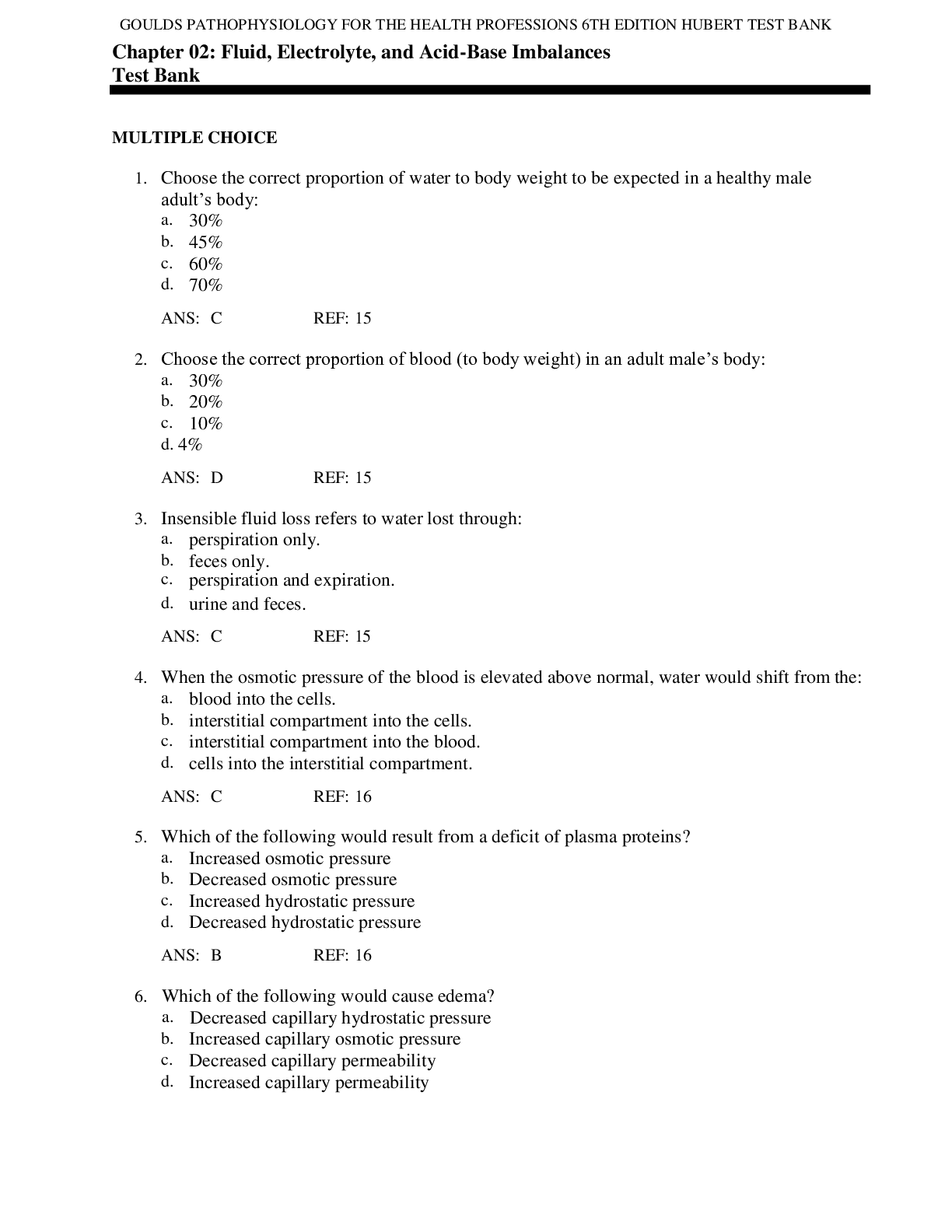
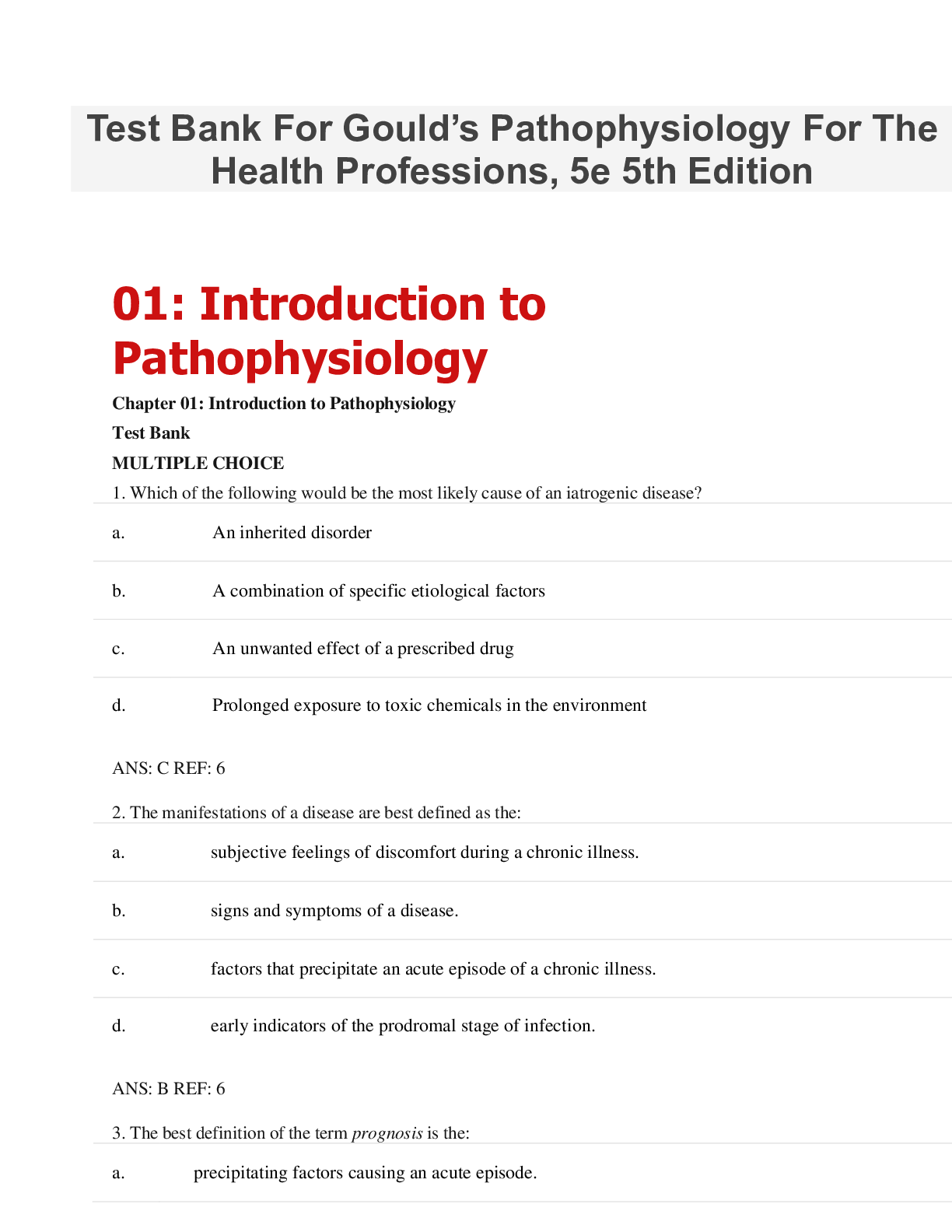
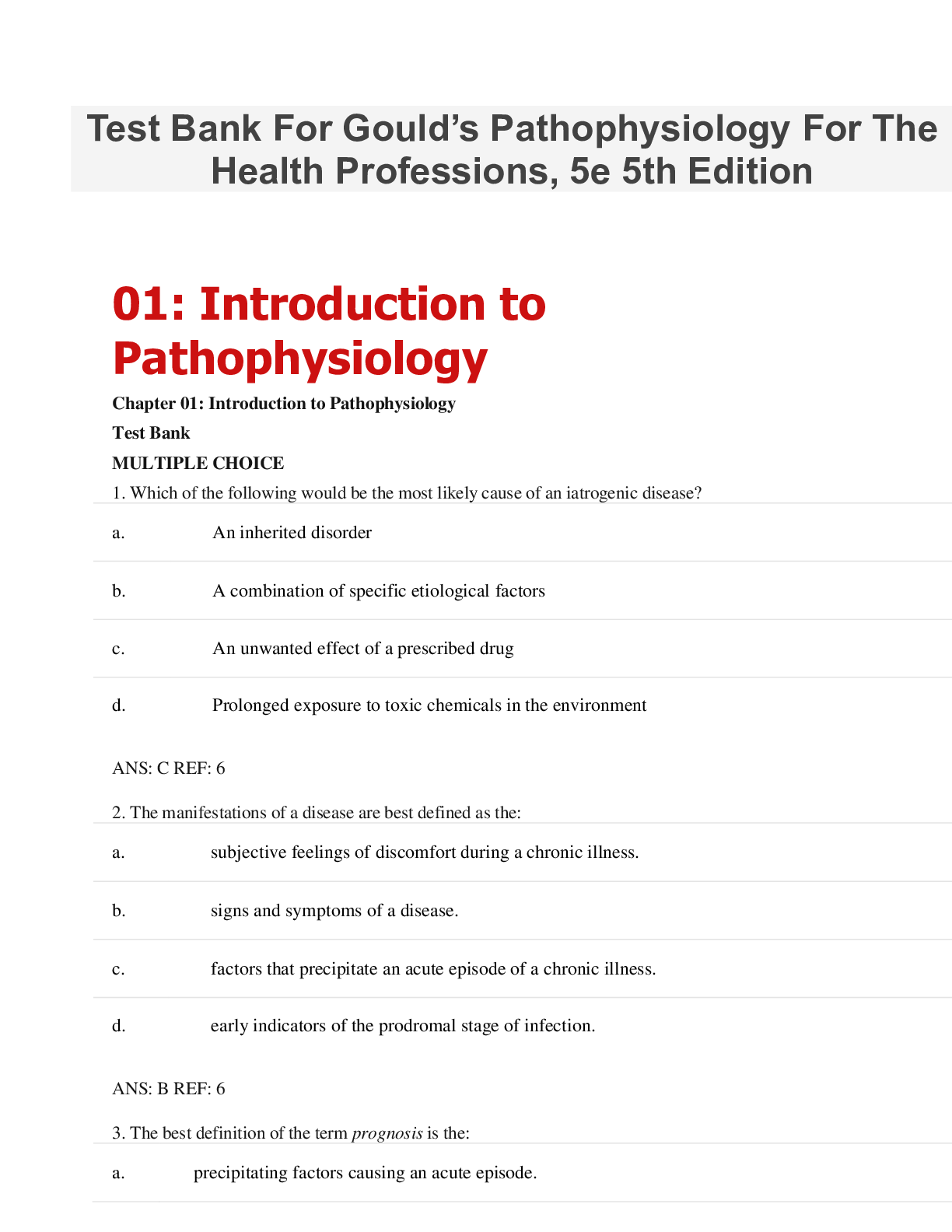
*NURSING > TEST BANK > TEST BANK for Gould’s Pathophysiology For The Health Professions, 5th Edition. All Chapters1-28 (C (All)
TEST BANK for Gould’s Pathophysiology For The Health Professions, 5th Edition. All Chapters1-28 (Complete Download). 421 Pages
Document Content and Description Below
Test Bank For Gould’s Pathophysiology For The Health Professions, 5e 5th Edition 01: Introduction to Pathophysiology Chapter 01: Introduction to Pathophysiology Test Bank MULTIPLE CHOICE 1. W... hich of the following would be the most likely cause of an iatrogenic disease? a. An inherited disorder b. A combination of specific etiological factors c. An unwanted effect of a prescribed drug d. Prolonged exposure to toxic chemicals in the environment 6 2. The manifestations of a disease are best defined as the: a. subjective feelings of discomfort during a chronic illness. b. signs and symptoms of a disease. c. factors that precipitate an acute episode of a chronic illness. d. early indicators of the prodromal stage of infection. 6 3. The best definition of the term prognosis is the: a. precipitating factors causing an acute episode. b. number of remissions to be expected during the course of a chronic illness. c. predicted outcome or likelihood of recovery from a specific disease. d. exacerbations occurring during chronic illness. 7 4. Which of the following is considered a systemic sign of disease? a. Swelling of the knee b. Fever c. Pain in the neck d. Red rash on the face 6 5. Etiology is defined as the study of the: a. causes of a disease. b. course of a disease. c. expected complications of a disease. d. manifestations of a disease. 5 6. A type of cellular adaptation in which there is a decrease in cell size is referred to as: a. hypertrophy. b. metaplasia. c. anaplasia. d. atrophy. 8 7. A change in a tissue marked by cells that vary in size and shape and show increased mitotic figures would be called: 8 8. A deficit of oxygen in the cells usually due to respiratory or circulatory problems is called: a. apoptosis. b. ischemia. c. hypertrophy. d. necrosis. 9 9. When a group of cells in the body dies, the change is called: a. ischemia. b. gangrene. a. metaplasia. b. atrophy. c. dysplasia. d. hypertrophy. c. hypoxia. d. necrosis. 10 10. Rigorous weight lifting/body building regimens may result in the skeletal muscle cells undergoing: 8 11. The term cancer refers to: a. dysplasia. b. hyperplasia. c. metaplasia. d. malignant neoplasm. 9 12. To which of the following does the term apoptosis refer? a. Increased rate of mitosis by certain cells b. Ischemic damage to cells a. hypertrophy. b. dysplasia. c. atrophy. d. regeneration. c. Liquefaction of necrotic tissue d. Preprogrammed cell self-destruction 9 13. Which of the following statements is TRUE? a. Alteration of DNA does not change cell function. b. Damaged cells may be able to repair themselves. c. All types of cells die at the same rate. d. Mild ischemia causes immediate cell death. 10 14. Caseation necrosis refers to an area where: a. cell proteins have been denatured. b. cell are liquefied by enzymes. c. dead cells form a thick cheesy substance. d. bacterial invasion has occurred. 10 15. Routine application of sun block to skin would be an example of: a. an iatrogenic cause of cancer. b. a preventive measure. c. a precipitating factor. d. a predisposing condition. 6 16. A circumstance that causes a sudden acute episode of a chronic disease to occur is termed: a. latent stage. b. predisposing factor. c. incidence. d. precipitating factor. 7 17. The term homeostasis refers to: a. the causative factors in a particular disease. b. maintenance of a stable internal environment. c. a condition that triggers an acute episode. d. a collection of signs and symptoms. 2 18. Which term is used to describe a new and secondary or additional problem that arises after the original disease has been established? a. Symptoms b. Occurrence c. Manifestations d. Complication 7 19. Pathophysiology involves the study of: a. the structure of the human body. b. the functions of various organs in the body. c. functional or structural changes resulting from disease processes. d. various cell structures and related functions. 2 20. Which of the following is the best definition of epidemiology? a. The science of tracking the occurrence and distribution of diseases b. The relative number of deaths resulting from a particular disease c. Identification of a specific disease through evaluation of signs and symptoms d. The global search for emerging diseases 7 21. Which of the following can cause cell injury or death? 1. Hypoxia 2. Exposure to excessive cold 3. Excessive pressure on a tissue 4. Chemical toxins a. 1, 2 b. 2, 4 c. 1, 3, 4 d. 1, 2, 3, 4 9 22. All of the following are part of the Seven Steps to Health EXCEPT: a. follow cancer screening guidelines. b. use sun block agents whenever exposed. c. participate in strenuous exercise on a regular daily basis. d. choose high fiber, lower fat foods. 2 23. The term disease refers to: a. the period of recovery and return to a normal healthy state. b. a deviation from the normal state of health and function. c. the treatment measures used to promote recovery. d. a basic collection of signs and symptoms. 2 24. A collection of signs and symptoms, often affecting more than one organ or system, that usually occur together in response to a certain condition is referred to as a (an): 7 25. All of the following statements are correct about cell damage EXCEPT: a. The initial stage of cell damage often causes an alteration in metabolic reactions. b. If the factor causing the damage is removed quickly, the cell may be able to recover and return to its nor c. If the noxious factor remains for an extended period of time, the damage becomes irreversible and the ce d. Initially, cell damage does not change cell metabolism, structure, or function. 9 26. Which of the following conditions distinguishes double blind studies used in health research? a. Neither the members of the control group or the experimental group nor the person administering the trea receiving the experimental therapy. b. Both groups of research subjects and the person administering the treatment know who is receiving the ex c. The research subjects do not know, but the person administering the treatment knows who is receiving pla therapy. d. Only members of the control group know they are receiving standard therapy. a. acute disease. b. multiorgan disorder. c. syndrome. d. manifestation. 3 | 4 27. If the data collected from the research process confirm that the new treatment has increased effectiveness and is safe, this is called: 4 28. A short-term illness that develops very quickly with perhaps a high fever or severe pain is called: a. acute. b. latent. c. chronic. d. manifestation. 6 29. The term prognosis refers to the: a. period of recovery and return to a normal state. b. expected outcome of the disease. c. mortality and morbidity rates for a given population. d. typical collection of signs and symptoms. a. the placebo effect. b. evidence-based research. c. blind research studies. d. approval for immediate distribution. 7 30. When prolonged ischemia occurs to an area of the heart, the resulting damage is referred to as: a. atrophy. b. liquefactive necrosis. c. apoptosis. d. infarction. 10 31. During the evaluation process for a new therapy’s effectiveness and safety, a double blind study may be conducted during: 3 32. Why are the predisposing factors for a specific disease important to health professionals? a. To predict the prognosis b. To determine treatments c. To develop preventive measures d. To develop morbidity statistics a. the first stage. b. the second stage. c. the third stage. d. any of these stages. 3 33. Cell damage may be caused by exogenous sources such as: a. abnormal metabolic processes. b. certain food additives. c. genetic defects. d. localized hypoxia. 9 | 10 34. Which of the following is usually included in a medical history? 1. Past illnesses or surgeries 2. Current illnesses, acute and chronic 3. Prescribed medication or other treatments 4. Nonprescription drugs and herbal remedies 5. Current allergies a. 1, 3 b. 2, 4, 5 c. 1, 3, 4 d. 1, 2, 3, 4, 5 4 | 5 35. A situation when there is a higher than expected number of cases of an infectious disease within a given area is called a/an: a. epidemic. b. exacerbation. c. morbidity. d. pandemic. 7 36. The term pathogenesis refers to: a. the development of a disease or sequence of events related to tissue changes involved in the disease proc b. the determination of the cause(s) involved in the development of a malignant neoplasm. c. the specific signs and symptoms involved in the change from an acute disease to a chronic disease. d. the changes in cells of affected tissue that result in necrosis. 6 02: Fluid, Electrolyte, and AcidBase Imbalances Chapter 02: Fluid, Electrolyte, and Acid-Base Imbalances Test Bank MULTIPLE CHOICE 1. Choose the correct proportion of water to body weight to be expected in a healthy male adult’s body: a. 30% b. 45% c. 60% d. 70% 15 2. Choose the correct proportion of blood (to body weight) in an adult male’s body: a. 30% b. 20% c. 10% d. 4% 15 3. Insensible fluid loss refers to water lost through: a. perspiration only. b. feces only. c. perspiration and expiration. d. urine and feces. 15 4. When the osmotic pressure of the blood is elevated above normal, water would shift from the: a. blood into the cells. b. interstitial compartment into the cells. c. interstitial compartment into the blood. d. cells into the interstitial compartment. 16 5. Which of the following would result from a deficit of plasma proteins? a. Increased osmotic pressure b. Decreased osmotic pressure c. Increased hydrostatic pressure d. Decreased hydrostatic pressure 16 6. Which of the following would cause edema? a. Decreased capillary hydrostatic pressure b. Increased capillary osmotic pressure c. Decreased capillary permeability d. Increased capillary permeability 16-19 7. Which of the following would likely be related to an elevated hematocrit reading? a. Fluid excess b. Fluid deficit c. Increased sodium level d. Decreased erythrocytes 23-24 8. Which of the following is a typical sign of dehydration? a. Rapid, strong pulse b. Low hematocrit c. Increased urine output d. Rough oral mucosa 21 9. Which of the following terms refers to a combination of decreased circulating blood volume combined with excess fluid in a body cavity? 21 10. Which of the following is the primary cation in the extracellular fluid? a. Sodium b. Potassium a. Dehydration b. Third-spacing c. Hypovolemia d. Water retention c. Calcium d. Iron 21 11. Which of the following is a common cause of hyponatremia? a. Loss of the thirst mechanism b. Excessive sweating c. Excessive aldosterone secretion d. Prolonged period of rapid, deep respirations 22-23 12. Which of the following is a common effect of both hypokalemia and hyperkalemia? a. Skeletal muscle twitch and cramps b. Oliguria c. Elevated serum pH d. Cardiac arrhythmias 26 13. Choose the correct effect of increased parathyroid hormone. a. Increased movement of calcium ions into the bones b. Increased activation of vitamin D c. Increased absorption of calcium from the digestive tract d. Decreased reabsorption of calcium in the kidneys 26 14. Which of the following results from hypocalcemia? 1. Low serum phosphate levels 2. Nausea and constipation 3. Skeletal muscle twitch and spasms 4. Weak cardiac contractions a. 1, 2 b. 1, 4 c. 2, 3 d. 3, 4 27 15. Which of the following causes tetany? a. Increased permeability of nerve membranes due to low serum calcium b. Excess calcium ions in skeletal muscle due to excess parathyroid hormone (PTH) c. Excess calcium ions inside somatic nerves as a result of neoplasms d. Increased stimulation of the nerves in the cerebral cortex 27 16. In which of the following processes is phosphate ion NOT a major component? a. Bone metabolism b. Metabolic processes involving adenosine triphosphate (ATP) c. Blood clotting d. Acid-base balance 28 17. Which of the following would be considered normal serum pH? a. 4.5-8 b. 7.0 c. 7.4 d. 8 28 18. When many excess hydrogen ions accumulate in the blood, what happens to serum pH? The pH: a. decreases. b. increases. c. remains constant. d. varies based on metabolism. 28 19. What is the slowest but most effective control for acid-base balance? a. Respiratory system b. Buffer systems in the blood c. Kidneys d. Brain 29 20. Which of the following is essential in order to maintain serum pH within normal range? a. Carbonic acid and bicarbonate ion must be present in equal quantities. b. All excess carbonic acid must be excreted by the kidneys. c. The concentration of bicarbonate ion must remain constant. d. The ratio of carbonic acid to bicarbonate ion must be 1:20. 30 21. Which is the correct effect on the body of abnormally slow respirations? a. Increased carbonic acid b. Decreased carbonic acid c. Increased bicarbonate ion d. Decreased bicarbonate ion 31 22. Which condition is likely to cause metabolic acidosis? a. Slow, shallow respirations b. Prolonged diarrhea c. Mild vomiting d. Excessive fluid in the body 32 23. What would a serum pH of 7.33 in a patient with kidney disease indicate? a. Metabolic alkalosis b. Metabolic acidosis c. Respiratory alkalosis d. Respiratory acidosis 32 24. Which serum value indicates decompensated metabolic acidosis? a. pH is below normal range b. pH is above normal range c. Bicarbonate level decreases d. Bicarbonate level increases 32 25. What is the effect on blood serum when excessive lactic acid accumulates in the body? a. Bicarbonate ion levels decrease b. Bicarbonate ion levels increase c. Carbonic acid levels increase d. pH increases 32 26. The direct effects of acidosis are manifested primarily in the functioning of the: a. Digestive system b. Urinary system c. Nervous system d. Respiratory system 32 27. Compensation mechanisms in the body for dehydration would include: a. increased antidiuretic hormone (ADH). b. decreased aldosterone. c. slow, strong heart contraction. d. peripheral vasodilation. 21 28. Which acid-base imbalance results from impaired expiration due to emphysema? a. Metabolic acidosis b. Metabolic alkalosis c. Respiratory acidosis d. Respiratory alkalosis 32 29. In patients with impaired expiration associated with emphysema, effective compensation for the acid-base imbalance would be: 32 30. An anxiety attack often causes hyperventilation leading to: a. increased PCO2. b. decreased PCO2. c. respiratory acidosis. d. metabolic acidosis. 32 31. One of the factors involved in the increased need for water in infants is: a. increased rate and depth of respiration. b. decreased rate and depth of respiration. c. increased urine pH and decreased serum bicarbonate. d. decreased urine pH and increased serum bicarbonate. a. proportionally smaller body surface area. b. higher metabolic rate. c. smaller respiratory capacity. d. greater surface area of exposed mucous membranes. 20 32. Compensation for respiratory system depression due to anesthesia and sedation would be: a. decreased reabsorption of bicarbonate ions in the kidneys. b. increased secretion of hydrogen ions into the filtrate. c. increased respiratory rate and depth. d. increased renin secretion. 32 33. A prolonged state of metabolic acidosis often leads to: a. hypokalemia. b. hyperkalemia. c. hyponatremia. d. hypercalcemia. 25 34. Strenuous physical exercise on a hot day is likely to result in: a. hypokalemia. b. hypernatremia. c. hyperchloremia. d. hypovolemia. 19 | 23 35. Place the following events in the correct sequence of events when ketoacids increase in the blood of a diabetic patient. Not all options are used in the answers. 1. Serum pH decreases 2. Serum bicarbonate decreases 3. PCO2 decreases 4. Respiration decreases 5. Respiration increases 6. Serum pH increases 7. Urine pH decreases a. 1, 3, 7, 4, 2, 6 b. 5, 2, 7, 3, 4, 1 c. 2, 1, 5, 3, 7, 6 d. 3, 1, 2, 5, 7, 6 34-37 36. Which of the following is a manifestation of respiratory alkalosis? a. Bradycardia and deep rapid breathing b. Drowsiness and general lethargy c. Increased nervous system irritability d. Decreased urine pH 33 37. Prolonged diarrhea results in: a. loss of fluid and bicarbonate ions, leading to metabolic acidosis. b. increased fluid and serum bicarbonate ions, leading to metabolic acidosis. c. loss of chloride ions only, leading to metabolic alkalosis. d. surplus bicarbonate ions, leading to respiratory alkalosis. 32 38. In the initial stage, vomiting results in: a. metabolic acidosis. b. metabolic alkalosis. c. respiratory alkalosis. d. None of the above 32 39. Which two ions are most important for acid-base balance in the body? a. K+, Na+ b. Cl– and HCO – 3 c. Ca++, Na+ d. Na+, Cl– 28 40. The bicarbonate-carbonic acid buffer system helps maintain serum pH. The balance of the carbonic acid and bicarbonate ion levels are controlled by the: 30 41. Alkalosis increases irritability and spontaneous stimulation of nerves by: a. blocking normal nerve conduction. b. increasing the permeability of nerve membranes. c. blocking movement of calcium ions. d. decreasing phosphate ion levels. 26 | 33 42. Hypocalcemia causes weak cardiac contractions because: a. liver and pancreas. b. lungs and kidneys. c. lungs and plasma proteins. d. kidneys and bone marrow. a. permeability of nerve membranes increases. b. insufficient calcium ions are available for muscle contraction. c. low phosphate ion levels prevent muscle contraction. d. excessive amounts of calcium are stored in cardiac muscle. 27 43. Serum potassium levels are affected by: 1. ADH. 2. aldosterone. 3. serum H+ levels. 4. insulin levels. a. 2 only b. 1, 2 c. 1, 3 d. 2, 3, 4 e. 1, 2, 3 24 | 25 44. Which of the following is the primary control of serum Na+ levels? a. ADH b. Aldosterone c. Serum H+ levels d. serum K+ levels 21 45. The control center for thirst is located in the: a. kidneys. b. thalamus. c. medulla. d. hypothalamus. 15 46. Which statements apply to atrial natriuretic peptide? 1. It is secreted by heart muscle cells. 2. It is a hormone secreted by the kidneys. 3. It helps to control water and sodium balance. 4. It is released in response to low blood pressure. a. 1, 3 b. 1, 4 c. 2, 3 d. 2, 4 15 47. What are the three mechanisms that control or compensate for serum pH? a. Hypothalamus, metabolic changes by digestive system, lymphatic system filtration b. Buffer pairs in blood, change in kidney excretion rate, change in respiration rate c. Neural feedback, increase in heart rate, decrease in calcium intake d. Modification of water intake, increased capillary permeability, decrease in blood volume 29-31 48. Hypokalemia refers to a condition in which the serum has a very low level of which ion? a. Sodium b. Phosphate c. Calcium d. Potassium 24 49. In the blood and extracellular fluids, hypernatremia refers to: a. a deficient sodium level. b. an excess phosphate level. c. an excess sodium level. d. an excessively low phosphate level. 23 50. Increased milk and/or antacid intake can contribute to development of “milk-alkali syndrome,” which can cause which of the following? 27 03: Introduction to Basic Pharmacology and Other Common Therapies Chapter 03: Introduction to Basic Pharmacology and Other Common Therapies Test Bank MULTIPLE CHOICE 1. Which of the following are considered to be the toxic effects of a drug? a. Additional, mild, unwanted effects b. Unusual, unexpected mild effects c. Serious, possibly life-threatening effects d. Reduction of the allergic response 41 2. What is the unique, simple, and official name assigned to a specific drug for worldwide use? a. Hyponatremia b. Hyperkalemia c. Hypercalcemia d. Hypovolemia a. Trade name b. Chemical name c. Proprietary name d. Generic name 46 3. Which is the route of administration by which the largest proportion of the drug dose is likely lost before reaching the site of action? 44 4. Ingesting a drug with a large meal may be likely to: a. immediately increase the blood level of the drug. b. prevent gastric irritation. c. ensure that the total dose is absorbed into the blood. d. cause more rapid excretion of the drug. 42 a. Oral b. Intramuscular c. Sublingual d. Intravenous 5. What is the reaction called when two drugs interact to produce a result much greater than the sum of individual effects? 42 6. At which site are most drugs metabolized and prepared for excretion? a. Liver b. Kidneys c. Circulating blood d. Lymphoid tissue 45 7. In traditional Asian medicine, acupoints are usually located: a. over pain or other sensory receptors. b. where blood vessels branch. c. over joints. d. on designated meridians. 49 a. Antagonism b. Beneficial c. Synergism d. Potentiation 8. Traditional drug or surgical therapy is incorporated with nontraditional methods by: a. chiropractors. b. naturopaths. c. homeopaths. d. osteopaths. 48 9. Contraindications printed on the label of a drug identify: a. those circumstances under which the drug should probably not be used. b. those typical side effects associated with this drug. c. the dosage limits associated with the use of the drug. d. the maximum shelf life of the medication. 41 10. After they are metabolized, most drugs are excreted through the: a. lungs. b. pancreas. c. kidneys. d. large intestine. 42 11. A drug that binds with selected specific cell receptors may: 1. stimulate activity in those cells. 2. inhibit activity in those cells. 3. change specificity and attach to other cells. 4. be disabled by macrophages. a. 1, 2 b. 2, 3 c. 3, 4 d. 1, 3, 4 45-46 12. A placebo may be described as a tablet or capsule: a. that does not contain an active drug. b. that contains a small amount of active drug for use in clinical trials. c. that contains a different drug to be used for its psychological effect. d. that contains high amounts of a drug to determine the maximum dose allowed. 47 13. The form of therapy that involves assessment of physical function and works to restore any problems and prevent any further dysfunction using methods such as appropriate exercises and ultrasound is referred to as: a. registered massage therapy. b. naturopathy. c. physiotherapy. d. reflexology. 47 14. A medical history should include all: 1. legally prescribed drugs. 2. vitamin or mineral supplements. 3. any medication not requiring a prescription (over-the-counter items). 4. herbal treatments. a. 1 only b. 1, 3 c. 1, 2, 4 d. 1, 2, 3, 4 47 15. Antagonistic drugs may be used to: a. increase the effectiveness of selected drugs. b. prolong the action of a drug. c. act as an antidote when necessary. d. speed up the excretion of a drug. 42 16. The full course of a prescribed antimicrobial drug should be completed so as to prevent: a. undesirable side effects. b. development of resistant microbes. c. an allergic response. d. proper metabolism and excretion of drug. 42 Chapter 04: Pain Chapter 04: Pain Test Bank MULTIPLE CHOICE 1. The impulses related to acute pain are usually transmitted by: a. nociceptors. b. myelinated A delta fibers. c. unmyelinated C fibers. d. any sensory fiber with a low pain threshold. 55 2. In which structure do pain impulses ascend the spinal cord? a. Reticular formation b. Corticospinal tract c. Spinothalamic tract d. Relevant dermatome 55 3. According to the gate-control theory, passage of pain impulses may be naturally blocked: a. at the synapse by entry of other sensory impulses. b. by the stress response. c. by administration of morphine directly into the spinal cord. d. by referring the pain to other parts of the body. 55 4. What is the term used to describe the degree of pain that is endured before an individual takes action? 55 5. What is the definition of endorphins? a. Neurotransmitters at the nociceptors b. Transmitters for sensory impulses c. Opiate-like blocking agents in the central nervous system a. Pain threshold b. Referred pain c. Phantom pain d. Pain tolerance d. Pain-causing chemical mediators 57 6. Pain perceived in the left arm during the course of a heart attack is an example of: a. referred pain. b. phantom pain. c. chronic pain. d. subjective pain response. 57 7. A headache that is related to changes in cerebral blood flow is classified as a/an headache. 60 8. What is a common analgesic administered to control a moderate level of pain? a. Meperidine b. Acetaminophen c. Codeine a. tension b. sinus c. migraine d. intracranial d. Ibuprofen 62 9. Which of the following applies to spinal anesthesia? a. It causes analgesia with loss of consciousness. b. The drug is injected into cerebrospinal fluid (CSF) or the epidural space of the spinal cord. c. The drug stimulates release of endorphins in the spinal cord. d. The transmission of pain impulses is blocked in a small area of the body. 62 10. Which of the following is a characteristic of acute pain but not of chronic pain? a. Depression and debilitation b. A perception of increased generalized pain and discomfort c. Fatigue and lower pain tolerance d. Severe but short term 55-57 11. What is the role of nociceptors? They are: a. pain receptors that are stimulated by thermal, chemical, or physical means. b. spinal nerves that conduct impulses from specific areas of the skin. c. responsible for the state of arousal with pain. d. useful in localizing pain to a specific area of the body. 54 12. Intractable pain is best defined as: a. pain that is perceived as occurring in an amputated limb. b. severe pain that cannot be controlled by medication. c. pain perceived as coming from a source other than the actual source. d. pain coming from a specific dermatome. 62 13. Which of the following statements is TRUE? a. The brain is more aware of pain impulses when the reticular activating system is depressed. b. Acute pain does not cause a reflex response at the spinal cord synapses. c. Young infants typically respond to pain with tachycardia and increased blood pressure. d. Chronic pain is easier to tolerate without negative effects. 57 14. Ibuprofen is classified as an NSAID and is particularly useful in treating: a. severe pain. b. pain caused by inflammation. c. intracranial pain. d. pain in young infants. 61 15. Which of the following analgesics acts to reduce pain at the peripheral site? a. Acetaminophen b. Morphine c. Codeine d. Intravenous general anesthesia 61 16. Cancer-related pain has been broken down into three basic categories: pain caused by the advance of the disease and resultant damage to the body, pain that is the result of a coexisting disease unrelated to the cancer, and: 61 17. Pain that is caused by trauma or disease involving the peripheral nerves is referred to as: a. neuropathic pain. b. central pain. a. phantom pain as a result of amputation. b. pain associated with the treatment of the disease. c. pain caused by emotional stress and metabolic changes. d. pain associated with damage to the peripheral nerves. c. neurogenic pain. d. referred pain. 61 18. Pain resulting from a profound, sudden loss of blood flow to an organ or tissues in a specific area of the body is referred to as: 61 19. Which of the following is a characteristic of chronic pain? a. It usually initiates a physiological stress response. b. It always involves a strong emotional response such as high anxiety. c. It is more difficult to diagnose and treat than is acute pain. d. It involves tissue damage to a specific organ. 59 | 60 20. A headache that results from pressure on the meninges surrounding the brain is referred to as a/an: a. chronic pain. b. central pain. c. cardiovascular pain. d. ischemic pain. a. intracranial headache. b. intrameningeal headache. c. migraine headache. d. cerebral headache. 60 Chapter 05: Inflammation and Healing Chapter 05: Inflammation and Healing Test Bank MULTIPLE CHOICE 1. Tears are considered to be part of the: 1. first line of defense. 2. second line of defense. 3. third line of defense. 4. specific defenses. 5. nonspecific defenses. a. 1, 4 b. 1, 5 c. 3, 4 d. 2, 5 66 2. A specific defense for the body is: a. phagocytosis. b. sensitized T lymphocytes. c. the inflammatory response. d. intact skin and mucous membranes. 66 3. The inflammatory response is a nonspecific response to: a. phagocytosis of foreign material. b. local vasodilation. c. any tissue injury. d. formation of purulent exudates. 66 4. Chemical mediators released during the inflammatory response include: a. albumin and fibrinogen. b. growth factors and cell enzymes. c. macrophages and neutrophils. d. histamine and prostaglandins. 69 5. Which of the following result directly from the release of chemical mediators following a moderate burn injury? 1. Pain 2. Local vasoconstriction 3. Increased capillary permeability 4. Pallor a. 1, 2 b. 1, 3 c. 2, 3 d. 2, 4 69 6. Granulation tissue is best described as: a. highly vascular, very fragile, and very susceptible to infection. b. an erosion through the wall of viscera, leading to complications. c. a type of adhesion with no vascularization. d. a form of stenosis, in a duct, that is extremely tough and resists attack by microbes. 76 7. Edema associated with inflammation results directly from: a. increased fluid and protein in the interstitial compartment. b. increased phagocytes in the affected area. c. decreased capillary permeability. d. general vasoconstriction. 70 8. The warmth and redness related to the inflammatory response results from: a. increased interstitial fluid. b. production of complement. c. a large number of white blood cells (WBCs) entering the area. d. increased blood flow into the area. 70 9. What is the correct order of the following events in the inflammatory response immediately after tissue injury? 1. Increased permeability of blood vessels 2. Dilation of blood vessels 3. Transient vasoconstriction 4. Migration of leukocytes to the area 5. Hyperemia a. 5, 3, 2, 1, 4 b. 1, 2, 4, 5, 3 c. 2, 3, 5, 4, 1 d. 3, 2, 5, 1, 4 69 10. The process of phagocytosis involves the: a. ingestion of foreign material and cell debris by leukocytes. b. shift of fluid and protein out of capillaries. c. formation of a fibrin mesh around the infected area. d. movement of erythrocytes through the capillary wall. 70 11. Systemic effects of severe inflammation include: a. erythema and warmth. b. loss of movement at the affected joint. c. fatigue, anorexia, and mild fever. d. abscess formation. 71 12. The term leukocytosis means: a. increased white blood cells (WBCs) in the blood. b. decreased WBCs in the blood. c. increased number of immature circulating leukocytes. d. significant change in the proportions of WBCs. 72 13. Which of the following statements applies to fever? a. Viral infection is usually present. b. Heat-loss mechanisms have been stimulated. c. It is caused by a signal to the thalamus. d. It results from release of pyrogens into the circulation. 71 14. Mechanisms to bring an elevated body temperature down to the normal level include: a. general cutaneous vasodilation. b. generalized shivering. c. increased heart rate. d. increased metabolic rate. 71 15. Replacement of damaged tissue by similar functional cells is termed: a. fibrosis. b. regeneration. c. resolution. d. repair by scar tissue. 73 16. Scar tissue consists primarily of: a. granulation tissue. b. epithelial cells. c. collagen fibers. d. new capillaries and smooth muscle fibers. 76 17. Which of the following promotes rapid healing? a. Closely approximated edges of a wound b. Presence of foreign material c. Exposure to radiation d. Vasoconstriction in the involved area 76 18. Glucocorticoids are used to treat inflammation because they directly: a. promote the release of prostaglandins at the site. b. decrease capillary permeability. c. mobilize lymphocytes and neutrophils. d. prevent infection. 74 19. Patients taking glucocorticoids for long periods of time are likely to develop all of the following EXCEPT: 75 20. Which of the following drugs relieves fever and some types of pain but is NOT an antiinflammatory agent? 74 21. A burn area in which the epidermis and part of the dermis is destroyed is classified as: a. full-thickness. b. deep partial-thickness. a. decreased bone density. b. wasting of skeletal muscle. c. opportunistic infections. d. increased leukocyte production. a. Acetaminophen b. Prednisone c. Aspirin d. Ibuprofen c. superficial partial-thickness. d. first-degree. 79 22. A woman has burns on the anterior surfaces of her right arm, chest, and right leg. The percentage of body surface area burned is approximately: 80 | 82 23. The characteristic appearance of a full-thickness burn is: a. painful with multiple blisters. b. heavy bleeding. c. red with some swelling. d. dry, firm, charred, or hard white surface. 79 24. A typical source of infection in burn areas is: a. the skin grafts. b. microbes surviving in the hair follicles in the burn area. a. 13.5%. b. 18%. c. 22.5%. d. 31.5%. c. circulating blood bringing microbes to the burn wound. d. opportunistic virus in digestive tract. 83 25. A large burn area predisposes to decreased blood pressure because: a. bleeding occurs under the burn surface. b. the heart is damaged by toxic materials from the burn. c. fluid and protein shift out of the blood. d. vasoconstriction occurs in the burn area. 82 26. During an inflammatory response, hyperemia is caused by: a. increased blood flow in the area. b. increased capillary permeability. c. irritation of sensory nerve endings by histamine. d. increased leukocytes in the area. 69 27. The advantages of applying a biosynthetic skin substitute to a large area of full-thickness burns include: 1. reduced risk of infection. 2. decreased loss of plasma protein and fluid. 3. developing stronger fibrous scar tissue. 4. more rapid healing. 5. regeneration of all glands, nerves, and hair follicles. a. 1, 3 b. 4, 5 c. 1, 2, 4 d. 2, 3, 5 84 28. Purulent exudates usually contain: a. small amounts of plasma protein & histamine in water. b. red blood cells & all types of white blood cells. c. numerous leukocytes, bacteria, and cell debris. d. large amounts of water containing a few cells. 71 29. Isoenzymes in the circulating blood: a. are a type of plasma protein normally present in the circulating blood. b. often indicate the precise location of an inflammatory response. c. are normally released from leukocytes during the inflammatory response. d. are pyrogens, causing low-grade fever. 72 30. A serous exudate is best described as a: a. thin, watery, colorless exudate. b. thick, sticky, cloudy secretion. c. thick, greenish material containing microbes. d. brownish, clotted material. 70 31. Systemic manifestations of an inflammatory response include: a. edema and erythema. b. area of necrosis and loss of function. c. pain and tenderness. d. fever and malaise. 71 32. Some local effects of a general inflammatory response would include: a. high, spiking fever and chills. b. redness, warmth, and swelling. c. leukopenia and reduced erythrocyte sedimentation rate (ESR). d. anorexia and headaches. 67 33. Prolonged administration of glucocorticoids such as prednisone may cause: 1. atrophy of lymphoid tissue. 2. increased resistance to infection. 3. thrombocytopenia. 4. decreased protein synthesis. a. 1, 2 b. 1, 3 c. 1, 4 d. 2, 4 75 34. Application of ice to an injured knee reduces edema by: a. promoting return of lymph fluid. b. causing local vasoconstriction. c. increasing the rate of tissue repair. d. causing systemic vasodilation. 75 35. Healing of large areas of skin loss (including dermis and epidermis) would be most successful through: a. rapid mitosis and regeneration of skin layers. b. resolution of damaged cells in the area. c. covering the area with biosynthetic skin substitute. d. graft of fibrous tissue to the area. 84 36. Prostaglandins are produced from and cause . a. activated plasma protein; increased capillary permeability b. mast cells; vasodilation and pain c. platelets; attraction of neutrophils, chemotaxis d. mast cell granules; activation of histamines and kinins 69 37. The number of neutrophils in the blood is increased significantly: a. during allergic reactions. b. during chronic inflammation. c. to produce antibodies. d. in order to promote phagocytosis. 69-70 38. An abscess contains: a. serous exudate. b. purulent exudate. c. fibrinous exudate. d. hemorrhagic exudate. 71 39. Nonspecific agents that protect uninfected cells against viruses are called: a. neutrophils. b. macrophages. c. interferons. d. pyrogens. 66 40. Causes of inflammation include: a. direct physical damage such as cuts and sprains. b. allergic reactions. c. infection. d. All the above 67 41. In normal capillary exchange, what is net hydrostatic pressure based on? a. The difference between the hydrostatic pressure within the capillary, as compared with the hydrostatic pre interstitial fluid b. The relative osmotic pressures in the blood and the interstitial fluid c. The difference between the hydrostatic pressure and osmotic pressure within the capillary d. The difference between the concentrations of blood cells, plasma proteins, and dissolved substances in th interstitial fluid 66 42. The cardinal signs of inflammation include all of the following EXCEPT: a. redness. b. loss of function. c. nausea. d. swelling. 67 43. Drugs that have anti-inflammatory, analgesic, and antipyretic activities include: 1. COX-2 inhibitors (NSAIDs). 2. glucocorticoids (e.g., prednisone). 3. ibuprofen (NSAID). 4. acetaminophen. 5. aspirin (ASA). a. 1, 2 b. 2, 4 c. 1, 3, 5 d. 1, 4, 5 74 44. Aspirin (ASA) is discouraged for treatment of viral infection in children because of: a. decreased bone growth after puberty. b. frequent production of blood clots. c. formation of a granuloma filled with virus. d. the risk of developing Reye’s syndrome. 74 45. Systemic manifestations of inflammation include all EXCEPT: a. pyrexia. b. malaise. c. local swelling. d. anorexia. 71 46. Which of the following cellular elements found in the inflammatory response are responsible for phagocytosis? a. Macrophages b. Basophils c. B lymphocytes d. T lymphocytes e. Eosinophils 66 47. Which chemical mediator is involved in prolonging the inflammatory response? a. Bradykinin b. Histamine c. Leukotrienes d. Chemotactic factors 69 48. Potential complications after healing by scar formation include all the following EXCEPT: a. lack of sensory function in the area. b. contractures and adhesions. c. increased hair growth. d. keloid formation. 77-78 49. All of the following are correct statements regarding wound healing EXCEPT: a. Resolution occurs where there is minimal tissue damage and the cells can recover. b. Granulation tissue forms a permanent replacement for damaged tissue. c. Regeneration occurs where the cells are capable of mitosis. d. Scar tissue forms where the surrounding cells are incapable of mitosis. 73 | 75-76 50. Which of the following statements regarding inflammation is incorrect? a. Inflammation caused by an allergen or a burn will typically produce a serous exudate. b. Infection is one cause of inflammation. c. Inflammation is the body’s nonspecific response to tissue injury. d. Disorders are named using the ending -sarcoma to indicate inflammation. 66 | 67 | 70 51. Which of the following helps to localize and “wall off” the foreign material during an inflammatory response? 69 52. Why is an application of cold recommended as part of the RICE first aid measures immediately following an inflammatory response due to injury? a. Lymphocytes b. Increased fluid c. Fibrinogen d. Antibodies a. It improves circulation in the area removing chemical mediators. b. It causes local vasoconstriction to reduce local edema. c. It draws more phagocytic cells to the area to remove debris. d. It promotes immediate healing. 75 53. One goal for current research in tissue engineering is to: a. create a functional replacement tissue when regeneration is not possible. b. adapt cells from the injured organ to produce replacement tissue. c. design a nonliving synthetic replacement tissue. d. use stem cells as a temporary covering for damaged tissue. 76 54. Identify the proper sequence in the healing process. a. A blood clot forms; granulation tissue grows into the gap; new blood vessels develop; phagocytosis of for cell debris occurs; and collagen fibers form a tight, strong scar. b. A blood clot forms; phagocytes remove foreign material and cell debris; granulation tissue grows into the vessels form; and collagen fibers promote formation of a tight, strong scar. c. Collagen fibers form in the damaged area; a blood clot forms; granulation tissue grows into the gap; angio and foreign material and cell debris are removed by phagocytes. d. Foreign material and cell debris are removed by phagocytes; a blood clot forms; granulation tissue grows blood vessels form; and collagen fibers grow and cross-link. 76 55. All of the following are factors that promote healing EXCEPT: a. good nutrition: protein, vitamins A and C. b. a clean, undisturbed wound. c. effective circulation. d. advanced age. 77 56. Identify the correct statement about burns: a. The severity of the burn depends on the temperature, duration, and extent of the burn. b. Young children are less likely to suffer severe burns from immersion in excessively hot water. c. Burns to the palms of the hands are more damaging than burns on the face. d. With a major burn, excessive bleeding usually causes shock. 78 57. Which statement applies to the recommended emergency care for burns? a. Drop and lie completely still on your back. b. Call a neighbor for help if the burn appears to be extensive. c. Apply lotion and cover burn tightly with a sheet or towel. d. Cover the burn area with clean, cool, or tepid water and remove nonsticking clothing. 82 58. Inhalation of carbon monoxide is a threat for many burn patients because this gas: a. causes swelling in the trachea. b. quickly reduces the available oxygen in the blood. c. prevents full expansion of the lungs. d. is toxic to the nervous system. 82 59. Hypermetabolism is common with major burns because of: a. increased heat loss from the burn wound. b. demand for tissue repair. c. recurrent stress response. d. All of the above 83 60. How does scar tissue usually cause obstructions to develop in tube-like structures? a. Scar tissue continues to grow and spread, causing a blockage. b. Scar tissue does not stretch, but rather shrinks in time, causing narrowing. c. Scar tissue twists and forms knots as it develops. d. Scar tissue attaches to nearby normal tissue, causing obstruction. 78 61. Which of the following is a serious potential complication found only with the anti-inflammatory COX-2 inhibitor drugs? a. Increased risk of infection at the site of inflammation b. Reye’s syndrome developing in children and young adults c. Increased incidence of heart attacks d. Greatly delayed blood clotting 74 Chapter 06: Infection Chapter 06: Infection Test Bank MULTIPLE CHOICE 1. Bacteria that form an irregular cluster of spheres are called: a. bacilli. b. diplococci. c. staphylococci. d. streptococci. 89 2. A strict anaerobe requires which specific environment? a. A dry environment b. An acidic medium c. Air at a temperature less than 61° F/16° C d. The absence of oxygen 89 3. The presence of the bacterial capsule: a. aids in the release of endotoxins. b. protects the microbe from phagocytosis. c. increases the release of toxins and enzymes. d. prevents replication of the bacterium. 90 4. Microbial mutation means that: a. genetic information has changed. b. pathogens become nonpathogens. c. the microbe survives adverse conditions but can no longer replicate. d. the immune response to that microbe is strengthened. 101 5. A bacterial endospore can: a. also be classified as an acid-fast bacterium. b. exist in latent form inside a host cell. c. reproduce very rapidly. d. survive high temperatures and a dry environment. 96 6. The structure of a virus includes: a. a cell wall and membrane. b. metabolic enzymes for replication. c. a protein coat and either DNA or RNA. d. a slime capsule and cilia. 92 7. What method do viruses use to replicate? a. Binary fission b. Budding of a daughter cell from the parent viral cell c. Producing reproductive spores d. Using a host cell to produce and assemble components 92 8. A retrovirus such as HIV contains: a. RNA and enzymes for its conversion. b. a double strand of DNA. c. many enzymes to limit budding of new virions. d. numerous mitochondria. 92 9. How do antiviral drugs act? a. They interfere with cell wall development. b. They decrease cell membrane permeability. c. They destroy new, immature viral particles. d. They reduce the rate of viral replication. 107 10. Which statement applies to yeasts? a. They are usually considered to be pathogenic. b. They seldom contain a distinct nucleus. c. They may cause opportunistic infection in the body. d. They are normally not found in large numbers in resident flora. 96 11. Fungi reproduce by: 1. budding. 2. extension of hyphae. 3. binary fission. 4. production of spores. a. 1, 2 b. 2, 4 c. 1, 2, 4 d. 2, 3, 4 96 12. Which of the following is NOT classified as a protozoan agent of disease? a. Plasmodium vivax b. Trichomonas vaginalis c. Tinea pedis d. Entamoeba histolytica 96-97 13. Which of the following is a characteristic of rickettsia? a. It is a very small gram-negative intracellular microbe. b. It exists in three forms. c. It causes sexually transmitted disease. d. It reproduces by budding. 93 14. Entamoeba histolytica is transmitted by which of the following? a. Mosquitoes (bites) b. Inhaling contaminated particles c. Sexual intercourse d. Cysts in feces 97 15. Which of the following is a characteristic of resident or normal flora (microflora)? a. It exists in all areas of the body. b. Different species inhabit various areas of the body. c. It is of no benefit to the human host. d. It consists only of bacteria. 98 16. Which of the following is normally considered sterile? a. Urine b. Pharynx c. Distal urethra d. Vagina 99 17. The term nosocomial infection means: a. transmission involves an insect or animal host. b. acquired in a hospital or medical facility. c. transmitted by a fomite. d. spread by direct contact with secretions from an open lesion. 99 18. Transmission of microbes by direct contact includes: a. touching a contaminated countertop. b. sexual intercourse. c. drinking contaminated water. d. inhaling dust-borne microbes. 99 19. What does the term carrier mean? a. A person with active infection who acts as a reservoir for microbes b. Animals, insects, objects, or surfaces contaminated by pathogens c. An individual who is contagious through infected secretions on the hands d. An asymptomatic person whose body harbors pathogens and can transmit them to others 99 20. Opportunistic infection may develop when: a. pathogens enter the body but cannot colonize the site of entry. b. an imbalance occurs in the normal resident flora. c. host resistance increases, and the balance of resident flora is restored. d. contaminated food or water is unknowingly ingested. 99 21. Host resistance is promoted by all of the following EXCEPT: a. prescribed immunizations. b. chronic respiratory disease. c. vitamin and mineral supplements. d. appropriate inflammatory or immune response. 100-101 22. Which of the following factors would NOT increase the virulence of a specific microbe? a. Secretion of endotoxin b. Presence of a bacterial capsule c. Production of interferons d. Secretion of invasive enzymes 101 23. That time in the course of an infection when the infected person may experience a headache or fatigue and senses he or she is “coming down with something” is referred to as which of the following? 104 24. The principle of Universal Precautions is based on: a. using disinfectants at all times to eliminate cross-infections. b. not touching any open or bleeding lesions. c. sterilizing all instruments and equipment after each use. d. assuming that all body fluids from all individuals are possible sources of infection. 102 25. The “incubation period” refers to the time period between: a. entry of the pathogen into the body and the first signs of infectious disease. b. the onset of the prodromal period and the peak of the acute infection. c. the onset of clinical signs and signs of recovery from infection. d. the acute period and establishment of chronic infection. 104 a. Subclinical period b. Eclipse period c. Prodromal period d. Presymptomatic period 26. What does “bacteremia” refer to? a. Numerous pathogens circulating and reproducing in the blood b. Uncontrolled sepsis throughout the body c. Multiple infections, primary and secondary, established in the body d. Microbes present in the blood 105 27. Which of the following is a local sign of infection? a. Fever and leukocytosis b. Headache and anorexia c. Pain, erythema, and swelling d. Nausea, weight loss, and fatigue 105 28. What are culture and sensitivity tests used for? a. To determine the type of microbe present in an exudate b. To provide a specific medium that supports maximum microbial growth c. To identify the causative microbe and the effective antimicrobial agent for it d. To provide living host cells for microbes requiring such for replication 106 29. A broad-spectrum bactericidal agent would be expected to: a. destroy many gram-positive and gram-negative bacteria. b. destroy all pathogenic microbes in contact with the agent. c. reduce the replication of many bacteria. d. inhibit the growth of most spores and acid-fast bacteria. 107 30. How does penicillin act as a bactericidal agent? a. It interferes with cell-wall synthesis. b. It blocks protein synthesis. c. It increases cell membrane permeability. d. It prevents DNA replication. 107 31. Secondary infection may occur with administration of antibacterial drugs because the: a. patient is allergic to the drug. b. balance of species in the resident flora is upset. c. mucosa of the stomach is irritated. d. infecting microbes spread to adjacent areas. 107-108 32. All of the following are mechanisms of antiviral drug action EXCEPT: a. interference with attachment to host cell. b. block assembly of viral particles. c. interference with mitosis. d. shedding of protein coat. 108 33. Secondary bacterial infections occur frequently during influenza epidemics primarily because: a. antiviral drugs lower host resistance. b. the virus causes extensive tissue inflammation and necrosis. c. respiratory droplets transmit infections. d. the viral infection is usually self-limiting. 110 34. The primary pathological effect of influenza virus is: a. destruction of the mucosa in the lower respiratory tract. b. replication of the virus in respiratory secretions. c. destruction of leukocytes and macrophages in the lungs. d. inflammation and necrosis of the upper respiratory epithelium. 110 35. What does leukocytosis frequently indicate? a. Immunosuppression b. Bone marrow damage c. Presence of bacterial infection d. An allergic or autoimmune reaction 105 36. When an infection or inflammation is suspected, what does leucopenia often indicate? a. Bacterial infection b. Viral infection c. Allergic reaction d. Septicemia 106 37. Which of the following statements applies to Chlamydia? a. The microbe exists as a chain of cells. b. It causes a common STD. c. It possesses many flagella. d. It is excreted in feces. 93 38. Which of the following microbes is classified as an obligate intracellular parasite? a. Fungus b. Bacterium c. Virus d. Protozoa 93 39. Which of the following are characteristics of influenza virus? 1. It is an obligate intracellular parasite. 2. It contains RNA. 3. It usually causes nausea and vomiting. 4. There are three subtypes: A, B, C. a. 1, 4 b. 1, 3 c. 2, 3, 4 d. 1, 2, 4 93 40. The widespread necrosis of respiratory mucosa caused by an influenza infection often gives rise to: a. severe anemia. b. secondary infections. c. asthma. d. emphysema. 110 41. Prions cannot be cultured in a PETRI plate of media because: a. they take so long to grow. b. they require extensive amounts of specialized nutrients. c. they are proteinaceous particles, not living organisms. d. they are viruses that don’t grow on conventional media. 98 42. Which of the following statements applies to Influenza A H1N1? a. It alters human chromosomes to cause manifestations. b. It usually causes severe respiratory distress and high fever. c. Infection is common in the elderly. d. It contains genetic material from avian, swine, and human viruses. 93 43. Which of the following does NOT directly determine the virulence of a microbe? a. Capacity for opportunism b. Production of toxins c. Ability to mutate d. Invasive qualities 101 44. Which of the following is a function of interferons? a. They block the invasion of pathogenic bacteria. b. They reduce the inflammatory response to local infection. c. They increase host cell resistance to viral invasion. d. They may facilitate the spread of some cancer cells. 100 45. Inflamed tissue is likely to become infected because: a. the immune system is not effective in inflamed tissue. b. the increased fluid and protein in the inflamed area supports microbial growth. c. phagocytes cannot penetrate the inflamed areas. d. capillaries are less permeable in the affected area. 105 46. When an infectious disease is occurring globally at a higher rate than usual, it may be designated as a/an: a. sporadic occurrence. b. epidemic. c. pandemic. d. emerging disease. 99 47. Which of the following is the primary difference between an antiseptic and a disinfectant? a. Antiseptic is used on living tissue, whereas disinfectant is designed for nonliving surfaces. b. Antiseptic is much stronger than the potency of a disinfectant. c. Antiseptic often causes allergic skin reactions, whereas disinfectant is always hypoallergenic. d. Antiseptic is effective against endospores; disinfectants are not effective against endospores. 103-104 48. Drugs that are designed to inhibit or slow down growth of microbes but not necessarily kill them are considered: 107 Chapter 07: Immunity Chapter 07: Immunity Test Bank MULTIPLE CHOICE a. ineffective. b. bacteriostatic. c. narrow-spectrum. d. bactericidal. 115 1. Neutrophils: a. are phagocytic cells. b. produce histamine. c. produce antibodies. d. are elevated during an allergic response. 115 2. Which cells are required to process and present antigens from foreign material as the initial step in the immune response? 115 3. Humoral immunity is mediated by: a. natural killer cells. b. T lymphocytes (T cells). c. B lymphocytes (B cells). d. neutrophils. a. T–helper cells b. Macrophages c. Eosinophils d. Monocytes 122 4. A secondary immune response differs from the primary immune response in that: a. it is more rapid than the primary response and results in higher antibody levels. b. it is slower than the primary response and doesn’t change the antibody levels. c. it occurs at the same time as the primary response but results in a decrease in antibodies. d. it only occurs in hyperallergic reactions and results in a decrease of antibodies. 118 5. Which type of immunity is provided by a vaccination? a. Active natural b. Active artificial c. Passive natural d. Passive artificial 119 6. When an allergen binds with IgE antibodies on mast cells, resulting in release of chemical mediators, this reaction is called: a. cytotoxic hypersensitivity. b. immune complex hypersensitivity. c. type I hypersensitivity. d. type IV hypersensitivity. 124 7. The role of memory cells is to: a. change into an antibody-secreting cell following activation. b. immediately secrete antibodies following the first exposure to antigen. c. recognize the antigen and stimulate the immune response. d. bind complement to the antibody. 115 8. Which statement applies to contact dermatitis? a. It occurs when IgE antibodies on the skin react with the causative substance. b. It may result from ingested foods. c. Urticaria (hives) gradually spread over the body. d. A type IV reaction occurs in affected areas. 126 9. Which of the following causes anaphylaxis? a. A severe, systemic allergic reaction b. Type III hypersensitivity c. Cell-mediated hypersensitivity d. Immune complex deposits in many tissues 127 10. Following a positive HIV antibodies blood test and ELISA test, what is the test commonly used for confirmation? 135 11. Incompatible blood transfusions result in: a. hemolysis of erythrocytes. b. a type I immune response. c. deposits in multiple organs. d. immune deficiency. 124 12. An autoimmune disease is: a. excessive formation of antibodies following exposure to foreign material. b. an extreme response to normally harmless material in the environment. c. an abnormal response to ingested food and drugs. d. failure of the immune system to distinguish self from nonself. a. Agglutination b. Double immunodiffusion test c. Western blot test d. Sedimentation rate test 13. Systemic lupus erythematosus is caused by: a. a chronic allergic condition. b. development of an immune-deficient state. c. a deficiency of T lymphocytes. d. immune complex deposits of antinuclear antibodies. 127-128 14. Distinguishing clinical features of systemic lupus erythematosus include: a. inflammation in multiple organs. b. lack of a specific diagnostic blood test. c. acute onset and nonprogressive course. d. typical skin rash on the chest and back. 128 15. Which of the following are the target cells for HIV? a. Helper T lymphocytes (CD4 lymphocytes) b. B lymphocytes c. Natural killer cells d. Macrophages 130 | 131 16. A diagnosis of HIV positive means that: a. the number of T lymphocytes in the circulating blood is decreased. b. significant opportunistic infection is present in the body. c. the individual has AIDS. d. the virus and its antibodies are present in the blood. 131 17. HIV infection impairs: a. humoral immunity. b. cell-mediated immunity. c. both humoral and cell-mediated immunity. d. neither type of immunity. 133 18. Immunodeficiencies may result in an increased risk of infections by normally harmless microorganisms. These infections are referred to as: 134 19. Serious infections frequently occurring in patients with AIDS include: a. opportunistic. b. prophylactic. c. abnormal. d. transient. 1. tuberculosis. 2. Pneumocystis carinii pneumonia. 3. influenza. 4. tetanus. a. 1, 2 b. 1, 4 c. 2, 3 d. 3, 4 135 20. Which of the following statements does NOT apply to major histocompatibility complex (MHC) proteins or molecules? 114 21. CD4-positive helper T cells function by: a. direct cytotoxic action. b. facilitating all immune system activity. a. They are genes on chromosome 6. b. All members of a family have identical MHCs. c. They alert the immune system to virus-infected cells. d. A close match is essential for successful tissue transplants. c. producing immunoglobulins. d. inactivating allergens. 117 22. Host-versus-graft disease refers to: a. hyperacute rejection of tissue. b. T cells in grafted tissue attacking host cells. c. infection resulting from immunosuppression therapy. d. transplant rejection by the recipient’s immune system. 121 23. Which of the following complications does NOT occur frequently in AIDS patients? a. Kaposi’s sarcoma b. Wasting syndrome c. Lymphoma d. Polyarthritis 135-136 24. Which of the following characteristics apply to HIV? 1. It contains two strands of DNA. 2. It tends to mutate frequently to form new strains. 3. The incubation period is extremely short. 4. It is inactivated by heat and many disinfectants. a. 1, 2 b. 1, 3 c. 2, 4 d. 3, 4 135 | 137 25. In cases of HIV infection, the “window period” refers to the time between: a. entry of the virus into the blood and the initial manifestations. b. entry of the virus into the body and the appearance of antibodies in the blood. c. entry of the virus into the body and a significant drop in CD4 T-helper lymphocyte count. d. diagnosis of “HIV positive” and diagnosis of “AIDS.” 133 26. Which of the following is an effect of cytokines? They: a. activate and stimulate proliferation of B and T lymphocytes. b. destroy antigens quickly. c. increase the rate of mitosis in tumors. d. cause immediate pain. 115 27. What does seroconversion mean in relation to HIV and AIDS? a. The virus has been identified in the blood and body fluids. b. Antibodies for HIV have been identified in the blood. c. HIV was found in lymphocytes. d. Active infection has developed in the patient. 119 | 132 28. Which of the following statements is TRUE regarding a patient who is HIV positive? a. No medication is required until the CD4 cell count drops below normal range. b. Antibodies are present, destroying the virus and preventing transmission to others. c. Antibodies in the blood indicate presence of virus and possible transmission to others. d. Enzymes have not yet converted RNA to DNA for replication. 134 29. The term tolerance refers to: a. surveillance and destruction of new cancer cells by the immune system. b. the ability of the immune system to ignore “self” cells. c. the ability of T and B lymphocytes to work together. d. the role of lymphoid tissue in the body defenses. 118 30. Which of the following statements applies to the complement system? a. It is activated by IgE. b. It blocks the inflammatory response. c. It consists of proteins in the blood that must be activated. d. It may destroy antibodies in the circulation. 118 31. Which of the following statements regarding immunoglobulins is TRUE? a. They consist of a unique sequence of amino acids. b. They are produced in the red bone marrow. c. They are attached to mucosal membranes at entry points into the body. d. IgA binds to allergens. 117 32. Which of the following is NOT a cause of immunodeficiency? a. Hypoplasia of the thymus b. Delayed hypersensitivity c. Immunosuppressive drugs d. Atrophy of the lymph nodes 130 33. Which statement is TRUE regarding infants born to HIV-infected mothers? a. Infants usually test negative for HIV after birth. b. There is little risk of infected mothers passing the virus to their infants during delivery. c. Breast milk does not contain HIV or antibodies. d. Infants test positive for HIV because of the presence of maternal antibodies. 134 34. The most common cause of death in patients who have AIDS is: a. HIV encephalopathy. b. tuberculosis. c. Pneumocystis carinii pneumonia. d. Candida infection. 135 35. Tissue transferred between two genetically identical twins is referred to as a/an: a. allograft. b. syngraft. c. isograft. d. autograft. 121 Chapter 08: Skin Disorders Chapter 08: Skin Disorders Test Bank MULTIPLE CHOICE 1. Which of the following areas lacks blood vessels and nerves? a. Epidermis b. Dermis c. Subcutaneous tissue d. Fatty tissue 142 2. What is a raised, thin-walled lesion containing clear fluid called? a. Papule b. Pustule c. Vesicle d. Macule 143 3. Which of the following is a common effect of a type I hypersensitivity response to ingested substances? a. Contact dermatitis b. Urticaria c. Discoid lupus erythematosus d. Psoriasis 145 4. What change occurs in the skin with psoriasis? a. Recurrent hypersensitivity reactions b. Autoimmune response c. Increased mitosis and shedding of epithelium d. Basal cell degeneration 147 5. Which of the following best describes the typical lesion of psoriasis? a. Purplish papules that can erode and become open ulcers b. Firm, raised pruritic nodules that can become cancerous c. Moist, red vesicles, which develop into bleeding ulcers d. Begins as a red papule and develops into silvery plaques 147 6. Why do secondary infections frequently develop in pruritic lesions? a. Loss of protective sebum b. Entry of resident flora while scratching the lesion c. Blockage of sebaceous glands d. Increased sweat production 148 7. Which disease is considered an autoimmune disorder? a. Pemphigus b. Erysipelas c. Contact dermatitis d. Scleroderma 147 8. Which of the following skin lesions are usually caused by Staphylococcus aureus? a. Furuncles b. Verrucae c. Scabies d. Tinea 148 9. Which of the following statements applies to impetigo? a. Lesions usually appear on the hands and arms. b. The cause is usually a virus. c. The infection is highly contagious. d. Scar tissue is common following infection. 148 10. What is the common signal that a recurrence of herpes simplex infection is developing? a. Severe pain around the mouth b. Malaise and fatigue c. Fever and severe headaches d. Mild tingling along the nerve or on the lips 150 11. Herpes virus is usually spread by all of the following EXCEPT: a. saliva during an exacerbation and for a short time thereafter. b. contact with the fluid in the lesion. c. contaminated blood. d. autoinoculation by fingers. 150 12. How are antiviral drugs effective in treating a viral infection? a. They destroy the virus if administered for at least 2 weeks. b. They limit the acute stage and viral shedding. c. They prevent any systemic effects of viruses. d. They prevent any secondary bacterial infection. 150 13. Tinea capitis is an infection involving the: a. trunk. b. feet. c. scalp. d. nails. 150 14. Plantar warts are caused by: a. the fungus aspergillus. b. a parasitic arthropod. c. human papillomavirus. d. the bacterium Streptococcus pyogenes. 150 15. Which of the following statements regarding acute necrotizing fasciitis is TRUE? a. Infection is localized in a small area of the epidermis. b. It is usually caused by S. aureus. c. Spontaneous recovery usually occurs in 48 hours. d. Infection rapidly causes extensive tissue necrosis and toxic shock. 149 16. Which type of microbe causes Tinea infections? a. Fungus b. Virus c. Gram-negative bacterium d. Mite 150 17. What causes the pruritus associated with scabies? a. An allergic reaction to the causative microbe due to endotoxins b. Mites burrowing into the epidermis and reaction to their feces c. Bleeding and injected toxin from bites of the larvae d. Neurotoxins secreted by mites on the skin surface 152-153 18. How can pediculosis be diagnosed? a. Pruritus in hairy areas of the body b. Loss of blood due to lice bites c. Finding lice in clothing d. The presence of nits at the base of hair shafts 153 19. What is the major predisposing factor to squamous cell carcinoma? a. Viral infection b. Presence of nevi (moles) on the skin c. Exposure to ultraviolet light d. Frequent hypersensitivity reactions 154 20. All of the following statements apply to malignant melanoma EXCEPT: a. The malignant cell is a melanocyte. b. They present as non-pruritic purplish macules. c. The neoplasm grows rapidly and metastasizes early. d. The lesion is usually dark or multicolored with an irregular border. 155 21. Which of the following factors has contributed to the increased incidence of Kaposi’s sarcoma? a. Excessive sun exposure b. Increased number of nevi c. Increase in immunosuppressed individuals d. Presence of more seborrheic keratoses 155 22. Which of the following applies to actinic keratoses? a. They predispose to malignant melanoma. b. They arise on skin exposed to ultraviolet radiation. c. They occur primarily on dark-skinned persons. d. They are malignant and invasive. 154-155 23. Which lesion distinguishes Tinea corporis? a. Small, brown pruritic lines b. Painful and pruritic fissures c. Erythematous ring of vesicles with a clear center d. Firm, red, painful nodule or pustule 150 24. Systemic effects of acute necrotizing fasciitis include: a. low-grade fever and malaise. b. toxic shock and disorientation. c. mild nausea and vomiting. d. headache and difficulty breathing. 149 25. The cause of contact dermatitis can often be identified by: a. using a culture and sensitivity test on the exudate. b. checking the frequency of the exacerbations. c. noting the location and size of the lesion. d. the type of pain associated with the lesion. 145 26. The pathological change associated with scleroderma is: a. abnormal activation of T lymphocytes and an increase of cytokines. b. an autoimmune reaction damaging the epidermis. c. collagen deposits in the small blood vessels of the skin and sometimes the viscera. d. Type I hypersensitivity and increased serum IgE levels. 147 27. Choose the best description of the typical lesion of impetigo. a. Large, red, painful nodule filled with purulent exudates b. Small vesicles that rupture to produce a crusty brown pruritic mass c. Red, swollen, painful areas often with projecting red streaks d. Firm, raised papules that may have a rough surface and may be painful 149 28. Choose the correct match of the skin condition and its usual location. a. Scabies—fingers, wrists, waist b. Impetigo—legs, feet c. Pediculosis humanus corporis—scalp d. Seborrheic keratosis—feet, hands 153 29. Leprosy (Hansen’s disease) is caused by: a. a fungus. b. a bacterium. c. a virus. d. a helminth. 149 30. One factor that is responsible for increasing the mortality rate among patients suffering with necrotizing fasciitis is: a. a delay in initial diagnosis. b. lack of proper antibiotics. c. the appearance of additional opportunistic infections. d. secondary fungal infections. 149 Chapter 09: Musculoskeletal Disorders Chapter 09: Musculoskeletal Disorders Test Bank MULTIPLE CHOICE 1. Which of the following cells produce new bone? a. Osteocytes b. Osteoblasts c. Osteoclasts d. Stem cells from the bone marrow 159 2. What is the chemical transmitter released at the neuromuscular junction? a. Norepinephrine b. GABA c. Serotonin d. Acetylcholine 161 3. What are the two types of bone tissue? a. Vascular and nonvascular b. Spongy and calcified c. Compact and cancellous d. Dense and pliable 159 4. Which of the following would identify an open or compound fracture? a. The skin and soft tissue are exposed at the fracture site. b. A bone is crushed into many small pieces. c. The bone appears bent with a partial fracture line. d. One end of a bone is forced into an adjacent bone. 164 5. Which of the following describes a Colles’ fracture? a. The distal radius is broken. b. The distal fibula is broken. c. A vertebra appears crushed. d. A spontaneous fracture occurs in weakened bone. 165 6. During the fracture healing process, the hematoma: a. is broken down and absorbed immediately. b. provides the base for bone cells to produce new bone. c. is the structure into which granulation tissue grows. d. produces fibroblasts to lay down new cartilage. 166 7. When a fracture is healing, the procallus or fibrocartilaginous callus: a. can bear weight. b. serves as a splint across the fracture site. c. is the tissue that lays down new cartilage. d. is made up of new bone. 166 8. The inflammation surrounding a fracture site during the first few days may complicate healing by causing: 166-167 9. What is a sign of a dislocation? a. excessive bone movement. b. severe ischemia and tissue necrosis. c. malunion or nonunion. d. fat emboli to form. a. Crepitus b. Pain and tenderness c. Increased range of motion at a joint d. Deformity at a joint 168 10. All of the following predispose to osteoporosis EXCEPT: a. weight-bearing activity. b. a sedentary lifestyle. c. long-term intake of glucocorticoids. d. calcium deficit. 169 11. Which of the following statements does NOT apply to osteoporosis? a. Bone resorption is greater than bone formation. b. It causes compression fractures of the vertebrae. c. Osteoporosis is always a primary disorder. d. It often leads to kyphosis and loss of height. 169 12. Which of the following best describes the typical bone pain caused by osteogenic sarcoma? a. Intermittent, increasing with activity b. Sharp, increased with joint movement c. Mild, aching when weight-bearing d. Steady, severe, and persisting with rest 171 13. How is Duchenne’s muscular dystrophy inherited? a. Autosomal recessive gene b. X-linked recessive gene c. Autosomal dominant gene d. Codominant gene 172 14. Which of the following is true about Duchenne’s muscular dystrophy? a. There is difficulty climbing stairs or standing up at 2 to 3 years of age. b. It involves only the legs and pelvis. c. Skeletal muscle atrophy can be seen in the legs of a toddler. d. It cannot be detected in any carriers. 172 15. The most common type of joint, which are freely movable, are called: a. Synarthroses b. Amphiarthroses c. Anarthroses d. Diarthroses 163 16. Which of the following is characteristic of osteoarthritis? a. Inflammation and fibrosis develop at the joints. b. Degeneration of articulating cartilage occurs in the large joints. c. It progresses bilaterally through the small joints. d. There are no changes in the bone at the affected joints. 173-174 17. What is a typical characteristic of the pain caused by osteoarthritis? a. Decreases over time b. Quite severe in the early stages c. Aggravated by general muscle aching d. Increased with weight-bearing and activity 174 18. What limits joint movement in osteoarthritis? a. The osteophytes and irregular cartilage surface b. The wider joint space c. Decreased amount of synovial fluid in the cavity d. Fibrosis involving the joint capsule and ligaments 174 19. Joints affected by osteoarthritis can sometimes affect healthy joints by: a. causing enzymes to be released that travel to other joints. b. bacteria traveling from the affected join to a healthy one through the bloodstream. c. inflammation and edema affecting the entire limb. d. the affected individual’s exerting stress on the normal joint to protect the damaged one. 174 20. What is the typical joint involvement with rheumatoid arthritis? a. Random single joints, progressing to involve other joints b. Bilateral small joints, symmetrical progression to other joints c. Abused or damaged joints first, then joints damaged by compensatory movement d. Progressive degeneration in selected joints 177 21. What is the basic pathology of rheumatoid arthritis? a. Degenerative disorder involving the small joints b. Chronic inflammatory disorder affecting all joints c. Systemic inflammatory disorder due to an autoimmune reaction d. Inflammatory disorder causing damage to many organs 175-177 22. How is the articular cartilage damaged in rheumatoid arthritis? a. Enzymatic destruction by the pannus b. Inflamed synovial membrane covers the cartilage c. Fibrous tissue connects the ends of the bones d. Blood supply to the cartilage is lost 175 23. How does the joint appear during an exacerbation of rheumatoid arthritis? a. Relatively normal b. Enlarged, firm, crepitus with movement c. Deformed, pale, and nodular d. Red, warm, swollen, and tender to touch 177 24. Ankylosis and deformity develop in rheumatoid arthritis because: a. skeletal muscle hypertrophies. b. fibrosis occurs in the joint. c. replacement cartilage changes alignment. d. ligaments and tendons shorten. 176 25. Systemic effects of rheumatoid arthritis are manifested as: a. nodules in various tissues, severe fatigue, and anorexia. b. headache, leukopenia, and high fever. c. swelling and dysfunction in many organs. d. progressive damage to a joint. 176 26. What is a common effect of long-term use of glucocorticoids to treat rheumatoid arthritis? a. Leukocytosis b. Osteoporosis c. Severe anemia d. Orthostatic hypotension 177 27. Juvenile rheumatoid arthritis (JRA) differs from the adult form in that: a. only small joints are affected. b. rheumatoid factor is not present in JRA, but systemic effects are more severe. c. onset is more insidious in JRA. d. deformity and loss of function occur in most children with JRA. 177 28. Which of the following distinguishes septic arthritis? a. Multiple joints that are swollen, red, and painful at one time b. Presence of mild fever, fatigue, and leukocytosis c. Purulent synovial fluid present in a single, swollen joint d. Presence of many antibodies in the blood 178 29. Which of the following may precipitate an attack of gout? a. A sudden increase in serum uric acid levels b. Severe hypercalcemia c. Mild trauma to the toes d. Development of a tophus 178 30. Where does inflammation usually begin in an individual with ankylosing spondylitis? a. Costovertebral joints with progression down the spine b. Cervical and thoracic vertebrae, causing kyphosis c. Sacroiliac joints with progression up the spine d. Peripheral joints and then proceeds to the vertebrae 178 31. What is a common outcome of fibrosis, calcification, and fusion of the spine in ankylosing spondylitis? 178-179 32. Which statement applies to menisci? a. They are found in the hip joints. b. They are secretory membranes in joints. c. They prevent excessive movement of joints. d. They are found in the shoulder joint. 163 33. Which factors delay healing of bone fractures? a. Damage to the spinal nerves and loss of function b. Frequent fractures of long bones c. Impaired heart function d. Rigidity, postural changes, and osteoporosis 1. Lack of movement of the bone 2. Prolonged inflammation and ischemia 3. Presence of osteomyelitis 4. Close approximation of bone ends a. 1, 2 b. 1, 3 c. 2, 3 d. 3, 4 166-167 34. What is the likely immediate result of fat emboli from a broken femur? a. Additional ischemia in the broken bone b. Nonunion or malunion of the fracture c. Pulmonary inflammation and obstruction d. Abscess and infection at a distant site 167 35. A sprain is a tear in a: a. ligament. b. tendon. c. skeletal muscle. d. meniscus. 168 36. Therapeutic measures for osteoporosis include: a. non–weight-bearing exercises. b. dietary supplements of calcium and vitamin D. c. transplants of osteoblasts. d. avoidance of all hormones. 170 37. What is the distinguishing feature of primary fibromyalgia syndrome? a. Joint pain and stiffness throughout the body b. Degeneration and atrophy of skeletal muscles in back and lower limbs c. Localized areas of constant pain d. Specific trigger points for pain and tenderness 173 38. Ewing’s sarcoma metastasizes at an early stage to the: a. brain. b. liver. c. lungs. d. other bones. 171 39. Immovable joints are called: a. amphiarthroses. b. synarthroses. c. diarthroses. d. synovial joints. 163 40. Rickets results from: a. excessive bone resorption by osteoclasts. b. a deficit of vitamin D and phosphates. c. replacement of bone by fibrous tissue. d. hyperparathyroidism. 170 41. Paget’s disease often leads to which of the following? a. A reduction in bone fractures b. Decreased intracranial pressure c. Cardiovascular disease d. Disintegration of joint cartilage 170 42. Bones classified as “irregular” would include: a. skull bones. b. the mandible. c. wrist bones. d. the femur. 159 43. A dislocation is: a. the tearing of a tendon in the joint. b. the separation of bones in the joint with a loss of contact. c. the twisting of a joint, causing excessive inflammation of the surrounding tissue. d. the overstressing of ligaments, causing loss of elasticity. 167 44. A diagnostic test that measures the electrical charge of muscle contraction and can help differentiate muscle disorders from neurological disease is a/an: a. electromyogram. b. arthroscopy. c. radiograph. d. electroencephalograph. 164 45. The type of compound fracture in which there are multiple fracture lines and bone fragments is referred to as a/an: 164 46. Fluid-filled sacs composed of synovial membrane located between structures such as tendons and ligaments and act as additional cushions are called: 179 Chapter 10: Blood and Circulatory System Disorders Chapter 10: Blood and Circulatory System Disorders Test Bank a. compression fracture. b. greenstick fracture. c. simple fracture. d. comminuted fracture. a. articular capsules. b. bursae. c. synovial sacs. d. hyaline chambers. MULTIPLE CHOICE 1. Which of the following would result from a reduced number of erythrocytes in the blood? a. Increased hemoglobin in the blood b. Decreased hematocrit c. Increased risk of hemostasis d. Decreased osmotic pressure of the blood 185 2. What term is used to describe a deficit of all types of blood cells? a. Leucopenia b. Neutropenia c. Pancytopenia d. Erythrocytosis 205 3. Capillary walls consist of: a. multiple endothelial layers. b. a thick layer of smooth muscle. c. two or three epithelial layers. d. a single endothelial layer. 183 4. Vitamin K is required by the liver to synthesize: a. heparin. b. prothrombin. c. amino acids. d. bilirubin. 190 | 202 5. Individuals with type O blood are considered to be universal donors because their blood: a. contains A and B antibodies. b. contains A and B antigens. c. lacks A and B antibodies. d. lacks A and B antigens. 192 6. What are the two circulations that comprise the overall circulatory system? a. Pulmonary and systemic circulations b. Peripheral and central circulations c. Cardiovascular and lymphatic circulations d. Cardiopulmonary and peripheral circulations 183 7. Chronic blood loss causes anemia because of the: a. shortened life span of the erythrocytes. b. lower metabolic rate. c. loss of protein and electrolytes. d. smaller amount of recycled iron available. 193 8. What is the cause of sickle cell anemia? a. A defective gene inherited from both parents b. A chronic bacterial infection c. Bone marrow depression d. An autoimmune reaction 198 9. Which of the following best describes the characteristic erythrocyte associated with pernicious anemia? 201 a. Hypochromic, microcytic b. Normochromic, normocytic c. Elongated, sickle-shaped d. Megaloblastic or macrocytic nucleated cells 10. What causes numbness and tingling in the fingers of individuals with untreated pernicious anemia? 195 11. Jaundice is one typical sign of: a. sickle cell anemia. b. aplastic anemia. c. iron deficiency anemia. d. acute leukemia. 198 12. What are the typical early general signs and symptoms of anemia? a. Chest pain, palpitations b. Jaundice, stomatitis c. Pallor, dyspnea, and fatigue d. Bradycardia, heat intolerance 193 a. Persistent hyperbilirubinemia b. Increasing acidosis affecting metabolism c. Vitamin B12 deficit causing peripheral nerve demyelination d. Multiple small vascular occlusions affecting peripheral nerves 13. What is the cause of oral ulcerations and delayed healing occurring with any severe anemia? a. Lack of folic acid for DNA synthesis b. Frequent microinfarcts in the tissues c. Deficit of oxygen for epithelial cell mitosis and metabolism d. Elevated bilirubin levels in blood and body fluids 193 14. Which of the following is present with pernicious anemia? a. Pancytopenia b. Hypochlorhydria c. Leukocytosis d. Multiple infarcts 195 15. Why is pernicious anemia treated with injections of vitamin B12? a. An immune reaction in the stomach would destroy the vitamin. b. Digestive enzymes would destroy the vitamin. c. The vitamin irritates the gastric mucosa. d. The ingested vitamin would not be absorbed into the blood. 195 16. Why do abnormally low hemoglobin values develop with pernicious anemia? a. Decreased production of erythrocytes b. Shorter life span of erythrocytes c. Abnormal structure of hemoglobin chains d. Deficit of folic acid 195 17. What are the common early signs of aplastic anemia? a. Painful joints and skeletal deformity b. Abdominal discomfort and splenomegaly c. Excessive bleeding and recurrent infections d. Palpitations and chest pain 197 18. Why do vascular occlusions and infarcts occur frequently with sickle cell anemia? a. The red blood cells are abnormally large. b. Increased hemolysis of erythrocytes occurs. c. Erythrocytes change to sickle shape when hypoxia occurs. d. HbS is unable to transport oxygen. 199 19. Which of the following applies to sickle cell trait? a. Most hemoglobin is in the form of HgS b. Sickling of erythrocytes occurs with severe hypoxia. c. Painful sickling crises with multiple infarctions occur frequently. d. A child’s skeletal growth is delayed. 198 20. What is the basic abnormality in thalassemia? a. Several amino acids in the globin chains have been replaced by substitute amino acids. b. More than four globin chains are found in the erythrocytes. c. The iron molecule is displaced in hemoglobin. d. There is failure to synthesize either the alpha or beta chains in the hemoglobin molecule. 200 21. Which of the following can result from a malabsorption problem? a. Aplastic anemia b. Sickle cell anemia c. Thalassemia major d. Pernicious anemia 195 22. In individuals with pernicious anemia, antibodies form to: a. vitamin B12. b. intrinsic factor or parietal cells. c. mucus-producing glands. d. hydrochloric acid. 195 23. In cases of polycythemia vera, blood pressure is elevated as a result of: a. increased blood volume. b. frequent infarcts in the coronary circulation. c. congested spleen and bone marrow. d. increased renin and aldosterone secretions. 205 24. Petechiae and purpura are common signs of: a. excessive hemolysis. b. leucopenia. c. increased bleeding. d. hemoglobin deficit. 201 25. Which statement applies to the disorder hemophilia A? a. It is transmitted as an X-linked dominant trait. b. There is usually a total lack of factor VIII in the blood. c. Males and females can be carriers. d. Hematomas and hemarthroses are common. 203 26. Which of the following occurs when disseminated intravascular coagulation develops? a. Increased thrombocytes and blood clotting b. Hemolysis with loss of blood cells c. Massive sepsis and hemorrhage d. Multiple thrombi and deficit of clotting factors 203-204 27. Which of the following substances acts as an anticoagulant? a. Prothrombin b. Heparin c. Fibrinogen d. Vitamin K 190 28. In individuals with acute leukemia, the increased number of malignant leukocytes leads to: 1. decreased hemoglobin. 2. thrombocytopenia. 3. bone pain with increased activity. 4. splenomegaly. a. 1, 3 b. 1, 2, 4 c. 2, 3, 4 d. 1, 2, 3, 4 206-208 29. Multiple opportunistic infections develop with acute leukemia primarily because: a. the number of white blood cells is decreased. b. many circulating leukocytes are immature. c. severe anemia interferes with the immune response. d. decreased appetite and nutritional intake reduce natural defenses. 206-207 30. Why is excessive bleeding a common occurrence with acute leukemia? a. Deficit of calcium ions b. Impaired production of prothrombin and fibrinogen c. Decreased platelets d. Dysfunctional thrombocytes 206-207 31. Predisposing factors to leukemia commonly include: a. exposure to radiation. b. certain fungal and protozoal infections. c. familial tendency. d. cigarette smoking. 207 32. Von Willebrand disease is caused by: a. defective erythrocytes that become deformed in shape, causing occlusions. b. excessive lymphocytes that do not mature. c. absence of a clotting factor that helps platelets clump and stick. d. a lack of hemoglobin due to iron deficiency. 203 33. Thrombophilia can result in conditions such as: a. severe chronic kidney disease. b. peripheral vascular disease. c. deficient calcium levels in the long bones. d. excessive bleeding of hematomas. 204 34. Multiple myeloma is a malignant tumor involving: a. plasma cells. b. granulocytes. c. bone cells. d. lymph nodes. 209 35. What is the primary treatment for the leukemias? a. Radiation b. Chemotherapy c. Surgery d. Immunotherapy 207 36. Which of the following statements applies to hemochromatosis. It is: a. caused by excessive iron intake in the diet. b. results from excessive hemolysis of RBCs. c. a metabolic error that leads to excess amounts of hemosiderin, causing damage to organs. d. an inherited defect that results in abnormal hemoglobin. 188 37. Thalassemia is caused by: a. a defect in one or more genes for hemoglobin. b. an abnormal form of heme. c. abnormal liver production of amino acids and iron. d. overproduction of hypochromic, microcytic RBCs. 200 38. Secondary polycythemia may be associated with: a. frequent angina attacks. b. certain types of anemia. c. severe chronic bronchitis. d. renal disease. 205 39. All of the following apply to vitamin K EXCEPT: a. it is used as an antidote for warfarin (Coumadin). b. the liver requires it to produce prothrombin. c. it is a fat-soluble vitamin. d. the bone marrow requires it to synthesize hemoglobin. ANS REF:189 | 190 | 202 40. Leukemia is sometimes linked to chromosome abnormalities, as evidenced by: a. the presence of Philadelphia chromosome translocation in cases of acute myelogenous leukemia (AML). b. very low incidence in persons with Down syndrome. c. little evidence of familial incidence. d. transmission as a recessive gene. 206-207 41. Iron deficiency anemia frequently results from any of the following EXCEPT: a. certain vegetarian diets. b. excessive menstrual flow. c. malabsorption syndromes. d. diabetes mellitus. 193 42. Which of the following applies to the leukemias? a. Chronic leukemias are more common in older people. b. AML is the most common childhood leukemia. c. Exposure to chemicals is not considered a predisposing factor. d. Lymphoid tissue produces abnormal leukocytes. 207 43. A high percentage of blast cells in the leukocyte population indicates a poor prognosis for an individual with: a. thalassemia. b. acute myelogenous leukemia (AML). c. myelodysplastic syndrome. d. multiple myeloma. 208 44. Which of the following applies to erythropoietin? a. It is produced by the liver. b. It increases iron absorption for heme production. c. It stimulates production of red blood cells. d. Hypoxia stimulates the red bone marrow to produce erythropoietin. 187 | 192 45. Which of the following diagnostic tests would be within the normal range for an individual with hemophilia A? 192 46. Which of the following applies to the condition disseminated intravascular coagulation (DIC)? a. Bleeding time b. Coagulation time c. PTT time d. Prothrombin time a. It is usually a secondary complication. b. It is always initiated by excessive bleeding. c. It results in an inability of platelets to adhere. d. It is not life threatening. 203-204 47. In which blood dyscrasia does pancytopenia develop? a. Pernicious anemia b. Aplastic anemia c. Iron deficiency anemia d. Sickle cell anemia 205 48. Which of the following applies to the etiology of aplastic anemia? It is: a. idiopathic in many cases. b. a genetic disorder. c. predisposed by exposure to myelotoxins. d. Both A and C. 197 49. Microcytic and hypochromic erythrocytes are commonly found as a result of: a. iron deficiency anemia. b. polycythemia. c. disseminated intravascular coagulation. d. hemophilia A. 201 Chapter 11: Lymphatic System Disorders Chapter 11: Lymphatic System Disorders Test Bank MULTIPLE CHOICE 1. The spleen has a number of important functions, which include: a. lymph production, hematopoiesis, platelet production. b. hematopoiesis, destruction of old erythrocytes, blood reservoir. c. defense from infection, metabolism of vitamins, platelet production. d. lipid metabolism, production of hemoglobin, water absorption. 213 2. The function of the hormones secreted by the thymus gland is to: a. break down old erythrocytes and recycle the hemoglobin. b. concentrate the lymph and filter out toxins. c. stimulate lymph production. d. enable lymphocytes to develop into mature T cells. 214 3. Malignant neoplasms involving lymphocyte proliferation in the lymph nodes are called: a. lymphomas b. myelomas c. lymphocytomas d. lymphedemas 216 4. The atypical cell that serves as a marker for diagnosing Hodgkin’s lymphoma is the: a. monocyte. b. Ann Arbor cell c. Hodgkin’s lymphocyte d. Reed-Sternberg cell 216 5. The staging system typically used in determining the stage of the Hodgkin’s lymphoma is the: a. Reed-Sternberg system. b. sequential staging system. c. Ann Arbor system. d. differential landmark system. 216 6. One of the reasons non-Hodgkin’s lymphomas are harder to treat than Hodgkin’s lymphomas is that they: 216 7. Multiple myeloma is a neoplastic disease of unknown etiology occurring in older adults and involving: 219 8. Elephantiasis, caused by the obstruction of lymphatic vessels by parasitic worms, is an example of the condition known as: a. tend to be much larger than Hodgkin’s lymphomas. b. involve multiple nodes and widespread metastases. c. are not affected by the newer drug treatments. d. are asymptomatic until they reach stage IV. a. plasma cells. b. T cells. c. NK cells. d. monocytes. a. plasma cell myeloma. b. diverticulitis. c. lymphedema. d. obstructive vessel disorder. 219-220 9. A rare illness that involves the overgrowth of lymphoid tissue, although not itself considered a cancer is: 220 10. Non-Hodgkin’s lymphomas are increasing in incidence, partly due to the numbers associated with: 216 a. Castleman disease. b. hyperlymphatic disease. c. hypolymphatic disease. d. Ann Arbor disease. a. an increase in resistant microorganisms. b. an increase in adult obesity. c. an increase in high cholesterol levels. d. an increase in HIV infections. Chapter 12: Cardiovascular System Disorders Chapter 12: Cardiovascular System Disorders Test Bank MULTIPLE CHOICE 1. Which of the following actions causes the atrioventricular (AV) valves to close? a. Increased intraventricular pressure b. Depolarization at the AV node c. Ventricular relaxation and backflow of blood d. Contraction of the atria 227 2. When stroke volume decreases, which of the following could maintain cardiac output? a. Decreased peripheral resistance b. Increased heart rate c. Decreased venous return d. General vasodilation 228 3. Which of the following describes the pericardial cavity? a. It contains sufficient fluid to provide a protective cushion for the heart. b. It is a potential space containing a very small amount of serous fluid. c. It is lined by the endocardium. d. It is located between the double-walled pericardium and the epicardium. 224 4. Which of the following factors greatly improves venous return to the heart during strenuous exercise? 224 5. The function of the baroreceptors is to: a. stimulate the parasympathetic or sympathetic nervous system at the sinoatrial (SA) node as needed. b. adjust blood pressure by changing peripheral resistance. c. sense a change in blood oxygen and carbon dioxide levels. d. signal the cardiovascular control center of changes in systemic blood pressure. 225 6. The normal delay in conduction through the AV node is essential for: a. preventing an excessively rapid heart rate. b. limiting the time for a myocardial contraction. a. Rapid emptying of the right side of the heart b. Forceful action of the valves in the veins c. Contraction and relaxation of skeletal muscle d. Peristalsis in the large veins c. allowing the ventricles to contract before the atria. d. completing ventricular filling. 225 7. Which of the following is a result of increased secretion of epinephrine? a. Increased heart rate and force of contraction b. Decreased stimulation of the SA node and ventricles c. Vasoconstriction in skeletal muscles and kidneys d. Vasodilation of cutaneous blood vessels 225 8. Which of the following causes increased heart rate? a. Stimulation of the vagus nerve b. Increased renin secretion c. Administration of beta-blocking drugs d. Stimulation of the sympathetic nervous system 230 9. The event that causes the QRS wave on an electrocardiogram (ECG) tracing is: a. atrial depolarization. b. atrial repolarization. c. ventricular depolarization. d. ventricular repolarization. 225 10. The cardiac reserve is: a. afterload. b. the difference between the apical and radial pulses. c. the ability of the heart to increase cardiac output when needed. d. the extra blood remaining in the heart after it contracts. 228 11. The term preload refers to: a. volume of venous return. b. peripheral resistance. c. stroke volume. d. cardiac output. 228 12. The first arteries to branch off the aorta are the: a. common carotid arteries. b. pulmonary arteries. c. coronary arteries. d. subclavian arteries. 226 13. Cardiac output refers to: a. the amount of blood passing through either of the atria. b. the volume of blood ejected by a ventricle in one minute. c. the volume of blood ejected by each ventricle in a single contraction. d. the total number of heartbeats in one minute. 228 14. Vasodilation in the skin and viscera results directly from: a. decreased blood pressure. b. increased parasympathetic stimulation. c. relaxation of smooth muscle in the arterioles. d. increased stimulation of alpha-adrenergic receptors. 229-230 15. Which of the following drugs decrease sodium and fluid retention in the body? a. warfarin (Coumadin) b. digoxin (Lanoxin) c. nitroglycerin (Isordil) d. hydrochlorothiazide (HydroDIURIL) 233 16. Which of the following are predisposing factors to thrombus formation in the circulation? 1. Decreased viscosity of the blood 2. Damaged blood vessel walls 3. Immobility 4. Prosthetic valves a. 1, 3 b. 2, 4 c. 1, 3, 4 d. 2, 3, 4 263 17. A drug taken in small doses on a continuing basis to reduce platelet adhesion is: a. acetylsalicylic acid (ASA). b. streptokinase. c. acetaminophen. d. heparin. 233 18. A partial obstruction in a coronary artery will likely cause: a. pulmonary embolus. b. hypertension. c. angina attacks. d. myocardial infarction. 237 19. Cigarette smoking is a risk factor in coronary artery disease because smoking: a. reduces vasoconstriction and peripheral resistance. b. decreases serum lipid levels. c. promotes platelet adhesion. d. increases serum HDL levels. 237-238 20. The term arteriosclerosis specifically refers to: a. development of atheromas in large arteries. b. intermittent vasospasm in coronary arteries. c. degeneration with loss of elasticity and obstruction in small arteries. d. ischemia and necrosis in the brain, kidneys, and heart. 234 21. A modifiable factor that increases the risk for atherosclerosis is: a. leading a sedentary lifestyle. b. being female and older than 40 years of age. c. excluding saturated fats from the diet. d. familial hypercholesterolemia. 238 22. An atheroma develops from: a. a torn arterial wall and blood clots. b. accumulated lipids, cells, and fibrin where endothelial injury has occurred. c. thrombus forming on damaged walls of veins. d. repeated vasospasms. 234 23. Low-density lipoproteins (LDL): a. promote atheroma development. b. contain only small amounts of cholesterol. c. transport cholesterol from cells to the liver for excretion. d. are associated with low intake of saturated fats. 235 24. Factors that may precipitate an angina attack include all of the following EXCEPT: a. eating a large meal. b. engaging in an angry argument. c. taking a nap. d. shoveling snow on a cold, windy day. 240 25. When comparing angina with myocardial infarction (MI), which statement is true? a. Both angina and MI cause tissue necrosis. b. Angina often occurs at rest; MI occurs during a stressful time. c. Pain is more severe and lasts longer with angina than with MI. d. Angina pain is relieved by rest and intake of nitroglycerin; the pain of MI is not. 234 26. The basic pathophysiology of myocardial infarction is best described as: a. cardiac output that is insufficient to meet the needs of the heart and body. b. temporary vasospasm that occurs in a coronary artery. c. total obstruction of a coronary artery, which causes myocardial necrosis. d. irregular heart rate and force, reducing blood supply to coronary arteries. 240 27. Typical early signs or symptoms of myocardial infarction include: a. brief, substernal pain radiating to the right arm, with labored breathing. b. persistent chest pain radiating to the left arm, pallor, and rapid, weak pulse. c. bradycardia, increased blood pressure, and severe dyspnea. d. flushed face, rapid respirations, left-side weakness, and numbness. 241 28. The most common cause of a myocardial infarction is: a. an imbalance in calcium ions. b. an infection of the heart muscle. c. atherosclerosis involving an attached thrombus. d. a disruption of the heart conduction system. 240 29. Calcium-channel blocking drugs are effective in: a. reducing the risk of blood clotting. b. decreasing the attraction of cholesterol into lipid plaques. c. reducing cardiac and smooth muscle contractions. d. decreasing all types of cardiac arrhythmias. 261 30. Which of the following confirms the presence of a myocardial infarction? a. A full description of the pain, including the sequence of development b. The presence of elevated serum cholesterol and triglycerides c. Serum isoenzymes released from necrotic cells and an ECG d. Leukocytosis and elevated C-reactive protein 242 31. The size of the necrotic area resulting from myocardial infarction may be minimized by all of the following EXCEPT: 243 32. The most common cause of death immediately following a myocardial infarction is: a. cardiac arrhythmias and fibrillation. b. ruptured ventricle or aorta. c. congestive heart failure. d. cerebrovascular accident. 241-242 33. Why does ventricular fibrillation result in cardiac arrest? a. previously established collateral circulation. b. immediate administration of thrombolytic drugs. c. maintaining maximum oxygen supply to the myocardium. d. removing the predisposing factors to atheroma development. a. Delayed conduction through the AV node blocks ventricular stimulation. b. Insufficient blood is supplied to the myocardium. c. The ventricles contract before the atria. d. Parasympathetic stimulation depresses the SA node. 245 34. The term cardiac arrest refers to which of the following? a. Condition where cardiac output is less than the demand b. A decreased circulating blood volume c. Missing a ventricular contraction d. The cessation of all cardiac function 246 35. Which change results from total heart block? a. A prolonged PR interval b. Periodic omission of a ventricular contraction c. A wide QRS wave d. Spontaneous slow ventricular contractions, not coordinated with atrial contraction 244 36. The term premature ventricular contraction refers to the condition where: a. atrial muscle cells are stimulating additional cardiac contractions. b. the ventricles contract spontaneously following a period without a stimulus. c. additional contractions arise from ectopic foci in the ventricular muscle. d. increased heart rate causes palpitations. 245 37. Which of the following is most likely to cause left-sided congestive heart failure? a. Incompetent tricuspid heart valve b. Chronic pulmonary disease c. Infarction in the right atrium d. Uncontrolled essential hypertension 246 38. The definition of congestive heart failure is: a. cessation of all cardiac activity. b. inability of the heart to pump enough blood to meet the metabolic needs of the body. c. insufficient circulating blood in the body. d. the demand for oxygen by the heart is greater than the supply. 246 39. Significant signs of right-sided congestive heart failure include: a. severe chest pain and tachycardia. b. edematous feet and legs with hepatomegaly. c. frequent cough with blood-streaked frothy sputum. d. orthopnea, fatigue, increased blood pressure. 247 40. Paroxysmal nocturnal dyspnea is marked by: a. hemoptysis and rales. b. distended neck veins and flushed face. c. bradycardia and weak pulse. d. cardiomegaly. 250 41. Compensation mechanisms for decreased cardiac output in cases of congestive heart failure include: 246 42. In which blood vessels will failure of the left ventricle cause increased hydrostatic pressure? a. slow cardiac contractions. b. increased renin and aldosterone secretions. c. decreased erythropoietin secretion. d. fatigue and cold intolerance. a. Veins of the legs and feet b. Jugular veins c. Pulmonary capillaries d. Blood vessels of the liver and spleen 247 43. Which of the following drugs improves cardiac efficiency by slowing the heart rate and increasing the force of cardiac contractions? 250 44. In an infant, the initial indication of congestive heart failure is often: a. distended neck veins. b. feeding problems. c. low-grade fever and lethargy. d. frequent vomiting. 250 45. Effects that may be expected from a beta-adrenergic blocking drug include: a. Furosemide b. Digoxin c. Epinephrine d. Nifedipine a. increasing systemic vasoconstriction. b. decreased sympathetic stimulation of the heart. c. blockage of an angiotensin receptor site. d. increased release of renin. 232 46. A sign of aortic stenosis is: a. increased cardiac output. b. congestion in the liver, spleen, and legs. c. flushed face and headache. d. a heart murmur. 250-251 47. An incompetent mitral valve would cause: a. increased blood to remain in the right atrium. b. hypertrophy of the right ventricle. c. decreased output from the left ventricle. d. decreased pressure in the left atrium. 253 48. Which of the following describes the blood flow occurring with a ventricular septal defect? a. From the left ventricle to the right ventricle b. From the right ventricle to the left ventricle c. Increased cardiac output from the left ventricle d. Mixed oxygenated and unoxygenated blood in the systemic circulation 252 49. Unoxygenated blood enters the systemic circulation in children with tetralogy of Fallot because: a. the aorta and pulmonary artery have exchanged positions. b. pulmonary stenosis changes the ventricular pressures. c. the left ventricular wall has hypertrophied. d. the septal defect allows exchange of blood between the atria. 254-255 50. Cyanosis occurs in children with tetralogy of Fallot because: a. more carbon dioxide is present in the circulating blood. b. a large amount of hemoglobin in the general circulation is unoxygenated. c. the pulmonary circulation is overloaded and congested. d. the circulation is sluggish (slow) throughout the system. 255 51. The initial effect on the heart in cases of rheumatic fever is: a. infection in the heart by hemolytic streptococci. b. highly virulent microbes causing vegetations on the heart valves. c. septic emboli obstructing coronary arteries. d. acute inflammation in all layers of the heart due to abnormal immune response. 255 52. Common signs of rheumatic fever include all of the following EXCEPT: a. arthritis, causing deformity of the small joints in the hands and feet. b. erythematous skin rash and subcutaneous nodules. c. epistaxis, tachycardia, and fever. d. elevated ASO titer and leukocytosis. 255-256 53. Rheumatic heart disease usually manifests in later years as: a. swollen heart valves and fever. b. cardiac arrhythmias and heart murmurs. c. thrombus formation and septic emboli. d. petechial hemorrhages of the skin and mucosa. 256 54. Septic emboli, a common complication of infective endocarditis, are a result of the fact that: a. vegetations are loosely attached and fragile. b. the valves are no longer competent. c. cardiac output is reduced. d. heart contractions are irregular. 257 55. Which of the following applies to subacute infective endocarditis? a. A microbe of low virulence attacks abnormal or damaged heart valves. b. Virulent microbes invade normal heart valves. c. No permanent damage occurs to the valves. d. Prophylactic medication does not prevent infection. 257 56. Pericarditis causes a reduction in cardiac output as a result of which of the following? a. Delays in the conduction system, interfering with cardiac rhythm b. Weak myocardial contractions due to friction rub c. Excess fluid in the pericardial cavity, which decreases ventricular filling d. Incompetent valves, which allow regurgitation of blood 258 57. Pericarditis may be caused by: 1. infection. 2. abnormal immune responses. 3. injury. 4. malignant neoplasm. a. 1, 2 b. 3, 4 c. 1, 3, 4 d. 1, 2, 3, 4 258 58. A source of an embolus causing an obstruction in the brain could be the: a. femoral vein. b. pulmonary vein. c. carotid artery. d. coronary artery. 242 59. The basic pathophysiological change associated with essential hypertension is: a. development of lipid plaques in large arteries. b. recurrent inflammation and fibrosis in peripheral arteries. c. degeneration and loss of elasticity in arteries. d. increased systemic vasoconstriction. 259 60. Uncontrolled hypertension is most likely to cause ischemia and loss of function in the: a. kidneys, brain, and retinas of the eye. b. peripheral arteries in the legs. c. aorta and coronary arteries. d. liver, spleen, and stomach. 260 61. When is a diagnosis of essential hypertension likely to be considered in young or middle-aged individuals? 259 62. Atherosclerosis in the iliac or femoral arteries is likely to cause which of the following? 1. Gangrenous ulcers in the legs 2. Strong rapid pulses in the legs 3. Intermittent claudication 4. Red, swollen legs a. 1, 2 a. Blood pressure remains consistently above 140/90 b. Blood pressure fluctuates between 130/85 and 180/105 c. Blood pressure increases rapidly and is unresponsive to medication d. Chronic kidney disease leads to consistently elevated blood pressure b. 1, 3 c. 2, 3 d. 2, 4 261 63. The term intermittent claudication refers to: a. sensory deficit in the legs due to damage to nerves. b. chest pain related to ischemia. c. ischemic muscle pain in the legs, particularly with exercise. d. dry, cyanotic skin with superficial ulcers. 261 64. What is the primary reason for amputation of gangrenous toes or feet in patients with peripheral vascular disease? 262 65. An echocardiogram is used to demonstrate any abnormal: a. activity in the conduction system. a. It promotes more rapid healing of ulcerated areas. b. It improves circulation to other areas. c. It prevents spread of infection and reduces pain. d. It reduces swelling in the peripheral areas. b. movement of the heart valves. c. change in central venous pressure. d. blood flow in coronary arteries. 225 66. A friction rub is associated with: a. infectious endocarditis. b. arrhythmias. c. pericarditis. d. an incompetent aortic valve. 258 67. A dissecting aortic aneurysm develops as: a. a dilation or bulge that develops at one point on the aortic wall. b. a thrombus that accumulates at a point in the aortic wall. c. a section of the aorta that weakens and dilates in all directions. d. a tear in the intimal lining, which allows blood flow between layers of the aortic wall. 262 68. The outcome for many aortic aneurysms is: b. thrombus formation and pulmonary embolus. c. rupture and hemorrhage. d. pressure on adjacent organs or structures. 262 69. Which factor predisposes to varicose veins during pregnancy? a. Compressed pelvic veins b. Stenotic valves in leg veins c. Thrombus formation d. Insufficient muscle support for veins 263 70. Phlebothrombosis is more likely to cause pulmonary emboli than is thrombophlebitis because: a. platelets attach to the inflamed wall. b. thrombus forms in a vein and is less firmly attached. c. leg cramps require massage. d. systemic signs of inflammation require treatment. 264 71. Shock is defined as: b. general hypoxia, causing damage to various organs. c. decreased circulating blood and tissue perfusion. d. loss of blood, causing severe hypoxia. 264 72. Shock follows a myocardial infarction when: a. the stress response causes general vasodilation. b. fluid is lost into ischemic tissues. c. heart valves are damaged. d. a large portion of the myocardium is damaged. 242 73. What are the early signs of circulatory shock? 1. Pale moist skin 2. Loss of consciousness 3. Anxiety and restlessness 4. Rapid strong pulse a. 1, 2 b. 1, 3 c. 1, 4 d. 3, 4 267 74. A compensation for shock would include: a. increased heart rate and oliguria. b. lethargy and decreased responsiveness. c. warm, dry, flushed skin. d. weak, thready pulse. 267 75. Why does anaphylactic shock cause severe hypoxia very quickly? a. Generalized vasoconstriction reduces venous return. b. Bronchoconstriction and bronchial edema reduce airflow. c. Heart rate and contractility are reduced. d. Metabolic rate is greatly increased. 267 76. Neurogenic (vasogenic) shock results from systemic vasodilation due to: a. increased peripheral resistance and less blood in the microcirculation. b. increased permeability of all the blood vessels, leading to hypovolemia. c. slower, less forceful cardiac contractions. d. increased capacity of the vascular system and reduced venous return. 265 | 266 77. A prolonged period of shock is likely to cause: a. damage to, and increased permeability of, pulmonary capillaries. b. increased permeability of the glomerular capillaries of the kidneys. c. increased pH of blood and body fluids. d. increased systemic vasoconstriction. 265 78. What would indicate decompensated acidosis related to shock? a. Serum bicarbonate level below normal b. PCO2 above normal c. Serum pH below normal range d. Urine pH of 4.5 267 79. With shock, anaerobic cell metabolism and decreased renal blood flow cause: a. metabolic alkalosis. b. metabolic acidosis. c. decreased serum potassium. d. increased serum bicarbonate. 267-268 80. Shock develops in patients with severe burns as a result of: a. extensive hemorrhage. b. pain and loss of plasma. c. direct damage to the heart. d. extensive hemolysis of erythrocytes. 265-266 81. The classic early manifestation(s) of left-sided congestive heart failure is/are , whereas the early indicator(s) of right-sided failure is/are . a. palpitations and periodic chest pain; shortness of breath on exertion b. swelling of the ankles and abdomen; chest pain c. shortness of breath on exertion or lying down; swelling of the ankles d. coughing up frothy sputum; hepatomegaly and splenomegaly 249-250 82. A common adverse effect of many antihypertensive medications is: a. orthostatic hypotension. b. bradycardia. c. altered blood coagulation. d. peripheral edema. 261 83. The cause of essential hypertension is considered to be: a. chronic renal disease. b. excessive intake of saturated fats and salt. c. sedentary lifestyle. d. idiopathic. 259 84. A cardiac pacemaker would most likely be inserted in cases of: a. angina pectoris. b. heart block. c. congestive heart failure. d. ventricular fibrillation. 245 85. Which of the following is considered to be the most dangerous arrhythmia? a. Tachycardia b. Bradycardia c. Ventricular fibrillation d. Second-degree heart block 245 86. Which of the following is NOT true of the drug nitroglycerin? a. It decreases myocardial workload by causing systemic vasodilation. b. It may be administered sublingually, transdermally, or by oral spray. c. Dizziness or syncope may follow a sublingual dose. d. It strengthens the myocardial contraction. 232 87. Confirmation of the diagnosis of a myocardial infarction would include: 1. specific changes in the ECG. 2. marked leukocytosis and increased erythrocyte sedimentation rate (ESR). 3. elevation of cardiac isoenzymes in serum. 4. a pattern of pain. a. 1, 2 b. 1, 3 c. 2, 4 d. 3, 4 242 88. Which of the following statements regarding aneurysms is true? a. Aneurysms are always caused by congenital malformations. b. The greatest danger with aneurysms is thrombus formation. c. Manifestations of aneurysms result from compression of adjacent structures. d. Aneurysms involve a defect in the tunica media of veins. 263 89. The most common factor predisposing to the development of varicose veins is: a. trauma. b. congenital valve defect in the abdominal veins. c. infection. d. increased venous pressure. 263 90. In the period immediately following a myocardial infarction, the manifestations of pallor and diaphoresis, rapid pulse, and anxiety result from: 267-269 91. Septic shock differs from hypovolemic shock in that it is frequently manifested by: a. fever and flushed face. b. elevated blood pressure. c. increased urinary output. a. onset of circulatory shock. b. the inflammatory response. c. release of enzymes from necrotic tissue. d. heart failure. d. slow bounding pulse. 267 92. Heart block, in which a conduction delay at the AV node results in intermittent missed ventricular contractions, is called: 244 93. More extensive permanent damage is likely when a myocardial infarction is caused by: a. a hemorrhage. b. an embolus. c. a thrombus. d. an arrhythmia. 242 94. A very rapid heart rate reduces cardiac output because: a. venous return is increased. b. ventricular fibrillation develops immediately. c. conduction through the AV node is impaired. a. first-degree block. b. second-degree block. c. bundle-branch block. d. total heart block. d. ventricular filling is reduced. 243 95. The right side of the heart would fail first in the case of: 1. severe mitral valve stenosis. 2. uncontrolled essential hypertension. 3. large infarction in the right ventricle. 4. advanced chronic obstructive pulmonary disease (COPD). a. 1, 2 b. 2, 3 c. 1, 4 d. 3, 4 246 96. Which of the following compensations that develop in patients with congestive heart failure eventually increase the workload of the heart? a. Faster heart rate and cardiomegaly b. Peripheral vasoconstriction c. Increased secretion of renin d. A and C e. A, B, and C 246 97. Which statement applies to paroxysmal nocturnal dyspnea? a. It indicates decreased CO2 diffusion in the lungs. b. It indicates swelling in the bronchioles and bronchi. c. It is caused by increased blood in the lungs when lying in a supine position. d. It results from pleural effusion. 249-250 98. In patients with congestive heart failure, ACE inhibitor drugs are useful because they: a. reduce renin and aldosterone secretion. b. slow the heart rate. c. strengthen myocardial contraction. d. block arrhythmias. 250 99. In a child with ventricular septal defect, altered blood flow: a. leads to increased stroke volume from the left ventricle. b. results in unoxygenated blood in the systemic circulation. c. is called a right-to-left shunt. d. is called a left-to-right shunt. 252-253 100. In a child with acute rheumatic fever, arrhythmias may develop due to the presence of: a. endocarditis. b. myocarditis. c. pericarditis. d. congestive heart failure. 256 101. Prophylactic antibacterial drugs such as amoxicillin are given to patients with certain congenital heart defects or damaged heart valves immediately before invasive procedures to prevent: 257 102. Varicose ulcers may develop and be slow to heal because: a. leg muscles are painful, restricting movement. b. edema reduces arterial blood supply to the area. c. emboli form in damaged veins, leading to local ischemia. d. valves in veins restrict blood flow. 264 a. formation of septic thrombi. b. infectious endocarditis. c. abscess formation. d. myocarditis. 103. Excessive fluid in the pericardial space causes: a. increased cardiac output. b. myocardial infarction. c. reduced venous return. d. friction rub. 258 104. Aortic stenosis means the aortic valve: a. allows blood to leak back into the left ventricle during diastole. b. cannot fully open during systole. c. functions to increase stroke volume. d. does not respond to the cardiac cycle. 251 105. Septic shock is frequently caused by infections involving: a. gram-negative endotoxin-producing bacteria. b. spore-forming saprophytic fungi. c. free-swimming, motile parasitic protozoa. d. parasitic nematodes. 265 Chapter 13: Respiratory System Disorders Chapter 13: Respiratory System Disorders Test Bank MULTIPLE CHOICE 1. What happens in the lungs when the diaphragm and external intercostal muscles relax? a. Air is forced out of the lungs. b. Lung volume increases. c. Intrapulmonic pressure decreases. d. Intrapleural pressure decreases. 275 2. The respiratory mucosa is continuous through the: 1. upper and lower respiratory tracts. 2. nasal cavities and the sinuses. 3. nasopharynx and oropharynx. 4. middle ear cavity and auditory tube. a. 1 only b. 1, 2 c. 2, 3 d. 1, 3, 4 e. 1, 2, 3, 4 273-274 3. Which of the following activities does NOT require muscle contractions and energy? a. Quiet inspiration b. Forced inspiration c. Quiet expiration d. Forced expiration 275 4. The maximum volume of air a person can exhale after a maximum inspiration is termed the: a. expiratory reserve volume. b. inspiratory reserve volume. c. total lung capacity. d. vital capacity. 276-277 5. Which of the following applies to the blood in the pulmonary artery? a. PCO2 is low. b. PO2 is low. c. Hydrostatic pressure is very high. d. It is flowing into the left atrium. 279 6. Which of the following causes bronchodilation? a. Epinephrine b. Histamine c. Parasympathetic nervous system d. Drugs that block β2-adrenergic receptors 302 7. The central chemoreceptors in the medulla are normally most sensitive to: a. low oxygen level. b. low concentration of hydrogen ions. c. elevated oxygen level. d. elevated carbon dioxide level. 277 8. Oxygen diffuses from the alveoli to the blood because: a. PO2 is higher in the blood. b. PO2 is lower in the blood. c. CO2 is diffusing out of the blood. d. more CO2 is diffusing out of cells into the blood. 278 9. Carbon dioxide is primarily transported in the blood: a. as dissolved gas. b. attached to the iron molecule in hemoglobin. c. as bicarbonate ion. d. as carbonic acid. 280 10. What would hypercapnia cause? a. Increased serum pH b. Decreased respirations c. Respiratory acidosis d. Decreased carbonic acid in the blood 278 11. Which of the following would result from hyperventilation? a. Respiratory acidosis b. Respiratory alkalosis c. Metabolic alkalosis d. Metabolic acidosis 278 12. Which of the following values is always decreased with respiratory alkalosis (compensated or decompensated)? 282-283 13. What would be the most effective compensation for respiratory acidosis? a. The kidneys eliminating more bicarbonate ions b. The kidneys producing more bicarbonate ions c. The kidneys reabsorbing more hydrogen ions d. An increase in respiratory rate 279-280 14. What is the acid-base status of a patient with the following values for arterial blood gases? serum bicarbonate 36.5 mmol/L (normal range: 22-28) PCO275 mm Hg (normal range: 35-45) serum pH 7.0 a. Serum bicarbonate b. PaCO2 c. Serum pH d. Urine pH a. Compensated metabolic acidosis b. Decompensated metabolic acidosis c. Compensated respiratory acidosis d. Decompensated respiratory acidosis 320 15. What does carbaminohemoglobin refer to? a. Replacement of oxygen by carbon monoxide on hemoglobin molecules b. Full saturation of all heme molecules by oxygen c. Carbon dioxide attached to an amino group on the hemoglobin molecule d. Oxygen combined with iron in the hemoglobin molecule 280 16. Approximately what percentage of bound oxygen is released to the cells for metabolism during an erythrocyte’s journey through the circulatory system? 279 17. The production of yellowish-green, cloudy, thick sputum is often an indication of: a. 80% b. 25% c. 10% d. 50% a. bacterial infection. b. cancer tumor. c. damage of lung tissue due to smoking. d. emphysema. 281 18. What does the term hemoptysis refer to? a. Thick, dark red sputum associated with pneumococcal infection b. Reddish-brown granular blood found in vomitus c. Bright red streaks of blood in frothy sputum d. Bloody exudate in the pleural cavity 281 19. Orthopnea is: a. very deep, rapid respirations. b. difficulty breathing when lying down. c. waking up suddenly, coughing, and struggling for breath. d. noisy breathing with stridor or rhonchi. 282 20. Light bubbly or crackling breathing sounds associated with serous secretions are called: a. rhonchi. b. stridor. c. rales. d. wheezing. 282 21. Choose the correct information applying to laryngotracheobronchitis: a. Viral infection in infant under 12 months b. Viral infection in child, 3 months to 3 years c. Bacterial infection in infant under 6 months d. Bacterial infection in child, 3 to 7 years 283 22. Signs and symptoms of acute sinusitis usually include: a. serous nasal discharge and chronic cough. b. copious frothy sputum and dyspnea. c. severe localized pain in the facial bone and tenderness in the face. d. fetid breath and sore throat. 283 23. What are early signs and symptoms of infectious rhinitis? a. Purulent nasal discharge and periorbital pain b. Serous nasal discharge, congestion, and sneezing c. Copious purulent sputum, particularly in the morning d. Harsh barking cough and wheezing 285 24. Why does the influenza virus cause recurrent infection in individuals? a. Elderly patients are predisposed to secondary infections. b. The virus is transmitted by numerous routes. c. The virus is very difficult to destroy. d. Viral mutation reduces immunity from prior infections. 285 25. What are typical signs and symptoms of epiglottitis? a. Hyperinflation of the chest and stridor b. Hoarse voice and barking cough c. Sudden fever, sore throat, and drooling saliva d. Sneezing, mild cough, and fever 289 26. What is the most common cause of viral pneumonia? a. Rhinovirus b. Influenza virus c. Haemophilus influenzae d. Pneumococcus 288 27. Which of the following describes lobar pneumonia? a. Sudden onset of fever and chills, with rales and rusty sputum b. Insidious onset, diffuse interstitial infection c. Viral infection causing nonproductive cough and pleuritic pain d. Opportunistic bacteria causing low-grade fever with cough and thick greenish sputum 288 28. How does severe hypoxia develop with pneumonia? a. Acidosis depresses respirations. b. Oxygen diffusion is impaired by the congestion. c. Inflammatory exudate absorbs oxygen from the alveolar air. d. Infection reduces effective compensation by the heart. 288 29. Rust-colored sputum in a patient with pneumonia usually indicates: a. secondary hemorrhage in the lungs. b. Streptococcus pneumoniae is the infecting agent. c. prolonged stasis of mucous secretions in the airways. d. persistent coughing has damaged the mucosa in the bronchi. 289 30. What is the cause of Legionnaires’ disease? a. Mycoplasma b. A fungus c. A gram-negative bacterium d. Pneumococcus 290 31. Select the statement related to tuberculosis: a. The microbe is present in the sputum of all patients with a positive TB skin test. b. The infection is transmitted primarily by blood from an infected person. c. TB is usually caused by an acid-fast bacillus, resistant to many disinfectants. d. The microbe is quickly destroyed by the immune response. 290-291 32. How is primary tuberculosis identified? a. Cavitation in the lungs and spread of the microbe to other organs b. Persistent productive cough, low-grade fever, and fatigue c. Caseation necrosis and formation of a tubercle in the lungs d. Multiple granulomas in the lungs and rapid spread of the microbe 291 33. When does active (secondary) infection by Mycobacterium tuberculosis with tissue destruction occur? 290 34. Which of the following statements does NOT apply to M. tuberculosis? a. Microbes can survive for a long time inside tubercles. b. The bacilli can survive some adverse conditions such as drying and heat. c. Infection is limited to the lungs. d. The bacilli can be destroyed by antibacterial drugs. 291 35. Which of the following confirms the presence of active (reinfection) tuberculosis? a. When host resistance is decreased b. When a hypersensitivity reaction is initiated c. When the BCG vaccine is not administered immediately following exposure to the microbe d. When Ghon complexes form in the lungs a. A positive skin test for TB b. A calcified tubercle shown on a chest X-ray c. Identification of acid-fast bacilli in a sputum sample d. A history of exposure to individuals being treated for TB 290 36. Areas in the United States that show higher rates than the national rate of TB are areas that have a high incidence of: 293 37. Histoplasmosis is caused by a: a. fungus. b. virus. c. bacillus. d. protozoa. 294 38. Cystic fibrosis is transmitted as a/an: a. HIV and homelessness. b. obesity and tobacco use. c. elderly persons and radon. d. steroid use and alcoholism. a. X-linked recessive gene. b. autosomal recessive gene. c. autosomal dominant gene. d. chromosomal defect. 294 39. The basic pathophysiology of cystic fibrosis is centered on a/an: a. defect of the exocrine glands. b. impaired function of the endocrine glands. c. chronic inflammatory condition of the lungs. d. abnormal immune response in the lungs and other organs. 294 40. Growth and development of a child with cystic fibrosis may be delayed because of: a. deficit of gastric enzymes for protein digestion. b. mucus plugs obstructing the flow of pancreatic enzymes. c. lack of available treatment for steatorrhea. d. abnormal salivary secretions. 294 41. Persistent thick mucus in the bronchioles of a child with cystic fibrosis may cause: 1. air trapping. 2. atelectasis. 3. repeated infections. 4. irreversible damage to lung tissue. a. 1, 2 b. 2, 4 c. 1, 3, 4 d. 1, 2, 3, 4 294 42. What is a common indicator of cystic fibrosis in the newborn? a. Infant respiratory distress syndrome b. Failure to excrete meconium c. Taste of ammonia on the skin d. Lack of bile secretions 297 43. What is an early sign of bronchogenic carcinoma? a. Air trapping and overinflation of the lung b. Weight loss c. Bone pain d. Chronic cough 296-297 44. Cigarette smoking predisposes to malignant neoplasms because smoking: a. can cause metaplasia and dysplasia in the epithelium. b. promotes malignant changes in all types of benign tumors in the lungs. c. causes paraneoplastic syndrome. d. increases exposure to carbon monoxide in the lungs. 297 45. Why does hypercalcemia occur with bronchogenic carcinoma? a. Invasion of the parathyroid gland by the tumor b. Secretion of parathyroid or parathyroid like hormones by the tumor c. Destruction of the ribs d. Failure of the kidney to excrete calcium ions 299 46. What is a sign indicating total obstruction of the airway by aspirated material? a. Hoarse cough b. Rapid loss of consciousness c. Dyspnea d. Inflammation of the mucosa 299 47. Which of the following predisposes to postoperative aspiration? a. Reduced pressure of the abdominal organs on the diaphragm b. Depression of the vomiting center by anesthetics and analgesics c. Vomiting caused by drugs or anesthesia d. Lack of food intake for the previous 24 hours 300 48. What is the pathophysiology of an acute attack of extrinsic asthma? a. Gradual degeneration and fibrosis b. Continuous severe attacks unresponsive to medication c. A hypersensitivity reaction involving release of chemical mediators d. Hyperresponsive mucosa 300 49. During an acute asthma attack, how does respiratory obstruction occur? 1. Relaxation of bronchial smooth muscle 2. Edema of the mucosa 3. Increased secretion of thick, tenacious mucus 4. Contraction of elastic fibers a. 1, 2 b. 1, 3 c. 2, 3 d. 2, 4 303 | 322 50. What cause the expanded anteroposterior (A-P) thoracic diameter (barrel chest) in patients with emphysema? 303 51. Which of the following is typical of progressive emphysema? a. Vital capacity increases. b. Residual lung volume increases. c. Forced expiratory volume increases. d. Tidal volume increases. 303 52. Destruction of alveolar walls and septae is a typical change in: a. chronic bronchitis. b. acute asthma. a. Air trapping and hyperinflation b. Persistent coughing to remove mucus c. Recurrent damage to lung tissues d. Dilated bronchi and increased mucous secretions c. emphysema. d. asbestosis. 302 53. A group of common chronic respiratory disorders characterized by tissue degeneration and respiratory obstruction is called: 303 54. Which statement does NOT apply to emphysema? a. The surface area available for gas exchange is greatly reduced. b. A genetic defect may lead to breakdown of elastic fibers. c. The ventilation/perfusion ratio remains constant. d. Expiration is impaired. 307 55. What is the cause of chronic bronchitis? a. Chronic irritation, inflammation, and recurrent infection of the larger airways b. A genetic defect causing excessive production of mucus a. mesothelioma. b. COPD. c. CF. d. MD. c. Hypersensitivity to parasympathetic stimulation in the bronchi d. Deficit of enzymes, preventing tissue degeneration 307 56. Which of the following is typical of chronic bronchitis? a. Decreased activity of the mucous glands b. Fibrosis of the bronchial wall c. Overinflation of bronchioles and alveoli d. Formation of blebs or bullae on the lung surface 307 57. What are typical pathological changes with bronchiectasis? a. Bronchospasm and increased mucous secretion b. Adhesions and fibrosis in the pleural membranes c. Airway obstructions and weak, dilated bronchial walls d. Fixation of the ribs in the inspiratory position 308 58. Which of the following are significant signs of bronchiectasis? a. Persistent nonproductive cough, dyspnea, and fatigue b. Persistent purulent nasal discharge, fever, and cough c. Chronic cough, producing large quantities of purulent sputum d. Wheezing and stridor 302 | 304 59. Why does cor pulmonale develop with chronic pulmonary disease? a. The right ventricle pumps more blood than the left ventricle. b. Pulmonary fibrosis and vasoconstriction increase vascular resistance. c. Demands on the left ventricle are excessive. d. Blood viscosity is increased, adding to cardiac workload. 308 60. Restrictive lung disorders may be divided into two groups based on: a. patient history of obesity and exposure to other COPD. b. smoking history and congenital defects. c. previous lung disease and cardiovascular disorders. d. anatomical abnormality and lung disease damage, impairing expansion. 303 61. What is caused by frequent inhalation of irritating particles such as silica? a. Fibrosis and loss of compliance b. Frequent bronchospasm c. Increased number of mucus-producing glands d. Distorted shape of the thorax 309 62. Pulmonary edema causes severe hypoxia because of: a. decreased diffusion of carbon dioxide from the alveoli. b. interference with expansion of the lungs. c. constant cough and hemoptysis. d. decreased recoil of lungs and ineffective expiration. 309 63. Which of the following is NOT a cause of pulmonary edema? a. Left-sided congestive heart failure b. Excessive blood volume (overload) c. Inhalation of toxic gases d. Hyperproteinemia and increasing osmotic pressure of the blood 309 64. Which of the following is a common source of a pulmonary embolus? a. Mural thrombus from the left ventricle b. Thrombus attached to atheromas in the aorta or iliac arteries c. Thrombus forming in the femoral veins d. A blood clot in the pulmonary vein 309-310 65. What is a large-sized pulmonary embolus likely to cause? a. Hypertension and left-sided heart failure b. Atelectasis and respiratory failure c. Hypotension and right-sided heart failure d. Pleural effusion and atelectasis 312 66. Which manifestation(s) of atelectasis is/are associated with airway obstruction? a. Bradycardia and dyspnea b. Tracheal deviation toward the unaffected side c. Decreased breath sounds on the affected side d. Rales and rhonchi 312 67. How does total obstruction of the airway lead to atelectasis? a. Decreased surfactant production impairs lung expansion. b. The involved lung is compressed. c. Air is absorbed from the alveoli distal to the obstruction. d. Air continues to be inspired but is trapped distal to the obstruction. 312 68. How does a large pleural effusion lead to atelectasis? a. The cohesion between the pleural membranes is disrupted. b. There is decreased intrapleural pressure. c. The mediastinal contents compress the affected side. d. Pleuritic pain causes very shallow breathing. 316 69. When does flail chest usually occur? a. An open puncture wound involves the pleural membranes. b. The visceral pleura is torn by a fractured rib. c. Several ribs are fractured at two sites. d. Increasing fluid in the pleural cavity causes atelectasis. 316 70. With a flail chest injury, events during inspiration include which of the following? a. Air is sucked into the lung through the chest wall. b. The mediastinum shifts toward the unaffected side. c. The floating segment is pushed outward. d. The trachea deviates toward the affected side. 316 71. How is cardiac output reduced with a flail chest injury? a. Atelectasis compresses the heart. b. Venous return is impaired. c. Intrapleural pressure is decreased. d. Air pressure continues to increase in the pleural space. 314 72. Which of the following is a manifestation of a simple closed pneumothorax? a. Decreased respiratory rate b. Tracheal deviation toward the unaffected lung c. Asymmetrical chest movements d. Increased breath sounds on the affected side 314 73. Which of the following is an effect of a large open pneumothorax (sucking wound)? a. Mediastinal flutter, impairing venous return b. Increased venous return c. Progressive atelectasis of both lungs d. Overexpansion of the unaffected lung 316 74. With a tension pneumothorax, which factors contribute to severe hypoxia? a. Decreasing compression of the inferior vena cava b. More air leaving the pleural cavity on expiration than entering with inspiration c. Shift of the mediastinal contents toward the affected lung d. Continually increasing pressure on the unaffected lung 319 75. Which of the following statements describe the pathophysiology of adult respiratory distress syndrome? 1. Damage leading to increased permeability of the alveolar capillary membranes 2. Decreased surface tension in the alveoli 3. Excessive fluid and protein interstitially and in the alveoli 4. Multiple diffuse hemorrhages in the lungs a. 1, 2 b. 1, 3 c. 2, 3 d. 3, 4 317 76. Infant respiratory distress syndrome results from: a. insufficient surfactant production. b. incomplete expiration shortly after birth. c. retention of fluid in the lungs after birth. d. immature neural control of respirations. 282 77. Obstruction in the upper airway is usually indicated by: a. stridor. b. rales. c. wheezing. d. orthopnea. 280 78. Which of the following does NOT apply to carbon dioxide? a. It diffuses across membranes much more easily than does oxygen. b. It is carried in blood as carbaminohemoglobin. c. It can be converted into bicarbonate ion. d. It is replaced on hemoglobin by oxygen in the lungs. 278 79. Whenever PO2 levels decrease below normal, PCO2 levels: a. increase. b. decrease also. c. may or may not change. d. increase slightly. 283 80. Laryngotracheobronchitis is typically manifested by: a. drooling and difficulty swallowing. b. hoarse voice and barking cough. c. sore and scratchy throat with fever. d. wheezing and dyspnea. 286 81. Lobar pneumonia is usually caused by: a. Mycoplasma pneumoniae. b. Streptococcus pneumoniae. c. Legionella pneumophila. d. Pneumocystis carinii. 290 82. Severe acute respiratory syndrome (SARS) is caused by a/an: a. rhinovirus. b. mycoplasma. c. influenza virus. d. coronavirus. 290 83. SARS typically begins as a flulike syndrome followed, after a few days, by: a. increased exudates in the bronchial tree and pleural cavity. b. productive cough and lobar consolidation. c. interstitial lung congestion, dyspnea, and dry cough. d. hemoptysis and necrosis of mucous membrane. 294 84. In addition to effects on the lungs and pancreas, cystic fibrosis results in: a. excess bile production. b. high sodium chloride content in saliva and sweat. c. gastric ulcers. d. frequent ear and sinus infections. 297 85. Which of the following is a significant early sign of bronchogenic carcinoma in a smoker? a. Frequent nonproductive cough b. Fever, dyspnea, generalized aching c. Production of large volumes of purulent sputum d. Hemoptysis and weight loss 297 86. Which of the following is likely to cause pneumothorax or hemothorax in a patient with bronchogenic carcinoma? 292 87. Which of the following would confirm a diagnosis of primary tuberculosis? a. A positive tuberculin skin test b. Occurrence of hemoptysis c. Unproductive cough with absence of sputum d. Small areas of calcification on a chest X-ray 293 a. The tumor obstructs a major bronchus. b. Compression of lung tissue by the tumor causes atelectasis. c. The tumor causes inflammation and erosion of the pleural membranes. d. Inflammation around the tumor causes exudate in the small bronchi. 88. Which of the following drugs is usually prescribed for prophylaxis in persons in close contact with a patient with active tuberculosis? 293 89. Which of the following statements is FALSE? a. TB bacilli are spread by oral droplet. b. TB bacilli are slow-growing bacteria. c. Active TB must be treated in hospital for many months. d. Active TB can be prevented by good host resistance. 309 90. Choose the correct reason for severe hypoxia occurring with pulmonary edema: a. Diffusion of oxygen into the alveoli is impaired. b. Fluid in the pleural cavity prevents normal lung expansion. c. Increased concentration of CO2 impairs diffusion of oxygen. d. Increased blood flow through the lungs prevents diffusion of gases. 302 a. Streptomycin b. Isoniazid c. Rifampin d. Streptomycin 91. Which of the following drugs in an inhaler would likely be carried by individuals to provide immediate control of acute asthma attacks? 304 92. Development of emphysema in a nonsmoker may be the result of: a. a genetic factor. b. obesity. c. vitamin deficiencies. d. a developmental defect. 312 93. Which factors contribute to postoperative atelectasis? 1. Decreased secretions in the airways 2. Drug-related respiratory depression 3. Abdominal distention and pain 4. Excessive deep-breathing and coughing a. 1, 2 b. 2, 3 a. A glucocorticoid b. Epinephrine c. Cromolyn d. A β2-adrenergic agent c. 3, 4 d. 1, 4 289 94. Primary atypical pneumonia (PAP) is caused by: a. Klebsiella oxytoca. b. Candida albicans. c. Mycoplasma pneumoniae. d. Streptococcus pneumoniae. 317 95. All of the following are expected with infant respiratory distress syndrome EXCEPT: a. severe hypoxia. b. respiratory alkalosis. c. pulmonary vasoconstriction. d. fluid and protein in the alveoli. 282 96. Which factor usually causes metabolic acidosis to develop in association with hypoxia? a. Anaerobic metabolism b. Failure to excrete CO2 c. Liver dysfunction d. Increased blood volume 316 97. Mediastinal flutter associated with chest injury is likely to: a. cause pulmonary edema. b. cause hypocapnia. c. increase lung expansion. d. decrease venous return to the heart. 292 98. Which of the following individuals is NOT considered to be at high risk for developing active tuberculosis? 285 99. Which of the following distinguishes influenza from infectious rhinitis? a. Influenza is a viral infection. b. Treatment is symptomatic a. Homeless individuals b. Individuals with AIDS c. Persons who experience acute asthma attacks d. Those living in institutions c. Influenza has a sudden onset with fever, marked muscle aching, and severe malaise. d. Complications can occur with influenza. 300 100. The use of a continuous positive airway pump in the treatment of sleep apnea will: a. reduce bronchospasm. b. force expansion of pleural membranes. c. maintain an open airway. d. awaken the person and increase respirations. 309 101. Hemoptysis is a significant sign of: a. pleural effusion. b. pulmonary embolus. c. pulmonary edema. d. atelectasis. 293 102. Which of the following applies to anthrax infection? a. It is caused by a virus that mutates frequently. b. When inhaled, it causes flulike symptoms followed by acute respiratory distress. c. There is a long incubation period, often months, following exposure. d. It is a common infection in North America. 294 103. The mutated gene for cystic fibrosis is located on the: a. seventh chromosome. b. tenth chromosome. c. fifteenth chromosome. d. X chromosome. 298 Chapter 14: Neurological Disorders Chapter 14: Neurological Disorders Test Bank MULTIPLE CHOICE 1. Through what area does the cerebrospinal fluid circulate around the brain and spinal cord? a. Between the double layers of the dura mater b. In the subdural space c. In the subarachnoid space d. Through the arachnoid villi 327 2. Which of the following is the usual location of language centers? a. Left hemisphere b. Right hemisphere c. Brainstem d. Hypothalamus 329 3. What would be the effect of damage to the auditory association area in the left hemisphere? a. Loss of hearing in both ears b. Inability to understand what is heard c. Loss of hearing in the left ear d. Inability to determine the source of the sound 329 4. Which of the following applies to the corticospinal tract? a. It is an ascending tract. b. The nerve fibers conduct sensory impulses. c. It is an extrapyramidal tract. d. It is a pyramidal tract for efferent impulses. ANS: D REF REF: 332 5. What is a major function of the limbic system? a. Overall control of fluid balance b. Required for logical thinking, reason, and decision making c. Determines emotional responses d. Responsible for artistic and musical talents 330 6. Where are β1-adrenergic receptors located? a. Bronchiolar walls b. Arteriolar walls c. Cardiac muscle d. Glands of the intestinal tract 337 7. What does a vegetative state refer to? a. Depression of the reticular activating system (RAS) and inability to initiate action b. Loss of awareness and intellectual function but continued brainstem function c. Continuing intellectual function but inability to communicate or move d. Disorientation and confusion with decreased responsiveness 338-339 8. Which of the following conditions is NOT part of the criteria for a declaration of “brain death”? a. No activity on EEG b. Absence of all reflexes c. No spontaneous respirations d. Presence of any head injury 339 9. What is the best definition of aphasia? a. The inability to comprehend or express language appropriately b. Difficulty swallowing c. Loss of the visual field contralateral to the area of damage d. The inability to articulate words clearly 340 10. What is an early indicator of increased intracranial pressure? a. Papilledema b. Bilateral fixed dilated pupils c. Decreasing responsiveness d. Rapid heart rate 342 11. What is the rationale for vomiting in a patient who has increased intracranial pressure? a. Chemoreceptors responding to changes in the blood b. Pressure extending to spinal nerves c. Pressure on the emetic center in the medulla d. Stimuli to the hypothalamic center for hunger and thirst 342 12. What is the typical change in blood pressure in a patient who has increased intracranial pressure? a. Erratic diastolic pressure b. Decreasing systolic pressure c. Systolic and diastolic pressures decreasing proportionately d. Increasing pulse pressure 342 13. The largest category of primary malignant brain tumors that arise from cells in the central nervous system (CNS) are called: 345 14. Which of the following causes papilledema? a. gliomas. b. sarcomas. c. lymphomas. d. myelomas. a. Increased pressure of cerebrospinal fluid (CSF) at the optic disc b. Increased intraocular pressure c. Pressure on the oculomotor nerve d. Pressure on the optic chiasm 342 15. What is the effect of an enlarging brain abscess on cardiovascular activity? a. Increased heart rate and systemic vasodilation b. Low blood pressure and irregular heart and respiratory rates c. Systemic vasoconstriction and slower heart rate d. Immediate depression of the cardiac control centers 342 16. As intracranial pressure rises, the pupil of the eye, ipsilateral to the lesion, becomes dilated and unresponsive to light because of pressure on the: 342 17. Which of the following characteristics indicates that the CSF is normal? a. optic nerve. b. peripheral nervous system (PNS) fibers in cranial nerve III. c. sympathetic nervous system (SNS) nerve to the eye. d. occipital lobe. a. Cloudy and pale yellow color b. Presence of erythrocytes c. Presence of numerous leukocytes d. Clear and colorless fluid 327 18. Which of the following statements is TRUE about malignant brain tumors? a. Most brain tumors arise from malignant neurons. b. Primary brain tumors rarely metastasize outside the CNS. c. The blood-brain barrier prevents secondary brain tumors. d. Brainstem tumors do not manifest signs until they are quite large. 345 19. Secondary brain tumors usually arise from: a. severe head trauma. b. metastasized breast or lung tumors. c. exposure to carcinogenic agents. d. exposure to radiation. 345 20. Why are focal or generalized seizures sometimes an early indication of a brain tumor? a. Surrounding inflammation stimulates neurons to discharge spontaneously. b. Malignant tumors cause alkalosis, exciting the CNS. c. Systemic effects of the brain tumor may cause seizures. d. Metabolic effects of cancer change blood chemistry to trigger seizures. 345 21. Which of the following is a TRUE statement about transient ischemic attacks (TIAs)? a. They usually cause necrosis and permanent brain damage. b. They may be caused by rupture of an aneurysm or a damaged artery. c. They usually indicate systemic hypertension. d. They can warn of potential cerebrovascular accidents. 346 22. What is the probable source of an embolus causing a cerebrovascular accident (CVA)? a. Right ventricle of the heart b. Femoral vein c. Common carotid artery d. Pulmonary artery 347 23. Collateral circulation is most likely to be present when a CVA results from: a. rupture of a cerebral artery. b. an embolus. c. atherosclerosis. d. vasospasm in the cerebral circulation. 347 24. All of the following apply to CVA EXCEPT: a. the common cause is an atheroma with thrombus. b. maximum necrosis and infarction develop within several hours of onset. c. warning signs may appear with partial obstruction of the artery. d. increasing neurological deficits usually develop during the first few days. 346-347 25. Signs and symptoms of a stroke depend upon: a. location of obstruction, size of artery, and area affected. b. duration of the blockage, distance from the heart, and type of obstruction. c. health of the victim, area affected, and collateral circulation. d. size of the obstruction, condition of the heart, and duration of blockage. 348 26. In the weeks following CVA, why might some neurological function return? 1. Presence of collateral circulation 2. Immediate therapy to dissolve thrombi and maintain perfusion 3. Reduced inflammation in the area 4. Development of alternative neuronal pathways a. 1 only b. 2 only c. 1, 3 d. 2, 3, 4 e. 1, 2, 3, 4 347 27. Which of the following statements about berry aneurysms in the brain is NOT true? a. They usually develop at points of bifurcation in the circle of Willis. b. They are usually asymptomatic for many years. c. CSF remains free of blood. d. Following rupture, blood appears in the subarachnoid space. 349-350 28. In a case of bacterial meningitis, where does swelling and purulent exudate form? a. In the pia mater, arachnoid, and surface of the entire brain b. In the dura mater and epidural space c. At the site of the injury or entry point of the microbes d. Primarily around the spinal cord 350 29. What are significant signs of acute bacterial meningitis? a. Severe headache, nuchal rigidity, and photophobia b. Fatigue and lethargy, fever, and anorexia c. Focal signs, such as progressive paralysis in a limb d. Ascending paralysis beginning in the legs 351 30. In many types of encephalitis, such as St. Louis encephalitis, how are the viruses transmitted? a. Carriers b. Mosquito and tick bites c. Respiratory droplet d. Septic emboli in the circulation 352 31. All of the following apply to tetanus infection EXCEPT: a. it is caused by an anaerobic, spore-forming bacillus. b. the exotoxin causes strong skeletal muscle spasms. c. death usually results from respiratory failure. d. signs of fever, vomiting, stiff neck, and paralysis. 353 32. In cases of Guillain-Barré syndrome, what does the pathophysiology include? a. Damage and loss of function in the motor neurons of the spinal cord and medulla b. Encephalopathy, with disorientation, headache, and coma c. Infection and inflammation of the motor cortex d. Inflammation and demyelination of peripheral nerves, leading to ascending paralysis 354 33. How does a depressed skull fracture cause brain damage? a. A bone fragment penetrates and tears brain tissue. b. A section of the skull is missing, leaving the brain unprotected. c. A section of skull bone is displaced below the level of the skull, causing pressure on the brain. d. Many fracture lines are present, causing instability. e. The contrecoup injury is the cause of brain damage. 355 34. Following a head injury, what is the most likely cause of secondary damage to the brain? a. Hematoma or infection b. Laceration by foreign objects c. Hypoxia or acidosis d. Tearing of blood vessels as the brain rotates across the inside of the skull 357 35. An epidural hematoma is located between the: a. dura mater and the arachnoid mater. b. dura mater and the skull. c. arachnoid mater and the pia mater. d. pia mater and the brain. 358 36. What does the term otorrhea mean? a. Bleeding from the nose. b. CSF leaking from the ear. c. Torn meninges but no skull fracture. d. Hemorrhage from the ear. 358 37. Vertebral fractures are classified as: a. simple, compression, wedge, dislocation. b. compound, open, closed, shattered. c. complex, torsion, open, multiple. d. pressure, complex, simple, variable. 359 38. Following a spinal injury at C5, what is the expected effect during the period of spinal shock? a. Spastic paralysis below the level of the injury b. Urinary incontinence c. Possible periods of apnea d. Normal blood pressure 360 39. Following an injury at L2 to L3, what would indicate recovery from spinal shock? a. Spastic paraplegia b. Urinary retention c. Labile body temperature d. Increased sensation in the legs 361 40. What are the signs of autonomic dysreflexia in a person with cervical spinal injury? a. Unexpected drop in blood pressure and apnea b. Sudden marked increase in blood pressure with bradycardia c. Hyperreflexia in the arms and legs d. Urinary and bowel incontinence 362 41. Expressive aphasia is most likely to result from damage to: a. the left frontal lobe. b. the left temporal lobe. c. the right motor cortex. d. Wernicke’s area. 340 42. What is the usual result of damage to the right occipital lobe? a. Left eye is blind b. Loss of left visual field c. Right eye is blind d. Visual loss in the medial half of each eye 341 43. How does the heart rate change as intracranial pressure increases? a. Rate decreases b. Rate increases c. No change in rate d. Irregular heart rate 342 44. Which statement best describes herniation resulting from increased intracranial pressure? a. Movement of brain tissue into ventricles b. Movement of brain stem upward c. Pushing of excess CSF and blood down around the spinal cord d. Displacement of brain tissue downward toward the spinal cord 342 | 344 45. Which type of cerebrovascular accident (CVA) has the poorest prognosis? a. CVA caused by thrombus b. Hemorrhagic CVA c. Embolic CVA d. No difference among types 347 46. Which of the following factors predispose(s) an individual to a CVA? 1. Hypertension 2. Smoking cigarettes 3. History of coronary artery disease 4. Diabetes mellitus a. 1, 3 b. 1, 2, 4 c. 2, 4 d. 1, 2, 3, 4 348 47. What are the significant early signs of a ruptured cerebral aneurysm? a. Impaired speech and muscle weakness b. Severe headache, nuchal rigidity, and photophobia c. Abnormal sensations and tremors d. Vomiting and visual abnormalities 350 48. The stroke scale used to rapidly diagnose a stroke includes: a. capacity for speech, level of consciousness, motor skills, eye movements. b. motor skills, spatial awareness, time awareness, facial recognition. c. short-term memory, cognitive skills, speech, name recognition. d. hand-eye coordination, problem solving, ability to stand or walk, consciousness. 348 49. With regard to meningitis, choose the correct combination of microbe and the age group commonly affected. 350 50. Which of the following statements applies to a lumbar puncture? a. It is usually performed at L3-L4. b. Fluid is withdrawn from the epidural space. c. It can be used to confirm any diagnosis. d. The tissue seals up immediately after puncture. 344 51. Which signs are indicative of post-polio syndrome? a. Progressive spastic paralysis b. Ascending flaccid paralysis c. Progressive fatigue and weakness d. Increasing numbness and paresthesias 354 a. E. coli: elderly b. H. influenzae: neonate c. N. meningitides: children and youth d. S. pneumoniae: young children 52. Which of the following does NOT apply to Reye’s syndrome? a. There is no permanent damage in the body. b. It is precipitated by a combination of viral infection and administration of acetylsalicylic acid (ASA). c. Cerebral edema develops. d. Liver damage is common. 354 53. Which type of fracture typically occurs at the base of the skull? a. Depressed b. Contrecoup c. Comminuted d. Basilar 355 54. The primary reason for seizures frequently occurring with head injuries is: a. presence of blood irritates the neurons. b. otorrhea or rhinorrhea changes intracranial pressure. c. inflammatory response causes general hypoxia. d. CNS is depressed. 357 55. Brain injury where the brain is injured when it bounces off of the skull due to sudden acceleration or deceleration is referred to as a/an: 355 56. The rabies virus is usually transmitted by: a. respiratory droplets. b. insects such as mosquitoes. c. bites from infected animals. d. the fecal-oral route. 353 57. Common manifestations of rabies infection include: a. headache, foaming at the mouth, and difficulty swallowing. b. difficulty walking and coordinating movements. c. decreased sensitivity to sound and touch. d. vomiting, liver and kidney damage. 353 a. linear fracture b. contusion c. basilar injury d. contrecoup injury 58. Which statement is TRUE about tetanus infection? a. It is caused by a virus. b. Infection usually develops in deep puncture wounds. c. It causes flaccid skeletal muscles, impairing mobility. d. It affects peripheral nerves initially in the legs and feet. 353 59. Which of the following impairments results from infection by the polio virus? a. Pain and paresthesia in a cranial nerve or dermatome b. Loss of motor and sensory function in the peripheral nerves c. Inflammation and increased intracranial pressure d. Loss of function of motor neurons of the spinal cord and medulla 353 60. Herpes zoster can be identified by a typical: a. unilateral rash and pain along a cranial nerve or dermatome. b. weakness and muscle atrophy in the legs. c. ascending paralysis commencing in the legs. d. skeletal muscle spasms in the face and neck. 353 61. Which of the following conditions is marked by focal signs? a. Meningitis b. Brain abscess c. Encephalitis d. Intracerebral hemorrhage 351 62. Typical signs of a TIA include: a. rapidly increasing intracranial pressure. b. loss of consciousness. c. transient muscle weakness in a hand or leg. d. headache, photophobia, and nuchal rigidity. 346 63. In cases of noncommunicating hydrocephalus, why does excess cerebrospinal fluid (CSF) accumulate? 364 64. All of the following are typical signs of hydrocephalus in the neonate EXCEPT: a. Absorption of CSF through the arachnoid villi is impaired. b. Excessive amounts of CSF are produced in the ventricles. c. An obstruction is present in the aqueduct of Sylvius or other channel. d. Flow around the spinal cord is blocked. a. enlarged head with bulging fontanels. b. vomiting, headache, and paralysis. c. irritability and feeding difficulties. d. eyes turned downward with sclerae showing above the pupils. 365 65. The best description of a myelomeningocele is: a. asymptomatic failure of the posterior spinous processes of the vertebrae to fuse. b. herniation of the meninges through a vertebral defect. c. herniation of the meninges, CSF, and spinal cord or nerves through a vertebral defect. d. herniation of brain tissue through a defect in the cranium. 365 66. How is the presence of spina bifida diagnosed? a. Prenatally by ultrasound or detection of alpha-fetoprotein (AFP) in maternal blood or amniotic fluid b. Only after birth by direct observation of the sac c. After birth when the sac herniates as CSF builds up d. Only with a spinal X-ray 366 67. What characteristic is common to all individuals with cerebral palsy? a. Some loss of cognitive function b. One or more types of seizure c. Serious multiple communication difficulties d. Some degree of motor disability 367 68. Which of the following applies to cerebral palsy? a. Nonprogressive brain damage to the fetus or neonate b. A genetic defect affecting metabolism and causing degeneration in the neurons c. A developmental error during early growth of the peripheral nervous system d. A chromosomal defect resulting in abnormalities in many body structures 366-367 69. Which of the following is characteristic of generalized seizures? a. The localization of the seizure activity b. The uncontrolled discharge of neurons in both hemispheres c. Seizures that persist for several hours d. Loss of consciousness and all motor function 368 70. From the following, choose the two events (in correct sequence) that immediately follow the aura during a tonic-clonic event: a. Prodromal signs, then the clonic stage b. Clonic stage, then the tonic stage c. Loss of consciousness, then the tonic stage d. Loss of consciousness and cessation of respiration 369 71. What does the clonic stage of a seizure consist of? a. A sudden strong skeletal muscle contraction and rigidity of trunk and limbs b. A cry and contraction of abdominal and thoracic muscles c. Alternating contractions and relaxation of skeletal muscles d. Cessation of all skeletal muscle activity 369 72. How would a seizure consisting of bizarre or inappropriate activity be classified? a. Absence seizure b. Psychomotor seizure c. Focal seizure d. Jacksonian seizure 370 73. Which of the following is characteristic of multiple sclerosis? a. Remissions and exacerbations b. Predictable pattern of progression in all patients c. Onset in men and women more than 60 years of age d. Full recovery of function during remissions 371 74. Which statement does NOT apply to the pathophysiology of multiple sclerosis? a. Demyelination of axons b. It affects the brain, spinal cord, and cranial nerves c. It affects motor, sensory, and autonomic fibers d. Progressive random degeneration of peripheral nerves 371 75. Which of the following are common early signs of multiple sclerosis? a. Paralysis of the lower body, impaired cognitive function b. Areas of numbness, weakness in the legs, visual problems c. Sensory deficit in the legs and trunk, memory loss, urinary incontinence d. Tremors, speech impairment, hearing loss 371 76. Which of the following applies to Parkinson’s disease? a. Usually develops in men and women over 60 years of age. b. There is no apparent genetic component. c. The majority of cases are predisposed by intake of antipsychotic medications. d. It rarely develops in women. 373 77. What is the pathophysiological change in Parkinson’s disease? a. Degeneration of motor fibers in the pyramidal tracts b. Excess secretion of stimulatory neurotransmitters in the CNS c. Degeneration of the basal nuclei with a deficit of dopamine d. Deficit of acetylcholine and degeneration of the motor cortex in the frontal lobe 372-373 78. Which of the following are common early manifestations of Parkinson’s disease? a. Tremors at rest in the hands and repetitive motion of the hands b. Extreme weakness in the legs and spastic movements in the arms c. Visual deficits and speech impairment d. Loss of facial expressions and altered posture and gait 373 79. In which type of neuron is progressive degeneration occurring with amyotrophic lateral sclerosis (ALS)? a. Upper motor neurons b. Upper and lower motor neurons c. Motor and sensory neurons d. Motor, sensory, and autonomic system neurons 374 80. Which of the following statements does NOT apply to myasthenia gravis? a. The cholinergic receptors at the neuromuscular junctions are damaged. b. It is an autoimmune disorder. c. Muscle weakness and fatigue occur in the face and neck. d. Dementia develops in the later stage. 374-375 81. Which statement applies to Huntington’s disease? a. It is inherited as an autosomal recessive trait. b. It is manifested in individuals by age 20 years. c. It presents with choreiform movements in the upper body and decreased ability to concentrate. d. It causes decreased levels of all neurotransmitters in the CNS. 376 82. What are the characteristic changes in the brain of a patient with Alzheimer’s disease? a. Cortical atrophy with plaques and neurofibrillary tangles, impairing conduction b. Increased acetylcholine (ACh) and decreased GABA and serotonin levels c. Obstruction of many small arteries and arterioles throughout the cerebral cortex d. Vacuoles forming in the neurons, rapidly destroying them 376 83. Which disease is associated with excessive dopamine secretion, decreased gray matter in the temporal lobes, and abnormal hippocampal cells in the brain? 378 84. In which disorders do biochemical abnormalities involving the neurotransmitters in the brain occur? 1. Bipolar disorder 2. Schizophrenia 3. Huntington’s disease 4. AIDS dementia a. 1, 3 b. 1, 4 a. Creutzfeldt-Jakob disease b. Schizophrenia c. Panic disorder d. Depression c. 1, 2, 3 d. 2, 3, 4 375 | 378 85. Which of the following are typical characteristics associated with schizophrenia? a. Disorganized thought processes, short attention span, delusions b. Lack of energy and motivation, poor concentration, insomnia c. Hyperventilation, tachycardia, intense anxiety d. Memory loss, mood swings, hostile behavior 378 86. What is the typical initial effect of a herniated intervertebral disc at the L4 to L5 level? a. Back pain and weakness at waist level b. Muscle weakness in both legs c. Lower back pain radiating down the leg d. Urinary incontinence 380 87. What causes a herniated intervertebral disc? a. A tear in the nucleus pulposus b. A protrusion of the nucleus pulposus through the annulus fibrosis a. cerebellum. c. Displacement of the annulus fibrosis between the laminae d. Failure of the spinous processes to restrict movement of the intervertebral disc 380 88. Which of the following dietary supplements has reduced the incidence of spina bifida in recent years? 366 89. Which of the following is the most common cause of brain damage in children with cerebral palsy? 366 90. The ataxic form of cerebral palsy results from damage to the: a. Vitamin B6 b. Folic acid c. Vitamins A and D d. Zinc and magnesium a. Hyperbilirubinemia b. Hypoglycemia c. Hypoxia d. Trauma a. Absence b. motor cortex. c. basal nuclei. d. pyramidal tracts. 367 91. Which of the following is used to confirm the diagnosis of, and classify, seizures? a. Characteristics of the aura b. Presence of precipitating factors c. Electroencephalogram d. Changes in the characteristics of cerebrospinal fluid 370 92. Which statement does NOT apply to status epilepticus? a. Seizures are recurrent or continuous without full recovery between episodes. b. Severe hypoxia and acidosis develop. c. Person does not lose consciousness during seizure. d. If the episode persists, there may be additional brain damage. 369 93. Which type of seizure commonly occurs in children? b. Tonic-clonic c. Focal d. Complex partial 369 94. All of the following may precipitate a seizure EXCEPT: a. hypoglycemia. b. hypoventilation. c. brain abscess. d. high fever in young child. 368-369 95. Which of the following is NOT a typical effect of advanced Parkinson’s disease? a. Difficulty chewing and swallowing b. Urinary retention c. Loss of vision d. Orthostatic hypotension 373 96. Which of the following is a typical early sign of amyotrophic lateral sclerosis (ALS)? a. Impaired ventilation b. Cognitive impairment c. Poor control of eye movement d. Weakness and muscle atrophy in upper limbs 374 97. Which of the following classes of drugs may provide temporary improvement in cases of myasthenia gravis? 374-375 98. Which of the following are typical early signs of Alzheimer’s disease? 1. Behavioral changes 2. Reduced ability to reason and problem solve 3. Decreased verbal responses 4. Urinary incontinence a. 1, 2 b. 1, 4 c. 2, 3 a. Skeletal muscle relaxants b. Dopamine replacement drugs c. Anticholinesterase agents d. GABA replacement drugs d. 1, 3, 4 377 99. Which of the following is NOT considered to be a common contributing factor to AIDS dementia? 378 100. Communicating hydrocephalus causes increased intracranial pressure because of: a. atresia at the foramen magnum. b. failure of the subarachnoid to absorb CSF. c. obstruction in the lumbar area of the spinal cord. d. scar tissue from encephalitis blocking flow of CSF. 364 101. Failure of the spinous processes to fuse, but without herniation of the meninges, is called: a. spina bifida occulta. b. meningocele. c. myelomeningocele. a. Invasion of the central nervous system by HIV b. Development of arteriosclerosis c. Secondary toxoplasmosis infection d. Development of cerebral lymphoma d. encephalocele. 365 102. Which statement is TRUE about amyotrophic lateral sclerosis (ALS)? a. Cognitive function remains normal. b. ALS affects primarily young women. c. Sensory neurons are damaged initially. d. Cause of death is usually a cardiac arrhythmia. 374 103. Creutzfeldt-Jakob disease is caused by: a. inheritance of an autosomal dominant trait. b. infection in the brain by HIV. c. an autoimmune reaction that damages nerve receptors. d. infection in the brain by a prion. 378 104. Huntington’s disease is diagnosed by: a. urinalysis. b. motor skills tests. c. DNA analysis. d. antibody agglutination test. 376 105. Which statement is TRUE about depression? a. It is classified as a mood disorder. b. Episodes of intense fear are recurrent. c. It is marked by increased appetite and libido. d. It is not a common condition. 379 Chapter 15: Disorders of the Eye, Ear, and Other Sensory Organs Chapter 15: Disorders of the Eye, Ear, and Other Sensory Organs Test Bank MULTIPLE CHOICE 1. What do the extrinsic muscles of the eye control? a. Movement of the eyeball b. Movement of the eyelid c. Size of the pupil d. Shape of the lens 387 2. What must happen for the pupil of the eye to dilate? a. The circular muscle of the iris must contract. b. Cranial nerve III must be activated. c. Stimulation of the sympathetic nervous system is required. d. The optic nerve must be stimulated. 387 3. Which of the following is caused by an irregular curvature of the cornea or lens? a. Nystagmus b. Astigmatism c. Hyperopia d. Strabismus 389 4. Trachoma is an eye infection caused by: a. influenza virus. b. Candida albicans. c. Staphylococcus bacteria. d. Chlamydia bacteria. 391 5. Which statement does NOT apply to chronic glaucoma? a. Degeneration and obstruction of the trabecular network b. Gradual increase in intraocular pressure c. Abnormally narrow angle between the cornea and iris d. Damage to the retina and optic nerve 391-392 6. Which disorder is manifested by loss of peripheral vision? a. Retinal detachment b. Chronic (wide-angle) glaucoma c. Cataract d. Macular degeneration 392 7. Which of the following involves a gradual clouding of the lens of the eye? a. Glaucoma b. Cataract c. Macular degeneration d. Keratitis 393 8. Which of the following is a likely consequence of an untreated detached retina? a. Lack of nutrients causing death of retinal cells b. Edema of the cornea causing blurred vision c. Cupping of the optic disc with damage to the optic nerve d. Damage to the fovea centralis 394 9. Which of the following is a sign of a detached retina? a. Painless blurring of vision b. Eye pain, halos around lights, and nausea c. Progressive loss of central vision d. No pain, development of a dark area in the visual field 394 10. What is the basic pathological change with macular degeneration? a. Increased amount of aqueous humor in the eye b. Movement of vitreous humor between the retina and the choroid c. Degeneration of the retinal cells in the fovea centralis d. Damage to the optic nerve and meninges 394 11. What does the inner ear contain? a. Malleus, incus, and stapes b. Organ of Corti and semicircular canals c. Tympanic membrane and auditory canal d. Ossicles and oval window 395 12. Which of the following is an example of conduction deafness? a. Damage to the organ of Corti b. Degeneration of cranial nerve VIII c. Adhesions reducing the movement of the ossicles d. Trauma affecting the temporal lobe 396 13. In a case of acute otitis media, what would a purulent discharge in the external canal of the ear and some pain relief likely indicate? 398 14. How does otosclerosis cause hearing loss? a. Infection of the external ear b. Obstruction of the auditory tube c. Rupture of the tympanic membrane d. Spread of infection into the mastoid cells a. Fixation of the stapes to the oval window b. Adhesions between the ossicles c. Fibrosis in the tympanic membrane d. Overgrowth of bone obstructing the auditory tube 399 15. Why does vertigo occur with Ménière’s syndrome? a. Fluid is lost from the inner ear. b. Increased blood pressure causes edema in the middle and inner ears. c. Damage occurs to the vestibular branch of the auditory nerve. d. Excessive endolymph impairs the function of hair cells in the labyrinth. 399 16. Which is the early effect of age-related macular degeneration? a. Loss of central visual acuity b. Intermittent pain and blurred vision c. Loss of peripheral vision d. Loss of night vision and color perception 394 17. Which of the following is often the first sign of ototoxicity from drugs or chemicals? a. Sudden total loss of hearing b. Tinnitus c. Severe pain in ear d. Fluid exudate draining from ear 396 18. Which of the following statements is TRUE? a. Conduction deafness results from inner ear damage. b. Cochlear implants may restore hearing in cases of sensorineural loss. c. Damage to the auditory area of the brain causes deafness in one ear. d. Cochlear implants can replace the auditory pathway in all deaf individuals. 396-397 19. Loss of the left visual field results from damage to the: a. left optic nerve. b. right optic nerve. c. left occipital lobe. d. right occipital lobe. 389 20. The involuntary abnormal movement of one or both eyes is referred to as: a. strabismus. b. nystagmus. c. presbyopia. d. diplopia. 389-390 21. An infection that damages the auditory nerve can cause what type of hearing loss? a. Sensorineural b. Conduction c. Semiacute d. Inflammatory 396 22. Which fluid is found surrounding the optic disc? a. Aqueous humor b. Vitreous humor c. Cerebrospinal fluid d. Tears 389 23. The area providing the greatest visual acuity is the: a. Macula lutea b. Fovea centralis c. Optic disc d. Lens 388 24. Narrow-angle glaucoma develops when the angle is decreased between the: a. retina and ciliary process. b. lens and ciliary body. c. iris and cornea. d. iris and lens. 391-392 25. The lens and cornea are nourished by: a. small capillaries. b. tears. c. vitreous humor. d. aqueous humor. 387 26. Which term refers to near-sightedness? a. Hyperopia b. Presbyopia c. Myopia d. Diplopia 389 27. Severe pain develops with narrow-angle glaucoma when the: a. pupils are constricted. b. pupils are dilated. c. lens changes shape. d. excess vitreous humor forms. 393 28. The semicircular canals of the inner ear are responsible for: a. balance and equilibrium. b. hearing in the upper frequency range. c. hearing in the lower frequency range. d. balancing the pressure in the auditory canal. 396 29. Trachoma is indicated by the presence of: a. purulent exudate and red sclerae. b. corneal abrasions by the infected eyelids. c. diplopia and cloudy lens. d. ptosis and fixed dilation of the pupil. 391 30. Which of the statements apply to infection of the eye by Staphylococcus aureus? 1. It involves the conjunctiva. 2. It is highly contagious. 3. It is commonly known as “pinkeye.” 4. It usually causes keratitis and permanent visual loss. a. 1, 3 b. 2, 3 c. 2, 4 d. 1, 2, 3 390 31. Herpes simplex virus is a common cause of: a. conjunctivitis. b. corneal ulceration and scarring. c. eye infection in the neonate. d. total blindness. 391 32. Sensory receptors that provide information about body movement, orientation, or muscle stretch are referred to as: 386 Chapter 16: Endocrine System Disorders Chapter 16: Endocrine System Disorders Test Bank MULTIPLE CHOICE 1. What kind of control mechanism is indicated when increased blood glucose levels stimulate increased secretion of insulin? 403-404 a. visceroceptors. b. exteroceptors. c. mechanoceptors. d. proprioceptors. a. Control by releasing hormones b. Control by tropic hormones c. Negative feedback control d. Hypothalamus/hypophysis coordination 2. What is the most common cause of endocrine disorders? a. Malignant neoplasm b. Infection c. Congenital defect d. Benign tumor 406 3. Choose the statement that applies to type 1 diabetes mellitus. a. Onset often occurs during childhood. b. Relative insufficiency of insulin or insulin resistance develops. c. It can be treated by diet, weight control and exercise, or oral hypoglycemics. d. Complications rarely occur. 406 4. Why does polyuria develop with diabetes mellitus? a. Increased thirst and hypoglycemia b. Ketoacidosis c. Osmotic pressure due to glucose d. Diabetic nephropathy 407 5. What is the cause of diabetic ketoacidosis? a. Excess insulin in the body b. Loss of glucose in the urine c. Failure of the kidney to excrete sufficient acids d. Increased catabolism of fats and proteins 408 6. What is a precipitating factor for diabetic ketoacidosis? a. Skipping a meal b. Anorexia c. Serious infection d. Insulin overdose 410 7. Which of the following may cause insulin shock to develop? a. Strenuous exercise b. Missing an insulin dose c. Eating excessively large meals d. Sedentary lifestyle 409 8. Which of the following indicates hypoglycemia in a diabetic? a. Deep, rapid respirations b. Flushed dry skin and mucosa c. Thirst and oliguria d. Staggering gait, disorientation, and confusion 409 9. Which of the following are signs of diabetic ketoacidosis in an unconscious person? a. Pale moist skin b. Thirst and poor skin turgor c. Deep rapid respirations and fruity breath odor d. Tremors and strong rapid pulse 410 10. Immediate treatment for insulin shock may include: a. administration of bicarbonates. b. consumption of fruit juice or candy. c. induced vomiting. d. consumption of large amounts of water. 409 11. What causes loss of consciousness in a person with diabetic ketoacidosis? a. Toxic effects of excessive insulin b. Excessive glucose in the blood c. Metabolic acidosis d. Lack of glucose in brain cells 411 12. Which of the following does NOT usually develop as a complication of diabetes? a. Osteoporosis b. Nephropathy c. Impotence d. Peripheral neuropathy 412-413 13. How do many oral hypoglycemic drugs act? a. To replace insulin in patients with insulin-dependent diabetes mellitus (IDDM) b. To transport glucose into body cells c. To prevent gluconeogenesis d. To stimulate the pancreas to produce more insulin 409 14. Diabetes may cause visual impairment through damage to the lens; this is referred to as: a. cataracts. b. macular degeneration. c. myopia. d. strabismus. 415 15. Which of the following applies to diabetic macro-angiography? 1. It affects the small arteries and arterioles. 2. It is related to elevated serum lipids. 3. It leads to increased risk of myocardial infarction and peripheral vascular disease. 4. It frequently causes damage to the kidneys. a. 1, 3 b. 1, 4 c. 2, 3 d. 2, 4 412 16. Why is amputation frequently a necessity in diabetics? a. Necrosis and gangrene in the feet and legs b. Lack of glucose to the cells in the feet and legs c. Severe dehydration in the tissues d. Elevated blood glucose increasing blood viscosity 412 17. A type of diabetes that may develop during pregnancy and disappear after delivery is called: a. temporary maternal diabetes. b. fetal diabetes. c. acute developmental diabetes. d. gestational diabetes. 407 18. Which one of the following develops hypoglycemia more frequently? a. Type 1 diabetic patients b. Type 2 diabetic patients c. Patients with a poor stress response d. Patients with a regular exercise and meal plan 406 19. Which of the following hormonal imbalances causes Addison’s disease? a. Increased glucocorticoids b. Decreased glucocorticoids c. Deficit of antidiuretic hormone (ADH) d. Deficit of T3 and T4 423 20. Which of the following hormonal imbalances causes myxedema? a. Increased glucocorticoids b. Decreased glucocorticoids c. Deficit of ADH d. Deficit of T3 and T4 422 21. Which of the following hormonal imbalances causes diabetes insipidus? a. Increased insulin b. Decreased glucocorticoids c. Deficit of ADH d. Deficit of T3 and T4 407 22. What is caused by hyperparathyroidism? a. Hypocalcemia b. Tetany c. Bone demineralization d. Deficit of vitamin D 416 23. What is caused by hypocalcemia due to hypoparathyroidism? 1. Skeletal muscle twitching or spasm 2. Weak cardiac contraction 3. Increased secretion of parathyroid hormone (PTH) 4. Decreased serum phosphate level a. 1, 2 b. 1, 3 c. 2, 3 d. 3, 4 415 24. Which of the following applies to acromegaly? a. It occurs in infants and children. b. It causes excessive longitudinal bone growth. c. It results from excessive secretion of growth hormone (GH). d. It does not change soft tissue growth. 416 25. Which of the following may cause goiter? 1. Hyperthyroidism 2. Hypothyroidism 3. Lack of iodine in the diet 4. Pheochromocytoma a. 1, 4 b. 2, 3 c. 1, 2, 3 d. 1, 2, 3, 4 419 26. Which signs are typical of Graves’ disease? a. Facial puffiness, bradycardia, and lethargy b. Exophthalmos and tachycardia c. delayed physical and intellectual development d. Goiter and decreased basal metabolic rate (BMR) 420 27. Characteristics of Cushing’s syndrome include all of the following EXCEPT: a. Heavy body and round face b. Atrophied skeletal muscle in the limbs c. Staring eyes with infrequent blinking d. Atrophy of the lymph nodes 422-423 28. Which of the following is an effect of long-term glucocorticoid therapy? a. Decreased secretion from the adrenal cortex gland b. An increased inflammatory response to irritants c. Hypotension and poor circulation d. Increased number of hypersensitivity reactions 422 29. Which of the following is an effect of Addison’s disease? a. Elevated blood glucose levels b. High blood pressure c. Low serum potassium levels d. Poor stress response 423 30. What is the most common cause of type 1 diabetes mellitus? a. Increased glucose production in the liver b. Destruction of pancreatic cells by an autoimmune reaction c. Increased resistance of body cells to insulin action d. Chronic obesity 406 31. Why does glucosuria occur in diabetics? a. Excess ketoacids displace glucose into the filtrate. b. Excess water in the filtrate draws more glucose into the urine. c. The amount of glucose in the filtrate exceeds the renal tubule transport limit. d. Sufficient insulin is not available for glucose reabsorption. 407 32. Which of the following are common early signs of a pituitary adenoma? 1. Persistent headaches 2. Hemianopia 3. Hypertension 4. Papilledema a. 1, 4 b. 2, 3 c. 1, 2 d. 1, 3, 4 422 33. Which of the following does NOT apply to inappropriate ADH syndrome? a. The cause is excess ADH secretion. b. Severe hyponatremia results. c. Excessive sodium is retained. d. Fluid retention increases. 418 34. What is/are the effect(s) of thyrotoxic crisis? a. Hyperthermia and heart failure b. Hypotension and hypoglycemia c. Toxic goiter and hypometabolism d. Decreased stress response 420 35. Which of the following conditions may precipitate or exacerbate hyperglycemia? a. Hypothyroidism b. Cushing’s disease c. Addison’s disease d. Growth hormone deficit 423 36. Which of the following conditions may cause immunosuppression? a. Graves’ disease b. Acromegaly c. Cushing’s disease d. Diabetes insipidus 423 37. Hyperosmolar hyperglycemic nonketotic coma (HHNC) more frequently develops in patients with: 411 38. Which of the following is recommended for immediate treatment of hypoglycemic shock? 1. If conscious, immediately give sweet fruit juice, honey, candy, or sugar. 2. If unconscious, give nothing by mouth (require intravenous glucose 50%). 3. Treat immediately with insulin. 4. Give large quantity of clear fluids for shock. a. 1, 2 b. 1, 3 a. type 1 diabetes. b. type 2 diabetes. c. Grave’s disease. d. hyperparathyroidism. c. 2, 3 d. 1, 3, 4 410 39. All these tissues use glucose without the aid of insulin EXCEPT: a. liver. b. digestive system. c. exercising skeletal muscle. d. brain. 406 40. Differences between type 1 and type 2 diabetes include which of the following? a. Type 1 diabetes weight gain is common, and type 2 weight loss often occurs. b. Type 1 diabetes leads to fewer complications than does type 2 diabetes. c. Type 1 diabetes may be controlled by adjusting dietary intake and exercise, but type 2 diabetes requires in d. Type 1 diabetes occurs more frequently in children and adolescents, and type 2 diabetes occurs more ofte 406-407 41. Complications of diabetes mellitus include: a. peripheral neuropathy. b. frequent infections. c. cataracts. d. A, B, and C. 412-413 42. Which of the following often causes hyperparathyroidism? a. A malignant tumor in the parathyroid glands b. End-stage renal failure c. Osteoporosis d. Radiation involving the thyroid gland and neck area 416 43. Dwarfism is caused by: a. excessive levels of somatotropin (GH). b. a deficit of somatotropin (GH). c. excessive levels of insulin. d. excessive levels of parathyroid hormone. 416 44. Which of the following results from a deficit of antidiuretic hormone (ADH)? a. Inappropriate ADH syndrome b. Gigantism c. Diabetes insipidus d. Myxedema 418 45. Goiters occur more frequently in persons living in the: a. Great Lakes or mountainous regions. b. southwest United States. c. temperate regions. d. areas bordering the oceans. 419 46. Which of the following is caused by Graves’ disease? a. Hypermetabolism b. Decreased size of thyroid gland c. Bradycardia and hypothermia d. Decreased blood levels of T3, T4, and TSH 420 47. Goiters may be caused by: a. hypothyroid conditions only. b. either hypothyroid or hyperthyroid conditions. c. hyperthyroid conditions only. d. fungal infections such as candidiasis. 419 48. Severe impairment of all aspects of growth and development, including difficulty feeding, mental retardation, and stunted skeletal growth, are associated with: 422 49. A benign tumor of the adrenal medulla that secretes epinephrine and norepinephrine is called: a. pheochromocytoma. b. Cushing’s syndrome. c. Graves’ disease. d. Addison’s disease. 422 50. The anterior pituitary gland secretes all of the following hormones EXCEPT: a. prolactin (PRL). a. myxedema. b. Cushing’s syndrome. c. diabetes insipidus. d. cretinism. e. Graves’ disease. b. glucagon. c. adrenocorticotropic hormone (ACTH). d. growth hormone (GH). 403 51. Which of the following applies to oxytocin? 1. It stimulates contraction of the uterus after delivery. 2. It stimulates ejection of breast milk during lactation. 3. It stimulates mammary gland production of milk. 4. It is released from the adenohypophysis. a. 1, 2 b. 1, 4 c. 1, 3, 4 d. 1, 2, 3, 4 404 52. Which of the following is a major function of the hormone norepinephrine? a. Inhibition of an excessive stress response b. Visceral and cutaneous vasoconstriction c. Increased force of heart contraction d. Vasodilation in skeletal muscle 404 53. Early signs of hyperglycemia include polyphagia, which means: a. thirst. b. increased urine output. c. hunger. d. glucose in the urine. 411 54. Which of the following hormones is involved in both the stress response and the antiinflammatory response? 404 55. Polydipsia occurs with diabetes mellitus when: a. lack of insulin causes hunger. b. ketone levels rise in the blood. c. polyuria causes dehydration. d. glucosuria causes ketoacidosis. a. Aldosterone b. Norepinephrine c. Thyroxine d. Cortisol 407 56. Metabolic syndrome is marked by: a. abnormal lipid and glucose metabolism. b. periodic hypotension. c. deficit of glucagon. d. early onset of type 1 diabetes mellitus. 407 57. Compensation mechanisms occurring in the early stage of diabetic ketoacidosis include: a. Kussmaul’s respirations. b. polydipsia. c. ketonuria. d. seizures. 410 58. Which of the following may occur with a pituitary adenoma? a. Low blood pressure and bradycardia b. Headache and seizures c. Vomiting and diarrhea d. Loss of vision in one eye 416 59. Which of the following may cause hypertension? a. Hypoparathyroidism b. Hypoglycemia c. Pheochromocytoma d. Addison’s disease 422 60. Catabolic effects of Cushing’s syndrome include: a. osteoporosis. b. hypertension. c. increased erythrocyte production. d. moon face and buffalo hump. 423 61. Blood glucose levels are increased by: 1. glucocorticoids. 2. glucagon. 3. epinephrine. 4. norepinephrine. 5. parathyroid hormone (PTH) a. 1, 2 b. 1, 2, 3 c. 2, 4, 5 d. 1, 3, 4, 5 403 62. Which of the following are likely present in a patient immobilized for a long period of time? a. Hypocalcemia and low serum parathyroid hormone (PTH) levels b. Hypocalcemia and high serum PTH levels c. Hypercalcemia and low serum PTH levels d. Hypercalcemia and high serum PTH levels 416 63. Which of the following may cause high serum levels of parathyroid hormone? a. Hypoparathyroidism b. Chronic renal failure c. Hypercalcemia d. Adenoma in the thyroid gland 416 64. Diabetic retinopathy results from: a. degeneration of large blood vessels supplying the eye. b. abnormal metabolism in the lens of the eye. c. neuropathy affecting the optic nerve. d. obstruction or rupture of retinal blood vessels. 412 65. Why does hypocalcemia cause tetany? a. Skeletal muscle contractions are weaker. b. Nerves to skeletal muscle are more excitable. c. Calcium is not stored in skeletal muscle cells. d. Serum phosphate levels are low. 415 Chapter 17: Digestive System Disorders Chapter 17: Digestive System Disorders Test Bank MULTIPLE CHOICE 1. Which of the following cells in the gastric mucosa produce intrinsic factor and hydrochloric acid? a. Parietal cells b. Chief cells c. Mucous cells d. Gastrin cells 433 2. Which of the following is the primary site for absorption of nutrients? a. Stomach b. Duodenum c. Ileum d. Ascending colon 434 3. When highly acidic chyme enters the duodenum, which hormone stimulates the release of pancreatic secretions that contains very high bicarbonate ion content? 435-436 4. Which of the following breaks protein down into peptides? a. Amylase b. Peptidase c. Lactase a. Gastrin b. Secretin c. Cholecystokinin d. Histamine d. Trypsin 432 5. In which structure is oxygenated blood (arterial) mixed with unoxygenated blood (venous) so as to support the functions of the structure? 433 6. Which of the following stimulates increased peristalsis and secretions in the digestive tract? a. Sympathetic nervous system b. Vagus nerve c. Increased saliva d. Absence of food in the system 435 7. Which of the following is contained in pancreatic exocrine secretions? a. Bicarbonate ion b. Hydrochloric acid c. Activated digestive enzymes a. Pancreas b. Liver c. Small intestine d. Spleen d. Insulin 435 8. The presence of food in the intestine stimulates intestinal activity but inhibits gastric activity through the: 435 9. Which of the following processes is likely to occur in the body immediately after a meal? a. Lipolysis b. Ketogenesis c. Gluconeogenesis d. Glycogenesis 433 10. What does the term gluconeogenesis refer to? a. Breakdown of glycogen to produce glucose b. Conversion of excess glucose into glycogen for storage c. Formation of glucose from protein and fat a. defecation reflex. b. enterogastric reflex. c. vomiting reflex. d. autodigestive reflex. d. Breakdown of glucose into carbon dioxide and water 433 11. Normally, proteins or amino acids are required to produce all of the following EXCEPT: a. peptide hormones. b. clotting factors and antibodies. c. cellular energy. d. hemoglobin. 434 12. Which of the following statements applies to bile salts? a. They give feces the characteristic brown color. b. They are enzymes used to break down fats into free fatty acids. c. They emulsify lipids and lipid-soluble vitamins. d. They are excreted in the feces. 434 13. The visceral peritoneum: a. lines the abdominal wall. b. hangs from the stomach over the loops of small intestine. c. contains many pain receptors. d. forms the outer covering of the stomach. 430 14. The early stage of vomiting causes: a. metabolic alkalosis. b. metabolic acidosis. c. increased respirations. d. increased excretion of hydrogen ions. 440 15. Yellow or greenish stained vomitus usually indicates the presence of: a. bile. b. blood. c. protein. d. bacteria. 438 16. Small, hidden amounts of blood in stool are referred to as: a. melena. b. occult blood. c. frank blood. d. hematemesis. 439 17. Severe vomiting can lead to metabolic acidosis because of increased: a. ketones produced. b. CO2 retained in the lungs and kidneys. c. hypovolemia and lactic acid production. d. metabolic rate. 440 18. Which of the following applies to the act of swallowing? a. It requires coordination of cranial nerves V, IX, X, and XII. b. It is entirely voluntary. c. It is controlled by a center in the hypothalamus. d. It does not affect respiration. 432 19. What does the defecation reflex require? a. Stimulation by the sympathetic nervous system b. Contraction of the internal anal sphincter c. Coordination through the sacral spinal cord d. Voluntary relaxation of pelvic muscles 435 20. What is the definition of dysphagia? a. A herniation of the gastric mucosa through a segment of weakened muscle b. Recurrent reflux of chyme into the esophagus c. Absence of a connection of the esophagus to the stomach d. Difficulty in swallowing 448 21. What does congenital esophageal atresia cause? a. Direct passage of saliva and food from the mouth into the trachea b. Repeated reflux of gastric secretions into the esophagus c. No fluid or food entering the stomach d. Gastric distention and cramps 448-449 22. Which of the following applies to cleft palate? a. The mandibular processes do not fuse. b. The hard and soft palates do not fuse during the first trimester of pregnancy. c. Exposure to environmental factors in the last trimester causes the defect. d. Speech and eating are not affected. 444 23. Oral candidiasis is considered to: a. be a common bacterial infection in infants and young children. b. cause painful ulcerations in the mucosa and tongue. c. cause white patches in the mucosa that cannot be scraped off. d. be an opportunistic fungal infection of the mouth. 444 24. Why does herpes simplex infection tend to recur? a. Active infection is usually asymptomatic. b. The virus builds up a resistance. c. The virus persists in latent form in sensory nerve ganglia. d. The virus mutates; therefore, no effective immunity develops. 444 25. What does the term periodontitis refer to? a. Erosion of the enamel tooth surface b. Bacterial damage to the teeth and surrounding alveolar bone c. Inflammation and infection of the gingivae d. Formation of calcified plaque on the tooth 446 26. What is/are common location(s) for oral cancer? a. Floor of the mouth or tongue borders b. Mucosa lining the cheeks c. Hard and soft palate d. Gingivae near the teeth 448 27. What is a common cause of hiatal hernia? a. An abnormally long esophagus b. Increased intra-abdominal pressure c. Stenosis of the hiatus in the diaphragm d. A small fundus in the stomach 450-451 28. What is a common sign of acute gastritis? a. Colicky right upper quadrant pain b. Vomiting and anorexia c. Projectile vomiting after eating d. Diarrhea with abdominal distention 451 29. What does the pathophysiology of chronic gastritis include? a. Atrophy of the gastric mucosa with decreased secretions b. Hyperchlorhydria and chronic peptic ulcers c. Frequent vomiting and diarrhea d. Episodes of acute inflammation and edema of the mucosa 451 30. What is a common cause of gastroenteritis due to Salmonella? a. Unrefrigerated custards or salad dressings b. Poorly canned foods c. Raw or undercooked poultry or eggs d. Contaminated water 452 31. Which of the following individuals is likely to develop acute gastritis? a. A long-term, heavy cigarette smoker b. Patient with arthritis taking enteric-coated aspirin on a daily basis c. A person with an autoimmune reaction in the gastric mucosa d. An individual with an allergy to shellfish 451-452 32. What does congenital pyloric stenosis involve? a. Absence of peristalsis in the lower section of the stomach b. Failure of an opening to develop between the stomach and duodenum c. Hypertrophy of smooth muscle in the pylorus d. Thickening of the gastric wall due to chronic inflammation 457 33. A patient with acquired pyloric stenosis would likely: a. have an increase in appetite. b. have chronic diarrhea. c. develop severe colicky pains. d. vomit undigested food from previous meals. 457 34. Prolonged or severe stress predisposes to peptic ulcer disease because: a. of reduced blood flow to the gastric wall and mucous glands. b. of reduced bicarbonate content in bile and pancreatic secretions. c. stress increases the number of acid- and pepsinogen-secreting cells. d. increased epinephrine increases motility. 455 35. The pathophysiology of peptic ulcer disease may involve any of the following EXCEPT: a. decreased resistance of the mucosal barrier. b. increased stimulation of pepsin and acid secretions. c. infection by H. pylori. d. increased stimulation of mucus-producing glands. 453-455 36. Which of the following would a perforated gastric ulcer likely cause? a. Severe anemia b. Chemical peritonitis c. Severe gastric hemorrhage d. Pyloric obstruction 455 37. What is frequently the first manifestation of stress ulcers? a. Abdominal discomfort between meals and at night b. Nausea and diarrhea c. Hematemesis d. Sharp colicky pain with food intake 456 38. What would be the result of chronic bleeding from gastric carcinoma? a. Occult blood in the stool and anemia b. Hematemesis and shock c. Abdominal pain and distention d. Red blood on the surface of the stool 457 39. Following gastric resection, the onset of nausea, cramps, and dizziness immediately after meals indicates: 457-458 40. Bilirubin is a product of: a. hemolysis of red blood cells (RBCs) and breakdown of hemoglobin. b. production of excess chyme and bile. c. mixing of undigested food and gastric secretions. a. a large volume of chyme has entered the intestines, causing distention. b. severe hypoglycemia has developed. c. the pylorus is restricting the flow of chyme. d. bile and pancreatic secretions are irritating the small intestine. d. accumulation of white blood cells (WBCs) due to infection. 460 41. Why does mild hyperbilirubinemia occur in newborns? a. Blood incompatibility between mother and child b. Damage to many erythrocytes during the birth process c. Poor circulation and albumin transport for bilirubin d. Immature liver cannot process bilirubin quickly enough 460 42. Predisposing factors to cholelithiasis include excessive: a. bilirubin or cholesterol concentration in the bile. b. water content in the bile. c. bile salts in the bile. d. bicarbonate ions in the bile. 488 43. What is the major effect when a gallstone obstructs the cystic duct? a. Intrahepatic jaundice b. Acute pancreatitis c. Severe colicky pain in upper right quadrant d. Inflammation and infection in the gallbladder 488 44. Obstruction of the biliary tract by gallstones is referred to as: a. cholelithiasis. b. cholecystitis. c. cholangitis. d. choledocholithiasis. 458 45. Which of the following applies to hepatitis A infection? a. It is also called serum hepatitis. b. It is transmitted by the fecal-oral route. c. It contains a double strand of DNA. d. It frequently leads to chronic hepatitis. 462 46. What can be concluded if the hepatitis B antigen level remains high in the serum? a. Acute infection is present. b. Chronic infection has developed. c. Liver failure is in progress. d. The usual prolonged recovery from any viral infection is occurring. 462 47. What is the most common type of hepatitis transmitted by blood transfusion? a. HAV b. HBV c. HCV d. HEV 464 48. During the course of a hepatitis B infection, the onset of jaundice occurs in the: a. incubation period. b. preicteric stage. c. icteric stage. d. posticteric stage. 464 49. What is the likely effect of long-term exposure to a hepatotoxin? a. Full recovery to normal tissue after the toxic material has been removed b. Acute onset of vomiting, steatorrhea, and jaundice c. Continued mild inflammation of the liver without permanent damage d. Gradual irreversible damage to the liver and cirrhosis 465 50. What indicates the presence of third-stage alcohol hepatitis? a. Below normal blood levels of AST and ALT b. Upper left quadrant tenderness and dull pain c. A small, firm, nodular liver and portal hypertension d. Decreased production of blood clotting factors 466 51. A factor that may precipitate encephalopathy with cirrhosis is the elevated: a. serum urea. b. conjugated bilirubin. c. serum ammonia. d. serum pH. 466 52. In patients with cirrhosis, serum ammonia may increase when: a. ingesting excessive lipids. b. bleeding occurs in the digestive tract. c. an increase in unconjugated bilirubin occurs in the serum. d. less bile is produced. 466 53. What is the primary cause of esophageal varices? a. Increased hydrostatic pressure in the veins b. Alcohol irritating the mucosa c. Failure to inactivate estrogen d. Poor nutritional status 466-467 54. What is the primary cause of increased bleeding tendencies associated with cirrhosis? a. Anemia and leucopenia b. Jaundice and pruritus c. Recurrent infections d. Deficit of vitamin K and prothrombin 466 55. Which factors contribute to ascites in patients with cirrhosis? a. Increased aldosterone and deficit of albumin b. Severe anemia and increased serum bilirubin c. Hypokalemia and increased serum ammonia d. Hyperproteinemia and persistent hypotension 466 56. Which of the following is a major cause of primary hepatocellular cancer? a. Metastatic tumors b. Acute hepatitis c. Long-term exposure to certain chemicals d. Chronic cholelithiasis 469 57. What causes massive inflammation and necrosis in acute pancreatitis? a. Formation of multiple thrombi and ischemia b. Infection by intestinal microbes c. Immune complex reaction d. Autodigestion of tissue by pancreatic enzymes 470 58. How does chemical peritonitis and shock frequently result from acute pancreatitis? a. Inflammation and increased vascular permeability of the peritoneum affect fluid balance. b. Erosion in the intestinal wall causes release of bacteria. c. Fat necrosis and hypocalcemia develop. d. Secretions from the pancreas and intestine become more acidic. 470 59. Malnutrition may develop in children with celiac disease because of: a. damage to the intestinal villi. b. obstruction in the pancreatic ducts. c. acidosis, preventing activation of digestive enzymes. d. insufficient bile for absorption. 471 60. Which of the following best describes steatorrhea? a. A light gray-colored stool b. A tarry black stool c. Bulky, fatty, foul-smelling stools d. Watery stools with mucus and blood 439 61. What is the dietary requirement for a child with celiac disease? a. Low sodium, high fat b. High carbohydrate, low protein c. High calorie with vitamin supplements d. Gluten-free 441 62. What are the typical changes occurring with Crohn’s disease? a. Degeneration and flattening of the villi in the small intestine b. Multiple herniations of the mucosa through weak areas of the muscularis c. A continuous area of mucosal inflammation and ulceration in the rectum and colon d. Inflamed areas of the wall of the ileum alternating with thick fibrotic or normal areas 471-474 63. Stools that are more liquid and contain mucus and frank blood are typical of: a. diverticulitis. b. ulcerative colitis. c. Crohn’s disease. d. celiac disease. 474 64. How may a fistula form with Crohn’s disease? a. Lack of peristalsis, leading to dilated areas of intestine b. Fibrosis and thickening of the wall, causing obstruction c. Erosion of the mucosa, causing bleeding d. Recurrent inflammation, necrosis, and fibrosis, forming a connection between intestinal loops 473 65. How does iron deficiency anemia frequently develop with ulcerative colitis? a. Loss of surface area for absorption in the ileum b. Bone marrow depression by toxic wastes c. Chronic blood loss in stools d. Insufficient hydrochloric acid for iron absorption 474 66. What is the cause of inflammatory bowel disease? a. Physical and emotional stress b. An autoimmune reaction c. A combination of recessive genes d. Idiopathic 475 67. What pain is typical of diverticulitis? a. Lower left quadrant b. Lower right quadrant c. Sharp, colicky, periumbilical d. Lower abdominal pain, radiating into the groin 478 68. What usually initiates acute appendicitis? a. Infection in the appendix b. An episode of severe diarrhea c. Obstruction of the lumen of the appendix d. Eating a low-fiber diet 475 69. With acute appendicitis, localized pain and tenderness in the lower right quadrant results from: a. increased peristalsis in the adjacent colon. b. inflammation and stretching of the appendiceal wall. c. increased gas and fluid inside the appendix. d. local inflammation of the parietal peritoneum. 476 70. How does localized peritonitis develop from acute appendicitis before rupture? a. The omentum walls off the inflamed area. b. Intestinal bacteria escape through the necrotic appendiceal wall. c. The obstructing object inside the appendix causes edema. d. Bacteria escape into the circulating blood. 476 71. What is a typical early sign of cancer in the ascending colon? a. Change in shape of the stool b. Incomplete emptying c. Mild but persistent pain in the lower left quadrant d. Occult blood in the stool 480 72. To which site does colon cancer usually first metastasize? a. Lungs b. Stomach c. Liver d. Spleen 479 73. How does a volvulus cause localized gangrene in the intestine? a. Hypotension and shock cause ischemia. b. The mesenteric arteries are compressed in the twisted section of intestine. c. A section of intestine herniates between the muscles of the abdominal wall. d. The distention of the intestinal wall causes increased permeability of the tissue. 476 74. Which of the following is a typical indicator of an intestinal obstruction caused by paralytic ileus? 484 75. A congenital condition in which parasympathetic innervation is missing from a section of the colon, impairing motility is referred to as: 484 76. What causes hypovolemic shock to develop with intestinal obstruction? a. Continued vomiting and fluid shift into the intestine b. Hemorrhage into the intestine a. Excessive audible bowel sounds b. Intermittent colicky pain c. Severe steady abdominal pain d. Visible peristalsis a. diverticulitis. b. Crohn’s disease. c. irritable bowel syndrome. d. Hirschsprung’s disease. c. Rupture of the intestinal wall d. Repeated bouts of severe diarrhea 485 77. What causes the characteristic rigid abdomen found in the patient with peritonitis? a. Increased fluid and gas, causing abdominal distention b. Inflammation of the peritoneum and organs, causing a firm mass in the abdomen c. Inflamed peritoneum, resulting in reflex abdominal muscle spasm d. Voluntary contraction of the abdominal muscles as a protective mechanism 486 78. What would be the likely outcome from chemical peritonitis related to a perforated gallbladder? a. Leakage of intestinal bacteria into blood and the peritoneal cavity b. Massive hemorrhage and shock c. Breakdown of the gallstones d. Increasing peristalsis with intermittent painful spasms 485 79. How does pelvic inflammatory disease frequently lead to bacterial peritonitis? a. Chemical irritation by excessive ovarian and uterine secretions causes inflammation. b. Ulceration and perforation of the uterus allow the bacteria to spread. c. Infection spreads through the fallopian tubes directly into the peritoneal cavity. d. Gangrene in the uterine wall spreads through into the pelvic cavity. 484-485 80. Choose the significant change in arterial blood gases expected with prolonged severe vomiting: a. Increased bicarbonate ion, increased PCO2, serum pH 7.4 b. Decreased bicarbonate ion, decreased PCO2, serum pH 7.35 c. Increased bicarbonate ion, decreased PCO2, serum pH 7.35 d. Decreased bicarbonate ion, increased PCO2, serum pH 7.45 440 81. When dehydration reduces the compensation possible for acidosis resulting from prolonged diarrhea, what significant change in arterial blood gases indicates this? 438-439 82. Bile pigment gallstones are more common in individuals dealing with: a. obesity. b. high cholesterol levels. a. Serum pH would rise above 7.45. b. Serum bicarbonate levels would increase, and serum pH would remain in normal range. c. Serum bicarbonate levels would decrease, and serum pH would drop below 7.35. d. Serum PCO2 would rise, and serum pH would be around 7.4. c. alcoholic cirrhosis. d. use of oral contraceptives. 459 83. Dehydration limits compensation available for an acid-base imbalance resulting from prolonged vomiting and diarrhea because: 439-440 84. Which of the following is the most frequent location of peptic ulcers? a. Lower esophagus b. Antrum of the stomach c. Proximal duodenum d. Distal duodenum 453-454 85. In peptic ulcer disease, which of the following does NOT decrease the resistance of the mucosal barrier? a. hypovolemia limits renal function. b. increased respirations cannot remove more H+. c. increased ADH blocks secretion of H+. d. more sodium and potassium ions are retained. b. Excessive glucocorticoid intake c. Proteases and cytotoxins from H. pylori d. Decreased vagal stimulation 453-454 86. An individual with peptic ulcer disease exhibits hematemesis. What does this probably indicate? a. Perforation b. Obstruction c. Erosion of a large blood vessel d. Development of malignancy 455 87. What does the term melena mean? a. Blood in a dark-colored stool b. Occult blood in the stool c. Blood in the sputum d. Blood in vomitus 439 88. Which of the following is NOT a common predisposing factor to gastric carcinoma? b. Genetic factors c. Ingestion of foods preserved with nitrates d. Anti-inflammatory medications such as ASA 457 89. Which of the following frequently occurs 2 to 3 hours after meals in post-gastrectomy patients? a. Hypoglycemia b. Hypovolemia c. Abdominal cramps and distention d. Increased peristalsis and diarrhea 457 90. Which term refers to an inflammation usually related to infection of the bile ducts? a. Cholelithiasis b. Cholecystitis c. Cholangitis d. Choledocholithiasis 458 91. Which of the following is NOT usually present during the icteric stage of viral hepatitis? b. Elevated serum liver enzymes c. Esophageal varices d. Lighter-colored stools 464 92. Which of the following statement(s) about jaundice is/are true? 1. It is often the first manifestation of hepatitis. 2. Jaundice indicates permanent liver damage. 3. Individuals with hepatitis are always jaundiced. 4. Jaundice usually develops with hepatocellular carcinoma. a. 1 only b. 4 only c. 1, 3 d. 2, 4 460 | 464 93. Which type(s) of hepatitis increase(s) the risk of hepatocellular carcinoma? a. HBV b. HCV c. HBV and HCV d. Neither HBV nor HCV 461 | 464 94. Which of the following is/are related to post-hepatic jaundice? a. Pruritic skin and light-colored stools b. Dark-colored stools and urine c. Increased serum levels of unconjugated bilirubin d. Loss of all metabolic functions 464 95. Which of the following occurs with hepatitis B? a. The liver is inflamed and enlarged. b. Blood clotting delays are apparent at onset. c. Hepatocytes cannot regenerate when the virus is present. d. Infection is self-limiting. 462 | 464 96. Identify a major reason making it difficult to prevent the spread of hepatitis B. a. A vaccine is not available. b. The incubation period is too short to track contacts. c. Infection is often asymptomatic. d. Antibodies are not produced. 462 97. What is the initial pathological change in alcoholic liver disease? a. Formation of nodules with shrinkage of the liver b. Inflammation with necrosis c. Development of fibrous bands of tissue d. Accumulation of fat in hepatocytes with hepatomegaly 465 98. How does serum bilirubin change with cirrhosis? a. Increased unconjugated bilirubin b. Increased conjugated bilirubin c. Increased conjugated and unconjugated bilirubin d. Decreased conjugated and unconjugated bilirubin 466 99. Which type of hepatitis virus requires the presence of hepatitis B virus so as to replicate? a. HAV b. HCV c. HDV d. HEV 464 100. At what stage of alcoholic liver disease can the damage be reversed? a. It can never be reversed b. Initial stage c. Alcoholic hepatitis stage d. End-stage cirrhosis 465 101. Although many factors may precipitate pancreatitis, the two major causes are: a. obesity and smoking. b. high-fat diet and hypertension. c. congenital defects and drug abuse. d. gallstones and alcohol abuse. 470 102. Which factor(s) appear(s) to have a role in the etiology of inflammatory bowel diseases? a. Dietary factors b. Environmental toxins c. Genetic and immunological factors d. Chronic alcoholism 471-472 103. Gastroesophageal reflux disease involves: a. periodic flow of gastric contents into the esophagus. b. constant flow of intestinal and gastric contents into the esophagus. c. spasmodic and violent vomiting of gastric contents. d. violent spasming of the esophagus, causing choking. 451 104. When a portion of the proximal stomach and the paraesophageal junction move above the diaphragm, this is called a: 450-451 105. Which of the following applies to gastric cancer? a. It usually appears as polyp or protruding mass. b. Most cases involve an adenocarcinoma of the mucous glands. c. Genetics or geographical area does not affect the incidence. d. It is usually diagnosed in an early stage because of pyloric obstruction. 456 a. dysphagia. b. rolling hernia. c. sliding hernia. d. pyloric stenosis. 106. Pancreatic cancer may be diagnosed early if obstruction of bile or pancreatic secretions develops when the tumor is located: 471 107. “A gluten-free diet as required” for the client with celiac disease means avoiding: a. products containing lactose. b. any trans-fat. c. certain grains. d. proteins containing certain amino acids. 471 108. The telescoping of one section of bowel inside another section is called: a. volvulus. b. hernia. c. adhesion. d. intussusceptions. 482 | 484 a. at the head of the pancreas. b. in the body of the pancreas. c. in the tail of the pancreas. d. in the endocrine glands of the pancreas. 109. A viral infection of the parotid gland is commonly known as: a. tonsillitis. b. mumps. c. chickenpox. d. scarlet fever. 448 Chapter 18: Urinary System Disorders Chapter 18: Urinary System Disorders Test Bank MULTIPLE CHOICE 1. Which of the following structures is most likely to be located in the renal medulla? a. Proximal convoluted tubule b. Glomerulus c. Loop of Henle d. Afferent arteriole 492-493 2. Which of the following is NOT a function of the kidney? a. Regulation of body fluid concentrations b. Removal of nitrogenous and acidic wastes c. Activation of vitamin D d. Production of albumin 491 3. Which of the following describes the correct flow of blood in the kidney? a. Afferent arteriole to the peritubular capillaries to the venule b. Efferent arteriole to the glomerular capillaries to the peritubular capillaries c. Peritubular capillaries to the glomerular capillaries to the venule d. Afferent arteriole to the glomerular capillaries to the efferent arteriole 494 4. Which of the following describes the flow of filtrate in the kidney? a. The collecting duct to the distal convoluted tubule to the renal pelvis b. Bowman’s capsule to the proximal convoluted tubule to the loop of Henle c. The loop of Henle to the collecting duct to Bowman’s capsule d. The distal convoluted tubule to the loop of Henle to the collecting duct 492 5. Which of the following describes the normal flow of urine? a. Collecting duct to the renal pelvis to the ureter to the bladder b. Renal pelvis to the urethra to the bladder to the ureter c. Ureter to the renal pelvis to the urethra to the bladder d. Collecting duct to the ureter to the urethra 496 6. Which statement about the bladder is TRUE? a. The bladder wall lacks rugae. b. Three openings from the urinary bladder form the trigone. c. It contracts when stimulated by the sympathetic nervous system. d. Continuous peristalsis in the bladder wall promotes urine flow. 496 7. Which of the following increases glomerular filtration rate? a. Increased plasma osmotic pressure b. Dilation of the efferent arteriole c. Increased hydrostatic pressure in the glomerular capillaries d. Constriction of the afferent arteriole 495 8. By what process is water reabsorbed from the filtrate? a. Osmosis b. Active transport c. Cotransport d. Capillary action 492 9. Which substance directly controls the reabsorption of water from the collecting ducts? a. Renin b. Aldosterone c. Angiotensin d. Antidiuretic hormone 492 10. Under what circumstances do cells in the kidneys secrete renin? a. The urine pH decreases. b. Blood flow in the afferent arteriole decreases. c. Serum potassium levels are high. d. Serum osmotic pressure increases. 495 11. Which of the following should be present in the filtrate in the proximal convoluted tubule? a. Plasma proteins b. Erythrocytes c. Sodium ions d. Leukocytes 492 12. From the following, choose the substance likely to appear in the urine when the glomerulus is inflamed. 497 13. Involuntary urination by a child after age 4 or 5, when bladder control is expected, is referred to as: 496 14. When a respiratory infection with high fever is present in the body, how would the kidney tubules maintain normal pH of body fluids? a. Albumin b. Urea c. Sodium d. Creatinine a. enuresis. b. stress incontinence. c. micturition. d. overflow incontinence. b. Secrete more acids and reabsorb more bicarbonate ions. c. Excrete a larger volume of more dilute urine. d. Retain more potassium ions in exchange for sodium ions. 502-503 15. When comparing normal kidney function with dialysis, which of the following mechanisms is not possible in dialysis? 500 16. What is the cause of most cases of pyelonephritis? a. An ascending infection by E. coli b. Abnormal immune response, causing inflammation c. Dialysis or other invasive procedure d. Severe pH imbalance of urine 500 17. Which disease is manifested by dysuria and pyuria? a. Diffusion b. Osmosis c. Ultrafiltration d. Active transport b. Cystitis c. Glomerulonephritis d. Urolithiasis 502 18. Why may acute pyelonephritis and cystitis follow untreated prostatitis? a. Microbes spread through the circulation. b. Antibodies have not yet formed. c. There is no effective treatment. d. There is a continuous mucosa along the involved structures. 502 19. Pyelonephritis may be distinguished from cystitis by the presence in pyelonephritis of: a. microbes, leukocytes, and pus in the urine. b. painful micturition. c. urgency and frequency. d. urinary casts and flank pain. 502 20. In a case of acute pyelonephritis, what is the cause of flank pain? b. Inflammation, stretching the renal capsule c. Increasing glomerular permeability, creating an increased volume of filtrate in the kidney d. Microbes irritating the tissues 502 21. Which pathophysiological process applies to acute post-streptococcal glomerulonephritis? a. Streptococcal infection affects both the glomerular and tubule functions b. Ischemic damage occurs in the tubules, causing obstruction and decreased glomerular filtration rate (GF c. Immune complexes deposit in glomerular tissue, causing inflammation d. Increased glomerular permeability for unknown reasons 502-503 22. What causes the dark urine associated with acute post-streptococcal glomerulonephritis? a. Blood and protein leaking through the capillary into the filtrate b. Proteinuria and microscopic hematuria from the inflammation c. Pyuria from inflammatory exudate d. Bleeding from ulcerations in the kidneys 503 23. Renal disease frequently causes hypertension because: b. congestion and ischemia stimulate release of renin. c. antidiuretic hormone (ADH) secretion is decreased. d. damaged tubules absorb large amounts of filtrate. 503 24. Urinary casts are present with acute post-streptococcal glomerulonephritis because: a. large numbers of microbes and leukocytes enter the filtrate. b. ruptured capillaries release debris into the tubules. c. normal reabsorption of cells and proteins cannot take place. d. inflamed tubules compress red blood cells (RBCs) and protein into a typical mass. 508 25. Which disease would cause an increased ASO titer and elevated serum ASK? a. Nephrotic syndrome b. Acute post-streptococcal glomerulonephritis c. Pyelonephritis d. Polycystic kidney 503-504 26. Why does metabolic acidosis develop with bilateral kidney disease? b. GFR is increased. c. Serum urea is increased. d. More bicarbonate ion is produced. 510 27. What is the first indicator in the arterial blood gases of acidosis caused by glomerulonephritis? a. Increased carbonic acid b. Increased bicarbonate ion c. A pH less than 7.35 d. Decreased bicarbonate ion 503 28. What would be the long-term effects of chronic infection or inflammation of the kidneys? a. Dehydration and hypovolemia b. Gradual necrosis, fibrosis, and development of uremia c. Sudden anuria and azotemia d. Severe back or flank pain 504 29. What factors contribute to headache, anorexia, and lethargy with kidney disease? 1. Increased blood pressure 2. Elevated serum urea 3. Anemia 4. Acidosis a. 1 only b. 2, 4 c. 1, 3, 4 d. 1, 2, 3, 4 513 30. What are the significant signs of nephrotic syndrome? a. Hyperlipidemia and lipiduria b. Pyuria and leucopenia c. Hypertension and heart failure d. Gross hematuria and pyuria 504 31. Why does blood pressure often remain near normal in patients with nephrotic syndrome? a. Massive amounts of fluid are lost from the body with polyuria. b. Renin and aldosterone are no longer secreted. c. Tubules do not respond to ADH and aldosterone. d. Hypovolemia results from fluid shift to the interstitial compartment. 504 32. Common causes of urolithiasis include all of the following EXCEPT: a. hypercalcemia. b. hyperlipidemia. c. inadequate fluid intake. d. hyperuricemia. 506 33. Which of the following results from obstruction of the left ureter by a renal calculus? a. Mild flank pain on the affected side b. Hydronephrosis in both kidneys c. Immediate cessation of urine production d. An attack of renal colic 506 34. What does hydronephrosis lead to? a. Ischemia and necrosis in the compressed area b. Multiple hemorrhages in the kidney c. Severe colicky pain radiating into the groin d. Increased GFR 507 35. Which of the following is a predisposing factor to bladder cancer? a. Prostatic cancer b. Hormonal abnormalities c. Exposure to chemicals and cigarette smoke d. Presence of embryonic tissue 508 36. What is the common initial sign of adenocarcinoma of the kidney? a. Gross hematuria b. Microscopic hematuria c. Sharp flank pain d. Oliguria 507 37. Which of the following does NOT usually result from nephrosclerosis? a. Secondary hypertension b. Chronic renal failure c. Acute renal failure d. Increased renin and aldosterone secretions 508 38. Which of the following relates to polycystic kidney disease? a. It affects only one of the kidneys. b. It results in gradual degeneration and chronic renal failure. c. The kidneys are displaced and the ureters are twisted. d. The prognosis is good because there is adequate reserve for normal life. 510 39. Which of the following is related to Wilms’ tumor? a. Direct exposure to carcinogens b. Hormonal imbalance c. Repeated infections d. A genetic defect 509 40. With severe kidney disease, either hypokalemia or hyperkalemia may occur and cause: a. cardiac arrhythmias. b. encephalopathy. c. hypervolemia. d. skeletal muscle twitch or spasm. 513 41. Which of the following indicates the early stage of acute renal failure? a. Polyuria with urine of fixed and low specific gravity b. Hypotension and increased urine output c. Development of decompensated acidosis d. Very low GFR and increased serum urea 510 42. What is/are a cause(s) of acute tubule necrosis and acute renal failure? a. Prolonged circulatory shock b. Sudden significant exposure to nephrotoxins c. Crush injuries or burns d. All of the above 510 43. Which of the following would likely cause chronic renal failure? a. Cystitis with pyelonephritis in the right kidney b. Circulatory shock c. Diabetes d. Obstruction of a ureter by a renal calculus 510 44. What causes polyuria during the stage of renal insufficiency? a. Loss of tubule function b. Increased blood pressure c. Decreased aldosterone secretion d. Increased GFR 510 45. What is the primary reason for hypocalcemia developing during end-stage renal failure or uremia? 513 46. Cystitis is more common in females because: a. the mucosa in the urinary tract is continuous. b. the urethra is short, wide, and adjacent to areas with resident flora. c. the pH of urine is more acidic in females. d. females have a higher incidence of congenital anomalies. 500 47. Which of the following indicate a decreased GFR? a. Decreased parathyroid hormone secretion b. Insufficient calcium in the diet c. Excessive excretion of calcium ions in the urine d. A deficit of activated vitamin D and hyperphosphatemia a. Increased serum urea and decreased serum bicarbonate b. Urine with low specific gravity and dark color c. Albuminuria and hematuria d. Hyponatremia and hypokalemia 497 48. Which of the following is NOT likely to lead to hydronephrosis? a. Renal calculi b. Pyelonephritis c. Nephrosclerosis d. Benign prostatic hypertrophy ANS:CREF:502 | 506 | 507 | 515 49. Which of the following congenital defects is a common cause of cystitis in young children? a. Polycystic kidney b. Horseshoe kidney c. Hypoplasia of the kidney d. Vesicoureteral reflux 500 50. Which factor contributes to severe anemia in individuals with chronic renal failure? a. Increased erythropoietin secretion b. Limited protein intake c. Compensatory increase in bone marrow activity d. Inability to absorb vitamin B12 and iron 513 51. When acidosis becomes decompensated in renal failure, a key indicator is: a. increased PCO2. b. increased bicarbonate ion. c. serum pH dropping below 7.35. d. serum buffer ratio of 20 bicarbonate ions to 1 carbonic acid. 513 52. What is the primary action of the diuretic furosemide? a. Decreased reabsorption of sodium and water b. Decreased reabsorption of H+ in the tubules c. Increased secretion of antidiuretic hormone d. Inhibition of renin 498 53. Which of the following causes acute renal failure? a. Polycystic kidney disease b. Pyelonephritis in the right kidney c. Nephrosclerosis d. Bilateral acute glomerulonephritis 510 54. Which of the following is a significant indicator of renal insufficiency? a. Urine with pH of 5 b. Increased serum urea and creatinine c. Urine with high specific gravity d. Decreased blood pressure 510 55. Uremic signs of renal failure include all of the following EXCEPT: a. encephalopathy. b. high blood pressure. c. osteodystrophy. d. azotemia and acidosis. 513 56. Choose the basic cause of osteodystrophy associated with chronic renal failure. a. Development of hypercalcemia b. Deficit of parathyroid hormone c. Failure of the kidney to activate vitamin D d. Excessive loss of phosphate ion 513 57. Agenesis is often not diagnosed because: a. the kidney is displaced from its normal position. b. it is a genetic defect and asymptomatic until mid-life. c. the two functioning kidneys are fused together. d. it is usually asymptomatic as one kidney provides adequate function. 509 58. The normal pH of urine is: a. 7.35-7.45. b. 4.5- 8.0. c. 1.5-7.5. d. 1.0-7.0. 596-597 59. Wilms’ tumor is: a. a malignant tumor in the bladder. b. an encapsulated mass in one kidney. c. not considered to have a genetic origin. d. manifested in adulthood. 509 60. Reduced urine output resulting from inflammation and necrosis of the tubules is called: a. oliguria. b. anuria. c. pyuria. d. polyuria. 510 61. The micturition reflex is initiated by: a. sympathetic nerves in the sacral spinal cord. b. relaxation of the internal sphincter of the bladder. c. increased pressure distending the bladder. d. contraction of the bladder. 496 62. Which of the following results from decreased blood flow into the kidneys? a. Decreasing blood pressure b. Dilation of the afferent arterioles c. Decreased aldosterone secretion d. Increased angiotensin and systemic vasoconstriction 496 63. In acute post-streptococcal glomerulonephritis, the glomerular inflammation results from: a. toxins produced by the bacteria. b. a type III hypersensitivity reaction. c. an ascending infection from the bladder. d. spread of infection from the tubules. 502 64. In acute post-streptococcal glomerulonephritis, the inflammation causes: a. increased permeability of the glomerular capillaries. b. glomerular congestion and decreased GFR. c. decreased blood pressure and edema. d. A and B 503 65. Circulatory shock causes: a. decreased GFR and increased renin secretion. b. increased ADH and decreased aldosterone secretion. c. immediate tubule necrosis and obstruction. d. sympathetic nervous system (SNS) stimulation and vasodilation of afferent and efferent arterioles. 510 66. Autoregulation in the kidneys refers to: a. control of blood flow by the SNS. b. the secretion of renin and activation of angiotensin. c. local minor reflex adjustments in the arterioles to maintain normal blood flow. d. the control of systemic blood pressure by the kidneys. 495 67. The reabsorption of water and electrolytes by the kidneys is directly controlled by: 1. atrial natriuretic hormone. 2. antidiuretic hormone. 3. angiotensin. 4. the levels of bicarbonate ion. a. 2 only b. 3 only c. 1, 2 d. 2, 4 492 68. Uncontrolled essential hypertension may cause chronic renal failure because of: a. predisposition to recurrent urinary tract infections. b. damage to afferent arterioles and renal ischemia. c. failure of tubules to respond to hormonal controls. d. glomerular congestion causes damaged capillaries. 508 69. Urine with a low specific gravity is usually related to: a. an infection of the gallbladder. b. renal failure due to tubule damage. c. lack of sufficient fluid intake. d. presence of numerous renal calculi. 510 | 512 70. Excess urea and other nitrogen wastes in the blood is referred to as: a. dysuria. b. azotemia. c. bacteremia. d. hematuria. 513 Chapter 19: Reproductive System Disorders Chapter 19: Reproductive System Disorders Test Bank MULTIPLE CHOICE 1. Which statement about the testes is TRUE? a. Each testis contains the ductus deferens. b. The testes are suspended by the spermatic cord. c. Each testis has its own scrotal sac and seminal vesicle. d. The testes must be kept at a temperature slightly above body temperature. 517 2. Which statement about spermatogenesis is TRUE? a. The complete process takes about 28 days. b. Maturation of sperm takes place in the seminal vesicles. c. It is controlled by follicle-stimulating hormone (FSH) and testosterone. d. The process is initiated after each ejaculation. 518 3. Which of the following may result from cryptorchidism? a. Infertility b. Testicular cancer c. Both A and B d. Neither A nor B 519 4. Which term refers to excessive fluid collecting between the layers of the tunica vaginalis? a. Varicocele b. Hypospadias c. Spermatocele d. Hydrocele 519 5. Which of the following are common early significant signs of acute prostatitis? a. A hard nodule in the gland and pelvic pain b. Soft, tender, enlarged gland and dysuria c. Hesitancy and increased urinary output d. Mild fever, vomiting, and leucopenia 520 6. Which of the following applies to benign prostatic hypertrophy? a. The tumor usually becomes malignant in time. b. The gland becomes small, nodular, and firm. c. Manifestations include hesitancy, dribbling, and frequency. d. Lower abdominal or pelvic pain develops. 521 7. Why does frequent need for urination occur with benign prostatic hypertrophy? a. Increased volume of dilute urine b. Irritation of the bladder and urethra c. Impaired micturition reflex d. Incomplete emptying of the bladder 521 8. Which of the following is the common first site for metastasis from prostatic cancer? a. Bone b. Lungs c. Liver d. Testes 522 9. What is a useful serum marker during treatment for prostatic cancer? a. Human chorionic gonadotropin b. Alpha-fetoprotein c. Prostate-specific antigen d. Luteinizing hormone 522 10. Which of the following is NOT a characteristic of leukorrhea during the reproductive years? a. It is clear or whitish. b. It has a pH of 4 to 5. c. It does not contain any cells. d. It contains mucus. 524 11. Which of the following applies to the corpus luteum? a. It forms a mature ovarian follicle. b. It secretes human chorionic gonadotropin (hCG). c. It secretes estrogen and progesterone during the latter half of the menstrual cycle. d. It produces gonadotropins for the next cycle. 527 12. Why does severe pain occur with each menstrual cycle in endometriosis? a. Obstruction in the fallopian tubes b. Inflammation due to blood irritating the endometrial tissue c. Hormonal imbalance causing uterine contractions d. Fibrous tissue responding to hormonal changes 529 13. With pelvic inflammatory disease, why does infection spread easily into the peritoneal cavity? a. The fallopian tubes are obstructed, and purulent exudate cannot drain into the uterus. b. The uterus is perforated because of infection, allowing bacteria to leak out. c. Most of the primary infections do not respond to antimicrobial drugs. d. Microbes are highly virulent. 531 14. Which of the following is a common complication of leiomyomas? a. Development of malignancy b. Irregular menstrual cycles c. Interference with ovulation d. Abnormal bleeding such as menorrhagia 533 15. Which of the following refers to fibrocystic breast disease? a. Progressive development of fluid-filled cysts and fibrous tissue b. Proliferation of atypical cells with high risk of malignancy c. Benign tumors that develop after menopause d. Any tissue changes other than the normal response to hormonal changes 534-535 16. Which of the following applies to carcinoma of the breast? a. It presents as a tender, painful, firm nodule. b. Tumor cells may demonstrate estrogen receptors on the membrane. c. Occasionally, a genetic factor may have a small role in tumor development. d. The tumor is invasive but does not metastasize until very late. 535 17. Which is considered to be the stage of carcinoma in situ in cervical cancer? a. The invasive stage b. The stage of mild dysplasia c. The time before it can be detected by a Pap test d. Noninvasive severe dysplasia 537 18. What is a major predisposing factor to cervical cancer? a. High estrogen levels b. Familial incidence c. Infection with herpes simplex virus (HSV) d. Early age for onset of menstrual cycles 538 19. What is a significant early sign of endometrial carcinoma? a. A positive Pap test b. Minor vaginal bleeding or spotting c. Infection resistant to treatment d. Painful intercourse 539 20. Which sexually transmitted infection(s) is/are usually considered asymptomatic in women? a. Chlamydia b. Gonorrhea c. Syphilis d. All of the above 541 21. Which of the following frequently causes pelvic inflammatory disease (PID) and subsequent infertility? a. Chlamydia b. Genital warts c. Trichomoniasis d. Herpes simplex 531 22. Which of the following causes inflammation of the vagina with a copious yellow discharge and foul odor? 545 23. What is the cause of syphilis? a. A gram-negative diplococcus b. An anaerobic protozoa c. A virus d. An anaerobic spirochete 542 a. Candidiasis b. Trichomoniasis c. Syphilis d. Gonorrhea 24. Which of the following infections may be transmitted from the mother to the fetus during delivery? 542 | 544 25. Which of the following STDs is considered to be a systemic infection? a. Gonorrhea b. Chlamydia c. Syphilis d. Condylomata acuminate 542 26. Which of the following is the most common cause of acute bacterial prostatitis? a. N. gonorrhoeae b. Pseudomonas aeruginosa c. S. aureus d. E. coli 520 a. Gonorrhea b. Chlamydia c. Herpes simplex d. All of the above 27. The most common solid tumor found in young men is: a. prostatic cancer. b. testicular cancer. c. bladder cancer. d. penile cancer. 523 28. A hard nodule in the peripheral area of the prostate gland is typical of: a. prostatic cancer. b. benign prostatic hypertrophy. c. acute prostatitis. d. chronic prostatitis. 522 29. How do testicular tumors usually present? a. Soft, tender mass b. Multiple firm nodules c. Hard, painless unilateral mass d. Small, fluid-filled cyst 523 30. Which term refers to bleeding between menstrual periods? a. Amenorrhea b. Dysmenorrhea c. Oligomenorrhea d. Metrorrhagia 529 31. Which statement does NOT apply to vaginal candidiasis? a. It is classified as an STD. b. The cause is an opportunistic yeast. c. It causes dysuria and dyspareunia. d. The mucosa becomes red and pruritic. 531 32. Testicular cancer usually spreads first to the: a. lungs. b. bone. c. pelvic lymph nodes. d. brain. 523 33. When the uterus is located in the vagina with the cervix at the opening to the vagina, this is called: a. first-degree prolapse. b. second-degree prolapse. c. third-degree prolapse. d. procidentia. 529 34. Painful menstruation is called: a. polymenorrhea. b. premenstrual syndrome. c. dysmenorrhea. d. endometriosis. 529 35. Vaginal candidiasis is frequently predisposed by: a. systemic antibacterial therapy. b. insertion of an intrauterine device. c. sexual intercourse with an infected partner. d. previous viral infection. 531 36. A chancre is best described as: a. a vesicle surrounded by a red inflamed area. b. a pustule filled with purulent exudate. c. an area of necrosis and fibrosis. d. a firm painless ulcerated nodule. 542 37. Adjuvant chemotherapy and radiation may be used in cases of breast cancer in order to: a. slow the growth of the primary tumor. b. destroy any micrometastases. c. prevent the removal of any lymph nodes. d. reduce the need for a mastectomy. 536 38. Ovarian cancer has a poor prognosis because: a. it does not respond to chemotherapy or radiation. b. vague signs and hidden location lead to late diagnosis. c. premenopausal women are not likely to notice changes. d. hormone therapy is ineffective. 539-540 39. Specific genetic links have been shown for: 1. cervical cancer. 2. testicular cancer. 3. breast cancer. 4. prostatic cancer. a. 1, 2 b. 3, 4 c. 1, 3, 4 d. 2, 3, 4 ANS REF:522-523 | 535 40. In which cancers has there been a recent significant increase in incidence? a. Uterine cancer b. Breast cancer c. Ovarian cancer d. Cervical cancer in situ 546 41. Adenocarcinomas make up the most common cancers found in the: a. prostate. b. testes. c. ovary. d. cervix. 522 42. Infertility in women may result from: a. endometriosis. b. hormonal imbalances. c. A and B d. Neither A nor B 520 | 540 43. Viable sperm may not be able to access an ovum when: a. cervical mucus is highly viscous. b. vaginal pH is abnormal. c. structural abnormalities are present. d. A, B, and C 540 44. Balanitis is the infection and inflammation of the: a. vagina. b. glans penis. c. fallopian tubes. d. testes. 520 45. Structural abnormalities of the uterus may lead to dyspareunia, which is: a. painful intercourse. b. obstructed urination. c. a form of infertility. d. fungal infection of the uterus. 530 Chapter 20: Neoplasms and Cancer Chapter 20: Neoplasms and Cancer Test Bank MULTIPLE CHOICE 1. What is a benign neoplasm originating from adipose tissue called? a. Adenoma b. Lipoma c. Fibrosarcoma d. Adenocarcinoma 550 2. What are malignant neoplasms arising from connective tissue cells called? a. Carcinomas b. Sarcomas c. Melanomas d. Fibromas 550 3. Which of the following is a characteristic of a benign tumor? a. It is unencapsulated and invasive. b. It consists of undifferentiated cells. c. It exerts systemic effects. d. Cells appear relatively normal. 550 4. Which factor provides the basis for the grading of newly diagnosed malignant tumors? a. Size of the tumor b. Number of metastases c. Degree of differentiation of the cells d. Number of lymph nodes involved 551 5. A warning sign of possible cancer would be any of the following EXCEPT: a. persistent, unusual bleeding. b. a change in bowel habits. c. sudden development of fever, nausea, and diarrhea. d. a change in shape, color, or surface of a skin lesion. 552 6. The common local effects of an expanding tumor mass include: 1. obstruction of a tube or duct. 2. anemia and weight loss. 3. cell necrosis and ulceration. 4. tumor markers in the circulation. a. 1, 2 b. 1, 3 c. 2, 4 d. 3, 4 552 7. Which of the following does paraneoplastic syndrome refer to? a. The effects of substances such as hormones secreted by the tumor cells b. Severe weight loss and cachexia associated with advanced cancer c. The decreased resistance to infection resulting from malignant tumors d. The effects of multiple metastatic tumors 553 8. Which term refers to the spread of malignant cells through blood and lymph to distant sites? a. Invasiveness b. Seeding c. Metastasis d. Systemic effect 554 9. One reason for staging a malignant tumor at the time of diagnosis is to: a. identify the original cell from which the tumor developed. b. locate and identify the primary tumor. c. decide the initiating factor for a particular tumor. d. determine the best treatment and prognosis. 556 10. The process of carcinogenesis usually begins with: a. exposure to promoters causing dysplasia. b. development of defective genes. c. an irreversible change in the cell DNA. d. a single exposure to a known risk factor causing temporary cell damage. 557 11. What would be an external source of ionizing radiation? a. A needle containing a radioisotope implanted beside the tumor b. Gamma rays delivered by a cobalt machine c. A dose of a radioactive drug to be ingested d. A fluid containing radioactive material instilled in a body cavity 560 12. Radiation therapy destroys: a. all cells in the tumor at one time. b. the cells in the center of the tumor. c. primarily rapidly dividing cells. d. radioresistant cells. 560 13. The most critical adverse effects of chemotherapy and radiation therapy are: a. thrombocytopenia and leucopenia. b. headache and lethargy. c. nausea and constipation. d. alopecia and weight loss. 567 14. Chemotherapy usually involves a combination of drugs in order to: 1. reduce the adverse effects. 2. guarantee that all cancer cells are destroyed. 3. be effective in more phases of the cell cycle. 4. totally block the mitotic stage. a. 1, 3 b. 1, 4 c. 2, 3 d. 3, 4 561 15. Why does ovarian cancer have a poor prognosis? a. The ovaries are inaccessible for examination. b. Specific signs rarely appear until after secondary tumors have developed. c. The same tumor markers are present with many types of cancer. d. No effective treatment is available. 565 16. Select the correct pair representing a malignant tumor and its marker: a. colon cancer: carcinoembryonic antigen (CEA) b. hepatic cancer: CA125, AFP c. prostate cancer: human chorionic gonadotropin (hCG) d. testicular cancer: Philadelphia chromosome 553 17. Antiangiogenesis drugs act on a malignant tumor by: a. promoting the immune response and removal of abnormal tumor cells. b. blocking hormonal stimulation of tumor cells. c. reducing blood flow and nutrient supply to tumor cells. d. transporting radioisotopes into the tumor. 563 18. The development of neutropenia during chemotherapy for cancer means: a. the cancer cells are being destroyed quickly. b. the patient is likely to hemorrhage. c. higher doses of chemotherapy could be tolerated by this patient. d. the patient is at high risk for infection. 562 19. Malignant brain tumors: a. metastasize quickly to all parts of the body. b. spread first to lungs and bone. c. spread to other parts of CNS. d. do not metastasize anywhere at any time. 565-566 20. Identify the common dose-limiting factor for chemotherapy: a. Alopecia b. Bone marrow depression c. Nausea and vomiting d. Weight loss 562 21. Glucocorticoids are often prescribed during a course of chemotherapy and radiation because: a. glucocorticoids greatly potentiate the effect of chemotherapy. b. the immune system is stimulated. c. skeletal muscle atrophy will be decreased. d. inflammation around the tumor may be reduced. 563 22. Vomiting frequently follows a chemotherapy treatment because: a. the gastrointestinal tract is irritated. b. the chemicals stimulate the emetic center. c. the drugs have an unpleasant odor. d. A and B 562 23. What type of normal cells are often damaged during chemotherapy and radiation treatments? a. Epithelial cells b. Skeletal muscle cells c. Nerve tissue d. Collagen and fibrous tissue 561 24. Remission for cancer is generally defined as a period in which: a. chemotherapy cannot be used. b. signs and symptoms are absent. c. complications are evident. d. metastases occur. 564 25. All of the following are correct statements about skin cancers EXCEPT: a. They are difficult to diagnose and treat. b. They usually develop slowly on the head, neck, or back of individuals with fair skin. c. The number of skin cancer cases is increasing. d. Basal cell carcinoma is the most common form of skin cancer. 564 26. High risk factors for cancer include: 1. human papilloma virus. 2. chronic irritation and inflammation. 3. repeated sun exposure. 4. high family incidence. a. 1, 3 b. 3, 4 c. 1, 2, 4 d. 1, 2, 3, 4 556 | 557 27. The term apoptosis refers to: a. programmed cell death. b. abnormal or immature cells. c. degree of differentiation of cells. d. the development of new capillaries in a tumor. 549 28. The warning signs for cancer include: a. unusual bleeding. b. change in a wart or mole (e.g., color). c. a new solid lump, often painless. d. All the above 552 29. A classification process that applies to a specific malignant tumor and describes the extent of the disease at a given time is called: 556 30. Benign tumors can often be differentiated from malignant tumors because benign tumors: a. often have systemic effects. b. contain cells showing increased mitosis and atypical rapid growth. c. are encapsulated and slow-growing. a. seeding. b. mutation. c. staging. d. grading. d. can metastasize or invade nearby tissue. 550 31. Benign tumors in the brain are often life-threatening because they: a. metastasize early in their development. b. create excessive pressure within the skull. c. cannot be removed. d. cause serious systemic effects. 565 32. Drugs or agents that augment the natural immune response in the body to improve identification and removal of abnormal cells are called: 563 33. The method that can be used as an alternative to surgical removal of a tumor by using heat generated by a needle inserted into the tumor is referred to as: a. biological response modifiers. b. angiogenesis stimulators. c. analgesic complements. d. targeted receptor modifiers. a. radiation therapy. b. thermolysis intervention. c. brachytherapy. d. radiofrequency ablation. 559 34. Staging systems used to classify a malignant tumor at the time of diagnosis are based on which of the following factors? 556 35. One of the general effects of a malignant cancer is cachexia, which is: a. severe bleeding. b. severe tissue wasting. c. severe fatigue. d. multiple opportunistic infections. 552 Chapter 21: Congenital and Genetic Disorders Chapter 21: Congenital and Genetic Disorders a. Size of the tumor, involvement of lymph nodes, metastases b. Location of tumor, size, type of cellular abnormality c. Size, encapsulated or non-encapsulated, invasion into neighboring tissue d. Type of cellular abnormality, size of secondary tumors, location/tissue affected Test Bank MULTIPLE CHOICE 1. Which of the following statements applies to the sex chromosomes? a. They are identified as XY in the female. b. They are numbered pair 23 in the karyotype. c. They contain the same genes as in the other pairs of chromosomes. d. They are found only in the cells in the gonads (the ovaries and the testes). 569 2. What is the term for an arrangement of the chromosomes from an individual’s cell, organized in pairs based on size and shape? 569 3. What is characteristic of a congenital disorder? a. Genes are not involved. b. It is strictly a developmental anomaly. c. A cause is known. d. It is usually manifested in the neonatal period. a. Pedigree b. Punnett squares c. Karyotype d. Genotype 573 4. What is the probability of two parents, both carriers of a defective recessive gene, producing a homozygous child (with each pregnancy)? 575 5. In the case of an X-linked recessive disorder, a carrier mother and unaffected father could produce a/an: 575 6. Down syndrome is an example of a/an: a. autosomal dominant disorder. b. multifactorial disorder. c. developmental defect. d. chromosomal disorder. 576 a. 0% b. 25% c. 50% d. 75% a. normal female. b. affected female. c. male carrier. 7. Agents that cause damage during embryonic or fetal development are called: a. teratogenic. b. mutagenic. c. multifactorial agents. d. polygenic agents. 574 8. What is an example of a multifactorial congenital disorder? a. Type AB blood b. Down syndrome c. Color blindness d. Cleft lip and palate 572 9. Ultrasonography during pregnancy would be helpful in detecting fetal: a. enzyme deficits. b. structural anomalies. c. chromosomal defects. d. hormonal abnormalities. 578 10. Which of the following statements regarding Down syndrome is TRUE? a. The typical physical characteristics are present at birth. b. All children with Down syndrome have the same organ defects and medical problems. c. The extent of cognitive impairment can be assessed at birth. d. The birth of a child with Down syndrome is only a risk to mothers over age 35. 580 11. Which of the following statements applies to Huntington’s disease? a. The effects are obvious at birth. b. There is a test for the defective gene. c. There is a 50% probability that the child of an affected parent will be a carrier. d. The child must inherit the defective gene from both parents in order to be affected. 575 12. A mother is a carrier of Duchenne muscular dystrophy; the father is unaffected. They have one son with muscular dystrophy. Another male child is expected. The probability of the second son having muscular dystrophy is: 574-575 a. 100% b. 50% c. 25% d. 0% 13. Hemophilia A has been diagnosed in a young boy. He has inherited this defective gene from: a. his father. b. his mother. c. both parents. 575 14. A father affected with hemophilia A, whose wife is unaffected, will pass on the defective gene to: a. all of his sons, who will be affected. b. 50% of his sons, who will be affected. c. all of his daughters, who will be carriers. d. 50% of his daughters, who will be carriers. 575 15. Which of the following are common manifestations of Down syndrome? 1. Congenital heart defect 2. Cleft lip and palate 3. Large protruding tongue 4. Limited intellectual development a. 1, 2 b. 1, 3 c. 2, 4 d. 1, 3, 4 580 16. A spontaneous alteration in genetic material that may result from exposure to harmful substances is termed: 570 17. A person with sickle cell trait that is heterozygous has: a. an incomplete dominant gene. b. a multifactorial condition. c. co-dominant genes. d. X-linked dominant trait. 575 18. TORCH is an acronym for routine prenatal screening tests for high-risk maternal infections; TORCH stands for: a. autosome. b. genotype. c. meiosis. d. mutation. a. toxoplasmosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rubella, cytomegalovir b. tuberculosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rabies, cytomegalovirus, c. toxoplasmosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rabies, cytomegaloviru d. tuberculosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rabies, cytomegalovirus, 577 19. Which statement applies to the effects of exposure to harmful substances during embryonic life? 1. During the first two weeks, exposure will usually cause death of the embryo. 2. Organs or body structures may be altered by exposure during the first two months. 3. The effects of exposure depend on the stage of development at the time of exposure. 4. Metabolic abnormalities usually follow exposure to teratogens. a. 1, 3 b. 2, 4 c. 1, 2, 3 d. 2, 3, 4 577 20. Exposure to cocaine during pregnancy leads to increased risk of: a. premature birth. b. respiratory problems. c. sudden infant death syndrome. d. A, B, and C 577 21. Which term refers to prenatal diagnosis through examination of amniotic fluid? a. Chorionic villus testing b. Preparing a family pedigree c. Amniocentesis d. Triple-screen test 578 22. The laboratory practice of changing DNA sequences in microorganisms is called: a. the genotype. b. gene mutation. c. genetic engineering. d. gene therapy. 579 23. The purpose of the Human Genome Project was to: a. map the nucleotide sequence and identify the genes on each human chromosome. b. study the common patterns of inheritance of single-gene disorders. c. manipulate the sequence of DNA in microorganisms and animals. d. identify spontaneous alterations in genetic material caused by teratogens. 581 24. Developmental disorders can result from all the following EXCEPT: a. exposure to radiation. b. mercury in foods and water. c. drugs and alcohol. d. folic acid. 577 25. Genes located at the same site on a pair of homologous chromosomes that are also matched for function are called: 569 26. Which of the following can easily pass through the placental barrier? a. Many viruses b. Some heavy metals c. Certain chemicals d. All of the above 577 27. The term proteomics refers to the study of: a. alleles. b. genotypes. c. autosomes. d. phenotypes. a. DNA sequences with unknown functions. b. gene sequences in individual chromosomes. c. the proteins resulting from activation of specific genes. d. identifying certain base pairs in DNA. 579 28. The most invasive prenatal screening test for fetal abnormalities is: a. ultrasonography. b. amniocentesis. c. X-ray. d. blood tests. 578 29. Which of the following can be detected using amniotic fluid? a. Chromosomal abnormalities b. Metabolic disorders c. Certain structural abnormalities d. All the above 578 30. Blood tests are performed on neonates primarily to: a. determine need for immediate surgical correction of anomalies. b. identify disorders requiring immediate treatment. c. identify the presence of any inherited disorders. d. rule out the presence of any infection. 579 31. When genetic influences combine with environmental factors to cause an abnormality, the result is called a: 574 32. The cellular division process that produces the chromosomes that are in the sperm and ova is called: 569 a. chromosomal disorder. b. developmental disorder. c. multifactorial disorder. d. single-gene disorder. a. meiosis. b. mitosis. c. organogenesis. d. polysomy. Chapter 22: Complications due to Pregnancy Chapter 22: Complications due to Pregnancy Test Bank MULTIPLE CHOICE 1. What is the usual time period between the first day of the last menstrual period and the time of birth? 585 2. Common effects of the expanding uterus during pregnancy include all of the following EXCEPT: a. compression of the urinary bladder. b. restricted inspiratory volume. c. low blood pressure. d. varicose veins. 585 | 587 3. Which of the following indicates development of pregnancy-induced hypertension? a. 38 weeks b. Termed the gestation period c. Referred to as gravidity d. The embryonic period a. Proteinuria, edema, and weight gain b. Persistent blood pressure measuring above 140/90 c. Vaginal bleeding d. Blood clots forming in the legs 587 4. What is the usual cause of hemolysis of fetal erythrocytes during pregnancy? a. The mother’s blood is Rh negative and the fetus is Rh positive. b. The parents differ in blood type. c. The mother receives Rh immunoglobulin early in the second pregnancy. d. Fetal antibodies enter the maternal circulation. 588 5. What is the likely cause of painless, bright red, vaginal bleeding during the last trimester? a. Ectopic pregnancy b. Abruptio placentae c. Disseminated intravascular coagulation (DIC) d. Placenta previa 588 6. Adolescent pregnancy is often considered high risk because of: b. poor nutrition and lack of vitamin supplements. c. iron deficiency anemia. d. All of the above 590 7. Which of the following is a serious potential complication of abruptio placentae indicated by low serum levels of clotting factors? 588 8. The term primigravida refers to: a. length of time since the first day of the last menstrual period. b. a woman who is pregnant for the first time. c. estimated date of delivery. d. withdrawal of a small amount of amnionic fluid. 585 9. During which time period do teratogens cause major developmental damage to organs? a. First week following fertilization a. Severe hypertension b. Disseminated intravascular coagulation (DIC) c. Jaundice d. Thromboembolism b. First 2 months c. Any time up to 6 months d. During labor and delivery 584 10. Diagnosis of pregnancy is confirmed through elevated serum levels of: a. hCG. b. testosterone. c. AFP. d. aldosterone. 584 11. Edema and congestion normally develop in many tissues during pregnancy as a result of: a. reduced kidney function. b. decreased serum albumin. c. increased blood volume. d. increases in blood pressure. 587 12. Which of the following statements applies to eclampsia? a. Elevated blood pressure returns to normal after delivery. b. Kidney and liver function remain normal. c. It commonly develops with ectopic pregnancies. d. Blood pressure is very high and seizures may occur. 587 13. Gestational diabetes in the mother usually results in: a. normal maternal blood glucose levels until the last month of pregnancy. b. no further indication of diabetes mellitus following delivery. c. delivery of a high birth-weight infant. d. no additional complications for the infant or mother. 588 14. Place the following statements regarding Rh incompatibility in the correct sequence. Not all choices are included in each answer. 1. Hemolysis of fetal erythrocytes and anemia occur. 2. Maternal Rh-negative cells enter fetal blood. 3. Fetal Rh-positive cells enter maternal blood. 4. Elevated serum bilirubin levels develop in the fetus. 5. Antibodies to Rh-positive cells form in maternal blood. 6. Maternal Rh antibodies enter the fetal circulation. a. 3, 1, 4, 6, 5 b. 6, 2, 4, 3, 5, 1 c. 3, 5, 6, 1, 4 d. 2, 3, 6, 1, 4 588 Chapter 23: Complications due to Adolescence Chapter 23: Complications due to Adolescence Test Bank MULTIPLE CHOICE 1. The biological changes associated with adolescence are stimulated primarily by: a. the peripheral nervous system. b. the thalamus. c. increased secretion of estrogen and progesterone. d. the pituitary gland. 592 2. What is a lateral curvature of the spine called? a. Lordosis b. Kyphosis c. Scoliosis d. Kyphoscoliosis 595 3. How is scoliosis identified? a. Bowed or hunched-over position of head and shoulders b. Unevenly aligned hips and shoulders c. A swayback posture d. One arm and leg shorter than the other 595 4. What are common local signs of osteomyelitis? a. Joint swelling, limited movement b. Deformity of a limb, pain at rest c. Fever, leukocytosis, and malaise d. A red, swollen area, pain increasing with movement 597 5. Which of the following comprise typical early signs of Still’s disease, a form of juvenile rheumatoid arthritis? 1. Presence of rheumatoid factor in the blood 2. High fever and skin rash 3. Swollen painful knees, wrists, and elbows 4. Deformity of the hands and feet a. 1, 3 b. 1, 4 c. 2, 3 d. 2, 4 597 6. Which of the following might fluid and electrolyte deficits cause in a patient with anorexia nervosa? 598 7. Bulimia nervosa is characterized by: a. a refusal to eat. b. extreme weight loss. c. alternating binge eating and purging. d. chronic diarrhea. 598 8. Acne vulgaris can best be described as an infection involving the: a. sweat glands of the upper body. b. dermis and epidermis of the skin. a. Cardiac arrhythmias b. Weight loss c. Dental caries and esophagitis d. Amenorrhea c. apocrine glands. d. sebaceous glands and hair follicles. 599 9. Infectious mononucleosis can be diagnosed by the presence of: a. sore throat, fever, and lymphadenopathy. b. abnormal lymphocytes and positive antibody test. c. the causative bacteria in the saliva. d. extreme fatigue and malaise. 599-600 10. Which statement applies to testicular cancer? a. It often develops in untreated, undescended testes. b. It is related to chromosome abnormalities such as monosomy X. c. The tumor presents as a painful red lump in the scrotum. d. The cancer usually causes sterility. 600 11. An autoimmune disease that causes chronic inflammation in the joints of children is: a. lordosis. b. juvenile rheumatoid arthritis (JRA). c. osteomyelitis. d. metabolic syndrome. 597 12. Which of the following would confirm reduced normal linear growth during adolescence? a. Levels of androgens b. Abnormally thin epiphyseal plate seen on X-ray c. Lack of a broader pelvis in males d. Development of kyphosis 593 13. Obesity in adolescents is: a. determined by calculating body mass index (BMI). b. a significant factor in a teen’s self-image. c. related to increased intake of high fat and high carbohydrate snacks, “fast foods.” d. All of the above 593-594 14. Three factors common to metabolic syndrome include: a. presence of significant abdominal fat mass, changes in glucose metabolism, and changes in lipoprotein m b. increased fat mass throughout the body, changes in glucose metabolism, and delayed sexual maturation. 594 15. Infectious mononucleosis is characterized by all EXCEPT: a. sore throat, fever, fatigue, malaise, and rash on trunk. b. enlarged lymph nodes (lymphadenopathy) and spleen (splenomegaly). c. increased occurrence in infants and young children. d. the presence of atypical T lymphocytes. 599-600 Chapter 24: Complications due to Aging Chapter 24: Complications due to Aging Test Bank MULTIPLE CHOICE 1. All of the following changes are associated with aging EXCEPT: a. loss of elastic fibers. b. decreased metabolic rate. c. decreased secretion of all hormones. d. degenerative vascular changes. 604 c. significant increase of fat on hips and thighs, delayed linear growth, and change in calcium and vitamin D d. BMI at the 85th percentile, type 2 diabetes mellitus, and hypertension. 2. Predisposing factors to osteoporosis in older women include all of the following EXCEPT: a. decreased estrogen secretion. b. genetic factors. c. sedentary lifestyle. d. decreased parathyroid hormone. 606 3. Lung expansion in the elderly may be reduced because of decreased: 1. tissue elasticity. 2. rib mobility. 3. control by the respiratory center. 4. skeletal muscle strength. a. 1, 3 b. 1, 4 c. 2, 3, 4 d. 1, 2, 4 607 4. Vision in the elderly may be impaired when the eyeball becomes less elastic, thus preventing accommodation and resulting in: a. presbyopia. b. cataracts. c. glaucoma. d. damage to the retina. 608 5. What is a major factor leading to increased occurrence of cancer in the elderly? a. Widespread vascular degeneration b. Cumulative exposure to carcinogens c. Hereditary factors d. Increased immune surveillance 609 6. Senescence refers to the period of time when: a. mitosis is accelerated. b. apoptosis is reduced. c. aging changes become apparent. d. cell death exceeds cell replacement. 603 7. Theories about the causes of aging include: a. apoptosis. b. wear and tear. c. altered protein (amyloid) accumulation. d. All the above 604 8. Which of the following does NOT contribute to the increasing life span of the general population? a. Reduced cognitive and social activities b. Improved living conditions c. Better nutrition d. Advancements in health care 603 9. The term given to the change that occurs in women at around age 50 with the cessation of the menstrual cycle is: 604 10. Recommendations to reduce the risk factors and the progression of osteoporosis with aging include: a. menopause. b. dysmenorrhea. c. amenorrhea. d. menarche. a. reducing vitamin D intake. b. maintaining walking and weight-bearing exercise. c. increasing bone resorption. d. maintaining glucocorticoid therapy. 607 11. All are physiological changes that occur with aging EXCEPT: a. reduced skeletal muscle mass. b. degeneration of fibrocartilage in intervertebral discs in the spine. c. increased basal metabolic rate (BMR). d. reduced bladder capacity and incomplete bladder emptying. 607 | 609 12. With advancing age, the major change in the cardiovascular system involves: a. irregular impulse conduction in the heart. b. a reduced number of collagen fibers to support cardiac muscle. c. vascular degeneration, leading to arteriosclerosis and atherosclerosis. d. the heart valves becoming thin and weak. 605 13. Which of the following factors lead to delayed wound healing in the elderly? 1. Reduced rate of mitosis 2. Inadequate circulation 3. High risk of infection 4. More effective immune system a. 1, 2 b. 1, 3 c. 2, 4 d. 1, 2, 3 609 14. Which of the following may develop in an elderly patient who has several medical problems and is markedly obese? 609 Chapter 25: Immobility and Associated Problems Chapter 25: Immobility and Associated Problems Test Bank MULTIPLE CHOICE 1. Which of the following is likely to develop when a leg is immobilized in a cast? a. Osteoarthritis and cardiovascular complications b. Decreased activity and diabetes mellitus c. Undesirable interactions with multiple prescription drugs and over-the-counter (OTC) medications d. A, B, and C a. Contracture b. Muscle hypertrophy c. Muscle atrophy d. Increased osteoblastic activity 613 2. Which of the following frequently causes decubitus ulcers? a. Infection by resident flora b. Ischemia at pressure points c. Normal degenerative changes d. Allergic reaction to adhesive tape or dressings 614 3. What do prolonged periods of immobility frequently lead to? 1. Orthostatic hypotension 2. Increased blood pressure and increased heart rate 3. Increased risk of both thrombi and emboli 4. Rapid, deep respirations a. 1, 2 b. 1, 3 c. 2, 4 d. 3, 4 614-615 4. What is a major factor predisposing to pulmonary infection in immobilized patients? a. Decreased activity and demand for oxygen b. Increased retention of CO2 c. Inability to sneeze forcefully d. Stasis of secretions in the lungs 615 5. Bladder infections are more likely to develop in immobilized patients because of: a. stasis of urine in the urinary system. b. development of hypocalcemia with immobility. c. fluid overload in the system. d. lack of neurological control of the bladder. 616 6. Which of the following is/are common effect(s) of prolonged immobility in children? a. Delayed linear growth b. Contractures and deformities involving the hips, spine, legs, and feet c. Skeletal muscle weakness d. A, B, and C 616 7. Paralysis of the lower part of the body is called: a. hemiplegia. b. paraplegia. c. quadriplegia. d. None of the above 613 8. Prolonged immobility may predispose to in the kidneys. a. urinary stasis b. renal calculi c. infection d. All of the above 616-617 9. Inactive muscle quickly loses strength as it becomes . a. less elastic. b. atrophied. c. contracted. d. spastic. 613 10. The major problem associated with immobility and the gastrointestinal tract is: a. constipation. b. diarrhea. c. nausea. d. increased rate of peristalsis. 615 11. Lack of weight-bearing and skeletal muscle activity for a prolonged period leads to: a. bone demineralization. b. lengthening of tendons and ligaments. c. decreased skeletal muscle mass. d. A and C 613 12. Which of the following applies/apply to orthostatic hypotension associated with prolonged immobility? a. Sudden changes in body position from supine to upright may cause low blood pressure. b. Venous return and cardiac output are decreased with immobility. c. All cardiovascular reflexes are lost with prolonged immobility. d. A and B 614 13. Atelectasis may occur with a prolonged period of bed rest because of: a. reduced removal of pulmonary secretions. b. increased expansion of the lower lobes of the lungs. c. increased risk of aspiration in a sitting position. d. loss of cough reflex. 615 14. Immobility may lead to dehydration primarily as a result of: a. changes in hormonal secretions due to increased blood in the thorax. b. destruction of the kidneys as a result of ischemia and necrosis. c. blockage of the ureters, causing retention of urine. d. toxins being produced by infectious microorganisms. 616 15. Virchow’s triad refers to: a. an anatomical structure in the kidneys. b. a combination of factors affecting potential thrombus formation. c. factors that predispose an individual toward urinary tract infections. d. psychological factors leading to stress associated with immobility. 615 Chapter 26: Stress and Associated Problems Chapter 26: Stress and Associated Problems Test Bank MULTIPLE CHOICE 1. Hans Selye defined his general adaptation syndrome concept, which is also known as: a. fight or flight. b. compensate or compromise. c. restrain or release. d. avoid and flee. 618 2. Improved function of the heart and brain during a stress response results from: 1. glycogenesis. 2. bronchodilation. 3. vasoconstriction in the skin and viscera. 4. decreased metabolic rate. a. 1, 2 b. 2, 3 c. 2, 4 d. 3, 4 619 3. In which of the following situations would the stress response be used to prevent blood pressure from dropping too low? 619 4. During the stress response, endorphins act as: a. pain blockers. b. cerebral function depressors. c. stimulators of increased secretion of aldosterone and insulin. d. an enhancer of the immune response. 619 5. Severe, prolonged stress may cause acute renal failure or stress ulcers to develop as a result of: a. a deficit of glucose and oxygen in the body. b. the development of decompensated acidosis. a. Increasing anger during an argument b. Writing a final examination c. Fear about a medical diagnosis d. Internal hemorrhage from injuries in a car accident c. prolonged vasoconstriction and ischemia. d. the supply of hormones having been exhausted. 621 6. Selye defined three stages in the stress response. The third stage is designated as the: a. alarm stage. b. resistance stage. c. stage of exhaustion. d. maladaptive stage. 619 7. The stress response involves the integrated action of the: 1. hypothalamus. 2. hypophysis. 3. sympathetic nervous system. 4. adrenal glands. a. 1, 3 b. 2, 3 c. 1, 2, 4 d. 1, 2, 3, 4 619 8. Possible complications caused by prolonged, severe stress include all of the following EXCEPT: a. hypertension. b. tension headache. c. diabetes mellitus. d. blindness. 620-621 9. A serious consequence of a major disaster, first recognized in war veterans is: a. stress ulcers. b. delayed tissue healing. c. posttraumatic stress disorder (PTSD). d. cancer. 622 10. Which of the following may alter a person’s perception of a stressor? a. The presence of several stressors at the same time b. Past experiences c. Lack of effective coping mechanisms d. A, B, and C 618-619 Promoted Chapter 27: Substance Abuse and Associated Problems Chapter 27: Substance Abuse and Associated Problems Test Bank MULTIPLE CHOICE 1. What is/are the typical effect(s) of psychedelic substances? a. Drowsiness and euphoria b. Marked stimulation of the central nervous system (CNS) c. Lethargy and decreased metabolic rate d. Altered perception and awareness as well as hallucinations 625 2. Which of the following statements is characteristic of alcohol? a. It is primarily a CNS stimulant. b. It may cause congenital defects in infants born to alcoholic mothers. c. It does not interact with other drugs in the CNS. d. It usually causes severe kidney damage. 628 3. What is physiological dependence? a. An intense emotional need for a drug in order to function b. Adaptation of the body to a drug, resulting in withdrawal signs after the drug is discontinued c. The need for an ever-increasing dose to produce the same effect d. Continuing to take a drug when it is not required medically 625 4. What is a common indication of substance abuse? a. Behavioral change b. Weight gain c. Depression d. Loss of sensory function 627 5. A patient who has developed a tolerance for codeine will: a. demonstrate physical signs when the drug is discontinued. b. require a larger dose than expected to control pain. c. require a smaller dose than expected to control pain. d. show signs or symptoms of drug toxicity. 625 6. Chemical dependency has been associated with all the following EXCEPT: a. hereditary factors. b. disease requiring certain prescription drugs. c. easy access to many kinds of drugs. d. increased acceptance of alcohol or marijuana to cope with stress. e. increased work productivity. 626 7. Which of the following is/are NOT a common sign(s) of withdrawal? a. Irritability b. Respiratory depression c. Nausea and vomiting d. Psychotic episodes and convulsions e. Tremors 628 8. When an increased dosage of a drug causes toxic effects, it is called: a. synergism. b. neurostimulant. c. overdose. d. detoxification. 627 9. Withdrawal from any drug is best accomplished: a. with medical support. b. with legally prescribed drugs. c. following intensive counseling. d. using CNS stimulants. 628 10. Chronic alcoholism is likely to cause all of the following EXCEPT: a. cirrhosis. b. mental confusion. c. loss of motor coordination. d. altered personality and amnesia. e. respiratory failure. 628-629 11. Which of the following is a synthetic opioid that prevents withdrawal symptoms and improves function? 629 a. Antabuse b. Methadone c. Cocaine d. Diazepam 12. Synergism can cause an emergency situation when: a. antidotes for respiratory depression are given too quickly. b. a combination of alcohol and drugs has been taken. c. a large dose of a drug affects the CNS. d. an individual involuntarily develops a habit. 627 13. Which of the following drugs causes headache and vomiting when an alcoholic ingests small amounts of alcohol? 629 14. Which of the following applies to abuse of anabolic steroids? a. They cause CNS depression, deep sleep, and amnesia. b. They often cause permanent damage to the cardiovascular system. c. They help to relax skeletal muscle spasms. d. They help to relieve the pain of athletic injuries. 627 a. Methadone b. Diazepam c. Disulfiram d. Naloxone Chapter 28: Environmental Hazards and Associated Problems Chapter 28: Environmental Hazards and Associated Problems Test Bank MULTIPLE CHOICE 1. Which of the following is likely to result from lead poisoning? a. Damage to the brain and peripheral nerves b. Inflammation and fibrosis in the lungs c. Various cancers d. Displacement of oxygen from hemoglobin 633 2. During the development of hyperthermia, the state of heat exhaustion is indicated when: a. body core temperature is very high. b. skeletal muscle spasms occur. c. hypovolemia and fainting occur. d. the cool-down process is too rapid. 634 3. What is/are signs of hypothermia? a. Systemic vasodilation b. Lethargy and confusion c. Nausea and cramps d. Rapid but strong pulse 635 4. Which of the following types of cells are most likely to be damaged by exposure to radiation? a. Bone and cartilage b. Skeletal and smooth muscle c. Peripheral and central neurons d. Epithelial tissue and bone marrow 635 5. Which of the following events would most likely cause a person to faint and experience difficulty breathing? 636-637 6. Bites and stings cause disease in which three ways? a. Injection of toxins, transmission of infectious agents, or allergic reactions a. Exposure to gamma rays b. Eating fish containing mercury c. An insect sting d. Inhalation of asbestos particles b. High fever and chills, transmission of infectious agents, or nausea and vomiting c. Bone marrow damage, extensive skin rashes, or allergic reactions d. Injection of neurotoxins, transmission of infectious agents, or kidney damage 636-637 7. Which statement applies to food poisoning? 1. It results from consuming contaminated food and water. 2. It often causes gastroenteritis, including vomiting and diarrhea. 3. Outbreaks occur frequently in institutions. 4. It is often caused by Escherichia coli, normally found in the stomach. a. 1, 3 b. 2, 4 c. 1, 2, 3 d. 1, 3, 4 636 8. Institutions frequently have outbreaks of infection associated with poultry products contaminated by: a. E. coli b. Salmonella c. Listeria d. HIV 636 9. The amount of radiation absorbed by the body is measured in rads, or . a. radiation-absorbed doses. b. roentgen-absorbed doses. c. radiation-emission number. d. radiation ionizing rate. 635 10. The term pica refers to: a. the consumption of nonfood substances such as clay. b. diffuse edema and degeneration of neurons in the brain. c. particulates in the respiratory tract. d. high levels of mercury in the blood. 633 11. Inhalants can be: a. a particulate such as asbestos. b. gaseous, such as sulfur dioxide. c. a solvent, such as benzene. d. A, B, and C 633-634 12. Choose the correct effects of exposure of the ears to very cold temperatures: a. Loss of sensation b. Lethargy and confusion c. Vascular occlusions d. A and C 635 13. During the development of hyperthermia, the stage of heat stroke is marked by: a. shock and coma. b. hypervolemia and headache. c. diaphoresis and decreasing body temperature. d. dizziness, fainting, and headache. 634 14. Which of the following is a potential effect of a bite or sting? a. Immediate heart failure b. Anaphylaxis c. Severe nausea, vomiting, and diarrhea d. Bone marrow damage 636-637 15. Bites from both wild and domesticated animals may cause: a. anaphylaxis. b. Shigella outbreaks. c. rabies. d. severe pain and headache. 636-637 16. Which of the following is considered carcinogenic? a. Lead b. Carbon monoxide c. Inhaled particulates d. Mercury 633 17. Illness in institutions may be traced back to food handlers who: a. are carriers of pathogens. b. do not practice adequate hand-washing or sanitization. c. bring in pathogens from home or the community. d. A, B, and C 636 18. A common illness for tourists in developing countries is “traveler’s diarrhea,” often caused by: a. Salmonella b. Shigella c. E. coli d. Listeria 636 19. Radiation damage may occur from repeated exposure to: a. ultraviolet rays. b. X-rays. c. radioactive substances. d. A, B, and C 635-636 20. Two types of eye damage that can be caused by a laser beam are: a. chemical and structural. b. thermal burn and photochemical damage. c. tissue necrosis and vascular occlusions. d. formation of deep lesions in the optic nerve and in the sclera. 636 [Show More]
Last updated: 1 year ago
Preview 1 out of 421 pages
Instant download

Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 25, 2021
Number of pages
421
Written in
Additional information
This document has been written for:
Uploaded
Apr 25, 2021
Downloads
0
Views
271