*NURSING > STUDY GUIDE > Med Surg Exam 3 Complete study guide|Galen College of Nursing - NUR 242 MS Exam 3 (All)
Med Surg Exam 3 Complete study guide|Galen College of Nursing - NUR 242 MS Exam 3
Document Content and Description Below
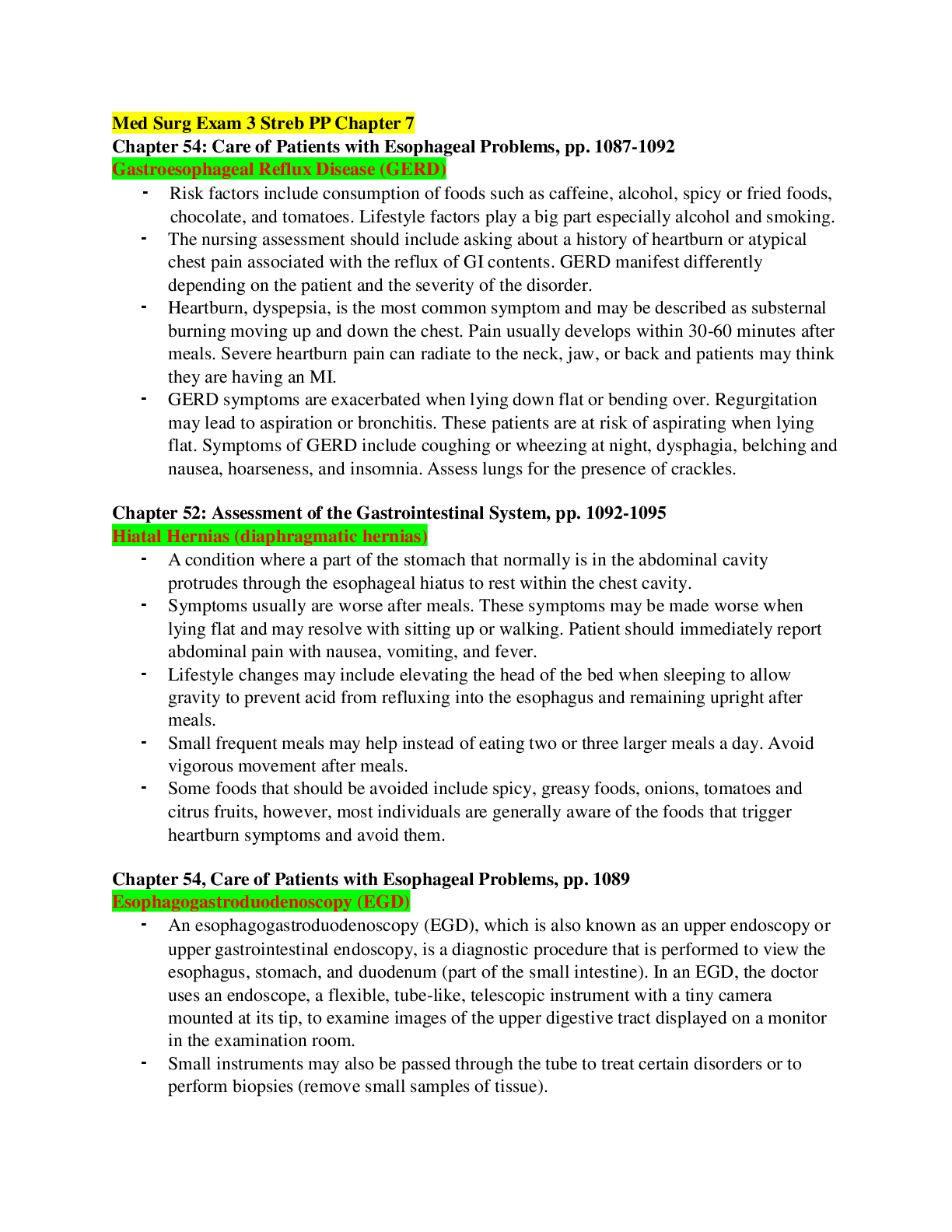
Gastroesophageal Reflux Disease (GERD) Risk factors include consumption of foods such as caffeine, alcohol, spicy or fried foods, chocolate, and tomatoes. Lifestyle factors play a big part espec... ially alcohol and smoking. The nursing assessment should include asking about a history of heartburn or atypical chest pain associated with the reflux of GI contents. GERD manifest differently depending on the patient and the severity of the disorder. Heartburn, dyspepsia, is the most common symptom and may be described as substernal burning moving up and down the chest. Pain usually develops within 30-60 minutes after meals. Severe heartburn pain can radiate to the neck, jaw, or back and patients may think they are having an MI. GERD symptoms are exacerbated when lying down flat or bending over. Regurgitation may lead to aspiration or bronchitis. These patients are at risk of aspirating when lying flat. Symptoms of GERD include coughing or wheezing at night, dysphagia, belching and nausea, hoarseness, and insomnia. Assess lungs for the presence of crackles. Chapter 52: Assessment of the Gastrointestinal System, pp. 1092-1095 Hiatal Hernias (diaphragmatic hernias) A condition where a part of the stomach that normally is in the abdominal cavity protrudes through the esophageal hiatus to rest within the chest cavity. Symptoms usually are worse after meals. These symptoms may be made worse when lying flat and may resolve with sitting up or walking. Patient should immediately report abdominal pain with nausea, vomiting, and fever. Lifestyle changes may include elevating the head of the bed when sleeping to allow gravity to prevent acid from refluxing into the esophagus and remaining upright after meals. Small frequent meals may help instead of eating two or three larger meals a day. Avoid vigorous movement after meals. Some foods that should be avoided include spicy, greasy foods, onions, tomatoes and citrus fruits, however, most individuals are generally aware of the foods that trigger heartburn symptoms and avoid them. Chapter 54, Care of Patients with Esophageal Problems, pp. 1089 Esophagogastroduodenoscopy (EGD) An esophagogastroduodenoscopy (EGD), which is also known as an upper endoscopy or upper gastrointestinal endoscopy, is a diagnostic procedure that is performed to view the esophagus, stomach, and duodenum (part of the small intestine). In an EGD, the doctor uses an endoscope, a flexible, tube-like, telescopic instrument with a tiny camera mounted at its tip, to examine images of the upper digestive tract displayed on a monitor in the examination room. Small instruments may also be passed through the tube to treat certain disorders or to perform biopsies (remove small samples of tissue). Certain medications (such as aspirin, anticoagulants and the anti-inflammatory drugs called NSAIDs) should be discontinued at least five to seven days before an EGD to reduce the risk of bleeding. NPO - Patients will be asked not to eat or drink anything for at least 8 hours before the procedure to ensure that the upper intestinal tract will be empty. Before the procedure, patients may be given a moderate sedative and/or pain medication, usually by intravenous injection. Monitor gag reflex, the sedation will block the gag reflex to prevent aspiration. Keep NPO until they get their gag reflex back. (1 to 2 hours before the anesthetic is out the system). Patient must have someone accompany them home after recovery. Chapter 55: Care of Patients with Stomach Disorders, pp. 1103-1107 Gastritis Gastritis occurs when the lining of the stomach known as the mucosa becomes inflamed or swollen. When the stomach mucosa becomes inflamed edema, hemorrhage and erosion of the mucosa occur. Medical treatment for gastritis depends on the specific cause. Patients will be instructed to stop taking irritating medications such as ASA and NSAIDS. Medications to decrease the amount of hydrochloric acid in the stomach are usually prescribed. These would include Antacids, H2 antagonists, and Proton pump inhibitors. The patient with gastritis is at risk for deficient fluid volume. A nursing priority is to access for the patient’s hydration status. This would include I&O, daily weights, & VS. Chapter 55: Care of Patients with Stomach Disorders, pp. 1107-1115 Peptic Ulcer Disease (PUD) Peptic ulcers are a break in the mucous lining of gastrointestinal tract from continued contact with gastric juice. This results in inflammation. Pain that is worsened by the ingestion of food. Ulcers in the mucosa of GI tract occur from several different causes. Duodenal ulcers are associated with a H. pylori infection. Gastric ulcers may cause a dull, aching pain, often right after a meal; eating does not relieve the pain and may even worsen it. Pain may also occur at late at night. Other symptoms associated with PUD are nausea with or without vomiting, weight loss, anorexia, belching and dyspepsia or indigestion. Patient may report a distended abdomen that is painful. Smoking contributes to the pathogenesis of peptic ulcer disease. Smoking causes an acceleration of gastric emptying of liquids, promotes of duodenogastric reflux and causes a reduction in mucosal blood flow. Patient should attend a smoking cessation course. Chapter 55, Care of Patients with Stomach Disorders, pp. 1116-1119 Gastric Cancer Stomach cancers tend to develop slowly over many years. Before a true cancer develops, pre-cancerous changes often occur in the inner lining (mucosa) of the stomach. These early changes rarely cause symptoms and therefore often go undetected. The decline of stomach cancer has been linked to the frequent use of antibiotics to treat infections. Antibiotics can kill the bacteria called Helicobacter pylori (H. pylori), which is thought to be a major cause of stomach cancer. Administer protein and vitamin supplements to foster wound repair and tissue building. Eat small, frequent meals rather than three large meals. Reduce fluids with meals but take them between meals. Stress the importance of long-term vitamin B12 injections after gastrectomy to prevent surgically induced pernicious anemia. Chapter 56, Care of Patients with Noninflammatory, pp. 1135-1137 Irritable Bowel Syndrome (IBS) Irritable bowel syndrome (IBS) refers to a disorder that involves abdominal pain and cramping, as well as changes in bowel movements Risk factors include consuming a diet high in fats and gas producing foods. Consuming carbonated beverages, caffeine and alcohol contribute to the development of IBS. Smoking and stress are other related factors. Emotional experiences such as anxiety and depression are also a factor as this affects the autonomic nervous system and its innervation to the bowel. Nursing care for the patient with IBS focuses on education and emotional support. Help the patient implement lifestyle changes that reduce stress. Remind the patient about regular exercise, discourage smoking while encouraging the need for regular physical examinations. Chapter 56, Care of Patients with Noninflammatory, pp. 1137-1139 Herniation A weakness in the abdominal muscle wall through which a segment of the bowel or other abdominal structure protrudes. Hernias can also penetrate through any other defect in the abdominal wall, through the diaphragm, or through other structures in the abdominal cavity. The most significant factors contributing to increased intra-abdominal pressure are obesity, pregnancy, and lifting heavy objects. Indirect Inguinal Hernia is a sac formed from the peritoneum that contains a portion of the intestine or omentum. The hernia pushes downward at an angle into the inguinal canal. In males, indirect inguinal hernias can become large and often descend into the scrotum. Direct Inguinal Hernias, in contrast, pass through a weak point in the abdominal wall. Femoral Hernias protrudes through the femoral ring. A plug of fat in the femoral canal enlarges and eventually pulls the peritoneum and often of the urinary bladder into the sac. Umbilical Hernias are congenital or acquired. Congenital umbilical hernias appear in infancy. Acquired umbilical hernias directly result from increased intraabdominal pressure. They are most commonly seen in people who are obese. Incisional, or Ventral Hernias occur at the site of a previous surgical incision. These hernias result from inadequate healing of the incision, which is usually caused by post-operative wound infections, inadequate NUTRITION, and obesity. Chapter 56: Care of Patients with Noninflammatory Intestinal Disorders, pp. 1121-1126 Intestinal Obstruction Intestinal obstruction is a partial or complete blockage of the bowel that results in the failure of the intestinal contents to pass through. With obstruction, gas and fluid accumulate proximal to and within obstructed segment causing bowel distention. A bowel obstruction is divided into two basic categories: mechanical and non-mechanical. Treatment of intestinal obstruction is directed toward relieving symptoms, managing fluid and electrolyte imbalances, preventing complications, and treating the cause of the obstruction. Surgery may be needed to relieve the obstruction if gastric decompression does not relieve the symptoms, or if there are signs of bowel necrosis. The type of surgery will depend on the type and area of obstruction and may include intestinal resection with an anastomosis or creation of an ileostomy or colostomy. SMALL BOWEL: If the small bowel obstruction is complete, the peristaltic waves become quite vigorous, assuming reverse direction, propelling intestinal contents toward the mouth rather than the rectum. The patient vomits stomach contents first, then the bilious contents of the duodenum, and finally the fecal contents of the ileum. A distended abdomen, a bloated sensation, and altered bowel sounds may indicate a small bowel obstruction. Patients with Ileostomy who develops distention and cramping should apply warm, moist towels to abdomen or lightly massage abdomen. LARGE BOWEL: Constipation may be the only symptom for several days. Barium enema may be ordered to reveal a distended, air-filled colon. Monitor the patient for bowel movement after a barium enema. Patients with large bowel obstructions may experience intermittent persistent lower abdominal cramping. Severe pain may result from strangulation or bowel perforation. Chapter 57, Care of Patients with Inflammatory Intestinal Disorders, pp. 1117-1119 Dumping Syndrome (postop) (No treatment, patient waits it out). Rapid emptying of gastric contents into the small intestines. This results in a fluid shift into the gut causing abdominal distention. Observe for early manifestation of this syndrome, which typically occur within 30 minutes of eating. [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 14, 2021
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Nov 14, 2021
Downloads
0
Views
87

 - Latest 2022.png)
 - A Graded, Quality Work.png)
_Score 2831 Art history 1 Challenge Milestone 1 unit 1 Sophia Course (solution).png)