*NURSING > TEST BANK > Advanced Practice Nursing: Essential Knowledge for the Profession 3rd Edition Denisco Test Bank (All)
Advanced Practice Nursing: Essential Knowledge for the Profession 3rd Edition Denisco Test Bank
Document Content and Description Below
Advanced Practice Nursing: Essential Knowledge for the Profession 3rd Edition Denisco Test Bank Chapter1 Introduction to the Role of Advanced Practices Nursing Multiple Choice 1. In which y... ear did the American Association of College of Nursing (AACN) introduced the Doctorate of Nursing Practice (DNP)? a. 2006 b. 2004 c. 2000 d. 2002 TAhNeSA: ABCN introduced the DNP degree in 2004 to prepare advanced practice nurses (APRNs) to meet challenges and standardize practice beyond master’s degree programs. 2. Which of the following is the best explanation for the creation of the Doctorate of Nursing Practice (DNP) degree? a. To compete against master’s degree programs b. To ensure standardized curriculum ensuring independent practice c. To validate APRN’s for financial reimbursement d. To address increasing curriculum requirements of master’s degree programs ANS: D Although all answers are influenced by the DNP core competencies, the DNP program creation in 2004 by the AACN was designed to address curriculum requirements of master’s degree programs. 3. Which of the following was the first recognized area of advanced practice nursing? a. Clinical Nurse Specialist b. Family nurse practitioner c. Pediatric nurse practitioner d. Certified Registered Nurse Anesthetist ANS: D In 1931, the National Association of Nurse Anesthetists (NANA), renamed in 1939 to the American Association of Nurse Anesthetists (AANA) was the first recognized group promoting advanced nursing practice. Agatha Hodgins founded the AANM at Lakeside Hospital in Cleveland, Ohio. 4. Which factor is broadly perceived to solidify and standardize the role of the APNs over the last 25 years? a. Lack of access to health care providers b. Standardized curriculum development c. Payment for services d. Societal forces ANS: B As the evolution of Advanced Practice Nursing advances specific specialties and needs are identified. Through the evolution of organization and standardization these roles have solidified the APN’s role in today’s health care environment. 5. During the formation of early APN roles in anesthesia, which of the following increased demand for access to health care? a. Poverty b. War c. Rural access to care d. Availability of training ANS: B Earliest demand for nursing-provided anesthesia spiked during periods of war when numbers of physicians were inadequate. The earliest records date back to the American Civil War with the administration of chloroform. During World War I in 1917 more than 1000 nurses, some trained anesthetists, traveled into battle. Other factors such as need for rural health care came later in the validation and need for APNs. 6. In 1889, Dr. William Worrall Mayo built and opened St. Mary’s hospital in Rochester, NY. He is known for some of the earliest recruitment and specialized training of nurses in which of the following roles? a. Pediatrics b. Anesthesia c. Obstetrics d. Research and statistics e. Family nursing ANS: B In 1889, Dr. William Worrall Mayo began formally training and recognizing nurse anesthetists. This has been regarded as the earliest training in nurse-provided anesthesia. 7. In 1893, Lillian Wald established the Henry Street Settlement (HSS) House for which purpose? a. Access to health care of rural areas b. Create inner-city nursing awareness c. Provide the disadvantaged access to care d. Establish guidelines for advanced nursing roles ANS: C The HHS was established to provide nursing services to immigrants and low-income patients and their families in Manhattan. As resistance to nurse-provided care grew, standing orders were drafted from a group of Lower East Side physicians thereby circumventing then-existing legal ramifications. 8. The Frontier Nursing Service (FNS) founded in Kentucky in 1925 by Mary Breckenridge initially provided Appalachia with nursing resources and which type of advanced nursing care? a. Pediatric care b. Anesthesia c. Midwifery d. Surgical services ANS: C The original FNS provided nursing services and obstetric services to Appalachian residents. Later working from standard orders developed from their medical advisory committee nurses treated patients, made diagnoses, and dispensed medications. 9. Which organization founded in 1941 under Mary Breckenridge’s leadership merged with the American College of Nurse-Midwives (ACNM) in 1969? a. American Association of Nurse-Midwives (AANM) b. American Nurses Association (ANA) c. Association for National Nurse-Midwifery (ANNM) d. Council of Nursing Midwifery (ANM) ANS: A The American College of Nurse-Midwives (ACNM) formed under the leadership of Mary Breckenridge in 1941 to provide nurse-midwife development and collaboration for midwife development. In 1955, the American College of Nurse-Midwives was formed and the two organizations merged in 1969 after the death of Mary Breckenridge. 10. In a landmark ruling by the Supreme Court as a result of Chalmers-Frances v. Nelson, 1936, what legal precedent was established? a. Nurse anesthesia was allowed under the nurse practice act b. Nurse anesthesia scope of practice included anesthesia c. Nurse anesthesia was legal, if under guidance of a supervising physician d. Only trained nursing professionals could administer anesthesia independently ANS: C The landmark decision from the Chalmers-Frances v. Nelson case set national precedent for the advanced nursing practice role. It proved to be the basis for other cases over the following few decades and established that trained nurses could legally provide anesthesia care under supervision of a physician. 11. The first known establishment of the nurse practitioner role occurred in 1965 at theUniversity of Colorado. In which area of training did this role specialize? a. Pediatrics b. Geriatrics c. Midwifery d. Anesthesia ANS: A The establishment of the first pediatric nurse practitioner program was in 1965 at the University of Colorado. Loretta Ford, RN and Henry Silver, MD provided a 4-month course to certified registered nurses to provide education on managing childhood health problems. 12. The DNP program curriculum outlined which of the following clinical requirements in an effort to standardize training? a. 1000 supervised clinical hours and 200 unsupervised clinical hours b. 1000 supervised clinical hours c. 900 supervised clinical hours d. 800 supervised clinical hours and 200 unsupervised clinical hours ANS: B In 2004, the AACN outlined the DNP curriculum in an effort to standardize and relieve challenges of master’s degree programs. This includes a standardized curriculum requiring 1000 supervised clinical hours. 13. Which state became the first to recognize diagnosis and treatment as part of the scope of practice of specialty nurses? a. Idaho b. Oklahoma c. South Dakota d. Maryland ANS: A Idaho Governor Cecil Andrus signed HB 46 and HB 207 into law on February 11, 1971. This amended the states’ nurse practice act making it the first state to officially recognize diagnosis and treatment of specialty nurses. The recognition of the ability to diagnose and treat overcame an initial hurdle toward independent nursing practice. 14. The American Nursing Association (ANA) defines which requirement for the designation of a clinical nurse specialist in any specialty? a. Specialty training certificate b. Successful completion of certification examination c. Masters or doctoral degree d. 1000 hours relevant supervised training e. Two or more years of clinically relevant experience ANS: C In 1980, the ANA specifically outlined criteria for the acknowledgment of clinical nurse specialist training programs. At that time they required graduate level training to become an expert in a relevant specialty area of nursing. Additionally, they must meet any requirements set forth by the specific professional society. Chapter2 The Nurse Practitioner: Historical Perspective on the Art and Science of Nurse Practitionering 1. Which of the following is the primary mission of the National Organization of Nurse Practitioner Faculties (NONPF)? a. Provide leadership in promoting quality NP education b. NP Faculty training program assistance c. Provide financial assistance to NP students d. Lobbying legislature on behalf of NPs ANS: A The NONPF’s primary mission is to provide leadership in promoting quality NP education. The organization has published domains and core competencies for primary care and these serve as a framework for NP education and practice. 2. A model of competencies that are encompassed around three spheres of influence known as patient, nurses and nursing practice, and organization and influence is known as? a. NACNS Model of clinical nurse specialist competencies b. Fenton’s and Brykczynski’s Expert Practice c. Calkin’s model of Advanced Nursing Practice d. Shuler’s Model of NP Practice ANS: A The NACNS’s initial 2008 statement was revised in 2004. The statement outlined competencies that aligned to each of the three spheres of influence: patient, nurses and nursing practice, and organization and influence. 3. Building upon Benner’s seven domains of expert nursing practice, which conceptual model adds an additional domain “The consulting role of the nurse”? a. Calkin’s model of Advanced Nursing Practice b. Fenton’s and Brykczynski’s Expert Practice c. Strong Memorial Hospital’s Model of Advanced Nursing Practice d. Shuler’s Model of NP Practice e. NACNS Clinical Nurse Specialists Model ANS: B Fenton’s and Brykczynski’s Expert Practice Domains of the CNS and NP expanded on Benner’s seven domains adding consultation provided by CNS’s to other nurses and management of health and illness in ambulatory care settings. 4. Which model of conceptual practice was the first to explicitly distinguish the experience level of advanced practitioners? a. Calkin’s model of Advanced Nursing Practice b. Shuler’s Model of NP Practice c. NACNS Clinical Nurse Specialists Model d. Strong Memorial Hospital’s Model of Advanced Nursing Practice e. Fenton’s and Brykczynski’s Expert Practice ANS: A Calkins model of Advanced Nursing Practice was the first to explicitly distinguish experience levels of advanced practitioners for nurse administrators to differentiate advanced practice nursing from other levels of clinical practice. 5. The circular and continuous threads of direct comprehensive patient care, support of systems, education, research, and publication and professional leadership make up the five domains of which advanced nursing conceptual model? a. Strong Memorial Hospital’s Model of Advanced Nursing Practice b. Calkin’s model of Advanced Nursing Practice c. NACNS Clinical Nurse Specialists Model d. Fenton’s and Brykczynski’s Expert Practice e. Shuler’s Model of NP Practice ANS: A Direct and indirect activities across five domains including: direct comprehensive patient care, support of systems, education, research, and publication and professional leadership make up the Strong Memorial Hospital’s Model of Advanced Practice Nursing. 6. Texas Children’s Hospital Transformational Advanced Professional Practice (TAPP) APRN Model added what unifying conceptual strand? a. Ethics b. Culture c. Informatics d. Education ANS: A The TAPP model added two additional domains: quality and safety, and credentialing and regulatory practice, to the Strong model. It additionally added professional ethics as a unifying conceptual strand. 7. Poghosyan, Boyd, and Clarke (2016) proposed a comprehensive conceptual model including three factors: scope of practice regulations, institutional policies, and practice environments. What was their primary purpose? a. To discourage role ambiguity among CNS providers b. To enhance patient education provided by the APRN c. To maximize NP Contributions to primary care d. To provide educational practice guidelines to enhance NP education ANS: C The 2016 model provided a comprehensive review of literature and described potential factors that affect NP care and patient outcomes. This included scope of practice regulations that often cause barriers for NP provided primary care. 8. Which model of practice intended to impact the NP domain at four levels: theoretical, clinical, educational, and research in 1993? a. Hamric’s model b. Calkin’s model of Advanced Nursing Practice c. Strong Memorial Hospital’s Model of Advanced Nursing Practice d. Shuler’s Model of NP Practice ANS: D Shuler’s Model of NP Practice is a holistic and wellness oriented model that was designed to impact the NP domain at four levels: theoretical, clinical, educational, and research. It is designed to elaborate the NP’s expanded knowledge and skills into medicine including a template for conducting a visit. 9. Which model for APRN practice addresses all four APRN roles: CNS, CRNA, CNM, and NP? a. Calkin’s model of Advanced Nursing Practice b. Hamric’s model c. Strong Memorial Hospital’s Model of Advanced Nursing Practice d. Donabedian Model ANS: B Many models highlight core competencies among specific APRN roles, while others emphasize competencies for hiring managers. At the time of this writing, only the Hamric’s model encompasses all four APRN roles. 10. Which of the following is one of the eight published essentials included in the Essentials of Doctoral Education for Advanced Nursing Practice developed by the AACN in 2006? a. Algorithms for advanced patient care b. Informatics and health care technologies c. Scientific underpinnings of practice d. Liberal education for general nursing practice ANS: C The AACN publishes their national consensus to provide the core elements for nursing curriculum creation. Currently published are Baccalaureate Essentials, Master’s Essentials, DNP Essentials, and Clinical Resources Essentials. Although they are similar in their core approach to education, listed first in DNP essentials is the scientific underpinnings of practice. 11. Which model of conceptualization identifies that health care needs are not met in a system dominated by medical language as a basis for reimbursement? a. Donabedian Model b. Dunphy and Winland-Brown’s Circle of Caring model c. Shuler’s Model of NP Practice d. Calkin’s model of Advanced Nursing Practice ANS: B Dunphy and Winland-Brown’s transformative model (Dunphy, Winland-Brown, Porter, Thomas, and Gallagher, 2011; Fig. 2.12) proposed a circle of caring to encourage medical collaboration and enhance the nursing presence in the health care system. Their model incorporates both strengths of medicine and nursing with process of assessment, planning, intervention, and evaluation, with a feedback loop. 12. Without additional application of conceptual models which model would be best chosen to model the skill level of beginning nurses, experienced nurses, or advanced nurse practitioners with the appropriate level of patient care? a. Dunphy and Winland-Brown’s Circle of Caring model b. Strong Memorial Hospital’s Model of Advanced Nursing Practice c. Donabedian Model d. Calkin’s model of Advanced Nursing Practice ANS: D Calkin’s model of Advanced Nursing Practice outlines skills and knowledge of beginning nurses, experienced nurses, and advance practice nurses as they relate the patient responses for health care problems. 13. The 2005 Donabedian model has been used to evaluate the quality of APRN care using which conceptual outline? a. Assessment, diagnosis, planning, intervention, and evaluation b. Structure, process, and outcome c. Diagnosis and outcome d. Diagnosis, morbidity, and mortality ANS: D The Donabedian model encompasses structure (health care systems and facilities), process (diagnosis, treatment, education), and outcomes. 14. Which of the following are the functions of a conceptualization ofadvanced practice nursing? (Select all that apply.) a. Basis for furthermore development of knowledge b. Articulate professional role identity and function c. Identify specific procedures to provide d. Deliver holistic and collaborative care e. Provide guidelines on billing ANS: A, B, D Conceptual models allow for articulation of professional role identity, provide a basis for furthermore development of knowledge and assist in clinical practice for the delivery of holistic, comprehensive, and collaborative care. Models may assist but in general do not provide assistance with clinical decision making or billing. Test Bank Multiple Choice 15. A registered nurse completes an informal education and training course at his or her place of work authorizing him or her to use ultrasound guided imagery when placing intravenous lines. How is this best classified? a. Advanced practice nursing b. Nursing Skill Advancement c. Advanced Licensure d. Advanced Certification ANS: B The addition or advancement of individual skills to the nursing practice is common and encouraged but does not meet the requirements set forth for advanced practice nursing. Licensure and certification were not obtained or expressed. 16. The core foundations of all APN education curricula contain advanced courses covering which of the following? a. Human anatomy, health and physical assessment, and pharmacology b. Pathophysiology, research, and pharmacology c. Health and physical assessment, pathophysiology, and obstetrics and gynecology d. Pathophysiology, health and physical assessment, and pharmacology ANS: D While specific specialties may focus on individual areas of clinical knowledge, all aspects of advanced practice nursing include advanced knowledge of pathophysiology, health and physical assessment, and pharmacology. 17. Which of the following criteria is required for the attainment of classification as an advanced practice nurse (APN)? a. Practice focused on research b. Baccalaureate degree in area of focus c. Specialized skill attainment d. Graduate degree in area of focus ANS: D The three basic criteria or qualifications for APNs include graduate education in advanced practice nursing role, national certification in an advanced role, and a practice focused on patients and their families. Research and skills are components of core competencies of advanced practice nurses who achieve a graduate level of education. 18. Which of the following is the central, core competency for advanced practice nursing? a. Evidence-based practice b. Direct clinical practice c. Leadership d. Ethical decision making ANS: B Direct clinical practice is the core competency that lends itself to all others. It also provides the foundation for APNs to carry out the other competencies adequately. 19. The legal authority granted to a professional to provide and be reimbursed for health care services refers to: a. Certification b. Scope of practice c. Practicing Role d. Education ANS: B Many things including state and federal laws define scope of practice. The APN NCSBN defines scope of practice as characterized by specialization, expansion of services provided, including diagnosing and prescribing, and autonomy to practice. An individual certification would fall under the umbrella of scope of practice. 20. Which of the following most accurately describes the current four established advanced practice nurse roles? a. RN, BSN, MSN, DNP b. CNM, FNP, CNS, CRNA c. CNM, FNP, AGNP, PNP d. CNS, CRNA, NP, CNM ANS: D The four established advanced practice nurse roles include CNS, CRNA, CNM, and NP. FNP and AGNP are specializations of nurse practitioners (NP). 21. Which advanced practice nursing role has seen the largest expansion of growth and is currently the largest in number? a. CNS b. CRNA c. CNM d. NP ANS: D Nurse practitioner continues to be the largest in number of APN roles. According to the American Academy of Nurse Practitioners National NP Database there are over 220,000 trained NPs. 22. Which advanced practice nursing role is currently the smallest in number? a. CNM b. NP c. CNS d. CRNA ANS: A The CNM role according to the American College of Nurse-Midwives currently has around 11,000 trained providers based on current estimates. The CNM role is specialized in the care of women’s health and childbearing. 23. A practicing, certified CNM wishes to change roles and work as a family nurse practitioner (FNP). Which of the following is required? a. Complete education and training as an NP b. Take the FNP board examination c. Nothing is required d. Apply for immediate reciprocity ANS: A The four roles of APN (CNS, CRNA, CNM, and NP) are not interchangeable without additional training and education. Although there are specific instances of overlap, each of the four roles should not be confused as interchangeable. Specialty certifications under the NP role may allow for more flexibility under today’s regulations and are not standard practice. Scenarios are usually handled on an individual basis. 24. True or False. A registered nurse in an emergency room successfully completes a critical care course and meets all requirements for certification. He or she is now classified as an advanced practice nurse. a. True b. False ANS: B This registered nurse has completed advanced training that increases skill and knowledge and may have also obtained a certification; however, this does not meet the basic criterion of advanced practice nurse. He or she may be expertly skilled but requires the completion of a graduate degree focused in an area of nursing to appropriately be classified as an APN. The acute care nurse practitioner specialty would be required in this particular setting. Chapter3 Overview of the Doctor of Nursing Practice Degree 1. A registered nurse completes an informal education and training course at his or her place of work authorizing him or her to use ultrasound guided imagery when placing intravenous lines. How is this best classified? a. Advanced practice nursing b. Nursing Skill Advancement c. Advanced Licensure d. Advanced Certification ANS: B The addition or advancement of individual skills to the nursing practice is common and encouraged but does not meet the requirements set forth for advanced practice nursing. Licensure and certification were not obtained or expressed. 2. The core foundations of all APN education curricula contain advanced courses covering which of the following? a. Human anatomy, health and physical assessment, and pharmacology b. Pathophysiology, research, and pharmacology c. Health and physical assessment, pathophysiology, and obstetrics and gynecology d. Pathophysiology, health and physical assessment, and pharmacology ANS: D While specific specialties may focus on individual areas of clinical knowledge, all aspects of advanced practice nursing include advanced knowledge of pathophysiology, health and physical assessment, and pharmacology. 3. Which of the following criteria is required for the attainment of classification as an advanced practice nurse (APN)? a. Practice focused on research b. Baccalaureate degree in area of focus c. Specialized skill attainment d. Graduate degree in area of focus ANS: D The three basic criteria or qualifications for APNs include graduate education in advanced practice nursing role, national certification in an advanced role, and a practice focused on patients and their families. Research and skills are components of core competencies of advanced practice nurses who achieve a graduate level of education. 4. Which of the following is the central, core competency for advanced practice nursing? a. Evidence-based practice b. Direct clinical practice c. Leadership d. Ethical decision making ANS: B Direct clinical practice is the core competency that lends itself to all others. It also provides the foundation for APNs to carry out the other competencies adequately. 5. The legal authority granted to a professional to provide and be reimbursed for health care services refers to: a. Certification b. Scope of practice c. Practicing Role d. Education ANS: B Many things including state and federal laws define scope of practice. The APN NCSBN defines scope of practice as characterized by specialization, expansion of services provided, including diagnosing and prescribing, and autonomy to practice. An individual certification would fall under the umbrella of scope of practice. 6. Which of the following most accurately describes the current four established advanced practice nurse roles? a. RN, BSN, MSN, DNP b. CNM, FNP, CNS, CRNA c. CNM, FNP, AGNP, PNP d. CNS, CRNA, NP, CNM ANS: D The four established advanced practice nurse roles include CNS, CRNA, CNM, and NP. FNP and AGNP are specializations of nurse practitioners (NP). 7. Which advanced practice nursing role has seen the largest expansion of growth and is currently the largest in number? a. CNS b. CRNA c. CNM d. NP ANS: D Nurse practitioner continues to be the largest in number of APN roles. According to the American Academy of Nurse Practitioners National NP Database there are over 220,000 trained NPs. 8. Which advanced practice nursing role is currently the smallest in number? a. CNM b. NP c. CNS d. CRNA ANS: A The CNM role according to the American College of Nurse-Midwives currently has around 11,000 trained providers based on current estimates. The CNM role is specialized in the care of women’s health and childbearing. 9. A practicing, certified CNM wishes to change roles and work as a family nurse practitioner (FNP). Which of the following is required? a. Complete education and training as an NP b. Take the FNP board examination c. Nothing is required d. Apply for immediate reciprocity ANS: A The four roles of APN (CNS, CRNA, CNM, and NP) are not interchangeable without additional training and education. Although there are specific instances of overlap, each of the four roles should not be confused as interchangeable. Specialty certifications under the NP role may allow for more flexibility under today’s regulations and are not standard practice. Scenarios are usually handled on an individual basis. 10. True or False. A registered nurse in an emergency room successfully completes a critical care course and meets all requirements for certification. He or she is now classified as an advanced practice nurse. a. True b. False ANS: B This registered nurse has completed advanced training that increases skill and knowledge and may have also obtained a certification; however, this does not meet the basic criterion of advanced practice nurse. He or she may be expertly skilled but requires the completion of a graduate degree focused in an area of nursing to appropriately be classified as an APN. The acute care nurse practitioner specialty would be required in this particular setting. Chapter4 Emerging Roles for the DNP Nurse Educator Test Bank Multiple Choice 25. In 1990, Cooper and Sparacino postulate than an APRN’s maximum potential may not be attained until: a. After 1 year b. After 7 years c. After 3 years d. After 5 years ANS: D Studies have shown that the first-year position of an APRN is one of transition, and Cooper and Sparacino estimate that an APRN’s maximum potential may not be attained until after 5 years or more in practice. 26. An NP student is performing a thorough neurologic examination for the first time in the clinical setting. This is an example of: a. Role implementation b. Role acquisition c. Role confusion d. Role conflict ANS: B The changes occurring during role transitions experienced during the educational component of an APN role are classified as role acquisition. Additionally, role transition is described as when an APRN begins to practice for the first time in a new role. 27. A new NP student is completing a rotation at an outpatient urgent care clinic and completes an examination on a patient with chest pain. The nursing assistant hands a 12-lead ECG to the NP student and asks: “What should we do?” The NP student’s preceptor did not provide clear instructions on the role of the NP student at this time even though the student is capable of interpreting ECGs. This is an example of: a. Role ambiguity b. Role transition c. Role strain d. Role supplementation ANS: A Role ambiguity is created by unclear expectations, diffuse responsibilities, and uncertainty of subroles. The NP student’s preceptor did not provide clear roles to the NP student about what he or she should do in the absence of the preceptor. If the NP student was placed in a role where he or she was unaware of how to interpret ECGs this would be an example of role incongruity. 28. An NP is completing the first month in his or her first job. He or she receives a phone call from an administrator telling him or her that he or she will need to see 30% more patients starting next week. He or she is told that this is the minimum requirement of all NPs in the same position. The NP has difficulty using the electronic health record (EHR) software efficiently and feels overwhelmed. This is an example of: a. Role supplementation b. Role ambiguity c. Role conflict d. Role insufficiency ANS: D Role insufficiency is often seen as APRN graduates’ transition to the workforce or change positions. This may include feelings of inadequacy or slow speed due to the new role or barriers such as electronic health record documentation requirements. 29. Which of the following is an example of role acquisition? a. NP student learning leadership roles in the classroom b. NP student on graduation day from his or her program c. NP student beginning a new job as a family nurse practitioner d. A practicing NP advancing central line skills ANS: A The changes occurring during role transitions experienced during the educational component of an APN role are classified as role acquisition. All of the others are examples of role implementation. 30. The changes occurring as an APRN performs procedures during job duties are classified as? a. Role supplementation b. Role transition c. Role implementation d. Role acquisition ANS: C The job duties and responsibilities performed by the APRN are an example of role implementation. Role transition is the transition from student to practicing NP. 31. Which of the following is best classified as roll stress? a. Maintaining family responsibilities while in school b. An APN’s feelings of poor self-esteem c. Starting a first job as an NP d. Multiple failed attempts to master a procedure during education ANS: A There are many examples of role stress. Role stress may include any situation that requires increased performance above and beyond the expectation of others. This is easily classified as examples of things that require additional demand in addition to school or work such as work/family responsibilities or keeping up with new and advancing technologies. Starting a first job as an NP is an example of role transition. 32. Which of the following is best classified as role strain? a. A difficult disagreement with a physician b. An APN’s feelings of poor self-esteem after failing two examinations c. Maintaining family responsibilities while in school d. Starting a first job as an NP ANS: B Role strain is defined as the subjective feeling of frustration, tension, or anxiety in response to role stress. Examples of role strain typically include subjective feelings of decreased self-esteem when performance is below the expectations of self or others. A difficult disagreement with a physician is an example of role conflict. Starting a first job as an NP is an example of role transition. Maintaining family responsibilities while in school is an example of role stress. 33. Which of the following is an example of role conflict? a. Difficult work-life balance b. A difficult disagreement with a physician c. Starting a first job as an NP d. Maintaining family responsibilities while in school ANS: B Role conflict occurs when role expectations are perceived to be mutually exclusive or contradictory. Role conflict does not have to be with superiors but can occur between APRNs and nurses, other APRNs, or physicians. Starting a first job as an NP is an example of role transition. Maintaining family responsibilities while in school is an example of role stress. 34. The four-stage process to NP role development first identified by Anderson, Leonard, and Yates (1974) and validated by Roberts et al. (1997) included which four components? a. Finding a niche, coping with pressures, feeling competent, internalizing the role b. Complete dependence, developing competence, independence, interdependence c. Novice, developing competence, competent, advanced d. Developing competence, partial independence, complete independence, interdependence e. Dependence, independence, interdependence, role model ANS: B Complete dependence, developing competence, independence, and interdependence are the four- stage process of NP development outlined by Anderson, Leonard, and Yates in 1974 and validated by Roberts et al. (1997). 35. A trained nurse enters the first semester of an NP training program. He or she is required to learn new and more advanced techniques beginning with conducting an advanced physical examination. The overwhelming feeling and stress of learning additional skills is most likely classified by the studies of Anderson, Leonard, and Yates in 1974 as: a. Independence b. Developing competence c. Interdependence d. Complete dependence ANS: D The initial learning of skills and additional techniques experienced by NPs in the beginning of their training has been described as complete dependence. 36. A trained NP is working at an outpatient care clinic. He or she encounters a difficult patient, is unaware of treatment options, and consults one of his or her colleagues for advice. This is best classified as: a. Independence b. Interdependence c. Developing competence d. Complete dependence ANS: B As initially defined by Anderson, Leonard, and Yates in 1974, NP roles as they transition to the workplace as seasoned practitioners transition to interdependence as they work with colleagues to enhance patient care. 37. Fleming and Carberry’s research in 2011 studied two cohorts of critical care nurse advanced practice trainees in Scotland. They found that transition occurred in which four areas? a. Complete dependence, developing competence, independence, interdependence b. Developing competence, partial independence, complete independence, interdependence c. Coping with pressures, feeling competent, internalizing the role, leading others d. Finding a niche, overcoming obstacles, advanced practice, interdependence e. Finding a niche, coping with pressures, feeling competent, internalizing the role ANS: E Fleming and Carberry’s research in 2011 studied two cohorts of critical care nurse advanced practice trainees in Scotland showing transition occurred in four areas: finding a niche, coping with pressures, feeling competent, internalizing the role. 38. A strategy to promote role acquisition in school that involves a ceremony at the beginning of the NP students training is the best example of: a. Role rehearsal b. Creating a support network c. Role development d. Developing clinical knowledge of skills ANS: A Role rehearsal may include many facets including a rite of passage such as a ceremony to mark the beginning of a new training program. 39. Which initial strategy would provide the best role acquisition for a student or potential student about to begin a new NP program? a. Provide case scenarios of patients that may be encountered b. Preadmission testing c. Provide a handout detailing the APRN curriculum d. Clinical faculty mentoring by preceptors ANS: C An initial strategy for role acquisition includes components for role rehearsal. Providing the overall framework for the APRN curriculum would allow for the best-case scenario of role acquisition. Clinical faculty mentoring by preceptors is an example of role acquisition but is best suited to develop clinical knowledge and skills. 40. Which of the following is the best strategy for transition of an APRN into a new position? a. Ensuring adequate pre-position training b. Development of a structured orientation plan c. Scheduling time-based evaluations d. Providing immediate feedback from supervisors ANS: B APRNs in new roles regardless of previous experience benefit most from structured orientation plans, networking with peers, appropriate mentors and preceptors, and an understanding of appropriate expectations. 41. Which three major purposes are categorized and can be utilized to facilitate role acquisition of NPs in school? a. Knowledge expansion, skill practice, creation of a supportive network b. Role rehearsal, development of clinical knowledge and skills, creation of a supportive network c. Role acquisition, role rehearsal, creation of a supportive network d. Knowledge foundation development, development of clinical skills, tracking outcomes ANS: B An adaptation of Brykczynski’s (2000) “Strategies to promote NP role acquisition in school” allows for specific strategies for role acquisition to be categorized into three major purposes: role rehearsal, development of clinical knowledge and skills, and creation of a supportive network. 42. Which of the following examples would best enhance the development of clinical knowledge and skills as part of role acquisition of the NP? a. Establishment of a peer support system b. Clinical conferences c. Identifying a role model d. Subscription to APRN journals and conferences ANS: B Role acquisition strategies include three major purposes: role rehearsal, development of clinical knowledge and skills, and creation of a supportive network. Establishment of clinical conferences to discuss clinical experiences with faculty and peers can promote clinical understanding and enhance the development of clinical knowledge and skills. Subscription to APRN journals and conferences would establish a pattern for continuing education and help create a support network. Establishment of a peer support system would also help create a support network. Identifying a role model or mentor would facilitate role rehearsal. 43. A faculty member at an NP education program has identified that students are experiencing difficulty with role rehearsal during the first few semesters of the program. Which of the following strategies would likely enhance role rehearsal and facilitate role acquisition? a. Subscription to APRN journals and conferences b. Identifying a role model c. Clinical conferences d. Establishment of a peer support system ANS: B Role acquisition strategies include three major purposes: role rehearsal, development of clinical knowledge and skills, and creation of a supportive network. Identification of a role model or mentor and developing a mentee relationship that can be maintained throughout an APRN program is an excellent strategy to promote role rehearsal and support role acquisition while in school. Clinical conferences support developing clinical knowledge and skills. Establishment of a peer support system or subscriptions to APRN journals help create a support network. 44. In 2010, researchers Sullivan-Bentz et al. used Brown and Olshansky’s four-stage transition model to study recent NP graduates as they undergo role transition to practicing NPs. What did the study demonstrate? a. New NPs transitioned from feeling overwhelmed to feeling confident in 6 months only with support networks b. New NPs did not transition from feeling overwhelmed to feeling confident in the study c. New NPs transitioned from feeling overwhelmed to feeling confident in 1 year only with support networks d. New NPs transitioned from feeling overwhelmed to feeling confident in 1 year e. New NPs transitioned from feeling overwhelmed to feeling confident in 6 months ANS: D APRN role development processes have been supported by a number of studies identifying that the first year is most likely to be observed as the transition from feeling overwhelmed to feeling confident. 45. A questionnaire study conducted by Hart and Macnee (2007) at two national NP conferences found that 51% of NPs perceived that they were only somewhat or minimally prepared for actual practice. Which of the following would most likely facilitate the role transition issues for a beginning NP? a. Clinical NP residency program b. Additional time requirement as a practicing registered nurse c. Longer NP education program d. Additional NP clinical training hours ANS: A As many studies have shown the role transition issues of APRN graduates, clinical residency programs have been developed to address these issues. Clinical residency programs ease new graduate transition into practice and increase NP retention and overall satisfaction. Chapter5 Influencing and Leading Change in the Complex Health Environment : The Role of the Advanced Practice Nurse Multiple Choice 46. A nurse develops an interest in more effective medication management and seeks additional training to enhance his or her daily care of patients and for peers at the facility for which he or she works. This is an example of: a. Specialization b. Subspecialty c. Specialty d. Advanced practice nursing ANS: A Specialization involves focusing on practice in a specific area derived from the field of professional nursing. Specialties can be further characterized as nursing practice that intersects with another body of knowledge, has a direct impact on nursing practice, and is supportive of the direct care provided to patients by other registered nurses (American Nurses Association [ANA], 2010a). If the nurse changed his or her focus of practice this could be considered a specialty. 47. A nurse develops an interest in effective medication management and seeks additional training. The nurse then focuses the majority of his or her time on medication management aspects of nursing. This is an example of: a. Advanced practice nursing b. Subspecialty c. Specialization d. Specialty ANS: D The term specialty suggests that the focus of practice is limited to parts of the whole (ANA, 2010b). Since this nurse has refocused his or her care entirely on medication management as part of the nursing role it is considered a specialty. 48. A registered nurse is planning to extend his or her education beyond baccalaureate education into an advanced practice role. When choosing between CRNA, CNM, and NP these are delineations of which type? a. Reasoning b. Subspecialty c. Specialty d. Specialization ANS: C The term specialty suggests that the focus of practice is limited to parts of the whole (ANA, 2010b). Deciding on advanced practice nursing among CRNA, CNM, and NP requires knowledge that they are independent specialties. Specialties of NP at the highest level are psychiatric and mental health, pediatrics, and adult-gerontology. Subspecialties further differentiate the focus of practice such as family practice nurse practitioner, adult-gerontology nurse practitioner, and acute care among others. 49. A student is evaluating a program to attend. He or she finds an adult-gerontology nurse practitioner program that will also prepare him or her as a hospitalist. How is the hospitalist training best defined? a. Specialty b. Subspecialty c. Reasoning d. Specialization ANS: B Subspecialization further delineates the focus of practice. In subspecialty practice, knowledge and skill in a delimited clinical area is expanded further. Examples of subspecialties include diabetes care, acute care, pain management, and clinical transplant coordinator. 50. Which of the following most accurately describes the four stages in the evolution ofadvanced practice nursing? a. Interest occurs, specialty begins, specialty organizes, and pressures mount for standardization b. Specialty begins, specialty organizes, laws require standardization, maturity, and growing interprofessionalism c. Specialty begins, specialty organizes, pressures mount for standardization, maturity, and growing interprofessionalism d. Interest occurs, specialty begins, specialty organizes, and specialty matures ANS: C The four stages in the evolution of advanced practice nursing include: stage I: specialty begins, stage II: specialty organizes, stage III: pressures mount for standardization, and stage IV: maturity and growing interprofessionalism. 51. An adult-gerontology nurse practitioner works to enhance education for polypharmacy in elderly patients through the creation of standardized education tools. The NP works with other professionals at his or her facility to research and develop criteria for education and practice. This example is best classified as which stage? a. Specialty organizes b. Specialty standardizes c. Specialty begins d. Specialty matures and grows interprofessionally ANS: C Specialty stages are not concrete, but specialties that are in the beginning of development are in stage I: specialty beginning. Stage II: specialty organization is typically considered when a professional organization of like-minded individuals is officially formed. 52. A clinical transplant coordinator works with many aspects of the patient transplant process. Two national organizations currently provide education and preparation for certification of nurses. Which stage of organization is this specialty? a. Stage IV b. Stage II c. Stage I d. Stage III ANS: B The clinical transplant coordinator is currently a stage II specialty as it organizes and begins plans for standardization of care. 53. A national specialty committee is formed for a specific nursing specialty. This is an example of what stage of evolution of advanced practice nursing? a. Stage II: specialty organizes b. Stage I: specialty begins c. Stage IV: specialty matures d. Stage III: specialty standardizes ANS: A As national organizations form around specific specialties they are considered to be in stage II of the evolution of advanced practice nursing. 54. Two organizations are formed for a specific advanced practice nursing specialty. As interest in the specialty grows, legislation is required to govern aspects of care. To answer this call, the organizations must meet what stage of evolution of advanced practice nursing? a. Stage I: specialty begins b. Stage IV: specialty matures c. Stage III: specialty standardizes d. Stage II: specialty organization ANS: C As pressures mount for standardization, often for curriculum development or legislative pressure, standardization of practice must be obtained. This is often a difficult and lengthy process of stage III of the evolution of advanced practice nursing. 55. Hospitalist practice by advanced practice nurses are in significant need. What stage of development is hospitalist practice? a. Specialty standardizes b. Specialty begins c. Specialty matures and grows interprofessionally d. Specialty organizes ANS: B Hospitalist practice is a relatively new field for advanced practice nursing and has yet to be organized. Hospitalist practice is a stage I specialty. 56. Which of the following specialties is classified as stage II, organized but yet to be standardized? a. Wound and Ostomy Nursing b. Interventional Pain Specialist c. Advanced Diabetes Manager d. Clinical Transplant Coordinator ANS: D The clinical transplant coordinator is currently a stage II specialty as it organizes and begins plans for standardization of care. Wound and Ostomy nursing and Interventional Pain Practice are both stage III specialties. Advanced Diabetes manager and Genetics Advanced Practice are stage IV specialties. 57. As first addressed in 1985 at Surgeon General’s workshop on Violence and Public Health, the need for which specialty began? a. CRNA b. Forensic Nursing c. Public Health Nursing d. Wound and Ostomy Nursing ANS: B The need for Forensic Nursing specialty was first addressed in 1985 at Surgeon General’s workshop on Violence and Public Health. 58. Wound and Ostomy nursing, through the WOCNS, offers four levels of care providers. This organization is currently in what stage of evolution of advanced practice nursing? a. Specialty organizes b. Specialty begins c. Specialty standardizes d. Specialty matures and grows interprofessionally ANS: C The WOCNS offers four levels of WOC specialty nurse training and has been developing curricula and education that are offered in postbaccalaureate and some graduate-level programs. 59. Although not required for practice, the AAPM offers a credentialing examination requiring at least 2 years of pain management experience prior to examination for Interventional Pain Practice. This organization’s efforts to standardize care classify as what stage of evolution of advanced practice nursing? a. Stage I b. Stage II c. Stage IV d. Stage III ANS: D The AAPM offers two credentialing examinations: diplomate and fellow. This allows for initial standardization of practice in chronic pain management and paves for care as the organization begins to mature along with the Interventional Pain Specialist specialty. 60. What specialty has two levels of certification available, focused on the management of diabetes and prescribing medications? a. Diabetes and Wellness Specialty b. Endocrine Specialty c. Advanced Diabetes Manager d. Diabetes Clinical Specialist ANS: C The American Association of Diabetes Education (AADE) offers two levels for the specialty of Advanced Diabetes Manager: Certified Diabetes Educator (CDE) and Board Certified Advanced Diabetes Manager (BC-ADM). Specifically, the BC-ADM focuses less on education and moreon the management of diabetes and prescribing of medications. 61. A father and mother have been identified as carriers of cystic fibrosis, a genetic disease. Their primary care provider suggests they obtain genetic counseling prior to starting a family. Which provider is the best for this couple? a. Pediatric nurse practitioner b. Pediatric Physician c. Genetics Specialty RN d. Genetics advanced practice nurse ANS: D The Genetics advanced practice nurse is a specialty that requires a graduate degree. This stage IV specialty ensures specialized training in genetics. These practitioners offer genetic counseling, case management, consultation, and evaluation of patients and their families. An RN would only offer information or identify the need for referral to a genetics specialist. A Pediatric nurse practitioner or Pediatric physician would likely not have specialized training in genetic counseling. Chapter6 Interprofessional Collaboration for Improving Patient and Population Health Knowledge Multiple Choice 62. Which metric is key for validating the need for the role of the Nurse-Midwife (NM) worldwide? a. Infant mortality b. Number of OBGYN Physicians c. Average distance to nearest obstetric center d. Number of births per capita ANS: A Infant morbidity and mortality is a statistic of countries worldwide and is a key driver of expansion of the nurse-midwife role into developing countries. Low- and middle-income countries often have the highest rates of infant morbidity and mortality. Another factor increasing the expansion of the NM’s role is the increasing costs of medical care. 63. Which organization’s primary goal is aiming to become an international resource for APNs and NPs on a global scale? a. ICN’s International Nurse Practitioner/APN Network (INP/APNN) b. American Nurses Association (ANA) c. World Health Organization (WHO) d. Bill & Melinda Gates Foundation ANS: A The INP/APNN’s primary goal is to provide resources to advanced practitioners on a global scale. This includes providing resources to countries and organizations that are forming NP programs. 64. Which three countries were the first to officially establish the NP role? a. Canada, United States, and China b. Canada, United States, and United Kingdom c. United States, Canada, and Australia d. United States, Canada, and Jamaica ANS: D The United States was the first country to establish the NP role in 1965, followed by Canada and Jamaica in the mid-1970s. 65. According to a 2014 study, nurse-midwives who obtain the appropriate education and who are regulated to meet ICM competencies for practice and care can deliver what percentage of midwifery care? a. 87% b. 79% c. 73% d. 93% ANS: A The UNFPA 2014 study showed that nurse-midwives who obtain the appropriate education and who are regulated to meet ICM competencies for practice and care can deliver 87% of midwifery care. 66. Which three countries were the first to officially establish the clinical nurse specialist (CNS) role? a. United States, Canada, and Netherlands b. Canada, United States, and China c. United States Canada, and United Kingdom d. United States, Canada, and Australia ANS: C The CNS role was first introduced in the United States, Canada, and the United Kingdom in the 1960s due to increasing complexity and specialization of health care as well as increased demand for clinical expertise, education, and leadership. 67. Which role was first developed in Australia in 1986 and was formed from the United States’ model of the CNS role? a. Advanced Nurse Practitioner b. Clinical Nurse Advanced Specialist c. Clinical Nurse Practitioner d. Nurse Consultant ANS: D The Nurse Consultant role exists in Australia, the United Kingdom, and Hong Kong. It was first introduced in Australia in 1986 and was modeled after the CNS role in the United States. 68. A nurse in Australia obtains clinical experience and expands his or her knowledge and experience with a master’s degree with a focus on education and training in a specialty area of medicine. He or she most likely obtains which role? a. Clinical nurse specialist b. Advanced Registered Nurse c. Nurse Consultant d. Nursing physician assistant ANS: C In Australia, the Nurse Consultant role varies in requirements from a hospital certificate to a master’s degree. The role has different grade levels and increases responsibilities across five domains. 69. As of the writing of this text, which of the following regions is considered the “next frontier” of APN role development? a. China b. Europe c. Latin America d. Africa ANS: C Latin America is considered the next frontier of APN role development. This region is an area of the world where few such roles exist as of the writing of this text. Development of APN roles in this region is driven by the policies that include: primary health care reform, access to health care, and universal health care coverage. 70. Which of the following strategies is best to support the development of APN roles at the international level? a. Create communities of practice to develop APNs b. Using evidence-based approaches to role development c. Build consensus among stakeholders on health systems solutions utilizing APN roles d. Leverage and share resources for APN education with another country ANS: D While all approaches may be beneficial to support role development, leveraging and sharing resources with another country are most likely to benefit role development internationally. The other options are most beneficial in the development of APN roles at the country level. 71. Which of the following strategies is best to support the initial development of APN roles at the country level? a. Showing support for policies of world organizations to prevent out-migration of nursing leaders and educators b. Collaborating with another country to understand policy decisions c. Joining policy discussions to advocate for the APN role d. Obtaining an advanced nursing practice degree in another country ANS: C The initial development of APN roles at country level is multifaceted. The importance of advocacy for the role to key stakeholders and policymakers is often the first step. The other options are best suited for development at the international level. Chapter7 An Overview of U.S. Healthcare Delivery 72. Which of the following is the most essential component to lead clinical staff and programs effectively as an advanced practice registered nurse? a. Clinical credibility b. Appropriate education c. Years of experience d. Age ANS: A All of the options may attribute to effectively leading clinical staff and programs as an APRN. Direct care is the central competency of advanced practice nursing and excellence in direct care requires clinical credibility to lead other clinical staff. Years of experience or age may or may not be related to direct care. Appropriate education is important for clinical leadership, but clinical credibility requires experience combined with direct care. 73. An advanced practice registered nurse in an outpatient clinic has a phone conference with a cardiologist regarding a patient’s condition. This is an example of: a. Social services b. Point-of-care encounter c. Indirect care d. Direct care ANS: C This is an example of indirect care of clinical practice. Direct care or direct clinical practice refers to those activities and functions that the APRN performs within the patient-nurse interface. 74. Which of the following is considered indirect care? a. Forming a therapeutic relationship during patient examination b. Discharge planning c. Consideration of which medication to prescribe a patient d. Patient education regarding medication side effects ANS: B Indirect care or indirect clinical practice refers to those activities and responsibilities that occur outside of the patient-nurse interface. They may include consultation with other health care providers, discharge planning, care coordination, communication with insurance companies, education or supervision of other medical staff, or billing and coding for services rendered. The other options are examples of direct care. 75. Which of the following is considered direct care? a. Forming a therapeutic relationship during patient examination b. Increasing knowledge of a disease process to better care for a complex patient c. Prior authorization of prescriptions d. Consultant phone call about patient condition ANS: A Direct care or direct clinical practice refers to those activities and functions that the APRN performs within the patient-nurse interface. Examples of direct care include physical acts of diagnosis, monitoring, treatment, or direct patient education that occur in the patient-nurse interface. It can be with the patient or family members. The other options are examples of indirect care. 76. An APRN is preparing a patient to be discharged from an emergency department. Which of the following activities is considered direct care? a. Speaking with the patient’s primary care provider b. Electronically transmitting prescriptions to pharmacy c. Discharge planning documentation d. Discharge patient education ANS: D The decision to discharge a stable patient requires that the APRN evaluated the patient and his or her clinical condition and determined it to be stable; this most likely required direct clinical care including a physical examination and medical decision making and discharge-related patient education. 77. An APRN evaluates and modifies his or her clinical practice routines by reading and following updates and recommendations from various journals and organizations such as the United States Preventative Task Force (USPSTF). Which characteristic of advanced direct care practice is the APRN utilizing? a. Use of reflective practice b. Use of a holistic perspective c. Expert clinical performance d. Use of evidence as a guide for practice ANS: D Using evidence as a guide for practice is one of six characteristics for advanced direct care practice. Reading research reports, searching health care databases, acquiring skills to analyze evidence, and working with colleagues regarding evidence-based improvements in care are all examples of using evidence as a guide for practice. 78. During a patient encounter the APRN remembers the patient mentioned during a previous visit that the patient’s child was applying to colleges. The APRN asks which college the patient’s child chose to attend. Discussing this at the beginning of the patient encounter utilizes what characteristic of advanced direct care practice? a. Formation of therapeutic partnerships with patients b. Expert clinical performance c. Use of a holistic perspective d. Use of reflective practice ANS: A The formation of therapeutic partnerships with patients is one of six characteristics for advanced direct care practice. The APRN is effectively using good conversational style to create a strong therapeutic relationship with the patient. Use of a holistic perspective would only be correct if this conversation was used in relation to the patient’s care. 79. An APRN starts a patient on a specific medication chosen over a compatible medication due to a decreased risk of sedation. The medication was chosen because the patient has an occupation driving a truck. Which characteristic of advanced direct care practice is the APRN utilizing? a. Formation of therapeutic partnerships with patients b. Use of a holistic perspective c. Expert clinical performance d. Use of reflective practice ANS: B Using a holistic perspective includes identifying patterns of symptoms combined with the effect of the individual patient. This may include the patient’s view of his or her own health or the impact that his or her disease or treatments may affect his or her overall quality of life. Expert clinical performance is incorrect because the medication was chosen solely based on the effect of medication side effects on the patient’s social life. 80. An APRN encounters an angry and combative patient during his or her shift. The next day he or she meets and speaks with a colleague involved with the patient to discuss how the department handled the incident as well as his or her personal beliefs regarding the care of combative patients. Which characteristic of advanced direct care practice is the APRN utilizing? a. Use of evidence as a guide for practice b. Expert clinical performance c. Diverse approaches to and interventions for Health and Illness Management d. Use of reflective practice ANS: D The use of reflective practice is an important characteristic of advanced direct practice care. Meeting with colleagues and teachers regarding clinical scenarios are important aspects of reflective practice as you explore personal values, social beliefs, and behaviors. Since the meeting was not regarding evidence-based improvements of care or strategies to improve the outcome of similar patients the other options are incorrect. 81. An APRN works in a critical care environment. He or she identifies a patient he or she believes to be at risk for decompensation and intervenes quickly. Which characteristic of advanced direct care practice is the APRN utilizing? a. Use of evidence as a guide for practice b. Expert clinical performance c. Use of reflective practice d. Diverse approaches to and interventions for Health and Illness Management ANS: B Expert clinical performance is the development of specialized knowledge, experience, and complex situations the APRN will encounter during patient care. Deeply understanding clinical knowledge and interpretation of data are aspects of expert clinical performance. 82. An APRN encounters an angry and combative patient during his or her shift. The next day he or she begins analyzing patient outcomes as they correlate with different treatment modalities. Which characteristic of advanced direct care practice is the APRN utilizing? a. Expert clinical performance b. Use of evidence as a guide for practice c. Use of reflective practice d. Diverse approaches to and interventions for Health and Illness Management ANS: B Systematic reviews of existing journals, health care statistics, and working with colleagues in an attempt to improve outcomes and understand clinical scenarios are examples of excellent use of evidence as a guide for practice. In this scenario the other options are incorrect; the APRN had not just discussed his or her personal beliefs, nor was specifically reviewing patient data for his or her personal knowledge development. 83. An APRN is working in a rural community health center providing community health services to poverty-stricken families He or she works at government agencies and regional medical centers to coordinate care for patients who cannot afford it. At these facilities the APRN gains experience using lower cost strategies to provide effective care. Which characteristic of advanced direct care practice is the APRN utilizing? a. Expert clinical performance b. Use of reflective practice c. Diverse approaches to and interventions for Health and Illness Management d. Use of evidence as a guide for practice ANS: C Diverse approaches to and interventions for health and illness management include the interpersonal interventions to guide or coach patients, acquiring new ways to treat patients, providing preventative services, coordinating services among care sites and multiple providers, and acquiring knowledge about complementary therapies. 84. An APRN in an emergency department is utilizing a new type of IV catheter for the first time. He or she seeks out a colleague more familiar with the device for supervision. Which characteristic of advanced direct care practice is the APRN utilizing? a. Expert clinical performance b. Use of reflective practice c. Formation of therapeutic partnerships with patients d. Use of a holistic perspective ANS: A Expert clinical practice includes more than just providing excellent care at your current level. It also includes having an understanding of scenarios, situations, and procedures where you may be overwhelmed or less confident and then seeking out expert assistance or guidance. This provides the best outcomes for the patient and furthers the clinical understanding. 85. A female patient is undergoing an elective surgery that has a risk of blood loss. She is a Jehovah’s Witness and due to her religious beliefs does not want blood transfusions to be administered. The APRN delays the patient’s surgery and recommends she donate her own blood to be administered during the surgery if needed. Which characteristic of advanced direct care practice is the APRN utilizing? a. Use of evidence as a guide for practice b. Expert clinical performance c. Use of a holistic perspective d. Formation of therapeutic partnerships with patients ANS: C Understanding the patient’s spiritual and life values, additional context of the patient’s life, possible life changes, and the effects of their disease or treatments are all factors that must be considered when using a holistic perspective. 86. Which of the following will most likely enhance the patient-APRN relationship and increase communication? a. Longer appointment duration b. Printed education guides c. Having a caregiver present at the time of examination d. Active listening ANS: D A foundation of excellent communication begins with listening to the patient. Each of the other options may improve the outcome of the patient but establishing effective therapeutic relationships with patients involves listening to their concerns to establish trust, increase patient satisfaction, increase adherence to treatment plans, and improve patient outcomes. 87. With which of the following types of patients would it be most difficult to establish a therapeutic partnership? a. Mentally disabled patient b. Toddler c. Elderly patient d. A patient with tonal hearing loss ANS: A While all of the patients in this question may be more challenging, only the mentally disabled patient has expressed limitations in communication. A mentally disabled patient may not be able to comprehend instructions, and the level of understanding may not be able to be fully expressed. An elderly patient, a patient with hearing loss, and a toddler are still able to effectively communicate their level of understanding. Modifications in communication strategies may be required in all of the patients. 88. Which of the following techniques should be utilized when communicating with all elderly patients who have hearing loss? a. Administer testing for understanding b. Face the patient c. Use verbal aids d. Write down instructions ANS: B During the initial encounter with a patient with a communication barrier, the level of the barrier should first be assessed. Additional therapies may not be needed if simply sitting directly facing the patient can achieve effective communication. The same methods for ensuring understanding should be used in patients with hearing loss, such as having them repeat instructions or voice their level of understanding. 89. An elderly male patient is being seen by the APRN. Which of the following techniques for effective communication should be initially avoided? a. Speaking in a louder voice b. Appropriate touch c. Maintain eye contact d. Face the patient ANS: A Remember that assumptions should never be initially made about any patient and always speaking in a louder voice may be considered offensive. An elderly patient does not always have hearing loss or dementia, and strategies to assess the level of understanding should be used if suspicions exist. 90. An APRN is working in an outpatient care clinic for diabetics. He or she is responsible for starting newly diagnosed diabetic patients on long-acting basal insulin to control their fasting morning blood glucose levels. The APRN starts a 55-year-old obese patient 35 units of long- acting insulin nightly. The APRN chooses this dose solely based on the weight of the patient and does not review the patient’s current medication list. The APRN has previously used this method successfully in many patients who were admitted to the hospital. Three days later the patient is found unconscious at home by family members, transported to the emergency department, and expires. After an investigation the patient had administered only the prescribed amount of insulin as directed by the APRN. Which of the following factors most likely attributed to the patient’s poor outcome? a. Patient education b. Lack of knowledge c. Thinking error d. Lack of evidence-based practice ANS: C The APRN in this clinical scenario made a thinking error. While it is possible that other factors could have influenced the poor outcome, the dose of the insulin was unlikely individualized to this patient. Tunnel vision and treating each patient the same are examples of thinking errors. Failing to review the patient’s medication list for short-duration medications like steroids and antibiotics, as well as other comorbidities, increases risks for medication side effects. Although the APRN had administered similar doses to other patients previously, those patients were inside medical facilities with close observation to avoid adverse events. 91. An APRN is treating a 44-year-old female patient with 10/10 chest pain in an emergency department. This patient has a history of severe anxiety and has run out of her anxiety medication. She has been seen three times in the previous month for the same pain. The APRN discharges the patient home with a refill of her anxiety mediations but without a full cardiac workup. The patient dies at home and an autopsy reveals a myocardial infarction as the cause of death. Which of the following would have most likely prevented the poor outcome of the patient? a. Proper documentation b. Therapeutic communication c. Avoiding premature closure d. Patient education ANS: C Avoidance of thinking errors of medical providers is imperative to excellent patient care. While therapeutic communication may have elicited additional information about this patient the APRN should remain constantly open to re-evaluation of patients, be aware of personal biases and assumptions, and ensure critical data are obtained on each patient. The use of a diagnosed “time- out” procedure sometimes is important to review a situation with fresh eyes and to prevent assumptive diagnosis and premature closure. 92. Use of which of the following strategies by an APRN would best prevent ethical conflicts during end-of-life care? a. Discussion with healthy patient during outpatient clinic b. Use of an ethics committee c. Discussion when life-threatening disease/accident occurs d. Discussion upon admission of a patient to a hospital ANS: A Avoiding ethical conflicts with patients, families, and their surrogates can best be avoided by having ethical discussions as early as possible. While all scenarios will avoid ethical conflicts, discussion and documentation with a healthy patient allows for prevention of ethical conflicts in end-of-life care. Remember that prevention is always the best treatment. 93. Which of the following scenarios is the best example of the concept of moral distress? a. 75-Year-old nursing colleague fired for being too old b. 45-Year-old female diagnosed with lung cancer who refuses appropriate treatment c. 4-Year-old child who died after receiving an incorrect medication d. Amputation of the incorrect limb during a surgical procedure ANS: B The most common cause of moral distress identified in a 2004 study is patient refusal of appropriate life-saving treatment. By definition, moral distress is when a provider knows an ethically appropriate action should be taken but barriers are encountered that discourage the action from being taken. Wrong site surgeries and medication errors are negligence. The firing of a person based on age is considered discrimination. 94. Which of the following strategies has been recommended when communicating about adverse events? a. Avoid apologizing or acknowledging the error occurred b. Notify the patient immediately that an adverse event has occurred c. Complete all documentation thoroughly prior to reporting the event to anyone d. Explain all known details to the patient immediately ANS: B Four steps recommended by a consensus group of Harvard hospitals in 2006 include the following: (1) tell the patient what happened immediately, but leave details of how and why for later when a thorough review has occurred; (2) take responsibility for the incident; (3) apologize and communicate remorse; (4) inform the patient and family what will be done to prevent similar events. 95. Which of the following are characteristics of direct clinical care provided by APRNs? (Select all that apply.) a. Use of reflective practice b. Use of evidence as a guide for practice c. Formation of therapeutic partnerships with patients d. Adequate supervision of others e. Use of a holistic perspective ANS: A, B, C, E The six characteristics of direct clinical care are use of a holistic perspective, formation of therapeutic partnerships with patients, expert clinical performance, use of reflective practice, use of evidence as a guide to practice, and use of diverse approaches to health and illness management. Adequate supervision of others is an example of indirect care. 96. A newly licensed APRN is working in a busy outpatient clinic. He or she continually runs late and cannot adequately gather all of the pertinent patient information during each patient encounter. This has caused the APRN to misdiagnose multiple patients. Which of the following may best alleviate the time pressures experienced by the APRN? (Select all that apply.) a. Avoid interruptions b. Increase visit length time c. Limit patient complaints allowed for each visit d. Use a systematic approach e. Set a timer to end each patient encounter ANS: A, B, D Time pressures are experienced at an even higher frequency in novice APRNs. Avoiding interruptions and increasing visit length time are the best options to alleviate time pressures. Setting a timer to end each patient encounter or limiting patient complaints would be inappropriate strategy for a novice APRN. Rushed or truncated encounters often lead to lack of therapeutic communication, incomplete physical examinations, and withholding of patient questions. Development of a systematic approach to each patient encounter is one of the best strategies to implement to increase APRN efficiency and is usually paramount as an APRN develops experience. Chapter8 Beliefs, Values, and Health 97. Which of the following scenarios is an example of patient engagement? a. Physical therapy b. APRN prescribing the lowest effective dose of medication c. Coaching about weight loss d. Patient maintaining follow-up appointments ANS: D Patient engagement includes the actions and initiatives that are the sole responsibility of the patients regarding their own health maintenance and monitoring. A patient is responsible for things such as attending appointments, taking health measurements at home, and adhering to medication regimes. 98. Which of the following is an example of patient guidance? a. Increased self-awareness after reflecting on bad habits b. Education provided about a new medication side effect c. Patient-set agenda for weight loss d. Patient taking medications as prescribed ANS: B Patient guidance requires the provision of advice or education. Patient coaching involves agenda setting, awareness raising, actions and goal setting, and accountability. A patient taking medications as prescribed is an example of patient engagement. 99. A newly diagnosed diabetic patient does not know what types of foods are best to consume to help control his or her disease. An APRN teaches the patient about food choices and options. This is an example of: a. Patient coaching through patient education b. Patient guidance through empathy c. Patient guidance through patient education d. Patient coaching through awareness raising ANS: C This is an example of patient education, a component of patient guidance, since advice or education was provided to the patient. Empathy would be if the APRN provided guidance after a deep understanding of the reasoning for not understanding food choices. Patient coaching does not involve providing education or advice. 100. A domestic violence victim presents to the emergency department. The victim was struck by his or her partner several times with a baseball bat and suffered multiple broken ribs and lacerations to the face. Which of the following coaching and guidance skills should the APRN use for this patient first? a. Build strengths b. Cultivate a culture of empathy c. Create a safe environment d. Support small changes ANS: C Coaching and guidance skills are not always used in the same order. While all of the skills may be used in a patient who is the victim of domestic violence it is important that these patients feel safe. Creating a safe environment is paramount to establishing a therapeutic relationship and fostering changes in the future. 101. Which of the following is an example of patient coaching versus patient guidance? a. APRN education of smoking health risks b. Obtaining daily weight measurements c. Informational guide for weight loss d. Questioning that inspires self-awareness ANS: D Patient coaching involves agenda setting, awareness raising, actions and goal setting, and accountability. Raising awareness typically involves deep listening from the APRN as the APRN asks questions that challenge the patient’s mindset and assumptions about an issue. 102. Which of the following theories or research supporting APRN guidance and counseling defines a framework based on loving kindness that focuses on the science of caring and moving from carative to caritas (love)? a. Transtheoretical Model b. Watson’s Model of Caring c. Midrange Theory of Integrative Nurse Coaching d. Positive Psychology e. Nightingale’s Environmental Theory ANS: B Watson’s Model of Caring defines a framework based on loving kindness that focuses on the science of caring and moving from carative to caritas (love). This is the process of relating to others in an authentically present way, going beyond the ego (Watson, 2017). 103. Which theory or research supporting APRN guidance and counseling fundamentally states that external factors associated with patients’ surroundings greatly affect their lives, their development, and their biologic and physiologic processes? a. Watson’s Model of Caring b. Positive Psychology c. Midrange Theory of Integrative Nurse Coaching d. Transtheoretical Model e. Nightingale’s Environmental Theory ANS: E Nightingale’s Environmental Theory centers on the basis that external factors associated with patients’ surroundings greatly affect their lives, their development, and their biologic and physiologic processes. 104. Which model supporting APRN guidance and counseling defines a nursing role with the patient at the center to assist him or her with health goals, changing lifestyle behaviors, and implementing integrative modalities? a. Positive Psychology b. Nightingale’s Environmental Theory c. Watson’s Model of Caring d. Transtheoretical Model e. Midrange Theory of Integrative Nurse Coaching ANS: E The authors of the Midrange Theory of Integrative Nurse Coaching identified five components that place clients/patients at the center over five components: (1) self-reflection, self-assessment, self-evaluation, and self-care; (2) integral perspectives and change; (3) integrative lifestyle health and well-being; (4) awareness and choice; and (5) listening with HEART (healing, energy, awareness, resiliency, and transformation) (Dossey et al., 2015, p. 29). 105. What is the most important first step for an APRN prior to coaching a patient? a. Asking permission b. Liability release c. Providing guidance d. Prepare an action plan ANS: D Medical providers should first ask for permission to provide coaching about an issue. If the patient does not give permission the APRN should then provide guidance. 106. A 40-year-old female has smoked two packs of cigarettes per day for the past 25 years. She has no current health issues. When questioned by the APRN if she is interested in quitting she immediately states, “I like smoking, and I’m still healthy. I don’t want to quit.” Which stage of change best classifies this patient’s willingness to stop smoking? a. Contemplation b. Precontemplation c. Preparative d. Action e. Maintenance ANS: B The patient is in the precontemplation phase based on the information provided and is either not ready or resistant to change. It appears she may not understand the risks of her actions to her health, does not wish to acknowledge them, or does not believe she is capable of quitting. Further exploring should be done by the APRN to build a therapeutic relationship to foster change. 107. A 40-year-old female has smoked two packs of cigarettes per day for the past 25 years. She has no current health issues. When questioned by the APRN if she is interested in quitting she immediately states, “I like smoking, and I’m still healthy. I don’t want to quit.” Which of the following is the next best step by the APRN? a. Document her response b. Assess her knowledge of smoking cessation programs c. Educate her about the health risks of smoking d. Understand her level of understanding about the health risks of smoking ANS: B It appears the patient is in the precontemplation phase based on the information provided. Further questioning should be done to first assess her understanding about the health risks of smoking. After providing education an assessment of her willingness to quit should be completed. You would not want to educate her about the health risks if she is already aware of them, nor understand her knowledge of smoking cessation programs if she is not ready to quit. 108. A male patient with uncontrolled diabetes visits the APRN in the health clinic. After discussion about the patient’s uncontrolled disease the patient becomes emotional. The patient states he has tried before and wants to do better but has never been able to afford diabetic testing supplies. He does not currently take his prescribed insulin because he is aware that if he administers it without being able to check his blood glucose he could suffer serious health consequences. This patient is best classified as which stage of change? a. Contemplation b. Precontemplation c. Action d. Preparative e. Maintenance ANS: D This patient is in the action preparative stage of change. In this stage the patient is ready to take action but previous barriers (blood glucose monitoring costs) prevented the patient from taking action on any proposed plan previously. To move the patient into action all barriers whether real or perceived must be overcome. 109. An APRN is evaluating a female patient who is morbidly obese in a follow-up evaluation for weight loss. The patient states that she was doing well with weight loss until she went on a vacation. Since returning she has been gaining weight again. Which best characterizes the state of change this patient is experiencing? a. Action b. Preparative c. Contemplation d. Maintenance e. Precontemplation ANS: D The maintenance stage of change includes ongoing monitoring of the patient’s adherence to the plan and any relapses or difficulties the patient may occur. 110. Which of the following questions would be best used by the APRN regarding accountability when coaching a patient? a. “What do you need from our time together?” b. “What will you do if you go off your plan?” c. “What’s going to get in your way?” d. “What would your life be like if you achieved your goal?” ANS: B The accountability portion of the coaching phase involves helping the person use resources, not just pursue goals alone. The patient should implement technology and supportive others as well as be able to confirm that they are meeting their agenda. The other options are applicable to earlier coaching phases. 111. A patient has identified a weight loss goal of 100 pounds that he or she wishes to lose to reach a healthy weight. The patient has failed multiple weight loss attempts in the past. The APRN is coaching this patient regarding their weight loss plan. Which of the following skills should the APRN use for best success in this patient? a. Accountability b. Support small changes c. Raise awareness d. Use courage to challenge ANS: B All of the skills for coaching should be used but this patient has a very large ambitious goal with previous failures. It would be best to support small changes in this patient. This will allow the patient to gain confidence in his or her own success to promote success of his or her larger goal. Chapter9 The Healthcare Interdisciplinary Context: A Focus on the Microsystem Concept Multiple Choice 1. Although it is applicable across all APRN specialties, Caplan’s Principles of Consultation was first defined for which specialty? a. Hospitalist b. Mental Health c. Family Practice d. Nurse midwifery ANS: B Caplan’s Principles of Consultation first defined consultation as it is applied for mental health. 2. Which of the following attributes is included in the focus of consultation as defined by Caplan’s Principles of Consultation? a. Consultant will manage areas of care specific to his or her specialty b. Consultant will always directly coordinate care of the patient with the consultee c. Consultant must see patient directly d. Degree of focus provided by consultant is determined based on consultee’s skill level ANS: D The focus of consultation is always the patient, the consultant is not responsible for implementing interventions or remedial actions, the consultee continues to have professional responsibility for any corrective actions, and the consultee is free to accept or reject any of the consultant’s suggestions. The consultant may or may not directly evaluate the patient. The degree of focus provided by any consultant is determined based on consultee’s skill level, but should always be focused to enhance the patient’s care. 3. An APRN obtains a cardiology consultation for a patient. As part of the patient’s care the consultant recommends a medication that is contraindicated based on the patient’s comorbidities. Which is the best next action by the APRN? a. Disregard all of the consultant’s recommendations b. Follow the consultant’s recommendations c. Obtain a second cardiology consultation d. Withhold the contraindicated medication ANS: D Obtaining consultations can be a difficult process as the consultant is often not as deeply involved in the patient’s care as the consultee. There are often changes in the patient’s condition after the time the consultant has evaluated the patient. The best first step is to withhold the medication and clarify with the consultant directly about the medication. If the consultants continue to recommend the medication the APRN must then use his or her best judgment about obtaining a separate consultation. 4. A provider is working in an inpatient facility and is managing the care of a patient who he or she believes to have an infection. The provider requests for the services of an infectious disease clinician to evaluate the patient in person and provide recommendations for treatment. This is an example of which of the following? a. Comanagement b. Collaboration c. Clinical consultation d. Referral e. Supervision ANS: C This is an example of clinical consultation. The original provider may be unsure of a patient’s clinical condition and seeks the recommendations of an infectious disease specialist. For a consultation there does not have to be direct clinical physical examination. The recommendations that are provided by the consultant may be accepted or rejected by the initial provider. In real- world scenarios it is important to remember that billing and hospital policies may require in-person clinical evaluation and physical examination but this is not required for the initial provider to seek out the textbook definition of consultation. 5. A provider is working in an inpatient facility and is managing the care of a patient who he or she believes to have an infection. The provider requests for the services of an infectious disease clinician via telephone. The patient’s condition is discussed and antibiotic recommendations are made to the initial provider. The provider does not physically see the patient or perform a physical examination. This is an example of which of the following? a. Collaboration b. Comanagement c. Referral d. Clinical consultation e. Supervision ANS: D This is an example of clinical consultation. The original provider may be unsure of a patient’s clinical condition and seeks the recommendations of an infectious disease specialist. For a consultation there does not have to be direct clinical physical examination. The recommendations that are provided by the consultant may be accepted or rejected by the initial provider. In real- world scenarios it is important to remember that billing and hospital policies may require in-person clinical evaluation and physical examination but this is not required for the initial provider to seek out the textbook definition of consultation. 6. A provider is working in an inpatient facility and is managing the care of a patient taking the antibiotic vancomycin. The provider wishes to work with another provider so that they can manage the through and safe dosing levels of the antibiotic while they continue to manage the aspects of the patient’s condition, including side effects and clinical decision making. Both providers will share responsibility for the clinical outcome of the patient. This is an example of which of the following? a. Comanagement b. Collaboration c. Clinical consultation d. Referral e. Supervision ANS: A This is an example of comanagement. While it may be difficult to distinguish between the different types of interactions among other providers, these providers are clearly working together managing aspects of the antibiotic. The pharmacy manages dosing and lab values while the original provider focuses on the clinical response of the antibiotic. This is different than when a clinical provider asks for a consultation for a choice of antibiotic from an infectious disease clinician (clinical consultation) or requests a referral from an infectious disease clinician to manage portions or all aspects of an infection and care (referral or comanagement). 7. An NP in an outpatient care center specializes in family medicine. The NP’s patient needs to be evaluated by a specialist in gastroenterology. The NP would like the specialist to take over the aspects of care regarding gastroenterology for this patient. This is an example of which of the following? a. Referral b. Supervision c. Collaboration d. Comanagement e. Clinical consultation ANS: A A referral would be the best example for this scenario. The NP wishes to enhance the patient’s care by relinquishing an aspect of that care to another provider whose expertise is perceived to be more essential to the patient’s condition. 8. A novice APRN has started his or her first position in an emergency department. For the initial 3 months the APRN reviews each patient and all aspects of his or her care and discusses it with an attending physician working in the department. The attending physician also reviews all aspects of the patient’s care and assumes responsibility for any actions or patient outcomes for the care the APRN provides. This is an example of which of the following? a. Supervision b. Clinical consultation c. Collaboration d. Comanagement e. Referral ANS: A This is an example of supervision. Supervision can be multilevel based on laws, policies, or skill level. APRNs, physician assistants, and Medical Residents all undergo supervision whether supervised or unsupervised, at some point in their career. The hallmark of supervision is that the provider being supervised is responsible for his or her own actions; however, the ultimate responsibility almost always resides with the supervisor. 9. An APRN is working in an emergency department. The APRN works alongside several other APRNs and physicians in a community work area. The APRN is assigned a complex patient and asks a fellow APRN: “What duration of antibiotics would you prescribe a patient with pneumonia?” No relevant details about the patient’s condition are shared with the second APRN. This is an example of which of the following? a. Collaboration b. Supervision c. Clinical consultation d. Comanagement e. Referral ANS: A Collaboration is meant to foster a dynamic, interpersonal process in which two or more individuals interact authentically and constructively to solve problems. This process could be with a peer or more seasoned provider. Collaboration typically does not involve many expansive patient details unless used retrospectively. Responsibility of the care of the patient remains with the individual making the request. 10. An APRN requests a consultation from another provider. The information is brief and the responses are framed in generic terms. What type of consultation best describes this interaction? a. Formal consultation b. Informal consultation c. Collaboration d. Supervisory role ANS: B An informal consultation includes brief responses and contains only limited information. A formal consultation typically involves the consultant fully into the patient’s case and is very detailed. 11. An APRN requests a consultation from another provider. The patient is complex requiring detailed explanation of the patient. The responses are framed in specific terms outlining recommendations. What type of consultation best describes this interaction? a. Supervisory role b. Formal consultation c. Informal consultation d. Collaboration ANS: B An informal consultation includes brief responses and contains only limited information. A formal consultation typically involves the consultant fully into the patient’s case and is very detailed. A formal consultation is often required for complex patient cases. 12. Which of the following most likely increases the chances of a successful consult? a. Poor documentation b. Excellent documentation c. Electronic health records d. Closed-loop communication e. Open-loop communication ANS: D Closed-loop communication between the consulting and the consultee is best to increase the chances of a successful consult. The use of an EHR along with excellent documentation may increase the ease of communication but without a closed-loop communication, misinformation and errors may occur. Chapter10 Microeconomics in the Hospital Firm: Competition, Regulation, the Profit Motive, and Patient Care Multiple Choice 112. Which of the following is defined as the conscientious, explicit, and judicious use of current best research-based evidence when making decisions about the care of individual patients? a. Research theory b. Evidence-based practice c. Nursing research d. Current best evidence ANS: B Evidence-based practice is defined as the conscientious, explicit, and judicious use of current best research-based evidence when making decisions about the care of individual patients (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996). 113. Which of the following is defined as systematic inquiry that generates knowledge about issues of importance to the nursing profession; individual studies may focus on clinical practice, education, administration, and informatics? a. Evidence-based practice b. Nursing research c. Current best evidence d. Research theory ANS: B 114. Which of the following entails the application of research findings from studies that evaluate interventions or assessments used by nurses and other care providers to improve patient outcomes? a. Research theory b. Nursing research c. Current best evidence d. Evidence-based practice ANS: C Current best evidence entails the application of research findings from studies that evaluate interventions or assessments used by nurses and other care providers to improve patient outcomes. 115. Which of the following would best prepare a registered nurse to play a more active role in generating original research? a. Advocating for evidence-based practice b. Complete a doctoral program with a focus on research c. Complete a master’s degree program d. Join the current research team at his or her facility ANS: B All responses may improve the understanding and application of research to the nurse. Completing a doctoral program with a focus on research would best prepare a nurse who wishes to play a more active role in generating original research. 116. Which of the following is the first step of the process for identifying and determining evidence-based practice? a. Identification and retrieval of pertinent research findings based on literature review b. Extraction and critical appraisal of data from pertinent studies c. Formulation of a clinical question d. Clinical decision making based on results of this process ANS: C The formal, four-step process for identifying and determining evidence-based practice includes formulation of a clinical question, identification and retrieval of pertinent research findings based on literature review, extraction and critical appraisal of data from pertinent studies, and clinical decision making based on results of this process. 117. Which form of clinical decision making relies on findings from a wide variety of studies, including pathophysiologic research designed to identify the principal action of an intervention or the main reason it exerts a particular effect, and in vitro or in vivo research models? a. Tradition-based practice b. Evidence-based practice c. Rationale-based practice d. Nursing-based research ANS: C Rationale-based practice is a form of clinical decision making that relies on a rational explanation for an intervention. This form involves findings from a wide variety of studies, including pathophysiologic research designed to identify the principal action of an intervention or the main reason it exerts a particular effect, and in vitro or in vivo research models. 118. Which of the following is based on clinical and anecdotal experience, combined with received wisdom, often provided by instructors or clinical preceptors and expert opinion from those perceived as experts or expert clinicians in a given area of care? a. Tradition-based practice b. Rationale-based practice c. Evidence-based practice d. Nursing-based research ANS: A Tradition-based research is based on clinical and anecdotal experience, combined with received wisdom, often provided by instructors or clinical preceptors and expert opinion from those perceived as experts or expert clinicians in a given area of care. 119. Which of the following is the overall goal of a research study? a. Enhance quality of care by evaluating the effect of a specific action b. Application of best evidence to clinical decision making c. Combine the wisdom of experts in a given area of care d. Produce generalizable new knowledge ANS: D The overall goal of a research study is to produce generalizable new knowledge using various methods. The unit of study typically varies but is often an aggregate of individual patients, families, or communities. A research study typically involves a review and approval from an Institutional Review Board (IRB) and is produced into a research report that may be presented in many modalities. 120. Which of the following is the overall goal of evidence-based practice? a. Produce generalizable new knowledge b. Combine the wisdom of experts in a given area of care c. Enhance quality of care by evaluating the effect of a specific action d. Application of best evidence to clinical decision making ANS: D The overall goal of evidence-based practice is to apply the current best evidence to clinical decision making for an individual patient, facility, or large group. 121. Which of the following is the overall goal of a quality improvement project? a. Combine the wisdom of experts in a given area of care b. Application of best evidence to clinical decision making c. Produce generalizable new knowledge d. Enhance quality of care by evaluating the effect of a specific action ANS: D The overall goal of a quality improvement project is to enhance quality of care by evaluating the effect of a specific action plan on a local unit, clinic, facility, or health system. 122. Which of the following would best help a nurse formulate a measurable question that can be meaningfully addressed using evidence-based clinical decision strategies? a. PICO(T) b. ROPI c. IRB d. GRADE ANS: A The PICO(T) model is the best model for a nurse to formulate a measurable question that can be meaningfully addressed using evidence-based clinical decision strategies. PICO(T) stands for patient/population and problem, intervention, comparison, outcome, and time. 123. Based on the pyramid of evidence, which of the following studies has the highest potential to contribute to evidence based on its design? a. Systematic reviews b. Cohort study c. Randomized controlled trial d. Case study e. Meta-analysis ANS: E A meta-analysis has the highest potential contribution to evidence based on design. Case studies and in vivo and in vitro studies have the least potential contribution due to their limited size. 124. Based on the pyramid of evidence, which of the following studies has the lowest potential to contribute to evidence based on its design? a. Meta-analysis b. Randomized controlled trial c. Cohort study d. Case study e. Systematic reviews ANS: D Case studies and in vivo and in vitro studies have the least potential contribution due to their limited size. A meta-analysis has the highest potential contribution to evidence based on design. 125. Which of the following rankings of recommendations for clinical practice as provided by the US Preventative Services Task Force (USPSTF) should always be offered or provided by the APRN when indicated? a. A, B, and C b. A c. A and B d. All recommendations e. B ANS: C Rankings A and B should be offered or provided when indicated. 126. Which of the following rankings of recommendations for clinical practice as provided by the US Preventative Services Task Force (USPSTF) should be offered or provided by the APRN only when other considerations support offering or providing the service? a. C b. D c. B d. All recommendations e. B and C ANS: A A USPSTF ranking of C states that evidence suggests that the service only provides a small benefit and should be provided only when other considerations support offering or providing this service. 127. Which of the following rankings of recommendations for clinical practice as provided by the US Preventative Services Task Force (USPSTF) should the APRN discourage use of? a. D b. I c. B d. C e. C and D ANS: A A USPSTF ranking of D states that evidence demonstrates no benefit from the service or potential harm outweighs the service. The APRN should discourage the use of this service. Chapter11 Government Regulation: Parallel and Powerful Multiple Choice 128. A nurse sees the “big picture” regarding multiple aspects of care. He or she begins evaluating projects with a clinical information committee at his or her hospital system. They focus on how the project will interoperate with many departments at the hospital. This is best defined as which type of leadership? a. Health policy leadership b. Clinical leadership c. Professional leadership d. Systems leadership ANS: D Systems leadership includes leading at the organizational or delivery system level and requires a multifaceted understanding of systems. Professional leadership overlaps with systems leadership but has less of a specific focus on the larger picture of systems. 129. An APRN joins a committee at his or her hospital system involved in improving clinical outcomes. This is best defined as which type of leadership? a. Clinical leadership b. Systems leadership c. Professional leadership d. Health policy leadership ANS: A Clinical leadership focuses on the needs and goals of the patient and family and ensures quality patient care is achieved. This may also be considered an example of professional leadership but clinical leadership is the most correct answer. 130. An APRN joins state organization for nurses and begins actively participating. This is best defined as which type of leadership? a. Health policy leadership b. Systems leadership c. Clinical leadership d. Professional leadership ANS: D Professional leadership is best defined as the active participation in interprofessional organizations that are typically organized at the local, state, or national level. 131. An APRN advocates for the development of laws regarding independent authority of APRNs in his or her state. This is best defined as which type of leadership? a. Health policy leadership b. Systems leadership c. Clinical leadership d. Professional leadership ANS: A Participation or involvement in policymaking that affects patient care, health care funding, and national priorities in health among other issues make up health policy leadership. 132. Which strategy for implementing leadership competency involves the personal vision, goals and objectives, and the APRN role? a. Promoting collaboration b. Leadership portfolio c. Networking d. Followship ANS: B Developing a leadership component as part of a professional portfolio is helpful to novice APRNs who desire to individualize continuing development of leadership competency consistent with their personal vision, goals, timeline, and APRN role in the practice setting. 133. Which leadership model asserted that transformational leaders constantly ask themselves and their team questions about what the goal is, how to try things differently, and what arethe costs of maintaining the status quo? a. Sense b. Covey c. Vernon d. DePree ANS: C Vernon (2015) asserted that transformational leaders constantly ask themselves and their team questions about what the goal is, how to try things differently, and what are the costs of maintaining the status quo. 134. Which leadership model defined leadership as an art form in which the leader does what is required in the most effective and humane way? a. Sense b. Vernon c. Covey d. DePree ANS: D DePree (2011) defined leadership as an art form in which the leader does what is required in the most effective and humane way. 135. Which of the following is defined as the overall interaction between an individual’s leadership style and the features of the environment or situation in which he or she is operating? a. Professional leadership b. Roving leadership c. Appreciative inquiry d. Situational leadership ANS: D Situational leadership is defined as the interaction between an individual’s leadership style and the features of the environment or situation in which he or she is operating. Roving leadership is an expanded definition that describes the participatory process in which leadership may shift among team members. 136. Rather than focusing on a problem, which leadership model seeks to find positives through conversations and relationship building? a. Roving leadership b. Appreciative inquiry c. Systems leadership d. Situational leadership ANS: B Appreciative inquiry seeks to find positives through appreciative conversations and relationship building. 137. A well-trusted and liked clinician at an institution speaks to groups of APRNs about his or her experiences as a means to influence others to improve. This is an example of which type of leadership? a. Opinion leadership b. Appreciative inquiry c. Roving leadership d. Spiritual leadership ANS: A Opinion leaders are clinicians who are identified by their colleagues as likeable, trustworthy, and influential (Flodgren et al., 2007). 138. An APRN is leading others about success and informs a group that it is okay to make mistakes. This is an example of which characteristic of APRN leadership? a. Innovation b. Mentoring c. Likeability d. Fiscal responsibility e. Empowering others ANS: E Empowering others is a defining characteristic of APRN leadership. Other ways to empower others to succeed include sharing information, creating clear goals and objectives, teaching it is okay to make mistakes, creating an environment that celebrates both successes and failures, support of a learning environment, and letting teams become the hierarchy. 139. Which of the following broad qualities is a necessary attribute of APRN leaders? a. Failure to mentor b. Horizontal violence c. Risk taking d. Documentation ANS: C Risk taking is a broad quality that is a necessary attribute of APRN leaders. This includes getting involved, demonstrating self-confidence and assertiveness, creative thinking, a willingness to fail, and coping with change among others. 140. Which of the following are the three defining characteristics of APRN leadership? (Select all that apply.) a. Likeability b. Mentoring c. Innovation d. Empowering others e. Fiscal responsibility ANS: B, C, D The three defining characteristics of APRN leadership are mentoring, empowering others, and innovation. Chapter12 Factors Influencing the Application and Diffusion of CQI in Health Care 1. A 45-year-old female is being prepared for elective surgery. A registered nurse goes over the patient’s medication list and allergies and then the patient is seen by a CRNA prior to surgery who also goes over the patient’s medication list. The registered nurse and the CRNA do not work together to form a medication list for the patient. This is best defined as: a. Collaboration b. Parallel communication c. Parallel functioning d. Faux collaboration e. Information exchange ANS: B Parallel communication occurs when two clinicians do not talk together prior to seeing the patient, see the patient separately, and have no expectation of joint interactions. If the two made separate plans of care for the same aspect of the patient’s care this could be defined as parallel functioning. 2. Which of the following has the highest likelihood for medical errors and decrease patient outcomes? a. Collaboration b. Parallel functioning c. Referral d. Consultation ANS: B Parallel functioning is when providers are caring for patients and address the same clinical problems without joint or collaborative planning. This could lead to additional interventions, confusion for the patient, medication errors, and poor outcomes. 3. Two APRNs work together to evaluate a patient, develop a plan of care, and implement different aspects of care while communicating about the patient’s overall clinical course. This is an example of: a. Parallel communication b. Collaboration c. Coordination d. Referral e. Parallel functioning ANS: B Collaboration with other team members involves the facilitation of teamwork to ensure the delivery of safe, effective, high-quality care leading to positive outcomes. 4. A novice APRN begins working at a cardiovascular outpatient clinic with a more senior APRN. The novice APRN always goes along with recommendations of the other APRN due to a feeling of a lack of skill to engage in conversations about the patient’s care. Which of the following is the novice APRN experiencing? a. Information exchange b. Faux collaboration c. One-sided compromise d. Parallel functioning e. Parallel communication ANS: C One-sided compromise is communication where one side consistently yields to other health care providers and senses a personal lack of integrity in the care. The compromise may occur when there is a lack of will or skill to engage in collaborative negotiation. 5. A novice APRN begins working at a cardiovascular outpatient clinic with a more senior APRN. The novice APRN always goes along with recommendations of the senior APRN. The senior APRN does not feel the need for meaningful dialogue since the novice APRN has agreed with all of the plans of care. Which of the following best describes this situation? a. Parallel communication b. One-sided compromise c. Parallel functioning d. Coordination e. Faux collaboration ANS: E Faux collaboration can be subtle and difficult to identify. It occurs when a person in a position of authority believes he or she is being collaborative because those around him or her are agreeable and there is no meaningful dialogue. 6. Two providers are caring for the same patient and address the same clinical problems without joint or collaborative planning. Which of the following is the best example of this scenario? a. Parallel functioning b. Faux collaboration c. Parallel communication d. Referral e. One-sided compromise ANS: A Parallel functioning is when providers caring for patients address the same clinical problems without joint or collaborative planning. 7. An APRN suspects a patient has tuberculosis and has the patient placed in isolation in a negative pressure room. The APRN notifies the nurse caring for the patient that anyone entering the room must wear a special mask. This example is best defined by which of the following? a. Collaboration b. Comanagement c. Information exchange d. Faux collaboration e. Parallel communication ANS: C Information exchange or informing may be one-sided or two-sided and may or may not require an action or decision making. Information exchange that requires decision making is typically unilateral and risks a negative outcome if the situation actually required joint planning and information exchange. 8. An APRN calls the laboratoryand medical imaging department regarding his or her patient. The APRN informs the medical imaging department that they must wait to perform imaging until after the laboratory has completed with the patient. This example best represents which of the following? a. Collaboration b. Coordination c. Parallel communication d. Faux collaboration e. Parallel functioning ANS: B Coordination is a form of communication that lends structure to an encounter and often includes actions that minimize duplication of efforts or ensure continuity of care. 9. Which of the following is necessary to create an environment of collaboration? a. Common purpose b. Similar ideologies c. Poor communication d. Ineffective methods e. Poor patient outcomes ANS: A Although all of the responses may lend to collaboration, only the presence of a common purpose or goal will facilitate ease of collaboration, as it is one of the key elements for collaboration. The most common goal in health care is to improve patient outcomes. Poor outcomes do not need to be present to have collaboration. 10. Which of the following strategies is most likely to facilitate organizational collaboration? a. Understanding another person’s viewpoint b. Cooperation without losing integrity c. Collaborative research d. Interprofessional education programs ANS: D A strategy to facilitate organizational collaboration would be interprofessional education programs. These programs allow different providers to meet face to face in an educational environment with a common goal of learning. Collaborative research is a strategy for team building. 11. Which of the following strategies is most likely to increase individual collaboration? a. Knowledge of what is negotiable and nonnegotiable b. Team-building exercises c. Interprofessional education programs d. Collaborative research ANS: A There are many strategies to promote effective communication and collaboration on an individual basis. These include being respectful and professional, listening, acknowledging others’ viewpoints, knowing what is negotiable, knowing the bottom line, and not taking things personally among many others. 12. Which of the following decreases defensiveness, relieves tension, and deflects anger as part of the collaborative process? a. Common purpose b. Humor c. Clinical competence d. Accountability ANS: B Humor helps individuals maintain perspective and acknowledge the lack of perfection needed. It also sets the tone for trust and acceptance among colleagues during difficult situations so that defensiveness and tensions can be relieved. 13. Which of the following are restraining forces on interprofessional practice, education, or research? (Select all that apply.) a. Shared competencies b. Cultural silos c. Lack of expertise d. Physician-based reimbursement e. Care of older adults and their families ANS: B, C, D Restraining forces for interprofessional practice, education, and research include lack of expertise, cultural silos, existing infrastructure, and reimbursement. Driving forces for interprofessional practice, education, and research include older adults and their families, professions (shared competencies), business (workforce shortages), and policy (health care reform). 14. Which of the following are driving forces on interprofessional practice, education, or research? (Select all that apply.) a. Lack of expertise b. Workforce shortages c. Shared competencies d. Care of older adults and their families e. Physician-based reimbursement ANS: B, C, D Driving forces for interprofessional practice, education, and research include older adults and their families, professions (shared competencies), business (workforce shortages), and policy (health care reform). Chapter13 Patient Safety Movement: The Progress and the Work That Remains 1. An APRN is about to examine a patient in the emergency department. A colleague states to the APRN “This patient is probably just seeking pain medication.” Regardless of his or her colleague’s comment he or she enter the examination room and treat the patient as if he or she is trustworthy and has good motives. Which of the ten essential elements of dignity is the APRN utilizing? a. Inclusion b. Benefit of the doubt c. Acceptance of identity d. Recognition ANS: B Treating others as if they are trustworthy, starting with the premise that they have good motives and are acting with integrity are all key points of benefit of the doubt. Benefit of the doubt is one of the ten essential elements of dignity. 2. An APRN approaches his or her patients as neither inferior nor superior and gives others the freedom to express their authentic selves without being judged. Which of the ten essential elements of dignity is the APRN utilizing? a. Safety b. Accountability c. Acceptance of identity d. Benefit of doubt ANS: C The acceptance of identity is one of the ten essential elements of dignity. Approaching people as neither inferior nor superior to you, giving others the freedom to express their authentic selves without fear of being negatively judged, interacting without prejudice or bias, accepting how race, religion, gender, class, sexual orientation, age, disability, and so on are at the core of someone’s identities, and assuming they have integrity are all included in the essential elements of acceptance of identity. 3. Communication problems often plague ethical dilemmas, which of the following is often at the forefront of communication problems regarding clinicians? a. Poor knowledge of the situation b. Language barriers c. Poor independence d. Failure to speak up ANS: D All of the answers may contribute to ethical dilemmas but failure of a clinician to speak up about a real or potential ethical problem is commonly identified. Erosion of open and honest communication is typically the first theme encountered in many ethical dilemmas. 4. A 76-year-old patient is admitted to the hospital after suffering a spinal compression fracture. The patient is unable to ambulate adequately on his or her own and requires assistance for basic needs. Your assessment is that the patient will recover their strength within 2 weeks. The billing department at the facility notifies you that the patient may not stay in the hospital for more than 2 days. The patient does not wish to be transferred to a nursing facility and wishes to remain in the hospital for the remaining 12 days to gain strength. Which of the following best defines this scenario? a. Interprofessional conflict b. Communication problems c. Legal issues d. Multiple commitments ANS: A This ethical scenario plays out routinely in medical care as an element of interprofessional conflict. The clinician wishes to respect patient autonomy but must understand and express the best interests of the patient to a multidisciplinary team. 5. An APRN is scheduled to complete his or her shift at 7 p.m. on a particular day. A new patient arrives 5 minutes prior to the time the APRN is expected to leave. He or she is asked by a supervisor to stay beyond their scheduled time to assess the patient and provide care. Which of the following best defines this scenario? a. Interprofessional conflict b. Multiple commitments c. Communication problems d. Legal issues ANS: B APRNs often fail to practice self-care and it is a significant threat to ethical practice. Multiple commitments including obligations to multiple parties involving the patient, employer, and legal system may create a scenario for ethical issues in nursing practice. Societal issues including cost containment pressures in health systems are likely partially responsible for development of this scenario. 6. An APRN works in a primary care clinic. The APRN wishes to treat a patient’s disease with a specific medication that is far superior to other treatments. The APRN has never encountered issues prescribing this therapy as first-line treatment in the past. The APRN is informed by this particular patient’s insurance that they require proof that the APRN has tried a far less effective therapy for 1 month prior to paying for the medication. Which of the following best describes the forces at work in this scenario? a. Communication problems b. Legal issues c. Interprofessional conflict d. Societal issues ANS: D Societal issues including cost containment pressures in health systems are likely responsible for development of this scenario. Interprofessional conflicts would best be involved in this scenario if this is applied in a multidisciplinary team scenario. 7. Which of the following are defined as the four elements of core competency development in ethical decision making for APRNs? a. Knowledge development, knowledge application, creating an ethical environment, promoting social justice b. Knowledge development, educating others, creating an ethical environment, promoting social justice c. Knowledge development, knowledge application, effective communication, promoting social justice d. Knowledge development, knowledge application, creating an ethical environment, understanding legal barriers ANS: A The core competency of ethical decision making for APRNs is best organized into four key elements: knowledge development, knowledge application, creating an ethical environment, and promoting social justice. 8. Which of the following examples best describes the knowledge development element of core competency development for ethical decision making? a. Analyzing the policymaking process b. Using self-reflection during patient case reviews c. Applying ethical decision-making model to a clinical problem d. Mentoring others to develop ethical practice ANS: B The use of knowledge development is a key element of core competency development for ethical decision making. It involves gaining knowledge of ethical theories and developing the ability to distinguish a true ethical dilemma from a situation of moral distress or other clinically problematic situation. Becoming sensitive to ethical dimensions of clinical practice and fidelity conflicts, developing values clarification (self-reflection), and interpreting reactions and emotions of others are all elements of knowledge development and moral sensitivity. 9. An APRN joins a group promoting awareness about abuse in long-term nursing care facilities. He or she advocates for policies that protect the health care rights of individuals who are not able to care for themselves independently. The APRN most likely employed which of the following elements of core competency development for ethical decision making? a. Promoting social justice b. Knowledge development c. Creating an ethical environment d. Knowledge application ANS: A Skills or behaviors for promoting social justice within a health care system include the ability to analyze the policy process and advocacy, communication, and leadership skills that promote involvement in health policy initiatives supporting social justice. 10. An APRN interacts with a patient and another colleague to achieve the best outcome ofan ethical dilemma. The APRN most likely used which of the following elements of core competency development for ethical decision making? a. Knowledge application b. Creating an ethical environment c. Promoting social justice d. Knowledge development ANS: A Applying ethical decision-making models to clinical problems, using skilled communication regarding ethical issues, and facilitating decision making by using select strategies are involved in the use of knowledge application. 11. An APRN works at a hospital system that provides care to a large proportion of Asian- American citizens. The APRN develops a presentation for newly hired employees about the cultural belief systems held by many in this population group. This describes the use of which of the following elements of core competency development for ethical decision making? a. Creating an ethical environment b. Promoting social justice c. Knowledge application d. Knowledge development ANS: A Creating an ethical environment may include the use of preventative ethics and awareness of environmental barriers to ethical practice. 12. Application of existing rules and doctrine as a guide for ethical decision making is best described as which ethical approach? a. Narrative ethics b. Care-based ethics c. Casuistry d. Principle-based ethics e. Virtue-based ethics ANS: D In principle-based ethical decision making, the principles or rules in contention are balanced and interpreted with the contextual elements of the situation. However, the final decision and moral justification for actions are based on principles. 13. Which ethical approach uses comparisons of precedent-setting cases and current scenarios? a. Principle-based ethics b. Casuistry c. Care-based ethics d. Narrative ethics e. Virtue-based ethics ANS: B Casuistry is an ethical approach which uses comparisons of precedent-setting cases and current scenarios. 14. Which approach emphasizes the particulars of a case or story as a vehicle for discerning the meaning and values embedded in the ethical decision making? a. Principle-based ethics b. Casuistry c. Virtue-based ethics d. Care-based ethics e. Narrative ethics ANS: E Narrative ethics emphasizes the particulars of a case or story as a vehicle for discerning the meaning and values embedded in the ethical decision making. 15. Which ethical approach sees individuals as interdependent rather than independent and focuses on parties in a relationship? a. Principle-based ethics b. Care-based ethics c. Narrative ethics d. Casuistry e. Virtue-based ethics ANS: B Care-based ethics emphasizes creating and sustaining responsive connections with others, importance of contact and subjectivity in discerning ethical action, and sees individuals as interdependent rather than independent and focuses on parties in a relationship. Chapter14 Accelerating Patient Safety Improvement Multiple Choice 141. As defined by Kilpatrick et al. (2016), which of the following is a hallmark of the role of the CNS? a. Adapting to changing needs of patients, nurses, and health care systems b. Advanced knowledge and skills c. Lack of educational requirements d. Ability to independently practice ANS: A A hallmark of the role is the ability of the CNS to adapt to changing needs of patients, nurses, and health care systems (Kilpatrick, Tchouaket, Carter, Bryant-Lukosius, & DiCenso, 2016). This versatility allows for a CNS to transition between positions as a primary caregiver or educator depending on the environment. 142. Which of the following has complicated clarifying the work and core competency of all CNSs? a. Varying educational, competency, and practice standards b. Bureau of Labor Statistics’ failure to capture data c. Lack of interest d. Advancement of the nurse practitioner role ANS: A Varying educational, competency, and practice standards have complicated clarifying the work and core competencies of all CNSs, regardless of specialty. The failure of the Bureau of Labor Statistics to track CNS providers only creates barriers when it comes to counting the number of CNSs in the United States. 143. Which of the following is a central competency for CNSs according to the Hamric model? a. Indirect care of patients and families b. Ethical decision making c. Direct care of patients and families d. Systems leadership e. Conduct of research ANS: C Direct care of patients or clients is the central core competency of the Hamric model and links each of the other competencies. 144. According to the NACNS model, emphasis on which of the following competencies is largest? a. Indirect care of patients and families b. Ethical decision making c. Conduct of research d. Direct care of patients and families e. Systems leadership ANS: D Direct care of patients or clients is the largest competency of the three spheres according to the NACNS model and encompasses the other two. 145. A CNS relocates to another state and begins a new job. Which of the following would guide his or her ability to practice certain procedures or skills? a. State scope of practice and facility policy b. American Medical Association policy c. State scope of practice d. Facility policy ANS: A The scope of practice is those activities a health care individual is allowed to perform within his or her profession. It is the responsibility of the CNS to adhere to each state’s rules in which they practice. Additionally, facilities may impose additional restrictions or limitations for a CNS to perform procedures or skills. 146. The National Association of Clinical Nurse Specialists has seven core competencies published for the CNS role. Which of the following is not included at the highest level? a. Coaching competency b. Professionalism competency c. Direct care competency d. Systems leadership competency ANS: B The National Association of Clinical Nurse Specialists’ Core Competencies include at the highest level seven competencies: direct care, consultation, systems leadership, collaboration, coaching, research, and ethical decision making, moral agency, and advocacy. 147. Each of the following is specifically described in the NACNS’s three spheres of influence for the CNS role except: a. Nurses/nursing practice b. Organization/system c. Leadership d. Patient ANS: C The NACNS has defined the CNS role as operating between the three spheres of influence: the patient, the organization/system, and the nurse/nursing practice. The CNS should employ Hamric’s seven competencies across the three spheres of influence. 148. According to a 2016 ruling, how has the Department of Veterans Affairs alleviated state- based practice regulations at VA facilities? a. Allows CNS to work at full practice authority b. Allows CNS to practice according to their home state’s regulation c. Provides immediate licensures d. Provides malpractice insurance free of charge ANS: A In 2016, the Department of Veterans Affairs alleviated state-based practice regulations by allowing CNS to work at full practice authority inside VA facilities and not within a state’s scope of practice. 149. Which of the following is major regulatory barrier for many CNS specialties in relation to the Consensus Model? a. Poor reimbursement for services b. Lack of specialty certification examinations c. Lack of education d. Poor CNS involvement in advocacy ANS: B A lack of specialty certification examinations in some areas is a major regulatory barrier for many CNS specialties in relation to the Consensus Model. 150. With regard to prescriptive authority, how did Oregon manage CNSs whose original education curriculum did not include prescription of pharmacologic agents? a. Take a specialized state-specific examination regarding prescriptive authority b. Permanent exclusion from prescriptive authority c. An advanced pharmacology course and complete 150 supervised hours d. 2080 hours involved in a collaborative agreement ANS: C Oregon’s regulation for inclusions of CNSs whose original education curriculum did not include prescription of pharmacologic agents includes the completion of an advanced pharmacology course and a minimum of 150 hours of supervised pharmacologic management. Minnesota requires 2080 hours of practice within a collaborative agreement with a licensed CNP, CNS, or physician experienced with similar patients. Wisconsin requires advanced practice nurse prescribers to pass an examination on Wisconsin’s statutes and rules of practice. 151. States have each independently created regulation regarding advanced practice. With regard to prescriptive authority, what requirement has Wisconsin implemented regarding authorization of CNSs as advanced practice nurse prescribers? a. 2080 hours involved in a collaborative agreement b. An advanced pharmacology course and complete 150 supervised hours c. Permanent exclusion from prescriptive authority d. Take a specialized state-specific examination regarding prescriptive authority ANS: D Wisconsin requires advanced practice nurse prescribers to pass an examination on Wisconsin’s statutes and rules of practice. Oregon’s regulation for inclusions of CNSs whose original education curriculum did not include prescription of pharmacologic agents includes the completion of an advanced pharmacology course and a minimum of 150 hours of supervised pharmacologic management. Minnesota requires 2080 hours of practice within a collaborative agreement with a licensed CNP, CNS, or physician experienced with similar patients. 152. Which factor led to a decrease of CNSs entering CNS programs in 1990s? a. Repurposing CNSs into quality managers and educator roles b. Increased job positions c. Increase in facility funding for NP programs d. Lack of emphasis on primary care ANS: A Several forces led to the initial decline in the number of students entering CNS programs. Fiscal restraints of health care facilities, repurposing CNSs into other roles, increased emphasis in primary care, and rapid growth of NP programs have previously and continue to contribute to decreased numbers of students entering CNS programs. 153. Which of the following is an important defining characteristic of the difference of the CNS role from an NP? a. Time spent among three spheres of influence b. Primarily involved in direct care c. Does not provide consultations d. Time spent primarily as patient advocate ANS: A One key defining difference of the CNS role is that the time spent performing competencies is across three spheres of influence. In the NP role, most time is spent in direct care management of patients. Both may provide consultations and all clinicians should act as a patient advocate. 154. Which of the following is most important to stabilize the future of the CNS role? a. Decreased educational requirements b. CNS conducted independent research c. Unity around NCSBN affirmation of CNSs being APRNs d. NP restrictions of roles ANS: C There are several important factors that influence the stability of the CNS role in the future. These include unity around NCSBN affirmations of CNSs as APRNs, articulating contributions to patients, families, and health care systems, ensuring educational curricula are upheld and helpful, partnering with others in practice and research, and seeking national recognition for the role. 155. Which of the following is provided as part of the Consensus Model? a. Decrease educational requirements b. Collaboration among physicians c. Reimbursement for services d. Title protection ANS: D The Consensus Model provides title protection for CNSs and provides for a grandfather clause to include APRNs who graduated from accredited programs and began practicing prior to the implementation of the Consensus Model. Chapter15 Health Information Technology Multiple Choice 156. The federal government’s criterion to establish health professional shortage areas (HPSAs) is based on which of the following statistics? a. Average family income less than two-thirds of national poverty level b. An area in which there are less than 500 individuals for every primary care physician (PCMD) c. Average family income less than half of national poverty level d. An area in which there are more than 4500 individuals for every primary care physician (PCMD) e. An area in which there are more than 3500 individuals for every primary care physician (PCMD) ANS: E The federal government establishes health professional shortage areas (HPSAs) that are primarily based on the criterion that an area has more than 3500 individuals for every primary care physician (PCMD). 157. What is a downfall of the HPSA’s calculation? a. Is only recalculated every 10 years b. Does not include other PCP designations (PAs, NPs) c. Does not adjust for inflation d. Has a lower weighted average for NP versus MD providers ANS: B The health professional shortage areas (HPSAs) are currently only calculated based on primary care physicians (PCMDs) and do not take into account other primary care providers such as PAs and NPs. 158. Some community health centers can apply for a special designation if they are an entity that serves a population that is medically underserved or a specially medically underserved population comprised of migratory and seasonal agricultural workers, the homeless, and residents of public housing. What is this designation? a. Federally qualified health center (FQHC) b. Patient-centered medical home (PCMH) c. School-based health center (SBHC) d. Nurse-led health center (NLHC) ANS: A The HRSA Bureau of Primary Care enables these safety net organizations to receive a variety of enhanced federal support by applying for designation as a federally qualified health center (FQHC). 159. Which of the following is not a common characteristic of a school-based health center (SBHC)? a. No parental requirement for consent for treatment b. Close integration with the school c. Comprised of a multidisciplinary team d. Located in schools or on school grounds ANS: A Nearly all SBHCs require parental consent for full treatment of adolescents, except in states where such adolescents can consent for certain treatments like contraception, pregnancy, drug abuse, and/or sexually transmitted infections. 160. A nurse practitioner provides care at a veteran’s clinic managed by the Department of Veterans Affairs. The state in which he or she practices prohibits many procedures. Which of the following is most accurate regarding the care the NP provides? a. Additional licensure is required to practice in VA systems by the state b. NP must be supervised for all skills c. State practice regulations override VA regulations d. Full practice authority is allowed inside the VA system ANS: D In 2016, The Department of Veterans Affairs granted full practice authority to NPs, CNSs, and CNMs. This allows these providers to work at full practice authority inside VA facilities and not confined within a state’s scope of practice. 161. Medical care provided by primary care providers (PCMD, PCNP) as part of the patient- centered medical home (PCMH) model encompasses the full spectrum of primary care including standards of accessibility, continuity, comprehensiveness, integrated care, and interprofessional care. This model was first defined for what population group? a. Geriatrics b. Gynecology c. Pediatrics d. Mental health ANS: C The patient-centered medical home (PCMH) model was first developed for the pediatric medical community for development of children with complex medical conditions. 162. Which of the following is reducing the restrictions of access to consultations for patients with complex or high-risk conditions, effectively reducing the burden of primary care practices? a. PCMH Model b. CONNECT Project c. Project ECHO d. PCT-LEAP Project ANS: C Technical innovations such as Project ECHO and eConsults are increasing access and advancing care by easing the burden of connecting primary care practices and patients with consultants through the use of technology. This allows for faster access to consultants for patients with complex or high-risk medical conditions. 163. A medical visit that comprises several patients in a group with similar conditions where patients discuss their health status, therapeutic regimes, behavioral modifications, and how to handle them is called: a. Project ECHO b. Convenient care clinics c. Shared medical appointments d. Group therapy ANS: C Shared medical appointments are a reimbursable type of visit that may include a multidisciplinary team where patients with similar conditions discuss their health status, therapeutic regimes, behavioral modifications, and how to handle them in a group setting. 164. According to the American Association of Nurse Practitioners: 2017 NP Fact Sheet, NPs have been in practice an average of how many years? a. 9 years b. 14 years c. 7 years d. 11 years ANS: D In 2017, the average NP has been in practice for 11 years. 165. According to the American Association of Nurse Practitioners: 2017 NP Fact Sheet, which of the following is the largest area of certification? a. Pediatrics b. Acute care c. Psychiatric/mental health d. Primary care e. Tertiary Care ANS: D About 89.2% of NPs are certified in an area of primary care as of 2017 including Adult, Adult- Gerontology, Family, Gerontology, Pediatric-Primary Care, and Women’s Health. 166. According to the American Association of Nurse Practitioners: 2017 NP Fact Sheet and the AANP National Nurse Practitioners Database, approximately how many NPs are licensed in the United States? a. 1,26,000 b. 2,34,000 c. 3,18,000 d. 3,81,000 e. 4,08,000 ANS: B As of 2017, there are more than 2,34,000 NPs licensed to practice in the United States. 167. Which of the following has shown promising outcomes for NPs in achievement of competence, confidence, and mastery as well as increased levels of NP satisfaction? a. NP Postgraduate Residency Programs b. Work in Underserved population areas c. Increased NP Pay d. Decreased malpractice claims e. Advancement of NP care practices ANS: A NP Postgraduate Residency Programs still need additional research on outcomes, policy considerations, and academic arrangements. Early studies have suggested that NPs who complete a residency program acquire higher achievement of competence, confidence, and mastery as well as increased levels of NP satisfaction. 168. The Triple Aim Initiative was launched in 2007 by the Institute for Healthcare Improvement (HIT) which focused on three dimensions of health care: experience of care, per capita cost, and population health. Which fourth aim was proposed in 2014 by Bodenheimer and Sinsky in a call to redesign the initiative? a. Improved clinician experience b. Prevention c. Increased reimbursements d. Decreased adverse events ANS: A Bodenheimer and Sinsky proposed a fourth aim “improved clinician experience” which brings to light the facts that the “joy” has gone out of practicing medicine. Other studies have shown that patient outcomes suffer if providers feel overwhelmed, overworked, or powerless. 169. The American Academy of Pediatrics questioned which of the following negative outcomes of Community Care Clinics (CCCs)? (Select all that apply.) a. Uneven EHR interoperability with community primary care providers b. Lack of longitudinal relationships with providers c. Incentives to overprescribe d. Increased patient satisfaction e. Decreased wait times ANS: A, B, C In 2014, the American Academy of Pediatrics had questions regarding CCCs and their possible incentives to overprescribe, lack of longitudinal relationships with providers, and uneven EHR interoperability with community primary care providers that may negatively impact the health care system. Chapter16 The Electronic Health Record and Clinical Informatics Multiple Choice 170. All of the following are reasons that attributed to the rise of AG-ACNP except: a. Intensivist physician shortages b. Rising cost of malpractice insurance for physicians c. Changes to medical resident work hour restrictions d. Increase in patients with complex medical conditions ANS: B The role of AG-ACNP rose out of an increased demand for practitioners to manage patients with complex medical conditions, shortages of intensivist physicians, and changes to medical resident and fellows work hour restrictions. 171. An increased spectrum of care affords the AG-ACNP the ability to provide medical care to a broader age group. Which of the following is age-range appropriate for an AG-ACNP to treat? a. Age 7 and older b. Age 13 and older c. Age 18 and older d. Age 21 and older ANS: B An AG-ACNP can provide care to patients aged 13 and older unless additional state or facility- specific restrictions exist. The age ranges are grouped into young adults, middle-age adults, and older adults. 172. As identified in a 2012 study by the ANCC, which of the following top workactivities for the AG-ACNP was number one when arranged by criticality? a. Conducting history and physical examinations b. Maintaining patient privacy and confidentiality c. Evaluating patients for safety and efficacy of interventions d. Assessing patients for urgent and emergent conditions ANS: B In 2012, the ANCC surveyed ACNP clinicians and identified top work activities for the AG-ACNP role. These activities were organized by criticality, or importance of the skill and determined by the requirement to perform the skill accurately each time, as a novice NP, and based on the risk of harm by performing the skill incorrectly. Maintaining patient privacy and confidentiality scored at the top. 173. Based on a survey of ACNPs, the following procedures are performed in a hospital-based setting most commonly by ACNPs except: a. Vasoactive intravenous drips b. Lumbar puncture c. Sutures d. Radiologic studies ANS: B Based on survey data, procedures that are formed least routinely by ACNPs include lumbar punctures, surgical first assist, thoracostomy tubes, cutdowns, paracentesis, joint aspirations, and bladder aspirations. 174. Based on a survey of ACNPs, which of the following procedures are performed in a hospital-based setting most commonly by ACNPs? a. Defibrillation b. Lumbar puncture c. Pacemakers d. Chest tubes ANS: A Based on survey data, procedures that are formed most commonly by ACNPs include radiologic studies, vasoactive intravenous drips, resuscitative efforts, defibrillation, wound care, sutures, incisions, and ventilation. 175. Which of the following is more commonly attributed to the AG-ACNP role versus that of a CNS? a. Patient-centered care b. System change responsibilities c. Performing procedures d. Staff education and development ANS: C The AG-ACNP and CNS both focus on patient-centered care. The AG-ACNP is more likely to spend a larger percentage of his or her time at the bedside using clinical skills to assess, diagnose, and treat patients with complex or acute medical conditions including performing procedures. Staff education and development and system change responsibilities are typically a larger portion of the CNS role. 176. Which of the following locations would be most appropriate for an AG-ACNP? a. Tertiary care management b. Billing and coding c. Primary care management d. Secondary care management ANS: A Tertiary care management includes the intensive care unit or emergency department and would be the best choice for this question. Although secondary care management is common, such as an inpatient unit or hospitalist position, most acute scenarios are encountered in the ICU or ED and more appropriate for the specialized skills of the AG-ACNP. It is important to note that any NP should have working knowledge of all practice areas, regardless of clinical specialty. 177. Educational programs that prepare students for AG-ACNP practice adhere to which of the following? a. Incorporates graduate core and NP curricula and adds AG-ACNP specialtycurricula b. Incorporates graduate core but replaces NP curricula with AG-ACNP specialtycurricula c. Requires additional training that is separate and in addition to the Adult-Gerontology curriculum and is only provided in DNP programs d. Deviates from the graduate core allowing full specialization of the AG-ACNP specialty curricula ANS: A The AG-ACNP curriculum incorporates the graduate core, advanced practice core, NP population curricula, and AG-ACNP specialty curricula. Programs that prepare AG-ACNPs at the DNP level do not negate the master’s core but, rather, build on it (AACN, 2006). 178. Which of the following organizations issue certification for AG-ACNPs? a. American Nurses Credentialing Center and the American Association of Gerontology b. The state where he or she intends to practice c. American Nurses Credentialing Center and the American Association of Critical-Care d. American Association of Critical-Care and the Emergency Nurses Association ANS: C American Nurses Credentialing Center and the American Association of Critical-Care issue certification for the AG-ACNP program. 179. An AG-ACNP is part of a practice group that employs both physicians and AG-ACNPs. The NP and a physician in the group both evaluate a patient on the same day. The NP sees the patient first. How should the services be billed to CMS using shared service guidelines? a. Combined and billed under the NP’s provider number b. Billed separately under each provider’s individual number c. Combined and billed under the physician’s provider number d. Billed under the AG-ACNP’s provider number ANS: C Shared E/M services can be billed under CMS guidelines as combined services if both the NP and the physician see the patient in a face-to-face visit on the same calendar day, regardless of order. If the physician does not have a face-to-face encounter the services should be billed under the NP’s provider number. Additionally, critical care time cannot be billed under shared billing. 180. How are provided critical care services billed by AG-ACNPs according to CMS? a. Standard charge per face-to-face encounter b. As part of DRG allocation monies bundled with hospitalist services c. Single charge per calendar day of service d. The number of critical care minutes spent ANS: D Critical care involves high-complexity decision making in the care of patients. Reimbursement is based on the number of critical care time in minutes spent by the provider and must be billed separately because care provided by NPs and PAs is billed at a lower rate. The first 30-74 minutes are billed and then separate billing for each additional 30 minutes of critical care time spent with the patient. 181. An AG-ACNP is part of a practice group that employs both physicians and AG-ACNPs. The NP and a physician in the group both evaluate a patient in the intensive care unit. The NP assesses and evaluates the patient first for 32 minutes followed by the physician for 20 minutes. How should the initial critical care time be billed? a. Combined and billed under the NP’s provider number b. Combined and billed under the physician’s provider number c. Billed under the AG-ACNP’s provider number d. Billed under the physician’s provider number ANS: C Billing of critical care time for the initial 30 minutes is billed under the provider number of whoever provided the service. It cannot be combined. Subsequent critical care minutes should be billed separately and also cannot be combined or linked. 182. Which of the following is a specialization opportunity most appropriate for an AG-ACNP? a. Rapid response ream b. Advanced diabetes manager c. Outpatient clinic supervisor d. Wound ostomy nurse ANS: A Although the AG-ACNP may be eligible to specialize in all of the areas, he or she would best be suited for a specialization that utilizes the acute care nature of his or her skills. Chapter17 IOM Core Competency: Utilize Informatics Multiple Choice 183. What distinct emphasis is made in midwifery practice when compared to that of physician OBGYNs? a. Surgical interventions b. Improved patient outcomes c. Patient autonomy d. Woman-centered care ANS: D Midwives and midwifery practice are different than that of physician obstetricians and gynecologists as midwifery is focused on woman-centered care with a strong belief in pregnancy and birth. Midwives focus on the normal life transitions as they relate to physiologic events, utilizing medical interventions only when needed based on a woman’s health status. 184. A registered nurse furthers his or her education in the discipline of midwifery, completes an accredited midwifery education program, and earns a graduate degree. What title does he or she receive after passing the certification examination? a. Licensed midwife (LM) b. Certified nurse-midwife (CNM) c. Certified midwife (CM) d. Certified professional midwife (CPM) e. Direct entry midwife (DEM) ANS: B A certified nurse-midwife (CNM) is a registered nurse who furthers his or her education in the discipline of midwifery, completes a program accredited by the Accreditation Commission for Midwifery Education, earns a graduate degree, and successfully passes the certification examination administered by the American Midwifery Certification Board (AMCB). 185. An individual obtains education in health and sciences, completes education in the discipline of midwifery, earns a graduate degree, and completes a midwifery education program accredited by Accreditation Commission for Midwifery Education (ACME). What certification does he or she receive? a. Certified professional midwife (CPM) b. Certified nurse-midwife (CNM) c. Certified midwife (CM) d. Direct entry midwife (DEM) e. Licensed midwife (LM) ANS: C The certified midwife (CM) allows for a non-nursing pathway to midwifery. It is not recognized in all 50 states. An individual may only take the CM certification examination administered by the American Midwifery Certification Board (AMCB) after obtaining the required health and sciences courses, completing education in the discipline of midwifery through an accredited program by the ACME, and obtaining a graduate degree. 186. An individual who completes the certification requirements set forth by the North American Registry of Midwives (NARM) may or may not complete an advanced degree. What certification does he or she receive? a. Certified midwife (CM) b. Certified professional midwife (CPM) c. Certified nurse-midwife (CNM) d. Direct entry midwife (DEM) ANS: B The certified professional midwife (CPM) certification is administered by the North American Registry of Midwives (NARM) and has two pathways to certification. An individual may complete a portfolio evaluation process (PEP) and complete an apprenticeship with no degree required or separately complete a formal education pathway. Currently, a CPM is not authorized to practice in all 50 states. 187. An individual wishes to have the ability to become licensed and practice midwifery in all 50 states. As of 2017, which certification should he or she obtain? a. Certified nurse-midwife (CNM) b. Licensed midwife (LM) c. Certified professional midwife (CPM) d. Certified midwife (CM) e. Direct entry midwife (DEM) ANS: A As of 2017, the certified nurse-midwife (CNM) is the only midwifery practice that is regulated and allows for certification and licensure in all 50 states. 188. All of the following are accurate statements regarding the CM certification except: a. Does not require a nursing degree b. Requires recertification every 5 years c. Requires a graduate degree d. Authorized to practice in all 50 states ANS: D Only the CNM is currently authorized to obtain licensure to practice in all 50 states. The certified midwife (CM) allows for a non-nursing pathway to midwifery. An individual may only take the CM certification examination administered by the American Midwifery Certification Board (AMCB) after obtaining the required health and sciences courses, completing education in the discipline of midwifery through an accredited program by the ACME, and obtaining a graduate degree. 189. How often is recertification required for a CNM by the AMCB? a. Every 2 years b. Annually c. Every 10 years d. Every 5 years ANS: D CNMs and CMs are required to complete recertification every 5 years. This includes completing three modules provided by the AMCB and two approved education units or retaking the AMCB certification examination every 5 years. 190. A CNM is unable to complete the required training modules for recertification in the timeline required by the AMCB. Which of the following will allow the CNM to recertify his or her certification? a. Complete five additional modules b. Retake the AMCB certification examination c. The CNM has forfeited his or her licensure d. Apply for partial certification ANS: B CNMs and CMs are required to complete recertification every 5 years. This includes completing three modules provided by the AMCB and two approved education units or retaking the AMCB certification examination every 5 years. 191. In 2015, CNMs/CMs attended many live births. Where did the majority of these births take place? a. Home or residence b. Hospitals c. Freestanding birth centers d. Other ANS: B CNMs/CMs attended 3,38,663 births according to 2015 data. The majority of midwife-attended births occurred in hospitals (94.2%) followed by freestanding birth centers (3%), and women’s homes (2.7%) (Martin, Hamilton, Osterman, Driscoll, & Matthews, 2017). 192. In 2015, CNMs/CMs attended what number of estimated live births in the United States? a. 3,93,345 b. 2,88,533 c. 3,64,234 d. 3,38,663 ANS: D CNMs/CMs attended 3,38,663 births according to the recorded 2015 data; this was an increase from previous years (Martin, Hamilton, Osterman, Driscoll, & Matthews, 2017). 193. The American College of Nurse-Midwives’ (ACNM) Code of Ethics ensures that CNMs and CMs follow three ethical mandates in achieving the mission of midwifery to promote the health and well-being toward women and newborns within their families and communities. Which of the following ethical responsibilities is not included in those three mandates? a. Toward the profession of midwifery b. For the public good for the benefit of all women and their families c. Toward the individual woman d. Toward the institutions ANS: D CNMs and CMs follow three ethical mandates in achieving the mission of midwifery to promote the health and well-being toward women and newborns within their families and communities. These mandates are directed toward the individual woman and their families, for the public good for the benefit of all women, and toward the profession of midwifery to fulfill the mission of midwifery. 194. As outlined in the Core Competencies for Basic Midwifery Practice by the ACNM which of the following is a CNM not trained to manage? a. Intrapartum care b. Prenatal care c. Basic care of a 35-day-old newborn d. Basic care of a 23-day-old newborn ANS: C Standard VI of the Core Competencies for Basic Midwifery Practice outlined by the ACNM states that CNMs should develop a plan and provide basic care of a newborn up to the first 28 days of life. 195. As outlined in the Core Competencies for Basic Midwifery Practice by the ACNM which of the following is a CNM not trained to manage? a. 30-year-old female for well woman care b. 30-year-old male for wellness care c. Sexually transmitted infection of a woman’s male partner d. Prenatal care ANS: B The Core Competencies for Basic Midwifery Practice outlined by the ACNM states that CNMs may manage sexually transmitted infections in women and their partners. It would not be appropriate for a CNM to treat an adult male routinely. 196. In a position statement published by the ACNM, how do requirements for signed collaborative agreements create an unfair economic disadvantage for CNMs and CMs? a. Limit ability for care to be provided in emergency relief situations b. Imply that CNMs and CMs require supervision in all situations c. Limit the number of midwives who can practice collaboratively with one physician d. Raise physician insurance premiums ANS: C The ACNM published a position statement regarding the requirements of collaborative agreements between physicians and CNMs and CMs. While all of the scenarios are created by the requirement of collaborative agreements, limiting the number of midwives who can practice collaboratively with one physician often restricts the number of midwives that can practice in a geographic region and also may allow economic competitors to dictate whether or not midwives can practice in a community. 197. A 2017 position statement published by the ACNM had recommendations for which of the following in an effort to reduce medical errors by CNMs and CMs? a. Violence against women b. Addiction in pregnancy c. Fatigue and sleep deprivation d. Depression in women ANS: C There is increasing evidence regarding the relationship of sleep deprivation and fatigue as they correlate to medical errors and burnout. The other titles are publications by the ACNM but pertain to the care of patients with those disorders rather than the safety and well-being of the CNMs and CMs. Chapter18 The Evolution of Nursing Science Test Bank Multiple Choice 198. Which of the following is true regarding CRNA practice? a. Youngest organized APN specialty b. Last APN specialty to require certification c. Oldest organized APN specialty d. Not considered an APN specialty ANS: C CRNAs are the oldest organized APN specialty. Alumnae from nurse anesthesia programs formed the National Association of Nurse Anesthetists (NANA) in 1931; the organization was renamed the American Association of Nurse Anesthetists (AANA) in 1939. 199. National Board of Certification and Recertification of Nurse Anesthetists (NBCRNA) prior to 2016 required CRNAs to be recertified at what interval? a. Every year b. Every 2 years c. Every 4 years d. Every 8 years ANS: B Prior to 2016 the NBCRNA required CRNAs to be recertified every 2 years. In 2016, the Continued Professional Certification (CPC) program took effect. This programrequires assessing continuing education credits, professional development credits, four core modules every 4 years, and a recertification examination every 8 years. 200. The current NBCRNA standards require recertification of CRNAs over what time period? a. Every 2 years b. Every 8 years c. Every 5 years d. Every 10 years ANS: B In 2016, the Continued Professional Certification (CPC) program took effect. This program requires assessing continuing education credits, professional development credits, four core modules every 4 years, and a recertification examination every 8 years. Prior to 2016 the NBCRNA required CRNAs to be recertified every 2 years. 201. Which of the following will be required to obtain CRNA certification for studentsstarting anesthesia programs in 2022? a. Doctoral degree b. Master’s degree or equivalent c. Master’s degree plus 320 hours supervised training d. Master’s degree plus 120 hours supervised training ANS: A Beginning January 1, 2022, all students entering anesthesia training will be required to be enrolled in a doctoral degree to obtain certification. 202. Due to increased requirements of CRNA education, the current required minimum length of programs is 24 months. When has the COA mandated a 36-month curriculum doctoral degree? a. By 2020 b. By 2019 c. By 2025 d. By 2023 ANS: C Beginning January 1, 2022, all students entering anesthesia training will be required to be enrolled in a doctoral degree to obtain certification for the 2025 deadline that requires 36 months of training. 203. CRNA students are required to perform a variety of specialized cases during their programs. How many total cases are required per the COA practice doctoral accreditation standards? a. 550 b. 600 c. 700 d. 500 ANS: B The COA requires participation in no less than 600 anesthesia cases including a variety of cases outlined in the COA guidelines. In 2017, the guideline for counting clinical experiences removed anatomic categories and articulates how students should document case experiences during their education. 204. According to an AANA member survey, approximately how many anesthesia cases are administered each year by CRNAs? a. 900 b. 1100 c. 1000 d. 1400 ANS: A AANA member surveys estimate that an average CRNA participates in approximately 900 cases per year. 205. Which of the following did CRNAs receive the ability to do in 1986? a. Direct billing under Medicare Part B b. Licensure in all 50 states c. Unrestricted practice authority d. Certification for invasive procedures ANS: A Direct billing was authorized by the Congress for CRNAs under Medicare part B in 1986. 206. Which of the following is most accurate regarding 2016 malpractice insurance premiums when compared to 1988 premiums for self-employed CRNAs according to AANA data? a. No change in premiums b. Premiums have decreased 33% c. Premiums have increased 25% d. Premiums have increased 33% e. Premiums have decreased 25% ANS: B In 2016, average malpractice premium for self-employed CRNAs was 33% lower than in 1988, or 65% lower when adjusted for inflation. 207. Which of the following statements about CRNA supervision and facility CMS billing is most accurate? a. CRNAs must be supervised by an anesthesiologist based on state requirements b. CRNAs must be supervised by an anesthesiologist for at least 1 year after initial certification c. CRNAs must be supervised by an anesthesiologist at all times d. CRNAs do not require supervision by an anesthesiologist ANS: A In a 2001 ruling by CMS, states were allowed to opt out of supervision requirement for CRNAs by anesthesiologists as it pertained to facility reimbursement requirements. There are no current statutory requirements for CRNAs to be supervised by anesthesiologists in general and they act as independent providers. The supervision is only required in a state that has not opted out of the federal supervision rule as it pertains to billing CMS. Currently, 17 states have opted out. 208. Which of the following is true regarding CRNAs and anesthesiologists with regard to the care provided? a. CRNAs providing anesthesia are considered to be practicing medicine b. Anesthesiologists may not supervise student nurse anesthetists c. CRNAs provide limited care only under supervision of anesthesiologists d. Both adhere to same standards of care ANS: D CRNAs and anesthesiologists both adhere to the same standards of care in practice. Student nurse anesthetists may be supervised by a CRNA or anesthesiologist at various times. 209. An anesthesiologist is supervising two CRNAs in a surgery center. Each of the CRNAs is supervising two student nurse anesthetists, for a total of four surgery cases. What percentage of physician reimbursement can the CRNA bill for each of the services? a. 75% b. 100% c. 25% d. 50% ANS: D There is a disincentive for CRNAs to supervise student nurse anesthetists when billing Medicare. The CRNAs may only bill for 50% of the physician reimbursement for services when supervising students. However, an anesthesiologist who supervises two medical anesthesiology residents may bill 100% of the physician reimbursement rate. Chapter19 Theory-Based Advanced Nursing Practice Test Bank Multiple Choice 210. Who promoted policy change first for the Crimean war soldiers and then later for the poor of London? a. Clara Barton b. Florence Nightingale c. Margaret Sanger d. Virginia Lynch ANS: B Florence Nightingale was a major promoter of policy change. She vowed to improve quality, dignity, and equity first for the Crimean war soldiers and then later for the poor of London. 211. Florence Nightingale was the first woman elected as a member of which of the following? a. The Nursing & Midwifery Council b. International Council of Nurses c. The Royal Statistical Society d. National Health Service e. American Nursing Association ANS: C The Royal Statistical Society elected Florence Nightingale as a member in 1858, making her the first female member. 212. Which of the following is the definition of policy? a. Decisions made by a judge resulting in law changes b. Variation among the interpretations by individuals of existing laws c. Decisions that result in a law or regulation d. Nonviolent process used to reach an agreement between differing viewpoints ANS: C Policy is the decisions that result in a law or regulation in society. Politics is best defined as the nonviolent process used to reach an agreement between differing viewpoints, often lawmakers. The other options are variations of specific points of policy and politics. 213. Which of the following is the best definition of politics? a. Nonviolent process used to reach an agreement between differing viewpoints b. Variation among the interpretations by individuals of existing laws c. Decisions made by a judge resulting in law changes d. Decisions that result in a law or regulation ANS: A Politics is best defined as the nonviolent process used to reach an agreement between differing viewpoints, often lawmakers. Policy is the decisions that result in a law or regulation in society. The other options are variations of specific points of policy and politics. 214. How does the US health system differ from that of other developed countries? a. No single entity responsible for health care policy development b. Poor access to health resources c. Single entity responsible for health care policy development d. State policies must always mimic national policies for conformity ANS: A In the US health care system no single entity is responsible for health care policy development. This often causes variable and fragmented health care changes. 215. Which of the following factors may make health care shift the most dramatical in the United States? a. Natural disaster b. Increase in retirement of providers c. Increase in cancer diagnosis rates d. Decrease in cancer diagnosis rates e. Political administration changes ANS: E Health care in the United States is political and may change with administration changes, sometimes radically. Natural disasters and the change in numbers of providers would more likely cause a slow change in how we provide health care over time. 216. The common practice in the United States where policies are modified on an ongoing basis rather than being reformed is referred to as: a. Professionalism b. Liberal advancement c. Federalism d. Theorism e. Incrementalism ANS: E Incrementalism is a common practice of US policymaking. It is where modest modifications are made to existing policies rather than reforming them entirely. Federalism is the practice of allocating governing responsibility among the federal government and the states. 217. Which model or concept of policymaking defines a policy formulation phase, implementation phase, and a modification phase? a. Policy Modification Model b. The Kingdon or Garbage Can Model c. Longest Model d. Knowledge Transfer Framework ANS: C The Longest Model highlights the cyclical and incremental nature of policymaking. It outlines three phases of policymaking: formulation phase, implementation phase, and modification phase. 218. Which of the following models or concepts specifies three conditions that open a “policy window” that allows policies to gain attention and passage? a. Longest Model b. Knowledge Transfer Framework c. The Kingdon or Garbage Can Model d. Policy Modification Model ANS: C The Kingdon or Garbage Can Model outlines a conceptualized open policy window where three conditions (problems coming to the attention of a policymaker, possible solutions that are tangible and available, and correct political circumstances) must be met to successfully make progress on the issue. 219. Which of the following models or concepts highlights the fact that previous policies may create unintended consequences? a. Longest Model b. Knowledge Transfer Framework c. Policy Modification Model d. The Kingdon or Garbage Can Model ANS: C Policy modification is the concept that policies that are enacted may have unintended consequences which is only learned after implementation of the policy. 220. Which of the following models or concepts highlights the importance of framing research in a policy context? a. Knowledge Transfer Framework b. Longest Model c. Policy Modification Model d. The Kingdon or Garbage Can Model ANS: A The Knowledge Transfer Framework highlights the importance of researchers to frame their research in a policy context to improve the transfer of information and subsequent policy changes. 221. Which of the following is a new focus for the US health care system to improve theissues that lead to poor quality of care? a. Correlating certification level to payment b. Increasing payment reimbursements for more experienced providers c. Linking medical professionalism to payment d. Linking quality to payment ANS: D One area to improve issues that lead to poor quality of care in the US health care system is the practice of linking quality of the care provided to payments. 222. Which of the following is a focus aimed at preventing payment for erroneous or poor care situations in the US health care system? a. Publicizing reports for total annual payments to providers b. Provider toxicology screening c. Reporting serious reportable events d. Background checks ANS: C Reporting of serious reportable events allow for the US health care system to identify negative or possibly negative outcomes and identify trends, thus penalizing payment for services to those providers or facilities. This brings attention to the importance of providing high-quality care without serious events. 223. Accountable care organizations (ACOs) who provide services to Medicare Fee-For- Service beneficiaries require what minimum number of beneficiaries to be enrolled? a. 1000 b. 7500 c. 12,500 d. 5000 e. 10,000 ANS: D ACOs provide an incentive for health care providers and hospitals to collaborate in the care of Medicare patients. ACOs are incentivized with payments that result from the percentage of shared savings for care provided to enrolled patients. ACOs must provide coverage for more than 5000 beneficiaries. 224. The US health care system is at a disadvantage due to which of the following? (Select all that apply.) a. Poor health behaviors b. Automobile domination of the built environment c. Poor social and economic conditions d. Fragmented health system ANS: A, B, C, D The US health care system is unfortunately not the best in the world although the United States spends at least 50% more per capita than other developed nations. Four factors that place the United States at a disadvantage are a fragmented health system, poor health behaviors, poor social and economic conditions, and automobile domination of the built environment, which minimizes walking as an important physical activity. Chapter20 Research: How Health Care Advances 225. An APRN questions the status quo and seeks out solutions that innovate upon practices at the hospital system where he or she is employed. This approach best defines which of the following? a. Modicum b. Freelancer c. Entrepreneurship d. Intrapreneurship e. Professionalism ANS: D Intrapreneurship by an APRN is the practice of innovation and creation of ideas that improve an existing institution or facility. A modicum is a small or limited amount of something. 226. An APRN begins his or her first job. Later he or she creates an independent network of APRNs eventually creating a new practice group that charges for services. This approach best defines which of the following? a. Professionalism b. Entrepreneurship c. Modicum d. Intrapreneurship e. Independent contractor ANS: B Entrepreneurship can take many forms for the APRN. It is the practice of building a business or practice that often is larger than themselves. 227. Which of the following factors likely has the largest impact on the success of intrapreneurship for an APRN in a health care environment? a. Financial support b. Level of education obtained c. Cash flow d. Organizational environment ANS: D Intrapreneurial success can depend on many factors, but the organizational environment, support, and flexibility often create the largest barriers to success in the health care industry. The other examples are more likely factors in entrepreneurship. 228. Which of the following examples would be best suited for an APRN seeking an intrapreneurial approach to practice? a. Innovating new ideas and strategies in a hospital system b. Providing services for an organization on a salaried basis c. Negotiating the purchase of an existing health care practice d. Starting his or her own outpatient clinic e. Volunteering at health care clinic for the underserved ANS: A Intrapreneurship by an APRN is the practice of innovation and creation of ideas that improve an existing institution or facility, often challenging the status quo. 229. Which of the following examples would be best suited for an APRN seeking an entrepreneurial approach to practice? a. Volunteering at health care clinic for the underserved b. Innovating new ideas to improve cost-effectiveness in a hospital system c. Obtaining a job as a staff APRN in a critical care unit d. Starting his or her own outpatient clinic e. Developing methods to decrease overtime costs in a hospital ICU ANS: D Entrepreneurship can take many forms for the APRN. It is the practice of building a business or practice that often is larger than themselves. Simply obtaining a job is not the best example of entrepreneurship. Innovating inside of an existing facility or business is best defined as intrapreneurship. 230. Which of the following is most likely an entrepreneurship activity? a. Developing telehealth services b. Using informatics to develop and implement new models of care delivery c. CRNA-owned anesthesia company d. CRNA-managed anesthesia services ANS: C Each of the examples could be construed as entrepreneurship; however, the formation of a company or clearly providing services for a fee is the best example. The other examples are examples of intrapreneurship as they are likely performed in an existing organization. 231. Which of the following is most likely an intrapreneurship activity? a. A nurse-midwifery consultant b. CRNA-owned anesthesia company c. Interprofessional health care business ventures d. CRNA-managed anesthesia services ANS: D Only the example that clearly defines an innovation or challenge to the status quo at an existing company organization would classify as intrapreneurship. 232. An APRN has enlisted the services of a professional recruiter for a job search. Which of the following could create a disadvantage when utilizing a recruiter? a. Recruiters are often more connected to multiple organizations b. Recruiters often have unpublished job opportunities c. A recruiter typically only gets paid based on successful placement of a candidate d. A recruiter may have an in-depth understanding of practice conditions ANS: C Using the services of a recruiter often has many advantages. However, it is important to highlight that all recruiters and staffing agencies are not created equal. Recruiters often receive payment only for candidates who are successfully placed in positions and may hold an institution’s success in higher regard to that of the interviewee. Recruiters should be used when there is a full understanding of the risks and benefits. 233. An APRN is interested in employment at a facility that does not currently have anyposted job openings, which of the following should the APRN do? a. Send his or her résumé b. Send an inquiry letter c. Send his or her curriculum vitae d. Wait until a job opening is posted ANS: B An inquiry letter is the best option. Inquiry letters may be sent individually or with an accompanying résumé highlighting the interest of the applicant for employment. 234. An APRN is applying for a new job. The prospective employer requires submission of a concise one-page document summarizing the APRN’s experience and education. Which of the following should the APRN submit? a. Inquiry letter b. Cover letter c. Curriculum vitae d. Résumé ANS: D A résumé is typically a one-page document that outlines the applicant’s experience. A curriculum vitae (CV) is a longer format document outlining the experiences and accomplishments of the applicant, typically without length restrictions. An inquiry letter is a submission to a prospective employer. A cover letter is a one-page document that is included with a résumé or CV. 235. Which of the following can be used by an APRN as a strategy to answer behavior-based and hypothetical questions? a. STATE Model® b. SHARE Model® c. CARE Model® d. DARE Model® ANS: B The SHARE Model® provides a strategy for answering behavior-based and hypothetical questions by (1) describing a specific situation, (2) identifying hindrances or challenges, (3) explaining the action taken, (4) discussing the results or outcomes, and (5) evaluating or summarizing what was learned. 236. Which of the following is the most important factor an APRN should know prior to requesting flexibility in a salary? a. Interviewer’s perception of APRNs b. Local area salary range c. Number of practicing APRNs d. APRN’s last salary ANS: B Although all of the items are important when negotiating salary ranges, local and regional geographic areas have varying needs or demands for APRN roles. Knowing the local area salary range for the position is paramount prior to accepting or negotiating salaries. 237. Which of the following is applicable if an APRN accepts an agreement to work as an independent contractor at a health care organization? a. APRN maintains behavioral control and organization maintains financial control of services provided b. Organization can require the APRN to work specific hours c. Organization maintains behavioral and financial control of services provided d. APRN maintains behavioral and financial control of services provided ANS: D The Internal Revenue Service places specific restrictions and regulations for independent contractors. Independent contractors must maintain behavioral and financial control of services provided for the classification. 238. An APRN is reviewing a contract with a potential employer and encounters a “covenant not to compete.” Which of the following is the best explanation of the purpose of these clauses? a. Protect investments by organizations in a geographical area b. Prevent competition from reasonable sources c. Prevent APRNs to earn a reasonable income d. Protect organizations from litigation in the future ANS: A Noncompete clauses are designed to protect an organization’s intellectual property, know-how, reputation, or investments in a geographical area or region. They typically require specific restrictions that require distance, length of time, and scope of limitations to be enforceable. Broad restrictions that prevent an APRN from earning a reasonable income are typically not upheld in a court of law. 239. An APRN has received an employment contract from a potential employer for his or her first job. The contract is 22 pages long and the APRN does not understand some of the terminology. Which of the following is the best next step by the APRN? a. Review the contract with a colleague who works at the organization b. Hire a contract attorney who specializes in health care employment contracts c. Request to review the contract with the organization’s attorney d. Review the contract entirely and research specific terms independently e. Read the contract and sign it since the organization may not hire the APRN if they refuse ANS: B Employment contracts can be confusing. As a new APRN the best option is to hire an attorney who specializes in health care employment contracts to review the contract. 240. An APRN is reviewing an employment contract as it pertains to malpractice insurance coverage. The insurance offers payment for claims but only if the claim occurs and is reported during the policy coverage period of time. This describes which type of coverage? a. Institutional liability coverage b. Occurrence coverage c. Tail coverage d. Claims-made coverage ANS: D Claims-made malpractice insurance covers claims that occur during the policy coverage period but only if the claim is also reported during the same policy period. Tail coverage must be purchased additionally to cover claims that may be reported after the policy period has ended. 241. An APRN is reviewing an employment contract as it pertains to malpractice insurance coverage. The insurance offers payment for claims that occur during the policy period and generally has no restrictions regarding when the claims are reported. This describes which type of coverage? a. Tail coverage b. Claims-made coverage c. Occurrence coverage d. Personal balloon liability coverage ANS: C Occurrence malpractice insurance covers claims that occur during the policy coverage period and has no restriction of time regarding when the claim must be reported. 242. An APRN who has practiced for 20 years is nearing retirement. He or she has no plans to continue working at his or her practice. Which of the following insurance malpractice types would be of greatest interest to the APRN at this time? a. Institutional liability coverage b. Tail coverage c. Occurrence coverage d. Claims-made coverage ANS: B When an APRN is changing jobs or nearing retirement they should obtain tail coverage malpractice insurance. Some employment contracts include this and can be a large financial incentive. Tail coverage covers claims that are made during a previous policy period but are reported after the policy has ended. Tail coverage is typically purchased in addition to claims- made policies. 243. Which of the following will most likely increase the success of employment of an APRN in a new market? (Select all that apply.) a. Sending multiple résumés b. Joining local or national organizations c. Volunteer opportunities d. Understanding geographical limitations ANS: B, C, D APRNs are typically well suited to enter the job market but commonly encounter many hurdles. Professional networking whether through peers, volunteer opportunities, online support groups, or national organizations as well as understanding geographic limitations or restrictions can further the APRN’s success. Simply sending multiple résumés is inappropriate without adequate understanding of the APRN’s unique value to an organization or institution, geographic restrictions, and other issues that may arise. Chapter21 Evidence-Based Practice Multiple Choice 244. Which of the following must an APRN obtain to be classified as a provider by an insurer such as CMS? a. APRN education completion b. DEA number c. National Provider Identifier d. National certification number ANS: C The National Provider Identifier (NPI) number is a unique number that is provided by CMS for all covered professionals. The NPI number is the core requirement to be classified as a provider. The NPI number does not necessitate that claims will be approved or that state or local certifications or educational requirements have been met. 245. An APRN is working in an outpatient care clinic. He or she is required to select a level of service code to bill for services provided after evaluating and providing care to a patient. Which of the following type of codes should be selected? a. CPT codes b. ICD-9 codes c. ICD-10 codes d. HCPCS codes e. MS-DRG codes ANS: A The Current Procedural Terminology (CPT) codes are numbers that are assigned across six areas of inpatient and outpatient services provided. HCPCS are similar to CPT codes but are for services not included in CPT codes and for durable medical equipment. MS-DRG codes are for inpatient hospital stays. ICD codes are for diagnosis identification and link to CPT codes. 246. An APRN is viewing a report for his or her billed outpatient clinic visits by CPT code. He or she notices the following totals: 25 coded as 99212, 15 coded as 99213, and 5 coded as 99214. Which of the following assumptions can be made regarding the APRN’s practice? a. There was an equal distribution of the level of services provided b. No assumptions can be made c. The billing practices of the APRN are suspicious d. The majority of visits were at a higher level of service e. The majority of visits were at a lower level of service ANS: E CPT codes include a five-digit number. The last number in the sequence is the complexity of the service provided with 1 being the lowest level of service and 5 as the highest. The majority of visits provided by this APRN were at a lower level of service or complexity. 247. How are CPT codes used by the APRN for initial hospital visits? a. Time in minutes spent by provider b. Complexity of documentation c. Severity of illness d. Number of patient medical conditions ANS: B CPT codes used for the initial hospital visit of a patient are based on the complexity of documentation of the APRN. The severity of illness of the patient, number of patient medical conditions, and time spent should typically be reflected in the complexity of the documentation completed. If complex patients are evaluated and poorly documented there may not be an appropriate billing of CPT code, leading to loss of revenue for time spent. 248. How are ICD-10-CM codes used by an APRN for identification of medical conditions? a. Identify the etiology, anatomic location, and severity but not external causes b. Identify the etiology and anatomic location only c. None of the above is accurate regarding ICD-10-CM codes d. APRNs do not utilize ICD-10-CM codes e. Identify etiology, anatomic location, external causes, and severity ANS: E ICD-10-CM codes are complex identifiers of diagnosis and include etiology, anatomic location, external causes, and severity as well as other identification types. 249. Of the six sections for CPT codes, which of the following would be utilized when billing for the services he or she provided as an APRN in a clinic setting? a. Surgery b. Anesthesia c. Medicine d. Pathology and laboratory e. Evaluation and management ANS: E CPT codes include billing for inpatient and outpatient services provided. They include six areas: evaluation and management, pathology and laboratory, surgery, anesthesia, medicine, and radiology. Evaluation and management CPT codes are most commonly used by APRNs in a clinic setting. 250. A patient’s progress during a hospital stay must be documented. A subsequent hospital visit code is used each day after admission. Which of the following is true regarding the use of CPT codes used by the APRN on progress notes? a. Requires repetition of all content from admission notes b. Level of service does not vary c. Does not require repetition of all content from admission notes d. Medical decision making is not taken into account ANS: C Subsequent hospital visit CPT codes are used for each day the patient is in the hospital after the admission or initial hospital visit code. They still vary in level of service and take into account the medical decision making and complexity of documentation. Subsequent hospital visit bills do not require the repetition of all details from the initial hospital visit, only relevant details pertaining to the patient’s current condition. 251. Which of the following services would be billed under Medicare Part A? a. Ambulance transportation b. Durable medical equipment c. Outpatient diagnostic testing d. Inpatient hospital stay e. Prescription drugs ANS: D Medicare Part A covers services for critical access hospitals, short-term care in skilled nursing facilities, postinstitutional home health care, and hospice care. 252. Which of the following primarily provides funding for Medicare Part A coverage? a. Excise taxes b. Sales taxes c. Monthly premiums of subscribers d. Payroll taxes ANS: D Medicare Part A is primarily funded by payroll taxes. Medicare Part B is primarily funded by monthly premium payments from subscribers. 253. Which of the following services would be billed under Medicare Part B? a. Maintenance therapy prescription drugs b. Hospice services c. Inpatient hospital stay d. Ambulance transportation e. Acute therapy prescription drugs ANS: D Medicare Part B covers physician and nonphysician provider services, outpatient hospital services, home health care not covered by Part A, and other services including diagnostic testing, durable medical equipment, and ambulance costs. 254. Which of the following allows for private health insurance companies, such as HMOs and PPOs, to provide Medicare benefits? a. Medicare Part D b. Medicare Part C c. Medicare Part B d. Medicare Part A ANS: B Medicare Part C is also referred to as the Medicare Advantage plan. It allows private health insurance companies to provide benefits to Medicare recipients. They may vary in requirements and rules but must provide the same benefits as Medicare. 255. Which of the following would be billed under Medicare Part D? a. Outpatient diagnostic testing b. Inpatient hospital stay c. Durable medical equipment d. Ambulance transportation e. Prescription drugs ANS: E Medicare Part D provides payment for prescription drugs. Each recipient must enroll in a program operated by a commercial insurer. 256. Which of the following is the primary purpose of the CHIP? a. Provide health coverage to elderly patients who cannot afford Medicare premiums b. Provide health coverage to children whose families earn too much to qualify Medicaid c. Increase access to Medicaid services for all ages d. Provide health coverage to the homeless ANS: B The CHIP, or Children’s Health Insurance Program, provides well-baby/well-child care and immunizations to children who may not be eligible or covered by other services. 257. An APRN is reviewing billing charges at an outpatient care clinic where he or she works. They notice that the billing charges reflect higher charges than that of the care that was actually provided. Which of the following is true? a. The clinic is solely responsible for the increased billing charges b. Inflating coding charges is common and has no negative consequences c. The provider is responsible d. The provider has no responsibility for the actions of the clinic ANS: C While both the organization and the provider could be held liable for the inflated billing charges, ultimately the provider is responsible for ensuring that the charges submitted for payment accurately reflect the level of care provided. 258. Which of the following billing practices is considered a middle ground between providers being paid for each individual service provided and “lump sum” payments for patients regardless of the number of services provided? a. Bundled payment b. Government fee-for-service c. Capitation d. Private health fee-for-service e. Managed care contracts ANS: A Bundled payments or global bundled payments are considered a middle ground for payment extremes. They provide payment for episodes of care and are based on an estimated total cost of care. Capitation is a lump sum payment for all services, regardless of services provided. 259. How do bundled payments decrease overall health care expenditures? a. Increased focus on the care of chronic disease processes b. Require organizations to reduce their direct costs of each individual service c. Link payment reimbursements to patient outcomes d. Highlight importance of patient satisfaction e. Require organizations to focus on decreasing unnecessary testing or patient complications ANS: E Bundled payments provide a single payment for a service (such as cardiac surgery) that includes all ancillary services attributed to that service. The health care system that receives a bundled payment is responsible for the costs of any complications and follow-up care related to the service. This requires organizations to decrease unnecessary testing and reduce complications and readmissions relating to the original service. 260. All of the following are requirements for an APRN regarding shared visit billing at a 100% reimbursement rate except: a. Proper physician note linked to APRN note b. Within APRN’s scope of practice c. Face-to-face visit by the physician encountered on same day d. Physician present in office suite or practice at time of APRN visit e. Provide the same service as physician ANS: D Shared visit billing for 100% reimbursement requires that the APRN provide the same level of service as the physician, on the same day of encounter, within the APRN’s scope of practice, and the physician must perform a face-to-face encounter with the patient and document a physician note that links to the APRN’s note. 261. All of the following are requirements for an APRN regarding incident to billing at a 100% reimbursement rate except: a. Physician present in office suite or practice at time of APRN visit b. Proper physician note that is linked to APRN note c. Physician sees patient on initial visit d. Some frequency of physician participation in plan of care ANS: B Incident to billing by an APRN at 100% reimbursement rate includes three major criteria including that the physician sees the patient on the initial visit, is present in the office suite or practice on subsequent visits, and maintains some frequency of physician participation in the plan of care. Physician note documentation that is linked to APRN care is required for shared visit billing. 262. If all of the criteria are not met for shared visit or incident to billing, which of the following rates of reimbursement must the APRN adhere to? a. 85% of physician rate b. There are no reductions in billing rates c. 90% of physician rate d. 75% of physician rate e. 50% of physician rate ANS: A If all of the criteria are not met for shared visit or incident to billing the visit is billed at 85% under the APRN’s provider number. 263. Which of the following are used by Medicare to calculate the relative value unit (RVU) that drives the payment amount for a particular service or procedure? (Select all that apply.) a. Malpractice insurance b. Payor mix c. Practice expenses d. Time or work ANS: A, C, D Medicare reimbursement for services is based on a mathematical calculation for each service provided. The calculation includes the time or work, costs of running a practice, and professional liability insurance premiums in addition to a modifier for geographic location. The number derived from this calculation is known as the relative value unit or RVU. Chapter22 Clinical Scholarship and Evidence-Based Practice Multiple Choice 264. Which of the following are components of the LACE network that support implementation of the Consensus Model for APRN regulation? a. Licensure, acceptance, certification, and education b. Liability, acknowledgment, compliance, and excellence c. Licensure, accreditation, compliance, and education d. Licensure, accreditation, certification, and education ANS: D The organizations that make up the LACE network include those for licensure, accreditation, certification, and education. They work together to move forward the process of implementation of the Consensus Model. 265. Which of the following is an optional process for educational organizations to obtain? a. Licensure b. Certification c. Credentialing d. Accreditation ANS: D Accreditation is an optional process for educational institutions in many instances. Accreditation is performed by outside agencies that review the processes and strategies of the institution thereby creating a metric of the quality of education. 266. Which of the following provides authorization through a state agency to engage in the APRN role? a. Licensure b. Certification c. Accreditation d. Regulation e. Credentialing ANS: A Licensure is completed by state agencies to provide authorization to engage in the APRN role. Certification is often a prerequisite to licensure. 267. Which of the following must an APRN undergo to validate their knowledge, skills, and abilities to perform their desired role? a. Credentialing b. Regulation c. Accreditation d. Licensure e. Certification ANS: E Certification involves a formal process to review a candidate’s knowledge, skills, and abilities to perform a specific role. This formal process is often completed through examination in the APRN role. 268. Which of the following is the process of collecting and verifying an individual’s professional qualifications that may grant their eligibility to sit for an examination? a. Regulation b. Accreditation c. Credentialing d. Certification e. Licensure ANS: C Credentialing is an umbrella term that refers to regulatory mechanisms that can be applied broadly to individuals, programs, or organizations (Styles, 1998). 269. An APRN has recently graduated from his or her program of choice, obtained national certification, and is applying for licensure in his or her home state. Which of the following is true regarding prescriptive authority? a. Requires additional CE requirements to maintain b. Provided in all states with APRN licensure c. Requires separate licensure d. Varies among individual states and regulating agencies ANS: D Prescriptive authority remains as a regulatory hurdle for APRNs. Requirements for obtaining prescriptive authority vary among states and have various requirements to maintain licensure. 270. An APRN has obtained prescriptive authority in his or her state and obtained Drug Enforcement Administration (DEA) number. All of the following pertain to controlled substances except: a. An APRN individually cannot prescribe controlled substances without a DEA number b. DEA numbers are site-specific and an APRN must obtain a DEA number for each site where he or she prescribes controlled substances c. Obtaining a DEA number authorizes the prescription of controlled substances without additional regulation d. An APRN who does not prescribe controlled substances is not required to obtain a DEA number e. A DEA number authorizes prescription of controlled substances as it pertains to state regulation ANS: C DEA numbers authorize the prescription of controlled substances but are still regulated by both federal and state regulations. APRNs may be subjected to additional regulation in the state where he or she practices. 271. All of the factors must be present for a malpractice case to demonstrate negligence by an APRN except: a. Direct causation must be linked to the APRN b. The patient must be under the direct care of the APRN c. A duty of care must be owed to the injured party d. Damages or sustained injuries to the patient e. The accepted standard of care was breached ANS: B Four factors must be established for the basis of a malpractice claim including a duty of care being owed, a breach of accepted standards of care, resulting damages or injury to the patient, and direct causation that is linked to the APRN. The patient does not have to be under the direct care of the provider to be included in a malpractice suit. 272. Which of the following requires compliance with HIPAA while functioning as an APRN? a. Transmission of health information for payment of medical claims b. All of the above c. Transmission of health information in any form d. Regular care of patients e. Discussion of patient conditions with consultants ANS: B The Health Insurance Portability and Accountability Act (HIPPA) originally became law in 1996 and mandates all medical professionals adhere to patient privacy standards when pertaining to personally identifiable patient information, regardless of transmission method. Chapter23 Birth of Transcultural Nursing to Current Theories and Conceptual Models for Cultural Diversity Multiple Choice 1. All of the following are purposes for patient outcomes to be reported except: a. Improve care delivery b. Satisfy federal requirements c. Supplemental revenue stream d. Improve patient outcomes ANS: C It is a requirement of both federal and state regulatory agencies that outcomes are measured and reported. Additionally, they allow institutions to improve patient outcomes and improve care that is delivered through careful analysis. Measuring outcomes does not correlate with additional revenue, but instead with the maximum revenue available. A percentage of payments are withheld and, upon successfully reporting and achieving outcomes that meet the benchmarks set forth by The Patient Protection and Affordable Care Act’s Value-Based Purchasing initiative, the additional withheld funds are then dispersed. The percentage withheld of Diagnosis-Related Group (DRG) payments in 2017 was 2%. This practice will likely change under MACRA in 2019. 2. Which of the following is an identified reason for not tracking APRN-specific outcomes today? a. Fear of superior APRN outcomes b. Underutilization of APRNs c. Lack of funding d. Lack of systems matching provider to patient ANS: D While all of the factors may contribute to the lack of tracking and reporting APRN-specific outcomes, a lack of ability for institutions to match specific patients to APRN-specific provided care is the largest identified challenge as of the writing of this text. The importance of APRN- provided care will continue to need to be validated and reinforced. 3. A conceptual model that was developed in Canada for ACNPs and adapted from a nurse role effectiveness model comprised of primary components that focus on structure, process, and outcome is best known as: a. Nurse Practitioner Role Effectiveness Model b. Outcomes Evaluation Model c. Hamrick Model d. Donabedian Model ANS: A The Nurse Practitioner Role Effectiveness Model was developed in Canada as a derivative of the Donabedian Model and adapted the nurse role effectiveness model. 4. The Donabedian Model identifies which of the following as predicting a higher likelihood of successfully identifying APRN impact on outcomes? a. Comparing components directly to physician care b. Inclusion of at least two components c. Measuring components nationwide d. Isolation of a single component ANS: B The inclusion of all or at least two of the components of the Donabedian Model is correlated with a more successful identification of an APRN’s impact on care delivery outcomes. 5. Multiple studies have compared APRN care to physician care in the United States and Canada. What have these results mostly shown? a. The care provided is equivalent across all categories b. The care provided is mostly equivalent, with patient satisfaction from APRN care superior to physician care in some studies. c. Physician care is superior to APRN care d. APRN care is superior to physician care ANS: B APRN care as compared to physician care has shown that APRN care is equivalent and in some outcomes such as patient satisfaction, APRN care is higher. 6. Which of the following should be the focus of APRN care in the future? a. National APRN outcomes compared to physician outcomes b. APRN patient wait times c. APRN mortality rates d. The unique aspects of APRN-provided care ANS: D Many studies have demonstrated that APRN care is comparable to physicians and other providers. The future benefit for furthering the APRN role should be to highlight the unique aspects of APRN- provided care and benefits for further expansion of the role. 7. In an analysis of CNM-provided services compared to physicians, which of the following was reported in 2006 when analyzing pregnant women and cesarean delivery rates? a. Physician and CNM care showed no difference in deliveries b. Physician care resulted in 1.7 times less cesarean deliveries c. APRN care resulted in 1.7 times more live births d. CNM care resulted in 1.7 times less cesarean deliveries ANS: D A 2006 report showed that when comparing CNM to physician care, patients cared for by CNMs were 1.7 times less likely to undergo cesarean delivery. 8. All of the following factors make comparisons between APRN and physicianproductivity difficult except: a. Inequality of APRN role b. Lack of focus on patient outcomes c. Unequal provider reimbursement rates d. Increased time spent with patients by APRNs ANS: A Comparing APRN to physician productivity is especially difficult. A lack of focus on patient outcomes and primary focus on reimbursement rates often skew an analysis since APRNs historically spend more time with their patients than physicians. Conversely, an inequality of roles is a specific reason of why productivity must be measured to validate APRN practice rather than a barrier to measure productivity. Chapter24 Global Diversity Test Bank Multiple Choice 273. In 1999, the IOM reported that at least 44,000 people die in hospitals each year as a result of which of the following? a. Falls b. Medical errors c. Unaffordable health care d. Lack of access to primary care ANS: B The 1999 IOM report To Err Is Human: Building a Safer Health System revealed that at least 44,000 and as many as 98,000 people die in hospitals each year due to preventable medical errors. 274. The American Recovery and Reinvestment Act was signed by President Barack Obama in 2009 and mandated which of the following for health care? a. National standards for APRNs b. EHR use c. Increased funding for APRN education programs d. Expansion of the APRN role ANS: B The American Recovery and Reinvestment Act provided up to $29 billion for the adoption and utilization of EHRs in health care facilities and also led to the development of meaningful use requirements of electronic medical records by January 1, 2014, to maintain Medicaid and Medicare funding levels. 275. The requirement that outlines that a facility must utilize an EHR and technology that meets government criteria, exchanges standardized health data and information, advances clinical processes, and reports quality measures is defined as: a. Adverse event reduction b. Meaningful use c. Informatics d. Health care standardization ANS: B Meaningful use is the specific utilization of technology in health care to improve outcomes, engage patients and families in their own care, improve care coordination, increase population health, and improve diagnostic accuracy while decreasing costs and test duplication. 276. In 2016, the Office of National Coordinator for Health Information Technology devised a 10-year road map detailing which of the following? a. Interoperability b. HIPAA c. EHR utilization d. Adverse events ANS: A The Interoperability Road Map released in 2016 highlights the importance for connectedness among EHRs to improve access to patient records and test results to increase continuity of care. 277. The design and implementation of health information exchanges (HIE) offer the opportunity for which of the following? a. Decreased cost of testing b. Access to standardized health data c. Reduced dependence of EHR vendors d. Increased billing efficiency ANS: B Health information exchanges offer access to medical records and patient health data so that they may be accessed by providers at any time. This allows for increased continuity of care and decreases the need for duplicate testing whether it be inside of an organization or nationwide. 278. Improved documentation through more detail by an APRN will directly affect which of the following coding types as related to increased reimbursement? a. CPT b. SNOMED CT c. MS-DRG d. RxNorm e. LOINC ANS: C Medicare Severity Diagnosis-Related Groups (MS-DRGs) are utilized by hospitals for reimbursement for a patient’s hospitalization costs. They are weighted on the detail of the examination and level of medical decision making as represented solely by the documentation completeness. 279. Alphanumeric designations maintained by the World Health Organization that correlate with nearly every procedure, diagnosis, symptom, and cause of death are known as which of the following? a. LOINC b. SNOMED CT c. ICD-10-CM d. CPT e. HCPCS ANS: C The WHO maintained the ICD taxonomy, now in its tenth revision. 280. Which of the following coding taxonomies is used worldwide to best identify medical laboratory tests and clinical observations? a. MS-DRG b. RxNorm c. CPT d. SNOMED CT e. LOINC ANS: E LOINC is a naming taxonomy that focuses on medical laboratory tests and clinical observations. In 2015 an alpha version forged from an agreement with SNOMED CT allowed for a more powerful integration of these two taxonomies. 281. Which of the following provides a standardized naming convention allowing forsemantic interoperation between systems for pharmaceuticals from the National Library of Medicine? a. ICD-10-CM b. RxNorm c. ICT-10-PCH d. CPT e. MS-DRG ANS: B RxNorm is a normalized data set maintained by the National Library of Medicine to allow for interoperability between systems for pharmaceutical trade names, brand names, and dosages. 282. Documentation through the use of ICD or SNOMED CT codes allows for documentation to be queried. This is best described as: a. Discrete or unstructured data b. Nondiscrete or structured data c. Nondiscrete or unstructured data d. Discrete or structured data ANS: D Discrete or structured data that are “coded” through the use of systems such as ICD, SNOMED CT, and others allow for compilation, evaluation, and analysis of the information in a quick and efficient way. 283. Documentation that is hand written in long form or dictated without the use of diagnosis codes cannot be easily queried. This is best described as: a. Discrete or unstructured data b. Nondiscrete or unstructured data c. Discrete or structured data d. Nondiscrete or structured data ANS: B Nondiscrete or unstructured data refer to information that is not systematically organized such as dictated reports, handwritten progress notes, or those that contain natural language. This type of data requires additional effort and time for analysis and compilation. 284. An APRN wishes to become familiar with all of the reporting measures or metrics required by his or her specific practice. Which of the following would be the best resource for this information? a. National Institutes of Health b. The Joint Commission c. National Quality Forum d. Medicaid Adult Health Care Quality Measures Program ANS: C The National Quality Forum (NQF) Community Tool to Align Measurement provides a resource and hyperlinks to quality measures and the information they collect. 285. Many reporting requirements of APRNs require data that are patient, provider, or facility specific and reported to CMS directly from the organization. Which of the following aggregates the subjective patient experience information regarding the care received? a. MACRA b. CAHPS c. NQF d. HIPAA ANS: C The Consumer Assessment of Health Care Providers (CAHPS) is a format for surveying patients to collect their patient experiences. They include those on providers (CAHPS), hospitals, home health agencies, and hospice care (HCAHPS), among others. CAHPS is not a measure of patient satisfaction but a measure for patient experience that is made available to the public. 286. Which of the following legislation will change Medicare payments beginning January 1, 2019, away from the existing fee-for-service system to one that is based on as well asrewards quality in care? a. CAHPS b. Values-Based Modifier c. MACRA d. Meaningful use ANS: C The Medicare Access and CHIP Reauthorization Act took effect on January 1, 2017, with final implementation on January 1, 2019. This combines three existing programs: the Physician Quality Reporting System (PQRS), the Value-Based Payment Modifier, and meaningful use into one system that provides both financial incentives and penalties based on quality of care, outcomes, and efficiencies. The initial 2 years are intended to collect and analyze data and for hospital systems and providers to see the future impact to their reimbursement. 287. In an effort to further link care, such as that provided by an APRN to patient outcomes and reporting measures, which of the following additional requirements was included in MACRA? a. Individual billing by each provider b. Limiting the number of specialists for each area of care per patient c. Assigning patient-provider relationship identifiers d. Estimating percentages of time care was given by each provider ANS: C MACRA mandated the assignment reporting the relationships of patients to providers’ NPI numbers to CMS for the purpose of individualizing care reports. 288. What is the purpose of the TIGER Competencies as applicable for an APRN? a. Identify new quality outcomes metrics specific for APRNs b. Increase awareness for health literacy in technology-challenged geographic areas c. Improve nursing practice, education, and delivery of patient care through the use of HIT d. Implement standardization for EHR documentation for APRNs ANS: C The Technology Informatics Guiding Education Reform (TIGER) initiative was formed in 2004 to bring together nursing stakeholders to collaborate to improve nursing practice, education, and delivery of patient care through the use of HIT. This involves recommendations for basic computer competencies, information literacy, and information management. 289. The practice of designing measurement process, collecting and analyzing data, and presenting the data back to stakeholders in a timely and understandable manner is known as which of the following? a. Information technology b. Scientific theory c. Scientific method d. Data analytics ANS: D Data analytics is the process of designing processes, collecting and analyzing data, and then presenting the same data in an understandable manner. It specifically focuses on the identification of metrics and analysis of those metrics to be formed into reports. 290. An APRN is reviewing his or her CAHPS scores for his or her facility and personal provider number. The patient experience information is displayed as a list of monthly percentage of hospital readmissions. This is best described as: a. Statistical process control b. Predictive analytics c. Descriptive analytics d. Prescriptive analytics ANS: C Descriptive analytics describes a retrospective trend or outcome. They are simply values based on data that are displayed as a means to identify positive or negative deviation above or below a target, typically in percentages, rates, means, and ratios. Descriptive analytics answers the question: “What has happened?” Descriptive analytics that are displayed in a graphic format over time is an example of a statistical process control analysis. 291. An APRN is reviewing outcomes measures regarding the number of falls at the facility where he or she is employed. The APRN utilizes several tools to identify possible interventions for improvement. Which of the following would best be used for indicating possible changes in falls in the future? a. Prescriptive analytics b. Data mining c. Statistical process control analysis d. Predictive analytics e. Descriptive analytics ANS: D Predictive analytics uses previous trends to identify interventions that can be implemented to impact results in the future. Predictive analytics are heavily being utilized for outcomes like readmission rates as EHRs allow for quicker analysis of large groups of data to implement education strategies. Predictive analytics best answers the question: “What could happen?” 292. An APRN wishes to analyze his or her patients in a primary care practice. He or she wishes to identify patient trends of vitals and laboratory results and then automatically intervene to recommend global changes in case based on evidence-based practice to improve quality metrics. This type of data analysis is best known as which of the following? a. Descriptive analytics b. Statistical process control analysis c. Prescriptive analytics d. Predictive analytics e. Data mining ANS: C Prescriptive analytics best answers the question: “What should we do?” This type of data analysis is not too far off in the health care information technology world as EHR use and widespread interoperability of systems increase. Automatically suggesting diagnosis, treatments, calculating risks, and other metrics for the APRN are no doubt to be the new standard of care. Chapter25 Health Services for Special Populations 1. The inhabitants of Yulupa, California, form which of the following? 1) Aggregate 2) Community 3) Population 4) Vulnerable population ANS: 3 A population is all of the people inhabiting a specified area. In contrast, a community is a group of like-minded individuals or one whose members have a common purpose, and an aggregate has shared characteristics. A vulnerable population is an aggregate with increased risk for poor health outcomes. PTS: 1 DIF: Moderate REF: p. 1499 KEY: Nursing process: Assessment | Client need: SECE | Cognitive level: Application 2. A community health nurse prepares for a new assignment. She has been assigned census tracts 131 and 132. This large area crosses the border of two towns and includes 4,000 people. What components of the community must the community health nurse assess prior to beginning her new assignment? 1) Income levels, health status, and relationships among groups 2) Structure of the tracts, effectiveness of the community, and current status 3) Number of clients with health problems compared to the number of healthcare providers 4) Community organizations and beliefs about their role in the community ANS: 2 To understand a community and its needs, the nurse must assess the communitys structure, status (the biological, social, and emotional outcome components of the community), and process (overall effectiveness of the community). Income level and demographic data, such as community organizations and healthcare providers, are included in the assessment of the community structure. The number of clients with health problems is only a part of the assessment of the community status. PTS:1DIFifficultREF:p. 1500 KEY: Nursing process: Assessment | Client need: SECE | Cognitive level: Analysis 3. A community health nurse is evaluating the current health programs in the community. Which of these outcomes would indicate a healthy community? 1) Ninety percent of members report adequate access to primary care services. 2) Immunization services are available at hospitals and clinics. 3) Affordable housing in the community is under construction. 4) Mortality rates have been stable over the past 5 years. ANS: 1 Evidence of health in a community can be judged by examining progress in the focus areas delineated in Healthy People 2020. Access to primary care services is a measurable outcome that provides evidence of effectiveness of health programs. The availability of immunization services at the hospital or at many offices does not provide evidence that these services are being utilized. Similarly, the fact that affordable housing is under construction does not mean that it is being accepted and used or that enough is being built. Mortality rates may be stable but could be quite high and within unacceptable parameters. PTS:1DIFifficultREF:p. 1500 KEY: Nursing process: Evaluation | Client need: SECE | Cognitive level: Analysis 4. What is the type of nursing with a focus on the community as a whole and the health status of individuals as an aggregate? 1) School nursing 2) Community health nursing 3) Community-oriented nursing 4) Public health nursing ANS: 4 Public health nursing focuses on the community at large and the eventual effect of the communitys health status on the health of individuals, families, and groups. Community health nursing focuses on the health of individuals, families, and groups and on how their health affects the health of the community. Community-oriented care combines elements of community health nursing and public health. School nursing focuses on optimizing health for a community of students in a school setting. PTS: 1 DIF: Moderate REF: p. 1501 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 5. The community health nurse is working with the residents of government-subsidized senior housing. She meets with them regularly to discuss concerns and evaluate whether they receive healthcare that meets their needs. Which of the following nursing roles best describes these actions? 1) Case manager 2) Client advocate 3) Collaborator 4) Counselor 5) Educator ANS: 3 As a collaborator, the nurse forges partnerships and coalitions that can effectively address common concerns among different communities. In this role, the nurse facilitates discussion to work toward problem resolution. As a case manager, the nurse makes referrals to or collaborates with other health and social agencies. In the client advocate role, the nurse supports the identified or voiced concerns of the client or community. As an educator, the nurse focuses on wellness and disease prevention through patient teaching. A counselor offers practical solutions to resolve problems. PTS:1DIF:ModerateREF:p. 1502 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 6. A community health nurse gathers information about how individuals in a low-income neighborhood perceive the community and its state of health. Which of the following assessment strategies would be appropriate? 1) Conducting a windshield survey while driving 2) Reviewing a multitude of community databases 3) Interviewing residents living on every fifth block 4) Analyzing demographic data on the community ANS: 3 To assess community perceptions, the nurse will need to interact with a cross-section of the community. Interviewing residents is one way to find out about community concerns and opinions. The other methods are assessment strategies that will provide data about the community but do not offer information on how community members view the community. PTS:1DIF:ModerateREF:pp. 1506-1507 KEY: Nursing process: Assessment | Client need: SECE | Cognitive level: Application 7. The community health nurse has gathered data about the community. She identifies many weaknesses in the community health system that contribute to poor health outcomes. What should be her next step? 1) Prioritize the list of problems. 2) Validate the data. 3) Evaluate the effectiveness of the interventions. 4) Plan the care. ANS: 1 After a thorough assessment, the nurse compiles a list of community strengths and weaknesses. Once this list is in place, the nurse must prioritize the list considering the client needs, funding, and political feasibility. PTS:1DIF:ModerateREF:p. 1507 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Analysis 8. The similarities between the Omaha System and the NANDA-I taxonomy are that both contain which of the following? 1) Evaluation tools expressed in standardized language 2) Nursing diagnoses expressed in standardized language 3) Diagnoses, outcomes, and interventions 4) Labels that are intended for use in any healthcare setting ANS: 2 NANDA-I and the Omaha System both contain nursing diagnoses expressed in standardized language. The Omaha System also contains outcomes and interventions. The Omaha System was developed for use in community settings, whereas NANDA-I may be used in all settings. PTS:1DIF:ModerateREF:p. 1507 KEY: Nursing process: Diagnosis | Client need: SECE | Cognitive level: Analysis 9. A nurse serving the community in a public health role would likely perform which of the following functions within a particular community? 1) Tracking the prevalence of gonorrhea between January and June 2) Screening for scoliosis among 12- to 14-year-old girls in middle school 3) Weighing premature infants receiving phototherapy at home 4) Giving the H1N1 vaccine to fire and police personnel ANS: 1 Public health nursing focuses on the community at large and the eventual effect of the communitys health status on the health of individuals, families, and groups. The goal of public health is to prevent individual disease and disability, in addition to promoting and protecting the health of the community as a whole, such as tracking the prevalence of disease. Activities, such as scoliosis screening, home care, and vaccination program, are examples of community health nursing. PTS:1DIF:ModerateREF:p. 1501 KEY: Nursing process: Interventions | Client need: HPM | Cognitive level: Application 10. A community health nurse planning a new program for teen pregnancy prevention designs a community assessment covering the structure of her target. Which of the following areas would she include? 1) Number of residential and commercial buildings 2) Demographic data of the residents 3) Morbidity and mortality rates of the population 4) Common strategies for conflict resolution ANS: 2 Structure refers to the general characteristics of a community. These include demographic data, such as gender, age, ethnicity, and educational and income levels, as well as data about healthcare services, such as the number of primary care providers or emergency departments in the area. PTS:1DIF:ModerateREF:p. 1500 KEY: Nursing process: Assessment | Client need: HPM | Cognitive level: Application 11. A patient was involved in a motor vehicle accident that resulted in multiple traumatic injuries. He was hospitalized for 8 days in the intensive care unit and 3 days on the surgical floor. He has been discharged home with home health support. Identify the primary goal of his home care: 1) Provide comprehensive direct care. 2) Promote sleep and rest for healing. 3) Teach the patient and family how to provide care. 4) Explain how home care differs from hospital care. ANS: 3 The primary goal in home healthcare is to promote self-care. Nursing activities are directed at fostering independence or teaching the family or other caregivers to assist the client with ongoing needs. Care continues to be comprehensive; however, rather than providing direct care for all needs, the emphasis shifts toward fostering independence. PTS:1DIF:ModerateREF:p. 1510 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Application 12. Today is the last day of work on the medical-surgical unit for a nurse who has decided to work in home care. A patient asks her why she is going to home care. Select a response that best illustrates the advantages of home care. 1) Care is much more comprehensive and unhurried in the home; it is more enjoyable for nurses to work in home care. 2) Home care is much more organized than hospital care; you have access to the whole team, and there is less interference from others. 3) A home health nurse has more autonomy and skills than a hospital nurse; Ill get to do more. 4) In home care I can see my patients in their personal environment; this will help me understand them more and allow me to give personalized care. ANS: 4 The home is the clients personal environment: a window into the patients life. The nurse is able to see how the patient lives, interacts, and negotiates the world. Care, in the home and hospital, is comprehensive. In both locations, the nurse has obligations to other patients and will need to watch her schedule. The level of enjoyment a nurse has with her job is dependent on many factors. A disadvantage to home care is the lack of immediate assistance from other members of the health team. Home care nurses may be more autonomous than hospital nurses; however, their scope of practice is identical. PTS:1DIF:ModerateREF:p. 1511 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 13. A 56-year-old man is hospitalized because of poorly controlled diabetes and a leg ulcer that developed as a complication of diabetes. He is awake, alert, and oriented but fatigued and in need of wound care. In the hospital, he was placed on insulin and started on a variety of oral medications. He is learning how to check his blood sugar and administer insulin. He has never given himself insulin, and he does not understand how to interpret his blood sugar readings. The physician has prescribed discharge from the hospital with home health follow-up. Is this an appropriate referral? 1) Yes; the patient is in need of skilled services and, therefore, is eligible for home care services. 2) Yes; the patient has been unable to control his diabetes, is noncompliant, and needs to be monitored. 3) No; the patient should remain hospitalized; he has too many needs for home care services. 4) No; the patient is relatively young and oriented; he should be able to provide his own care. ANS: 1 A client must require skilled services in order to be eligible for home care services. This patient needs wound care, to be taught about diabetes care, and to be monitored. These are all skilled services. All of these needs can be met with home care services. He is alert and oriented, which is important for planning teaching sessions. PTS:1DIFifficultREF:p. 1511 KEY: Nursing process: Assessment | Client need: SECE | Cognitive level: Synthesis 14. A home health nurse is working with a physical therapist and home health aides to work out a schedule for their visits that will best address the patients needs. Which nursing role does this demonstrate? 1) Direct care provider 2) Client and family educator 3) Client advocate 4) Care coordinator ANS: 4 A care coordinator manages and coordinates the services of members of the healthcare team and develops a plan of care that addresses the clients needs. Direct care involves hands-on tasks, such as dressing wounds and administering medications. The educator role involves communicating with clients and families to help them develop the skills involved to administer self-care. A client advocate supports the clients right to make decisions and protects the client from harm if he is unable to make decisions. PTS:1DIF:EasyREF:p. 1512 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Application 15. A home health nurse has called his patient to arrange an initial home visit and has driven to the home. What is the nurses objective in the first few minutes of the visit? 1) Develop rapport and trust with the patient and family. 2) Gather demographic data and complete the referral form. 3) Assess the patients most important health needs. 4) Determine the patients needs for ongoing care. ANS: 1 All of these objectives are appropriate for the home health visit. However, the first few minutes of the initial visit set the tone for the relationship among client, nurse, family, and agency. In that time, the nurse focuses on developing rapport and trust. Once rapport and trust have been developed, the nurse can gather data, assess the client, and determine the need for ongoing care. PTS: 1 DIF: Moderate REF: p. 1516 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Synthesis 16. Documentation in home healthcare may take many forms. Some nurses use NANDA-I terminology for diagnoses, whereas others use the Clinical Care Classification (CCC) system. The chief benefit of the CCC system is that it: 1) Contains diagnoses specific to home care, whereas NANDA-I does not. 2) Is simpler to use and more readily understood by other disciplines. 3) Is linked to the OASIS reporting forms required by Medicare. 4) Uses standardized terminology, whereas NANDA-I does not. ANS: 3 Home care nurses more commonly use the CCC because it is linked to the OASIS reporting forms required by Medicare. The CCC was developed for use in home care; however, the diagnoses themselves are not specific to home care. They can be used in any setting. NANDA-I, NIC, and NOC all use standardized language that may be used in any setting, including home healthcare. NIC and NOC have some interventions and outcomes that are specific to home care use. PTS:1DIF:ModerateREF:p. 1517 KEY: Nursing process: Diagnosis | Client need: SECE | Cognitive level: Analysis 17. A 56-year-old woman provides care to her 91-year-old widowed father. She says she is frequently fatigued and that she no longer socializes with her friends. Im so busy taking care of my dad. Its really hard work because he is bedridden. Sometimes it breaks my heart when I have to feed and bathe him. He always seemed so strong when I was a child. The most appropriate nursing diagnosis for this woman is: 1) Caregiver Role Strain 2) Impaired Home Maintenance 3) Interrupted Family Processes 4) Risk for Caregiver Role Strain ANS: 1 This caregiver is experiencing fatigue, isolation, and difficulty adjusting to role changes. These are signs of Caregiver Role Strain. Because symptoms exist, this is an actual problem as opposed to a potential problem. There is no evidence of Impaired Home Maintenance. Although family processes have been altered, this is not the best nursing diagnosis based on the defining characteristics given. PTS: 1 DIF: Moderate REF: p. 1517 KEY: Nursing process: Diagnosis | Client need: SECE | Cognitive level: Application 18. The nurse is visiting a patient who lives in a single-room occupancy hotel. The patient requires wound care and medication management. There is no running water in the room, and the bathroom down the hall is in disrepair and filthy. The patients room is not clean. What supplies would be essential for the nurse to bring with him when visiting this client? 1) All wound care supplies needed for the duration of the care 2) Reclosable plastic bags for disposal of old dressings 3) Small, biohazard sharps container to be left in the room 4) Waterless, antibacterial hand sanitizer solution ANS: 4 The nurse should use a waterless antibacterial hand sanitizer in place of soap and water because there is no sink and conditions are filthy. The nurse should limit the supplies brought into the home if the conditions are not clean. Wound care supplies, for example, would be ordered and kept in the home. Old dressings should be double-bagged to prevent leakage, and discarded in the home. There is no evidence that a sharps disposal container is needed. PTS: 1 DIF: Moderate REF: p. 1520 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Application 19. Which of the following unique aspects of home care do Medicare reimbursement regulations require that the nurse include in documentation? 1) Patient assessment data and interventions performed 2) Patient response to care and assessment of environment 3) Evidence of homebound status and continued need for skilled care 4) Skilled care delivered and communication with other providers ANS: 3 All of the aspects mentioned should be documented. However, the unique requirements of home care include documentation of homebound status and the continued need for skilled care. PTS:1DIF:ModerateREF:p. 1513 KEY: Nursing process: Evaluation | Client need: SECE | Cognitive level: Application 20. At a home visit, the nurse asks the patient, Have you taken your blood pressure medicine today? The patient replies, I dont remember. Maybe. On the table are several bottles of medication, some open, some not. They have all been prescribed for the patient. The patient cannot say how often to take each one, when asked. A compartmentalized medication organizer is on the table, with a few capsules in it, and some compartments left open. What should the nurse do? 1) Show the patient how to put the medications in the organizer for the next 2 days, and observe while he fills the rest of the organizer. 2) Arrange for a home health aide to come each day to show the patient which pills to take. 3) Administer todays medications and arrange for the pharmacy to put medications in easy-to-open containers in the future. 4) Fill the organizer for each day of the week, explain how to use it, and return in a day or two to evaluate ANS: 4 From the cues given, it seems likely the patient would not be able to accurately load the medication organizerand, in fact, may not be able to use it properly to take the correct medications at the correct time. The nurse would need to return every day or so until he is certain that the patient can actually administer his own meds after someone else loads the organizer. Showing the patient how to load the organizer solves part of the problem; however, this would not allow the nurse to evaluate whether the patient would then know to take the medications each day. Home health aides cannot be responsible for patient medications. There is no indication that the patient is having difficulty opening his medication containers, so there is no need to talk to the pharmacy. PTS:1DIFifficult REF: p. 1519; critical thinking needed to answer question KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 21. A family caregiver is learning to administer insulin injections to her homebound sister. What should the nurse advise her to do with the used needles? 1) Discard the needle and syringe in a thick plastic milk jug with a lid. 2) Securely recap them and place them a paper bag in the household trash. 3) Remove the needle and put it in a coffee can with a lid; put the syringe in the trash. 4) Do not recap the needle; break it by bending it on the tabletop. ANS: 1 The caregiver should discard the syringe and needle in a thick plastic milk jug with a lid, a metal coffee can with a lid, or a commercial sharps container. Patients and caregivers should not recap used needles. They should not remove the needle from the syringe or attempt to break it because this increases the risk of needlestick injury. PTS:1DIF:ModerateREF:p. 1520 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application Multiple Response Identify one or more choices that best complete the statement or answer the question. 1. A community health nurse prepares for a new assignment. She has been assigned census tracts 131 and 132. This large area crosses the border of two towns and includes 4,000 people. As a community health nurse, she recognizes that assignments are based on census tracts because census tracts do which of the following? Choose all that apply. 1) Define the geopolitical boundaries of a community. 2) Are made up of persons who share a common heritage and customs. 3) Divide populations into smaller groups that can be assessed more readily. 4) Are natural divisions in communities that are based on voting patterns. ANS: 1, 3 Census tracts are derived from the national census. They typically include 1,500 to 8,000 people. The area of the tract varies based on the density. Census tracts show geopolitical boundaries that are useful to anyone who studies the characteristics and concerns of smaller groups of people. PTS:1DIF:ModerateREF:p. 1499 KEY: Nursing process: Assessment | Client need: SECE | Cognitive level: Comprehension 2. A community health nurse is assigned to work in a different area of the city. Which of the following assessment techniques would she likely use to develop an overview of the community? Choose all that apply. 1) Windshield survey 2) Review of demographic data 3) Physical assessment of a sample of the inhabitants 4) Review of the records of area providers ANS: 1, 2 A windshield survey and review of demographic data provide data about the community. She may interview area residents about their experiences or ideas about this community; however, physical examination of a sample of the inhabitants would not give her community-level data. Similarly, she may wish to meet with area providers, but reviewing their records violates HIPAA laws and assumes that the records accurately reflect the health concerns of the population. PTS:1DIF:ModerateREF:p. 1506 KEY: Nursing process: Assessment | Client need: SECE | Cognitive level: Application 3. Which of the following groups represents a vulnerable population? Choose all that apply. 1) Homeless persons with no known illnesses 2) Women who have experienced domestic violence 3) Fifth-grade students at the local elementary school 4) Persons with type 1 diabetes mellitus ANS: 1, 2, 4 Vulnerable populations include those with limited economic or social resources, the very young and the very old, those with chronic disease, and people who have experienced abuse or trauma. PTS:1DIF:ModerateREF:pp. 1500-1501 KEY: Nursing process: Assessment | Client need: Physiological Integrity | Cognitive level: Application 4. Which of the following is a primary intervention? Choose all that apply. 1) Immunization for meningitis of college-bound students 2) Safer sex education for high school students 3) Lobbying for health education in the schools 4) Tuberculosis screening via PPD testing ANS: 1, 2, 3 Primary interventions are interventions that occur before disease appears. The goal of primary interventions is to promote health and prevent disease. Secondary interventions aim to reduce the impact of the disease process by early detection and treatment. Tertiary interventions aim to halt disease progression and restore client functioning. PTS:1DIF:ModerateREF:p. 1503 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 5. Identify the nurse who is acting as a community health nurse. Choose all that apply. 1) School nurse who provides screening and direct care in the elementary school 2) Parish nurse who offers health education after services each Sunday 3) Nurse who works for the Red Cross by providing disaster relief 4) A nurse administering vaccines to inmates in a correctional facility ANS: 1, 2, 3, 4 Community health nurses function as client advocates, counselors, case managers, educators, and collaborators for patients and their families in the community setting. All of these nurses are working in community health settings in roles as school nurse, parish nurse, disaster nurse, and prison nurse. PTS: 1 DIF: Easy REF: pp. 1501-1503 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Comprehension 6. Which of the following interventions has a public health focus? Choose all that apply. 1) Controlling the blood sugar of a diabetic client with cardiovascular disease 2) Assisting with the launch of an after-school program in a high-crime neighborhood 3) Providing an influenza vaccination program for seniors and persons with chronic illness 4) Offering counseling to the family of a child with severe cognitive deficits ANS: 2, 3 Public health nursing focuses on the community at large and the eventual effect of the communitys health status on the health of individuals and families. Diabetic care is focused on individual health. Family counseling is focused on family health. PTS:1DIF:Moderate REF:p. 1501; question involves critical thinking with synthesis of information acquired from reading this passage KEY: Nursing process: Interventions | Client need: HPM | Cognitive level: Application 7. Which of the following clients would most likely require home health services? Choose all that apply. 1) 45-year-old man with an injured rotator cuff that requires surgery 2) 32-year-old terminally ill woman with a supportive family 3) 92-year-old man living independently with multiple medical problems 4) 6-year-old with a fractured hip requiring a leg and pelvic cast ANS: 2, 3 Home care is appropriate for a client with health needs that exceed the abilities of family and friends. Older adults who wish to avoid placement in a skilled nursing facility, those who require ongoing skilled care after discharge from the hospital, the terminally ill, and persons with chronic illness that must be monitored to avoid hospitalization are the most likely home health clients. PTS:1DIF:Moderate REF: p. 1510; critical-thinking item requires synthesis of knowledge acquired from passage KEY: Nursing process: Assessment | Client need: PHSI | Cognitive level: Application 8. Which of the following services are provided by home health agencies? Choose all that apply. 1) Direct care of clients in the home, performing treatments 2) Indirect care such as provision of medication and supplies 3) Acute care services for clients with complex diseases 4) Respite care of clients to relieve family caregivers ANS: 1, 2, 4 Home care agencies provide direct, indirect, and respite care in the home. Acute care services are provided in the hospital. PTS:1DIF:ModerateREF:p. 1511 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Comprehension 9. Home healthcare and home hospice care are two different types of home health services. What are the differences between these services? Choose all that apply. 1) Home healthcare promotes independence in clients; home hospice care promotes comfort and quality of life. 2) Home healthcare promotes comfort and symptom management; hospice care promotes self-care. 3) Home healthcare is focused on teaching self-care; home hospice care is focused on teaching skilled care to caregivers. 4) Home hospice care is focused on managing symptoms; home healthcare is focused on fostering independence. ANS: 1, 4 The purpose of home healthcare is to promote self-care and foster independence. The purpose of home hospice care is to promote comfort and quality of life by managing symptoms. PTS: 1 DIF: Moderate REF: p. 1512 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Analysis 10. The nurse has been assigned to a caseload of home health clients. Before making home visits, which two planning activities must she perform first? 1) Order supplies for the home care services. 2) Review the cases to determine the reasons for the visits. 3) Contact the clients to arrange for the visits. 4) Develop a schedule for the day so that all visits can be made. ANS: 2, 3 All of these interventions are appropriate. However, it is essential to determine the nature of the visits and to secure permission for visiting before the nurse can order supplies and plan her day. PTS: 1 DIF: Difficult REF: p. 1514 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Application 11. The nurse is visiting a client who resides in a single-room occupancy hotel. Groups of people are leaning against the building and smoking on the steps. There is obvious drug abuse occurring in the lobby and halls of the building. There is no running water in the room, and the bathroom down the hall is in disrepair and filthy. A primary concern that the nurse must consider when making this visit is safety. Which of the following actions are appropriate safety measures? Choose all that apply. 1) Notify the police that the nurse plans to visit this site. 2) Carry something that can be used as a weapon if necessary. 3) Inform the home health agency of the nurses route and time of visit. 4) Do not visit if the nurse senses danger when he arrives at the site. ANS: 3, 4 Safety is a primary consideration in home care. The nurse should file a route and planned schedule with the agency. In addition, he should not enter the building if he feels he may be in danger. He should notify the police if he senses danger, but not to tell them of a planned visit. The nurse should always carry a cell phone to alert police when security is threatened. It is not recommended that the nurse carry a weapon. PTS:1DIF:ModerateREF:pp. 1514-1515 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 12. The nurse is visiting a patient who lives alone in a two-room house. The patient requires wound care and medication management, but his health is not expected to improve much, even with care. There is no running water in the house, and the bathroom is in disrepair and filthy. At the first home visit, which of the following should the nurse assess? Choose all that apply. 1) Wound status 2) Patient concerns 3) Ability to perform care independently 4) End-of-life planning ANS: 1, 2, 3 The nurse should assess the patients status, condition of the wound, concerns, and ability to perform care independently. End-of-life care is a topic the nurse may wish to explore after a relationship has developed. PTS:1DIF:Easy REF:pp. 1516-1517; critical-thinking item requiring synthesis of previously acquired knowledge KEY: Nursing process: Assessment | Client need: PHSI | Cognitive level: Application True/False Indicate whether the statement is true or false. 1. Florence Nightingale is known as the first community health nurse. ANS: F Florence Nightingale was influential in community health because she established the importance of promoting health by manipulating the environment. Lillian Wald is known as the first community health nurse. PTS:1DIF:ModerateREF:p. 1502 Chapter26 Introduction to Ethics 1. A 77-year-old woman with an inoperable brain tumor has been hospitalized for the past 5 days. Her daughter comes to visit her. The patient has asked that her daughter not be told her diagnosis. After visiting with her mother, the daughter asks to speak to the nurse. She says, My mother claims she has pneumonia, but I know she is not telling me the truth. The daughter asks the nurse to tell her what is truly wrong with her mother. The nurse should tell her that: 1) Her mother has an inoperable brain tumor, but does not wish anyone to know. 2) She needs to speak to the physician in charge of her mothers care. 3) Her mother has requested that her case not be discussed with anyone, not even family. 4) Her mother is very sick with a serious case of pneumonia that could lead to death. ANS: 3 The nurses first allegiance is to the patient and her desire for confidentiality. Telling the daughter to speak to the physician would place the physician in the same position as the nurse. Telling her that her mother has pneumonia would be a lie. The nurse, of course, should inform the physician of the patients wishes so that he will be prepared if the daughter questions him about her mothers health condition. PTS:1DIF:ModerateREF:p. 1529 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 2. Which of the following terms refers to the ethical questions that arise out of nursing practice? 1) Nursing ethics 2) Bioethics 3) Ethical dilemma 4) Moral distress ANS: 1 Nursing ethics refers to ethical questions that arise out of nursing practice. Bioethics is a broader field that refers to the application of ethics to healthcare. An ethical dilemma occurs when a choice must be made between two equally undesirable actions, and there is no clearly right or wrong option. Moral distress occurs when someone is unable to carry out his or her moral decision. PTS:1DIF:ModerateREF:V1, p. 1526 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 3. A belief about the worth of something that serves as a principle or a standard that influences decision making is called which of the following? 1) Morals 2) Attitudes 3) Beliefs 4) Values ANS: 4 A value is a belief you have about the worth of something that serves as a principle or a standard that influences decision making. Morals are private, personal, or group standards of right and wrong. Attitudes are mental dispositions or feelings toward a person, object, or idea. A belief is something that one accepts as true. PTS: 1 DIF: Difficult REF: p. 1530 KEY: Nursing process: N/A | Client need: N/A | Cognitive level: Recall 4. A 45-year-old patient is ventilator dependent after a high cervical neck injury. He is conscious and competent and has decided that he wants to be removed from the ventilator. His family and the multidisciplinary team agree. The nurse believes the patient intends suicide and would prefer he choose differently but says nothing. The nurse remains at the bedside holding the patients hand. In this instance the nurse is displaying which of the following? 1) Value set 2) Value system 3) Value neutrality 4) Value awareness ANS: 3 Value neutrality occurs when we put aside our own values regarding an issue in order to provide nonjudgmental care to clients. A value set is your list of values. A value system is your value set with the values ranked on a continuum from most important to least important. PTS:1DIF:ModerateREF:p. 1532 KEY: Nursing process: Interventions | Client need: PSI | Cognitive level: Application 5. A 45-year-old patient is ventilator dependent after a high cervical neck injury. He is alert and oriented and, after giving it much thought, has decided that he wants to be removed from the ventilator. The nurse believes the patient intends suicide but supports his final decision. When the ventilator is removed, the nurse remains with the patient to support him. The nurses action demonstrates respect for what moral principle? 1) Nonmaleficence 2) Autonomy 3) Beneficence 4) Fidelity ANS: 2 Autonomy refers to a persons right to choose and his ability to act on that choice. In this case, the nurse respects the patients right to choose to die. Nonmaleficence is the twofold principle of doing no harm and preventing harm. Beneficence is the duty to do or promote good. Fidelity is the obligation to keep promises. PTS:1DIF:ModerateREF:p. 1534 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Comprehension 6. Which of the following consequentialist theories takes the position that the value of an action is determined by its usefulness? 1) Ethics of care 2) Utilitarianism 3) Deontology 4) Categorical imperative ANS: 2 Utilitarianism is a consequentialist theory that takes the position that the value of an action is determined by its usefulness. An ethics of care is a nursing philosophy that directs attention to the specific situations of individual patients viewed within the context of their life narrative. Deontology considers an action to be right or wrong independent of its consequences. A categorical imperative is a principle, established by Immanuel Kant, that states that one should act only if the action is based on a principle that is universal. PTS:1DIF:EasyREF:p. 1532 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Comprehension 7. The ability of nurses to base their practice on professional standards of ethical conduct and to participate in ethical decision making is known as which of the following? 1) Ethical agency 2) Attitudes 3) Belief 4) Value neutrality ANS: 1 Ethical agency is the ability of nurses to base their practice on professional standards of ethical conduct and to participate in ethical decision making. Attitudes are mental dispositions or feelings toward a person, object, or idea. A belief is something that one accepts as true. Value neutrality is when we attempt to understand our own values regarding an issue and to know when to put them aside, if necessary, to become nonjudgmental when providing care to clients. PTS: 1 DIF: Moderate REF: p. 1527 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Comprehension 8. Identify the third step in the MORAL decision-making model. 1) Reassess the dilemma 2) Resolve the dilemma 3) Review the problem 4) Recall the history of the problem ANS: 2 MORAL is an acronym for the following steps: M, Massage the dilemma; O, Outline the options; R, Resolve the dilemma; A, Act by applying the chosen option; L, Look back and evaluate. PTS: 1 DIF: Easy REF: pp. 1540-1541 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 9. A patient has asked the nurse to explain her laboratory results. The nurse informs the patient that he must first assist another patient to the bathroom and then he will explain the results. The nurse assists the other patient to the bathroom and then returns to explain the results to the patient. What moral principle has the nurse displayed? 1) Nonmaleficence 2) Autonomy 3) Beneficence 4) Fidelity ANS: 4 Fidelity is the obligation to keep promises. Autonomy refers to a persons right to choose and his ability to act on that choice. Nonmaleficence is the twofold principle of doing no harm and preventing harm. Beneficence is the duty to do or promote good. PTS:1DIF:ModerateREF:p. 1535 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 10. The nurse is a member of the ethics committee. An alert, oriented, and competent 87- year-old man has asked to have a DNAR order put on his chart. The patients family does not agree with his decision and requests the ethics committee to intervene on their behalf. The ethics committee would most likely use which model in this patients case? 1) Social justice 2) Patient benefit 3) Autonomy 4) DNAR determination ANS: 3 The autonomy model is useful when the patient is competent to decide. This model emphasizes patient autonomy and choice as the highest values. The patient benefit model assists in decision making for the incompetent patient by using substituted judgment. The social justice model focuses more on broad social issues involving the entire institution rather than on a single patient issue. There is no DNAR determination model. PTS:1DIF:ModerateREF:p. 1542 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Synthesis 11. A 60-year-old patient with a treatable form of breast cancer has decided not to pursue radiation or chemotherapy. The nurse believes that the patient should be treated. She coerces her into receiving treatment by continuing to remind the patient about her responsibilities for raising her children. What type of behavior has the nurse displayed? 1) Nonmaleficence 2) Autonomy 3) Paternalism 4) Beneficence ANS: 3 Paternalistic behavior occurs when the nurse thinks she knows what is best for a competent patient and coerces the patient to act as she wishes rather than to act as the patient originally desired. Autonomy refers to a persons right to choose and his ability to act on that choice. Nonmaleficence is the twofold principle of doing no harm and preventing harm. Beneficence is the duty to do or promote good. PTS:1DIF:ModerateREF:p. 1535 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 12. Nursing codes are: 1) Legally binding. 2) Not legally binding. 3) Legally binding in some circumstances. 4) Not admissible in court. ANS: 2 Codes of ethics are open to public scrutiny. The ethical aspects of nursing work, just like the technical aspects, are subject to review by professional groups and licensure boards, which may use sanctions to punish code violations. However, nursing codes are not legally binding. PTS:1DIFifficultREF:p. 1536 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 13. An alert, oriented, and competent frail older adult man has been told that he is dying and has asked to have a DNAR order put on his chart. The patients family does not agree with his decision and asks the healthcare team to ignore the request. After a great deal of discussion among the physician, nurse, and family, they are no closer to resolution of the conflict. The nurse asks the hospital chaplain to come and help the family and the team understand each others opposing views. Which step of the MORAL model does this illustrate? 1) MMassage the dilemma 2) OOutline the options 3) RResolve the dilemma 4) LLook back and evaluate ANS: 2 This illustrates the Outlining-options step. In Massaging the dilemma, the team would already have identified and defined the issues in the dilemma, and considered the values and options of all the major players. At the Outlining the options step, someone should delineate all of the options to all parties, including those that are less realistic and conflicting. In that step, someone often asks a member of the ethics committee or the hospital chaplain to help the parties understand the opposing viewpoints. Resolving the dilemma is the step in which all the options are reviewed and basic moral principles and frameworks are applied to arrive at a decision. Looking back to evaluate is done after a decision has been made and acted on. At that time, the entire process, including the consequences, is evaluated to determine how well it worked. PTS: 1 DIF: Difficult REF: pp. 1540-1541 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Application 14. An alert, oriented, and competent frail older adult man has been told that he is dying, and has asked to have a DNAR order put on his chart. The patients family does not agree with his decision and asks the healthcare team to ignore the request. The healthcare team does not comply with the familys wishes, and after several days the family takes the matter to court. The court sides with the family and orders the healthcare team to remove the DNAR order. This is an example of which of the following? 1) An integrity-producing (good) compromise 2) An ethically sound compromise 3) Settlement of an issue by force 4) An effort to keep peace on the unit ANS: 3 This is clearly an example of settling an issue by force, bringing in a more powerful entity (the court) to force the healthcare team to do what the family wants. It is not a compromiseof any sortbecause neither party backed away from its original position, and the action that was taken was not agreed on by both parties. This was not an effort to keep peace. The familys effort was to settle the disagreement in their favor. If the healthcare teams goal had been to keep peace on the unit, they would have acceded to the familys wishes without the need for court order. PTS:1DIFifficultREF:p. 1542 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Application Multiple Response Identify one or more choices that best complete the statement or answer the question. 1. Which of the following is an example of whistle-blowing? Choose all that apply. 1) Reporting fraudulent billing practices 2) Reporting patients health status against the patients wishes 3) Reporting unsafe work practices 4) Reporting a coworker for working under the influence of drugs ANS: 1, 3, 4 Reporting a patients health status against the patients wishes is a breach of patient confidentiality. Whistle-blowing is identifying incompetent, unethical, or illegal situations or actions of others in the workplace and reporting to someone who may be in a position to rectify the situation. Fraudulent billing practices are illegal and unethical; unsafe work practices are unethical and illegal; and a coworker under the influence of drugs is a risk to patients, as well acting in an illegal and unethical manner. PTS: 1 DIF: Moderate REF: p. 1528; requires critical thinking KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Analysis 2. The nurses obligations in ethical decisions include which of the following? Choose all that apply. 1) Be a patient advocate. 2) Involve institutional ethics committees. 3) Improve ones own ethical decision making. 4) Respect patient confidentiality. ANS: 1, 2, 3, 4 The nurses obligations in ethical decisions include being a patient advocate, using and participating in institutional ethics committees, and improving ethical decision making. Confidentiality is a basic patient right. The nurses role is to uphold that right. PTS:1DIF:ModerateREF:p. 1542 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application Completion Complete each statement. 1. refer to private, personal, or group standards of right and wrong. ANS: Morals PTS:1DIF:EasyREF:p. 1526 KEY: Nursing process: N/A | Client need: N/A | Cognitive level: Comprehension 2. refers to the application of ethical principles to healthcare. ANS: Bioethics Chapter27 Advanced Practice Nursing: The Nurse—Patient Relationships and General Ethical Concerns 1. The nurse can best ensure that communication is understood by: a. speaking slowly and clearly in the patients native language. b. asking the family members whether the patient understands. c. obtaining feedback from the patient that indicates accurate comprehension. d. checking for signs of hearing loss or aphasia before communicating. ANS: C The best way to determine understanding is to ask the patient. Factors such as anxiety, hearing acuity, language, aphasia, or lack of familiarity with medical jargon or routines can all contribute to misunderstanding. DIF: Cognitive Level: Comprehension REF: pp. 100-101 OBJ: Theory #1 TOP: Feedback KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: basic care and comfort 2. The nurse recognizes a verbal response when the patient: a. nods her head when asked whether she wants juice. b. writes the answer to a question asked by the nurse. c. begins sobbing uncontrollably when asked about her daughter. d. is moaning and restless and appears to be in pain. ANS: B Verbal communication involves words, either written or spoken. Nodding, sobbing, and moaning are nonverbal communication. DIF: Cognitive Level: Comprehension REF: p. 99 OBJ: Theory #1 TOP: Verbal Communication Feedback KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort 3. The nurse recognizes the patient who demonstrates communication congruency when the patient: a. smiles and laughs while speaking of feeling lonely and depressed. b. wrings her hands and paces around the room while denying that she is upset. c. is tearful and slow in speech when talking about her husbands death. d. states she is comfortable while she frowns and her teeth are clenched. ANS: C Congruent communication is the agreement of verbal and nonverbal messages. DIF: Cognitive Level: Comprehension REF: p. 99 OBJ: Theory #1 TOP: Congruence KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: basic care and comfort 4. A Hispanic patient approaches the Asian nurse and, standing very close, touches the nurses shoulder during their conversation. The nurse begins to step back to 18 to 24 inches, while smiling and nodding to the patient. This situation is most likely an example of: a. the nurses need to maintain a professional role rather than a social role. b. a patients attempt to keep the nurses attention. c. a nurses need to establish a more appropriate location for conversation. d. a difference in culturally learned personal space of the nurse and the patient. ANS: D Personal space between people is a culturally learned behavior; Asians, North American natives, and Northern European people generally prefer more personal space than people of Hispanic, Southern European, or Middle Eastern cultures. DIF: Cognitive Level: Comprehension REF: p. 100 OBJ: Theory #2 TOP: Cultural Differences KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 5. A nurse says to a patient, I am going to take your TPR, and then Ill check to see whether you can have a PRN analgesic. In considering factors that affect communication, the nurse has: a. used terminology to clearly inform the patient of what she is doing. b. given information that is unnecessary for the patient to know. c. used medical jargon, which might not be understood by the patient. d. taken into consideration the patients need to know what is happening. ANS: C Medical jargon such as abbreviations or medical terminology is often misunderstood, even by well-educated people. DIF: Cognitive Level: Comprehension REF: p. 101 OBJ: Theory #3 TOP: Blocks to Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 6. A nurse using active listening techniques would: use nonverbal cues such as leaning forward, focusing on the speakers face, and slightly nodding to i a. message has been heard. b. avoid the use of eye contact to allow the patient to express herself without feeling stared at or deme anticipate what the speaker is trying to say and help the patient express herself when she has difficu c. sentence. d. ask probing questions to direct the conversation and obtain the information needed as efficiently as ANS: A Eye contact is a culturally learned behavior and in some cases may not be appropriate. Probing questions or finishing the patients sentence is not part of active listening and is detrimental to an interview. DIF: Cognitive Level: Comprehension REF: p. 101 OBJ: Theory #3 TOP: Active Listening KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 7. When the patient says, I dont want to go home, the nurses best therapeutic verbal response would be: a. Im sure everything will be fine once you get home. b. You dont want to go home? c. Doesnt your family want you to come home? d. I felt like that when I had surgery last year. ANS: B The use of reflecting encourages the patient to expand on his or her feelings or thoughts. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 8. To begin talking with a newly admitted patient about pain management, the nurse would most appropriately state: a. You look pretty comfortable. Are you having any pain? b. Tell me about the pain youve been having. c. Is this pain the same as the pain you had yesterday? d. Dont worry; this pain wont last forever. ANS: B An open-ended question allows the patient to express his or her feelings or needs. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 9. When a patient begins crying during a conversation with the nurse about the patients upcoming surgery for possible malignancy, the nurses most therapeutic response would be: a. Your surgeon is excellent, and I know hell do a great job. b. Oh, dear, your gown is way too big, let me get you another one. c. Dont cry; think about something else and youll feel better. d. Here is a tissue. Id like to sit here for a while if you want to talk. ANS: D Offering self, or presence, and accepting a patients need to cry is supportive. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Therapeutic Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 10. To enhance the establishment of rapport with a patient, the nurse should: a. identify himself by name and title each time he introduces himself. b. share his own personal experiences so that the patient gets to know him as a friend. c. act in a trustworthy and reliable manner; respect the individuality of the patient. d. share information with the patient about other patients and why they are hospitalized. ANS: C Trust and reliability, as well as conveying respect for the individual, all promote rapport. Identifying oneself is important but in itself does not promote rapport. Sharing personal experiences or divulging the confidential nature of other patients conditions is not appropriate in the nursepatient relationship. DIF: Cognitive Level: Comprehension REF: p. 107 OBJ: Clinical Practice #2 TOP: Rapport KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 11. The nurse explains that the therapeutic nursepatient relationship differs from the social relationship because: a. a social relationship does not have goals or needs to be met. b. the nursepatient relationship ends when the patient is discharged. c. the focus is mainly on the nurse in the nursepatient relationship. d. a social relationship does not require trust or sharing of life experiences. ANS: B The nursepatient relationship is limited to the patients stay in the facility and is focused on the patient. A social relationship may have goals or needs and does require trust and sharing of life experiences. DIF: Cognitive Level: Comprehension REF: pp. 106-107 OBJ: Theory #4 TOP: Relationships KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 12. The nurse has selected an outcome for the patient to eat all of the food on the breakfast tray each day. Assessing that the patient has eaten all of the breakfast, the nurse would give positive feedback by saying: a. Wow! That breakfast must have been pretty good. b. I like pancakes too. Everyone on the hall seemed to enjoy them. c. I hope you can keep all that breakfast down. d. Hurray! You finished your whole meal! What would you like for tomorrow? ANS: D Giving positive feedback increases the likelihood of the desired behavior to be repeated. Commenting on the tastiness of the food or the fact that others liked it is not responding directly to the patients having eaten the whole meal. DIF: Cognitive Level: Application REF: p. 100 OBJ: Theory #9 TOP: Positive Feedback KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: basic care and comfort 13. A 67-year-old woman had major abdominal surgery yesterday. She has IV lines, a urinary catheter, and an abdominal wound dressing, and she is receiving PRN pain medication. The end- of-shift report that best conveys the patient status is: a. Doing great, was up in the chair most of the day. No complaints of pain or discomfort. Voiding ade Abdominal surgery yesterday, dressing is dry and intact, her IVs are on time and shes had pain med b. stable. Abdominal dressing dry, IVs800 mL left in #6; NS running at 125 mL/hr; urine output 800 mL this c. 15 mg for pain at 8:00 AM and at 1:30 PM. Shes comfortable now. Vital signs are stable, no fever. Unchanged since this morning. She wanted to know how soon she can have something to eat, so ma d. ANS: C check with her doctor this evening. Her husband has been visiting all day and will let you know if s This brief clear report addresses the major concerns of the abdominal dressing, the status of the IV fluids, vital signs, and analgesia needs. DIF: Cognitive Level: Application REF: pp. 109-110 OBJ: Clinical Practice #4 TOP: Shift Report KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe Effective Care Environment: coordinated care 14. An aspect of computer use in patient care in which the LPN may need to be proficient includes: a. input of data such as requests for radiographs or laboratory services. b. programming the computer to record data from physicians and other health care workers. teaching patients how to use hospital computers to access information such as discharge instruction c. relative to specific medications. d. scheduling admissions, discharges, and nurse staffing to keep the unit at the best occupancy and uti ANS: A Many facilities use computers for data entry relative to requesting radiograph or lab services and physical assessment and medication administration. Programming such computers is not a nursing task, and patients need to have individualized information about discharge and medications. DIF: Cognitive Level: Knowledge REF: pp. 110-111 OBJ: Theory #8 TOP: Computer Use KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 15. A patient with a nursing diagnosis of Sensory perception, disturbed auditory, would most appropriately require the nurse to: a. obtain a sign language interpreter when a family member is unavailable. b. speak slowly and distinctly, but not shout. c. provide bright lighting without glare and orient frequently. d. reorient frequently to time, place, staff, and events. ANS: B A patient with disturbed auditory perception cannot hear well (or at all); therefore, speaking slowly and distinctly without shouting increases patient comprehension. DIF: Cognitive Level: Application REF: pp. 107-108 OBJ: Clinical Practice #3 TOP: Hearing-Impaired Patient Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 16. When an office nurse asks the patient to repeat information that he has just given to the patient over the telephone, the nurse is: a. testing the patients intelligence and memory. b. acting in a cautious way to avoid charges of negligence. c. verifying that the patient understands the information. d. saving the extra time it would take to mail the information. ANS: C Obtaining feedback from a patient to ascertain that the patient understands instructions is an important part of the communication process, especially over the phone, when the nurse does not have nonverbal cues. DIF: Cognitive Level: Comprehension REF: pp. 100-101 OBJ: Theory #3 TOP: Telephonic Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 17. A 36-year-old woman who is in traction for a fractured femur that she received in an auto accident is found crying quietly. The nurse can best address this situation by saying: a. Whats the matter? Why are you crying? Are you in pain? b. Stop crying and tell me what your problem is. c. This could have been much worse. Youre lucky no one was killed. d. You are upset. Can you tell me whats wrong? ANS: D The nurse offers a general lead as to what is causing the distress. The other options are judgmental or clichs or offer no opportunity for the patient to express feelings. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Reflecting Observations KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 18. When the nurse is giving direction to a nursing assistant who is being delegated part of the patient care, the nurses most effective direction would be: a. Do the morning care first on the patients in 205 and 206 who cant get out of bed. b. You take care of all the patients in 205 and 206. Let me know how youre doing and whether you ne c. Give the patient in 204A a shower after breakfast, and call me to check her feet before you get her d d. Take the vital signs on all the patients in the lounge and tell me whether there are problems. ANS: C The clarity and brevity of the direction makes the delegated task clear and leaves the responsibility of assessment to the nurse. DIF: Cognitive Level: Application REF: p. 110 OBJ: Theory #7 TOP: Delegation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe Effective Care Environment: coordinated care 19. When the patient says, I get so anxious just lying here in this hospital bed. I have a million things I should be doing at home, the most empathetic response would be: a. Id feel the same way you do. I know just what youre going through. b. It sounds like youre having a tough time dealing with this situation. c. Its always darkest before the dawn. Hang in there; it will get better. d. You sound pretty sorry for yourself. Why dont you look at the positives? ANS: B Empathy recognizes a patients situation and encourages expression of feelings. DIF: Cognitive Level: Application REF: p. 107 OBJ: Theory #3 TOP: Empathy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 20. A patient asks the nurse, What would you do if you had cancer and had to choose between surgery and chemotherapy? The reply that can best help the patient is: a. If I were you, I would choose surgery and then consider chemo afterward. b. What solutions have you considered? c. I would talk it over with my friends first. d. I dont know. Im glad it isnt my decision. ANS: B Nurses can help by reminding patients of alternatives open to them and should refrain from giving advice but can encourage the patient to consider options. The nurse may be glad not to face a decision a patient must, but it is not helpful to the patient to say this. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Offering Alternatives KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 21. The nurse chooses to use touch in the nursepatient relationship because touch: a. can convey caring and support when words are difficult. b. should be avoided because of problems of cultural misinterpretation. c. is appropriate only in special circumstances, such as with young children. d. is a nursing intervention of choice in almost all situations. ANS: A Touch is a powerful and supportive nonverbal communication in many situations. It is appropriate for all ages, but not in some situations. Careful assessment of the patients situation and cultural values should determine its use, but it should not be avoided because of stereotypes. DIF: Cognitive Level: Comprehension REF: p. 103 OBJ: Theory #4 TOP: Caring Touch KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 22. When the nurse makes the statement, We can come back to that laterright now I need to know about when your symptoms started, the nurse is: a. letting the patient know that topic of conversation was inappropriate. b. setting limits on the expression of feelings. c. refocusing the patient to the issue at hand when the conversation has wandered. d. closing off the conversation by quickly getting to the point of the interview. ANS: C Refocusing is often necessary to accomplish data collection. It does not block communication and is not used to close a conversation or stop an inappropriate topic. DIF: Cognitive Level: Comprehension REF: p. 102 OBJ: Theory #3 TOP: Refocusing Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 23. A patient who has had a stroke is unable to speak clearly and has right-sided hemiplegia. The nurse will design the approach to the assessment interview by: a. asking questions and explaining procedures to the patients daughter. b. speaking slowly and giving the patient time to respond. c. telling the patient he will get all necessary information from the daughter. d. prompting the answers and finishing the sentences for the patient. ANS: B Speaking slowly recognizes that the patient may process (if able) information more slowly. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Clinical Practice #3 TOP: Impaired Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 24. When a nurse is conducting an assessment interview, the most efficient technique would be: a. explaining the purpose of the interview. b. excluding relatives and friends from the interaction. c. telling the patient what data are already available. d. asking closed questions to obtain essential information. ANS: D Closed questions have a definite place when the nurse wants to obtain specific essential data. Closed questions force the patient to stick to the topic. DIF: Cognitive Level: Comprehension REF: p. 102 OBJ: Clinical Practice #1 TOP: Interview KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 25. While interviewing a Native American man for the admission history, the nurse should expect to: a. wait patiently through long pauses in the conversation. b. maintain eye contact with the patient. c. give the patient permission to speak. d. have another family member speak for the patient. ANS: A Native Americans use long pauses in their conversation to better consider their answer and consider the question. The culturally sensitive nurse would wait quietly through the pauses. DIF: Cognitive Level: Comprehension REF: p. 102 OBJ: Clinical Practice #1 TOP: Cultural Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation 26. The nurse is aware that the purpose of therapeutic communication is to: a. gather as much information as possible about the patients problem. b. direct the patient to communicate about his deepest concerns. c. focus on the patient and the patient needs to facilitate interaction. d. gain specific medical information and history of illness. ANS: C Therapeutic communication is a conversation that is focused on the patient and promotes understanding between the sender and the receiver. DIF: Cognitive Level: Comprehension REF: p. 102 OBJ: Theory #4 TOP: Therapeutic Communication KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: coping and adaptation 27. The practical nursing student who is engaged in a therapeutic communication with a patient will have the most difficulty with the technique of: a. closed questions. b. restating. c. using general leads. d. silence. ANS: D The use of silence is the hardest for most students to develop because it makes them uncomfortable, so they tend to end it prematurely. DIF: Cognitive Level: Comprehension REF: p. 102 OBJ: Theory #31 TOP: Silence KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 28. To convey the intervention of active listening, the nurse would: a. maintain eye contact by staring at the patient. b. prompt the patient when the patient stops talking for a moment. c. make a conscious effort to block out other sounds in the immediate environment. d. write down remarks on a clipboard to facilitate later topics of conversation. ANS: C An active listener maintains eye contact without staring, gives the patient full attention, and makes a conscious effort to block out other sounds and distractions. DIF: Cognitive Level: Comprehension REF: p. 101 OBJ: Theory #3 TOP: Active Listening KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 29. When the nurse enters the room, the patient is laughing out loud at something on TV. The patient stops and apologizes for the laughter, saying, I guess I ought not be laughing at all since I am stuck here with two broken legs. The nurse can use evidence-based information when she responds: a. Laughter is nearly always a cover-up for anxiety when facing a long rehabilitation. b. Long periods of laughter decrease the amount of oxygen available to your body for healing. c. Laughter in a hospital is often distracting and depressing to other patients nearby. d. Laughter truly is the best medicine as it has a positive effect on the immune system. ANS: D Hasen and Hasen (2009) found that laughter and appropriate use of humor decreased stress and anxiety and had a positive effect on the immune system. DIF: Cognitive Level: Application REF: p. 101 OBJ: Clinical Practice #2 TOP: Use of Laughter KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 30. When interacting with an elderly patient, the nurse would enhance communication by: a. speaking slowly in order to allow the patient to process the message. b. addressing him by his first name to encourage a therapeutic relationship. c. standing in the doorway rather than entering the room to give the elderly patient more privacy. d. speaking in simple sentences, as if to a child. ANS: A When interacting with an elderly person, the nurse should try not to speak too quickly or expect an immediate answer because the elderly take more time to process the message. Do not use baby talk or speak to them as if they were children. DIF: Cognitive Level: Comprehension REF: p. 101 OBJ: Theory #2 TOP: Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 31. When the nurse observes a resident in a long-term facility pounding his fists on his legs and grinding his teeth, the nurse will validate her perception of the patients non-verbal expression of anger by: a. documenting that the patient was agitated and appeared angry. b. asking the male nursing assistant if it is his perception that the patient appears angry. c. accessing the nursing care plan to ascertain if there is a nursing diagnosis relative to anger. d. sitting down near the patient and saying, You seem upsetcan I help? ANS: D All perceptions based on the observation of non-verbal behavior should be validated by consulting the patient. DIF: Cognitive Level: Application REF: p. 100 OBJ: Theory #9 TOP: Validating Perceptions KEY: Nursing Process Step: Assessment | Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 32. When a patient states, I dont feel like walking today, the nurses most therapeutic verbal response would be: a. You have to walk today. b. You dont want to walk today? c. I dont feel like walking today either. d. Why dont you want to walk today? ANS: B Reflection is a way to restate the message. The idea is simply reflected back to the speaker in a statement to encourage continued dialogue on the topic. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 33. When a patient states, My son hasnt been to see me in months, the nurses best verbal response is: a. Dont worry; Im sure your son will visit. b. Your son hasnt been around much lately? c. My son doesnt come to visit me either. d. How terrible that he doesnt visit you. ANS: B Restating in different words what the patient said encourages further communication on that topic. DIF: Cognitive Level: Application REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 34. An example of a nurse communicating with a patient using open-ended questions would be: a. Is your pain less today than it was yesterday? b. Did you sleep all night without waking? c. How many bowel movements have you had today? d. What was your daughters reaction to your desire for hospice? ANS: D An open-ended question is broad, indicating only the topic, and it requires an answer of more than a word or two. Use of an open-ended question or statement allows the patient to elaborate on a subject or to choose aspects of the subject to be discussed. Open-ended questions or statements are helpful to open up the conversation or to proceed to a new topic. They usually cannot be answered with one word or just yes or no. DIF: Cognitive Level: Comprehension REF: p. 103, Table 8-1 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 35. The nurse tells a patient, For the last 2 days we have talked about whether to notify your daughter of your upcoming surgery in 2 days. You have indicated you do not want to be a burden to her, but you also would like to have her here. You may have to decide rather quickly because of the time constraint. The nurse is using the technique of: a. focusing. b. reflection. c. restatement. d. summarizing. ANS: D Summarizing presents the problem and possible solutions with the attendant difficulties. This technique unclutters the problem and presents it back to the patient for his or her choice of a solution. DIF: Cognitive Level: Comprehension REF: p. 104 OBJ: Theory #3 TOP: Communication Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 36. The nurse is caring for a patient who states, I tossed and turned last night. The nurse responds to the patient, You feel like you were awake all night? This is an example of: a. an open-ended question. b. restatement. c. reflection. d. offering self. ANS: B Restatement is a therapeutic communication technique in which the nurse restates in different words what the patient said. This encourages further communication on that topic. DIF: Cognitive Level: Comprehension REF: pp. 102-103 OBJ: Theory #3 TOP: Restatement KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 37. The nurse is caring for a patient who has just had a mastectomy (breast removal). The patient expresses concern that her husband will no longer find her attractive because of her mastectomy. The nurse appropriately responds: a. Youre concerned your husband will find you unattractive because of your mastectomy? b. Youre a beautiful woman; of course your husband will find you attractive after your mastectomy. c. Dont worry; when I had my mastectomy, my husband still found me very attractive. d. You should leave your husband immediately if he thinks youre unattractive after a mastectomy. ANS: A This is an example of restatement, which allows the patient to know her message was understood and encourages the patient to continue about her concerns on the topic. DIF: Cognitive Level: Application REF: pp. 102-103 OBJ: Theory #3 TOP: Restatement/Reflection KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 38. A patient states, Im so worried that I might have cancer. The nurse responds, It is time for you to eat breakfast. The nurses response is an example of: a. using clichs. b. judgmental response. c. changing the subject. d. giving false reassurance. ANS: C Changing the subject is a block to effective communication in which the patient is deprived of the chance to verbalize concerns. DIF: Cognitive Level: Comprehension REF: p. 104 OBJ: Theory #3 TOP: Changing the Subject KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 39. The nurse is aware that the use of false reassurance is harmful to the nursepatient relationship, because this communication block: a. discounts the patients stated concerns. b. shows a judgmental attitude on the part of the nurse. c. summarizes the patients concerns and closes communication. d. confuses the patient by giving information. ANS: A Giving false reassurance is a block to effective communication in which the patients feelings are negated and in which the patient may be given false hope, which, if things turn out differently, can destroy trust in the nurse. DIF: Cognitive Level: Comprehension REF: p. 104 OBJ: Theory #3 TOP: False Reassurance KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 40. A home health patient with a bleeding ulcer informs the nurse that she ate a bowl of chili with jalapenos. An inappropriate communication block with a judgmental tone by the nurse would be: a. Well, you have had this problem long enough to know what will happenyou certainly cant blame m b. I dont think that was a smart thing for you to do considering your ulcer. c. Well, you better watch your stool for evidence of blood so you can notify your physician. d. Oh, poo! A bowl of chili every now and then wont make a lot of difference to your ulcer. ANS: B Judgmental response is a block to effective communication in which the nurse is judging the patients action. It implies that the patient must take on the nurses values and is demeaning to the patient. DIF: Cognitive Level: Analysis REF: p. 105, Table 8-2 OBJ: Theory #3 TOP: Judgmental Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 41. A patient tells the nurse that she dislikes the food that is served in the hospital. The nurse responds, Our cooks work very hard; the food that is served is very good. The nurses response is an example of the communication block of: a. judgmental response. b. giving advice. c. defensive response. d. using clichs. ANS: C Defensive response is a block to effective communication in which the nurse responds by defending the hospital food. This prevents the patient from feeling that she is free to express her feelings. DIF: Cognitive Level: Comprehension REF: p. 105 OBJ: Theory #3 TOP: Defensive Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 42. A nurse caring for a patient who fell off the roof while he was intoxicated asks the patient, Why in the world were you on the roof when you had been drinking? The nurses statement is an example of which type of communication? a. Changing the subject b. Defensive response c. Inattentive listening d. Asking probing questions ANS: D Asking probing questions is a block to effective communication in which the nurse pries into the patients motives and therefore invades privacy. DIF: Cognitive Level: Comprehension REF: p. 105 OBJ: Theory #3 TOP: Probing KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 43. The nurse caring for a patient who is concerned about her 10-pound weight loss relative to her chemotherapy tells the patient, Lucky you! Every cloud has a silver lining. The nurses statement is an example of which type of communication block? a. Defensive response b. Asking probing questions c. Using clichs d. Changing the subject ANS: C Using clichs is a block to effective communication in which the patients individual situation is negated, and the patient is stereotyped. This type of response sounds flippant and prevents the building of trust between the patient and the nurse. DIF: Cognitive Level: Comprehension REF: pp. 105-106 OBJ: Theory #3 TOP: Clichs KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 44. The nurse is caring for a patient with a diagnosis of lung cancer. The nurse states, If I were you, I would have radiation therapy. The nurses statement is an example of which type of communication block? a. Inattentive listening b. Giving advice c. Using clichs d. Defensive response ANS: B Giving advice is a block to effective communication and tends to be controlling and diminishes patients responsibility for taking charge of their own health. DIF: Cognitive Level: Comprehension REF: p. 105, Table 8-2 OBJ: Theory #3 TOP: Giving Advice KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 45. The nurse is caring for a patient who is concerned about living alone. The best response by the nurse is: a. Where have you considered living? b. Why dont you live with your family? c. I think you should live with your family. d. If you were my mom, Id have you live with me. ANS: A Rephrasing will help the patient explore various alternatives. The nurse should not use phrases such as Why dont you, When that happened to me, I did, or I think you should. Rephrasing, for example, Have you thought of your options? or You might want to think about, or Have you considered? will help the patient explore various alternatives. DIF: Cognitive Level: Application REF: p. 104 OBJ: Theory #3 TOP: Offering Alternatives KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: coping and adaptation 46. The characteristic that is representative of the nursepatient relationship is that this relationship: a. focuses on the nurses ability to build rapport. b. continues after discharge. c. does not include humor. d. focuses on the assessed patient health problems. ANS: D The nursepatient relationship focuses on the patient, has goals, and is defined by specific boundaries. The relationship takes place in the health care setting, and boundaries are defined by the patients problems, the help needed, and the nurses professional role. When the patient is discharged, the relationship ends. DIF: Cognitive Level: Knowledge REF: pp. 106-107 OBJ: Theory #4 TOP: NursePatient Relationship KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 47. When communicating with an aphasic patient, the nurse appropriately: a. speaks quickly and shouts so the patient can hear. b. assumes the patient can understand what is heard. c. speaks to the patients caregiver about the patient. d. assumes the patient cannot understand what is heard. ANS: B When communicating with an aphasic patient, the nurse assumes the patient can understand what is heard even though speech is jargon or the person is mute, unless deafness has been diagnosed. The nurse should talk to the patient, and not talk to someone else in the room about the patient. The nurse should speak slowly and distinctly and should not shout. Chapter28 Leadership and Role Transition for the Advanced Practice Nurse Multiple Choice 1. Which of the following statements accurately reflects the nurses responsibility for patient outcomes in todays workplace? A) Tasks can be delegated, but accountability cannot be delegated. B) In todays environment, authority is more often given to management. C) Most nurses who are accountable have the authority to affect the situation or effect change. D) Nurses are protected against legal action being taken in cases of malpractice in the hospital setting. Ans: A Client Needs: A-1 Cognitive Level: Comprehension Difficulty: Moderate Integrated Process: Nursing Process Objective: 1, 2 Page and Header: 428, Differentiating Between Accountability and Authority Feedback: Tasks can be delegated, but accountability cannot; nurses who delegate tasks to assistive personnel continue to be accountable for that care. Many nurses experience frustration because they must be accountable for activities without the authority to affect the situation or create change. Authority is often shared in contemporary care settings. Nurses are legally responsible for the care they provide and are vulnerable to malpractice suits. 2. Which of the following statements accurately describes a basic guideline for using communication skillfully? A) Managers should communicate how to perform a task even if it is something the subordinate has already learned. B) Managers should not be afraid of making judgmental statements when dealing with a subordinate who has broken policy rules. C) Managers should attempt to formulate a response to an individual who is still speaking to avoid awkward pauses in the conversation. D) Managers should present direction as briefly as possible while still providing adequate data. Ans: D Client Needs: C Cognitive Level: Application Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 9 Page and Header: 445, Using Communication Skills in the Leadership Role Feedback: Effective managers state the necessary information as briefly as possible while still providing enough data to be clear. Interruptions, judgmental statements, and repeated explanations are characteristics of ineffective communication. 3. What is the primary objective of a performance appraisal? A) Establish written documentation of incompetent behavior to facilitate dismissal B) Maintain and develop employee performance C) Establish criteria for accreditation standards D) Determine who receives pay raises Ans: B Client Needs: A-1 Cognitive Level: Comprehension Difficulty: Easy Integrated Process: Communication and Documentation Objective: 11 Page and Header: 447, Performance Appraisal Feedback: The primary objectives of performance appraisal are to maintain or improve employee performance and to enhance the development of employees. They are not intended to be punitive measures or criteria for accreditation. Performance appraisals may have an influence on a nurses pay but this is not their primary objective. 4. Which of the following is a characteristic of an effective performance evaluation system? A) The appraisal system operates outside of the scope of administration. B) Employees do not know in advance who will be evaluating them. C) The final disposition of the appraisal is shared with the employee. D) Evaluation concentrates on the personality of the employee. Ans: C Client Needs: A-1 Cognitive Level: Comprehension Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 11 Page and Header: 448, Display 12.4 Feedback: A sound performance appraisal is shared with the employee who is the subject of the appraisal. The appraisal system should be strongly supported by administration and employees should be made aware of who will appraise them. An employees personality should not be the focus for appraisal. 5. A nursing student finds that she has difficulty with procrastination. Which of the following is a recommended guideline to help this student manage her time? A) Start working on a project for 10 minutes, and quit if tired or bored. B) Schedule 2 or 3 days a week in which to concentrate her tasks. C) Avoid spending the time it takes to make to-do lists. D) Schedule down-time first and work second. Ans: A Client Needs: A-1 Cognitive Level: Application Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 12 Page and Header: 455, Dealing with Procrastination and Time Wasters Feedback: Kanarek (1996) provides five suggestions for dealing with procrastination. First, she suggests that you start working on a project for 10 minutes and quit if tired or bored. Work times should be prioritized carefully and spread out over time. The creation of lists is a useful tool. 6. A nursing leader has expressed a desire to foster the characteristics and behaviors associated with transformational leadership. Which of the following actions best demonstrates transformational leadership? A) The leader makes it clear to employees that positive work performance will be rewarded and that sub-standard performance will bring consequences. B) The leader ensures that decisions are based on the consensus of every employee. C) The leader prioritizes the needs of each individual employee over the interests of the larger organization. D) The leader takes action to build trust and relationships between him or her and the employees. Ans: D Client Needs: C Cognitive Level: Application Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 3 Page and Header: 430, Table 12.1 Feedback: Leader activities associated with transformational leadership include creating a vision, building relationships, developing trust, and building self-esteem. An emphasis on rewards and punishment is associated with transactional leadership. Consensus is not appropriate for every decision, and the interests of individual employees cannot always supersede the interests of the organization. 7. The manager of a hospital unit has unilaterally decided on a change in the way that overtime is distributed among the nursing staff and has followed up this decision with an e-mail to all employees. What leadership style is exemplified by this manager? A) Participative leadership B) Permissive leadership C) Laissez-faire leadership D) Autocratic leadership Ans: D Client Needs: C Cognitive Level: Analysis Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 4 Page and Header: 431, Leadership/Management Styles Feedback: In autocratic or authoritarian leadership, the leader/manager makes the majority of the decisions without direct consultation with employees. Laissez-faire or permissive leadership occurs when little or no direction or guidance is provided. Participative leadership involves extensive input from employees. 8. Experts have identified a close relationship between the practice of transformational leadership and the empowerment of employees. What action should a nursing leader take to foster employee empowerment? A) Have the performance of each employee appraised by his or her peers rather than by a manager or leader. B) Share information as openly as possible in order to make employees aware of problems. C) Adopt a hands-off approach in order to allow leadership to organically emerge from within the group of employees. D) Eliminate the practice of conducting performance appraisals of employees. Ans: B Client Needs: C Cognitive Level: Application Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 5, 6 Page and Header: 436, Empowerment Feedback: Transformational leaders foster empowerment by openly sharing information with workers so that everyone is aware of problems and the need for action. Performance appraisals are not necessarily contrary to the philosophy or practice of transformational leadership, and these should not be conducted by an employees peers. Transformational leadership is characterized by constructive engagement, not a hands-off approach. 9. Jennifer is a registered nurse who works in a busy emergency department. As one of her goals for the current year, Jennifer has resolved to develop her emotional intelligence. How should Jennifer best meet her goal? A) Try to remove emotion from her clinical decision-making whenever possible. B) Become more assertive when responding to the emotional responses of patients, families, and coworkers. C) Become more aware of the way that her emotions function and how they influence her actions. D) Try to limit her expressions of emotion to times when she is not interacting with others. Ans: C Client Needs: C Cognitive Level: Application Difficulty: Difficult Integrated Process: Communication and Documentation Objective: 7 Page and Header: 439, Enhancing Your Emotional Intelligence Feedback: Self-awareness is one of the central aspects of emotional intelligence. Emotional intelligence does not necessarily involve removing emotion from decision-making or removing emotion from interpersonal interactions. Awareness of others emotions is a dimension of emotional intelligence, but the appropriate response to this is not normally increased assertiveness. 10. A recent nursing graduate has asked an expert nurse how best to foster her leadership abilities, since she wishes to explore leadership opportunities later in her career. How should the expert nurse best respond? A) Even if you dont trust a decision that you have to make, act like you chose the best option. B) Become as specialized as possible in your nursing experience. C) Develop your interpersonal skills by having a wide variety of interactions. D) Become as assertive as you can and take every opportunity to guide the behavior of others. Ans: C Client Needs: C Cognitive Level: Application Difficulty: Difficult Integrated Process: Communication and Documentation Objective: 8 Page and Header: 443, Developing Your Leadership Style Feedback: The development of sophisticated interpersonal skills is important to building leadership abilities. Effective leadership does not depend on feigned confidence, though self- confidence is a trait that can be fostered. In most cases, variety and depth of experience are superior to narrow specialization. Effective leadership is more nuanced and complex than simply directing the behavior of others or demonstrating assertiveness. 11. A nurse has responded to a patients call light for the fourth time in the past hour only to be berated by the patient for taking so long to come to the bedside. Rather than responding in a confrontational tone the nurse has paused to think of the best response to the patients statements. In doing so, the nurse has exhibited A) self-regulation. B) sympathy. C) manipulation. D) self-strategy. Ans: A Client Needs: C Cognitive Level: Analysis Difficulty: Easy Integrated Process: Communication and Documentation Objective: 7 Page and Header: 440, Self-Regulation Feedback: Self-regulation refers to the ability to control inappropriate impulses and to think before acting or speaking. Research on mindfulness training indicates it is a positive strategy for managing emotionally charged situations. The nurse has not acted in a manipulative way. Sympathy involves feeling sorrow for another persons pain, a dynamic that is not evident in this interaction. 12. A patient is receiving a transfusion of packed red blood cells and consequently requires frequent vital signs. A set of vital signs was just due during the nurses scheduled lunch break and so a colleague took the patients vital signs. After returning from lunch, the nurse confirmed with the colleague that the scheduled vital signs were taken, to which the colleague replied, Yes, it seems like Im covering you a whole lot lately. How should the nurse best respond to the colleagues statement? A) I dont think thats a fair thing to say because I cant help when a set of vitals are due. B) If youre implying that I dont pull my weight I think that youre badly mistaken. C) Well, what goes around comes around, right? D) Could you explain what you mean by that? Ans: D Client Needs: C Cognitive Level: Application Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 10 Page and Header: 444, Communicating Effectively Feedback: An important principle of communication is to ensure that meanings are clearly understood by both parties. This is especially true in the case of a statement that may be accusatory. Responding confrontationally or sarcastically is rarely appropriate. 13. The nurse manager of a busy medical unit prioritizes effective communication with the employees of the unit. In recent years, an increasing amount of this communication has involved e-mails and text messages. When using these communication media, the nurse should A) take action to ensure that patient confidentiality is maintained. B) cc upper management and human resources with all e-mails. C) avoid using a smartphone on the unit whenever possible. D) follow up e-mails with a paper copy of important messages. Ans: A Client Needs: C Cognitive Level: Application Difficulty: Moderate Integrated Process: Communication and Documentation Objective: 10 Page and Header: 444, Communicating Effectively Feedback: Patient privacy can be difficult to ensure when communicating electronically. As a result, nurse leaders must take measures to protect confidentiality. Electronic messages do not always need be followed up with paper copies and it is unnecessary to cc superiors on all communications. Smartphones are an effective communication tool, provided they are used in an appropriate manner. 14. It has been a frantic morning on the hospital unit and the nurse is unsure whether she will be able to complete her required tasks on time before her scheduled lunch break. Which of the following is the nurses most appropriate response to this problem? A) Skip lunch or trade her lunch break with a colleague who is scheduled for a later break. B) Determine if more of her tasks could be delegated to another member of the care team. C) Ask the unit manager for advice. D) Explain to a colleague that she will likely be unable to complete her required work. Ans: B Client Needs: A-1 Cognitive Level: Application Difficulty: Difficult Integrated Process: Communication and Documentation Objective: 12 Page and Header: 454, Principles of Time Management Feedback: Delegation is an appropriate and useful strategy for effective time management. This would be a preferred approach over changing the lunch schedule. The nurse should attempt to delegate before approaching her manager for a solution or resigning herself to the fact that she will not complete her work. Multiple Selection 15. All performance evaluations, whether formal or informal, should be based on appropriate standards of performance. In the context of a performance appraisal, which of the following are appropriate performance criteria? (Select all that apply.) A) The managers experience base B) The nurses written job description C) The institutions policies and procedures D) Nursing standards of practice E) The nurses career goals Ans: B, C, D Client Needs: A-1 Cognitive Level: Analysis Difficulty: Difficult Integrated Process: Communication and Documentation Objective: 11 Page and Header: 448, Criteria for Evaluation Feedback: Standards of performance include job descriptions, policies and procedures, and professional standards of practice. A leaders personal experience base and the nurses goals may be relevant but neither is an objective measure for appraising the nurses performance. Chapter29 Managing Personal Resources: Time and Stress Management 1.When released in response to alarm, which of the following substances promotes a sense of well-being? 1) Aldosterone 2) Thyroid-stimulating hormone 3) Endorphins 4) Adrenocorticotropic hormone ANS:3 Endorphins act like opiates to produce a sense of well-being; they are released by the hypothalamus and posterior pituitary gland in response to alarm. Aldosterone promotes fluid retention by increasing the reabsorption of water by renal tubules. Thyroid-stimulating hormone increases the efficiency of cellular metabolism and fat conversion to energy for cell and muscle needs. Adrenocorticotropic hormone stimulates the adrenal cortex to produce and secrete glucocorticoids and mineralocorticoids. PTS:1DIF:ModerateREF:p. 253 KEY:Nursing process: N/A | Client need: PHSI | Cognitive level: Recall 2.After sustaining injuries in a motor vehicle accident, a patient experiences a decrease in blood pressure and an increase in heart rate and respiratory rate despite surgical intervention and fluid resuscitation. Which stage of the general adaptation syndrome is the patient most likely experiencing? 1) Alarm 2) Resistance 3) Exhaustion 4) Recovery ANS:3 Physiological responses in the exhaustion stage include low blood pressure and high respiratory and heart rates. During the alarm stage, heart rate and blood pressure both increase. In the resistance stage, the body tries to maintain homeostasis; blood pressure and heart rate normalize. If adaptation is successful, recovery takes place. PTS:1DIFifficultREF:p. 254 KEY: Nursing process: Assessment | Client need: PHSI | Cognitive level: Analysis 3.You are caring for a patient who suddenly experiences a cardiac arrest. As you respond to this emergency, which substance will your body secrete in large amounts to help prepare you to react in this situation? 1) Epinephrine 2) Corticotrophin-releasing hormone 3) Aldosterone 4) Antidiuretic hormone ANS:1 During the shock phase of the general adaptation syndrome, large amounts of epinephrine prepare the body to react in an emergency situation. In response to the epinephrine release, the endocrine system releases corticotrophin-releasing hormone, aldosterone, and antidiuretic hormone. PTS: 1 DIF: Moderate REF: p. 252 KEY: Nursing process: N/A | Client need: PHSI | Cognitive level: Application 4.What is the function of antidiuretic hormone when released in the alarm stage of the general adaptation syndrome? 1) Promotes fluid retention by increasing the reabsorption of water by kidney tubules 2) Increases efficiency of cellular metabolism and fat conversion to energy for cells and muscle 3) Increases the use of fats and proteins for energy and conserves glucose for use by the brain 4) Promotes fluid excretion by causing the kidneys to reabsorb more sodium ANS:1 Antidiuretic hormone promotes fluid retention by increasing the reabsorption of water by kidney tubules. Thyroid-stimulating hormone increases efficiency of cellular metabolism and fat conversion to energy for cells and muscle. Cortisol increases the use of fats and proteins for energy and conserves glucose for use by the brain. Aldosterone promotes fluid retention by causing the kidneys to reabsorb more sodium. PTS:1DIF:ModerateREF:p. 252 KEY:Nursing process: N/A |Client need: PHSI | Cognitive level: Recall 5.A patient sustains a laceration of the thigh in an industrial accident. Which step in the inflammatory process will the patient experience first? 1) Cellular inflammation 2) Exudate formation 3) Tissue regeneration 4) Vascular response ANS:4 Immediately after the injury, the vascular response occurs. Blood vessels at the site constrict to control bleeding. After the injured cells release histamine, the vessels dilate, causing increased blood flow to the area. During the next phase, known as the cellular response phase, white blood cells migrate to the site of injury. In the exudate-formation phase, the fluid and white blood cells move from circulation to the site of injury, forming an exudate. Tissue regeneration occurs in the healing phase. PTS:1DIF:ModerateREF:p. 254 KEY: Nursing process: Assessment | Client need: PHSI | Cognitive level: Comprehension 6.A patient complains of a vague, uneasy feeling of dread, and his heart rate is elevated. Which of the following nursing diagnoses is most appropriate for this patient? 1) Anger 2) Fear 3) Anxiety 4) Hopelessness ANS:3 NANDA-International defines Anxiety as a vague, uneasy feeling of discomfort or dread accompanied by an autonomic response. This patient is most likely feeling anxious. Anger is not a nursing diagnosis. Fear, which is also a nursing diagnosis, is an emotion or feeling of apprehension from an identified danger, threat, or pain. Hopelessness is a nursing diagnosis defined as a state in which the patient sees few or no available alternatives and cannot mobilize energy on his own behalf. PTS:1DIF:ModerateREF:p. 256 KEY: Nursing process: Diagnosis | Client need: PSI | Cognitive level: Application 7.A patient who has been hospitalized for weeks becomes angry and tells the nurse who is caring for him, I hate this place; nobody knows how to take care of me or Id be home by now. Which response by the nurse is best in this situation? 1) You seem angry; whats going on that makes you hate this place? 2) Im sorry that we arent caring for you according to your expectations. 3) You were very sick; dont be angry; youre lucky to be alive. 4) You shouldnt be angry with us; were trying to help you. ANS:1 You seem angry; whats going on . . . encourages the patient to express his feelings and may provide you with more information. The nurse should not take responsibility for the patients anger by apologizing (Im sorry . . .). Advising the patient dont be angry or you shouldnt be angry diminishes the patients right to be angry. PTS:1DIF:ModerateREF:p. 266 KEY: Nursing process: Interventions | Client need: PSI | Cognitive level: Analysis 8.You are caring for a patient with numerous physiological complaints. A family member tells you that the patient is pretending to have the symptoms of a stomach ulcer to avoid going to work. Which somatoform disorder is this patient most likely experiencing? 1) Hypochondriasis 2) Somatization 3) Somatoform pain disorder 4) Malingering ANS:4 Malingering is a conscious effort to escape unpleasant situations by pretending to have symptoms of a disorder. With hypochondriasis, the patient is preoccupied with the idea that he is or will become seriously ill. In somatization, anxiety and emotional turmoil are expressed in physical symptoms. With somatoform pain disorder, emotional pain manifests physically. PTS:1DIF:ModerateREF:p. 259 KEY: Nursing process: Diagnosis | Client need: PSI | Cognitive level: Application 9.After a patient has an argument with her husband, she becomes verbally abusive to the nurse who is caring for her. Which coping mechanism is this patient exhibiting? 1) Reaction formation 2) Displacement 3) Denial 4) Conversion ANS:2 This patient is using displacement. She is transferring the emotions she feels toward her husband to the nurse. When a patient uses the coping mechanism of reaction formation, the patient is aware of her feelings but acts in an opposite manner to what she is really feeling. With the coping mechanism of denial, the patient transforms reality by refusing to acknowledge thoughts, feeling, desires, or impulses. With conversion, emotional conflict is changed into physical symptoms that have no physical basis. PTS:1DIF:ModerateREF:p. 257 KEY: Nursing process: Assessment | Client need: PSI | Cognitive level: Application 10.A patient who has been diagnosed with breast cancer decides on a treatment plan and feels positive about her prognosis. Assuming the cancer diagnosis represents a crisis, this patient is most likely experiencing which phase of crisis? 1) Precrisis 2) Impact 3) Crisis 4) Adaptive ANS:4 When a patient begins to think rationally and problem-solve, she is most likely experiencing the adaptive phase of crisis. During the precrisis phase, the patient finds success using her previous coping strategies. Anxiety and confusion increase during the impact phase if usual coping strategies are ineffective. The patient may use new coping strategies, such as withdrawal, during the crisis phase. PTS: 1 DIF: Moderate REF: pp. 259-260 KEY: Nursing process: Diagnosis | Client need: PSI | Cognitive level: Application 11.A nurse identifies the nursing diagnosis Diarrhea related to stress for a patient. Which nursing intervention should be included in the nursing care plan to help the patient relieve the cause of the diarrhea? 1) Monitor and record the frequency of stools on the graphic record. 2) Administer prescribed antidiarrheal medications as needed. 3) Encourage the patient to verbalize about stressors and anxiety. 4) Provide oral fluids on a regular schedule. ANS:3 The nurse should encourage the patient to verbalize about stressors and anxiety to help relieve stress, which is the cause of the patients diarrhea. Monitoring stool frequency is an assessment, not a nursing intervention. The other interventions may be necessary to treat diarrhea, but they do not alleviate the cause of the diarrhea. PTS: 1 DIF: Moderate REF: p. 259 KEY: Nursing process: Interventions | Client need: PSI | Cognitive level: Analysis 12.When counseling a patient about behaviors to reduce stress, which of the following goals should the nurse put on the care plan? 1) The patient will limit his intake of fat to no more than 15% of the daily calories consumed. 2) The patient will eat three meals per day at approximately the same time each day. 3) The patient will limit his intake of sugar and salt, as well as sweet and salty foods. 4) The patient will consume no more than three alcoholic beverages a day. ANS:3 The nurse should advise the client to limit the intake of sugar and salt; limit the intake of fat to no more than 30% (not 15%) of daily calories; eat smaller, more frequent meals (not three meals a day); and consume no more than two alcoholic beverages per day but not necessarily every day. PTS:1DIF:ModerateREF:p. 265 KEY: Nursing process: Planning | Client need: PHSI | Cognitive level: Application 13.At the end of a guided imagery session, which physical assessment finding would suggest that the relaxation technique was successful? 1) Decreased blood pressure 2) Decreased peripheral skin temperature 3) Increased heart rate 4) Increased respiratory rate ANS:1 Reassessment findings that suggest relaxation has been effective include decreased blood pressures, increased peripheral skin temperature, decreased heart rate, and decreased respiratory rate. PTS:1DIF:ModerateREF:pp. 266-267 KEY: Nursing process: Evaluation | Client need: PHSI | Cognitive level: Comprehension 14.The nurse is caring for a patient with unresolved anger. For which associated complication should the nurse assess? 1) Depression 2) Hypochondriasis 3) Somatization 4) Malingering ANS:1 Depression is sometimes associated with unresolved anger and may result from stress. A person with hypochondriasis is preoccupied with feelings that he will become seriously ill. In somatization, anxiety and emotional turmoil are expressed in physical symptoms, loss of physical function, pain that changes location often, and depression. Malingering is a conscious effort to avoid unpleasant situations. Hypochondriasis, somatization, and malingering are not associated with unresolved anger. PTS:1DIF:EasyREF:p. 256 KEY: Nursing process: Assessment | Client need: PSI | Cognitive level: Comprehension 15.Before entering the room of a patient who is angry and yelling, the nurse removes her stethoscope from around her neck. The best rationale for doing so is that the stethoscope 1) Could be used by the patient to hurt her 2) Might cause the patient not to trust her 3) Would distract her from focusing on the patient 4) Will function as another stressor for the patient ANS:1 When dealing with an angry patient, the nurse must be alert to her own safety needs. A stethoscope, dangling jewelry, or anything else the patient might use as to harm the nurse should be removed before entering the patients room. It is unlikely that a stethoscope would cause the patient not to trust the nurse, nor function as a stressor because stethoscopes are common in the healthcare setting; nearly every caregiver carries a stethoscope. For the same reason, it would not likely distract the nurse. Nurses carry stethoscopes so routinely that they likely dont even notice their presence. PTS:1DIF:ModerateREF:p. 266 KEY: Nursing process: Implementation | Client need: SECE | Cognitive level: Analysis 16.A patient is in crisis. After assessing the situation, what should the nurse do first? 1) Determine the imminent cause of the crisis. 2) Intervene to relieve the patients anxiety. 3) Decide on the type of help the patient needs. 4) Ensure the safety of both the nurse and patient. ANS:4 The first goal of crisis intervention is to assess the situation. Then ensure safety of self and patient, defuse the situation, decrease the persons anxiety, determine the problem (cause of the crisis), and decide on the type of help needed. Safety is always foremost. PTS:1DIF:ModerateREF:p. 269 KEY:Nursing process: Implementation | Client need: SECE | Cognitive level: Application Multiple Response Identify one or more choices that best complete the statement or answer the question. 1.During the alarm stage of the general adaptation syndrome, which metabolic change(s) occur(s)? Choose all that apply. 1) Rate of metabolism decreases. 2) Liver converts more glycogen to glucose. 3) Use of amino acids decreases. 4) Amino acids and fats are more available for energy. ANS:2, 4 The metabolic changes that occur during the alarm stage of the general adaptation syndrome include the following: The rate of metabolism increases, the liver converts more glycogen to glucose, and there is increased use of amino acids and mobilization of fats for energy. PTS:1DIF:ModerateREF:pp. 252-253 KEY: Nursing process: N/A | Client need: Physiological integrity | Cognitive level: Comprehension 2.Two days after a patient undergoes abdominal surgery, his surgical incision is red and slightly edematous; it is oozing a small amount of serosanguineous (pink-tinged serous) fluid. On the basis of these data, what can you conclude? Choose all that apply. 1) The wound is most likely infected. 2) This is a vascular response to inflammation. 3) Damaged cells are being regenerated. 4) Exudate formation is occurring. ANS:2, 4 During the vascular response phase of the inflammatory process, blood vessels constrict to control bleeding. Fluid from the capillaries moves into tissues, causing edema. The fluid and white blood cells that move to the site of injury are called exudates; this includes the serosanguineous exudate that commonly appears at surgical incisions. When a wound becomes infected, yellow, foul-smelling drainage may form at the site; there is no mention of pus in the scenario. Regeneration occurs when identical or similar cells replace damaged cells; although this may be occurring, you cannot prove it with the data given here. PTS:1DIF:ModerateREF:pp. 254-255 KEY: Nursing process: Assessment | Client need: PHSI | Cognitive level: Application 3.A 75-year-old patient is tearful, shaky, and withdrawn. She tells you that she is worrying herself to death about losing her aging husband and being all alone. You recognize this reaction as Anxiety rather than Fear because (choose all that apply) 1) It concerns future or anticipated events 2) It concerns anticipation of danger rather than a present danger 3) There is no shakiness or tearfulness present 4) There is a psychological rather than a physical threat ANS:1, 2, 4 Anxiety is an emotional response related to future or anticipated events. Fear is a cognitive response to a present, usually identifiable, source. Anxiety results from psychological conflict, whereas fear can result from either a psychological or physical threat. Shakiness and tearfulness may occur in both anxiety and fear, which share several defining characteristics. Chapter30 Role Transition: Strategies for Success in the Marketplace 1. Theories that focus on what the leader does are called: 1) Trait theories. 2) Behavioral theories. 3) Situational theories. 4) Transformational theories. ANS: 2 Behavioral theories are concerned with what a leader does, whereas trait theories are concerned with what a leader is. Situational theories recognize that each situation is different and that leaders must consider a number of factors when deciding how to take action. Transformational theories focus on the ability of the leader to communicate her vision in such a way that it inspires commitment among workers. PTS:1DIF:ModerateREF:p. 3 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 2. At a recent nurse staff meeting, the chief nursing officer (CNO) announced that all nursing staff would work 12-hour shifts on a daynight rotation schedule that would alternate every 6 weeks. The CNO announced that she made this decision as a means to solve discord between the day- and night-shift nurses. She explained that this plan will allow the staff to experience the work on each shift and to appreciate the various job responsibilities on each shift. What type of leadership is the CNO displaying? 1) Management 2) Laissez-faire 3) Democratic 4) Authoritarian ANS: 4 The authoritarian leader makes decisions for the group as a whole, gives orders, and bears most of the responsibility for the outcomes. A laissez-faire leader postpones making decisions or may never make a decision at all. Thus, laissez-faire leadership is really a lack of leadership. A democratic leader shares the planning, decision making, and responsibility for outcomes with other members of the group. This type of leader tends to provide guidance rather than control. There is no leadership style called management. PTS:1DIF:ModerateREF:p. 3 KEY: Nursing process: Implementation | Client need: SECE | Cognitive level: Application 3. A graduate nurse completed her nursing education 3 weeks ago and has just begun work at the local hospital. She is orienting to her new position with an experienced nurse, one who has been an RN for 15 years and an employee at the hospital for 7 years. She will provide guidance and practical teaching to the new graduate as she assumes a new position in the nursing unit. What role is the experienced RN assuming? 1) Mentor 2) Manager 3) Preceptor 4) Leader ANS: 3 A preceptor is someone with more experience who provides practical teaching and guidance for a student or new employee. In contrast, a mentor is someone more experienced who provides career development information and serves as a role model. A manager is an employee of an organization who has the power, authority, and responsibility for planning, organizing, coordinating, and directing the work of others. A leader is someone who has the ability to influence others and commit them to action. PTS:1DIF:ModerateREF:p. 7 KEY: Nursing process: Implementation | Client need: SECE | Cognitive level: Application 4. What is the first stage of the complex process of change? 1) Recognizing resistance 2) Unfreezing 3) Forming a comfort zone 4) Actively resisting ANS: 2 The first stage in the change process is unfreezing. In this stage, the person leaves the stable comfort zone that has existed and begins to make changes. Recognizing resistance and actively resisting are activities associated with change, but they are not the first stage of the process. PTS:1DIF:ModerateREF:p. 13 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Comprehension 5. Within the past month, there has been a change in the nursing documentation requirements at the hospital. The nurses have been trained in the new requirements and are documenting as requested, with the exception of one nurse. This nurse has been unable to attend any of the documentation in-service meetings and has been too busy to attend a private training session with the nurse manager. Meanwhile, she continues to use the old documentation process. What do the nurses actions illustrate? 1) Unfreezing 2) Active resistance 3) Passive resistance 4) Comfort zone ANS: 3 Passive resistance behaviors include avoidance; canceling appointments to discuss implementing change; being too busy to make the change; agreeing to the change but doing nothing to change; and simply ignoring the entire process as much as possible. In the above situation, the nurse is not actively refusing to comply with the new documentation requirements; however, her actions are a passive approach to resisting change. When a person knows what to expect and how to deal with whatever problems arise in the course of a day, that person is operating within her comfort zone. The first stage in the change process is when the person begins moving out of the comfort zone, unfreezing. This nurse is resisting, not unfreezing. PTS:1DIF:ModerateREF:p. 13 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Application 6. The surgical unit is experiencing difficulty recruiting new RNs, although the hospital has an excellent reputation in the community and has no difficulty recruiting nurses for other units. A task force has been formed, consisting of one nurse from each shift on the unit, the unit manager, and the hospital nurse recruiter. The group has gathered data and identified the problem. What is the next step in this process? 1) Generate possible solutions. 2) Evaluate whether the problem has been resolved. 3) Implement the solution changes. 4) Evaluate suggested solutions. ANS: 1 The next step in the process is to generate possible solutions. Once several possibilities have been identified, each of the suggested solutions should be evaluated. From among that list, the best solution is chosen and then implemented. Finally, the task force critiques the process by evaluating whether the problem has been resolved. PTS:1DIFifficultREF:pp. 15-16 KEY: Nursing process: Planning | Client need: SECE | Cognitive level: Application 7. A nurse with 2 years experience frequently appears stressed and has difficulty completing his work. He is clocking out 30 to 45 minutes late every day, even when his assignment load is light. The charge nurse describes his problem as running from one duty to the next and having no organization or daily routine. Which situation most likely describes this nurse? 1) Has time management problems 2) Has a heavy patient load 3) Works at a hospital that is understaffed 4) Is in a management position ANS: 1 This nurse most likely has trouble managing his time. Time management entails setting your own goals and organizing your work. Although there will be difficult days, the nurse who consistently finishes late and has no organization to his daily schedule has a problem managing time. Time management includes efficiently meeting clients care needs during a nursing shift and organizing ones workload. PTS:1DIF:EasyREF:pp. 16-17 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Analysis 8. An expert nurse feels confident in her role as a clinician on the unit. The nurse enjoys her work and feels in charge of her career. Which leadership state is she experiencing? 1) Power-based authority 2) Effective management skills 3) Empowerment in her role 4) Followership skills ANS: 3 Empowerment is a psychological state, a feeling of competence, control, and entitlement that a person experiences. Empowerment refers to feelings, whereas power refers to action. The person who feels empowered has feelings of self-determination, meaning, competence, and impact. This nurse may have power on the unit because of her expertise, but there is no evidence that she is an authority figure. Empowerment is not always associated with management. Managers have authority by virtue of their position but do not always thrive in that role. There is not enough information in the scenario to judge the nurses followership skills. PTS:1DIFifficultREF:p. 10 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Application 9. The physical therapy department and the nursing department at a local rehabilitation hospital are in conflict over which department is responsible for transporting patients to and from therapy appointments. The members of the therapy department state they do not have sufficient time to come to the nursing unit to pick up the patients and that patients often are not ready to be transported. Nursing staff members state that they do not have the time to transport the patients from the unit and this leaves a shortage of nursing personnel on the floor. Managers from both departments have attempted to resolve the conflict with input from nursing and therapy staff members. All attempts at conflict resolution have failed. What is the next step the managers should take? 1) Inform the nurses that they must take the patients to and from therapy. 2) Inform the therapists that they must take the patients to and from therapy. 3) Ask the hospital administrator to make an unbiased decision. 4) Begin informal negotiation between the two departments. ANS: 4 One of a managers responsibilities is to function as an informal negotiator when a resolution to conflict cannot be reached. PTS:1DIF:ModerateREF:pp. 15-16 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Application 10. The manager is conducting an informal negotiation between two staff members who have had ongoing difficulty working together peacefully. Most recently there was an argument about who would be scheduled for first lunch each day. At this stage of the informal negotiation, the manager is focusing on managing the emotions and setting the ground rules. Which stage does this demonstrate? 1) Setting the stage 2) Conducting the negotiation 3) Making offers and counteroffers 4) Agreeing on resolution of the conflict ANS: 2 The manager has begun conducting informal negotiation. This includes managing the emotions, setting ground rules, and clarifying the problem. The first step of conflict resolution is introspective and is similar to data gathering. The negotiator thinks, What am I trying to achieve? What problems am I likely to encounter? The next step, setting the stage, may involve confronting the two parties with their behavior toward one another and making direct statements designed to open communication and challenge them to seek resolution of the situation. After conducting the negotiation, the parties move to making offers and counteroffers, and then to agreeing on the resolution of the conflict. PTS:1DIF:ModerateREF:p. 16 KEY: Nursing process: Implementation | Client need: SECE | Cognitive level: Application 11. A nurse observes a nursing assistant (NAP) fail to wash her hands before and after placing a patient on a bedpan. When giving negative feedback to the NAP, the nurse should: 1) Be certain to offer constructive criticism about the task and do so in private. 2) Ask the unit manager to be present to document responses of both parties. 3) Call a meeting of all NAPs and stress hand washing to the entire group. 4) Keep a record of the NAPs actions and save them for her annual formal review. ANS: 1 It is important to provide negative feedback in private. It is not necessary for the nurse manager to be present because staff nurses are responsible for delegating to and supervision of NAPs. The nurse should not call a meeting. It would be a waste of time for those who are already washing their hands properly, and it dilutes the effect of the feedback to the NAP who is not washing her hands. She might think, Oh, everybody does it; no big deal. It is important to allow some time every day for timely feedback. This allows the worker to know what she is doing right and wrong, and allows her to make corrective actions. The nurse should not allow this NAP to continue with her hand washing errors until her annual formal review because this can pose a threat to patient safety and increase the risk of transmitting infectious microbes. PTS: 1 DIF: Moderate REF: pp. 7-8 KEY: Nursing process: Implementation | Client need: SECE | Cognitive level: Application Multiple Response Identify one or more choices that best complete the statement or answer the question. 1. Which of the following are characteristics of an effective nurse manager? Choose all that apply. 1) Clinical expertise 2) Business sense 3) Masters degree 4) Leadership skills ANS: 1, 2, 4 An effective nurse manager possesses a combination of qualities: leadership skills, clinical expertise, and business sense. It is the combination of all these that prepares a person for the complex task of managing a group or team of healthcare providers. The extent of education that a person has does not determine her effectiveness as a manager. PTS:1DIF:ModerateREF:p. 5 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Comprehension 2. Which of the following activities is/are involved when delegating tasks to other members of the nursing team? Choose all that apply. 1) Supervising patient care that is given 2) Determining the skill mix of unit personnel 3) Assessing the needs of the clients involved 4) Deciding which tasks to assign to a team member ANS: 1, 2, 3, 4 Delegation of patient care tasks to other healthcare workers is one of the most important responsibilities of the registered nurse. When delegating tasks, the nurse must take into consideration the skills and competency of the team members as well as the condition and needs of the clients receiving care. The nurse is also responsible for supervising patient care to ensure that it is competently delivered. PTS:1DIFifficultREF:pp. 12-13 KEY: Nursing process: Interventions | Client need: SECE | Cognitive level: Comprehension 3. An experienced nurse serves as a mentor to a new graduate. Which of the following are responsibilities of the person being mentored? Choose all that apply. 1) Demonstrates an ability to move toward independence 2) Has the ability to encourage excellence in others 3) Seeks feedback and uses it to modify behaviors 4) Demonstrates flexibility and an ability to change ANS: 1, 3, 4 The ability to encourage excellence in others is a responsibility of the mentor. Responsibilities of the person being mentored are the following: demonstrates an ability to move toward independence; seeks feedback and uses it to modify behaviors; and demonstrates flexibility and an ability to change. PTS:1DIF:ModerateREF:p. 8; Box 45-2 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Comprehension Completion Complete each statement. 1. Compared with management, is the ability to influence other people with or without an official appointment to a position in the organization. ANS: leadership PTS: 1 DIF: Easy REF: p. 2 KEY: Nursing process: N/A | Client need: SECE | Cognitive level: Comprehension 2. is the ability to influence other people despite resistance from them. Said another way, it is the ability of one person or group to impose his, or their, will on another person or group. ANS: Power PTS:1DIF:ModerateREF:p. 10 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 3. A(n) is someone with more experience who provides career development behaviors. ANS: mentor PTS:1DIF:EasyREF:pp. 6-7 KEY:Nursing process: N/A | Client need: SECE | Cognitive level: Recall 4. A(n) is an employee of an organization who has the power, authority, and responsibility for planning, organizing, coordinating, and directing the work of others. [Show More]
Last updated: 1 year ago
Preview 1 out of 195 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 29, 2021
Number of pages
195
Written in
Additional information
This document has been written for:
Uploaded
May 29, 2021
Downloads
1
Views
55

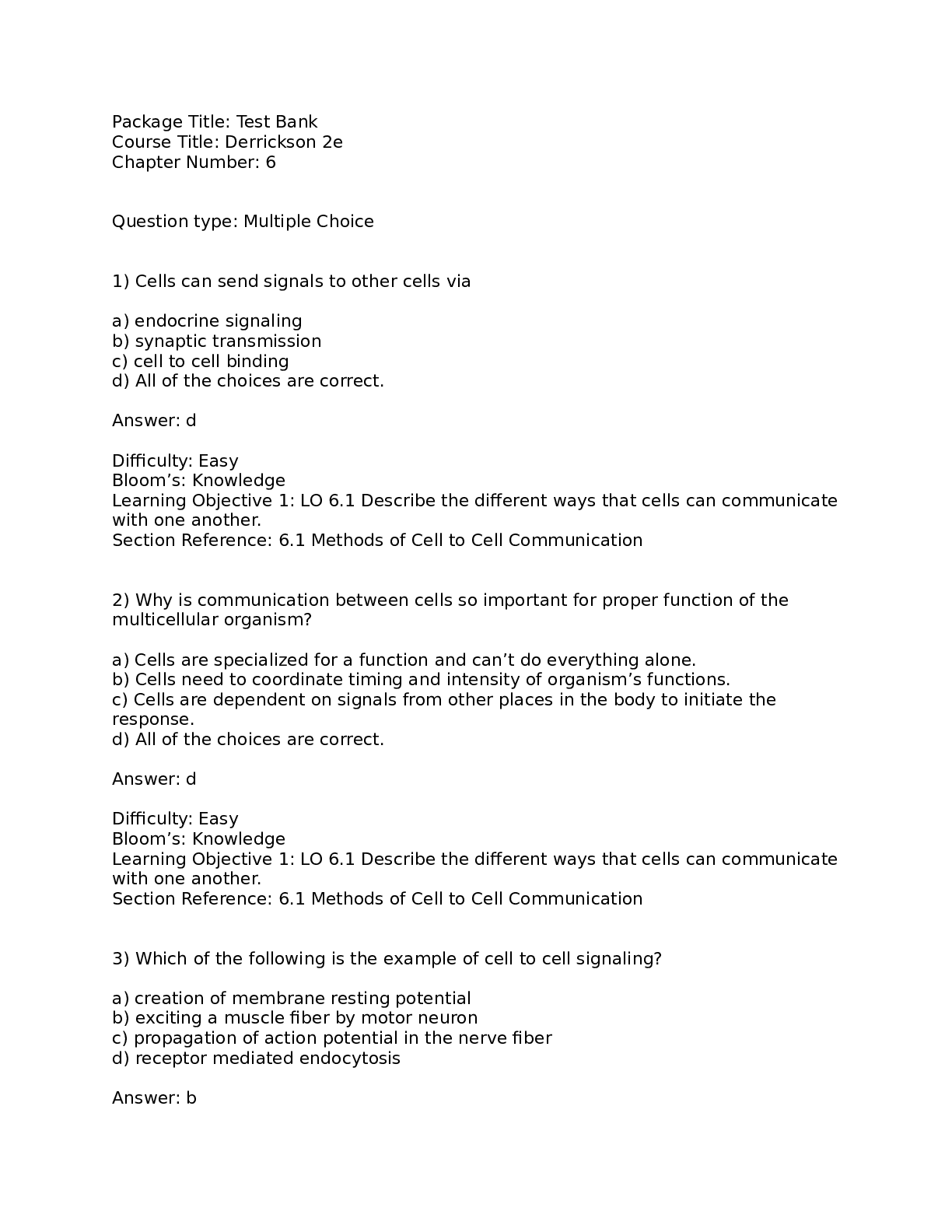
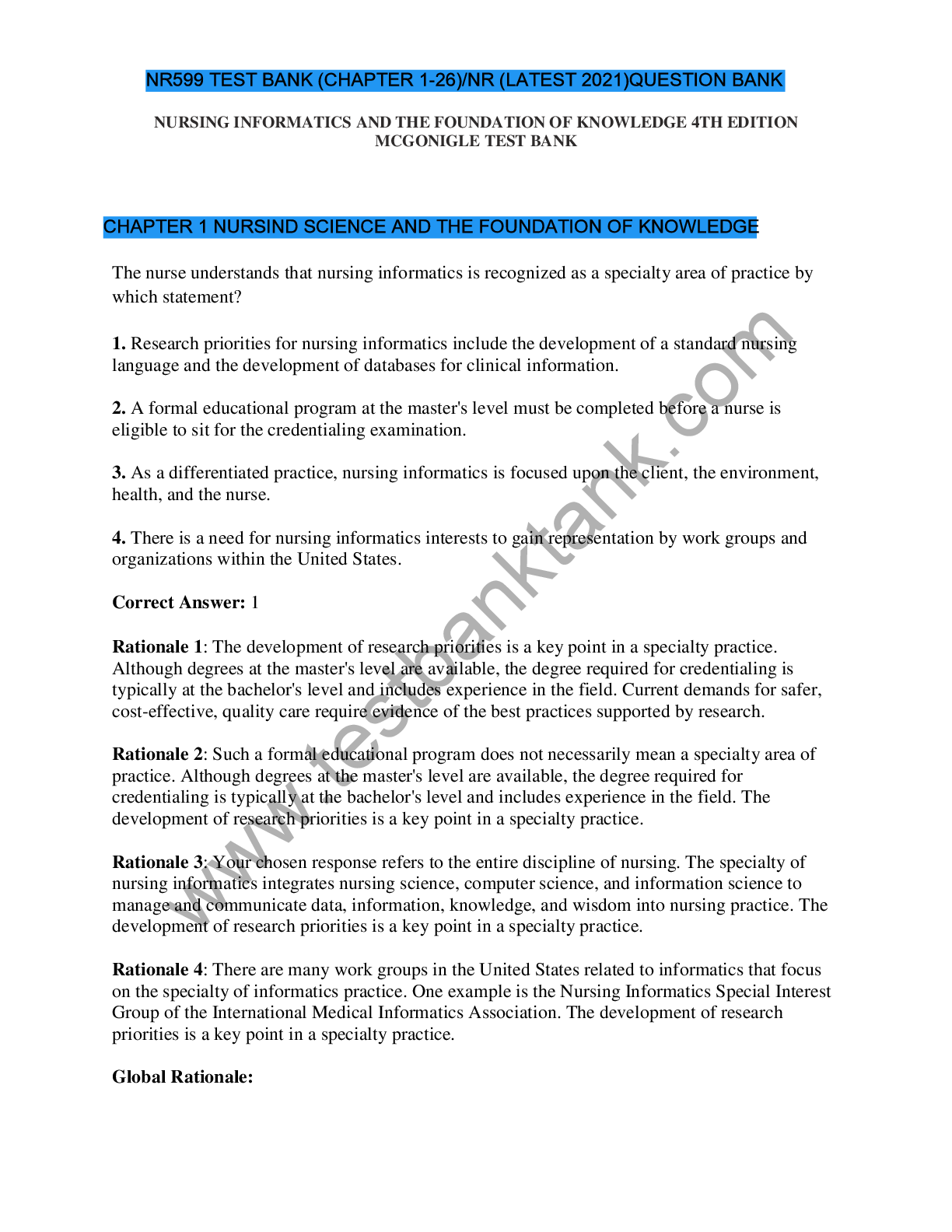
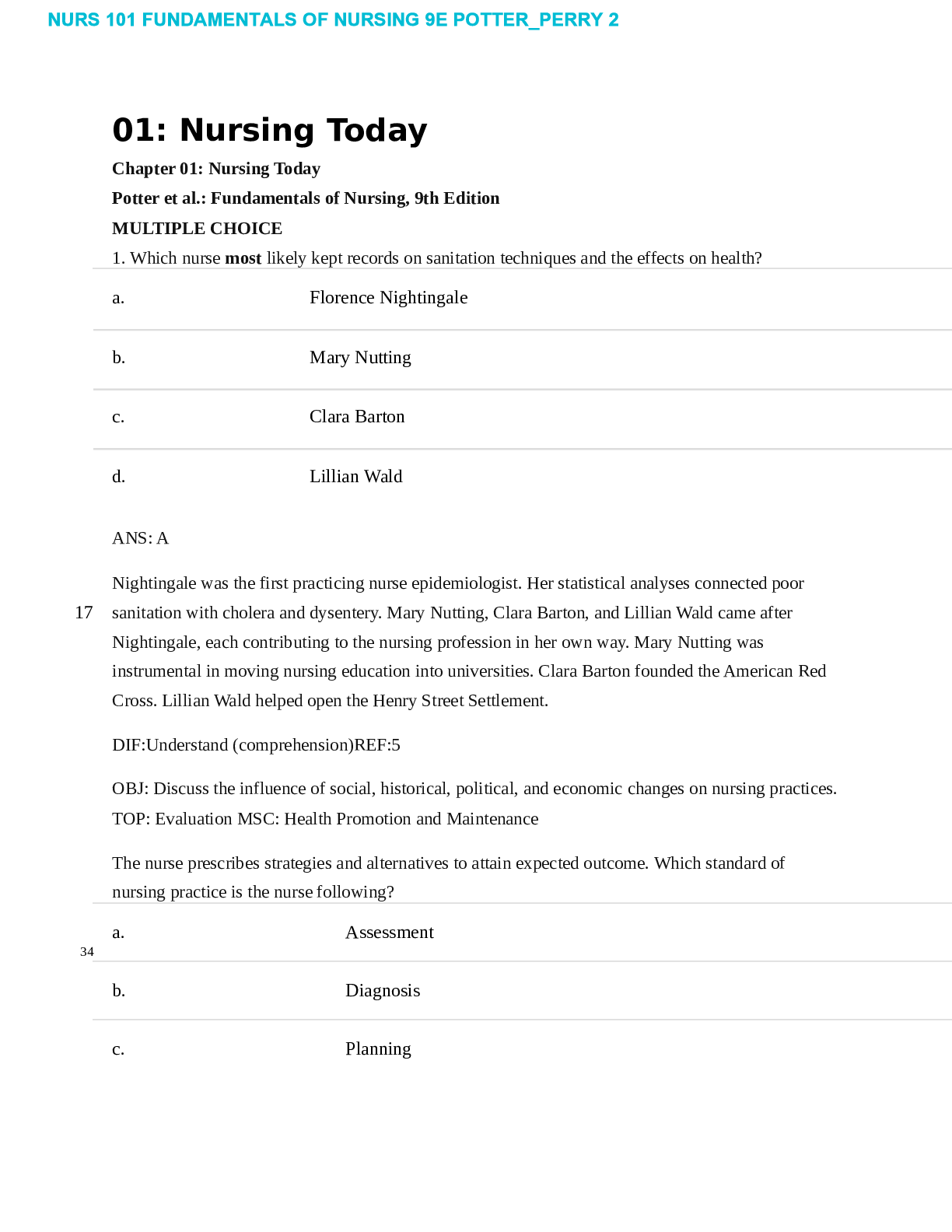

.png)