*NURSING > STUDY GUIDE > NR 283 Exam 1 Study Guide Questions and Answers,100% CORRECT (All)
NR 283 Exam 1 Study Guide Questions and Answers,100% CORRECT
Document Content and Description Below
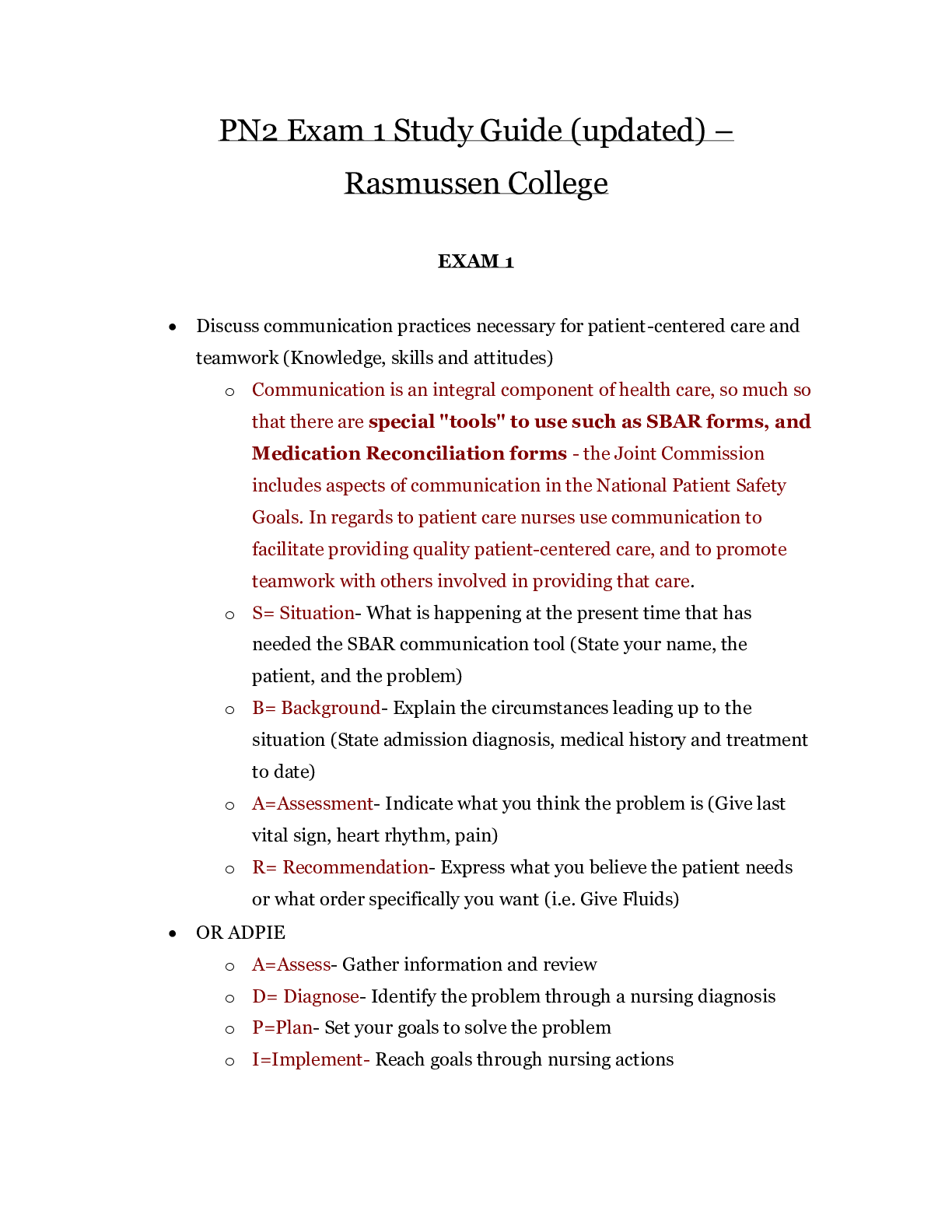
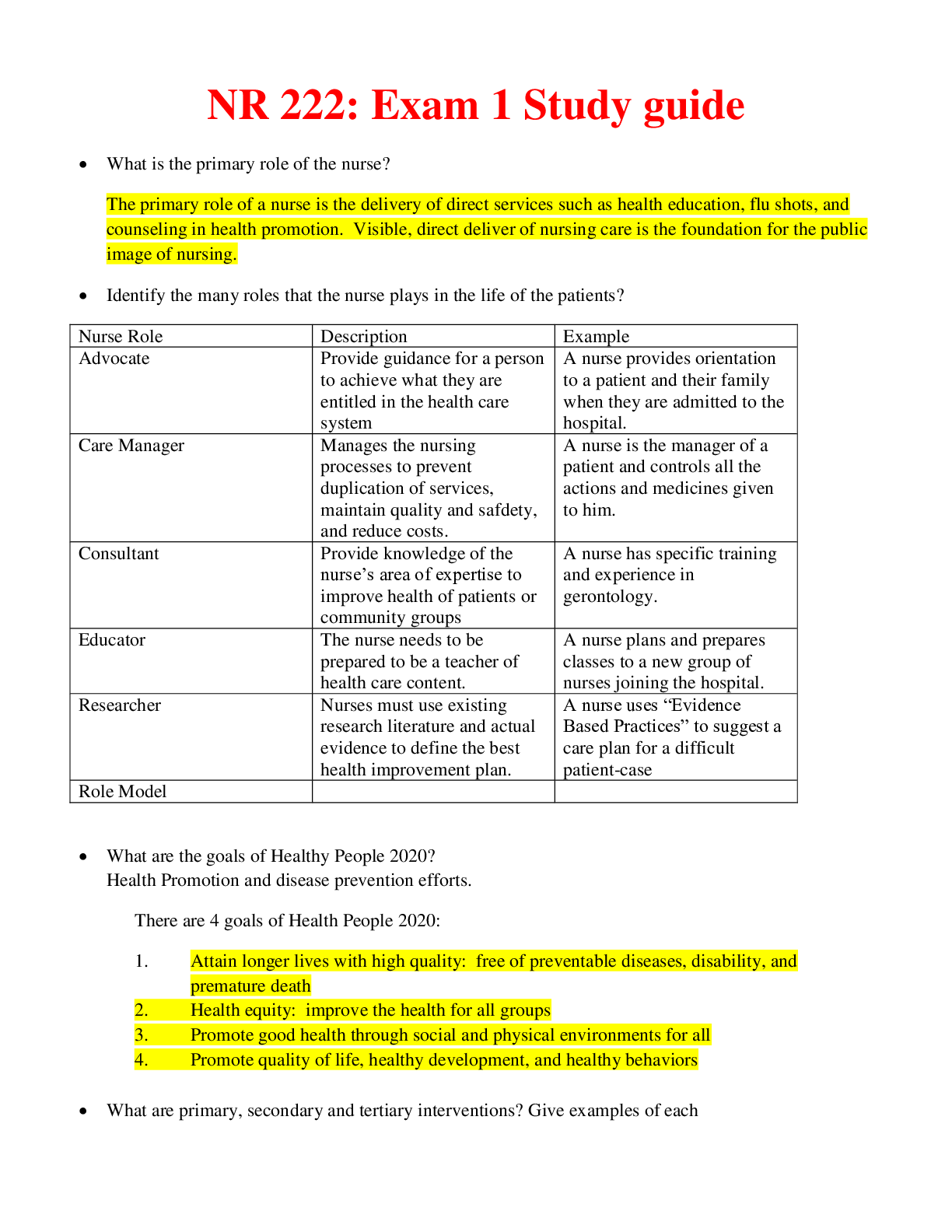
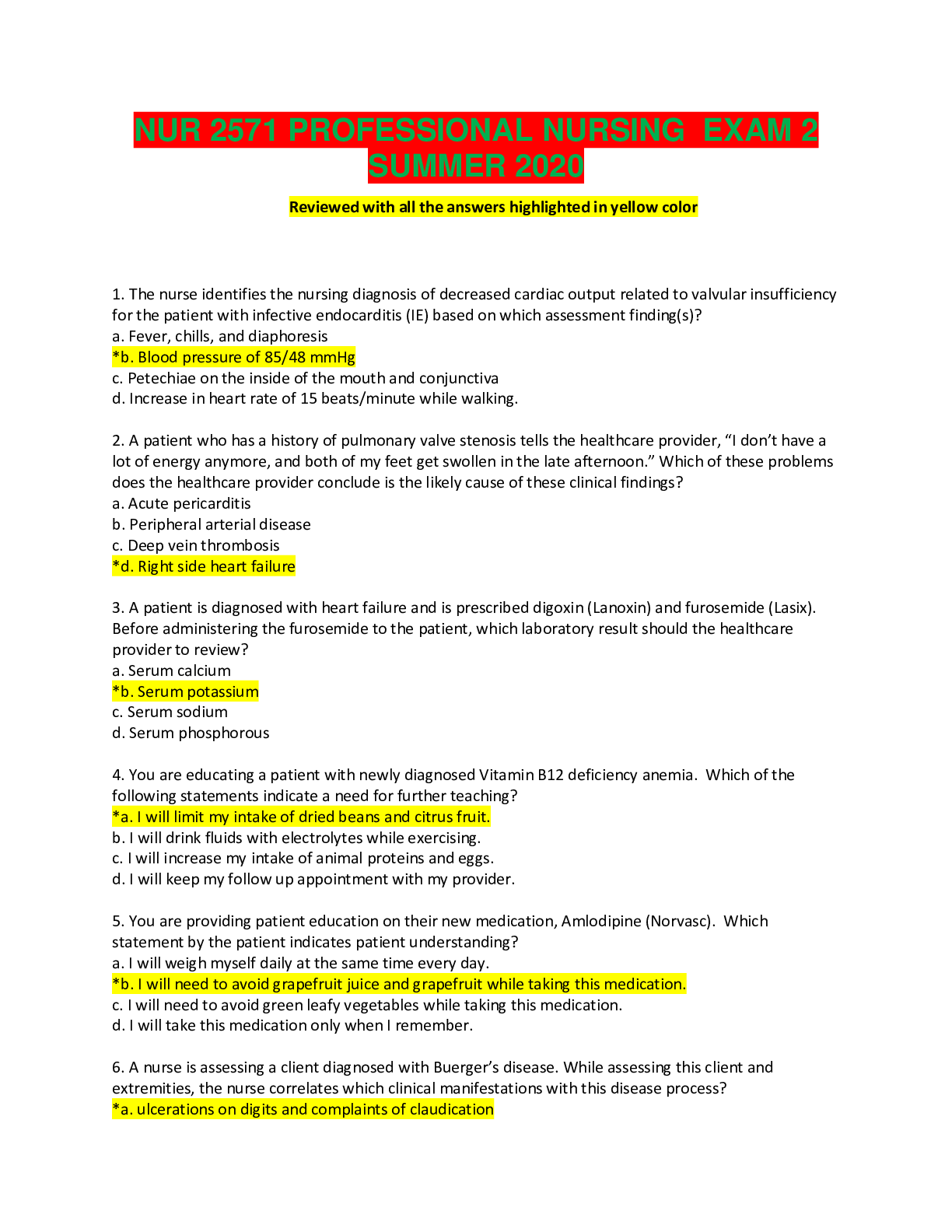
NR283 Exam 1 Study Guide Questions and Answers (Chapters 1, 2, 5, 6, 7, 20, & 21) *Make sure that you understand all of the terms you are studying, if you don’t know what a term means, look it u... p before you continue studying. Take your thinking a step further by asking yourself “why” as you are reviewing material. This will lead to understanding of the material versus memorization which will better help you answer questions. Remember, this study guide does not mirror the exam and you are responsible for all course content; ensure that you have an understanding of concepts. That being said, if you complete and understand this study guide, you will be well prepared for the next exam. *Ensure that you understand all highlighted terms in each chapter * Answer the question and supplemental questions included with the original question Chapter 1: Introduction to Pathophysiology 1. What are the 7 steps of health? -Don’t smoke, avoid 2nd hand smoke -Eat 5-10 servings of vegetables & Fruit daily. High fiber, lower-fat foods. Limit alcoholic drinks to 1 or 2 a day. -Be active -Protect yourself & family from the sun -Follow cancer screening guidelines -Visit doctor or dentist if any change in normal state of health -Follow health & safety instructions at home and work when using, storing and disposing of hazardous materials. 2. What is the definition of disease? Deviation from normal state or homeostasis: structure or function of any part, organ, system (or combination of these) or from a state of wellness. 3. Describe what homeostasis is: maintenance of stable internal environment of the body despite external changes. a. Which factors indicate how well the body is maintaining homeostasis? (3 listed) -Blood pressure -Body Temp -Fluid Balance 4. Describe the following & list examples: a. Primary Prevention: Prevention of disease or experiencing an injury in the first place (doctors, vaccines) Ex.) immunizations, screenings controlling potential hazards at home, education i. When is this implemented? Before disease is present b. Secondary Prevention: Baby aspirin-hypertension, frequent monitoring, modified work i. When is this implemented? After illness or risk factors have been diagnosed to prevent complications. To slow progress of disease, limit long-term disability and prevent re-injury. c. Tertiary Prevention: Pain management, support groups, rehab i. When is this implemented? Diagnosed after complication to prevent & preserve quality of life. Helping people manage complicated, long term health problems 5. What are the 3 major health professional organizations who conduct research, publish findings, track certain diseases and are responsible for signaling warning about predisposing conditions or current treatments? -United States Public Health Service -Centers for Disease Control and Prevention (CDC) -State & Local authorities *Findings are gathered by World Health Organization (WHO) 6. Describe each characteristic of disease: -Pathogenesis: development of the disease or events involved in tissue changes related to specific disease process -Onset: sudden and obvious or acute -insidious: gradual progression with vague or mild signs -acute: short-term illnesss developing quickly with marked signs (fever, severe pain) -Chronic: milder condition developing gradually. Persisting for a long time (rheumatoid arthritis) -Subclinical state: pathologic changes occur, no obvious manifestations show by patient -Latent stage: no clinical signs. Also referred to incubation period, time between exposure to microorganism and onset of signs or symptoms. Disease may be communicable or contagious. -Prodromal period: early development of disease when aware of a change in the body, but signs aren’t specific. Ex.) fatigue, headache. -Manifestations: clinical evidence or signs and symptoms. Ex.) redness, swelling. May also be systemic=general indicators of illness like a fever -Signs: objective or observed by someone other than affected individual. Ex.) fever, rash -Symptoms: subjective feelings felt and said by patient. Ex.) pain, lethargy etc. -Lesion: specific local change in a tissue . Ex.) blister or pimple -Syndrome: collection of signs and symptoms, affecting more than one organ and occur together due to certain condition -Diagnostic Tests -Remissions & exacerbations: course or progress of disease. -Precipitating factor: condition that triggers an acute episode. Ex.) seizure in individual with a seizure disorder. Predisposed factor: at higher risk for disease because of life style habits/genetics. Ex.) coronary artery disease b/c high cholesterol diet Sequelae: potential unwanted outcomes of primary condition. Ex.) paralysis following a stroke Convalescence or Rehab: period of recovery, returning to normal state 7. What is prophylaxis and why is it important? What are some examples of prophylactic measures in health care? Measures designed to preserve health and prevent the incidence or spread of disease. Provides information that benefit patients’ needs and allows them to make better decisions about their health. Ex.) Treatment for myocardial infarction for high risk patient= 1 baby aspirin daily. 8. Describe the difference between acute and chronic disease: Acute is the sudden onset of short term illness with marked signs such as fever, severe pain etc. Chronic is more mild gradually developing that persists for a long time. 9. Describe the difference between morbidity and mortality: Morbidity is the disease rates within a group such as stroke cause within a population. Mortality is the number of deaths resulting from a particular disease. 10. Describe each term of cellular adaptation and list examples: a. Atrophy: “shrink” decrease in size of cells=reduced tissue mass i. Ex: limb in cast for several weeks b. Hypertrophy: “grow in size” increase in size of cells=enlarged tissue mass i. Ex: exercise on skeletal muscle or weight lifting c. Hyperplasia: “grow in numbers” increased number of cells=enlarged tissue mass i. Ex: Uterine enlargement during pregnancy d. Metaplasia: “replace w/ diff. mature cell” mature cell type is replaced by diff mature cell type. i. Ex: In smokers lining of lungs (ciliated columnar epithelium) gets replaced with more resistant tissue (stratified squamous epithelium). Decreases defense for lungs. e. Dysplasia: “dysfunctional” cells vary in size and shape w/in a tissue i. Ex: Pap smear f. Anaplasia: “undifferentiated cells” un.diff. cells with variable nuclear and cell structures i. Ex: Characteristic of cancer, basis for grading aggressiveness of tumors g. Neoplasia: “new growth” new growth of a tumor, these are differentiated cells i. Ex: malignant or benign tumors 11. Describe each term related to cell damage and list examples: a. Apoptosis: Programmed cell death b. Ischemia/Hypoxia Ischemia: reduced blood flow to tissue or organ due to circulatory obstruction blocked artery, resp. impairment (chest pain) (Oxygen, nutrients, WBC/RBC) Hypoxia: reduced oxygen in the tissue. Interferes with ATP production. Sodium pump stops as well as other cell functions. i. What is the difference between ischemia and hypoxia? Ischemia reduced blood flow & hypoxia reduced oxygen c. Physical injury: related to heat or mechanical pressures. Impair blood supply to cells or metabolic processes. Ex.) Radiation damages cells by altering chem. Constituents, changing DNA, toxic materials inside cell 12. What is necrosis? When a group of cells die a. Describe each type of necrosis and give examples: i. Liquefaction necrosis: dead cells liquefy due to certain cell enzymes Ex.) brain issue dies, cavities, ulcers ii. Coagulative necrosis (scar tissue): cell proteins are altered or denatured, cell keeps form for a little bit after death. Ex.) Heart attack due to lack of oxygen causing cell death. iii. Fat necrosis: fatty tissue broke down into fatty acids due to infection or certain enzymes. Ex.) gangrene iv. Caseous necrosis: coagulation, with thick, yellowish cheesy substance forming. Ex.) TB (development of granuloma, small solid mass of macrophages&lymphocytes) 13. What is infarction? Area of dead cells remaining from lack of oxygen a. What happens to the tissue after it experiences infarction? It is replaced with scar tissue b. Is that tissue functional like the previous tissue that died off? No, b/c it is replaced by scar tissue. Scar tissue isn’t flexible. c. What is a common classic example of infarction? Heart attack 14. What is gangrene? Necrotic tissue invaded by bacteria a. Why is it so dangerous? Buildup of gases w/in a tissue reducing blood supply b. How is it treated? Surgically removed (amputation) sometimes antibiotics Chapter 2: Fluid Electrolyte and Acid-Base Imbalances 15. What is the difference between intracellular compartment (ICF) and extracellular compartment (ECF)? -ICF: fluid inside the cells. 40% in males 33% in females 40% in infants -ECF: fluid outside the cells. 20% in males 17% in females 30% in infants a. Where is the ECF found? -Intravascular Fluid (IVF) or blood -Interstitial fluid (ISF) or intercellular fluid “around” 15% in males 9% in females 25% in infants -Cerebrospinal Fluid (CSF) -Transcellular Fluids: In secretions of Pericardial cavity (heart), Synovial cavities (joints). Serves as lubrication. *60% of adults body weight is water *70% of infants body weight is water *Females-higher percentage of fatty tissue=lower water content than males 16. Where is the thirst mechanism controlled in the brain? In the Hypothalamus by the osmoreceptor cells that sense the internal environment (goes down w/ age) 17. Which hormone controls the amount of fluid leaving the body in urine? ADH (antidiuretic hormone) promotes reabsorption of water into the blood from the kidney tubules a. Where does the reabsorption of water take place? Kidney tubules into the blood 18. Describe the term, causes, and examples of the following: a. Edema: excessive amount of fluid in the interstitial compartment i. What are local effects (symptoms/clinical manifestations) of edema? -Swelling -Pitting edema: depression or “pit” on affected area when pressure is applied -Increased body weight -Functional Impairment: restricts movement, reduced vital capacity, impaired diastole -Impaired arterial circulation: ischemia leading to tissue break down. Blood isn’t moving & too much pressure in area -Dental Practice -Tearing of Skin ii. Why does edema cause pain? Puts pressure on surrounding nerves, headache in cerebral edema (brain swelling), stretching of capsule in organs (liver, kidney) iii. What is the consequences of edema causing arterial circulation impairment? ischemia leading to tissue break down. Blood isn’t moving & too much pressure in area b. Dehydration: insufficient body fluids from inadequate intake or excessive loss of fluids i. Which is hematocrit increased during dehydration?% of RBCs in a volume of blood. Higher proportion of RBCs compared with water in the blood. Due to the fluid imbalance by the protein shift ii. How does the body attempt to compensate for the fluid loss? -increase thirst -increase heart rate -constricting cutaneous blood vessels=pale & cold skin -producing less urine & concentrating urine -renal vasoconstriction & increased secretion of aldosterone and ADH c. Compare and contrast the clinical manifestations of edema (fluid volume overload) and dehydration (fluid volume deficit) [Table 2-3]: Edema: localized swelling, pale or red skin, weight gain, slow pulse, high BP, decreased hematocrit, decreased serum sodium, high urine volume. Dehydration: sunken eyes, thirst, weight loss, rapid, weak pulse, low BP, and orthostatic hypotension, fatigue, weakness, dizziness, increased body temp, increased hematocrit, increased electrolytes, low urine volume. 19. Describe each electrolytes function, causes for imbalance and clinical manifestations of hyper/hypo imbalance: a. Sodium: cation, ECF, Diffusion between vascular & interstitial fluids. Controlled by Sodium-potassium pump or active transport=high Na levels in ECF, low inside cell. Secreted in mucus & other secretions (urine, sweat, feces). Form of sodium chloride & sodium bicarbonate. Controlled by kidneys through action of Aldosterone. -Hyponatremia:” Decreased Sodium” Sodium concen. Below 3.8 to 5mmol per liter or 135-145 milliequivalent. Causes: Losses from excessive sweating, vomiting, diarrhea or excess of water in the ECF=dilution of sodium. -Use of certain diuretic (make you urinate a lot) drugs combined w/ low salt diet -Hormonal imbalances: insufficient aldosterone, adrenal insufficiency, excess ADH secretion -Early chronic renal failure Effects: Low Na levels: Impair nerve conduction=fluid imbalance in compartments=fatigue, muscle cramps, abdominal discomfort, nausea, vomiting -Decreased osmotic pressure in ECF=Fluid shift into cells leads to Hypovolemia & decreased BP -Cerebral edema: brain swelling Hypernatremia: Excessive Na level in blood an ECF “To much Sodium” more than 145mEq per liter Causes: Excess Na from ingestion of large amounts of Na w/out enough water intake or faster loss of water from the body than loss of Na. Imbalance in Na & water -Insufficient ADH (diabetes insipidus) = large vol. of dilute urine -Loss of thirst mechanism -Watery diarrhea -Prolonged periods of rapid respiration Effects: *fluid shift out of cells=increased osmotic press. Of interstitial/extracellular fluid -Weakness/agitation -Dry, rough mucous membranes -Increased BP -Decreased urine output b/c ADH is secreted manifestations can change depending on cause of problem/ If caused by fluid loss due to lack of ADH urine output is high b. Potassium: intracellular cation, serum levels are low 3.5-5mEq. Intracellular concen level are 160mEq. Ingested in foods, excreted primarily in urine under influence of ADH, insulin promotes movement of potassium into cells. Potassium levels influenced by acid- base balance in body. Acidosis tends to shift potassium ions out of the cells into the extracellular fluids (hydrogen ions diffuse from blood-interstitial fluid b/c of high H concen in the blood, K+ is sent out of cell, excessive K+ in ICF diffuse into the blood leading to hyperkalemia) Acidosis promotes H+ excretion by kidneys & retention of K+ in the body and alkalosis tends to move more potassium into the cells. abnormal levels of K cause changes in cardiac conduction can be life threatening Hypokalemia: “To low Potassium” serum level less than 3.5mEq/L Causes: Excessive losses due to diarrhea -Diuresis assoc. w/ some diuretic drug. Pts may have to increase K+ intake -Excessive aldosterone or glucocorticoids-retaining sodium & excreting potassium Effects: Cardiac dysrhythmias-prolonged repolarization lead to cardiac arrest -Interferes with neuromuscular function-muscles less responsive to stimuli -Paresthesias: “pins and needles” -Decreased digestive tract motility: decreased appetite & nausea -Shallow Respirations -Impaired renal function: failure to concentrate urine with increased urine output (polyuria=to much water in urine) Hyperkalemia: “To much Potassium” serum level is greater than 5mEq/L Causes: Renal Failure -Deficit of aldosterone -“Potassium-sparing” diuretic drugs”: prevent K+ from being excreted in adequate amounts (get rid of water in urine & keep K+) -Leaking of ICF k+ into ECF (pts w/ extensive tissue damage) -Prolonged or severe acidosis Effects: Cardiac dysrhythmias, may lead to cardiac arrest -muscle weakness, may lead to paralysis -Neuromuscular impairment -Fatigue, nausea, paresthesias c. Calcium: Extracellular cation, ingested in food, stored in bone, excreted in urine & feces, balance controlled by parathyroid hormone (PTH) & calcitonin, vitamin D promotes absorption from intestine, activated in kidneys Functions: structural strength for bones & teeth, stability of nerve membranes, muscle contractions, metabolic processes & enzyme reactions, blood clotting calcium increases, phosphate decreased. Calcium decreases phosphate increases Hypocalcemia: “To low calcium” serum level less than 4mEg/L Causes: Hypoparathyroidism: decreased parathyroid hormone=decreased intestinal calcium absorption -Malabsorption syndrome: decreased intestinal absorption of vitamin D or calcium -Deficient serum albumin -Increased pH level (alkalotic or basic) -Renal Failure: retention of phosphate causes loss of calcium; vitamin D is not activated=decrease intestinal absorption of calcium Effects: Increased permeability & excitability of nerve membranes-spontaneous stimulation of skeletal muscle; muscle twitching, Trousseau;s sign carpopedal spasm: when BP cuff blocks circ. To hand -Cheosteks: spasm of lip or face when face is tapped in front of the ear -tetany (skeletal muscle spasms) -Laryngospasm: obstructs airway -Weak heart contractions from insufficient calcium needed for muscle action: delayed conduction, may lead to dysrhythmias & decreased BP Skeletal muscle spasms result from the increased irritability of the nerves associated with the muscle fibers, whereas the weaker contraction of cardiac muscle (which lacks nerves). adequate calcium is stored in the skeletal muscle cells to provide for contractions, whereas contraction of cardiac muscle relies on available extracellular calcium ions passing through the calcium channels Hypercalcemia: “To much calcium” serum greater than 5mEq/L Causes: uncontrolled release of calcium ions from bones due to neoplasms (directly destroy bones releasing excess calcium also may secrete excess PTH) -Hyperparathyroidism -Immobility (demineralization): decrease stress on bone -Increased Calcium intake: excessive vitamin D or excess dietary calcium -Milk-alkali syndrome: increased milk & antacid intake elevating calcium serum levels Effects: Depressed neuromuscular activity=muscular weakness, lethargy, personality changes, anorexia, nausea -Interference with the function of ADH in kidneys=less absorption of water & polyuria, decrease in renal function -increased strength in cardiac contractions, dysrhythmias may occur d. Magnesium: Intracellular ion, serum level 0.7-1.1mol/L. Serum levels are linked to potassium & calcium levels -Important in enzyme reactions, protein & DNA synthesis Hypomagnesemia: from malabsorption or malnutrition assoc. w/ alcoholism Causes: diuretics, diabetic ketoacidosis, hyperthyroidism, hyperaldosteronism Effects: neuromuscular irritability, tremors, insomnia, personality changes, increased heart rate w/ arrhythmias Hypermagnesemia: occurs with renal failure, depresses neuromuscular function, decreased reflexes, lethargy, cardiac arrhythmias e. Phosphate: Serum level 0.85 to 1.45mol/L -Important in: bone & tooth mineralization -Metabolic processes, involving cellular energy source (ATP) -Phosphate buffer system (acid-base balance) Removes H+ from the body through kidneys -Reciprocal relationship with serum calcium Hypophosphatemia: low serum phosphate levels Causes: mal absorption, diarrhea, excessive use of antacids, alkalosis, hyperparathyroidism Effects: Neurological function impairment -Tremors -weak reflexes -paresthesias -confusion, anorexia, difficulty swallowing(dysphagia) Hyperphosphatemia: High serum levels of phosphate Causes: Renal failure f. Chloride: extracellular anion normal serum level 98-106mol/L -Chloride levels are related to sodium levels (High Na=High Cl) (Low Na=Low Cl) -Assists with bicarbonate ions to maintain acid-base balance by exchanging places as the blood circulates through the body Hypochloremia: Low serum chloride Causes: Alkalosis, vomiting when hydrochloric acid is lost from the stomach -Excessive perspiration assoc. w/ fever or hard labor on hot a day may lead to loss of sodium chloride=hyponatremia & hypochloremia also dehydration Hyperchloremia: Excessive chloride Causes: excessive intake of sodium chloride taken orally or intravenously, hypernatremia from other causes, leading to edema & weight gain Chapter 21: Congenital and Genetic Disorders 20. Describe the difference between karyotype, genotype, and phenotype: Karyotype is the visual representation of chromosomes that are arranged in order of size, used to diagnosis chromosomal disorders. Genotype is the genetic info carried by the individual all cells except gametes. Phenotype is the physical appearance of individual’s characteristics this is the expression of genes. 21. Describe the difference between meiosis & mitosis: Meiosis (sexual repro) sperm & ovum receive 23 chromosomes, 1 chromosome from each pair, ovum is fertilized by sperm=zygote that has 46 chromosomes, or 23 pairs, of genetic info inherited from each parent. During mitosis (cell division) chromosome replicate and each daughter cell get a copy of DNA that is identical to the parent cell, same genetic info is carried on. 22. List examples of the following: a. Single-Gene Disorders: Trait controlled by one set of alleles, classified by inheritance patterns, single gene may control a limited function i. Autosomal dominant disorders: inheritance of one alleles causes disorder, only one parent needs to carry allele. Ex.) Huntington’s disease ii. Autosomal recessive disorders: Both parents must pass on the allele for disorder. Heterozygous Cc & Cc parents are not affected of disease but possibility of passing recessive trait “c” onto children, they are a carrier OR Homozygous: cc & cc parents are affected & child has the disorder. Ex.) Cystic Fibrosis iii. X-linked dominant disorders (can happen in male & female): Inherited as a dominant allele on the X chromosome, mutation causes affected X chromosome to appear constricted or broken. Ex.) Fragile X chromosome iv. X-linked recessive disorders: Allele carried on X chromosome not Y chromosome. Heterozygous males lacking matching unaffected gene on the Y chromosome XA Y=normal, Xa Y=affected male. Heterozygous females Xa XA=carriers. Homozygous recessive female may be affected Xa Xa. Ex.) Hemophilia A b. Multifactorial Disorders: Genes/ genetic influences combined with environmental factors. Ex.) cleft palate c. Chromosomal Disorders: Extra or missing chromosomes on a pair of chromosomes. Ex.) Down syndrome 23. Explain the probability of a child being affected by the following: a. Autosomal recessive disorders b. Autosomal dominant disorders c. X-linked recessive disorders 24. Describe each disorder: a. Fragile X Syndrome: Mental retardation, cognitive deficit. Inherited as a dominant allele carried on X chromosome-mutation causes affected X to appear constricted or broken. b. Down Syndrome (Trisomy 21): Can be caused by nondisjunction/ translocation. 3 chromosomes rather than two on the 21st pair of chromosome. Individual has 47 chromosomes instead of the normal 46. Delayed development & delayed/incomplete sexual development, loose joints. c. Turner Syndrome (Monosomy X) XO: When only one sex chromosome, X chromosome is present. Person only has 45 chromosomes. Affects females, short stature, infertility. d. Klinefelter Syndrome XXY: Extra X chromosome is present. 47 chromosomes. 25. What needs to be present in order for a multifactorial disorder to occur? Number of genes/genetic influences combined with environmental factors 26. Describe an amniocentesis procedure: extraction of amniotic fluid from the uterus & extraction of a sample of the chorionic villus of the fetus. To examine sample of fetal tissue a. Why is it done? To detect chromosomal abnormalities b. What are the risks? (2) 1. Physical risk to mother and baby 2. Some tests may not show conclusive results Chapter 6: Infection 27. Does bacteria need living tissue to survive? No 28. What are exotoxins secreted by bacteria, how are they harmful? Produced by gram-pos. bacteria, they diffuse through body fluids affecting nerve conduction (tetanus). Stimulate antibody/antitoxin production which are than used as toxoids to induce immune response. 29. What are endotoxins secreted by bacteria, how are they harmful? Present in cell wall of gram- neg. bacteria that are released when bacterium dies. They cause fever, weakness, effected circulatory system=increased capillary permeability, loss of vascular fluid & endotoxic shock. 30. How do we try to limit bacterial growth? Besides antibiotics. Locate/remove or isolate reservoir of infection -Identify & restrict access to contamination -Reduce contact between infected persons & non-infected persons -block portals of exit/entry -Remove or block modes of transmission -Reduce susceptibility by immunizations, adequate nutrition & access to health care 31. Do viruses require a living host? Why? Yes, uses the host’s cell to synthesize viral proteins & nucleic acids (replication). 32. Why is it difficult to become immune or get the right vaccine for certain viruses? What do they do to prevent this immunity? What are some examples? Viruses are constantly changing during replication. They also lack their own metabolic processes/structures that would normally be attacked by drugs. 33. What is the candida fungi? Yeast a. What infections can it cause? Thrush (oral infection), vaginal infections (yeast infection) 34. What is the purpose of resident (normal) flora? Help in preventing other or foreign organisms from growing or forming a colony 35. What 3 areas of the body do not have normal flora and should be sterile? Blood, cerebrospinal fluid, lungs 36. Describe the different modes of transmission for infection: a. Direct contact: Touching infectious lesion, sexual activity, contact w/ infected blood or bodily secretions. b. Indirect contact: Intermediary object or organism, contaminated by hand or food, or fomite-inanimate object (toys, phones, stethoscope etc.) c. Droplet transmission: Resp. or salivary secretions are expelled from infected individual (coughing, sneezing etc.) d. Aerosol transmission: “airborne” small particles from the resp. tract, suspended in the air and can travel farther than droplets. (TB) e. Vector-borne: Insect or animal is an intermediate host 37. What is the major body part for transmitting infection?! HANDS a. That being said, HAND WASHING is one of the most important interventions anyone can do to prevent the spread of infection – remember this for the rest of your life. 38. What are nosocomial infections? Infections that occur in health care facilities Ex.) UTI from Foley 39. What are two main nosocomial infections that are extremely dangerous and often deadly? C. diff (Clostridium difficile) & MRSA (Methicillin-resistant Staphylococcus aureus) 40. Describe ways that a host can be resistant to infection? 41. What is an interferon and why are they important?? Interferons are the bodies 2nd line of defense that help fight against viruses, they also protect uninfected cells against viruses. 42. What are factors that decrease host resistance? Age, pregnancy, malnutrition, chronic disease, severe physical/emotional distress. 43. What is the difference between virulence and pathogenicity? Pathogenicity is the capability of a microbe to cause disease & virulence is the degree of pathogenicity. Virulence is based on invasive qualities, toxic qualities, adherence & ability to avoid host defenses (how bad is it?) 44. Describe each stage of the chain of infection & how to break it at each stage if applicable (Figure 6-12): a. Reservoir: Source of infection. Environmental source such as contaminated soil. Infected person or animals b. Portal of exit: mouth, skin, intestine (minimize coughing & sneezing, disposal of contaminated items) c. Transmission: i. Direct: saliva, blood, feces, semen, exudates from skin (gloves, glasses, gowns, safe waste disposal) ii. Indirect: resp. droplet on hands, surfaces, insect bites (vectors), contaminated food or water (hand-washing, disinfect, sterilize, food handling & cooking, water treatment) d. Entry: mouth, nose, vagina (covering nose & mouth w/ mask, covering open wounds or mucous membranes e. Susceptible host: Health status, point of entry, # of microbes f. Incubation period: Time between entry of organism into the body and the appearance of clinical signs of the disease. asymptomatic g. Infectious disease: Infectious disease fully develops, clinical manifestations reach a peak i. Carrier: Person with subclinical signs of the disease (no signs or symptoms) 45. Describe each technique to reduce transmission of infection: a. Sterilization: exposure to heat such as autoclaving & incineration b. Disinfectants: Chemical solutions that destroy microorganisms or their toxins on inanimate objects (bleach, alcohol wipes) c. Antiseptics: Chemicals applied to the body (skin) that do not cause damage (before surgery or iodine, isopropyl alcohol-70% or hand sanitizer) 46. Describe the following periods of infection and give signs and symptoms: a. Incubation period: Time between entry of organism into the body and the appearance of clinical signs of the disease b. Prodromal period: Time when infected person may feel fatigued, lose appetite. Typical “I’m not feeling well.” c. Acute period: Infectious disease fully develops, clinical manifestations reach a peak d. Recovery/convalescent period: Signs subside & body processes return to normal 47. Describe the patterns of infection: a. Local infections: organism enters the body and remains confined to a specific location b. Focal infections: pathogen spreads from a local infection to other tissues c. Systemic infections: infection spreads to several sites and tissue fluids, typically through the circulatory system. i. Septicemia: caused by multiple pathogens in the blood. This is the cause of sepsis (toxic inflammatory condition that comes from the spread of microbes). ii. Bacteremia: Presence of bacteria in the blood iii. Toxemia: Presence of toxins in the blood iv. Viremia: Presence of viruses in the blood b. Mixed infections: several infectious agents concurrently establish themselves at the same site c. Acute infections: appear rapidly w/ severe symptoms, but are short lived d. Chronic infections: less severe symptoms than acute, but persist for a long period e. Primary infections: initial infection followed by complications caused by another microbe f. Secondary infections: follows primary infection & caused by a microbe other than that causing the primary infection. Opportunistic pathogens are often the cause of a secondary infection g. Subclinical infections: does not cause & apparent signs or symptoms, may persist over long periods of time 48. Describe local and systemic signs of infection: a. Local: inflammation: pain or tenderness, swelling, redness, and warmth. If the infection is caused by bacteria, a purulent exudate, or pus, is usually present, whereas a viral infection results in serous, clear exudates. b. Systemic: Signs & Symptoms common to significant infections in any area of the body. Fever, fatigue, weakness, headache, nausea. Chapter 7: Immunity 49. Describe the function of the following terms: a. Antigens: Foreign substances or human cell surface antigens that are unique. Composed of proteins or polysaccharides. Antigens activate the Immune system to produce specific antibodies. b. Macrophages: Developed from monocytes, initiate the immune response. Engulf foreign material, secrete chemicals such as monokines and interleukins these are chemical mediators for inflammation. c. Lymphocyte: i. T lymphocytes (T cells): White blood cells 1. Where are they produced? From bone marrow stem cells 2. Where do they mature? Thymus 3. What immunity are they responsible for? Cell-mediated immunity: lymphocytes are programmed to attack non-self cells to protect the body ii. CD4+ T cell: 1. What disease destroys these cells which caused dangerous immunosuppression? HIV/AIDS iii. B lymphocytes (b cells): Become an antibody-producing plasma cell or a B memory cell 1. Where are they produced? Bone marrow 2. Where do they mature? spleen 3. What immunity are they responsible for? Humoral immunity-activated: antibodies are produced to protect the body iv. Natural killer cells: lymphocytes from T & B lymphocytes. Destroy w/out prior exposure. d. Antibodies: Specific protein produced in humoral response to bind with antigen 50. Describe the following types of immunity, their mechanism, and list examples: (Table 7-3) a. Natural active: Pathogen enter body & cause illness, active antibodies form in host. Have memory cell. Ex.) chicken pox b. Artificial active: Vaccine is injected into person. No illness results, antibodies form. Ex.) measles vaccine person gains immunity. Have memory cells c. Natural passive: Antibodies passed directly from mother to child to provide temporary protection. Don’t have memory cells. Ex.) Placenta passage during pregnancy/ingestion of breast milk d. Artificial passive: Antibodies injected into person to provide temporary protection or minimize severity of infection. Don’t have memory cells Ex.) Anti-venom 51. Describe the different types of tissue or organ transplants: a. Allograft (homograft): from human to human (of the same species) b. Isograft: Tissue transferred between two genetically identical bodies (Twins) c. Autograft: Tissue transferred from one part of the body to another part on the same individual skin or bone d. Xenograft: Tissue transferred from a member of one species to different species. Pig to human 52. What type of hypersensitivity reaction is organ/tissue rejection? 53. Describe the following rejections: a. Hyperacute: wrong tissue type & wrong blood type. Immediate after transplant b. Acute: Develops after several weeks c. Chronic or late: Occurs months or even years. Haven taken immunosuppressant meds. 54. How do we try to prevent rejection? What type of drugs? Immunosuppression drugs used to reduce the immune response to prevent rejection. Ex.) cyclosporine, azathioprine, prednisone. Individuals are at high risk for infection from opportunistic organisms (normal flora, bacteria, viruses etc) 55. Describe each type of hypersensitivity reaction, clinical manifestations and examples: a. Type I Allergic Reactions: immediate reactions caused by allergens, skin rashes, hay fever. This is the development of IgEs i. Why is epinephrine so helpful for the treatment of anaphylaxis? Vasoconstriction of blood vessels, directs blood to vital organs. Also bronchodilates the lungs, increases BP b. Type II: Cytotoxic Hypersensitivity: take longer. Antigen is present on cell membrane, Normal body component or exogenous, circulating IgGs react w/ antigen, destruction by phagocytosis or cytolytic enzymes. Ex.) Incompatible blood transfusion c. Type III: Immune Complex Hypersensitivity: Happens in a couple of days or can be chronic. Antigen combines with body, forms immune complexes deposited in tissue, activation of complement system. This causes inflammation & tissue destruction. Ex.) Rheumatoid arthritis d. Type IV: Cell-Mediated or Delayed Hypersensitivity: Can happen in weeks, months or even years. Delayed response by sensitized T lymphocytes, release of lymphokines, inflammatory response, destruction of antigen. Ex.) TB skin test 56. Explain how autoimmune disorders occur: Development of antibodies against own cells or tissues. Autoantibodies are antibodies formed against self-antigens-loss of self-tolerance. Can affect single organs or tissues. a. What are some examples? Ex.) Systemic Lupus, Scleroderma 57. Explain possible causes of immunodeficiency: Partial or total loss of one or more immune system components. Increases risk of infection & cancer 58. What type of virus is human immunodeficiency virus (HIV)? Secondary or acquired immunodeficiency. Or a retrovirus: Containing RNA, with the enzyme reverse transcriptase & coat is covered w/ lipid envelope covered in “spikes” of glycoproteins that the virus uses to attach to human cells 59. HIV mainly attacks what type of cells? Helper T cells & CD4 lymphocytes a. What is the function of these cells in the body? Helper T-cells: Activate B & T cells, control or limit specific immune response CD4 lymphocytes: role in humoral & cell-mediated immunity 60. When do symptoms of HIV usually develop? Late is the disease process b/c of latent asymptomatic period 61. How is HIV transmitted? Sexual activity. Contact with semen or blood of infected individual 62. How is HIV not transmitted? Protected sex, not sharing needles, proper gloving when coming in contact with bodily secretions (blood or semen) 63. When is AIDS diagnosed? 2 ways (Answered for you already) a. Major decrease in CD4+ T cells b. Presence of an opportunistic infection or unusual cancer i. Candida infection in the lungs, blood, or tissues: Herpes complex ii. Pneumocystis carinii: common in HIV/AID patients. Pneumonia or cancer iii. Kaposi’s sarcoma: Termed AIDS indicator disease. Affects skin, mucous membranes & internal organs iv. Non-Hodgkin’s lymphoma v. Tuberculosis 64. When are antiretroviral therapies indicated? a. Severe symptoms b. CD4 count over 500 c. Pregnancy d. HIV-related kidney disease e. When treated for hepatitis B 65. For antiretroviral therapies to be effective, they MUST be taken at the same time every day, those who cannot adhere to this generally are not given antiretroviral medications due to the virus becoming resistant to the medications. Chapter 20: Neoplasms and Cancer 66. What does oncology refer to? The study of malignant tumors 67. What are the warning signs of cancer? -Unusual bleeding or discharge anywhere in the body -Change in bowel or bladder habits (prolonged diarrhea/discomfort) -Change in wart or mole -Sore that does not heal -Unexplained weight loss -Anemia/ low hemoglobin & persistent fatigue -Persistent cough or hoarseness w/out reason -Solid lump, often painless, in breast or testes or anywhere on the body 68. Describe local effects of tumors: -Pain: press on nerves, occurs when tumor is well advanced -Obstruction: When tumor compresses a duct or passageway, blood supply or lymphatic flow may be restricted -Tissue necrosis & ulceration: may lead to bleeding or infection around the tumor 69. Describe systemic effects of malignant tumors: -Weight loss & cachexia (severely emaciated), anorexia, fatigue, pain, stress -Anemia: caused by blood loss at tumor site, nutritional deficits -Severe fatigue: inflammatory changes -Effusions: Inflammation causes fluid buildup in body cavities -Infections: occur frequently as resistance declines -Bleeding: Tumor cells may erode the blood vessels -Paraneoplastic syndrome: Assoc. with certain tumor types, release substances that affect neurological function may have hormonal effects 70. What are tumor markers? Substances, enzymes, antigens or hormones produced by some neoplastic cells. a. How are they useful? They can be used to screen high-risk people to confirm diagnosis, or monitor malignant tumor. 71. Explain the difference between primary and secondary tumors: Secondary tumors are additional sites that the primary tumor has spread to. Secondary tumors are known as metastases. 72. Describe the three basic mechanisms for the spread of cancer: a. Invasion: Local spread, tumor cells grow to adjacent tissues b. Metastasis: Spread to distant sites via blood, lymph or other body fluids i. What nodes of the body are involved in metastasis? Lymph ii. How do we prevent micrometastases? Removing the lymph nodes or treating them. c. Seeding: the spread of cancer cells in body fluids or along membranes in body cavities 73. When staging cancer, what are staging systems based on? (3 things) -Size of primary tumor (T) -Involvement of regional lymph nodes (N) -Spread (metastasis) of tumor (M) 74. Which cells in the body are responsible for identifying and destroying cancer cells and cells that are labeled as foreign? (3 total) Interferons, Macrophages, T lymphocytes 75. Describe each treatment for surgery: a. Curative: if tumor is small and localized b. Palliative: Cancer advanced. Reduces manifestations & complications related to the cancer c. Chemotherapy: Antineoplastic drug used to treat cancer sometimes alongside radiation and surgery. (Adriamycin, Bleomycin, Vinblastine, Dacarbazine). Interferes w/ protein synthesis & DNA replication i. What are adverse side effects of chemotherapy? -Bone depression -Low blood counts -vomiting -Damage to epithelial cells -Fibrosis in the lungs, damage to myocardial cells -Nausea, hair loss d. Radiation: Causes mutations or alterations in targeted DNA i. What does it prevent in order to cause immediate cell death? Prevents mitosis, damaging blood vessels cutting off the blood supply to the tumor cells ii. Describe the adverse effects of radiation? -Bone marrow depression -Epithelial cell damage & damage to blood vessels -Damage to repro. Organs -Fatigue, lethargy, mental depression 76. What are the factors that contribute to malnourishment in cancer patients? Change in taste sensations, anorexia, vomiting, sore mouth/loss of teeth, pain, fatigue, inflammation of the digestive tract leading to malabsorption, altered metabolism, tumor taking nutrients from the body. 77. If cancer patients are extremely malnourished, what nutrition therapy may be used? Explain. Total parenteral nutrition. This is the administration of a nutrient mixture directly into a peripheral vein. 78. What is the most common skin cancer? Basal Cell carcinoma 79. What are high risk factors for developing skin cancer? Fair skin, over 40 yrs old, live in southern climates, high exposure to sun w/out protection 80. What are clinical manifestations of ovarian cancer? Why are these tumors called “silent” tumors? B/c it is hidden in the peritoneal cavity. Pressure on the bladder or intestine, inflammatory exudate forms in abdominal cavity. Altered bowel/bladder function, increased abdominal girth. 81. Whether benign or malignant brain tumors cause pressure/swelling in the brain which cause serious issues. 82. Which location of the brain are brain tumors most deadly, why? Brainstem or cerebellum b/c very little room for surgery. Usually primary tumor is fatal 83. List the three most common cancers found in men: Prostate, lung, colorectal 84. List the three most common cancer found in women: Breast, lung, colorectal [Show More]
Last updated: 1 year ago
Preview 1 out of 43 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$18.00
Document information
Connected school, study & course
About the document
Uploaded On
Oct 25, 2021
Number of pages
43
Written in
Additional information
This document has been written for:
Uploaded
Oct 25, 2021
Downloads
0
Views
64

.png)




.png)