*NURSING > STUDY GUIDE > NURS 6541 Peds Midterm Study Guide, Latest 2020 Complete A+ guide. (All)
NURS 6541 Peds Midterm Study Guide, Latest 2020 Complete A+ guide.
Document Content and Description Below
Section 1 Emily Turner 1. Children are able to sit without extra support at what age? 6-8 month olds should be able to sit briefly without extra support, 7-9 months old sit well independently. ... 2. Types of car seats (see also #60): Appropriate ages and weights for forward and rear facing seats. When can kids ride in the front seat of the car? 13 years old. When should they use booster seat? 4-8 years old The AAP recommends: ● Infants and toddlers should ride in a rear-facing car safety seat as long as possible, until they reach the highest weight or height allowed by their seat. Most convertible seats have limits that will allow children to ride rear-facing for 2 years or more. ● Once they are facing forward, children should use a forward-facing car safety seat with a harness for as long as possible, until they reach the height and weight limits for their seats. Many seats can accommodate children up to 65 pounds or more. ● When children exceed these limits, they should use a belt-positioning booster seat until the vehicle’s lap and shoulder seat belt fits properly. This is often when they have reached at least 4 feet 9 inches in height and are 8 to 12 years old. ● When children are old enough and large enough to use the vehicle seat belt alone, they should always use lap and shoulder seat belts for optimal protection. ● All children younger than 13 years should be restrained in the rear seats of vehicles for optimal protection. 3. Recommended vaccine schedule (many questions): https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html (Items 3, 6, 46, and 85 in this study guide address vaccines) 4. Child abuse questions: ○ What age is it appropriate to have certain types of fractures? Metaphyseal fractures, multiple differently aged posterior rib fractures, complex or multiple skull fractures, spinous process or scapular fractures are suspicious in children. ○ When should you be concerned about a young infant with tons of bruises (eg - if they are not walking yet would be unusual)? Long bone fx are unusual in young infants. ○ When is it necessary for you to report? Anytime you suspect any sort of abuse. ○ Who do you report to? CPS. ○ Do you face any repercussions? Should not. ○ Any fracture in a non-ambulatory infant without clear accidental and consistent mechanism should raise a red flag. (items 4, 5 and 29 in this guide address child abuse) 5. Toddler abuse: There will be a list of injuries. Which would be caused by abuse? ○ Bruises TEN4 by AAP i. T- torso; E- ear; N- neck; 4- in children less than or equal to 4 years and ANY bruise in children less than 4 months ○ Injuries tend to occur away from bony prominences (neck, head, buttocks, trunk, hands, and upper arms) 6. Contraindications of vaccinating children. Who should not receive a live vaccine? Immunocompromised, allergic reaction to a previous dose or component of vaccine, history of intussusception for Rotavirus See CDC sheet “vaccines by medical indication” https://www.cdc.gov/vaccines/schedules/hcp/imz/child-indications.html Immunocompromised should not receive: Rotavirus, MMR, influenza (LAIV) or varicella HIV infection should not receive: Influenza (LAIV), MMR or varicella Kidney disease should only cautiously receive influenza (LAIV) Asthma: No influenza (LAIV) CSF leaks: No influenza (LAIV) (Items 3, 6, 46, and 85 in this study guide address vaccines) 7. Young boy with mental retardation. He was a premie. They give a scenario. What caused his mental retardation? eg - understand congenital abnormalities, infections, preemie complications, chromosomal aberrations, brain tumor, serum blood levels ○ Important risk factors for intellectual disability (ID) include low level of maternal education, advanced maternal age, and poverty. ○ The causes of ID are extensive and include conditions that interfere with brain development and functioning. Among the known causes of ID, the majority are genetic abnormalities. i. A genetic cause can be identified in >50 percent of cases of ID in populations referred for specialty evaluation. Down syndrome is the single most common genetic cause of ID. X-linked disorders (including fragile X syndrome) account for approximately 5 to 10 percent of ID in males. De novo dominant mutations are an important cause of severe ID. ○ Metabolic disorders can cause ID or may be comorbid. ID can present alone or with neurologic abnormalities such as epilepsy or structural brain defects, or with other congenital anomalies. ○ Nongenetic prenatal causes of ID include congenital infections, and teratogens such as alcohol, lead, and valproate. Perinatal abnormalities account for up to 5 percent of ID and include preterm birth, hypoxia, infection, trauma, and intracranial hemorrhage. Postnatal and acquired causes of ID include accidental or nonaccidental trauma, central nervous system (CNS) hemorrhage, congenital hypothyroidism, hypoxia (eg, near-drowning), environmental toxins, psychosocial deprivation, malnutrition, intracranial infection, and CNS malignancy. i. Blood lead testing should be performed if the child has not had prior lead screening and/or risk factors for exposure are present (eg, persistent mouthing behavior, pica, living in a house or child care facility built before 1950, recent immigration or home renovation, ethnic remedies, and some parental occupations [smelting, soldering, and auto body repair]). Section 2 Melissa Burris 8. Newborns: What type of vitamin deficienc\ies cause problems? eg - vitamin A, B1, C, D and K Vitamin A Deficiency: Anorexia, dry skin, increased risk for infection, keratinization of epithelial cells of the respiratory tract,night blindness, corneal lesions. Vitamin B1 Deficiency: Beriberi: Muscle weakness, ataxia, confusion, anorexia, tachycardia, heart failure in infants. Vitamin C Deficiency: Scurvy, cracked lips, bleeding gums, slow wound healing, easily bruises. Vitamin D Deficiency: Inadequate bone mineralization, rickets or skeletal malformations, delayed dentition Vitamin K Deficiency: Defective coagulation of blood, hemorrhages, liver injury. 9. Failure to thrive in a 6 mo old: What exams would you think about doing? The reason for failure to thrive in children between the ages of 4 to 8 months is typically feeding problems. A thorough physical exam is important of each body system. Also assess skinfold measurements, vital signs, height, weight, head circumference, hydrations status, presence of dysmorphic features, skin, hair, nails mucus membranes, oral cavity, signs of abuse or neglect. Diagnostic testing: A feeding assessment should be performed including nutritional and feeding history for calories, protein, and micronutrient intake. Assess quality of food for age and ability to suck, chew and swallow. Assess meal patterns such as social nature of feedings with family. Assess feeding history with a 24 hour diet recall. Assess parental understanding of nutrition and feeding children. Assess developmental milestones If the child has inadequate caloric intake then a basic metabolic profile, vitamin D, lead, zinc, iron screening may be done. Albumin may be drawn if severe failure to thrive. If the child has inadequate caloric absorption then a cbc/esr, basic metabolic profile and newborn metabolic screening tests 10. What are the benefits of breastfeeding? eg - lower incidence of many diseases Breast milk is rich in vitamins,minerals,fat, proteins (including immunoglobulins and antibodies), carbohydrates (especially lactose), and promotes growth and development. Breast milk lowers the infants risks for gastroenteritis, necrotizing enterocolitis, acute otitis media, severe lower respiratory tract infections, asthma, atopic dermatitis, type 1&2 diabetes mellitus, obesity, SIDS, and childhood leukemia. Breast milk provides added protection against bacterial, viral, and protozoan illness during infancy. 11. How quickly will babies double, triple, etc their birth weight? Birth to 3 months 25 to 30g/day 3 to 6 months 15 to 20g/day 6 to 12 months 10 to 15g/day 12 months and older 5 to 10g/day The infant should have doubled their birth weight by 4-6 months. 12. Review early reflexive responses in newborns. eg -babinski, moro, swimming and rooting Babinski Reflex:Occurs after the sole of the foot has been firmly stroked. The big toe then moves upward or toward the surface of the foot and the other toes fan out. This reflex is normal in children up to age years old and will disappear as the child gets older and my disappear as early as 12 months. Abnormal reflex is often a sign of CNS disorder. Moro Reflex: Appears at birth and disappears by 4 months.This reflex is tested by a loud noise or drop the infant’s head slightly. The response is the infant will spread their arms and fingers extended and then flex; then the arms come toward each other; crying is possible. Asymmetry indicates paralysis, or fractured clavicle, absence indicates brainstem problem, usually severe persistence also abnormal. Swimming Reflex: A primitive fetal activity marked by well coordinated movements that are exhibited when the infant’s face is placed in water. It normally disappears at 6 months of age. Rooting Reflex: Present at birth disappears between 3-4 months. How to perform: the head is placed midline and then the perioral area is stroked. The response should be that the infant opens their mouth and turns head toward the stimulated side. Absence indicates CNS disease or severely depressed infant. A sleeping infant may not respond. Sucking Reflex: Present at birth and disappears between 3-4 months. Perform by placing nipple or finger 3-4cm inside of mouth. Suck should be strong:push finger up and back and note rate. Absence indicates CNS depression; satiated or sleeping baby may not respond well. Asymmetric Tonic Neck Reflex (ATNR): Present at birth and disappears between age 4-6 months. Place baby supine, turn head to one side; hold for 15 seconds. Arm and leg extend on facial side; arm and leg on other side flex. Obligatory response when a child cannot get out of the position is abnormal; persistence beyond 4-6 months indicates CNS lesion. Palmar Grasp: Present at birth and disappears between 3-6 months. Place finger into infant's palm and press against palm. Infant flexes all fingers around examiner’s finger. Grasp should be strong and equal. Trunk Incurvation(Galant): Present at birth and disappears at 2 months. Suspend baby prone; stroke 2-3cm from spine with fingernail. Baby should flex toward stimulus. Asymmetry is significant tests for spinal cord lesion; should not persist after 6 months. Stepping: Present at birth until 6-8 weeks. Infant is held as though weight bearing with feet on the surface. Infant steps along raising one foot at a time. Tests brainstem, spinal column; absence indicates paralysis or depressed baby. Crossed Extension: Present from birth to 4 months. Passively extend one leg and press knee to table; prick sole of foot with pin. Toes should curl down. Plantar Grasp: Present at birth and disappears between 8-10 months. Place finger firmly against base of toes. Toes should curl down. Tests S1-S2 spinal nerves; lessens by 8 months; suspect any asymmetry. Section 3 Sarah Lynn Hughes 13. Be familiar with language development. eg - red flags, when should kids be speaking in 3-4 word sentences, complete sentences, etc. 12-18M - uses all vowels, may constants, articulates 15-20 words and understands 50 18-24M -imitates two word combinations, begins to combine words, begins to use pronouns, names self 24-30M- bables less, 2-3 word sentences, repeats two numbers, asks simple questions, can repeat simple phrases and sentences 30-36M -answers questions, repeats three numbers, uses regular plurals, help tell simple story 36-42M- understands and answers (Cold, hungry), mostly three to four word sentences, gives full name, begins to relate events, lots of questions 42-48M- uses prepositions, tells stories, can give function of objects. Repeats longer than 6 word sentences, repeat four numbers, gives age 14. Which adolescent is at greatest risk for developing anorexia nervosa? Be familiar with this disorder. Females greater than males (9:1), Athletes more likely to develop eating disorders esp. Those who participate in sports that are based on weight. Individual risk factors: middle to high socioeconomic status, divorced families, chornic disease, recent weight loss in a prev obese person, personality disorders, strong will, hx of child abuse Pg 381-382 15. Fine motor skills under 2 years old - 6 months - Children should be reaching for toys and bringing everything into their mouths. They use their whole hand to grasp objects and should be able to transfer objects from one hand to the other. 9 months - Fine motor skills should allow them to poke at a small pellet-sized object with their index finger. Their grasp should have developed such that they now use their finger and thumb in a scissor fashion. 12 months- uses pincer grasps, points at objects, stacks two blocks, clasps hands together 15 months- puts blocks in a cup, drinks from a cup, holds utensils, some attempt to use. Stacks two blocks 18 months- builds tower of 4 cubes, scribbles spontaneously, puts blocks in large holes, drinks from a cup with little spilling, remove socks, stacks 4 to 6 blocks 24 months-building tower of seven cubes, circular scribbling, imitated folding paper once, turns doorknob, turns pages one at a time, unbuttons or unzips clothing, washes hands with assistance, uses a spoon Gross Motor 12 months- pulls self to stand, stands alone for 3 to 5 seconds, walks holding furniture, lowers self from standing to sitting without falling 15 months-stands alone well, walks forward and backward, stoops and recovers, climbs up stairs without alternating feet, pulls a pull toy 18 months-throws while aiming, walks well independently, pushes and pulls toys, pulls toy while walking backward 24 months-throws overhand, runs well, climbs up on furniture, kicks ball, walks up and down stairs, may not alternate feet, walks with control, runs, jumps up, assists with dressing, able to pull pants down with assist 16. Head and chest circumference 1-3M Length increases 1.4 inches per month and head circumference increases about 0.8 inches per month with more rapid growth for the younger infant. 4-5M Length increases 0.8 inches per month, head circumference 0.4 inches month 6-8M length increases 0.5-0.6 inches per month, head circumference 0.2 inches per month A newborn's head is usually about 2 cm larger than the chest size. Between 6 months and 2 years, both measurements are about equal. After 2 years, the chest size becomes larger than the head. Measurements over time that show an increased rate of head growth often provide more valuable information than a single measurement that is larger than expected. 17. Breast milk and what signs that there is not enough -continued weight loss after 5 to 7 days -failure to regain birth weight by 2 to 3 weeks -failure to maintain an ongoing weight gain of 0.5 to 1 oz/day -weight below the third percentile for age (this finding can be a pattern over time or a sudden change) -lethargic, sleepy, inactive, unresponsive infant -newborn or young infant sleeping longer than 4 hours between feedings -dry mucous membranes -poor skin turgor Section 4 Myesha Shultz 18. When to start measuring blood pressure P. 759 annually beginning at 3 y/o 19. Role play with exam techniques and when to start toddlers and young preschoolers p. 362 20. Abnormal language development 21. Onset of male and female puberty Female Tanner I: no gla AGE MOTOR SOCIAL Newborn (1 week-1 month) Fixates on faces, lifts head for moments when prone and turns side to side, sleeps 3-4 hours at a time (16-18 total in 24 hours) Blinks, Cries, comforted by being held and fed 2 months Lifts head, neck, and upper chest when prone, some head control when upright, will shake rattle before 4 months Coos, smiles, shows interest in visual and auditory stimulus 4 months Reaches for objects, open hands to grasp objects, raises body on hands (prone), rolls front to back, good head control, recognizes parents voice/touch, sleep 6 hours Babbles, coos, smile, laugh, squeals, social smile, can comfort self (to an extent) 6 months No head lag, sits with support, rolls over both ways, Stands when placed on feet, bears weight, starts to feed self and drink from cup, transfers objects from hand to hand, raking grasp (fingers to palms without thumbs) Says “dada” “mama”, babbles reciprocally, turns to sounds 9 months Crawls, creeps, moves forward by scooting, sits independently, may pull to stand, pokes with index finger, uses (imprecise) pincer grasp or finger grasp, plays interactive games (peek-a-boo & pat-a-cake), feeds self with fingers, sleep through the night Stranger danger, responds to name, understands no and bye, babbles, starts vowel-consonant combinations, 12 months Pulls to stand, creeps, may take a few steps alone, precise pincer grasp, points with index finger, plays social games games (peek-a-boo & pat-a-cake), drinks from cup, feeds self finger foods, Waves bye, says 1-3 words (mama, dada, baba), reaches and points at things they want, starts to follow one stop commands, names pictures, points to familiar objects 18 months Walks fast, runs stiff, walk backwards, stacks 3-4 blocks, throws ball standing, points to body parts, scribble with crayon, uses spoon, drinks from cup 15 word vocabulary, imitates words, listens to stories, follows simple directions, voice 2 or more wants, shows affection (Kisses) 2 years Goes up and down stairs one leg at a time, kicks balls, stacks 5-6 blocks, makes circular strokes with crayons 2 word phrases, 20 word vocabulary, understand 25% of what they say, imitates adults 2.5 years Walks on tiptoes, jumps with both feet, speeds up and slow down while running, puts together simple puzzles, stacks 9 blocks, imitates circles, button large buttons, uses fork Elaborate play, short phrases 2-3 words, has fun playing/socializing, enjoys rhyming 3 years Goes up and down stairs, alternating feet, jumps in place, balance on one foot, kicks a ball, riding a tricycle, dresses self (with assistance), feeds self Knows name, knows age, knows gender, has bladder/bowel control, imagination develops, follows two step instructions, understands “on” “in” and “under”, can understand 75% of time 4 years Builds tower 10 blocks, throws overhand, hops, jumps on one foot, strings small beads, copies (cross, square, bridge), cuts curves with scissors Sings songs, draws 3 part person, knows things at home (fridge, mop, broom ect…), knows fantasy from reality, talks about day, aware of gender, can understand 100% of time 5-6 years Participate in group sports, dress self without assistance, play more in groups, prints name, cuts out simple shape, copy triangle, pours from a small pitcher, bathes self, open a lock with a key Start school, learning delays may become evident, want to be independent (not able to make good decisions), safety (strangers, riding bike, crossing street), not able to adapt to rules, still need supervision, draws a person with 6 parts, recognizes simple colors, understands future tense follows 3 part commands 7-8 years Chores (set table, trash, put away clothes), independent hygiene Understand safety (needs supervision still), play with children of same sex (best friends age), understand feelings of others, uses logic 9-10 years Concerned about pre-pubertal changes Independence, peers have greater influence than parents, self-esteem is directly related to ability to handle peer pressure, risk taking behaviors (dares, swearing, tobacco use), Tanner Stage 1 11-14 years Acne Tanner Stages 1-4, moody, egocentric, concrete thinking (here and now), MVA & cyclist deaths, parents role models (peer influence increases), girls start puberty 2 years prior to boys 15-17 years Acne, puberty changes, size and height matter Tanner stages 4-5, concrete to operational thinking, work outside the home, risky behaviors escalate (sex, alcohol, drugs, cigarettes), MVA major cause of death, social norms determine attitude *Much of school age and adolescent history includes asking about their typical day, their friends, their activities, how they feel about themselves, do they feel they are maturing like their friends, ask about risky behaviors (sex, drugs, smoking ect…), offer advice to overcome peer pressure. Refer as needed to counseling for low self-esteem. Educate parents on how to increase self-esteem in their child. Section 5 Ann Quinlan 23. Piaget’s development stages, ex: sensory motor etc. Sensorimotor stage (age birth-2yrs): Dramatic growth and learning occurs. At this stage they acquire knowledge through sensory experiences and manipulating objects. Their entire experience occurs through basic reflexes, seses, and motor responses.They learn how to perform physical actions like crawling and walking. They learn all about language. Preoperational stage (2-7yrs): This stage is the emergence of language. They begin to think symbolically and learn to use words and pictures to represent objects. They tend to be egocentric and struggle to see things from the perspective of others. They think about things in very concrete terms. They become skilled at pretend play and struggle with understanding the idea of consistency. Concrete Operational stage (7-11yrs): They begin to think logically about concrete events. They begin to understand the concept of conversation (it becomes logical and organized but is still very concrete). Egocentrism begins to diminish. They struggle with abstract/hypothetical concepts. They begin to understand that their thoughts, feelings, and opinions are unique and different from everyone else. Formal Operational stage (12yrs and up): They begin to think abstractly and reason about hypothetical problems. They think more about moral, philosophical, ethical, social, and political issues that require theoretical abstract reasoning. They become able to see multiple potential solutions to an issue and think more scientifically about them. 24. Temperament ○ Activity: Does the child move all the time or are they not very active? What is the activity level? Recognize their normal level of activity and plan high energy activities as much as possible. ○ Rhythmicity: How predictable is the sleep/wake, feeding, and elimination pattern? Keep sleep/wake, feeding and elimination schedule as regular as possible. Avoid activities during “normal” nap times. Use elimination patterns as a guide to toilet training. ○ Adaptability: How quickly do they get used to new things? Teach young children how to deal with disappointment. Provide reassurance when things don’t go as planned. ○ Approach or Withdrawl: What is their response when they are presented with something new? Do they approach it openly or turn away? Teach young children the skills necessary to deal with discomfort felt with meeting new people or new experiences. Provide opportunities for them to experience new things. ○ Threshold: How much stimulation do they require for calming? Do they respond better to a quiet voice and light touch or to a loud voice with a firm grasp? Recognize that not all children require the same amount of stimulation for calming. Adapt redirection strategies and approaches to the situation. Use care not to over respond. ○ Intensity of Reaction: Are the child’s responses (laughing or crying) very subtle or extremely intense? ○ Quality of Mood: Are they usually outgoing, happy, joyful and pleasant or instead, unfriendly, withdrawn, and quiet? ○ Distractibility: How easily are they distracted by outside disturbances? ○ Attention span/ Persistence: How long will they play with a particular toy or engage in a certain activity? Do they continue to engage even if there are distractions? 25. Dietary: When to wean? Start table foods? The American Academy of Pediatrics recommends breastfeeding as the sole source of nutrition for your baby for about 6 months. When you add solid foods to your baby’s diet, continue breastfeeding until at least 12 months. You can continue to breastfeed after 12 months if you and your baby desire. However, mothers in the United States have tended to wean much earlier than in most other countries. The AAP recommends weaning bottle-fed infants completely by 15 months. Prolonged bottle feeding has been associated with excessive milk intake and iron deficiency due to displacement of iron-containing food choices. They recommend beginning the child on vitamin D milk at 12 months of age. Breastfeeding should be encouraged for at least 12 months if possible and weaning from breast is highly dependant upon the child, mother, and numerous other factors. It is a personal choice/preference. 26. Comprehensive development and when to refer. (Warning signs of when to refer for a comprehensive developmental eval. Speech, developmental milestones, etc.) THIS IS A VERY VERY BROAD QUESTION. I RECOMMEND REVIEWING FROM THE BOOK. 27. Physical development of female puberty: The process that begins with breast development (thelarche), then the growth of pubic and axillary hair (pubarche), and finally the first menses (menarche). Tanner Stages: 1. (Preadolescent): No growth of pubic hair and no glandular breast tissue is present. 2. Scarce, pigmented, straight hair along the medial border. Breast buds are palpable under the areola (1st sign). 3. Sparse, dark, curly pubic hair is present. Breast tissue is palpable outside of the areola. Still no development of the areola. 4. Pubic hair is course, curly, and abundant, but less than that of an adult. The areola is elevated above the contour of the breast, forming a “double scoop” appearance. 5. Lateral spreading of pubic hair occurs in a triangle onto the thigh. The areolar mound recedes back into a single breast contour with areolar hyperpigmentation, papillae development, and nipple protrusion. 6. There is further extension of pubic hair laterally, upward, or dispersed. Section 6 Amy Gass Roberts 28. Abnormal language development Textbook Pg 78 Red Flags Language disorders ○ Aphasia (difficulty understanding or speaking parts of language due to a brain injury or how the brain works). ○ Auditory processing disorder (difficulty understanding the meaning of the sounds that the ear sends to the brain) Always listen to parents! 29. The most common form of child abuse in pediatric care - Neglect, then Physical Abuse (items 4, 5 and 29 in this guide address child abuse) pg 332-333 in text. Four categories: Neglect, psychological, physical, and sexual. Children less than 1 yr have highest rate of victimization. Repeated injuries that are unusual Overly compliant or exaggerated fearfulness Clingy or indiscriminate attachment, Extremes in behaviors Wary of physical contact with adults Frightened of a parent or caretaker Withdraw from family or friends, poor school performance, depression, anxiety, mistreating animal or pets, self mutilation Suicidal Sleeping or eating disorders Child physical abuse should be considered in each of the following: ● A non-ambulatory infant with any injury ● Injury in a nonverbal child ● Injury inconsistent with child’s physical abilities and a statement of harm from the verbal child ● Mechanism of injury not plausible; multiple injuries, particularly at varying ages ● Bruises on the torso, ear or neck in a child younger than 4 years of age ● Burns to genitalia ● Stocking or glove distributions or patterns ● Caregiver is unconcerned about injury ● An unexplained delay in seeking care or inconsistencies or discrepancies in the histories provided. "TEN 4" is a useful mnemonic device used to recall which bruising locations are of concern in cases involving physical abuse: Torso, Ear, Neck and 4 (less than four years of age or any bruising in a child less than four months of age). A few injuries that are highly suggestive of abuse include retinal hemorrhages, posterior rib fractures, and classic metaphyseal lesions. 30. Explanation for small size in infant - weight below the 10th percentile for gestational age, Babies born weighing less than 5 pounds, 8 ounces are considered low birth weight. Some babies are small because their parents are small. But most babies who are small for gestational age have growth problems that happen during pregnancy. Many of these babies have a condition called intrauterine growth restriction. This happens when the unborn baby doesn’t get the nutrients and oxygen needed to grow and develop organs and tissues. This can begin at any time in pregnancy. Problems with the mother · High blood pressure · Chronic kidney disease · Diabetes · Heart disease or respiratory disease · Malnutrition or anemia · Infection · Alcohol or drug use · Cigarette smoking · Weighing less than 100 pounds Problems with the uterus and placenta · Decreased blood flow in the uterus and placenta · Placenta detaches from the uterus · Placenta attaches low in the uterus · Infection in the tissues around the baby Problems with the developing baby · Multiple pregnancy, such as twins or triplets · Infection · Birth defects · Chromosome problems 31. Presentation of congenital cytomegalovirus, down syndrome, craniopharyngioma (all cause low birth weight) Cytomegalovirus (CMV)1117- maternal CMV infection, SGA, jaundice, hepatosplenomegaly, petechial rash, chorioretinitis, cerebral calcifications, microcephaly Down Syndrome- 1163- short stature, brachycephaly, midface hypoplasia with flat nasal bridge, brushfield spots, epicanthal folds with palpebral fissures that slant down to midline, small mouth with protruding tongue, myopia, small ears, lax joints, short broad hands, feet and digits, single palmar crease, clinodactyly, exaggerated space between great and second toes, congenital heart disease, at risk for: leukemia, Alzheimer's disease and hypothyroid Craniopharyngioma- most often affects children bw 5-14 years. vision problems, nausea and vomiting, poor balance, heachaches, sleepiness, mood swings, personality changes, slowed growth, weight gain, excessive thirst 32. Failure to thrive: sweat chloride, testing of the stool, MRI brain Section 7 Courtney Kunze 33. Poor weight gain (what type of therapy might they need?) Scenario: lab studies with electrolytes, H&H. What is causing poor weight gain? Look up sweat chloride testing, growth hormone determination, etc. 34. Advice for well-child at visits. eg - 2 week old, what info do you give mom and dad? Accept help from family, friends. • Never hit or shake baby. What makes you get upset with the baby? What do you do when you get upset? • Take care of yourself; make time for yourself, partner. • Feeling tired, blue, or overwhelmed in first weeks is normal. If it continues, resources are available for help. 35. Diet info: eg - What food should a healthy 6 mo old be eating? Exclusive breastfeeding during the first 4-6 months is ideal; iron-fortified formula is recommended substitute; recognize slowing rate of growth. • Determine whether baby is ready for solids; introduce single-ingredient foods one at a time; provide iron-rich foods; respond to baby’s cues. • Begin cup; limit juice (2-4 oz a day). • If breastfeeding: Continue as long as mutually desired. • If formula feeding: Don’t switch to milk; contact WIC/community resources for help. 36. Normal sequencing of development in a toddler. List of questions about developmental abilities of a toddler. 37. Teething toddler recommendations p 891 Cold teething ring, wet, chilled washcloth, massaging the guns, for older children, may use chilled hard food. Tylenol Ok. Do not use frozen anything or orajel. 38. More questions about language development issues Section 8 Danielle LeBlanc 39. Sleep patterns in young children (this image is bigger on #47) 40. Refusal bowel patterns on toilet Two behaviors associated with stool toileting refusal may require the intervention of the pediatrician. The first is stool withholding causing constipation which can result in rectal impaction and primary encopresis. The second is lack of successful toilet training by 42 months of age. 41. 2 year-old breath holding spells A spell typically lasts less than a minute before a child starts breathing normally again. Breath-holding spells can happen in healthy children between 6 months and 6 years old, but are most common during the second year of life. They can be more common in kids with a family history of them. -not voluntary or intentional, not harmful, worst case seizure with no lasting effects, two types: cyanotic (usually doesn’t breath during a crying fit and passes out) and pallid (scared, turns white and passes out), should only last one minute at the longest 42. Bilingual child advice It preserves culture, increases mental flexibility, increases employment and lifestyle opportunities, suggest one-parent use one language, language milestones met in primary language, but secondary language lags, if significant delays then evaluation similar as with monolingual children 43. Walking around with object at what age - 18 months. Section 9 Shana Light What are some common features of 12 mo old, 2yo, 5yo behavior? 44. Stranger anxiety - Fearfulness in the presence of strangers is thought to emerge around 6 months of age and extends through about 36 months of age. At 12 month WCC, warn parents that stranger anxiety reaches a peak in the next few months. The onset of stranger fear is believed to be adaptive, offering balance to infants’ propensities for approach and exploration. Some fear is normal, excessive fear can be a predictor for social anxiety later in life. Some experts suggest that Infants who develop Autism Spectrum Disorder have an absent, delayed, or modified Stranger Anxiety Response. 45. Parallel play - From the age of two to three, children move to playing alongside other children without much interaction with each other. They may be engaged in similar activities or totally different activities but they like being around others their own age. Non-parallel play - Negativism - to increase independence- 18-30 months (lots of saying “no”) 46. Catch up vaccines - https://www.cdc.gov/vaccines/schedules/hcp/imz/catchup.html (Items 3, 6, 46, and 85 in this study guide address vaccines) 47. Normal sleep pattern for infants - As compared with older children and adults, newborns have longer sleep duration, an increased proportion of REM sleep, and shorter REM-NREM cycles. Sleep-wake patterns become more diurnal and sleep times gradually decrease from infancy through adolescence. Identification of sleep problems in children is important because a growing body of evidence suggests that sleep disorders may interfere with physical, cognitive, emotional, and social development. Conversely, children with neurodevelopmental problems, learning differences, or behavior problems may be at heightened risk for sleep problems compared wi Mantoux skin test is an intradermal injection of 0.5-5ml tuberculin units that should produce a palpable wheal of 6-10mm induration. Read the test at 48-72 hours, measuring induration not erythema. The following are considered positive for latent infection or active TB: -induration of 5mm or greater in children who are in close contact with a patient who is in active or previously active TB, have HIV, immunosuppression or are recieveing immunosuppressive drugs. - Induration of 10mm or greater in children younger than 4 with any of the above higher risk factors - Induration of 15mm or greater in children 4 and older with no other risk factors - If the skin test shows any induration after 72 hours it should be considered positive Interferon Gamma release assay is a screening that rests for t-cell response to the specific M. Tuberculosis antigens. They have an advantage over the Mantoux in that they are not affected by prior BCG vaccine. positive result is indicative of TB infection. This is the recommended test for those 3 and older who received the BCG vaccine, or who are unlikely to RTC for TST reading 50. Breastfeeding and what we should tell breastfeeding moms for reassurance 51. Screening refugee children for TB. What other types of screening are required for refugee children?tuberculosis-guidelines.html 52. Adolescent patient labs: fasting and postprandial glucose FBG 126 or greater, Hgb AIC of 6.5% or greater, post prandial glucose of 200 or greater is indicative of diabetes 53. Regular screening tests for patients with a history of hyperlipidemia and obesity Section 11 Beth Lax 54. Well child check-ups help track growth and development, prevention by administering vaccines, time to discuss concerns, and builds a team approach to care. Schedule per Bright Futures Newborn, First week (3-5 days), 1 month, 2 month, 4 month, 6 month, 9 month, 12 month, 15 month, 18 month, 2 year-18 years. 55. Drug screen of children and STIs All children over 14 can request STI testing and treatment confidentially without parent approval. Children under 13 will need to have parent approval or child protective services involved. High risk individuals: youth in detention centers, male homosexuals, and IV drug users. Highest rates in 15-24 yo. 56. Anticipatory guidance for 5 year old and 8 year old 5 yr olds Social determinants of health: Risks (neighborhood and family violence, food security, family substance use), strengths and protective factors (emotional security and self-esteem, connectedness with family) Teach your child nonviolent conflict-resolution techniques Talk with parents/trusted adult if you are bullied Contact community resources, like SNAP, for help with food assistance Don’t use tobacco/e-cigarettes. Call 800-QUIT-NOW for help to quit smoking. Talk with me if you are worried about family member drug/alcohol use. Encourage independence, self-responsibility; show affection; praise appropriately Spend time with your child. Make time to talk Development and mental health: Family rules and routines, concern for others, respect for others; patience and control over anger. Continue family routines; assign household chores Use discipline for teaching, not punishment Model anger management/self-discipline Solve conflict/anger by talking, going outside and playing, walking away School: Readiness, established routines, school attendance, friends; after-school care and activities, parent-teacher communication. Ensure child is ready to learn (regular bedtime routine, healthy breakfast) Tour school; attend back-to-school events. Be sure after-school care is safe, positive Talk with child about school experiences If child has special health care needs, be active in IEP process Physical growth and development: Oral health (regular visits with dentist, daily brushing and flossing, adequate fluoride, limits on sugar-sweetened beverages and snacks), nutrition (healthy weight; increased vegetable, fruit, whole-grain consumption; adequate calcium and vitamin D intake; healthy foods at school), physical activity (60 minutes of physical activity a day) Help child with brushing teeth if needed. Visit dentist twice a year Brush teeth twice a day; floss once Help child choose healthy eating (provide healthy foods, eat together as a family, be a role model) Eat breakfast; eat vegetables/fruits Eat when you’re hungry; stop when you’re satisfied Drink milk 2 to 3 times per day Limit sugary drinks/foods Consider making family media use plan (www.helathychildren.org/MediaUsePlan), which can help balance child’s needs for physical activity, sleep, school activities, and unplugged time; decide on rules for media time in time left over after all other activities; take into account quantity, quality, location of media use. Be physically active often during the day Safety: Car safety (also see #2 and #60), outdoor safety, water safety, sun protection, harm from adults, home fire safety, firearm safety. Use properly positioned belt-positioning booster seat in backseat Teach safe street habits (crossing/riding school bus) Ensure child uses safety equipment (helmet, pads) Teach child to swim; supervise around water Use sunscreen; wear hat; avoid prolonged exposure when sun is strongest, between 11:00 am and 3:00 pm Teach rules for how to be safe with adults: (1) no adult should tell a child to keep secrets from parents; (2) no adult should express interest in private parts; (3) no adult should ask a child for help with his/her private parts; explain “privates” Install smoke detectors and carbon monoxide detector/alarms; make fire escape plan Remove firearms from home; if firearm necessary, store unloaded and locked, with ammunition locked separately 8 year olds Social determinants of health: Risks (neighborhood and family violence, food security, family substance use, harm from the internet), strengths and protective factors (emotional security and self-esteem, connectedness with family and peers) Teach your child nonviolent conflict-resolution techniques Talk with parents/trusted adult if you are bullied Contact community resources, like SNAP, for help with food assistance Don’t use tobacco/e-cigarettes. Call 800-QUIT-NOW for help to quit smoking. Talk with me if you are worried about family member drug/alcohol use. Put family computer in easily seen place, monitor computer use; install safety filter Don’t give out personal information online Encourage independence, self-responsibility; show affection; praise appropriately Spend time with your child. Make time to talk. Know child’s friends. Development and mental health: Independence, rules and consequences, temper problems and conflict resolution; puberty and pubertal development Encourage competence/independence/self-responsibility Discuss rules, consequences Be positive role model; do not hit or let others hit Talk about worries Be aware of pubertal changes; answer questions simply School: Adaptation to school, school problems (behavior or learning issues), school performance and progress, school attendance, IEP or special education services, involvement in school activities and after-school programs, parental involvement Ensure child is ready to learn (regular bedtime routine, healthy breakfast) Show interest in school and activities If concerns, ask teacher about evaluation for special help/tutoring; help with bullying If child has special health care needs, be active in IEP process Physical growth and development: Oral health (regular visits with dentist, daily brushing and flossing, adequate fluoride, avoidance sugar-sweetened beverages and snacks), nutrition (healthy weight; adequate calcium and vitamin D intake; limiting added sugar intake), physical activity (60 minutes of physical activity a day, screen time) Take child to dentist twice a year Give fluoride supplement if dentist recommends Limit sweetened drinks/snacks Brush teeth twice a day; floss once Wear mouth guard during sports Help child choose healthy eating (provide healthy foods, eat together as a family, be a role model) Eat breakfast; eat vegetables/fruits Eat when you’re hungry; stop when you’re satisfied Drink milk 3 or more times a day Limit sugary drinks/foods Be physically active often during the day Consider making family media use plan (www.healthychildren.org/MediaUsePlan), which can help balance child’s needs for physical activity, sleep, school activities, and unplugged time; decide on rules for media time in time left over after all other activities; take into account quantity, quality, location of media use. Safety: Car safety (also see #2 and #60), safety during physical activity, water safety, sun protection, harm from adults, firearm safety Use belt-positioning booster seat in the backseat Ensure child uses safety equipment (helmet, pads). Be a role model and always wear a helmet Teach child to swim; supervise around water Use sunscreen; wear hat; avoid prolonged exposure when sun is at its strongest, between 11:00 am and 3:00 pm Know child’s friends; teach home safety rules for fire/emergencies; teach rules for how to be safe with adults: (1) no adult should tell a child to keep secrets from parents; (2) no adult should express interest in private parts; (3) no adult should ask a child for help with his/her private parts. Remove firearms from the home; if firearm necessary, store unloaded and locked, with ammunition locked separately 57. A mother states her daughter cheats when playing certain games. What is your best response? 58. 7 year old accidents at night and bedwetting Nocturnal enuresis-monosymptomatic nocturnal enuresis (no problems during the day just at night)-non-monosymptomatic nocturnal enuresis (bowel, bladder symptoms during the day as well as problems at night). Diagnosing 1) Determine if the child is constipated or impacted. 2) Neurological developmental delay. 3) Behavioral comorbidities. Link to ADHD and enuresis (especially daytime enuresis) 4) Functional small bladder capacity. Seems normal but at night functionality is reduced. 5) Sleep disorders-obstructive sleep apnea. 6) Stress and family issues. Divorce, move, new family member. 7) Polyuria-drinking through the night or too much caffeine intake. 8) Inappropriate toilet training. Gather information History Voiding characteristics (urgency, dysuria, dribbling), cluster voiding (waiting till after school), bowel and bladder postponing behavior, number of voids per day, frequency of wetting (day or night). Pediatric urology referral (weak or interrupted urinary stream, need to use abdominal pressure to urinate, Both daytime incontinence and nocturnal enuresis combined. How much fluid intake and when. UTI Family history-treatment, age of resolution Toilet training history-age, how, did child ever remain dry and for how long What happens when enuresis occurs, punishment, who changes bed, what previous tx Sleep patterns-does child have obstructive sleep disordered breathing or apnea General health Behavior issues Have there been any changes in the home, was enuresis present before Physical exam Assess external genitalia checking for irritation, infection, labial fusion, and or meatal stenosis. Check for fecal impaction-looking for masses at the suprapubic midline and LLQ Check lower back for dimples and hair tufts Assess for neurologic function and deep tendon reflexes Diagnostics UA with culture if warranted Management Urotherapy-voiding schedule and regulate fluid intake, using appropriate posture when urinating, voiding before bed and immediately upon waking. Aggressive treatment of constipation. Enuresis alarm-an alarm sounds when it is getting wet. It is first-line therapy when kidney disease, diabetes, or urogenital malformations have been ruled out. Drug therapy-not a curative, but helps when used in conjunction with other interventions. Desmopressin is most effective in children with large nocturnal urine production and normal nocturnal bladder capacity. Short term 4-8 weeks. (Often used for sleepovers) Must awaken children 10 hours after taking to urinate. Take on an empty stomach avoid caffeine, chocolate, NutraSweet and carbonated beverages. 59. Erickson’s stages of development Erickson expanded on Freud’s theories-each stage presents problems that an individual seeks to master. He believed if problems were not resolved, they would be revisited again at future stages. Psychological Crisis Themes 0-12 mo Trust vs Mistrust To get; to give in return 12-18 mo Autonomy vs Shame To hold on; to let go 18-36 mo 3-6 yr Initiative vs Guilt To make things; to play 6-11 yr Industry vs Inferiority To make things; to complete 12-17 yr Identity vs Role Confusion To be oneself; to share being oneself or not being oneself. 17-30 yr Intimacy vs Isolation To lose and find oneself in another Section 12 Lizzie Yager 60. Car safety (also see #2) ○ All infants and toddlers should ride in a rear-facing seat until they reach the highest weight or height allowed by their car seat manufacturer. Most convertible seats have limits that will allow children to ride rear facing for 2 years or more. ○ Children who have outgrown the rear-facing weight or height limit for their convertible seat should use a forward-facing seat with a harness for as long as possible, up to the highest weight or height allowed by their car seat manufacturer. Many seats can accommodate children up to 65 pounds or more. ○ All children whose weight or height exceeds the forward-facing limit for their car safety seat should use a belt-positioning booster seat until the vehicle seat belt fits properly, typically when they have reached 4 feet 9 inches in height and are 8 through 12 years of age. All children younger than 13 years should ride in the back seat. 61. Bullying - Ultimate goal is to stop bullying before it starts through prevention programs in schools and community resources. ○ Defined by CDC as unwanted aggressive behaviors by another youth or group of youths-- very common in school setting (higher in middle than in high schoolI ○ Involves an observed or perceived power imbalance and behaviors are likely to be repeated multiple times ○ Can include physical, verbal or relation/social (i.e. rumors, isolation) i. Cyber bullying now included with the recent advent of social media 1. Girls more often than boys ○ Bullying behaviors can cause harm and distress both physically and psychologically i. Can cause social isolation and academic decline ii. Stress of bullying can increase risk of suicide ○ Bullies can be considered perpetrator and/or victim: multiple factors can increase the risk of engaging in bullying i. Intolerance of violence ii. Externalizing behaviors iii. Low self-esteem iv. Poor peer relationships v. Perception of being different vi. Can include siblings and relationship partners ○ PCP should treat and manage any injuries and refer to mental health and social work for continued followup i. Report to CPS and law enforcement when necessary. ii. Interview child separately from parent: determine if bully, victim, or both iii. Use HEEADSSS assessment 1. Assess for drug/alcohol use 2. Assess for weapon use iv. Open ended questions 62. Puberty in Males ○ Initial sign is testicular enlargement (avg of 11 years old) i. This happens about 6 months before pubic hair development ii. Left testis hangs lower than right ○ First release of spermatozoa (spermarche) generally at mean of 13.5 to 14.5 yrs ○ Rapid growth in height, peak height late in puberty i. Generally lag 2 years behind girls ii. Growth spurts usually between 12 and 16 years iii. Change in voice coincides with peak height ○ Development of axillary, facial and body hair ○ 65% of males experience gynecomastia, enlargement of breast tissue, within a year of PHV. Generally lasts 12 to 18 months. ○ Acne early in puberty 63. Role of the NP in helping children and adolescents have healthy sexual development provides an opportunity for the teen to ask questions to explore their sexuality -APRN ROLE: ensure confidential environment where each can freely exchange information providing guidance toward sexual, moral, social, physical development responsible sexual behavior teaching educate about use of condoms appropriate methods of BC and how to use annually interviewing about sex, alcohol and drug use asking questions about sexual orientation, number of partners, exchanging sex for drugs and unintentional pregnancies assessing sexual maturity phases for normal progression screening sexually active use for STIs (gonorrhea and chlamydia), and providing pregnancy and partner notification for referral and treatment Providing confidential HIV and syphilis screening for at risk youth Initiating routine cervical cytology at 21 y/o initiating Hep B series for those 11 and older recommending HPV vaccinations to 11-12 y/o 64. Adolescent substance abuse, what is true and not true pgs 383-385 *s/sx: decreased school performance, lethargy, hyperactivity or agitation, decreased attention, disinhibition, acting out, sleep changes, mood swings, change in appetite weight loss, red eyes, chronic cough, frequent cold or allergy sx, accidents, trauma or injuries, intoxication, amnesia, dilated or constricted pupils, gynecomastia, irregular periods, small testes (pot), needle tracks, generalized pruritus (opioids), reflux, diarrhea, gastritis (opiate and alcohol use) perioral sores and pyodermas Section 13 Amy Holt 65. Regular screening in adolescents 66. Peak height velocity by Tanner stage for adolescent girls 67. Erickson’s Stage for adolescent: *12-17 y/o Identity vs Role Confusion- To be oneself; to share being oneself or not being oneself. 68. 14 year-old on too many meds, our role after emergent care and stabilization is completed 69. Findings with diagnosis of school phobia -separation anxiety d/o, simple and social phobias, depression s/sx: -severe difficulty attending school or refusal to go to school - severe emotional upset when goes to school - absence of significant antisocial d/o - staying at home with the parent’s knowledge - may complain of headaches, stomach aches, dizziness or fatigue diagnostic tools: - depression/anxiety screen - ADHD screen - assess for sexual or physical abuse - assess for learning disability - assess for family dysfunction Management: - support parents in insisting on full time school participation - notify school personnel to gain their support and encouragement - assess home situation - refer to psychiatrist if not improvement after 2 weeks Section 14 Ashley Esquibel 70. Common substance abuse middle school p.384 Alcohol is the most common, followed by marijuana 71. What to keep confidential with an adolescent ● Preserving confidentiality with the teenager is essential. ● Adolescents must be actively included in decisions about sharing information with others. For many sensitive health issues, providers need to help the teenager understand and evaluate the risks and benefits of involving family members. They must also provide guidance and support on how to best inform the family, if that is the final choice. This approach can help protect a teen from the parent who may be abusive or unsafe. It can also reduce the problem of parents who are upset if they feel they are denied information about the child they love and for whom they feel responsible. ● Adolescents should be reassured that the provider will not share information with the child's parent or caregiver (general confidentiality) unless the adolescent agrees, or unless the health of the child or others may be compromised (e.g., threat of potential suicide, violence, evidence of an eating disorder). ● Providers must inform the teenager that there are limits to confidentiality (limited confidentiality). As “mandatory reporters,” primary health care providers are required by law to report information that puts the child or others in danger (e.g., physical or sexual abuse; some states require reporting teen sexual activity, even if consensual, if an age difference of 3 or more years exists between the couple). 72. First line attention deficit disorder drug for child ● The first-line medications for uncomplicated ADHD treatment are the stimulants, methylphenidate and amphetamine compounds, which are each equally effective and available in a variety of forms (Table 20-7). ● First line therapy for a preschooler dxed with ADD: Dose titration for preschool children — The metabolism of methylphenidate is slower in preschool children than in older children and adolescents. Preschool children usually are started at a lower dose that is increased in smaller increments. In the Preschool ADHD Treatment Study (PATS), the authors concluded that it may be best to begin methylphenidate at 2.5 mg orally twice per day, and during the course of one week, increase the dose as necessary up to 7.5 mg orally three times per day. We agree with this regimen. (Per UpToDate). 73. Illegal street drug presentation ● Cocaine: Dilated pupils, excitability, runny nose, weight loss, mood swings, burn marks on hands or lips, nosebleeds, changes in sleeping or eating patterns, increased need for privacy ● Heroin: weight loss, scabs on skin, agitation or irritability, hallucinations, increased sleep, paranoia, apathy, slurred speech, dry mouth, constricted pupils, itching, track marks ● Methamphetamines: anxiety, euphoria, depression, increased HR, high BP, increased energy, insomnia, increased arousal ● Opiates: changes in sleep, needle marks, pinpoint pupils, flushed itchy skin, withdrawal, shallow breathing, blurred vision, hallucinations, N/V ● Marijuana: red, bloodshot eyes, glassy eyes, tachycardia, sleepiness, impaired coordination, heart attack,memory loss 74. Eye findings that are an ophthalmic emergency ● Herpes simplex conjunctivitis requires immediate hospitalization for topical and systemic antivirals ● Fixed pupil with bulging iris (iritis, cyclitis, chorditis) ● Keratitis is a medical emergency (inflammation of the cornea) that can progress to blindness ● Retinal detachment is an ophthalmic emergency ● Orbital hematoma, contusion of the globe ● Orbital fracture is an ophthalmic emergency 75. s/s assessments for dx such as pupillary reaction, optic disk papilledema, conjunctival inflammation, ocular mobility ● Pupillary reaction: The ‘swinging light test’ is used to detect a relative afferent pupil defect (RAPD): a means of detecting differences between the two eyes in how they respond to a light shone in one eye at a time. The test can be very useful for detecting unilateral or asymmetrical disease of the retina or optic nerve. When a bright light shone into one eye leads to an equal constriction of both pupils. When the light source is taken away, the pupils of both eyes enlarge equally. This is called the consensual light reflex. ● Papilledema: swelling of the optic nerve due to increased intracranial pressure; No early symptoms, visual acuity and pupillary response may be normal ○ seconds-long graying out of vision, flickering, or blurred or double vision may occur ○ Ophthalmoscopic examination reveals engorged and tortuous retinal veins, a hyperemic and swollen optic disk (optic nerve head), and retinal hemorrhages around the disk but not into the retinal periphery. ● Ocular mobility: The Hirschberg test ( corneal light reflex) evaluates extra ocular muscle function by projecting a small light source onto the cornea of the eye with the child looking straight ahead. A normal test reveals the reflected light as a small white dot symmetrically located in the same position of each eye). The cover-uncover test and the alternating cover test should be performed with the child fixating straight ahead, first on a near point object and then on a far point object about 20 feet away (Fig. 29-3). Any orbital movement is an indication of misalignment. ● Symptoms or indications of eye dysfunction or disease: 1. Older children may report visual loss or change in vision, such as blurring, diplopia, spots, and halos. Younger children may be observed to have problems with fixing or focusing (holding objects up close to see), tracking, squinting, head tilt, eye-hand coordination, grasp, gait, balance, behavior, and changes in the ability to maintain eye contact; eyelid droop 2. Photophobia may present as irritability, shielding, or rubbing of the eyes 3. Swollen eyelids, pruritus, excessive tearing or discharge, erythema, burning, eye fatigue, strabismus 4. Constant blinking, chronic bulbar conjunctival injection 76. Organisms for Conjunctivitis & Otitis Media ● Pathogens for conjunctivitis include H. influenzae, Streptococcus pneumoniae, and Moraxella with both gram-negative and gram-positive organisms implicated (Types of conjunctivitis, Table 29-6 in textbook) Type Incidence/Etiology Clinical Findings Diagnosis Management* Ophthalmia neonatorum Neonates: Chlamydia trachomatis, Staphylococcus aureus, Neisseria gonorrhoeae, HSV (silver nitrate reaction occurs in 10% of neonates) Erythema, chemosis, purulent exudate with N. gonorrhoeae; clear to mucoid exudate with chlamydia Culture (ELISA, PCR), Gram stain, R/O N. gonorrhoeae,chlamydia Saline irrigation to eyes until exudate gone; follow with erythromycin ointment For N. gonorrhoeae:ceftriaxone or IM or IV For chlamydia: erythromycin or possibly azithromycin PO For HSV: antivirals IV or PO Bacterial conjunctivitis In neonates 5 to 14 days old, preschoolers, and sexually active teens: Haemophilus influenzae(nontypeable), Streptococcus pneumoniae, S. aureus, N. gonorrhoeae Erythema, chemosis, itching, burning, mucopurulent exudate, matter in eyelashes; ↑ in winter Cultures (required in neonate); Gram stain (optional); chocolate agar (for N. gonorrhoeae) R/O pharyngitis, N. gonorrhoeae, AOM, URI, seborrhea Neonates: Erythromycin 0.5% ophthalmic ointment ≥1 year old: Fourth-generation fluoroquinolone For concurrent AOM: Treat accordingly for AOM Warm soaks to eyes three times a day until clear No sharing towels, pillows No school until treatment begins Chronic bacterial conjunctivitis (unresponsive conjunctivitis previously treated as bacterial in etiology) School-age children and teens: Bacteria, viruses, C. trachomatis Same as above; foreign body sensation Cultures, Gram stain; R/O dacryostenosis, blepharitis, corneal ulcers, trachoma Depends on prior treatment, laboratory results, and differential diagnoses Review compliance and prior drug choices of conjunctivitis treatment Consult with ophthalmologist Inclusion conjunctivitis Neonates 5 to 14 days old and sexually active teens: C. trachomatis Erythema, chemosis, clear or mucoid exudate, palpebral follicles Cultures (ELISA, PCR), R/O sexual activity Neonates: Erythromycin or azithromycin PO Adolescents: Doxycycline, azithromycin, EES, erythromycin base, levofloxacin PO Viral conjunctivitis Adenovirus 3, 4, 7; HSV, herpes zoster, varicella Erythema, chemosis, tearing (bilateral); HSV and herpes zoster: unilateral with photophobia, fever; zoster: nose lesion; spring and fall Cultures, R/O corneal infiltration Refer to ophthalmologist if HSV or photophobia present Cool compresses three or four times a day Allergic and vernal conjunctivitis Atopy sufferers, seasonal Stringy, mucoid exudate, swollen eyelids and conjunctivae, itching (key finding), tearing, palpebral follicles, headache, rhinitis Eosinophils in conjunctival scrapings Naphazoline/pheniramine, naphazoline/antazoline ophthalmic solution (see text) Mast cell stabilizer (see text) Refer to allergist if needed ● Pathogens for otitis media include S. pneumoniae, nontypeable Haemophilus influenzae, Moraxella catarrhalis, and S pyogenes (group A streptococci). S. pneumoniae continues to be the most common bacteria responsible for AOM. Section 15 Liz Garza 77. Fluorescein stain 1st choice (this question gets missed a lot) Liz Garza Corneal Abrasion- physical findings: epithelial injury visible with the use of fluorescein stain and cobalt blue light (Wood’s lamp). The dye stains the area of the missing epithelium (the abraded area). Foreign body eye injury- foreign body in the eye. Physical findings: positive fluorescein examination if corneal abrasion if present. (pediatric nurse practitioner certification pg. 93). ○ Fluorescein examination — A working diagnosis of corneal abrasion should be made based upon the history, physical findings, and lack of signs of other disorders. Fluorescein examination should be performed to confirm the diagnosis only after completion of visual acuity measurement and the penlight and fundus examination. Earlier instillation of dye may interfere with visual acuity measurement and visualization of the anterior segment and fundus. ○ The fluorescein examination is performed as follows. The lower lid is pulled down, and a fluorescein impregnated paper strip is moistened with saline or topical anesthetic, allowing a drop to run off into the eye or the inferior cul-de-sac. When the patient blinks, the dye is distributed over the ocular surface. Alternatively, the strip is gently swiped against the bulbar or tarsal conjunctiva below the cornea and the patient is allowed to blink to distribute the fluorescein. 78. Management of otitis externa Liz Garza ● Withdraw any foreign bodies or debris from external canal by gentle irrigation with warm water or normal saline; do not irrigate if perforated TM is suspected. ● Topical antibiotic otic drops are sufficient: those containing combinations of neomycin, polymyxin, and fluoroquinolone are effective (ofloxacin is safe with PE tubes or TM perforation); the addition of hydrocortisone (Cipro HC) is helpful when canal is edematous. ● If significant swelling, insert cotton wick saturated with antibiotic solution for first 24-48 hrs. ● Systemic analgesic often required for severe pain. ● Reexamine 1-2 weeks for evaluation of TM and removal of any debris. ● Systemic antibiotics when OE accompanied by fever, lymphadenitis, facial cellulitis. ● Refer to ENT if no improvement after 2-3 days; sooner if worsening. ● (pediatric nurse practitioner certification pg. 95). 79. Teaching otitis externa Liz Garza ● Avoid swimming and getting ear wet during the acute phase. ● Prevention: instillation of white vinegar and rubbing alcohol (50/50) in both ear canals after swimming. ● Avoid water in canals, vigourse cleaning, scratching, or prolonged use of cerumenolytic agents. ● Properly fitted ear plugs may be helpful. ● (pediatric nurse practitioner certification pg. 95). 80. Otitis media stepwise treatment. What are the 1st, 2nd, 3rd line treatments? Liz Garza Antibiotics: ● First line high dose amoxicillin (80-90 mg/kg/dy) or amoxicillin-clavulanate. If allergic, cefdinir, cefuroxime, cefpodoxime, and ceftriaxone are acceptable. ● Second line for treatment failures are amoxicillin-clavulanate with clindamycin as an alternative treatment. ● Use tympanocentesis sparingly, only used for retreatment failures with severe symptoms (performed by ENT). ● (pediatric e to environmental allergens Signs & Symptoms: nasal pruritus, sneezing, rhinorrhea, and nasal congestion. Frequently there is associated palate, throat, ear, and eye itching as well as eye redness, puffiness, and watery discharge. Boggy, white nasal mucosa Differential Diagnosis: nonallergic rhinitis, acute/chronic sinusitis, viral rhinosinusitis Treatment: Second-generation oral antihistamines are preferred to first-generation agents because they cause less or no sedation. Cetirizine has been found to be particularly effective in allergic rhinitis. Sedation is possible with cetirizine and levocetirizine; unlikely with loratadine, desloratadine, and fexofenadine; and likely with chlorpheniramine and diphenhydramine. Avoidance of the allergen. Leukotriene receptor antagonists are an alternative to antihistamines, especially in those who also have mild persistent asthma. Although effective for nasal congestion, they are less effective than antihistamines for rhinorrhea, sneezing, and itching. 83. Organisms that cause hand foot and mouth Hand, foot, and mouth disease is caused by viruses that belong to the Enterovirus genus (group), which includes polioviruses, coxsackieviruses, echoviruses, and other enteroviruses: ● Coxsackievirus A16 ● Glomerulonephritis ○ Acute glomerulonephritis is associated with group A Streptococcus (GAS) infection of the pharynx or skin 1 to 3 weeks after infection. Treating the underlying disorder and managing HTN, hyperlipidemia, and proteinuria is the mainstay of therapy. Most individuals recover without long-term renal impairment. Some patients may eventually need dialysis or transplant. Antibiotics probably do not prevent glomerulonephritis, but we cannot be certain. 85. Vaccines that have decreased what diseases (Items 3, 6, 46, and 85 in this study guide address vaccines) ● Smallpox ● Hib - epiglottitis ● IPV - polio ● DTaP - tetanus, diphtheria, pertussis ● HepB ● HepA ● MMR - measles, mumps, rubella ● Varicella - chicken pox ● Prevnar ● Meningococcal 86. Epligotitis s/s ● Nonvaccination with Hib vaccine ● Sore throat ● Dysphagia ● Difficulty in controlling secretions ● Toxic appearance - especially in children ● Acute distress - especially in children ● Fever - especially in children ● Tripod position ● Difficulty breathing ● Decreased oral intake ● Muffled voice ● Stridor ● Irritability ● Drooling Section 17 Monica Hevron 87. Requires hospitalizations: epilglotitis, retropharyngeal abscess, cervical adenitis, orbital cellulitis *Epiglottitis (815-817) requires hospitalization because of the risk of sudden airway occlusion *Retropharyngeal abcess is a collection of pus in the tissues in the back of the throat. It can be a life-threatening medical condition *Cervical adenitis is an infection of a lymph node in the neck. Lymph nodes are part of the immune system and help fight infections. Another term for this infection is lymphadenitis (No hospitalization) *orbital cellulitis iis an infection of the soft tissues within the eye socket. It is a serious condition that, without treatment, can lead to permanent vision loss and life-threatening complications. 88. Normal visual acuity at what age p.704 Visual acuity is developed by 12 months 89. Esotropia, exotropia, Nystagmus, strabismus Esotropia is when one or both eyes turn inward exotropia is when one or both eyes turn outward Strabismus is : “lazy eye” p. 715. Nystagmus is involuntary rhythmic movements of the eye p. 716 90. How to remove foreign body in ear ○ Must have adequate visualization and a cooperative patient. If it is not able to be removed on the first attempt, refer to ENT ○ Can try straightening the ear, pulling on the pinna and shaking the patient’s head insects: suffocate with mineral oil and send to ENT iron, nickel or cobalt can try magnet round or breakable objects: a wire loop, curette or right angle hook may be used- advance past the object and retract. soft, irregularly shaped objects: bayonet forceps, alligator forceps, curved hook spherical objects should be referred to ENT Disc batteries must be removed emergently. 91. Teeth grinding and what to look for Also called bruxism common during sleep for 12 and under, during waking hours 13 and older parent reports grinding primary teeth show wear jaw muscle. fatigue **Look for: Underlying stressors and secondhand smoke exposure, OSA, enlarged tonsils, could be an adverse effect of antipsychotics and antidepressants The main risk factors for sleep-related bruxism are comorbid sleep disorders, especially obstructive sleep apnea (OSA) and parasomnias; anxiety and other psychiatric and neurologic disorders; and certain medications and substances (table 1). In a population-based study of over 13,000 individuals 15 years of age and older who were assessed for sleep-related bruxism and other comorbidities by telephone-based questionnaire, the following factors were associated with an increased risk of sleep-related bruxism [5]: ●OSA (odds ratio [OR] 1.8) ●Heavy alcohol use (OR 1.8) ●Loud snoring (OR 1.4) ●Caffeine intake (OR 1.4) ●Smoking (OR 1.4) ●Anxiety (OR 1.3) ●Highly stressful life circumstances (OR 1.3) Section 18 Luis Sanchez 92. How long is head circumference routinely measures: birth to 3 years at routine wellness visits 93. Snellen test results are and be able to explain Visual acuity is usually measured with a Snellen chart. ... "Normal" vision is 20/20. This means that the test subject sees the same line of letters at 20 feet that person with normal vision sees at 20 feet. 20/40 vision means that the test subject sees at 20 feet what a person with normal vision sees at 40 feet. 94. Hyphema and what to do A hyphema is a pooling or collection of blood inside the anterior chamber of the eye (the space between the cornea and the iris). The blood may cover most or all of the iris and the pupil, blocking vision partially or completely. A hyphema is usually painful. If left untreated, it can cause permanent vision problems. Symptoms: visible blood in the front of the eye sensitivity to light pain blurry, clouded, or blocked vision blood might not be visible if the hyphema is small Send referral to opthamologist WHILE WAITING ON OPTHAMOLOGIST VISIT: The following general measures are recommended in patients with hyphema and comprise appropriate initial care (table 1) [2-4]: Eye shield – An eye shield should be placed over the affected eye as soon as possible and subsequently removed only as required for examination and imaging. ● Bed rest and dim lighting – Limitation of activity to bed rest with bathroom privileges should occur until initial evaluation is complete. The patient should be placed in a dim, quiet room and should not read so that visual accommodation does not further stress injured blood vessels. Elevate the head of the bed – Elevation of the head to 30 degrees promotes inferior settling of blood in the anterior chamber away from the visual axis while maintaining arterial blood flow to the eye relative to the fully erect position [2,3]. Thirty degree elevation of the head also improves diagnosis of secondary hemorrhage and aids in clearance of the hyphema. ● Control pain – Pain control improves patient comfort and facilitates eye examination [3]. Topical analgesia with proparacaine or tetracaine may be applied temporarily in patients without an open globe; long term use may cause corneal toxicity. Dilating eye drops, discussed below, may also provide some pain relief. Nonsteroidal antiinflammatory agents (NSAIDS) are discouraged because of their platelet inhibiting properties. For patients in whom topical analgesia is inadequate, the clinician may consider oral or intravenous opioids. Hydrocodone or oxycodone in combination with acetaminophen is preferred to codeine because they are less prone to cause nausea and vomiting. Intravenous therapy with morphine or fentanyl may be needed in patients with large hyphemas (grade III to IV (figure 1)) or associated traumatic injury. ● Treat nausea and prevent vomiting – Patients with nausea or vomiting require treatment with antiemetics, such as ondansetron, to prevent sudden increase in intraocular pressure caused by emesis [3]. ● Dilating eye drops – For patients without narrow angle glaucoma, Cycloplegia, topically with cyclopentolate one percent (eg, Cyclogyl, Cylate, or Ocu-Pentolate), one drop, or scopolamine 0.25 percent one drop, often provides pain relief and allows for optimal examination of the posterior segment [2-4]. Dilating eye drops are contraindicated in patients with suspected open globe injury or narrow angle glaucoma [4]. ● Correct coagulopathy – Patients with bleeding tendency, such as hemophilia, von Willebrand disease, or thrombocytopenia should receive appropriate treatment to restore clotting capability [5,6]. Per UpToDate 95. Bacterial, viral, allergic conjunctivitis discharge (Valentina N). Conjunctivitis is a common patient complaint. It is the most likely diagnosis in a patient with a red eye and discharge. Acute conjunctivitis is usually a benign, self-limited condition or one that is easily treated. When making a diagnosis of acute conjunctivitis, one needs to make certain that sight-threatening and pathologic processes have been ruled out. In contrast to acute conjunctivitis, these entities, such as acute angle-closure glaucoma, iritis, and infectious keratitis, must be managed by ophthalmologists and will not be discussed here. Acute conjunctivitis can be classified as infectious or noninfectious and further divided into four main types: ●Infectious (Bacterial - Viral) ●Noninfectious (Allergic - Nonallergic) Studies suggest that the majority of cases in children are bacterial the prevalence of bacterial conjunctivitis seen in studies presumably reflects the greater likelihood that patients with copious discharge will present for care. Clinical experience suggests that most infectious conjunctivitis is viral in both adults and children. Bacterial conjunctivitis — Bacterial conjunctivitis is commonly caused by Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. S. aureus infection is common in adults; the other pathogens are more common in children. Bacterial conjunctivitis is spread by direct contact with the patient and his or her secretions or with contaminated objects and surfaces. It is highly contagious. The purulent discharge continues throughout the day. The discharge is thick and globular; it may be yellow, white, or green. The appearance differs from that of viral or allergic conjunctivitis, which often present with a mostly watery discharge during the day, with a scanty, stringy component that is mucus rather than pus. On examination, patients with bacterial conjunctivitis typically have purulent discharge at the lid margins and in the corners of the eye. More purulent discharge appears within minutes of wiping the lids. This contrasts with patients with viral or allergic conjunctivitis, in whom the eyes appear watery; there may be mucus present on close inspection of the tear film or if one pulls down the lower lid, but pus does not appear spontaneously and continuously at the lid margin and in the corners of the eye. Hyperacute bacterial conjunctivitis — Neisseria species, particularly N. gonorrhoeae, can cause a hyperacute bacterial conjunctivitis that is severe and sight-threatening, requiring immediate ophthalmologic referral. The organism is usually transmitted from the genitalia to the hands and then to the eyes. Concurrent urethritis is typically present. The eye infection is characterized by a profuse purulent discharge present within 12 hours of inoculation, the amount of discharge is striking. Other symptoms are rapidly progressive and include redness, irritation, and tenderness to palpation. There is typically marked chemosis, lid swelling, and tender preauricular adenopathy. Gram-negative diplococci can be identified on Gram stain of the discharge. These patients require hospitalization for systemic and topical therapy and for monitoring of the ocular component. Keratitis and perforation can occur. Viral conjunctivitis — Viral conjunctivitis is typically caused by adenovirus, with many serotypes implicated. The conjunctivitis may be part of a viral prodrome followed by adenopathy, fever, pharyngitis, and upper respiratory tract infection, or the eye infection may be the only manifestation of the disease. Viral conjunctivitis is highly contagious; it is spread by direct contact with the patient and his or her secretions or with contaminated objects and surfaces. Viral conjunctivitis typically presents as injection; watery or mucoserous discharge and a burning, sandy, or gritty feeling in one eye. Patients may report "pus" in the eye, but on further questioning they have morning crusting followed by watery discharge, perhaps with some scanty mucus throughout the day. The second eye usually becomes involved within 24 to 48 hours, although unilateral signs and symptoms do not rule out a viral process. Patients often believe that they have a bacterial conjunctivitis that has spread to the fellow eye; On examination there is typically only mucoid discharge if one pulls down the lower lid or looks very closely in the corner of the eye. Usually there is profuse tearing rather than discharge. The tarsal conjunctiva may have a follicular or "bumpy" appearance. There may be an enlarged and tender preauricular node. Viral conjunctivitis is a self-limited process. The clinical course parallels that of the common cold. While recovery can begin with days, the symptoms frequently get worse for the first three to five days, with very gradual resolution over the following one to two weeks for a total course of two to three weeks. Just as a patient with a cold can have morning coughing and nasal congestion or discharge two weeks after symptoms first arise, patients with viral conjunctivitis may have morning crusting two weeks after the initial symptoms, although the daytime redness, irritation, and tearing should be much improved. Allergic conjunctivitis — Allergic conjunctivitis is caused by airborne allergens contacting the eye that, with specific immunoglobulin E (IgE) and the release of chemical mediators including histamine, eosinophil chemotactic factors, and platelet-activating factor, among others. It typically presents as bilateral redness, watery discharge, and itching. Itching is the cardinal symptom of allergy, distinguishing it from a viral etiology, which is more typically described as grittiness, burning, or irritation. Eye rubbing can worsen symptoms. Patients with allergic conjunctivitis often have a history of atopy, seasonal allergy, or specific allergy (eg, to cats). Similar to viral conjunctivitis, allergic conjunctivitis causes diffuse injection with a follicular appearance to the tarsal conjunctiva and profuse watery or mucoserous discharge. There may be morning crusting. It is the complaint of itching and the history of allergy or hay fever as well as a recent exposure that allows the distinction between allergic and viral conjunctivitis; the clinical findings are the same. In some cases of allergic conjunctivitis, there is marked chemosis (conjunctival edema); in extreme instances, there can be bullous chemosis, in which the bulging, edematous conjunctiva extends forward beyond the lid margins. Bullous chemosis is most commonly seen in patients with extreme hypersensitivity to cats. A detailed discussion of allergic disease is presented separately. 96. Antibiotics with acute otitis media (Brandi Thompson) ○ Antibiotics are prescribed in a stepwise fashion beginning with a first-line antibiotic. A lack of improvement in the patient's condition may require a change to a second- or third-line agent. ○ Primary Options i. amoxicillin : children: 80-100 mg/kg/day orally given in divided doses every 12 hours for 10 days ii. amoxicillin/clavulanate : children >3 months of age: 80-100 mg/kg/day orally given in divided doses every 12 hours for 10 days more ○ Secondary Options i. cefdinir : children >6 months of age: 14 mg/kg/day for 10 days ii. cefuroxime axetil : children: 30 mg/kg/day orally given in divided doses every 12 hours for 10 days ○ Tertiary Options i. azithromycin : children ≥6 months of age: 10 mg/kg/day orally (immediate-release) on the first day, followed by 5 mg/kg/day for 4 days; or 10 mg/kg/day orally (immediate-release) for 3 days; or 30 mg/kg/day orally (immediate-release) as a single dose; or 60 mg/kg/day orally (extended-release) as a single dose ii. ceftriaxone : children: 50 mg/kg/day intramuscularly/intravenously for 3 days 97. Method to remove ear wax at various ages ○ Symptoms of Earwax Buildup i. Too much earwax can cause rubbing of the ear or poking in the canal. ii. A piece of earwax can become dry and hard in the ear canal. This creates a feeling that an object is in the ear. iii. Complete blockage (plugging) of the ear canal by wax causes more symptoms. These include decreased or muffled hearing. iv. A large piece of earwax may be seen inside the ear canal. ○ Causes of Earwax Buildup i. Cotton Swabs. Earwax buildup is usually from using cotton swabs. They push the wax back in and pack it down. ii. Fingers. A few children (perhaps 5%) normally produce more wax than others. It usually will come out if it's not pushed back by fingers. iii. Ear Plugs. Wearing ear plugs of any type can also push wax back. ○ Age 6 Years and Older - Ear Canal Flushing with Water: Under age 6, use only if advised by your child's doctor. i. Buy a soft rubber ear syringe or bulb from the pharmacy. No prescription is needed. ii. Have your child lean over the sink. Reason: To catch the water. iii. Use lukewarm water (body temperature). Reason: To prevent dizziness. iv. Gently squirt the water into the ear canal. Then tilt your child's head and let the water run out. You may need to do this several (3-4) times. v. If the earwax does not seem to be coming out, tilt the head. Then, flush it with the head tilted. Have the ear with the wax in it facing downward. Gravity will help the water wash it out (the waterfall effect). vi. Endpoint: Flush until the water that comes out is clear of wax. Also, the ear canal should be open when you look in with a light. vii. Afterwards dry the ear thoroughly. You can do this by putting a drop of rubbing alcohol in the ear canal. Or you can set a hair dryer on low. Hold it a foot away from the ear for 10 seconds. ○ Ear Drops - Use for 4 Days to Soften the Earwax: i. If the earwax is hard, soften it before flushing the ear canal. Use ear drops to break up the earwax. ii. Homemade ear drops: 15% baking soda solution. Make it by adding ¼ teaspoon (1.25 mL) of baking soda to 2 teaspoons (10 mL) of water. iii. Other option for homemade ear drops: hydrogen peroxide and water solution. Mix equal parts of each. iv. Drug store option: Earwax removal ear drops (such as Debrox). No prescription is needed. v. Use 5 drops in affected ear, 2 times daily, for 4 days. ○ How to Put in Ear Drops: i. Lie on the side with blocked ear upward. ii. Place 5 drops into the ear canal. Pull the ear down and back to open the ear canal iii. Keep drops in ear for 10 minutes by continuing to lie down. iv. Then lie with the blocked side down. Let the ear drops run out onto some tissue. v. Use twice daily for up to four days. vi. Then flushing should be able to get everything out. 98. s/s of buccal tumors, bennars apthay, epstein pearls ○ Epstein pearls- small white or yellow-tinted bump on the gum line or roof of the mouth. They do not cause and symptoms. They are common to babies who are born to older mothers, past the due dates, and has higher birth weights. Keratin entrapment within the soft and hard palates causes Epstein pearls. ○ Buccal Tumors (cancer of oral cavity, lining of the cheeks and back of the lips)- white or red lump in the mouth that does not go away for 2 weeks, red raised patch in the mouth that bleeds easily, lump or thickening in the mouth, pain increases when eating or drinking, soreness or feeling that something is caught in the throat, difficult moving the jaw or tongue, hoarseness, numbness of the tongue or areas of the mouth ○ Bednar's aphthae is a type of oral ulceration (mouth ulcers) which occurs in infants. The lesions are located on the palate and are caused by trauma. Bednar's aphthae are small, shallow ulcers on the edge of newborns' palates and are typically caused by traumatic action of a bottle nipple or even the mother's breast during feeding9). 99. Dx, s/s of strep throat, viral tonsillitis, epiglottitis, diphtheria ○ Strep throat- streptococcal pharyngitis bacterial infection of throat. Signs and symptoms fever of 101 or higher, red swollen tonsils, white patches in the throat, tiny red spots on the roof of the mouth, appetite loss, upset stomach, headache, nausea, vomiting, rash. Rapid Strep test is used for diagnosis or throat culture. ○ Viral Tonsillitis- acute or chronic inflammation of the tonsils. Sudden onset of sore throat, fever, malaise, cough, headache, myalgias, and fatigue. Patients may also report rhinitis, conjunctivitis (adenovirus) congestions, cough with sputum production Clinical presentation indicated the diagnosis. Rapid antigen detection rest, antistreptolysin O titer test differential viral from bacterial. GAS infection indicated bacterial infection. ○ Epiglottitis- is an acute inflammation of the supraglottic region of the oropharynx. Characterized by inflammation and edema of the epiglottitis, vallecular, arytenoids, and aryepiglottic folds. Life-threatening because of potential laryngospasm and irrevocable loss of the airway. Cause by bacteria Haemophilus influenzae type B (Hib). Signs and symptoms dysphagia, fever, shortness of breath, leaning forward in effort to enhance air flow or sitting up. Other complications stridor, drooling, cough, respiratory distress and hoarseness. Triad position (leaning forward with hands braced on the knees). Definitive diagnosis of epiglottis is made by direct visualization via laryngoscopy with flexible fiberoptic scope. Sonography can be used noninvasive for emergent results. ○ Diphtheria- Diphtheria is an infection caused by the bacterium Corynebacterium diphtheriae. Bacteria that causes diphtheria can get into and attach to the lining of the respiratory system, which includes parts of the body that help you breathe. When this happens, the bacteria can produce a poison (toxin) that can cause: i. A thick, gray membrane covering your throat and tonsils ii. A sore throat and hoarseness iii. Swollen glands (enlarged lymph nodes) in your neck iv. Difficulty breathing or rapid breathing v. Nasal discharge vi. Drooling vii. Cyanosis viii. Fever and chills ix. Malaise x. The poison destroys healthy tissues in the respiratory system. Within two to three days, the dead tissue forms a thick, gray coating that can build up in the throat or nose. Medical experts call this thick gray coating a “pseudomembrane.” It can cover tissues in the nose, tonsils, voice box, and throat, making it very hard to breathe and swallow. 100. Sinusitis and the location of sinuses - Sinusitis is an inflammation or swelling of the tissue lining the sinuses. Healthy sinuses are filled with air. But when they become blocked and filled with fluid, germs can grow and cause an infection ○ Signs and symptoms- Facial pain or pressure, nasal congestion, runny nose, loss of smell, cough, fever, bad breath, fatigue, or dental pain, purulent nasal discharge, headache that becomes more intense when you bend or lean forward, postnasal drip. Pain of teeth or forehead are worse in the morning and when the patient bends forward from the waist. ○ The sinuses are in your forehead (frontal sinuses), inside your cheekbones (maxillary sinuses), and behind the nose (ethmoid and sphenoid sinuses) 101. What to do when a mother is being rough ○ As a healthcare provider it is our duty to protect the child and intervene if the mother is being rough. Parental insufficiency in action. It causes all kinds of impacts later, and it is preventable with a little focus, consciousness raising by educating parents about parenting and child development, love, and patience. Calling child protective services for further home investigation is required. Section 20 102. When to refer for stuttering: Children with any of the criteria listed below should be referred for a speech and language assessment: ● Concern by the parent, teacher, professional, or other caregiver about the child's speech or language ● Slowed or stagnant speech and language development ● Excessive drooling ● Difficulty sucking, chewing, or swallowing ● Difficulty coordinating movements of lips, tongue, and jaw ● No babbling by nine months ● No first words by 15 months ● No consistent words by 18 months ● No word combinations by 24 months ● Speech is difficult for parents to understand at 24 months ● Speech is difficult for strangers to understand at 36 months ● Dysfluencies (stutters) consist of more than tension-free whole-word repetitions ● Child is frustrated by communication difficulty ● Child is teased by peers for "talking funny" ● Child avoids talking situations ● Child acquires vocabulary and sentence structure but does not use language appropriately for communicative purposes ● Language is unusual or confused, or ideas are not expressed clearly ● Child cannot follow instructions without supplemental visual cues ● Loss of milestones ● Poor memory skills at five to six years 103. Diagnostic criteria for autism spectrum disorder: The diagnosis of ASD is made clinically in children who meet established diagnostic criteria for ASD based on history and observation of behavior. ○ DSM, Fifth edition criteria – According to the DSM, Fifth edition (DSM-5) criteria, a diagnosis of ASD requires ALL of the following: i. Persistent deficits in social communication and social interaction in multiple settings; demonstrated by deficits in all three of the following (either currently or by history): 1. Social-emotional reciprocity (eg, failure to produce mutually enjoyable and agreeable conversations or interactions because of a lack of mutual sharing of interests, lack of awareness or understanding of the thoughts or feelings of others) 2. Nonverbal communicative behaviors used for social interaction (eg, difficulty coordinating verbal communication with its nonverbal aspects [eye contact, facial expressions, gestures, body language, and/or prosody/tone of voice]) 3. Developing, maintaining, and understanding relationships (eg, difficulty adjusting behavior to social setting, lack of ability to show expected social behaviors, lack of interest in socializing, difficulty making friends even when interested in having friendships) ii. Restricted, repetitive patterns of behavior, interests, or activities; demonstrated by ≥2 of the following (either currently or by history): 1. Stereotyped or repetitive movements, use of objects, or speech (eg, stereotypies such as rocking, flapping, or spinning); echolalia (repeating parts of speech; repeating scripts from movies or prior conversations) 2. Insistence on sameness, unwavering adherence to routines, or ritualized patterns of verbal or nonverbal behavior (eg, ordering toys into a line) 3. Highly restricted, fixated interests that are abnormal in strength or focus (eg, preoccupation with certain objects [trains, vacuum cleaners, or parts of trains or vacuum cleaners]); perseverative interests (eg, excessive focus on a topic such as dinosaurs or natural disasters) 4. Increased or decreased response to sensory input or unusual interest in sensory aspects of the environment (eg, adverse response to particular sounds; apparent indifference to temperature; excessive touching/smelling of objects) iii. The symptoms must impair function (eg, social, academic, completing daily routines). iv. The symptoms must be present in the early developmental period. However, they may become apparent only after social demands exceed limited capacity; in later life, symptoms may be masked by learned strategies. v. The symptoms are not better explained by intellectual disability (formerly referred to as mental retardation) or global developmental delay. 104. Eating disorders with purging s/s 105. Obesity with treatment plan: info on pgs 185-190, 617-618 -children 2-18 years old with a BMI equal to or greater than the 95th percentile for their age and gender are considered obese. -children with a BMI of 30 are also considered obese. -Children with a BMI between the 85th and 94th percentile are considered overweight Causes: -Biological mechanisms: -stress -decreased activity -poor diet - Food addiction -Decreased Physical activity - Temperament -shorter attention span -psychosocial and environmental factors Treatment: -lifestyle changes -goal is to normalize weight so the child can “grow into” their weight -community changes -encouraging physical activity -encouraging breastfeeding - providing safe spaces to exercise - Medications -Primary treatment: lifestyle changes - Meds only when lifestyle changes fail or if extremely obese, with comorbidities -Orlistat- decreases fat absorption, children 12 and older OTC and c./rx *contraindicated in gallbladder disease, pregnancy, malabsorption syndromes and in sensitivity to the drug ** Side effects: fatty stool, GI upset: fiber supplements may help with these S/E [Show More]
Last updated: 1 year ago
Preview 1 out of 47 pages
Instant download
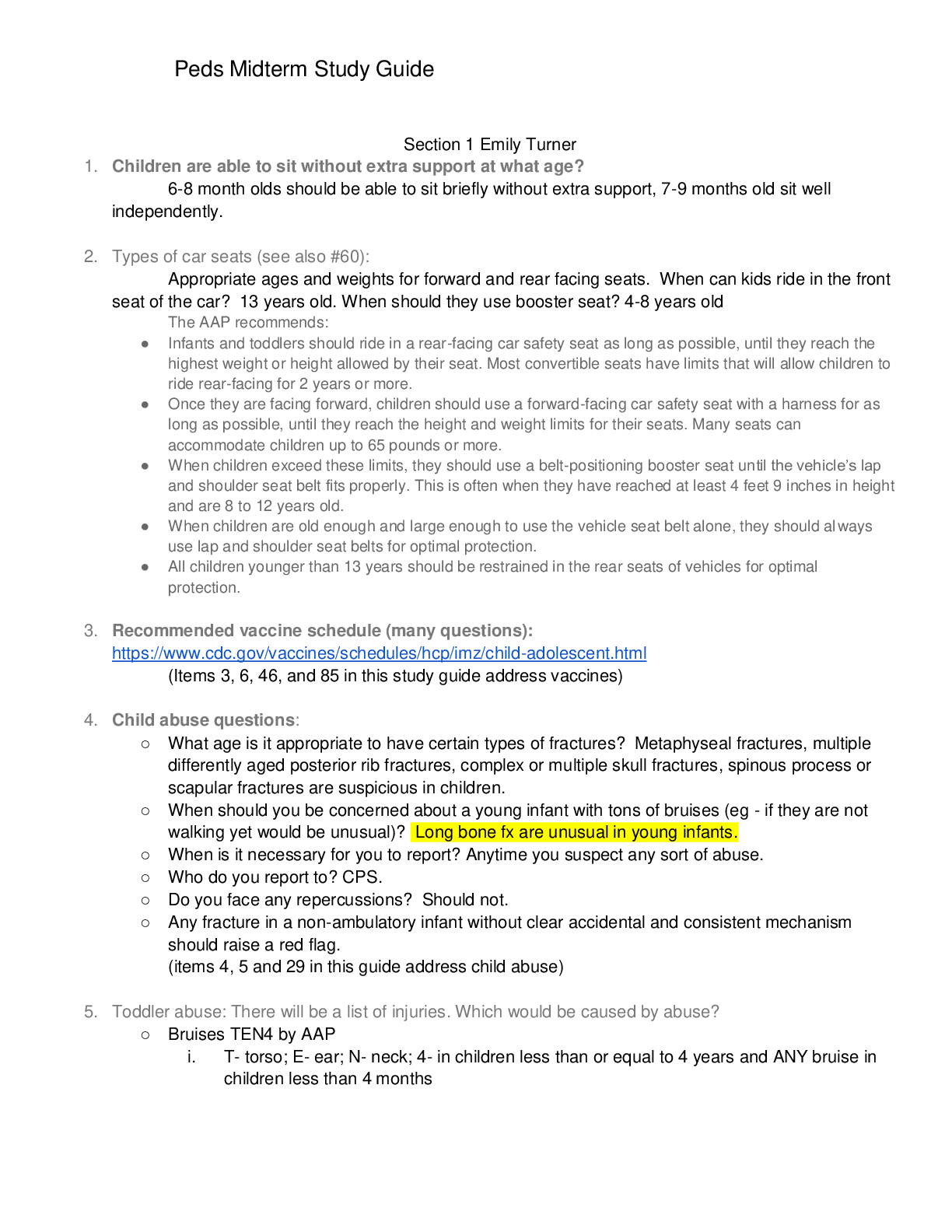
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 05, 2020
Number of pages
47
Written in
Additional information
This document has been written for:
Uploaded
Aug 05, 2020
Downloads
0
Views
57

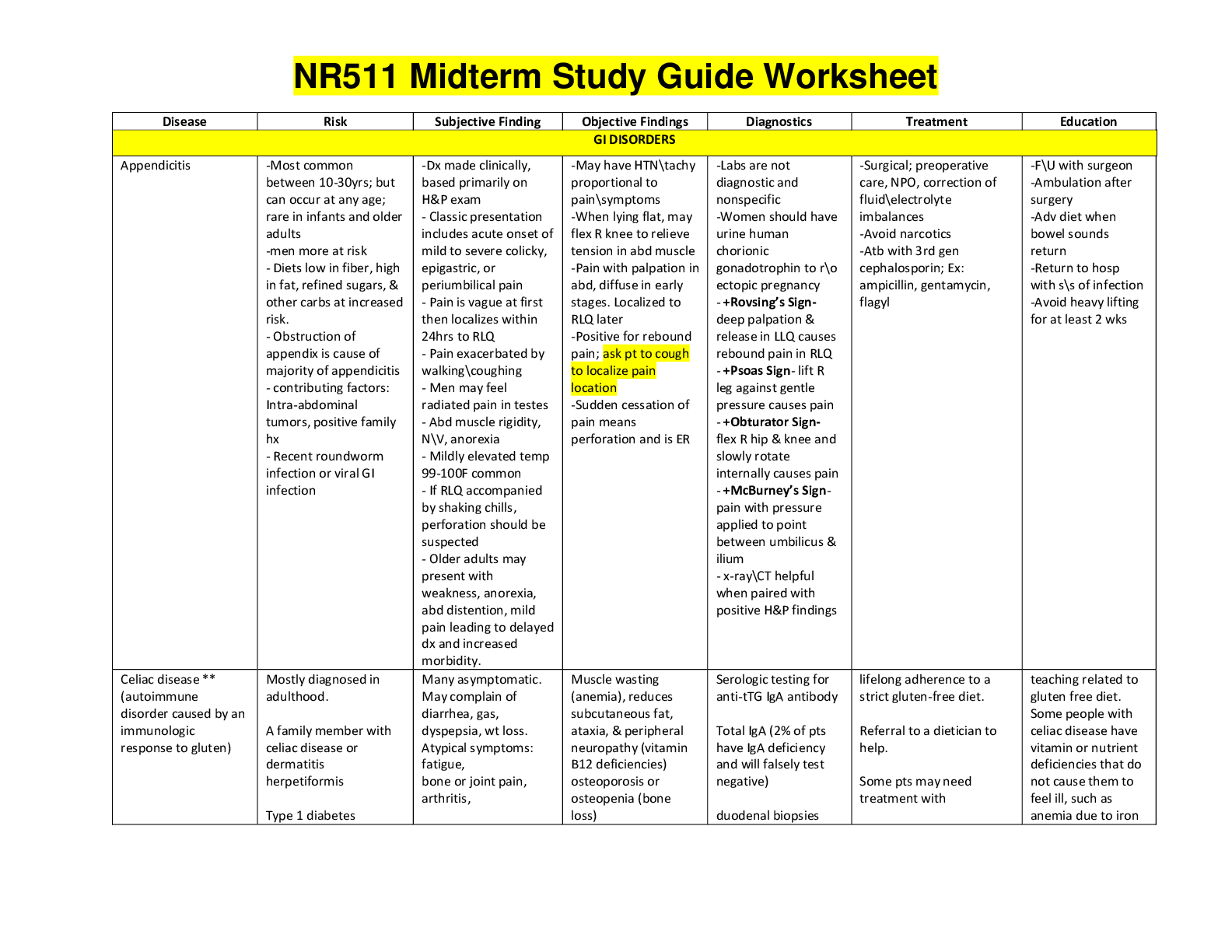
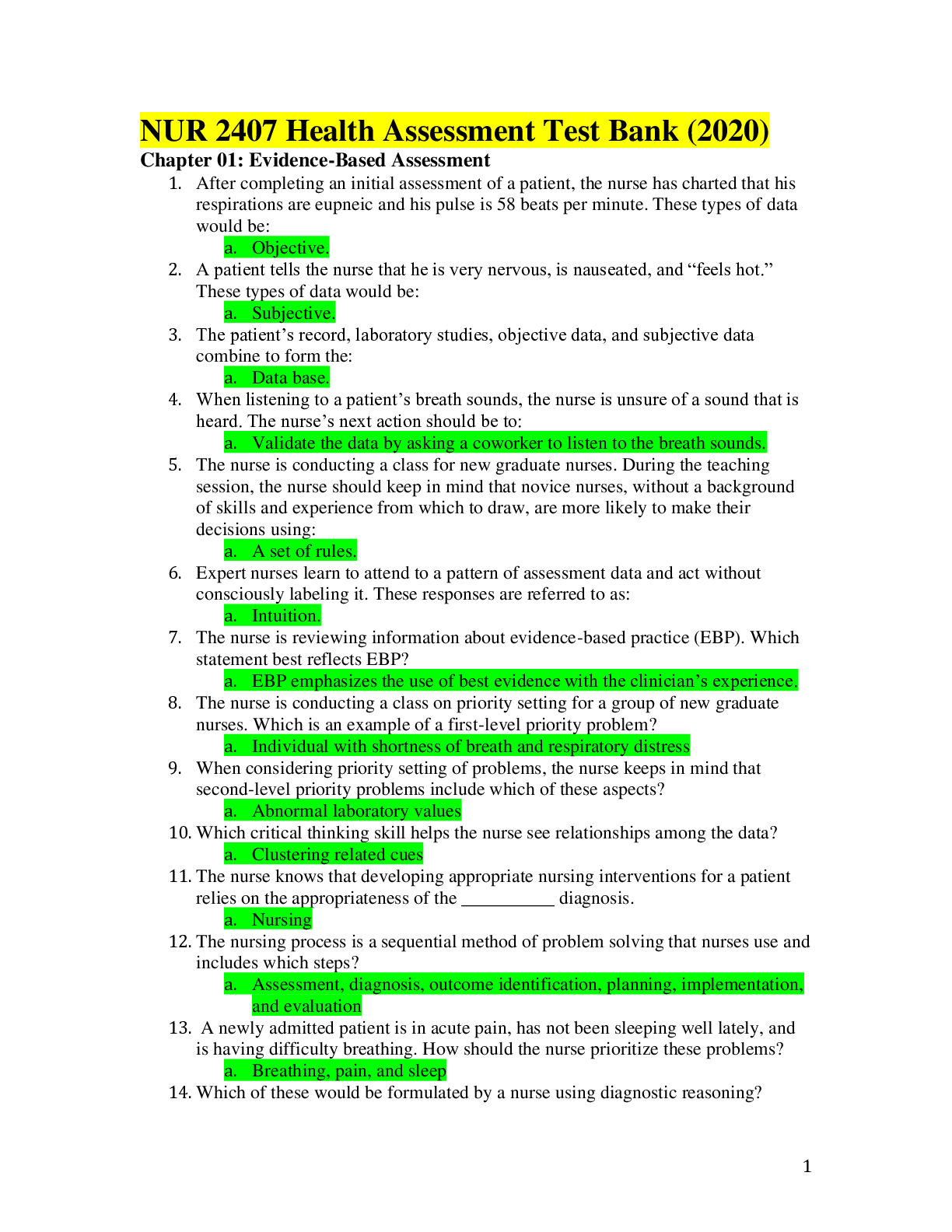
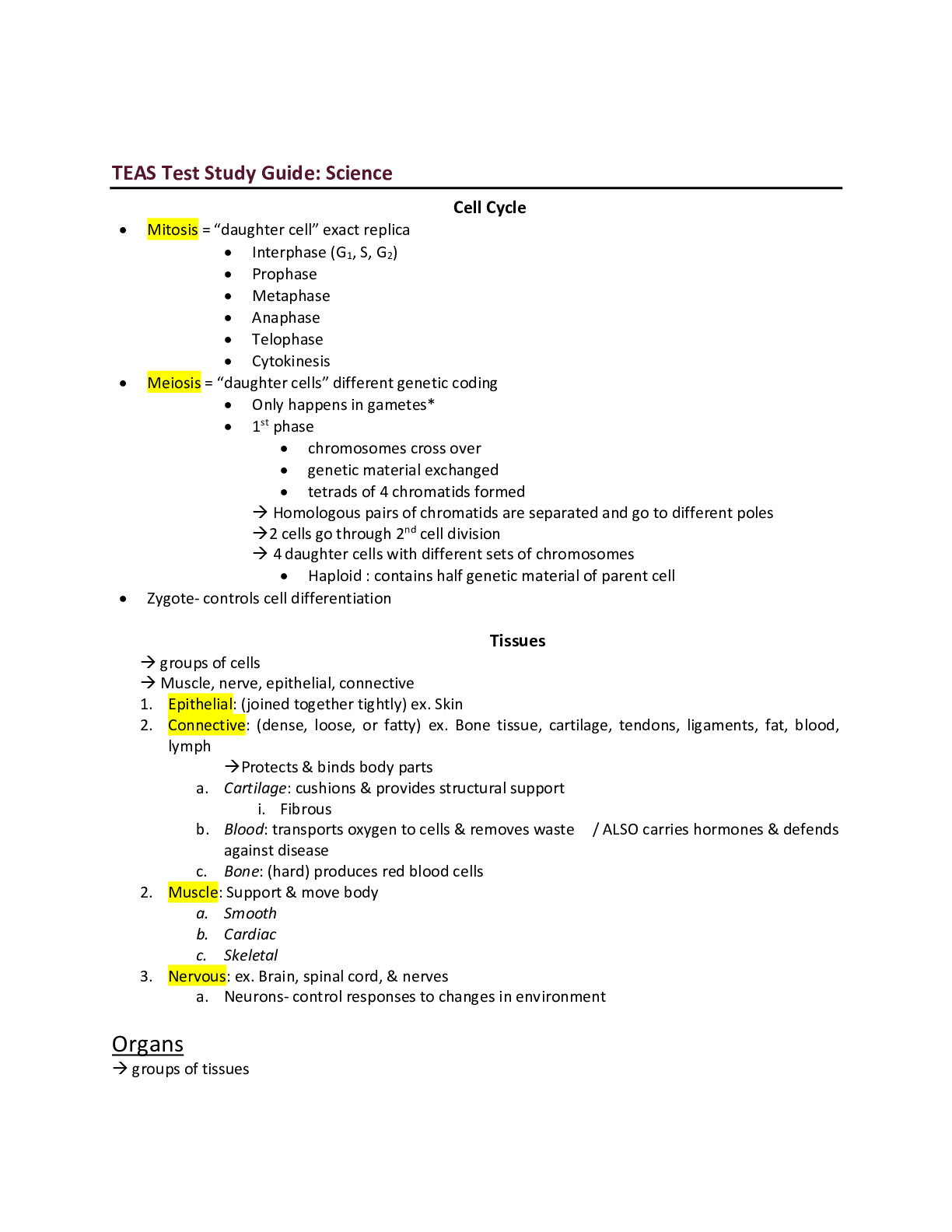
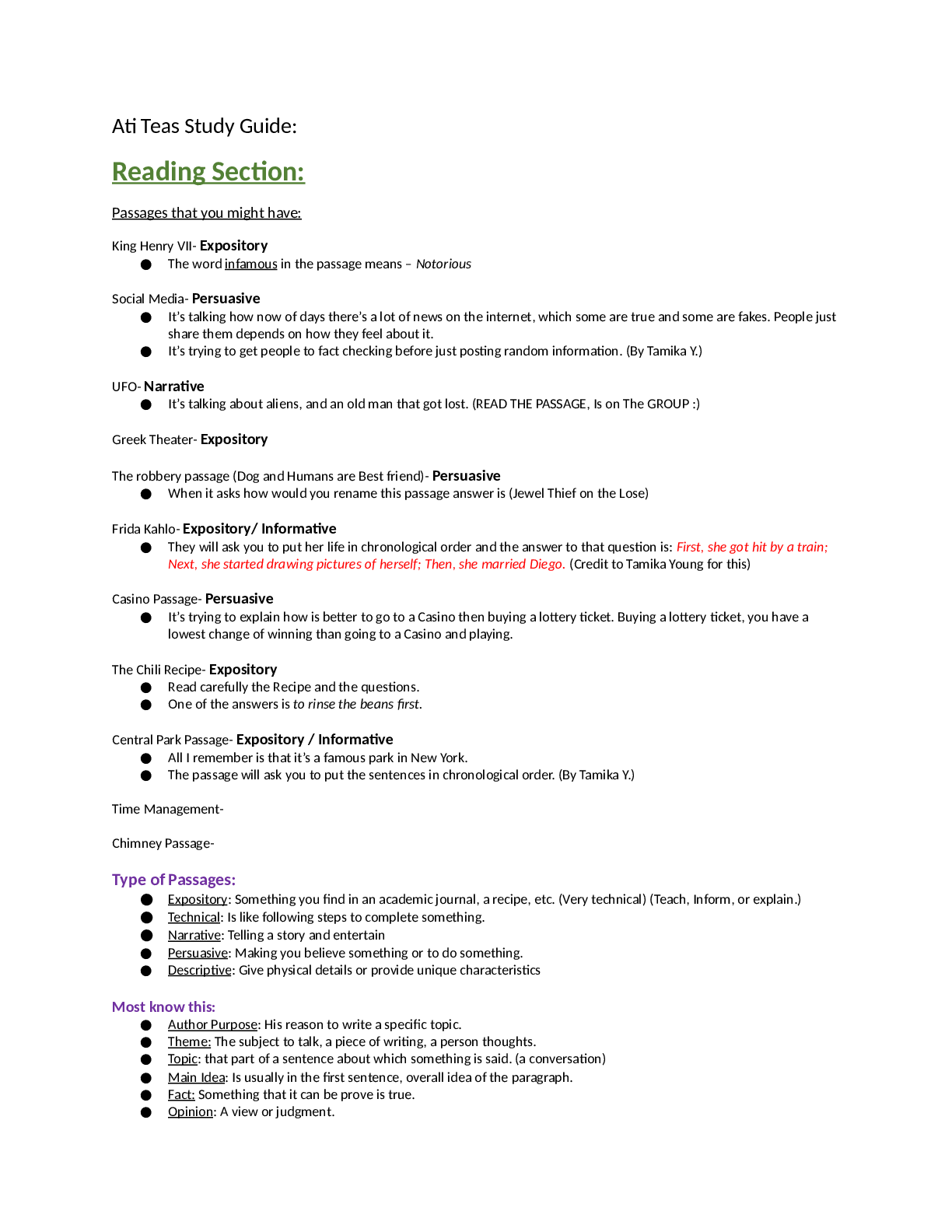

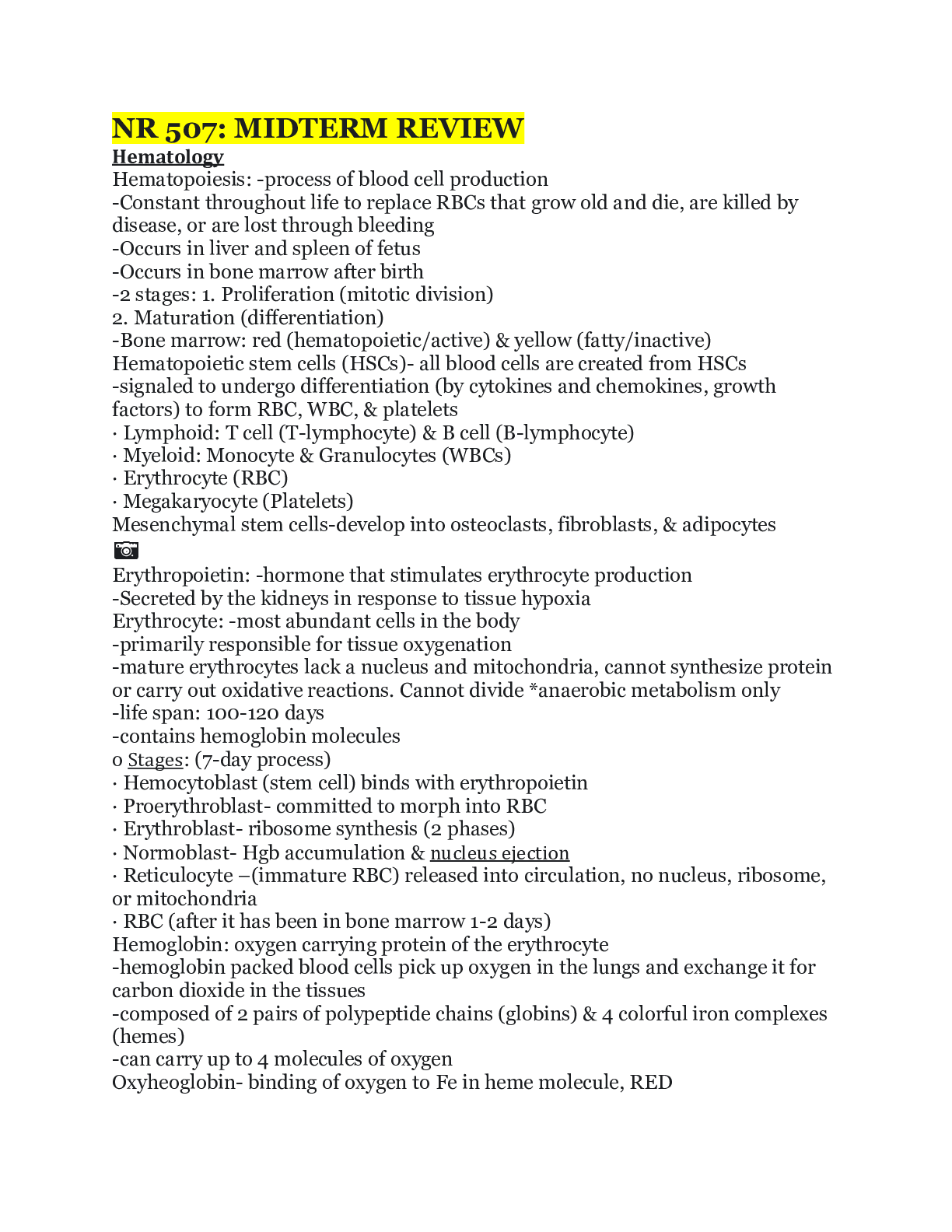
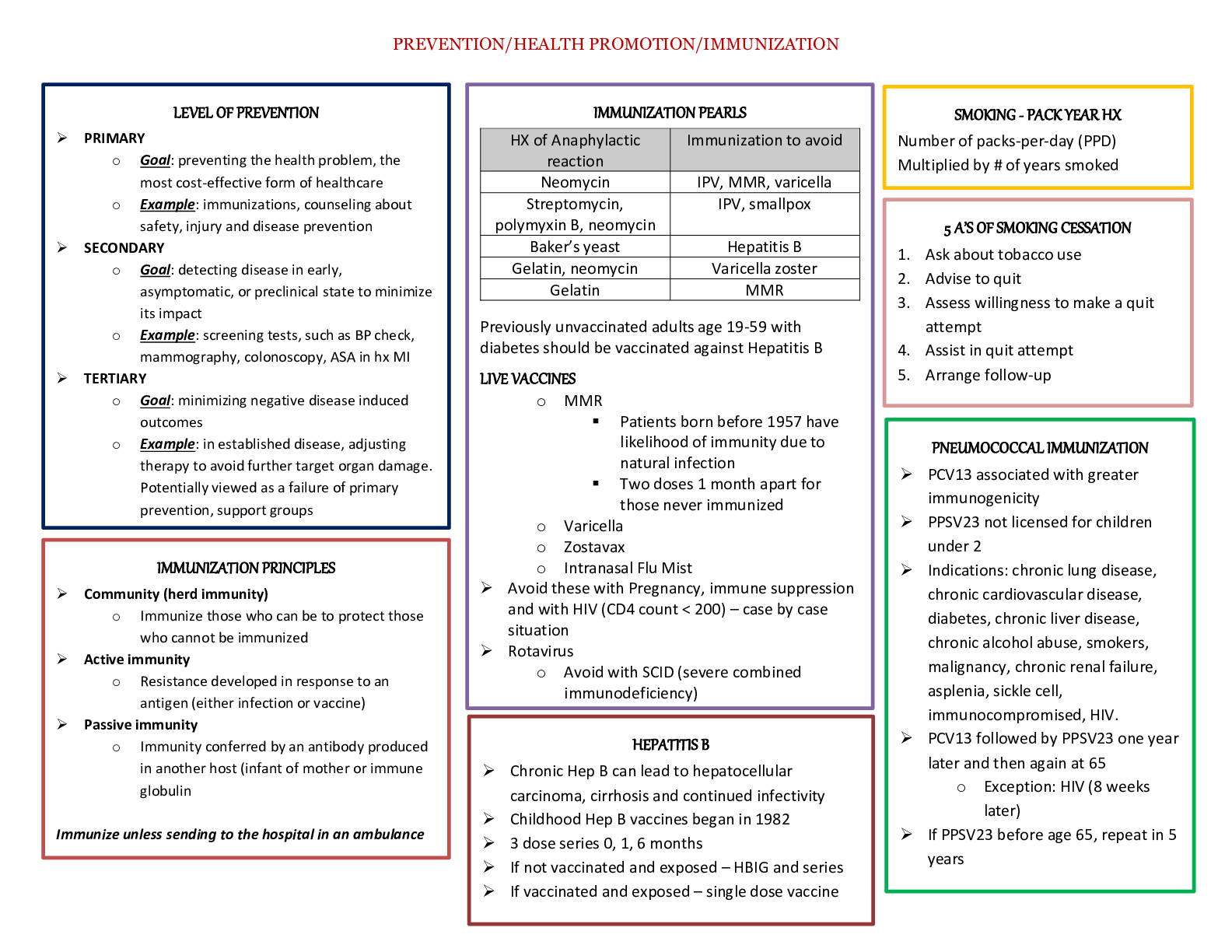
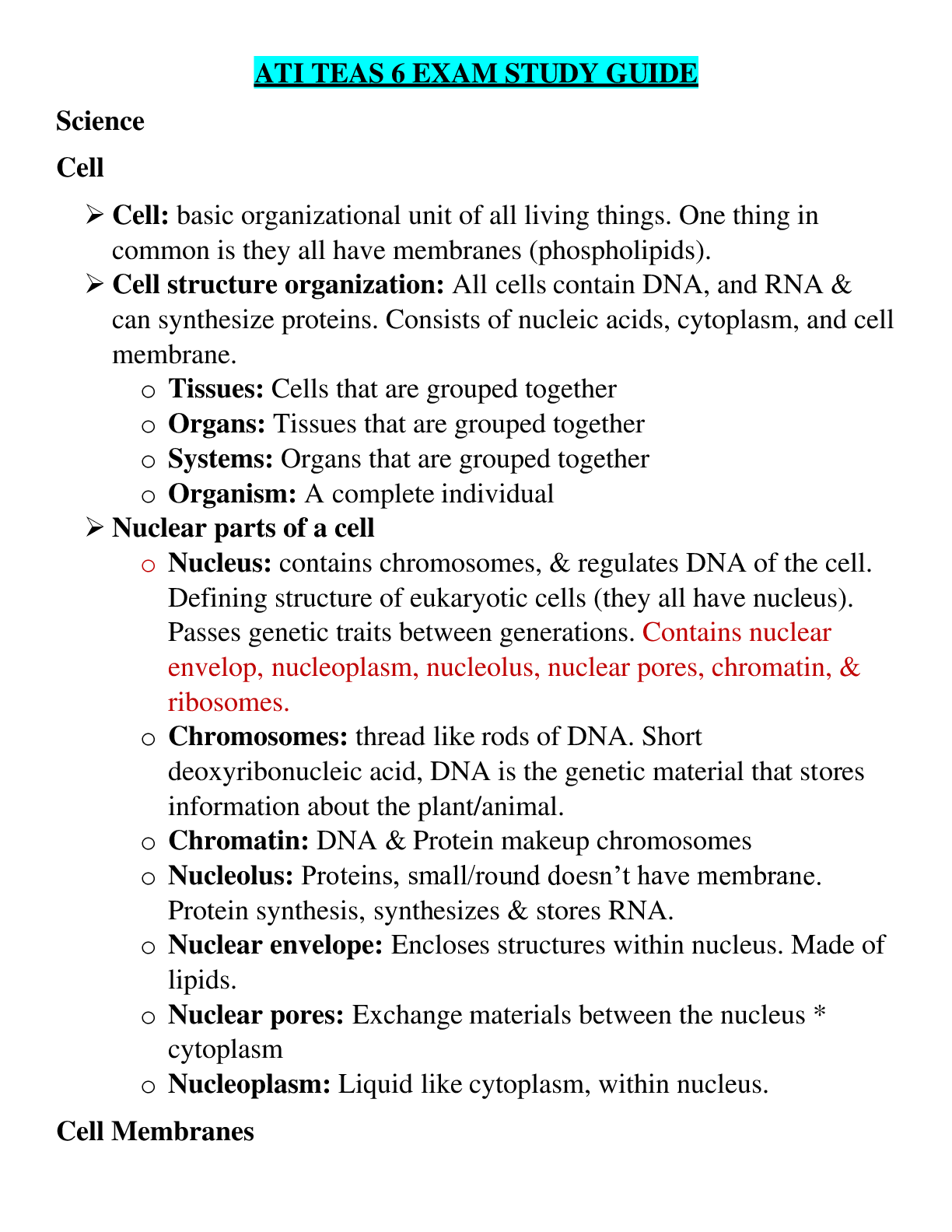
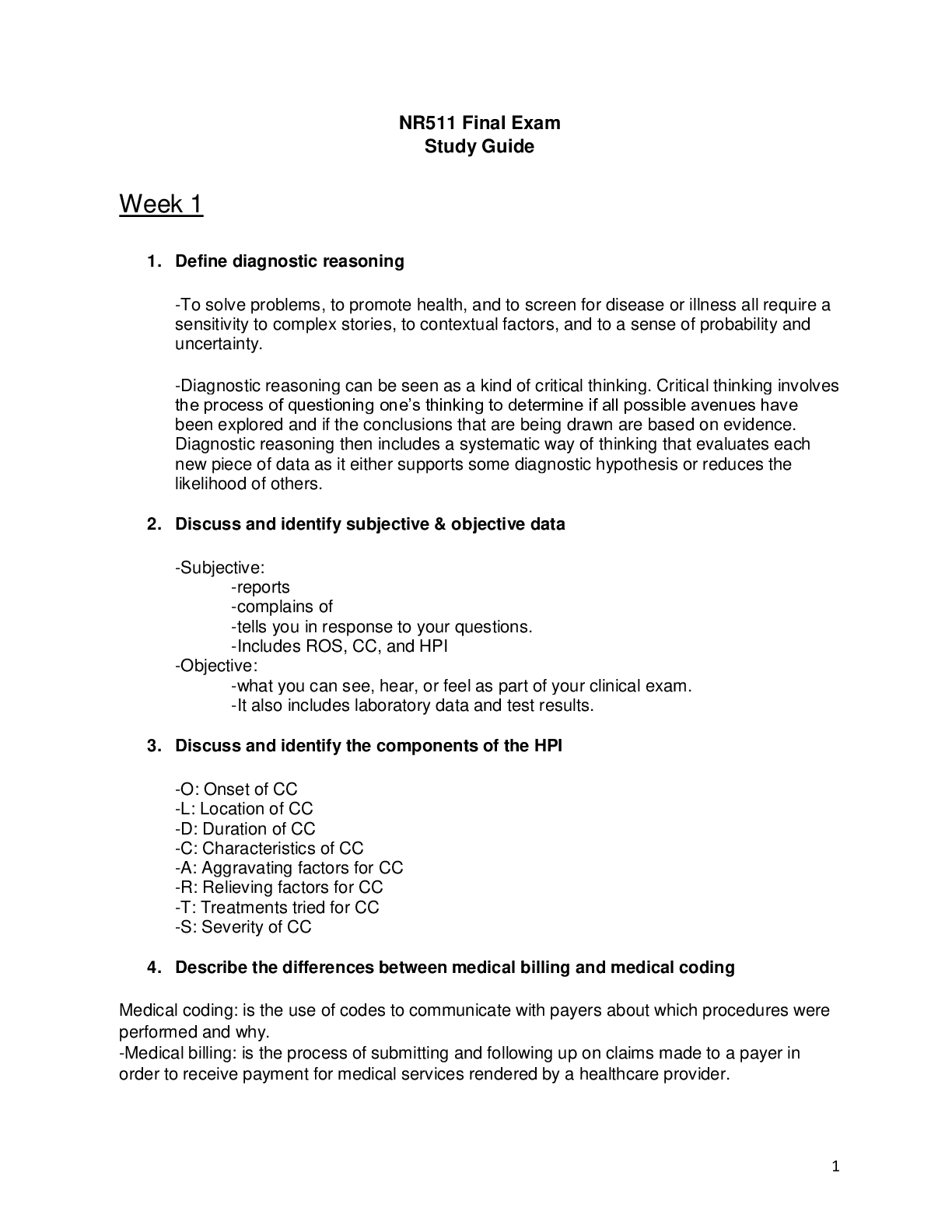
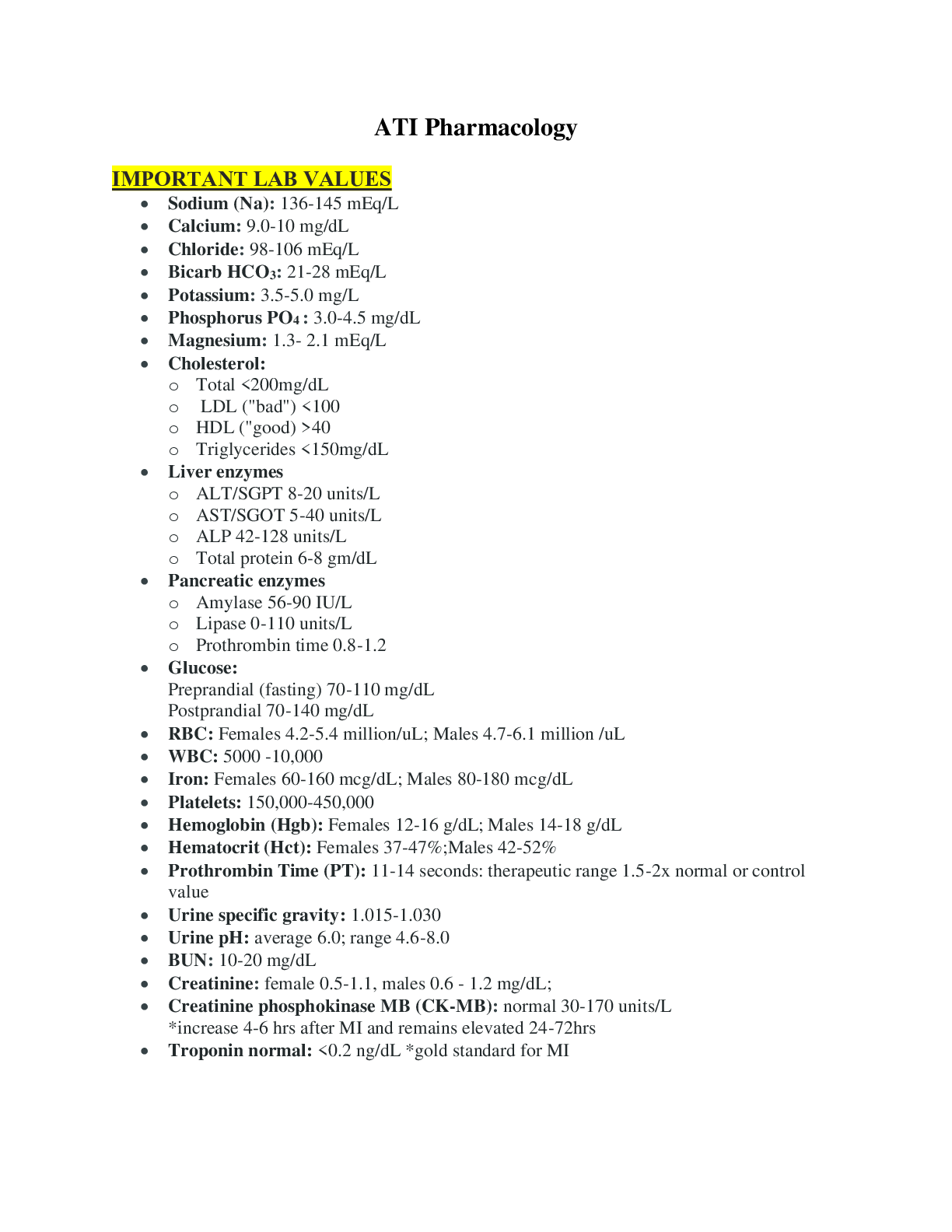
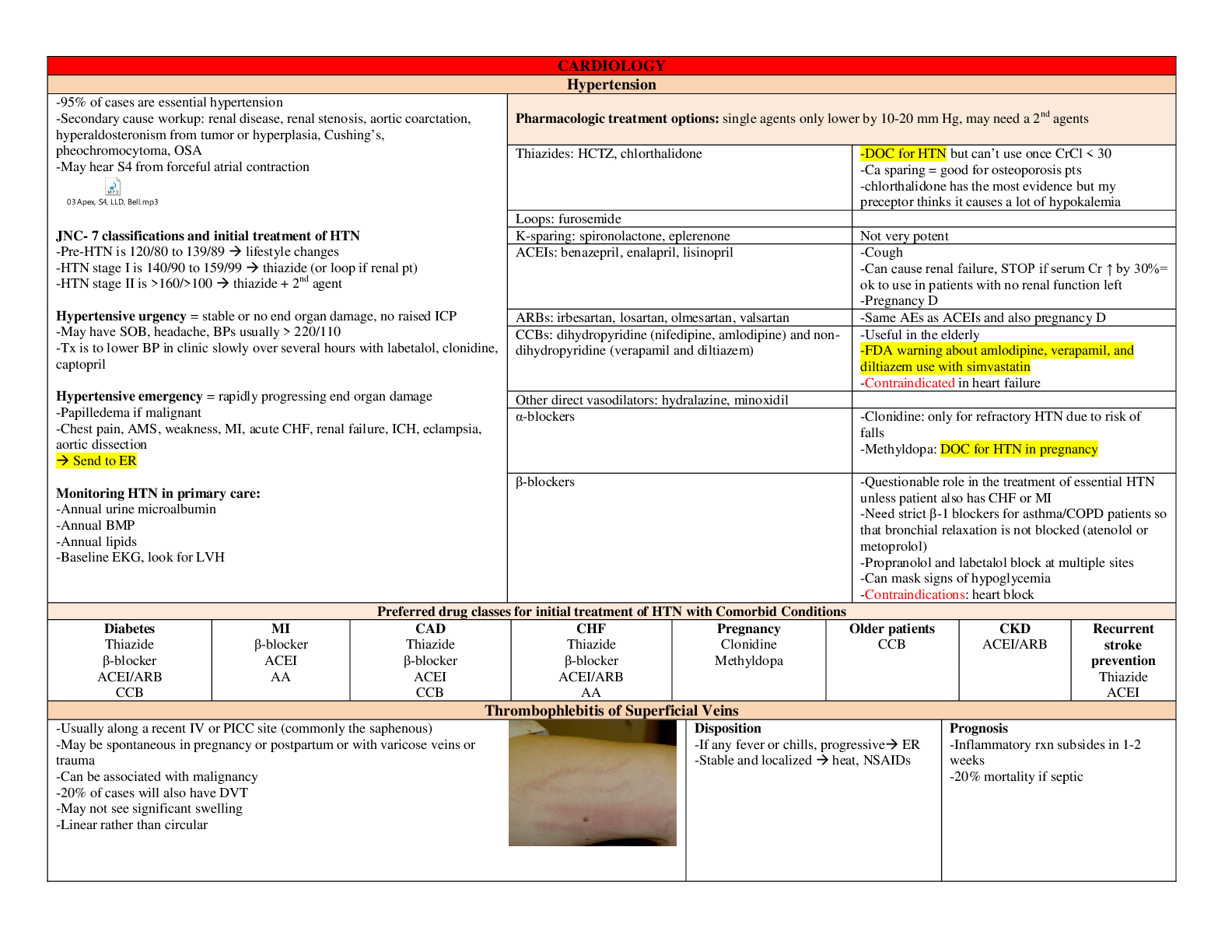
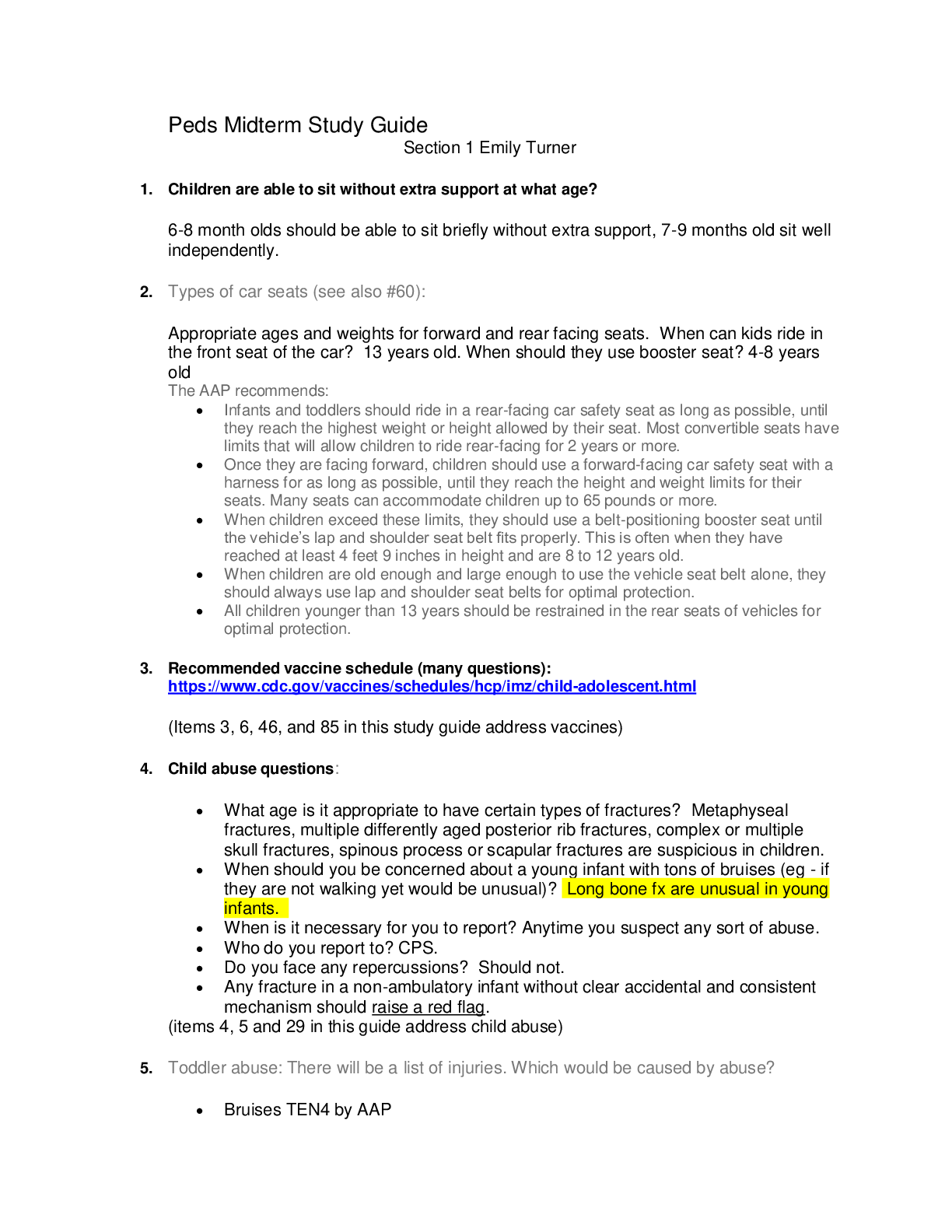
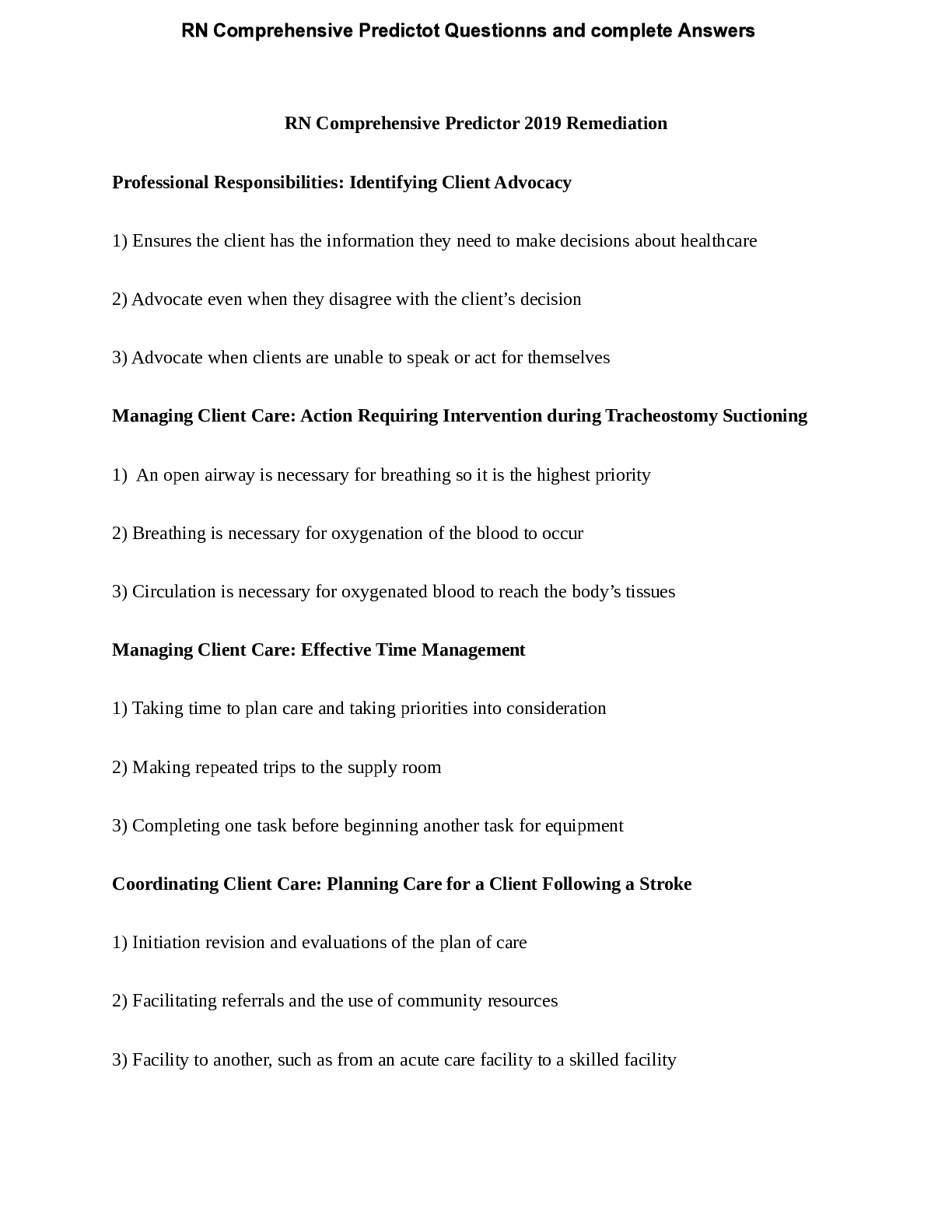
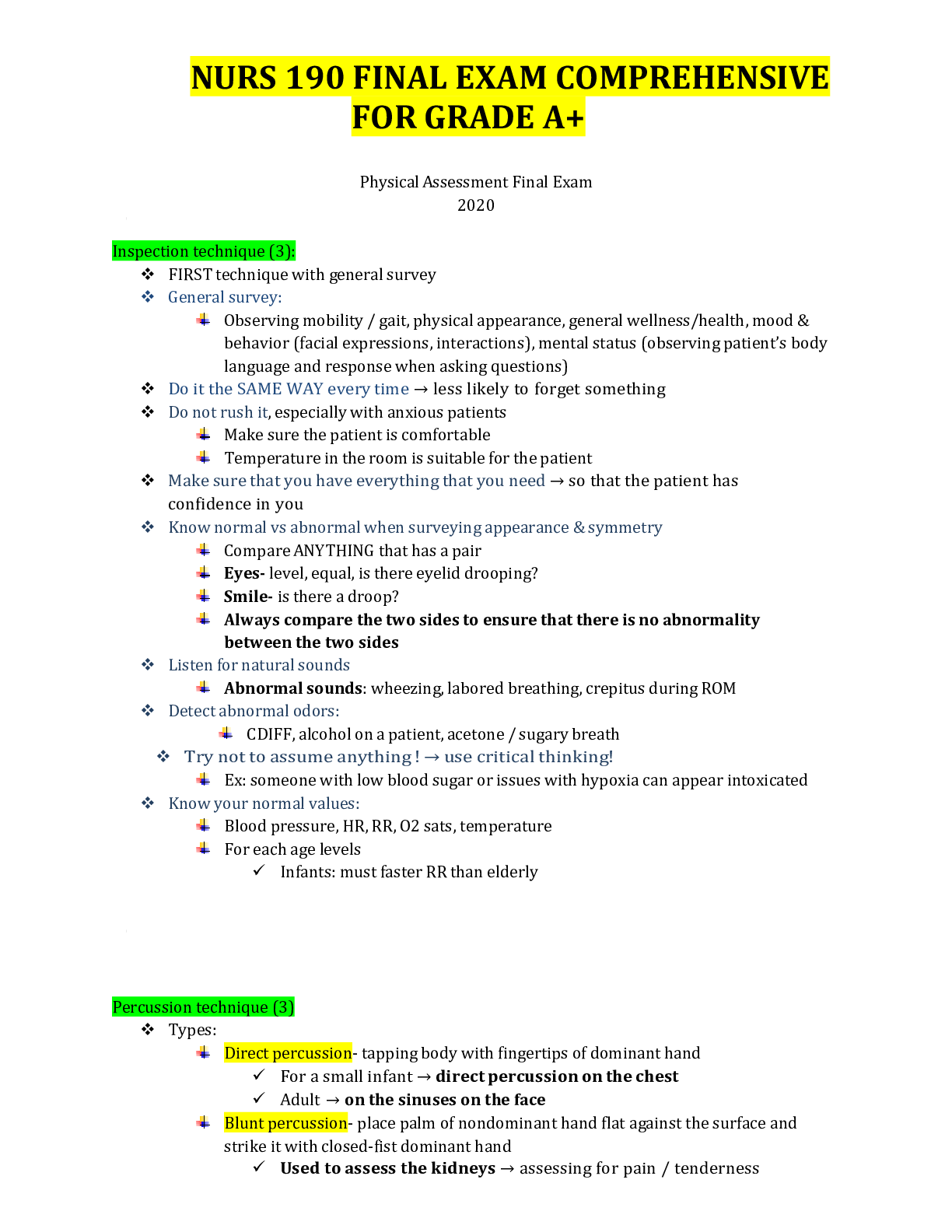
.png)
.png)