*NURSING > STUDY GUIDE > Rasmussen College: PN3-Exam-3-Study-Guide-1_LATEST ,100% CORRECT (All)
Rasmussen College: PN3-Exam-3-Study-Guide-1_LATEST ,100% CORRECT
Document Content and Description Below
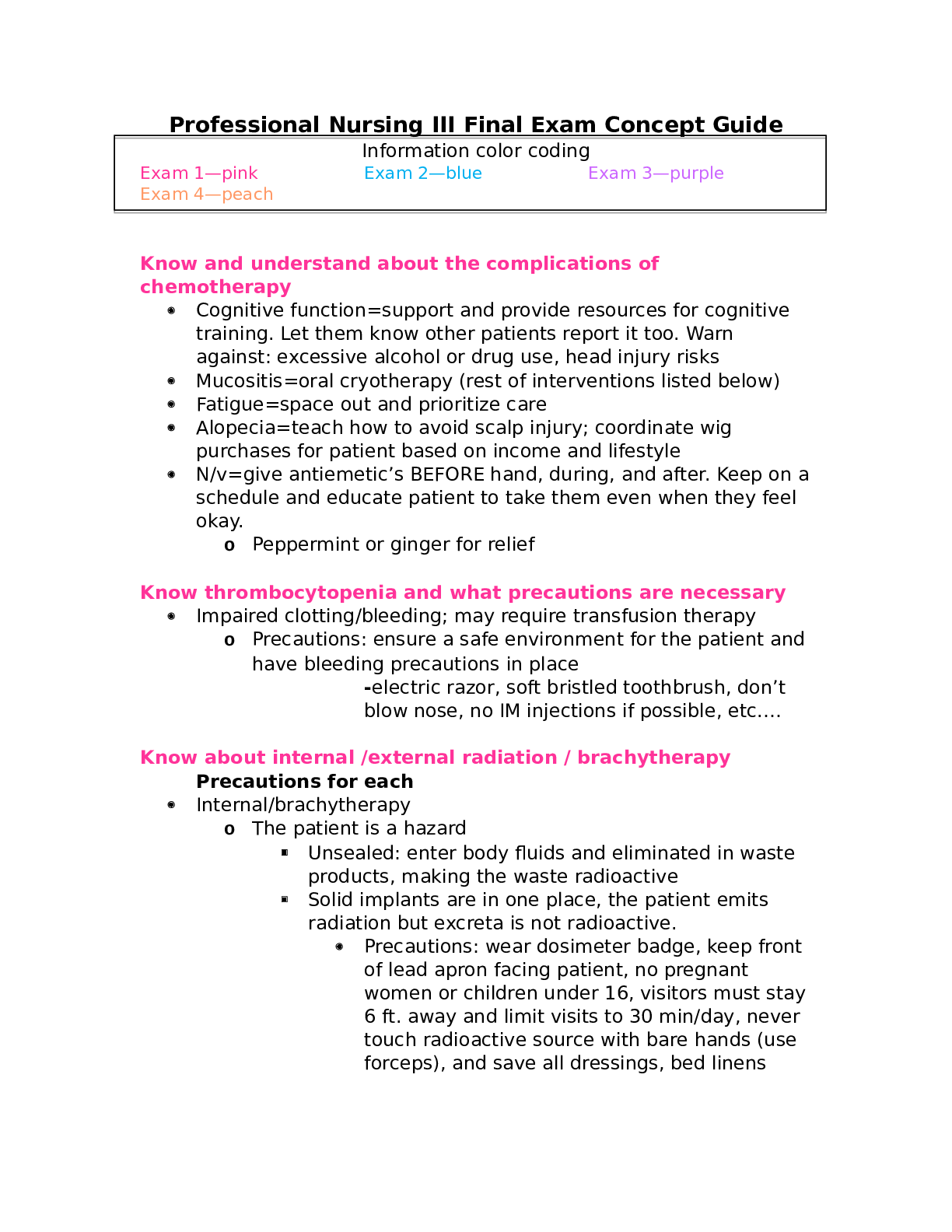
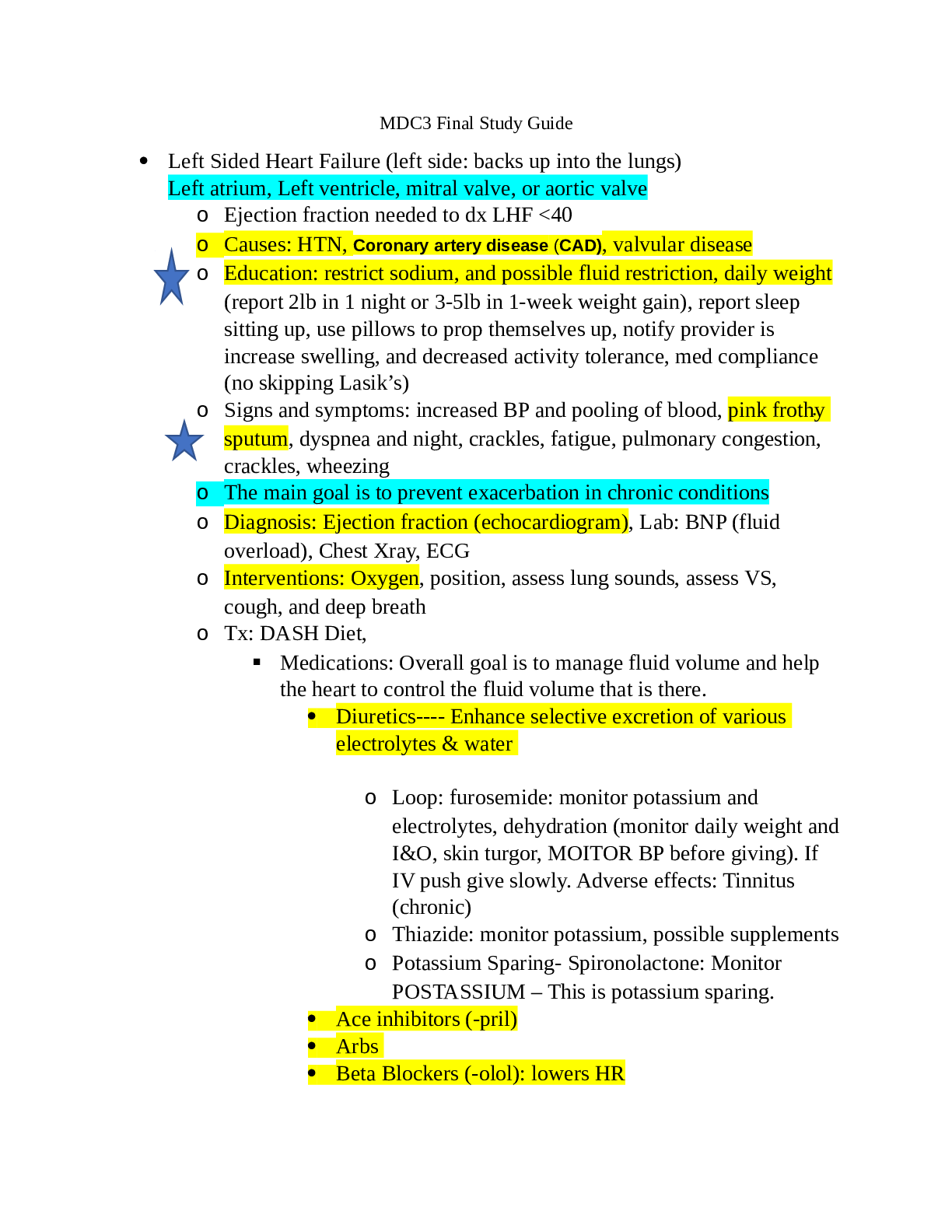
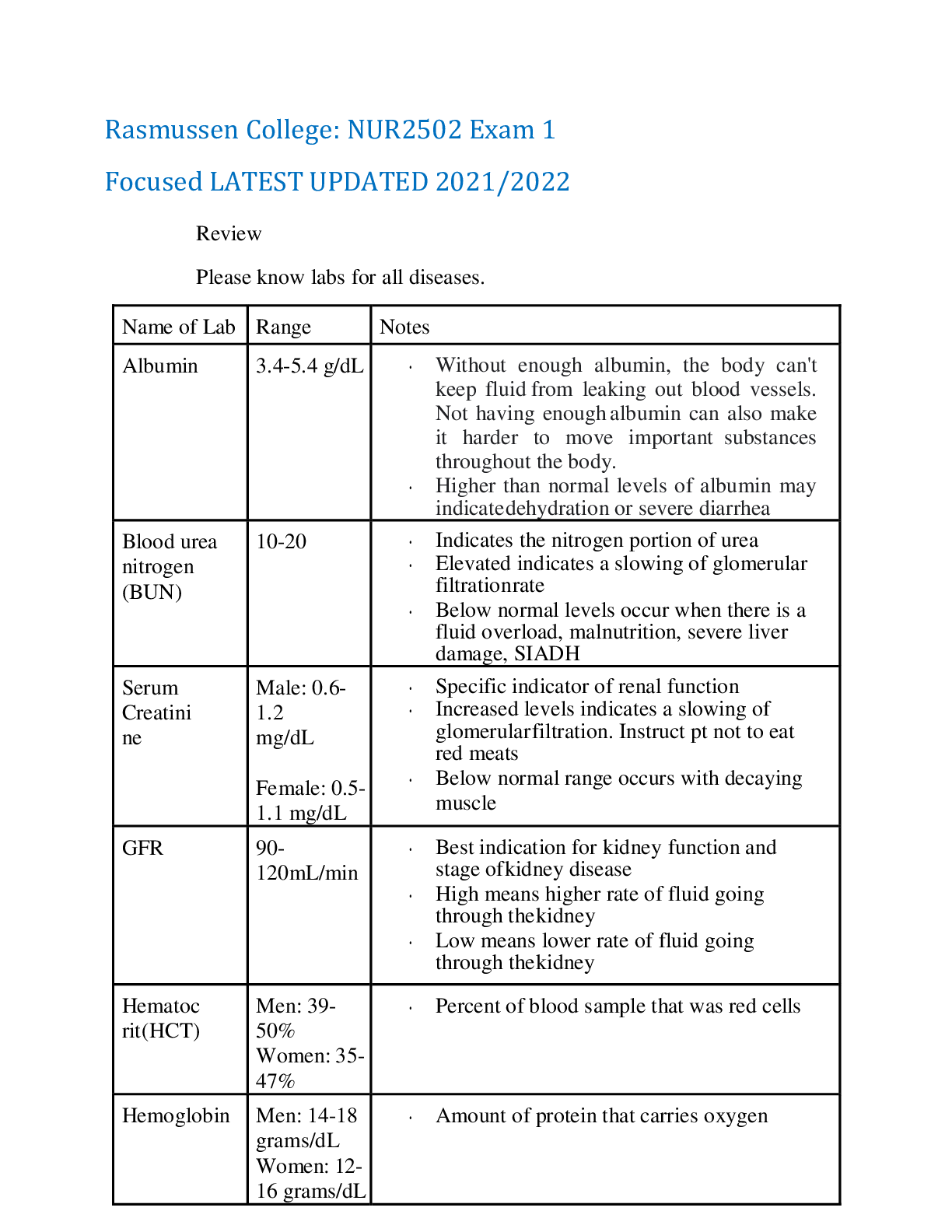
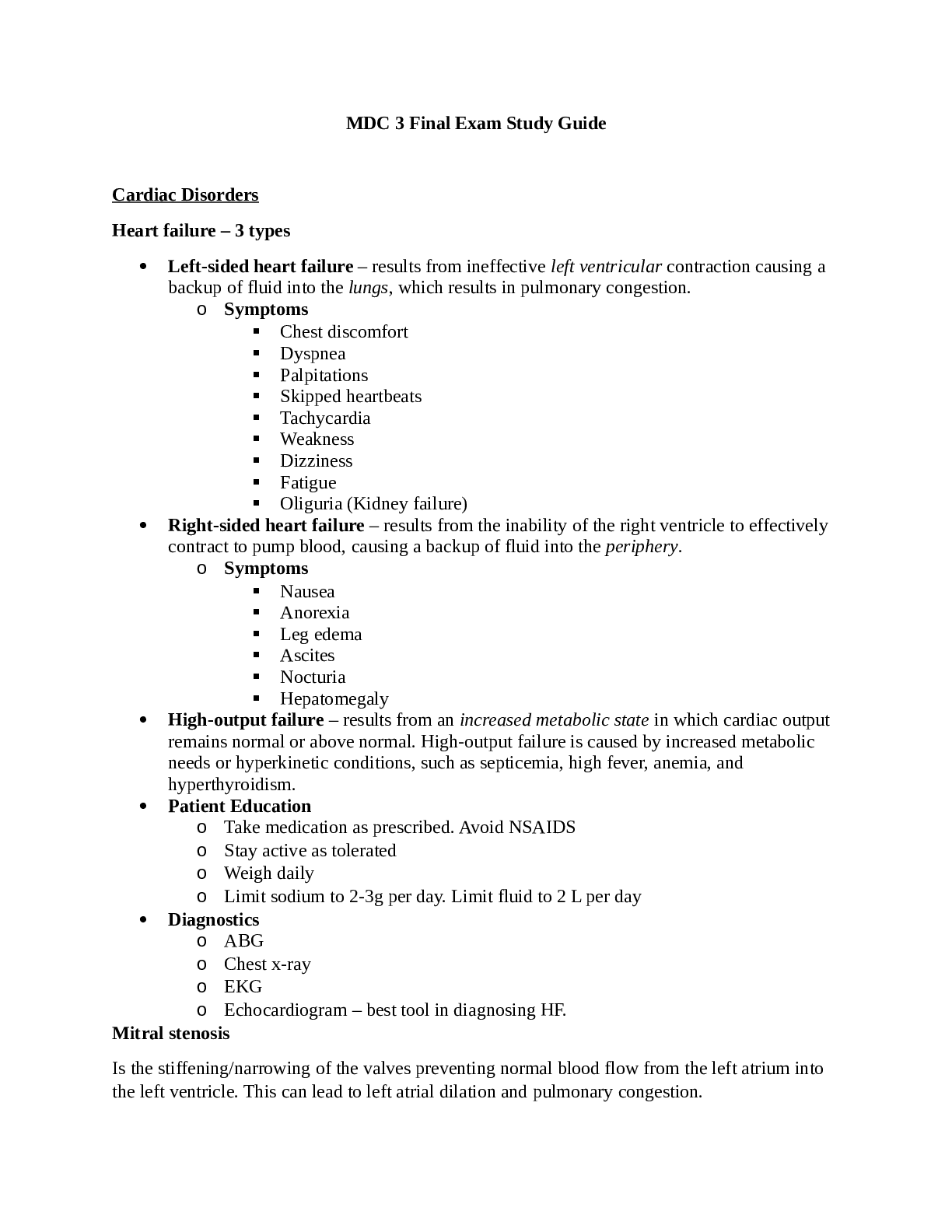
Rasmussen College: PN3-Exam-3-Study-Guide-1_LATEST Multisystem Failures Acute IIR cardinal signs Rubor = redness (due to vasodilation) Tumor = swelling (due to release of fluid containing RBC and... protein) Callor = heat (due to increase blood flow) Dollor = pain (swelling cause pain and pressure of the nerve endings) Types of all shock and complications Hypovolemic, cardiogenic anaphylactic, neurogenic, septic Hypovolemic Lack of circulating blood volume Blood loss, dehydration, burn, vasodilation due to neurogenic shock or anaphylactic shock, N/V diarrhea, NG suction. Drop of blood pressure Interventions: replace fluid! Monitor fluid replacement, monitor vital signs, assess S/S of fluid overload, WBC Hemoglobin and hematocrit., positioning for comfort. Cardiogenic Weakened forward pumping function of the heart, right, left, ventricles or both. MI, decreased cardiac output, irregular rate or rhythm Example if left ventricle is affected you will see pulmonary edema, adventives lung sounds HR > 100 bpm, weak or thready pulse, diminished heart sounds, dysrhythmia, cool moist pale skin, chest pain Renal failure, watch output > 30 ml a hour, 400 ml a day (less than that is oliguria, anuria is absent of urine) Generized edema, legs, arms face, watch weight (2 # in 24 hours or 5# a week sign of additional cardiac and/or kidney failure) Treatment: oxygen, mechanical intubation, diuretics, inotropic drugs (to stimulate the contractibility of the heart such as dopamine, dobutamine, inamrinone), ECG, morphine (improve coronary perfusion) Anaphylactic Occurs when an allergen such as food (shellfish, peanuts, chocolate strawberries and tomatoes)food additive, iodine, latex, mold fungus cats or medications (penicillin) insects (bees) venom, enter the body causing release of histamines (widespread antibody response), which results in capillaries dilation, and smooth muscle contracting. Life threatening situation. Difficult to diagnose, symptoms look like PE Comprehensive health history is important to prevent anaphylactic shock. Remember the different of sensitivity (rash) or allergy. History of an allergy can make second time worse. Prevent latex Washing hand with soap and water, avoid oil- based cream, prevent dust damp rag. Make sure they have an epipen, or administer epinephrine S/S Edema tongue airway, SOB, stridor, hypotension, anxiety. Neurogenic shock Absence or suppression of the sympathetic nervous system tone and is considered in the hypovolemic shock class. Caused by disruption of brain or hypothalamus, spinal cord injury at or above T6. Massive peripheral vasodilation, loss of temp regulation, loss of sympathetic tone in the heart, diminished baroreceptive responses to change blood pressure Paralysis, warm dry skin, (You do not see decreased reflexes with neurogenic shock). Treatment: reestablish blood volume, replace fluid! Monitoring fluid overload, medication inotropic and vasoconstriction meds (dopamine), low dose of corticosteroids, atropine if bradycardia, ECG, Glasgow coma scale, monitor MODS. Interventions prevent hypovolemic shock correct hypovolemia, promote normal temp, prevent hypoxemia, monitor ECG (dysrhytmias), identify patient at risk for neurogenic shock, patient with DVT. ( stress is related to increased sympathetic nervous system arousal and involves a wide physiological response) Septic shock Circulation and coagulation is altered severe sepsis is associated with one or more organ dysfunction. S/S Hypotension, blood pressure has a widened pulse, tachycardia, high temp, lactic acidosis, oliguria, mental status changes, cellular and humoral responses. Aches and chills, decreased skin perfusion It mimic SIRS, sign of at least one organ failure Diagnosis, WBC, identify the source, history Causes bowel surgery, severe malnutrition, multiple antibiotic therapy, multiple immune suppressant therapy (patient on chemo, radiation), prolonged hospitalization, nosocomial infection.!! Gram negative bacteria is a major cause of septic shock!! Treatment: antibiotic specific for the type, and fluid resuscitation. Main cause of shock Gram negative bacteria is a major cause of septic shock hypovolemia Interventions with Disseminated IV coagulations Excessive clotting and hemorrhage. Hypoxia, acidosis and shock occur. Interventions: clots and bleeding precautions. handle the patient very gently, changing positions very delicate. Avoid sharp objects, no IM injections, no razors Patient can have constipation, avoid straining ARDS management and treatment Treating underlying cause, promote gas exchange, oxygen, prevent further complications. Patient are intubated and on mechanical ventilation (to help prevent further damage of the lung) (book) bedrest, Stages of shock syndrome MODs assessment of patient- use what for assessing? Primary multiple organ dysfunction Major trauma to the chest, severe aspiration, inhaled fumes TOXIC shock can lead to SEPTIC shock caused by staphylococcus aurus Flu like symptoms, high fever, N/V, diarrhea, hyperactive bowels, abdominal pain, muscle and joint aches STRAWBERRY TONGUE, reddish rash, peeling of the skin in 7 to 10 days. This can cause necrotic vecitis severe infection of the muscle in the extremities of trunk -> gangrene is happening,-> amputation -> very high mortality rate. MODS Assess renal function, urine < 30 ml per hour or 400 ml per day Failure to control infection Persistent hypo perfusion Presence of necrotic tissue / abscess Altered oxygenation Coronary Artery Dysfunction ➢ Cardiac Angiogram o Done via heart catheterization. It is an invasive procedure. It is the gold standard for diagnosing CAD o It directly visualizes the coronary artery anatomy. It assesses ventricular function and hemodynamic function. ➢ Cardiac Rehabilitation Phases Cardiac Rehab Phases Description Phase I In the hospital after an MI. The nurse should get to know the patient. The nurse determines the ability of the patient to exercise and care for themselves. Phase II Transitional phase from the hospital to home. It focuses on increasing activity. Low intensity exercise program. Phase III Supervised variety of exercises with recording and assessments on the patient to see how well they tolerate activity. Phase IV Maintenance phase. Emphasizes the long-term life change. Exercise (no sedentary lifestyle). Diet. ➢ CAD o Risk Factors: Modifiable vs. Non-Modifiable ▪ Modifiable: Smoking, hyperlipidemia, hypertension (long term or chronic over 140/90), diabetes, obesity, diet, inactivity, stress, and alcohol ▪ Non-Modifiable: Age, gender, family history, and ethnic background o Diagnostic Test Teachings ▪ Electrocardiogram • 12-lead electrical recording of the heart used to determine areas of ischemia or infarction ▪ Holter Monitor • Ambulatory ECG that monitors the patient to see if ischemia is present. Goes directly to the telemonitor nurse. Like a pager looking device. Relates the ischemic episode to what the patient is doing ▪ Chest X-ray • Not diagnostic worthy, but can reveal clues of CAD ▪ ECG Stress Test • Exercise induced stress test. It evaluates effectiveness of therapies. Shows how exercise is affecting the cardiac system ▪ Labs • Creatine Kinase: looks overall if there is muscle damage in the body. It is a marker but is nondistinctive. • Troponin: a myocardial protein that is only released in circulation when there is a myocardial injury. It will rise quickly and remain elevated for 2 weeks. ▪ STEMI • More extensive damage, occurs very quickly, usually correlated with prolonged and complete blockage ▪ NSTEMI • Incomplete blockage o Medications for Treatment (All work by decreasing the workload of the heart and increasing myocardial perfusion) ▪ Nitrates • Nitroglycerin o PRN o Watch for hypotension (stand slowly) o Common/expected side effects: tingling sensations and headache o Avoid use of Viagra or Cialis because it vasodilates as well so the combination of both could cause death to occur ▪ Beta Blockers • Atenolol & Metoprolol o Decrease afterload and increase diastolic time to increase coronary perfusion o Monitor for bradycardia, hypotension, SOB, and wheezing ▪ It can also constrict the bronchioles o Do not give to someone with asthma ▪ Calcium Channel Blockers • Verapamil, Diltiazem, & Amlodipine o Dilate coronary arteries, prevents vasospasms, and decreases preload and afterload o Monitor for edema, hypotension, bradycardia o Start prevention attempts for constipation (laxatives) ▪ Antiplatelet Therapy • Aspirin o Inhibits blood clots, decreases pain, and decreases the risk of death in elderly patients. o Take with food o Common dose: baby aspirin (81 mg/day) ➢ HDL vs. LDL Differences and Levels o LDL (bad cholesterol): main component of atherosclerotic plaque buildup. LDL transports cholesterol to the liver and other organs. o HDL (good cholesterol): Transports plasma cholesterol away from the plaque to be excreted. If HDL goes up the tendency for CAD decreases. Classification Total Cholesterol (mg/dl) LDL (mg/dl) HDL (mg/dl) Triglyceride (mg/dl) Optimal Less than or Less than or Greater than or Less than or equal to 200 equal to 100 (less than or equal to 70 in patients with CAD or equivalent) equal to 60 (counts as a negative risk factor) equal to 150 Near Optimal 100-129 Borderline High 201-239 130-159 151-199 High Greater than or equal to 240 160-189 Less than or equal to 40 200-499 Very High Greater than or equal to 190 Greater than or equal to 500 ➢ BP Numbers and Stages BP Classification SBP mm Hg DBP mm Hg Normal Less than or equal to 120 Or less than or equal to 80 Prehypertension 120-139 Or 80-90 Stage I Hypertension 140-159 Or 90-99 Stage II Hypertension Great than or equal to 160 Or greater than or equal to 100 ➢ Discharge Home Teachings Post MI o After an MI and stable angina is present, the patient needs to understand cardiac condition. Teach the patient how to manage chest pain with nitro and alleviating factors. Explain that the patient must decrease activity when experiencing chest pain. Explain medications and how and when to take them. Teach risk factors. o The goal of treatment is to improve quality of life by decreasing episodes of angina and ischemia and to increase the quantity of life by preventing or altering CAD. o Teach complications that may occur after an MI ▪ Arrhythmias: occur in 80% of acute MI patients ▪ CHF: occurs with slight dyspnea, restlessness, agitation, and little increase in heart rate (subtle signs) ▪ Cardiogenic shock ▪ Sudden cardiac death o Teach symptoms: chest pain, pain that radiates to left arm or other arm, pain that radiates to neck, jaw, or scapulae. Cool clammy and pale skin, altered LOC, syncope (fainting), vertigo, dyspnea, SOB, crackles, tachypnea, tachycardia, bradycardia, alternating weak and strong heartbeats, arrhythmias, presence of s3 or s4, hypo or hypertension, development of a murmur, decreased urine output ➢ Nitroglycerin Use and Education ➢ Stable vs. Unstable Angina o Management ▪ Stable • Occurs due to a stable fixed obstructive type of plaque with a thick fibrous cap in one or more coronary arteries. Ischemia episodes will start to precipitate from reduced oxygen supply. Can occur from exercise or anemia. Occurs predictably with the same onset, duration, and frequency and is going to be relieved when the precipitating factor is removed or with nitroglycerin administration. Described as a steady discomfort that lasts for minutes. Relieved with rest. ▪ Unstable • Increase in frequency, duration, and symptoms with lower levels of activity and at rest. It is a precursor for MI. It is classified as acute coronary syndrome. It is a direct occurrence of a rupture of plaque. Management of chest pain: morphine, oxygen, nitroglycerin, aspirin, and heparin (MONAH). Stop activity. o PCI (Percutaneous intervention): used for emergent treatment of acute coronary syndrome. Minimal discomfort and short hospital stay, short recovery, fast return to work. Stent that opens up coronary artery. o NSTEMI: partial blockage o STEMI: ST segment elevation: complete blockage o Goal of Treatment ▪ Decrease in ischemia and episodes of angina o Angina vs. Musculoskeletal ▪ Angina Pain • Pain in the chest that is described as steady discomfort and lasts for minutes (normally not longer than 5-10 minutes). Is relieved with rest or nitroglycerin. ▪ Musculoskeletal Pain • The patient will know exactly where it hurts. There is increased pain with palpitation. The quality of pain varies with changes in position. Pain is relieved with an NSAID. Endocrine Dysfunction Renal Dysfunction Acromegaly (gigantism) clinical manifestations • Overproduction of GH (growth hormone) in children results in acromegaly • Condition involves multiple tumors on pituitary gland; these tumors measure over 1cm • In adults, hey keep growing after growth platelets fuse, due to the excess presence of GH • Hyperglycemia may be present due to a decrease in glucose uptake by peripheral tissues, and an increase release of glucose by the liver • The onset may be gradual with slow progression, and changes may remain unnoticed for years before diagnosis of the disorder. • Early detection and treatment are essential to prevent irreversible enlargement of the face, hands, and feet. • Note: Will see notable vision changes, increase size of tongue due to increase GH • Other changes include increased skeletal thickness, hypertrophy of the skin, and enlargement of many organs such as the liver and heart. • Some changes may be reversible after treatment, but skeletal changes are permanent. • Bone thinning and bone cell overgrowth occur slowly. Breakdown of joint cartilage and hypertrophy of ligaments, vocal cords, and Eustachian tubes are common. • Nerve entrapment and hyperglycemia (elevated blood glucose levels) are common. • Normal GH levels in men is less than 5 mg/ml, and less than 10 mg/ml in women. • Drug being used post-surgery if there is residual hypersecretion of GH is Octreotide, given sub q, three times a day Cushing’s syndrome clinical manifestations and intervention focuses/teachings * Cushing's syndrome is caused from chronic use of exogenous corticosteroids is more common because these drugs are often used to control serious chronic inflammatory conditions. Seen more in women between ages of 20-40 years old. Clinical Manifestations Typical symptoms include: easy bruising, poor wound healing, excessive growth of hair or nails, voice changes, hypertension, amenorrhea, decreased libido. General Appearance • Moon face • Buffalo hump • Truncal obesity • Weight gain • Increases in the breakdown of tissue protein result in decreased muscle mass and muscle strength, thin skin, and fragile capillaries. The effects on minerals lead to bone density loss. Intervention focuses/teachings • The patient with hypercortisolism is expected to achieve and maintain a normal or near-normal FLUID AND ELECTROLYTE BALANCE. Indicators include that these parameters are within or close to the normal range: o Blood pressure o Stable body weight o Serum electrolytes, especially sodium and potassium • Medication use may include diuretics, antihypertensive or cardiotonic drug therapy. • Monitor for indicators of fluid overload; general cardiac monitoring • These patients need to remain infection free due to compromised immune system; more susceptible to bacterial and nosocomial infections. Safety precautions need to be taken. Patient should try to remain at home and away from infected patients. • Monitor intake and output and weight to assess therapy effectiveness. o Weigh the patient at the same time daily (before breakfast) • Monitor Blood sugar • Encourage patient to wear a medical alert bracelet • Assess the skin for reddened areas, excoriation, breakdown, and edema. If mobility is decreased, turn the patient every 2 hours and pad bony prominences. • Coordinate with a dietitian to teach the patient about nutrition therapy. A high-calorie diet that includes increased amounts of calcium and vitamin D is needed. • Antacids buffer stomach acids and protect the GI mucosa. Teach the patient that these drugs should be taken on a regular schedule rather than on an as-needed basis. • Instruct the patient to reduce alcohol or caffeine consumption, smoking, and fasting because these actions cause gastric irritation. NSAIDs and drugs that contain aspirin or other salicylates can cause gastritis and intensify GI bleeding. These should be avoided or limited. • Glucocorticoids reduce both the inflammation and the immune responses of IMMUNITY, increasing the risk for infection. For the patient who is taking glucocorticoid replacement therapy, the risk is ongoing. o All personnel must use extreme care during all nursing procedures. Thorough handwashing is important. Anyone with an upper respiratory tract infection who enters the patient's room must wear a mask. Observe strict aseptic technique when performing dressing changes or any invasive procedure. o Monitor the patient's daily complete blood count (CBC) with differential WBC count, especially neutrophils. Inspect the mouth during every shift for lesions and mucosa breakdown. Assess the lungs every 8 hours for crackles, wheezes, or reduced breath sounds. Assess all urine for odor and cloudiness. Ask about any urgency, burning, or pain on urination. o Take vital signs at least every 4 hours to assess for fever. A temperature elevation of even 1° F (or 0.5° C) above baseline is significant for a patient who has reduced IMMUNITY and indicates infection until it has been proven otherwise. • Teach him or her and the family to monitor the patient's weight. Suggest that a record of these daily weights be kept to show the primary health care provider at any checkups. Also instruct the patient to call the health care provider if more than 3 lb are gained in a week or more than 1 to 2 lb are gained in a 24-hour period. • Osteoporosis is a concern for these patients as well. Diabetes insipidus clinical manifestations • Greatly increased urine output • Low urine specific gravity (<1.005) • Hypotension • Dehydration • Increased plasma osmolarity • Increased thirst • Output does not decrease when fluid intake decreases Grave’s disease interventions * is an autoimmune disorder resulting from Hashimoto's thyroiditis (HT) • Visual changes may be the earliest problem the patient or family notices, especially exophthalmos with Graves' disease. Ask about changes in vision, such as blurring or double vision and tiring of the eyes • Two other eye problems are common in all types of hyperthyroidism: eyelid retraction (eyelid lag) and globe (eyeball) lag. In eyelid lag, the upper eyelid fails to descend when the patient gazes slowly downward. In globe lag, the upper eyelid pulls back faster than the eyeball when the patient gazes upward. During assessment, ask the patient to look down and then up and document the response. • These patients will need small, frequent meals in order to keep up with energy demands • The most common interventions are drug therapy and radio-ablation. • Monitoring includes measuring the patient's apical pulse, blood pressure, and temperature at least every 4 hours. Instruct the patient to report immediately any palpitations, dyspnea, vertigo, or chest pain. Increases in temperature may indicate a rapid worsening of the patient's condition and the onset of thyroid storm, a life-threatening event that occurs with uncontrolled hyperthyroidism and is characterized by high fever and severe hypertension • Surgery to remove all or part of the thyroid gland is used for Graves' disease that does not respond to other therapies. • Eye and vision problems of Graves' disease are not corrected by treatment for hyperthyroidism, and management is symptomatic. Teach the patient with mild problems to elevate the head of the bed at night and use artificial tears. Myxedema vs thyroid crisis Myxedema • Dry, waxy swelling of the skin that is accompanied by non-pitting edema (especially around the eyes, in the hands and feet, and between the shoulder blades) and is associated with primary hypothyroidism. Thyroid crisis • A life-threatening event that occurs in patients with uncontrolled hyperthyroidism and is usually caused by Graves' disease. Likely to occur in patients that haven’t been diagnosed or those who are not treated for hyperthyroidism properly. Those who had a recent infection or those who are pregnant may experience this. Key manifestations include high fever, diaphoresis tachycardia, and systolic hypertension. Renal Dysfunction Pyelonephritis etiology, interventions, and risk factors- Is an infection of the upper urinary tract. If untreated it can lead to renal failure. -S/s are urinating bacteria, FLANK PAIN at the costovertebral angle, fever chills, painful urination, frequency, nocturia, nausea, vomiting, and colicky abdominal pain. -Causes are urinary retention from medications, BPH, bed ridden, surgery, anesthesia, too much sodium in diet, spinal cord injury- neurogenic bladder, dementia- loses ability to use muscle, mass, urinary calculi and sloughed papillae. Interventions: Diagnostic testing includes a urine sample- remember to catch mid-stream. Catheter may need to be used in order to get urine sample. The primary goal is to get rid of the UTI and prevent damage to the renal system- do not want any scarring. Secondary is to prevent further infections and find out why UTI occurred. Education= cranberry juice, wipe front to back, urinating before and after intercourse, staying hydrated, do not use soaps in the area, compliance with antibiotics, do not hold urine in and avoid taking baths. Other interventions include vitals and fluid balance, weight, ensure adequate hydration- at least 2 mL per day! Maintain IV access, monitor electrolytes, WBC, BUN, and creatinine. Remember that creatinine looks only at the kidney and BUN looks at both the kidney and the muscle. PYRIDIUM and URICEPT are given. Remember to control pain. Rhabdomyolysis This with what can create an emergent situation and why This with COMPARTMENT SYNDROME=Red flag. Compartment syndrome occurs when a patient has a fracture and needs a cast. Edema occurs underneath the cast and cuts off circulation. The cast will need to be taken off and a fasciotomy will be done to relieve all of the pressure. Compartment syndrome can develop with extensive muscle damage and with this injury causes acute swelling of the muscular compartment which becomes rigid. Those come together and form a compartment in the muscle. When swelling and increased pressure occur, this can cause necrosis, reduced circulation, and nerve damage. Compartment syndrome can occur immediately or be delayed up to 3 days. Monitor patients who have injuries, casts, or wounds. Surgery is needed before any permanent damage occurs. Acute Renal Failure Causative factors of and teachings for: Prerenal, Intrarenal, and Postrenal failure S/S- rapid decline within a few hours to days. Oliguria and elevated BUN and creatinine. Prerenal: Most common. Caused by decreased blood flow to the kidneys- dehydration, vascular expansion, sepsis or cardiac failure. Intrarenal: inside of kidneys. Causes are clotting, tubular necrosis and toxins from nephrotoxic medications. NSAIDs can cause this. Postrenal: caused from obstruction from enlarged prostate or renal calculi. -Remember that renal failure can’t get rid of hyperkalemia. NEED CARDIAC MONITORING. T wave will be peaked and PR and QRS intervals will be wider. Need to give KAYEXALETE- will bind to the potassium in the gut and leave through the GI system. -Hypokalemia can still occur. Causes cardiac arrest. Worried when potassium is less than 2.5. Need to watch digoxin- Causes toxicity. -Goals are to maintain proper BP and monitor cardiac and respiratory. Dopamine is immediate precursor to norepinephrine- small doses are given to increase renal perfusion. Want to prevent azotemia- the flapping of hands- need to make sure toxins have not reached the brain. Maintain mineral and electrolyte imbalance. Avoid foods that are high in potassium- fresh fruits and veggies, citrus, tomatoes and potatoes. Potassium is 2 g per day. Diagnostic tests of concern Respiratory acidosis will promote potassium movement in the cells. The kidneys filter out 80% of potassium every day. In renal failure, the kidneys are not filtering out potassium. Hyperkalemia: When a patient has hyperkalemia, they need cardiac monitoring. Hyperkalemia can be seen through a dysrhythmia on an ECG. This will be shown as a high peaked T-wave or a prolonged PR and QRS interval (wider) leading to cardiac arrest. (Kayexalate will be given to bind to the potassium in the gut and pull it out of the GI system). Patient will have loose bowel movements upon administration. Hypokalemia: Can cause cardiac arrest. It the potassium level is less than 2.5 this is an emergent situation. (Potassium stimulates heart contraction and if it is not stimulated, we worry about cardiac arrest). Also worried about digoxin- strengthens contraction of the myocardium. This will enhance digoxin and cause digoxin toxicity. Hypovolemic: Not enough fluid, kidneys will begin to shut down and can cause cardiac issues. Types of surgeries Angioplasty or renal artery bypass surgery: Performed for renal artery stenosis or renal vein thrombosis. This is the same thing as a bypass surgery of the heart, just at the kidneys instead. Ureteral stent: placed for obstruction. Nephrostomy tubes: treatment of choice in people who have obstructed conditions with hyperkalemia or who are prone to sepsis. The tube will be like a catheter. Medication treatment with education Chronic Renal Failure Hemodialysis vs peritoneal Hemodialysis: Fluid is removed by osmatic gradient. The solution used is dialysate dextrose concentration. This provides higher osmotic pressure. Capillary pore size will allow protein loss but it is not a large amount. Phosphate binding is required inside along with dextrose mechanisms (in the solution). The fresh dialysate solution (shown in picture) fills up the peritoneal cavity in the stomach. Let it dwell for a certain time frame and volume (prescribed by a provider) and after that time and fluid is done, it drains and discards the effluent (waste materials). Advantages: it’s portable, higher level of self-independence, lower cost, and continuously lowers levels of waste products in the blood. There are only moderate dietary fluid and diet restrictions. Disadvantage: includes protein loss and potential life threatening infection. Nutrition teaching Prevent malnutrition and prevent complications of electrolyte imbalances (high potassium and high phosphorus) Low-protein diet: protein sources are broken down and converted into urea. This needs to be filtered by the kidneys and the kidneys don’t have the ability to excrete this, so you will have urea floating around in the blood. Hemodialysis: amino acid loss, you may have an increase in catabolism (wasting of the muscles). Hemodialysis fluid intake: 1,000mL day to replace urine output Peritoneal: May not have a fluid restriction Goal is to limit weight drain between dialysis treatments. Goal is to limit weight gain to 2-5% of the established dry weight. There is a formula that physicians figure out to determine what weight they should be at. Potassium restricting foods Teach not to eat fresh fruits and veggies, citrus, potatoes and tomatoes. Potassium should be 2 g per day. Expected appearances Cardiac: hypertension and fluid volume overload (swelling, edema) Endocrine: anemic Skeletal: renal bone disease (high levels of phosphorus) GI: occult blood loss (bleeding through stool), anorexia, nausea, vomiting, and constipation Hematological: electrolytes altering (hyperkalemia, hypermagnesemia, hypocalcemia) Neuro: myoclonus (mild twitching contractions that are uncontrolled) - restless leg syndrome Psych: depression and anxiety Teaching for autosomal dominant polycystic kidney disease Be aware of positive findings of the gene because it may compromise employment opportunities related to prohibited life or health insurance (considered a pre-existing condition) Promote ways to avoid a UTI: take showers, void after intercourse, good perineal hygiene, void frequently Minimize the opportunity for a UTI to be created to eliminate more issues with the kidneys (acquiring an infection could cause renal failure to kick in) Other teachings: low sodium diet, weight control, exercising regularly, and proper fluid intake (Dietary referrals or PT referrals may be necessary) AV shunt assessment Need to assess for both- listen for bruit and palpate for thrill. Pheochromocytoma clinical manifestations- is a rare noncancerous tumor that develops in the adrenal glands. Symptoms are high blood pressure, sweeting, tachycardia, tremors and paleness in the face, dyspnea. [Show More]
Last updated: 1 year ago
Preview 1 out of 29 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 04, 2022
Number of pages
29
Written in
Additional information
This document has been written for:
Uploaded
Feb 04, 2022
Downloads
0
Views
30