*NURSING > CASE STUDY > Sheila Dalton, 52 Years UNFOLDING Reasoning Case Study: STUDENT Post-op Pain Management 2/2: Cardiac (All)
Sheila Dalton, 52 Years UNFOLDING Reasoning Case Study: STUDENT Post-op Pain Management 2/2: Cardiac Arrest
Document Content and Description Below
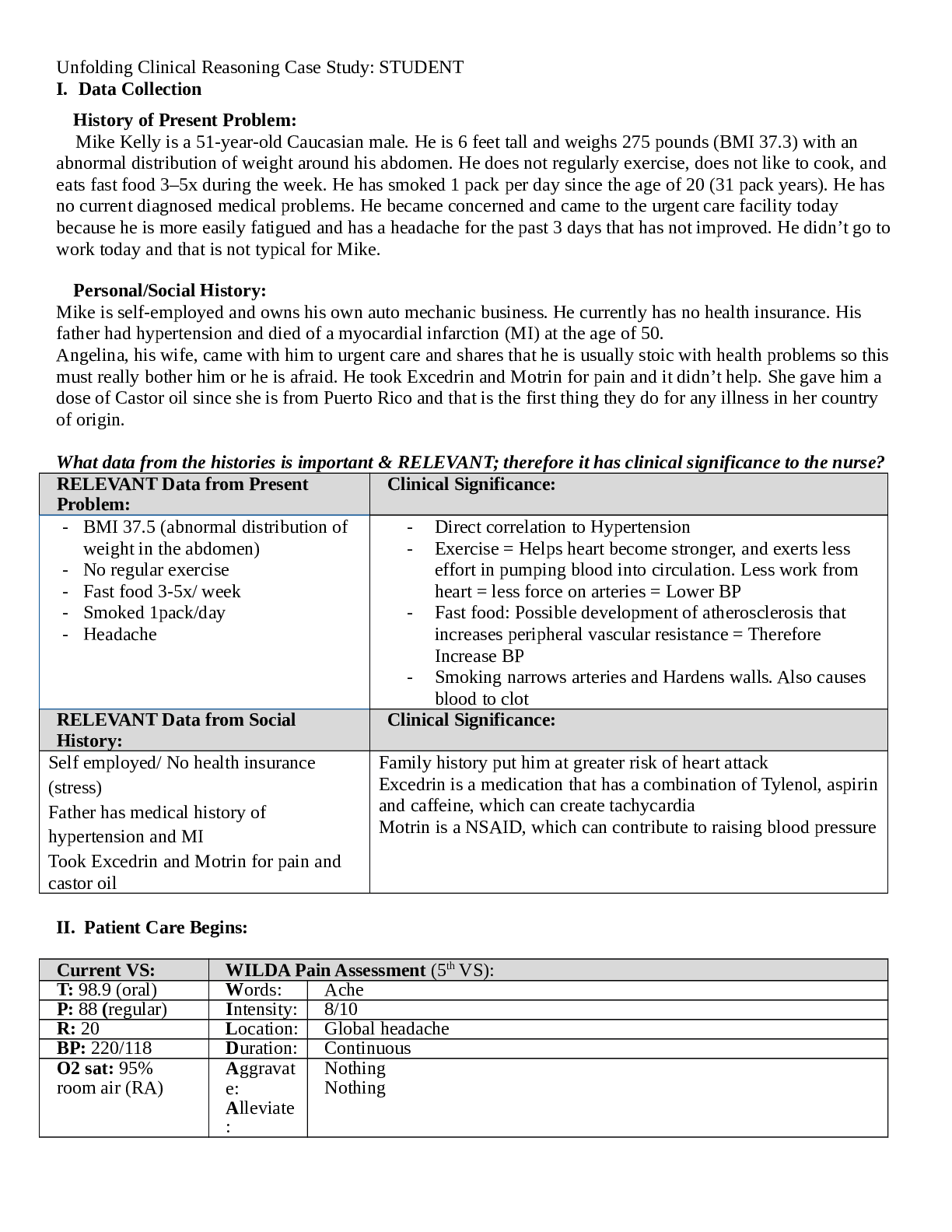
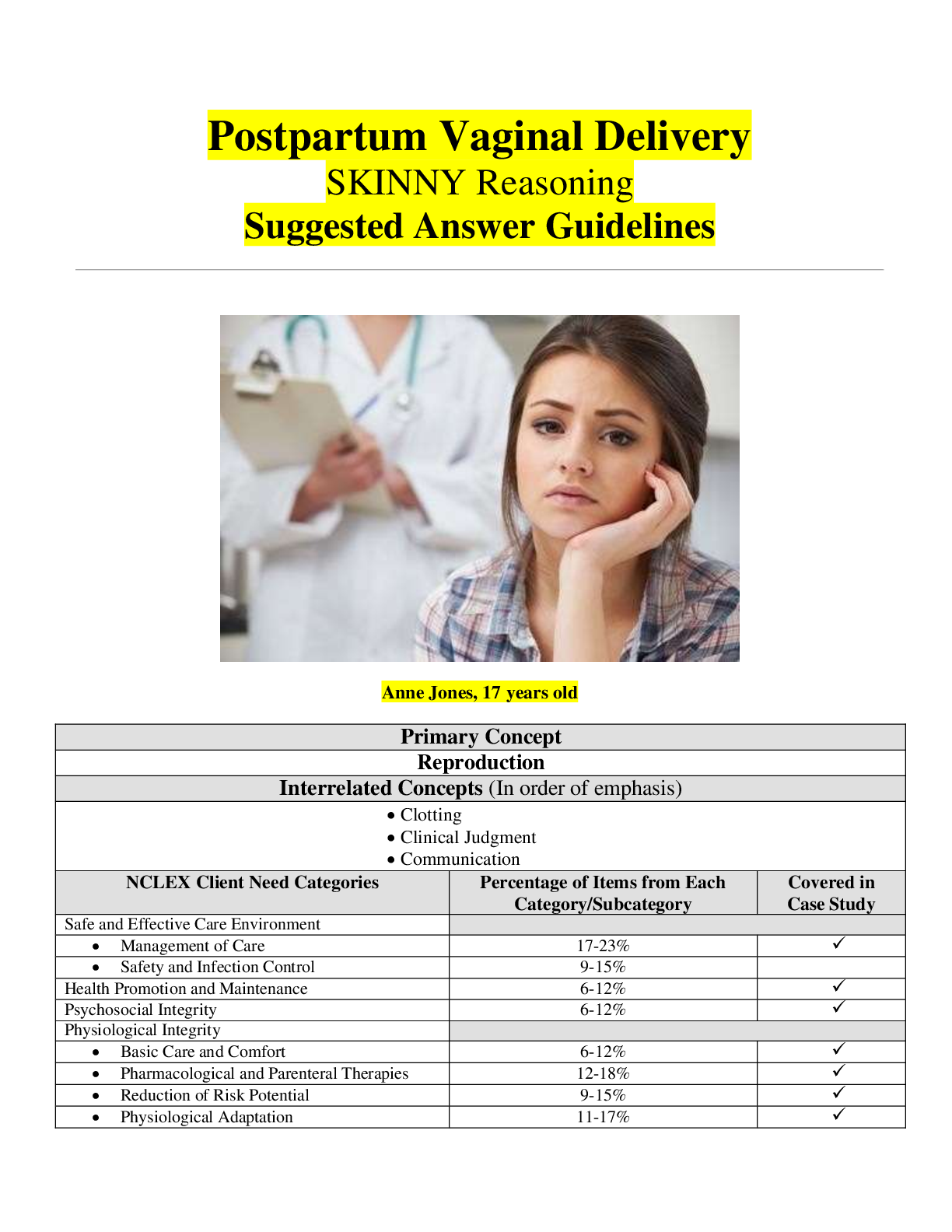
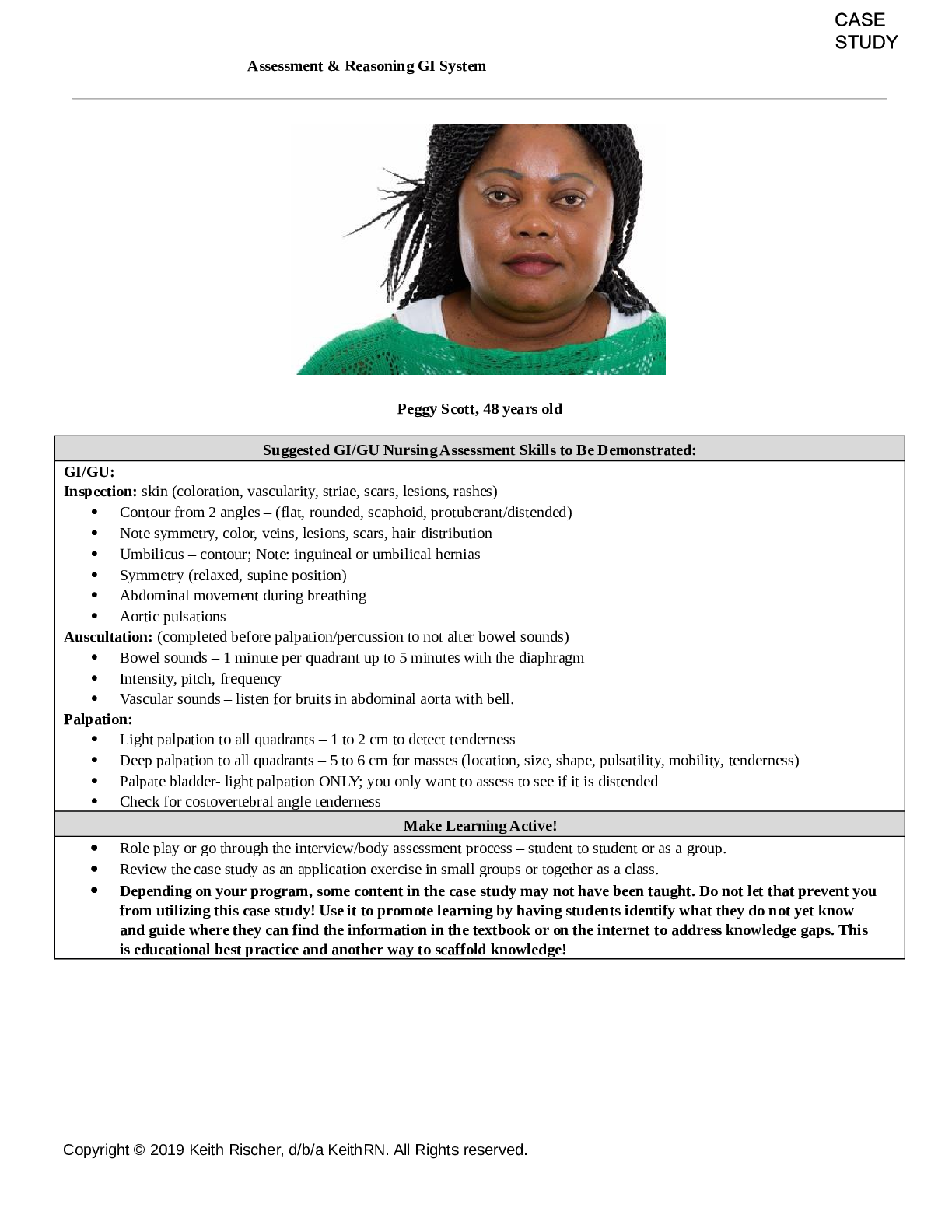
Post-op Pain Management 2/2: Cardiac Arrest History of Present Problem: Sheila Dalton is a 52-year-old woman who has a history of chronic low back pain and COPD. She had a posterior spinal fusion o... f L4-S1 earlier today. Her pain is currently controlled at 2/10 and increases with movement. She was started on a hydromorphone patient-controlled analgesia (PCA) with IV bolus dose that is 0.2 mg and continuous rate of 0.2 mg/hour. The nurse reported that her nausea has improved after receiving ondansetron IV four hours ago. She was having increased pain despite using the PCA every 10 minutes. Her pain has decreased from 6/10 to 2/10 since the PCA bolus was increased from 0.1 mg to 0.2 mg of hydromorphone IV one hour ago. Patient Care Begins: RELEVANT Data from History: Clinical Significance: COPD Chronic low back pain Recent spinal fusion surgery Hydromorphone use with worsened pain Nausea, relieved with Zofran Low SpO2 89% Low BP 92/48 History of respiratory issues, likely retains CO2, potential alveoli dysfunction Use of pain medication with chronic back pain? Post-op day 0, need to assess for surgical complications/expected findings, risk for infection/bleeding Narcotic use (decr. RR) Low oxygenation status on 4L NC Is BP complication of meds, sign of bleeding? Current VS: T: 99.8 F/37.7 C (oral) P: 78 R: 12 BP: 92/48 O2 sat: 89% room air 4 liters n/c Your shift continues... Thirty minutes later she is feeling more nauseated, and you administer ondansetron 4 mg IV push prn. Five minutes later she puts the call light on again. You are not able to respond immediately because you are helping your other patient get on the commode. Little do you know that Sheila is going to depend on your ability to THINK LIKE A NURSE and clinically reason to save her life. When you arrive in her room you observe the following... © 2016 Keith Rischer/www.KeithRN.com What assessment data is RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: Unresponsive Ashen pale Minimal resp. effort Liquid emesis in mouth Weak carotid pulse 24 bpm Does not awake or arouse to painful stimuli signs of cardiac arrest, heart is not pumping blood and shunting to core is likely occurring Loss of consciousness from sudden lack of blood flow Aspiration of gastric contents during arrest could have occurred Needs immediate intervention!!! Current VS: T: not assessed P: 24 R: 4 BP: 72/40 O2 sat: 76% 4 liters n/c What VS data is RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: HR 24 RR 4 BP 72/40 O2 76% This is still consistent with cardiac arrest, the heart has suddenly stopped pumping blood resulting in bradycardia, hypotension, and loss of perfusion to brain, minimal to no respiratory effort is occurring Clinical Reasoning Begins... 1. What is the primary problem that your patient is most likely presenting with? Cardiac Arrest 2. What is the underlying cause/pathophysiology of the primary problem? The heart suddenly stops pumping blood due to an electrical malfunction. 3. What nursing priority(ies) will guide your plan of care? (if more than one-list in order of PRIORITY) CABC… Compressions, airway, breathing, then circulation. Call for help and immediately perform compressions to start perfusing the tissues. Maintain patent airway, potential for intubation. Manually breath patient with ambu bag. Perform defibrillation to allow the SA node to take control of the electrical impulses of the heart for return to functioning. Airway, Breathing, Circulation! © 2016 Keith Rischer/www.KeithRN.com 4. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Expected Outcome: Compressions Ambu bag breathing Defibrillation Manual pumping of the heart to perfuse the tissues Oxygenate the pt during CPR between compressions Allow the SA node to take over control of the heart improved circulation Improved oxygenation Return of heart functioning 5. What body system(s) will you most thoroughly assess based on the primary/priority concern? Respiratory and Cardiovascular 6. What is the worst possible/most likely complication to anticipate? Sudden Cardiac Death or organ failure from lack of blood flow 7. What nursing assessments will identify this complication EARLY if it develops? Attaching pt to monitor to assess heart rate/rhythm to monitor for improvement, monitor pt response to interventions, does pt become responsive or breath independently?, assessing perfusion and vital signs to see if there is adequate cerebral blood flow 8. What nursing interventions will you initiate if this complication develops? Continue resuscitation and assess extent of organ damage if possible… Comfort care and family support is SCD occurs. A crash cart is brought into the .........................CONTINUED [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 02, 2021
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Sep 02, 2021
Downloads
0
Views
77


.png)
 SHEILA DALTON.png)