanding by the nurse will contribute to culturally competent care for this patient? Persons of an Asian American heritage a. often express emotional distress with physical symptoms. b. will probably respond best to a therapist who is impersonal. c. will require prolonged treatment to stabilize these symptoms. d. should be given direct information about the diagnosis and prognosis. ANS: A Asian Americans commonly express psychological distress as a physical problem. The patient may believe psychological problems are caused by a physical imbalance. Treatment will likely be short. The patient will probably respond best to a therapist who is perceived as giving. Asian Americans usually have strong family ties and value hope more than truth. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 5-10, 35 (Table 5-5) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 9. Which communication strategy would be most effective for a nurse to use during an assessment interview with an adult Native American patient? a. Open and friendly; ask direct questions; touch the patient’s arm or hand occasionally for reassurance. b. Frequent nonverbal behaviors, such as gestures and smiles; make an unemotional face to express negatives. c. Soft voice; break eye contact occasionally; general leads and reflective techniques. d. Stern voice; unbroken eye contact; minimal gestures; direct questions. ANS: C Native American culture stresses living in harmony with nature. Cooperative, sharing styles rather than competitive or intrusive approaches are preferred; thus, the more passive style described would be best received. The other options would be more effective to use with patients of a Western orientation. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 5-17, 29 (Table 5-2) | Page 5-31 (Table 5-3) | Page 5-37 (Box 5-1) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 10. A Native American patient sadly describes a difficult childhood. The patient abused alcohol as a teenager but stopped 10 years ago. The patient now says, “I feel stupid and good for nothing. I don’t help my people.” How should the treatment team focus planning for this patient? a. Psychopharmacological and somatic therapies should be central techniques. b. Apply a psychoanalytical approach, focused on childhood trauma. c. Depression and alcohol abuse should be treated concurrently. d. Use a holistic approach, including mind, body, and spirit. ANS: D Native Americans, because of their beliefs in the interrelatedness of parts and about being in harmony with nature, respond best to a holistic approach. No data are present to support dual diagnosis, because the patient has resolved the problem of excessive alcohol use. Psychopharmacological and somatic therapies may be part of the treatment, but the focus should be more holistic. Psychoanalysis is a long-term expensive therapy; cognitive therapy might be a better choice. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-6 | Page 5-29 (Table 5-2) | Page 5-33 (Table 5-4) TOP: Nursing Process: Planning/Outcomes Identification MSC: Client Needs: Psychosocial Integrity 11. A Native American patient describes a difficult childhood and dropping out of high school. The patient abused alcohol as a teenager to escape feelings of isolation but stopped 10 years ago. The patient now says, “I feel stupid. I’ve never had a good job. I don’t help my people.” Which nursing diagnosis applies? a. Risk for other-directed violence b. Chronic low self-esteem c. Deficient knowledge d. Social isolation ANS: B The patient has given several indications of chronic low self-esteem. Forming a positive self-image is often difficult for Native American individuals because these indigenous people must blend together both American and Native American worldviews. No defining characteristics are present for the other nursing diagnoses. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 5-6, 20 TOP: Nursing Process: Diagnosis/Analysis MSC: Client Needs: Psychosocial Integrity 12. Which viewpoint of an Asian American family will most affect decision making about care? a. The father is the authority figure. b. The mother is head of the household. c. Women should make their own decisions. d. Emotional communication styles are desirable. ANS: A Asian American families traditionally place the father in the position of power as the head of the household. Mothers, as well as other women, are usually subservient to fathers in these cultures. Asian Americans are more likely to be reserved. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 5-6, 17, 35 (Table 5-5) TOP: Nursing Process: Planning/Outcomes Identification MSC: Client Needs: Psychosocial Integrity 13. Which intervention best demonstrates that a nurse correctly understands the cultural needs of a hospitalized Asian American patient diagnosed with a mental illness? a. Encouraging the family to attend community support groups b. Involving the patient’s family to assist with activities of daily living c. Providing educational pamphlets to explain the patient’s mental illness d. Restricting homemade herbal remedies the family brings to the hospital ANS: B The Asian community values the family in caring for each other. The Asian community uses traditional medicines and healers, including herbs for mental symptoms. The Asian community describes illness in somatic terms. The Asian community attaches a stigma to mental illness, so interfacing with the community would not be appealing. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 5-6, 17, 35 (Table 5-5) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 14. A nurse speaks with family members of a Chinese American parent recently diagnosed with major depressive disorder. Which comment by the nurse will the family find most comforting? “The nursing staff will a. take good care of your parent.” b. pray with your parent several times a day.” c. teach your parent important self-care strategies.” d. educate your parent about safety information regarding medication.” ANS: A Chinese Americans hold an Eastern (balance) worldview. Persons who are ill or need health care are vulnerable and need protection. The family will find comfort in a nurse’s statement that good care will be provided. The distracters apply to persons with a Western or indigenous worldview. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Page 5-29 (Table 5-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 15. A patient in the emergency department shows a variety of psychiatrical symptoms, including restlessness and anxiety. The patient says, “I feel sad because evil spirits have overtaken my mind.” Which worldview is most applicable to this individual? a. Eastern/balance b. Southern/holistic c. Western/scientific d. Indigenous/harmony ANS: D Persons of an indigenous worldview believe disease results from a lack of personal, interpersonal, environmental, or spiritual harmony and that evil spirits exist. The holism of body–mind–spirit is a key component of this view. If one believes an evil spirit has taken control, distress results. Western and Eastern worldviews do not embrace spirits. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: MSC: Page 5-29 (Table 5-2) TOP: Nursing Process: Assessment Client Needs: Psychosocial Integrity 16. A nurse prepares to teach important medication information to a patient of Mexican heritage. How should the nurse manage the teaching environment? a. Stand very close to the patient while teaching. b. Maintain direct eye contact with the patient while teaching. c. Maintain a neutral emotional tone during the teaching session. d. Sit 4 feet or more from the patient during the teaching session. ANS: A Latin American cultures use close personal space, closer than many other minority groups. Standing very close to the patient frequently indicates acceptance. Direct eye contact should not be prolonged with this patient. Persons of this cultural heritage have high emotionality. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-31 (Table 5-3) TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 17. A Chinese American patient diagnosed with an anxiety disorder says, “My problems began when my energy became imbalanced.” The nurse asks for the patient’s ideas about how to treat the imbalance. Which comment would the nurse expect from this patient? a. “My family will bring special foods to help me get well.” b. “I hope my health care provider will prescribe some medication to help me.” c. “I think I would benefit from talking to other patients with a similar problem.” d. “I would like to have a native healer perform a ceremony to balance my energy.” ANS: A The concept of energy imbalance as a source of illness is an explanatory model familiar to Asian cultures. A source of healing is dietary change to include either “hot” or “cold” foods to correct the imbalance. “Hot” and “cold” in this case do not refer to thermal properties of the foods. Medication would not be a treatment suggested by a patient with an Eastern worldview. Someone from an indigenous culture may suggest rituals. Group discussion of mental illness would not be appealing to a Chinese American. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-29 (Table 5-2) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Planning 18. An experienced psychiatric nurse plans to begin a new job in a community-based medication clinic. The clinic sees culturally diverse patients. Which action should the nurse take first to prepare for this position? a. Investigate cultural differences in patients’ responses to psychotropic medications. b. Contact the clinical nurse specialist for guidelines regarding cultural competence. c. Examine the literature on various health beliefs of members of diverse cultures. d. Complete an online continuing education offering about psychopharmacology. ANS: A An experienced nurse working on a mental health inpatient unit would be familiar with the action and side effects of most commonly prescribed psychotropic medications. However, because the clinic serves a culturally diverse population, reviewing cultural differences in patients’ responses to these medications is helpful and vital to patient safety. The distracters identify actions the nurse would take later. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Page 5-12 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 19. A psychoeducational session will discuss medication management for a culturally diverse group of patients. Group participants are predominantly members of minority cultures. Of the four staff nurses below, which nurse should lead this group? a. Very young registered nurse b. Older, mature registered nurse c. Newly licensed registered nurse d. A registered nurse who is very thin ANS: B Persons of minority cultures value age and wisdom. Persons with a Western worldview tend to value youth. An older, mature registered nurse would be the most credible leader of this group. The nurse’s size has no bearing on credibility. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-33 (Table 5-4) TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 20. A nurse wants to engage an interpreter for a severely anxious 21-year-old male who immigrated to the United States 2 years ago. Of the four interpreters below who are available and fluent in the patient’s language, which one should the nurse call? a. 65-year-old female professional interpreter b. 24-year-old male professional interpreter c. A member of the patient’s family d. The patient’s best friend ANS: B A professional interpreter will be most effective because he/she will be able to interpret both language and culture. When an interpreter is engaged, the interpreter should be matched to the patient as closely as possible in gender, age, social status, and religion. Interpreters should not be relatives or friends of the patient. The stigma of mental illness may prevent the openness needed during the encounter. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 5-8, 33 (Table 5-4) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Planning 21. A patient who has been hospitalized for 3 days with a serious mental illness says, “I’ve got to get out of here and back to my job. I get 60 to 80 messages a day, and I’m getting behind on my email correspondence.” What is this patient’s perspective about health and illness? a. Fateful, magical b. Eastern, holistic c. Western, biomedical d. Harmonious, religious ANS: C The Western biomedical perspective holds the belief that sick people should be as independent and self-reliant as possible. Self-care is encouraged; one gets better by “getting up and getting going.” An ability to function at a high level is valued. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 5-35 (Table 5-5) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 22. A white patient of German descent rocks back and forth, grimaces, and rubs both temples. What is the nurse’s best action? a. Assess the patient for extrapyramidal symptoms. b. Sit beside the patient and rock in sync. c. Offer to pray with the patient. d. Assess the patient for pain. ANS: D This patient of German descent would hold a Western worldview and be stoic about pain. This patient will keep pain as silent as possible and be reluctant to disclose pain unless the nurse actively assesses for it. The patient’s nonverbal communication suggests pain rather than EPS (extrapyramidal symptoms). The patient would probably not respond positively to prayer or the nurse’s rocking behavior. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-35 (Table 5-5) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 23. A Vietnamese patient’s family reports that the patient has wind illness. Which menu selection will be most helpful for this patient? a. Iced tea b. Ice cream c. Warm broth d. Gelatin dessert ANS: C Wind illness is a culture-bound syndrome found in the Chinese and Vietnamese population. It is characterized by a fear of cold, wind, or drafts. It is treated by keeping very warm and avoiding foods, drinks, and herbs that are cold. Warm broth would be most in sync with the patient’s culture and provide the most comfort. The distracters are cold foods. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Page 5-38 (Box 5-2) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Implementation 24. A Mexican American patient puts a picture of the Virgin Mary on the bedside table. What is the nurse’s best action? a. Move the picture so it is beside a window. b. Send the picture to the business office safe. c. Leave the picture where the patient placed it. d. Send the picture home with the patient’s family. ANS: C Cultural heritage is expressed through language, works of art, music, dance, customs, traditions, diet, and expressions of spirituality. This patient’s prominent placement of the picture is an example of expression of cultural heritage and spirituality. The nurse should not move it unless the patient’s safety is jeopardized. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 5-3, 16, 19 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 25. A nurse begins work in an agency that provides care to members of a minority ethnic population. The nurse will be better able to demonstrate cultural competence after a. identifying culture-bound issues. b. implementing scientifically proven interventions. c. correcting inferior health practices of the population. d. exploring commonly held beliefs and values of the population. ANS: D Cultural competence is dependent on understanding the beliefs and values of members of a different culture. A nurse who works with an individual or group of a culture different from his or her own must be open to learning about the culture. The other options have little to do with cultural competence or represent only a portion of the answer. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 5-15, 16 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 26. A nurse cares for a first-generation American whose family emigrated from Germany. Which worldview about the source of knowledge would this patient likely have? a. Knowledge is acquired through use of affective or feeling senses. b. Science is the foundation of knowledge and proves something exists. c. Knowledge develops by striving for transcendence of the mind and body. d. Knowledge evolves from an individual’s relationship with a supreme being. ANS: B The European-American perspective of acquiring knowledge evolves from science. The distracters describe the beliefs of other cultural groups. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 5-35 (Table 5-5) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment 27. The nurse administers medications to a culturally diverse group of patients on a psychiatric unit. What expectation should the nurse have about pharmacokinetics? a. Patients of different cultural groups may metabolize medications at different rates. b. Metabolism of psychotropic medication is consistent among various cultural groups. c. Differences in hepatic enzymes will influence the rate of elimination of psychotropic medications. d. It is important to provide patients with oral and written literature about their psychotropic medications. ANS: A Cytochrome enzyme systems, which vary among different cultural groups, influence the rate of metabolism of psychoactive drugs. Renal function influences elimination of psychotropic medication; hepatic function influences metabolism rates. Information about medication is important but does not apply to pharmacokinetics. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 5-12 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 28. A nurse prepares to assess a newly hospitalized patient who moved to the United States 6 months ago from Somalia. The nurse should first determine a. if the patient’s immunizations are current. b. the patient’s religious preferences. c. the patient’s specific ethnic group. d. whether an interpreter is needed. ANS: D The assessment depends on communication. The nurse should first determine whether an interpreter is needed. The other information can be subsequently assessed. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 5-8 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity MULTIPLE RESPONSE 1. Which questions should the nurse ask to determine an individual’s worldview? (Select all that apply.) a. What is more important: the needs of an individual or the needs of a community? b. How would you describe an ideal relationship between individuals? c. How long have you lived at your present residence? d. Of what importance are possessions in your life? e. Do you speak any foreign languages? ANS: A, B, D The answers provide information about cultural values related to the importance of individuality, material possessions, relational connectedness, community needs versus individual needs, and interconnectedness between humans and nature. These will assist the nurse to determine a patient’s worldview. Other follow-up questions are needed to validate findings. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 5-3, 7, 29 (Table 5-2) TOP: Nursing Process: Assessment Client Needs: Psychosocial Integrity 2. Why is the study of culture so important for psychiatric nurses in the United States? (Select all that apply.) a. Psychiatric nurses often practice in other countries. b. Psychiatric nurses must advocate for the traditions of the Western culture. c. Cultural competence helps protect patients from prejudice and discrimination. d. Patients should receive information about their illness and treatment in terms they understand. e. Psychiatric nurses often interface with patients and their significant others over a long period of time. ANS: C, D, E One purpose of cultural competence is for the psychiatric nurse to relate and explain information about the patient’s illness and treatment in an understandable way, incorporating the patient’s own beliefs and values. A fundamental aspect of nursing practice is advocacy. Cultural competence promotes recognition of prejudices in care, such as stigma and misdiagnosis. Psychiatric nurses often interface with patients and families over years and in community settings. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 5-15, 16 TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 3. The nurse should be particularly alert to expression of psychological distress through physical symptoms among patients whose cultural beliefs include (Select all that apply) a. mental illness reflects badly on the family. b. mental illness shows moral weakness. c. intergenerational conflict is common. d. the mind, body, and spirit are merged. e. food choices influence one’s health. ANS: A, B, D Physical symptoms are seen as more acceptable in cultural groups in which interdependence and harmony of the group are emphasized. Mental illness is often perceived as reflecting a failure of the entire family. In groups in which mental illness is seen as a moral weakness and both the individual and family are stigmatized, somatization of mental distress is better accepted. In groups in which mind, body, and spirit are holistically perceived, somatization of psychological distress is common. Somatization and food are not commonly related. Intergenerational conflict has not been noted as a risk factor for somatization. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 5-10, 11 MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment Chapter 06: Legal and Ethical Considerations Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. Which action by a psychiatric nurse best applies the ethical principle of autonomy? a. Exploring alternative solutions with the patient, who then makes a choice. b. Suggesting that two patients who were fighting be restricted to the unit. c. Intervening when a self-mutilating patient attempts to harm self. d. Staying with a patient demonstrating a high level of anxiety. ANS: A Autonomy is the right to self-determination, that is, to make one’s own decisions. By exploring alternatives with the patient, the patient is better equipped to make an informed, autonomous decision. The distracters demonstrate beneficence, fidelity, and justice. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-3, 4 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 2. A nurse finds a psychiatric advance directive in the medical record of a patient currently experiencing psychosis. The directive was executed during a period when the patient was stable and competent. The nurse should a. review the directive with the patient to ensure it is current. b. ensure that the directive is respected in treatment planning. c. consider the directive only if there is a cardiac or respiratory arrest. d. encourage the patient to revise the directive in light of the current health problem. ANS: B The nurse has an obligation to honor the right to self-determination. An advanced psychiatric directive supports that goal. Since the patient is currently psychotic, the terms of the directive now apply. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 6-16 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 3. Two hospitalized patients fight whenever they are together. During a team meeting, a nurse asserts that safety is of paramount importance, so treatment plans should call for both patients to be secluded to keep them from injuring each other. This assertion a. reinforces the autonomy of the two patients. b. violates the civil rights of both patients. c. represents the intentional tort of battery. d. correctly places emphasis on safety. ANS: B Patients have a right to treatment in the least restrictive setting. Safety is important, but less restrictive measures should be tried first. Unnecessary seclusion may result in a charge of false imprisonment. Seclusion violates the patient’s autonomy. The principle by which the nurse is motivated is beneficence, not justice. The tort represented is false imprisonment. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-16 to 18, 53 (Table 6-3) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 4. In a team meeting a nurse says, “I’m concerned about whether we are behaving ethically by using restraint to prevent one patient from self-mutilation, while the care plan for another self-mutilating patient requires one-on-one supervision.” Which ethical principle most clearly applies to this situation? a. Beneficence b. Autonomy c. Fidelity d. Justice ANS: D The nurse is concerned about justice, that is, fair distribution of care, which includes treatment with the least restrictive methods for both patients. Beneficence means promoting the good of others. Autonomy is the right to make one’s own decisions. Fidelity is the observance of loyalty and commitment to the patient. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 6-3 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 5. Select the example of a tort. a. The plan of care for a patient is not completed within 24 hours of the patient’s admission. b. A nurse gives a prn dose of an antipsychotic drug to an agitated patient because the unit is short-staffed. c. An advanced practice nurse recommends hospitalization for a patient who is dangerous to self and others. d. A patient’s admission status changed from involuntary to voluntary after the patient’s hallucinations subside. ANS: B A tort is a civil wrong against a person that violates his or her rights. Giving unnecessary medication for the convenience of staff controls behavior in a manner similar to secluding a patient; thus, false imprisonment is a possible charge. The other options do not exemplify torts. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 6-26, 27 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 6. What is the legal significance of a nurse’s action when a patient verbally refuses medication and the nurse gives the medication over the patient’s objection? The nurse a. has been negligent. b. committed malpractice. c. fulfilled the standard of care. d. can be charged with battery. ANS: D Battery is an intentional tort in which one individual violates the rights of another through touching without consent. Forcing a patient to take medication after the medication was refused constitutes battery. The charge of battery can be brought against the nurse. The medication may not necessarily harm the patient; harm is a component of malpractice. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 6-27, 53 (Table 6-3) TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 7. Which nursing intervention demonstrates false imprisonment? a. A confused and combative patient says, “I’m getting out of here, and no one can stop me.” The nurse restrains this patient without a health care provider’s order and then promptly obtains an order. b. A patient has been irritating and attention seeking much of the day. A nurse escorts the patient down the hall saying, “Stay in your room, or you’ll be put in seclusion.” c. An involuntarily hospitalized patient with suicidal ideation runs out of the psychiatric unit. The nurse rushes after the patient and convinces the patient to return to the unit. d. An involuntarily hospitalized patient with homicidal ideation attempts to leave the facility. A nurse calls the security team and uses established protocols to prevent the patient from leaving. ANS: B False imprisonment involves holding a competent person against his or her will. Actual force is not a requirement of false imprisonment. The individual needs only to be placed in fear of imprisonment by someone who has the ability to carry out the threat. If a patient is not competent (confused), then the nurse should act with beneficence. Patients admitted involuntarily should not be allowed to leave without permission of the treatment team. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: TOP: MSC: Page 6-27 | Page 6-53 (Table 6-3) | Page 6-59 (Box 6-4) Nursing Process: Evaluation Client Needs: Safe, Effective Care Environment 8. Which patient meets criteria for involuntary hospitalization for psychiatric treatment? The patient who a. is noncompliant with the treatment regimen. b. fraudulently files for bankruptcy. c. sold and distributed illegal drugs. d. threatens to harm self and others. ANS: D Involuntary hospitalization protects patients who are dangerous to themselves or others and cannot care for their own basic needs. Involuntary commitment also protects other individuals in society. The behaviors described in the other options are not sufficient to require involuntary hospitalization. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 6-7 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 9. A nurse prepares to administer a scheduled intramuscular injection of an antipsychotic medication to an outpatient diagnosed with schizophrenia. As the nurse swabs the site, the patient shouts, “Stop! I don’t want to take that medicine anymore. I hate the side effects.” Select the nurse’s best action. a. Assemble other staff for a show of force and proceed with the injection, using restraint if necessary. b. Stop the medication administration procedure and say to the patient, “Tell me more about the side effects you’ve been having.” c. Proceed with the injection but explain to the patient that there are medications that will help reduce the unpleasant side effects. d. Say to the patient, “Since I’ve already drawn the medication in the syringe, I’m required to give it, but let’s talk to the doctor about delaying next month’s dose.” ANS: B Patients diagnosed with mental illness retain their civil rights unless there is clear, cogent, and convincing evidence of dangerousness. The patient in this situation presents no evidence of dangerousness. The nurse, as an advocate and educator, should seek more information about the patient’s decision and not force the medication. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-12, 13 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 10. A nurse is concerned that an agency’s policies are inadequate. Which understanding about the relationship between substandard institutional policies and individual nursing practice should guide nursing practice? a. Agency policies do not exempt an individual nurse of responsibility to practice according to professional standards of nursing care. b. Agency policies are the legal standard by which a professional nurse must act and therefore override other standards of care. c. Faced with substandard policies, a nurse has a responsibility to inform the supervisor and discontinue patient care immediately. d. Interpretation of policies by the judicial system is rendered on an individual basis and therefore cannot be predicted. ANS: A Nurses are professionally bound to uphold standards of practice regardless of lesser standards established by a health care agency or a state. Conversely, if the agency standards are higher than standards of practice, the agency standards must be upheld. The Courts may seek to establish the standard of care through the use of expert witnesses when the issue is clouded. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 6-29 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 11. A newly admitted acutely psychotic patient is a private patient of the medical director and a private-pay patient. To whom does the psychiatric nurse assigned to the patient owe the duty of care? a. Medical director b. Hospital c. Profession d. Patient ANS: D Although the nurse is accountable to the health care provider, the agency, the patient, and the profession, the duty of care is owed to the patient. This duty reflects both legal and ethical standards of nursing practice. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 6-3, 4, 29 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 12. Which action by a nurse constitutes a breach of a patient’s right to privacy? a. Documenting the patient’s daily behavior during hospitalization b. Releasing information to the patient’s employer without consent c. Discussing the patient’s history with other staff during care planning d. Asking family to share information about a patient’s pre-hospitalization behavior ANS: B Release of information without patient authorization violates the patient’s right to privacy. The other options are acceptable nursing practices. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-20 to 22, 37 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 13. An adolescent hospitalized after a violent physical outburst tells the nurse, “I’m going to kill my father, but you can’t tell anyone.” Select the nurse’s best response. a. “You are right. Federal law requires me to keep clinical information private.” b. “I am obligated to share that information with the treatment team.” c. “Those kinds of thoughts will make your hospitalization longer.” d. “You should share this thought with your psychiatrist.” ANS: B Breach of nurse–patient confidentiality does not pose a legal dilemma for nurses in these circumstances because a team approach to delivery of psychiatric care presumes communication of patient information to other staff members to develop treatment plans and outcome criteria. The patient should also know that the team has a duty to warn the father of the risk for harm. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-20 to 22, 37 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 14. A voluntarily hospitalized patient tells the nurse, “Get me the forms for discharge. I want to leave now.” Select the nurse’s best response. a. “I will get the forms for you right now and bring them to your room.” b. “Since you signed your consent for treatment, you may leave if you desire.” c. “I will get them for you, but let’s talk about your decision to leave treatment.” d. “I cannot give you those forms without your health care provider’s permission.” ANS: C A voluntarily admitted patient has the right to demand and obtain release in most states. However, as a patient advocate, the nurse is responsible for weighing factors related to the patient’s wishes and best interests. By asking for information, the nurse may be able to help the patient reconsider the decision. Facilitating discharge without consent is not in the patient’s best interests before exploring the reason for the request. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-7, 8| Page 6-59 (Box 6-4) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 15. Insurance will not pay for continued private hospitalization of a mentally ill patient. The family considers transferring the patient to a public hospital but expresses concern that the patient will not get any treatment if transferred. Select the nurse’s most helpful reply. a. “By law, treatment must be provided. Hospitalization without treatment violates patients’ rights.” b. “All patients in public hospitals have the right to choose both a primary therapist and a primary nurse.” c. “You have a justifiable concern because the right to treatment extends only to provision of food, shelter, and safety.” d. “Much will depend on other patients, because the right to treatment for a psychotic patient takes precedence over the right to treatment of a patient who is stable.” ANS: A The right to medical and psychiatric treatment is conferred on all patients hospitalized in public mental hospitals under federal law. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 6-5, 6, 12 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 16. Which individual diagnosed with mental illness may need emergency or involuntary admission? The individual who a. resumes using heroin while still taking naltrexone (ReVia). b. reports hearing angels playing harps during thunderstorms. c. does not keep an outpatient appointment with the mental health nurse. d. throws a heavy plate at a waiter at the direction of command hallucinations. ANS: D Throwing a heavy plate is likely to harm the waiter and is evidence of dangerousness to others. This behavior meets the criteria for emergency or involuntary hospitalization for mental illness. The behaviors in the other options evidence mental illness but not dangerousness. See related audience response question. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Page 6-7 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 17. A patient in alcohol rehabilitation reveals to the nurse, “I feel terrible guilt for sexually abusing my 6-year-old before I was admitted.” Select the nurse’s most important action. a. Anonymously report the abuse by phone to the local child protection agency. b. Reply, “I’m glad you feel comfortable talking to me about it.” c. File a written report with the agency’s ethics committee. d. Respect nurse–patient relationship confidentiality. ANS: A Laws regarding child abuse reporting discovered by a professional during the suspected abuser’s alcohol or drug treatment differ by state. Federal law supersedes state law and prohibits disclosure without a court order except in instances in which the report can be made anonymously or without identifying the abuser as a patient in an alcohol or drug treatment facility. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 6-24 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 18. A family member of a patient with delusions of persecution asks the nurse, “Are there any circumstances under which the treatment team is justified in violating a patient’s right to confidentiality?” The nurse should reply that confidentiality may be breached a. under no circumstances. b. at the discretion of the psychiatrist. c. when questions are asked by law enforcement. d. if the patient threatens the life of another person. ANS: D The duty to warn a person whose life has been threatened by a psychiatric patient overrides the patient’s right to confidentiality. The right to confidentiality is not suspended at the discretion of the therapist or for legal investigations. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 6-22, 43 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 19. A new antidepressant is prescribed for an elderly patient diagnosed with major depressive disorder, but the dose is more than the usual geriatric dose. The nurse should a. consult a reliable drug reference. b. teach the patient about possible side effects and adverse effects. c. withhold the medication and confer with the health care provider. d. encourage the patient to increase oral fluids to reduce drug concentration. ANS: C The dose of antidepressants for elderly patients is often less than the usual adult dose. The nurse should withhold the medication and consult the health care provider who wrote the order. The nurse’s duty is to practice according to professional standards as well as intervene and protect the patient. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-30, 31, 55 (Box 6-1) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 20. A patient diagnosed with schizophrenia believes a local minister stirred evil spirits. The patient threatens to bomb a local church. The psychiatrist notifies the minister. Select the answer with the correct rationale. The psychiatrist a. released information without proper authorization. b. demonstrated the duty to warn and protect. c. violated the patient’s confidentiality. d. avoided charges of malpractice. ANS: B It is the health care professional’s duty to warn or notify an intended victim after a threat of harm has been made. Informing a potential victim of a threat is a legal responsibility of the health care professional. It is not a violation of confidentiality. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 6-22, 43 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 21. A patient experiencing psychosis became aggressive, struck another patient, and required seclusion. Select the best documentation. a. Patient struck another patient who attempted to leave day room to go to bathroom. Seclusion necessary at 1415. Plan: Maintain seclusion for 8 hours and keep these two patients away from each other for 24 hours. b. Seclusion ordered by physician at 1415 after command hallucinations told the patient to hit another patient. Careful monitoring of patient maintained during period of seclusion. c. Seclusion ordered by MD for aggressive behavior. Begun at 1415. Maintained for 2 hours without incident. Outcome: Patient calmer and apologized for outburst. d. Patient pacing, shouting. Haloperidol 5 mg given PO at 1300. No effect by 1315. At 1415 patient yelled, “I’ll punch anyone who gets near me,” and struck another patient with fist. Physically placed in seclusion at 1420. Seclusion order obtained from MD at 1430. ANS: D Documentation must be specific and detail the key aspects of care. It should demonstrate implementation of the least restrictive alternative. Justification for why a patient was secluded should be recorded, along with interventions attempted in an effort to avoid seclusion. Documentation should include a description of behavior and verbalizations, interventions tried and their outcomes, and the name of the health care provider ordering the use of seclusion. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-35, 36 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 22. A person in the community asks, “Why aren’t people with mental illness kept in state institutions anymore?” Select the nurse’s best response. a. “Less restrictive settings are available now to care for individuals with mental illness.” b. “There are fewer persons with mental illness, so less hospital beds are needed.” c. “Most people with mental illness are still in psychiatric institutions.” d. “Psychiatric institutions violated patients’ rights.” ANS: A The community is a less restrictive alternative than hospitals for treatment of persons with mental illness. The distracters are incorrect and part of the stigma of mental illness. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-6, 9 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 23. A patient experiencing psychosis asks a psychiatric technician, “What’s the matter with me?” The technician replies, “Nothing is wrong with you. You just need to use some self-control.” The nurse who overheard the exchange should take action based on a. the technician’s unauthorized disclosure of confidential clinical information. b. violation of the patient’s right to be treated with dignity and respect. c. the nurse’s obligation to report caregiver negligence. d. the patient’s right to social interaction. ANS: B Patients have the right to be treated with dignity and respect. The technician’s comment disregards the seriousness of the patient’s illness. The Code of Ethics for Nurses requires intervention. Patient emotional abuse has been demonstrated, not negligence. An interaction with the technician is not an aspect of social interaction. The technician did not disclose clinical information. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 6-55 (Box 6-1) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 24. Which documentation of a patient’s behavior best demonstrates a nurse’s observations? a. Isolates self from others. Frequently fell asleep during group. Vital signs stable. b. Calmer; more cooperative. Participated actively in group. No evidence of psychotic thinking. c. Appeared to hallucinate. Frequently increased volume on television, causing conflict with others. d. Wore four layers of clothing. States, “I need protection from evil bacteria trying to pierce my skin.” ANS: D The documentation states specific observations of the patient’s appearance and the exact statements made. The other options are vague or subjective statements and can be interpreted in different ways. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-35, 36 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 25. After leaving work, a nurse realizes documentation of administration of a prn medication was omitted. This off-duty nurse phones the nurse on duty and says, “Please document administration of the medication for me. My password is alpha1.” The nurse receiving the call should a. fulfill the request promptly. b. document the caller’s password. c. refer the matter to the charge nurse to resolve. d. report the request to the patient’s health care provider. ANS: C Fraudulent documentation may be grounds for discipline by the state board of nursing. Referring the matter to the charge nurse will allow observance of hospital policy while ensuring that documentation occurs. Notifying the health care provider would be unnecessary when the charge nurse can resolve the problem. Nurses should not provide passwords to others. PTS: 1 DIF: REF: Pages 6-35, 36 Cognitive Level: Apply (Application) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 26. Which individual diagnosed with a mental illness may need involuntary hospitalization? An individual a. who has a panic attack after her child gets lost in a shopping mall. b. with visions of demons emerging from cemetery plots throughout the community. c. who takes 38 acetaminophen tablets after the person’s stock portfolio becomes worthless. d. diagnosed with major depression who stops taking prescribed antidepressant medication. ANS: C Involuntary hospitalization protects patients who are dangerous to themselves or others and cannot care for their own basic needs. Involuntary hospitalization also protects other individuals in society. An overdose of acetaminophen indicates dangerousness to self. The behaviors described in the other options are not sufficient to require involuntary hospitalization. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-7, 8 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 27. An aide in a psychiatric hospital says to the nurse, “We don’t have time every day to help each patient complete a menu selection. Let’s tell dietary to prepare popular choices and send them to our unit.” Select the nurse’s best response. a. “Thanks for the suggestion, but that idea may not work because so many patients take MAOI (monoamine oxidase inhibitor) antidepressants.” b. “Thanks for the idea, but it’s important to treat patients as individuals. Giving choices is one way we can respect patients’ individuality.” c. “Thank you for the suggestion, but the patients’ bill of rights requires us to allow patients to select their own diet.” d. “Thank you. That is a very good idea. It will make meal preparation easier for the dietary department.” ANS: B The nurse’s response to the aide should recognize patients’ rights to be treated with dignity and respect as well as promote autonomy. This response also shows respect for the aide and fulfills the nurse’s obligation to provide supervision of unlicensed personnel. The incorrect responses have flawed rationale or do not respect patients as individuals. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 6-3, 4 | Page 6-55 (Box 6-1) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 28. In order to release information to another health care facility or third party regarding a patient diagnosed with a mental illness, the nurse must obtain a. a signed consent by the patient for release of information stating specific information to be released. b. a verbal consent for information release from the patient and the patient’s guardian or next of kin. c. permission from members of the health care team who participate in treatment planning. d. approval from the attending psychiatrist to authorize the release of information. ANS: A Nurses have an obligation to protect patients’ privacy and confidentiality. Clinical information should not be released without the patient’s signed consent for the release. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-20, 21, 22 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment MULTIPLE RESPONSE 1. In which situations would a nurse have the duty to intervene and report? (Select all that apply.) a. A peer has difficulty writing measurable outcomes. b. A health care provider gives a telephone order for medication. c. A peer tries to provide patient care in an alcohol-impaired state. d. A team member violates relationship boundaries with a patient. e. A patient refuses medication prescribed by a licensed health care provider. ANS: C, D Both keyed answers are events that jeopardize patient safety. The distracters describe situations that may be resolved with education or that are acceptable practices. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 6-55 (Box 6-1) | Page 6-32, 33 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 2. Which actions violate the civil rights of a psychiatric patient? The nurse (Select all that apply) a. performs mouth checks after overhearing a patient say, “I’ve been spitting out my medication.” b. begins suicide precautions before a patient is assessed by the health care provider. c. opens and reads a letter a patient left at the nurse’s station to be mailed. d. places a patient’s expensive watch in the hospital business office safe. e. restrains a patient who uses profanity when speaking to the nurse. ANS: C, E The patient has the right to send and receive mail without interference. Restraint is not indicated because a patient uses profanity; there are other less restrictive ways to deal with this behavior. The other options are examples of good nursing judgment and do not violate the patient’s civil rights. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 6-5, 53 (Table 6-3) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment Chapter 07: The Nursing Process and Standards of Care Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. A new staff nurse completes an orientation to the psychiatric unit. This nurse will expect to ask an advanced practice nurse to perform which action for patients? a. Perform mental health assessment interviews. b. Prescribe psychotropic medication. c. Establish therapeutic relationships. d. Individualize nursing care plans. ANS: B Prescriptive privileges are granted to master’s-prepared nurse practitioners who have taken special courses on prescribing medication. The nurse prepared at the basic level performs mental health assessments, establishes relationships, and provides individualized care planning. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 7-23, 24 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 2. A newly admitted patient diagnosed with major depressive disorder has gained 20 pounds over a few months and has suicidal ideation. The patient has taken antidepressant medication for 1 week without remission of symptoms. Select the priority nursing diagnosis. a. Imbalanced nutrition: more than body requirements b. Chronic low self-esteem c. Risk for suicide d. Hopelessness ANS: C Risk for suicide is the priority diagnosis when the patient has both suicidal ideation and a plan to carry out the suicidal intent. Imbalanced nutrition, hopelessness, and chronic low self-esteem may be applicable nursing diagnoses, but these problems do not affect patient safety as urgently as would a suicide attempt. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: MSC: Page 7-19 TOP: Nursing Process: Diagnosis/Analysis Client Needs: Psychosocial Integrity 3. A patient diagnosed with major depressive disorder has lost 20 pounds in one month, has chronic low self-esteem, and a plan for suicide. The patient has taken antidepressant medication for 1 week. Which nursing intervention has the highest priority? a. Implement suicide precautions. b. Offer high-calorie snacks and fluids frequently. c. Assist the patient to identify three personal strengths. d. Observe patient for therapeutic effects of antidepressant medication. ANS: A Implementing suicide precautions is the only option related to patient safety. The other options, related to nutrition, self-esteem, and medication therapy, are important but are not priorities. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-19, 39 (Table 7-3) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 4. The desired outcome for a patient experiencing insomnia is, “Patient will sleep for a minimum of 5 hours nightly within 7 days.” At the end of 7 days, review of sleep data shows the patient sleeps an average of 4 hours nightly and takes a 2-hour afternoon nap. The nurse will document the outcome as a. consistently demonstrated. b. often demonstrated. c. sometimes demonstrated. d. never demonstrated. ANS: D The correct response to this question involves applying the evaluation step of nursing process. Although the patient is sleeping 6 hours daily, the total is not one uninterrupted session at night. Therefore, the outcome must be evaluated as never demonstrated. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-18, 19, 24 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 5. The desired outcome for a patient experiencing insomnia is, “Patient will sleep for a minimum of 5 hours nightly within 7 days.” At the end of 7 days, review of sleep data shows the patient sleeps an average of 4 hours nightly and takes a 2-hour afternoon nap. What is the nurse’s next action? a. Continue the current plan without changes. b. Remove this nursing diagnosis from the plan of care. c. Write a new nursing diagnosis that better reflects the problem. d. Examine interventions for possible revision of the target date. ANS: D The correct response to this question involves applying the evaluation step of nursing process. Sleeping a total of 5 hours at night remains a reasonable outcome. Extending the period for attaining the outcome may be appropriate. Examining interventions might result in planning an activity during the afternoon rather than permitting a nap. Continuing the current plan without changes is inappropriate. Removing this nursing diagnosis from the plan of care would be correct when the outcome was met and the problem resolved. Writing a new nursing diagnosis is inappropriate because no other nursing diagnosis relates to the problem. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-18, 19, 24 TOP: Nursing Process: Evaluation 6. A patient begins a new program to assist with building social skills. In which part of the plan of care should a nurse record the item, “Encourage patient to attend one psychoeducational group daily”? a. Assessment b. Analysis c. Implementation d. Evaluation ANS: C Interventions are the nursing prescriptions to achieve the outcomes. Interventions should be specific. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-20 to 22 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 7. Before assessing a new patient, a nurse is told by another health care worker, “I know that patient. No matter how hard we work, there isn’t much improvement by the time of discharge.” The nurse’s responsibility is to a. document the other worker’s assessment of the patient. b. assess the patient based on data collected from all sources. c. validate the worker’s impression by contacting the patient’s significant other. d. discuss the worker’s impression with the patient during the assessment interview. ANS: B Assessment should include data obtained from both the primary and reliable secondary sources. The nurse, bearing in mind the possible effects of counter-transference, should evaluate biased assessments by others as objectively as possible. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-4 to 6 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 8. A patient presents to the emergency department with mixed psychiatric symptoms. The admission nurse suspects the symptoms may be the result of a medical problem. Lab results show elevated BUN (blood urea nitrogen) and creatinine. What is the nurse’s next best action? a. Report the findings to the health care provider. b. Assess the patient for a history of renal problems. c. Assess the patient’s family history for cardiac problems. d. Arrange for the patient’s hospitalization on the psychiatric unit. ANS: B Elevated BUN and creatinine suggest renal problems. Renal dysfunction can often imitate psychiatric disorders. The nurse should further assess the patient’s history for renal problems and then share the findings with the health care provider. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-10, 44 (Box 7-3) TOP: Nursing Process: Assessment 9. A patient states, “I’m not worth anything. I have negative thoughts about myself. I feel anxious and shaky all the time. Sometimes I feel so sad that I want to go to sleep and never wake up.” Which nursing intervention should have the highest priority? a. Self-esteem–building activities b. Anxiety self-control measures c. Sleep enhancement activities d. Suicide precautions ANS: D The nurse would place a priority on monitoring and reinforcing suicide self-restraint because it relates directly and immediately to patient safety. Patient safety is always a priority concern. The nurse should monitor and reinforce all patient attempts to control anxiety, improve sleep patterns, and develop self-esteem, while giving priority attention to suicide self-restraint. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-9, 19, 36 (Table 7-2) | Page 7-39 (Table 7-3) TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 10. Select the best outcome for a patient with the nursing diagnosis: Impaired social interaction related to sociocultural dissonance as evidenced by stating, “Although I’d like to, I don’t participate because I don’t speak the language very well.” Patient will a. show improved use of language. b. demonstrate improved social skills. c. become more independent in decision making. d. select and participate in one group activity per day. ANS: D The outcome describes social involvement on the part of the patient. Neither cooperation nor independence has been an issue. The patient has already expressed a desire to interact with others. Outcomes must be measurable. Two of the distracters are not measurable. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-18, 19, 39 (Table 7-3) TOP: MSC: Nursing Process: Outcomes Identification Client Needs: Psychosocial Integrity 11. Nursing behaviors associated with the implementation phase of nursing process are concerned with a. participating in mutual identification of patient outcomes. b. gathering accurate and sufficient patient-centered data. c. comparing patient responses and expected outcomes. d. carrying out interventions and coordinating care. ANS: D Nursing behaviors relating to implementation include using available resources, performing interventions, finding alternatives when necessary, and coordinating care with other team PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 7-20, 21, 33 (Figure 7-1) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 12. Which statement made by a patient during an initial assessment interview should serve as the priority focus for the plan of care? a. “I can always trust my family.” b. “It seems like I always have bad luck.” c. “You never know who will turn against you.” d. “I hear evil voices that tell me to do bad things.” ANS: D The statement regarding evil voices tells the nurse that the patient is experiencing auditory hallucinations and may create risks for violence. Safety is the nurse’s first concern. The other statements are vague and do not clearly identify the patient’s chief symptom. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-11, 12, 19, 43 (Box 7-2) TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. Which entry in the medical record best meets the requirement for problem-oriented charting? a. “A: Pacing and muttering to self. P: Sensory perceptual alteration related to internal auditory stimulation. I: Given fluphenazine HCL 2.5 mg po at 0900 and went to room to lie down. E: Calmer by 0930. Returned to lounge to watch TV.” b. “S: States, ‘I feel like I’m ready to blow up.’ O: Pacing hall, mumbling to self. A: Auditory hallucinations. P: Offer haloperidol 2 mg po. I: Haloperidol 2 mg po given at 0900. E: Returned to lounge at 0930 and quietly watched TV.” c. “Agitated behavior. D: Patient muttering to self as though answering an unseen person. A: Given haloperidol 2 mg po and went to room to lie down. E: Patient calmer. Returned to lounge to watch TV.” d. “Pacing hall and muttering to self as though answering an unseen person. haloperidol 2 mg po administered at 0900 with calming effect in 30 minutes. Stated, ‘I’m no longer bothered by the voices.’” ANS: B Problem-oriented documentation uses the first letter of key words to organize data: S for subjective data, O for objective data, A for assessment, P for plan, I for intervention, and E for evaluation. The distracters offer examples of PIE charting, focus documentation, and narrative documentation. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-24, 25, 40 (Table 7-4) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 14. A nurse assesses an older adult patient brought to the emergency department by a family member. The patient was wandering outside saying, “I can’t find my way home.” The patient is confused and unable to answer questions. Select the nurse’s best action. a. Record the patient’s answers to questions on the nursing assessment form. b. Ask an advanced practice nurse to perform the assessment interview. c. Call for a mental health advocate to maintain the patient’s rights. d. Obtain important information from the family member. ANS: D When the patient (primary source) is unable to provide information, secondary sources should be used, in this case, the family member. Later, more data may be obtained from other information sources familiar with the patient. An advanced practice nurse is not needed for this assessment; it is within the scope of practice of the staff nurse. Calling a mental health advocate is unnecessary. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 7-6 TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 15. A nurse asks a patient, “If you had fever and vomiting for 3 days, what would you do?” Which aspect of the mental status examination is the nurse assessing? a. Behavior b. Cognition c. Affect and mood d. Perceptual disturbances ANS: B Assessing cognition involves determining a patient’s judgment and decision making. In this case, the nurse would expect a response of “Call my doctor” if the patient’s cognition and judgment are intact. If the patient responds, “I would stop eating” or “I would just wait and see what happened,” the nurse would conclude that judgment is impaired. The other options refer to other aspects of the examination. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-11, 47 (Box 7-4) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment 16. An adolescent asks a nurse conducting an assessment interview, “Why should I tell you anything? You’ll just tell my parents whatever you find out.” Which response by the nurse is appropriate? a. “That isn’t true. What you tell us is private and held in strict confidence. Your parents have no right to know.” b. “Yes, your parents may find out what you say, but it is important that they know about your problems.” c. “What you say about feelings is private, but some things, like suicidal thinking, must be reported to the treatment team.” d. “It sounds as though you are not really ready to work on your problems and make changes.” ANS: C Adolescents are very concerned with confidentiality. The patient has a right to know that most information will be held in confidence but that certain material must be reported or shared with the treatment team, such as threats of suicide, homicide, use of illegal drugs, or issues of abuse. The incorrect responses are not true, will not inspire the confidence of the patient, or are confrontational. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 7-7 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 17. A nurse wants to assess an adult patient’s recent memory. Which question would best yield the desired information? a. “Where did you go to elementary school?” b. “What did you have for breakfast this morning?” c. “Can you name the current president of the United States?” d. “A few minutes ago, I told you my name. Can you remember it?” ANS: B The patient’s recall of a meal provides evidence of recent memory. Two incorrect responses are useful to assess immediate and remote memory. The other distracter assesses the patient’s fund of knowledge. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 7-47 (Box 7-4) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment 18. When a nurse assesses an older adult patient, answers seem vague or unrelated to the questions. The patient also leans forward and frowns, listening intently to the nurse. An appropriate question for the nurse to ask would be a. “Are you having difficulty hearing when I speak?” b. “How can I make this assessment interview easier for you?” c. “I notice you are frowning. Are you feeling annoyed with me?” d. “You’re having trouble focusing on what I’m saying. What is distracting you?” ANS: A The patient’s behaviors may indicate difficulty hearing. Identifying any physical need, the patient may have at the onset of the interview and making accommodations are important considerations. By asking if the patient is annoyed, the nurse is jumping to conclusions. Asking how to make the interview easier for the patient may not elicit a concrete answer. Asking about distractions is a way of asking about auditory hallucinations, which is not appropriate because the nurse has observed that the patient seems to be listening intently. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-7, 8 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 19. At what point in an assessment interview would a nurse ask, “How does your faith help you in stressful situations?” During the assessment of a. childhood growth and development b. substance use and abuse c. educational background d. coping strategies ANS: D When discussing coping strategies, the nurse might ask what the patient does when upset, what usually relieves stress, and to whom the patient goes to talk about problems. The question regarding whether the patient’s faith helps deal with stress fits well here. It would be out of place if introduced during exploration of the other topics. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-12, 13, 49 (Box 7-5) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 20. When a new patient is hospitalized, a nurse takes the patient on a tour, explains rules of the unit, and discusses the daily schedule. The nurse is engaged in a. counseling. b. health teaching. c. milieu management. d. psychobiological intervention. ANS: C Milieu management provides a therapeutic environment in which the patient can feel comfortable and safe while engaging in activities that meet the patient’s physical and mental health needs. Counseling refers to activities designed to promote problem solving and enhanced coping and includes interviewing, crisis intervention, stress management, and conflict resolution. Health teaching involves identifying health education needs and giving information about these needs. Psychobiological interventions involve medication administration and monitoring response to medications. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 7-22, 23 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 21. After formulating the nursing diagnoses for a new patient, what is a nurse’s next action? a. Designing interventions to include in the plan of care b. Determining the goals and outcome criteria c. Implementing the nursing plan of care d. Completing the spiritual assessment ANS: B The third step of the nursing process is planning and outcome identification. Outcomes cannot be determined until the nursing assessment is complete and nursing diagnoses have been formulated. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 7-18, 19, 33 (Figure 7-1) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 22. Select the most appropriate label to complete this nursing diagnosis: related to feelings of shyness and poorly developed social skills as evidenced by watching television alone at home every evening. a. Deficient knowledge b. Ineffective coping c. Social isolation d. Powerlessness ANS: C Nursing diagnoses are selected based on the etiological factors and assessment findings, or evidence. In this instance, the evidence shows social isolation that is caused by shyness and poorly developed social skills. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-16, 17 TOP: Nursing Process: Diagnosis/Analysis MSC: Client Needs: Psychosocial Integrity 23. “QSEN” refers to a. Qualitative Standardized Excellence in Nursing. b. Quality and Safety Education for Nurses. c. Quantitative Effectiveness in Nursing. d. Quick Standards Essential for Nurses. ANS: B QSEN represents national initiatives centered on patient safety and quality. The primary goal of QSEN is to prepare future nurses with the knowledge, skills, and attitudes to increase the quality, care, and safety in the health care setting in which they work. PTS: 1 DIF: REF: Page 7-42 (Box 7-1) Cognitive Level: Remember (Knowledge) TOP: Nursing Process: N/A MSC: Client Needs: Safe, Effective Care Environment 24. A nurse documents: “Patient is mute despite repeated efforts to elicit speech. Makes no eye contact. Inattentive to staff. Gazes off to the side or looks upward rather than at speaker.” Which nursing diagnosis should be considered? a. Defensive coping b. Decisional conflict c. Risk for other-directed violence d. Impaired verbal communication ANS: D The defining characteristics are more related to the nursing diagnosis of impaired verbal communication than to the other nursing diagnoses. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-16, 17 TOP: Nursing Process: Diagnosis/Analysis MSC: Client Needs: Psychosocial Integrity 25. A nurse prepares to assess a new patient who moved to the United States from Central America 3 years ago. After introductions, what is the nurse’s next comment? a. “How did you get to the United States?” b. “Would you like for a family member to help you talk with me?” c. “An interpreter is available. Would you like for me to make a request for these services?” d. “Are you comfortable conversing in English, or would you prefer to have a translator present?” ANS: D The nurse should determine whether a translator is needed by first assessing the patient for language barriers. Accuracy of the assessment depends on the ability to communicate in a language that is familiar to the patient. Family members are not always reliable translators. An interpreter may change the patient’s responses; a translator is a better resource. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 7-8, 9 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 26. The nurse records this entry in a patient’s progress notes: Patient escorted to unit by ER nurse at 2130. Patient’s clothing was dirty. In interview room, patient sat with hands over face, sobbing softly. Did not acknowledge nurse or reply to questions. After several minutes, abruptly arose, ran to window, and pounded. Shouted repeatedly, “Let me out of here.” Verbal intervention unsuccessful. Order for stat dose 2 mg haloperidol PO obtained; medication administered at 2150. By 2215, patient stopped shouting and returned to sit wordlessly in chair. Patient placed on one-to-one observation. How should this documentation be evaluated? a. Uses unapproved abbreviations b. Contains subjective material c. Too brief to be of value d. Excessively wordy e. Meets standards ANS: E This narrative note describes patient appearance, behavior, and conversation. It mentions that less-restrictive measures were attempted before administering medication and documents patient response to medication. This note would probably meet standards. A complete nursing assessment would be in order as soon as the patient is able to participate. Subjective material is absent from the note. Abbreviations are acceptable. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: TOP: Pages 7-24, 25, 40 (Table 7-4), 51 (Box 7-6) Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment MULTIPLE RESPONSE 1. A nurse assessed a patient who reluctantly participated in activities, answered questions with minimal responses, and rarely made eye contact. What information should be included when documenting the assessment? (Select all that apply.) a. The patient was uncooperative b. The patient’s subjective responses c. Only data obtained from the patient’s verbal responses d. A description of the patient’s behavior during the interview e. Analysis of why the patient was unresponsive during the interview ANS: B, D Both content and process of the interview should be documented. Providing only the patient’s verbal responses would create a skewed picture of the patient. Writing that the patient was uncooperative is subjectively worded. An objective description of patient behavior would be preferable. Analysis of the reasons for the patient’s behavior would be speculation, which is inappropriate. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-24, 25, 40 (Table 7-4), 51 (Box 7-6) TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 2. A nurse performing an assessment interview for a patient with a substance use disorder decides to use a standardized rating scale. Which scales are appropriate? (Select all that apply.) a. Addiction Severity Index (ASI) b. Brief Drug Abuse Screen Test (B-DAST) c. Abnormal Involuntary Movement Scale (AIMS) d. Cognitive Capacity Screening Examination (CCSE) e. Recovery Attitude and Treatment Evaluator (RAATE) ANS: A, B, E Standardized scales are useful for obtaining data about substance use disorders. The ASI, B-DAST, and RAATE are scales related to substance abuse. AIMS assesses involuntary movements associated with antipsychotic medications. The CCSE assesses cognitive function. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 7-15, 34 (Table 7-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 3. What information is conveyed by nursing diagnoses? (Select all that apply.) a. Medical judgments about the disorder b. Unmet patient needs currently present c. Goals and outcomes for the plan of care d. Supporting data that validate the diagnoses e. Probable causes that will be targets for nursing interventions ANS: B, D, E Nursing diagnoses focus on phenomena of concern to nurses rather than on medical diagnoses. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 7-16, 17 TOP: Nursing Process: Diagnosis/Analysis MSC: Client Needs: Safe, Effective Care Environment 4. A patient is very suspicious and states, “The FBI has me under surveillance.” Which strategies should a nurse use when gathering initial assessment data about this patient? (Select all that apply.) a. Tell the patient that medication will help this type of thinking. b. Ask the patient, “Tell me about the problem as you see it.” c. Seek information about when the problem began. d. Tell the patient, “Your ideas are not realistic.” e. Reassure the patient, “You are safe here.” Chapter 08: Therapeutic Relationships Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. A nurse assesses a confused older adult. The nurse experiences sadness and reflects, “This patient is like one of my grandparents … so helpless.” Which response is the nurse demonstrating? a. Transference b. Countertransference c. Catastrophic reaction d. Defensive coping reaction ANS: B Countertransference is the nurse’s transference or response to a patient that is based on the nurse’s unconscious needs, conflicts, problems, or view of the world. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-10 to 12, 35 (Table 8-2) TOP: MSC: Client Needs: Psychosocial Integrity Nursing Process: Assessment 2. Which statement shows a nurse has empathy for a patient who made a suicide attempt? a. “You must have been very upset when you tried to hurt yourself.” b. “It makes me sad to see you going through such a difficult experience.” c. “If you tell me what is troubling you, I can help you solve your problems.” d. “Suicide is a drastic solution to a problem that may not be such a serious matter.” ANS: A Empathy permits the nurse to see an event from the patient’s perspective, understand the patient’s feelings, and communicate this to the patient. The incorrect responses are nurse-centered (focusing on the nurse’s feelings rather than the patient’s), belittling, and sympathetic. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 8-22, 23 TOP: Nursing Process: Evaluation Client Needs: Psychosocial Integrity 3. After several therapeutic encounters with a patient who recently attempted suicide, which occurrence should cause the nurse to consider the possibility of countertransference? a. The patient’s reactions toward the nurse seem realistic and appropriate. b. The patient states, “Talking to you feels like talking to my parents.” c. The nurse feels unusually happy when the patient’s mood begins to lift. d. The nurse develops a trusting relationship with the patient. Strong positive or negative reactions toward a patient or over-identification with the patient indicate possible countertransference. Nurses must carefully monitor their own feelings and reactions to detect countertransference and then seek supervision. Realistic and appropriate reactions from a patient toward a nurse are desirable. One incorrect response suggests transference. A trusting relationship with the patient is desirable. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-10 to 12, 35 (Table 8-2) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 4. A patient says, “Please don’t share information about me with the other people.” How should the nurse respond? a. “I will not share information with your family or friends without your permission, but I will share information about you with other staff.” b. “A therapeutic relationship is just between the nurse and the patient. It is up to you to tell others what you want them to know.” c. “It depends on what you choose to tell me. I will be glad to disclose at the end of each session what I will report to others.” d. “I cannot tell anyone about you. It will be as though I am talking about my own problems, and we can help each other by keeping it between us.” ANS: A A patient has the right to know with whom the nurse will share information and that confidentiality will be protected. Although the relationship is primarily between the nurse and patient, other staff needs to know pertinent data. The other incorrect responses promote incomplete disclosure on the part of the patient, require daily renegotiation of an issue that should be resolved as the nurse–patient contract is established, and suggest mutual problem solving. The relationship must be patient centered. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-18, 19 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 5. A nurse is talking with a patient, and 5 minutes remain in the session. The patient has been silent most of the session. Another patient comes to the door of the room, interrupts, and says to the nurse, “I really need to talk to you.” The nurse should a. invite the interrupting patient to join in the session with the current patient. b. say to the interrupting patient, “I am not available to talk with you at the present time.” c. end the unproductive session with the current patient and spend time with the interrupting patient. d. tell the interrupting patient, “This session is 5 more minutes; then I will talk with you.” When a specific duration for sessions has been set, the nurse must adhere to the schedule. Leaving the first patient would be equivalent to abandonment and would destroy any trust the patient had in the nurse. Adhering to the contract demonstrates that the nurse can be trusted and that the patient and the sessions are important. The incorrect responses preserve the nurse–patient relationship with the silent patient but may seem abrupt to the interrupting patient, abandon the silent patient, or fail to observe the contract with the silent patient. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-18, 19, 35 (Table 8-2) | Page 8-39 (Table 8-3) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 6. Termination of a therapeutic nurse–patient relationship has been successful when the nurse a. avoids upsetting the patient by shifting focus to other patients before the discharge. b. gives the patient a personal telephone number and permission to call after discharge. c. discusses with the patient changes that happened during the relationship and evaluates outcomes. d. offers to meet the patient for coffee and conversation three times a week after discharge. ANS: C Summarizing and evaluating progress help validate the experience for the patient and the nurse and facilitate closure. Termination must be discussed; avoiding discussion by spending little time with the patient promotes feelings of abandonment. Successful termination requires that the relationship be brought to closure without the possibility of dependency-producing ongoing contact. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-20, 21 TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 7. What is the desirable outcome for the orientation stage of a nurse–patient relationship? The patient will demonstrate behaviors that indicate a. self-responsibility and autonomy. b. a greater sense of independence. c. rapport and trust with the nurse. d. resolved transference. ANS: C Development of rapport and trust is necessary before the relationship can progress to the working phase. Behaviors indicating a greater sense of independence, self-responsibility, and resolved transference occur in the working phase. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-17 to 19 TOP: Nursing Process: Outcomes Identification MSC: Client Needs: Psychosocial Integrity 8. During which phase of the nurse–patient relationship can the nurse anticipate that identified patient issues will be explored and resolved? a. Preorientation b. Orientation c. Working d. Termination ANS: C During the working phase, the nurse strives to assist the patient in making connections among dysfunctional behaviors, thinking, and emotions and offers support while alternative coping behaviors are tried. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-19, 20 TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 9. At what point in the nurse–patient relationship should a nurse plan to first address termination? a. During the orientation phase b. At the end of the working phase c. Near the beginning of the termination phase d. When the patient initially brings up the topic ANS: A The patient has a right to know the conditions of the nurse–patient relationship. If the relationship is to be time-limited, the patient should be informed of the number of sessions. If it is open-ended, the termination date will not be known at the outset, and the patient should know that the issue will be negotiated at a later date. The nurse is responsible for bringing up the topic of termination early in the relationship, usually during the orientation phase. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-17, 18 MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Implementation 10. A nurse introduces the matter of a contract during the first session with a new patient because contracts a. specify what the nurse will do for the patient. b. spell out the participation and responsibilities of each party. c. indicate the feeling tone established between the participants. d. are binding and prevent either party from prematurely ending the relationship. ANS: B A contract emphasizes that the nurse works with the patient rather than doing something for the patient. “Working with” is a process that suggests each party is expected to participate and share responsibility for outcomes. Contracts do not, however, stipulate roles or feeling tone, and premature termination is forbidden. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-17 to 19 TOP: Nursing Process: Planning MSC: Client Needs: Safe, Effective Care Environment 11. As a nurse escorts a patient being discharged after treatment for major depression, the patient gives the nurse a necklace with a heart pendant and says, “Thank you for helping mend my broken heart.” Which is the nurse’s best response? a. “Accepting gifts violates the policies and procedures of the facility.” b. “I’m glad you feel so much better now. Thank you for the beautiful necklace.” c. “I’m glad I could help you, but I can’t accept the gift. My reward is seeing you with a renewed sense of hope.” d. “Helping people is what nursing is all about. It’s rewarding to me when patients recognize how hard we work.” ANS: C Accepting a gift creates a social rather than therapeutic relationship with the patient and blurs the boundaries of the relationship. A caring nurse will acknowledge the patient’s gesture of appreciation, but the gift should not be accepted. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-4 to 6, 34 (Table 8-1) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 12. Which remark by a patient indicates passage from orientation to the working phase of a nurse–patient relationship? a. “I don’t have any problems.” b. “It is so difficult for me to talk about problems.” c. “I don’t know how it will help to talk to you about my problems.” d. “I want to find a way to deal with my anger without becoming violent.” ANS: D Thinking about a more constructive approach to dealing with anger indicates a readiness to make a behavioral change. Behavioral change is associated with the working phase of the relationship. Denial is often seen in the orientation phase. It is common early in the relationship, before rapport and trust are firmly established, for a patient to express difficulty in talking about problems. Stating skepticism about the effectiveness of the nurse–patient relationship is more typically a reaction during the orientation phase. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: MSC: Pages 8-18, 19 TOP: Nursing Process: Evaluation Client Needs: Safe, Effective Care Environment 13. A nurse explains to the family of a mentally ill patient how a nurse–patient relationship differs from social relationships. Which is the best explanation? a. “The focus is on the patient. Problems are discussed by the nurse and patient, but solutions are implemented by the patient.” b. “The focus shifts from nurse to patient as the relationship develops. Advice is given by both, and solutions are implemented.” c. “The focus of the relationship is socialization. Mutual needs are met, and feelings are shared openly.” d. “The focus is creation of a partnership in which each member is concerned with growth and satisfaction of the other.” ANS: A Only the correct response describes elements of a therapeutic relationship. The remaining responses describe events that occur in social or intimate relationships. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-4 to 6 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 14. A nurse wants to demonstrate genuineness with a patient diagnosed with schizophrenia. The nurse should a. restate what the patient says. b. use congruent communication strategies. c. use self-revelation in patient interactions. d. consistently interpret the patient’s behaviors. ANS: B Genuineness is a desirable characteristic involving awareness of one’s own feelings as they arise and the ability to communicate them when appropriate. The incorrect options are undesirable in a therapeutic relationship. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 8-22 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 15. A nurse caring for a withdrawn, suspicious patient recognizes development of feelings of anger toward the patient. The nurse should a. suppress the angry feelings. b. express the anger openly and directly with the patient. c. tell the nurse manager to assign the patient to another nurse. d. discuss the anger with a clinician during a supervisory session. ANS: D The nurse is accountable for the relationship. Objectivity is threatened by strong positive or negative feelings toward a patient. Supervision is necessary to work through countertransference feelings. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 8-10 to 12 TOP: Nursing Process: Evaluation Client Needs: Psychosocial Integrity 16. A nurse wants to enhance growth of a patient by showing positive regard. The nurse’s action most likely to achieve this goal is a. making rounds daily. b. staying with a tearful patient. c. administering medication as prescribed. d. examining personal feelings about a patient. ANS: B Staying with a crying patient offers support and shows positive regard. Administering daily medication and making rounds are tasks that could be part of an assignment and do not necessarily reflect positive regard. Examining feelings regarding a patient addresses the nurse’s ability to be therapeutic. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 8-10 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 17. A patient says, “I’ve done a lot of cheating and manipulating in my relationships.” Select a nonjudgmental response by the nurse. a. “How do you feel about that?” b. “I am glad that you realize this.” c. “That’s not a good way to behave.” d. “Have you outgrown that type of behavior?” ANS: A Asking a patient to reflect on feelings about his or her actions does not imply any judgment about those actions, and it encourages the patient to explore feelings and values. The remaining options offer negative judgments. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 8-10 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 18. A patient says, “People should be allowed to commit suicide without interference from others.” A nurse replies, “You’re wrong. Nothing is bad enough to justify death.” What is the best analysis of this interchange? a. The patient is correct. b. The nurse is correct. c. Neither person is correct. d. Differing values are reflected in the two statements. ANS: D Values guide beliefs and actions. The individuals stating their positions place different values on life and autonomy. Nurses must be aware of their own values and be sensitive to the values of others. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: MSC: Page 8-10 TOP: Nursing Process: Evaluation Client Needs: Psychosocial Integrity 19. Which issues should a nurse address during the first interview with a patient with a psychiatric disorder? a. Trust, congruence, attitudes, and boundaries b. Goals, resistance, unconscious motivations, and diversion c. Relationship parameters, the contract, confidentiality, and termination d. Transference, countertransference, intimacy, and developing resources ANS: C Relationship parameters, the contract, confidentiality, and termination are issues that should be considered during the orientation phase of the relationship. The remaining options are issues that are dealt with later. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 8-18, 19 TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 20. An advanced practice nurse observes a novice nurse expressing irritability regarding a patient with a long history of alcoholism and suspects the new nurse is experiencing countertransference. Which comment by the new nurse confirms this suspicion? a. “This patient continues to deny problems resulting from drinking.” b. “My parents were alcoholics and often neglected our family.” c. “The patient cannot identify any goals for improvement.” d. “The patient said I have many traits like her mother.” ANS: B Countertransference occurs when the nurse unconsciously and inappropriately displaces onto the patient feelings and behaviors related to significant figures in the nurse's past. In this instance, the new nurse’s irritability stems from relationships with parents. The distracters indicate transference or accurate analysis of the patient’s behavior. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 8-10 to 12, 34 (Table 8-1) | Page 8-35 (Table 8-2) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 21. Which behavior shows that a nurse values autonomy? The nurse a. suggests one-on-one supervision for a patient who has suicidal thoughts. b. informs a patient that the spouse will not be in during visiting hours. c. discusses options and helps the patient weigh the consequences. d. sets limits on a patient’s romantic overtures toward the nurse. ANS: C A high level of valuing is acting on one’s belief. Autonomy is supported when the nurse helps a patient weigh alternatives and their consequences before the patient makes a decision. Autonomy or self-determination is not the issue in any of the other behaviors. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 8-6, 7, 16 TOP: Nursing Process: Evaluation Client Needs: Safe, Effective Care Environment 22. As a nurse discharges a patient, the patient gives the nurse a card of appreciation made in an arts and crafts group. What is the nurse’s best action? a. Recognize the effectiveness of the relationship and patient’s thoughtfulness. Accept the card. b. Inform the patient that accepting gifts violates policies of the facility. Decline the card. c. Acknowledge the patient’s transition through the termination phase but decline the card. d. Accept the card and invite the patient to return to participate in other arts and crafts groups. ANS: A The nurse must consider the meaning, timing, and value of the gift. In this instance, the nurse should accept the patient’s expression of gratitude. See relationship to audience response question. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-24, 34 (Table 8-1) TOP: Nursing Process: Evaluation MSC: Client Needs: Safe, Effective Care Environment 23. A patient says, “I’m still on restriction, but I want to attend some off-unit activities. Would you ask the doctor to change my privileges?” What is the nurse’s best response? a. “Why are you asking me when you’re able to speak for yourself?” b. “I will be glad to address it when I see your doctor later today.” c. “That’s a good topic for you to discuss with your doctor.” d. “Do you think you can’t speak to a doctor?” ANS: C Nurses should encourage patients to work at their optimal level of functioning, which in turn promotes autonomy. A nurse does not act for the patient unless it is necessary. Acting for a patient increases feelings of helplessness and dependency. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-6, 7, 16, 34 (Table 8-1) TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 24. A community mental health nurse has worked with a patient for 3 years but is moving out of the city and terminates the relationship. When a novice nurse begins work with this patient, what is the starting point for the relationship? a. Begin at the orientation phase. b. Resume the working relationship. c. Initially establish a social relationship. d. Return to the emotional catharsis phase. ANS: A After termination of a long-term relationship, the patient and new nurse usually have to begin at ground zero, the orientation phase, to build a new relationship. If termination is successfully completed, the orientation phase sometimes progresses quickly to the working phase. Other times, even after successful termination, the orientation phase may be prolonged. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-17, 18 TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 25. As a patient diagnosed with a mental illness is being discharged from a facility, a nurse invites the patient to the annual staff picnic. What is the best analysis of this scenario? a. The invitation facilitates dependency on the nurse. b. The nurse’s action blurs the boundaries of the therapeutic relationship. c. The invitation is therapeutic for the patient’s diversional activity deficit. d. The nurse’s action assists the patient’s integration into community living. ANS: B The invitation creates a social relationship rather than a therapeutic relationship. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 8-9, 10, 34 (Table 8-1) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 26. A nurse says, “I am the only one who truly understands this patient. Other staff members are too critical.” The nurse’s statement indicates a. boundary blurring. b. sexual harassment. c. positive regard. d. advocacy. ANS: A When the role of the nurse and the role of the patient shift, boundary blurring may arise. In this situation the nurse is becoming overinvolved with the patient as a probable result of unrecognized countertransference. When boundary issues occur, the need for supervision exists. The situation does not describe sexual harassment. Data are not present to suggest positive regard or advocacy. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-10 to 12, 34 (Table 8-1) | Page 8-35 (Table 8-2) TOP: Nursing Process: Assessment MSC: Client Needs: Safe, Effective Care Environment 27. Which comment best indicates that a patient perceived the nurse was caring? “My nurse a. always asks me which type of juice I want to help me swallow my medication.” b. explained my treatment plan to me and asked for my ideas about how to make it better.” c. spends time listening to me talk about my problems. That helps me feel like I am not alone.” d. told me that if I take all the medicines the doctor prescribes, then I will get discharged sooner.” ANS: C Caring evidences empathetic understanding as well as competency. It helps change pain and suffering into a shared experience, creating a human connection that alleviates feelings of isolation. The distracters give examples of statements that demonstrate advocacy or giving advice. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-2, 24 TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity MULTIPLE RESPONSE 1. A nurse ends a relationship with a patient. Which actions by the nurse should be included in the termination phase? (Select all that apply.) a. Focus dialogues with the patient on problems that may occur in the future. b. Help the patient express feelings about the relationship with the nurse. c. Help the patient prioritize and modify socially unacceptable behaviors. d. Reinforce expectations regarding the parameters of the relationship. e. Help the patient to identify strengths, limitations, and problems. ANS: A, B The correct actions are part of the termination phase. The other actions would be used in the working and orientation phases. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-20, 21 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 2. A novice psychiatric nurse has a parent diagnosed with bipolar disorder. This nurse angrily recalls feelings of embarrassment about the parent’s behavior in the community. Select the best ways for this nurse to cope with these feelings. (Select all that apply.) a. Seek ways to use the understanding gained from childhood to help patients cope with their own illnesses. b. Recognize that these feelings are unhealthy. The nurse should try to suppress them when working with patients. c. Recognize that psychiatric nursing is not an appropriate career choice. Explore other nursing specialties. d. The nurse should begin new patient relationships by saying, “My own parent had mental illness, so I accept it without stigma.” e. Recognize that the feelings may add sensitivity to the nurse’s practice, but supervision is important. ANS: A, E The nurse needs support to explore these feelings. An experienced psychiatric nurse is a resource that may be helpful. The knowledge and experience gained from the nurse’s relationship with a mentally ill parent may contribute sensitivity to compassionate practice. Self-disclosure and suppression are not adaptive coping strategies. The nurse should not give up on this area of practice without first seeking ways to cope with the memories. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 8-6, 7, 9, 13 TOP: Nursing Process: Implementation Client Needs: Psychosocial Integrity 3. A novice nurse tells a mentor, “I want to convey to my patients that I am interested in them and that I want to listen to what they have to say.” Which behaviors will be helpful in meeting the nurse’s goal? (Select all that apply.) a. Sitting behind a desk, facing the patient b. Introducing self to a patient and identifying own role c. Maintaining control of discussions by asking direct questions d. Using facial expressions to convey interest and encouragement e. Assuming an open body posture and sometimes mirror imaging ANS: B, D, E Trust is fostered when the nurse gives an introduction and identifies his or her role. Facial expressions that convey interest and encouragement support the nurse’s verbal statements to that effect and strengthen the message. An open body posture conveys openness to listening to what the patient has to say. Mirror imaging enhances patient comfort. A desk would place a physical barrier between the nurse and patient. A face-to-face stance should be avoided when possible and a less intense 90- or 120-degree angle used to permit either party to look away without discomfort. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 8-25, 26 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity Chapter 09: Therapeutic Communication Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. A patient says to the nurse, “I dreamed I was stoned. When I woke up, I felt emotionally drained, as though I hadn’t rested well.” Which response should the nurse use to clarify the patient’s comment? a. “It sounds as though you were uncomfortable with the content of your dream.” b. “I understand what you’re saying. Bad dreams leave me feeling tired, too.” c. “So you feel as though you did not get enough quality sleep last night?” d. “Can you give me an example of what you mean by ‘stoned’?” ANS: D The technique of clarification is therapeutic and helps the nurse examine the meaning of the patient’s statement. Asking for a definition of “stoned” directly asks for clarification. Restating that the patient is uncomfortable with the dream’s content is parroting, a nontherapeutic technique. The other responses fail to clarify the meaning of the patient’s comment. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 9-47 (Table 9-2) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Implementation 2. A patient diagnosed with schizophrenia tells the nurse, “The Central Intelligence Agency is monitoring us through the fluorescent lights in this room. The CIA is everywhere, so be careful what you say.” Which response by the nurse is most therapeutic? a. “Let’s talk about something other than the CIA.” b. “It sounds like you’re concerned about your privacy.” c. “The CIA is prohibited from operating in health care facilities.” d. “You have lost touch with reality, which is a symptom of your illness.” ANS: B It is important not to challenge the patient’s beliefs, even if they are unrealistic. Challenging undermines the patient’s trust in the nurse. The nurse should try to understand the underlying feelings or thoughts the patient’s message conveys. The correct response uses the therapeutic technique of reflection. The other comments are nontherapeutic. Asking to talk about something other than the concern at hand is changing the subject. Saying that the CIA is prohibited from operating in health care facilities gives false reassurance. Stating that the patient has lost touch with reality is truthful, but uncompassionate. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-14, 15, 47 (Table 9-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 3. The patient says, “My marriage is just great. My spouse and I always agree.” The nurse observes the patient’s foot moving continuously as the patient twirls a shirt button. The conclusion the nurse can draw is that the patient’s communication is a. clear. b. distorted. c. incongruous. d. inadequate. ANS: B The patient’s verbal and nonverbal communication in this scenario are incongruous. Incongruous messages involve transmission of conflicting messages by the speaker. The patient’s verbal message that all was well in the relationship was modified by the nonverbal behaviors denoting anxiety. Data are not present to support the choice of the verbal message being clear, explicit, or inadequate. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-9, 10 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 4. A nurse interacts with a newly hospitalized patient. Select the nurse’s comment that applies the communication technique of “offering self.” a. “I’ve also had traumatic life experiences. Maybe it would help if I told you about them.” b. “Why do you think you had so much difficulty adjusting to this change in your life?” c. “I hope you will feel better after getting accustomed to how this unit operates.” d. “I’d like to sit with you for a while to help you get comfortable talking to me.” ANS: D “Offering self” is a technique that should be used in the orientation phase of the nurse–patient relationship. Sitting with the patient, an example of “offering self,” helps to build trust and convey that the nurse cares about the patient. Two incorrect responses are ineffective and nontherapeutic. The other incorrect response is therapeutic but is an example of “offering hope.” PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-47 (Table 9-2), 58 (Table 9-4) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 5. Which technique will best communicate to a patient that the nurse is interested in listening? a. Restating a feeling or thought the patient has expressed. b. Asking a direct question, such as “Did you feel angry?” c. Making a judgment about the patient’s problem. d. Saying, “I understand what you’re saying.” ANS: A Restating allows the patient to validate the nurse’s understanding of what has been communicated. Restating is an active listening technique. Judgments should be suspended in a nurse–patient relationship. Close-ended questions such as “Did you feel angry?” ask for specific information rather than showing understanding. When the nurse simply states that he or she understands the patient’s words, the patient has no way of measuring the understanding. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-14, 47 (Table 9-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 6. A patient discloses several concerns and associated feelings. If the nurse wants to seek clarification, which comment would be appropriate? a. “What are the common elements here?” b. “Tell me again about your experiences.” c. “Am I correct in understanding that.” d. “Tell me everything from the beginning.” ANS: C Asking, “Am I correct in understanding that …” permits clarification to ensure that both the nurse and patient share mutual understanding of the communication. Asking about common elements encourages comparison rather than clarification. The remaining responses are implied questions that suggest the nurse was not listening. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 9-47 (Table 9-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 7. A patient tells the nurse, “I don’t think I’ll ever get out of here.” Select the nurse’s most therapeutic response. a. “Don’t talk that way. Of course you will leave here!” b. “Keep up the good work, and you certainly will.” c. “You don’t think you’re making progress?” d. “Everyone feels that way sometimes.” ANS: C By asking if the patient does not believe that progress has been made, the nurse is reflecting or paraphrasing by putting into words what the patient is hinting. By making communication more explicit, issues are easier to identify and resolve. The remaining options are nontherapeutic techniques. Telling the patient not to “talk that way” is disapproving. Saying that everyone feels that way at times minimizes feelings. Telling the patient that good work will always result in success is falsely reassuring. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 9-13, 14, 47 (Table 9-2) TOP: Nursing Process: Implementation Client Needs: Psychosocial Integrity 8. Documentation in a patient’s chart shows, “Throughout a 5-minute interaction, patient fidgeted and tapped left foot, periodically covered face with hands, and looked under chair while stating, ‘I enjoy spending time with you.’” Which analysis is most accurate? a. The patient is giving positive feedback about the nurse’s communication techniques. b. The nurse is viewing the patient’s behavior through a cultural filter. c. The patient’s verbal and nonverbal messages are incongruent. d. The patient is demonstrating psychotic behaviors. ANS: C When a verbal message is not reinforced with nonverbal behavior, the message is confusing and incongruent. It is inaccurate to say that the patient is giving positive feedback about the nurse’s communication techniques. The concept of a cultural filter is not relevant to the situation because a cultural filter determines what we will pay attention to and what we will ignore. Data are insufficient to draw the conclusion that the patient is demonstrating psychotic behaviors. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-9, 10 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 9. While talking with a patient diagnosed with major depressive disorder, a nurse notices the patient is unable to maintain eye contact. The patient’s chin lowers to the chest. The patient looks at the floor. Which aspect of communication has the nurse assessed? a. Nonverbal communication b. A message filter c. A cultural barrier d. Social skills ANS: A Eye contact and body movements are considered nonverbal communication. There are insufficient data to determine the level of the patient’s social skills or an existing cultural barrier. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-7, 8 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 10. During the first interview with a parent whose child died in a car accident, the nurse feels empathic and reaches out to take the patient’s hand. Select the correct analysis of the nurse’s behavior. a. It shows empathy and compassion. It will encourage the patient to continue to express feelings. b. The gesture is premature. The patient’s cultural and individual interpretation of touch is unknown. c. The patient will perceive the gesture as intrusive and overstepping boundaries. d. The action is inappropriate. Psychiatric patients should not be touched. ANS: B Touch has various cultural and individual interpretations. Nurses should refrain from using touch until an assessment is completed regarding the way in which the patient will perceive touch. The incorrect options present prematurely drawn conclusions. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-24, 25 TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 11. During a one-on-one interaction with the nurse, a patient frequently looks nervously at the door. Select the best comment by the nurse regarding this nonverbal communication. a. “I notice you keep looking toward the door.” b. “This is our time together. No one is going to interrupt us.” c. “It looks as if you are eager to end our discussion for today.” d. “If you are uncomfortable in this room, we can move someplace else.” ANS: A Making observations and encouraging the patient to describe perceptions are useful therapeutic communication techniques for this situation. The other responses are assumptions made by the nurse. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-47 (Table 9-2), 58 (Table 9-4) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 12. A black patient says to a white nurse, “There’s no sense talking about how I feel. You wouldn’t understand because you live in a white world.” The nurse’s best action would be to a. explain, “Yes, I do understand. Everyone goes through the same experiences.” b. say, “Please give an example of something you think I wouldn’t understand.” c. reassure the patient that nurses interact with people from all cultures. d. change the subject to one that is less emotionally disturbing. ANS: B Having the patient speak in specifics rather than globally will help the nurse understand the patient’s perspective. This approach will help the nurse engage the patient. Reassurance and changing the subject are not therapeutic techniques. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-47 (Table 9-2), 54 (Table 9-3) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 13. A Filipino American patient had a nursing diagnosis of situational low self-esteem related to poor social skills as evidenced by lack of eye contact. Interventions were applied to increase the patient’s self-esteem but after 3 weeks, the patient’s eye contact did not improve. What is the most accurate analysis of this scenario? a. The patient’s eye contact should have been directly addressed by role playing to increase comfort with eye contact. b. The nurse should not have independently embarked on assessment, diagnosis, and planning for this patient. c. The patient’s poor eye contact is indicative of anger and hostility that were unaddressed. d. The nurse should have assessed the patient’s culture before making this diagnosis and plan. ANS: D The amount of eye contact a person engages in is often culturally determined. In some cultures, eye contact is considered insolent, whereas in others eye contact is expected. Asian Americans, including persons from the Philippines, often prefer not to engage in direct eye contact. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 9-23, 24, 33, 34 TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 14. When a female Mexican American patient and a female nurse sit together, the patient often holds the nurse’s hand. The patient also links arms with the nurse when they walk. The nurse is uncomfortable with this behavior. Which analysis is most accurate? a. The patient is accustomed to touch during conversation, as are members of many Hispanic subcultures. b. The patient understands that touch makes the nurse uncomfortable and controls the relationship based on that factor. c. The patient is afraid of being alone. When touching the nurse, the patient is reassured and comforted. d. The patient is trying to manipulate the nurse using nonverbal techniques. ANS: A The most likely answer is that the patient’s behavior is culturally influenced. Hispanic women frequently touch women they consider to be their friends. Although the other options are possible, they are less likely. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-24, 25 TOP: MSC: Client Needs: Psychosocial Integrity Nursing Process: Assessment 15. A Puerto Rican American patient uses dramatic body language when describing emotional discomfort. Which analysis most likely explains the patient’s behavior? The patient a. has a histrionic personality disorder. b. believes dramatic body language is sexually appealing. c. wishes to impress staff with the degree of emotional pain. d. belongs to a culture in which dramatic body language is the norm. ANS: D Members of Hispanic American subcultures tend to use high affect and dramatic body language as they communicate. The other options are more remote possibilities. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-22, 23 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 16. During an interview, a patient attempts to shift the focus from self to the nurse by asking personal questions. The nurse should respond by saying: a. “Why do you keep asking about me?” b. “Nurses direct the interviews with patients.” c. “Do not ask questions about my personal life.” d. “The time we spend together is to discuss your concerns.” ANS: D When a patient tries to focus on the nurse, the nurse should refocus the discussion back onto the patient. Telling the patient that interview time should be used to discuss patient concerns refocuses discussion in a neutral way. Telling patients not to ask about the nurse’s personal life shows indignation. Saying that nurses prefer to direct the interview reflects superiority. “Why” questions are probing and nontherapeutic. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 9-47 (Table 9-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 17. Which principle should guide the nurse in determining the extent of silence to use during patient interview sessions? a. A nurse is responsible for breaking silences. b. Patients withdraw if silences are prolonged. c. Silence can provide meaningful moments for reflection. d. Silence helps patients know that what they said was understood. ANS: C Silence can be helpful to both participants by giving each an opportunity to contemplate what has transpired, weigh alternatives, and formulate ideas. A nurse breaking silences is not a principle related to silences. It is inaccurate to say that patients withdraw during long silences or that silence helps patients know that they are understood. Feedback helps patients know they have been understood. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-11, 12, 47 (Table 9-2) TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 18. A patient is having difficulty making a decision. The nurse has mixed feelings about whether to provide advice. Which principle usually applies? Giving advice a. is rarely helpful. b. fosters independence. c. lifts the burden of personal decision making. d. helps the patient develop feelings of personal adequacy. ANS: A Giving advice fosters dependence on the nurse and interferes with a patient’s right to make personal decisions. It robs the patient of the opportunity to weigh alternatives and develop problem-solving skills. Furthermore, it may contribute to a patient’s feelings of personal inadequacy. Giving advice also keeps the nurse in control and feeling powerful. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-20, 33, 54 (Table 9-3) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 19. A school age child tells the school nurse, “Other kids call me mean names and will not sit with me at lunch. Nobody likes me.” Select the nurse’s most therapeutic response. a. “Just ignore them and they will leave you alone.” b. “You should make friends with other children.” c. “Call them names if they do that to you.” d. “Tell me more about how you feel.” ANS: D The correct response uses exploring, a therapeutic technique. The distracters give advice, a nontherapeutic technique. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-15, 47 (Table 9-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 20. A patient with acute depression states, “God is punishing me for my past sins.” What is the nurse’s most therapeutic response? a. “You sound very upset about this.” b. “God always forgives us for our sins.” c. “Why do you think you are being punished?” d. “If you feel this way, you should talk to your minister.” ANS: A The nurse reflects the patient’s comment, a therapeutic technique to encourage sharing for perceptions and feelings. The incorrect responses reflect probing, closed-ended comments, and giving advice, all of which are nontherapeutic. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-10, 14, 15, 47 (Table 9-2) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Implementation MULTIPLE RESPONSE 1. A patient cries as the nurse explores the patient’s feelings about the death of a close friend. The patient sobs, “I shouldn’t be crying like this. It happened a long time ago.” Which responses by the nurse facilitate communication? (Select all that apply.) a. “Why do you think you are so upset?” b. “I can see that you feel sad about this situation.” c. “The loss of a close friend is very painful for you.” d. “Crying is a way of expressing the hurt you are experiencing.” e. “Let’s talk about something else because this subject is upsetting you.” ANS: B, C, D Reflecting (“I can see that you feel sad,” “This is very painful for you”) and giving information (“Crying is a way of expressing hurt”) are therapeutic techniques. “Why” questions often imply criticism or seem intrusive or judgmental. They are difficult to answer. Changing the subject is a barrier to communication. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 9-14, 15, 47 (Table 9-2) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 2. Which benefits are most associated with use of telehealth technologies? (Select all that apply.) a. Cost savings for patients b. Maximize care management c. Access to services for patients in rural areas d. Prompt reimbursement by third-party payers e. Rapid development of trusting relationships with patients ANS: A, B, C Telehealth has shown that it can maximize health and improve disease management skills and confidence with the disease process. Many rural parents have felt disconnected from services; telehealth technologies can solve those problems. Although telehealth’s improved health outcomes regularly show cost savings for payers, one significant barrier is the current lack of reimbursement for remote patient monitoring by third-party payers. Telehealth technologies have not shown rapid development of trusting relationships. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 9-26, 27 TOP: Nursing Process: Implementation MSC: Client Needs: Safe, Effective Care Environment 3. Which comments by a nurse demonstrate use of therapeutic communication techniques? (Select all that apply.) a. “Why do you think these events have happened to you?” b. “There are people with problems much worse than yours.” c. “I’m glad you were able to tell me how you felt about your loss.” d. “I noticed your hands trembling when you told me about your accident.” e. “You look very nice today. I’m proud you took more time with your appearance.” ANS: C, D The correct responses demonstrate use of the therapeutic techniques making an observation and showing empathy. The incorrect responses demonstrate minimizing feelings, probing, and giving approval, which are nontherapeutic techniques. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 9-47 (Table 9-2) | Page 9-54 (Table 9-3) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 4. A nurse interacts with patients diagnosed with various mental illnesses. Which statements reflect use of therapeutic communication? (Select all that apply.) a. “Tell me more about that situation.” b. “Let’s talk about something else.” c. “I notice you are pacing a lot.” d. “I’ll stay with you a while.” e. “Why did you do that?” ANS: A, C, D The correct responses demonstrate use of the therapeutic techniques making an observation and showing empathy. The incorrect responses demonstrate changing the subject and probing, which are nontherapeutic techniques. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 9-47 (Table 9-2) | Page 9-54 (Table 9-3) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity Chapter 10: Stress Responses and Stress Management Halter: Varcarolis’ Foundations of Psychiatric Mental Health Nursing: A Clinical Approach, 8th Edition MULTIPLE CHOICE 1. The adult child of a patient diagnosed with major depressive disorder asks, “Do you think depression and physical illness are connected? Since my father’s death, my mother has had shingles and the flu, but she’s usually not one who gets sick.” Which answer by the nurse best reflects current knowledge? a. “It is probably a coincidence. Emotions and physical responses travel on different tracts of the nervous system.” b. “You may be paying more attention to your mother since your father died and noticing more things such as minor illnesses.” c. “So far, research on emotions or stress and becoming ill more easily is unclear. We do not know for sure if there is a link.” d. “Negative emotions and prolonged stress interfere with the body’s ability to protect itself and can increase the likelihood of illness.” ANS: D The correct answer best explains the research. Research supports a link between negative emotions and/or prolonged stress and impaired immune system functioning. Activation of the immune system sends proinflammatory cytokines to the brain, and the brain in turn releases its own cytokines that signal the central nervous system to initiate myriad responses to stress. Prolonged stress suppresses the immune system and lowers resistance to illness. Although the adult child may be more aware of issues involving the mother, the pattern of illnesses described may be an increase from the mother’s baseline. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-7, 8 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. A patient diagnosed with emphysema has severe shortness of breath and needs portable oxygen when leaving home. Recently the patient has reduced activity because of fear that breathing difficulty will occur. A nurse suggests using guided imagery. Which image should the patient be encouraged to visualize? a. Engaging in activity without using any supplemental oxygen b. Sleeping comfortably and soundly, without respiratory distress c. Feeling relaxed and taking regular deep breaths when leaving home d. Having a younger, healthier body that knows no exercise limitations ANS: C The patient has dysfunctional images of dyspnea. Guided imagery can help replace the dysfunctional image with a positive coping image. Athletes have found that picturing successful images can enhance performance. Encouraging the patient to imagine a regular breathing depth and rate will help improve oxygen–carbon dioxide exchange and help achieve further relaxation. Other options focus on unrealistic goals (being younger, not needing supplemental oxygen) or restrict her quality of life. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-16, 40 (Box 10-3) TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 3. A nurse leads a psychoeducational group for patients experiencing depression. The nurse plans to implement an exercise regime for each patient. The rationale to use when presenting this plan to the treatment team is that exercise a. has an antidepressant effect comparable to selective serotonin reuptake inhibitors. b. prevents damage from overstimulation of the sympathetic nervous system. c. detoxifies the body by removing metabolic wastes and other toxins. d. improves mood stability for patients with bipolar disorders. ANS: A -Endorphins produced during exercise result in improvement in mood and lowered anxiety. The other options are not accurate. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 10-12, 19, 37 (Box 10-1) TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. A recent immigrant from Honduras comes to the clinic with a family member who has been a U.S. resident for 10 years. The family member says, “The immigration to America has been very difficult.” Considering cultural background, which expression of stress by this patient would the nurse expect? a. Motor restlessness b. Somatic complaints c. Memory deficiencies d. Sensory perceptual alterations ANS: B Honduras is in Central America. Many people from Central American cultures express distress in somatic terms. The other options are not specific to this patient’s cultural background and are less likely to be observed in persons from Central America. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 10-11 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 5. A patient nervously says, “Financial problems are stressing my marriage. I’ve heard rumors about cutbacks at work; I am afraid I might get laid off.” The patient’s pulse is 112/minute; respirations are 26/minute; and blood pressure is 166/88. Which nursing intervention will the nurse implement? a. Advise the patient, “Go to sleep 30 to 60 minutes earlier each night to increase rest.” b. Direct the patient in slow and deep breathing using abdominal muscles. c. Suggest the patient consider that a new job might be better than the present one. d. Tell the patient, “Relax by spending more time playing with your pet.” ANS: B The patient is responding to stress with increased arousal of the sympathetic nervous system, as evident by elevated vital signs. These will have a negative effect on his health and increase his perception of being anxious and stressed. Stimulating the parasympathetic nervous system will counter the sympathetic nervous system’s arousal, normalizing these vital sign changes and reducing the physiological demands stress is placing on his body. Other options do not address his physiological response pattern as directly or immediately. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-3, 4, 15, 16, 39 (Box 10-2) TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 6. According to the Recent Life Changes Questionnaire, which situation would most necessitate a complete assessment of a person’s stress status and coping abilities? a. A person who has been assigned more responsibility at work b. A parent whose job required relocation to a different city c. A person returning to college after an employer ceased operations d. A man who recently separated from his wife because of marital problems ANS: C A person returning to college after losing a job is dealing with two significant stressors simultaneously. Together, these stressors total more life change units than any of the single stressors cited in the other options. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 10-12, 13, 31 (Table 10-3) MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment 7. A patient newly diagnosed as HIV-positive seeks the nurse’s advice on how to reduce the risk of infections. The patient says, “I went to church years ago and I was in my best health then. Maybe I should start going to church again.” Which response will the nurse offer? a. “Religion does not usually affect health, but you were younger and stronger then.” b. “Contact with supportive people at a church might help, but religion itself is not especially helpful.” c. “Studies show that spiritual practices can enhance immune system function and coping abilities.” d. “Going to church would expose you to many potential infections. Let’s think about some other options.” ANS: C Studies have shown a positive correlation between spiritual practices and enhanced immune system function and sense of well-being. The other options wrongly suggest that spiritual practices have little effect on the immune system or reject the patient’s preferences regarding health management. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-11, 12 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 8. When a nurse asks a newly admitted patient to describe social supports, the patient says, “My parents died last year and I have no family. I am newly divorced, and my former in-laws blame me. I don’t have many friends because most people my age just want to go out drinking.” Which action will the nurse apply? a. Advise the patient that being so particular about potential friends reduces social contact. b. Suggest using the Internet as a way to find supportive others with similar values. c. Encourage the patient to begin dating again, perhaps with members of the church. d. Discuss how divorce support groups could increase coping and social support. ANS: D High-quality social support enhances mental and physical health and acts as a significant buffer against distress. Low-quality support relationships affect a person’s coping negatively. Resuming dating soon after a divorce could place additional stress on the patient rather than helping her cope with existing stressors. Developing relationships on the Internet probably would not substitute fully for direct contact with other humans and could expose her to predators misrepresenting themselves to take advantage of vulnerable persons. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-10, 11 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 9. A patient experiencing significant stress associated with a disturbing new medical diagnosis asks the nurse, “Do you think saying a prayer would help?” Select the nurse’s best answer. a. “It could be that prayer is your only hope.” b. “You may find prayer gives comfort and lowers your stress.” c. “I can help you feel calmer by teaching you meditation exercises.” d. “We do not have evidence that prayer helps, but it wouldn’t hurt.” ANS: B Many patients find that spiritual measures, including prayer, are helpful in mediating stress. Studies have shown that spiritual practices can enhance the sense of well-being. When a patient suggests a viable means of reducing stress, it should be supported by the nurse. Indicating that prayer is the patient’s only hope is pessimistic and would cause further distress. Suggesting meditation or other alternatives to prayer implies that the nurse does not think prayer would be effective. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: MSC: Pages 10-11, 12 TOP: Nursing Process: Implementation Client Needs: Psychosocial Integrity 10. A patient is brought to the Emergency Department after a motorcycle accident. The patient is alert, responsive, and diagnosed with a broken leg. The patient’s vital signs are pulse (P) 72 and respiration (R) 16. After being informed surgery is required for the broken leg, which vital sign readings would be expected? a. P 64, R 14 b. P 68, R 12 c. P 72, R 16 d. P 80, R 20 ANS: D The patient would experience stress associated with anticipation of surgery. In times of stress, the sympathetic nervous system takes over (fight or flight response) and sends signals to the adrenal glands, thereby releasing norepinephrine. The circulating norepinephrine increases the heart rate. Respirations increase, bringing more oxygen to the lungs. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 10-3, 4 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 11. A patient tells the nurse, “I know that I should reduce the stress in my life, but I have no idea where to start.” What would be the best initial nursing response? a. “Physical exercise works to elevate mood and reduce anxiety.” b. “Reading about stress and how to manage it might be a good place to start.” c. “Why not start by learning to meditate? That technique will cover everything.” d. “Let’s talk about what is going on in your life and then look at possible options.” ANS: D In this case, the nurse lacks information about what stressors the patient is coping with or about what coping skills are already possessed. Further assessment is indicated before potential solutions can be explored. Suggesting exploration of the stress facing the patient is the only option that involves further assessment rather than suggesting a particular intervention. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-12 to 14 MSC: Client Needs: Psychosocial Integrity TOP: Nursing Process: Assessment 12. A patient tells the nurse, “My doctor thinks my problems with stress relate to the negative way I think about things and suggested I learn new ways of thinking.” Which response by the nurse would support the recommendation? a. Encourage the patient to imagine being in calm circumstances. b. Provide the patient with a blank journal and guidance about journaling. c. Teach the patient to recognize, reconsider, and reframe irrational thoughts. d. Teach the patient to use instruments that give feedback about bodily functions. ANS: C Cognitive reframing focuses on recognizing and correcting maladaptive patterns of thinking that create stress or interfere with coping. Cognitive reframing involves recognizing the habit of thinking about a situation or issue in a fixed, irrational, and unquestioning manner. Helping the patient to recognize and reframe (reword) such thoughts so that they are realistic and accurate promotes coping and reduces stress. Thinking about being in calming circumstances is a form of guided imagery. Instruments that give feedback about bodily functions are used in biofeedback. Journaling is effective for helping to increase self-awareness. However, none of these last three interventions is likely to alter the patient’s manner of thinking. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-19, 20, 36 (Table 10-4) TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 13. A patient who had been experiencing significant stress learned to use progressive muscle relaxation and deep breathing exercises. When the patient returns to the clinic 2 weeks later, which finding most clearly shows the patient is coping more effectively with stress? a. The patient’s systolic blood pressure has changed from the 140s to the 120s mm Hg. b. The patient reports, “I feel better, and that things are not bothering me as much.” c. The patient reports, “I spend more time napping or sitting quietly at home.” d. The patient’s weight decreased by 3 pounds. ANS: A Objective measures tend to be the most reliable means of gauging progress. In this case, the patient’s elevated blood pressure, an indication of the body’s physiological response to stress, has diminished. The patient’s report regarding activity level is subjective; sitting quietly could reflect depression rather than improvement. Appetite, mood, and energy levels are also subjective reports that do not necessarily reflect physiological changes from stress and may not reflect improved coping with stress. The patient’s weight change could be a positive or negative indicator; the blood pressure change is the best answer. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 10-15, 16, 39 (Box 10-4) TOP: MSC: Client Needs: Psychosocial Integrity Nursing Process: Evaluation 14. A patient tells the nurse, “I will never be happy until I’m as successful as my older sister.” The nurse asks the patient to reassess this statement and reframe it. Which reframed statement by the patient is most likely to promote coping? a. “People should treat me as well as they treat my sister.” b. “I can find contentment in succeeding at my own job level.” c. “I won’t be happy until I make as much money as my sister.” d. “Being as smart or clever as my sister isn’t really important.” ANS: B Finding contentment within one’s own work, even when it does not involve success as others might define it, is likely to lead to a reduced sense of distress about achievement level. It speaks to finding satisfaction and happiness without measuring the self against another person. Focusing on salary is simply a more specific way of being as successful as the sister, which would not promote coping. Expecting others to treat her as they do her sister is beyond her control. Dismissing the sister’s cleverness as unimportant indicates that the patient continues to feel inferior to the sibling. PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: Pages 10-19, 20, 36 (Table 10-4) TOP: Nursing Process: Evaluation MSC: Client Needs: Psychosocial Integrity 15. A patient says, “One result of my chronic stress is that I feel so tired. I usually sleep from 11:00 PM to 6:30 AM. I started setting my alarm to give me an extra 30 minutes of sleep each morning, but I don’t feel any better and I’m rushed for work.” Which nursing response would best address the patient’s concerns? a. “You may need to speak to your doctor about taking a sedative to help you sleep.” b. “Perhaps going to bed a half-hour earlier would work better than sleeping later.” c. “A glass of wine in the evening might take the edge off and help you to rest.” d. “Exercising just before retiring for the night may help you to sleep better.” ANS: B Sleeping later in the morning may disturb circadian rhythms and in this case is adding, rather than reducing, stress. Going to bed earlier and arising at the usual time alleviates fatigue more effectively. Sedatives may offer some benefit but are a short-term intervention with potential side effects, and other nonpharmacological interventions might work as well or better. Exercise earlier in the evening could induce tiredness and ease the process of falling asleep, but doing so right before bedtime would stimulate and interfere with sleep. Alcohol is sedating but potentially addictive; encouraging its use could increase the risk of using alcohol maladaptively as a response to stress in general. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Page 10-37 (Box 10-1) TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 16. A patient reports, “I am overwhelmed by stress.” Which question by the nurse would be most important to use in the initial assessment of this patient? a. “Tell me about your family history. Do you have any relatives who have problems with stress?” b. “Tell me about your exercise. How much activity do you typically get in a day?” c. “Tell me about the kinds of things you do to reduce or cope with your stress.” d. “Stress can interfere with sleep. How much did you sleep last night?” ANS: C The most important data to collect during an initial assessment is that which reflects how stress is affecting the patient and how he is coping with stress at present. This data would indicate whether or not his distress is placing him in danger (e.g., by elevating his blood pressure dangerously or via maladaptive responses, such as drinking) and would help the nurse understand how he copes and how well his coping strategies and resources serve him. Of the choices presented, the highest priority would be to determine what he is doing to cope at present, preferably via an open-ended inquiry. Family history, the extent of his use of exercise, and how much sleep he is getting are all helpful but seek data that is less of a priority. Also, the manner in which such data is sought here is likely to provide only brief responses (e.g., how much sleep he got on one particular night is probably less important than how much he is sleeping in general). PTS: 1 DIF: Cognitive Level: Analyze (Analysis) REF: MSC: Pages 10-12 to 14 TOP: Nursing Process: Assessment Client Needs: Psychosocial Integrity 17. Which scenario best demonstrates an example of eustress? An individual a. loses a beloved family pet. b. prepares to take a vacation to a tropical island with a group of close friends. c. receives a bank notice that there were insufficient funds in his/her account for a recent rent payment. d. receives notification that his/her current employer is experiencing financial problems and some workers will be terminated. ANS: B Eustress is beneficial stress; it motivates people to develop skills they need to solve problems and meet personal goals. Positive life experiences produce eustress. Going on a tropical vacation is an exciting, relaxing experience and is an example of eustress. Losing the family pet, worrying about employment security, and having financial problems are examples of distress, a negative experience that drains energy and can lead to significant emotional problems. See related audience response question. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 10-6 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 18. A person with a fear of heights drives across a high bridge. Which structure will stimulate a response from the autonomic nervous system? a. Thalamus b. Parietal lobe c. Hypothalamus d. Pituitary gland ANS: C The individual will find this experience stressful. The hypothalamus functions as the command-and-control center when receiving stressful signals. The hypothalamus responds to signals of stress by engaging the autonomic nervous system. The parietal lobe is responsible for interpretation of other sensations. The thalamus processes messages associated with pain and wakefulness. The pituitary gland may be involved in other aspects of the person’s response but would not stimulate the autonomic nervous system. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Page 10-4 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 19. A person with a fear of heights drives across a high bridge. Which division of the autonomic nervous system will be stimulated in response to this experience? a. Limbic system b. Peripheral nervous system c. Sympathetic nervous system d. Parasympathetic nervous system ANS: C The autonomic nervous system is comprised of the sympathetic (fight or flight response) and parasympathetic nervous system (relaxation response). In times of stress, the sympathetic nervous system is stimulated. A person fearful of heights would experience stress associated with the experience of driving across a high bridge. The peripheral nervous system responds to messages from the sympathetic nervous system. The limbic system processes emotional responses but is not specifically part of the autonomic nervous system. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 10-3, 4 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity MULTIPLE RESPONSE 1. Which changes reflect short-term physiological responses to stress? (Select all that apply.) a. Muscular tension, blood pressure, and triglycerides increase. b. Epinephrine is released, increasing heart and respiratory rates. c. Corticosteroid release increases stamina and impedes digestion. d. Cortisol is released, increasing glucogenesis and reducing fluid loss. e. Immune system functioning decreases, and risk of cancer increases. f. Risk of depression, autoimmune disorders, and heart disease increases. ANS: A, B, C, D The correct answers are all short-term physiological responses to stress. Increased risk of immune system dysfunction, cancer, cardiovascular disease, depression, and autoimmune disease are all long-term (chronic) effects of stress. PTS: 1 DIF: Cognitive Level: Understand (Comprehension) REF: Pages 10-3 to 5, 8 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. Which comments by a nurse are likely to help a patient cope by addressing the mediators of the stress response? (Select all that apply.) a. “A divorce, while stressful, can be the beginning of a new, better phase of life.” b. “You mentioned your spirituality. Are there aspects of your faith that could be helpful to you at this time?” c. “Journaling often promotes awareness of how experiences have affected people.” d. “It seems to me you are overreacting to this change in your life.” e. “There is a support group for newly divorced persons in your neighborhood.” ANS: A, B, C, E Stress mediators are factors that can help persons cope by influencing how they perceive and respond to stressors; they include personality, social support, perceptions, and culture. Suggesting that a divorce may have positive as well as negative aspects helps the patient to alter perceptions of the stressor. Journaling increases self-awareness regarding how life experiences may have shaped how we perceive and respond to stress (or how our personality affects how we respond to stressors). A loan could help the patient by reducing the financial pressures. Participation in support groups is an excellent way to expand one’s support network relative to specific issues. Many persons derive comfort and support from participation in faith-based interventions. The incorrect response demonstrates judging, which is non-therapeutic communication by the nurse and would not facilitate coping. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-9 to 11, 13, 14, 19, 37 (Box 10-1) TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 3. The nurse wishes to use guided imagery to help a patient relax. Which comments would be appropriate to include in the guided imagery script? (Select all that apply.) a. “Imagine others treating you the way they should, the way you want to be treated …” b. “With each breath, you feel calmer, more relaxed, almost as if you are floating …” c. “You are alone on a beach, the sun is warm, and you hear only the sound of the surf …” d. “You have taken control, nothing can hurt you now. Everything is going your way …” e. “You have grown calm, your mind is still, there is nothing to disturb your well-being …” f. “You will feel better as work calms down, as your boss becomes more understanding …” ANS: B, C, E The intent of guided imagery to assist patients manage stress is to lead the patient to envision images that are calming and health-enhancing. Statements that involve the patient calming progressively with breathing, feeling increasingly relaxed, being in a calm and pleasant location, being away from stressors, and having a peaceful and calm mind are therapeutic and should be included in the script. However, items that raise stressful images or memories or that involve unrealistic expectations or elements beyond the patient’s control (e.g., that others will treat the patient as he desires, that everything is going the patient’s way, that bosses are understanding) interfere with relaxation and/or do not promote effective coping. Thus these are not health-promoting and should not be included in the script. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-16, 40 (Box 10-3) TOP: MSC: Client Needs: Psychosocial Integrity Nursing Process: Planning 4. An individual says to the nurse, “I feel so stressed out lately. I think the stress is affecting my body also.” Which somatic complaints are most likely to accompany this feeling? (Select all that apply.) a. Headache b. Neck pain c. Insomnia d. Anorexia e. Myopia ANS: A, B, C, D When individuals feel “stressed-out,” they often have accompanying somatic complaints, especially associated with sleep, eating, and headache or back pain. Changes in vision, such as myopia, would not be expected. PTS: 1 DIF: Cognitive Level: Apply (Application) REF: Pages 10-7, 29 (Table 10-1) TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity [Show More]
Last updated: 1 year ago
Preview 1 out of pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 18, 2021
Number of pages
Written in
Additional information
This document has been written for:
Uploaded
Apr 18, 2021
Downloads
0
Views
2

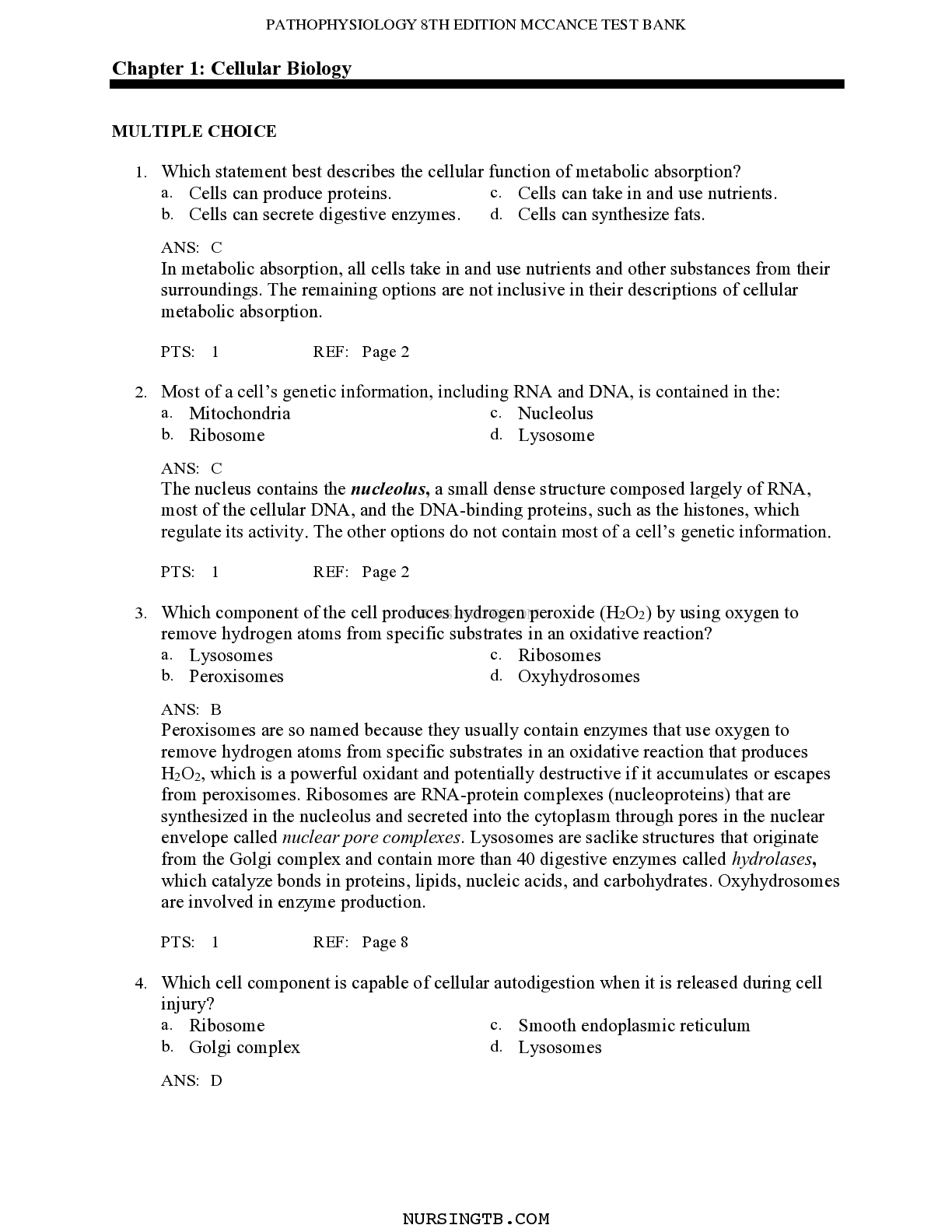
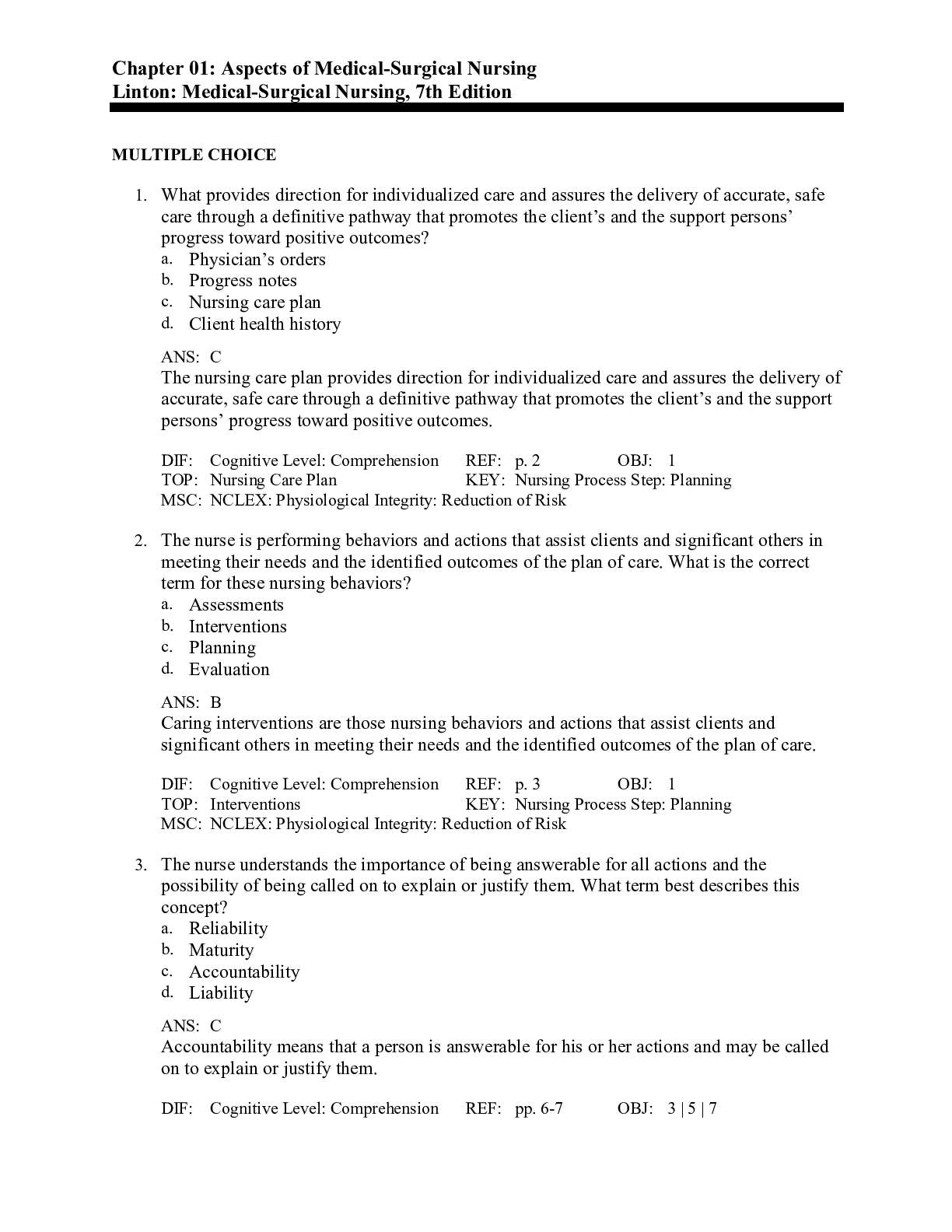
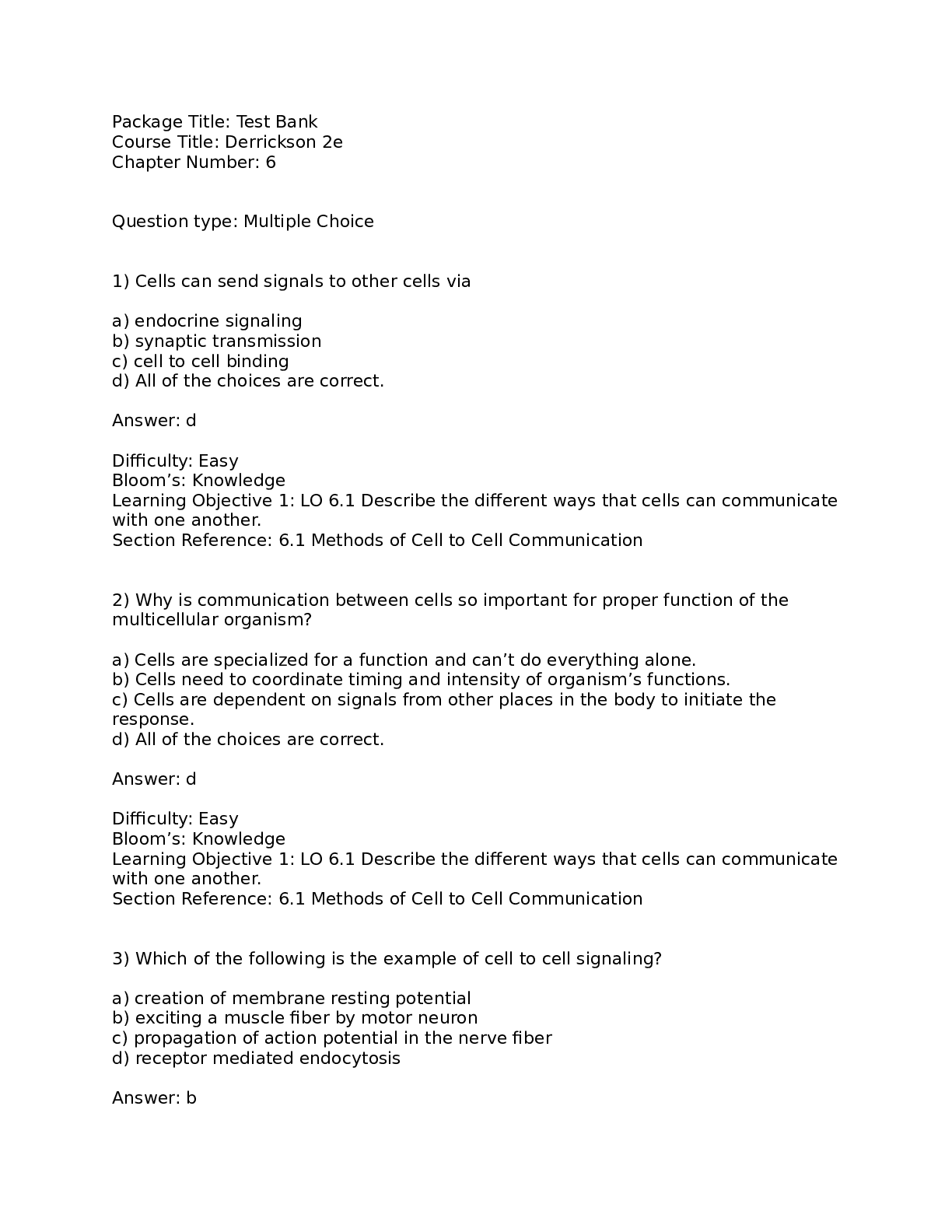
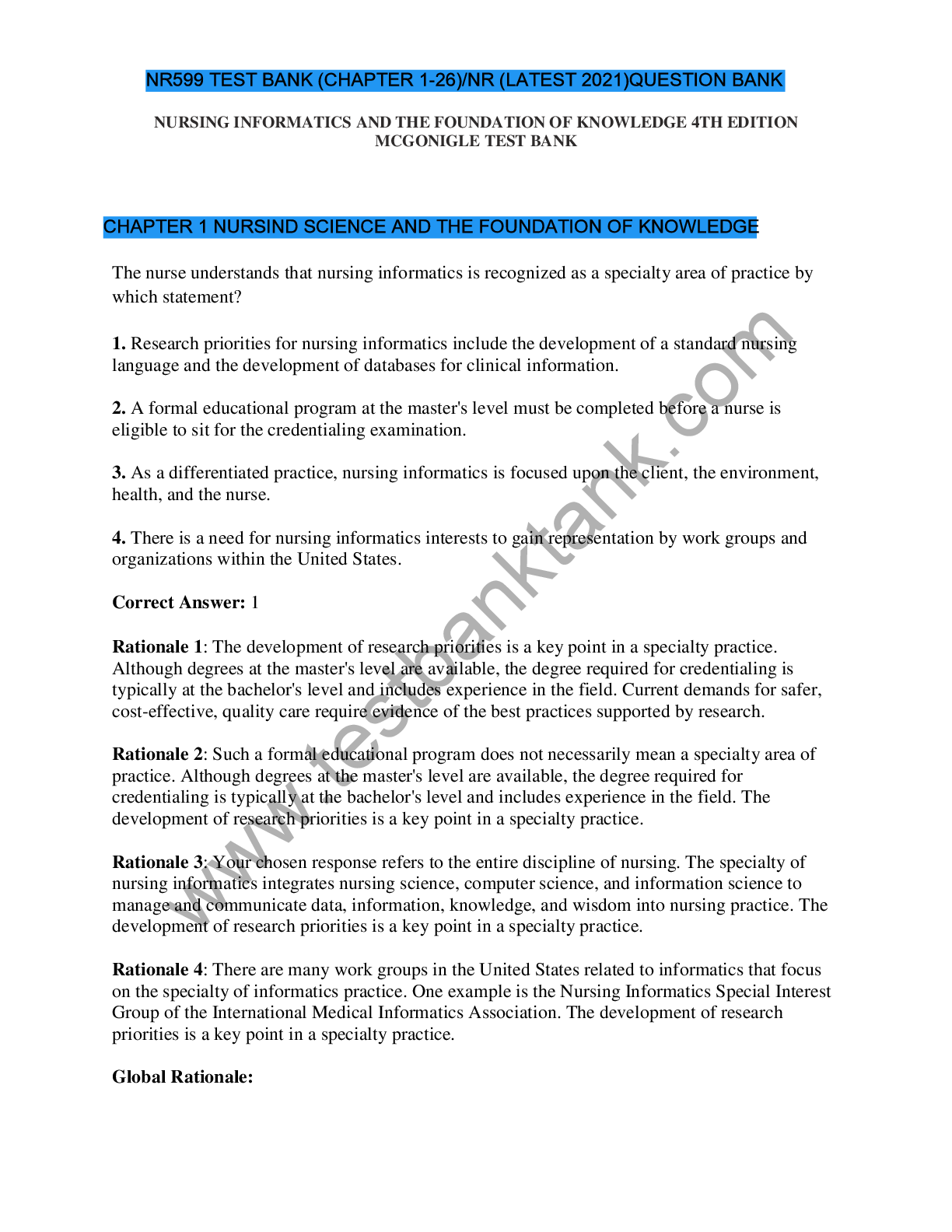
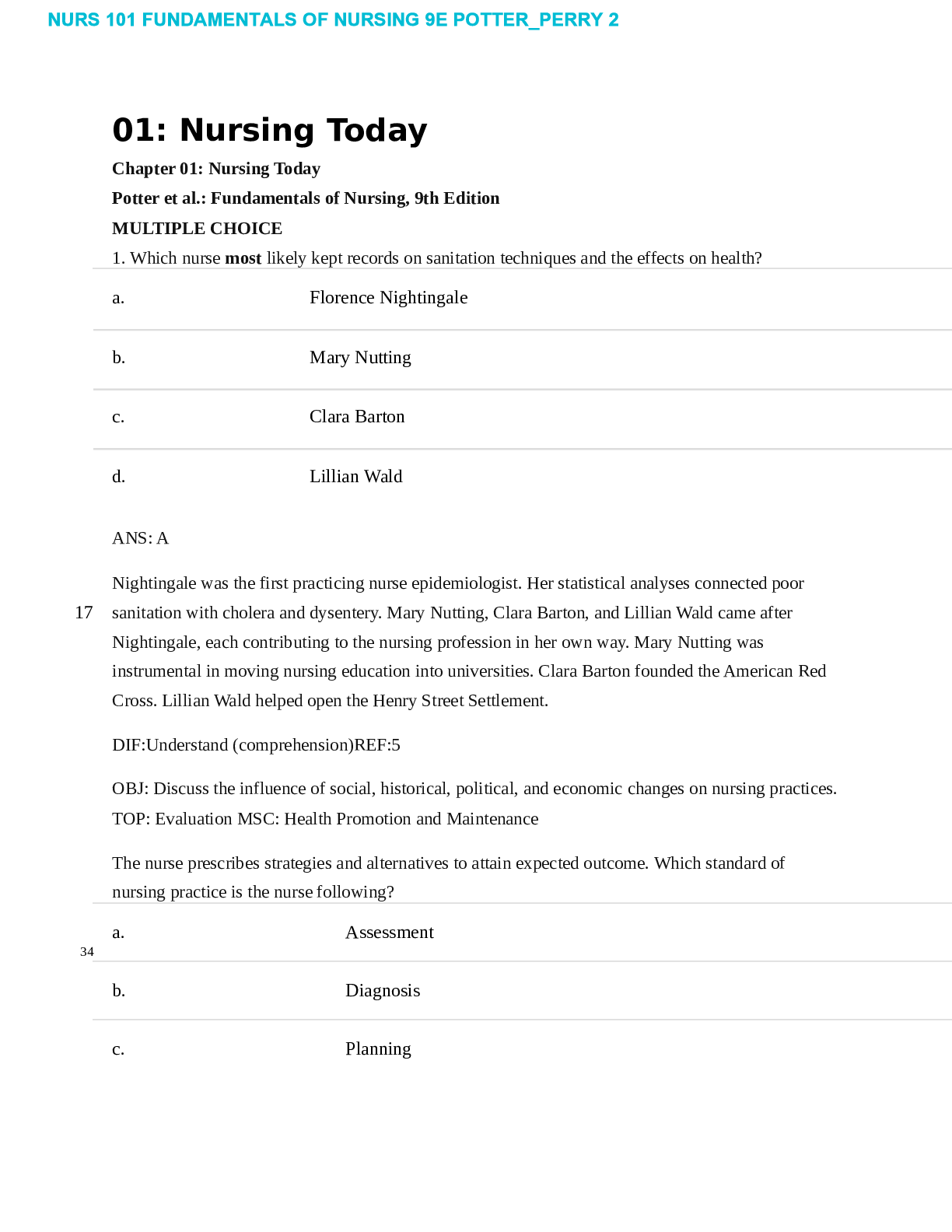

.png)