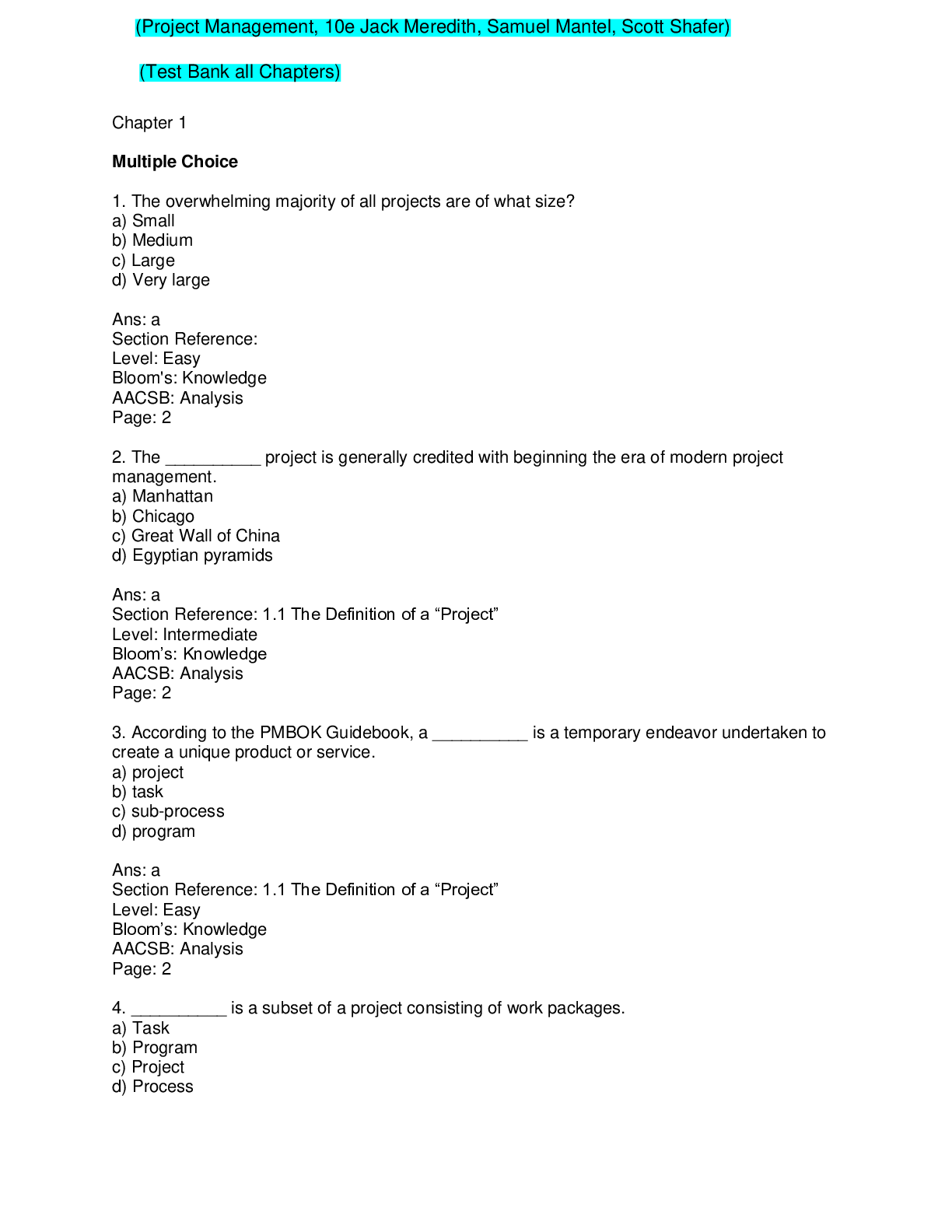
*NURSING > TEST BANK > Rubin’s Pathology: Clinicopathologic Foundations Of Medicine Seventh Edition Test Bank (All)
Rubin’s Pathology: Clinicopathologic Foundations Of Medicine Seventh Edition Test Bank
Document Content and Description Below
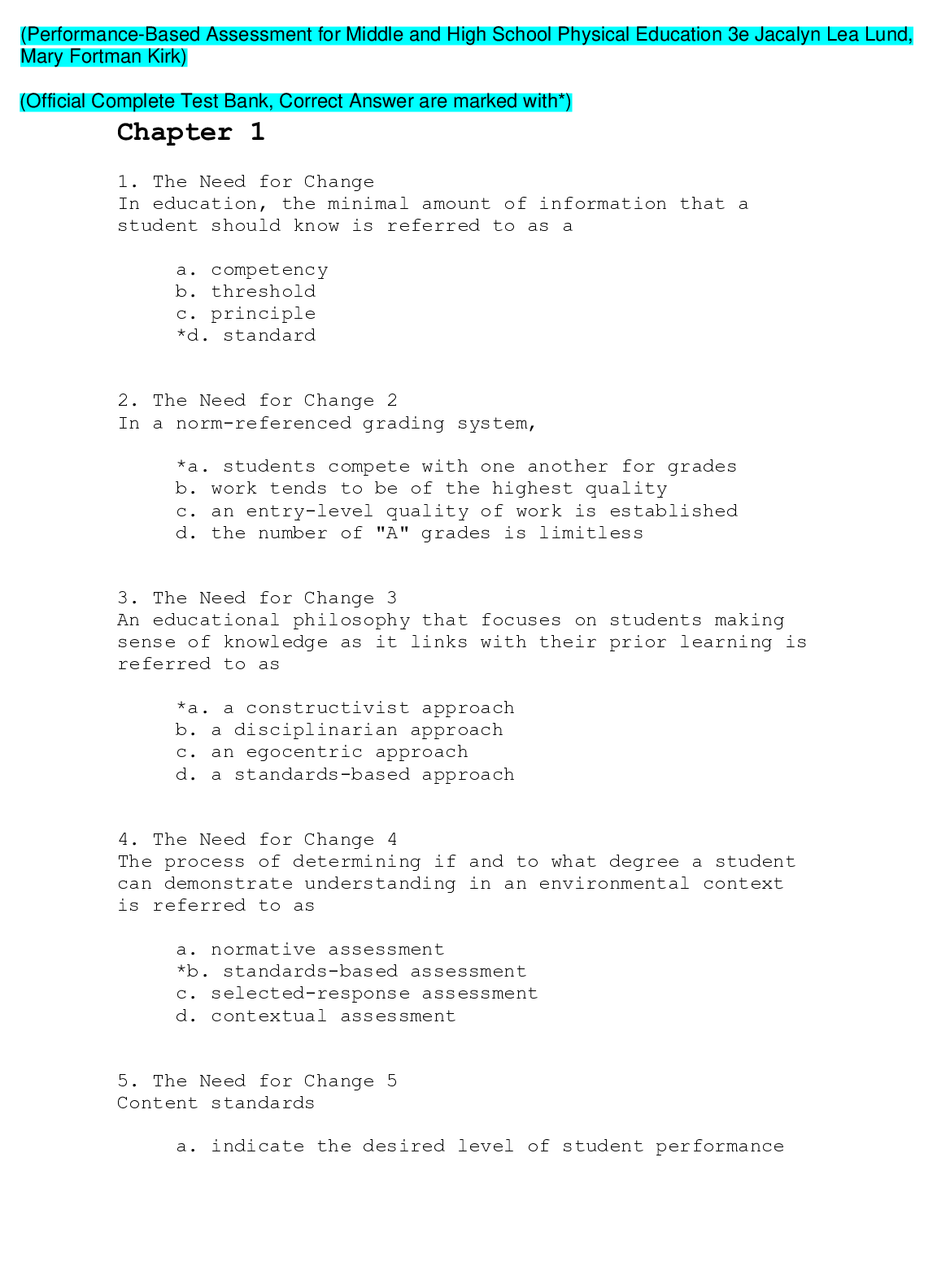
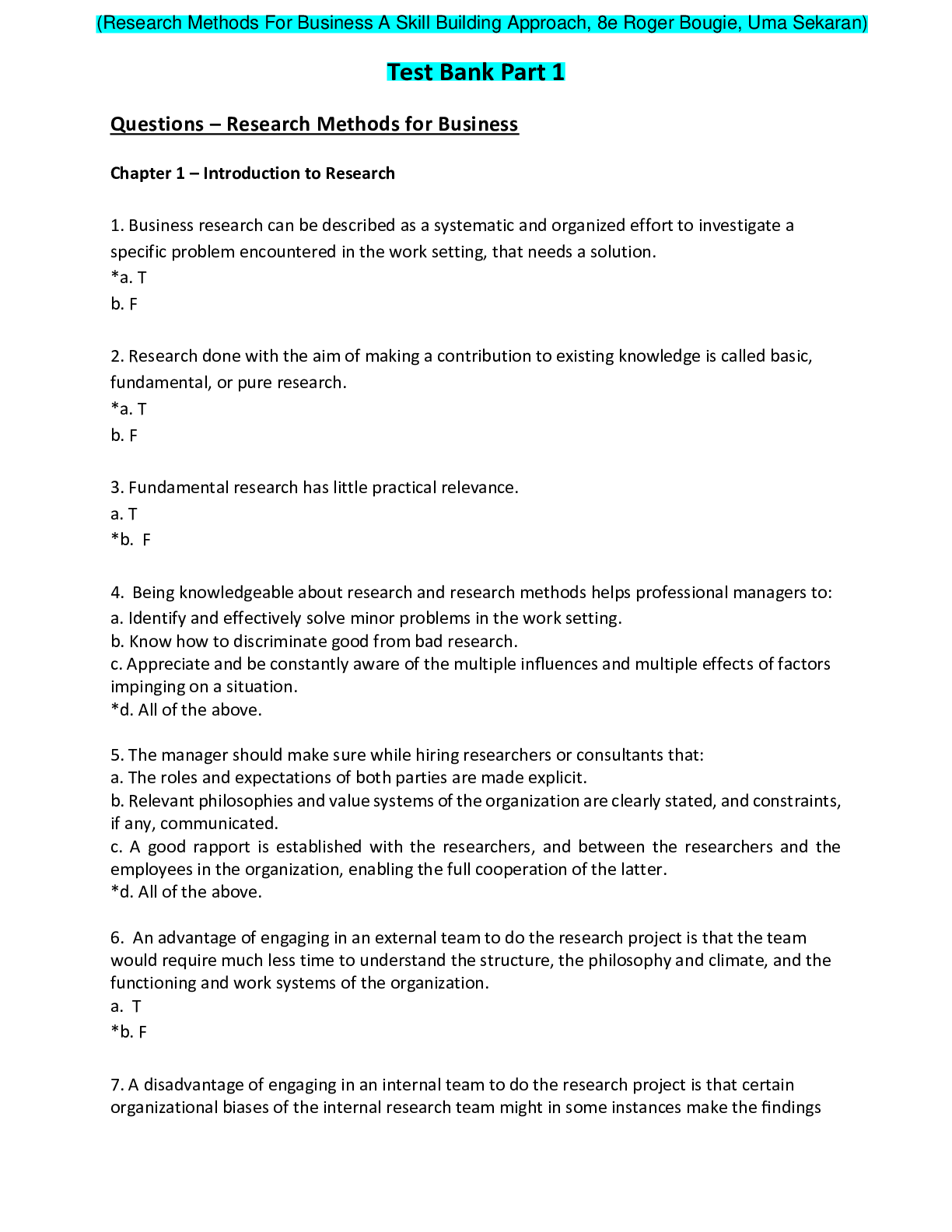
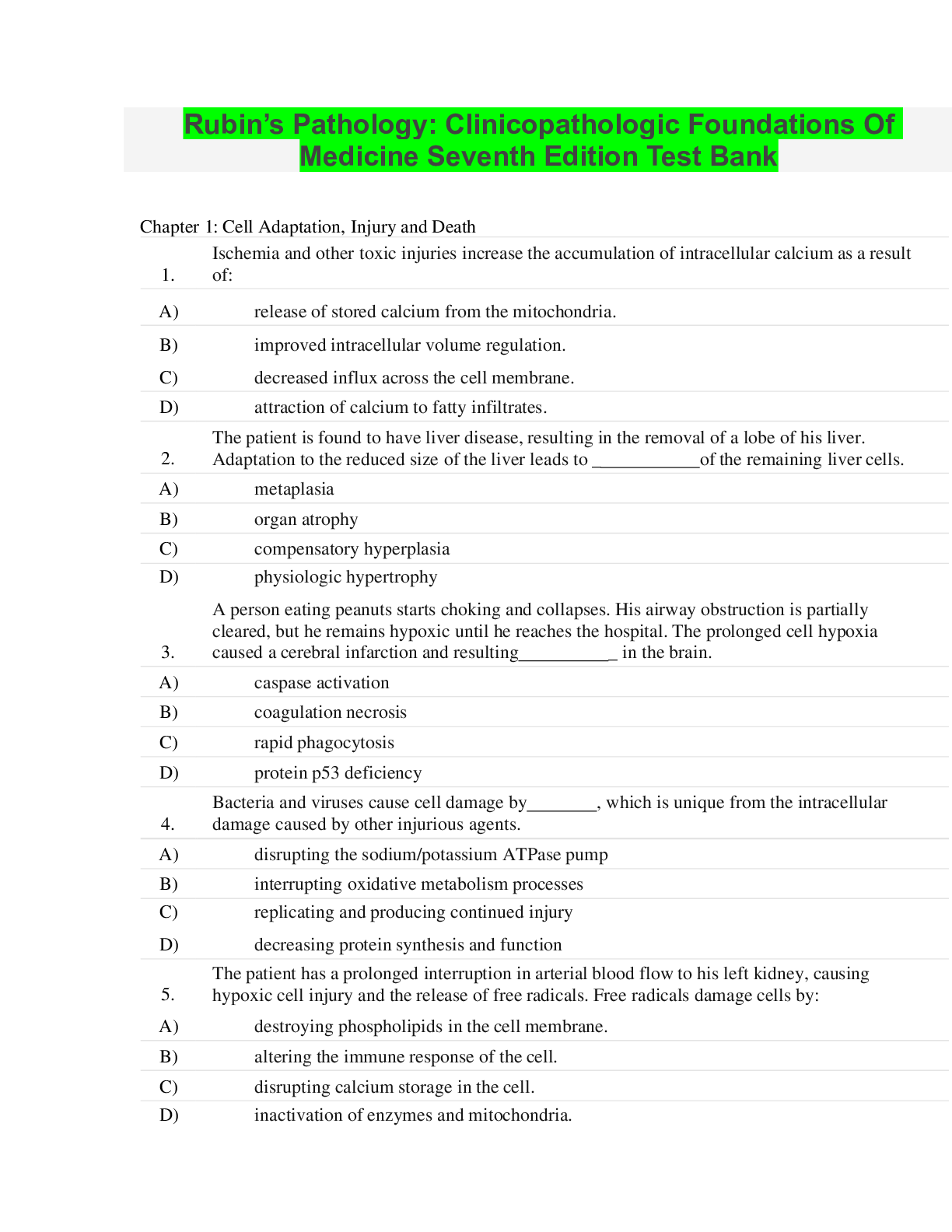
Rubin’s Pathology: Clinicopathologic Foundations Of Medicine Seventh Edition Test Bank Chapter 1: Cell Adaptation, Injury and Death 1. Ischemia and other toxic injuries increase the accumulation of ... intracellular calcium as a result of: A) release of stored calcium from the mitochondria. B) improved intracellular volume regulation. C) decreased influx across the cell membrane. D) attraction of calcium to fatty infiltrates. 2. The patient is found to have liver disease, resulting in the removal of a lobe of his liver. Adaptation to the reduced size of the liver leads to _ of the remaining liver cells. A) metaplasia B) organ atrophy C) compensatory hyperplasia D) physiologic hypertrophy 3. A person eating peanuts starts choking and collapses. His airway obstruction is partially cleared, but he remains hypoxic until he reaches the hospital. The prolonged cell hypoxia caused a cerebral infarction and resulting _ in the brain. A) caspase activation B) coagulation necrosis C) rapid phagocytosis D) protein p53 deficiency 4. Bacteria and viruses cause cell damage by , which is unique from the intracellular damage caused by other injurious agents. A) disrupting the sodium/potassium ATPase pump B) interrupting oxidative metabolism processes C) replicating and producing continued injury D) decreasing protein synthesis and function 5. The patient has a prolonged interruption in arterial blood flow to his left kidney, causing hypoxic cell injury and the release of free radicals. Free radicals damage cells by: A) destroying phospholipids in the cell membrane. B) altering the immune response of the cell. C) disrupting calcium storage in the cell. D) inactivation of enzymes and mitochondria. 6. Injured cells have impaired flow of substances through the cell membrane as a result of: A) increased fat load. B) altered permeability. C) altered glucose utilization. D) increased surface receptors. 7. Reversible adaptive intracellular responses are initiated by: A) stimulus overload. B) genetic mutations. C) chemical messengers. D) mitochondrial DNA. 8. Injured cells become very swollen as a result of: A) increased cell protein synthesis. B) altered cell volume regulation. C) passive entry of potassium into the cell. D) bleb formation in the plasma membrane. 9. A diabetic patient has impaired sensation, circulation, and oxygenation of his feet. He steps on a piece of glass, the wound does not heal, and the area tissue becomes necrotic. The necrotic cell death is characterized by: A) rapid apoptosis. B) cellular rupture. C) shrinkage and collapse. D) chronic inflammation. 10. A 99-year-old woman has experienced the decline of cell function associated with age. A group of theories of cellular aging focus on programmed: A) changes with genetic influences. B) elimination of cell receptor sites. C) insufficient telomerase enzyme. D) DNA mutation or faulty repair. 11. An 89-year-old female patient has experienced significant decreases in her mobility and stamina during a 3-week hospital stay for the treatment of a femoral head fracture. Which of the following phenomena most likely accounts for the patients decrease in muscle function that underlies her reduced mobility? A) Impaired muscle cell metabolism resulting from metaplasia B) Dysplasia as a consequence of inflammation during bone remodeling C) Disuse atrophy of muscle cells during a prolonged period of immobility D) Ischemic atrophy resulting from vascular changes while on bedrest 12. A 20-year-old college student has presented to her campus medical clinic for a scheduled Papanicolaou (Pap) smear. The clinician who will interpret the smear will examine cell samples for evidence of: A) changes in cell shape, size, and organization. B) the presence of unexpected cell types. C) ischemic changes in cell samples. D) abnormally high numbers of cells in a specified field. 13. Which of the following pathophysiologic processes is most likely to result in metastatic calcification? A) Benign prostatic hyperplasia B) Liver cirrhosis C) Impaired glycogen metabolism D) Hyperparathyroidism 14. Despite the low levels of radiation used in contemporary radiologic imaging, a radiology technician is aware of the need to minimize her exposure to ionizing radiation. What is the primary rationale for the technicians precautions? A) Radiation stimulates pathologic cell hypertrophy and hyperplasia. B) Radiation results in the accumulation of endogenous waste products in the cytoplasm. C) Radiation interferes with DNA synthesis and mitosis. D) Radiation decreases the action potential of rapidly dividing cells. 15. The parents of a 4-year-old girl have sought care because their daughter has admitted to chewing and swallowing imported toy figurines that have been determined to be made of lead. Which of the following blood tests should the care team prioritize? A) White blood cell levels with differential B) Red blood cell levels and morphology C) Urea and creatinine levels D) Liver function panel 16. A 70-year-old male patient has been admitted to a hospital for the treatment of a recent hemorrhagic stroke that has left him with numerous motor and sensory deficits. These deficits are most likely the result of which of the following mechanisms of cell injury? A) Free radical injury B) Hypoxia and ATP depletion C) Interference with DNA synthesis D) Impaired calcium homeostasis 17. Which of the following processes associated with cellular injury is most likely to be reversible? A) Cell damage resulting from accumulation of fat in the cytoplasm B) Cellular changes as a result of ionizing radiation C) Cell damage from accumulation of free radicals D) Apoptosis 18. The extrinsic pathway of apoptosis can be initiated by: A) damage to cellular DNA. B) decreased ATP levels. C) activation of the p53 protein. D) activation of death receptors on the cell surface. 19. A patient with severe peripheral vascular disease has developed signs of dry gangrene on the great toe of one foot. Which of the following pathophysiologic processes most likely contributed to this diagnosis? A) Inappropriate activation of apoptosis B) Bacterial invasion C) Impaired arterial blood supply D) Metaplastic cellular changes 20. Which of the following facts underlies the concept of replicative senescence? A) Genes controlling longevity are present or absent in varying quantities among different individuals. B) Telomeres become progressively shorter in successive generations of a cell. C) The damaging influence of free radicals increases exponentially in later generations of a cell. D) Aging produces mutations in DNA and deficits in DNA repair. Chapter 2: Inflammation MULTIPLE CHOICE 1. Tears are considered to be part of the: 1. first line of defense. 2. second line of defense. 3. third line of defense. 4. specific defenses. 5. nonspecific defenses. a. 1, 4 b. 1, 5 c. 3, 4 d. 2, 5 ANS: B 2. A specific defense for the body is: a. phagocytosis. b. sensitized T lymphocytes. c. the inflammatory response. d. intact skin and mucous membranes. ANS: B 3. The inflammatory response is a nonspecific response to: a. phagocytosis of foreign material. b. local vasodilation. c. any tissue injury. d. formation of purulent exudates. ANS: C 4. Chemical mediators released during the inflammatory response include: a. albumin and fibrinogen. b. growth factors and cell enzymes. c. macrophages and neutrophils. d. histamine and prostaglandins. ANS: D 5. Which of the following result directly from the release of chemical mediators following a moderate burn injury? 1. Pain 2. Local vasoconstriction 3. Increased capillary permeability 4. Pallor a. 1, 2 b. 1, 3 c. 2, 3 d. ANS: B 6. Granulation tissue 2, 4 is best described as: a. highly vascular, very fragile, and very susceptible to infection. b. an erosion through the wall of viscera, leading to complications. c. a type of adhesion with no vascularization. d. a form of stenosis, in a duct, that is extremely tough and resists attack by microbes. ANS: A 7. Edema associated with inflammation results directly from: a. increased fluid and protein in the interstitial compartment. b. increased phagocytes in the affected area. c. decreased capillary permeability. d. general vasoconstriction. ANS: A 8. The warmth and redness related to the inflammatory response results from: a. increased interstitial fluid. b. production of complement. c. a large number of white blood cells (WBCs) entering the area. d. increased blood flow into the area. ANS: D 9. What is the correct order of the following events in the inflammatory response immediately after tissue injury? 1. Increased permeability of blood vessels 2. Dilation of blood vessels 3. Transient vasoconstriction 4. Migration of leukocytes to the area 5. Hyperemia a. 5, 3, 2, 1, 4 b. 1, 2, 4, 5, 3 c. 2, 3, 5, 4, 1 d. 3, 2, 5, 1, 4 ANS: D 10. The process of phagocytosis involves the: a. ingestion of foreign material and cell debris by leukocytes. b. shift of fluid and protein out of capillaries. c. formation of a fibrin mesh around the infected area. d. movement of erythrocytes through the capillary wall. ANS: A 11. Systemic effects of severe inflammation include: a. erythema and warmth. b. loss of movement at the affected joint. c. fatigue, anorexia, and mild fever. d. abscess formation. ANS: C 12. The term leukocytosis means: a. increased white blood cells (WBCs) in the blood. b. decreased WBCs in the blood. c. increased number of immature circulating leukocytes. d. significant change in the proportions of WBCs. ANS: A 13. Which of the following statements applies to fever? a. Viral infection is usually present. b. Heat-loss mechanisms have been stimulated. c. It is caused by a signal to the thalamus. d. It results from release of pyrogens into the circulation. ANS: D 14. Mechanisms to bring an elevated body temperature down to the normal level include: a. general cutaneous vasodilation. b. generalized shivering. c. increased heart rate. d. increased metabolic rate. ANS: A 15. Replacement of damaged tissue by similar functional cells is termed: a. fibrosis. b. regeneration. c. resolution. d. repair by scar tissue. ANS: B 16. Scar tissue consists primarily of: a. granulation tissue. b. epithelial cells. c. collagen fibers. d. new capillaries and smooth muscle fibers. ANS: C 17. Which of the following promotes rapid healing? a. Closely approximated edges of a wound b. Presence of foreign material c. Exposure to radiation d. Vasoconstriction in the involved area ANS: A 18. Glucocorticoids are used to treat inflammation because they directly: a. promote the release of prostaglandins at the site. b. decrease capillary permeability. c. mobilize lymphocytes and neutrophils. d. prevent infection. ANS: B 19. Patients taking glucocorticoids for long periods of time are likely to develop all of the following EXCEPT: a. decreased bone density. b. wasting of skeletal muscle. c. opportunistic infections. d. increased leukocyte production. ANS: D 20. Which of the following drugs relieves fever and some types of pain but is NOT an anti-inflammatory agent? a. Acetaminophen b. Prednisone c. Aspirin d. Ibuprofen ANS: A 21. A burn area in which the epidermis and part of the dermis is destroyed is classified as: a. full-thickness. b. deep partial-thickness. c. superficial partial-thickness. d. first-degree. ANS: B 22. A woman has burns on the anterior surfaces of her right arm, chest, and right leg. The percentage of body surface area burned is approximately: a. 13.5%. b. 18%. c. 22.5%. d. 31.5%. ANS: C 23. The characteristic appearance of a full-thickness burn is: a. painful with multiple blisters. b. heavy bleeding. c. red with some swelling. d. dry, firm, charred, or hard white surface. ANS: D 24. A typical source of infection in burn areas is: a. the skin grafts. b. microbes surviving in the hair follicles in the burn area. c. circulating blood bringing microbes to the burn wound. d. opportunistic virus in digestive tract. ANS: B 25. A large burn area predisposes to decreased blood pressure because: a. bleeding occurs under the burn surface. b. the heart is damaged by toxic materials from the burn. c. fluid and protein shift out of the blood. d. vasoconstriction occurs in the burn area. ANS: C 26. During an inflammatory response, hyperemia is caused by: a. increased blood flow in the area. b. increased capillary permeability. c. irritation of sensory nerve endings by histamine. d. increased leukocytes in the area. ANS: A 27. The advantages of applying a biosynthetic skin substitute to a large area of full- thickness burns include: 1. reduced risk of infection. 2. decreased loss of plasma protein and fluid. 3. developing stronger fibrous scar tissue. 4. more rapid healing. 5. regeneration of all glands, nerves, and hair follicles. a. 1, 3 b. 4, 5 c. 1, 2, 4 d. 2, 3, 5 ANS: C 28. Purulent exudates usually contain: a. small amounts of plasma protein & histamine in water. b. red blood cells & all types of white blood cells. c. numerous leukocytes, bacteria, and cell debris. d. large amounts of water containing a few cells. ANS: C 29. Isoenzymes in the circulating blood: a. are a type of plasma protein normally present in the circulating blood. b. often indicate the precise location of an inflammatory response. c. are normally released from leukocytes during the inflammatory response. d. are pyrogens, causing low-grade fever. ANS: B 30. A serous exudate is best described as a: a. thin, watery, colorless exudate. b. thick, sticky, cloudy secretion. c. thick, greenish material containing microbes. d. brownish, clotted material. ANS: A 31. Systemic manifestations of an inflammatory response include: a. edema and erythema. b. area of necrosis and loss of function. c. pain and tenderness. d. fever and malaise. ANS: D 32. Some local effects of a general inflammatory response would include: a. high, spiking fever and chills. b. redness, warmth, and swelling. c. leukopenia and reduced erythrocyte sedimentation rate (ESR). d. anorexia and headaches. ANS: B 33. Prolonged administration of glucocorticoids such as prednisone may cause: 1. atrophy of lymphoid tissue. 2. increased resistance to infection. 3. thrombocytopenia. 4. decreased protein synthesis. a. 1, 2 b. 1, 3 c. 1, 4 d. 2, 4 ANS: C 34. Application of ice to an injured knee reduces edema by: a. promoting return of lymph fluid. b. causing local vasoconstriction. c. increasing the rate of tissue repair. d. causing systemic vasodilation. ANS: B 35. Healing of large areas of skin loss (including dermis and epidermis) would be most successful through: a. rapid mitosis and regeneration of skin layers. b. resolution of damaged cells in the area. c. covering the area with biosynthetic skin substitute. d. graft of fibrous tissue to the area. ANS: C 36. Prostaglandins are produced from and cause . a. activated plasma protein; increased capillary permeability b. mast cells; vasodilation and pain c. platelets; attraction of neutrophils, chemotaxis d. mast cell granules; activation of histamines and kinins ANS: B 37. The number of neutrophils in the blood is increased significantly: a. during allergic reactions. b. during chronic inflammation. c. to produce antibodies. d. in order to promote phagocytosis. ANS: D 38. An abscess contains: a. serous exudate. b. purulent exudate. c. fibrinous exudate. d. hemorrhagic exudate. ANS: B 39. Nonspecific agents that protect uninfected cells against viruses are called: a. neutrophils. b. macrophages. c. interferons. d. pyrogens. ANS: C 40. Causes of inflammation include: a. direct physical damage such as cuts and sprains. b. allergic reactions. c. infection. d. All the above ANS: D 41. In normal capillary exchange, what is net hydrostatic pressure based on? a. The difference between the hydrostatic pressure within the capillary, as compared with the hydrosta pressure of the interstitial fluid b. The relative osmotic pressures in the blood and the interstitial fluid c. The difference between the hydrostatic pressure and osmotic pressure within the capillary d. The difference between the concentrations of blood cells, plasma proteins, and dissolved substances the blood and the interstitial fluid ANS: A 42. The cardinal signs of inflammation include all of the following EXCEPT: a. redness. b. loss of function. c. nausea. d. swelling. ANS: C 43. Drugs that have anti-inflammatory, analgesic, and antipyretic activities include: 1. COX-2 inhibitors (NSAIDs). 2. glucocorticoids (e.g., prednisone). 3. ibuprofen (NSAID). 4. acetaminophen. 5. aspirin (ASA). a. 1, 2 b. 2, 4 c. 1, 3, 5 d. 1, 4, 5 ANS: C 44. Aspirin (ASA) is discouraged for treatment of viral infection in children because of: a. decreased bone growth after puberty. b. frequent production of blood clots. c. formation of a granuloma filled with virus. d. the risk of developing Reyes syndrome. ANS: D 45. Systemic manifestations of inflammation include all EXCEPT: a. pyrexia. b. malaise. c. local swelling. d. anorexia. ANS: C 46. Which of the following cellular elements found in the inflammatory response are responsible for phagocytosis? a. Macrophages b. Basophils c. B lymphocytes d. T lymphocytes e. Eosinophils ANS: A 47. Which chemical mediator is involved in prolonging the inflammatory response? a. Bradykinin b. Histamine c. Leukotrienes d. Chemotactic factors ANS: C 48. Potential complications after healing by scar formation include all the following EXCEPT: a. lack of sensory function in the area. b. contractures and adhesions. c. increased hair growth. d. keloid formation. ANS: C 49. All of the following are correct statements regarding wound healing EXCEPT: a. Resolution occurs where there is minimal tissue damage and the cells can recover. b. Granulation tissue forms a permanent replacement for damaged tissue. c. Regeneration occurs where the cells are capable of mitosis. d. Scar tissue forms where the surrounding cells are incapable of mitosis. ANS: B 50. Which of the following statements regarding inflammation is incorrect? a. Inflammation caused by an allergen or a burn will typically produce a serous exudate. b. Infection is one cause of inflammation. c. Inflammation is the bodys nonspecific response to tissue injury. d. Disorders are named using the ending -sarcoma to indicate inflammation. ANS: D 51. Which of the following helps to localize and wall off the foreign material during an inflammatory response? a. Lymphocytes b. Increased fluid c. Fibrinogen d. Antibodies ANS: C 52. Why is an application of cold recommended as part of the RICE first aid measures immediately following an inflammatory response due to injury? a. It improves circulation in the area removing chemical mediators. b. It causes local vasoconstriction to reduce local edema. c. It draws more phagocytic cells to the area to remove debris. d. It promotes immediate healing. ANS: B 53. One goal for current research in tissue engineering is to: a. create a functional replacement tissue when regeneration is not possible. b. adapt cells from the injured organ to produce replacement tissue. c. design a nonliving synthetic replacement tissue. d. use stem cells as a temporary covering for damaged tissue. ANS: A 54. Identify the proper sequence in the healing process. a. A blood clot forms; granulation tissue grows into the gap; new blood vessels develop; phagocytosis foreign material and cell debris occurs; and collagen fibers form a tight, strong scar. b. A blood clot forms; phagocytes remove foreign material and cell debris; granulation tissue grows in gap; new blood vessels form; and collagen fibers promote formation of a tight, strong scar. c. Collagen fibers form in the damaged area; a blood clot forms; granulation tissue grows into the gap angiogenesis takes place; and foreign material and cell debris are removed by phagocytes. d. Foreign material and cell debris are removed by phagocytes; a blood clot forms; granulation tissue into the gap; new blood vessels form; and collagen fibers grow and cross-link. ANS: B 55. All of the following are factors that promote healing EXCEPT: a. good nutrition: protein, vitamins A and C. b. a clean, undisturbed wound. c. effective circulation. d. advanced age. ANS: D 56. Identify the correct statement about burns: a. The severity of the burn depends on the temperature, duration, and extent of the burn. b. Young children are less likely to suffer severe burns from immersion in excessively hot water. c. Burns to the palms of the hands are more damaging than burns on the face. d. With a major burn, excessive bleeding usually causes shock. ANS: A 57. Which statement applies to the recommended emergency care for burns? a. Drop and lie completely still on your back. b. Call a neighbor for help if the burn appears to be extensive. c. Apply lotion and cover burn tightly with a sheet or towel. d. Cover the burn area with clean, cool, or tepid water and remove nonsticking clothing. ANS: D 58. Inhalation of carbon monoxide is a threat for many burn patients because this gas: a. causes swelling in the trachea. b. quickly reduces the available oxygen in the blood. c. prevents full expansion of the lungs. d. is toxic to the nervous system. ANS: B 59. How does scar tissue usually cause obstructions to develop in tube-like structures? a. Scar tissue continues to grow and spread, causing a blockage. b. Scar tissue does not stretch, but rather shrinks in time, causing narrowing. c. Scar tissue twists and forms knots as it develops. d. Scar tissue attaches to nearby normal tissue, causing obstruction. ANS: B 60. Which of the following is a serious potential complication found only with the anti- inflammatory COX-2 inhibitor drugs? a. Increased risk of infection at the site of inflammation b. Reyes syndrome developing in children and young adults c. Increased incidence of heart attacks d. Greatly delayed blood clotting ANS: C Chapter 3: Repair, Regeneration and Fibrosis MULTIPLE CHOICE 1. A public health nurse is teaching the community about health promotion. Which information should the nurse include for innate immunity? Innate immunity is gained: a. Following an illness b. At birth c. Via injection of specific antibodies d. In adulthood ANS: B Innate immunity is present at birth. Innate immunity is present at birth and does not require an illness. Innate immunity is present at birth and does not require injection. Innate immunity is present at birth. REF: 2. Which statement indicates teaching was successful regarding collectins? Collectins are produced by the: a. Kidneys b. Bowel c. Lungs d. Integument ANS: C Collectins are produced by the lungs. Collectins are produced by the lungs, not the kidneys. Collectins are produced by the lungs, not the bowel. Collectins are produced by the lungs, not the integument. REF: 3. A 20-year-old male received a knife wound to the arm during an altercation. Which of the following types of immunity was compromised? a. Innate immunity b. Inflammatory response c. Adaptive immunity d. Specific immunity ANS: A The epithelial cells of the skin are a part of innate immunity. The inflammatory response is not a type of immunity. Adaptive immunity is represented by the normal flora of the bowel. Specific immunity is a type of adaptive immunity and is not associated with a break in skin integrity. REF: 4. Biochemical secretions that trap and kill microorganisms include: a. Hormones b. Neurotransmitters c. Earwax d. Gastric acid ANS: C Epithelial cells secrete several substances that protect against infection, including earwax. Hormones do not contain biochemical secretions that trap and kill microorganisms. Neurotransmitters carry important messages, but they do not contain biochemical secretions. Gastric acid helps break down food into its component parts, but does not contain biochemical secretions. 5. A 25-year-old female presents to her primary care provider reporting vaginal discharge of a white, viscous, and foul-smelling substance. She reports that she has been taking antibiotics for the past 6 months. Which finding will the nurse most likely see on the microorganism report? a. Clostridium difficile overgrowth b. Decreased Lactobacillus c. Streptococcus overgrowth d. Decreased Candida albicans ANS: B Diminished colonization with Lactobacillus that occurs as a result of prolonged antibiotic treatment increases the risk for vaginal infections, such as vaginosis. Clostridium difficile occurs in the colon, not the vagina. Streptococcus overgrowth will occur in the mouth. Candida albicans occurs in the colon, not the vagina. 6. When an aide asks the nurse what is a purpose of the inflammatory process, how should the nurse respond? a. To provide specific responses toward antigens b. To lyse cell membranes of microorganisms c. To prevent infection of the injured tissue d. To create immunity against subsequent tissue injury ANS: C One purpose of the inflammatory process is to prevent infection and further damage by contaminating microorganisms. Specific response toward antigens is a part of the complement system that assists in the inflammatory response, but not its purpose. Lysis of cell membranes is part of the process of phagocytosis, which removes foreign material, but this is not the purpose of the inflammatory response. Immunity cannot be achieved against future tissue injury. 7. A child fell off the swing and scraped the right knee. The injured area becomes painful. What else will the nurse observe upon assessment? a. Vasoconstriction at injured site b. Decreased RBC concentration at injured site c. Pale skin at injured site d. Edema at injured site ANS: D Increased vascular permeability and leakage of fluid out of the vessel cause edema at the site of injury. Vasodilation occurs, not vasoconstriction. Increased RBCs come to the site, not fewer. Redness occurs, not paleness, during inflammation. 8. A nurse recalls the mast cell, a major activator of inflammation, initiates the inflammatory response through the process of: a. Chemotaxis b. Endocytosis c. Degranulation d. Opsonization ANS: C Degranulation of mast cells is a major cellular component of inflammation. Chemotaxis is the process of white cell migration. Endocytosis is a part of phagocytosis and is not a factor in mast cell response. Opsonization is part of phagocytosis and is not a factor in mast cell response. 9. Which of the following individuals would be at greatest risk for an opportunistic infection? a. 18-year-old with diabetes b. 70-year-old with congestive heart failure c. 24-year-old who is immunocompromised d. 30-year-old with pneumonia ANS: C Opportunistic microorganisms can cause disease if the individuals defenses are compromised. An 18-year-old with diabetes would not be immunocompromised and would not be at risk. A 70-year-old with congestive heart failure would not be immunocompromised and would not be at risk. A 30-year-old with pneumonia would not be immunocompromised and would not be at risk. 10. The directional migration of leukocytes along a chemical gradient is termed: a. Chemotaxis b. Endocytosis c. Margination d. Diapedesis ANS: A Chemotaxis is the process by which leukocytes undergo directed migration. Endocytosis is a form of engulfment and a part of phagocytosis. Margination occurs when leukocytes adhere to endothelial cells in the walls of vessels. Diapedesis is the emigration of the cells through cell junctions that have loosened in response to inflammatory mediators. 11. A 20-year-old male shoots his hand with a nail gun while replacing roofing shingles. Which of the following cell types would be the first to aid in killing bacteria to prevent infection in his hand? a. Eosinophils b. Neutrophils c. Leukotrienes d. Monocytes ANS: B Neutrophils are the predominant phagocytes in the early inflammatory site, arriving within 6 to 12 hours after the initial injury. Eosinophils help limit and control inflammation. Leukotrienes are activators of the inflammatory response. Monocytes enter much later and replace leukocytes. 12. The predominant phagocyte of early inflammation is the: a. Eosinophil b. Neutrophil c. Lymphocyte d. Macrophage ANS: B Neutrophils are the predominant phagocytes in the early inflammatory site, arriving within 6 to 12 hours after the initial injury. Eosinophils help limit and control inflammation, but they are not the prominent phagocyte. Lymphocytes are part of the innate immune response. Macrophages kill microorganisms. 13. A 25-year-old female experiences a headache and takes aspirin for relief. A nurse recalls aspirin relieves the headache by: a. Decreasing leukotriene production b. Increasing histamine release c. Decreasing prostaglandin production d. Increasing platelet-activating factor ANS: C Aspirin is a prostaglandin inhibitor. Aspirin inhibits prostaglandins; it does not affect leukotriene production. Aspirin inhibits prostaglandins; it does not affect histamine release. Aspirin does not play a role in the platelet activating factor; this is a leukotriene response. 14. Which factor will help the nurse differentiate leukotrienes from histamine? a. Site of production b. Vascular effect c. Chemotactic ability d. Time of release ANS: D Leukotrienes are released slower and longer than histamine. Leukotrienes and histamine are produced from mast cells. Leukotrienes and histamine have similar vascular effects. Leukotrienes and histamine have similar chemotactic ability. 15. A 25-year-old male is in a car accident and sustains a fracture to his left femur with extensive soft tissue injury. The pain associated with the injury is related to: a. Histamine and serotonin b. Kinins and prostaglandins c. Vasoconstriction d. Immune complex formation ANS: B Prostaglandins cause increased vascular permeability, neutrophil chemotaxis, and pain by direct effects on nerves. Kinins also promote pain. Prostaglandins produce pain; histamine promotes vasodilation. Prostaglandins produce pain, not vasoconstriction. Prostaglandins produce pain, not the immune complex. 16. The complement, clotting, and kinin systems share which of the following characteristics? a. Activation of a series of proenzymes b. Phagocytosis initiation c. Granulocyte production d. Activated by interferon ANS: A The complement system, the clotting system, and the kinin system are normally in inactive forms, but can activate in a series as proenzymes and are involved in the inflammatory process. The complement system, the clotting system, and the kinin system do not play a role in phagocytosis, but do play a role in the inflammatory response as proenzymes. The complement system, the clotting system, and tje kinin system do not play a role in granulocyte production, but they function as proenzymes in the inflammatory response. The complement system, the clotting system, and the kinin system are not activated by interferon, but are activated by enzymatic action. 17. Which statement indicates teaching was successful regarding the classic pathway of the complement system? The classic pathway of the complement system is activated by: a. Histamine b. Antigen-antibody complexes c. Leukotrienes d. Prostaglandins ANS: B The classic pathway of the complement system is activated by antibodies of the immune system. The classic pathway of the complement system is activated by antibodies, not by histamine. The classic pathway of the complement system is activated by antibodies, not by leukotrienes. The classic pathway of the complement system is activated by antibodies, not by prostaglandins. 18. A patient has researched bradykinin on the Internet. Which information indicates the patient understands the functions of bradykinin? Bradykinin is involved in: a. Increasing vascular permeability b. Vasoconstricting blood vessels c. Stimulating the clotting system d. Increasing degradation of prostaglandins ANS: A Bradykinin increases vascular permeability. Bradykinin increases vascular permeability; it does not promote vasoconstriction. Bradykinin increases vascular permeability; it does not stimulate clotting. Bradykinin promotes pain; thus, it does not degrade prostaglandins but supports them. 19. After teaching the staff about the clotting system, which statement indicates teaching was successful? The end product of the clotting system is: a. Plasmin b. Fibrin c. Collagen d. Factor X ANS: B The end product of the clotting system is fibrin. Plasmin activates the complement cascade. Collagen plays a factor in wound healing. Factor X is a first step in the clotting system. 20. A 5-year-old male is diagnosed with a bacterial infection. Cultures of the bacteria revealed lipopolysaccharides on the bacterial cell surface. Which of the complement pathways would be activated in this case? a. Classical pathway b. Lectin pathway c. Alternative pathway d. Kinin pathway ANS: C The alternative pathway is activated by several substances found on the surface of infectious organisms, such as those containing lipopolysaccharides. The classical pathway is primarily activated by antibodies that are proteins of the acquired immune system. The lectin pathway is similar to the classic pathway but is independent of antibody. It is activated by several plasma proteins. The kinin pathway is involved in coagulation. 21. An 8-year-old female presents with edema of the cutaneous and mucosal tissue layers. Her mother reports that the condition is recurrent and seems to occur more often during stressful situations. The child is diagnosed with hereditary angioedema. Which of the following is deficient in this child? a. C1 esterase inhibitor b. Carboxypeptidase c. Neutrophils d. Plasmin ANS: A A genetic defect in C1 esterase inhibitor (C1 INH deficiency) results in hereditary angioedema. Hereditary angioedema is due to C1 esterase inhibitor. Carboxypeptidase degrades kinins. Hereditary angioedema is due to C1 esterase inhibitor, not a disorder of neutrophils. Plasmin is not associated with hereditary angioedema, but is associated with clots. 22. A nurse is preparing to teach on the subject of opsonins. Which information should the nurse include? Opsonins are molecules that: a. Are composed of fatty acids b. Regulate inflammation c. Degranulate mast cells d. Enhance phagocytosis ANS: D Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized. Opsonins are not composed of fatty acids; they are antibodies. Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized. They do not regulate inflammation; mast cells do. Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized; they do not react with mast cells. 23. A 10-year-old male is diagnosed with a parasite. Which lab result should the nurse check for a response to the parasite? a. Monocytes b. Eosinophils c. Neutrophils d. Macrophages ANS: B Eosinophils serve as the bodys primary defense against parasites. Monocytes are not the bodys primary defense against parasite; eosinophils are. Monocytes are phagocytic. Neutrophils are phagocytic; they are not the bodys defense against parasites. Macrophages are not active against parasites; they act as long-term defense against infections. 24. A 65-year-old female is diagnosed with metastatic breast cancer. She has developed muscle wasting. Which of the following substances would be produced in large quantities to eliminate the tumor cells and cause muscle wasting? a. Interleukin-6 b. Eosinophils c. Tumor necrosis factor d. Platelets ANS: C Tumor necrosis factor causes muscle wasting. Interleukin-6 stimulates growth and differentiation of blood cells. Eosinophils are stimulated for parasites. Platelets stimulate clotting. 25. When phagocytes begin to stick avidly to capillary walls, which process is occurring? a. Margination b. Exudation c. Integration d. Emigration ANS: A Both leukocytes and endothelial cells secrete substances that increase adhesion, or stickiness, causing the leukocytes to adhere more avidly to the endothelial cells in the walls of the capillaries and venules in a process called margination. Exudation is the process of pus formation and does not result in stickiness. Integration occurs in cells but is not a major function and does not lead to stickiness. Emigration is similar to diapedesis and is not associated with increased stickiness. 26. An infant develops a fever secondary to a bacterial infection. Which of the following most likely triggered the fever? a. Interleukin-1 b. Interleukin-6 c. Interleukin-10 d. Interferons (INFs) ANS: A Interleukin-1 is responsible for fever production. Interleukin-6 stimulates growth and differentiation of blood cells. Interleukin-10 helps decrease the immune response. INFs are members of a family of cytokines that protect against viral infections. 27. A 54-year-old male intravenous (IV) drug user is diagnosed with chronic hepatitis C. Testing revealed that he is a candidate for treatment. Which of the following could be used to treat his condition? a. Interleukin-1 b. Interleukin-6 c. Interleukin-10 d. INFs ANS: D INFs are members of a family of cytokines that protect against viral infections. Interleukin-1 is responsible for fever production. Interleukin-6 stimulates growth and differentiation of blood cells. Interleukin-10 helps decrease the immune response. 28. A 35-year-old male is diagnosed with lobar pneumonia (lung infection). Which of the following exudates would be present in highest concentration at the site of this advanced inflammatory response? a. Serous b. Purulent c. Hemorrhagic d. Fibrinous ANS: D Fibrinous exudates occur in the lungs of individuals with pneumonia. Serous fluid is watery fluid, as in a blister. Purulent is characterized by an abscess, such as pus. Hemorrhagic occurs when the exudates are filled with erythrocytes. 29. During inflammation, the liver is stimulated to release plasma proteins, collectively known as: a. Opsonins b. Acute phase reactants c. Antibodies d. Phagolysosome ANS: B The synthesis of many plasma proteins by the liver is increased during inflammation. These proteins, which can be either proinflammatory or antiinflammatory in nature, are referred to as acute phase reactants. Opsonins coat the surface of bacteria and increase their susceptibility to being phagocytized. Antibodies are proteins of the immune system. Phagolysosome destroys bacterium. 30. A 3-year-old is making play cakes in a sandbox and is eating the play cakes. The sand was also being used by cats as a litter box and was contaminated with toxoplasmosis. Which of the following would most likely also be present? a. Granuloma formation b. Degranulation c. Blood clots d. Exudate production ANS: A Infections caused by bacteria such as toxoplasmosis can result in granuloma formation. Degranulation is a part of mast cell destruction. Blood clots are not expected with chronic inflammation. Exudate production is pus formation. 31. A 12-year-old male is fighting with another child when he receives a puncture wound from a pencil. The school nurse cleans and bandages the wound. After about 1 week, the wound would be in which phase of healing? a. Debridement b. Primary intention c. Resolution d. Maturation ANS: C Resolution occurs when repaired tissue is approaching close to normal. Debridement is the scraping away of dead tissue and is not a phase of wound healing. Primary intention is the stage of healing of wounds that are closely proximated. Maturation is the result of severe wounds which would begin several weeks after injury and may take 2 years. 32. The macrophage secretion that stimulates procollagen synthesis and secretion is: a. Angiogenesis factor b. Matrix metalloproteinase c. Vascular endothelial growth factor d. Transforming growth factor-beta ANS: D Macrophages secrete transforming growth factor-beta to stimulate fibroblasts to secrete the collagen precursor procollagen. Angiogenesis factor supports the growth of new vessels. Matrix metalloproteinase remodels proteins at the site of injury. Vascular endothelial growth factors are also involved in vessel growth. 33. A 30-year-old male was involved in a motor vehicle accident. The glass from the shattered window cut his face and neck. The scar, however, was raised and extended beyond the original boundaries of the wound. This pattern of scarring is caused by impaired: a. Nutritional status b. Collagen synthesis c. Epithelialization d. Contraction ANS: B Impaired production of collagen can cause surface overhealing, leading to a keloid or a hypertrophic scar. Nutritional deficiencies would lead to healing problems, but not extended scarring. Necrosis or steroid use leads to impaired epithelialization. Impaired contraction would lead to drawing of tissues, not raised. 34. The nurse is reviewing the lab data of a newly admitted patient. The nurse notes the patient had an erythrocyte sedimentation done, and the results are quite elevated. The nurse would focus the care plan on which of the following conditions? a. Anemia b. Infection c. Inflammation d. Electrolyte imbalance ANS: C Common laboratory tests for inflammation measure levels of acute phase reactants. An increase in fibrinogen is associated with an increased erythrocyte sedimentation rate, which is considered a good indicator of an acute inflammatory response. Anemia would not result in an increased erythrocyte sedimentation rate. An infection would result in an increase in white blood cell count, but not the erythrocyte sedimentation rate. An electrolyte imbalance would not cause a rise in the sedimentation rate. 35. Healing by secondary intention would occur in which of the following patients? A patient with a: a. Sutured surgical wound b. Stage IV pressure ulcer c. Paper cut d. Sunburn ANS: B A patient with a stage IV pressure ulcer would heal by secondary intention. A patient with a surgical wound would heal by primary intention. A patient with a paper cut would heal by primary intention. A patient with a sunburn would heal without needing either primary or secondary intention. 36. The post-surgical patient is experiencing delayed wound healing. The dietician believes the delay is related to nutritional intake. A deficiency in which of the following substances could directly affect healing? a. Vitamin D b. Ascorbic acid c. Melanin d. Cholesterol ANS: B Most of the factors that interfere with the production of collagen in healing tissues are nutritional. Scurvy, for example, is caused by lack of ascorbic acidone of the cofactors required for collagen formation by fibroblasts. The results of scurvy are poorly formed connective tissue and greatly impaired healing. Vitamin D deficiency will not directly affect healing; ascorbic acid does. Melanin deficiency will not directly affect healing; ascorbic acid does. Cholesterol deficiency will not directly affect healing; ascorbic acid does. MULTIPLE RESPONSE 1. A nurse remembers the primary actions of the complement cascade include (select all that apply): a. Increased vascular permeability b. Vasoconstriction c. Chemotaxis d. Opsonization e. Cell killing f. Increased clotting ANS: A, C, D, E The actions of the complement cascade include increased vascular permeability and vasodilation, chemotaxis, opsonization, and cell killing. It does not involve vasoconstriction or increased clotting. 2. The nurse is assessing a patient with a diagnosis of inflammation. The nurse would expect to find which of the following signs and symptoms consistent with acute inflammation? (Select all that apply.) a. Heat b. Erythema c. Pain d. Swelling e. Exudates f. Loss of function ANS: A, B, C, D, F The classic symptoms of acute inflammation include redness (erythema), heat, swelling, pain, and loss of function. Exudates would indicate infection, not inflammation. 3. The nurse identified each of the following clinical manifestations of inflammation. Which would the nurse classify as a local response? (Select all that apply.) a. Fever b. Redness c. Swelling d. Heat e. Pain ANS: B, C, D, E Local manifestations of inflammation are the result of the vascular changes associated with the inflammatory process, including vasodilation and increased capillary permeability. The symptoms include redness, heat, swelling, and pain. 4. Physical barriers that offer the body protection from damage and infection are located in the (select all that apply): a. Gastrointestinal tract b. Genitourinary tract c. Respiratory tract d. Lymph system e. Hematopoietic system ANS: A, B, C The physical barriers that cover the external parts of the human body offer considerable protection from damage and infection. These barriers are composed of tightly associated epithelial cells of the skin and of the linings of the gastrointestinal, genitourinary, and respiratory tracts. Chapter 4: Immunopathology MULTIPLE CHOICE 1. Neutrophils: a. are phagocytic cells. b. produce histamine. c. produce antibodies. d. are elevated during an allergic response. ANS: A 2. Which cells are required to process and present antigens from foreign material as the initial step in the immune response? a. Thelper cells b. Macrophages c. Eosinophils d. Monocytes ANS: B 3. Humoral immunity is mediated by: a. natural killer cells. b. T lymphocytes (T cells). c. B lymphocytes (B cells). d. neutrophils. ANS: C 4. A secondary immune response differs from the primary immune response in that: a. it is more rapid than the primary response and results in higher antibody levels. b. it is slower than the primary response and doesnt change the antibody levels. c. it occurs at the same time as the primary response but results in a decrease in antibodies. d. it only occurs in hyperallergic reactions and results in a decrease of antibodies. ANS: A 5. Which type of immunity is provided by a vaccination? a. Active natural b. Active artificial c. Passive natural d. Passive artificial ANS: B 6. When an allergen binds with IgE antibodies on mast cells, resulting in release of chemical mediators, this reaction is called: a. cytotoxic hypersensitivity. b. immune complex hypersensitivity. c. type I hypersensitivity. d. type IV hypersensitivity. ANS: C 7. The role of memory cells is to: a. change into an antibody-secreting cell following activation. b. immediately secrete antibodies following the first exposure to antigen. c. recognize the antigen and stimulate the immune response. d. bind complement to the antibody. ANS: C 8. Which statement applies to contact dermatitis? a. It occurs when IgE antibodies on the skin react with the causative substance. b. It may result from ingested foods. c. Urticaria (hives) gradually spread over the body. d. A type IV reaction occurs in affected areas. ANS: D 9. Which of the following causes anaphylaxis? a. A severe, systemic allergic reaction b. Type III hypersensitivity c. Cell-mediated hypersensitivity d. Immune complex deposits in many tissues ANS: A 10. Following a positive HIV antibodies blood test and ELISA test, what is the test commonly used for confirmation? a. Agglutination b. Double immunodiffusion test c. Western blot test d. Sedimentation rate test ANS: C 11. Incompatible blood transfusions result in: a. hemolysis of erythrocytes. b. a type I immune response. c. deposits in multiple organs. d. immune deficiency. ANS: A 12. An autoimmune disease is: a. excessive formation of antibodies following exposure to foreign material. b. an extreme response to normally harmless material in the environment. c. an abnormal response to ingested food and drugs. d. failure of the immune system to distinguish self from nonself. ANS: D 13. Systemic lupus erythematosus is caused by: a. a chronic allergic condition. b. development of an immune-deficient state. c. a deficiency of T lymphocytes. d. immune complex deposits of antinuclear antibodies. ANS: D 14. Distinguishing clinical features of systemic lupus erythematosus include: a. inflammation in multiple organs. b. lack of a specific diagnostic blood test. c. acute onset and nonprogressive course. d. typical skin rash on the chest and back. ANS: A 15. Which of the following are the target cells for HIV? a. Helper T lymphocytes (CD4 lymphocytes) b. B lymphocytes c. Natural killer cells d. Macrophages ANS: A 16. A diagnosis of HIV positive means that: a. the number of T lymphocytes in the circulating blood is decreased. b. significant opportunistic infection is present in the body. c. the individual has AIDS. d. the virus and its antibodies are present in the blood. ANS: D 17. HIV infection impairs: a. humoral immunity. b. cell-mediated immunity. c. both humoral and cell-mediated immunity. d. neither type of immunity. ANS: C 18. Immunodeficiencies may result in an increased risk of infections by normally harmless microorganisms. These infections are referred to as: a. opportunistic. b. prophylactic. c. abnormal. d. transient. ANS: A 19. Serious infections frequently occurring in patients with AIDS include: 1. tuberculosis. 2. Pneumocystis carinii pneumonia. 3. influenza. 4. tetanus. a. 1, 2 b. 1, 4 c. 2, 3 20. Which of the following statements does NOT apply to major histocompatibility complex (MHC) proteins or molecules? a. They are genes on chromosome 6. b. All members of a family have identical MHCs. c. They alert the immune system to virus-infected cells. d. A close match is essential for successful tissue transplants. ANS: B 21. CD4-positive helper T cells function by: a. direct cytotoxic action. b. facilitating all immune system activity. c. producing immunoglobulins. d. inactivating allergens. ANS: B 22. Host-versus-graft disease refers to: a. hyperacute rejection of tissue. b. T cells in grafted tissue attacking host cells. c. infection resulting from immunosuppression therapy. d. transplant rejection by the recipients immune system. ANS: D 23. Which of the following complications does NOT occur frequently in AIDS patients? a. Kaposis sarcoma b. Wasting syndrome c. Lymphoma d. Polyarthritis ANS: D 24. Which of the following characteristics apply to HIV? 1. It contains two strands of DNA. 2. It tends to mutate frequently to form new strains. 3. The incubation period is extremely short. 4. It is inactivated by heat and many disinfectants. a. 1, 2 b. 1, 3 c. 2, 4 d. 3, 4 ANS: C 25. In cases of HIV infection, the window period refers to the time between: a. entry of the virus into the blood and the initial manifestations. b. entry of the virus into the body and the appearance of antibodies in the blood. c. entry of the virus into the body and a significant drop in CD4 T-helper lymphocyte count. d. diagnosis of HIV positive and diagnosis of AIDS. ANS: B 26. Which of the following is an effect of cytokines? They: a. activate and stimulate proliferation of B and T lymphocytes. b. destroy antigens quickly. c. increase the rate of mitosis in tumors. d. cause immediate pain. ANS: A 27. What does seroconversion mean in relation to HIV and AIDS? a. The virus has been identified in the blood and body fluids. b. Antibodies for HIV have been identified in the blood. c. HIV was found in lymphocytes. d. Active infection has developed in the patient. ANS: B 28. Which of the following statements is TRUE regarding a patient who is HIV positive? a. No medication is required until the CD4 cell count drops below normal range. b. Antibodies are present, destroying the virus and preventing transmission to others. c. Antibodies in the blood indicate presence of virus and possible transmission to others. d. Enzymes have not yet converted RNA to DNA for replication. ANS: C 29. The term tolerance refers to: a. surveillance and destruction of new cancer cells by the immune system. b. the ability of the immune system to ignore self cells. c. the ability of T and B lymphocytes to work together. d. the role of lymphoid tissue in the body defenses. ANS: B 30. Which of the following statements applies to the complement system? a. It is activated by IgE. b. It blocks the inflammatory response. c. It consists of proteins in the blood that must be activated. d. It may destroy antibodies in the circulation. ANS: C 31. Which of the following statements regarding immunoglobulins is TRUE? ..................................CONTINUED...................................... [Show More]
Last updated: 11 months ago
Preview 1 out of 227 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 08, 2021
Number of pages
227
Written in
Additional information
This document has been written for:
Uploaded
Jun 08, 2021
Downloads
0
Views
45

.png)
.png)