*NURSING > EXAM > NR 340 Week 7 Exam Three – Questions & Answers (View Questions) PLUS Rationales | (Traumatic brain (All)
NR 340 Week 7 Exam Three – Questions & Answers (View Questions) PLUS Rationales | (Traumatic brain injury, Global Rationale) | Already Graded A+
Document Content and Description Below
NR 340 Week 7 Exam Three – Questions & Answers (View Questions) 1) A client admitted to the hospital with a subarachnoid hemorrhage has complaints of severe headache, nuchal rigidity, and proje... ctile vomiting. The nurse knows lumbar puncture (LP) would be contraindicated in this client in which of the following circumstances? 1. Vomiting continues 2. Intracranial pressure (ICP) is increased 3. The client needs mechanical ventilation 4. Blood is anticipated in the cerebralspinal fluid (CSF) 2. Sudden removal of CSF results in pressures lower in the lumbar area than the brain and favors herniation of the brain; therefore, LP is contraindicated with increased ICP. Vomiting may be caused by reasons other than increased ICP; therefore, LP isn’t strictly contraindicated. An LP may be preformed on clients needing mechanical ventilation. Blood in the CSF is diagnostic for subarachnoid hemorrhage and was obtained before signs and symptoms of ICP. 2) A client with a subdural hematoma becomes restless and confused, with dilation of the ipsilateral pupil. The physician orders mannitol for which of the following reasons? 1. To reduce intraocular pressure 2. To prevent acute tubular necrosis 3. To promote osmotic diuresis to decrease ICP 4. To draw water into the vascular system to increase blood pressure 3. Mannitol promotes osmotic diuresis by increasing the pressure gradient, drawing fluid from intracellular to intravascular spaces. Although mannitol is used for all the reasons described, the reduction of ICP in this client is a concern. 3) A client with subdural hematoma was given mannitol to decrease intracranial pressure (ICP). Which of the following results would best show the mannitol was effective? 1. Urine output increases 2. Pupils are 8 mm and nonreactive 3. Systolic blood pressure remains at 150 mm Hg 4. ICP level of 12 4. Mannitol promotes osmotic diuresis by increasing the pressure gradient in the renal tubes, so urine output would increase; however, the reason mannitol was given was to decrease ICP. An ICP level of 12 is within normal limits. Fixed and dilated pupils are symptoms of increased ICP or cranial nerve damage. No information is given that mannitol is being given for renal dysfunction or blood pressure maintenance. 4) Which of the following values is considered normal for ICP? 1. 0 to 15 mm Hg 2. 25 mm Hg 3. 35 to 45 mm Hg 4. 120/80 mm Hg 1. Normal ICP is 0-15 mm Hg. 5) Which of the following signs and symptoms of increased ICP after head trauma would appear first? 1. Bradycardia 2. Large amounts of very dilute urine 3. Restlessness and confusion 4. Widened pulse pressure 3. The earliest symptom of elevated ICP is a change in mental status. Bradycardia, widened pulse pressure, and bradypnea occur later. The client may void large amounts of very dilute urine if there’s damage to the posterior pituitary. 6) The nurse is assessing the motor function of an unconscious client. The nurse would plan to use which of the following to test the client’s peripheral response to pain? 1. Sternal rub 2. Pressure on the orbital rim 3. Squeezing the sternocleidomastoid muscle 4. Nail bed pressure 4. Motor testing on the unconscious client can be done only by testing response to painful stimuli. Nailbed pressure tests a basic peripheral response. Cerebral responses to pain are testing using sternal rub, placing upward pressure on the orbital rim, or squeezing the clavicle or sternocleidomastoid muscle. 7) The client is having a lumbar puncture performed. The nurse would plan to place the client in which position for the procedure? 1. Side-lying, with legs pulled up and head bent down onto the chest 2. Side-lying, with a pillow under the hip 3. Prone, in a slight Trendelenburg’s position 4. Prone, with a pillow under the abdomen. 1. The client undergoing lumbar puncture is positioned lying on the side, with the legs pulled up to the abdomen, and with the head bent down onto the chest. This position helps to open the spaces between the vertebrae. 8) A nurse is assisting with caloric testing of the oculovestibular reflex of an unconscious client. Cold water is injected into the left auditory canal. The client exhibits eye conjugate movements toward the left followed by a rapid nystagmus toward the right. The nurse understands that this indicates the client has: 1. A cerebral lesion 2. A temporal lesion 3. An intact brainstem 4. Brain death 3. Caloric testing provides information about differentiating between cerebellar and brainstem lesions. After determining patency of the ear canal, cold or warm water is injected in the auditory canal. A normal response that indicates intact function of cranial nerves III, IV, and VIII is conjugate eye movements toward the side being irrigated, followed by rapid nystagmus to the opposite side. Absent or dysconjugate eye movements indicate brainstem damage. 9) The nurse is caring for the client with increased intracranial pressure. The nurse would note which of the following trends in vital signs if the ICP is rising? 1. Increasing temperature, increasing pulse, increasing respirations, decreasing systolic blood pressure. 2. Increasing temperature, decreasing pulse, decreasing respirations, increasing systolic blood pressure. 3. Decreasing temperature, decreasing pulse, increasing respirations, decreasing systolic blood pressure. 4. Decreasing temperature, increasing pulse, decreasing respirations, increasing systolic blood pressure. 2. A change in vital signs may be a late sign of increased intracranial pressure. Trends include increasing temperature and systolic blood pressure, and decreasing pulse and respirations. Respiratory irregularities also may arise. (Cushing’s Triad) 10) The nurse is evaluating the status of a client who had a craniotomy 3 days ago. The nurse would suspect the client is developing meningitis as a complication of surgery if the client exhibits: 1. A positive Brudzinski’s sign 2. A negative Kernig’s sign 3. Absence of nuchal rigidity 4. A Glascow Coma Scale score of 15 1. Signs of meningeal irritation compatible with meningitis include nuchal rigidity, positive Brudzinski’s sign, and positive Kernig’s sign. Nuchal rigidity is characterized by a stiff neck and soreness, which is especially noticeable when the neck is fixed. Kernig’s sign is positive when the client feels pain and spasm of the hamstring muscles when the knee and thigh are extended from a flexed-right angle position. Brudzinski’s sign is positive when the client flexes the hips and knees in response to the nurse gently flexing the head and neck onto the chest. A Glascow Coma Scale of 15 is a perfect score and indicates the client is awake and alert with no neurological deficits. 11) During the acute stage of meningitis, a 3-year-old child is restless and irritable. Which of the following would be most appropriate to institute? 1. Limiting conversation with the child 2. Keeping extraneous noise to a minimum 3. Allowing the child to play in the bathtub 4. Performing treatments quickly 2. A child in the acute stage of meningitis is irritable and hypersensitive to loud noise and light. Therefore, extraneous noise should be minimized and bright lights avoided as much as possible. There is no need to limit conversations with the child. However, the nurse should speak in a calm, gentle, reassuring voice. The child needs gentle and calm bathing. Because of the acuteness of the infection, sponge baths would be more appropriate than tub baths. Although treatments need to be completed as quickly as possible to prevent overstressing the child, any treatments should be performed carefully and at a pace that avoids sudden movements to prevent startling the child and subsequently increasing intracranial pressure. 12) Which of the following would lead the nurse to suspect that a child with meningitis has developed disseminated intravascular coagulation? 1. Hemorrhagic skin rash 2. Edema 3. Cyanosis 4. Dyspnea on exertion 1. DIC is characterized by skin petechiae and a purpuric skin rash caused by spontaneous bleeding into the tissues. An abnormal coagulation phenomenon causes the condition. 13) The nurse is assessing a child diagnosed with a brain tumor. Which of the following signs and symptoms would the nurse expect the child to demonstrate? Select all that apply. 1. Head tilt 2. Vomiting 3. Polydipsia 4. Lethargy 5. Increased appetite 6. Increased pulse 1, 2, 4. Head tilt, vomiting, and lethargy are classic signs assessed in a child with a brain tumor. Clinical manifestations are the result of location and size of the tumor. 14) A lumbar puncture is performed on a child suspected of having bacterial meningitis. CSF is obtained for analysis. A nurse reviews the results of the CSF analysis and determines that which of the following results would verify the diagnosis? 1. Cloudy CSF, decreased protein, and decreased glucose 2. Cloudy CSF, elevated protein, and decreased glucose 3. Clear CSF, elevated protein, and decreased glucose 4. Clear CSF, decreased pressure, and elevated protein 2. A diagnosis of meningitis is made by testing CSF obtained by lumbar puncture. In the case of bacterial meningitis, findings usually include an elevated pressure, turbid or cloudy CSF, elevated leukocytes, elevated protein, and decreased glucose levels. 15) A nurse is reviewing the record of a client with increased ICP and notes that the client has exhibited signs of decerebrate posturing. On assessment of the client, the nurse would expect to note which of the following if this type of posturing was present? 1. Abnormal flexion of the upper extremities and extension of the lower extremities 2. Rigid extension and pronation of the arms and legs 3. Rigid flexion of all extremities 4. Flaccid paralysis of all extremities 2. Decebrate posturing is characterized by the rigid extension and pronation of the arms and legs. 16. If a client experienced a cerebrovascular accident (CVA) that damaged the hypothalamus, the nurse would anticipate that the client has problems with: a. body temperature control. b. balance and equilibrium. c. visual acuity. d. thinking and reasoning. Answer A. The body’s thermostat is located in the hypothalamus; therefore, injury to that area can cause problems of body temperature control. Balance and equilibrium problems are related to cerebellar damage. Visual acuity problems would occur following occipital or optic nerve injury. Thinking and reasoning problems are the result of injury to the cerebrum. 17. After striking his head on a tree while falling from a ladder, a young man, age 18, is admitted to the emergency department. He’s unconscious and his pupils are nonreactive. Which intervention would be the most dangerous for the client? a. Give him a barbiturate. b. Place him on mechanical ventilation. c. Perform a lumbar puncture. d. Elevate the head of his bed. Answer C. The client’s history and assessment suggest that he may have increased intracranial pressure (ICP). If this is the case, lumbar puncture shouldn’t be done because it can quickly decompress the central nervous system and, thereby, cause additional damage. After a head injury, barbiturates may be given to prevent seizures; mechanical ventilation may be required if breathing deteriorates; and elevating the head of the bed may be used to reduce ICP. 18. The nurse is performing a mental status examination on a client diagnosed with subdural hematoma. This test assesses which of the following? a. Cerebellar function b. Intellectual function c. Cerebral function d. Sensory function Answer C. The mental status examination assesses functions governed by the cerebrum. Some of these are orientation, attention span, judgment, and abstract reasoning. Intellectual functioning isn’t the only cerebral activity. Cerebellar function testing assesses coordination, equilibrium, and fine motor movement. Sensory function testing involves assessment of pain, light-touch sensation, and temperature discrimination. 19. Shortly after admission to an acute care facility, a client with a seizure disorder develops status epilepticus. The physician orders diazepam (Valium) 10 mg I.V. stat. How soon can the nurse administer a second dose of diazepam, if needed and prescribed? a. In 30 to 45 seconds b. In 10 to 15 minutes c. In 30 to 45 minutes d. In 1 to 2 hours Answer B. When used to treat status epilepticus, diazepam may be given every 10 to 15 minutes, as needed, to a maximum dose of 30 mg. The nurse can repeat the regimen in 2 to 4 hours, if necessary, but the total dose shouldn’t exceed 100 mg in 24 hours. The nurse must not administer I.V. diazepam faster than 5 mg/minute. Therefore, the dose can’t be repeated in 30 to 45 seconds because the first dose wouldn’t have been administered completely by that time. Waiting longer than 15 minutes to repeat the dose would increase the client’s risk of complications associated with status epilepticus. 20. A client is admitted with a cervical spine injury sustained during a diving accident. When planning this client’s care, the nurse should assign highest priority to which nursing diagnosis? a. Impaired physical mobility b. Ineffective breathing pattern c. Disturbed sensory perception (tactile) d. Self-care deficient: Dressing/grooming Answer B. Because a cervical spine injury can cause respiratory distress, the nurse should take immediate action to maintain a patent airway and provide adequate oxygenation. The other options may be appropriate for a client with a spinal cord injury — particularly during the course of recovery — but don’t take precedence over a diagnosis of Ineffective breathing pattern. 21. A client who was trapped inside a car for hours after a head-on collision is rushed to the emergency department with multiple injuries. During the neurologic examination, the client responds to painful stimuli with decerebrate posturing. This finding indicates damage to which part of the brain? a. Diencephalon b. Medulla c. Midbrain d. Cortex Answer C. Decerebrate posturing, characterized by abnormal extension in response to painful stimuli, indicates damage to the midbrain. With damage to the diencephalon or cortex, abnormal flexion (decorticate posturing) occurs when a painful stimulus is applied. Damage to the medulla results in flaccidity. 22. The nurse is caring for a client diagnosed with a cerebral aneurysm who reports a severe headache. Which action should the nurse perform? a. Sit with the client for a few minutes. b. Administer an analgesic. c. Inform the nurse manager. d. Call the physician immediately. Answer D. The headache may be an indication that the aneurysm is leaking. The nurse should notify the physician immediately. Sitting with the client is appropriate but only after the physician has been notified of the change in the client’s condition. The physician will decide whether or not administration of an analgesic is indicated. Informing the nurse manager isn’t necessary. 23. A patient with a spinal cord injury (SCI) complains about a severe throbbing headache that suddenly started a short time ago. Assessment of the patient reveals increased blood pressure (168/94) and decreased heart rate (48/minute), diaphoresis, and flushing of the face and neck. What action should you take first? a. Administer the ordered acetaminophen (Tylenol). b. Check the Foley tubing for kinks or obstruction. c. Adjust the temperature in the patient’s room. d. Notify the physician about the change in status. Answer: B – These signs and symptoms are characteristic of autonomic dysreflexia, a neurologic emergency that must be promptly treated to prevent a hypertensive stroke. The cause of this syndrome is noxious stimuli, most often a distended bladder or constipation, so checking for poor catheter drainage, bladder distention, or fecal impaction is the first action that should be taken. Adjusting the room temperature may be helpful, since too cool a temperature in the room may contribute to the problem. Tylenol will not decrease the autonomic dysreflexia that is causing the patient’s headache. Notification of the physician may be necessary if nursing actions do not resolve symptoms. 24. A patient with a spinal cord injury at level C3-4 is being cared for in the ED. What is the priority assessment? a. Determine the level at which the patient has intact sensation. b. Assess the level at which the patient has retained mobility. c. Check blood pressure and pulse for signs of spinal shock. d. Monitor respiratory effort and oxygen saturation level. Answer: D – The first priority for the patient with an SCI is assessing respiratory patterns and ensuring an adequate airway. The patient with a high cervical injury is at risk for respiratory compromise because the spinal nerves (C3 – 5) innervate the phrenic nerve, which controls the diaphragm. The other assessments are also necessary, but not as high priority. 25. You are providing care for a patient with an acute hemorrhage stroke. The patient’s husband has been reading a lot about strokes and asks why his wife did not receive alteplase. What is your best response? a. “Your wife was not admitted within the time frame that alteplase is usually given.” b. “This drug is used primarily for patients who experience an acute heart attack.” c. “Alteplase dissolves clots and may cause more bleeding into your wife’s brain.” d. “Your wife had gallbladder surgery just 6 months ago and this prevents the use of alteplase.” Answer: C – Alteplase is a clot buster. With patient who has experienced hemorrhagic stroke, there is already bleeding into the brain. A drug like alteplase can worsen the bleeding. The other statements are also accurate about use of alteplase, but they are not pertinent to this patient’s diagnosis. 26. While working in the ICU, you are assigned to care for a patient with a seizure disorder. Which of these nursing actions will you implement first if the patient has a seizure? a. Place the patient on a non-rebreather mask will the oxygen at 15 L/minute. b. Administer lorazepam (Ativan) 1 mg IV. c. Turn the patient to the side and protect airway. d. Assess level of consciousness during and immediately after the seizure. Answer: C – The priority action during a generalized tonic-clonic seizure is to protect the airway. Administration of lorazepam should be the next action, since it will act rapidly to control the seizure. Although oxygen may be useful during the postictal phase, the hypoxemia during tonic-clonic seizures is caused by apnea. Checking the level of consciousness is not appropriate during the seizure, because generalized tonic-clonic seizures are associated with a loss of consciousness. 27. A 70-year-old alcoholic patient with acute lethargy, confusion, and incontinence is admitted to the hospital ED. His wife tells you that he fell down the stairs about a month ago, but “he didn’t have a scratch afterwards.” She feels that he has become gradually less active and sleepier over the last 10 days or so. Which of the following collaborative interventions will you implement first? a. Place on the hospital alcohol withdrawal protocol. b. Transfer to radiology for a CT scan. c. Insert a retention catheter to straight drainage. d. Give phenytoin (Dilantin) 100 mg PO. Answer: B – The patient’s history and assessment data indicate that he may have a chronic subdural hematoma. The priority goal is to obtain a rapid diagnosis and send the patient to surgery to have the hematoma evacuated. The other interventions also should be implemented as soon as possible, but the initial nursing activities should be directed toward treatment of any intracranial lesion. 28. The nurse in the Emergency Room is treating a patient suspected to have a Peptic Ulcer. On assessing lab results, the nurse finds that the patient’s blood pressure is 95/60, pulse is 110 beats per minute, and the patient reports epigastric pain. What is the priority intervention? A. Start a large-bore IV in the patient’s arm B. Ask the patient for a stool sample C. Prepare to insert an NG Tube D. Administer intramuscular morphine sulphate as ordered A. Start a large-bore IV in the patient’s arm Correct – The nurse should suspect that the patient is haemorrhaging and will need need a fluid replacement therapy, which requires a large bore IV. Ask the patient for a stool sample Incorrect – While this is useful in the diagnosis and assessment of Peptic Ulcer Disease, it is not the priority intervention. Prepare to insert an NG Tube Incorrect – While this intervention may be used in the later stages of Peptic Ulcer Disease, it is not the first and priority intervention. Administer intramuscular morphine sulphate as ordered Incorrect – While this is an important intervention to manage pain, it is not the priority intervention. 29. The optimal measurement of intravascular fluid status during the immediate fluid resuscitation phase of burn treatment is: A. BUN B. Daily Weight C. Urine output D. K+ C. During initial fluid resuscitation, urine output helps guide therapy. 30. What is the total amount of fluid (in the first 24 hours) that will need to be administered to a 70kg man with a burn injury that covers 50% of his body surface area? A. 2800 mL B. 7000 mL C. 14 L D. 28 L C. 4 × 70 kg × 50 = 14,000 mL or 14 liters. 31. Which of the following is an essential nursing action for a patient who has circumferential full thickness burns on an extremity? A. Keeping the extremity in a dependent position B. Monitoring distal pulses of the extremity C. Performing an escharotomy as a prophylactic measure D. Putting on sequential compression stockings B. Distal pulses on the extremity must be assessed to detect compartment syndrome A: Keeping the extremity in a dependent position will increase edema and compromise blood flow. C: Performing an escharotomy is a physician responsibility. D: Sequential compression devices should not be used in a burned extremity. Question 9 Type: MCMA A patient is diagnosed with hyperglycemic hyperosmolar state (HHS). Which interventions would the nurse anticipate? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Potassium supplementation 2. Testing for sources of infection 3. Increasing amount of NPH insulin administered 4. Increasing IV fluid administration 5. Monitoring arterial blood gases Correct Answer: 1,2,4 Rationale 1: HHS can cause either potassium deficit or excess. Potassium supplementation may be necessary. Rationale 2: Infection can cause HHS. Identification and management of causative factors is important. Rationale 3: HHS management requires administration of IV insulin. Rationale 4: HHS results in dehydration that is managed with IV fluids. Rationale 5: Monitoring patient’s level of consciousness Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 31-4 Question 12 Type: MCSA The nurse has adequately managed a patient’s airway, breathing, and circulation. What is the next nursing action? 1. Assess level of consciousness. 2. Administer prophylactic tetanus toxoid as prescribed. 3. Auscultate heart sounds. 4. Assess the chest for paradoxical movements. Correct Answer: 1 Rationale 1: The nurse should assess the patient's neurological status or level of consciousness as the next step. Rationale 2: Administering prophylactic tetanus toxoid and transferring the patient should happen after the assessment is complete. Rationale 3: Auscultation of heart sounds is part of the secondary survey, which is done after the primary survey. The primary survey is not yet complete. Rationale 4: Assessment for paradoxical movement of the chest is part of the secondary survey, which occurs after the primary survey. The primary survey is not yet completed. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 34-5 Question 15 Type: MCMA The nurse is providing care to a farmworker who was pinned against a steel gate by a horse. Deformation of the patient’s pelvis and femurs is obvious, but little blood is present on the patient’s clothing. Initial blood pressure is 110/68 mm Hg. What nursing interventions are indicated? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Initiate intravenous access with a 16 gauge catheter. 2. Start fluid resuscitation with normal saline. 3. Prepare to administer vasopressor medication. 4. Turn the patient to assess for injuries to the back. 5. Prepare to insert a chest tube. Correct Answer: 1,2 Rationale 1: This patient’s mechanism of injury and assessment indicates potential for femur and pelvic fractures, which can result in massive blood loss. The “normal” blood pressure may be related to pain and adrenaline release. Venous access with large gauge catheters is essential. Rationale 2: This patient may be bleeding internally. Fluid resuscitation is indicated. Rationale 3: Vasopressor medications are not useful until fluid volume is restored. Rationale 4: This patient should not be moved until further assessment is conducted. Rationale 5: Nothing in the patient’s assessment indicates need for a chest tube at this point. The nurse should continue to assess airway and breathing. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 34-6 Question 19 Type: MCSA The nurse is caring for a patient who sustained a lacerated spleen from a motorcycle accident. Which complication is this patient most prone to experience because of the trauma? 1. Acute renal failure 2. Sepsis 3. Deep vein thrombosis 4. ARDS Correct Answer: 1 Rationale 1: Abdominal trauma, specifically a lacerated spleen, makes the patient prone to developing the complication of acute renal failure, abdominal compartment syndrome, or disseminating intravascular coagulation. Rationale 2: Sepsis is associated with an open pneumothorax and perforated intestine. Rationale 3: Deep vein thrombosis is not associated with any particular organ system and can occur at any time with any health problem that restricts mobility or increases blood coagulation. Rationale 4: ARDS is seen more often with thoracic traumatic injuries. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 34-7 Question 20 Type: MCSA A patient is in the intensive care unit with a pulmonary contusion sustained from a motor vehicle accident. Which post-traumatic complication should the nurse focus on when providing care to this patient? 1. Abdominal compartment syndrome 2. Sepsis 3. ARDS 4. Acute renal failure Correct Answer: 3 Rationale 1: Abdominal compartment syndrome is more common in patients with abdominal trauma. Rationale 2: Sepsis is more common in patients with abdominal trauma or open wounds. Rationale 3: The patient with a thoracic injury is prone to developing the post-traumatic complications of ARDS and DIC. Rationale 4: Acute renal failure can occur with any massive trauma that involves blood loss, but is more common if injuries to the abdomen exist. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 34-8 Question 2 Type: MCSA A patient recovering from a frontal craniotomy is positioned with the head of the bed elevated 45 degrees at all times. What rationale would the nurse provide for this position? 1. The brain will compress the cerebral veins less in this position. 2. The ventricles of the brain will drain better in this position. 3. This position allows for less pain for the patient. 4. The cerebral spinal veins are valveless and drain by gravity. Correct Answer: 4 Rationale 1: This statement is not physiologically correct. Rationale 2: This statement is not physiologically correct. Rationale 3: There is no reason that pain would be reduced in this position. Rationale 4: The cerebral spinal veins drain best via gravity, an important characteristic to remember when caring for patients with the risk for increased intracranial pressure as would be present in intracranial surgeries. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 15-1 Question 3 Type: MCSA The nurse is providing care for a patient who sustained a severe head injury. The nurse would intervene to prevent which occurrence that increases cerebral blood flow? 1. Oversedation 2. Hypothermia 3. Fever 4. Paralysis Correct Answer: 3 Rationale 1: Sedation will decrease cerebral blood flow. Rationale 2: Hypothermia will decrease cerebral blood flow. Rationale 3: Fever increases the body’s metabolic rate and will increase cerebral blood flow. Rationale 4: Paralysis, often initiated chemically, will decrease cerebral blood flow. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 15-1 Question 4 Type: MCSA The nurse is providing care for a patient who is at risk for developing an increase in intracranial pressure due to swelling of the brain. The nurse is aware that this increased brain size must be accompanied by which other change if intracranial pressure is to remain stable? 1. There will be an increase in the blood flow to the brain. 2. There is a decrease in the blood–brain barrier. 3. There must be a decrease in another of the intracranial compartments. 4. There will be an increase in the production of cerebrospinal fluid. Correct Answer: 3 Rationale 1: Blood flow to the brain would decrease as more space is taken up by the brain. Rationale 2: The blood–brain barrier does not increase or decrease in response to changes in the brain. Rationale 3: The contents of the intracranial vault include the brain, cerebral blood volume, and cerebrospinal fluid. The Monro–Kellie hypothesis states that as the content of one of the intrancranial compartments increases, it is at the expense of the other two. The correct answer is that if there is an increase in the volume of brain tissue, there will need to be a decrease in another of the intracranial compartments. Rationale 4: An increased amount of cerebrospinal fluid would increase the pressure in the intracranial vault. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 15-2 Question 5 Type: MCSA A nurse is monitoring the intracranial pressure of a patient with a closed-head injury. Which pressure would the nurse evaluate as requiring no additional intervention? 1. 12 mm Hg 2. 22 mm Hg 3. 25 mm Hg 4. 30 mm Hg Correct Answer: 1 Rationale 1: The normal intracranial pressure ranges from 0 to 15 mm Hg. Rationale 2: This pressure exceeds normal. Rationale 3: This pressure exceeds normal. Rationale 4: This pressure exceeds normal. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 15-2 Question 7 Type: MCSA A patient with a head injury has a mean arterial pressure of 70 mm Hg and an intracranial pressure of 20 mm Hg. Which cerebral perfusion pressure would the nurse document for this patient? 1. 50 mm Hg 2. 90 mm Hg 3. 70/40 mm Hg 4. 40/70 mm Hg Correct Answer: 1 Rationale 1: The cerebral perfusion pressure is calculated as the mean arterial pressure minus the intracranial pressure. In this patient the cerebral perfusion pressure would be inadequate and intervention is needed. Rationale 2: This calculation is incorrect for the values given. Rationale 3: This calculation is incorrect for the values given. Rationale 4: This calculation is incorrect for the values given. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 15-3 Question 8 Type: MCSA A nurse is monitoring a patient who sustained a head injury. The nurse recognizes which finding as the earliest sign of change in neurologic status? 1. The patient cannot remember where he is. 2. The patient’s pupil size is increased. 3. The patient’s blood pressure has increased. 4. The patient exhibits decorticate posturing when stimulated. Correct Answer: 1 Rationale 1: The level of consciousness is the most important indicator of neurological function in the high-acuity patient. Rationale 2: Pupillary changes do occur with neurological damage but are not the earliest signs. Rationale 3: Changes in vital sign can indicate neurological damage, but are not the earliest signs. Rationale 4: Posturing is an important finding associated with neurologic damage, but is not the earliest sign. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 15-3 Question 9 Type: MCSA A nurse is monitoring a patient’s Glasgow Coma Scale (GSC). At which point would the nurse document that the patient is comatose? 1. 11 2. 15 3. 7 4. 9 Correct Answer: 3 Rationale 1: A score of 11 indicates some impairment, but does not indicate coma. Rationale 2: A GCS of 15 is normal. Rationale 3: A score of 7 or less indicates a significant alteration in the level of consciousness and the development of coma. Rationale 4: A GCS score of 9 indicates significant neurological changes, but does not indicate coma. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 15-3 Question 19 Type: MCSA A nurse is starting an intravenous line in a patient being treated for a head injury. Suddenly the patient extends his legs and demonstrates extreme plantar flexion. What action should be taken by the nurse? 1. Document the presence of decorticate posturing. 2. Immediately stop the attempt at intravenous insertion and obtain a blood pressure reading. 3. Assess the position of the patient’s arms. 4. Administer intravenous sedation as quickly as possible after access is obtained. Correct Answer: 3 Rationale 1: It is not possible to assess decorticate posturing from this scenario. Rationale 2: It is important to gain IV access for this patient. Posturing to noxious stimuli indicates brain damage. Blood pressure is not pertinent at this time. Rationale 3: The nurse should assess the position of the patient’s arms to determine if decorticate or decerebrate posturing is present. Rationale 4: Administering sedation is not indicated at this time as assessment is continuing. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 15-3 Question 1 Type: MCMA The nurse is providing community education regarding stroke. Which information should be included? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Stroke is caused by interruption of blood flow to the brain. 2. Stroke is the third-leading cause of death in the United States. 3. Stroke usually occurs simultaneously with myocardial infarction. 4. Rapid recognition of stroke symptoms can help decrease poor outcomes. 5. Stroke causes neurological defects. Correct Answer: 1,2,4,5 Rationale 1: Stroke occurs when a localized area of the brain is not receiving adequate blood flow. The resultant ischemia causes injury to the brain tissue. Rationale 2: Stroke is the third cause of death and a leading cause of disability in the United States. Rationale 3: There is no evidence that stroke and MI generally occur together. Rationale 4: Rapid recognition of stroke symptoms along with rapid intervention can help to decrease poor outcomes from stroke. Rationale 5: Neurological changes and deficits are common when stroke occurs. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 17-1 Question 2 Type: MCSA A patient comes into the emergency department with complaints of partial loss of vision in one eye, numbness and tingling of the arm and leg, and dizziness. Which additional information should the nurse initially seek from the patient? 1. If the patient has high blood pressure 2. If the symptoms are still present 3. If this is a recurrent problem 4. If the patient fell Correct Answer: 2 Rationale 1: Although important, determining if the patient has a history of high blood pressure can be determined at a later time. Rationale 2: Although all of these issues are important in the assessment of the patient, it is essential to determine if the patient still has the symptoms or if they were time limited. If symptoms are no longer present they are still significant as the patient may have experienced a transient ischemic attack. Rationale 3: It is important to discern if the patient has ever experienced these symptoms before, but this is not the most important information. Rationale 4: Assessing if the patient has fallen is not important for the nurse to ask initially. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 17-1 Question 3 Type: MCSA When developing a teaching plan for a patient who had an embolic stroke, the nurse considers which history as a significant risk factor? 1. Hypertension 2. Use of anticoagulants 3. History of atherosclerosis of cerebral arteries 4. Atrial fibrillation Correct Answer: 4 Rationale 1: Hypertension is more likely associated with thrombotic stroke. Rationale 2: Use of anticoagulants and hypertension together are associated with hemorrhagic cerebral vascular accidents. Rationale 3: Atherosclerosis of cerebral arteries is associated with ischemic stroke. Rationale 4: Atrial fibrillation, in addition to endocarditis, rheumatic heart disease, and recent myocardial infarction, are the most common causes of embolic cerebral vascular accidents. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 17-1 Question 4 Type: MCSA When planning nursing care for a patient with a cerebral vascular accident, the nurse should consider which primary goal of medical management? 1. Restoration of cerebral blood flow and limiting the size of the infarcted area of the brain 2. Keeping the blood pressure under control pharmacologically 3. Transferring the patient for rehabilitation as soon as medically stable 4. Reestablishing blood flow to the infarcted area surgically Correct Answer: 1 Rationale 1: The goal is to recover as much function as possible. The most vulnerable area of the brain is the penumbra, and the sooner the circulation can be restored to that area the better the cells in that area will recover. Rationale 2: The patient’s blood pressure should be controlled, but this goal is not global enough to be the primary goal. Rationale 3: Transferring the patient to a long-term care facility as soon as medically stable is a goal for patients to recover enough function to return to their former settings. This is not the primary goal for medical management. Rationale 4: Surgical options are not available for most stroke patients. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 17-5 Question 12 Type: MCSA A patient who has been admitted with symptoms of stroke is to have a CT scan. What rationale for this testing would the nurse provide to the patient and family? 1. CT scans are used to determine the effectiveness of the cerebral circulation to perfuse all areas of the brain. 2. The CT scan will evaluate how much brain swelling is associated with this stroke. 3. The CT scan will pinpoint the exact area of the brain affected by the stroke. 4. The CT scan can guide treatment by differentiating hemorrhagic from ischemic causes of the stroke. Correct Answer: 4 Rationale 1: A CT alone will not determine the effectiveness of cerebral circulation. Rationale 2: CT scans cannot determine the extent of brain swelling. Rationale 3: CT scans cannot pinpoint the exact area of the brain affected by stroke, but can help to establish the anatomical region in which the stroke occurred. Rationale 4: A CT scan will be used to rule out a hemorrhagic stroke from an ischemic stroke especially if thrombolytic therapy is being considered and to determine any areas of localized hematoma formation as a result of a hemorrhage. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 17-4 Question 13 Type: MCMA A patient is receiving tissue plasminogen activator (tPA) for the treatment of an ischemic stroke. Which nursing interventions are indicated? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Insert a nasogastric tube for nutritional support. 2. Monitor for renal stone formation. 3. Monitor for deterioration of neurological status. 4. Reposition every 15 minutes. Correct Answer: 3 Rationale 1: Insertion of a nasogastric tube can cause injury and should be avoided in this patient. Rationale 2: Renal stone formation is not a complication of this medication. Rationale 3: Deterioration of neurological status can occur as a result of bleeding or if tPA is not effective in lysing the clot. The nurse should monitor for this evolving situation. Rationale 4: Frequent moving can increase the risk of bleeding therefore the patient should not be repositioned every 15 minutes. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 17-6 Question 1 Type: MCSA A patient comes into the emergency department with complaints of headache, lethargy, and vomiting. He reports being hit in the head by a batted baseball during a company picnic “about 6 weeks ago.” The nurse would ask additional assessment questions regarding which condition? 1. Acute subdural hematoma 2. Subacute subdural hematoma 3. Epidural hematoma 4. Chronic subdural hematoma Correct Answer: 4 Rationale 1: An acute subdural hematoma occurs less than 48 hours from injury so this is an unlikely injury pattern. Rationale 2: Subacute subdural hematoma occurs 48 hours to 2 weeks from injury so this is an unlikely injury pattern. Rationale 3: With an epidural hematoma, there is a brief loss of consciousness immediately following the injury, followed by an episode of being alert and oriented, and then a loss of consciousness again. The patient did not describe a loss of consciousness. Rationale 4: There are three categories of subdural hematoma, based on time of onset of symptoms. Chronic hematoma develops greater than 2 weeks from injury. Since the patient had a head injury a few weeks prior, the nurse would have highest concern regarding a chronic subdural hematoma. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 18-3 Question 2 Type: MCSA The nurse is caring for a patient recovering from surgery to evacuate an epidural hematoma. Which assessment finding would warrant immediate collaboration with the surgeon? 1. Urine output has dropped from 100 mL each hour to 60 mL per hour. 2. The patient’s hand grasps are weak bilaterally. 3. Fine crackles can be auscultated in the lung bases bilaterally. 4. The pupil on the side of the injury has become fixed and dilated. Correct Answer: 4 Rationale 1: Urine output of 60 mL per hour is considered normal and would not require emergency collaboration. If urine output continues to drop, increasing intravenous fluid administration rate may be considered. Rationale 2: Weak hand grasps bilaterally may or may not indicate a worsening neurological condition. Bilateral weakness is not as significant for emergent conditions as is unilateral weakness. Rationale 3: Fine crackles auscultated bilaterally in lung bases can be due several conditions, such as immobility, and is not indicative of an emergent neurological condition. Rationale 4: Nursing care associated with epidural hematoma focuses on diligent neurological assessment. The nurse must look for sudden changes in level of consciousness and for the presence of a fixed and dilated pupil on the side of injury. These findings suggest bleeding has recurred and represents an emergent medical situation. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 18-3 Question 5 Type: MCSA A patient with a moderate diffuse head injury is demonstrating a variety of neurological symptoms. What is the priority when caring for this patient? 1. Electrolyte replacements 2. Maintain adequate fluid volume. 3. Supporting nutritional needs 4. Maintain stable cerebral perfusion pressure. Correct Answer: 4 Rationale 1: Electrolyte management is important to patients with head injury but is not the intervention of highest priority. Rationale 2: Fluid volume management is important when caring for patients with brain injury, but is not the highest priority. Rationale 3: Support of nutritional needs is important for all patients, but is not the intervention of highest priority for patients with brain injury. Rationale 4: Since diffuse head injuries are not limited to a localized area, this makes them more difficult to detect and treat. Management in the acute care phase includes diligent and frequent neurological assessments and pain management. When moderate-to-severe injury is present, priority management includes interventions to lower intracranial pressure, increase cerebral perfusion pressure, and stabilize vital signs, which all contribute to an improved outcome. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 18-3 Question 6 Type: MCSA A patient is admitted with a traumatic brain injury. The nurse would anticipate participating in interventions toward which immediate goal? 1. Reducing cerebral swelling 2. Confining inflammation to one area 3. Supporting absorption of debris from neuronal death 4. Limiting ischemic tissue injury Correct Answer: 4 Rationale 1: Cerebral swelling can cause secondary injury, but this is not the immediate goal. Rationale 2: Inflammation can cause secondary injury but this is not the immediate goal when caring for someone with TBI. Rationale 3: Eventually the body will rid itself for debris from death of any cells, but this is not the immediate goal. Rationale 4: The first goal in treating traumatic brain injury is to limit the primary ischemic tissue injury by aggressive prevention and treatment of hypoxia and hypotension. If efforts to meet this goal are successful, cerebral swelling neuronal death and cerebral inflammation can be limited as well. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 18-5 Question 7 Type: MCMA A patient with traumatic brain injury has had placement of an intraventricular catheter (IVC). The nurse participates in level two interventions to reduce intracranial pressure (ICP) through which uses of this catheter? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Assessing of color of the cerebral spinal fluid 2. Assessing of the amount of cerebral spinal fluid 3. Instillation of hyperosmolar therapy via the catheter 4. Draining CSF 5. Directly monitoring the ICP Correct Answer: 1,2,4,5 Rationale 1: By assessing the color of the cerebral spinal fluid the nurse can identify variation from normal. These variations may indicate bleeding or infection that would increase ICP. Rationale 2: By using IVC measurements, the nurse can monitor amount of CSF. Rationale 3: Hyperosmolar therapy is not instilled via this catheter. Rationale 4: Therapeutic drainage of CSF via the IVC can reduce ICP. Rationale 5: Insertion of an IVC allows for direct measurement of the ICP. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 18-5 Question 8 Type: MCSA A patient with traumatic brain injury continues to have increased intracranial pressure despite conventional therapeutic interventions. The nurse would anticipate which level four intervention? 1. High-dose barbiturate therapy 2. High-volume intravenous fluids 3. Hyperbaric oxygen therapy 4. Hyperosmolar therapy Correct Answer: 1 Rationale 1: Medical intervention for the treatment of increased intracranial pressure refractory to all other medical interventions may include the use of high-dose barbiturates. This intervention induces a comatose state and significantly decreases cerebral oxygen requirements. Rationale 2: High-volume intravenous fluid administration would be more likely to increase intracranial pressure. Rationale 3: Hyperbaric oxygen therapy is not a treatment identified to help with refractory increased intracranial pressure. Rationale 4: Hyperosmolar therapy is used as a level two intervention, not to treat refractory increase in intracranial pressure. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 18-5 Question 10 Type: MCSA A patient being treated for increased intracranial pressure from a traumatic brain injury demonstrates an increase in pressure with minimal care activity. What instruction should the nurse provide the nursing student assisting with care for this patient? 1. “We will let this patient rest between his bath and changing his linens.” 2. “We are going to bath this patient, get his linens changed, suction him, and do all of our other care early this morning, so he can get a long rest this afternoon.” 3. “Be certain that we don’t raise this patient’s head above 10 degrees during his bath.” 4. “You have to learn to suction patients with traumatic brain injury very quickly, taking no more than 30 seconds.” Correct Answer: 1 Rationale 1: When simple activities result in an increase in intracranial pressure it is necessary to space care in such a way to allow the patient’s ICP to recover between events. Rationale 2: Stacking care activities will be detrimental to this patient. Rationale 3: The head of the bed should be elevated to 30 degrees to reduce intracranial pressure without compromising cerebral perfusion pressure. Rationale 4: The patient should be suctioned for 10 seconds or less to reduce an increase in intracranial pressure caused by the suctioning. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 18-6 Question 11 Type: MCMA The admission orders for a patient with traumatic brain injury say to keep the patient’s head elevated with neutral body positioning. Which patient positioning would the nurse consider as meeting this requirement? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. The patient’s head is supported on two pillows. 2. The head of the patient’s bed is elevated to 20 degrees. 3. The patient’s hips are flexed at less than 90 degrees. 4. The neck is in the patient’s position of comfort, which is rotated to the left. 5. The patient is facing forward. Correct Answer: 3,5 Rationale 1: Placing the head on two pillows flexes the neck which violates the idea of a “neutral” position. Rationale 2: Typically the head of the patient’s bed should be elevated to 30 degrees. Rationale 3: Hip flexion of greater than 90 degrees should be avoided. Rationale 4: The neck should not be rotated. Rationale 5: Neutral positioning for the head and neck is a forward facing position. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Evaluation Learning Outcome: 18-6 Question 12 Type: MCSA A patient being treated for a traumatic brain injury is febrile with a temperature of 100°F. What is the priority nursing intervention? 1. Culture the patient’s urine. 2. Contact the primary health care provider. 3. Administer the prn antipyretic. 4. Have the patient cough and deep breath more frequently. Correct Answer: 3 Rationale 1: Urinary tract infection will cause increased temperature and this may be a necessary intervention. It is not, however, the primary intervention. Rationale 2: It is important to keep the primary health care provider apprised of the patient’s condition, but this is not the primary intervention. Rationale 3: Hyperthermia will increase cerebral metabolic rates, which will increase cerebral oxygen demands. The patient with a temperature should be provided with antipyretics or other measures to cool the body and reduce the temperature. Rationale 4: Implementing pulmonary hygiene activities will not reduce the patient's body temperature. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 18-6 Question 13 Type: MCMA The patient with traumatic brain injury has been intubated and placed on mechanical ventilation. Which nursing interventions would help optimize oxygenation? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Preoxygenate the patient prior to suctioning. 2. Use very low vacuum pressure when suctioning the patient. 3. Limit suction passes to 10 seconds or less. 4. Suction when PaCO2 levels rise above 40 mm Hg. 5. Suction the patient before and after scheduled turns. Correct Answer: 1,3 Rationale 1: To maintain adequate oxygenation during suctioning, preoxygenation is indicated. Rationale 2: Low vacuum pressure will not adequately remove secretions, making suctioning ineffective or necessary more often. This will not increase oxygenation. Rationale 3: For patients at risk for increased ICP, total suction time should be limited to no more than 10 seconds. Rationale 4: Increased PaCO2 level may or may not be associated with need to suction. Desired PaCO2 level is 35 to 45 mm Hg. Rationale 5: The patient should be suctioned as needed, but nursing activities should be spaced as much as possible. Routine suctioning both before and after scheduled turns is not likely to be necessary and would decrease oxygenation. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 18-6 Question 15 Type: MCSA A patient with a traumatic brain injury is being treated for diabetes insipidus. Which finding would the nurse evaluate as indicating treatment is effective? 1. Potassium level has decreased. 2. Blood pressure has decreased. 3. Serum sodium level is increased. 4. Urine output has decreased. Correct Answer: 4 Rationale 1: Potassium level assessment is not an essential indicator of success in the treatment of a patient with diabetes insipidus. Rationale 2: The large amount of fluid lost in diabetes insipidus causes hypotension. Continued decrease in blood pressure does not indicate that treatment is successful. Rationale 3: Continued elevation of serum sodium level would indicate that treatment is not effective. Rationale 4: Treatment for diabetes insipidus includes replacing intravascular volume and providing synthetic antidiuretic hormone. Evidence that a patient is improving would include a decrease in urine output with an increase in specific gravity. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Evaluation Learning Outcome: 18-7 Question 14 Type: MCSA A patient in the intensive care unit begins to seize. The nurse would anticipate initial management of this seizure to include which intravenous medication? 1. Fosphenytoin 2. Lorazepam 3. Propofol 4. Diazepam Correct Answer: 2 Rationale 1: Fosphenytoin would be administered if the first line class of drugs was ineffective in controlling the seizure. Rationale 2: Intravenous benzodiazepines are effective in stopping seizures 65–80% of the time. Lorazepam is the treatment of choice over diazepam because it lasts longer. Rationale 3: Propofol could be administered if the first and second line drugs are ineffective in controlling the seizure. Rationale 4: Diazepam is a benzodiazepine that can be administered intravenously; however, it does not last as long as the preferred drug. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 16-4 Question 7 Type: MCSA A patient is admitted with the diagnosis of possible acute pancreatitis. Upon assessment, the nurse notes faint bruising over the patient's flank region. How would the nurse report and document this finding? 1. Homan's sign 2. Cullen's sign 3. Grey Turner's sign 4. Chvostek's sign Correct Answer: 3 Rationale 1: Homan’s sign is an indicator of the presence of deep vein thrombosis, not acute pancreatitis. Rationale 2: The Cullen's sign is a bluish discoloration around the umbilicus. Rationale 3: While assessing the patient's integumentary status, the nurse might observe a bluish discoloration over the patient's flank region. This discoloration is considered the Grey Turner's sign. Rationale 4: Chvostek's sign is seen in hypocalcemia and is characterized by numbness and tingling around the mouth. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 23-3 Question 12 Type: MCSA A patient with acute pancreatitis is demonstrating signs of hypovolemic shock. The nurse will conduct additional assessment for which expected cause of this hypovolemia? 1. Increased urine output 2. Undiagnosed gastrointestinal ulcerations 3. Pulmonary edema 4. Fluid shifts and decreased vascular resistance Correct Answer: 4 Rationale 1: An increase in urine output will not place a patient into hypovolemic shock in this situation. Rationale 2: Even though hypovolemic shock can be caused by undiagnosed gastrointestinal ulcerations, there is not enough information to support this reason in the patient. Rationale 3: Pulmonary edema would be another symptom of third spacing of fluid being shifted from compartments. Rationale 4: Vasoactive substances, released from damaged pancreatic tissue, are responsible for vasodilation, decreased systemic vascular resistance, and increased permeability of endothelial linings of vessels. As vessels become more porous, intravascular fluids shift into other compartments and into the retroperitoneal cavity, causing hypovolemia, third spacing and hypovolemic shock. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 23-4 Question 13 Type: MCMA The nurse is caring for a patient with acute pancreatitis demonstrating signs of hypovolemic shock. Which interventions will be included in this patient's plan of care? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Administer high doses of potassium. 2. Monitor pulmonary arterial wedge pressure. 3. Administer several liters of intravenous fluids in the first few hours of treatment. 4. Administer anticholinergic medication. 5. Monitor central venous pressure. Correct Answer: 2,3,5 Rationale 1: Administering electrolyte replacements as prescribed would be useful to prevent or treat complications. Which electrolytes and the amount of electrolytes will be guided by laboratory results. High doses of potassium are not likely. Rationale 2: In hypovolemia, the goal is to stabilize the patient's hemodynamic status. Monitoring pulmonary wedge pressure will provide valuable information about fluid balance. Rationale 3: Fluid resuscitation generally involves an initial several-liter fluid bolus followed by 250–500 mL/hour continuous infusion. Rationale 4: Administering anticholinergic medication may decrease pancreatic stimulation but is not indicated to treat hypovolemia. Rationale 5: Central venous pressure is a standard intervention for monitoring hydration status. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 23-5 Question 15 Type: MCSA The nurse is caring for a patient with acute pancreatitis experiencing pain. How would the nurse expect to treat this pain? 1. Acetaminophen 2. NSAIDs 3. Demerol 4. Morphine Correct Answer: 4 Rationale 1: The pain of acute pancreatitis is not likely to be controlled with acetaminophen. Rationale 2: The pain of acute pancreatitis is not likely to be controlled with NSAIDs. Rationale 3: Meperidine (Demerol) is not considered a drug of choice as its major metabolite can accumulate in the body and is neurotoxic. Rationale 4: Since acute pancreatitis is extremely painful, pain control is needed for comfort and to decrease the secretion of pancreatic enzymes. Fentanyl, morphine, and hydromorphone are effective pain relievers for patients with acute pancreatitis. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 23-5 Question 19 Type: MCSA A patient with acute pancreatitis has been treated to minimize pancreatic stimulation, but vomiting continues. The nurse would anticipate which intervention? 1. NPO status 2. Placement of a nasogastric tube to intermittent suction 3. Administration of morphine 4. Increased ambulation Correct Answer: 2 Rationale 1: NPO status is part of resting the GI tract and would already be part of minimizing pancreatic stimulation. Rationale 2: Vomiting should stop when the patient is placed on GI tract rest. If this does not occur placement of a nasogastric tube to intermittent suction is considered. Rationale 3: Drug therapy will include antacids, proton pump inhibitors, or anticholinergics. Rationale 4: Increasing ambulation is not indicated when the patient is vomiting. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 23-5 Question 2 Type: MCSA A patient with acute pancreatitis asks the nurse why everyone is concerned about his blood glucose level. Which nursing response is appropriate? 1. Pancreatitis can injure the cells that produce insulin. 2. Since you are not eating, there is concern you won’t have enough glucose in your system. 3. Nearly everyone with pancreatitis develops diabetes. 4. Pancreatitis requires treatment with high amounts of intravenous fluids that can increase blood glucose. Correct Answer: 1 Rationale 1: Insulin is a polypeptide produced by the beta cells of the islets of Langerhans in the pancreas whose role is to lower the blood glucose level. An injury to the pancreas can injure these cells. Rationale 2: This is not the reason for concern regarding this patient’s blood glucose. Rationale 3: This is not a true statement. Rationale 4: This is not the reason for monitoring this patient’s glucose. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 32-1 Question 5 Type: MCSA The nurse is preparing to administer an intravenous insulin drip to a patient admitted with diabetic ketoacidosis. Which laboratory is of most concern to the nurse? 1. Phosphorus level of 2.8 mEq/L 2. Bicarbonate level of 16 mEq/L 3. Sodium level of 130 mEq/L 4. Potassium level of 3.2 mEq/L Correct Answer: 4 Rationale 1: The phosphorus level is within normal limits. Rationale 2: The bicarbonate level is low, which is expected with acidosis, but it often corrects itself with insulin and IV fluid replacement. Rationale 3: The sodium level is low but is not as critical as another option. Rationale 4: Insulin treatment when potassium is below 3.3 mEq/L increases the risk for cardiac dysrhythmia or cardiac arrest. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 32-6 Question 6 Type: MCSA The nurse is planning the care for a patient admitted with diabetic ketoacidosis. How does the nurse anticipate this condition will be medically managed? 1. BID dosing of NPH insulin and PRN coverage with regular insulin 2. A continuous low-dose intravenous infusion of regular insulin 3. Once-per-evening dose of Lantus insulin with daytime coverage with regular insulin 4. sliding scale coverage with regular insulin Correct Answer: 2 Rationale 1: Twice a day dosing of NPH insulin and as needed coverage with regular insulin is frequently used to regulate patients with type 1 diabetes experiencing blood sugar fluctuations secondary to physiological stressors. Rationale 2: A low-dose continuous source of insulin provides for stricter regulation and control of the blood sugar because dosing can be regulated hourly. Rationale 3: Once-per-evening dose of Lantus insulin with daytime coverage of regular insulin is frequently used to regulate patients with type 1 diabetes experiencing blood sugar fluctuations secondary to physiological stressors. Rationale 4: Sliding scale coverage with regular insulin is frequently used to regulate blood sugars in a patient with type 2 diabetes who does need a daily insulin dose but is experiencing elevated blood sugars. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 32-5 Question 8 Type: MCSA The nurse is preparing to administer an intravenous infusion containing regular insulin for a patient diagnosed with diabetic ketoacidosis. Which nursing intervention added to the patient’s plan of care has the highest priority? 1. Check urine for ketone bodies every shift 2. Check blood glucose levels every 2 hours 3. Monitor serum calcium levels closely 4. Adjust infusion rate according to glucose readings. Correct Answer: 4 Rationale 1: The presence of ketones in the urine is significant, but is not an accurate method of evaluating the effectiveness of this treatment. Rationale 2: Blood glucose levels need to be checked hourly. Rationale 3: Serum calcium levels are important but are not the most important intervention. Rationale 4: The most important intervention is to adjust insulin administration in response to glucose readings. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 32-6 Question 9 Type: MCSA A patient with type 2 diabetes mellitus, lethargy, and a blood glucose level of 650 mg/dL has been diagnosed with hyperglycemic hyperosmolar syndrome. The nurse monitors this patient for the development of which complication? 1. Hyperkalemia 2. Seizures 3. Metabolic acidosis 4. Fluid volume overload Correct Answer: 2 Rationale 1: HHS results in a substantial loss of electrolytes. Rationale 2: HHS is associated with severe neurological changes secondary to profound dehydration. Rationale 3: Acidosis is usually not seen with this type of diabetes because sufficient insulin is produced to prevent lipolysis and ketogenesis. Rationale 4: HHS results is osmotic diuresis and resultant dehydration. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 32-4 Question 14 Type: MCMA A patient is brought to the emergency department by her son who reports that she was recently diagnosed with diabetes and “is not acting like herself” today. Which additional findings would the nurse consider as suggesting hyperglycemic hyperosmolar state? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. The son reports his mother’s diabetes is type 2. 2. The patient’s plasma glucose reading is 638 mg/dL. 3. The patient’s bicarbonate level is 14. 4. The patient’s blood pH is 7.28. 5. The patient is 60 years of age. Correct Answer: 1,2,5 Rationale 1: HHS is more common in patients with type 2 diabetes. Rationale 2: Very high serum glucose levels are associated with HHS. Rationale 3: Low bicarbonate levels are associated with DKA. Rationale 4: Acidosis in often not present in HHS. Rationale 5: HHS is seen in older patients, while DKA typically occurs in those younger than 44. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 32-4 Question 15 Type: MCMA A patient diagnosed with hyperglycemic hyperosmotic syndrome (HHS) will be started on rehydration fluids. How will the nurse anticipate managing this treatment? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Initial treatment will be with rapidly infused lactated Ringer’s solution. 2. Once the patient’s blood glucose has decreased to around 200 mg/dL a glucose containing solution will be used for the remaining hydration. 3. The patient will be encouraged to drink as much fluid as possible. 4. The nurse will monitor the patient’s lungs for signs of overload. 5. The fluid used for resuscitation will contain insulin. Correct Answer: 2,4 Rationale 1: Lactated Ringer’s solution will not be used for this patient’s fluid resuscitation. Rationale 2: In order to prevent hypoglycemia as the blood glucose approaches “normal,” the original fluid used for resuscitation is changed to a fluid containing glucose. Rationale 3: The patient will be held NPO until the crisis state is resolved. Rationale 4: This rapid fluid resuscitation places the patient at risk for fluid overload. The nurse should conduct careful assessment for this complication. Rationale 5: The patient will receive intravenous insulin by infusion, but this fluid will not be used for fluid resuscitation. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 32-5 Question 5 Type: MCSA A patient comes into the emergency department with severe burns over the face, arms, legs, and back after spending the day boating with friends. The skin is dry and very red with brisk capillary refill. How would the nurse classify this patient's burn injuries? 1. Superficial 2. Deep partial thickness 3. Superficial partial thickness 4. Full thickness Correct Answer: 1 Rationale 1: Superficial burns involve the epidermis only and are associated with burns from the sun. The burns are red and no blisters are present. Rationale 2: Deep partial-thickness burns involve the epidermis and the deep layer of the dermis. They are caused by contact with flame, hot liquids, tar, or hot objects. Skin may be red or pale and capillary refill is sluggish or absent. Rationale 3: Superficial partial-thickness burns involve the epidermis and papillary layer of the dermis and are caused by contact with hot objects, hot liquids, or flash flame. The skin is red with brisk capillary refill and blisters. Rationale 4: Full-thickness burns involve the epidermis, dermis, and subcutaneous tissue. These are caused by contact with flame, electricity, or chemicals. The skin is dry and leathery or white with absent capillary refill. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 35-2 Question 9 Type: MCSA The nurse is caring for a 154-pound patient with 50 percent total body surface area burns. If using the Parkland formula, the nurse will calculate which amount of intravenous solution to provide this patient in the first 24 hours of care? 1. 14,000 mL 2. 42,000 mL 3. 3,500 mL 4. 7,000 mL Correct Answer: 1 Rationale 1: Based on the Parkland formula, the total amount of fluids required in the first 24 hours = 4 mL of Ringer's lactate × TBSA of burns × patient's weight in kgs. For this patient, 4 mL × 50 × 70 kg = 14,000 mL; 7, 000 mL should be given in the first 8 hours; 3,500 mL in the second 8 hours; and 3,500 mL in the last 8 hours. Rationale 2: This is an inaccurate calculation based on this patient’s weight and TBSA. Rationale 3: This patient will require 3,500 mL in the last 8-hour period of the next 24 hours, not for the entire 24 hours. Rationale 4: This patient will require 7, 000 mL of fluid in the first 8 hours of the next 24 hours. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 35-1 Question 10 Type: MCSA A patient, recovering from being struck by lightning 36 hours prior to admission, is demonstrating an acute onset of confusion and muscle weakness. Which rationale would the nurse provide for this assessment? 1. The patient has is suffering a stroke unrelated to the injury. 2. The patient likely has an electrolyte imbalance. 3. The patient has developed a seizure disorder from the injury. 4. The patient is having delayed onset of neurological symptoms, which are common after a lightning injury. Correct Answer: 4 Rationale 1: There is not enough information for the nurse to determine that the patient is suffering a stroke. Rationale 2: Without more information the nurse cannot attribute this finding to an electrolyte imbalance. Rationale 3: This assessment does not support the diagnosis of a seizure disorder. Rationale 4: Neurological effects are common with electrical and lightning injuries. The onset of clinical manifestations may be acute or delayed. Patients may experience confusion, exhibit a flat affect, lose the ability to concentrate, or have short-term memory problems. Seizures, headaches, peripheral nerve damage, and loss of muscle strength may also be observed. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 35-4 Question 16 Type: MCSA The nurse caring for a patient admitted for burns over his torso and upper arms has clothing adhered to the skin. Which nursing action is indicated? 1. Leave the clothing in place and flush the areas with cooled water 2. Flush the clothing with hydrogen peroxide to clean the skin underneath 3. Cover the areas with gauze 4. Apply a topical antiseptic over the clothing areas Correct Answer: 1 Rationale 1: Clothing, jewelry, belts, or anything containing heat is removed from the patient however adhered clothing or tar is left in place and cooled with water because removing it will cause further damage to the skin. Rationale 2: The nurse should not use hydrogen peroxide on this wound. Rationale 3: Simply covering the areas with gauze is an insufficient intervention. Rationale 4: Applying a topical antiseptic over the clothing is an insufficient intervention. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 35-6 Question 19 Type: MCSA A patient is rehabilitating after a severe burn 6 months ago that left her with scars across her chest and abdomen. She says, “I don’t care what people think, I am going to the beach in a bikini next week.” What most important information should the nurse provide? 1. “This may be difficult since you are still supposed to be wearing your compression garment.” 2. “You need to avoid sun exposure to your scars for at least one year.” 3. “You should prepare yourself for how others will react to your scars.” 4. “Remember that you are prone to getting too hot easily.” Correct Answer: 2 Rationale 1: The patient probably is still supposed to be wearing her compression garment, but this is not the most important consideration. Rationale 2: Scars should be protected from sun exposure for one year or until the scar turns silvery white. Otherwise the scar will “tan” and remain permanently pigmented, leaving a less than satisfactory cosmetic result. Rationale 3: This is an important consideration but is not the most important information for the nurse to share. Rationale 4: This may be the case, but it is not the most important information for the nurse to share. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 35-8 Question 20 Type: MCSA A female patient recovering from a burn to the left side of her face tells the nurse that she has no idea how she is going to return home and resume her regular life since she is so "ugly and disfigured." What nursing response is indicated? 1. “It is good that your work does not include having to meet the public everyday.” 2. “I don’t think your scars are so bad.” 3. “I think you should see a plastic surgeon before you try to go back to work.” 4. “Would you like a referral to the Phoenix Society?” Correct Answer: 4 Rationale 1: This statement reinforces that the patient needs to “hide” from others and is not appropriate. Rationale 2: This statement devalues the patient’s concern and is not appropriate. Rationale 3: Suggesting plastic surgery reinforces the idea that the patient should not be seen in public and is not appropriate. Rationale 4: The Phoenix Society maintains a registry of professionals who specialize in scar therapy and camouflage makeup techniques. This offer of a referral addresses the patient’s concerns, but puts the patient in charge of her decision. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Implementation Learning Outcome: 35-8 Question 5 Type: MCSA A patient with history of chronic liver disease is admitted with acute hemorrhage from esophageal varices. The nurse would expect treatment interventions for which causative condition? 1. The patient has developed gall stones as a result of poor liver function. 2. The patient has portal hypertension with shunting of blood. 3. The NSAID use that caused the patient’s chronic liver failure has also resulted in gastritis. 4. The abdominal distention caused by ascites has resulted in reflux esophagitis. Correct Answer: 2 Rationale 1: Esophageal varices are not associated with gall stones. Rationale 2: Esophageal varices are a complication of portal hypertension. Since the esophageal veins in the lower part of the esophagus are a common collateral flow diversion, any rapid increase in pressure of the engorged veins will lead to an acute hemorrhage. Rationale 3: Gastritis is not associated with esophageal varices. Rationale 4: Esophageal varices are not caused by reflux esophagitis. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 22-4 Question 6 Type: MCSA A patient with acute hepatic dysfunction has abdominal ascites. The nurse would anticipate which laboratory finding? 1. Serum sodium less than135 mEq/L 2. Hematocrit less than 36% 3. HDL level greater than 40 mg/dL 4. Albumin level lower than 3.5 g/L Correct Answer: 4 Rationale 1: Hyponatremia is not associated with abdominal ascites. Rationale 2: Hematocrit will generally rise as fluid is shifted out of the circulating system and into the abdomen. Rationale 3: An elevated high density lipoprotein level is not typically associated with ascites. Rationale 4: Ascites, an abnormal collection of fluid in the abdominal cavity, develops from decreased colloid osmotic pressure and portal hypertension. Colloid osmotic pressure decreases as a result of a reduction in albumin. Hypoalbuminemia is caused by the inability of the liver to carry out its usual protein metabolism functions causing a drop in colloid osmotic pressure and shifting fluid from the intravascular compartment into other body compartments. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 22-4 Question 7 Type: MCMA A patient with acute hepatic dysfunction is prescribed lactulose (Cephulac) 45 mL by mouth four times a day. Which findings will the nurse evaluate as indicating the medication is having its desired effect? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. The patient’s abdominal girth is smaller. 2. The patient has no more oozing from esophageal varices. 3. The patient’s hemoglobin has increased. 4. The patient’s mentation is clearer. 5. The patient has had three stools in the last 24 hours. Correct Answer: 4,5 Rationale 1: Reduction in abdominal girth is not the intended effect of administration of lactulose; however, some reduction may occur. Rationale 2: Decrease in oozing from esophageal varices is not the intended effect of administration of lactulose. Rationale 3: Lactulose is not intended to increase the patient’s hemoglobin. Rationale 4: Lactulose helps to decrease ammonia, which will result in clearer mentation. Rationale 5: Lactulose, a synthetic disaccharide, helps prevent the absorption of ammonia through the bowel by moving the stool through the intestines more rapidly to prevent bacteria from breaking down. Three to five stools daily is the intended effect. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Pharmacological and Parenteral Therapies Nursing/Integrated Concepts: Nursing Process: Evaluation Learning Outcome: 22-3 Question 9 Type: MCMA A patient with acute hepatic dysfunction is experiencing a gastrointestinal bleed. The nurse should be prepared to administer which products? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Mannitol 2. Antibiotics 3. Albumin 4. Vitamin K 5. Fresh frozen plasma Correct Answer: 4,5 Rationale 1: Mannitol would be administered for increased cerebral edema, not bleeding. Rationale 2: The patient may require antibiotics, but this is not the immediate priority. Rationale 3: Albumin is not administered to treat GI bleed. Rationale 4: Treatment for an acute gastrointestinal bleed due to acute hepatic dysfunction includes the administration of vitamin K. Rationale 5: Since this patient is actively bleeding the administration of fresh frozen plasma is indicated. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Planning Learning Outcome: 22-3 Question 11 Type: MCSA A male patient admitted with a gastrointestinal bleed and a hematocrit level of 40% receives fluid resuscitation. In a few hours, the hematocrit level drops to 32%. How should the nurse evaluate this finding? 1. It is very likely that this patient has underlying renal disease. 2. There must be an undiagnosed second site of bleeding. 3. The patient is experiencing hemodilution caused by fluid resuscitation. 4. Efforts to stop the bleeding have not been successful. Correct Answer: 3 Rationale 1: Alterations in the blood urea nitrogen level could indicate underlying renal disease. Rationale 2: This drop is hematocrit level is not unexpected, so a secondary source of bleeding is not a likely causative factor. Rationale 3: During acute hemorrhage, the hematocrit may not reflect the volume of blood loss. Prior to fluid resuscitation, the hematocrit may be higher than expected as a result of hemoconcentration from volume loss. The hematocrit may fall precipitously after aggressive fluid resuscitation because of hemodilution effects. It takes up to 72 hours for the hematocrit to equilibrate following a sudden loss of blood. Rationale 4: This change in hematocrit is not unexpected, so continued bleeding is not a likely reason for the result. Global Rationale: Cognitive Level: Analyzing Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Evaluation Learning Outcome: 20-5 Question 13 Type: MCMA A patient was admitted with acute abdominal and back pain. Which test results would the nurse evaluate as indicating additional testing for acute pancreatitis is likely? Note: Credit will be given only if all correct choices and no incorrect choices are selected. Standard Text: Select all that apply. 1. Secretin stimulation test 2. Hematocrit level 3. Hemoglobin level 4. Serum lipase level 5. Amylase Correct Answer: 4,5 Rationale 1: The secretin stimulation test helps determine pancreatic activity but will not necessarily aid in the diagnosis of acute pancreatitis. Rationale 2: Hematocrit level is not used to help diagnose the presence of acute pancreatitis. Rationale 3: Hemoglobin level is not used to help diagnose the presence of acute pancreatitis. Rationale 4: Lipase levels in the serum will be elevated if pancreatic inflammation is present. Lipase is currently the best enzyme to identify acute pancreatitis. Rationale 5: Amylase is often used as a screening test for pancreatitis. Elevated amylase levels indicate the need for additional testing as they can be elevated for multiple reasons. Global Rationale: Cognitive Level: Applying Client Need: Physiological Integrity Client Need Sub: Physiological Adaptation Nursing/Integrated Concepts: Nursing Process: Assessment Learning Outcome: 20-5 1. What is the likely depth of injury in a patient with injuries described as moist, red, with some blister formation, and very painful? a. Superficial, first-degree burn b. Partial-thickness, second-degree burn c. Deep dermal partial-thickness, second-degree burn d. Full-thickness, third-degree burn 2. Which of the following causes can lead to excessive burn edema and shock in the patient with injuries totaling more than 50% total body surface area (TBSA) burn? a. The heat from the burn leads to immediate vascular wall destruction and extravasation of intravascular fluid. b. A positive interstitial hydrostatic pressure occurs in the dermis leading to burn wound edema. c. Plasma colloid osmotic pressure is decreased due to protein leakage into the extravascular space. d. Capillary permeability decreases in burned and unburned tissue, leading to hypovolemia. 3. A patient involved in a house fire is brought by ambulance to your emergency department. He is breathing spontaneously but appears agitated. He does not respond appropriately to questions. You assume he has inhaled carbon monoxide and is suffering from carbon monoxide (CO) poisoning. Your first action is to a. ask the physician to order a STAT chest radiograph to rule out a pneumothorax. b. apply a pulse oximeter to one of his unburned fingers. c. call the local hyperbaric chamber to check on their availability. d. Apply 100% O2 via facemask 7. A 68-year-old patient is brought to the emergency department after a house fire. He fell asleep with a lit cigarette and the couch ignited. What do you do first? a. Clean the wounds and remove blisters. b. Assess the airway and provide 100% oxygen. c. Place a Foley catheter and assess for myoglobin. d. Place a central intravenous access and provide antibiotics. 11. Which of the following conditions is most likely to result in increased ICP? a) Hypoxia b) Hyperoxia c) Hypocapnia d) Hypercapnia 12. Which of the following medications is prescribed to decrease cerebral vasospasm? a) Phenytoin (Dialantin) b) Phenobarbital c) Nimodipine (Nimotop) d) Vecuronium (Norcuron) 13. Mr. P becomes flaccid with fixed and dilated pupils. His ICP falls from 65 mm Hg to 12 mm Hg. What should the nurse suspect is happening? a) Mr. P is having a seizure. b) Mr. P’s brain has herniated. c) Mr. P’s cerebral edema is resolving. d) Mr. P is excessively dehydrated from the mannitol. 5. The patient has had a stroke or brain attack, believed to be ischemic in nature. The causes of an ischemic stroke are least likely to include which of the following? A) Thrombus of a cerebral artery B) Embolus of a cerebral artery C) Ruptured cerebral aneurysm D) Cerebrovascular obstruction Ans: C Client Needs: D-4 Cognitive Level: Application Difficulty: Easy Integrated Process: Nursing Process Objective: 3 Page and Header: 891, Etiology Feedback: Ischemic strokes are caused by cerebrovascular obstruction from thrombi or emboli resulting in ischemia and infarction. Hemorrhagic strokes are caused by intracerebral hemorrhage, ruptured cerebral aneurysm, or ruptured cerebral arteriovenous malformation. 6. A patient is being cared for in the CCU after a ruptured cerebral aneurysm. The nurse finds new onset of hemiparesis, slight lethargy, and complaints of diplopia. What complication does the nurse suspect? A) Aneurysm rebleed B) Increased intracranial pressure C) Cerebral artery vasospasm D) Carbon dioxide retention Ans: C Client Needs: D-4 Cognitive Level: Analysis Difficulty: Moderate Integrated Process: Nursing Process Objective: 2 Page and Header: 886, Medical Management of Complications Feedback: Signs of vasospasm are hemiparesis, visual disturbances, seizures, and a decreasing level of consciousness. An aneurysm rebleed and increased intracranial pressure are less likely to produce hemiparesis or visual disturbances. There is no evidence of carbon dioxide retention in the scenario. 9. A patient has been diagnosed with partial seizures. What behaviors during this patient's seizures that would not occur during a generalized seizure does the nurse expect? A) Aura prior to seizure B) Twitching confined to one arm C) Absence of purposeful movement D) Postictal period or state Ans: B Client Needs: A-2 Cognitive Level: Application Difficulty: Moderate Integrated Process: Nursing Process Objective: 5 Page and Header: 902, Clinical Manifestations Feedback: A partial seizure involves only part of the body, whereas a generalized seizure involves the entire body. Aura, absence of purposeful movement, and postictal state can occur in both partial and generalized seizures. Critical Care – Nervous System Alterations 1. . Mr. Jones is in the intensive care unit following a motor vehicle crash. He is oriented to person, place, and time; can move all extremities; and follows commands. His pulse is 75 beats/min, his blood pressure is 120/70 mm Hg, and his respirations are 18 breaths/min and regular. Which assessment finding by the nurse best indicates the earliest finding that Mr. Jones' intracranial pressure is increasing? A. Blood pressure of 130/60 B. Flexion posturing C. Heart rate of 53 beats/min D. Orientation to person only 2. 2. A patient with a head injury has an intracranial pressure (ICP) of 18 mm Hg. Her blood pressure is 144/90 mm Hg, and her mean arterial pressure (MAP) is 108 mm Hg. What is the cerebral perfusion pressure (CPP)? A. 54 mm Hg B. 72 mm Hg C. 90 mm Hg D. 126 mm Hg 3. 3. While caring for a patient with a traumatic brain injury, the nurse assesses an ICP of 20 mm Hg and a CPP of 85 mm Hg. What is the best interpretation by the nurse? A. Both pressures are high B. Both pressures are low C. ICP is high; CPP is normal D. ICP is high; CPP is low 4. 4. The nurse is caring for a patient with a sustained ICP of 18 mm Hg for the past 30 minutes during the morning assessment and hygiene interventions. What is the best nursing action? A. Avoid hyperoxygenation during endotracheal suctioning. B. Change ventriculostomy dressing using strict aseptic technique. C. Place the patient in the Trendelenburg position. D. Provide rest periods between interventions. 5. 5. While caring for a patient with a basilar skull fracture, the nurse assesses clear drainage from the patient’s left naris. What is the best nursing action? A. Have the patient blow the nose until clear. B. Insert bilateral cotton nasal packing. C. Place a nasal drip pad under the nose. D. Suction the left nares until the drainage clears. 6. 6. The nurse is caring for a patient who was hit on the head with a hammer. The patient was unconscious at the scene briefly but is now conscious upon arrival at the emergency department (ED) with a GCS score of 15. One hour later the nurse assesses a GCS score of 3. What is the best nursing action? A. Apply noxious stimuli to arouse the patient. B. Continue to monitor the patient. C. Lower the patient’s head of the bed. D. Notify the physician immediately. 7. 7. The nurse is caring for a patient with an ICP of 18 mm Hg and a GCS score of 3. Following the administration of mannitol (Osmitrol), which assessment finding by the nurse indicates an appropriate response to therapy? A. A decrease in CPP and low urine specific gravity B. A decrease in ICP and an increase in urine output C. An improvement in GCS score and a decrease in urine output D. An increase in CPP and high urine specific gravity 8. 8. The nurse is caring for a mechanically ventilated, brain injured patient. Arterial blood gas values indicate a PaCO2 of 60 mm Hg. The nurse understands this value to have which effect on cerebral blood flow? A. Altered cerebral spinal fluid production and reabsorption B. Decreased cerebral blood volume due to vessel constriction C. Increased cerebral blood volume due to vessel dilation D. No effect on cerebral blood flow (PaCO2 of 60 mm Hg is normal) 9. 9. The nurse assesses a patient’s GCS score to be 3. What is the best interpretation by the nurse? A. Does not open eyes, no motor response, and no verbal response B. Opening eyes spontaneously, obeys verbal commands, and is oriented C. Opening eyes to voice, localizing to pain, and is disoriented but converses D. Opens eyes to pain, localizes to pain, and uses inappropriate words 10. 10. The nurse is caring for a patient with a previous GCS score of 15. Nursing assessment 4 hours later notes a GCS score of 8. The nurse anticipates which action? A. Bispectral index (BIS) monitoring B. Computerized axial tomography (CAT) scan C. Continuous electroencephalography (EEG) D. Jugular bulb oxygen saturation monitoring 11. 11. The nurse is caring for a patient who has a diminished level of consciousness and who is mechanically ventilated. While performing endotracheal suctioning, the patient reaches up in an attempt to grab the suction catheter. What is the best interpretation by the nurse? A. The patient is exhibiting extension posturing. B. The patient is exhibiting flexion posturing. C. The patient is exhibiting purposeful movement. D. The patient is withdrawing to stimulation. 12. 12. An awake, alert patient arrives at the ED following a fall down a flight of stairs. The physician suspects a basilar skull fracture. Which assessment findings should the nurse anticipate? A. Babinski’s reflex and tinnitus B. Brudzinski’s and Kernig’s signs C. Flexion and extension posturing D. Rhinorrhea and raccoon eyes 13. 13. While caring for a patient with a closed head injury, the nurse assesses the patient to be alert with a blood pressure 130/90 mm Hg, heart rate 60 beats/min, respirations 18/min, and a temperature of 102° F. To reduce the risk of increased ICP in this patient, what are the priority nursing actions? A. Ensure adequate periods of rest between nursing interventions. B. Insert an oral airway and monitor respiratory rate and depth. C. Maintain neutral head alignment and avoid extreme hip flexion. D. Reduce ambient room temperature and administer antipyretics. 14. 15. Ten days following surgery to clip an anterior communicating artery aneurysm, a transcranial Doppler detects cerebral vasospasm in a patient. The nurse anticipates which therapeutic intervention? A. Fluid restriction B. Nicardipine (Nimodipine) C. Nitroprusside (Nipride) D. Phenytoin (dilantin) 15. 16. The nurse is caring for a patient from a rehabilitation center with a preexisting complete cervical spine injury who is complaining of a severe headache. The nurse assesses a blood pressure of 180/90 mm Hg, heart rate 60 beats/min, respirations 24/min, and 50 mL of urine via Foley catheter for the past 4 hours. What is the best action by the nurse? A. Administer acetaminophen as ordered for the headache. B. Assess for a kinked Foley catheter or bowel impaction. C. Begin an infusion of sodium nitroprusside (Nipride). D. Notify the physician of the patient’s blood pressure. 16. 17. The nurse admits a patient to the ED with new onset of slurred speech and rightsided weakness. What is the priority nursing action? A. Assess for the presence of a headache. B. Assess the patient’s general orientation. C. Determine the patient’s drug allergies. D. Determine the time of symptom onset. 17. 19. The nurse admits a patient to the ED with a suspected cervical spine injury. What is the priority nursing action? A. Keep the neck in the hyperextended position. B. Maintain proper head and neck alignment. C. Prepare for immediate endotracheal intubation. D. Remove cervical collar upon arrival to the ED. 18. 22. The nurse is preparing to monitor ICP with a fluidfilled monitoring system. The nurse understands which principles and/or components to be essential when implementing ICP monitoring (choose all that apply)? A. Administer a heparin flush solution B. Manually flush the device “prn” to maintain catheter patency C. Record ICP as a “mean” value D. Use a pressurized flush system E. Zeroreference the transducer system at the level of the foramen of Munro 19. 24. The nurse is caring for a patient admitted with new onset of slurred speech, facial droop, and left sided weakness 8 hours ago. Diagnostic computed tomography scan rules out the presence of an intracranial bleed. Which actions are most important to include in the patient’s plan of care (choose all that apply)? A. Compare frequent neurological assessments with baseline. B. Maintain CO2 level at 50 mm Hg. C. Maintain mean arterial pressure less than 130 mm Hg and systolic blood pressure less than 220 mm Hg. D. Prepare for therapeutic thrombolytic administration. E. Restrain affected limb to prevent injury. 9) The nurse would expect to find which assessment finding for a patient with a tension pneumothorax? 1. Tracheal deviation to the unaffected side 2. Bilateral equal chest movement 3. Decreased muscular effort by chest muscles 4. Decreasing central venous pressure (CVP) Answer: 1 Explanation: 1. As air accumulates on the pleural space with no place to escape, the affected lung collapses and the resulting increase on intrathoracic pressure puts pressure on the trachea, which causes displacement to the unaffected side. #2 is incorrect. Normal breathing is bilaterally equal. In a tension pneumothorax, one or more areas of the lung tissue collapses and does not expand, therefore limiting the chest movement on that side. Therefore, the movement is bilaterally unequal. #3 is incorrect. Increased muscle effort will be the response to decreasing lung activity. Extra muscles of the chest are called into place to try to increase the effort to move the air within the lung tissues. #4 is incorrect. The CVP will increase to try to compensate for decreased pulmonary perfusion from a decrease in the surface area for oxygen to be exchanged. Learning Outcome: 8-4: Compare and contrast manifestations and management of various types of thoracic strategies 12) Immediate intervention for a sucking chest wound would include which of the following? (Select all that apply.) 1. Prepare the patient for chest tube insertion. 2. Administer pain medication. 3. Prepare for emergency intubation. 4. Apply a dressing that is taped on three sides. 5. Continue to monitor pulse oximetry and respiratory characteristics. Answer: 1, 2, 4, 5 Explanation: 1. (Note: This requires multiple responses to be correct.) A sucking chest wound sucks atmospheric air into the chest cavity with each breath. Closing off this air will decrease the collapse of lung tissue by using a dressing that allows air to leave the chest cavity (thus not taping all four sides) but decreasing the intake of air on inhalation. Chest tubes are used to reinflate lung tissue by creating a negative pressure. Pain medication will allow an ease in the breathing effort and reduce pain on insertion of the chest tube. #3 is an incorrect response. Emergency intubation may not be required because the patient can still breathe. The problem is not the effort to inhale or exhale air but to expand the collapsed lung tissue and prevent pressure buildup in the enclosed lung cavity. 17) A nurse notes that a patient with a traumatic brain injury is having a rapid decline in level of consciousness. If the nurse suspects, cerebral herniation, the most appropriate intervention would be to: 1. Briefly hyperventilate the patient. 2. Take measures to increase intracranial pressures by Trendelenburg positioning. 3. Prepare for emergency surgical repair. 4. Contact the family to come say their last words with the patient. Answer: 1 Explanation: 1. Hyperventilating the patient lowers the ICP by lowering the PaCO2 that is causing vasoconstriction of the cerebral blood vessels and reducing cerebral blood flow (CBF). #2 is incorrect. By increasing ICP pressures by lowering the head of the bed below the feet, the herniation is receiving even less oxygen and at greater risk of permanent damage from decreased CBF. #3 is incorrect. Emergency surgery might be needed but hyperventilating the patient will temporarily allow more time for informed decision making. #4 is incorrect. Although this may be a life and death event, the activity that might reduce this risk can be temporarily avoided by hyperventilation first. 18) Which of the following goals would receive highest priority for the patient with a cervical spine injury? 1. Relieve muscle spasm pain 2. Maintain cervical alignment 3. Support respiratory effort and prevent atelectasis 4. Promote hypothermia Answer: 3 Explanation: 1. Due to the risk of airway obstruction and damage to nerves that stimulate respiratory function, ventilation may need to be controlled or assisted. Air is one of the priority needs according to Maslowʹs theory of hierarchy of needs. #1 and #2 are incorrect responses. Although these goals do apply to this type of patient, airway maintenance and ventilation take a higher status. #4 is incorrect. Hypothermia has been shown to preserve some spinal cord functions but is still a lower need than air. 19) The mother of a patient just admitted with a spinal cord injury is asking if her son will be given steroids. Which of the following would be an accurate way for the nurse to explain the role of steroids in treating spinal cord injuries? 1. Steroids will make the patient feel better overall and retain muscle strength due to its ʺmuscle-bulkingʺ effects. 2. Steroids have few side effects and remove all symptoms while healing the problem. 3. Steroids can lead to ʺroad-rage and anger outburstsʺ and therefore are avoided except under extreme emergencies. 4. Steroids limit spinal cord edema and ischemia if initiated within 3 hours of the trauma and given for 48 hours. Answer: 4 Explanation: 1. This is due to the anti-inflammatory effect of steroid therapy. #1, #2, and #3 are incorrect responses. Emotional highs, anger, and road rage are not common side effects for this category of drugs. These drugs do have some major side effects such as hyperglycemia, hypertension, redistribution of fat pads, and edema as well as others that can be life threatening. Nursing Process: Implementation Cognitive Level: Comprehension Category of Need: Health Promotion and Maintenance; Physiological Integrity–Pharmacological and Parenteral Therapies Chapter 9 Care of the Patient Experiencing an Intracranial Dysfunction 1) A patient with a head injury has a pO2 of 88 and a pCO2 of 58. The nurse realizes that which of the following will occur? 1. Cerebral blood vessels will dilate 2. Cerebral blood vessels will constrict 3. Blood will be shunted from the cerebral cortex 4. Blood flow to the cerebral cortex will slow Answer: 1 Explanation: 1. Autoregulation is the ability of the brain to maintain a constant perfusion despite wide variations in blood pressures. Autoregulation also ensures that cerebral blood vessels dilate in response to a perceived increase in requirements for cerebral blood flow such as when there is an increase in cerebral metabolism, a drop in cerebral oxygen levels, or an increase in cerebral carbon dioxide levels. 3) When providing care to a patient who has increased intracranial pressure, the nurse should be concerned about which of the following patient findings because it is likely to result in an additional increase in intracranial pressure? 1. Blood pressure of 150/65 2. Respiratory rate of 24 3. Temperature of 99°F (37.2°C) 4. Serum sodium of 110 mEq/L Answer: 4 Explanation: 1. The secondary causes are extracranial or systemic processes that contribute to increases in ICP. If these conditions are allowed to exist, they often contribute to secondary injury, producing ongoing increases in ICP and additional damage to the patient who has sustained a brain injury. However, they are often remediable and how to manage them is discussed in detail throughout this chapter. These secondary causes include airway obstruction, hypoxia or hypercarbia from hypoventilation, hypertension or hypotension, position, hyperthermia, seizures, and metabolic disorders, including hyponatremia. 4) A patientʹs mean arterial pressure (MAP) decreases to 50 while his ICP is 20. The nurse realizes that this drop in MAP is likely to lead to: 1. Increased intracranial pressure. 2. Bradycardia. 3. Increased urine output. 4. Hypoxic cerebral tissue. Answer: 4 Explanation: 1. Cerebral perfusion is dependent on the blood pressure and the intracranial pressure. It is the difference between the pressure of the incoming blood or MAP and the force opposing perfusion of the brain, or the intracranial pressure. Normal values for cerebral perfusion pressure should be greater than 50 to 60. A pressure less than 40 to 50 usually results in the loss of autoregulation and leads to hypoxia of cerebral tissue. 5) The nurse is preparing to conduct an hourly neurological assessment on a patient in the intensive care unit. Which of the following would be included in this assessment? 1. ECG 2. Brainstem functioning 3. Level of consciousness 4. Reflexes Answer: 3 Explanation: 1. Components of an hourly neurological assessment usually include, at least, the Glasgow Coma Scale or another assessment of level of consciousness, pupillary response to light, motor function, and vital signs. Assessment of cranial nerves, reflexes, and sensation may be added if indicated. On occasion, the nurse might be involved with assessing brainstem functioning. 6) A patient in the neurological intensive care unit has an endotracheal tube. When the nurse does the hourly Glasgow Coma Scale assessment, what rating would this patient have for verbal response? 1. 4 2. 3 3. 2 4. 1 Answer: 4 Explanation: 1. The Glasgow Coma Scale assesses both level of consciousness and motor response to a stimulus. The scale has three sections: eye opening, motor response, and verbal response. Initially the patient is asked her name, the year, and her location. If the patient is able to respond accurately to these, the score is a 5. If unable to respond or has an endotracheal tube, the score is a 1. 11) The nurse is providing care to a patient with an intracranial pressure monitoring device. Which of the following should be a priority when providing care to this patient? 1. Use clean technique when working with the system. 2. Use strict aseptic technique when working with the system. 3. Perform neurological assessment checks every 2 hours. 4. Monitor intracranial pressure every 4 hours. Answer: 2 Explanation: 1. The most common complication in patients with intracranial monitoring devices is infection. To avoid infection, the nurse should maintain strict aseptic technique when working with the system. Neurological checks and intracranial pressure monitoring should be done every hour. 13) A patient is admitted with a fracture to the base of his skull. Which of the following might the nurse assess in this patient? 1. Cerebral spinal fluid leak from the nose 2. Ecchymoses of the neck 3. Increased intracranial pressure 4. Depressed respiratory rate Answer: 1 Explanation: 1. Basilar fractures occur at the base of the skull. Patients may develop a dural tear and have cerebral spinal fluid draining from their nose and/or ears. Eventually the patient may develop ʺraccoon eyesʺ and Battleʹs sign, ecchymoses about the eyes and behind the ears. There is no evidence to suggest that the patient will have increased intracranial pressure or a depressed respiratory rate. 14) A patient with a skull fracture was admitted unconscious, became conscious, and has since moved into unconsciousness again. This patient is demonstrating findings indicative of: 1. A subdural hematoma. 2. A subarachnoid hemorrhage. 3. An epidural hematoma. 4. A cerebral spinal fluid leak. Answer: 3 Explanation: 1. Epidural hematomas usually occur in conjunction with a skull fracture and result from a laceration of the middle meningeal artery, causing bleeding between the dura mater and the skull. Approximately half of the patients who suffer this injury demonstrate the classic presentation of an initial loss of consciousness followed by a lucid interval then a sudden reloss of consciousness with rapid deterioration in neurological status. Acute subdural hematomas are collections of thick, jelly-like blood that accumulate within the first 24 to 48 hours after blunt trauma. Patients usually present with a loss of consciousness and they may have focal signs such as hemiparesis or dysphagia. Subacute subdural hematomas usually develop over days to weeks following the injury. Chronic subdural hematomas are more common in older adults during the 2 to 3 weeks following the injury. Patient usually develop nonspecific symptoms such as headache, confusion, and speech deficits. Subarachnoid hemorrhage, or bleeding between the arachnoid and pia matter, may result from rupture of a preexisting or a traumatic cerebral aneurysm. 16) A ventilated patient with a head injury needs to be suctioned. Which of the following should the nurse do to limit problems related to suctioning? 1. Limit the duration of each suctioning pass to less than 20 seconds. 2. Reduce the flow of oxygen prior to suctioning. 3. Preoxygenate before suctioning. 4. Medicate with opiates after suctioning. Answer: 3 Explanation: 1. Suctioning the patientʹs endotracheal tube may result in transient reductions in oxygenation. Suctioning is a noxious procedure and for both these reasons may impact ICP. The nurse should preoxygenate the patient prior to suctioning; may medicate the patient prior to suctioning with lidocaine or opiates; limit the duration of each suctioning pass to less than 10 seconds and the number of passes; and observe the effect of PEEP on the patientʹs blood pressure and intracranial pressure to be certain that they are not deleteriously affected. 19) The nurse is planning care for a patient with increased intracranial pressure. Which of the following interventions would be appropriate for this patient? 1. Cluster care activities. 2. Maintain head of bed at a 15-degree angle with knee elevation. 3. Assess for daily bowel movement and provide intervention as appropriate. 4. Encourage family and physician to discuss patientʹs care and prognosis in the patientʹs room. Answer: 3 Explanation: 1. When a patient engages in a Valsalva maneuver such as when he strains when having a bowel movement or pushes himself up in bed, his ICP usually rises. Many neurosurgeons will provide orders for a variety of stool softeners or laxatives. The nurse then uses whichever is necessary to ensure that the patient has a daily soft bowel movement without straining. The patientʹs ICP may rise when nursing activities are delivered in a traditional ʺclusterʺ fashion, with one activity following another. The ICP may rise with the first activity and continue to rise with each additional activity. The patientʹs ICP should be permitted to return to baseline before continuing with other activities. The head of the patientʹs bed should be elevated at 30 degrees to allow for adequate cerebral perfusion while promoting venous return from the head. The body and neck should be in alignment without knee elevation. Keeping external stimulation to a minimum has been demonstrated to limit the rise in ICP. This includes discussion around the patient by both the family and the health care team. Some studies have demonstrated a rise in a patientʹs ICP when discussions about the patient were conducted around him that did not include him. 20) A patient comes into the emergency department with a fever, stiff neck, and change in mental status. On assessment it is learned that this patient also has a positive Kernigʹs sign. These findings suggest the patient: 1. Has meningeal irritation. 2. Needs to be intubated. 3. Should receive 100% oxygen via face mask. 4. Needs surgery to reduce intracranial pressure. Answer: 1 Explanation: 1. Signs of meningeal irritation are observed in approximately 50% of patients with bacterial meningitis. They include the Kernigʹs sign, which is assessed with the patient in a supine position. The hip is flexed at 90 degrees while the knee is flexed at 90 degrees. Extending the knee produces pain in the hamstrings and resistance to further extension. The Brudzinskiʹs sign is assessed with the patient supine and extremities extended and the neck is passively flexed. The patient responds with flexion of the hips when there is meningeal irritation. Intubation, oxygen, and surgery are not treatments for a positive Kernigʹs sign. 21) A patient with acute meningitis is receiving antibiotic therapy. The nurse realizes that another medication is used as adjuvant therapy. This medication is: 1. An anticonvulsant. 2. A barbiturate. 3. A pain medication. 4. A steroid. Answer: 4 Explanation: 1. Steroids are currently recommended as adjunctive treatment of bacterial meningitis. Dexamethasone is believed to interrupt the neurotoxic effects resulting from the lysis of bacteria during the first days of antibiotic use. When steroids are given, they should be administered prior to or during the administration of antibiotics on the first 2 days of therapy. 23) The nurse is providing medication to a patient with status epilepticus. The medication of choice for this patient would be: 1. A steroid. 2. A barbiturate. 3. A benzodiazepine. 4. An opioid. Answer: 3 Explanation: 1. The initial drug of choice is a benzodiazepine, usually lorazepam administered at the rate of 2 to 4 mg IV over 1 minute because it terminates seizures 75% to 80% of the time. The dose may be repeated after 5 to 10 minutes if the seizure has not stopped. The nurse monitors the patientʹs blood pressure, respirations, and oxygen saturation closely because the major adverse effects are respiratory depression, hypotension, and sedation. 9) The nurse is preparing to administer a medication to help decrease the cerebral edema around a patientʹs brain tumor. This medication is most likely a(n): 1. Antiseizure medication. 2. Pain medication. 3. Glucocorticoid. 4. Antispasmodic. Answer: 3 Explanation: 1. Glucocorticoids are the mainstay of treatment for vasogenic cerebral edema. These agents decrease the tissue swelling associated with brain tumors and manage some of the signs and symptoms that patients experience. The decrease in cerebral edema may occur because glucocorticoids directly affect vascular endothelial cell function and restore normal capillary permeability. Dexamethasone may cause cerebral vasoconstriction. Glucocorticoid therapy with dexamethasone has been the standard treatment for tumor-associated edema. #1 is not correct. Antiseizure medication is used to reduce the excitability threshold of brain cells to the stimuli that result in seizure activity. These medications do not reduce cerebral edema. #2 is not correct. Pain medications do not cerebral edema or lower intracranial pressure. These medications can be dangerous in the neuro patient as they can alter level of consciousness. The opiod class is usually contraindicated. The usual pain medication given for comfort is codeine as it provides good pain relief without altering level of consciousness. #4 is not correct. Antispasmodic medications do not cross the blood-brain barrier and have no effect on cerebral tissue. 17) A patient is diagnosed with an intracerebral hemorrhage. Which of the following is the most common cause of this disorder? 1. Hypertension 2. Atrial fibrillation 3. Atherosclerosis 4. Hyperinsulinemia Answer: 1 Explanation: 1. The most common causes of intracerebral hemorrhage are hypertension, trauma, illicit drug use (particularly amphetamines and cocaine), vascular malformations, and bleeding diathesis. Intracerebral hemorrhage results from hypertension when the arteries in the brain become brittle, susceptible to cracking, and rupture. #2 is not correct. Atrial fibrillation increases the risk of the development of an ischemic cerebrovascular accident. This is due to the pooling of blood in the atria that occurs with the loss of atrial kick. #3 is not correct. Atherosclerosis is the cause of hypertension which can lead to intracranial hemorrhage. #4 is not correct. Hyperinsulinemia is a risk factor for the development of atherosclerosis and hypertension which may eventually lead to an intracranial hemorrhage, however, is not a primary cause. 18) A patient tells the nurse that he is experiencing the ʺworst headacheʺ he has ever had. The nurse realizes that this description is often seen in: 1. Intracranial hemorrhage. 2. Ischemic stroke. 3. Subarachnoid hemorrhage. 4. A brain tumor. Answer: 3 Explanation: 1. Subarachnoid hemorrhage is rupture of an aneurysm that releases blood directly into the cerebrospinal fluid under arterial pressure. The blood spreads rapidly, immediately increasing intracranial pressure. If bleeding continues, deep coma or death may result. Typically the bleeding lasts only a few seconds but there is risk of rebleeding. The classic symptom is a sudden, severe headache that begins abruptly and is described as ʺthe worst headache of my life.ʺ #1 is not correct. Intracrananial hemorrhage is a local hematoma in the brain that is manifested by neurologic symptoms such as a change in level of consciousness, sensory and motor deficits. #2 is not correct. Ischemic stroke is characterized confusion, difficulty speaking, visual disturbances, sensory and motor deficits. Headache does occur but the accompanying symptoms are the defining characteristics. #4 is not correct. The headache associated with a brain tumor is worse in the morning but improves during the day. It worsens with coughing, exercise, and changes in position. This type of headache does not respond to usual headache treatment. 20) A patient is diagnosed with an ischemic stroke with the onset of symptoms within the last 2 hours. The best course of treatment for this patient would be to: 1. Admit the patient to a neurosurgical unit for a surgery consultation. 2. Consider the administration of intravenous thrombolysis (rtPA). 3. Observe for continuing symptoms. 4. Provide intravenous fluids. Answer: 2 Explanation: 1. Computerized tomography is the current minimal standard imaging study to rule out hemorrhagic events and to identify patients who are eligible for rtPA therapy. It should be performed within 45 minutes and interpreted within 20 minutes of the patientʹs arrival to the hospital emergency department. . In the case of ischemic stroke, intravenous thrombolysis (rtPA) should be administered if the time since the onset of symptoms is less than 3 hours and the patient is eligible based on criteria. #1 is not correct. If the CT scan is positive for a hemorrhagic stroke, an immediate neurosurgical consult should be ordered. Immediate surgery for an ischemic stroke is not indicated at this time. The priority is to re-establish blood flow to limit neurologic deficits and preserve neurologic function. Once the patient has been stabilized and has recovered, carotid endartarectomy may be considered if indicated. #3 is not correct. Merely observing the patient is not sufficient because as the obstruction continues, the neurologic deficits worsen. The priority is to re-establish blood flow as soon as possible. #4 is not correct. The use of IV fluids is a means to administer antihypertensive medications to control blood pressure. Fluid restriction may be indicated to assist in controlling hypertension but not so restricted to cause dehydration which would increase blood viscosity and this would increase the risk of the development of more thromboemboli. 22) A patient being treated with Coumadin experiences an intracerebral hemorrhage. Which of the following should be considered to aid in the care of this patient? 1. Prepare the patient for surgery. 2. Prepare the patient for a ventriculostomy. 3. Prepare to administer Vitamin K. 4. Prepare to administer protamine sulfate. Answer: 3 Explanation: 1. Since the patient has been receiving the anticoagulant Coumadin (warfarin) the appropriate drug is the administration of Vitamin K to reverse the effects of this medication. #1 is incorrect. Surgery is indicated only after the cause of the bleed has been identified. This management will be based on the location and type of bleed. #2 is not correct. A ventriculostomy is not used as a therapy in the management of the intracerebral hematoma. This therapy is limited and would only indicated if it would be beneficial in reducing intracranial pressure by controlling cerebrospinal fluid. #4 is not correct. Protamine sulfate is the medication used to reverse heparin-associated ICH. The dose is dependent on the time since the cessation of heparin. 18) A patient with portal hypertension with hepatic encephalopathy has been started on a protein restricted diet. The patient asks why he is only being allowed a certain amount of meat. The nurse should explain that a reduced protein diet will: 1. Help to restore his liver function. 2. Help decrease the amount of ammonia in his blood. 3. Give his liver a chance to rest. 4. Prevent fluid from leaking into his abdomen. Answer: 2 Explanation: 1. The goal of treatment is to reduce ammonia production and/or increasing its removal and lower elevated ammonia levels. This may occur by a variety of methods. One of the simplest is bowel cleansing. Another method is limiting the amount of protein in the diet. #1 is not correct. Dietary restriction does not restore liver function but instead lower the production of ammonia. #3 is not correct. #4 is not correct. Ascites can be controlled with sodium and fluid restriction, the use of diuretics, and intermittent administration of salt-poor albumin. 19) A patient with esophageal varices is being treated with an esophageal tamponade (Blakemore) tube. Which of the following should receive the highest priority by the nurse taking care of the patient? 1. Ensuring that the gastric balloon remains inflated 2. Keeping a pair of scissors at the bedside at all times. 3. Keeping the patient sedated and quiet 4. Maintaining the esophageal balloon pressure between 15 and 20 mm Hg Answer: 2 Explanation: 1. Accidental migration of the tube can result in airway obstruction. This requires immediate intervention by cutting all the lumens of the tube to rapidly deflate them and removing the tube. Maintenance of the airway is priority. #1 is not correct. This is important but airway always takes priority. The gastric balloon anchors the tube in place; should it become deflated, the tube could ride up and occlude the airway. It needs to be monitored via daily abdominal x-ray. #3 is not correct. Although this is important to keep the patient from pulling out the tube, airway takes priority. #4 is not correct. Although it is important to maintain this pressure against the varices to prevent bleeding, again airway is the priority. 24) A patient with bleeding esophageal varices is scheduled to receive a bolus followed by a continuous infusion of octreotide (Sandostatin). The nurse preparing the medication should: 1. Anticipate that the medication will stop the bleeding immediately in all patients. 2. Notify the physician if the patient has cardiac disease because the medication is contraindicated. 3. Recognize that doses of 100 mcg/hour and higher are associated with better outcomes. 4. Review serial hematocrits to determine if the patient is continuing to bleed. Answer: 4 Explanation: 1. To evaluate response to the octreotide (Sandostatin) infusion, the nurse would continue to monitor the patientʹs hemodynamic status and expect to see the patientʹs vital signs return to normal, urine output increase, and a decrease in overt bleeding: hematemesis, melena, and hematochezia. Serial hematocrits should be evaluated. #1 is not correct. Octreotide is effective in temporarily stopping the bleeding in approximately 80% of the patients. #2 is not correct. Octreotide (Sandostatin) has an excellent safety margin and is safe for patients with cardiac disease. #3 is not correct. Higher doses of octreotide of greater than 50 mcg/hr may increase systemic venous pressure and do not increase the portal hypotensive effects. Chapter 12 Care of the Patient with an Acute Gastrointestinal Bleed or Pancreatitis 1) A patient arrives in the emergency department with clinical manifestations consistent with a lower gastrointestinal bleed. Which of the following should the nurse assess to determine the patientʹs stability? The patientʹs: 1. Hemoglobin. 2. Hematocrit. 3. Vital signs. 4. Abdominal rigidity to determine the amount of blood being lost. Answer: 3 Explanation: 1. The evaluation of vital signs is the best means to determine the patientʹs stability. Vital signs provide information concerning cardiac and vascular compensation. #1 and #2 are not correct. Initially the patientʹs hemoglobin and hematocrit will not illustrate the true blood loss. This is due to a 6-12 hour delay in intravascular equilibrium related to blood loss. #4 is not correct. Abdominal rigidity will provide a key to the presence of blood in the abdomen but it does not distinguish the amount of bleeding or the patientʹs level of homeostasis nor does it pinpoint the location. 2) A nurse has completed a shift assessment on a patient who has been hospitalized for treatment of a lower gastrointestinal bleed. During the assessment the nurse notes that the patient has a capillary refill of 3 seconds, urinary output of 20 mL/hour, heart rate 88, and reports ʺfeeling tired.ʺ Which of these findings should the nurse report to the physician? 1. Capillary refill of 3 seconds 2. Urinary output of 20 mL/hour 3. Heart rate of 88 bpm 4. Reports of fatigue Answer: 2 Explanation: 1. The patientʹs urinary output is indicative of a worsening condition related to hypovolemia and reduced renal perfusion. Urinary output less than 30 cc/hour should be reported to the physician. A normal urine output is 0.5 - 1 mL/kg/hour. #2 and #3 are not correct. A capillary refill of 3 seconds and a heart rate of 88 bpm are normal findings. #4 is not correct. The hospitalized patient with a lower gastrointestinal bleed will likely report feelings of fatigue related to the blood loss. 3) An ED nurse is advised that a patient with a serious gastrointestinal bleed is en route via ambulance and the physician intends to initiate aggressive intravenous therapy. Which of the following solutions should the nurse anticipate would be utilized to manage this patientʹs condition? 1. Lactated Ringerʹs 2. D5W 3. 0.9% NS 4. 0.45% NS Answer: 3 Explanation: 1. Aggressive intravenous management of a patient with gastrointestinal bleeding is done with an isotonic crystalloid solution such as 0.9% NS. This type of fluid will provide intravascular fluid replacement to the depleted circulating fluid. This is done until the patient can be typed & crossed-matched for blood replacement therapy. #1 is not correct. Lactated Ringerʹs is not used for aggressive fluid resuscitation in patientʹs experiencing blood loss. It contains potassium which could be dangerous in a hypovolemic patient who may be having reduced renal perfusion. #2 and #4 are not correct. Both D5W and 0.45% NS are hypotonic fluid which do not stay in the vascular space but are absorbed by the cells. Therefore, these fluids will not increase intravascular volume. 4) A patient has been transferred to the nursing unit after stabilization in the emergency department for a gastrointestinal bleed. During the initial assessment, the nurse documents the following: Temperature 97.2°F, blood pressure 99/70 mm Hg, heart rate 74 bpm, capillary refill of 3 seconds, and oxygen saturation 94%. Four hours after admission to the unit, the nurse performs a second assessment and notes changes in the patientʹs condition. Which of the following changes is associated with complications from management of the condition? (Select all that apply.) 1. Temperature 98.2°F 2. Heart rate 98 bpm 3. Oxygen saturation 85% 4. Capillary refill of 2 seconds Answer: 2, 3 Explanation: 1. (Note: This requires multiple responses to be correct.) The patient is demonstrating clinical manifestations consistent with fluid overload. Signs of fluid overload include tachycardia, oxygen desaturation, tachypnea, hypotension, and the presence of bibasilar rales. #1 and #4 are not correct. The patientʹs temperature and capillary refill are within normal limits. 9) The nurse is preparing to administer pantoprazole (Protonix) to the patient. The patient asks the nurse for an explanation about the medication. Which of the following responses by the nurse is most appropriate? 1. ʺThe medication will reduce the pH of your gastric secretions.ʺ 2. ʺThe medication will provide a protective coating to your gastrointestinal system.ʺ 3. ʺThe medication is used to reduce the acid in your gastric secretions and reduce the chance of an ulcer.ʺ 4. ʺThe medication will eliminate any potential gastrointestinal infection you may have.ʺ Answer: 3 Explanation: 1. Pantoprazole (Protonix) is a proton pump inhibitor. This classification of medication is used in patients with gastrointestinal disorders. It suppresses the production of gastric acid from the gastric parietal cells. This aids in the reduction of irritation of the mucosa from gastric acid and reduces the risk of ulcer formation. #1 is not correct. A reduction in gastric pH is accomplished with use of antacids. This will result in an increase in acidity of gastric secretions. #2 is not correct. The provision of a protective coating is accomplished with the use of medications such as carafate and cytotec. These medications do not decrease gastric acid production. #4 is not correct. The management of H. pylori infection is treated in association with pantoprazole (Protonix) and the use of antibiotics such as amoxicillin, flagyl, and tetracycline. 12) A patient presents to the physicianʹs office with complaints consistent with pancreatitis. During the history and physical, the patient indicates feeling ill for the past week. Which of the following tests will likely provide the most definitive diagnosis of pancreatitis? 1. Erythrocyte sedimentation rate 2. Serum lipase 3. Serum amylase 4. Complete blood count Answer: 2 Explanation: 1. The patient indicates that the illness has lasted for a week. The serum lipase results are more sensitive and will be most beneficial given the delay in seeking treatment. The serum lipase results will remain elevated for up to 14 days whereas the serum amylase remains elevated for 3 - 5 days. The serum amylase results along with serum lipase are most definitive during the early stages of the disorder. #1 is not correct. The erythrocyte sedimentation rate is used to assess for the presence of inflammation but is not specific to pancreatitis. #3 is not correct. Serum amylase alone is not specific for pancreatitis as it will become elevated with other conditions. #4 is not correct. A complete blood count will reflect the presence of infection but will not be specific for pancreatitis. 14) The patient with severe acute pancreatitis has had aggressive fluid replacement therapy. Which of the following assessment findings is indicative of successful management? 1. Oxygen desaturation 2. Elevated heart rate 3. Decreasing hematocrit 4. Reduced blood pressure Answer: 3 Explanation: 1. Initially the hematocrit may be elevated as a result of fluid volume deficits. A reduction of the hematocrit toward the normal value is a sign that the fluid therapy has been successful. #1 is not correct. Oxygen desaturation is a complication that may indicate that the patientʹs condition is worsening. It most likely would be to fluid volume overload. #2 and #4 are not correct. An elevated heart rate or reduced blood pressure indicates hemodynamic instability related to hypovolemia. 16) A patient with acute pancreatitis voices concerns that she will become addicted to the morphine prescribed for pain management. What response by the nurse is appropriate? 1. ʺYou must only take the medication when the pain is intolerable.ʺ 2. ʺYou may want to consider Demerol to manage your pain because it is less strong.ʺ 3. ʺAddiction during this period of acute pain is not likely.ʺ 4. ʺAddiction is a very real concern and should be considered when requesting medication.ʺ Answer: 3 Explanation: 1. The use of narcotic analgesics during periods of acute pain is unlikely to result in addiction. Prompt pain management is a key to care of this disorder. #1 is not correct. Waiting until the patient is unable to tolerate any additional pain would be inefficient in managing this disorder. Once the acute period of pain has passed, the patient may be managed with nonsteroidal anti-inflammatory medications. #2 is not correct. Demerol is not currently recommended as highly in the management of pancreatitis as morphine. There is better pain control with morphine. #4 is not correct. During times of intense pain, there is little to no risk of addiction as the medications block the pain receptors in the brain. 20) The ICU nurse is caring for a patient with an active gastrointestinal bleed. The patientʹs vitals are BP 80/50 mm Hg, heart rate of 102 bpm, respiratory rate of 24, and oxygen saturation of 80%. The patient is currently receiving a large bolus of normal saline. The physician states that the patient is to receive a transfusion. What component of blood does the nurse anticipate the physician to order? 1. Whole blood 2. Packed red blood cells 3. Platelets 4. Fresh frozen plasma Answer: 2 Explanation: 1. Patients who are hemodynamically unstable and have had considerable blood loss will require blood transfusions of packed red blood cells. Packed RBCʹs are preferred as it replaces the lost red blood cells which will help improve oxygenation. The plasma will help expand volume. #1 is not correct. Whole blood may be ordered in an emergent situation while awaiting cross-matched blood. Packed RBCʹs are more readily available. #3 and #4 are not correct. Platelets and fresh frozen plasma are not indicated at this time with this situation. 21) The ICU nurse is reviewing the labs of a patient newly diagnosed with acute pancreatitis. Which lab values would the nurse expect to be elevated? 1. Amylase and lipase 2. Hemoglobin 3. Platelets 4. PT Answer: 1 Explanation: 1. Amylase and lipase are enzymes excreted by the pancreas. In acute pancreatitis these levels will be increased to at least 3 times the normal level. #2 is not correct. Hemoglobin may be initially elevated if the patient is hypovolemic but with fluid resuscitation it will quickly drop. It may be decreased if the patient has hemorrhagic pancreatitis. #3 is not correct. Platelets are not initially affected with acute pancreatitis. #4 is not correct. Changes in PT are not indicators of pancreatic disease. However this may change with the progression of acute pancreatitis. 22) The critical care nurse is admitting a patient with the diagnosis of acute pancreatitis. The nurse would expect to find the patient has a history of: 1. Alcohol abuse. 2. CHF. 3. Diabetes. 4. Asthma. Answer: 1 Explanation: 1. Alcohol abuse and gallbladder disease are the most common risk factors for acute pancreatitis. #2, #3, and #4 are not correct. CHF, diabetes, and asthma are not common risk factors for acute pancreatitis. 23) The nurse in the emergency department is assisting in the care of a patient with acute gastrointestinal bleeding. The patient has two large-bore IVs in place and is receiving 0.9% normal saline at 200 mL/hour in both IVs. What assessment findings would the nurse need to report to the physician immediately? 1. Crackles in both lung bases 2. Urinary output of 50 mL in 1 hour 3. Capillary refill of less than 2 seconds 4. Approximately 200 mL of coffee ground emesis Answer: 1 Explanation: 1. Crackles on auscultation of the lungs suggest fluid overload. #2 is not correct. Urinary output of 50 mL/hour indicates the fluid volume resuscitation has been successful and that renal perfusion has been maintained. #3 is not correct. A capillary refill of less than 2 seconds is a normal finding of adequate perfusion. #4 is not correct. The presence of coffee ground emesis indicates slowed or stopped bleeding. Chapter 13 Care of the Patient with Endocrine Disorders 1) The patient has an admitting diagnosis of diabetic ketoacidosis. Which of the following problems causes the cascade to diabetic ketoacidosis (DKA)? 1. Ketosis 2. Insulin deficiency 3. Hypoglycemia 4. Dehydration Answer: 2 Explanation: 1. If inadequate insulin is present the cells starve (lack glucose) and use fats as an energy source. Ketoacids are released as a waste product. Lactic acids are produced as a result of anaerobic cellular metabolism. #1, #3, and #4 are incorrect responses. Although ketosis and dehydration are present, they are not the cause of DKA, but rather a result of it. Hyperglycemia, rather than hypoglycemia, is present. 2) The nurse is explaining the pathophysiology of hyperglycemic hyperosmolar nonketotic syndrome (HHNS). Which statement is most accurate? HHNS: 1. Is accompanied by severe metabolic acidosis. 2. Results in cellular overhydration and interstitial space dehydration. 3. Causes severe dehydration from very high osmolarity. 4. Causes a severe decline in glucose production, resulting in increased metabolic rates to burn fat for energy. Answer: 3 Explanation: 1. HHNS is a hyperglycemic state. The body removes glucose with water through the kidneys (osmotic diuresis). This causes severe vascular, interstitial, and cellular water losses, resulting in severe dehydration. #1, #2, and #4 are incorrect responses. If present at all, metabolic acidosis is minimal in HHNS because there is some insulin present to allow glucose into the cells for cellular metabolism. Cells are not overhydrated but instead are dehydrated. Glucose production is increased rather than decreased. 3) When comparing diabetic ketoacidosis (DKA) to hyperglycemic hyperosmolar nonketotic syndrome (HHNS), which statement is accurate? 1. DKA and HHNS are caused by too much insulin in the body. 2. No insulin is present in DKA, whereas some insulin is present in HHNS. 3. DKA results in metabolic acidosis; HHNS results in metabolic alkalosis. 4. Dehydration is greater or more severe in DKA than in HHNS. Answer: 2 Explanation: 1. Although high blood sugars are present in both DKA and HHNS, there is still insulin production with HHNS. #1, #3, and #4 are incorrect responses. In both conditions there is too little, rather than too much, insulin. DKA does result in metabolic acidosis; however, HHNS does not result in metabolic alkalosis. Dehydration is more severe in HHNS than in DKA. 5) When differentiating between diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar nonketotic syndrome (HHNS), which evaluation would be accurate? 1. Clients with DKA exhibit Kussmaulʹs respirations to blow off CO2 and reduce pH levels. 2. Clients with HHNS have lower arterial pH levels than those with DKA. 3. Clients with DKA have more visual disturbances than clients with HHNS. 4. Clients with HHNS have moderate hyperglycemia, whereas clients with DKA have more severe hyperglycemia. Answer: 1 Explanation: 1. Clients with DKA exhibit Kussmaulʹs respirations to blow off CO2 and reduce pH levels. #2, #3, and #4 are incorrect. Clients with DKA are commonly in metabolic acidosis (have lower arterial pH). Clients with HHNS have more visual disturbances due to more severe (and sometimes chronic) dehydration. Clients with DKA have moderate hyperglycemia, whereas clients with HHNS have more severe hyperglycemia. 7) When planning care for the patient with diabetes in diabetic ketoacidosis (DKA) or hyperglycemic hyperosmolar nonketotic syndrome (HHNS), which goals would be included in the plan of care? (Select all that apply.) 1. To reestablish fluid balance through rehydration 2. To effectively treat the precipitating cause for DKA or HHNS 3. To stabilize blood glucose levels to within normal limits 4. To restore A1C blood levels to at or above 8% 5. To increase understanding of self-management to prevent future episodes Answer: 1, 2, 3, 5 Explanation: 1. (Note: This requires multiple responses to be correct.) Dehydration is prevalent due to the excessive glucose that causes severe diuresis. The cause of HHNS or DKA needs to be identified and treated. Normalizing blood glucose levels is important. The goal is less occurrences of HHNS or DKA through self-management. #4 is an incorrect response. The goal is to keep the A1C below 6.5%. 8) Which of the following nursing diagnoses would the nurse NOT use for the plan of care of a patient with diabetic ketoacidosis (DKA) or hyperglycemic hyperosmolar nonketotic syndrome (HHNS)? 1. Excessive fluid volume related to (RT) fluid shifts from hyperosmolarity 2. Imbalanced nutrition, less than body requirements RT inability to utilize glucose 3. Ineffective tissue perfusion RT hypovolemia and decreased peripheral blood flow 4. Risk for infection RT increased blood glucose and decreased peripheral blood flow Answer: 1 Explanation: 1. The patient will have severe dehydration, not fluid overload. High osmolarity is present in HHNS; therefore, this diagnosis is incorrect. #2, #3, and #4 apply to patients with diabetic ketoacidosis (DKA) or hyperglycemic hyperosmolar nonketotic syndrome (HHNS). 10) What should the nurse assess before beginning insulin therapy in a newly admitted patient with diabetes with hyperglycemic hyperosmolar nonketotic syndrome (HHNS)? 1. Sodium level (Na+) 2. Previous history of cardiac dysrhythmias 3. Potassium level (K+) 4. Arterial blood gas results Answer: 3 Explanation: 1. Potassium levels need to be monitored before insulin is given to avoid either hypo- or hyperkalemia from developing because insulin facilitates intracellular transport of glucose and potassium. The rapid shift of the K+ could leave the serum potassium levels dangerously low. #1, #2, and #4 are incorrect responses. Though the nurse would expect to assess and monitor all responses, potassium is important to assess prior to the initiation of insulin therapy. 14) What is the rationale for decreasing serum glucose levels gradually (50-70 mg/dL/hour) in the presence of DKA/HHNS? 1. When blood glucose drops rapidly fluids shift out of the cell, which increases dehydration, causing severe hypovolemic shock. 2. When blood glucose drops rapidly severe damage to the brain results from metabolic alkalosis. 3. A rapid drop in blood glucose can result in hypokalemia, causing life-threatening arrhythmias. 4. A rapid drop in blood glucose can result in formation of thromboses as a result of dehydration. Answer: 3 Explanation: 1. A rapid shift in potassium from the serum into the intracellular compartment may result because IV insulin facilitates the transport of glucose into the cells. This rapid electrolyte shift can cause life-threatening cardiac arrhythmias as a result of hypokalemia. #1, #2, and #4 are incorrect. Dehydration is caused by hyperglycemia and osmotic diuresis rather than the infusion of insulin. Rapidly dropping glucose does not result in metabolic alkalosis or in the formation of thromboses. 17) Which of the following statements explains the reason for seizure precautions in a patient with diabetic ketoacidosis (DKA)? The patient may be at risk for seizures because: 1. Potassium shifts may cause cerebral ischemia. 2. Intracellular fluid shifts may cause cerebral edema. 3. High blood glucose levels overstimulate brain cells. 4. Drugs used to treat the DKA have a side effect of seizures. Answer: 2 Explanation: 1. Rapid fluid shifts into the cell can cause swelling of brain tissues. This puts the patient at risk for seizures. #1, #3, and #4 are incorrect. 3) A patient rescued from a small house fire is brought to the emergency department. There is no burn injury to the patientʹs skin. Lab results show the only abnormality as a CO level of 22%. Which intervention would the nurse expect to implement? 1. Administer high-flow nebulizer treatment. 2. Infuse a fluid bolus of lactated Ringerʹs solution. 3. Begin a sodium bicarbonate drip. 4. Give 100% oxygen by mask. Answer: 4 Explanation: 1. Carbon monoxide has a stronger affinity for hemoglobin than oxygen does so it displaces oxygen as it binds with the hemoglobin. This impairs oxygen transport and tissue perfusion. The treatment is high-flow 100% oxygen. If hyperbaric oxygen therapy is available, it should be used if the patient has a decreased level of consciousness. #1 is not correct. This treatment will only open airways but not displace the carbon monoxide. #2 is not correct. This treatment would be used for fluid resuscitation, not gas exchange treatment. #3 is not correct. A bicarbonate drip is only used for severe metabolic acidosis that is not responsive to other treatment. 5) In assessing a first-degree burn, the nurse would consider which of the following assessments to be accurate? 1. The involved skin is deep reddish-brown in color and edematous. 2. Blisters begin to form on the skin within the first hour of exposure. 3. The skin remains intact because only the epidermal layer is involved. 4. Scarring can be minimized if treatment is sought immediately after injury. Answer: 3 Explanation: 1. Superficial, or first-degree burns, involve only the epidermal layer of the skin, leaving the skin intact. The involved skin is pink to red in color and slightly edematous. #1 is not correct. Blisters will not form until after 24 hours, if at all. #2 is not correct. The TBSA of first-degree burns is not usually included in burn size estimates. #4 is not correct. These burns will heal without scarring in 3 to 6 days. 7) A patient comes to the emergency department with thermal burns to the left arm and shoulder. Which of the following findings requires immediate attention? 1. Complaint of excessive thirst 2. Loss of range of motion to the affected side 3. Pain rating of ʺ8ʺ on a 1 to 10 scale 4. Presence of coughing and hoarseness Answer: 4 Explanation: 1. Immediate signs of inhalation injury are changes to the mucosal lining of the oropharynx and larynx, including the presence of soot, hoarseness, edema, or blisters. The ABCs of resuscitation should be followed. #1 is not correct. Complaint of thirst would be expected due to dehydration. The patient should be kept NPO until an assessment is completed. #2 and #3 are not correct. A high pain rating and limited range of motion to the affected side are also expected findings. 9) A patient in ICU with a burn circling the left upper leg suddenly experiences excruciating pain, pallor in the lower extremity, and loss of pedal pulse. The nurse would immediately notify the physician that this patient has developed which of the following? 1. A deep vein thrombosis 2. Inability to perform ADLs 3. Nosocomial infection 4. Compartment syndrome Answer: 4 Explanation: 1. Compartment syndrom is the correct choice because circumferential extremity burns are at risk for developing compartment syndrome in which the pressure within the muscle compartments is greater than that within the microvasculature. These symptoms are characteristic of a loss of circulation due to compression of the blood vessels. #1 is not correct. Patients often do not have symbpoms with a DVT but if they do, the symptoms are more likely to be swelling,warmth and pain in the extremity. #2 is not correct. The ability to perform ADLs would likely not differ based on the location of the burn. #3 is not correct. All hospitalized patients experiencing burns are at risk for nosocomial infections. 11) An alert patient at the scene of an explosion has a respiratory rate of 24 breaths per minute, a faint stridor, and soot on his face. His heart rate is 120 beats per minute. Which of the following actions would be most appropriate to implement first? 1. Administering humidified oxygen 2. Placing him on a cardiac monitor 3. Inserting a large-bore angiocath 4. Prophylactically intubating the patient Answer: 4 Explanation: 1. This is the most appropriate first action because the first assessment of a burn patient, whether at the scene or in the emergency department, should be a primary trauma survey beginning with the ABCs (airway, breathing, circulation). In order to secure an airway, this patient may be prophylactically intubated because there are signs of progressing respiratory stress and airway edema related to the tachypnea, stridor, and presence of soot, which put him at increased risk for inhalation injury. Procuring a secure endotracheal tube is very important because it is very difficult to reintubate a burn patient due to severe airway edema and neck swelling. #1, #2, and #3 are incorrect. Providing humidified oxygen, placing the patient on a cardiac monitor, and obtaining intravenous access would be appropriate after an airway is secured. 14) A middle-aged man who weighs 220 pounds incurred burns to 40% of his total body surface area. Using the Parkland formula, calculate his fluid resuscitation needs for the first 24 hours. 1. 1,600 mL 2. 16,000 mL 3. 3,520 mL 4. 35,200 mL Answer: 2 Explanation: 1. 16,000mL is the correct amount of IV fluid for resuscitation. The most commonly used formula is the Parkland formula, which recommends 4 mL/kg/% TBSA administered during the first 24 hours following a burn injury. Half of the total resuscitation volume is given in the first 8 hours. To solve the problem, first convert 220 pounds to kilograms: (220 ÷ 2.2 = 100 kg) 4 mL × 100 kg × 40% = 16,000 mL. 16) A patient is complaining of increased pain to a third-degree burn covering the entire arm. The nurse suspects compartment syndrome. Which of the following treatments should the nurse immediate prepare in treating this? 1. Transporting the patient to the whirlpool 2. Applying multiple ace wraps over the current gauze dressing 3. An escharotomy performed by the physician 4. Skin grafting performed by the physician Answer: 3 Explanation: 1. Circumferential burn wounds to the neck, chest, abdomen, and extremities are at risk for developing compartment syndrome. The burn eschar constricts the burned area at the same time that edema is causing subcutaneous fluid expansion. The net result is impaired circulation to the involved area. Compartment syndrome is prevented by performing an escharotomy whereby the physician uses a scalpel or electrocautery to cut through the eschar, which releases tension and permits blood flow to the area. Escharotomies are usually performed at the bedside. The nurse should be prepared to assist in draping and monitoring the patient during the procedure. #1, #2, and #4 are not correct. The whirlpool, ace wraps, and skin grafting treatments would provide no remedy for the impaired circulation. 1. A patient has a spinal cord injury at C6T1. During his bath the nurse notes piloerection. What nursing interventions are indicated? (SATA) a) Ask the patient about the presence of a headache. b) Ignore the occurrence and continue with the bath. c) Determine if the patient’s indwelling urinary catheter tubing is twisted. d) Lower the head of the patients bed. e) Cover the exposed portions of the patients body with a warm bath blanket. Answer: A,C Piloerection and headache may be indicators of autonomic dysreflexia, which is a serious complication and should not be ignored. Occlusion of the tubing from an indwelling urinary catheter may result in a full bladder, which is sufficient noxious stimulus to trigger a serious complication. Simply untwisting the tubing and allowing the bladder to drain may reverse this complication. The head of the bed should be raised. 1. The newly admitted client has burns on both legs. The burned areas appear white and leatherlike. No blisters or bleeding are present, and the client states that he or she has little pain. How should this injury be categorized? a. Superficial b. Partial thickness superficial c. Partial thickness deep d. Full thickness Answer: D The characteristics of the wound meet the criteria for a full-thickness injury (color that is black, brown, yellow, white or red; no blisters; pain minimal; outer layer firm and inelastic). 2. The newly admitted client has a large burned area on the right arm. The burned area appears red, has blisters, and is very painful. How should this injury be categorized? a. Superficial b. Partial thickness superficial c. Partial thickness deep d. Full thickness Answer: B The characteristics of the wound meet the criteria for a superficial partialthickness injury (color that is pink or red; blisters; pain present and high). 3. The burned client newly arrived from an accident scene is prescribed to receive 4 mg of morphine sulfate by IV push. What is the most important reason to administer the opioid analgesic to this client by the intravenous route? a. The medication will be effective more quickly than if given IM. b. It is less likely to interfere with the clients breathing and oxygenation c. The danger of an overdose during fluid remobilization is reduced d. The client delayed gastric emptying. Answer: C Although providing some pain relief has a high priority, and giving the drug by the IV route instead of IM, SC, or orally does increase the rate of effect, the most important reason is to prevent an overdose from accumulation of drug in the interstitial space during the fluid shift of the emergent phase. When edema is present, cumulative doses are rapidly absorbed when the fluid shift is resolving. This delayed absorption can result in lethal blood levels of analgesics. 4. The burned client is ordered to receive intravenous cimetidine, an H2 histamine blocking agent, during the emergent phase. When the client’s family asks why this drug is being given, what is the nurse’s best response? A. “To increase the urine output and prevent kidney damage.” B. “To stimulate intestinal movement and prevent abdominal bloating.” C. “To decrease hydrochloric acid production in the stomach and prevent ulcers.” D. “To inhibit loss of fluid from the circulatory system and prevent hypovolemic shock.” Answer: C Ulcerative gastrointestinal disease may develop within 24 hours after a severe burn as a result of increased hydrochloric acid production and decreased mucosal barrier. Cimetidine inhibits the production and release of hydrochloric acid. 7. At what point after a burn injury should the nurse be most alert for the complication of hypokalemia? A. Immediately following the injury B. During the fluid shift C. During fluid remobilization D. During the late acute phase Answer: C Hypokalemia is most likely to occur during the fluid remobilization period as a result of dilution, potassium movement back into the cells, and increased potassium excreted into the urine with the greatly increased urine output. 8. What clinical manifestation should alert the nurse to possible carbon monoxide poisoning in a client who experienced a burn injury during a house fire? A. Pulse oximetry reading of 80% B. Expiratory stridor and nasal flaring C. Cherry red color to the mucous membranes D. Presence of carbonaceous particles in the sputum Answer: C The saturation of hemoglobin molecules with carbon monoxide and the subsequent vasodilation induces a “cherry red” color of the mucous membranes in these clients. The other manifestations are associated with inhalation injury, but not specifically carbon monoxide poisoning. 9. What clinical manifestation indicates that an escharotomy is needed on a circumferential extremity burn? A. The burn is full thickness rather than partial thickness. B. The client is unable to fully pronate and supinate the extremity. C. Capillary refill is slow in the digits and the distal pulse is absent. D. The client cannot distinguish the sensation of sharp versus dull in the extremity. Answer: C Circumferential eschar can act as a tourniquet when edema forms from the fluid shift, increasing tissue pressure and preventing blood flow to the distal extremities and increasing the risk for tissue necrosis. This problem is an emergency and, without intervention, can lead to loss of the distal limb. This problem can be reduced or corrected with an escharotomy. 11. Which type of fluid should the nurse expect to prepare and administer as fluid resuscitation during the emergent phase of burn recovery? A. Colloids B. Crystalloids C. Fresh-frozen plasma D. Packed red blood cells Answer: B Although not universally true, most fluid resuscitation for burn injuries starts with crystalloid solutions, such as normal saline and Ringer‟s lactate. The burn client rarely requires blood during the emergent phase unless the burn is complicated by another injury that involved hemorrhage. Colloids and plasma are not generally used during the fluid shift phase because these large particles pass through the leaky capillaries into the interstitial fluid, where they increase the osmotic pressure. Increased osmotic pressure in the interstitial fluid can worsen the capillary leak syndrome and make maintaining the circulating fluid volume even more difficult. 13. The client who experienced an inhalation injury 6 hours ago has been wheezing. When the client is assessed, wheezes are no longer heard. What is the nurse’s best action? A. Raise the head of the bed. B. Notify the emergency team. C. Loosen the dressings on the chest. D. Document the findings as the only action. Answer: B Clients with severe inhalation injuries may sustain such progressive obstruction that they may lose effective movement of air. When this occurs, wheezing is no longer heard and neither are breath sounds. The client requires the establishment of an emergency airway and the swelling usually precludes intubation. 15. On admission to the emergency department the burned client’s blood pressure is 90/60, with an apical pulse rate of 122. These findings are an expected result of what thermal injury–related response? A. Fluid shift B. Intense pain C. Hemorrhage D. Carbon monoxide poisoning Answer: A Intense pain and carbon monoxide poisoning increase blood pressure. Hemorrhage is unusual in a burn injury. The physiologic effect of histamine release in injured tissues is a loss of vascular volume to the interstitial space, with a resulting decrease in blood pressure. 16. Twelve hours after the client was initially burned, bowel sounds are absent in all four abdominal quadrants. What is the nurse’s best action? A. Reposition the client onto the right side. B. Document the finding as the only action. C. Notify the emergency team. D. Increase the IV flow rate. Answer: B Decreased or absent peristalsis is an expected response during the emergent phase of burn injury as a result of neural and hormonal compensation to the stress of injury. No currently accepted intervention changes this response, and it is not the highest priority of care at this time. 19. All of the following laboratory test results on a burned client’s blood are present during the emergent phase. Which result should the nurse report to the physician immediately? A. Serum sodium elevated to 131 mmol/L (mEq/L) B. Serum potassium 7.5 mmol/L (mEq/L) C. Arterial pH is 7.32 D. Hematocrit is 52% Answer: B All these findings are abnormal; however, only the serum potassium level is changed to the degree that serious, life-threatening responses could result. With such a rapid rise in the potassium level, the client is at high risk for experiencing severe cardiac dysrhythmias and death. 20. The client has experienced an electrical injury, with the entrance site on the left hand and the exit site on the left foot. What are the priority assessment data to obtain from this client on admission? A. Airway patency B. Heart rate and rhythm C. Orientation to time, place, and person D. Current range of motion in all extremities Answer: B The airway is not at any particular risk with this injury. Electric current travels through the body from the entrance site to the exit site and can seriously damage all tissues between the two sites. Early cardiac damage from electrical injury includes irregular heart rate, rhythm, and ECG changes. 21. In assessing the client’s potential for an inhalation injury as a result of a flame burn, what is the most important question to ask the client on admission? A. “Are you a smoker?” B. “When was your last chest x-ray?” C. “Have you ever had asthma or any other lung problem?” D. “In what exact place or space were you when you were burned?” Answer: D The risk for inhalation injury is greatest when flame burns occur indoors in small, poorly ventilated rooms. although smoking increases the risk for some problems, it does not predispose the client for an inhalation injury. 25. The burned client relates the following history of previous health problems. Which one should alert the nurse to the need for alteration of the fluid resuscitation plan? A. Seasonal asthma B. Hepatitis B 10 years ago C. Myocardial infarction 1 year ago D. Kidney stones within the last 6 month Answer: C It is likely the client has a diminished cardiac output as a result of the old MI and would be at greater risk for the development of congestive heart failure and pulmonary edema during fluid resuscitation. 26. The burned client on admission is drooling and having difficulty swallowing. What is the nurse’s best first action? A. Assess level of consciousness and pupillary reactions. B. Ask the client at what time food or liquid was last consumed. C. Auscultate breath sounds over the trachea and mainstem bronchi. D. Measure abdominal girth and auscultate bowel sounds in all four quadrants. Answer: C Difficulty swallowing and drooling are indications of oropharyngeal edema and can precede pulmonary failure. The client‟s airway is in severe jeopardy and intubation is highly likely to be needed shortly. 31. During the acute phase, the nurse applied gentamicin sulfate (topical antibiotic) to the burn before dressing the wound. The client has all the following manifestations. Which manifestation indicates that the client is having an adverse reaction to this topical agent? A. Increased wound pain 30 to 40 minutes after drug application B. Presence of small, pale pink bumps in the wound beds C. Decreased white blood cell count D. Increased serum creatinine level Answer: D Gentamicin does not stimulate pain in the wound. The small, pale pink bumps in the wound bed are areas of re-epithelialization and not an adverse reaction. Gentamicin is nephrotoxic and sufficient amounts can be absorbed through burn wounds to affect kidney function. Any client receiving gentamicin by any route should have kidney function monitored. 39. Nurse Faith should recognize that fluid shift in an client with burn injury results from increase in the: a. Total volume of circulating whole blood b. Total volume of intravascular plasma c. Permeability of capillary walls d. Permeability of kidney tubules Answer: C In burn, the capillaries and small vessels dilate, and cell damage cause the release of a histamine-like substance. The substance causes the capillary walls to become more permeable and significant quantities of fluid are lost. A. Critically ill patients, especially those with trauma, burns, and sepsis should receive prophylaxis for: o esophageal varices. o gastroesophageal reflux. o portal hypertension. o stress ulcers. Correct B. 4.ID: 43101388 Esophageal varices occur as a result of: o gastroesophageal tearing. o peptic ulcer disease. o portal hypertension. Correct o traumatic injury. C. 5.ID: 43101393 Which of the following assessments may be seen in the first 24 hours after acute gastrointestinal bleeding? o Hypoactive bowel sounds o Low white blood cell (WBC) count o Normal hematocrit level Correct o STsegment elevation on electrocardiogram D. 8.ID: 43101625 The patient is admitted with acute pancreatitis. He is complaining of severe abdominal pain and nausea. He has hyperactive bowel sounds and abdominal distention. His temperature is 103° F and his blood pressure is 86/40 mm Hg. His WBC count is over 20,000/mL. He is jaundiced and the nurse notes a bluish discoloration around the umbilical area. Which of the following is indicated first in managing this patient? o Administration of fluids to manage hypotension Correct o Administration of narcotics to manage acute pain o Application of a cooling blanket to manage fever o Collection of blood culture specimens to assess etiology of infection E. 9.ID: 43101632 The patient with acute pancreatitis would likely have which of the following laboratory values? o Decreased Creactive protein levels o Decreased triglyceride levels o Elevated serum amylase and lipase Correct o Elevated serum potassium and glucose Awarded 0.0 points out of 1.0 possible points. F. 10.ID: 43101639 In patients with pancreatitis, which of the following laboratory results represents the physiological effects of fluid shifts? o Elevated serum glucose level o Elevated WBC count o Low serum albumin level Correct o Low serum calcium level G. 11.ID: 43101646 A priority treatment for patients with severe pancreatitis is: o administration of 50% dextrose to avoid hypoglycemia. o small, frequent oral feedings to stimulate the pancreas. o surgical repair of the pancreas. o volume replacement to treat hypovolemia. Correct H. 14.ID: 43101673 Your patient with ascites has the following nursing diagnoses. Which is your highest nursing priority to address? o Activity intolerance o Altered nutrition o Fluid volume excess o Ineffective breathing Correct I. 15.ID: 43101682 A patient with hepatic failure becomes increasingly confused. What is a likely diagnosis, and what test is done to confirm the diagnosis? o Cerebral edema; computed tomography scan o Encephalopathy; serum ammonia level Correct o Hypoxemia; arterial blood gas analysis o Infection; WBC count 1. 17.ID: 43102009 Which of the following are treatments for hepatic encephalopathy (choose all that apply)? A. Kayexalate B. LactuloseCorrect C. Limited protein intakeCorrect D. NeomycinCorrect 2. Collaborative management of the patient with acute pancreatitis includes which of the following (choose all that apply)? A. Fluid and electrolyte replacementCorrect B. Glycemic controlCorrect C. Managing respiratory dysfunctionCorrect D. Nasogastric suctioningCorrect 3. 19.ID: 43102032 The patient is admitted with esophageal varices. Which of the following medications are considered first linemedications in the treatment of varices (choose all that apply)? A. Neomycin B. OctreotideCorrect C. SomatostatinCorrect D. Vasopressin A. 9.ID: 43103033 Why are narcotics given intravenously to manage pain during initial management of the patient with burns? o Additional skin disruption is to be avoided at all costs. o Burn pain is so severe it requires relief by the fastest route available. o Thrombosis may occur at injection sites. o Tissue edema may interfere with drug absorption via other routes. Correct B. 10.ID: 43103045 When paramedics notice singed hairs in the nose of a burn patient, it is recommended that the patient be intubated at the scene. What is the reasoning for the immediate intubation? o Carbon monoxide poisoning always occurs when soot is visible. o Inhalation injury above the glottis may cause edema that is sufficient to obstruct the airway. Correct o The patient will have a copious amount of mucus that will need to be suctioned. o The singed hairs and soot in the nostrils will cause dysfunction of cilia in the airways. C. 11.ID: 43103055 You are caring for a patient with circumferential burns on his right leg. You note that the capillary refill in his right big toenail is not as brisk as it was 2 hours ago and that the pedal and tibial pulses are only noted by Doppler. What is your best plan of action? o Apply a heating pad to increase the circulation. o Elevate the injured leg more to see if the edema will decrease. o Notify the physician and prepare for a fasciotomy. Correct o Observe and do nothing for another hour to see if the condition gets worse. D. 13.ID: 43103071 Silver is an ingredient in many burn dressings. It is used because it: o functions as a dermal layer to the skin. o is effective against a widespectrum of wound pathogens. Correct o is used as a temporary wound cover. o stimulates wound healing. E. 15.ID: 43103087 Patients with electrical injury are at a high risk for renal failure secondary to: o hypervolemia from burn resuscitation. o increased incidence of ureteral stones. o nephrotoxic antibiotics for prevention of infection. o release of myoglobin from injured tissues. Correct F. 23.ID: 43103454 Which of the following statements about the pain management of a burn victim are true (choose all that apply)? o Additional pain medication may be needed because of rapid body metabolism.Correct o Pain medication should be given before procedures such as debridement, dressing changes, and hydrotherapy.Correct o Patients with a history of drug and alcohol abuse will require higher doses of pain medication.Correct o The intramuscular route is preferred for pain medication administration. A. 7.ID: 43103792 Which of the following interventions would not be appropriate for a patient who is admitted with a suspected basilar skull fracture? o Insertion of a nasogastric tube Correct o Insertion of a Foley catheter o Endotracheal intubation o Placement of an oral airway B. 9.ID: 43103909 In the trauma patient, symptoms of decreased cardiac output are most commonly caused by: o cardiac contusion. o cardiogenic shock. o hypovolemia. Correct o pericardial tamponade. C. 10.ID: 43103916 A patient with multiple traumatic injuries receives fluid to maintain a systolic blood pressure at 90 mm Hg. Despite the administration of 3 L of crystalloids, his systolic blood pressure is in the 80s and is very labile. A focused assessment with sonography for trauma (FAST) test identifies peritoneal hemorrhage. What action is anticipated at this time? o Administration of colloids to maintain intravascular volume o Administration of a vasoactive drip, such as a dopamine drip o Computed tomography scan of the abdomen to assess for a lacerated liver o Emergent surgical intervention to determine the site of bleeding Correct D. 13.ID: 43103942 You are caring for a patient who sustained rib fractures after hitting the steering wheel of his car. He is spontaneously breathing and receiving oxygen via a face mask. His oxygen saturation is 95%. During your assessment, the oxygen saturation drops to 80%. The patient's blood pressure has dropped from 128/76 mm Hg to 84/50 mm Hg. You do not auscultate any breath sounds on the left side of the chest. You notify the physician and anticipate: o administration of lactated Ringer's solution (1 L) wide open. o chest xray study to determine the etiology of the symptoms. o endotracheal intubation and mechanical ventilation. o needle thoracostomy and chest tube insertion. Correct E. 15.ID: 43103956 Patients with musculoskeletal injury are at increased risk for compartment syndrome. What is an initial symptom of a suspected compartment syndrome? o Absence of pulse in affected extremity o Pallor in the affected area o Paresthesia in the affected area o Severe, throbbing pain in the affected area Correct F. 18.ID: 43103983 Which of the following interventions is a strategy to prevent fat embolism syndrome? o Administer lipidlowering statin medications. o Intubate the patient early after the injury to provide mechanical ventilation. o Provide prophylaxis with lowmolecularweight heparin. o Stabilize extremity fractures early. Correct G. 20.ID: 43103997 Treatment and/or prevention of rhabdomyolysis in atrisk patients includes aggressive fluid resuscitation to achieve urine output of: o 30 mL/hr. o 50 mL/hr. o 100 mL/hr. Correct o 300 mL/hr. H. 21.ID: 43104405 Fluid resuscitation is an important component of managing the trauma patient. Which of the following statements are true regarding the care of a trauma patient (choose all that apply)? o 5% Dextrose is recommended for rapid crystalloid infusion. o IV fluids may need to be warmed to prevent hypothermia.Correct o Massive transfusions should be avoided to improve patient outcomes.Correct o Only fully crossmatched blood products are administered I. 23.ID: 43104432 During your assessment of a patient after a motor vehicle crash, which of the following assessments would increase your suspicion of a basilar skull fracture (choose all that apply)? o Battle’s signCorrect o Mucus drainage from the nose o Pinktinged drainage from the ear; positive for glucoseCorrect o Raccoon eyesCorrect J. 25.ID: 43104452 Which of the following patients would require greater amounts of fluid resuscitation to prevent renal failure associated with rhabdomyolysis (choose all that apply)? o Crush injury to right armCorrect o Gunshot wound to the abdomen o Lightning strike of the left arm and torsoCorrect o Pulmonary contusion and rib fracture [Show More]
Last updated: 1 year ago
Preview 1 out of 109 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 08, 2021
Number of pages
109
Written in
Additional information
This document has been written for:
Uploaded
Sep 08, 2021
Downloads
0
Views
121

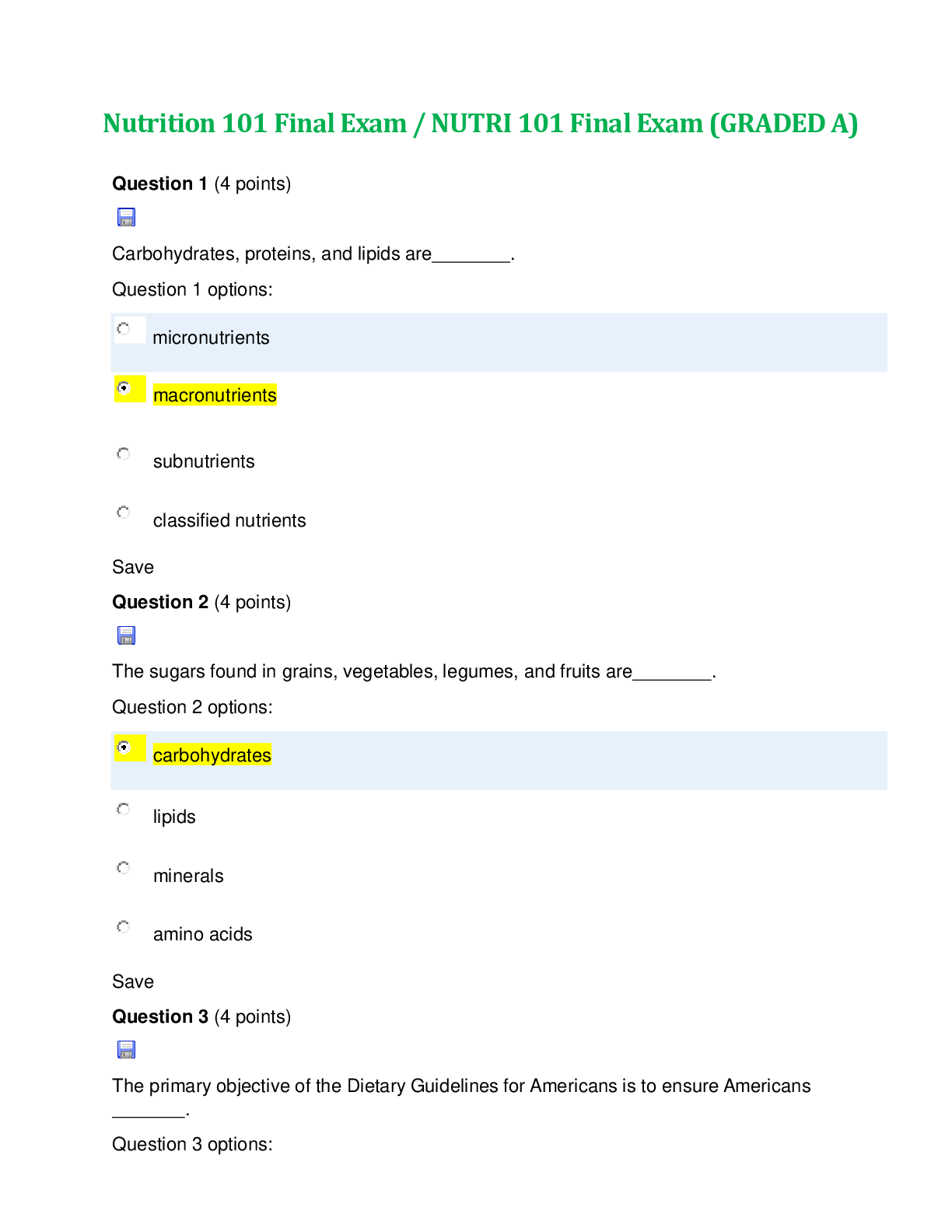

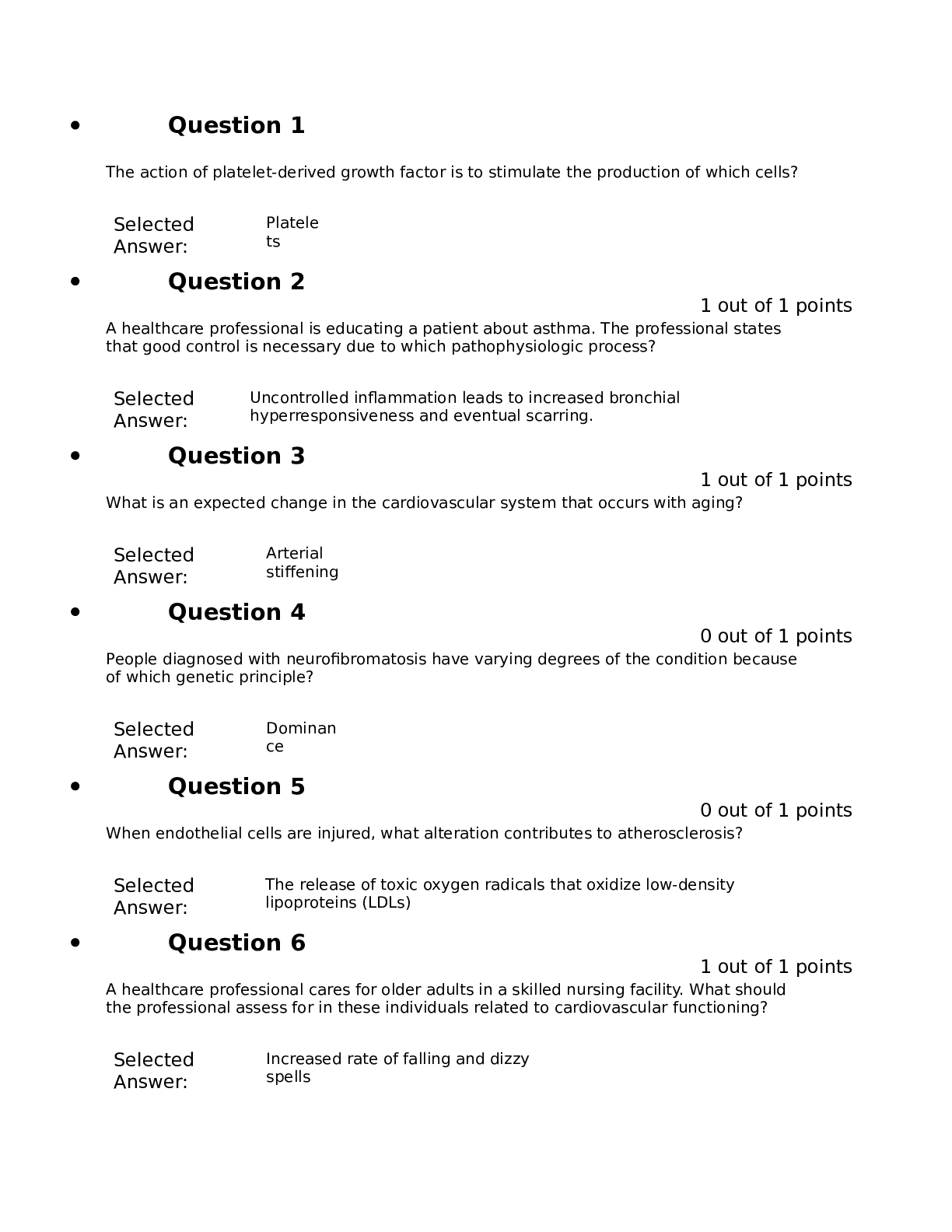
.png)
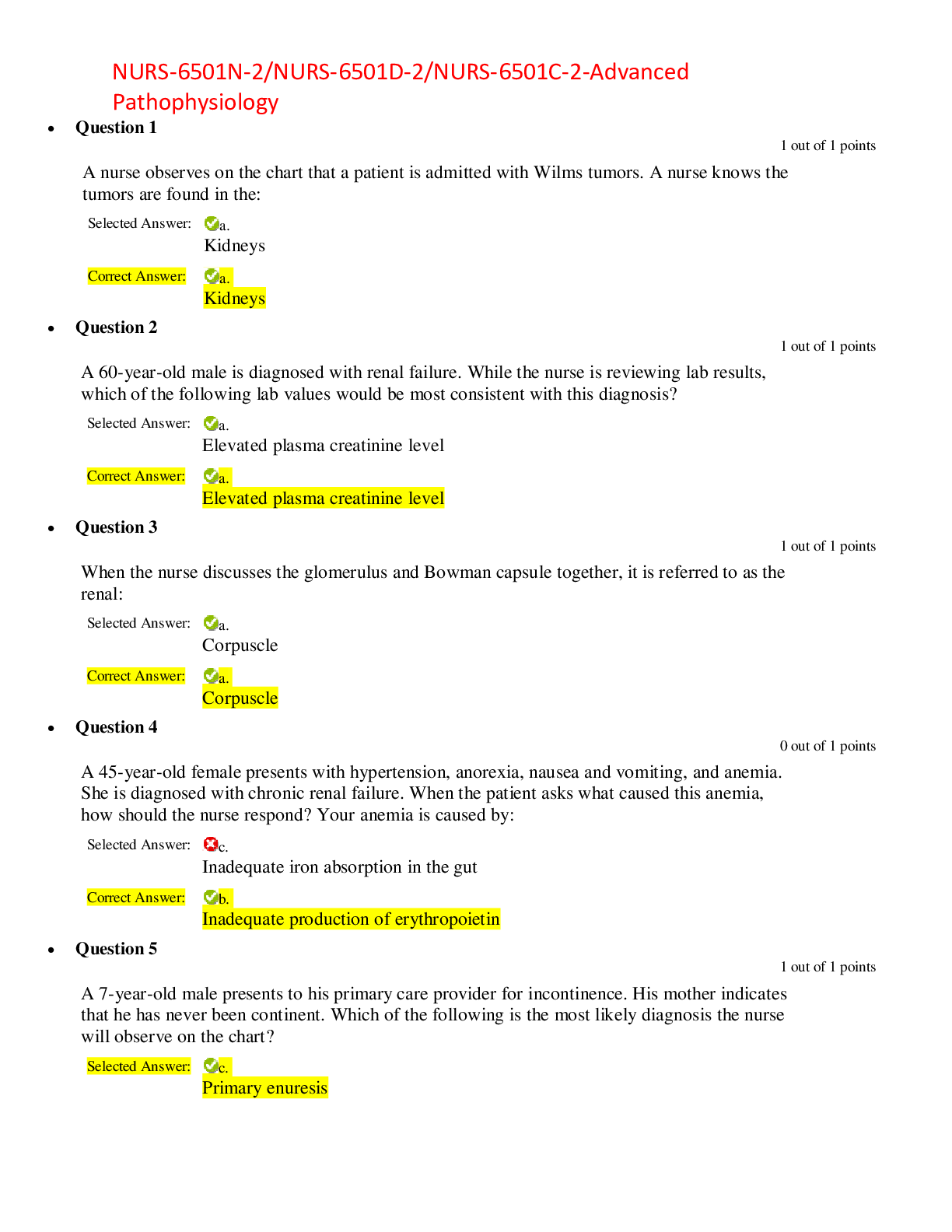

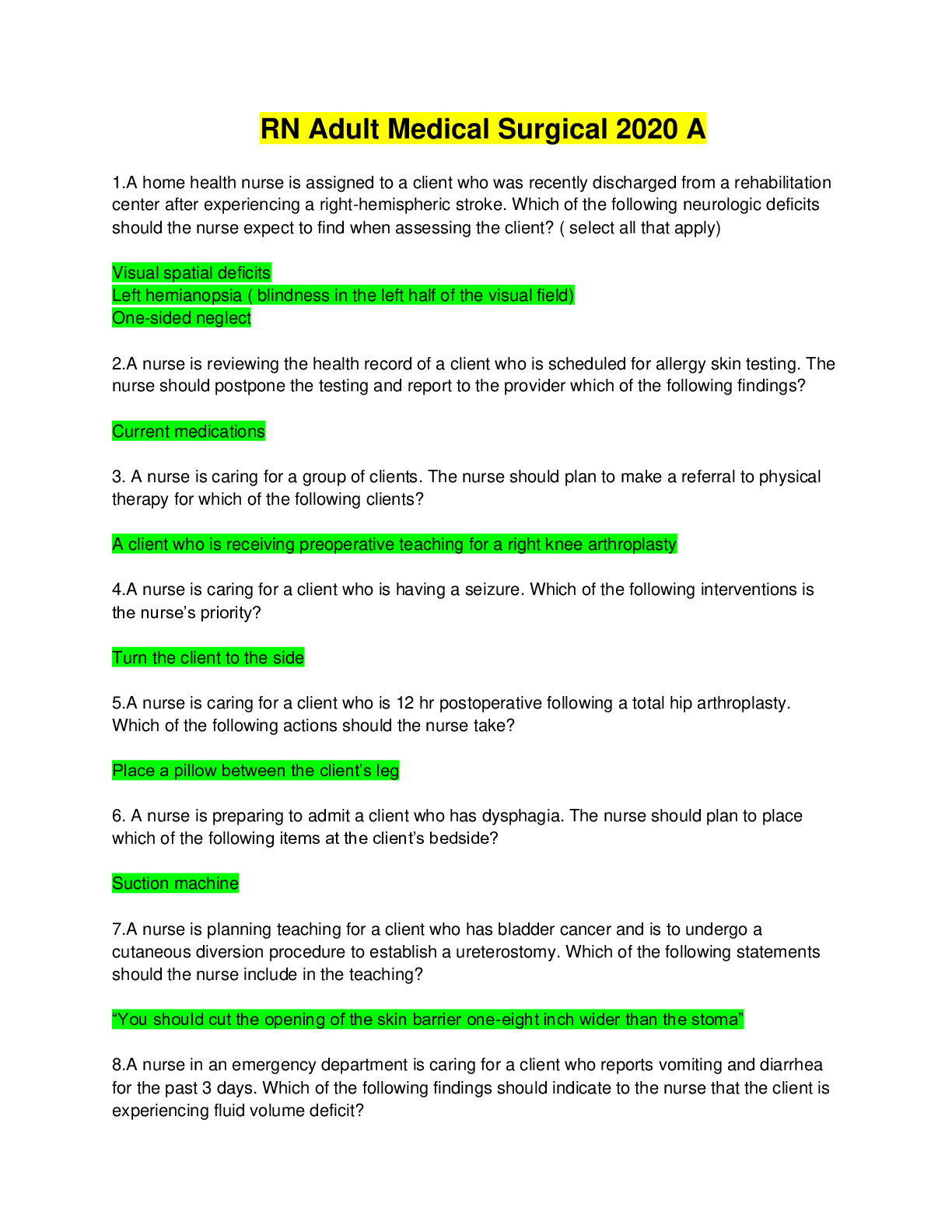
.png)