MED-SURG NUR1211 NCLEX Review _ UWORLD,100% CORREC
Document Content and Description Below
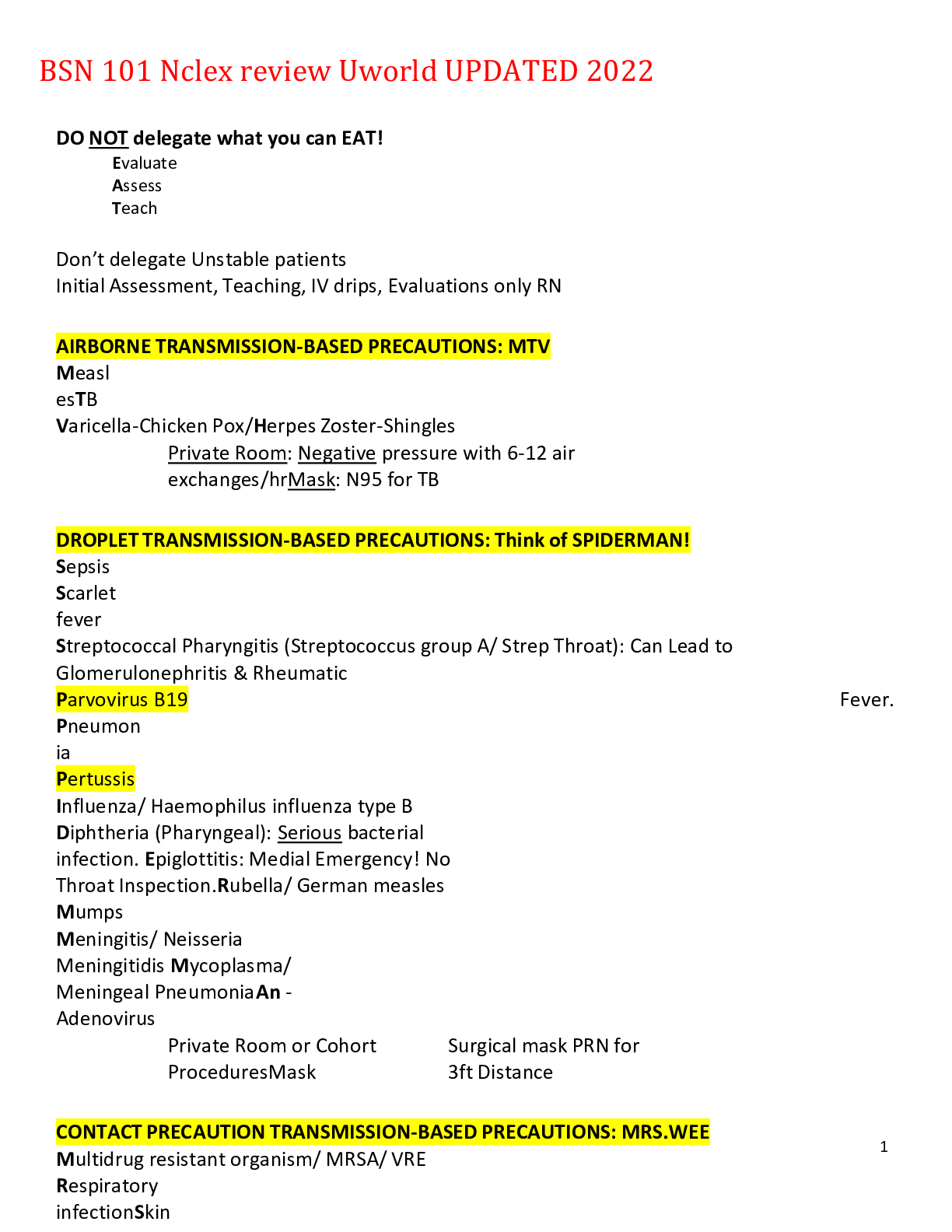
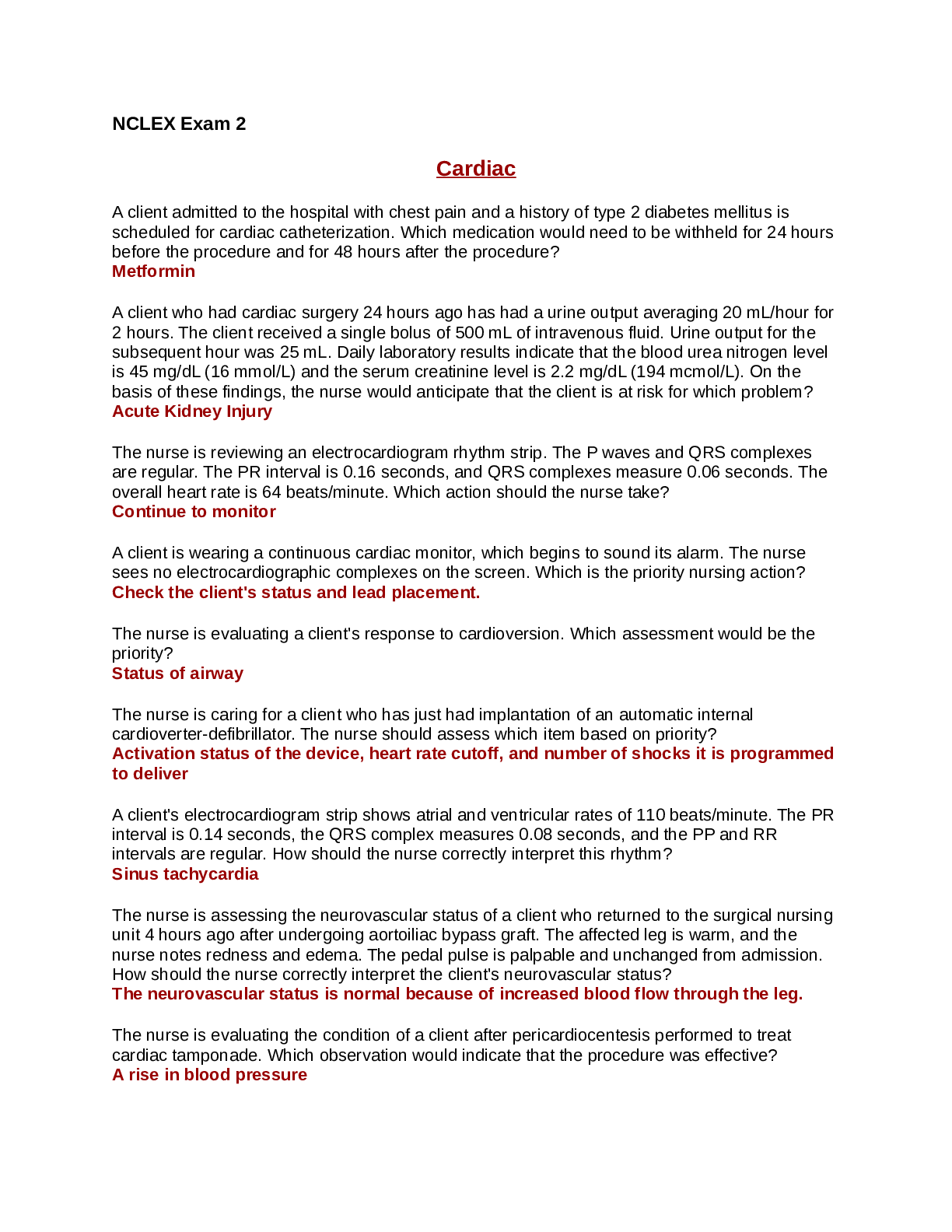
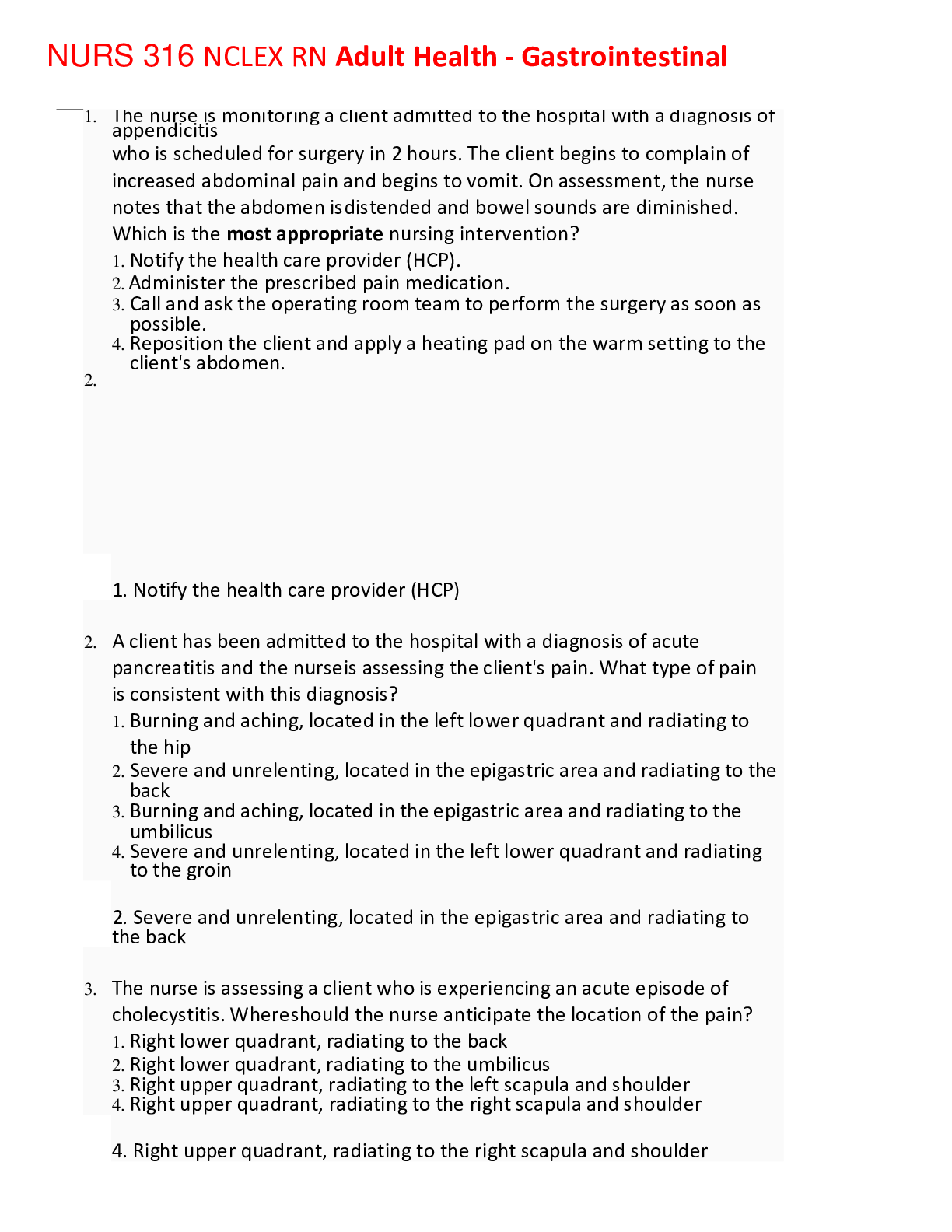
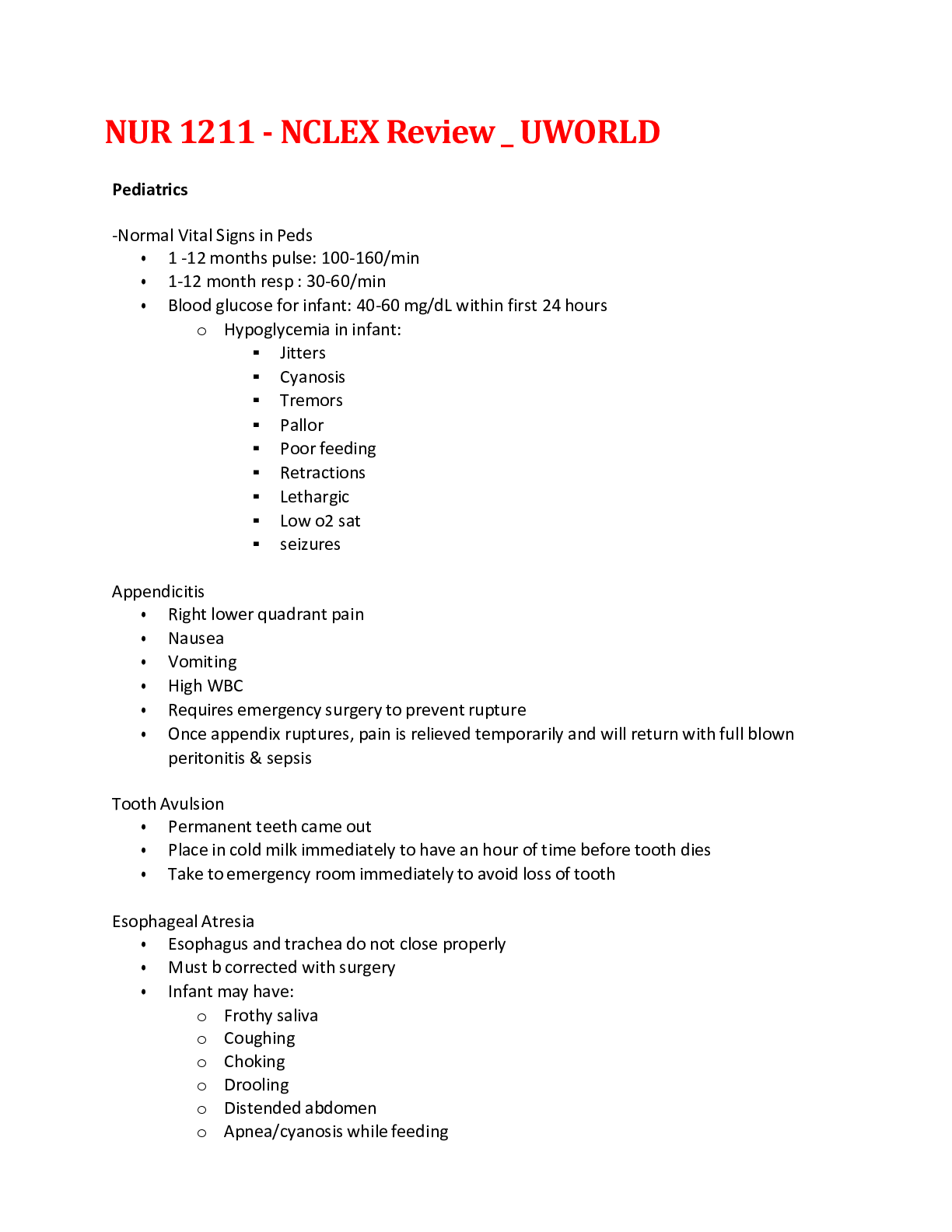
MED-SURG NUR1211 NCLEX Review _ UWORLD Pediatrics -Normal Vital Signs in Peds • 1 -12 months pulse: 100-160/min • 1-12 month resp : 30-60/min • Blood glucose for infant: 40-60 mg/dL with... in first 24 hours o Hypoglycemia in infant: ▪ Jitters ▪ Cyanosis ▪ Tremors ▪ Pallor ▪ Poor feeding ▪ Retractions ▪ Lethargic ▪ Low o2 sat ▪ seizures Appendicitis • Right lower quadrant pain • Nausea • Vomiting • High WBC • Requires emergency surgery to prevent rupture • Once appendix ruptures, pain is relieved temporarily and will return with full blown peritonitis & sepsis Tooth Avulsion • Permanent teeth came out • Place in cold milk immediately to have an hour of time before tooth dies • Take to emergency room immediately to avoid loss of tooth Esophageal Atresia • Esophagus and trachea do not close properly • Must b corrected with surgery • Infant may have: o Frothy saliva o Coughing o Choking o Drooling o Distended abdomen o Apnea/cyanosis while feeding Hypertrophic Pyloric Stenosis • Apnea • Choking • Cyanosis due to aspiration of fluid while eating • Projectile vomiting is CLASSIC manifestation Retinoblastoma • Tumor in childhood • Intraocular malignancy occurring in kids less than 2 • Recognized when parents report white glow of pupil while taking photograph • Absent red reflex • Strabismus is another common sign • Visual impairment is late sign indicating advance disease • Tx: o Radiation o Enucleation (removal of eye) & fit for prosthesis o May be hereditary Neonatal Abstinence Syndrome • Born to opioid dependent mother • Experiences withdrawal 24-48 hrs after birth • Baby is irritiable, jittery, high pitch cry, sneezes, diarrhea, vomit, poor feeding • Place baby in side lying position while swaddled to minimize stimulation • Use pacifier between feedings • Place in quiet, dim lit part of nursery • Tx with opioid therapy Chicken Pox • Airborne spread of secretions and direct contact of open lesions • Most contagious 1-2 before rash and after onset but before crusted lesions • Negative air flow room • Antihistamine for itchy and acetaminophen for fever…no aspirin! Strabismus • Disorder of misalignment of eye from birth defect or acquired weakness • Crosseyed • Common treatment is to wear patch over strong eye; surgery may be required if this is not successful RSV • Common cause of infection in infants and kids • Winter time • Bronchiolar swelling and a lot of mucus • Rhinorrhea, fever, cough, lethargy irritability, poor feeding • Severe causing tachypnea, dyspnea, poor air exchange Treatment: • Supplemental oxygen & suction • Elevate head of bed to improve breathing and secretion clearance • Antipyretics for fever and comfort • IV fluids for dehydration from fever, tachypnea, poor oral intake • Transmitted via direct contact with respiratory secretions; contact isolation required w/ droplet precautions if 3 ft from client • Palivizumab is given IM once monthly during winter/ spring to prevent RSV in kids with high risk CPR in kids • Kids often develop resp distress & bradycardia before cardiac arrest • Perform rescue breathing for 2 min • If pulse still less than 60 with signs of poor perfusion, treat as pulseless; start compressions • Rescue breaths: 1 breath every 3-5 secs / 12-20 breaths/min -Intusuception in 6-36 months: one section of bowel telescopes over another blocking passage of intestinal contents, interrupts blood supply, intestinal tears; EMERGENCY • Inconsolable crying • Drawing up of legs towards abdomen • Stools with mucus & blood (currant jelly stools) • Vomiting • Peritonitis can occur o Fever o Abdominal rigidity o Guarding o Rebound tenderness o Fatal if not treated quickly!! -Hirschprung disease: kid is born with missing nerve cells in large intestine making anal spincter unable to relax o Bilious vomit o Abdominal distension o Failure to pass meconium within 24-48 hrs o Tight anal sphincter o Tx: o Surgical removal of defective section o Colostomy o Complications: o Enterocolitis sepsis and death; fever, lethargy, explosive, foul smelling diarrhea, worsening abdominal distension -ADHD inattentive type o Trouble holding attention; easily distracted o Provide calm, structured, organized, consistent environment o Written chart/list of daily activities helps remind child of what to expect o Helps child organize thoughts o Core symptoms are: o Hyperactivity o Impulsiveness o Inattention o Low self esteem & impaired social skills o Academic or work failure o Trouble interacting with peers -Bed bugs • Can inhabit clean or dirty environments • Travel and spread in clothing, bags, furniture, bedding • Itchy red rash • Must call pest control and exterminate in entire home • Pets and other family members are at risk of bed bugs -Pediculosis capitis (head lice) • Female lice eggs hatch in 7-10 days • Adult lice can not survive away from host head for >48 hours • Nits (baby lice) can live away from host on brushes, carpet and hats for up to 10 days Tx: • Pediculicide (permethrin 1% cream) with nit comb or by hand for 2-3 days for 2 weeks • Carpets, rugs, furniture must be vacuumed often to remove lice/nits and bedding should be washed in hot water and dried in hottest dryer setting • Brush, comb, ornaments soaked in boiling water for 10 min or in lice-killing product for 10 min • Pets do not transmit lice Ventriculoperitoneal shunt • Used to treat hydrocephalus and placed at age 3-4 months • Blockage and infection are complications • Blockage results in signs of increased ICP • Cushings triad can occur (bradycardia, slowed respiration, widened pulse pressure) signs of increased ICP Developmental dysplasia of the hip (DDH) • Risk factors include breech birth, large infant size, family history • Proper swaddle technique: should be swaddled with hips bent up (flexion) and out (abduction) • Infant car seats with wide basis – hips always abducted; avoiding having feet straight together Tetralogy of Fallot • Cyanotic heart defect • Will maintain o2 levels of 65%-85% until surgically corrected • Polycythemia may occur o Normal hgb in 1 month old is 12.5-20.5 o May occur as compensatory mechanism due to hypoxia o Place infant at risk for stroke or thromboembolism • Poor weight gain Normal Finding in Term newborn • Many/deep plantar creases; indicates maturity • Babinski reflex toes hyperextend and fan out when foot is stroked in upward motion; disappears at 1 year; absent Babinski may indicate neurological defect • Epstein pearls are white, pearl like epithelial cysts on gums and palate; disappear in few weeks • Cord should have two arteries and one vein and covered with wharton’s jelly; one artery & one vein is associated with heart/kidney malformation • Jaundice within first 24 hours is pathological; after first 24 hours its physiological jaundice Tonsillectomy/adenoidectomy signs of bleeding • At risk for hemorrhage 14 days after surgery • May lead to airway compromise • Restlessness • Frequent swallowing/clearing of throat • Vomiting of blood • Pallor Signs of Heart Failure in kids • Rapid breathing • Rapid hr at rest • Dyspnea • Activity intolerance (during feedings in infants) • Pale cool extremities • Weight gain • Reduction in wet diapers • Puffy around eyes Phenylketonuria • Inborn error where they lack phenylalanine hydroxylase that converts phenylalanine to tyrosine • Neurologic damage may occur • Low phenylalaline diet needed • Safe range 2-6 for kids less than 12 • Special formula required • Eliminate eggs, meat , milk (high in phenylalanine) • Eat more fruits and veggies (low in phenyl) Epistaxis • Tilt head forward and apply pressure to nose 5-10 min • Apply pressure to nose and hold cold cloth to nasal bridge for vasoconstriction • Keep calm • Never tilt head back to avoid swallowing or aspiration Absence Seizures • Usually occur in kids • Daydreaming/staring spells • Unresponsive • No memory of it • No tonic clonic • No warning Basilar Skull Fracture • Battle sign: bruising behind ear • Blood behind tympanice membraine • Periorbital hematomas (raccoon eyes) • CSF leakage • Requires cervical spine immobilization, monitor neuro, support ABC Autism Spectrum Disorder • Impaired social interaction/behavior • Provide brief, concrete communication that is age appropriate • Caregivers should remain by child • Reduce staff in room/stimulation • Introduce staff/ equipment slowly with caregivers nearby • Limit physical contact until u know what is soothing and what will trigger outburst ICU/ Critical Care Positive end expiratory pressure • Applies pressure at end of expiration during mechanic ventilation • Counteracts small air way collapse & keeps alveoli open • Usually kept at 5 cm H2o but higher levels is good for ARDS • High levels can cause over distension and rupture of alveoli causing barotrauma (10-20 ) to lung o May result in pneumothorax & subcutaneous emphysema -Mechanical Ventilator High Pressure Alarm (obstruction): • Kinked vent tubing • Kinked endotracheal tube • Secretions (obstruction) in tube • Biting endotracheal tube • Excessive secretions in client • Decrease lung compliance (pneumothorax, atelectasis, pulmonary edema, ARDS) • Anxiety, pain, coughing Low Pressure Alarm (leaks): • Tube disconnect or leak • Endo-trach cuff leak • Loss of airway • When getting ABG from client on mechanical ventilator after a ventilator setting change, avoid suctioning the client, administering ABG or reducing amount of sedation as these will all affect the ABG results. After a change in settings, ABG’s are drawn to evaluate how the patient is tolerating it. • Monitor level of sedation; minimum sedation necessary for comfort • Maintain semi-fowler position • Oral care with chlorhexidine & endotracheal suctioning -Chest tubes: to drain air, blood or other fluids • Water seal chamber: o Filled with sterile water & is one way valve preventing air entering chest cavity o Rises and falls with clients inspiration & expiration tidaling which indicates its functioning properly • Suction control chamber: o Usually set at -20 cm H2O o Bubbling occurs when suction is applied • Air leak gauge: o Part of water seal chamber o Assess this for leaks o Continuous bubbling here means air leak in system • Drainage collection chamber: o Fluid from clients pleural cavity will collect here; assess color and amount and record • If chest tube becomes dislodged, a sterile occlusive dressing must be placed over insertion site until health care provider arrives; if one not available, cover with something clean and occlusive to prevent air from entering then reassess; may cause pneumothorax; tape only on 3 sides to prevent tension pneumothorax Cardiac Tamponade: life threatening complication of pericardial effusion where fluid builds up in pericardial sac & compresses heart • Narrowed pulse pressure • Hypotension • JVD • Unable to contract effectively • Cardiac output drops drastically • Muffled or distant heart tones • Pulsus paradoxus • Dyspnea • Tachypnea • tachycardia Tx: emergency pericardiocentesis Bacterial Meningitis: inflammation of the membranes that cover brain and spinal cord; bacterial infection You must: • Assign client to private room • Don mask before entering • Elevate bed only 10-30 degrees • Maintain dim lighting Signs & Symptoms o Headache o Neck stiffness o Nausea o Vomiting o Photophobia o Fever o Altered mental status o At risk for seizure o Requires strict droplet precautions (caused by Neisseria meningitides): surgical mask, private room, client mask during transport Seizure Precautions o Padded bed rails o Oxygen at bed side o Suction equipment at bedside o NO!!! PADDED TONGUE BLADE Increased Intracranial Pressure • ICP should not exceed 25 mm hg • Elevate head of bed to 30 degrees and maintain head in neutral position • Stool softeners to reduce straining • Manage pain • Manage fever/prevent shivers • Maintain calm environment • Adequate o2 • Avoid clustering care • Suction no more than 10 secs Adults Miscellaneous Lab Values • Hematocrit: 39%-50% males; 35%-47% females • Hemoglobin: 13.2-17.3 in male; 11.7-15.5 females • BUN: 6-20 • Creatinine: 0.6-1.3 • Albumin: 3.5-5.0 o Maintains intravascular oncotic pressure and prevents fluid from leaking out vessels o Severe liver disease develop hypoalbuminemia fluid leaks from intravascular space to interstitial causing pitting edema of Lower extrem., periorbital edema, ascites • Potassium: 3.5-5.0 • Calcium: 8.6-10.2 • Platelet: 150,000 – 400,000 • aPTT: 46-70 sec • INR: 2-3 Sec • Hemoglobin A1C: should be <7% Causes of metabolic acidosis • GI bicarbonate loss (diarrhea) • Ketoacidosis (diabetes, alcoholism, starvation) • Lactic acidosis ( sepsis, hypoperfusion) • Renal failure • Salicylate toxicity Meniere disease • Excess fluid accumulation in inner ear • Client may experience: o Vertigo o Tinnitus o Hearing loss o Aural fullness o Reports of being pulled to the ground Central Venous Catheter • Inserted by doctor in central vein ( subclavian, internal jugular, femoral) • Administer fluids, meds, TPN • Disinfect hubs and wash hands • Multiple hubs used to administer incompatible drugs simultaneously, blood draws, hemodynamic monitoring • 10 units/mL OR 100 units/mL heparin are standard of care for flushing CVC Open Angle Glaucoma • Increased intraocular pressure • Loss of peripheral vision (tunnel vision) • Normal central vision • Difficulty with vision in dim lighting • Sensitivity to glare • Halos around bright lights • Can lead to blindness if untreated Guillan Barre Syndrome • Immune-mediated polyneuropathy • Ascending muscle weakness • Absent deep tendon reflex • Hx of respiratory tract or GI infection • Resp failure most life threatening complication o Inability to cough o Shallow respiration o Dyspnea/hypoxia o Inability to lift head or eye brows • Measurement of forced vital capacity is gold standard for assessing ventilation o Decline may indicate impending resp arrest o May require endotracheal intubation Addisons Disease • Adrenocortical insufficiency of adrenal cortex • Addisonion crisis o Life threatening complication of addisons disease o Hypotension & tachycardia o Dehydration o Hyperkalemia & hyponatremia o Hypoglycemia o Fever o Weakness/ confusion • Management o Shock management o Fluid resuscitation w/ 0.9% NS and 5% dextrose o High dose hydrocortisone IV push Pessary • Vaginal device to support bladder • Can remain sexually active while wearing • Client may be able to insert themselves Malignant Hyperthermia • Rare, life threatening inherited muscle abnormality triggered by drugs used to induce anesthesia • Excess release of calcium from muscles leading to muscle rigidity • Hypercapnia, generalized muscle rigidity, hyperthermia • Immediate tx with dantrolene, cool blanket, fluid resuscitation 2nd degree AV block type 2 • more p waves than QRS • rapidly deteriorate to complete heart block = 3 rd degree which is life threatening • assess for bradycardia, hypotension, syncope • get transcutaneous pacemaker Psoriasis • chronic autoimmune causing rapid turnover of epidermal cells • silver plaque on reddened skin on elbows, knees, scalp, lower back, buttocks • no cure; mgmt. includes avoiding triggers like stress, trauma, infection. • Topical therapy like corticosteroids and moisturizers • Phototherapy is good (sunlight) • Systemic meds like cytotoxic methotrexate & biologic infliximab • Avoid alcohol which worsen psoriasis PPD skin test • Screening for TB • Assessed 48-72 hrs after administration • Positive results > 15 mm induration in healthy people; > 10 mm in mild immunosuppression; redness without induration is negative • Sometimes the Calmette-Guerin vaccine from other countries cause false positive • Obtain chest xray Hypoglycemia • Low blood glucose • Serious complication • Epinephrine released during hypoglycemic reaction causing symptoms like trembling, palpitations, anxiety/ arousal, restlessness • Diaphoresis/pallor • If prolonged, confusion, seizure, coma occur Informed Consent • Mentally competent adult; understand procedure, risks, benefits, alternatives, sign voluntarily • Can only give consent if effects of sedation have worn off Venous Thromboembolism • Thrombus forms and embolizes to bloodstream • Risks are venous stasis from prolonged immobility, endothelial damage from surgery, IV catheter placement • Prophylaxis includes: o Anticoagulants o Compression devices o Frequent ambulation 4-6 times daily as tolerated for circulation and venous return o Activate calf muscles with foot/leg exercise o No crossing legs Emphysema • Alveolar wall destruction • Lung tissue recoils/lose elasticity due to enlarged, floppy alveoli • Hyperinflation of lung occurs/ air trapping manifested by hyper resonance on percussion • Prolonged expiration • Barrel chest • Activity intolerance/ anxiety • Tripod position; accessory muscle use; pursed lip breathing Potassium IV administration • Cardiac monitoring • Vesicant; may cause extravasation and tissue necrosis; monitor site frequently • Max infusion rate in peripheral line is 10 mEq/hr/ max concentration is 40 mEq/LL (HIGHER RATES only in central line) • Assess renal function • Always dilute never bolus Blood Transfusions • Do not delay transfusion more than 30 min due to risk of bacterial growth • If it is delayed, send back to blood bank to be refrigerated at precise temp • Transfusions should not be interrupted except with reaction to blood due to increased risk of infection • Transfuse within 4 hours of removal from fridge Thrombolytic Therapy (tissue plasminogen activator tpa) • Dissolves blood clots & restore perfusion in clients with ischemic stroke • Must be given within 3-4.5 hour windw from onset of symptoms • Surgery in past 14 days, coagulation disorders, hemorrhagic stroke, uncontrolled htn, stroke/ head trauma in past 3 months are contraindications Anaphylactic Shock • 20-30 min onset caused by IgE-mediated sensitivity • Results in circulatory failure, laryngeal edema, broncho-restriction Management • Stop infusion and call for help (rapid response) • Ensure patent airway and administer oxygen & prepare for intubation • Give IM epinephrine & maintain BP with normal saline IV Fluid • Administer adjunctive therapies like Benadryl, corticosteroids, or bronchodilator • Reassess vitals EEG teachings • Wash hair to remove oils and accessories should be removed. Hair may need to be washed after to remove electrode gel • Avoid caffeine, stimulants CNS depressants • Not painful MRI • Screen clients for contraindications before exposure to magnetic field to avoid damage to implanted device or metallic implants like: o Cardiac pacemaker o Implanted cardiodefribilator o Cochlear implant o Retained metallic foreign body o Prosthetic heart valve o Verify metal plate, pin, brain aneurysm clip, joint prosthesis o Implanted device insulin pump, medication port • Transdermal patches are not contraindications but should be removed prior to MRI to avoid burns; replace after testing Alcoholic Cirrhosis/ esophageal varices • Associated with gastritis, clotting abnormalities and esophageal varices that increase risk of bleeding; signs of blood bloss: o Coffee ground emesis from oxidized blood o Hypotension o Tachycardia • Hemodynamic instability: o Hypotension o Decreased urine output o Peripheral constriction o Pallor • Treatment o Esophagogastroduodenoscopy to determine bleeding site o Heat probe or sclerotherapy Cirrhosis • Pt may be given lactulose to decrease intestinal ammonia absorption to avoid and tx hepatic encephalopathy o Encephalopathy occurs when liver does not detox ammonia leading to mental status change or death o Lactulose to ensure 2-3 soft stools per day o Sweet breath - fetor hepaticus Paralytic Ileus • Non-mechanical intestinal obstruction that can occur after surgery • Absent or hypoactive bowel sounds due to lack of bowel motility/peristalsis • Abdominal distension • Nausea due to accumulated gas and fluids in bowel Hospice Care • Assists clients who have terminal illness to improve quality of life through comfort measures • Medicare benefit usually provided in client’s home, hospice inpatient unit or skilled nursing facility • Must have 6 months or less to live • Curative tx not allowed but if clients condition improves or client chooses additional tx to cure disease, they may be discharged from hospice Hospital-Acquired Pressure injuries -Risk Factors: • Advanced age • Impaired sensation • Nutritional deficits o Decreased albumin level: (3.5-5); decreased prealbumin: (16-35) o Anemia o Decreased intake/weight loss • Perfusion/oxygenation deficits • Skin moisture Facilitating airway clearance (Pneumonia) • Hydration; fluids, oral intake (2-3 L per day) humidification • Huff coughing technique: used to raise secretions from lower to upper airway for excretion • Chest physiotherapy: percussion, vibration, postural drainage • Fowlers position: promotes lung expansion Abdominal Aortic Aneurism • Blood-filled bulge in abdominal aorta caused by weakening in vessel wall due to increased pressure • Risk factor: o Male o Age >65 o Coronary artery & peripheral vascular disease o HTN o Family and smoking history • Signs may include: o Acute-onset abdominal pain radiating to back o Hemorrhagic shock symptoms: decreased systolic pressure, weak pulse, pallor o May indicate impending rupture life threatening hemorrhage • Monitor for kidney injury after abdominal aneurysm repair o Hypotension, dehydration, prolonged aortic clamping during surgery, blood loss, embolization can lead to injury o Monitor BUN and creatinine and urine output o Should be at least 30 mL/hr Hypokalemia • Muscle cramps • Weakness • Paralysis • And talks with leg muscles Gout • Inflammatory condition caused by ineffective metabolism of purines which causes uric acid accumulation in blood • Forms in joints • Risk factors: o Obesity o HTN o Dyslipidemia o Insulin resistance o Poor diet o Alcohol consumption o Sedentary life style • Uric acid control will be done with: o Weight loss o Increase fluid intake to eliminate uric acid o Low-purine diet; avoid organ meats and sardines, shellfish o Limit alcohol intake; beer especially o Healthy low fat diet o Allopurinol works to prevent gout attacks not treat acute; may need ibuprofen or colchicine Pharmacologic Nuclear Stress Test • Uses vasodilators to simulate exercise when clients can’t tolerate continuous physical activity ot target hr isn’t achieved with exrcise • Used in clients suspected with coronary artery disease • Used radioactive dye Pre-Procedure: • Do not eat, drink, smoke on day of test (NPO for at least 4 hours) • Avoid caffeine for 24 hrs • Avoid decaffeinated products too may have trace amounts of caffeine • Don’t take theophylline • Hypoglycemia may occur if they take insulin since not eating • Do not take these cardiac meds: o Nitrates o Dipyridamole o Beta blockers Pneumothorax • Hyperresonance to percussion • Diminished breath sounds • Decreased tactile vocal fremitus • Hypotension; decreased venous return • Tracheal deviation • Mediastinal shift towards left side • Increased respiratory effort • Respiratory distress • Low o2 sat • Altered loc due to decreased o2 to brain Thoracentesis • Complications are pneumothorax • Bleeding SIADH: too much ADH is produced causing: • Water retention • Increased total body water • Dilutional hyponatremia (low serum Na) Causes are: • CNS disruption • Malignancies • Drugs • Pulmonary disorders Thyroid Storm • Life threatening condition that may occur in uncontrolled hyperthyroidism when stressful incident occurs • Rapid onset of fever • Tachycardia • Elevated BP • Anxious, tremulous, restless • Rapid tx necessary Diverticular Disease • Sac like protrusions that happen because of extra intraabdominal pressure like strain, lift, tight clothes, constipation • The sacs may get infected causing diverticulitis • Tx with NPO to rest bowel • IV for hydration while NPO • Pain relief IV to maintain NPO • No straining • Avoid laxative/enemas IV Lines in Mastectomy Patients • Insert IV in most distal site on unaffected site • Signs above bed for precautions • No bp on affected arm Mastectomy o Immediately after, place in semi fowler with arm elevated on pillows to promote drainage and prevent lymph pooling Near Drowning Hypothermia • Airway management; patent airway possible mechanical ventilation • Continuous cardiac monitoring in vase of v fib which may occur with frequent handling of patient • Rewarming IV fluids • Cover in warm blankets; remove wet clothing and replace with dry clothing Myasthenia Gravis • Neuro autoimmune disorder involving damaged acetylcholine receptors at neuromuscular junction • Initial symptoms ocular ptosis, weak facial muscle, muscle for chewing and swallowing • May progress to weak resp muscles • Tx with pyridostigmine which inhibits acetylcholine break down to temporarily increase muscle strength in clients with MG • Infection, undermedication, stress can precipitate life-threatening myasthenic crisis o Oropharyngeal/ respiratory muscle weakness o Respiratory failure o This needs immediate intervention Urine Specimens • Must be collected aseptically from port on catheter tubing not from collection bag • Clean collection port with alcohol swab • Aspirate with sterile syringe • Use aseptic technique to transfer to specimen cup Peripheral Arterial Disease • Hais loss • Thick, brittle nails • Gangrene • Sool, dry, shiny skin • Intermittent claudication (ischemic muscle pain) • Reduce blood flow because of atherosclerotic plaque For good bone healing: • Adequate nutrition • Adequate circulation • Age Ventricular Trigemeny • PVC occur every 3rd heart beat Percutaneous Coronary Intervention • Stent placement • Increased risk for retroperitoneal hemorrhage signs: o Hypotension o Back pain o Flank ecchymosis o Hematoma formation o Diminished distal pulses Sickle Cell Crisis • Inadequate oxygenation or hydration exacerbates sickling • RBC clumps together causing vasoocclusion ischemic pain, hypoxia, organ dysfunction if untreated • Priority is fluids because RBC cannot carry enough oxygen even with supplemented oxygen if not rehydrated Total Parenteral Nutrition • Glucose is primary component • Monitor for signs of hyperglycemia: polyuria, polydipsia, headache, blurry vision • Hyperglycemia may lead to seizures, coma, or death; treat immediately • If not available asap when ran out, use dextrose in water until ptn available Colostomy Care • Make sure appliance opening fits well around the stoma to prevent skin irritation • Do not change appliance too frequently as it also causes irritation; change every 5-10 days • Encourage fluids to prevent dehydration • Avoid gas forming stools like beans, onion, broccoli • Empty when 1/3 full; to avoid leaking or pulling on skin from heaviness Ulcerative Colitis • Inflammation/ ulcerations in large intestine • Urgent/ bloody diarrhea • Abd pain • Fever • Fatigue • Hyperactive bowel sounds Psych Psychomotor Retardation • Clinical symptom of major depressive disorder • Slowed speech, decreased movement, impaired cognitive function • Movement impairment • Downcast gaze • Lack of facial expression • Downcast gaze • Speech impairment: reduced voice volume, slurred speech, delayed response • Reduced/no interaction Seratonin Syndrome • Caused by excessive serotonin intake • Mild symptoms like shivering and diarrhea • To severe muscle rigidity, fever, seizures • Fatal if not treated • Taking st john wort with other antidepressant may cause this Neuroleptic malignant syndrome: uncommon life threatening adverse reaction to anti-psychotic medications • High fever • Muscular rigidity • Altered mental status • Autonomic dysfunction Tx: • Supportive care including rehydration • Cooling body temperature • Immediate discontinuation of medication Extrapyramidal Symptoms • Acute dystonia reaction: sudden onset, sustained muscle contraction • Akathisia: restlessness w/ inability to stay still • Parkinsonism: tremor, rigidity, bradykinesia, masked face • May treat with Benzodiazepine or benadryl Tardive Dyskinesia • Involuntary movements after chronic use o Lip smacking o Choreoathetoid movements Electroconvulsive Therapy • Induces seizure with electrical currents to the scalp • Treats mood disorders like major depression, bipolar and schizophrenia • Client should be NPO 6-8 before tx except water • Anesthesia and muscle relaxant given; client is unconscious & will not feel pain • Driving not permitted • Temporary memory loss and confusion during immediate recovery • Do not have anticonvulsant med before therapy • Post treatment nurse must: monitor vitals, ensure patent airway, assess mental status, reorient patient Schizophrenia • Types of impaired thought processes seen in schizophrenia individuals: • Neologisms: made up words or phrases of bizarre nature; may have meaning to client only • Concrete thinking: literal interpretation of data; difficulty with abstract thinking • Loose associations: rapid shift form one idea to the other with no connection or logic • Echolalia: repetition of words • Tangentiality: going from one topic to next w/o getting to the point • Word salad: mix of words/phrases having no meaning except to client • Clang associations: rhyming words in meaningless, illogical manner • Preservation: repeating same words or phrases in response to different questions Bipolar Disorder- acute manic episodes are characterized by: • Excessive psychomotor activity • Euphoric mood • Imbalanced nutrition because wont sit long enough to eat • Poor impulse control • Flight of ideas/ non stop talking • Poor attention span/ distractibility • Hallucinations & delusions • Insomnia • Wear bizarre and inappropriate clothing, jewelery, make up • Neglected hygiene & inadequate nutritional intake Care Plan for manic episode client • Reduce environmental stimuli; one on one interaction • Structured schedule of activities to keep focus • Physical activities to relieve excess energy • High protein, high calorie meal and snacks easy to eat • Setting limits on behavior Social Anxiety Disorder • Excessive fear of social or performance situation • Fear criticism, embarrassment, humiliation, rejection • Pt may sweat, tremble, palpitations, diarrhea, blushing • May experience anticipatory anxiety days / weeks before feared event Risk for Suicide • Client suddenly feels more energetic • Prior attempts/ psych issues • Hopelessness • Alone • Elderly white man • Unemployed/unskilled • Physical illness • Fire arm access • Substance abuse L/D & Woman’s Health Heart Attack signs in women • Atypical symptoms like: o Nausea o Vomit o Belching o Indigestion o Dizzy o Fatigue Tachysystole • More than 5 contractions in 10 min • Adverse effect of oxytocin • Excess uterine contraction can decrease placental blood flow & compromise fetal oxygen • Must decrease/ stop oxytocin and giving IV fluid bolus/ tocolytic drug like terbutaline Meds with teratogenic effects • ACE inhibitors (Lisinopril, enalipril) and ARB (losartan) have black box warnings • Renal and cardiac defects to baby • Labetalol and methyldopa are SAFE to take in pregnancy Back Labor • Client may experience lower back pain w/ contraction when fetus is in right occiput posterior • Right occiput anterior is the best for birthing baby Rubin theory (Phases of postpartum adaptation) • Taking in: 24-48 hours post partum, the mother is more dependant on health care team • Taking hold: 2-10 days postpartum, learning skills of motherhood but may feel inadequate • Letting go: 10 days post partum, mother is comfortable with new role Abruptio Placentae • Possible complication of preeclampsia; life threatening to mom and baby • Placenta tears away from wall of uterus due to stress causing bleeding and deprive baby of oxygen • May require immediate delivery of baby • May be concealed or visible bleeding Placental Previa • Do not perform vaginal examination • Painless vaginal bleeding • Previa is completely or partially covering cervical os Preeclampsia • Manifests with high BP and protein in urine • Edema is present and expected but still should be assess frequently • Complications include eclampsia, placental abruption and HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets • Place on seizure precautions • End organ dysfunction(cerebral/visual symptoms; pulmonary edema; impaired liver dysfunction etc) • Give magnesium sulfate to prevent seizures; cns depressant • Deep tendon reflexes should be assessed o Hyperreflexia/clonus indicates impending seizure o Hyporeflexia is magnesium toxicity • Calcium gluconate available in case of toxicity HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets) • Complication of preeclampsia • Additional lab work needed • If diagnosed, only tx is immediate delivery • Often mistaken for viral gastroenteritis • RUQ pain, nausea, vomiting, malaise Vaginal Hematoma • Trauma to tissues of perineum occurs during delivery • May occur after forceps or vacuum assisted birth or episiotomy • Severe vaginal bleeding/ feeling of fullness • Unchanged bleeding • Uterus is firm and at midline on palpation • Hgb and vital signs change significantly Inversion of uterus • Large, red mass protruding from introitus • Severe pain • Uterus not at midline • Hemorrhage HPV • Associated with genital warts and cervical cancer • Usually asymptomatic; genital warts are painless; can reoccur; treated w/ topical podophyllin, cryotherapy, laser surgery • Prevention with vaccination against HPV before sex from age 9-12 and up to age 26 • Can be spread through skin to skin contact even w/ condoms • Pap done at 21 regardless of sexual history Bishop Score • Assessment & rating of cervical favorability & readiness for induction of labor • Scored 0-3 on: o Consistency o Position o Dilation o Effacement o Station • Nulliparious woman score of > 8 indicated induction will be successful Non-stress Test • Reactive; indicates fetus is well-oxygenated & establish fetal well-being o Baseline hr 110-160/min o Moderate variability 6-25 min o > acceleration in 20 min lasting 15 secs • non reactive; doesn’t meet above criteria Medications • Antibiotics o Prolonged or high dose tx with antibiotics put client at increased risk for oral thrush since normal flora in mouth is reduced giving rise to opportunistic infections • Antidiabetic o Metformin ▪ Manage hyperglycemia in type 2 diabetics ▪ Increases sensitivity of insulin receptors and reduces glucose production by liver ▪ Increases efficacy of insulin already in body • Abciximab o Platelet inhibitors that prevent occlusion of treated coronary arteries during percutaneous coronary intervention procedures and prevent acute ischemic complications o May cause bleeding: ▪ Bleeding at puncture sites ▪ Hypotension ▪ Tachycardia ▪ Changes in heart ryhtym ▪ Blood in urine ▪ Abd/back pain ▪ Mental status change ▪ Black tarry stools o Nursing assessments: ▪ Assess invasive sites for bleeding ▪ Assess baseline CBC ▪ Continuous cardiac monitoring ▪ Report signs of bleeding • Epinephrine o Counteracts the effects histamines released o Dilates bronchial smooth muscles and providing vasocontriction o Most deaths occur from delay of epinephrine administration • Trimenthoprim-sulfomethoxazole (Bactrim) o Sulfonamide antibiotic referred to as sulfa drug o Contraindication include hypersenetivity to sulfa drugs, pregnancy and breast feeding; prescribe alternate antibiotics if possible o Sulfa derived drugs may cause cross sensitivity (sulfonylurea like glyburide and diuretics like thiazides and furosemide which have sulfa) • Nitroglycerin o Vasodilator to treat stable angina o Placed under clients tongue to relieve pain in about 3 min lasting 30-40 min o If symptoms are unchanged or worse 5 min after first dose, call EMS o Store away from light and heat sources to prevent degradation o Keep in original container o Once opened, must be replaced every 6 months as they lose potency • Clozapine o Atypical antipsychotic medication used to tx schizophrenia for clients who has not responded to traditional tx o Risk for agranulocytosis so only used with tx-resistant schizo o Client MUST have WBC of > 3500/mm3 and absolute neutrophil count > 2000/mm3 before starting clozapine; obtain baseline CBC & ANC and checked once a week o Agranulocytosis is reversible if caught early o Contact health care provider if fever or sore throat develops (indication of underlying infection from neutropenia) o seizures o Assess for weight gain, hyperglycemia, dyslipidemia metabolic syndrome • Enoxaparin o Low-molecular weight heparin used to prevent and treat DVT o Administered in deep subcutaneous given in abdomen o Right or left side of abdomen, 2 in from umbilicus o Inch of skin pinched up and insert needle in 90 degree angle • Ketorolac (toradol) o Highly potent NSAID o Nephrotoxic and should be avoided in clients with kidney disease o Avoid giving 2 NSAIDS as once as can be toxic to stomach and kidney • Medications commonly prescribed for open fracture: o Cefazolin: bone penetrating cephalosporin antibiotic active against skin flora; prophylactic before and after surgery to prevent infection o Cyclobenzaprine (flexeril): muscle relaxant given to tx pain associated with muscle spasm o Tetanus/diphtheria toxoid: vaccine given prophylactic to prevent tetanus infection if not up to date or unknown; within last 10 yrs o Ketorolac: nsaid to decrease inflammation/pain o Opioids: for analgesia • Benzodiazepines o Antianxiety drugs o May cause sedation; give at bedtime • Monoamine oxidase inhibitors o For depressive disorders o Eliminate foods with tyramine like aged cheese and processed meats • Digoxin o Cardiac glycoside that increases heart contractility/ slows hr & conduction o HF & AFib patients o Excreted exclusively by kidney o Take apical hr for full minute Early signs of toxicity o Nausea o Vomit Late signs of toxicity o Arrhythmias including heart blocks -azithromycin • Macrolide antibiotic • Can cause prolonged QT interval which can lead to torsades de pointes • Monitor ekg • May cause hepatotoxicity -methotrexate o Antirheumatic drug for rheumatoid arthritis o Can cause bone marrow suppression, hepatotoxicity, GI irritation o Can cause anemia, leukopenia, thrombocytopenia o Low platelet may give signs like petechiae , pupura etc o immunosuppresant -lithium • Mood stabilizer for bipolar affective disorders • Therapeutic index 0.6-1.2 • Thiazide diuretics, nsaids, antidepressant can cause increased lithium levels especially thiazides • Lithium toxicity o Nausea, vomit o Diarrhea, neuro symptoms o Ataxia, sluggish, confusion o Agitation, coarse tremor • Avoid sodium depletion which precipitates toxicity Dabigatran (pradaxa) • Thrombin inhibitor anticoagulant • For a fib thrombotic event prevention • Risk for bleeding Oxybutynin (Ditropan) • Anticholinergic frequently used for overactive bladder • May cause s/e like: o New onset constipation o Dry mouth o Flushing o Heat intolerance o Blurry vision o Drowsy o Decreased sweat production avoid real hot places Heparin & Warfarin • Warfarin takes effect 48-72 hrs & takes several more days to achieve max effect • Overlap of parenteral anticoagulant heparin/warfarin required • Typical overlap is 5 days or when INR is therapeutic • They do not dissolve clots prevent clots; tpa dissolve clots Aripiprazole (abilify) • Atypical antipsychotic acts as dopamine system stabilizer • For agitation & hallucination in client with dementia Donepezil (Aricept) • Prevent alzheimers dementia; does not decrease agitiation • Preventative medication Sildenafil (Viagra) • Treat erectile dysfunction • Cannot be used concurrently with nitrate drugs; causes life threatening hypotension Carbidopa Levodopa • Treats bradykinesia slow movement • Never stop suddenly to avoid akinetic crisis which is complete loss of movement • Prolonged use can result in dyskinesia (spontaneous involuntary movement) • Carbidopa prevents breakdown of levodopa before It gets to brain Sucralfate • Protective layer in GI mucosa providing barrier against stomach acid and enzymes • For stomach/ duodenal ulcers • Give 1 hour before meals and at bed time • Give on empty stomac with glass of water • Give all other meds 1-2 hours before or after this med • Constipation is common s/e SSRI • For major depressive/ anxiety disorders • Well tolerated except for sexual dysfunction • Fluoxetine, paroxetine, citalopram, escitalopram, sertraline Phenytoin • Avoid excess alcohol, sleep deprivation • Do not stop abruptly • Practice good oral hygiene to avoid hyperplasia from phenytoin • Do not take w/ oral contraceptive • Wear medic alert • Therapeutic range: 10-20 mcg • For tonic-clonic seizures • Signs of toxicity: o Horizontal nystagmus o Gait unsteadiness o Slurred speech o Lethargy o Confusion o coma Fondaparinux • Anticoagulant commonly used for deep vein thrombosis & pulmonary embolism prophylaxis after hip/knee replacement or abd surgery • Can not be administered until 6 hours after surgery • NEVER give with epidural in place o Associated with epidural hematoma o Bleeding in epidural space can cause cord compression o Signs of this are severe back pain and paralysis Theophylline • Therapeutic range is 10-20 mcg • Can cause seizures and life threatening arrhythmias • Stay away from cimetidine and ciprofloxacin because they increase serum theophylline levels • Signs of toxicity: o Anorexia o Nausea o Vomit o Restlessness o insomnia [Show More]
Last updated: 1 year ago
Preview 1 out of 57 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 11, 2021
Number of pages
57
Written in
Additional information
This document has been written for:
Uploaded
May 11, 2021
Downloads
0
Views
48