*NURSING > EXAM > PATHO 2410 Protection/Adaptation Test Bank Questions And Answers( Complete Solution Rated A) (All)
PATHO 2410 Protection/Adaptation Test Bank Questions And Answers( Complete Solution Rated A)
Document Content and Description Below
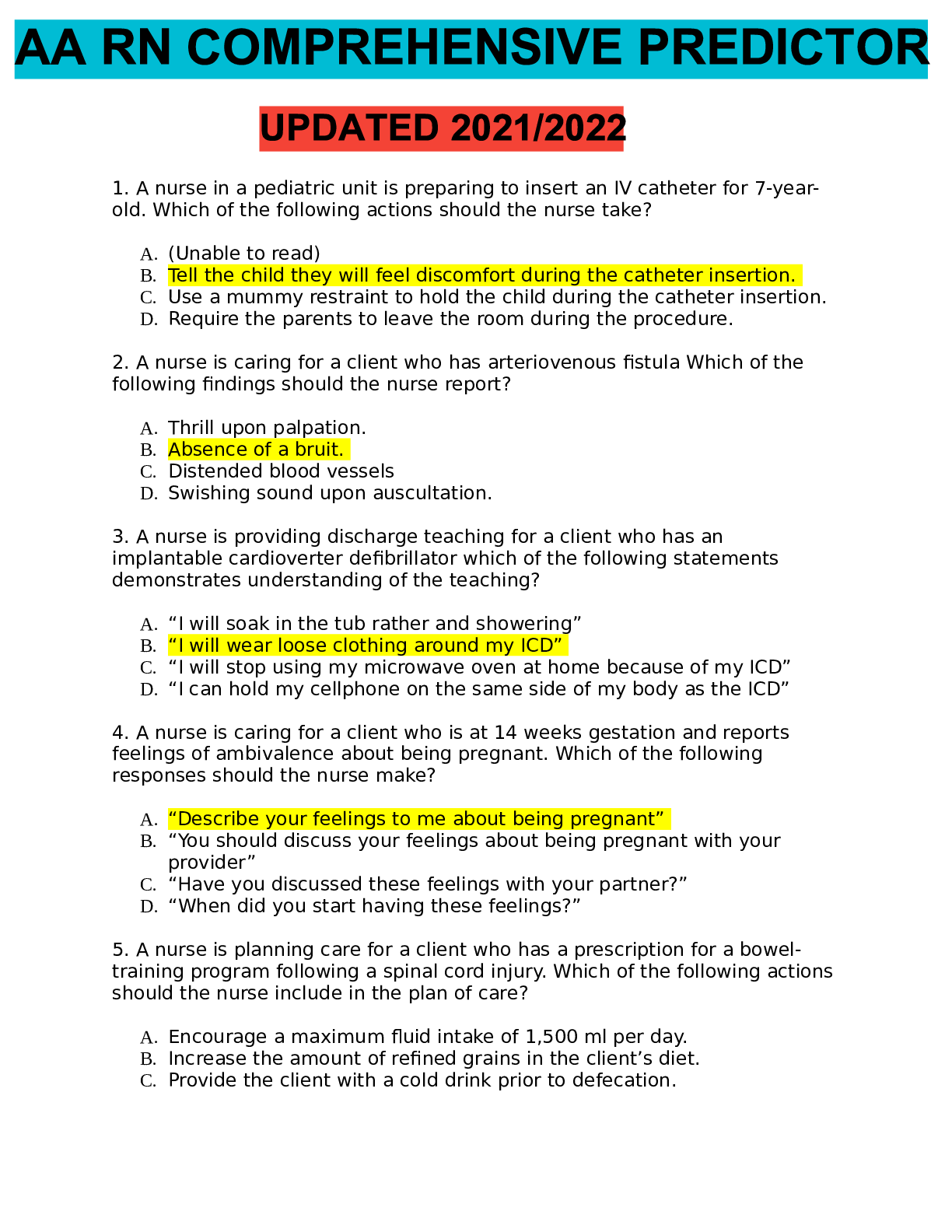
PATHO 2410 Protection/Adaptation (CP #1) Test Bank Chapter 1 1. Which of the following would be the most likely cause of an iatrogenic disease? a. An inherited disorder b. A combination of speci... fic etiological factors c. An unwanted effect of a prescribed drug d. Prolonged exposure to toxic chemicals in the environment 2. The manifestations of a disease are best defined as the: a. Subjective feelings of discomfort during a chronic illness. b. Signs and symptoms of a disease. c. Factors that precipitate an acute episode of a chronic illness. d. Early indicators of the prodromal stage of infection. 3. The best definition of the term prognosis is the: a. Precipitating factors causing an acute episode. b. Number of remissions to be expected during the course of a chronic illness. c. Predicted outcome or likelihood of recovery from a specific disease. d. Exacerbations occurring during chronic illness. 4. Which of the following is considered a systemic sign of disease? a. Swelling of the knee b. Fever c. Pain in the neck d. Red rash on the face 5. Etiology is defined as the study of the: a. Causes of a disease b. Course of a disease c. Expected complications of a disease d. Manifestations of a disease 6. A type of cellular adaptation in which there is a decrease in cell size is referred to as: a. Hypertrophy b. Metaplasia c. Anaplasia d. Atrophy 7. A change in a tissue marked by cells that vary in size and shape and show increased mitotic figures would be called: a. Metaplasia b. Atrophy c. Dysplasia d. Hypertrophy 8. A deficit of oxygen in the cells usually due to respiratory or circulatory problems is called: a. Apoptosis b. Ischemia c. Hypertrophy d. Necrosis 9. When a group of cells in the body dies, the change is called: a. Ischemia b. Gangrene c. Hypoxia d. Necrosis 10. Rigorous weight lifting/body building regimens may result in the skeletal muscle cells undergoing: a. Hypertrophy b. Dysplasia c. Atrophy d. Regeneration 11. The term cancer refers to: a. Dysplasia b. Hyperplasia c. Metaplasia d. Malignant neoplasm 12. To which of the following does the term apoptosis refer? a. Increased rate of mitosis by certain cells b. Ischemic damage to cells c. Liquefaction of necrotic tissue d. Preprogrammed cell self-destruction 13. Which of the following statements is TRUE? a. Alteration of DNA does not change cell function. b. Damaged cells may be able to repair themselves. c. All types of cells die at the same rate. d. Mild ischemia causes immediate cell death. 14. Caseation necrosis refers to an area where: a. Cell proteins have been denatured. b. Cell are liquefied by enzymes. c. Dead cells form a thick cheesy substance. d. Bacterial invasion has occurred. 15. Routine application of sun block to skin would be an example of: a. An iatrogenic cause of cancer b. A preventative measure c. A precipitating factor d. A predisposing condition 16. A circumstance that causes a sudden acute episode of a chronic disease to occur is termed: a. Latent stage b. Predisposing factor c. Incidence d. Precipitating factor 17. The term homeostasis refers to: a. The causative factors in a particular disease. b. Maintenance of a stable internal environment. c. A condition that triggers an acute episode. d. A collection of signs and symptoms. 18. Which term is used to describe a new and secondary or additional problem that arises after the original disease has been established? a. Symptoms b. Occurrence c. Manifestations d. Complication 19. Pathophysiology involves the study of: a. The structure of the human body. b. The functions of various organs in the body. c. Functional or structural changes resulting from disease processes. d. Various cell structures and related functions. 20. Which of the following is the best definition of epidemiology? a. The science of tracking the occurrence and distribution of diseases b. The relative number of deaths resulting from a particular disease c. Identification of a specific disease through evaluation of signs and symptoms d. The global search for emerging diseases 21. Which of the following can cause cell injury or death? (Select all that apply) a. Hypoxia b. Exposure to excessive cold c. Excessive pressure on a tissue d. Chemical toxins 22. All of the following are part of the Seven Steps to Health EXCEPT: a. Follow cancer screening guidelines. b. Use sun block agents whenever exposed. c. Participate in strenuous exercise on a regular daily basis. d. Choose high fiber, lower fat foods. 23. The term disease refers to: a. The period of recovery and return to a normal healthy state. b. A deviation from the normal state of health and function. c. The treatment measures used to promote recovery. d. A basic collection of signs and symptoms. 24. A collection of signs and symptoms, often affecting more than one organ or system, that usually occur together in response to a certain condition is referred to as a (an): a. Acute disease b. Multiorgan disorder c. Syndrome d. Manifestation 25. All of the following statements are correct about cell damage EXCEPT: a. The initial stage of cell damage often causes an alteration in metabolic reactions. b. If the factor causing the damage is removed quickly, the cell may be able to recover and return to its normal state. c. If the noxious factor remains for an extended period of time, the damage becomes irreversible and the cell dies. d. Initially, cell damage does not change cell metabolism, structure, or function. 26. Which of the following conditions distinguishes double blind studies used in health research? a. Neither the members of the control group or the experimental group nor the person administering the treatment knows who is receiving the experimental therapy. b. Both groups of research subjects and the person administering the treatment know who is receiving the experimental therapy. c. The research subjects do not know, but the person administering the treatment knows who is receiving placebo or standard therapy. d. Only members of the control group know they are receiving standard therapy. 27. If the data collected from the research process confirm that the new treatment has increased effectiveness and is safe, this is called: a. The placebo effect b. Evidence-based research c. Blind research studies d. Approval for immediate distribution 28. A short-term illness that develops very quickly with perhaps a high fever or severe pain is called: a. Acute b. Latent c. Chronic d. Manifestation 29. The term prognosis refers to the: a. Period of recovery and return to a normal state. b. Expected outcome of the disease. c. Mortality and morbidity rates for a given population. d. Typical collection of signs and symptoms. 30. When prolonged ischemia occurs to an area of the heart, the resulting damage is referred to as: a. Atrophy b. Liquefactive necrosis c. Apoptosis d. Infarction 31. During the evaluation process for a new therapy’s effectiveness and safety, a double blind study may be conducted during: a. The first stage b. The second stage c. The third stage d. Any of these stages 32. Why are the predisposing factors for a specific disease important to health professionals? a. To predict the prognosis b. To determine treatments c. To develop preventative measures d. To develop morbidity statistics 33. Cell damage may be caused by exogenous sources such as: a. Abnormal metabolic processes b. Certain food additives c. Genetic defects d. Localized hypoxia 34. Which of the following is usually included in a medical history? (Select all that apply) a. Past illnesses or surgeries b. Current illnesses, acute and chronic c. Prescribed medication or other treatments d. Nonprescription drugs and herbal remedies e. Current allergies 35. A situation when there is a higher than expected number of cases of an infectious disease within a given area is called a/an: a. Epidemic b. Exacerbation c. Morbidity d. Pandemic 36. The term pathogenesis refers to: a. The development of a disease or sequence of events related to tissue changes involved in the disease process. b. The determination of the cause(s) involved in the development of a malignant neoplasm. c. The specific signs and symptoms involved in the change from an acute disease to a chronic disease. d. The changes in cells of affected tissue that result in necrosis. Chapter 5 1. Tears are considered to be part of the: (Select all that apply) a. First line of defense b. Second line of defense c. Third line of defense d. Specific defenses e. Nonspecific defenses 2. A specific defense for the body is: a. Phagocytosis b. Sensitized T lymphocytes c. The inflammatory response d. Intact skin and mucous membranes 3. The inflammatory response is a nonspecific response to: a. Phagocytosis of foreign material b. Local vasodilation c. Any tissue injury d. Formation of purulent exudates 4. Chemical mediators released during the inflammatory response include: a. Albumin and fibrinogen. b. Growth factors and cell enzymes. c. Macrophages and neutrophils. d. Histamine and prostaglandins. 5. Which of the following result directly from the release of chemical mediators following a moderate burn injury? (Select all that apply) a. Pain b. Local vasoconstriction c. Increased capillary permeability d. Pallor 6. Granulation tissue is best described as: a. Highly vascular, very fragile, and very susceptible to infection. b. An erosion through the wall of viscera, leading to complications. c. A type of adhesion with no vascularization. d. A form of stenosis, in a duct, that is extremely tough and resists attack by microbes. 7. Edema associated with inflammation results directly from: a. Increased fluid and protein in the interstitial compartment. b. Increased phagocytes in the affected area. c. Decreased capillary permeability. d. General vasoconstriction. 8. The warmth and redness related to the inflammatory response results from: a. Increased interstitial fluid. b. Production of complement. c. A large number of white blood cells (WBCs) entering the area. d. Increased blood flow into the area. 9. What is the correct order of the following events in the inflammatory response immediately after tissue injury? 1. Increased permeability of blood vessels 2. Dilation of blood vessels 3. Transient vasoconstriction 4. Migration of leukocytes to the area 5. Hyperemia a. 5, 3, 2, 1, 4 b. 1, 2, 4, 5, 3 c. 2, 3, 5, 4, 1 d. 3, 2, 5, 1, 4 10. The process of phagocytosis involves the: a. Ingestion of foreign material and cell debris by leukocytes. b. Shift of fluid and protein out of capillaries. c. Formation of a fibrin mesh around the infected area. d. Movement of erythrocytes through the capillary wall. 11. Systemic effects of severe inflammation include: a. Erythema and warmth b. Loss of movement at the affected joint c. Fatigue, anorexia, and mild fever d. Abscess formation 12. The term leukocytosis means: a. Increased white blood cells (WBCs) in the blood. b. Decreased WBCs in the blood. c. Increased number of immature circulating leukocytes. d. Significant change in the proportions of WBCs. 13. Which of the following statements applies to fever? a. Viral infection is usually present. b. Heat-loss mechanisms have been stimulated. c. It is caused by a signal to the thalamus. d. It results from release of pyrogens into the circulation. 14. Mechanisms to bring an elevated body temperature down to the normal level include: a. General cutaneous vasodilation. b. Generalized shivering. c. Increased heart rate. d. Increased metabolic rate. 15. Replacement of damaged tissue by similar functional cells is termed: a. Fibrosis b. Regeneration c. Resolution d. Repair by scar tissue 16. Scar tissue consists primarily of: a. Granulation tissue b. Epithelial cells c. Collagen fibers d. New capillaries and smooth muscle fibers 17. Which of the following promotes rapid healing? a. Closely approximated edges of a wound b. Presence of foreign material c. Exposure to radiation d. Vasoconstriction in the involved area 18. Glucocorticoids are used to treat inflammation because they directly: a. Promote the release of prostaglandins at the site. b. Decrease capillary permeability. c. Mobilize lymphocytes and neutrophils. d. Prevent infection. 19. Patients taking glucocorticoids for long periods of time are likely to develop all of the following EXCEPT: a. Decreased bone density. b. Wasting of skeletal muscle. c. Opportunistic infections. d. Increased leukocyte production. 20. Which of the following drugs relieves fever and some types of pain but is NOT an anti-inflammatory agent? a. Acetaminophen b. Prednisone c. Aspirin d. Ibuprofen 21. A burn area in which the epidermis and part of the dermis is destroyed is classified as: a. Full-thickness b. Deep partial-thickness c. Superficial partial-thickness d. First-degree 22. A woman has burns on the anterior surfaces of her right arm, chest, and right leg. The percentage of body surface area burned is approximately: a. 13.5% b. 18% c. 22.5% d. 31.5% 23. The characteristic appearance of a full-thickness burn is: a. Painful with multiple blisters b. Heavy bleeding c. Red with some swelling d. Dry, firm, charred, or hard white surface 24. A typical source of infection in burn areas is: a. The skin grafts b. Microbes surviving in the hair follicles in the burn area c. Circulating blood bringing microbes to the burn wound d. Opportunistic virus in digestive tract 25. A large burn area predisposes to decreased blood pressure because: a. Bleeding occurs under the burn surface. b. The heart is damaged by toxic materials from the burn. c. Fluid and protein shift out of the blood. d. Vasoconstriction occurs in the burn area. 26. During an inflammatory response, hyperemia is caused by: a. Increased blood flow in the area. b. Increased capillary permeability. c. Irritation of sensory nerve endings by histamine. d. Increased leukocytes in the area. 27. The advantages of applying a biosynthetic skin substitute to a large area of full-thickness burns include: (Select all that apply) a. Reduced risk of infection b. Decreased loss of plasma protein and fluid c. Developing stronger fibrous scar tissue d. More rapid healing e. Regeneration of all glands, nerves, and hair follicles 28. Purulent exudates usually contain: a. Small amounts of plasma protein & histamine in water. b. Red blood cells & all types of white blood cells. c. Numerous leukocytes, bacteria, and cell debris. d. Large amounts of water containing a few cells. 29. Isoenzymes in the circulating blood: a. Are a type of plasma protein normally present in the circulating blood. b. Often indicate the precise location of an inflammatory response. c. Are normally released from leukocytes during the inflammatory response. d. Are pyrogens, causing low-grade fever. 30. A serous exudate is best described as a: a. Thin, watery, colorless exudate. b. Thick, sticky, cloudy secretion. c. Thick, greenish material containing microbes. d. Brownish, clotted material. 31. Systemic manifestations of an inflammatory response include: a. Edema and erythema. b. Area of necrosis and loss of function. c. Pain and tenderness. d. Fever and malaise. 32. Some local effects of a general inflammatory response would include: a. High, spiking fever and chills. b. Redness, warmth, and swelling c. Leukopenia and reduced erythrocyte sedimentation rate (ESR) d. Anorexia and headaches 33. Prolonged administration of glucocorticoids such as prednisone may cause: (Select all that apply) a. Atrophy of lymphoid tissue. b. Increased resistance to infection. c. Thrombocytopenia. d. Decreased protein synthesis. 34. Application of ice to an injured knee reduces edema by: a. Promoting return of lymph fluid. b. Causing local vasoconstriction. c. Increasing the rate of tissue repair. d. Causing systemic vasodilation. 35. Healing of large areas of skin loss (including dermis and epidermis) would be most successful through: a. Rapid mitosis and regeneration of skin layers. b. Resolution of damaged cells in the area. c. Covering the area with biosynthetic skin substitute. d. Graft of fibrous tissue to the area. 36. Prostaglandins are produced from and cause . a. Activated plasma protein; increased capillary permeability b. Mast cells; vasodilation and pain c. Platelets; attraction of neutrophils, chemotaxis d. Mast cell granules; activation of histamines and kinins 37. The number of neutrophils in the blood is increased significantly: a. During allergic reactions. b. During chronic inflammation. c. To produce antibodies. d. In order to promote phagocytosis. 38. An abscess contains: a. Serous exudate b. Purulent exudate c. Fibrinous exudate d. Hemorrhagic exudate 39. Nonspecific agents that protect uninfected cells against viruses are called: a. Neutrophils b. Macrophages c. Interferons d. Pyrogens 40. Causes of inflammation include: a. Direct physical damage such as cuts and sprains b. Allergic reactions c. Infection d. All of the above 41. In normal capillary exchange, what is net hydrostatic pressure based on? a. The difference between the hydrostatic pressure within the capillary, as compared with the hydrostatic pressure of the interstitial fluid b. The relative osmotic pressures in the blood and the interstitial fluid c. The difference between the hydrostatic pressure and osmotic pressure within the capillary d. The difference between the concentrations of blood cells, plasma proteins, and dissolved substances in the blood and the interstitial fluid 42. The cardinal signs of inflammation include all of the following EXCEPT: a. Redness b. Loss of function c. Nausea d. Swelling 43. Drugs that have anti-inflammatory, analgesic, and antipyretic activities include: (Select all that apply) a. COX-2 inhibitors (NSAIDs). b. Glucocorticoids (e.g., prednisone). c. Ibuprofen (NSAID). d. Acetaminophen. e. Aspirin (ASA). 44. Aspirin (ASA) is discouraged for treatment of viral infection in children because of: a. Decreased bone growth after puberty. b. Frequent production of blood clots. c. Formation of a granuloma filled with virus. d. The risk of developing Reye’s syndrome. 45. Systemic manifestations of inflammation include all EXCEPT: a. Pyrexia b. Malaise c. Local swelling d. Anorexia 46. Which of the following cellular elements found in the inflammatory response are responsible for phagocytosis? a. Macrophages b. Basophils c. B lymphocytes d. T lymphocytes e. Eosinophils 47. Which chemical mediator is involved in prolonging the inflammatory response? a. Bradykinin b. Histamine c. Leukotrienes d. Chemotactic factors 48. Potential complications after healing by scar formation include all the following EXCEPT: a. Lack of sensory function in the area. b. Contractures and adhesions. c. Increased hair growth. d. Keloid formation. 49. All of the following are correct statements regarding wound healing EXCEPT: a. Resolution occurs where there is minimal tissue damage and the cells can recover. b. Granulation tissue forms a permanent replacement for damaged tissue. c. Regeneration occurs where the cells are capable of mitosis. d. Scar tissue forms where the surrounding cells are incapable of mitosis. 50. Which of the following statements regarding inflammation is incorrect? a. Inflammation caused by an allergen or a burn will typically produce a serous exudate. b. Infection is one cause of inflammation. c. Inflammation is the body’s nonspecific response to tissue injury. d. Disorders are named using the ending -sarcoma to indicate inflammation. 51. Which of the following helps to localize and “wall off” the foreign material during an inflammatory response? a. Lymphocytes b. Increased fluid c. Fibrinogen d. Antibodies 52. Why is an application of cold recommended as part of the RICE first aid measures immediately following an inflammatory response due to injury? a. It improves circulation in the area removing chemical mediators. b. It causes local vasoconstriction to reduce local edema. c. It draws more phagocytic cells to the area to remove debris. d. It promotes immediate healing. 53. One goal for current research in tissue engineering is to: a. Create a functional replacement tissue when regeneration is not possible. b. Adapt cells from the injured organ to produce replacement tissue. c. Design a nonliving synthetic replacement tissue. d. Use stem cells as a temporary covering for damaged tissue. 54. Identify the proper sequence in the healing process. a. A blood clot forms; granulation tissue grows into the gap; new blood vessels develop; phagocytosis of foreign material and cell debris occurs; and collagen fibers form a tight, strong scar. b. A blood clot forms; phagocytes remove foreign material and cell debris; granulation tissue grows into the gap; new blood vessels form; and collagen fibers promote formation of a tight, strong scar. c. Collagen fibers form in the damaged area; a blood clot forms; granulation tissue grows into the gap; angiogenesis takes place; and foreign material and cell debris are removed by phagocytes. d. Foreign material and cell debris are removed by phagocytes; a blood clot forms; granulation tissue grows into the gap; new blood vessels form; and collagen fibers grow and cross-link. 55. All of the following are factors that promote healing EXCEPT: a. Good nutrition: protein, vitamins A and C. b. A clean, undisturbed wound. c. Effective circulation. d. Advanced age. 56. Identify the correct statement about burns: a. The severity of the burn depends on the temperature, duration, and extent of the burn. b. Young children are less likely to suffer severe burns from immersion in excessively hot water. c. Burns to the palms of the hands are more damaging than burns on the face. d. With a major burn, excessive bleeding usually causes shock. 57. Which statement applies to the recommended emergency care for burns? a. Drop and lie completely still on your back. b. Call a neighbor for help if the burn appears to be extensive. c. Apply lotion and cover burn tightly with a sheet or towel. d. Cover the burn area with clean, cool, or tepid water and remove nonsticking clothing. 58. Inhalation of carbon monoxide is a threat for many burn patients because this gas: a. Causes swelling in the trachea. b. Quickly reduces the available oxygen in the blood. c. Prevents full expansion of the lungs. d. Is toxic to the nervous system. 59. Hypermetabolism is common with major burns because of: a. Increased heat loss from the burn wound. b. Demand for tissue repair. c. Recurrent stress response. d. All of the above 60. How does scar tissue usually cause obstructions to develop in tube-like structures? a. Scar tissue continues to grow and spread, causing a blockage. b. Scar tissue does not stretch, but rather shrinks in time, causing narrowing. c. Scar tissue twists and forms knots as it develops. d. Scar tissue attaches to nearby normal tissue, causing obstruction. 61. Which of the following is a serious potential complication found only with the anti-inflammatory COX-2 inhibitor drugs? a. Increased risk of infection at the site of inflammation b. Reye’s syndrome developing in children and young adults c. Increased incidence of heart attacks d. Greatly delayed blood clotting Chapter 6 1. Bacteria that form an irregular cluster of spheres are called: a. Bacilli b. Diplococci c. Staphylococci d. Streptococci 2. A strict anaerobe requires which specific environment? a. A dry environment b. An acidic medium c. Air at a temperature less than 61 F/16 C d. The absence of oxygen 3. The presence of the bacterial capsule: a. Aids in the release of endotoxins b. Protects the microbe from phagocytosis c. Increases the release of toxins and enzymes d. Prevents replication of the bacterium 4. Microbial mutation means that: a. Genetic information has changed. b. Pathogens become nonpathogens. c. The microbe survives adverse conditions but can no longer replicate. d. The immune response to that microbe is strengthened. 5. A bacterial endospore can: a. Also be classified as an acid-fast bacterium. b. Exist in latent form inside a host cell. c. Reproduce very rapidly. d. Survive high temperatures and a dry environment. 6. The structure of a virus includes: a. A cell wall membrane b. Metabolic enzymes for replication c. A protein coat and either DNA or RNA d. A slime capsule and cilia 7. What method do viruses use to replicate? a. Binary fission b. Budding of a daughter cell from the parent viral cell c. Producing reproductive spores d. Using a host cell to produce and assemble components 8. A retrovirus such as HIV contains: a. RNA and enzymes for its conversion. b. A double strand of DNA. c. Many enzymes to limit budding of new virions. d. Numerous mitochondria. 9. How do antiviral drugs act? a. They interfere with cell wall development. b. They decrease cell membrane permeability. c. They destroy new, immature viral particles. d. They reduce the rate of viral replication. 10. Which statement applies to yeasts? a. They are usually considered to be pathogenic. b. They seldom contain a distinct nucleus. c. They may cause opportunistic infection in the body. d. They are normally not found in large numbers in resident flora. 11. Fungi reproduce by: (Select all that apply) a. Budding b. Extension of hyphae c. Binary fission d. Production of spores 12. Which of the following is NOT classified as a protozoan agent of disease? a. Plasmodium vivax b. Trichomonas vaginalis c. Tinea pedis d. Entamoeba histolytica 13. Which of the following is a characteristic of rickettsia? a. It is a very small gram-negative intracellular microbe. b. It exists in three forms. c. It causes sexually transmitted disease. d. It reproduces by budding. 14. Entamoeba histolytica is transmitted by which of the following? a. Mosquitoes (bites) b. Inhaling contaminated particles c. Sexual intercourse d. Cysts in feces 15. Which of the following is a characteristic of resident or normal flora (microflora)? a. It exists in all areas of the body. b. Different species inhabit various areas of the body. c. It is of no benefit to the human host. d. It consists only of bacteria. 16. Which of the following is normally considered sterile? a. Urine b. Pharynx c. Distal urethra d. Vagina 17. The term nosocomial infection means: a. Transmission involves an insect or animal host. b. Acquired in a hospital or medical facility. c. Transmitted by a fomite. d. Apread by direct contact with secretions from an open lesion. 18. Transmission of microbes by direct contact includes: a. Touching a contaminated countertop. b. Sexual intercourse. c. Drinking contaminated water. d. Inhaling dust-borne microbes. 19. What does the term carrier mean? a. A person with active infection who acts as a reservoir for microbes b. Animals, insects, objects, or surfaces contaminated by pathogens c. An individual who is contagious through infected secretions on the hands d. An asymptomatic person whose body harbors pathogens and can transmit them to others 20. Opportunistic infection may develop when: a. Pathogens enter the body but cannot colonize the site of entry. b. An imbalance occurs in the normal resident flora. c. Host resistance increases, and the balance of resident flora is restored. d. Contaminated food or water is unknowingly ingested. 21. Host resistance is promoted by all of the following EXCEPT: a. Prescribed immunizations. b. Chronic respiratory disease. c. Vitamin and mineral supplements. d. Appropriate inflammatory or immune response. 22. Which of the following factors would NOT increase the virulence of a specific microbe? a. Secretion of endotoxin b. Presence of a bacterial capsule c. Production of interferons d. Secretion of invasive enzymes 23. That time in the course of an infection when the infected person may experience a headache or fatigue and senses he or she is “coming down with something” is referred to as which of the following? a. Subclinical period b. Eclipse period c. Prodromal period d. Presymptomatic period 24. The principle of Universal Precautions is based on: a. Using disinfectants at all times to eliminate cross-infections. b. Not touching any open or bleeding lesions. c. Sterilizing all instruments and equipment after each use. d. Assuming that all body fluids from all individuals are possible sources of infection. 25. The “incubation period” refers to the time period between: a. Entry of the pathogen into the body and the first signs of infectious disease. b. The onset of the prodromal period and the peak of the acute infection. c. The onset of clinical signs and signs of recovery from infection. d. The acute period and establishment of chronic infection. 26. What does “bacteremia” refer to? a. Numerous pathogens circulating and reproducing in the blood b. Uncontrolled sepsis throughout the body c. Multiple infections, primary and secondary, established in the body d. Microbes present in the blood 27. Which of the following is a local sign of infection? a. Fever and leukocytosis b. Headache and anorexia c. Pain, erythema, and swelling d. Nausea, weight loss, and fatigue 28. What are culture and sensitivity tests used for? a. To determine the type of microbe present in an exudate b. To provide a specific medium that supports maximum microbial growth c. To identify the causative microbe and the effective antimicrobial agent for it d. To provide living host cells for microbes requiring such for replication 29. A broad-spectrum bactericidal agent would be expected to: a. Destroy many gram-positive and gram-negative bacteria. b. Destroy all pathogenic microbes in contact with the agent. c. Reduce the replication of many bacteria. d. Inhibit the growth of most spores and acid-fast bacteria. 30. How does penicillin act as a bactericidal agent? a. It interferes with cell-wall synthesis. b. It blocks protein synthesis. c. It increases cell membrane permeability. d. It prevents DNA replication. 31. Secondary infection may occur with administration of antibacterial drugs because the: a. Patient is allergic to the drug. b. Balance of species in the resident flora is upset. c. Mucosa of the stomach is irritated. d. Infecting microbes spread to adjacent areas. 32. All of the following are mechanisms of antiviral drug action EXCEPT: a. Interference with attachment to host cell. b. Block assembly of viral particles. c. Interference with mitosis. d. Shedding of protein coat. 33. Secondary bacterial infections occur frequently during influenza epidemics primarily because: a. Antiviral drugs lower host resistance. b. The virus causes extensive tissue inflammation and necrosis. c. Respiratory droplets transmit infections. d. The viral infection is usually self-limiting. 34. The primary pathological effect of influenza virus is: a. Destruction of the mucosa in the lower respiratory tract. b. Replication of the virus in respiratory secretions. c. Destruction of leukocytes and macrophages in the lungs. d. Inflammation and necrosis of the upper respiratory epithelium. 35. What does leukocytosis frequently indicate? a. Immunosuppression b. Bone marrow damage c. Presence of bacterial infection d. An allergic or autoimmune reaction 36. When an infection or inflammation is suspected, what does leucopenia often indicate? a. Bacterial infection b. Viral infection c. Allergic reaction d. Septicemia 37. Which of the following statements applies to Chlamydia? a. The microbe exists as a chain of cells. b. It causes a common STD. c. It possesses many flagella. d. It is excreted in feces. 38. Which of the following microbes is classified as an obligate intracellular parasite? a. Fungus b. Bacterium c. Virus d. Protozoa 39. Which of the following are characteristics of influenza virus? (Select all that apply) a. It is an obligate intracellular parasite. b. It contains RNA. c. It usually causes nausea and vomiting. d. There are three subtypes: A, B, C. 40. The widespread necrosis of respiratory mucosa caused by an influenza infection often gives rise to: a. Severe anemia b. Secondary infections c. Asthma d. Emphysema 41. Prions cannot be cultured in a PETRI plate of media because: a. They take so long to grow. They block the invasion of pathogenic bacteria. b. They require extensive amounts of specialized nutrients. c. They are proteinaceous particles, not living organisms. d. They are viruses that don’t grow on conventional media. 42. Which of the following statements applies to Influenza A H1N1? a. It alters human chromosomes to cause manifestations. b. It usually causes severe respiratory distress and high fever. c. Infection is common in the elderly. d. It contains genetic material from avian, swine, and human viruses. 43. Which of the following does NOT directly determine the virulence of a microbe? a. Capacity for opportunism b. Production of toxins c. Ability to mutate d. Invasive qualities 44. Which of the following is a function of interferons? a. They block the invasion of pathogenic bacteria. b. They reduce the inflammatory response to local infection. c. They increase host cell resistance to viral invasion. d. They may facilitate the spread of some cancer cells. 45. Inflamed tissue is likely to become infected because: a. The immune system is not effective in inflamed tissue. b. The increased fluid and protein in the inflamed area supports microbial growth. c. Phagocytes cannot penetrate the inflamed areas. d. Capillaries are less permeable in the affected area. 46. When an infectious disease is occurring globally at a higher rate than usual, it may be designated as a/an: a. Sporadic occurrence b. Epidemic c. Pandemic d. Emerging disease 47. Which of the following is the primary difference between an antiseptic and a disinfectant? a. Antiseptic is used on living tissue, whereas disinfectant is designed for nonliving surfaces. b. Antiseptic is much stronger than the potency of a disinfectant. c. Antiseptic often causes allergic skin reactions, whereas disinfectant is always hypoallergenic. d. Antiseptic is effective against endospores; disinfectants are not effective against endospores. 48. Drugs that are designed to inhibit or slow down growth of microbes but not necessarily kill them are considered: a. Ineffective b. Bacteriostatic c. Narrow-spectrum d. Bactericidal Chapter 7 1. Neutrophils: a. Are phagocytic cells b. Produce histamine c. Produce antibodies d. Are elevated during an allergic response 2. Which cells are required to process and present antigens from foreign material as the initial step in the immune response? a. T–helper cells b. Macrophages c. Eosinophils d. Monocytes 3. Humoral immunity is mediated by: a. Natural killer cells b. T lymphocytes (T cells) c. B lymphocytes (B cells) d. Neutrophils 4. A secondary immune response differs from the primary immune response in that: a. It is more rapid than the primary response and results in higher antibody levels. b. It is slower than the primary response and doesn’t change the antibody levels. c. It occurs at the same time as the primary response but results in a decrease in antibodies. d. It only occurs in hyperallergic reactions and results in a decrease of antibodies. 5. Which type of immunity is provided by a vaccination? a. Active natural b. Active artificial c. Passive natural d. Passive artificial 6. When an allergen binds with IgE antibodies on mast cells, resulting in release of chemical mediators, this reaction is called: a. Cytotoxic hypersensitivity b. Immune complex hypersensitivity c. Type I hypersensitivity d. Type IV hypersensitivity 7. The role of memory cells is to: a. Change into an antibody-secreting cell following activation. b. Immediately secrete antibodies following the first exposure to antigen. c. Recognize the antigen and stimulate the immune response. d. Bind complement to the antibody. 8. Which statement applies to contact dermatitis? a. It occurs when IgE antibodies on the skin react with the causative substance. b. It may result from ingested foods. c. Urticaria (hives) gradually spread over the body. d. A type IV reaction occurs in affected areas. 9. Which of the following causes anaphylaxis? a. A severe, systemic allergic reaction b. Type III hypersensitivity c. Cell-mediated hypersensitivity d. Immune complex deposits in many tissues 10. Following a positive HIV antibodies blood test and ELISA test, what is the test commonly used for confirmation? a. Agglutination b. Double immunodiffusion test c. Western blot test d. Sedimentation rate test 11. Incompatible blood transfusions result in: a. Hemolysis of erythrocytes. b. A type I immune response. c. Deposits in multiple organs. d. Immune deficiency. 12. An autoimmune disease is: a. Excessive formation of antibodies following exposure to foreign material. b. An extreme response to normally harmless material in the environment. c. An abnormal response to ingested food and drugs. d. Failure of the immune system to distinguish self from nonself. 13. Systemic lupus erythematosus is caused by: a. A chronic allergic condition. b. Development of an immune-deficient state. c. A deficiency of T lymphocytes. d. Immune complex deposits of antinuclear antibodies. 14. Distinguishing clinical features of systemic lupus erythematosus include: a. Inflammation in multiple organs. b. Lack of a specific diagnostic blood test. c. Acute onset and nonprogressive course. d. Typical skin rash on the chest and back. 15. Which of the following are the target cells for HIV? a. Helper T lymphocytes (CD4 lymphocytes) b. B lymphocytes c. Natural killer cells d. Macrophages 16. A diagnosis of HIV positive means that: a. The number of T lymphocytes in the circulating blood is decreased. b. Significant opportunistic infection is present in the body. c. The individual has AIDS. d. The virus and its antibodies are present in the blood. 17. HIV infection impairs: a. Humoral immunity b. Cell-mediated immunity c. Both humoral and cell-mediated immunity d. Neither type of immunity 18. Immunodeficiencies may result in an increased risk of infections by normally harmless microorganisms. These infections are referred to as: a. Opportunistic b. Prophylactic c. Abnormal d. Transient 19. Serious infections frequently occurring in patients with AIDS include: (Select all that apply) a. Tuberculosis b. Pneumocystis carinii pneumonia c. Influenza d. Tetanus 20. Which of the following statements does NOT apply to major histocompatibility complex (MHC) proteins or molecules? a. They are genes on chromosome 6. b. All members of a family have identical MHCs. c. They alert the immune system to virus-infected cells. d. A close match is essential for successful tissue transplants. 21. CD4-positive helper T cells function by: a. Direct cytotoxic action. b. Facilitating all immune system activity. c. Producing immunoglobulins. d. Inactivating allergens. 22. Host-versus-graft disease refers to: a. Hyperacute rejection of tissue. b. T cells in grafted tissue attacking host cells. c. Infection resulting from immunosuppression therapy. d. Transplant rejection by the recipient’s immune system. 23. Which of the following complications does NOT occur frequently in AIDS patients? a. Kaposi’s sarcoma b. Wasting syndrome c. Lymphoma d. Polyarthritis 24. Which of the following characteristics apply to HIV? (Select all that apply) a. It contains two strands of DNA. b. It tends to mutate frequently to form new strains. c. The incubation period is extremely short. d. It is inactivated by heat and many disinfectants. 25. In cases of HIV infection, the “window period” refers to the time between: a. Entry of the virus into the blood and the initial manifestations. b. Entry of the virus into the body and the appearance of antibodies in the blood. c. Entry of the virus into the body and a significant drop in CD4 T-helper lymphocyte count. d. Diagnosis of “HIV positive” and diagnosis of “AIDS.” 26. Which of the following is an effect of cytokines? They: a. Activate and stimulate proliferation of B and T lymphocytes. b. Destroy antigens quickly. c. Increase the rate of mitosis in tumors. d. Cause immediate pain. 27. What does seroconversion mean in relation to HIV and AIDS? a. The virus has been identified in the blood and body fluids. b. Antibodies for HIV have been identified in the blood. c. HIV was found in lymphocytes. d. Active infection has developed in the patient. 28. Which of the following statements is TRUE regarding a patient who is HIV positive? a. No medication is required until the CD4 cell count drops below normal range. b. Antibodies are present, destroying the virus and preventing transmission to others. c. Antibodies in the blood indicate presence of virus and possible transmission to others. d. Enzymes have not yet converted RNA to DNA for replication. 29. The term tolerance refers to: a. Surveillance and destruction of new cancer cells by the immune system. b. The ability of the immune system to ignore “self” cells. c. The ability of T and B lymphocytes to work together. d. The role of lymphoid tissue in the body defenses. 30. Which of the following statements applies to the complement system? a. It is activated by IgE. b. It blocks the inflammatory response. c. It consists of proteins in the blood that must be activated. d. It may destroy antibodies in the circulation. 31. Which of the following statements regarding immunoglobulins is TRUE? a. They consist of a unique sequence of amino acids. b. They are produced in the red bone marrow. c. They are attached to mucosal membranes at entry points into the body. d. IgA binds to allergens. 32. Which of the following is NOT a cause of immunodeficiency? a. Hypoplasia of the thymus b. Delayed hypersensitivity c. Immunosuppressive drugs d. Atrophy of the lymph nodes 33. Which statement is TRUE regarding infants born to HIV-infected mothers? a. Infants usually test negative for HIV after birth. b. There is little risk of infected mothers passing the virus to their infants during delivery. c. Breast milk does not contain HIV or antibodies. d. Infants test positive for HIV because of the presence of maternal antibodies. 34. The most common cause of death in patients who have AIDS is: a. HIV encephalopathy. b. Tuberculosis. c. Pneumocystis carinii pneumonia. d. Candida infection. 35. Tissue transferred between two genetically identical twins is referred to as a/an: a. Allograft. b. Syngraft. c. Isograft. d. Autograft. Chapter 21 1. Which of the following statements applies to the sex chromosomes? a. They are identified as XY in the female. b. They are numbered pair 23 in the karyotype c. They contain the same genes as in the other pairs of chromosomes. d. They are found only in the cells in the gonads (the ovaries and the testes). 2. What is the term for an arrangement of the chromosomes from an individual’s cell, organized in pairs based on size and shape? a. Pedigree b. Punnett squares c. Karyotype d. Genotype 3. What is characteristic of a congenital disorder? a. Genes are not involved. b. It is strictly a developmental anomaly. c. A cause is known. d. It is usually manifested in the neonatal period. 4. What is the probability of two parents, both carriers of a defective recessive gene, producing a homozygous child (with each pregnancy)? a. 0% b. 25% c. 50% d. 75% 5. In the case of an X-linked recessive disorder, a carrier mother and unaffected father could produce a/an: a. Normal female b. Affected female c. Male carrier 6. Down syndrome is an example of a/an: a. Autosomal dominant disorder b. Multifactorial disorder c. Developmental defect d. Chromosomal defect 7. Agents that cause damage during embryonic or fetal development are called: a. Teratogenic b. Mutagenic c. Multifactorial agents d. Polygenic agents 8. What is an example of a multifactorial congenital disorder? a. Type AB blood b. Down syndrome c. Color blindness d. Cleft lip and palate 9. Ultrasonography during pregnancy would be helpful in detecting fetal: a. Enzyme deficits b. Structural anomalies c. Chromosomal defects d. Hormonal abnormalities 10. Which of the following statements regarding Down syndrome is TRUE? a. The typical physical characteristics are present at birth. b. All children with Down syndrome have the same organ defects and medical problems. c. The extent of cognitive impairment can be assessed at birth. d. The birth of a child with Down syndrome is only a risk to mothers over age 35. 11. Which of the following statements applies to Huntington’s disease? a. The effects are obvious at birth. b. There is a test for the defective gene. c. There is a 50% probability that the child of an affected parent will be a carrier. d. The child must inherit the defective gene from both parents in order to be affected. 12. A mother is a carrier of Duchenne muscular dystrophy; the father is unaffected. They have one son with muscular dystrophy. Another male child is expected. The probability of the second son having muscular dystrophy is: a. 100% b. 50% c. 25% d. 0% 13. Hemophilia A has been diagnosed in a young boy. He has inherited this defective gene from: a. His father b. His mother c. Both parents 14. A father affected with hemophilia A, whose wife is unaffected, will pass on the defective gene to: a. All of his sons, who will be affected. b. 50% of his sons, who will be affected. c. All of his daughters, who will be carriers. d. 50% of his daughters, who will be carriers. 15. Which of the following are common manifestations of Down syndrome? (Select all that apply) a. Congenital heart defect b. Cleft lip and palate c. Large protruding tongue d. Limited intellectual development 16. A spontaneous alteration in genetic material that may result from exposure to harmful substances is termed: a. Autosome b. Genotype c. Meiosis d. Mutation 17. A person with sickle cell trait that is heterozygous has: a. An incomplete dominant gene b. A multifactorial condition c. Co-dominant genes d. X-linked dominant trait 18. TORCH is an acronym for routine prenatal screening tests for high-risk maternal infections; TORCH stands for: a. Toxoplasmosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rubella, cytomegalovirus, and herpes. b. Tuberculosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rabies, cytomegalovirus, and HIV. c. Toxoplasmosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rabies, cytomegalovirus, and HIV. d. Tuberculosis, other (hepatitis B, mumps, rubeola, varicella, gonorrhea, syphilis), rabies, cytomegalovirus, and herpes. 19. Which statement applies to the effects of exposure to harmful substances during embryonic life? (Select all that apply) a. During the first two weeks, exposure will usually cause death of the embryo. b. Organs or body structures may be altered by exposure during the first two months. c. The effects of exposure depend on the stage of development at the time of exposure. d. Metabolic abnormalities usually follow exposure to teratogens. 20. Exposure to cocaine during pregnancy leads to increased risk of: a. Premature birth b. Respiratory problems c. Sudden infant death syndrome (SIDS) d. All of the above 21. Which term refers to prenatal diagnosis through examination of amniotic fluid? a. Chorionic villus testing b. Preparing a family pedigree c. Amniocentesis d. Triple-screen test 22. The laboratory practice of changing DNA sequences in microorganisms is called: a. The genotype b. Gene mutation c. Genetic engineering d. Gene therapy 23. The purpose of the Human Genome Project was to: a. Map the nucleotide sequence and identify the genes on each human chromosome. b. Study the common patterns of inheritance of single-gene disorders. c. Manipulate the sequence of DNA in microorganisms and animals. d. Identify spontaneous alterations in genetic material caused by teratogens. 24. Developmental disorders can result from all the following EXCEPT: a. Exposure to radiation b. Mercury in foods and water c. Drugs and alcohol d. Folic acid 25. Genes located at the same site on a pair of homologous chromosomes that are also matched for function are called: a. Alleles b. Genotypes c. Autosomes d. Phenotypes 26. Which of the following can easily pass through the placental barrier? a. Many viruses b. Some heavy metals c. Certain chemicals d. All of the above 27. The term proteomics refers to the study of: a. DNA sequences with unknown functions. b. Gene sequences in individual chromosomes. c. The proteins resulting from activation of specific genes. d. Identifying certain base pairs in DNA. 28. The most invasive prenatal screening test for fetal abnormalities is: a. Ultrasonography b. Amniocentesis c. X-ray d. Blood tests 29. Which of the following can be detected using amniotic fluid? a. Chromosomal abnormalities b. Metabolic disorders c. Certain structural abnormalities d. All the above 30. Blood tests are performed on neonates primarily to: a. Determine need for immediate surgical correction of anomalies. b. Identify disorders requiring immediate treatment. c. Identify the presence of any inherited disorders. d. Rule out the presence of any infection. 31. When genetic influences combine with environmental factors to cause an abnormality, the result is called a: a. Chromosomal disorder. b. Developmental disorder. c. Multifactorial disorder. d. Single-gene disorder. 32. The cellular division process that produces the chromosomes that are in the sperm and ova is called: a. Meiosis b. Mitosis c. Organogenesis d. Polysomy Chapter 20 1. What is a benign neoplasm originating from adipose tissue called? a. Adenoma b. Lipoma c. Fibrosarcoma d. Adenocarcinoma 2. What are malignant neoplasms arising from connective tissue cells called? a. Carcinomas b. Sarcomas c. Melanomas d. Fibromas 3. Which of the following is a characteristic of a benign tumor? a. It is unencapsulated and invasive. b. It consists of undifferentiated cells. c. It exerts systemic effects. d. Cells appear relatively normal. 4. Which factor provides the basis for the grading of newly diagnosed malignant tumors? a. Size of the tumor b. Number of metastases c. Degree of differentiation of the cells d. Number of lymph nodes involved 5. A warning sign of possible cancer would be any of the following EXCEPT: a. Persistent, unusual bleeding. b. A change in bowel habits. c. Sudden development of fever, nausea, and diarrhea. d. A change in shape, color, or surface of a skin lesion. 6. The common local effects of an expanding tumor mass include: (Select all that apply) a. Obstruction of a tube or duct b. Anemia and weight loss c. Cell necrosis and ulceration d. Tumor markers in the circulation 7. Which of the following does paraneoplastic syndrome refer to? a. The effects of substances such as hormones secreted by the tumor cells b. Severe weight loss and cachexia associated with advanced cancer c. The decreased resistance to infection resulting from malignant tumors d. The effects of multiple metastatic tumors 8. Which term refers to the spread of malignant cells through blood and lymph to distant sites? a. Invasiveness b. Seeding c. Metastasis d. Systemic effect 9. One reason for staging a malignant tumor at the time of diagnosis is to: a. Identify the original cell from which the tumor developed. b. Locate and identify the primary tumor. c. Decide the initiating factor for a particular tumor. d. Determine the best treatment and prognosis. 10. The process of carcinogenesis usually begins with: a. Exposure to promoters causing dysplasia. b. Development of defective genes. c. An irreversible change in the cell DNA. d. A single exposure to a known risk factor causing temporary cell damage. 11. What would be an external source of ionizing radiation? a. A needle containing a radioisotope implanted beside the tumor b. Gamma rays delivered by a cobalt machine c. A dose of a radioactive drug to be ingested d. A fluid containing radioactive material instilled in a body cavity 12. Radiation therapy destroys: a. All cells in the tumor at one time. b. The cells in the center of the tumor. c. Primarily rapidly dividing cells. d. Radioresistant cells. 13. The most critical adverse effects of chemotherapy and radiation therapy are: a. Thrombocytopenia and leucopenia b. Headache and lethargy c. Nausea and constipation d. Alopecia and weight loss 14. Chemotherapy usually involves a combination of drugs in order to: (Select all that apply) a. Reduce the adverse effects. b. Guarantee that all cancer cells are destroyed. c. Be effective in more phases of the cell cycle. d. Totally block the mitotic stage. 15. Why does ovarian cancer have a poor prognosis? a. The ovaries are inaccessible for examination. b. Specific signs rarely appear until after secondary tumors have developed. c. The same tumor markers are present with many types of cancer. d. No effective treatment is available. 16. Select the correct pair representing a malignant tumor and its marker: a. Colon cancer: carcinoembryonic antigen (CEA) b. Hepatic cancer: CA125, AFP c. Prostate cancer: human chorionic gonadotropin (hCG) d. Testicular cancer: Philadelphia chromosome 17. Antiangiogenesis drugs act on a malignant tumor by: a. Promoting the immune response and removal of abnormal tumor cells. b. Blocking hormonal stimulation of tumor cells. c. Reducing blood flow and nutrient supply to tumor cells. d. Transporting radioisotopes into the tumor. 18. The development of neutropenia during chemotherapy for cancer means: a. The cancer cells are being destroyed quickly. b. The patient is likely to hemorrhage. c. Higher doses of chemotherapy could be tolerated by this patient. d. The patient is at high risk for infection. 19. Malignant brain tumors: a. Metastasize quickly to all parts of the body. b. Spread first to lungs and bone. c. Spread to other parts of CNS. d. Do not metastasize anywhere at any time. 20. Identify the common dose-limiting factor for chemotherapy: a. Alopecia b. Bone marrow depression c. Nausea and vomiting d. Weight loss 21. Glucocorticoids are often prescribed during a course of chemotherapy and radiation because: a. Glucocorticoids greatly potentiate the effect of chemotherapy. b. The immune system is stimulated. c. Skeletal muscle atrophy will be decreased. d. Inflammation around the tumor may be reduced. 22. Vomiting frequently follows a chemotherapy treatment because: a. The gastrointestinal tract is irritated. b. The chemicals stimulate the emetic center. c. The drugs have an unpleasant odor. d. A and B 23. What type of normal cells are often damaged during chemotherapy and radiation treatments? a. Epithelial cells b. Skeletal muscle cells c. Nerve tissue d. Collagen and fibrous tissue 24. Remission for cancer is generally defined as a period in which: a. Chemotherapy cannot be used. b. Signs and symptoms are absent. c. Complications are evident. d. Metastases occur. 25. All of the following are correct statements about skin cancers EXCEPT: a. They are difficult to diagnose and treat. b. They usually develop slowly on the head, neck, or back of individuals with fair skin. c. The number of skin cancer cases is increasing. d. Basal cell carcinoma is the most common form of skin cancer. 26. High risk factors for cancer include: (Select all that apply) a. Human papilloma virus. b. Chronic irritation and inflammation. c. Repeated sun exposure. d. High family incidence. 27. The term apoptosis refers to: a. Programmed cell death. b. Abnormal or immature cells. c. Degree of differentiation of cells. d. The development of new capillaries in a tumor. 28. The warning signs for cancer include: a. Unusual bleeding b. Change in a wart or mole (e.g., color) c. A new solid lump, often painless d. All of the above 29. A classification process that applies to a specific malignant tumor and describes the extent of the disease at a given time is called: a. Seeding b. Mutation c. Staging d. Grading 30. Benign tumors can often be differentiated from malignant tumors because benign tumors: a. Often have systemic effects. b. Contain cells showing increased mitosis and atypical rapid growth. c. Are encapsulated and slow-growing. d. Can metastasize or invade nearby tissue. 31. Benign tumors in the brain are often life-threatening because they: a. Metastasize early in their development. b. Create excessive pressure within the skull. c. Cannot be removed. d. Cause serious systemic effects. 32. Drugs or agents that augment the natural immune response in the body to improve identification and removal of abnormal cells are called: a. Biological response modifiers. b. Angiogenesis stimulators. c. Analgesic complements. d. Targeted receptor modifiers. 33. The method that can be used as an alternative to surgical removal of a tumor by using heat generated by a needle inserted into the tumor is referred to as: a. Radiation therapy b. Thermolysis intervention c. Brachytherapy d. Radiofrequency ablation 34. Staging systems used to classify a malignant tumor at the time of diagnosis are based on which of the following factors? a. Size of the tumor, involvement of lymph nodes, metastases b. Location of tumor, size, type of cellular abnormality c. Size, encapsulated or non-encapsulated, invasion into neighboring tissue d. Type of cellular abnormality, size of secondary tumors, location/tissue affected 35. One of the general effects of a malignant cancer is cachexia, which is: a. Severe bleeding b. Severe tissue wasting c. Severe fatigue d. Multiple opportunistic infections [Show More]
Last updated: 1 year ago
Preview 1 out of 26 pages
Instant download
 (1).png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 03, 2021
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
May 03, 2021
Downloads
0
Views
59

.png)