*NURSING > STUDY GUIDE > NCLEX Practice Questions Review (All)
NCLEX Practice Questions Review
Document Content and Description Below
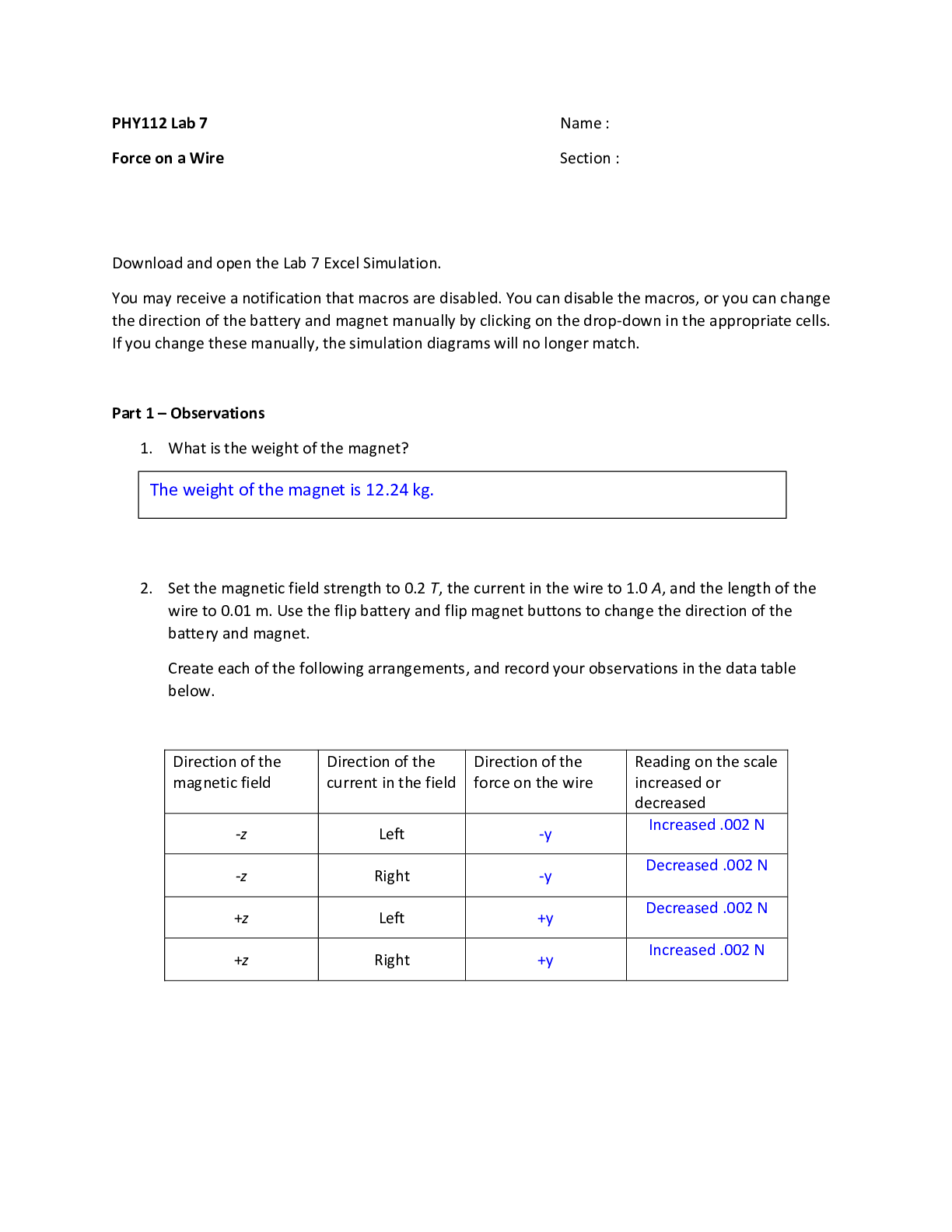
NCLEX Practice Questions Review Leopold maneuvers • 1st maneuver- determines fetal part lying in fundus and fetal presentation • 2nd- which direction fetus back facing • Third maneuver d... etermines part of fetus at inlet and mobility • 4th- fetal attitude and degree of flexion of head Meconium aspiration • Intubation and immediate suction needed-no longer than 5 sec • If HR low, PPV given and suction performed later • Don’t suction with bulb syringe when head pass-no longer recommended RR • 20-40breaths/min HR • 90-130 bpm BP • 90/56 Calories • An increase of 340 calories/day is recommended during the second trimester. • An increase of 462 calories/day is recommended during the third trimester. • Add 330 when breastfeeding Protein • Folic acid- prevent neural tube defects • Leafy green veggies, dry beans/peas, Orange juice Iron • Increase rbc mass • Take 1 hour before meals • Take empty stomach • Give with vit C • Don’t give with milk/caffeine • Can cause constipation- give fiber • Increase absorption of iron • Avoid calcium containing foods-milk and yogurt • Maternal PKU • Genetic disease • Increase levels phenylalanine • Resume diet 3 months before pregnancy and throughout pregnancy • Avoid high protein foods in phenylalanine • Mental retardation/behavior problems Pap Smear • Class 1 through Class V • Class 3- indicate abnormal but doesn’t confirm cancer diagnosis • Reveal abnormal cervical cell growth Supine Hypotension • Vena cava syndrome • Dizziness common sign Epidural anesthesia • Maternal blood pressure decrease(hypotension)-give fluids • CNS depressant • Most effective in active labor • Cause bradycardia in fetus-bolus mom with 500 mL of IV fluid before inserting epidural catheter • Given before active phase of labor- prolongs the labor-take longer for cervix to dilate and efface Spinal anesthesia • headaches Fundus • Displaced when bladder full • Post-delivery- found firm at midline Magnesium sulfate • Calcium gluconate antidote-reverse CNS depression • Given to women to prevent preterm labor/stop contractions • Can cause resp depression in mom • Treat PIH- decrease BP • Prevent seizures in pre-eclamptic women • Cause CNS depression in neonate-monitor for respiration depression • Smooth muscle relaxant • Report decreased U/O • Reduce RR • Depressed or absent reflexes • Hypotension • Decreased cardiac function • AE o Decreased bp o Depressed dtr o Lethargy Nalbuphine • Opioid pain relief Pre-eclampsia/PIH • Cause HTN and proteinuria-monitor closely • Edema of hands and face common finding • Indicate hepatic involvement • Report epigastric pain • Report pitting edema of ankles • Expect 3+ deep tendon reflex • Oliguria • Proteinuria greater than 0.3 q 24 hrs • Expect blurred vision and photophobia • Symptoms- sudden weight gain, swelling, edema, severe headache, reports of seeing spots, blood in urine, dizziness, nausea, vomiting • When worsened- baby may need to be delivered or mag sulfate given IV to prevent seizures • Call 911 to be evaluated • Can last for many weeks after delivery • Rest sidelying-increase tissue perfusion • Daily fetal kick count Drug Addiction • Increased muscle tone • Respirations greater than 60 • Hyperactivity –CNS irritability • Don’t stimulate infant-need calm environment with minimal stimulation to promote rest and reduce stress Active Labor • Check cervix before giving pain meds • Given too close to delivery can cause resp depression in neonate Contraction Stress Test • Fetus repeated decels of FHR response to contractions • Don’t give oxytocin for positive CST at 38 weeks- compromise fetal oxygen supply • Positive-abnormal-late decels • Neg- normal-no late decels • Nipple stiumation Ectopic Preg • Fertilized egg implant outside uterus • Scarring from tubal infection/surgery- PID Betamethasone(Celestone) • Glucocorticoid • Prevent resp distress syndrome in premature infants • No effect on neonatal VS • No effect on baby temp • Given at 30 weeks gestation • Given to stimulate fetal lung maturity-prevent resp distress • Cause hyperglycemia in mom • Can cause baby to have hypoglycemia 1st few hours after delivery PIH • Develop edema, elevated BP, proteinuria • Reflex normally plus 2 Nonstress Test(20 min) • Measure FHR accelerations with normal movement • Fetal acc. Positive sign • Increase 15/min and last 15 sec • Nonreactive- no acc. • Reactive- norm baseline/moderate variability • Sit in reclining chair or on left side/don’t walk • Give mom OJ and crackers to stimulate fetus movement • Press button when feel fetal movement FHR • V C- variable decels cord compression • E H-early decels- head compression • A O-accelerations ok • L P-late decels placenta insufficiency Oxytocin • Stimulate contractions • Can cause decreased FHR and hypoxia due to increased uterine pressure • • AE- subarachnoid hemorrhage, seizure, coma, HTN, abruption placenta • Don’t bolus • Give through IV pump • Always monitor FHR • Discontinue when contractions q 1-2 min lasting 90-100 sec Weight Gain • 25-30 lbs entire preg • 4 lb- 1st tri • 12 lb- 2/3 tri • normal- 1-3kg/month 2nd/3rd trimester ITP • Autoimmune response with decreased platelet count • Increased megakaryocytes 6 weeks gestation + 24 weeks • GBS done at 35-37 weeks • Rubella titer done at initial prenatal visit to determine rubella immunity • Glucose tolerance test • 3 hour gtt done in women with elevated glucose levels after 1 hour test is done at 28 weeks LGA(macrosomnic infant) • heel stick glucose 50 normal • respirations 50 notmal • acrocynaosis normal • jittery is sign of hypoglycemia Breastfeeding and engorgement • apply cold cabbage to relieve pain • breast binders suppress lactation • breast shells for patients with inverted nipples or flat or pts with sore nipples Prolapsed umbilical cord • call for help • apply internal upward pressure to presenting part Abruptio placenta • cocaine use increase risk for vasoconstriction and abrupted placenta Infant safety • set hot water heater no higher than 49 C 120 F • crib slats no more than 6.3 cm 2 3/8 in apart • no comforter in crib hyperemesis gravidarum • eat to taste to avoid nausea • eat healthy snack at bedtime • alternate liquids and solids every 2 hour • eat protein following sweet snack Vaginal hematoma • pressure in vagina • persistent vaginal pain terbutaline • protect from light • relax smooth muscle • primary action- bronchodilation • subqqa 4 hrs no longer than 24 hr • AE- headache, dizzy, arrhythmias, nausea, paradoxical bronchospasms, tachycardia, hyperglycemia, hypoklemia Hydatidiform mole • Placental abnormal • Chorionic villi of placenta develop into grape like mass-clear vesicles • With or w/o fetus present • Avoid preg for 1 year • As cells slough- discharge dark brown vaginal Jaundice • Pathological- 1st 24 hrs, inform HCP- stat bilirubin test • Physiological- breastfed after 24 hours Late decels • Placental insufficiency • Pressure on IVC-decrease O2 to placenta and fetus • Turn on left side, give O2, then give fluids Naloxone • Reverse respiratory depression, hypotension of opiods • AE- seizures, pulmonary edema, tachycardia, HTN, V FIB Diaphragm • Remove after 24 hrs-clean with mild soap water • Replace q 2 years • Insert on empty bladder • Weight gain greater/less 10-15 lbs refitted • Keep in place 6 hours after sex Chadwick sign • Blue discoloration in cervix, vagina Low Back pain • Posterior-face mom back • Rub lower back-help relax muscles in low back and relieve pressure of fetus head Cerclage • Reinforce weak cervix • Use sutures that go around cervix, hold it close • Go to hospital first sign of labor • Can have sex Polyhydramnios • Excessive fluid surrounding fetus • Increased fundal height • Increased weight gain • Increased urination • GI fetal malformations and neuro disorders-anticipate Oligohydraminos • Volume amniotic fluid less than 300 • Fetal renal dysfunction • Obstructive uropathy • Confirmed by US • IUGR Mineral oil • Treat constipation • Take at bedtime on empty stomach • Abruption placentae • Premature separation of placenta from uterine wall • Platelet count decreased • Prolonged partial thromboplastin • Decreased fibrinogen • Normal clotting time • Abdominal pain-sharp painful bleeding Placenta previa • Placenta attach low in uterus • Painless vaginal bleeding • Life threatening-need continued hospitalization and close monitoring • Near or covering cervix opening- partially or totally • Don’t perform vaginal exams • Monitor fetal heart tones- continuous EFM • Take vs q 15 min • Most common in 3rd trimester Abdominal US • Need full bladder • Ask when last voided Rubella • When mom titer neg, give another after delivery • Avoid preg at least one month after vaccine • Mild rash and joint ache 7-10 days after • Get each preg • May have low grade fever Erythromycin ophthalmic • Give within 1st hour • Gonorrhea/chlamydia Hep B vaccine • Given several hours after birth • Parent consent Vitamin K • Used for synthesis of clotting factors in liver • Given to prevent bleeding • Newborns risk of bleeding-lack of intestinal flora needed to make vit K Cephalhematoma • 2-6 weeks for edema and discoloration to disappear • no treatment needed caput succedaneum • resolve 2-3 days Ergotamine • treat migraine • one tab at onset of migraine • max 3 in 24 hr period • Methylergonovine(methergine) • treat PP hemorrhage • monitor VS and vag bleeding • AE- seizures, stroke, headache, nausea, chest pain, palpitations, increased BP • CI- high BP Bethanechol • Cholinergic stimulate muscarinic receptors Phenytoin • Don’t take with mil or calcium • Less than 10mcg subtherapeutic-cause seizures • Levels more than 20 toxic effects • Cause gingival hyperplasia- tell dentist • Report nystagmus Anticholinergic drugs • Worsen urinary retention • Atropine • Scopolamine • Benztropine o Constipation o Tachycardia o Glucose in infants • Normal ranges 40-95 mg/dL • Fasting glucose 60-90 for pregnant Bilirubin • Report greater than 8 Hct • Normal 48-69% LGA • Weight above 90th percent • Increase risk for hypoglycemia Congenital hip dysplasia • Limited abduction indicate head femur slipped out of acetabulum • Limited abduction of hip • Asymmetrical gluteal folds Stepping reflex • Should be gone by 4 weeks Moro reflex aka startle reflex • 8 weeks Babinski reflex • 1 years • Stroke bottom of foot Extrusion • Infant spit out food tonic neck • 3-4 months Jet hydrotherapy • Doppler device, fetoscope, wireless external monitor safe • Don’t use internal electrode Newborn assessment • Posterior fontanel should be larger than anterior • Assess apical pulse for 1 full minute-when baby quiet • Overlapping suture line • Lanugo over shoulders normal • Breast nodules up to 10mm • T 36.5-37.2C • Weight 2.5-4 kg • Length 45-55cm • Chest circumference in term 2 cm less than head circumference-measured at nipples • Head circumference greater than 37cm or less than 33cm investigate for neurologic involvement Neonatal sepsis • Temp instability • Tachypnea • Hypotonia • Lethargy • Nasal flaring • Irritability Vaginal hematoma • Pressure in vagina • Persistent vaginal pain Infant safety • Hot water heater no higher than 49 C 120 F • Crib slats no more than 2 3/8 inch • No loose bedding in crib Amniocentesis • Rhogam given following procedure • Potential of fetal RBC entering maternal circulation • Given at 28 wks Circumcision • Sterile gauze for bleed • Petroleum jelly each change • Don’t wipe off yellow exudate- normal • Document voids after- secondary • Change diaper at least q 4 hours • Avoid soap and water • Rim usually fall off in 1 wk • 1st priority is to monitor for bleeding q 15 min for 1st hour after procedure • DON’T APPLY petroleum jelly after circumcision when plastibell used • Complications-hemorrhage, infection, urethral fistula formation Mastitis • Unilateral breast pain with tenderness Reposition, increase fluids, give oxygen 8L Itp • Decreased platelet • Increased megakaryocytes GBS • 35-37 wks 3 hr glucose • 28 wks Heparin • don’t take aspirin • bedrest • don’t massage • apply warm compress not cold hperbilirubinemia • yellow mucous membranes, bron or gold urine, maculopapular rask normal • irritable complication Uterine Inversion • Don’t remove placenta if still attached- can cause larger SA for bleeding • Large amt blood suddenly gush from vagina • Fundus not palpable in abdomen • Don’t give oxytocics- compounds the inversion • Assess VS and establish IV access and fluids • Discontinue uterotonic drugs-allow uterine relaxation for replacement Pharmacology NCLEX practice questions Acetazolamide • Diuretic • For chronic open angle glaucoma, epilepsy, edema • AE o Paresthesia-tingling fingers o Hyperglycemia Oxybutynin • For urinary incontinence • Anticholinergic effects-dry mouth, photophobia, constipation, blurred vision, tachycardia Dopamine • Increase BP in cardiogenic shock • Cardiac stimulation • No effect on RR • Increase renal circulation- incr UO Doxycycline • Tetracycline antibiotic • CI o Pregnancy o Effects on developing bone and teeth Regular insulin • Manage gestational diabetes Baclofen • Decrease seizure threshold in pt with epilepsy • Decr freq and severity of muscle spasms • No effect on cognition • Inhibits reflexes at spinal level Tamoxifen • Treat breast cancer • AE o Menstrual irregular o Hot flashes-anti estrogen o Bruising Inhibitor overdose • Antidote- atropine sulfate Neuromuscular blocker overdose • Neostigmine- cause nausea, increased salivation, bradycardia Clindamycin • Can cause C dif-watery diarrhea • Topical application cause face swelling • Generalized muscle aches Sedative hypnotic anxiolytics Benzodiazepines • Prototype o Alprazolam • Antidote o Flumazenil • Meds o Diazepam o Lorazepam o Oxazepam o Clonazepam o Clorazepate o Chlordiazepoxide • Complications o CNS depression Sedation, lighthead o Anterograde amnesia o Resp Depression Hypotension Cardiac/resp arrest Gastric lavage Activated charcoal Monitor VS o Paradoxical response Insomnia Euphoria Anxiety Rage o Withdrawal effects Taper off over few weeks • Contraindication o Sleep apnea o Glaucoma o Resp depression o Liver disease o Used short term due to dependency • Interactions o CNS depressants Alcohol Opioids Barbituates Anticonvulsants Antihistamines o Grapefruit Reduce metabolism o Fatty meals Reduce absorption • Considerations o Take at bedtime o Take with meals Atypical anxiolytic/nonbarbituate • Prototype o Buspirone • Action o Bind serotonin and dopamine receptor o Dependency less likely o 2-6 wks full effect o Take on schedule • Complications o Dizzy o Nausea o Lighthead o Agitation o Constipation o Suicide ideation o Take with food • Contraindications o MAOI use- 14 days after use- hypertensive crisis • Interactions o Erythromycin o Ketoconazole o St johns wort o Grapefruit juice Increase effects of buspirone Avoid use o Increase risk for serotonin syndrome with SSRI Monitor for SS • Fever • Tremor • Diarrhea • Delirium • Considerations o Take with meals o A week to notice effects o Take on regular basis o Tolerance, dependence not issue SSRI-antidepressants • Prototype- paroxetine • Other o Sertraline o Citalopram o Escitalopram o Fluoxetine o Fluvoxamine • Action o Inhibit ssri reuptake o Paroxetine produce CNS stimulation –insomnia, wt loss and decreased appetite increase risk for birth defects o Long half life o Up to 4 weeks for therapeutic • Complications o Serotonin syndrome 2-72 hrs after o Nausea o Diaphoresis o Agitation o Confusion o Anxiety o Hallucinations o o Tremor o Headache o Dry mouth o Fatigue o Drowsy o Sex dysfunction Med holiday Sildenafil and buspirone use o Wt gain o GI bleed Report dark stool Coffee ground emesis o Hyponatremia o Serotonin syndrome Agitation Confusion Difficult concentration Tachycardia Abdominal pain- diarrhea Cardiovascular shock Hypertension Seizures death Myoclonus-spastic jerky muscle contractions Hyperreflexia Fever Begin 2-72 hrs after Report manifestations o Bruxism Grinding of teeth during sleep Use mouth guard Treat with low dose buspirone o Postural hypotension o Suicide ideation o Rash o GI bleed • Contraindications o Paroxetine- avoid alcohol o Use cautious pts with liver/renal dysfunction, seizure disorder, GI bleeding o MAOI or TCA use • Interactions o MAOI and TCAs and lithium Cause SS o Antiplatelet meds/anticoagulants Increase bleed risk Warfarin • Monitor PT/INR levels o St john wort- don’t take with o Considerations Take with food CNS stimulation • Take¬ in morning Take on daily basis 4 weeks to be therapeutic Don’t take with NSAIDS- can take Tylenol o Digoxin o Normal therapeutic range 0.5-2 ng/mL o Greater than that toxic call HCP o Cause blurred vision AE Depressive disorders SSRI- see above SNRI • Prototype o Venlafaxine • Other meds o Desvenlafaxine o Duloxetine • Action o Block reuptake NE • Complications o Nausea o Anorexia o Wt loss o Headache o Insomnia o Anxiety o HTN o Tachycardia o Dizzy o Blurred vision o Withdrawal syndrome o Suicide risk o Sex dysfunction o SSRIbronchitis o Dyspnea • Contraindications o SSRI o MAOI o TCA o Discontinue 2 weeks before starting MAOI • Interactions o Neuroleptic malignant syndrome if given with MAOIS Don’t take o NSAIDS/anticoag Increase bleed risk o Alcohol Increase risk CNS effects o Kava, Valerian Increase risk for CNS depression • Avoid Atypical antidepressants • Prototype o Bupropion • Other meds o Vilazodone o Mirtazapine o Reboxetine o Trazadone • Action o Inhibit NE and dopamine uptake o For pts who cant tolerate sex dysfunction o Smoking cessation • Complications-anticholinerggic effects o Headache o Dry mouth o GI distress o Constipation o Tachycardia o Htn o Restlessness o Insomnia o N/V/anorexia, wt loss o Seizures • Contraindication o MAOIs use o Seizure and eating disorders • Interactions o MAOIs-phenelzine Increase toxicity risk TCAs • Prototype o Amitriptyline o Take with food or immediately after • Other meds o Imipramine o Doxepin o Amoxapine o Trimipramine o Desipramine o Clomipramine o Notriptyline • Action o Block serotonin and NE reuptake o 10-14 days or longer for effects 4-8 wks o Fibromyalgia o Neuropathic pain • Complications o Orthostatic hypotension Monitor BP and HR before and 1 hr after giving o Anticholinergic effects o Htn o Bluish green urine o Constipation o Tachycardia o Photophobia o Sedation o Toxicity Cardiac dysrhythmias Mental confusion Seizures Coma Death o Decreased seizure threshold o Excessive sweating • Contraindications o Seizure disorders with MI o Cautious in diabetics, CAD, BPH, resp disorders o 1 wk supply for suicide risk increase • Interactions o MAOI/st john wort o Antihistamines o Anticholinergics o TCAs o Alcohol MAOI • Prototype o phenylzine • other meds o isocarboxazid o tranylcypromine o selegine-transdermal MAOI • Action o Increase NE, serotonin, dopamine and tyramine o Tyramine can cause hypertensive crisis • Complications o CNS stimulation o Orthostatic hypotension Monitor BP and HR before and after Hold less than 60 o HTN crisis Vasoconstriction and stimulation of heart Headache/N/increased HR and BP Give phentolamine IV- rapid acting adrenergic blocker or nifedipine Continuous cardiac monitoring and resp support o Considerations Reduce tyraine MED SURGE REVIEW Respiratory ATI Practice questions Crepitus o Aka subQ emphysema o Coarse crackling sensation palpated over skin surface o Indicate air leak ino subQ tissue o Indicate pneumothorax Friction rub o Scratching/squeaking sound o Don’t clear with coughing o Indicate pericarditis or pleurisy Cheyne stoke respirations o Rhythmic increase and decrease in rate with periods of apnea o Reflect severe brain dysfunction ARDS o Life threatening o Inflammation of lungs and accumulation of fluid in alveoli cause hypoxia o Initial manifestations- increased restlessness, apprehension, anxiety, increased respirations, dyspnea, air hunger, retraction of accessory muscles, cyanosis o Verconium- neuromuscular blocking agent facilitate vent and decrease o2 consumption o Gentamicn- nephrotoxic o PAWP(preload) normal in pt o Fluid in alveoli from increased permeability of the alveolar-cap membrane o o Increased RR indicate decline in condition-earliest sign ARF o Increased CO2 o Decreased pH- resp acidosis o Decrease in O2 sat o Lower pp oxygen Pneumonestomy o Must clear secretions from remaining lung o Pt splint incision while coughing o demonstrates dyspnea, cough, frothy sputum, crackles, and possibly cyanosis. o Pain with deep breathing is expected and is managed with analgesics. o The client with pneumonectomy most likely will not have a chest tube because the lung has been removed o May cause increased airway pressure because of resistance to lung inflation Pneumothorax o Pt has severe diminished or absent breath sounds on affected side o SOB o Chest pain o Hyperresonance on affected side Emphysema o Purse lipped breathing greatest effect on exhalation not inhalation- breath in through nose and out through lips o Help rid of CO2 COPD o Resp acidosis-hypoventilation dec ph increased co2 o Venturi mask- delivers most oxygen conc. o Delivers precise amt o2 o Manifestations- hypoxemia, hypercapnia, dyspnea on exertion or rest, accessory muscle use, oxygen desat o X-ray reveal hyperinflated chest, diaphragm flattened o PFT- decreased vital capactity o Difficult exhaling CO2-loss elastic recoil in lungs o Vomiting and diarrhea cause metabolic alkalosis o Schedule resp treatments before meals o Give diet high in calories and protein, low in carbs o Schedule short activities o Clubbing expected o Purse lip breathing expected-promote )2 elimination o Low o2 sat expected Chest physiotherapy o Helps mobilize secretions in airway- percussion and vibration performed Thoracentesis o Aspirate fluid or air from pleural space o Upright position sitting and leaning over bedside table o Wear goggles and mask o Cleanse area with antiseptic o Remain completely still o Apply pressure to site after removing needle ........................continued............................ [Show More]
Last updated: 1 year ago
Preview 1 out of 102 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$18.00
Document information
Connected school, study & course
About the document
Uploaded On
Feb 20, 2021
Number of pages
102
Written in
Additional information
This document has been written for:
Uploaded
Feb 20, 2021
Downloads
0
Views
104