*NURSING > STUDY GUIDE > Module 2 Chapters 11 to 27 complete questions with correct answers (All)
Module 2 Chapters 11 to 27 complete questions with correct answers
Document Content and Description Below
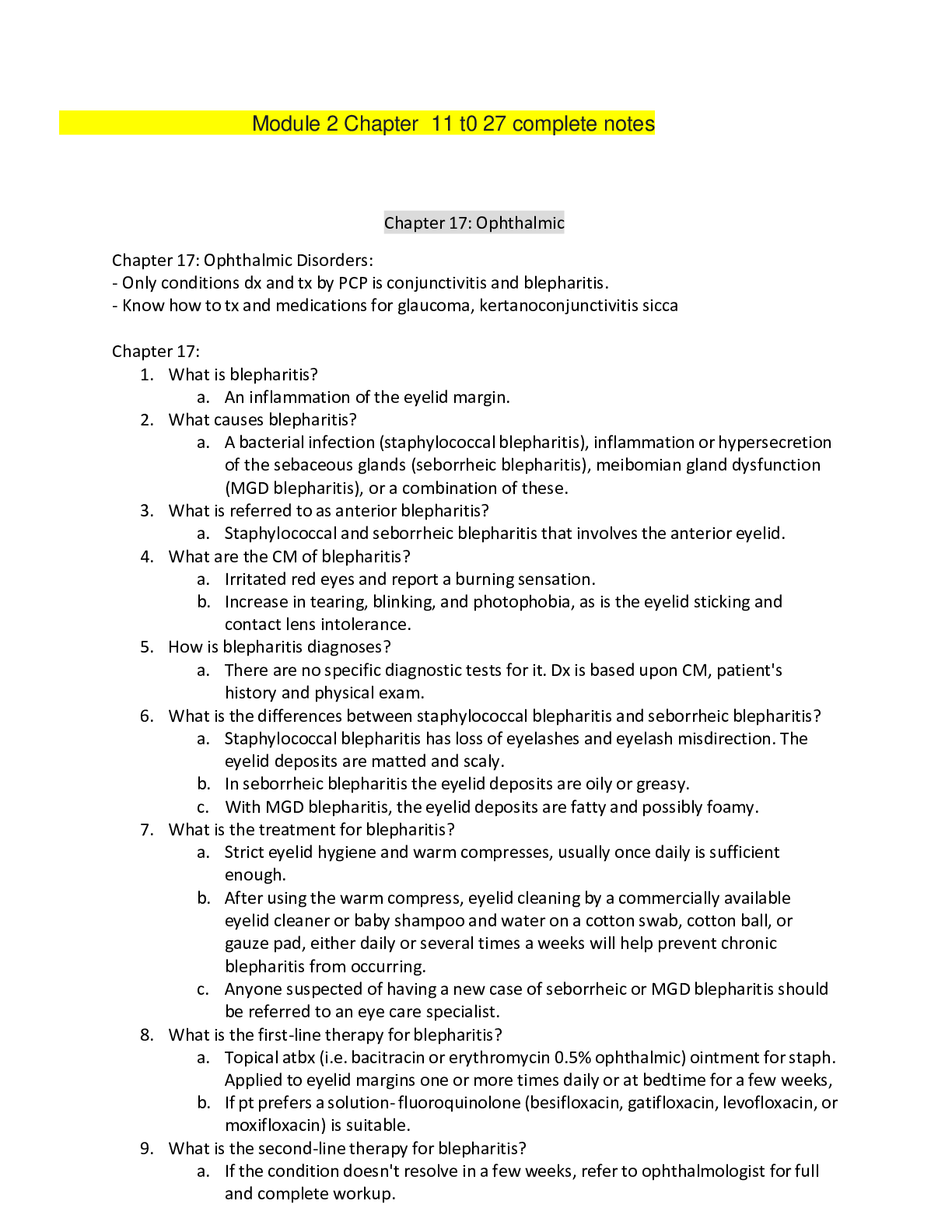
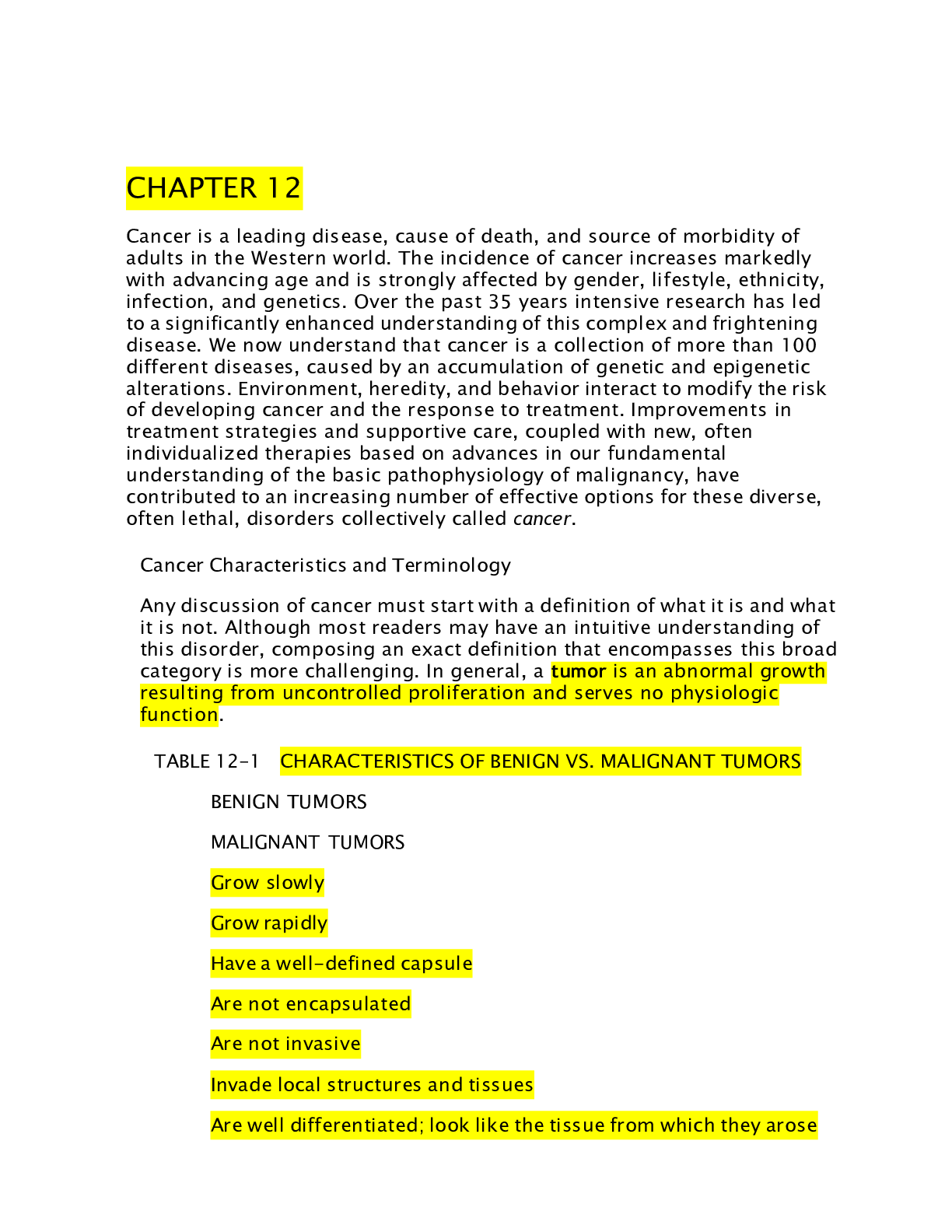
Chapter 11: Contact Dermatitis 1. What is dermatitis? 2. What are the causes of contact dermatitis? 3. What is the pharmacogenomics for dermatitis? 4. What is the diagnostic criteria for dermatiti... s? 5. When do you initiate drug therapy for dermatitis? 6. What are the goals of therapy? 7. What are the treatments for dermatitis? a. Table 11.1 on page 157 b. Topical corticosteroids- safer than systemic steroidal therapies. i. Dosage- intermediate or high-potency topical corticosteroid. ii. A lower-potency may be used after symptoms subside. iii. As a rule- short term therapy w/ more potent topical corticosteroids is preferred to long-term therapy w/ less potent corticosteroids. iv. Low-potency corticosteroids should be used in the facila and intertriginous regions b/c fluorinated and high-potency corticosteroids applied to the face may cause atrophy of the tissue or trigger steroidal rosacea. v. Preparations- available in creams, ointments, lotions, gels, solutions or sprays. Creams are most desirable. vi. Correct usage- chronic use isn’t recommended. vii. Application- penetration of a topical corticosteroid is enhanced when the skin is hydrated. Moisten skin prior to applying cream. viii. ADE- prolonged use causes fluorinated corticosteroids on the face can cause atrophy and acne-like symptoms. 1. With prolonged use ecchymosis may develop on the arms of elderly patients. Epidermal atrophy manifested by striae, shiny, thin skin, or telangiectases, can occur with prolonged use, or a hypersensitivity reaction may occur. c. Systemic corticosteroids i. Prescribed in tapering dose. Starting day 1 1mg/kg is decreased by 5mg every 2 days for 2-3 weeks. Taken at the same time in the morning. ii. Contraindications- suppress immune response and contraindicated in patients w/ systemic mycoses and in pts receiving vaccines. Used caution in pts w/ tuberculosis, hypothyroidism, cirrhosis, renal insufficiency, HTN, osteoporosis, and DM. iii. ADE- GI upset. Mood changes, hyperactivity, anxiety, depression, sleep disturbances. d. Topical immunosuppressives i. Act on T cells by suppressing cytokine transcription. ii. Tacrolimus and pimecrolimus are the preparations currently available. Applied BID until the lesions clear and then for an additional 7 days. Skin is dry before application. iii. Contraindications- shouldn’t be used under occlusive dressings. Care should be used when administering these drugs w/ drugs in the CYP3A family. iv. ADE- transient burning and pruritus which disappear with continued use. Concomitant ingestion of alcohol can cause redness and flushing. Sun protection is recommended. e. Antihistamines i. Used to relive pruritus associated w/ contact dermatitis. Best time to use them is before bed to promote sleep b/c the main side effect is drowsiness. 8. How do you select the most appropriate agent for treatment? a. Table 11.3 on page 159 b. c. Figure 11.1 on page 159 9. What is needed to know for special populations? a. Pediatric- topical corticosteroids should be used for only 7 days in children younger than 6 and at the lowest potency. Topical corticosteroids can cause skin atrophy. Topical immunosuppressants are considered for patients aged 2 and older. b. Geriatric- most common causes are topical medications. Adhesive patches may also cause contact dermatitis. 10. What is the monitoring information needed? a. Patients should follow up in 2-3 days after starting therapy. b. Educate patients on prevention strategies, application of creams, and apply an occlusive dressing to increase the efficacy of topical corticosteroids. 11. What are some complementary and alternative medicine for dermatitis? a. Ginkgo biloba antagonizes platelet-aggregating factors. b. Zinc can be used at a dosage of 50mg/day until the condition clears. c. Use of fish oil supplements incorporates omega-3 fatty acids into the membrane phospholipid pools d. Recommendations: i. Vitamin A 50,000 IU daily ii. Vitamin E 400 IU daily iii. Zinc 50mg daily, to be decreased as condition clears iv. EPA 540mg and DHA 360mg daily or flaxseed oil 10g daily v. Evening primrose oil 3000mg daily. Chapter 12: Fungal infections of the skin 1. What is tinea? .................................................................................continued....................................................................... [Show More]
Last updated: 1 year ago
Preview 1 out of 84 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 10, 2021
Number of pages
84
Written in
Additional information
This document has been written for:
Uploaded
Jul 10, 2021
Downloads
0
Views
45

.png)
.png)



.png)