Biology > QUESTIONS & ANSWERS > Chapter 22: Anaerobes of Clinical Importance. All Answers (All)
Chapter 22: Anaerobes of Clinical Importance. All Answers
Document Content and Description Below
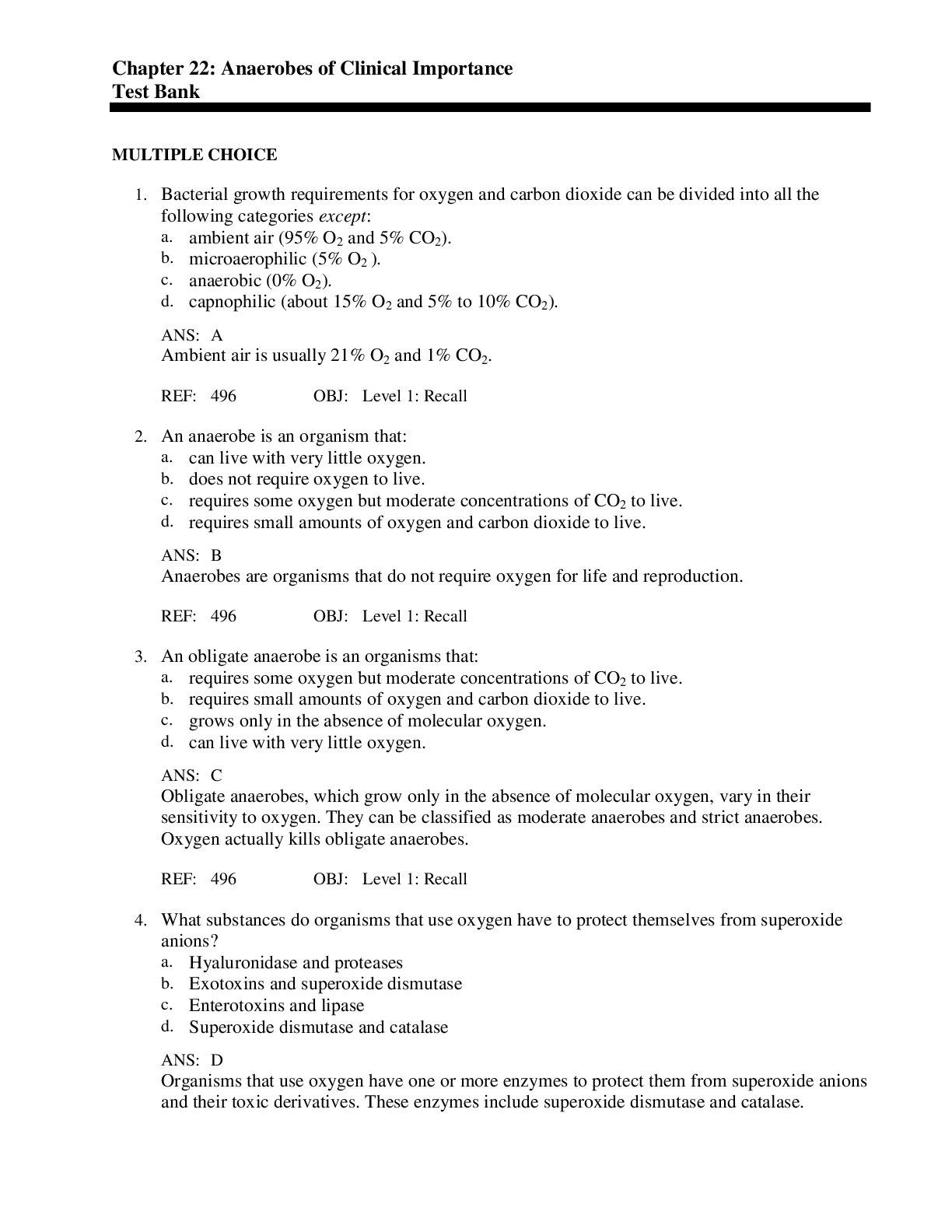
MULTIPLE CHOICE 1. Bacterial growth requirements for oxygen and carbon dioxide can be divided into all the following categories except: a. ambient air (95% O2 and 5% CO2). b. microaerophilic (5%... O2 ). c. anaerobic (0% O2). d. capnophilic (about 15% O2 and 5% to 10% CO2). A Ambient air is usually 21% O2 and 1% CO2. REF: 496 OBJ: Level 1: Recall 2. An anaerobe is an organism that: a. can live with very little oxygen. b. does not require oxygen to live. c. requires some oxygen but moderate concentrations of CO2 to live. d. requires small amounts of oxygen and carbon dioxide to live. B Anaerobes are organisms that do not require oxygen for life and reproduction. REF: 496 OBJ: Level 1: Recall 3. An obligate anaerobe is an organisms that: a. requires some oxygen but moderate concentrations of CO2 to live. b. requires small amounts of oxygen and carbon dioxide to live. c. grows only in the absence of molecular oxygen. d. can live with very little oxygen. C Obligate anaerobes, which grow only in the absence of molecular oxygen, vary in their sensitivity to oxygen. They can be classified as moderate anaerobes and strict anaerobes. Oxygen actually kills obligate anaerobes. REF: 496 OBJ: Level 1: Recall 4. What substances do organisms that use oxygen have to protect themselves from superoxide anions? a. Hyaluronidase and proteases b. Exotoxins and superoxide dismutase c. Enterotoxins and lipase d. Superoxide dismutase and catalase D Organisms that use oxygen have one or more enzymes to protect them from superoxide anions and their toxic derivatives. These enzymes include superoxide dismutase and catalase. REF: 497 OBJ: Level 1: Recall 5. Anaerobes outnumber aerobes in all of the following locations except: a. skin. b. oral cavity. c. gastrointestinal (GI) tract. d. genitourinary tract. A Anaerobes outnumber aerobes at mucosal surfaces, such as the linings of the oral cavity, GI tract, and genitourinary tract. These heavily colonized surfaces are the usual portals of entry into the tissues and bloodstream for endogenous anaerobes. REF: 498 OBJ: Level 1: Recall 6. All of the following organisms are found on the skin under normal conditions except: a. Propionibacterium. b. Peptostreptococcus. c. Streptococcus. d. Clostridium. D The indigenous members of the skin flora include anaerobes. Propionibacterium acnes is frequently isolated from blood cultures, but its presence often represents contamination from the patient’s skin resulting from poor site preparation during the venipuncture. Other anaerobes found on the skin include gram-positive cocci (e.g., Peptostreptococcus and Streptococcus). REF: 498 OBJ: Level 1: Recall 7. All the following organisms are found in the gastrointestinal (GI) tract except: a. Bacteroides. b. Clostridium. c. Propionibacterium. d. Bifidobacterium. C Bacteroides vulgatus, B. thetaiotaomicron, and B. distasonis are among the most common species of bacteria isolated from human feces. Other species commonly inhabiting the GI tract include Bifidobacterium, Clostridium, Eubacterium, and Peptostreptococcus. REF: 499 OBJ: Level 1: Recall 8. What type of bacteria are in the genus Clostridium? a. Anaerobic cocci b. Spore-forming anaerobic bacilli c. Spore-forming anaerobic cocci d. Anaerobic bacilli B All spore-forming anaerobic bacilli are classified in the genus Clostridium and collectively referred to as clostridia. REF: 500 OBJ: Level 1: Recall 9. What disease does Clostridium perfringens cause? a. Botulism b. Tetanus c. Food poisoning d. Toxic shock syndrome C C. perfringens is associated with two types of food poisoning: type A, a relatively mild and self-limited gastrointestinal (GI) tract illness, and type C, a more serious but rarely seen GI tract disease. C. perfringens foodborne disease usually follows ingestion of enterotoxin-producing strains in contaminated food. REF: 500 OBJ: Level 1: Recall 10. What disease does Clostridium botulinum cause? a. Botulism b. Tetanus c. Food poisoning d. Myonecrosis A Occasionally, intoxication may follow ingestion of preformed toxins produced by exogenous anaerobes. Foodborne botulism results from the ingestion of preformed botulinum toxin, a toxin produced in the food by C. botulinum. Seven antigenically different botulinum toxins, A-E, are known. Botulinum toxin is considered the most deadly substance in the world. REF: 501 OBJ: Level 1: Recall 11. What disease does Clostridium tetani cause? a. Botulism b. Tetanus c. Food poisoning d. Myonecrosis B The clinical manifestations of tetanus are attributed to the neurotoxin (tetanospasmin) produced by the causative agent C. tetani. REF: 501 OBJ: Level 1: Recall 12. What organism mostly commonly causes gas gangrene? a. Clostridium difficile b. C. tetani c. C. perfringens d. C. botulinum C Myonecrosis, or gas gangrene, usually occurs when organisms contaminate wounds, through either trauma or surgery. C. perfringens, C. histolyticum, C. septicum, C. novyi, and C. bifermentans are members of the histotoxic group and can cause myonecrosis. C. perfringens, however, is the most common cause. REF: 501 OBJ: Level 1: Recall 13. An elderly patient in a nursing home is recovering from bacterial pneumonia. The patient has been on a lengthy regiment of antibiotics to kill the organism causing the disease. A few days later, the patient is diagnosed with pseudomembranous colitis. What organism is the most likely cause? a. Clostridium difficile b. C. tetani c. C. perfringens d. C. botulinum A C. difficile is the most common but not the sole cause of antibiotic-associated diarrhea and pseudomembranous colitis. Following antimicrobial therapy, many organisms of the gastrointestinal flora other than C. difficile are killed, thus allowing C. difficile to multiply and produce abundant quantities of two types of toxins: toxin A and toxin B. Bloody diarrhea, with associated necrosis of colon mucosa, is seen in patients with pseudomembranous colitis. REF: 502 OBJ: Level 3: Synthesis 14. All of the following are non–spore-forming, anaerobic, gram-positive bacilli except: a. Actinomyces. b. Bifidobacterium. c. Eubacterium. d. Clostridium. D Non–spore-forming, anaerobic, gram-positive bacilli include Actinomyces, Bifidobacterium, Eubacterium, Mobiluncus, Lactobacillus, and Propionibacterium spp. REF: 502 OBJ: Level 2: Interpretation 15. An immunosuppressed patient notices sinus tracts that are draining pus. He also notices that there appear to be small, hard “nuggets” in the pus. What disease will his doctor most likely diagnose? a. Gas gangrene b. Pseudomembranous colitis c. Actinomycosis d. Myonecrosis C Actinomycosis is a chronic, granulomatous, infectious disease characterized by the development of sinus tracts and fistulae, which erupt to the surface and drain pus containing sulfur granules (small colonies of bacteria). REF: 502 OBJ: Level 3: Synthesis 16. Bacterial vaginosis is a synergistic infectious process involving all the following bacteria except: a. Eubacterium. b. Bacteroides. c. Gardnerella. d. Peptostreptococcus. A In bacterial vaginosis, a shift in the vaginal biota occurs resulting in the overgrowth of other endogenous anaerobes of the vagina such as Mobiluncus spp., Bacteroides spp., Prevotella spp., anaerobic gram-positive cocci, and the aerobic bacterium Gardnerella vaginalis. REF: 502 OBJ: Level 1: Recall 17. The four major groups of anaerobic gram-negative bacilli include all the following except: a. Bacteroides fragilis. b. Porphyromonas. c. Prevotella. d. Mobiluncus. D Most of the non–spore-forming, anaerobic, gram-negative bacilli involved in human infectious processes are found as members of the indigenous microflora. Fortunately, only a few of the genera are commonly encountered in clinical specimens, which include the four major groups: the B. fragilis group, Porphyromonas spp., Prevotella spp., and Fusobacterium spp. REF: 503 OBJ: Level 1: Recall 18. A patient goes to the dentist with an abscess. The physician cultures the tooth. Which of the following bacteria is most likely causing this infection? a. Bacteroides fragilis b. Porphyromonas asaccharolytica c. P. gingivalis d. Mobiluncus C Anaerobic gram-negative bacilli are frequently found in mixed infections, causing abscesses and sepsis. B. fragilis often is isolated from soft tissue infection. P. asaccharolytica is widely distributed in human tissues and fluids, whereas P. gingivalis and P. endodontalis are associated primarily with oral infections. REF: 503 OBJ: Level 3: Synthesis 19. What are two important factors that must be taken into consideration when transporting specimens for anaerobic culture? a. Making sure there is enough specimen in a tightly closed container b. Minimizing exposure to oxygen and preventing drying out c. Minimizing exposure to oxygen and making sure the specimen is transported in a tightly closed screw-cap container d. Drying out and proper nutrition B Regardless of the type of specimen submitted for anaerobic bacteriology, it must be transported and processed as rapidly as possible and with minimum exposure to oxygen. Specimens are usually collected from a warm, moist environment that is low in oxygen. Thus it is important to avoid “shocking” the anaerobes by exposing them to oxygen or permitting them to dry out. REF: 503 OBJ: Level 1: Recall 20. Which of the following is considered a better specimen for anaerobic culture than a swab? a. Aspirate b. Washing c. Scraping d. Lavage A Specimens collected by needle and syringe are better for anaerobic bacteriology than those collected by swab. They are less likely to be contaminated by indigenous microflora, including endogenous anaerobes. REF: 504 OBJ: Level 1: Recall 21. All of the following procedures should be performed on clinical specimens to recover anaerobic bacteria except: a. specimen plating on appropriate tubed and plated media. b. anaerobic incubation. c. Kinyoun stain. d. Gram stain. C The following procedures should be performed on clinical specimens for the recovery of anaerobic bacteria: macroscopic examination of the specimen; preparation of Gram-stained smears for microscopic examination; inoculation of appropriate plated and tubed media, including media specifically designed for culturing anaerobes; and anaerobic incubation of inoculated media. REF: 505 OBJ: Level 1: Recall 22. Gram stains of specimens for anaerobic cultures should be examined for all the following reasons except: a. the Gram stain reveals various types and relative number of bacteria present. b. certain morphotypes may provide a presumptive identification and will guide media selection. c. the Gram stain often reveals the presence of leukocytes. d. the Clinical and Laboratory Standards Institute (CLSI) guidelines recommend Gram stains on all anaerobic specimens. D Gram-stained smears must be examined for several reasons. The Gram stain reveals the various types and relative number of organisms present. The presence of multiple distinct morphologic forms suggests that a polymicrobic infectious process is present. Certain morphotypes may provide a presumptive identification of organisms and serve as a guide to media selection. The Gram stain often reveals the presence of leukocytes. However, certain anaerobes produce necrotizing toxins (leukocidins) that destroy leukocytes. Finally, the Gram stain can serve as a quality control technique. REF: 505 OBJ: Level 1: Recall 23. What is the ideal anaerobic incubation system? a. Anaerobic chamber b. Anaerobic jars c. Anaerobic bags d. Candle jars A The ideal anaerobic incubation system is an anaerobic chamber, which provides an oxygen-free environment for inoculating media and incubating cultures. REF: 508 OBJ: Level 1: Recall 24. How long are anaerobic cultures routinely held in the laboratory? a. 1 to 2 days b. 3 to 4 days c. 5 to 7 days d. 7 to 9 days C Cultures are routinely held 5 to 7 days to allow growth of particularly slow-growing anaerobes and up to 3 weeks whenever Actinomyces spp. are suspected. REF: 511 OBJ: Level 1: Recall 25. What evidence indicates the presence of anaerobes in cultures? a. A foul odor upon opening an anaerobic jar or bag b. Growth on the anaerobic plates, but not on the sheep blood agar (SBA) plates incubated in the CO2 incubator c. Colonies on kanamycin-vancomycin laked blood agar (KVLBA) that fluoresce brick-red under ultraviolet light d. All of the above D Several clues can alert the microbiologist that anaerobes may be present on the primary plates. These include (1) a foul odor upon opening an anaerobic jar or bag; (2) colonies present on the anaerobically incubated sheep blood agar plates but not on the CO2-incubated blood or chocolate agar plates; (3) good growth, more than 1 mm in diameter, of gray colonies on the Bacteroides bile esculin (BBE) plate; (4) colonies on either the KVLBA or anaerobic SBA plate that fluoresce brick-red under ultraviolet light or a double zone of hemolysis on SBA incubated anaerobically. REF: 511 OBJ: Level 2: Interpretation 26. How are suspected colonies of anaerobes processed? a. Gram stain morphology and reaction is observed. b. An aerotolerance test is set up. c. A pure culture/subculture plate is inoculated and appropriate disks are added. d. All of the above. D When anaerobes are suspected, the aforementioned steps must be performed and recorded for each colony morphotype present on the anaerobic blood agar plate to initiate presumptive identification of the isolates. REF: 511 OBJ: Level 1: Recall 27. How is the true Gram stain reaction of an anaerobe determined? a. Special potency disks b. Shape and colony morphology c. Aerotolerance d. Direct fluorescent antibody (DFA) A Although the Gram stain is helpful in the initial identification of an anaerobic isolate, certain species of Clostridium may stain pink and thus appear to be gram-negative bacilli. To determine the true Gram stain reaction of the isolate, special-potency disks can be used. REF: 513 OBJ: Level 1: Recall 28. Aerotolerant anaerobes include all the following except: a. Clostridium. b. Bacteroides. c. Actinomyces. d. Lactobacillus. B Some aerotolerant anaerobes (e.g., certain Clostridium, Actinomyces, Propionibacterium, and Lactobacillus) can grow on the CO2-incubated chocolate agar, but they usually grow much better on the anaerobically incubated plate. REF: 512 OBJ: Level 1: Recall 29. What disk is used to presumptively identify Peptostreptococcus anaerobius? a. Bile b. Nitrate c. Sodium polyanethol sulfonate d. Indole C Whenever an anaerobic, gram-positive coccus is isolated, a sodium polyanethol sulfonate (SPS) disk is used to presumptively identify P. anaerobius, which is susceptible to SPS. REF: 513 OBJ: Level 1: Recall 30. All of the following techniques are used for making definitive identification of anaerobes except: a. PRAS and non-PRAS tubed biochemical test media. b. gas-liquid chromatography of metabolic end products. c. preexisting enzyme-based minisystems. d. mass spectroscopy. D A wide variety of techniques exist for making definitive identification: PRAS and non-PRAS tubed biochemical test media, biochemical-based and preexisting enzyme-based minisystems, gas-liquid chromatography analysis of metabolic end products, and cellular fatty acid analysis by gas-liquid chromatography. REF: 517 OBJ: Level 1: Recall 31. A microbiology technologist is reading an anaerobic culture and observes a double zone of hemolysis on an anaerobically incubated sheep blood agar plate. The Gram stain of that organism was a boxcar-shaped, gram-positive bacillus. What organism is this? a. Clostridium perfringens b. C. difficile c. C. ramosum d. C. clostridioforme A A boxcar-shaped, anaerobic, gram-positive bacillus that produces a characteristic double zone of hemolysis on blood agar can be presumptively identified as C. perfringens. REF: 518 OBJ: Level 3: Synthesis 32. A microbiology technologist is reading an anaerobic plate from an intestinal abscess. There is growth on the Bacteroides bile esculin (BBE) plate: gray colonies with a brown color in the area around the colonies. There is also a dark precipitate in the medium in the areas of heavy growth. The microbiologist Gram stains the colonies and observes gram-negative coccobacilli. What is the presumptive identification of this organism? a. Bacteroides vulgatus b. B. fragilis c. B. pneumoniae d. B. denticola B Colonies of the B. fragilis group on the BBE agar plate are gray and a minimum of 1 mm in diameter. The originally light-yellow medium turns brown in the area around the colonies. A dark precipitate in the medium around the areas of heavy growth is suggestive of the species B. fragilis, although some strains of B. ovatus also cause stippling. REF: 523 OBJ: Level 3: Synthesis 33. All of the following reasons are cited for performing antimicrobial susceptibility testing on anaerobes by the Clinical and Laboratory Standards Institute (CLSI) except to: a. determine the resistance mechanisms in anaerobes. b. assist in the management of patients with serious illnesses. c. monitor local and regional resistance patterns. d. determine susceptibility of anaerobes to new antimicrobials. A The CLSI cites the following major reasons for susceptibility testing of anaerobic isolates: to assist in the management of infection in individual patients with serious or life-threatening infections, to periodically monitor local and regional resistance patterns so that such information is available as a guide for empiric antimicrobial choice, and to determine patterns of susceptibility of anaerobes to new antimicrobial agents as they are approved for treatment of infections involving anaerobes. REF: 525 OBJ: Level 2: Interpretation 34. All of the following are approaches to treating anaerobic infections except: a. surgical therapy. b. hyperbaric oxygen. c. antitoxins. d. enzyme inactivators. D Surgical therapy is the most important type of treatment, and in less serious cases, it may be the only type of therapy required. The use of hyperbaric oxygen to force oxygen into necrotic tissue not only delivers oxygen to oxygen-starved tissues but aids in killing anaerobes that are present at the site. The primary role of antimicrobial agents is to limit the local and systemic spread of the organism. In cases of tetanus and botulism, antitoxins are used to neutralize the effect of neurotoxins produced by Clostridium tetani and C. botulinum, respectively. REF: 526 OBJ: Level 1: Recall [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$6.00
Document information
Connected school, study & course
About the document
Uploaded On
Jan 23, 2020
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Jan 23, 2020
Downloads
0
Views
47