*NURSING > Summary > NURSING 306 OB Exam 2 Study Guide OB Hartman GOLD, A+ Guide - West Coast University. (All)
NURSING 306 OB Exam 2 Study Guide OB Hartman GOLD, A+ Guide - West Coast University.
Document Content and Description Below
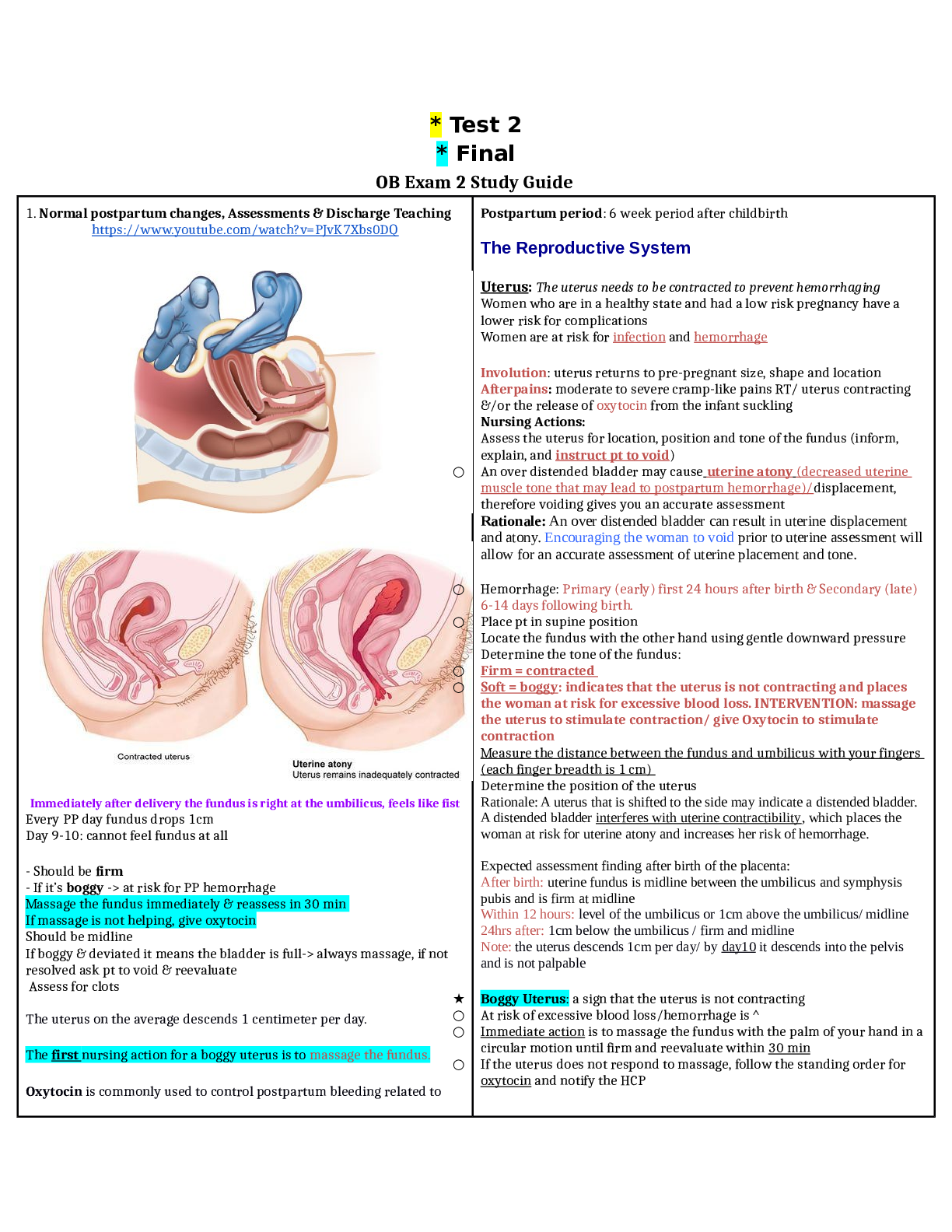
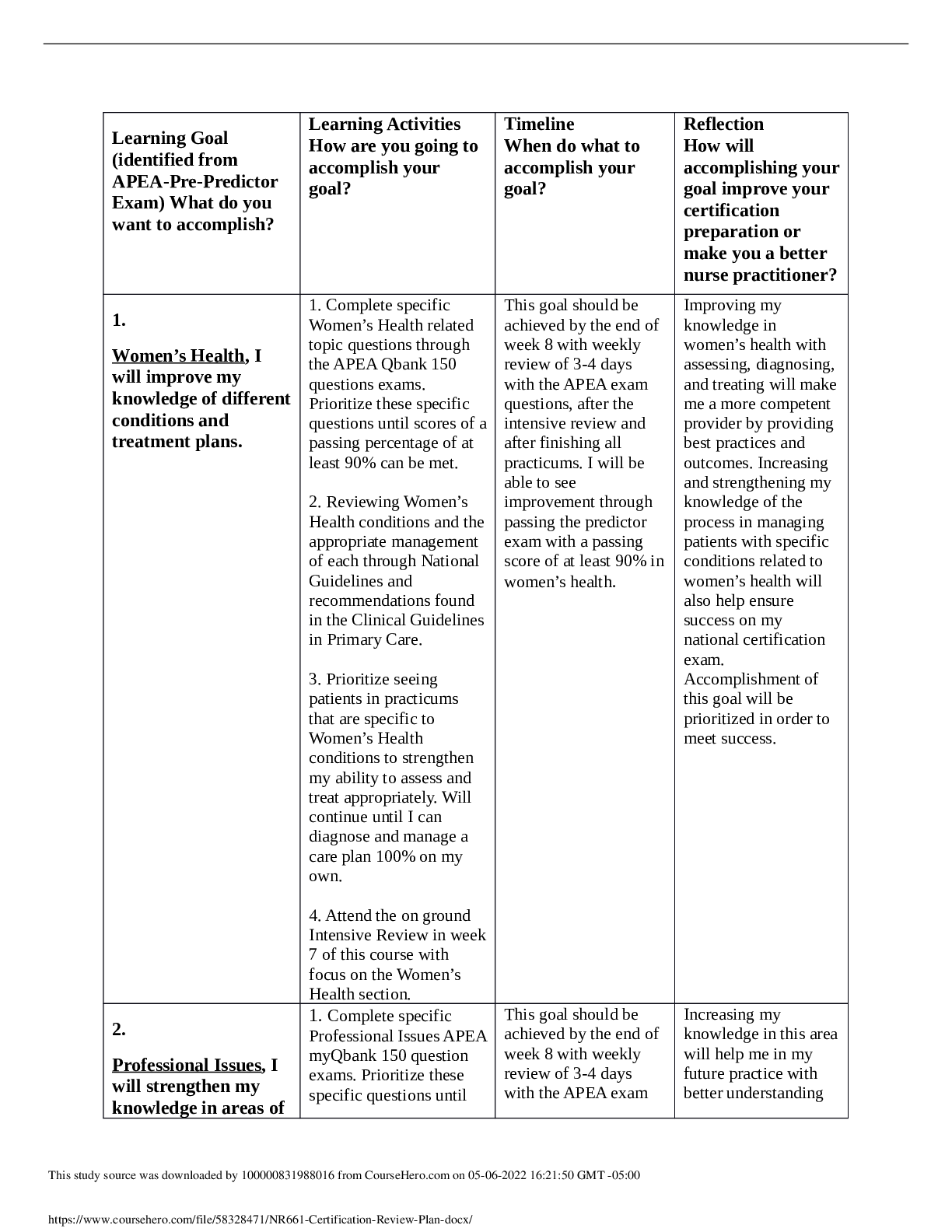
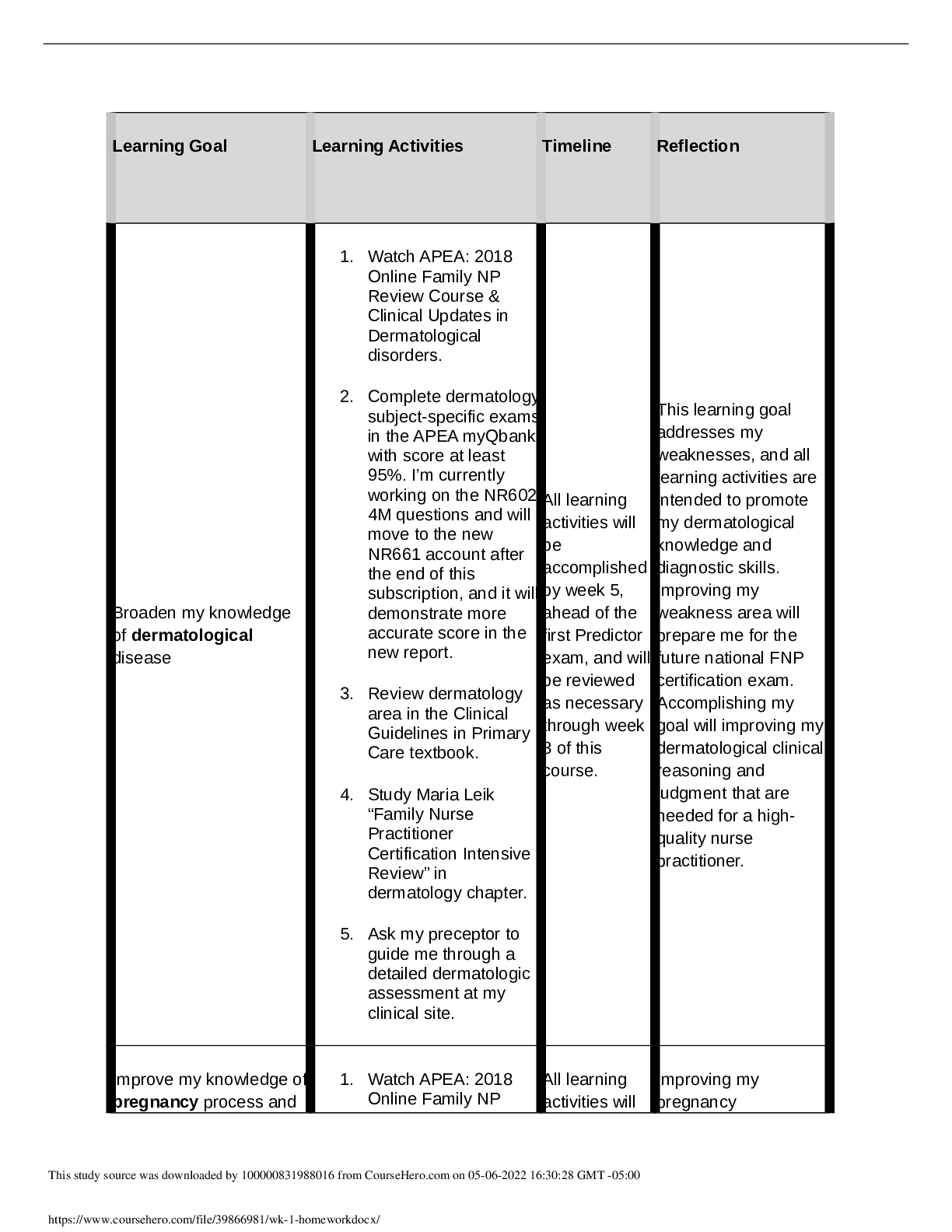
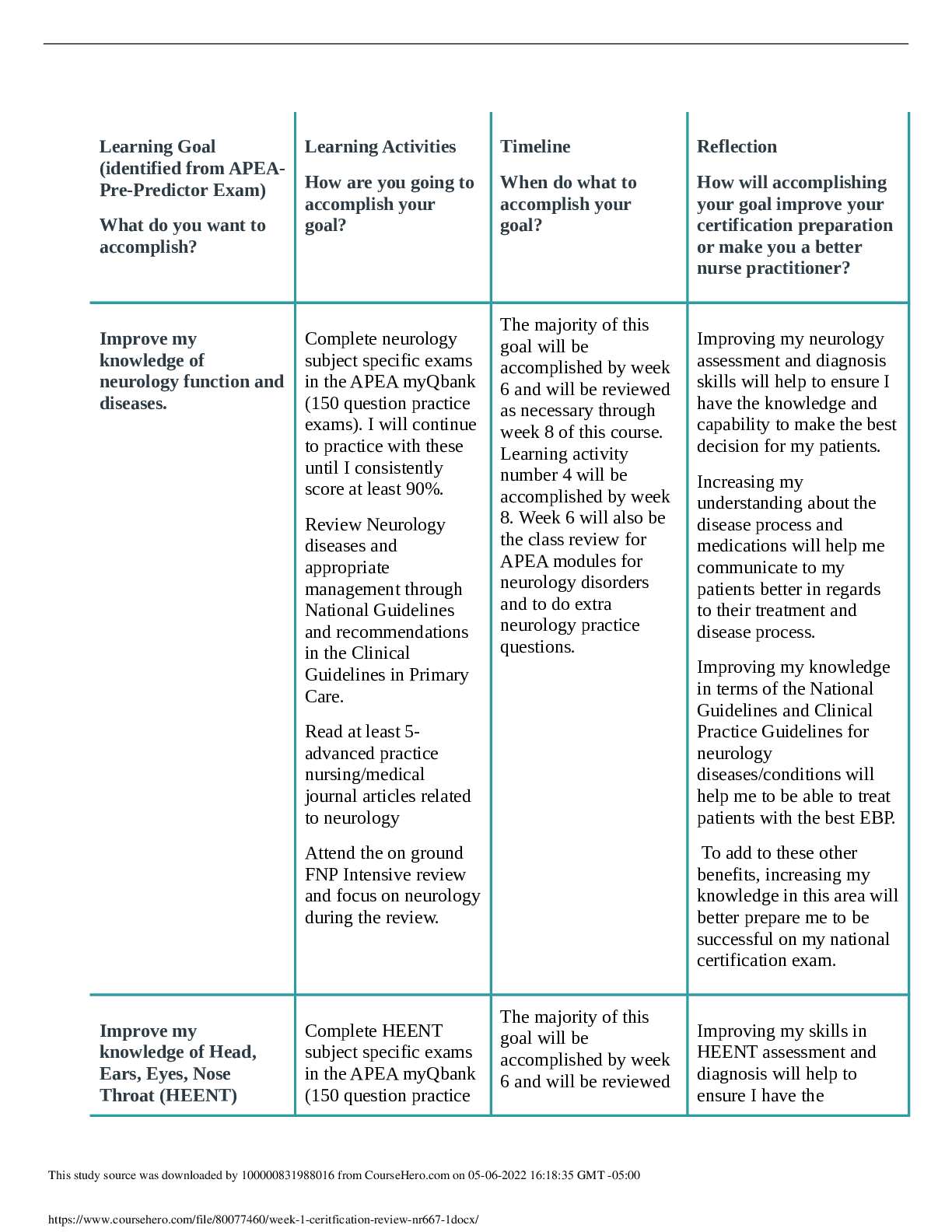
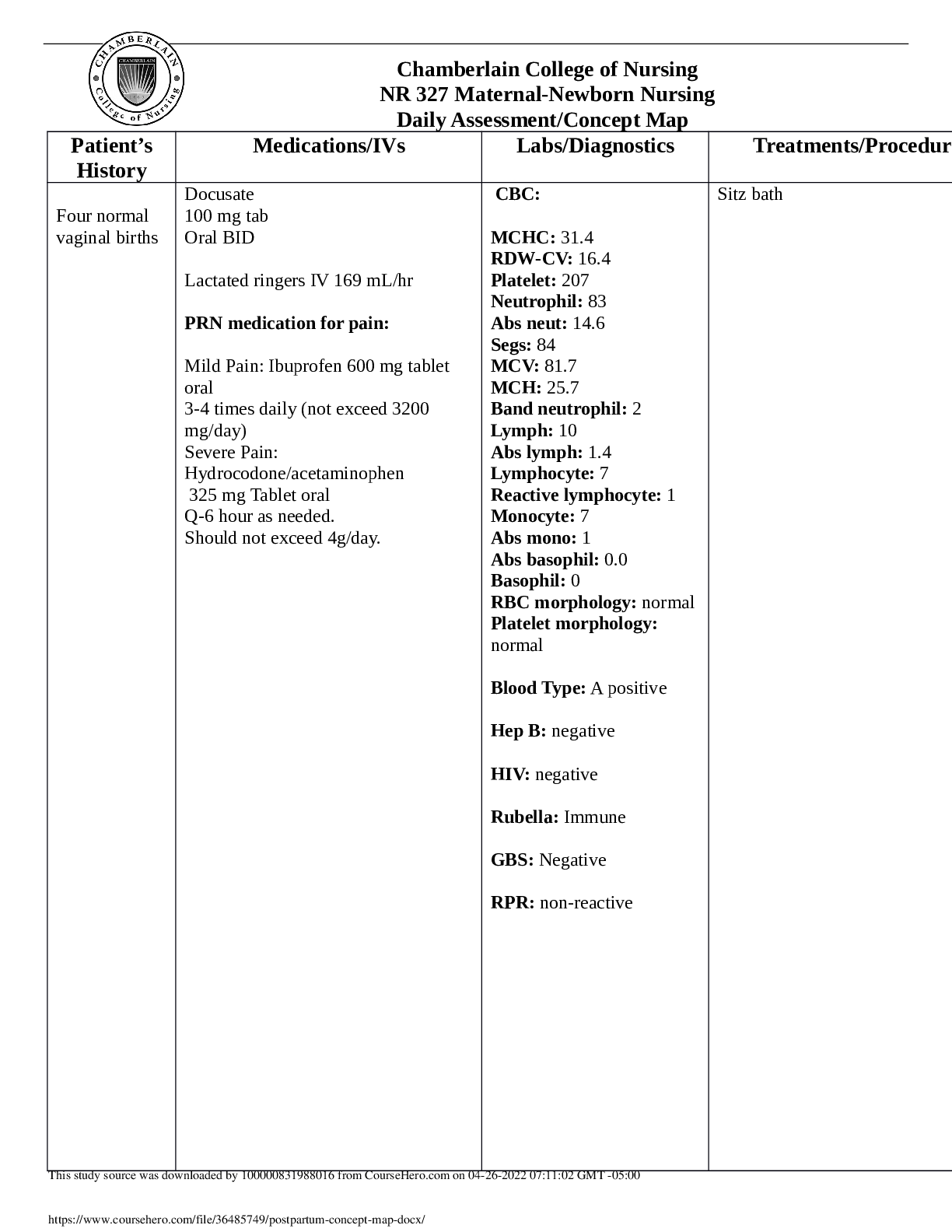
* Test 2 * Final OB Exam 2 Study Guide 1. Normal postpartum changes, Assessments & Discharge Teaching https://www.youtube.com/watch?v=PJvK7Xbs0DQ Immediately after delivery the fundus is right at... the umbilicus, feels like fist Every PP day fundus drops 1cm Day 9-10: cannot feel fundus at all - Should be firm - If it’s boggy -> at risk for PP hemorrhage Massage the fundus immediately & reassess in 30 min If massage is not helping, give oxytocin Should be midline If boggy & deviated it means the bladder is full-> always massage, if not resolved ask pt to void & reevaluate Assess for clots The uterus on the average descends 1 centimeter per day. The first nursing action for a boggy uterus is to massage the fundus. Oxytocin is commonly used to control postpartum bleeding related to Postpartum period: 6 week period after childbirth The Reproductive System Uterus: The uterus needs to be contracted to prevent hemorrhaging Women who are in a healthy state and had a low risk pregnancy have a lower risk for complications Women are at risk for infection and hemorrhage Involution: uterus returns to pre-pregnant size, shape and location Afterpains: moderate to severe cramp-like pains RT/ uterus contracting &/or the release of oxytocin from the infant suckling Nursing Actions: Assess the uterus for location, position and tone of the fundus (inform, explain, and instruct pt to void) ○ An over distended bladder may cause uterine atony (decreased uterine muscle tone that may lead to postpartum hemorrhage)/displacement, therefore voiding gives you an accurate assessment Rationale: An over distended bladder can result in uterine displacement and atony. Encouraging the woman to void prior to uterine assessment will allow for an accurate assessment of uterine placement and tone. ○ Hemorrhage: Primary (early) first 24 hours after birth & Secondary (late) 6-14 days following birth. ○ Place pt in supine position Locate the fundus with the other hand using gentle downward pressure Determine the tone of the fundus: ○ Firm = contracted ○ Soft = boggy: indicates that the uterus is not contracting and places the woman at risk for excessive blood loss. INTERVENTION: massage the uterus to stimulate contraction/ give Oxytocin to stimulate contraction Measure the distance between the fundus and umbilicus with your fingers (each finger breadth is 1 cm) Determine the position of the uterus Rationale: A uterus that is shifted to the side may indicate a distended bladder. A distended bladder interferes with uterine contractibility, which places the woman at risk for uterine atony and increases her risk of hemorrhage. Expected assessment finding after birth of the placenta: After birth: uterine fundus is midline between the umbilicus and symphysis pubis and is firm at midline Within 12 hours: level of the umbilicus or 1cm above the umbilicus/ midline 24hrs after: 1cm below the umbilicus / firm and midline Note: the uterus descends 1cm per day/ by day10 it descends into the pelvis and is not palpable ★ Boggy Uterus: a sign that the uterus is not contracting ○ At risk of excessive blood loss/hemorrhage is ^ ○ Immediate action is to massage the fundus with the palm of your hand in a circular motion until firm and reevaluate within 30 min ○ If the uterus does not respond to massage, follow the standing order for oxytocin and notify the HCP uterine atony. Oxytocin, the hormone of labor, also stimulates the uterus to contract in the postpartum period in order to reduce blood loss at the placental site. And oxytocin is the same hormone that regulates the milk ejection reflex. Whenever a mother breastfeeds, therefore, oxytocin stimulates her uterus to contract. In essence, therefore, breastfeeding naturally benefits the mother by contracting the uterus and preventing excessive bleeding. The uterine fundus is palpated by placing one hand on the base of the uterus immediately above the symphysis pubis and the other hand at the level of the umbilicus. The nurse presses inward and downward with the hand positioned on the umbilicus until the fundus is located. It should feel like a firm, globular mass located at or slightly above the umbilicus during the first hour after birth. The uterus should never be palpated without supporting the lower uterine segment. Failure to do so may result in uterine inversion and hemorrhage. Lochia is assessed as scant, light, moderate, or heavy: Scant is less than 1 inch on the pad. Light is less than 4 inches on the pad. Moderate is less than 6 inches on the pad. Heavy is when the pad is saturated within 1 hour Excessive lochia: saturating more than one pad in an hour indicates possible postpartum hemorrhage Endometrium: the mucous membrane that lines the uterus ● Lochia: bloody discharge from the uterus that contains sloughed off necrotic tissue ● Primary complication is Metritis: infection of the endometrial tissue Metritis: pg. 364. Early ambulation, 3,000mL/day fluid intake, high vitamin C and ^ protein, proper hand washing techniques, proper pericare (wipe front to back) Primary risk factor: cesarean birth Assess for clots: It is common for lochia to contain small clots: due to the pooling of lochia in the lower uterine segment/ note in pt chart LARGE CLOTS: should be weighed and finding reported to physician or midwife (Large clots can interfere with uterine contractions) Ex. 10grams = 10mL of blood loss Excessive bleeding: Note: Continued heavy bleeding with good fundal tone may indicate the presence of a genitourinary tract laceration or hematoma of the vulva or vagina LOCHIA ★ Lochia Rubra (1-3 days) ○ Moderate to scant amount ○ ^ Flow with standing/breastfeeding ○ Bloody with Small Clots Normal ○ Bright red ★ Lochia Serosa (4-10 days) ○ Pinkish to Brownish ○ Scant ○ ^ During physical activity ★ Lochia Alba (Day 10) ○ Yellow to White ○ Scant ★ COMPLICATIONS ○ Infection (prevent infection by changing the peripad) ■ Foul Odor BUBBLEHE (POSTPARTUM ASSESSMENT) B- Breasts U- Uterus B- Bladder B- Bowels and rectum L- Lochia E- Extremities H- Homan’s sign (dorsiflex foot) dx of thrombosis in the deep vein/ assess for pain (extended legs, flexed knees followed by dorsiflexion of the foot) E- Emotional status Homans' sign is often used in the assessment for deep venous thrombosis (DVT) in the leg. To assess for Homans' sign, the patient's legs should be extended and relaxed with the knees flexed. The examiner grasps the foot and sharply dorsiflexes it. No pain or discomfort should be present. The other leg is assessed in the same manner. If calf pain is elicited, a positive Homans' sign is present. The pain occurs from inflammation of the blood vessel and is believed to be associated with the presence of a thrombosis. Pain on dorsiflexion is indicative of DVT in approximately 50% of patients. A negative Homans' sign does not rule out DVT. Postpartum women should be advised to perform three actions to prevent infections: (1) Change their peripads at each toileting because blood is an excellent medium for bacterial growth (2) Spray the perineum, from front to back, with clear water to cleanse the area (3) Wipe the perineum after toileting from front to back to prevent the rectal flora from contaminating sterile sites. ■ Placental fragments ○ Hemorrhage ■ Large clots ■ Heavy amounts ■ Saturated pad within 15 min or less ■ Bright Red Bleeding Vagina and Peritoneum: lay patient in side lying position, assess for any lacerations in buttocks as well as hemorrhoids REEDA ❏ Redness ❏ Edema (mild edema is expected) ❏ Ecchymosis (minor ecchymosis is expected) ❏ Discharge ❏ Approximation – of the edges of episiotomy & laceration (a bright red trickle of blood from the episiotomy site in the early postpartum period is a NORMAL finding) Mild to moderate pain is expected > Interventions: ● Encourage ice packs for first 24 hours: vasoconstriction/ reduce edema ● Warm packs and sitz baths after 24 hours: promote circulation, healing and comfort ● Change pads frequently, wash hands, rinse perineum after elimination reduce risk of infection (wear pad snuggly to prevent rubbing) ● Encourage woman to lie on her side to decrease pressure ● Administer analgesia: Ibuprofen for pain and discomfort ● Tighten gluteal muscle as sitting down/ relax after sitting ● Clean the perineal area from front to back (urethra to anus) ● Sparingly use antiseptic topical agent / cream or spray Breasts: ● Primary Breast Engorgement: due to an increase in the vascular & lymphatic systems -precedes after the initiation of production of milk (Woman may feel a throbbing pain in the breast) ○ Occurs 2-3 days PP/ Subsides within 24-48 hours ○ S/S: ■ Breast become: ● Larger ● Firm ● Warm ● Tender ● Throbbing pain Primary engorgement subsides within 24-48 hours The best way to prevent engorgement is to breastfeed the baby every 2-3 hours ● Subsequent Breast Engorgement: RT/ distention of the milk glands > should be relieved with baby suckling ○ Complication = MASTITIS (infection of the breast: may be due to bacterial entry through cracks in the nipples, and is associated with milk stasis, stress and fatigue/ IMPROPER INFANT LATCH) pg316&365 ○ Typically occurs 3-4 weeks post birth ■ Fever, Chills & Flu-like symptoms ■ Unilateral breast pain ■ Malaise ■ Redness, Tenderness in infected area Which of the following nursing actions are important in the care of a postpartum woman who is at risk for orthostatic hypotension? (Select all that apply.) a. Have patient remain in bed for the first 4 hours post birth. b. Instruct patient to slowly rise to a standing position. c. Open an ammonia ampule and have the patient smell the ammonia prior to getting out of bed. d. Explain to the patient the cause and incidence of orthostatic hypotension. Normal Platelet count: 150,000-400,000/mm3 Colostrum: A clear, yellowish fluid precedes (before) milk production. It is higher in protein and lower in carbohydrates than breast milk. It contains immunoglobulins G and A that provide protection for the newborn during the early weeks of life. Assess for: engorgement, signs of irritation and nipple tissue breakdown & assess for plugged milk ducts (pg316) Women may have an elevated temperature: ● TX: Breastfeeding women vs. non-breastfeeding women ○ Frequent feedings preventing milk stasis & emptying of the breasts ○ Apply warm compresses to the breasts and massage them prior to breastfeeding ○ Pump the remaining milk after breastfeeding ○ Apply ice packs after breastfeeding ○ Take analgesics as breastfeeding so it does not affect the baby ○ Wear a supportive bra ■ If NOT Breastfeeding include all but DO NOT pump or stimulate breasts > COLD measures (ice packs to breasts) The Cardiovascular System CV System: Hypervolemic during L&D 200mL-500mL / 500cc of blood loss during delivery is normal Cardiac output returns to pre-pregnant levels within 48hrs. ORTHOSTATIC HYPOTENSION (due to decreased vascular resistance in the pelvis due to a sudden drop in blood pressure when the woman stands) is common = FALL RISK / assisted ambulation Use and ammonia ampule if the woman faints ELEVATED PULSE MAY INDICATE EXCESSIVE BLOOD LOSS, FEVER, OR INFECTION. Women are at risk for THROMBOSIS: RT/ increase of circulating clot factors (coagulation factors and fibrin levels ^)/ clotting factors return to normal within 2 -3 post partum weeks COMPLICATION: Pul. Emboli / Thrombus formation Check CBC, hemoglobin and hematocrit levels, VS, pulses, BP Assess extremities for venous thrombosis due to increased coagulability (asses for warmth, calf tenderness, edema, muscle pain @ each shift) -Encourage early ambulation - Apply antiembolism hose Assess pulse and blood pressure: Every 15 in for the first hour Every 30 min for the second hour Every 4hours for the next 22 hours Every shift after the first 24hours Rationale: Hemodynamic changes occur during labor and delivery and in the postpartum period. There are rapid changes in blood volume and cardiac output. Assessment of pulse and blood pressure is important in identification of potential complications such as excessive blood loss, orthostatic hypotension, infection, and gestational hypertension/preeclampsia. An elevated pulse may indicate excessive blood loss, fever, or infection. A client with critically low platelet count can indicate disseminated intravascular coagulation (DIC) 24. A woman who gave birth 2 hours ago has a temperature of 37.9°C (100.2F). Select all of the immediate nursing actions. a. Have patient drink two glasses of fluid over the next hour. b. Explain to the patient that she needs to rest and assist her into a comfortable position. c. Medicate the patient with 500 mg of acetaminophen as per orders. d. Call the patient’s physician or midwife to report the elevated temperature. A mild temperature elevation within a few hours of birth can be related to dehydration and exhaustion. POSTPARTUM CHILLS (due to vascular instability): assess temp, related to blood loss, LEUKOCYTOSIS: WBC may increase to 25,000/mm (as a result of stress of L&D) within a few hours of birth and return to normal levels within 7 days without the presence of infection ○ Due to decrease in ESTROGEN ○ Normal, losing the extra fluid ○ Normal occurrence Intervention: provide warm blankets and fluids A 100.4 F (38C) temp in 2 readings 6hrs apart = infection, call HCP / hydrate : (AFTER 24HRS POST BIRTH) May be due to DEHYDRATION in the early postpartum period (DURING THE FIRST 24 hours AFTER delivery); encourage the intake of water and fluid (In the early postpartum period up to 24hrs, the most common reason for temp elevation is dehydration. Respiratory System: normal RR postpartum is 16-24 breaths/min ❏ Diaphragm returns to normal after postpartum period ❏ Mother is able to breathe a lot easier ❏ Assess breath sounds: If given Tocolytics (meds stop contractions: Magnesium sulfate or Terbutaline), Oxytocin, Large amounts of intravenous fluids, women on bed rest, have an infection are at risk for: ❏ Risk factor: Pulmonary Edema ❏ Auscultate lung sounds Immune System: Temperature: A temperature greater than 100.4°F (38°C) after the first 24 hours on two occasions may be indicative of postpartum infection and requires further evaluation. Immunizations: Pertussis: Whooping cough Women may receive vaccinations such as: Rubella (for those who are rubella non-immune (should be immunized before discharge/ THE WOMAN SHOULD NOT BECOME PREGNANT 4 WEEKS AFTER THE VACINATION-> SEVERE BIRTH DEFECTS CAN DEVELOP), Tdap, Hep B, Varicella, and Influenza Because the vaccine is Teratogenic, the best time to administer it is when the woman is not pregnant/ after labor/ Encourage vaccinations If mother is Rh - give RhoGAM prophylactically incase fetus is Rh+ at 28 wks gestation Postpartum: test baby, if Rh+2nd shot of RhoGAM is given Rh-negative women who gave birth to an Rh-positive baby are screened for anti –Rh-antibodies (Coombs’ test), a second injection of Rho immune globulin is given to the woman if she is Coombs’ negative Dose: 300ug IM Urinary System: [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 23, 2021
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Sep 23, 2021
Downloads
0
Views
89


.png)

NSG110 AMERICANS RATE NURSES HIGHEST ON HONESTY, ETHICAL STANDARDS.png)