*NURSING > QUESTIONS and ANSWERS > NURSING 1025 ATI Chapter 56 - Fluid and Electrolyte Imbalances (study guide) (All)
NURSING 1025 ATI Chapter 56 - Fluid and Electrolyte Imbalances (study guide)
Document Content and Description Below
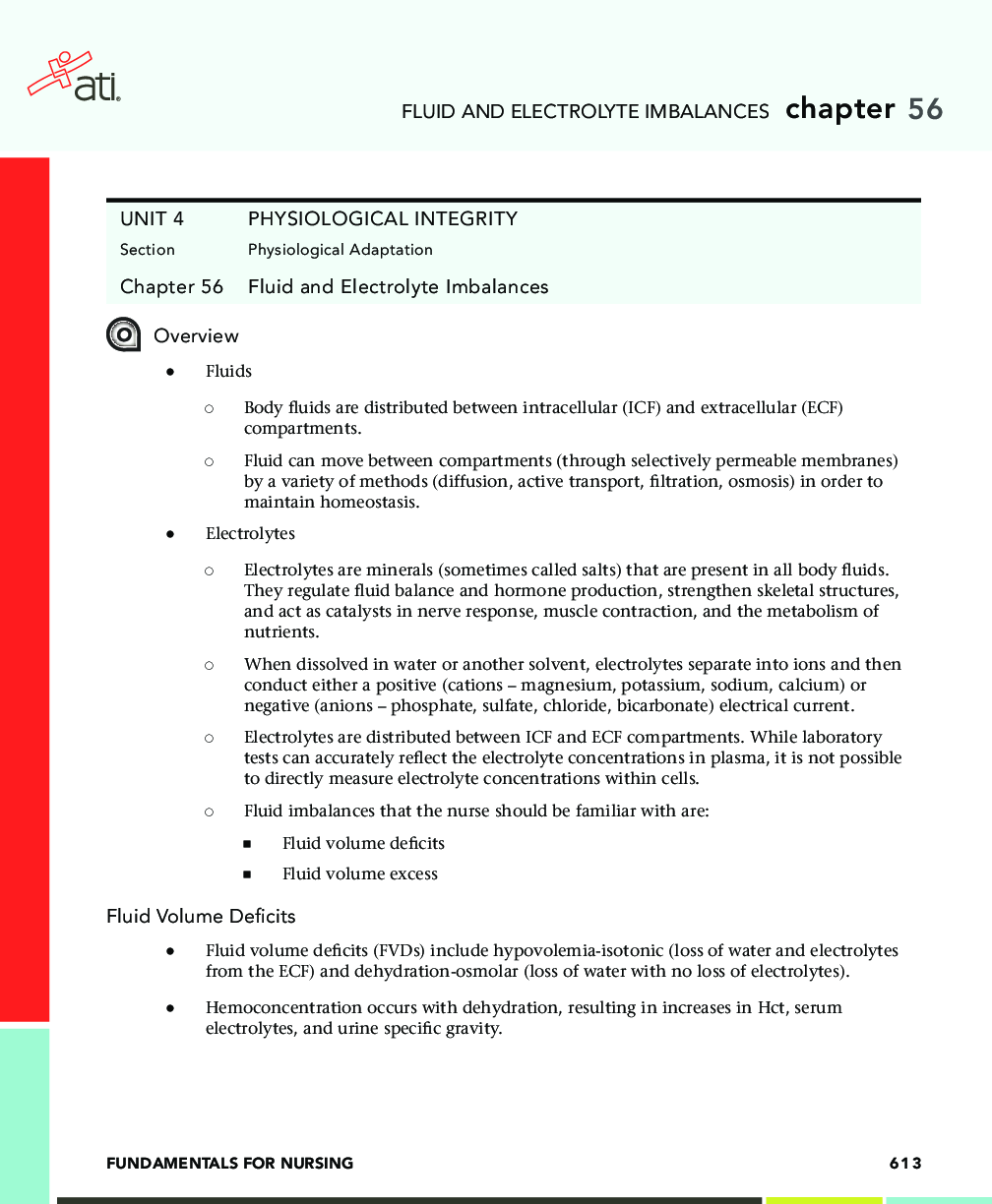
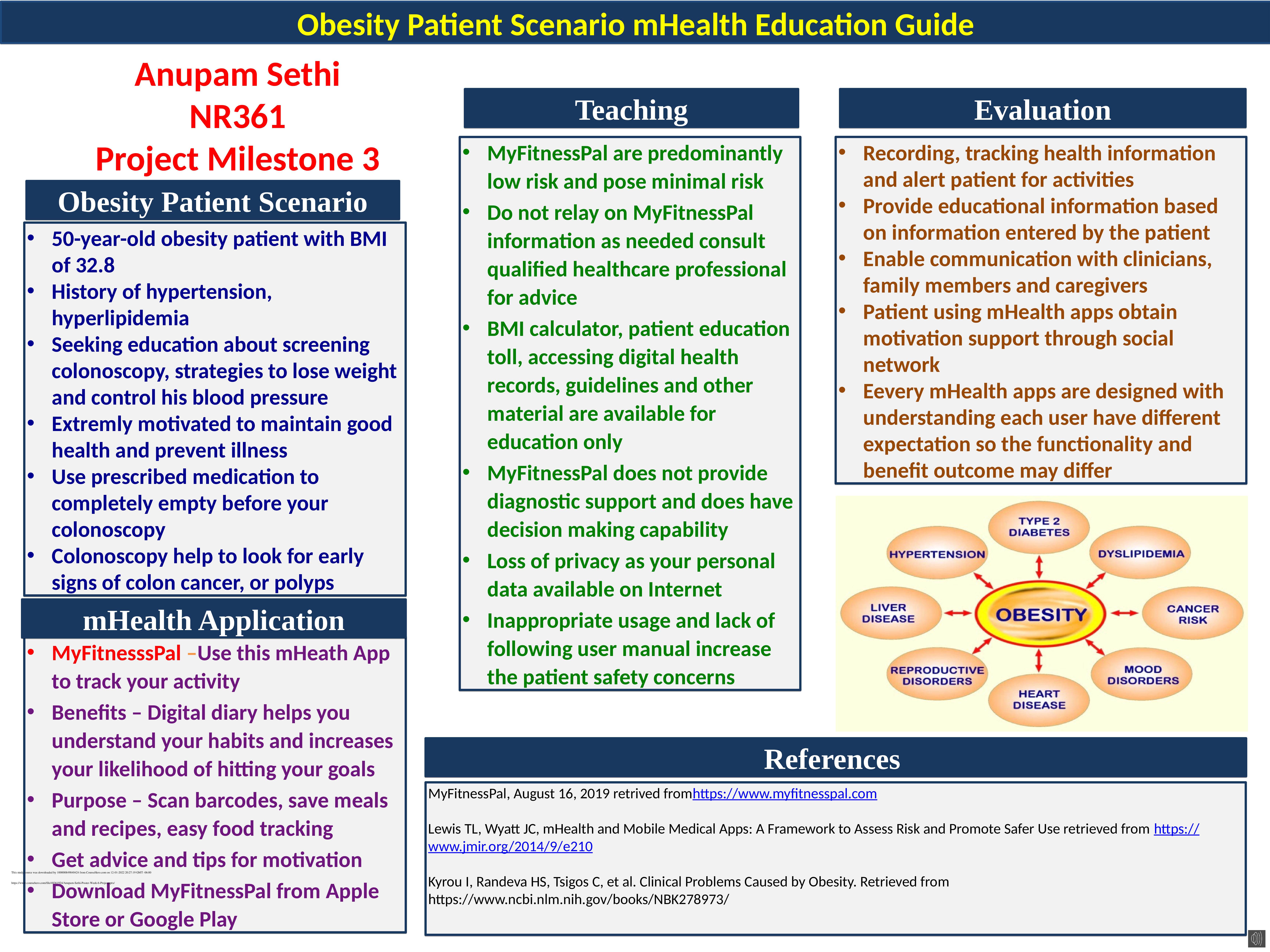
Overview ● Fluids ◯ Body fluids are distributed between intracellular (ICF) and extracellular (ECF) compartments. ◯ Fluid can move between compartments (through selectively permeable membrane... s) by a variety of methods (diffusion, active transport, filtration, osmosis) in order to maintain homeostasis. ● Electrolytes ◯ Electrolytes are minerals (sometimes called salts) that are present in all body fluids. They regulate fluid balance and hormone production, strengthen skeletal structures, and act as catalysts in nerve response, muscle contraction, and the metabolism of nutrients. ◯ When dissolved in water or another solvent, electrolytes separate into ions and then conduct either a positive (cations – magnesium, potassium, sodium, calcium) or negative (anions – phosphate, sulfate, chloride, bicarbonate) electrical current. ◯ Electrolytes are distributed between ICF and ECF compartments. While laboratory tests can accurately reflect the electrolyte concentrations in plasma, it is not possible to directly measure electrolyte concentrations within cells. ◯ Fluid imbalances that the nurse should be familiar with are: ■ Fluid volume deficits ■ Fluid volume excess Fluid Volume Deficits ● Fluid volume deficits (FVDs) include hypovolemia-isotonic (loss of water and electrolytes from the ECF) and dehydration-osmolar (loss of water with no loss of electrolytes). ● Hemoconcentration occurs with dehydration, resulting in increases in Hct, serum electrolytes, and urine specific gravity. FLUID AND ELECTROLYTE IMBALANCES ● Note – Compensatory mechanisms include sympathetic nervous system responses of increased thirst, antidiuretic hormone (ADH) release, and aldosterone release. ● Hypovolemia can lead to hypovolemic shock. ● Older adults have an increased risk for dehydration due to a decrease in total body mass, which includes total body water content. Assessment ● Risk Factors ◯ Causes of Hypovolemia ■ Abnormal gastrointestinal (GI) losses – Vomiting, nasogastric suctioning, diarrhea ■ Abnormal skin losses – Diaphoresis ■ Abnormal renal losses – Diuretic therapy, diabetes insipidus, renal disease, adrenal insufficiency, osmotic diuresis ■ Third spacing – Peritonitis, intestinal obstruction, ascites, burns ■ Hemorrhage ■ Altered intake, such as nothing by mouth (NPO) ◯ Causes of Dehydration ■ Hyperventilation ■ Diabetic ketoacidosis ■ Enteral feeding without sufficient water intake ● Subjective and Objective Data ◯ Vital signs – Hyperthermia, tachycardia, thready pulse, hypotension, orthostatic hypotension, decreased central venous pressure, tachypnea (increased respirations), hypoxia ◯ Neuromusculoskeletal – Dizziness, syncope, confusion, weakness, fatigue ◯ GI – Thirst, dry furrowed tongue, nausea/vomiting, anorexia, acute weight loss ◯ Renal – Oliguria (decreased production of urine) ◯ Other signs – Diminished capillary refill, cool clammy skin, diaphoresis, sunken eyeballs, flattened neck veins ● Laboratory Findings ◯ Hct ■ Hypovolemia – Increased Hct ■ Dehydration – Increased hemoconcentration but not present when dehydration is caused by hemorrhage FLUID AND ELECTROLYTE IMBALANCES ◯ Serum osmolarity ■ Dehydration – Increased hemoconcentration osmolarity (greater than 300 mOsm/L) – Increased protein, BUN, electrolytes, glucose ◯ Urine specific gravity and osmolarity ■ Dehydration – Increased concentration ◯ Serum sodium ■ Dehydration – Increased hemoconcentration Collaborative Care ● Nursing Care ◯ Assess respiratory rate, symmetry, and effort. ◯ Monitor for shortness of breath and dyspnea. ◯ Check urinalysis, oxygen saturation (SaO2), CBC, and electrolytes. ◯ Administer supplemental oxygen as prescribed. ◯ Measure the client’s weight daily at same time of day using the same scale. ◯ Observe for nausea and vomiting. ◯ Assess and monitor the client’s vital signs. (check for hypotension and orthostatic hypotension). ◯ Check neurological status to determine level of consciousness. ◯ Assess heart rhythm (may be irregular or tachycardic). ◯ Initiate and maintain IV access. ◯ Place the client in shock position (on the back with the legs elevated). ◯ Fluid replacement: Administer IV fluids as prescribed (isotonic solutions such as lactated Ringer’s, 0.9% sodium chloride; blood transfusions). ◯ Monitor I&O. Alert the provider to a urine output less than 30 mL/hr. ◯ Monitor level of consciousness and ensure client safety. ◯ Assess level of gait stability. ◯ Encourage the client to use the call-light and ask for assistance. ◯ Encourage the client to change positions slowly (rolling from side to side or standing up). ◯ Check capillary refill (expected reference range less than 2 seconds). FLUID AND ELECTROLYTE IMBALANCES Fluid Volume Excesses ● Fluid volume excesses (FVEs) include hypervolemia-isotonic (water and sodium retained in abnormally high proportions) and overhydration-osmolar (more water gained than electrolytes). ● Severe hypervolemia can lead to pulmonary edema and heart failure. ● Hemodilution occurs with overhydration, resulting in decreases in Hct, serum electrolytes, and protein. ● Note – Compensatory mechanisms include an increased release of natriuretic peptides, resulting in increased loss of sodium and water by the kidneys, and a decreased release of aldosterone. Assessment ● Risk Factors ◯ Causes of Hypervolemia ■ Chronic stimulus to the kidney to conserve sodium and water (heart failure, cirrhosis, increased glucocorticosteroids) ■ Abnormal renal function with reduced excretion of sodium and water (renal failure) ■ Interstitial to plasma fluid shifts (hypertonic fluids, burns) ■ Age-related changes in cardiovascular and renal function ■ Excessive sodium intake ◯ Causes of Overhydration ■ Water replacement without electrolyte replacement (strenuous exercise with profuse diaphoresis) ● Subjective and Objective Data ◯ Vital signs – Tachycardia, bounding pulse, hypertension, tachypnea, increased central venous pressure ◯ Neuromusculoskeletal – Confusion, muscle weakness ◯ GI – Weight gain, ascites ◯ Respiratory – Dyspnea, orthopnea, crackles ◯ Other signs – Edema, distended neck veins FLUID AND ELECTROLYTE IMBALANCES ● Laboratory Findings ◯ Hct ■ Hypervolemia – Decreased Hct ■ Overhydration – Decreased Hct = hemodilution ◯ Serum osmolarity ■ Overhydration – Decreased hemodilution (osmolarity less than 270 mOsm/L) ◯ Serum sodium ■ Hypervolemia – Sodium within expected reference range ◯ Electrolytes, BUN, and creatinine ■ Overhydration/hypervolemia – Decreased electrolytes, BUN, and creatinine ◯ Arterial blood gases ■ Respiratory alkalosis – Decreased PaCO2 (less than 35 mm Hg), increased pH (greater than 7.45) ● Diagnostic Procedures ◯ Chest x-rays may indicate pulmonary congestion. Collaborative Care ● Nursing Care ◯ Assess respiratory rate, symmetry, and effort. ◯ Assess breath sounds in all lung fields. Lung sounds may be diminished with crackles. ◯ Monitor for shortness of breath and dyspnea. ◯ Check ABGs, SaO2, CBC, and chest x-ray results. ◯ Position the client in semi-Fowler’s position. ◯ Measure the client’s weight daily. ◯ Monitor I&O. ◯ Administer supplemental oxygen as needed. ◯ Reduce IV flow rates. ◯ Administer diuretics (osmotic, loop) as prescribed. ■ Limit fluid and sodium intake as prescribed. ■ Monitor and document edema (pretibial, sacral, periorbital). FLUID AND ELECTROLYTE IMBALANCES Electrolytes ■ Monitor and document circulation to the extremities. ■ Reposition the client at least every 2 hr. ■ Support arms and legs to decrease dependent edema as appropriate. ● Major electrolytes in the body include sodium, potassium, chloride, magnesium, phosphorus, and calcium. Nurses monitor the client’s laboratory values to identify any electrolyte imbalances. ● It is important to recognize the signs and symptoms of electrolyte imbalance. Clients at greatest risk for electrolyte imbalance are infants and children, older adults, clients with cognitive disorders, and clients who are chronically ill. Sodium Imbalances ● Sodium (Na+) is the major electrolyte found in ECF. ● Sodium is essential for maintenance of acid-base balance, active and passive transport mechanisms, and irritability and conduction of nerve and muscle tissue. ● Expected serum sodium levels are between 136 and 145 mEq/L. Hyponatremia ● Hyponatremia is a serum sodium level less than 136 mEq/L. ● Hyponatremia is a net gain of water or loss of sodium-rich fluids. ● Hyponatremia delays and slows the depolarization of membranes. ● Water moves from the ECF into the ICF, which causes cells to swell (cerebral edema). ● Serious complications can result from untreated acute hyponatremia (coma, seizures, respiratory arrest). Assessment ● Risk Factors ◯ Causes of Hyponatremia (loss of sodium) ■ Deficient ECF volume ■ Abnormal GI losses – Vomiting, nasogastric suctioning, diarrhea, tap water enemas ■ Renal losses – Diuretics, kidney disease, adrenal insufficiency, excessive sweating ■ Skin losses – Burns, wound drainage, gastrointestinal obstruction, peripheral edema, ascites. FLUID AND ELECTROLYTE IMBALANCES ■ Increased or normal ECF volume – Excessive oral water intake, syndrome of inappropriate antidiuretic hormone (SIADH), which is the excess secretion of antidiuretic hormone (ADH) ■ Edematous states – Heart failure, cirrhosis, nephrotic syndrome ■ Excessive hypotonic IV fluids ■ Inadequate sodium intake (NPO status) ■ Age-related risk factors – Older adult clients are at greater risk due to an increased incidence of chronic illnesses, use of diuretic medications, and risk for insufficient sodium intake. ● Subjective and Objective Data ◯ Physical assessment findings – Vary with a normal, decreased, or increased ECF volume ◯ Vital signs – Hypothermia, tachycardia, rapid thready pulse, hypotension, orthostatic hypotension ◯ Neuromusculoskeletal – Headache, confusion, lethargy, muscle weakness with possible respiratory compromise, fatigue, decreased deep tendon reflexes (DTR) ◯ GI – Increased motility, hyperactive bowel sounds, abdominal cramping, nausea ● Laboratory Findings ◯ Serum sodium ■ Decreased – Less than 136 mEq/L ◯ Serum osmolarity ■ Decreased – Less than 280 mOsm/L Collaborative Care ● Nursing Care ◯ Report abnormal laboratory findings to the provider. ◯ Fluid overload – Restrict water intake as prescribed. ◯ Acute hyponatremia: ■ Administer hypertonic oral and IV fluids as prescribed. ■ Encourage foods and fluids high in sodium (cheese, milk, condiments). ◯ Restoration of normal ECF volume – Administer isotonic IV therapy (0.9% sodium chloride, lactated Ringer’s). ◯ Monitor I&O and weigh the client daily. ◯ Monitor vital signs and level of consciousness, reporting abnormal findings. ◯ Encourage the client to change positions slowly. ◯ Follow any prescribed fluid restrictions. FLUID AND ELECTROLYTE IMBALANCES Hypernatremia ● Hypernatremia is a serum sodium level that is greater than 145 mEq/L. ● Hypernatremia is a serious electrolyte imbalance. It can cause significant neurological, endocrine, and cardiac disturbances. ● Increased sodium causes hypertonicity of the serum. This causes a shift of water out of the cells, making the cells dehydrated. Assessment ● Risk Factors ◯ Causes of Hypernatremia (loss of sodium) ■ Water deprivation (NPO) ◯ Excessive sodium intake – Dietary sodium intake, hypertonic IV fluids, bicarbonate intake ◯ Excessive sodium retention – Renal failure, Cushing’s syndrome, aldosteronism, some medications (glucocorticosteroids) ◯ Fluid losses – Fever, diaphoresis, burns, respiratory infection, diabetes insipidus, hyperglycemia, watery diarrhea ◯ Age-related changes, specifically decreased total body water content and inadequate fluid intake related to an altered thirst mechanism ◯ Compensatory mechanisms – Increased thirst and increased production of ADH. ● Subjective and Objective Data ◯ Vital signs – Hyperthermia, tachycardia, orthostatic hypotension ◯ Neuromusculoskeletal – Restlessness, irritability, muscle twitching, muscle weakness, seizures, coma, reduced to absent DTRs ◯ GI – Thirst, dry mucous membranes, increased motility, hyperactive bowel sounds, abdominal cramping, nausea ◯ Other signs – Edema, warm flushed skin, oliguria ● Laboratory Findings ◯ Serum sodium ■ Increased – Greater than 145 mEq/L ◯ Serum osmolarity ■ Increased – Greater than 300 mOsm/L FLUID AND ELECTROLYTE IMBALANCES Collaborative Care ● Nursing Care ◯ Report abnormal laboratory findings to the provider. ◯ Fluid loss – Based on serum osmolarity ■ Administer hypotonic IV fluids (0.45% sodium chloride). ■ Administer isotonic IV fluids (0.9% sodium chloride). ◯ Excess sodium ■ Encourage water intake and discourage sodium intake. ■ Administer diuretics (loop diuretics). ◯ Monitor level of consciousness and ensure safety. ◯ Provide oral hygiene and other comfort measures to decrease thirst. ◯ Monitor I&O, and alert the provider if renal output is inadequate. Potassium Imbalances ● Potassium (K+) is the major cation in ICF. ● Potassium plays a vital role in cell metabolism; transmission of nerve impulses; functioning of cardiac, lung, and muscle tissues; and acid-base balance. ● Potassium has reciprocal action with sodium. ● Expected serum potassium levels are 3.5 to 5 mEq/L. Hypokalemia ● Hypokalemia is a serum potassium level below 3.5 mEq/L. ● Hypokalemia is the result of an increased loss of potassium from the body or movement of potassium into the cells. Assessment ● Risk Factors ◯ Causes of hypokalemia (loss of potassium) ◯ Abnormal GI losses – Vomiting, nasogastric suctioning, diarrhea, inappropriate laxative use ◯ Renal losses – Excessive use of diuretics such as furosemide (Lasix), corticosteroids ◯ Skin losses – Diaphoresis, wound losses ◯ Insufficient potassium ◯ Inadequate dietary intake (rare) FLUID AND ELECTROLYTE IMBALANCES ◯ Prolonged administration of non-electrolyte-containing IV solutions such as 5% dextrose in water ◯ ICF – Metabolic alkalosis, after correction of acidosis, during periods of tissue repair (burns, trauma, starvation), total parenteral nutrition ◯ Age-related risk factors – Older adult clients are at greater risk due to increased use of diuretics and laxatives. ● Subjective and Objective Data ◯ Vital signs – Hyperthermia, weak irregular pulse, hypotension, respiratory distress ◯ Neuromusculoskeletal – Weakness with respiratory collapse and paralysis, muscle cramping, decreased muscle tone and hypoactive reflexes, paresthesias, mental confusion ◯ ECG – Premature ventricular contractions (PVCs), bradycardia, blocks, ventricular tachycardia, inverted T waves, and ST depression ◯ GI – Decreased motility, abdominal distention, constipation, ileus, nausea, vomiting, anorexia ◯ Other signs – Polyuria (excretion of dilute urine) ● Laboratory Findings ◯ Serum potassium ■ Decreased – Less than 3.5 mEq/L ◯ Arterial blood gases ■ Metabolic alkalosis – pH greater than 7.45 ● Diagnostic Procedures ◯ Electrocardiogram (ECG) ■ Will show findings of dysrhythmias, such as PVCs, ventricular tachycardia, inverted T waves, and ST depression Collaborative Care ● Nursing Care ◯ Report abnormal findings to the provider. ◯ Treat the underlying cause. ◯ Replace potassium. ■ Encourage foods high in potassium (avocados, broccoli, dairy products, dried fruit, cantaloupe, bananas). ■ Provide oral potassium supplementation. FLUID AND ELECTROLYTE IMBALANCES ◯ IV potassium supplementation ■ Never IV bolus (high risk of cardiac arrest) ■ The maximum recommended rate is 5 to 10 mEq/hr. ◯ Monitor for phlebitis (tissue irritant). ◯ Monitor for and maintain an adequate urine output. ◯ Monitor for shallow, ineffective respirations and diminished breath sounds. ◯ Monitor the client’s cardiac rhythm and intervene promptly as needed. ◯ Monitor clients receiving digoxin. Hypokalemia increases the risk for digoxin toxicity. ◯ Monitor level of consciousness and ensure safety. ◯ Monitor bowel sounds and abdominal distention and intervene as needed. Hyperkalemia ● Hyperkalemia is a serum potassium level greater than 5.0 mEq/L. ● Hyperkalemia is the result of an increased intake of potassium, movement of potassium out of the cells, or inadequate renal excretion. Assessment ● Risk Factors ◯ Increased total body potassium – IV potassium administration, salt substitutes ◯ ECF shift – Decreased insulin, acidosis (diabetic ketoacidosis), tissue catabolism (sepsis, trauma, surgery, fever, myocardial infarction) ◯ Hypertonic states – Uncontrolled diabetes mellitus ◯ Decreased excretion of potassium – Renal failure, severe dehydration, potassium- sparing diuretics, ACE inhibitors, NSAIDs, adrenal insufficiency ◯ Older adult clients – At greater risk due to increased use of salt substitutes, angiotensin-converting enzyme inhibitors, and potassium-sparing diuretics ● Subjective and Objective Data ◯ Vital signs – Slow, irregular pulse; hypotension ◯ Neuromusculoskeletal – Restlessness, irritability, weakness with ascending flaccid paralysis, paresthesias ◯ ECG – Ventricular fibrillation, peaked T waves, widened QRS ◯ GI – Nausea, vomiting, increased motility, diarrhea, hyperactive bowel sounds ◯ Other signs – Oliguria FLUID AND ELECTROLYTE IMBALANCES ● Laboratory Findings ◯ Serum potassium ■ Increased – Greater than 5 mEq/L ◯ Arterial blood gases ■ Metabolic alkalosis – pH less than 7.45 ● Diagnostic Procedures ◯ ECG ■ Will show dysrhythmias (ventricular fibrillation, peaked T waves, widened QRS) Collaborative Care ● Nursing Care ◯ Report abnormal findings to the provider. ◯ Decrease potassium intake: ■ Stop infusion of IV potassium. ■ Withhold oral potassium. ■ Provide a potassium-restricted diet (avoiding avocados, broccoli, dairy products, dried fruit, cantaloupe, bananas). ■ If potassium levels are extremely high, dialysis may be required. ◯ Promote the movement of potassium from ECF to ICF: ■ Administer IV fluids with dextrose and regular insulin. ■ Administer sodium bicarbonate to reverse acidosis. ◯ Monitor the client’s cardiac rhythm and intervene promptly as needed. ◯ Medications to increase potassium excretion: ■ Administer loop diuretics, such as furosemide (Lasix), if renal function is adequate. Loop diuretics increase the depletion of potassium from the renal system. ◯ Maintain IV access. ◯ Prepare the client for dialysis if prescribed. Calcium Imbalances ● Calcium is found in the bones and the teeth. It is plentiful in the body. The expected calcium level is 9 to 10.5 mg/dL or 4.5 mg/dL for ionized calcium. ● Calcium balance is essential for proper functioning of the cardiovascular, neuromuscular, and endocrine systems, as well as blood clotting and bone and teeth formation. FLUID AND ELECTROLYTE IMBALANCES Hypocalcemia ● Hypocalcemia is a serum calcium level less than 9 mg/dL. ● Risk Factors ◯ Malabsorption syndromes, such as Crohn’s disease ◯ End-stage renal disease ◯ Post thyroidectomy ◯ Hypoparathyroidism ◯ Repeated transfusion ● Subjective and Objective Data ◯ Muscle twitches/tetany ■ Frequent, painful muscle spasms at rest ■ Hyperactive DTRs ■ Positive Chvostek’s sign (tapping on the facial nerve triggering facial twitching) ■ Positive Trousseau’s sign (hand/finger spasms with sustained blood pressure cuff inflation) ◯ Cardiovascular ■ Decreased myocardial contractility (decreased heart rate and hypotension) ◯ GI – Hyperactive bowel sounds, diarrhea, abdominal cramping ◯ Central nervous system – Seizures due to overstimulation of the CNS ● Laboratory Findings ◯ Calcium level less than 9 mg/dL ● Diagnostic Procedures ◯ ECG ■ Prolonged QT interval Collaborative Care ● Nursing Care ◯ Administer oral or IV calcium supplements. ◯ Initiate seizure precautions. ◯ Keep emergency equipment on standby. ◯ Encourage foods high in calcium, including dairy products and dark green vegetables. FLUID AND ELECTROLYTE IMBALANCES Magnesium Imbalances ● Most of the body’s magnesium is found in the bones. Magnesium in smaller amounts is found within the body cells. A very small amount is found in ECF. The expected magnesium level is 1.3 to 2.1 mEq/L Hypomagnesemia ● Hypomagnesemia is a serum magnesium level less than 1.3 mg/dL. Assessment ● Risk Factors ◯ Causes of hypomagnesemia ◯ Malnutrition (insufficient magnesium intake) ◯ Alcohol ingestion (magnesium excretion) ● Subjective and Objective Data ◯ Neuromuscular – Increased nerve impulse transmission (hyperactive DTRs, paresthesias, muscle tetany), positive Chvostek’s and Trousseau’s signs ◯ GI – Hypoactive bowel sounds, constipation, abdominal distention, paralytic ileus. ● Nursing Care ◯ Discontinue magnesium-losing medications (loop diuretics). ◯ Administer oral or IV magnesium sulfate following safety protocols. IV route is used because IM can cause pain and tissue damage. Oral magnesium can cause diarrhea and increase magnesium depletion. Monitor closely. ◯ Encourage foods high in magnesium, including dairy products and dark green vegetables. FLUID AND ELECTROLYTE IMBALANCES CHAPTER 56: FLUID AND ELECTROLYTE IMBALANCES Application Exercises 1. A nurse is collecting data from an older adult client who states he has had vomiting and diarrhea for the last 48 hr. Which of the following findings should indicate to the nurse that the client is hypovolemic? (Select all that apply.) Bradycardia Hypertension Tachypnea Furrowed tongue Sunken eyeballs 2. A nurse is providing teaching about a healthy lifestyle for a group of young adults who are training for a marathon. Which of the following should the nurse include in the teaching session? A. Decrease fluid intake after training. B. Decrease fluid intake in high altitudes. C. Increase fluid intake in dry climates. D. Increase intake of fluids containing caffeine. 3. A nurse is caring for a client who was admitted to the hospital for peritonitis and has signs of dehydration. Which of the following laboratory findings would be expected for this client? (Select all that apply.) Increased Hct Decreased serum osmolarity Increased serum sodium Decreased urine specific gravity Increased urine osmolarity 4. A nurse on a medical-surgical unit has been assigned to care for four clients. Which of the following clients is at risk for fluid volume excess (hypervolemia)? A. A client who is receiving a high-ceiling loop diuretic. B. A client who has heart failure. C. A client who lost 500 mL of blood during surgery. D. A client who is 4 hr postoperative and is receiving nasogastric suction. 5. A nurse is reviewing the laboratory findings for a group of clients. Which of the following findings should be reported to the provider? A. Serum sodium 143 mEq/L B. Serum potassium 4 mEq/L C. Serum calcium 8.5 mg/dL D. Serum chloride 99 mEq/L 6. A nurse on a medical-surgical unit is caring for a client who is hypernatremic. Which of the following should be included in the plan of care? A. Infuse hypotonic IV fluids. B. Restrict oral intake of water. C. Increase sodium intake. D. Administer a loop diuretic. FLUID AND ELECTROLYTE IMBALANCES CHAPTER 56: FLUID AND ELECTROLYTE IMBALANCES Application Exercises Answer Key 1. A nurse is collecting data from an older adult client who states he has had vomiting and diarrhea for the last 48 hr. Which of the following findings should indicate to the nurse that the client is hypovolemic? (Select all that apply.) Bradycardia Hypertension X Tachypnea X Furrowed tongue X Sunken eyeballs A client who has altered intake is at risk for hypovolemia. Older adults are at greater risk than younger adults. In the presence of hypovolemia, tachycardia, hypotension, tachypnea, a furrowed dry tongue, and sunken eyeballs may be seen. NCLEX® Connection: Physiological Adaptation, Fluid and Electrolyte Imbalances 2. A nurse is providing teaching about a healthy lifestyle for a group of young adults who are training for a marathon. Which of the following should the nurse include in the teaching session? A. Decrease fluid intake after training. B. Decrease fluid intake in high altitudes. C. Increase fluid intake in dry climates. D. Increase intake of fluids containing caffeine. Fluid intake should be increased with excessive, vigorous exercise in high altitudes. Fluid intake should also be increased in dry climates. Caffeine should be avoided because excessive intake may lead to dehydration. NCLEX® Connection: Physiological Adaptation, Fluid and Electrolyte Imbalances 3. A nurse is caring for a client who was admitted to the hospital for peritonitis and has signs of dehydration. Which of the following laboratory findings would be expected for this client? (Select all that apply.) X Increased Hct Decreased serum osmolarity X Increased serum sodium Decreased urine specific gravity X Increased urine osmolarity In the presence of dehydration (not related to hemorrhage), urine osmolarity and urine specific gravity are increased. Due to hemoconcentration, serum osmolarity and serum sodium are increased. NCLEX® Connection: Physiological Adaptation, Fluid and Electrolyte Imbalances 4. A nurse on a medical-surgical unit has been assigned to care for four clients. Which of the following clients is at risk for fluid volume excess (hypervolemia)? A. A client who is receiving a high-ceiling loop diuretic. B. A client who has heart failure. C. A client who lost 500 mL of blood during surgery. D. A client who is 4 hr postoperative and is receiving nasogastric suction. A client who has heart failure is at risk for fluid retention and fluid volume excess. The other clients are at risk for hypovolemia. NCLEX® Connection: Physiological Adaptation, Fluid and Electrolyte Imbalances 5. A nurse is reviewing the laboratory findings for a group of clients. Which of the following findings should be reported to the provider? A. Serum sodium 143 mEq/L B. Serum potassium 4 mEq/L C. Serum calcium 8.5 mg/dL D. Serum chloride 99 mEq/L A serum calcium level of 8.5 mg/dL is below the expected reference range and should be reported to the provider. The other findings are within the expected reference range. NCLEX® Connection: Physiological Adaptation, Fluid and Electrolyte Imbalances 6. A nurse on a medical-surgical unit is caring for a client who is hypernatremic. Which of the following should be included in the plan of care? A. Infuse hypotonic IV fluids. B. Restrict oral intake of water. C. Increase sodium intake. D. Administer a loop diuretic. The plan of care for a client who is hypernatremic should include hypotonic or isotonic fluids. Water intake is encouraged. Sodium intake is restricted. A loop diuretic will increase the excretion of sodium. NCLEX® Connection: Physiological Adaptation, Fluid and Electrolyte Imbalances [Show More]
Last updated: 1 year ago
Preview 1 out of 18 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$12.50
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2021
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2021
Downloads
0
Views
42






.png)
 Correct Study Guide, Download to Score A.png)

