Biology > STUDY GUIDE > NSG 331 Exam 1 study guide 2019/2020 – Marian University | NSG331 Exam 1 study guide 2019/2020 (All)
NSG 331 Exam 1 study guide 2019/2020 – Marian University | NSG331 Exam 1 study guide 2019/2020
Document Content and Description Below
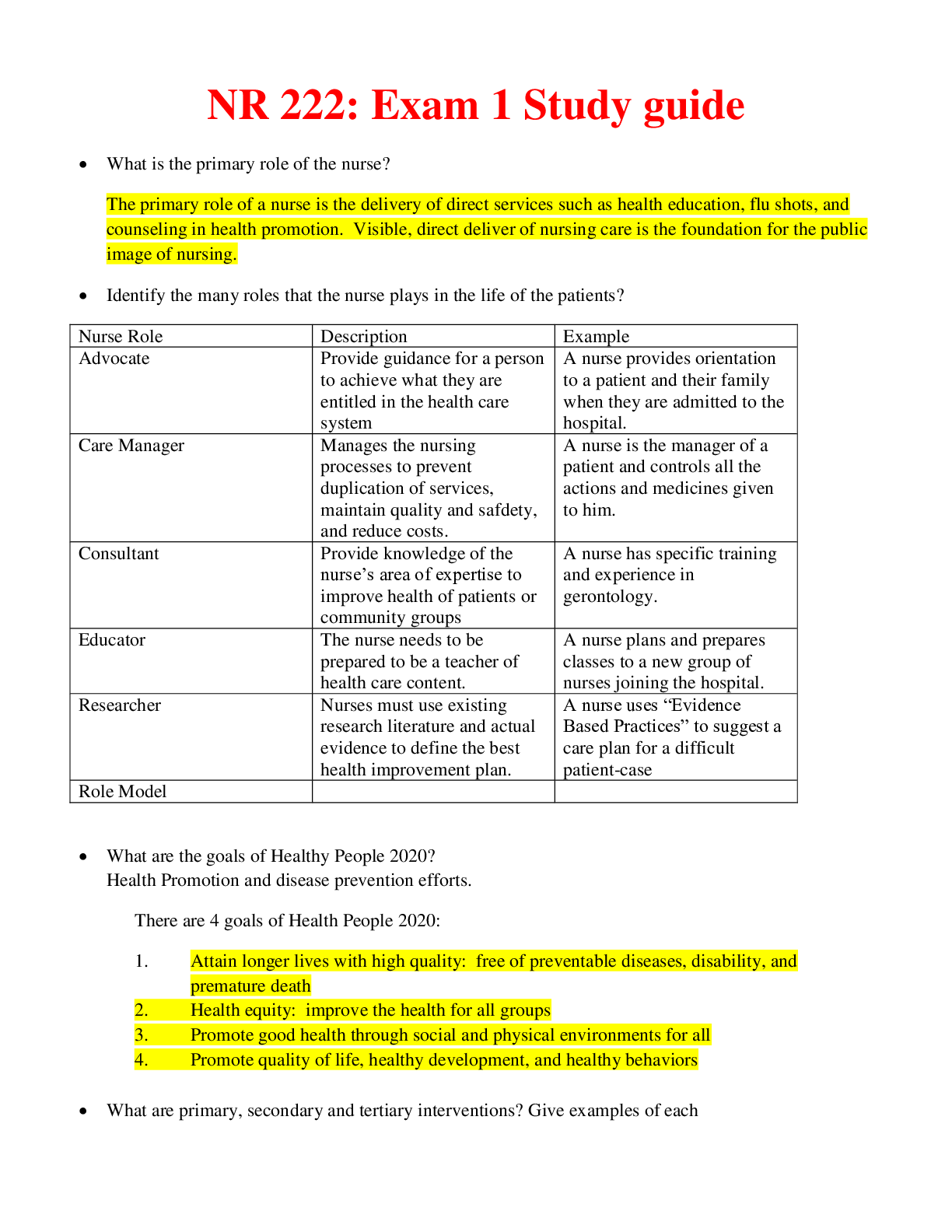
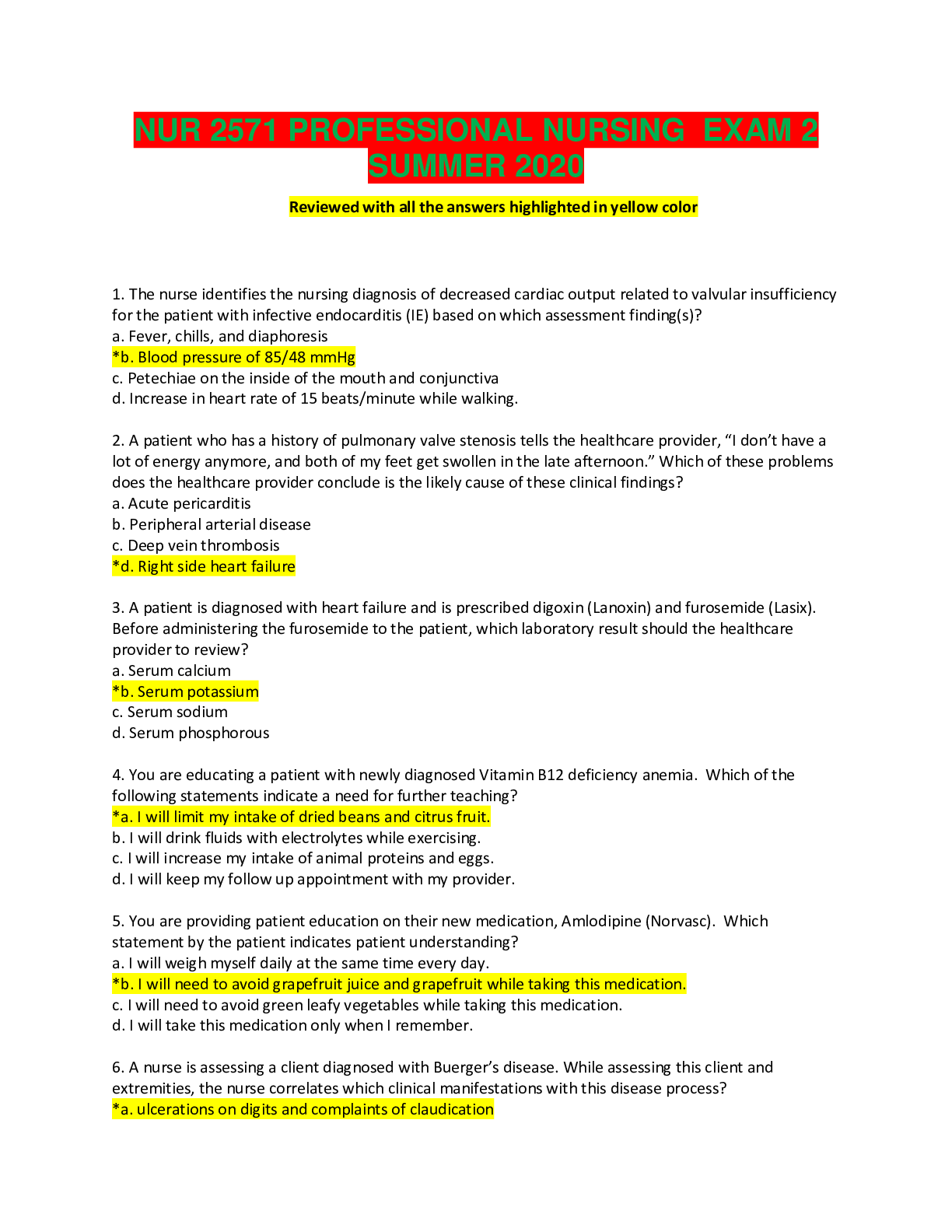
NSG 331 Exam 1 study guide 2019/2020 – Marian University Fluid and Electrolytes Distribution of Body Fluids • Water is most important nutrient of life. • Total body water is about 55-75% o... f body weight. • Can live without food for days. One must have water to live. • Daily weights are the most reliable measure of volume status. Changes in water content • • Higher fat = lower body water content • Women/elderly have lower water percentage d/t lower lean body mass o Older adults = 45-50% body water Compartments • Intracellular (ICF): fluid within the cells. 2/3 of body fluids in the ICF (40% of body weight) • Extracellular (ECF): outside the cells – 14L (70kg man = 10L in interstitial; 3L in plasma; 1L in transcellular) o Intravascular (1/3): liquid part of blood - AKA plasma. Fluid within the vascular system (blood) o Interstitial (2/3): space between cells & outside the blood vessels o Other: lymph, transcellular (secretions from epithelial cells: CSF, pleural, GI, liver, pancreas, salivary glands, urine, sweat, joint spaces, peritoneal, intraocular, pericardial) o In a 70kg man: about 42L of water distributed as… Calculation of Fluid Gain or Loss • One liter of water weighs 2.2 lb (1 kg) • Body weight change is an excellent indicator of overall fluid volume loss or gain o 240 mL (8 oz fluid) = 0.5 lbs / 0.23 kg weight gain o 4.4 lb loss = 2 kg = 2 Liters loss Body Fluid Functions • Transportation of nutrients, hormones, enzymes, blood platelets, RBC • Facilitates cellular metabolism & chemical functioning • Solvent for electrolytes • Maintains body temperature • Facilitates digestion & promotes elimination • Tissue lubricant Electrolytes • Substances whose molecules dissociate into ions when placed in water o Cations: positively charged – Na, K, Ca, Mg o Anions: negatively charged- Bicarbonate, chloride, phosphate – most proteins carry a negative charge • Concentration of electrolytes is expressed in milliequivalents (mEq)/L • Concentrations of cations & anions in ICF and Plasma Mechanisms Controlling Fluid and Electrolyte Movement • Diffusion: Movement of molecules across a permeable membrane from high to low concentration o Movement stops when concentration equalizes – uses no energy • Facilitated diffusion o Uses carrier protein in the cell membrane to move molecules o Requires no energy o i.e. glucose transport into cells • Active transport o Process in which molecules move against concentration gradient o External energy is required for this process o i.e. Na-k+ Pump • Osmosis: Osmosis is the movement of water through a semipermeable membrane that does not allow solutes to cross (less concentrated (more water) to more concentrated (less water)) o No energy required o Concentration of sol’n determines strength of osmotic pull o Stops when concentrations are equal or hydrostatic pressure equals that of opposing forces • Osmotic pressure (milliosmoles = mOsm) o Amt of pressure req’d to stop osmotic flow of water (higher concentration=greater osmotic pressure) o Osmolarity measures the total milliosmoles/L of solution ♣ Concentration of molecules per VOLUME of solution o Osmolality measures the number of milliosmoles/kg of water ♣ Concentration of molecules per WEIGHT of water ♣ Preferred measure to evaluate the concentration of plasma, urine, and body fluids • Sodium-Potassium Pump – active transport o Energy used to move sodium out and potassium in (ATP) Measurement of Osmolality (tonicity) • Osmolality usually the same in all body fluids – very useful in determining total body water balance • Calculate the plasma osmolality using the following formula o Plasma Osmolality = (2 x Na) + (BUN / 2.8) + (glucose / 18) o Urine osmolality = 100-1300mOsm/kg – depends on fluid intake, amt of ADH, and renal response to ADH • Normal plasma osmolality is between 280 and 295 mOsm/kg (>295 = water deficit; <275 = water excess) Osmotic Movement of Fluids • The osmolality of the fluid surrounding cells affects them o Isotonic – no fluid movement o Hypotonic – solutes less concentrated than cells – water into cell to o Hypertonic – solutes more concentrated than cells – water out of cell to dilute ECF o Effects of Water Status on RBC Mechanisms Controlling Fluid and Electrolyte Movement • Hydrostatic pressure o Blood pressure generated by heart contraction – pressure decreases as it reaches capillary bed o Force of fluid in a compartment that pushes against a cell membrane or vessel wall o Capillary (30 mm Hg) = forces that pushes water out of vascular system and into interstitial space • Oncotic pressure (colloidal) – i.e. albumin o Osmotic pressure caused by plasma proteins in sol’n - Attract h20 from tissue space into vascular space o Plasma (oncotic pressure = 25 mmHg) normally has much more proteins than interstitial fluids (1 mmHg) Fluid Exchange Between Capillary and Tissue • Amount and direction of movement determined by o Capillary hydrostatic pressure – move h20 out of capillaries ♣ Arterial end: exceeds plasma oncotic pressure which moves water into interstitial space ♣ Venous end: less than plasma oncotic pressure = fluid moves into capillary o Plasma oncotic pressure – move fluid into the capillaries o Interstitial hydrostatic pressure – move fluid into capillaries o Interstitial oncotic pressure – move water out of capillaries Edema/ Fluid Shifts • Plasma to interstitial fluid shift =edema o Elevation of VENOUS hydrostatic pressure (fluid overload, heart/liver failure, obstruction of venous return to heart (tourniquet, restrictive clothing, thrombosis) or venous insufficiency (varicose veins)) o Decrease in plasma oncotic pressure (decreased protein: renal disorders (loss); liver disorders (deficient synthesis); decreased dietary intake (malnutrition)) o Elevation of interstitial oncotic pressure (damage to capillary walls = protein accumulation in interstitial space: trauma, burns, inflammation) o Obstruction of lymphatic outflow causes decreased removal of interstitial fluid • Interstitial fluid to plasma – decreases edema o With increase in plasma osmotic or oncotic pressure (administration of colloids, dextran, mannitol, albumin, hypertonic solutions) o Compression stockings decrease peripheral edema via increasing tissue hydrostatic pressure Fluid Spacing • First spacing: Normal distribution of fluid in ICF and ECF • Second spacing: Abnormal accumulation of interstitial fluid (edema) • Third spacing: Fluid accumulation in part of body where it is not easily exchanged with ECF o Nonfunctional areas between cells – difficult/impossible to move back into cells or blood vessels o Example = Ascites - from peritonitis, pancreatitis, edema associated with burns trauma or sepsis Homeostatic Regulation • Hypothalamic-pituitary regulation o Body fluid deficit / Increases in plasma osmolarity activates osmoreceptors in hypothalamus ♣ Activates thirst and release of ADH from posterior pituitary to retain water (distal tubules) ♣ Thirst mechanism major defense against dehydration - Elderly have reduced thirst mechanism o Dec BP, nausea, painm hypoglycemia, hypoxemia all stimulate ADH release; ♣ postop stress response, receiving analgesics/anesthesia = ADH release and decreased osmolality o Dry mouth will cause a person to drink even when there is no body water deficit • Renal Regulation o Kidneys regulate water balance by adjusting urinary volume and excretion of electrolytes o Avg adult = kidneys reabsorb 99% of filtrate = 1.5L urine per day ♣ Kidney issues = less ability to regulate = edema, etc. • Adrenal cortical Regulation o Release of hormones to regulate water and electrolytes ♣ Glucocorticoids – cortisol – anti-inflammatory = increase serum glucose levels ♣ Mineralocorticoids – aldosterone =enhance Na retention/K+ excretion (dec Na = RAAS activation ♣ Hormones regulate amt of water is retained • Cardiac Regulation o Natriuretic peptide (antagonist to RAAS) – cardiomyocytes: response to incr atrial pressure & incr Na ♣ Decrease blood volume = atrial NP (ANP) and b-type NP (BNP) – renal tubules – excrete Na/H2O ♣ Activate to decrease volume – elevated = CHF – inhibit aldosterone, renin, ADH, angiotensin II • Gastrointestinal Regulation o Oral intake accounts for most water (D/V = losing fluid/electrolytes) o Secretes approximately 8000mL of digestive fluid that is reabsorbed (small amt eliminated in feces) ♣ D/V – prevents reabsorption – fluid and electrolyte loss • Insensible water loss = Sweating • Sensible water loss = Excessive sweating – exercise, fever, excessive environmental heat Effects of Stress on Fluid and Electrolyte Balance Normal Fluid Balance – avg healthy adult requires daily intake b/n 2000 and 3000 mL per day Gerontologic Considerations • Structural changes in kidneys decrease ability to conserve water – less able to concentrate urine • Hormonal changes include a decrease in renin and aldosterone and increase in ADH and ANP • Loss of subcutaneous tissue leads to increased moisture lost • Decreased thirst mechanism in hypothalamus = drink less • Decreased mobility = don’t want to have to go to bathroom so stop drinking as much Fluid and Electrolyte Imbalances • Interrupts normal homeostatic mechanism (deficits or excess – both types common to have in same Pt) • Directly caused by illness or disease (burns or heart failure) • Result of therapeutic measures (colonoscopy preparation, diuretics) Fluid Volume Excess (FVE): Hypervolemia • Causes: CHF, renal failure, cirrhosis, Na, excess iso/hypotonic fluids, primary polydipsia, SIADH, cushings • S&S: edema, wt gain, moist lung sounds, bounding pulse, intake > output, distended neck & hands veins o Headaches, confusions, muscle spasms, seizures, coma, S3 heart sounds, JVD • Treatments: treat underlying cause, diuretics, low Na diet, weights, I&0, measure abd girth, TEDs. o Remove fluid without producing abnormal changes in electrolyte composition/fluid osmolality o Pleuracentesis/thoracentesis necessary for ascites or pleural edema o If pt is hyponatremic and the cause is FVE then fluid restriction is the treatment Fluid Volume Deficit (FVD): Hypovolemia • Causes: decr intake, vomiting, fever, diarrhea, NG loss, hemorrhage, 3rd spacing, incr insensible loss, diab insipid • S&S: dry, pale cold clammy skin, wt loss, decreased turgor and cap refill, tachycardia, postural hypotension, high HCT level, low U/O, low grade temp, altered mental status, seizures, coma, restlessness, drowsiness • Treatment: underlying cause, oral/IV fluids (0.9% NS), blood (if d/t hemorrhage), rest, nutrition • Nursing measures: VS, I&O, postural hypotension (safety) Differential Assessment of ECF Volume Nursing Management: Nursing Diagnoses • Hypovolemia o Deficient fluid volume – r/t excess ECF losses or decr fluid intake o Decreased cardiac output – r/t excessive ECF losses or decr fluid intake o Risk for impaired oral mucous membranes o Potential complication: Hypovolemic shock • Hypervolemia o Excess fluid volume – r/t increased water or sodium retention o Impaired gas exchange – r/t water retention leading to pulmonary edema o Risk for impaired skin integrity (b/c peripheral edema) o Activity intolerance r/t incr water retention, weakness, lethargy o Disturbed body image (b/c edema) o Potential complications: Pulmonary edema, ascites Nursing Management: Nursing Implementation • Daily weights – most accurate (provided normal intake and not on NPO) – same time, scale, clothes, etc. • I & O – specific gravity also measured - >1.025 = concentrated urine; < 1.010 = dilute urine • Laboratory findings – serum osmolality – inc BUN, sodium, HCT levels (deficit); deficit = decreased values • Cardiovascular care – excess = full/bounding pulse and JVD • Respiratory care – pulse Ox /lung sounds – pulmonary congestion and edema d/t increased hydrostatic pressure o ECF deficit = inc RR d/t decreased tissure perfusion = hypoxia (administer O2 as ordered) • Patient safety – risk for falls d/t orthostatic hypotension and muscle weakness • Skin care – turgor and mobility – priority for Pts with fluid imbalances – pitting edema • Assessment of skin turgor Fluid Therapy • Administer IV fluids as ordered – should be easily accessible – serve at room temperature – every 1-2 hrs • Maintain adequate oral intake o Assess ability to express thirst and swallow o Assist those with physical limitations (make easier to get water/use restroom) or dysphagia In a patient with prolonged vomiting, the nurse monitors for fluid volume deficit because vomiting results in a. Fluid movement from the cells into the interstitial space and the blood vessels a. Loss of both sodium and water = fluid moved into interstitial spaces and blood vessels - - -- - - - - - - - - - - - - - - - - - - - - - - - Renal Cell Carcinoma: Adenocarcinoma • Arises from cortex or pelvis (and calyces) • Most common kidney cancer in adults • 3% of adult malignancies in 90-95% of cancers in the kidney • 10th leading cause of cancer deaths in males in the US • Risk factors: • Men>women (twice as common in men) • Age 50-70 • Cigarette smoking doubles the risk (1/3 of all cases) – risk increases with amount of cigarettes • Obesity (particularly in women), HTN, exposure to asbestos, cadmium and gasoline • Genetic disorders that contribute to development – acquired cystic disease • Clinical manifestations • No early symptoms • Symptoms of compression, stretching, invading structures • Hematuria, flank pain, palpable mass (only 10% present with this “triad”) • Wt. loss, fever, HTN, anemia, hypercalcemia, night sweats, malaise • Diagnosis • 30% metastasis at dx to Lungs, liver and long bones • CT scan • Ultrasound • Angiography • Needle aspiration/biopsy • MRI • IVP – intravenous pyelogram • Nuclear scans – radionuclide isotope – used to detect metastasis • Labwork – urinalysis, CBC w/ differential, electrolytes, renal and liver function tests, serum calcium ♣ Management • Deter. By stage o Stage 1 – up to 7cm and confined to kidney o Stage 2 – greater than 7cm and confined to kidney o Stage 3 – extends to surrounding tissue and perhaps local lymph node o Stage 4 – outside kidney to multiple nodes and distant parts of body • Radical nephrectomy (stage 1-2 best choice) – best curative option o Later stage – palliation and improve outcome in metastatic disease • Radiation (palliative in inoperable cases and with mets to bone or lungs) • When surgery is not an option o Cryoablation (freezing) o Radiofrequency ablation – radiofrequency heat to destroy tumor • Chemotherapy (mets) – only used occasionally – 5-fluorouracil, floxuridine, gemcitabine • Immunotherapy – alpha interferon and Interleukin-2 – metastatic disease o Nivolumab (Opdivo) – blocks protein (PD-1) on T cells – boosts immune response against cancer cells ♣ Can shrink some tumors and slow cancer growth • Targeted therapy – preferred Tx for metastatic kidney cancer o Kinase inhibitors – block kinases (proteins) that play a role in tumor growth ♣ Sunitinib, sorafenib, cabozantinib, axitinib o Bevacizumab and pazopanib – inhibit new blood vessel growth to the tumor o Temsirolimus and everolimus – inhibit specific protein called the mechanism target of rapamycin • Vaccines and nonmyeloablative stem cell transplantation - experimental Bladder Cancer • Incidence o 1 in 20 cancers dx o 74,000 new/yr o 16,000 deaths/yr o Ages 60-70 – rarely found in ppl younger than 40 o Men 4x women • Risk factors o Cigarette smoking, cigars, pipes – damage lining of bladder – ½ of bladder cancers o Exposure to dyes used in rubber and cable industries, arsenic, textiles, and paint products o Women treated with radiation and pts given Cytoxan (cyclophosphamide) o Diabetes drug Actos (pioglitazone) o Chronic, recurrent renal calculi o Chronic lower UTIs, cystitis, bladder infections o Indwelling catheters for long periods – chronic bladder inflammation o Parasitic disorder – schistosomiasis o If already had bladder cancer, more likely to get it again o 1st degree relative (parent, sibling, child) has it – it increases your risk o Not always clear what causes o Some have no obvious risk factors • Manifestations o Microscopic or gross painless hematuria (chronic or intermittent) • Bright red or cola colored (gross) or look normal (microscopic) o Bladder irritability (dysuria, frequency and urgency) o Painful urination, pelvic pain o Back pain • Diagnosis o Urine specimens o Urine cytology – analyzed urine under microscope o Retrograde pyelogram to see where it is o CT o Ultrasound o MRI, bone scan, chest x-ray to stage the cancer (metastasis) o Cystoscopy (common) and biopsy • Management o Staging • Stage 1 – inner lining of bladder but not bladder muscle wall • Stage 2 – invaded bladder wall but confined to bladder • Stage 3 – through bladder wall to surrounding tissue, and potentially the prostate or uterus • Stage 4 – spread to lymph nodes and other organs o Surgical Treatment • Transurethral resection of bladder tumor (TURBT) – remove Stage 1 cancers • Small wire loop through cystoscope and burns away cancer cells with electric current • May also put in chemo into the bladder to kill remaining cancer cells • Also used to control bleeding in Pt who is poor operative risk with advanced tumors • Disadvantage: destroys tumor so it cannot be pathologically evaluated or staged • Cystectomy (segmental, partial, or radical) – surgical removal or all or part of the bladder • Radical = all the bladder, ureter, and surrounding lymph nodes • Typically involves removal of prostate and seminal vesicles in men, and the uterus, ovaries, and vagina in women • Risk of infection and bleeding, and in men can cause erectile disfunction • Encourage lots of fluids after the procedure • Urine after procedure may be pink for the first several days and free of clots • 7-10 days after may see dark red flecks as baldder wall heals • Neobladder reconstruction – new way for urine to leave body after radical resection (cystectomy) • Allows person to urinate normally, but some have to self catheterize • Ileal conduit – surgeon creates tube using piece of intestine, that drains ureter to outside of body • Continent urinary reservoir –small pouch created inside body using intestine – needs catheterization o Radiation Therapy – aimed at destroying cancer cells with high energy beams • Usually in combination with chemo as an alternative to surgery or when surgery isn’t an option o Chemotherapy – cisplatin, vinblastine, doxorubicin, methotrexate o Immunotherapy: Atezolizumab (IV) – signals body’s immune system to fight cancer cells • Advanced or metastatic bladder cancer that got worse after Sx or didn’t respond to chemo o Intravesical Immunotherapy – given through urethra directly into the bladder and retained for 2 hours • Weekly for 6-12 weeks • Change position during therapy every 15 minutes • Bacille Calmette-Guerin (BCG) – vaccine used in other countries to protect against TB • Stimulates immune system • May cause flu-like symptoms, increased urinary frequency • Interferon alfa-2b – protein made by body to fight infections o Intravesical chemotherapy – can be used if BCG fails • Mitomycin – chemotherapy antibiotic • Thiotepa – alkalyting agent • Can significantly reduce WBC and platelet counts • Valrubicin - chemotherapy antibiotic • Typical chemo SEs like nausea, vomiting, hair loss not experienced with intravesical o Systemic chemotherapy – multiple chemo drugs – done before surgery to increases chances of removing during surgery and continue to kill calls after surgery o After surgery • Drink a large vol of fluid • Avoid alcoholic beverages • Self-monitor urine (Pink first day but not bright red) • Opoid analgesics • Stool softeners • Sitz baths • Regular follow up care o After intravesical therapy • Flu-like symptoms – treat symptomatically • Incr. urinary freq, hematuria, systemic infection – monitor these o General management • Encourage pt to incr. daily fluid intake • Quit smoking • Assess for secondary UTI • Stress need for urologic follow-up • Psychosocial needs • Bladder spasms (B & O suppositories) Urinary Diversion • • Treatment for • Cancer of bladder • Neurogenic bladder • Congenital anomalies • Strictures • Trauma to bladder • Chronic infections Ileal Conduit • • Most common incontinent (diversion to skin requiring appliance) urinary diversion • Segment of ileum converted into a conduit for urinary drainage. • Drops of urine flow from stoma every few seconds, so external device needed. Kock Diversion (Continent) • • Continent (intraabdominal urinary reservoir) • Need for self-catheterization every 4-6 hrs • No external appliance needed Surgery of the Urinary Tract: Postop Management • Urine Output • Record output at least every 1-2 hrs • 0.5 ml/kg/hr – roughly 30mL • Assess drssg • Weigh daily • Respiratory Status • Enc. TCDB • Pain control • Incentive spirometer q 2 hr. • Early and freq ambulation • Abdominal Distention • Paralytic ileus caused by manipulation and compression of bowel during surgery • NPO until bowel sounds are present (24-48 hrs postop) Urinary Stoma • • Symmetric • No skin breakdown • Protrudes about 1.5 cm • Mucosa is healthy red – dusky = circulation is cut off • Assess every 2 hours [Show More]
Last updated: 1 year ago
Preview 1 out of 77 pages
Instant download

Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 04, 2020
Number of pages
77
Written in
Additional information
This document has been written for:
Uploaded
Jul 04, 2020
Downloads
0
Views
60