*NURSING > Summary > PN3 Exam 3 Study Guide|PN 3 Exam 3 Study Guide (2019/20) A+ guide; Rasmussen College, Minneapolis (All)
PN3 Exam 3 Study Guide|PN 3 Exam 3 Study Guide (2019/20) A+ guide; Rasmussen College, Minneapolis
Document Content and Description Below
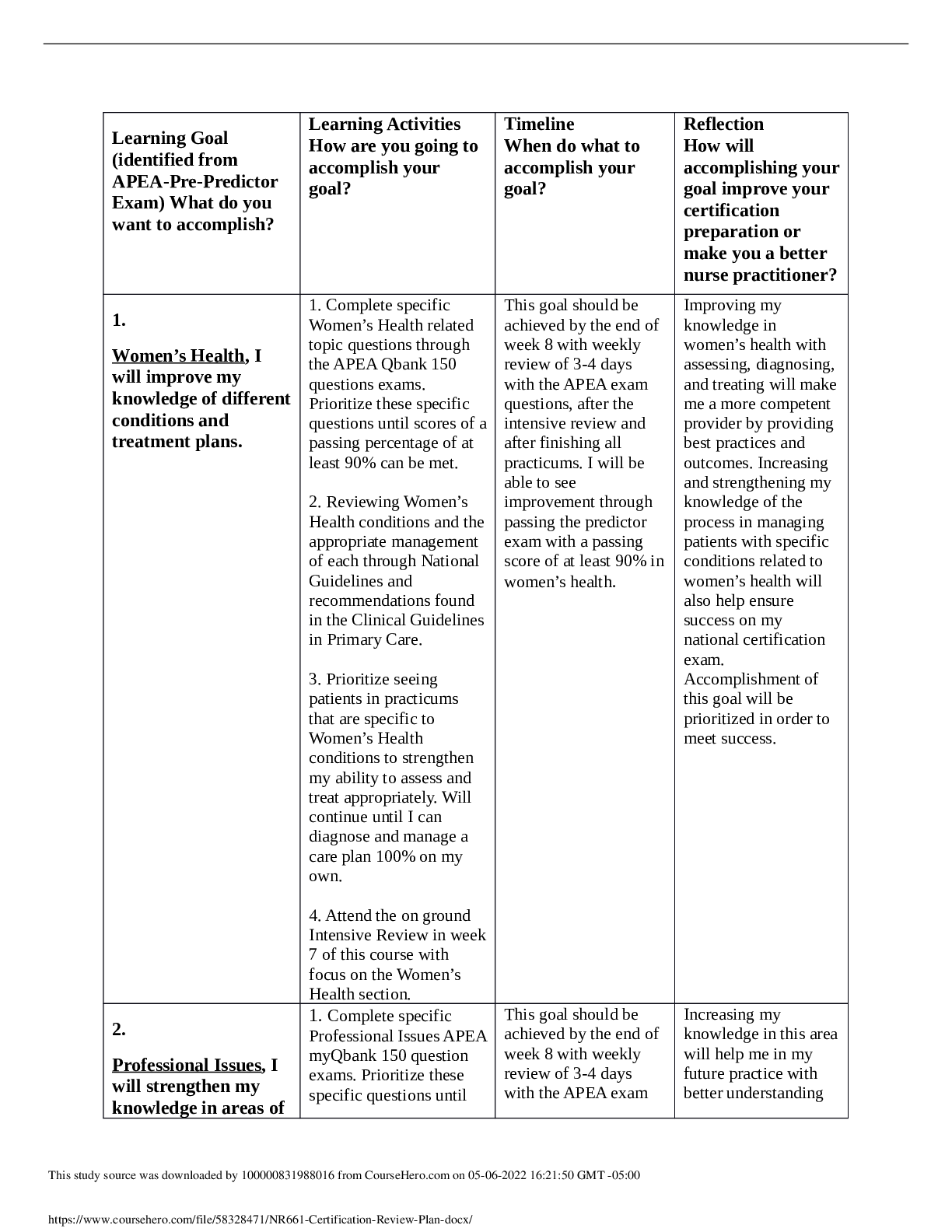
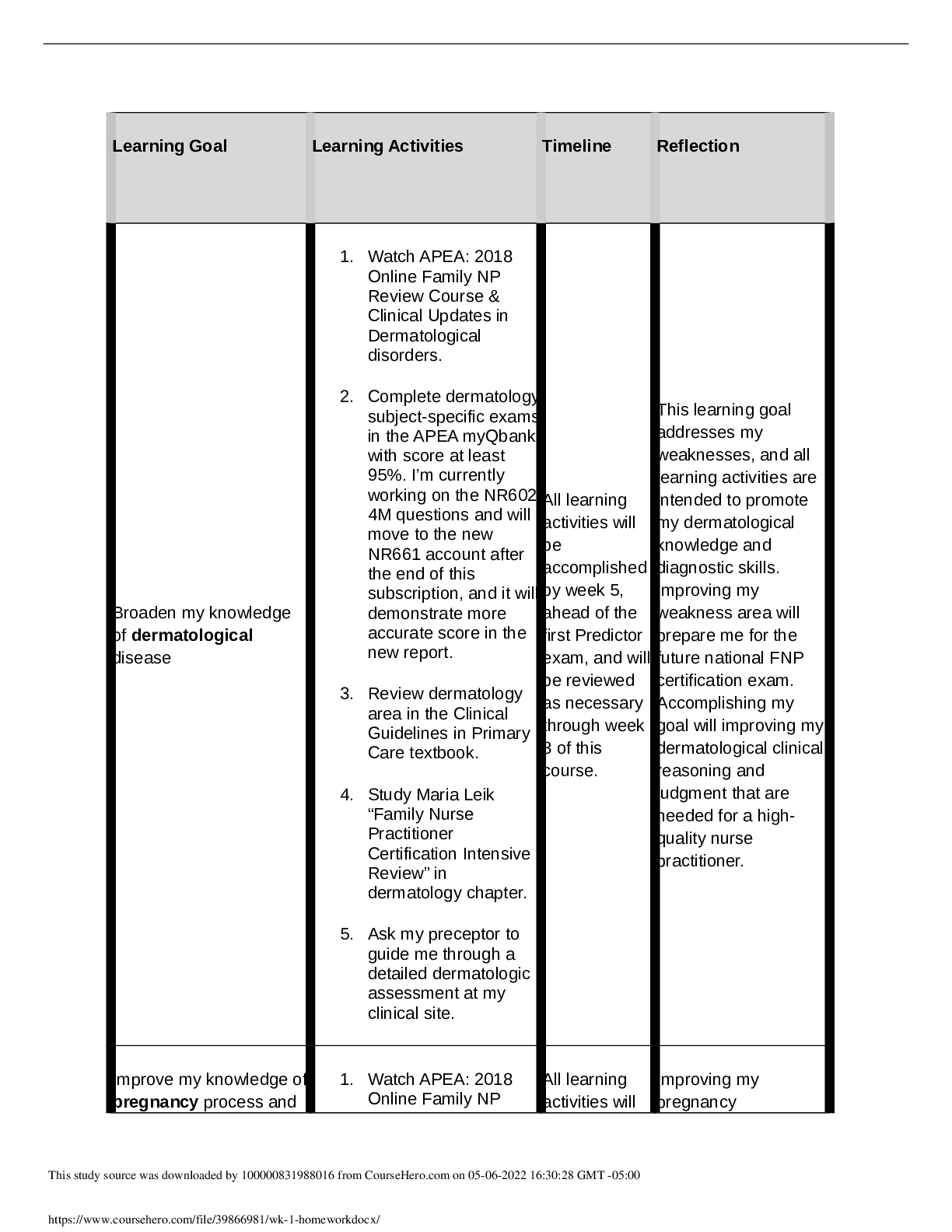
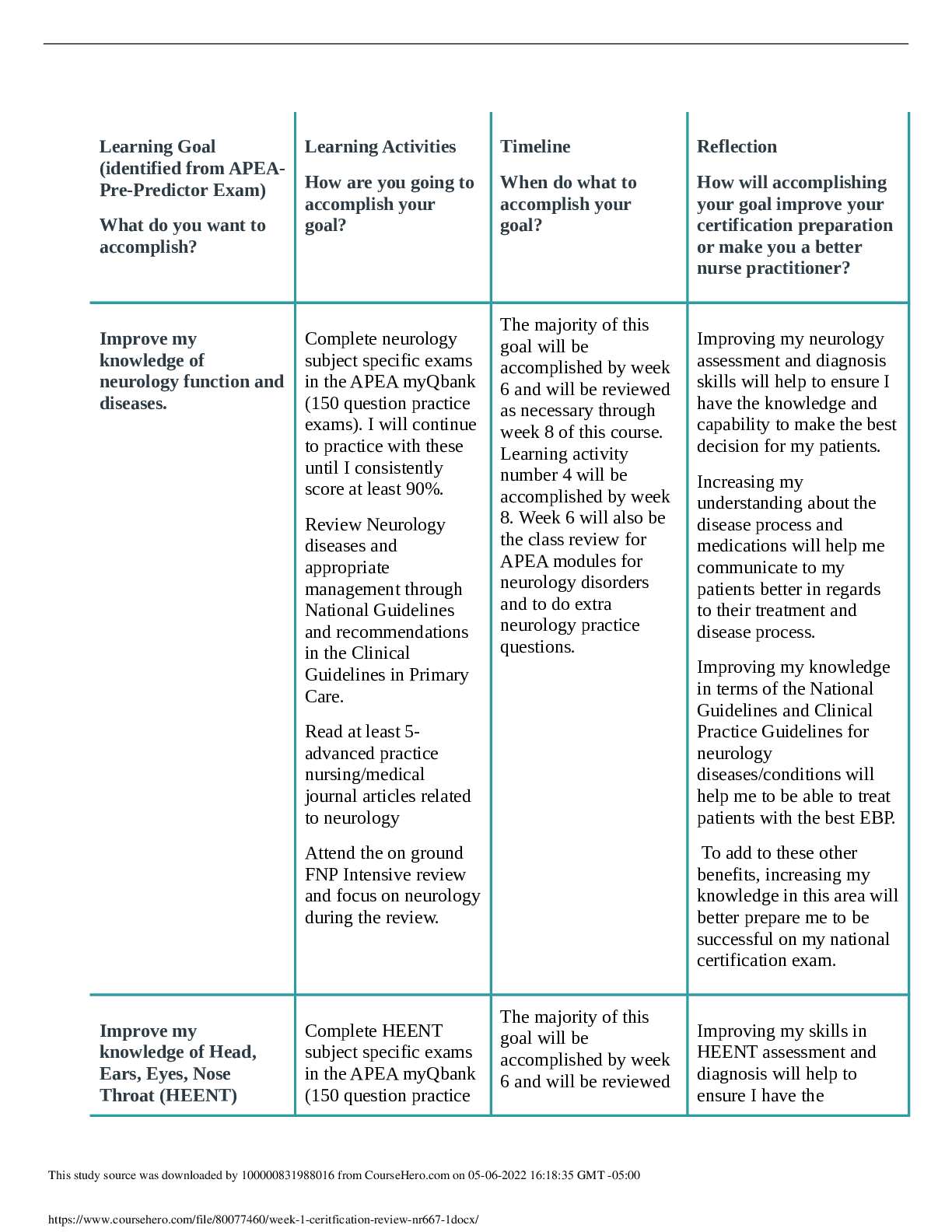
Exam 3 Study Guide Shock Syndromes: Shock is a systemic condition where there is an imbalance between the oxygen supply to the tissues/organs and the oxygen needs of those tissues/organs. There are... different types of shock. Any situation that decreases vascular volume, blood pressure, or cardiac function can lead to shock. Shock can be divided according to the cause. There are three main types of shock. Distributive shock is further divided into another three categories. Cardiogenic: pump (heart) failure Hypovolemic: lack of circulating volume in the vascular space Distributive: alteration in the vascular bed size ● Neurogenic: impaired sympathetic nervous system ● Anaphylactic: hypersensitivity response due to antigen-antibody reaction ● Septic: Due to systemic infection Complications of each type ● Multiple Organ Dysfunction Syndrome (MODS) ● Disseminated Intravascular Coagulation (DIC) ● Acute respiratory Distress Syndrome (ARDS) Treatment goals of each type ● Identify and treat the underlying cause ● Deliver oxygen to the tissues ● Maintain Circulation ● Monitor for complications ● Provide comfort and emotional support 4 stages of shock: ● Initial: decreased CO and impaired tissue perfusion ● Compensatory: activation of sympathetic nervous system (SNS) ● Progressive: every system in the body is affected and MOD happens ● Refractory: body will no longer respond to therapy SIRS is a clinical response to a nonspecific insult. Regardless of the etiology of the insult, the body responses are similar. If the process cannot be contained by the innate counter-inflammatory response, there is an increased activation of the inflammatory cells, including release of neutrophils, macrophages, and lymphocytes; and additional damage to the vascular epithelium, deterioration in distribution of nutrients to the organs, and subsequent complication of multiple organ dysfunction syndrome (MODS) or multiple organ failure (MOF). Conditions commonly associated with SIRS include infection, pancreatitis, ischemia, trauma, hemorrhagic shock, aspiration of gastric contents, massive transfusions, and host defense deficiencies It is essential that you assess all patients at risk for SIRS, especially for the cardinal signs of the body’s inflammatory response. At least two or more of the following findings will be present in SIRS: ● Change in temperature either higher than 38° C (100.4° F) or lower than 36° C (96.8° F) ● Pulse greater than 90 beats per minute ● Respiratory rate greater than 20 breaths per minute or a partial pressure of carbon dioxide (PC02) less than 32 mm Hg ● White blood cell (WBC) count higher than 12 × 103/mm3, or with more than 10% band cells BOX 65-3: ASSESSMENT AND DIAGNOSIS OF SHOCK Common clinical manifestations of the shock syndrome will vary according to the underlying cause, the stage of shock, and the individual person’s response to shock. The exact course of events can be variable. Each person must be assessed individually prior to any intervention: ● Regardless of the type of shock, it leads to a systolic blood pressure (SBP) of less than 90 mm Hg and the narrowing of pulse pressure that is inadequate to meet the tissue needs. (SBP may be elevated initially.) ● Early shock symptoms are subtle, requiring close surveillance to avoid overlooking their presence. ● All persons in shock are at risk of deterioration in status. Prompt intervention is required. ● Nurses must have a clear understanding of the pathophysiology of the different etiologies of shock. ● In all instances of shock following a trauma incident, consider hypovolemia or hemorrhage unless proven otherwise. ● Shock is a frightening experience for the patient and family. Effective psychological support is essential. Symptoms include: ● Hypothermia ● Tachycardia or bradycardia ● Rapid thready pulse, slow capillary refill, or collapse of superficial veins in extremities ● Altered mental status—dissociation from normal thought processes, detached, a feeling of numbness, and impaired sensory- emotional response. Loss of consciousness, restlessness, anxiety, irritability, and weakness may be present. ● Clinical findings correlated with organs compromised by inadequate oxygen supply and the phases of the shock syndrome. Examples: ○ a. Skin: cold, clammy, cyanotic, poor capillary refill, or warm dry skin due to pooling of blood in extremities. Cyanosis (circumoral, earlobes, finger tips, or toes). ○ b. Kidneys: decreased urine output; anuria, or oliguria. ○ c. Lungs: dyspnea, crackles, or wheezes. ○ d. GI system: thirst, dry mucous membranes; nausea and vomiting; or decreased bowel sounds. Acute Coronary Syndrome: Unstable Angina (VS stable angina) ● Unstable angina: condition in which your heart doesn’t get enough blood flow and oxygen--may lead to a heart attack. DO NOT KNOW THE TRIGGERS ● Stable angina: chest pain or discomfort that most often occurs with activity or emotional stress. KNOW WHAT POTENTIAL TRIGGERS ARE. Usually a chronic condition that causes stable angina. Non ST segment elevation myocardial infarction (NSTEMI)--> Indicates a partial thickness injury to the heart muscle. Less severe than a STEMI. Partial occlusion of a major coronary artery ST segment elevation myocardial infarction (STEMI)--> indicates a full thickness injury of the heart muscle. Assessment of chest pain: Including: Special populations assessment: elderly, women Onset: When did the pain begin? Location: Where is the pain? Duration: How long does the pain last? Characteristics:Describe the pain? Crushing, stabbing, ingestion like, dull, ache for example Associating Factors: Other symptoms associated with the pain such as nausea and/or vomiting, weakness, fatigue, breathlessness, syncope, cold and clammy? Relieving Factors/Radiation: Does the pain radiate such as down the arm, up into the neck for example? Relieving factors: pain stops when activity ceases, relieved by sitting forward or resting? Treatment/Temporal factors: Use of GTN, pain was relieved by rest or decrease in physical activity. Pain non comparable to previous ischemic chest pain Severity (Intensity): A numerical scale (1 no pain- 10 worse pain experienced ) is used to gauge pain severity Older adults: Typical chest pain→ Usually intense and unremitting for 30-60 minutes. Is retrosternal and often radiates up to the neck, shoulder, and jaws, and down to the left arm. The chest pain is usually described as a pressure sensation that can be perceived as squeezing, aching, burning, or even sharp. Anxiety, lightheadedness, cough, nausea, profuse sweating, shortness of breath, wheezing, rapid or irregular heart rate, fullness/indigestion/choking feeling Women may or may not experience chest pain but may experience any of the symptoms above. Treatments/Surgical Procedures ● Meds: Anticoagulatns, antiplatelets, ACE inhibitors, beta blockers, Calcium Channel Blocker, Statins, diuretics, vasodilators, pain relievers (morphine), Nitroglycerin ● Surgeries: coronary angioplasty and stenting, coronary artery bypass surgery Patient Education for Anginal Episodes ● Stop activity, sit or lie down. ● Place one nitroglycerin tablet under the tongue and allow to dissolve. (Do not chew or swallow.) ● Tablet will cause a tingling sensation, heart pounding, flushing, and headache. ● Stay in resting position for 15 to 20 minutes and get up slowly after taking nitroglycerin to prevent fainting from postural hypotension. ● If angina is not relieved in five minutes, the dose may be repeated two times at five-minute intervals for a total of three doses. ● If angina is not relieved after two doses, seek immediate medical attention. ● Report angina that increases in frequency, lasts longer, limits previous level of activity, and occurs at rest. ● Carry tablets at all times in the original prescription container. Pharmacology→(what Jenni told us to remember) MONA (Morphine, Oxygen, Nitro, Ativan) Antiplatelet agents-Aspirin, Varopaxar Nitrates-relax smooth muscles Analgesics-Morphine-decreases sympathetic stress, in addition to providing some preload reduction. Beta-adrenergic blocker-Esmolol, Metoprolol-Beta blockers have antiarrhythmic and antihypertensive properties, as well as the ability to reduce ischemia. They minimize the imbalance between myocardial supply and demand by reducing afterload and wall stress. Glycoprotein IIB/IIIA inhibitors-Glycoprotein IIb/IIIa receptor antagonists include abciximab, eptifibatide, and tirofiban. Glycoprotein IIb/IIIa antagonists prevent the binding of fibrinogen, thereby blocking platelet aggregation. Anticoagulants-Heparin augments the activity of antithrombin III and prevents the conversion of fibrinogen to fibrin. It does not actively lyse but is able to inhibit further thrombogenesis. This agent prevents recurrence of a clot after spontaneous fibrinolysis. Low molecular weight heparins-Lovenox Adenosine diphosphate receptor antagonists-Thienopyridine adenosine 5'-diphosphate (ADP) antagonists approved for antiplatelet activity in the United States include clopidogrel (Plavix), ticlopidine, prasugrel, and ticagrelor. Modifiable Risk factors→ The major modifiable risk factors are hyperlipidemia, hypertension (blood pressure greater than 140/90 mm Hg), cigarette smoking, diabetes mellitus, obesity, and sedentary lifestyle. In addition, the remaining modifiable risk factors include low daily fruit and vegetable intake, alcohol consumption, and psychosocial index Cholesterol: purpose of each type→ Total cholesterol–a measure of the total amount of cholesterol in your blood, including low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol. LDL (bad) cholesterol–the main source of cholesterol buildup and blockage in the arteries HDL (good) cholesterol–HDL helps remove cholesterol from your arteries Triglycerides–another form of fat in your blood that can raise your risk for heart disease Total Cholesterol Level Less than 200mg/dL Desirable 200-239 mg/dL Borderline high 240mg/dL and above High LDL (Bad) Cholesterol Level Less than 100mg/dL Optimal 100-129mg/dL Near optimal/above optimal 130-159 mg/dL Borderline high 160-189 mg/dL High 190 mg/dL and above Very High HDL (Good) Cholesterol Level Less than 40 mg/dL A major risk factor for heart disease 40—59 mg/dL The higher, the better 60 mg/dL and higher Considered protective against heart disease What Affects Cholesterol Levels: Diet. Saturated fat and cholesterol in the food you eat make your blood cholesterol level rise. Saturated fat is the main problem, but cholesterol in foods also matters. Reducing the amount of saturated fat and cholesterol in your diet helps lower your blood cholesterol level. Weight. Being overweight is a risk factor for heart disease. It also tends to increase your cholesterol. Losing weight can help lower your LDL and total cholesterol levels, as well as raise your HDL and lower your triglyceride levels. Physical Activity. Not being physically active is a risk factor for heart disease. Regular physical activity can help lower LDL (bad) cholesterol and raise HDL (good) cholesterol levels. It also helps you lose weight. You should aim to be physically active for 30 minutes on most, if not all, days. Things outside of your control that also can affect cholesterol levels include: Age and Gender. As women and men get older, their cholesterol levels rise. Before the age of menopause, women have lower total cholesterol levels than men of the same age. After the age of menopause, women's LDL levels tend to rise. Heredity. Your genes partly determine how much cholesterol your body makes. High blood cholesterol can run in families. HTN: values in each category→ TABLE 24-2: Blood Pressure Classification BP CLASSIFICATION SBP mm Hg DBP mm Hg Normal Less than or equal to 120 or less than or equal to 80 Prehypertension 120–139 or 80–90 Stage I hypertension 140–159 or 90–99 Stage II hypertension Less than or equal to 160 or less than or equal to 100 Diet: including specific food examples→ TLC diet: Total fat 25–30%, saturated fats to less than or equal to 7%, complex carbohydrates 50–60%, protein 15% of total daily calories, total cholesterol less than or equal to 200 mg/day, fiber 25 g/day Steam, bake, broil, grill, or stir fry foods Avoid high fat foods such as meat, avocados, olives, nuts, butter, salad dressing, organ meats and shrimp, egg yolks, palm and coconut oils, high fat dairy products, fried foods Choose fresh fruits and vegetables, egg substitutes or egg whites, lean meats, fish, vegetable oils, low fat dairy products Buy a heart-healthy cookbook Achieve and maintain a healthy weight After approval by the health care provider, exercise regularly Non-modifiable risk factors→ Primary causes of hyperlipidemia include dietary sources and genetic disorders. Secondary causes of hyperlipidemia are due to hormone imbalances, liver and kidney dysfunction, alcohol consumption, and certain drugs such [Show More]
Last updated: 1 year ago
Preview 1 out of 19 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 25, 2021
Number of pages
19
Written in
Additional information
This document has been written for:
Uploaded
Sep 25, 2021
Downloads
0
Views
105


.png)

NSG110 AMERICANS RATE NURSES HIGHEST ON HONESTY, ETHICAL STANDARDS.png)