*NURSING > NCLEX > NCLEX RN 515 EXAM DUMP QUESTIONS, ANSWERS AND EXPLANATIONS FOR HIGH SCORING GRADES (All)
NCLEX RN 515 EXAM DUMP QUESTIONS, ANSWERS AND EXPLANATIONS FOR HIGH SCORING GRADES
Document Content and Description Below
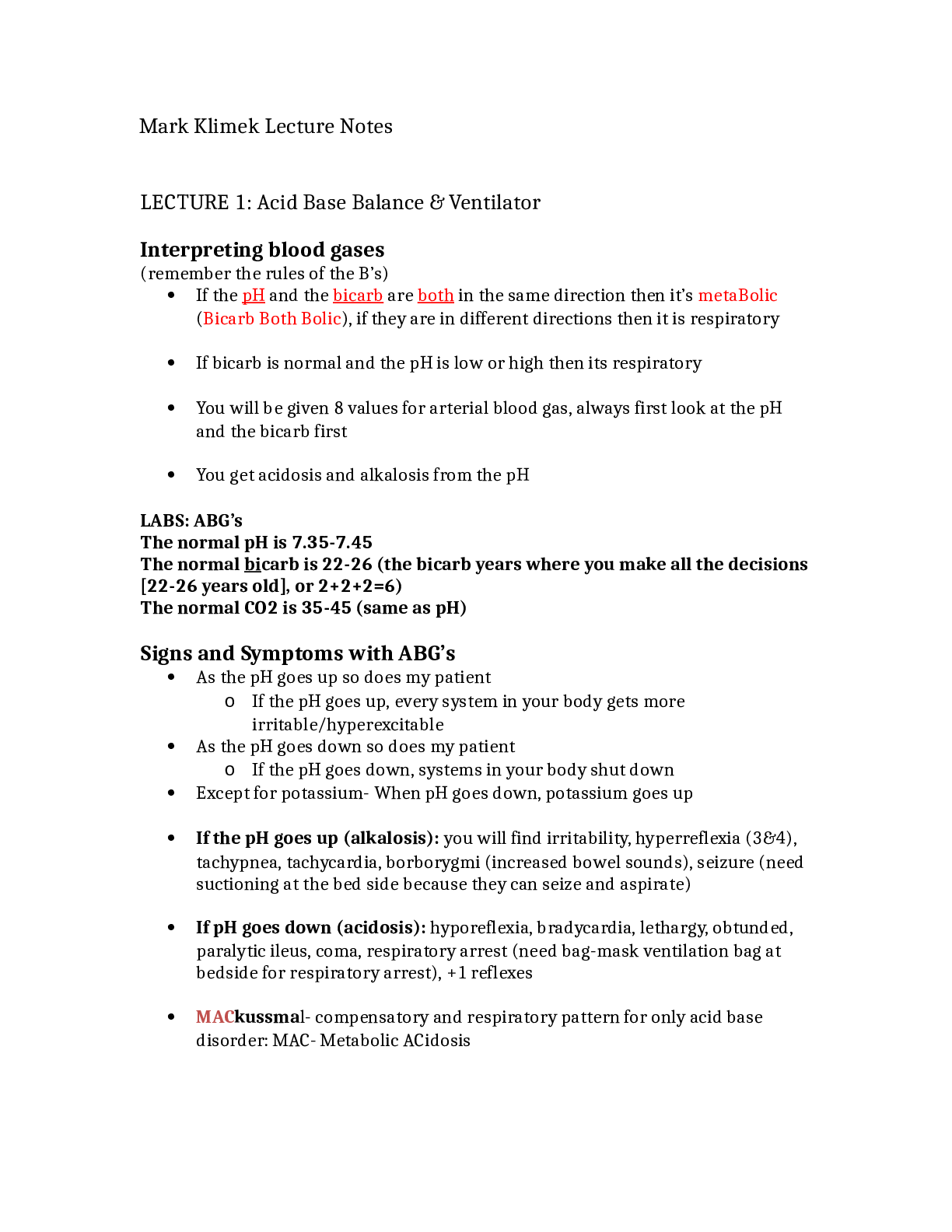
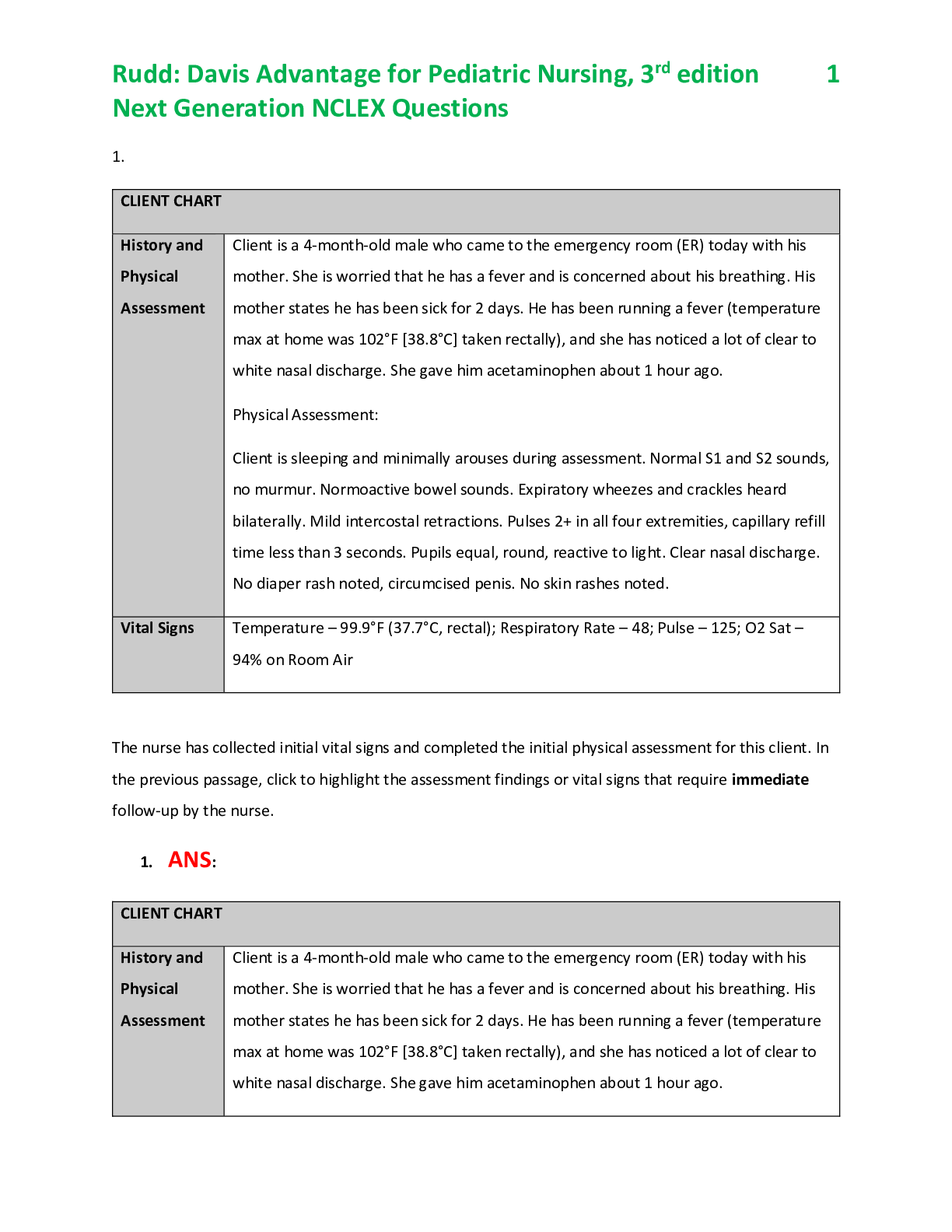
Exam A QUESTION 1 To appropriately monitor therapy and client progress, the nurse should be aware that increased myocardial work and O2 demand will occur with which of the following? A. Positive i... notropic therapy B. Negative chronotropic therapy C. Increase in balance of myocardial O2 supply and demand D. Afterload reduction therapy Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Inotropic therapy will increase contractility, which will increase myocardial O2 demand. (B) Decreased heart rate to the point of bradycardia will increase coronary artery filling time. This should be used cautiously because tachycardia may be a compensatory mechanism to increase cardiac output. (C) The goal in the care of the MI client with angina is to maintain a balance between myocardial O2 supply and demand. (D) Decrease in systemic vascular resistance by drug therapy, such as IV nitroglycerin or nitroprusside, or intra-aortic balloon pump therapy, would decrease myocardial work and O2 demand. QUESTION 2 The nurse would need to monitor the serum glucose levels of a client receiving which of the following medications, owing to its effects on glycogenolysis and insulin release? A. Norepinephrine (Levophed) B. Dobutamine (Dobutrex) C. Propranolol (Inderal) D. Epinephrine (Adrenalin) Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Norepinephrine’s side effects are primarily related to safe, effective care environment and include decreased peripheral perfusion and bradycardia. (B) Dobutamine’s side effects include increased heart rate and blood pressure, ventricular ectopy, nausea, and headache. (C) Propranolol’s side effects include elevated blood urea nitrogen, serum transaminase, alkaline phosphatase, and lactic dehydrogenase. (D) Epinephrine increases serum glucose levels by increasing glycogenolysis and inhibiting insulin release. Prolonged use can elevate serum lactate levels, leading to metabolic acidosis, increased urinary catecholamines, false elevation of blood urea nitrogen, and decreased coagulation time. QUESTION 3 Which of the following medications requires close observation for bronchospasm in the client with chronic obstructive pulmonary disease or asthma? A. Verapamil (Isoptin) B. Amrinone (Inocor) C. Epinephrine (Adrenalin) D. Propranolol (Inderal) Correct Answer: DSection: Questions Set A Explanation Explanation/Reference: Explanation: (A) Verapamil has the respiratory side effect of nasal or chest congestion, dyspnea, shortness of breath (SOB), and wheezing. (B) Amrinone has the effect of increased contractility and dilation of the vascular smooth muscle. It has no noted respiratory side effects. (C) Epinephrine has the effect of bronchodilation through β stimulation. (D) Propranolol, esmolol, and labetalol are all β- blocking agents, which can increase airway resistance and cause bronchospasms. QUESTION 4 The following medications were noted on review of the client’s home medication profile. Which of the medications would most likely potentiate or elevate serum digoxin levels? A. KCl B. Thyroid agents C. Quinidine D. Theophylline Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Hypokalemia can cause digoxin toxicity. Administration of KCl would prevent this. (B) Thyroid agents decrease digoxin levels. (C) Quinidine increases digoxin levels dramatically. (D) Theophylline is not noted to have an effect on digoxin levels. QUESTION 5 In the client with a diagnosis of coronary artery disease, the nurse would anticipate the complication of bradycardia with occlusion of which coronary artery? A. Right coronary artery B. Left main coronary artery C. Circumflex coronary artery D. Left anterior descending coronary artery Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Sinus bradycardia and atrioventricular (AV) heart block are usually a result of right coronary artery occlusion. The right coronary artery perfuses the sinoatrial and AV nodes in mostindividuals. (B) Occlusion of the left main coronary artery causes bundle branch blocks and premature ventricular contractions. (C) Occlusion of the circumflex artery does not cause bradycardia. (D) Sinus tachycardia occurs primarily with left anterior descending coronary artery occlusion because this form of occlusion impairs left ventricular function. QUESTION 6 When inspecting a cardiovascular client, the nurse notes that he needs to sit upright to breathe. This behavior is most indicative of:A. Pericarditis B. Anxiety C. Congestive heart failure D. Angina Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Pericarditis can cause dyspnea but primarily causes chest pain. (B) Anxiety can cause dyspnea resulting in SOB, yet it is not typically influenced by degree of head elevation. (C) The inability to oxygenate well without being upright is most indicative of congestive heart failure, due to alveolar drowning. (D) Angina causes primarily chest pain; any SOB associated with angina is not influenced by body position. QUESTION 7 When a client questions the nurse as to the purpose of exercise electrocardiography (ECG) in the diagnosis of cardiovascular disorders, the nurse’s response should be based on the fact that: A. The test provides a baseline for further tests B. The procedure simulates usual daily activity and myocardial performance C. The client can be monitored while cardiac conditioning and heart toning are done D. Ischemia can be diagnosed because exercise increasesO2 consumption and demand Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) The purpose of the study is not to provide a baseline for further tests. (B) The test causes an increase in O2 demand beyond that required to perform usual daily activities. (C) Monitoring does occur, but the test is not for the purpose of cardiac toning and conditioning. (D) Exercise ECG, or stress testing, is designed to elevate the peripheral and myocardial needs for O2 to evaluate the ability of the myocardium and coronary arteries to meet the additional demands. QUESTION 8 In assessing cardiovascular clients with progression of aortic stenosis, the nurse should be aware that there is typically: A. Decreased pulmonary blood flow and cyanosis B. Increased pressure in the pulmonary veins and pulmonary edema C. Systemic venous engorgement D. Increased left ventricular systolic pressures and hypertrophy Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) These signs are seen in pulmonic stenosis or in response to pulmonary congestion and edema and mitral stenosis. (B) These signs are seen primarily in mitral stenosis or as a late sign in aortic stenosis after left ventricular failure. (C) These signs are seen primarily in right-sided heart valve dysfunction. (D) Leftventricular hypertrophy occurs to increase muscle mass and overcome the stenosis; left ventricular pressures increase as left ventricular volume increases owing to insufficient emptying. QUESTION 9 The cardiac client who exhibits the symptoms of disorientation, lethargy, and seizures may be exhibiting a toxic reaction to: A. Digoxin (Lanoxin) B. Lidocaine (Xylocaine) C. Quinidine gluconate or sulfate (Quinaglute,Quinidex) D. Nitroglycerin IV (Tridil) Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Side effects of digoxin include headache, hypotension, AV block, blurred vision, and yellow-green halos. (B) Side effects of lidocaine include heart block, headache, dizziness, confusion, tremor, lethargy, and convulsions. (C) Side effects of quinidine include heart block, hepatotoxicity, thrombocytopenia, and respiratory depression. (D) Side effects of nitroglycerin include postural hypotension, headache, dizziness, and flushing. QUESTION 10 Which of the following ECG changes would be seen as a positive myocardial stress test response? A. Hyperacute T wave B. Prolongation of the PR interval C. ST-segment depression D. Pathological Q wave Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Hyperacute T waves occur with hyperkalemia. (B) Prolongation of the P R interval occurs with firstdegree AV block. (C) Horizontal ST-segment depression of>1 mm during exercise isdefinitely a positive criterion on the exercise ECG test. (D) Patho-logical Q waves occur with MI. QUESTION 11 Assessment of the client with pericarditis may reveal which of the following? A. Ventricular gallop and substernal chest pain B. Narrowed pulse pressure and shortness of breath C. Pericardial friction rub and pain on deep inspiration D. Pericardial tamponade and widened pulse pressure Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation:(A) No S3 or S4 are noted with pericarditis. (B) No change in pulse pressure occurs. (C) The symptoms of pericarditis vary with the cause, but they usually include chest pain, dyspnea, tachycardia, rise in temperature, and friction rub caused by fibrin or other deposits. The pain seen with pericarditis typically worsens with deep inspiration. (D) Tamponade is not typically seen early on, and no change in pulse pressure occurs. QUESTION 12 Clinical manifestations seen in left-sided rather than in right-sided heart failure are: A. Elevated central venous pressure and peripheral edema B. Dyspnea and jaundice C. Hypotension and hepatomegaly D. Decreased peripheral perfusion and rales Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A, B, C) Clinical manifestations of right-sided heart failure are weakness, peripheral edema, jugular venous distention, hepatomegaly, jaundice, and elevated central venous pressure. (D) Clinical manifestations of left-sided heart failure are left ventricular dysfunction, decreased cardiac output, hypotension, and the backward failure as a result of increased left atrium and pulmonary artery pressures, pulmonary edema, and rales. QUESTION 13 Which classification of drugs is contraindicated for the client with hypertrophic cardiomyopathy? A. Positive inotropes B. Vasodilators C. Diuretics D. Antidysrhythmics Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Positive inotropic agents should not be administered owing to their action of increasing myocardial contractility. Increased ventricular contractility would increase outflow tract obstruction in the client with hypertrophic cardiomyopathy. (B) Vasodilators are not typically prescribed but are not contraindicated. (C) Diuretics are used with caution to avoid causing hypovolemia. (D) Antidysrhythmics are typically needed to treat both atrial and ventricular dysrhythmias. QUESTION 14 To ensure proper client education, the nurse should teach the client taking SL nitroglycerin to expect which of the following responses with administration? A. Stinging, burning when placed under the tongue B. Temporary blurring of vision C. Generalized urticaria with prolonged use D. Urinary frequency Correct Answer: ASection: Questions Set A Explanation Explanation/Reference: Explanation: (A) Stinging or burning when nitroglycerin is placed under the tongue is to be expected. This effect indicates that the medication is potent and effective for use. Failure to have this response means that the client needs to get a new bottle of nitroglycerin. (B, C, D) The other responses are not expected in this situation and are not even side effects. QUESTION 15 When a client is receiving vasoactive therapy IV, such as dopamine (Intropin), and extravasation occurs, the nurse should be prepared to administer which of the following medications directly into the site? A. Phentolamine (Regitine) B. Epinephrine C. Phenylephrine (Neo-Synephrine) D. Sodium bicarbonate Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Phentolamine is given to counteract the-adrenergic effects that cause ischemia and necrosis of local tissue. (B) Epinephrine is an endogenous catecholamine that produces vasoconstriction and increases heart rate and contractility. (C) Phenylephrine causes constriction of arterioles of skin, mucous membranes, and viscera, which in turn can cause ischemia and necrosis. (D) Sodium bicarbonate is an alkalinizing agent that is incompatible with dopamine. QUESTION 16 Which of the following would differentiate acute from chronic respiratory acidosis in the assessment of the trauma client? A. Increased PaCO2 B. Decreased PaO2 C. Increased HCO3 D. Decreased base excess Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Increased CO2 will occur in both acute and chronic respiratory acidosis. (B) Hypoxia does not determine acid-base status. (C) Elevation of HCO3 is a compensatory mechanism in acidosis that occurs almost immediately, but it takes hours to show any effect and days to reach maximum compensation. Renal disease and diuretic therapy may impair the ability of the kidneys to compensate. (D) Base excess is a nonrespiratory contributor to acid-base balance. It would increase to compensate for acidosis. QUESTION 17 Which of the following signs and symptoms indicates a tension pneumothorax as compared to an open pneumothorax?A. Ventilation-perfusion (V./Q.) mismatch B. Hypoxemia and respiratory acidosis C. Mediastinal tissue and organ shifting D. Decreased tidal volume and tachypnea Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A, B, D) These occur in both tension pneumothorax and open pneumothorax. (C) The tension pneumothorax acts like a one- way valve so that the pneumothorax increases with each breath. Eventually, it occupies enough space to shift mediastinal tissue toward the unaffected side away from the midline. Tracheal deviation, movement of point of maximum impulse, and decreased cardiac output will occur. The other three options will occur in both types of pneumothorax. QUESTION 18 Hematotympanum and otorrhea are associated with which of the following head injuries? A. Basilar skull fracture B. Subdural hematoma C. Epidural hematoma D. Frontal lobe fracture Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Basilar skull fractures are fractures of the base of the skull. Blood behind the eardrum or blood or cerebrospinal fluid (CSF) leaking from the ear are indicative of a dural laceration. Basilar skull fractures are the only type with these symptoms. (B, C, D) These do not typically cause dural lacerations and CSF leakage. QUESTION 19 A client with a C-3–4 fracture has just arrived in the emergency room. The primary nursing intervention is: A. Stabilization of the cervical spine B. Airway assessment and stabilization C. Confirmation of spinal cord injury D. Normalization of intravascular volume Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) If cervical spine injury is suspected, the airway should be maintained using the jaw thrust method that also protects the cervical spine. (B) Primary intervention is protection of the airway and adequate ventilation. (C, D) All other interventions are secondary to adequate ventilation. QUESTION 20In a client with chest trauma, the nurse needs to evaluate mediastinal position. This can best be done by: A. Auscultating bilateral breath sounds B. Palpating for presence of crepitus C. Palpating for trachial deviation D. Auscultating heart sounds Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) No change in the breath sounds occurs as a direct result of the mediastinal shift. (B) Crepitus can occur owing to the primary disorder, not to the mediastinal shift. (C) Mediastinal shift occurs primarily with tension pneumothorax, but it can occur with very large hemothorax or pneumothorax. Mediastinal shift causes trachial deviation and deviation of the heart’s point of maximum impulse. (D) No change in the heart sounds occurs as a result of the mediastinal shift. QUESTION 21 Priapism may be a sign of: A. Altered neurological function B. Imminent death C. Urinary incontinence D. Reproductive dysfunction Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Priapism in the trauma client is due to the neurological dysfunction seen in spinal cord injury. Priapism is an abnormal erection of the penis; it may be accompanied by pain and tenderness. This may disappear as spinal cord edema is relieved. (B) Priapism is not associated with death. (C) Urinary retention, rather than incontinence, may occur. (D) Reproductive dysfunction may be a secondary problem. QUESTION 22 When evaluating a client with symptoms of shock, it is important for the nurse to differentiate between neurogenic and hypovolemic shock. The symptoms of neurogenic shock differ from hypovolemic shock in that: A. In neurogenic shock, the skin is warm and dry B. In hypovolemic shock, there is a bradycardia C. In hypovolemic shock, capillary refill is less than 2 seconds D. In neurogenic shock, there is delayed capillary refill Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Neurogenic shock is caused by injury to the cervical region, which leads to loss of sympathetic control.This loss leads to vasodilation of the vascular beds, bradycardia resulting from the lack of sympathetic balance to parasympathetic stimuli from the vagus nerve, and the loss of the ability to sweat below the level of injury. In neurogenic shock, the client is hypotensive but bradycardiac with warm, dry skin. (B) In hypovolemic shock, the client ishypotensive and tachycardiac with cool skin. (C) In hypovolemic shock, the capillary refill would be>5 seconds. (D) In neurogenic shock, there is no capillary delay, the vascular beds are dilated, and peripheral flow is good. QUESTION 23 Which of the following would have the physiological effect of decreasing intracranial pressure (ICP)? A. Increased core body temperature B. Decreased serum osmolality C. Administration of hypo-osmolar fluids D. Decreased PaCO2 Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) An increase in core body temperature increases metabolism and results in an increase in ICP. (B) Decreased serum osmolality indicates a fluid overload and may result in an increase in ICP. (C) Hypoosmolar fluids are generally voided in the neurologically compromised. Using IV fluids such as D5W results in the dextrose being metabolized, releasing free water that is absorbed by the brain cells, leading to cerebral edema. (D) Hypercapnia and hypoventilation, which cause retention of CO2 and lead to respiratory acidosis, both increase ICP. CO2 is the most potent vasodilator known. QUESTION 24 A client who has sustained a basilar skull fracture exhibits blood-tinged drainage from his nose. After establishing a clear airway, administering supplemental O2, and establishing IV access, the next nursing intervention would be to: A. Pass a nasogastric tube through the left nostril B. Place a 4 X 4 gauze in the nares to impede the flow C. Gently suction the nasal drainage to protect the airway D. Perform a halo test and glucose level on the drainage Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Basilar skull fracture may cause dural lacerations, which result in CSF leaking from the ears or nose. Insertion of a tube could lead to CSF going into the brain tissue or sinuses. (B) Tamponading flow could worsen the problem and increase ICP. (C) Suction could increase brain damage and dislocate tissue. (D) Testing the fluid from the nares would determine the presence of CSF. Elevation of the head, notification of the medical staff, and prophylactic antibiotics are appropriate therapy. QUESTION 25 A client with a diagnosis of C-4 injury has been stabilized and is ready for discharge. Because this client is at risk for autonomic dysreflexia, he and his family should be instructed to assess for and report: A. Dizziness and tachypnea B. Circumoral pallor and lightheadedness C. Headache and facial flushingD. Pallor and itching of the face and neck Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Tachypnea is not a symptom. (B) Circumoral pallor is not a symptom. (C) Autonomic dysreflexia is an uninhibited and exaggerated reflex of the autonomic nervous system to stimulation, which results in vasoconstriction and elevated blood pressure. (D) Pallor and itching are not symptoms. QUESTION 26 The initial treatment for a client with a liquid chemical burn injury is to: A. Irrigate the area with neutralizing solutions B. Flush the exposed area with large amounts of water C. Inject calcium chloride into the burned area D. Apply lanolin ointment to the area Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) In the past, neutralizing solutions were recommended, but presently there is concern that these solutions extend the depth of burn area. (B) The use of large amounts of water to flush the area is recommended for chemical burns. (C) Calcium chloride is not recommended therapy and would likely worsen the problem. (D) Lanolin is of no benefit in the initial treatment of a chemical injury and may actually extend a thermal injury. QUESTION 27 The most important reason to closely assess circumferential burns at least every hour is that they may result in: A. Hypovolemia B. Renal damage C. Ventricular arrhythmias D. Loss of peripheral pulses Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Hypovolemia could be a result of fluid loss from thermal injury, but not as a result of the circumferential injury. (B) Renal damage is typically seen because of prolonged hypovolemia or myoglobinuria. (C) Electrical injuries and electrolyte changes typically cause arrhythmias in the burn client. (D) Full-thickness circumferential burns are nonelastic and result in an internal tourniquet effect that compromises distal blood flow when the area involved is an extremity.Circumferential full-thickness torso burns compromise respiratory motion and, when extreme, cardiac return. QUESTION 28 During burn therapy, morphine is primarily administered IV for pain management because this route:A. Delays absorption to provide continuous pain relief B. Facilitates absorption because absorption from muscles is not dependable C. Allows for discontinuance of the medication if respiratory depression develops D. Avoids causing additional pain from IM injections Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Absorption would be increased, not decreased. (B) IM injections should not be used until the client is hemodynamically stable and has adequate tissue perfusion. Medications will remain in the subcutaneous tissue with the fluid that is present in the interstitial spaces in the acute phase of the thermal injury. The client will have a poor response to the medication administered, and a “dumping” of the medication can occur when the medication and fluid are shifted back into the intravascular spaces in the next phase of healing. (C) IV administration of the medication would hasten respiratory compromise, if present. (D) The desire to avoid causing the client additional pain is not a primary reason for this route of administration. QUESTION 29 The medication that best penetrates eschar is: A. Mafenide acetate (Sulfamylon) B. Silver sulfadiazine (Silvadene) C. Neomycin sulfate (Neosporin) D. Povidone-iodine (Betadine) Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Mafenide acetate is bacteriostatic against gram-positive and gram-negative organisms and is the agent that best penetrates eschar. (B) Silver sulfadiazine poorly penetrates eschar. (C) Neomycin sulfate does not penetrate eschar. (D) Povidoneiodine does not penetrate eschar. QUESTION 30 When the nurse is evaluating lab data for a client 18–24 hours after a major thermal burn, the expected physiological changes would include which of the following? A. Elevated serum sodium B. Elevated serum calcium C. Elevated serum protein D. Elevated hematocrit Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Sodium enters the edema fluid in the burned area, lowering the sodium content of the vascular fluid. Hyponatremia may continue for days to several weeks because of sodium loss to edema, sodium shiftinginto the cells, and later, diuresis. (B) Hypocalcemia occurs because of calcium loss to edema fluid at the burned site (third space fluid). (C) Protein loss occurs at the burn site owing to increased capillary permeability. Serum protein levels remain low until healing occurs. (D) Hematocrit level is elevated owing to hemoconcentration from hypovolemia. Anemia is present in the postburn stage owing to blood loss and hemolysis, but it cannot be assessed until the client is adequately hydrated. QUESTION 31 The nurse notes hyperventilation in a client with a thermal injury. She recognizes that this may be a reaction to which of the following medications if applied in large amounts? A. Neosporin sulfate B. Mafenide acetate C. Silver sulfadiazine D. Povidone-iodine Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) The side effects of neomycin sulfate include rash, urticaria, nephrotoxicity, and ototoxicity. (B) The side effects of mafenide acetate include bone marrow suppression, hemolytic anemia, eosinophilia, and metabolic acidosis. The hyperventilation is a compensatory response to the metabolic acidosis. (C) The side effects of silver sulfadiazine include rash, itching, leukopenia, and decreased renal function. (D) The primary side effect of povidone- iodine is decreased renal function. QUESTION 32 The primary reason for sending a burn client home with a pressure garment, such as a Jobst garment, is that the garment: A. Decreases hypertrophic scar formation B. Assists with ambulation C. Covers burn scars and decreases the psychological impact during recovery D. Increases venous return and cardiac output by normalizing fluid status Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Tubular support, such as that received with a Jobst garment, applies tension of 10–20 mm Hg. This amount of uniform pressure is necessary to prevent or reduce hypertrophic scarring. Clients typically wear a pressure garment for 6–12 months during the recovery phase of their care. (B) Pressure garments have no ambulatory assistive properties. (C) Pressure garments can worsen the psychological impact of burn injury, especially if worn on the face. (D) Pressure garments do not normalize fluid status. QUESTION 33 A client with emphysema is placed on diuretics. In order to avoid potassium depletion as a side effect of the drug therapy, which of the following foods should be included in his diet? A. Celery B. Potatoes C. Tomatoes D. LiverCorrect Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Celery is high in sodium. (B) Potatoes are high in potassium. (C) Tomatoes are high in sodium. (D) Liver is high in iron. QUESTION 34 Which of the following would the nurse expect to find following respiratory assessment of a client with advanced emphysema? A. Distant breath sounds B. Increased heart sounds C. Decreased anteroposterior chest diameter D. Collapsed neck veins Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Distant breath sounds are found in clients with emphysema owing to increased anteroposterior chest diameter, overdistention, and air trapping. (B) Deceased heart sounds arepresent because of the increased anteroposterior chest diameter. (C) A barrel- shaped chest is characteristic of emphysema. (D) Increased distention of neck veins is found owing to right-sided heart failure, which may be present in advanced emphysema. QUESTION 35 The nurse assists a client with advanced emphysema to the bathroom. The client becomes extremely short of breath while returning to bed. The nurse should: A. Increase his nasal O2 to 6 L/min B. Place him in a lateral Sims’ position C. Encourage pursed-lip breathing D. Have him breathe into a paper bag Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Giving too high a concentration of O2 to a client with em-physema may remove his stimulus to breathe. (B) The client should sit forward with his hands on his knees or an overbed table and with shoulders elevated. (C) Pursed-lip breathing helps the client to blow off CO2 and to keep air passages open. (D) Covering the face of a client extremely short of breath may cause anxiety and further increase dyspnea. QUESTION 36 Signs and symptoms of an allergy attack include which of the following? A. Wheezing on inspiration B. Increased respiratory rateC. Circumoral cyanosis D. Prolonged expiration Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Wheezing occurs during expiration when air movement is impaired because of constricted edematous bronchial lumina. (B) Respirations are difficult, but the rate is frequently normal. (C) The circumoral area is usually pale. Cyanosis is not an early sign of hypoxia. (D) Expiration is prolonged because the alveoli are greatly distended and air trapping occurs. QUESTION 37 A 55-year-old man is admitted to the hospital with complaints of fatigue, jaundice, anorexia, and claycolored stools. His admitting diagnosis is “rule out hepatitis.” Laboratory studies reveal elevated liver enzymes and bilirubin. In obtaining his health history, the nurse should assess his potential for exposure to hepatitis. Which of the following represents a high-risk group for contracting this disease? A. Heterosexual males B. Oncology nurses C. American Indians D. Jehovah’s Witnesses Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Homosexual males, not heterosexual males, are at high risk for contracting hepatitis. (B) Oncology nurses are employed in high-risk areas and perform invasive procedures that expose them to potential sources of infection. (C) The literature does not support the idea that any ethnic groups are at higher risk. (D) There is no evidence that any religious groups are at higher risk. QUESTION 38 A diagnosis of hepatitis C is confirmed by a male client’s physician. The nurse should be knowledgeable of the differences between hepatitis A, B, and C. Which of the following are characteristics of hepatitis C? A. The potential for chronic liver disease is minimal. B. The onset of symptoms is abrupt. C. The incubation period is 2–26 weeks. D. There is an effective vaccine for hepatitis B, but not for hepatitis C. Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Hepatitis C and B may result in chronic liver disease. Hepatitis A has a low potential for chronic liver disease. (B) Hepatitis C and B have insidious onsets. Hepatitis A has an abrupt onset. (C) Incubation periods are as follows: hepatitis C is 2–26 weeks, hepatitis B is 6–20 weeks, and hepatitis A is 2–6 weeks.(D) Only hepatitis B has an effective vaccine. QUESTION 39 The nurse is aware that nutrition is an important aspect of care for a client with hepatitis. Which of the following diets would be most therapeutic? A. High protein and low carbohydrate B. Low calorie and low protein C. High carbohydrate and high calorie D. Low carbohydrate and high calorie Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Protein increases the workload of the liver. Increased carbohydrates provide needed calories and promote palatability. (B) Dietary intake should be adequate to ensure wound healing. (C) Increased carbohydrates provide needed calories. (D) A highcalorie diet is best obtained from carbohydrates because of their palatability. Fats increase the workload of the liver. QUESTION 40 Which of the following nursing orders should be included in the plan of care for a client with hepatitis C? A. The nurse should use universal precautions when obtaining blood samples. B. Total bed rest should be maintained until the client is asymptomatic. C. The client should be instructed to maintain a low semi-Fowler position when eating meals. D. The nurse should administer an alcohol backrub at bedtime. Correct Answer: A Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) The source of infection with hepatitis C is contaminated blood products. (B) Modified bed rest should be maintained while the client is symptomatic. Routine activities can be slowly resumed once the client is asymptomatic. (C) Nausea and vomiting occur frequently with hepatitis C. A high Fowler position may decrease the tendency to vomit. (D) The buildup of bilirubin in the client’s skin may cause pruritus. Alcohol is a drying agent. QUESTION 41 Which of the following should be included in discharge teaching for a client with hepatitis C? A. He should take aspirin as needed for muscle and joint pain. B. He may become a blood donor when his liver enzymes return to normal. C. He should avoid alcoholic beverages during his recovery period. D. He should use disposable dishes for eating and drinking. Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation:(A) Aspirin is hepatotoxic, may increase bleeding, and should be avoided. (B) Blood should not be donated by a client who has had hepatitis C because of the possibility of transmission of disease. (C) Alcohol is detoxified in the liver. (D) Hepatitis C is not spread through the oral route. QUESTION 42 A 27-year-old man was diagnosed with type I diabetes 3 months ago. Two weeks ago he complained of pain, redness, and tenderness in his right lower leg. He is admitted to the hospital with a slight elevation of temperature and vague complaints of “not feeling well.” At 4:30 PM on the day of his admission, his blood glucose level is 50 mg; dinner will be served at 5:00 PM. The best nursing action would be to: A. Give him 3 tbsp of sugar dissolved in 4 oz of grape juice to drink B. Ask him to dissolve three pieces of hard candy in his mouth C. Have him drink 4 oz of orange juice D. Monitor him closely until dinner arrives Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) The combination of sugar and juice will increase the blood sugar beyond the normal range. (B) Concentrated sweets are not absorbed as fast as juice; consequently, they elevate the blood sugar beyond the normal limit. (C) Four ounces of orange juice will act immediately to raise the blood sugar to a normal level and sustain it for 30 minutes until supper is served. (D) There is an increased potential for the client’s blood sugar to decrease even further, resulting in diabetic coma. QUESTION 43 A male client receives 10 U of regular human insulin SC at 9:00 AM. The nurse would expect peak action from this injection to occur at: A. 9:30 AM B. 10:30 AM C. 12 noon D. 4:00 PM Correct Answer: C Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) This is too early for peak action to occur. (B) This is too early for peak action to occur. (C) Regular insulin peak action occurs 2–4 hours after administration. (D) This is too late for peak action to occur. QUESTION 44 A type I diabetic client is diagnosed with cellulitis in his right lower extremity. The nurse would expect which of the following to be present in relation to his blood sugar level? A. A normal blood sugar level B. A decreased blood sugar level C. An increased blood sugar level D. Fluctuating levels with a predawn increase Correct Answer: C Section: Questions Set AExplanation Explanation/Reference: Explanation: (A) Blood sugar levels increase when the body responds to stress and illness. (B) Blood sugar levels increase when the body responds to stress and illness. (C) Hyperglycemia occurs because glucose is produced as the body responds to the stress and illness of cellulitis. (D) Blood sugar levels remain elevated as long as the body responds to stress and illness. QUESTION 45 The physician has ordered that a daily exercise program be instituted by a client with type I diabetes following his discharge from the hospital. Discharge instructions about exercise should include which of the following? A. Exercise should be performed 30 minutes before meals. B. A snack may be needed before and/or during exercise. C. Hyperglycemia may occur 2–4 hours after exercise. D. The blood glucose level should be 100 mg or below before exercise is begun. Correct Answer: B Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) Exercise should not be performed before meals because the blood sugar is usually lower just prior to eating; therefore, there is an increased risk for hypoglycemia. (B) Exercise lowers blood sugar levels; therefore, a snack may be needed to maintain the appropriate glucose level. (C) Exercise lowers blood sugar levels. (D) Exercise lowers blood sugar levels. If the blood glucose level is 100 mg or below at the start of exercise, the potential for hypoglycemia is greater. QUESTION 46 Dietary planning is an essential part of the diabetic client’s regimen. The American Diabetes Association recommends which of the following caloric guidelines for daily meal planning? A. 50% complex carbohydrate, 20%–25% protein, 20%–25% fat B. 45% complex carbohydrate, 25%–30% protein, 30%–35% fat C. 70% complex carbohydrate, 20%–30% protein, 10%–20% fat D. 60% complex carbohydrate, 12%–15% protein, 20%–25% fat Correct Answer: D Section: Questions Set A Explanation Explanation/Reference: Explanation: (A) The percentage of carbohydrates is too low to maintain blood sugar levels. The percent range of protein is too high and may cause extra workload on the kidney as it is metabolized. (B) The percentage of carbohydrates is too low to maintain blood sugar levels. The percent range of protein is too high and may cause extra workload on the kidney. (C) The percentage of carbohydrates is too high; the percent range of protein is too high, and of fat, too low. (D) This combination provides enough carbohydrates to maintain blood glucose levels, enough protein to maintain body repair, and enough fat to ensure palatability. QUESTION 47 A 74-year-old female client is 3 days postoperative. She has an indwelling catheter and has been progressing well. While the nurse is in the room, the client states, “Oh dear, I feel like I have to urinate again!” Which of the following is the most appropriate initial nursing response?A. Assure her that this is most likely the result of bladder spasms. B. Check the collection bag and tubing to verify that the catheter is draining properly. C. Instruct her to do Kegel exercises to diminish the urge to void. D. Ask her if she has felt this way before. Correct Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Although this may be an appropriate response, the initial response would be to assure the patency of the catheter. (B) The most frequent reason for an urge to void with an indwelling catheter is blocked tubing. This response would be the best initial response. (C) Kegel exercises while a retention catheter is in place would not help to prevent a voiding urge and could irritate the urethral sphincter. (D) Though the nurse would want to ascertain whether the client has felt the same urge to void before, the initial response should be to assure the patency of the catheter. QUESTION 48 In cleansing the perineal area around the site of catheter insertion, the nurse would: A. Wipe the catheter toward the urinary meatus B. Wipe the catheter away from the urinary meatus C. Apply a small amount of talcum powder after drying the perineal area D. Gently insert the catheter another 1⁄2 inch after cleansing to prevent irritation from the balloon Correct Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Wiping toward the urinary meatus would transport microorganisms from the external tubing to the urethra, thereby increasing the risk of bladder infection. (B) Wiping away from the urinary meatus would remove microorganisms from the point of insertion of the catheter, thereby decreasing the risk of bladder infection. (C) Talcum powder should not be applied following catheter care, because powders contribute to moisture retention and infection likelihood. (D) The catheter should never be inserted further into the urethra, because this would serve no useful purpose and would increase the risk of infection. QUESTION 49 Nursing interventions designed to decrease the risk of infection in a client with an indwelling catheter include: A. Cleanse area around the meatus twice a day B. Empty the catheter drainage bag at least daily C. Change the catheter tubing and bag every 48 hours D. Maintain fluid intake of 1200–1500 mL every day Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation:(A) Catheter site care is to be done at least twice daily to prevent pathogen growth at the catheter insertion site. (B) Catheter drainage bags are usually emptied every 8 hours to prevent urine stasis and pathogen growth. (C) Tubing and collection bags are not changed this often, because research studies have not demonstrated the efficacy of this practice. (D) Fluid intake needs to be in the 2000–2500 mL range if possible to help irrigate the bladder and prevent infection. QUESTION 50 A client tells the nurse that she has had a history of urinary tract infections. The nurse would do further health teaching if she verbalizes she will: A. Drink at least 8 oz of cranberry juice daily B. Maintain a fluid intake of at least 2000 mL daily C. Wash her hands before and after voiding D. Limit her fluid intake after 6 PM so that there is not a great deal of urine in her bladder while she sleeps Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Cranberry juice helps to maintain urine acidity, thereby retarding bacterial growth. (B) A generous fluid intake will help to irrigate the bladder and to prevent bacterial growth within the bladder. (C) Hand washing is an effective means of preventing pathogen transmission. (D) Restricting fluid intake would contribute to urinary stasis, which in turn would contribute to bacterial growth. QUESTION 51 An 83-year-old client has been hospitalized following a fall in his home. He has developed a possible fecal impaction. Which of the following assessment findings would be most indicative of a fecal impaction? A. Boardlike, rigid abdomen B. Loss of the urge to defecate C. Liquid stool D. Abdominal pain Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) A boardlike, rigid abdomen would point to a perforated bowel, not a fecal impaction. (B) When a client is fecally impacted, a common symptom is the urge to defecate but the inability to do so. (C) When an impaction is present, only liquid stool will be able to pass around the impacted site. (D) Abdominal pain without distention is not a sign of a fecal impaction. QUESTION 52 The nurse provides a male client with diet teaching so that he can help prevent constipation in the future. Which food choices indicate that this teaching has been understood? A. Omelette and hash browns B. Pancakes and syrup C. Bagel with cream cheese D. Cooked oatmeal and grapefruit half Correct Answer: D Section: Question Set BExplanation Explanation/Reference: Explanation: (A) Eggs and hash browns do not provide much fiber and bulk, so they do not effectively prevent constipation. (B) Pancakes and syrup also have little fiber and bulk, so they do not effectively prevent constipation. (C) Bagel and cream cheese do not provide intestinal bulk. (D) A combination of oatmeal and fresh fruit will provide fiber and intestinal bulk. QUESTION 53 One of the medications that is prescribed for a male client is furosemide (Lasix) 80 mg bid. To reduce his risk of falls, the nurse would teach him to take this medication: A. On arising and no later than 6 PM B. At evenly spaced intervals, such as 8 AM and 8 PM C. With at least one glass of water per pill D. With breakfast and at bedtime Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation: (A) This option provides adequate spacing of the medication and will limit the client’s need to get up to go to the bathroom during the night hours, when he is especially at high risk for falls. (B) This option would result in the need to get up during the night to urinate and would thus increase the risk of falls. This option also does not take into consideration the client’s usual daily routine. (C) Taking this medication with at least one glass of water would not have an impact on the risk of falls. (D) This option would result in the need to get up during the night to urinate and would thus increase the risk of falls. QUESTION 54 The nurse teaches a male client ways to reduce the risks associated with furosemide therapy. Which of the following indicates that he understands this teaching? A. “I’ll be sure to rise slowly and sit for a few minutes after lying down.” B. “I’ll be sure to walk at least 2–3 blocks every day.” C. “I’ll be sure to restrict my fluid intake to four or five glasses a day.” D. “I’ll be sure not to take any more aspirin while I amon this drug.” Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation: (A) This response will help to prevent the occurrence of postural hypotension, a common side effect of this drug and a common reason for falls. (B) Although walking is an excellent exercise, it is not specific to the reduction of risks associated with diuretic therapy. (C) Clients on diuretic therapy are generally taught to ensure that their fluid intake is at least 2000–3000 mL daily, unless contraindicated. (D) Aspirin is a safe drug to take along with furosemide. QUESTION 55 A client is taught to eat foods high in potassium. Which food choices would indicate that this teaching has been successful?A. Pork chop, baked acorn squash, brussel sprouts B. Chicken breast, rice, and green beans C. Roast beef, baked potato, and diced carrots D. Tuna casserole, noodles, and spinach Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Both acorn squash and brussels sprouts are potassium-rich foods. (B) None of these foods is considered potassium rich. (C) Only the baked potato is a potassium-rich food. (D) Spinach is the only potassium-rich food in this option. QUESTION 56 The nurse would be sure to instruct a client on the signs and symptoms of an eye infection and hemorrhage. These signs and symptoms would include: A. Blurred vision and dizziness B. Eye pain and itching C. Feeling of eye pressure and headache D. Eye discharge and hemoptysis Correct Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Although blurred vision may occur, dizziness would not be associated with an infection or hemorrhage. (B) Eye pain is a symptom of hemorrhage within the eye, and itching is associated with infection. (C) Nausea and headache would not be usual symptoms of eye hemorrhage or infection. (D) Some eye discharge might be anticipated if an infection is present; hemoptysis would not. QUESTION 57 The nurse would teach a male client ways to minimize the risk of infection after eye surgery. Which of the following indicates the client needs further teaching? A. “I will wash my hands before instilling eye medications.” B. “I will wear sunglasses when going outside.” C. “I will wear an eye patch for the first 3 postoperative days.” D. “I will maintain the sterility of the eye medications.” Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Hand washing would be an important action designed to prevent transmission of pathogens from the hands to the eye. (B) Wearing sunglasses when going outside will prevent airborne pathogens from entering the eye. (C) Eye patches are most frequently ordered to be worn while the client sleeps or naps, not constantly for this length of time. (D) Eye medications are sterile; clients need to be taught how to maintain this sterility.QUESTION 58 With a geriatric client, the nurse should also assess whether he has been obtaining a yearly vaccination against influenza. Why is this assessment important? A. Influenza is growing in our society. B. Older clients generally are sicker than others when stricken with flu. C. Older clients have less effective immune systems. D. Older clients have more exposure to the causative agents. Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Although influenza is common, the elderly are more at risk because of decreased effectiveness of their immune system, not because the incidence is increasing. (B) Older clients have the same degree of illness when stricken as other populations. (C) As people age, their immune system becomes less effective, increasing their risk for influenza. (D) Older clients have no more exposure to the causative agents than do school-age children, for example. QUESTION 59 In evaluating the laboratory results of a client with severe pressure ulcers, the nurse finds that her albumin level is low. A decrease in serum albumin would contribute to the formation of pressure ulcers because: A. The proteins needed for tissue repair are diminished. B. The iron stores needed for tissue repair are inadequate. C. A decreased serum albumin level indicates kidney disease. D. A decreased serum albumin causes fluid movement into the blood vessels, causing dehydration. Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Serum albumin levels indicate the adequacy of protein stores available for tissue repair. (B) Serum albumin does not measure iron stores. (C) Serum albumin levels do not measure kidney function. (D) A decreased serum albumin level would cause fluid movement out of blood vessels, not into them. QUESTION 60 Which of the following menu choices would indicate that a client with pressure ulcers understands the role diet plays in restoring her albumin levels? A. Broiled fish with rice B. Bran flakes with fresh peaches C. Lasagna with garlic bread D. Cauliflower and lettuce salad Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation:(A) Broiled fish and rice are both excellent sources of protein. (B) Fresh fruits are not a good source of protein. (C) Foods in the bread group are not high in protein. (D) Most vegetables are not high in protein; peas and beans are the major vegetables higher in protein. QUESTION 61 The nurse observes that a client has difficulty chewing and swallowing her food. A nursing response designed to reduce this problem would include: A. Ordering a full liquid diet for her B. Ordering five small meals for her C. Ordering a mechanical soft diet for her D. Ordering a puréed diet for her Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Full liquids would be difficult to swallow if the muscle control of the swallowing act is affected; this is a probable reason for her difficulties, given her medical diagnosis of multiple sclerosis. (B) Five small meals would do little if anything to decrease her swallowing difficulties, other than assure that she tires less easily. (C) A mechanical soft diet should be easier to chew and swallow, because foods would be more evenly consistent. (D) A pureed diet would cause her to regress more than might be needed; the mechanical soft diet should be tried first. QUESTION 62 When a client with pancreatitis is discharged, the nurse needs to teach him how to prevent another occurrence of acute pancreatitis. Which of the following statements would indicate he has an understanding of his disease? A. “I will not eat any raw or uncooked vegetables.” B. “I will limit my alcohol to one cocktail per day.” C. “I will look into attending Alcoholics Anonymous meetings.” D. “I will report any changes in bowel movements to my doctor.” Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Raw or uncooked vegetables are all right to eat postdischarge. (B) This client must avoid any alcohol intake. (C) The client displays awareness of the need to avoid alcohol. (D) This action would be pertinent only if fatty stools associated with chronic hepatitis were the problem. QUESTION 63 A 54-year-old client is admitted to the hospital with a possible gastric ulcer. He is a heavy smoker. When discussing his smoking habits with him, the nurse should advise him to: A. Smoke low-tar, filtered cigarettes B. Smoke cigars instead C. Smoke only right after meals D. Chew gum instead Correct Answer: CSection: Question Set B Explanation Explanation/Reference: Explanation: (A, B, D) Cigarettes, cigars, and chewing gum would stimulate gastric acid secretion. (C) Smoking on a full stomach minimizes effect of nicotine on gastric acid. QUESTION 64 Iron dextran (Imferon) is a parenteral iron preparation. The nurse should know that it: A. Is also called intrinsic factor B. Must be given in the abdomen C. Requires use of the Z-track method D. Should be given SC Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Intrinsic factor is needed to absorb vitamin B12.(B) Iron dextran is given parenterally, but Z-track in a large muscle. (C) A Ztrack method of injection is required to prevent staining and irritation of the tissue. (D) An SC injection is not deep enough and may cause subcutaneous fat abscess formation. QUESTION 65 A nasogastric (NG) tube inserted preoperatively is attached to low, intermittent suctions. A client with an NG tube exhibits these symptoms: He is restless; serum electrolytes are Na 138, K 4.0, blood pH 7.53. This client is most likely experiencing: A. Hyperkalemia B. Hyponatremia C. Metabolic acidosis D. Metabolic alkalosis Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Sodium level is within normal limits. (B) Sodium level is within normal limits. (C) pH level is consistent with alkalosis. (D) With an NG tube attached to low, intermittent suction, acids are removed and a client will develop metabolic alkalosis. QUESTION 66 A client is experiencing muscle weakness and lethargy. His serum K+is 3.2. What other symptoms might he exhibit? A. Tetany B. Dysrhythmias C. Numbness of extremities D. HeadacheCorrect Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Tetany is seen with low calcium. (B) Low potassium causes dysrhythmias because potassium is responsible for cardiac muscle activity. (C) Numbness of extremities is seen with high potassium. (D) Headache is not associated with potassium excess or deficiency. QUESTION 67 Following a gastric resection, which of the following actions would the nurse reinforce with the client in order to alleviate the distress from dumping syndrome? A. Eating three large meals a day B. Drinking small amounts of liquids with meals C. Taking a long walk after meals D. Eating a low-carbohydrate diet Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Six small meals are recommended. (B) Liquids after meals increase the time food empties from the stomach. (C) Lying down after meals is recommended to prevent gravity from producing dumping. (D) A low-carbohydrate diet will prevent a hypertonic bolus, which causes dumping. QUESTION 68 Azulfidine (Sulfasalazine) may be ordered for a client who has ulcerative colitis. Which of the following is a nursing implication for this drug? A. Limit fluids to 500 mL/day. B. Administer 2 hours before meals. C. Observe for skin rash and diarrhea. D. Monitor blood pressure, pulse. Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Fluids up to 2500–3000 mL/day are needed to prevent kidney stones. (B) The client should be instructed to take oral preparations with meals or snacks to lessen gastric irritation. (C) Sulfasalazine causes skin rash and diarrhea. (D) Blood pressure and pulse are not altered by sulfasalazine. QUESTION 69 Other drugs may be ordered to manage a client’s ulcerative colitis. Which of the following medications, if ordered, would the nurse question? A. Methylprednisolone sodium succinate (Solu-Medrol) B. Loperamide (Imodium)C. Psyllium D. 6-Mercaptopurine Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Methylprednisolone sodium succinate is used for its anti-inflammatory effects. (B) Loperamide would be used to control diarrhea. (C) Psyllium may improve consistency of stools by providing bulk. (D) An immunosuppressant such as 6-mercaptopurine is used for chronic unrelenting Crohn’s disease. QUESTION 70 A male client is scheduled for a liver biopsy. In preparing him for this test, the nurse should: A. Explain that he will be kept NPO for 24 hours before the exam B. Practice with him so he will be able to hold his breath for 1 minute C. Explain that he will be receiving a laxative to prevent a distended bowel from applying pressure on the liver D. Explain that his vital signs will be checked frequently after the test Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) There is no NPO restriction prior to a liver biopsy. (B) The client would need to hold his breath for 5–10 seconds. (C) There is no pretest laxative given. (D) Following the test, the client is watched for hemorrhage and shock. QUESTION 71 After a liver biopsy, the best position for the client is: A. High Fowler B. Prone C. Supine D. Right lateral Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) This position does not help to prevent bleeding. (B) This position does not help to prevent bleeding. (C) This position does not help to prevent bleeding. (D) The right lateral position would allow pressure on the liver to prevent bleeding. QUESTION 72 A complication for which the nurse should be alert following a liver biopsy is: A. Hepatic coma B. JaundiceC. Ascites D. Shock Correct Answer: D Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Hepatic coma may occur in liver disease due to the increased NH3levels, not due to liver biopsy. (B) Jaundice may occur due to increased bilirubin levels, not due to liver biopsy. (C) Ascites would occur due to portal hypertension, not due to liver biopsy. (D) Hemorrhage and shock are the most likely complications after liver biopsy because of already existing bleeding tendencies in the vascular makeup of the liver. QUESTION 73 Which nursing implication is appropriate for a client undergoing a paracentesis? A. Have the client void before the procedure. B. Keep the client NPO. C. Observe the client for hypertension following the procedure. D. Place the client on the right side following the procedure. Correct Answer: A Section: Question Set B Explanation Explanation/Reference: Explanation: (A) A full bladder would impede withdrawal of ascitic fluid. (B) Keeping the client NPO is not necessary. (C) The client may exhibit signs and symptoms of shock and hypertension. (D) No position change is needed after the procedure. QUESTION 74 The nurse would assess the client’s correct understanding of the fertility awareness methods that enhance conception, if the client stated that: A. “My sexual partner and I should have intercourse when my cervical mucosa is thick and cloudy.” B. “At ovulation, my basal body temperature should rise about 0.5F.” C. “I should douche immediately after intercourse.” D. “My sexual partner and I should have sexual intercourse on day 14 of my cycle regardless of the length of the cycle.” Correct Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation: (A) At ovulation, the cervical mucus is increased, stretchable, and watery clear. (B) Under the influence of progesterone, the basal body temperature increases slightly after ovulation. (C) To enhance fertility, measures should be taken that promote retention of sperm rather than removal. (D) Ovulation, the optimal time for conception, occurs 14+2 days before the next menses; therefore, the date of ovulation is directly related to the length of the menstrual cycle. QUESTION 75A couple is planning the conception of their first child. The wife, whose normal menstrual cycle is 34 days in length, correctly identifies the time that she is most likely to ovulate if she states that ovulation should occur on day: A. 14+2 days B. 16+2 days C. 20+2 days D. 22+2 days Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Ovulation is dependent on average length of menstrual cycle, not standard 14 days. (B) Ovulation occurs 14+2 days before next menses (34 minus 14 does not equal 16). (C) Ovulation occurs 14+2 days before next menses (34 minus 14 equals 20). (D) Ovulation occurs 14+2 days before next menses (34 minus 14 does not equal 22). QUESTION 76 A client is pregnant with her second child. Her last menstrual period began on January 15. Her expected date of delivery would be: A. October 8 B. October 15 C. October 22 D. October 29 Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) Incorrect application of Nägele’s rule: correctly subtracted 3 months but subtracted 7 days rather than added. (B) Incorrect application of Nägele’s rule: correctly subtracted 3 months but did not add 7 days. (C) Correct application of Nägele’s rule: correctly subtracted 3 months and added 7 days. (D) Incorrect application of Nägele’s rule: correctly subtracted 3 months but added 14 days instead of 7 days. QUESTION 77 The nurse instructs a pregnant client (G2P1) to rest in a side-lying position and avoid lying flat on her back. The nurse explains that this is to avoid “vena caval syndrome,” a condition which: A. Occurs when blood pressure increases sharply with changes in position B. Results when blood flow from the extremities is blocked or slowed C. Is seen mainly in first pregnancies D. May require medication if positioning does not help Correct Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation:(A) Blood pressure changes are predominantly due to pressure of the gravid uterus. (B) Pressure of the gravid uterus on the inferior vena cava decreases blood return from lower extremities. (C) Inferior vena cava syndrome is experienced in the latter months of pregnancy regardless of parity. (D) There are no medications useful in the treatment of interior vena cava syndrome; alleviating pressure by position changes is effective. QUESTION 78 A pregnant client comes to the office for her first prenatal examination at 10 weeks. She has been pregnant twice before; the first delivery produced a viable baby girl at 39 weeks 3 years ago; the second pregnancy produced a viable baby boy at 36 weeks 2 years ago. Both children are living and well. Using the GTPAL system to record her obstetrical history, the nurse should record: A. 3-2-0-0-2 B. 2-2-0-2-2 C. 3-1-1-0-2 D. 2-1-1-0-2 Correct Answer: C Section: Question Set B Explanation Explanation/Reference: Explanation: (A) This answer is an incorrect application of the GTPAL method. One prior pregnancy was a preterm birth at 36 weeks (T =1, P= 1; not T = 2). (B) This answer is an incorrect application of the GTPAL method. The client is currently pregnant for the third time (G = 3, not 2), one prior pregnancy was preterm (T= 1, P= 1; not T= 2), and she has had no prior abortions (A =0). (C) This answer is the correct application of GTPAL method. The client is currently pregnant for the third time (G =3), her first pregnancy ended at term (>37 weeks) (T = 1), her second pregnancy ended preterm 20– 33 weeks) (P = 1), she has no history of abortion (A=0), and she has two living children (L = 2). (D) This answer is an incorrect application of the GTPAL method. The client is currently pregnant for the third time (G =3, not 2). QUESTION 79 A pregnant client comes to the office for her first prenatal examination at 10 weeks. She has been pregnant twice before; the first delivery produced a viable baby girl at 39 weeks 3 years ago; the second pregnancy produced a viable baby boy at 36 weeks 2 years ago. Both children are living and well. Using the gravida and para system to record the client’s obstetrical history, the nurse should record: A. Gravida 3 para 1 B. Gravida 3 para 2 C. Gravida 2 para 1 D. Gravida 2 para 2 Correct Answer: B Section: Question Set B Explanation Explanation/Reference: Explanation: (A) This answer is an incorrect application of gravida and para. The client has had two prior deliveries of more than 20 weeks’ gestation; therefore, para equals 2, not 1. (B) This answer is the correct application of gravida and para. The client is currently pregnant for the third time (G = 3), regardless of the length of the pregnancy, and has had two prior pregnancies with birth after the 20th week (P = 2), whether infant was alive or dead. (C) This answer is an incorrect application of gravida and para. The client is currently pregnant for the third time (G = 3, not 2); prior pregnancies lasted longer than 20 weeks (therefore, P = 2, not 1). (D) This is an incorrect application of gravida and para. Client is currently pregnant for third time (G = 3, not 2) [Show More]
Last updated: 1 year ago
Preview 1 out of 204 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 08, 2021
Number of pages
204
Written in
Additional information
This document has been written for:
Uploaded
Aug 08, 2021
Downloads
0
Views
39